User login
How to talk to patients and their family after a diagnosis of mild cognitive impairment
Mild cognitive impairment (MCI) is a transitional clinical stage between normal aging and dementia. Together with aging, it is considered the most significant risk factor for developing dementia, often the Alzheimer’s type.1
MCI is a challenging neuropsychiatric diagnosis to discuss with patients and their family because it is characterized by overlapping features of normal aging and because of its heterogeneity of etiology, clinical presentation, and outcome.2,3 The evolution to dementia and the lack of effective treatments for preventing or forestalling this outcome can be difficult to address—particularly when the patient is in good health and has been leading a productive life.
Successful communication is key
You can take steps to communicate in a helpful way, build a strong treatment alliance, and reduce the potential for the iatrogenic effects of disclosing this diagnosis and its prognostic implications.
Clarify that your findings are consistent with the patient’s or family’s report of sustained and concerning change in cognition and, depending on the patient, concurrent alterations in affect, behavior, or both. Emphasize that these changes are disproportionately severe relative to expectations for the patient’s age and are not caused by psychiatric or clear-cut medical factors.
Highlight contexts in which the patient’s symptoms are likely to become more disruptive and impaired, and situations in which the patient can be expected to function more effectively.
Provide evidence-based support for the rate of progression of symptoms and functional impairment.3
Emphasize that major lifestyle adjustments usually are unnecessary in the absence of progression, especially for patients who are retired or not involved in endeavors that involve significant cognitive and executive functioning demands.
Discuss the role that cognition-enhancing medications might play in managing symptoms.4
Address indications for additional services, including formal psychiatric care for patients who have concomitant affective or behavioral symptoms and who are highly distressed by the diagnosis. Pair these services with longitudinal monitoring for possible exacerbation of symptoms.
Identify psychiatric, medical, and lifestyle factors that can increase the risk of dementia. Depending on the patient’s history, this might include diabetes, hypertension, elevated lipid levels, obesity, smoking, head trauma, depression, physical inactivity, and lack of intellectual stimulation.
Review compensatory strategies. In MCI predominantly amnestic type, for example, having the patient make systematic lists for shopping and other activities of daily living, as well as establishing routines for organizaton, can bolster successful coping.
If psychometric testing was not utilized to establish the diagnosis, discussion can include the value of performing such an assessment for a more finely tuned profile of preserved and impaired neurobehavioral functions. Such a profile can include test patterns that 1) have prognostic value with regard to the likelihood of progression to dementia and 2) establish a baseline against which you can assess stability or progression over time.5
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270-279.
2. Ellison JM, Harper DG, Berlow Y, et al. Beyond the “C” in MCI: noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spectr. 2008;13(1):66-72.
3. Goveas JS, Dixon-Holbrook M, Kerwin D, et al. Mild cognitive impairment: how can you be sure? Current Psychiatry. 2008;7(4):36-40, 46-50.
4. Doody RS, Ferris SH, Salloway S, et al. Donepezil treatment of patients with MCI: a 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555-1561.
5. Summers MJ, Saunders NL. Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology. 2012;26(4):498-508.
Mild cognitive impairment (MCI) is a transitional clinical stage between normal aging and dementia. Together with aging, it is considered the most significant risk factor for developing dementia, often the Alzheimer’s type.1
MCI is a challenging neuropsychiatric diagnosis to discuss with patients and their family because it is characterized by overlapping features of normal aging and because of its heterogeneity of etiology, clinical presentation, and outcome.2,3 The evolution to dementia and the lack of effective treatments for preventing or forestalling this outcome can be difficult to address—particularly when the patient is in good health and has been leading a productive life.
Successful communication is key
You can take steps to communicate in a helpful way, build a strong treatment alliance, and reduce the potential for the iatrogenic effects of disclosing this diagnosis and its prognostic implications.
Clarify that your findings are consistent with the patient’s or family’s report of sustained and concerning change in cognition and, depending on the patient, concurrent alterations in affect, behavior, or both. Emphasize that these changes are disproportionately severe relative to expectations for the patient’s age and are not caused by psychiatric or clear-cut medical factors.
Highlight contexts in which the patient’s symptoms are likely to become more disruptive and impaired, and situations in which the patient can be expected to function more effectively.
Provide evidence-based support for the rate of progression of symptoms and functional impairment.3
Emphasize that major lifestyle adjustments usually are unnecessary in the absence of progression, especially for patients who are retired or not involved in endeavors that involve significant cognitive and executive functioning demands.
Discuss the role that cognition-enhancing medications might play in managing symptoms.4
Address indications for additional services, including formal psychiatric care for patients who have concomitant affective or behavioral symptoms and who are highly distressed by the diagnosis. Pair these services with longitudinal monitoring for possible exacerbation of symptoms.
Identify psychiatric, medical, and lifestyle factors that can increase the risk of dementia. Depending on the patient’s history, this might include diabetes, hypertension, elevated lipid levels, obesity, smoking, head trauma, depression, physical inactivity, and lack of intellectual stimulation.
Review compensatory strategies. In MCI predominantly amnestic type, for example, having the patient make systematic lists for shopping and other activities of daily living, as well as establishing routines for organizaton, can bolster successful coping.
If psychometric testing was not utilized to establish the diagnosis, discussion can include the value of performing such an assessment for a more finely tuned profile of preserved and impaired neurobehavioral functions. Such a profile can include test patterns that 1) have prognostic value with regard to the likelihood of progression to dementia and 2) establish a baseline against which you can assess stability or progression over time.5
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Mild cognitive impairment (MCI) is a transitional clinical stage between normal aging and dementia. Together with aging, it is considered the most significant risk factor for developing dementia, often the Alzheimer’s type.1
MCI is a challenging neuropsychiatric diagnosis to discuss with patients and their family because it is characterized by overlapping features of normal aging and because of its heterogeneity of etiology, clinical presentation, and outcome.2,3 The evolution to dementia and the lack of effective treatments for preventing or forestalling this outcome can be difficult to address—particularly when the patient is in good health and has been leading a productive life.
Successful communication is key
You can take steps to communicate in a helpful way, build a strong treatment alliance, and reduce the potential for the iatrogenic effects of disclosing this diagnosis and its prognostic implications.
Clarify that your findings are consistent with the patient’s or family’s report of sustained and concerning change in cognition and, depending on the patient, concurrent alterations in affect, behavior, or both. Emphasize that these changes are disproportionately severe relative to expectations for the patient’s age and are not caused by psychiatric or clear-cut medical factors.
Highlight contexts in which the patient’s symptoms are likely to become more disruptive and impaired, and situations in which the patient can be expected to function more effectively.
Provide evidence-based support for the rate of progression of symptoms and functional impairment.3
Emphasize that major lifestyle adjustments usually are unnecessary in the absence of progression, especially for patients who are retired or not involved in endeavors that involve significant cognitive and executive functioning demands.
Discuss the role that cognition-enhancing medications might play in managing symptoms.4
Address indications for additional services, including formal psychiatric care for patients who have concomitant affective or behavioral symptoms and who are highly distressed by the diagnosis. Pair these services with longitudinal monitoring for possible exacerbation of symptoms.
Identify psychiatric, medical, and lifestyle factors that can increase the risk of dementia. Depending on the patient’s history, this might include diabetes, hypertension, elevated lipid levels, obesity, smoking, head trauma, depression, physical inactivity, and lack of intellectual stimulation.
Review compensatory strategies. In MCI predominantly amnestic type, for example, having the patient make systematic lists for shopping and other activities of daily living, as well as establishing routines for organizaton, can bolster successful coping.
If psychometric testing was not utilized to establish the diagnosis, discussion can include the value of performing such an assessment for a more finely tuned profile of preserved and impaired neurobehavioral functions. Such a profile can include test patterns that 1) have prognostic value with regard to the likelihood of progression to dementia and 2) establish a baseline against which you can assess stability or progression over time.5
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270-279.
2. Ellison JM, Harper DG, Berlow Y, et al. Beyond the “C” in MCI: noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spectr. 2008;13(1):66-72.
3. Goveas JS, Dixon-Holbrook M, Kerwin D, et al. Mild cognitive impairment: how can you be sure? Current Psychiatry. 2008;7(4):36-40, 46-50.
4. Doody RS, Ferris SH, Salloway S, et al. Donepezil treatment of patients with MCI: a 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555-1561.
5. Summers MJ, Saunders NL. Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology. 2012;26(4):498-508.
1. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270-279.
2. Ellison JM, Harper DG, Berlow Y, et al. Beyond the “C” in MCI: noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spectr. 2008;13(1):66-72.
3. Goveas JS, Dixon-Holbrook M, Kerwin D, et al. Mild cognitive impairment: how can you be sure? Current Psychiatry. 2008;7(4):36-40, 46-50.
4. Doody RS, Ferris SH, Salloway S, et al. Donepezil treatment of patients with MCI: a 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555-1561.
5. Summers MJ, Saunders NL. Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology. 2012;26(4):498-508.
Avoid hospitalization for severe and enduring anorexia nervosa by personalizing your care
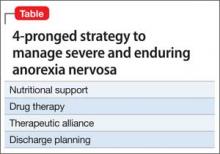
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2008;165(10):1281-1288.
2. Stiles-Shields C, Touyz S, Hay P, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783-789.
3. Sly R, Morgan JF, Mountford VA, et al. Predicting premature termination of hospitalised treatment for anorexia nervosa: the roles of therapeutic alliance, motivation, and behaviour change. Eat Behav. 2013;14(2):119-123.
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2008;165(10):1281-1288.
2. Stiles-Shields C, Touyz S, Hay P, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783-789.
3. Sly R, Morgan JF, Mountford VA, et al. Predicting premature termination of hospitalised treatment for anorexia nervosa: the roles of therapeutic alliance, motivation, and behaviour change. Eat Behav. 2013;14(2):119-123.
1. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2008;165(10):1281-1288.
2. Stiles-Shields C, Touyz S, Hay P, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783-789.
3. Sly R, Morgan JF, Mountford VA, et al. Predicting premature termination of hospitalised treatment for anorexia nervosa: the roles of therapeutic alliance, motivation, and behaviour change. Eat Behav. 2013;14(2):119-123.
Take caution: Look for DISTURBED behaviors when you assess violence risk
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
Take caution: Look for DISTURBED behaviors when you assess violence risk
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
Take caution: Look for DISTURBED behaviors when you assess violence risk
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impusivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be aware of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings—2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impusivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be aware of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings—2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impusivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be aware of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings—2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
A diverted or stolen prescription has been signed in your name. What do you do now?
For a busy clinician, learning that a prescription pad has been stolen, sub-mitted with a counterfeit signature, and used to acquire a controlled substance comes as a shock. It evokes a sense of betrayal and raises a number of medico-legal issues that can be avoided if you know how to protect yourself.
Prescription pad security
One of the simplest ways to reduce prescription pad theft is to lock the pads in a secure location when the office is closed.1 Establish and maintain an inventory of prescription pads; you should number and count pads weekly. For Schedule-II controlled substance prescription pads, document the control number on each new pad.1 The best way to ensure that all pads are accounted for is by using sequential numbering similar to bank check numbers.
Do not allow staff to sign your prescription pad. Limit access to prescription pads to authorized personnel; be sure that they keep the prescription pad in their pocket, not on their desk or a counter, and not in examining rooms, where they could be stolen. For electronic prescribing, always lock the drawer where the computer prescription paper sits.1
Some physicians might find it helpful to invest in tamper-resistant prescription pads. As of April 2008, the Centers for Medicare and Medicaid Services mandates that for a prescription pad to be considered tamper-resistant it must include 1 or more industry-recognized features designed to prevent unauthorized copying, erasure, or modification of prescriptions.2
When you order prescription pads, do not print your Drug Enforcement Administration (DEA) number on the pads. Also, check that your printer maintains strict process controls over prescription pad production, storage, and delivery.1
Other ways to prevent fraudulent prescriptions include using a gel pen to write prescriptions, because these pens contain pigments that are quickly absorbed, preventing ink from being washed away with chemical solvents.1 Never leave blank space on a written prescription and do not sign blank prescription pads beforehand.3 Write instructions clearly on each prescription, informing pharmacists of ways to verify the prescription’s authenticity.
Legal responsibilities
In case your prescription pads are stolen, even after taking precautionary measures, make the following actions to report and record fraudulent charges:
• If your prescription pads for Schedule-II medications—known as “triplicates”— are missing, give the control number of the first and last prescription in the pad to your state’s pharmacy organization. Some states have an electronic alert system to aid with filing a fraud claim (eg, the Texas Pharmacy Association has a section on its Web site for reporting prescription fraud and theft).
• Immediately inform the local police department and local DEA office of the theft.3 Keep a copy of all communications for future reference.
• If a pharmacy alerts you that a fraudulent prescription has been filled using one of your pads, request a copy of each filled prescription. Keep these records and file a copy with the police department and DEA.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Seven helpful tips to improve prescription security in your medical practice. Standard Register Healthcare. http:// www.standardregister. com/securescrip/guide-to-prescription-pad-security. asp. Accessed June 6, 2012.
2. Guide to tamper-resistant Rx pads. Standard Register Healthcare. http://www. securescrip.com/guide-to-tamper-resistant-rx-pads. asp. Accessed June 6, 2012.
3. U.S. Department of Justice. Drug Enforcement Administration. Office of Diversion Control. Practitioner’s manual. Section III – security requirements. http://www. deadiversion.usdoj.gov/pubs/ manuals/pract/section3. htm. Accessed June 6, 2012.
For a busy clinician, learning that a prescription pad has been stolen, sub-mitted with a counterfeit signature, and used to acquire a controlled substance comes as a shock. It evokes a sense of betrayal and raises a number of medico-legal issues that can be avoided if you know how to protect yourself.
Prescription pad security
One of the simplest ways to reduce prescription pad theft is to lock the pads in a secure location when the office is closed.1 Establish and maintain an inventory of prescription pads; you should number and count pads weekly. For Schedule-II controlled substance prescription pads, document the control number on each new pad.1 The best way to ensure that all pads are accounted for is by using sequential numbering similar to bank check numbers.
Do not allow staff to sign your prescription pad. Limit access to prescription pads to authorized personnel; be sure that they keep the prescription pad in their pocket, not on their desk or a counter, and not in examining rooms, where they could be stolen. For electronic prescribing, always lock the drawer where the computer prescription paper sits.1
Some physicians might find it helpful to invest in tamper-resistant prescription pads. As of April 2008, the Centers for Medicare and Medicaid Services mandates that for a prescription pad to be considered tamper-resistant it must include 1 or more industry-recognized features designed to prevent unauthorized copying, erasure, or modification of prescriptions.2
When you order prescription pads, do not print your Drug Enforcement Administration (DEA) number on the pads. Also, check that your printer maintains strict process controls over prescription pad production, storage, and delivery.1
Other ways to prevent fraudulent prescriptions include using a gel pen to write prescriptions, because these pens contain pigments that are quickly absorbed, preventing ink from being washed away with chemical solvents.1 Never leave blank space on a written prescription and do not sign blank prescription pads beforehand.3 Write instructions clearly on each prescription, informing pharmacists of ways to verify the prescription’s authenticity.
Legal responsibilities
In case your prescription pads are stolen, even after taking precautionary measures, make the following actions to report and record fraudulent charges:
• If your prescription pads for Schedule-II medications—known as “triplicates”— are missing, give the control number of the first and last prescription in the pad to your state’s pharmacy organization. Some states have an electronic alert system to aid with filing a fraud claim (eg, the Texas Pharmacy Association has a section on its Web site for reporting prescription fraud and theft).
• Immediately inform the local police department and local DEA office of the theft.3 Keep a copy of all communications for future reference.
• If a pharmacy alerts you that a fraudulent prescription has been filled using one of your pads, request a copy of each filled prescription. Keep these records and file a copy with the police department and DEA.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
For a busy clinician, learning that a prescription pad has been stolen, sub-mitted with a counterfeit signature, and used to acquire a controlled substance comes as a shock. It evokes a sense of betrayal and raises a number of medico-legal issues that can be avoided if you know how to protect yourself.
Prescription pad security
One of the simplest ways to reduce prescription pad theft is to lock the pads in a secure location when the office is closed.1 Establish and maintain an inventory of prescription pads; you should number and count pads weekly. For Schedule-II controlled substance prescription pads, document the control number on each new pad.1 The best way to ensure that all pads are accounted for is by using sequential numbering similar to bank check numbers.
Do not allow staff to sign your prescription pad. Limit access to prescription pads to authorized personnel; be sure that they keep the prescription pad in their pocket, not on their desk or a counter, and not in examining rooms, where they could be stolen. For electronic prescribing, always lock the drawer where the computer prescription paper sits.1
Some physicians might find it helpful to invest in tamper-resistant prescription pads. As of April 2008, the Centers for Medicare and Medicaid Services mandates that for a prescription pad to be considered tamper-resistant it must include 1 or more industry-recognized features designed to prevent unauthorized copying, erasure, or modification of prescriptions.2
When you order prescription pads, do not print your Drug Enforcement Administration (DEA) number on the pads. Also, check that your printer maintains strict process controls over prescription pad production, storage, and delivery.1
Other ways to prevent fraudulent prescriptions include using a gel pen to write prescriptions, because these pens contain pigments that are quickly absorbed, preventing ink from being washed away with chemical solvents.1 Never leave blank space on a written prescription and do not sign blank prescription pads beforehand.3 Write instructions clearly on each prescription, informing pharmacists of ways to verify the prescription’s authenticity.
Legal responsibilities
In case your prescription pads are stolen, even after taking precautionary measures, make the following actions to report and record fraudulent charges:
• If your prescription pads for Schedule-II medications—known as “triplicates”— are missing, give the control number of the first and last prescription in the pad to your state’s pharmacy organization. Some states have an electronic alert system to aid with filing a fraud claim (eg, the Texas Pharmacy Association has a section on its Web site for reporting prescription fraud and theft).
• Immediately inform the local police department and local DEA office of the theft.3 Keep a copy of all communications for future reference.
• If a pharmacy alerts you that a fraudulent prescription has been filled using one of your pads, request a copy of each filled prescription. Keep these records and file a copy with the police department and DEA.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Seven helpful tips to improve prescription security in your medical practice. Standard Register Healthcare. http:// www.standardregister. com/securescrip/guide-to-prescription-pad-security. asp. Accessed June 6, 2012.
2. Guide to tamper-resistant Rx pads. Standard Register Healthcare. http://www. securescrip.com/guide-to-tamper-resistant-rx-pads. asp. Accessed June 6, 2012.
3. U.S. Department of Justice. Drug Enforcement Administration. Office of Diversion Control. Practitioner’s manual. Section III – security requirements. http://www. deadiversion.usdoj.gov/pubs/ manuals/pract/section3. htm. Accessed June 6, 2012.
1. Seven helpful tips to improve prescription security in your medical practice. Standard Register Healthcare. http:// www.standardregister. com/securescrip/guide-to-prescription-pad-security. asp. Accessed June 6, 2012.
2. Guide to tamper-resistant Rx pads. Standard Register Healthcare. http://www. securescrip.com/guide-to-tamper-resistant-rx-pads. asp. Accessed June 6, 2012.
3. U.S. Department of Justice. Drug Enforcement Administration. Office of Diversion Control. Practitioner’s manual. Section III – security requirements. http://www. deadiversion.usdoj.gov/pubs/ manuals/pract/section3. htm. Accessed June 6, 2012.
Poor oral hygiene in the mentally ill: Be aware of the problem, and intervene
Poor oral health is common among mentally ill people and is related to inadequate nutrition, poor self-care, substance abuse, and medication side effects.1 Poor oral hygiene is a significant problem because it results in dental pathology that has an adverse influence on the whole body.
Compared with the general population, mentally ill patients are 3 times more likely to have their teeth removed.2 In a survey of mentally ill adults, 92% were found to have tooth decay—of which 23% were untreated and 40% smoked tobacco.3 Approximately 9% have periodontal disease, which most often occurs in those who smoke cigarettes.4
Lifestyle contributors
Drug abuse facilitates dental diseases, as evidenced by the high rate of caries among methamphetamine users.5 The drug induces xerostomia, encouraging users to drink sweetened beverages; this, combined with limited oral care, results in profound dental decay (“meth mouth”). Oral cocaine users often exhibit dental erosions or abrasions, gingival lacerations or necrosis, and mucosal lesions. Smoking Cannabis is associated with an increased rate of gingivitis, alveolar bone loss, leukoplakia, and oral papilloma or other cancers.5 Heroin users are at increased risk of tooth decay, periodontal disease, and oral infection.5
Alcohol consumption increases the risk of oral cancer. Long-term alcohol use suppresses bone marrow function, causing leukopenia and resulting in immunosuppression and an increased incidence of dental infections.6 Excessive alcohol consumption also can cause thrombocytopenia and bleeding, which can complicate dental procedures.
Smoking cigarettes increases the incidence of periodontal disease, especially necrotizing gingivitis and candidiasis.7 Ninety percent of patients with schizophrenia smoke—compared with up to 70% of patients with other psychiatric disorders, and 19% of the general population.7,8 Physiologic aspects of schizophrenia reinforce the smoking habit.7
Somatic ailments. Psychiatric disorders are strongly associated with diabetes, obesity, hypertension, stroke, heart disease, and arthritis, all of which contribute to oral pathology. Older age, greater dysfunction, longer duration of illness, and smoking are predictors of adverse dental outcomes.
Anxiety, depression, stress—all of these these disorders increase the circulating level of cortisol, thus raising the risk that periodontal disease will progress.9 Periodontitis increases the risk of stroke and heart attack by accelerating atherosclerotic plaque formation.10 Depression, anxiety, and substance abuse can lead to temporomandibular disorders that cause pain and restrict jaw movement.11 Stressed patients may experience muscle tension and bruxism, which can lead to temporomandibular joint discomfort.
Eating disorders. Patients who induce vomiting may exhibit enamel erosions (especially on the anterior maxillary teeth), increased tooth hypersensitivity, decay, and wear on dental restorative work.
Atypical odontalgia, characterized by chronic, burning pain in teeth and gums, is associated with depression and anxiety.11 Misdiagnosis can result in extractions or procedures without an appropriate indication and failure to alleviate the pain.
Medication side effects. Xerostomia can increase the risk for caries, periodontal disease, and oral infections such as candidiasis, glossitis, stomatitis, and parotitis.9 Extrapyramidal side effects (tardive dyskinesia, dystonia) may cause tooth damage and make managing dentures difficult.6
What to tell patients, and what you can do for them
Encourage your patients to reduce their sugar intake, brush and floss regularly, and work to stop smoking or ingesting substances of abuse. Teach appropriate hygiene and nutrition, which reduces the risk of dental caries, infection, and related problems. Recommend periodic oral health screening and how to secure such dental care.
From your position of familiarity with patients’ psychopharmacotherapy, make an effort to personalize and adjust their regimens when dental disease is present to address concerns about oral health that can be caused by medication side effects.
A multidisciplinary approach with patient advocacy, involving you and the patient’s dentist and primary care physician, facilitates health care and works to offer the patient access to global medical services.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mental Illness Fellowship of Australia Inc. Overview of the oral health of people affected by mental illness. http:// www.wfmh.com/links/external-contacts/mental-illness-fellowship-of-australia. Accessed June 18, 2014.
2. Kisely S, Quek LH, Pais J, et al. Advanced dental disease in people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. 2011;199(3):187-193.
3. Dental caries (tooth decay) in adults (age 20 to 64). National Institute of Dental and Craniofacial Research. http:// www.nidcr.nih.gov/DataStatistics/FindDataByTopic/ DentalCaries/DentalCariesAdults20to64.htm. Updated January 6, 2014. Accessed June 18, 2014.
4. Peridontal disease in adults (age 20 to 64). National Institute of Dental and Craniofacial Research. http://www.nidcr. nih.gov/DataStatistics/FindDataByTopic/GumDisease/ PeriodontaldiseaseAdults20to64.htm. Updated January 6, 2014. Accessed June 18, 2014.
5. Maloney WJ. The significance of illicit drug use to dental practice. http://www.webmedcentral.com/wmcpdf/ Article_WMC00455.pdf. Published July 28, 2010. Accessed June 18, 2014.
6. Oral health care for people with mental problems: guidelines and recommendations. British Society for Disability and Oral Health. http://www.bsdh.org.uk/guidelines/ mental.pdf. Updated January 2000. Accessed June 18, 2014.
7. Lohr JB, Flynn K. Smoking and schizophrenia. Schizophr Res. 1992;8(2):93-102.
8. Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years–United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207-1212.
9. Yoffee L. The link between oral health and medical illness. http://www.everydayhealth.com/dental-health/oral-conditions/oral-health-and-other-diseases.aspx. Updated November 9, 2012. Accessed June 18, 2014.
10. Demmer RT, Desvarieux M. Periodontal infections and cardiovascular disease: the heart of the matter. J Am Dent Assoc. 2006;137(suppl 2):14S-20S; quiz 38S.
11. Mental illness and the dental patient. American Dental Hygienists’ Association. http://www.adha.org/ce-course-10. Accessed June 18, 2014.
Poor oral health is common among mentally ill people and is related to inadequate nutrition, poor self-care, substance abuse, and medication side effects.1 Poor oral hygiene is a significant problem because it results in dental pathology that has an adverse influence on the whole body.
Compared with the general population, mentally ill patients are 3 times more likely to have their teeth removed.2 In a survey of mentally ill adults, 92% were found to have tooth decay—of which 23% were untreated and 40% smoked tobacco.3 Approximately 9% have periodontal disease, which most often occurs in those who smoke cigarettes.4
Lifestyle contributors
Drug abuse facilitates dental diseases, as evidenced by the high rate of caries among methamphetamine users.5 The drug induces xerostomia, encouraging users to drink sweetened beverages; this, combined with limited oral care, results in profound dental decay (“meth mouth”). Oral cocaine users often exhibit dental erosions or abrasions, gingival lacerations or necrosis, and mucosal lesions. Smoking Cannabis is associated with an increased rate of gingivitis, alveolar bone loss, leukoplakia, and oral papilloma or other cancers.5 Heroin users are at increased risk of tooth decay, periodontal disease, and oral infection.5
Alcohol consumption increases the risk of oral cancer. Long-term alcohol use suppresses bone marrow function, causing leukopenia and resulting in immunosuppression and an increased incidence of dental infections.6 Excessive alcohol consumption also can cause thrombocytopenia and bleeding, which can complicate dental procedures.
Smoking cigarettes increases the incidence of periodontal disease, especially necrotizing gingivitis and candidiasis.7 Ninety percent of patients with schizophrenia smoke—compared with up to 70% of patients with other psychiatric disorders, and 19% of the general population.7,8 Physiologic aspects of schizophrenia reinforce the smoking habit.7
Somatic ailments. Psychiatric disorders are strongly associated with diabetes, obesity, hypertension, stroke, heart disease, and arthritis, all of which contribute to oral pathology. Older age, greater dysfunction, longer duration of illness, and smoking are predictors of adverse dental outcomes.
Anxiety, depression, stress—all of these these disorders increase the circulating level of cortisol, thus raising the risk that periodontal disease will progress.9 Periodontitis increases the risk of stroke and heart attack by accelerating atherosclerotic plaque formation.10 Depression, anxiety, and substance abuse can lead to temporomandibular disorders that cause pain and restrict jaw movement.11 Stressed patients may experience muscle tension and bruxism, which can lead to temporomandibular joint discomfort.
Eating disorders. Patients who induce vomiting may exhibit enamel erosions (especially on the anterior maxillary teeth), increased tooth hypersensitivity, decay, and wear on dental restorative work.
Atypical odontalgia, characterized by chronic, burning pain in teeth and gums, is associated with depression and anxiety.11 Misdiagnosis can result in extractions or procedures without an appropriate indication and failure to alleviate the pain.
Medication side effects. Xerostomia can increase the risk for caries, periodontal disease, and oral infections such as candidiasis, glossitis, stomatitis, and parotitis.9 Extrapyramidal side effects (tardive dyskinesia, dystonia) may cause tooth damage and make managing dentures difficult.6
What to tell patients, and what you can do for them
Encourage your patients to reduce their sugar intake, brush and floss regularly, and work to stop smoking or ingesting substances of abuse. Teach appropriate hygiene and nutrition, which reduces the risk of dental caries, infection, and related problems. Recommend periodic oral health screening and how to secure such dental care.
From your position of familiarity with patients’ psychopharmacotherapy, make an effort to personalize and adjust their regimens when dental disease is present to address concerns about oral health that can be caused by medication side effects.
A multidisciplinary approach with patient advocacy, involving you and the patient’s dentist and primary care physician, facilitates health care and works to offer the patient access to global medical services.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Poor oral health is common among mentally ill people and is related to inadequate nutrition, poor self-care, substance abuse, and medication side effects.1 Poor oral hygiene is a significant problem because it results in dental pathology that has an adverse influence on the whole body.
Compared with the general population, mentally ill patients are 3 times more likely to have their teeth removed.2 In a survey of mentally ill adults, 92% were found to have tooth decay—of which 23% were untreated and 40% smoked tobacco.3 Approximately 9% have periodontal disease, which most often occurs in those who smoke cigarettes.4
Lifestyle contributors
Drug abuse facilitates dental diseases, as evidenced by the high rate of caries among methamphetamine users.5 The drug induces xerostomia, encouraging users to drink sweetened beverages; this, combined with limited oral care, results in profound dental decay (“meth mouth”). Oral cocaine users often exhibit dental erosions or abrasions, gingival lacerations or necrosis, and mucosal lesions. Smoking Cannabis is associated with an increased rate of gingivitis, alveolar bone loss, leukoplakia, and oral papilloma or other cancers.5 Heroin users are at increased risk of tooth decay, periodontal disease, and oral infection.5
Alcohol consumption increases the risk of oral cancer. Long-term alcohol use suppresses bone marrow function, causing leukopenia and resulting in immunosuppression and an increased incidence of dental infections.6 Excessive alcohol consumption also can cause thrombocytopenia and bleeding, which can complicate dental procedures.
Smoking cigarettes increases the incidence of periodontal disease, especially necrotizing gingivitis and candidiasis.7 Ninety percent of patients with schizophrenia smoke—compared with up to 70% of patients with other psychiatric disorders, and 19% of the general population.7,8 Physiologic aspects of schizophrenia reinforce the smoking habit.7
Somatic ailments. Psychiatric disorders are strongly associated with diabetes, obesity, hypertension, stroke, heart disease, and arthritis, all of which contribute to oral pathology. Older age, greater dysfunction, longer duration of illness, and smoking are predictors of adverse dental outcomes.
Anxiety, depression, stress—all of these these disorders increase the circulating level of cortisol, thus raising the risk that periodontal disease will progress.9 Periodontitis increases the risk of stroke and heart attack by accelerating atherosclerotic plaque formation.10 Depression, anxiety, and substance abuse can lead to temporomandibular disorders that cause pain and restrict jaw movement.11 Stressed patients may experience muscle tension and bruxism, which can lead to temporomandibular joint discomfort.
Eating disorders. Patients who induce vomiting may exhibit enamel erosions (especially on the anterior maxillary teeth), increased tooth hypersensitivity, decay, and wear on dental restorative work.
Atypical odontalgia, characterized by chronic, burning pain in teeth and gums, is associated with depression and anxiety.11 Misdiagnosis can result in extractions or procedures without an appropriate indication and failure to alleviate the pain.
Medication side effects. Xerostomia can increase the risk for caries, periodontal disease, and oral infections such as candidiasis, glossitis, stomatitis, and parotitis.9 Extrapyramidal side effects (tardive dyskinesia, dystonia) may cause tooth damage and make managing dentures difficult.6
What to tell patients, and what you can do for them
Encourage your patients to reduce their sugar intake, brush and floss regularly, and work to stop smoking or ingesting substances of abuse. Teach appropriate hygiene and nutrition, which reduces the risk of dental caries, infection, and related problems. Recommend periodic oral health screening and how to secure such dental care.
From your position of familiarity with patients’ psychopharmacotherapy, make an effort to personalize and adjust their regimens when dental disease is present to address concerns about oral health that can be caused by medication side effects.
A multidisciplinary approach with patient advocacy, involving you and the patient’s dentist and primary care physician, facilitates health care and works to offer the patient access to global medical services.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mental Illness Fellowship of Australia Inc. Overview of the oral health of people affected by mental illness. http:// www.wfmh.com/links/external-contacts/mental-illness-fellowship-of-australia. Accessed June 18, 2014.
2. Kisely S, Quek LH, Pais J, et al. Advanced dental disease in people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. 2011;199(3):187-193.
3. Dental caries (tooth decay) in adults (age 20 to 64). National Institute of Dental and Craniofacial Research. http:// www.nidcr.nih.gov/DataStatistics/FindDataByTopic/ DentalCaries/DentalCariesAdults20to64.htm. Updated January 6, 2014. Accessed June 18, 2014.
4. Peridontal disease in adults (age 20 to 64). National Institute of Dental and Craniofacial Research. http://www.nidcr. nih.gov/DataStatistics/FindDataByTopic/GumDisease/ PeriodontaldiseaseAdults20to64.htm. Updated January 6, 2014. Accessed June 18, 2014.
5. Maloney WJ. The significance of illicit drug use to dental practice. http://www.webmedcentral.com/wmcpdf/ Article_WMC00455.pdf. Published July 28, 2010. Accessed June 18, 2014.
6. Oral health care for people with mental problems: guidelines and recommendations. British Society for Disability and Oral Health. http://www.bsdh.org.uk/guidelines/ mental.pdf. Updated January 2000. Accessed June 18, 2014.
7. Lohr JB, Flynn K. Smoking and schizophrenia. Schizophr Res. 1992;8(2):93-102.
8. Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years–United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207-1212.
9. Yoffee L. The link between oral health and medical illness. http://www.everydayhealth.com/dental-health/oral-conditions/oral-health-and-other-diseases.aspx. Updated November 9, 2012. Accessed June 18, 2014.
10. Demmer RT, Desvarieux M. Periodontal infections and cardiovascular disease: the heart of the matter. J Am Dent Assoc. 2006;137(suppl 2):14S-20S; quiz 38S.
11. Mental illness and the dental patient. American Dental Hygienists’ Association. http://www.adha.org/ce-course-10. Accessed June 18, 2014.
1. Mental Illness Fellowship of Australia Inc. Overview of the oral health of people affected by mental illness. http:// www.wfmh.com/links/external-contacts/mental-illness-fellowship-of-australia. Accessed June 18, 2014.
2. Kisely S, Quek LH, Pais J, et al. Advanced dental disease in people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. 2011;199(3):187-193.
3. Dental caries (tooth decay) in adults (age 20 to 64). National Institute of Dental and Craniofacial Research. http:// www.nidcr.nih.gov/DataStatistics/FindDataByTopic/ DentalCaries/DentalCariesAdults20to64.htm. Updated January 6, 2014. Accessed June 18, 2014.
4. Peridontal disease in adults (age 20 to 64). National Institute of Dental and Craniofacial Research. http://www.nidcr. nih.gov/DataStatistics/FindDataByTopic/GumDisease/ PeriodontaldiseaseAdults20to64.htm. Updated January 6, 2014. Accessed June 18, 2014.
5. Maloney WJ. The significance of illicit drug use to dental practice. http://www.webmedcentral.com/wmcpdf/ Article_WMC00455.pdf. Published July 28, 2010. Accessed June 18, 2014.
6. Oral health care for people with mental problems: guidelines and recommendations. British Society for Disability and Oral Health. http://www.bsdh.org.uk/guidelines/ mental.pdf. Updated January 2000. Accessed June 18, 2014.
7. Lohr JB, Flynn K. Smoking and schizophrenia. Schizophr Res. 1992;8(2):93-102.
8. Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years–United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207-1212.
9. Yoffee L. The link between oral health and medical illness. http://www.everydayhealth.com/dental-health/oral-conditions/oral-health-and-other-diseases.aspx. Updated November 9, 2012. Accessed June 18, 2014.
10. Demmer RT, Desvarieux M. Periodontal infections and cardiovascular disease: the heart of the matter. J Am Dent Assoc. 2006;137(suppl 2):14S-20S; quiz 38S.
11. Mental illness and the dental patient. American Dental Hygienists’ Association. http://www.adha.org/ce-course-10. Accessed June 18, 2014.
Frontotemporal dementia and its variants: What to look for
Frontotemporal dementia (FTD) is a neurologic disease that affects the frontal and the temporal lobes of the cerebral cortex.1 This disorder is observed most often in people between age 45 to 65, but also can manifest in younger or older persons.1 The cause varies among a range of pathologies affecting the anterior portions of the brain.2
Presentations
FTD presents with changes in personality, social skills, ability to concentrate, motivation, reasoning, and language abnormality.3 Memory loss is less prominent in this condition compared with other dementias; therefore, identification may be a diagnostic challenge. FTD can be misdiagnosed as a psychiatric illness or not recognized because social symptoms dominate over cognitive dysfunction. As the disease progresses, patients may become increasingly unable to plan or organize activities of daily living, behave appropriately, and react normally in social interactions.1
FTD has 3 diagnostic variants1-4:
Behavioral variant. Known as Pick disease or the “frontal variant,”1,2 this type of FTD manifests as changes in personality, improper behavior in social settings, personal neglect, or impulsivity, such as shoplifting or hypersexuality.
Primary progressive aphasia. Two types of language dysfunction are observed in FTD:
• Semantic dementia (SD)3: Left-sided SD presents with “meaningless speech” or “word substitutions” (eg, “chair” instead of “table”). Right-sided SD, however, is characterized by forgetting the faces of familiar people or objects.
• Primary nonfluent aphasia3: Language fluency is compromised. Persons with such language dysfunction cannot produce words easily, and their speech is stumbling and nonfluent.
FTD with motor neuron disease.4 The most common type of motor neuron disease associated with FTD is amyotrophic lateral sclerosis. Afflicted patients exhibit muscle weakness, spasms, and rigidity. This leads to difficulty in swallowing or breathing because the diaphragm and pharynx are paralyzed. Other diseases associated with FTD include corticobasal degeneration and progressive supranuclear palsy.
Diagnosis
In DSM-5, FTD has been renamed “frontotemporal lobar degeneration” under the category of “Major and Mild Neurocognitive Disorders.”5 The workup begins with a history, physical examination, and mental status assessment. Physical signs can include frontal-release, primitive reflexes. Early in the disease course, a palmomental reflex often is observed; later, as disease progress, the rooting reflex or palmar grasp may become apparent.1,5
Diagnosing FTD requires recognizing its symptoms and ruling out conditions such as Alzheimer’s disease, depression, and schizophrenia.6 Laboratory studies may help identify other conditions. Brain imaging, such as MRI, can depict frontotemporal pathology and rule in or exclude other diseases.3,5
Psychometric testing can evaluate memory or cognitive ability, which might be unremarkable during the initial phases of FTD.4 Further psychological assessments may provide objective verification of frontal lobe deficiencies in social skills or activities of daily living.3 Positron emission tomography and single-photon emission computed tomography may demonstrate areas of decreased activity or hypoperfusion in frontal and temporal lobes.7
Interventions
Treatment of FTD is limited to symptomatic therapy8; there are no specific, approved countermeasures available. Comorbid conditions, such as diabetes mellitus or hypertension, should be treated medically. Social interventions such as day care, increased supervision, and emotional support from the family can be effective adjuvants.2
Disclosures
The authors report no financial relationship whose products are mentioned in this article or with manufacturers of competing products.
1. Snowden JS, Neary D, Mann DM. Frontotemporal dementia. Br J Psychiatry. 2002;180:140-143.
2. Frontotemporal degeneration. The Association for Frontotemporal Degeneration. http://www.theaftd.org/ frontotemporal-degeneration/ftd-overview. Accessed April 24, 2014.
3. Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51(6):1546-1554.
4. Clark CM, Forman MS. Frontotemporal lobar degeneration with motor neuron disease: a clinical and pathological spectrum. Arch Neurol. 2006;63(4):489-490.
5. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:614-618.
6. Frontotemporal dementia diagnosis. UCSF Medical Center. http://www.ucsfhealth.org/conditions/frontotemporal_ dementia/diagnosis.html. Accessed April 24, 2014.
7. McMurtray AM, Chen AK, Shapira JS, et al. Variations in regional SPECT hypoperfusion and clinical features in frontotemporal dementia. Neurology. 2006;66(4):517-522.
8. Miller BL, Lee SE. Frontotemporal dementia: treatment. Up To Date. http://www.uptodate.com/contents/frontotemporal-dementia-treatment?source=search_result&search=frontote mporal+dementia+treatment&selectedTitle=1~150. Updated December 30, 2013. Accessed April 24, 2014.
Frontotemporal dementia (FTD) is a neurologic disease that affects the frontal and the temporal lobes of the cerebral cortex.1 This disorder is observed most often in people between age 45 to 65, but also can manifest in younger or older persons.1 The cause varies among a range of pathologies affecting the anterior portions of the brain.2
Presentations
FTD presents with changes in personality, social skills, ability to concentrate, motivation, reasoning, and language abnormality.3 Memory loss is less prominent in this condition compared with other dementias; therefore, identification may be a diagnostic challenge. FTD can be misdiagnosed as a psychiatric illness or not recognized because social symptoms dominate over cognitive dysfunction. As the disease progresses, patients may become increasingly unable to plan or organize activities of daily living, behave appropriately, and react normally in social interactions.1
FTD has 3 diagnostic variants1-4:
Behavioral variant. Known as Pick disease or the “frontal variant,”1,2 this type of FTD manifests as changes in personality, improper behavior in social settings, personal neglect, or impulsivity, such as shoplifting or hypersexuality.
Primary progressive aphasia. Two types of language dysfunction are observed in FTD:
• Semantic dementia (SD)3: Left-sided SD presents with “meaningless speech” or “word substitutions” (eg, “chair” instead of “table”). Right-sided SD, however, is characterized by forgetting the faces of familiar people or objects.
• Primary nonfluent aphasia3: Language fluency is compromised. Persons with such language dysfunction cannot produce words easily, and their speech is stumbling and nonfluent.
FTD with motor neuron disease.4 The most common type of motor neuron disease associated with FTD is amyotrophic lateral sclerosis. Afflicted patients exhibit muscle weakness, spasms, and rigidity. This leads to difficulty in swallowing or breathing because the diaphragm and pharynx are paralyzed. Other diseases associated with FTD include corticobasal degeneration and progressive supranuclear palsy.
Diagnosis
In DSM-5, FTD has been renamed “frontotemporal lobar degeneration” under the category of “Major and Mild Neurocognitive Disorders.”5 The workup begins with a history, physical examination, and mental status assessment. Physical signs can include frontal-release, primitive reflexes. Early in the disease course, a palmomental reflex often is observed; later, as disease progress, the rooting reflex or palmar grasp may become apparent.1,5
Diagnosing FTD requires recognizing its symptoms and ruling out conditions such as Alzheimer’s disease, depression, and schizophrenia.6 Laboratory studies may help identify other conditions. Brain imaging, such as MRI, can depict frontotemporal pathology and rule in or exclude other diseases.3,5
Psychometric testing can evaluate memory or cognitive ability, which might be unremarkable during the initial phases of FTD.4 Further psychological assessments may provide objective verification of frontal lobe deficiencies in social skills or activities of daily living.3 Positron emission tomography and single-photon emission computed tomography may demonstrate areas of decreased activity or hypoperfusion in frontal and temporal lobes.7
Interventions
Treatment of FTD is limited to symptomatic therapy8; there are no specific, approved countermeasures available. Comorbid conditions, such as diabetes mellitus or hypertension, should be treated medically. Social interventions such as day care, increased supervision, and emotional support from the family can be effective adjuvants.2
Disclosures
The authors report no financial relationship whose products are mentioned in this article or with manufacturers of competing products.
Frontotemporal dementia (FTD) is a neurologic disease that affects the frontal and the temporal lobes of the cerebral cortex.1 This disorder is observed most often in people between age 45 to 65, but also can manifest in younger or older persons.1 The cause varies among a range of pathologies affecting the anterior portions of the brain.2
Presentations
FTD presents with changes in personality, social skills, ability to concentrate, motivation, reasoning, and language abnormality.3 Memory loss is less prominent in this condition compared with other dementias; therefore, identification may be a diagnostic challenge. FTD can be misdiagnosed as a psychiatric illness or not recognized because social symptoms dominate over cognitive dysfunction. As the disease progresses, patients may become increasingly unable to plan or organize activities of daily living, behave appropriately, and react normally in social interactions.1
FTD has 3 diagnostic variants1-4:
Behavioral variant. Known as Pick disease or the “frontal variant,”1,2 this type of FTD manifests as changes in personality, improper behavior in social settings, personal neglect, or impulsivity, such as shoplifting or hypersexuality.
Primary progressive aphasia. Two types of language dysfunction are observed in FTD:
• Semantic dementia (SD)3: Left-sided SD presents with “meaningless speech” or “word substitutions” (eg, “chair” instead of “table”). Right-sided SD, however, is characterized by forgetting the faces of familiar people or objects.
• Primary nonfluent aphasia3: Language fluency is compromised. Persons with such language dysfunction cannot produce words easily, and their speech is stumbling and nonfluent.
FTD with motor neuron disease.4 The most common type of motor neuron disease associated with FTD is amyotrophic lateral sclerosis. Afflicted patients exhibit muscle weakness, spasms, and rigidity. This leads to difficulty in swallowing or breathing because the diaphragm and pharynx are paralyzed. Other diseases associated with FTD include corticobasal degeneration and progressive supranuclear palsy.
Diagnosis
In DSM-5, FTD has been renamed “frontotemporal lobar degeneration” under the category of “Major and Mild Neurocognitive Disorders.”5 The workup begins with a history, physical examination, and mental status assessment. Physical signs can include frontal-release, primitive reflexes. Early in the disease course, a palmomental reflex often is observed; later, as disease progress, the rooting reflex or palmar grasp may become apparent.1,5
Diagnosing FTD requires recognizing its symptoms and ruling out conditions such as Alzheimer’s disease, depression, and schizophrenia.6 Laboratory studies may help identify other conditions. Brain imaging, such as MRI, can depict frontotemporal pathology and rule in or exclude other diseases.3,5
Psychometric testing can evaluate memory or cognitive ability, which might be unremarkable during the initial phases of FTD.4 Further psychological assessments may provide objective verification of frontal lobe deficiencies in social skills or activities of daily living.3 Positron emission tomography and single-photon emission computed tomography may demonstrate areas of decreased activity or hypoperfusion in frontal and temporal lobes.7
Interventions
Treatment of FTD is limited to symptomatic therapy8; there are no specific, approved countermeasures available. Comorbid conditions, such as diabetes mellitus or hypertension, should be treated medically. Social interventions such as day care, increased supervision, and emotional support from the family can be effective adjuvants.2
Disclosures
The authors report no financial relationship whose products are mentioned in this article or with manufacturers of competing products.
1. Snowden JS, Neary D, Mann DM. Frontotemporal dementia. Br J Psychiatry. 2002;180:140-143.
2. Frontotemporal degeneration. The Association for Frontotemporal Degeneration. http://www.theaftd.org/ frontotemporal-degeneration/ftd-overview. Accessed April 24, 2014.
3. Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51(6):1546-1554.
4. Clark CM, Forman MS. Frontotemporal lobar degeneration with motor neuron disease: a clinical and pathological spectrum. Arch Neurol. 2006;63(4):489-490.
5. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:614-618.
6. Frontotemporal dementia diagnosis. UCSF Medical Center. http://www.ucsfhealth.org/conditions/frontotemporal_ dementia/diagnosis.html. Accessed April 24, 2014.
7. McMurtray AM, Chen AK, Shapira JS, et al. Variations in regional SPECT hypoperfusion and clinical features in frontotemporal dementia. Neurology. 2006;66(4):517-522.
8. Miller BL, Lee SE. Frontotemporal dementia: treatment. Up To Date. http://www.uptodate.com/contents/frontotemporal-dementia-treatment?source=search_result&search=frontote mporal+dementia+treatment&selectedTitle=1~150. Updated December 30, 2013. Accessed April 24, 2014.
1. Snowden JS, Neary D, Mann DM. Frontotemporal dementia. Br J Psychiatry. 2002;180:140-143.
2. Frontotemporal degeneration. The Association for Frontotemporal Degeneration. http://www.theaftd.org/ frontotemporal-degeneration/ftd-overview. Accessed April 24, 2014.
3. Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51(6):1546-1554.
4. Clark CM, Forman MS. Frontotemporal lobar degeneration with motor neuron disease: a clinical and pathological spectrum. Arch Neurol. 2006;63(4):489-490.
5. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:614-618.
6. Frontotemporal dementia diagnosis. UCSF Medical Center. http://www.ucsfhealth.org/conditions/frontotemporal_ dementia/diagnosis.html. Accessed April 24, 2014.
7. McMurtray AM, Chen AK, Shapira JS, et al. Variations in regional SPECT hypoperfusion and clinical features in frontotemporal dementia. Neurology. 2006;66(4):517-522.
8. Miller BL, Lee SE. Frontotemporal dementia: treatment. Up To Date. http://www.uptodate.com/contents/frontotemporal-dementia-treatment?source=search_result&search=frontote mporal+dementia+treatment&selectedTitle=1~150. Updated December 30, 2013. Accessed April 24, 2014.
Clozapine: Talking about risks, benefits, and alternatives with patients
Clozapine is a life-saving medication for many patients with schizophrenia, including those who have a schizophrenia spectrum disorder with suicidality or treatment-resistant disease, but clinicians’ discomfort with managing its risk profile has led to it being underutilized. Clinicians who are prepared to discuss the risks and benefits of clozapine—and alternatives, including no treatment—with patients may encounter less reluctance when they recommend a time-limited trial of the drug.
Risks
Clinicians need to be aware of both 1) serious adverse effects that can occur when clozapine needs to be interrupted or discontinued (Table)1 and 2) common side effects associated with continued use that can be managed without stopping the drug.2 Common side effects that patients may experience as treatment is initiated include sedation, orthostatic hypotension, constipation, drooling, tachycardia, and metabolic side effects such as weight gain, diabetes, and hyperlipidemia, which are problematic in the long term.
Reassure patients that frequent monitoring of metabolic metrics (including baseline HbA1C, lipid panel, waist circumference, and body mass index, as well as weight monitoring at each visit and metabolic laboratory monitoring every 3 to 6 months thereafter) should be expected, along with early intervention (eg, adding metformin) as appropriate. Constipation is common and can lead to serious, large bowel ileus. Ask about drooling, which can be treated by reducing the dosage or adding glycopyrrolate.
Extrapyramidal symptoms (EPS) including parkinsonism, dystonia, akathisia are uncommon (clozapine was the first “atypical” antipsychotic for this reason), but neuroleptic malignant syndrome (NMS) can occur. Although tardive dyskinesia (TD) is a small risk, clozapine will improve established TD in many patients once they are switched to clozapine. Blood dyscrasias include granulocytopenia and the rare risk of agranulocytosis which are monitored by means of a prescribing registry. Myocarditis and pancreatitis are likely idiosyncratic immune-related side effects that are unique to clozapine among antipsychotics. Other dangerous side effects include a dosage-related risk of seizure, severe hyperglycemia, and diabetic ketoacidosis.
Benefits
Clozapine is FDA-approved for treatment-resistant schizophrenia and for schizophrenia spectrum disorders with recurrent suicidality. Clozapine can be the best antipsychotic for patients who are sensitive to EPS and for those with TD. Antipsychotic efficacy often can be determined in a 2 to 3 month time-limited trial, although, in practice, you might need to wait 6 to 12 months to observe how well clozapine’s benefits have accrued.
Alternatives
Not using the most effective antipsychotic, or using no antipsychotic when one is indicated, often results in unstable psychiatric illness, which increases the risk of adverse outcomes (eg, suicide, accidents). Unstable psychiatric disease also complicates treatment of medical problems. An 11-year follow-up study in Finland of patients with schizophrenia showed a lower all-cause mortality with clozapine than with other antipsychotics, all of which collectively were associated with lower mortality compared with no antipsychotic use.3 Clozapine also is associated with the lowest discontinuation rate of any antipsychotic, which suggests that patients perceive its risk-benefit ratio favorably. Last, patients who might benefit from clozapine, but do not receive it, often will receive polypharmacy, which poses its own risks.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Nielsen J, Correll CU, Manu P, et al. Termination of clozapine treatment due to medical reasons: when is it warranted and how can it be avoided? J Clin Psychiatry. 2013;74(6): 603-613.
2. Goldberg JF, Ernst CL. Managing the side effects of psychotropic medications. Arlington, VA: American Psychiatric Publishing; 2012.
3. Tiihonen J, Löngqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009; 374(9690):620-627.
Clozapine is a life-saving medication for many patients with schizophrenia, including those who have a schizophrenia spectrum disorder with suicidality or treatment-resistant disease, but clinicians’ discomfort with managing its risk profile has led to it being underutilized. Clinicians who are prepared to discuss the risks and benefits of clozapine—and alternatives, including no treatment—with patients may encounter less reluctance when they recommend a time-limited trial of the drug.
Risks
Clinicians need to be aware of both 1) serious adverse effects that can occur when clozapine needs to be interrupted or discontinued (Table)1 and 2) common side effects associated with continued use that can be managed without stopping the drug.2 Common side effects that patients may experience as treatment is initiated include sedation, orthostatic hypotension, constipation, drooling, tachycardia, and metabolic side effects such as weight gain, diabetes, and hyperlipidemia, which are problematic in the long term.
Reassure patients that frequent monitoring of metabolic metrics (including baseline HbA1C, lipid panel, waist circumference, and body mass index, as well as weight monitoring at each visit and metabolic laboratory monitoring every 3 to 6 months thereafter) should be expected, along with early intervention (eg, adding metformin) as appropriate. Constipation is common and can lead to serious, large bowel ileus. Ask about drooling, which can be treated by reducing the dosage or adding glycopyrrolate.
Extrapyramidal symptoms (EPS) including parkinsonism, dystonia, akathisia are uncommon (clozapine was the first “atypical” antipsychotic for this reason), but neuroleptic malignant syndrome (NMS) can occur. Although tardive dyskinesia (TD) is a small risk, clozapine will improve established TD in many patients once they are switched to clozapine. Blood dyscrasias include granulocytopenia and the rare risk of agranulocytosis which are monitored by means of a prescribing registry. Myocarditis and pancreatitis are likely idiosyncratic immune-related side effects that are unique to clozapine among antipsychotics. Other dangerous side effects include a dosage-related risk of seizure, severe hyperglycemia, and diabetic ketoacidosis.
Benefits
Clozapine is FDA-approved for treatment-resistant schizophrenia and for schizophrenia spectrum disorders with recurrent suicidality. Clozapine can be the best antipsychotic for patients who are sensitive to EPS and for those with TD. Antipsychotic efficacy often can be determined in a 2 to 3 month time-limited trial, although, in practice, you might need to wait 6 to 12 months to observe how well clozapine’s benefits have accrued.
Alternatives
Not using the most effective antipsychotic, or using no antipsychotic when one is indicated, often results in unstable psychiatric illness, which increases the risk of adverse outcomes (eg, suicide, accidents). Unstable psychiatric disease also complicates treatment of medical problems. An 11-year follow-up study in Finland of patients with schizophrenia showed a lower all-cause mortality with clozapine than with other antipsychotics, all of which collectively were associated with lower mortality compared with no antipsychotic use.3 Clozapine also is associated with the lowest discontinuation rate of any antipsychotic, which suggests that patients perceive its risk-benefit ratio favorably. Last, patients who might benefit from clozapine, but do not receive it, often will receive polypharmacy, which poses its own risks.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Clozapine is a life-saving medication for many patients with schizophrenia, including those who have a schizophrenia spectrum disorder with suicidality or treatment-resistant disease, but clinicians’ discomfort with managing its risk profile has led to it being underutilized. Clinicians who are prepared to discuss the risks and benefits of clozapine—and alternatives, including no treatment—with patients may encounter less reluctance when they recommend a time-limited trial of the drug.
Risks
Clinicians need to be aware of both 1) serious adverse effects that can occur when clozapine needs to be interrupted or discontinued (Table)1 and 2) common side effects associated with continued use that can be managed without stopping the drug.2 Common side effects that patients may experience as treatment is initiated include sedation, orthostatic hypotension, constipation, drooling, tachycardia, and metabolic side effects such as weight gain, diabetes, and hyperlipidemia, which are problematic in the long term.
Reassure patients that frequent monitoring of metabolic metrics (including baseline HbA1C, lipid panel, waist circumference, and body mass index, as well as weight monitoring at each visit and metabolic laboratory monitoring every 3 to 6 months thereafter) should be expected, along with early intervention (eg, adding metformin) as appropriate. Constipation is common and can lead to serious, large bowel ileus. Ask about drooling, which can be treated by reducing the dosage or adding glycopyrrolate.
Extrapyramidal symptoms (EPS) including parkinsonism, dystonia, akathisia are uncommon (clozapine was the first “atypical” antipsychotic for this reason), but neuroleptic malignant syndrome (NMS) can occur. Although tardive dyskinesia (TD) is a small risk, clozapine will improve established TD in many patients once they are switched to clozapine. Blood dyscrasias include granulocytopenia and the rare risk of agranulocytosis which are monitored by means of a prescribing registry. Myocarditis and pancreatitis are likely idiosyncratic immune-related side effects that are unique to clozapine among antipsychotics. Other dangerous side effects include a dosage-related risk of seizure, severe hyperglycemia, and diabetic ketoacidosis.
Benefits
Clozapine is FDA-approved for treatment-resistant schizophrenia and for schizophrenia spectrum disorders with recurrent suicidality. Clozapine can be the best antipsychotic for patients who are sensitive to EPS and for those with TD. Antipsychotic efficacy often can be determined in a 2 to 3 month time-limited trial, although, in practice, you might need to wait 6 to 12 months to observe how well clozapine’s benefits have accrued.
Alternatives
Not using the most effective antipsychotic, or using no antipsychotic when one is indicated, often results in unstable psychiatric illness, which increases the risk of adverse outcomes (eg, suicide, accidents). Unstable psychiatric disease also complicates treatment of medical problems. An 11-year follow-up study in Finland of patients with schizophrenia showed a lower all-cause mortality with clozapine than with other antipsychotics, all of which collectively were associated with lower mortality compared with no antipsychotic use.3 Clozapine also is associated with the lowest discontinuation rate of any antipsychotic, which suggests that patients perceive its risk-benefit ratio favorably. Last, patients who might benefit from clozapine, but do not receive it, often will receive polypharmacy, which poses its own risks.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Nielsen J, Correll CU, Manu P, et al. Termination of clozapine treatment due to medical reasons: when is it warranted and how can it be avoided? J Clin Psychiatry. 2013;74(6): 603-613.
2. Goldberg JF, Ernst CL. Managing the side effects of psychotropic medications. Arlington, VA: American Psychiatric Publishing; 2012.
3. Tiihonen J, Löngqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009; 374(9690):620-627.
1. Nielsen J, Correll CU, Manu P, et al. Termination of clozapine treatment due to medical reasons: when is it warranted and how can it be avoided? J Clin Psychiatry. 2013;74(6): 603-613.
2. Goldberg JF, Ernst CL. Managing the side effects of psychotropic medications. Arlington, VA: American Psychiatric Publishing; 2012.
3. Tiihonen J, Löngqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009; 374(9690):620-627.
Pills to powder: A clinician’s reference for crushable psychotropic medications
Many patients experience difficulty swallowing pills, for various reasons:
• discomfort (particularly pediatric and geriatric patients)
• postsurgical need for an alternate route of enteral intake (nasogastric tube, gastrostomy, jejunostomy)
• dysphagia due to a neurologic disorder (multiple sclerosis, impaired gag reflex, dementing processes)
• odynophagia (pain upon swallowing) due to gastroesophageal reflux or a structural abnormality
• a structural abnormality of the head or neck that impairs swallowing.1
If these difficulties are not addressed, they can interfere with medication adherence. In those instances, using an alternative dosage form or manipulating an available formulation might be required.
Crushing guidelines
There are limited data on crushed-form products and their impact on efficacy. Therefore, when patients have difficulty taking pills, switching to liquid solution or orally disintegrating forms is recommended. However, most psychotropics are available only as tablets or capsules. Patients can crush their pills immediately before administration for easier intake. The following are some general guidelines for doing so:2
• Scored tablets typically can be crushed.
• Crushing sublingual and buccal tablets can alter their effectiveness.
• Crushing sustained-release medications can eliminate the sustained-release action.3
• Enteric-coated medications should not be crushed, because this can alter drug absorption.
• Capsules can generally be opened to administer powdered contents, unless the capsule has time-release properties or an enteric coating.
The accompanying Table, organized by drug class, indicates whether a drug can be crushed to a powdered form, which usually is mixed with food or liquid for easier intake. The Table also lists liquid and orally disintegrating forms available, and other routes, including injectable immediate and long-acting formulations. Helping patients find a medication formulation that suits their needs strengthens adherence and the therapeutic relationship.
1. Schiele JT, Quinzler R, Klimm HD, et al. Difficulties swallowing solid oral dosage forms in a general practice population: prevalence, causes, and relationship to dosage forms. Eur J Clin Pharmacol. 2013;69(4): 937-948.
2. PL Detail-Document, Meds That Should Not Be Crushed. Pharmacist’s Letter/Prescriber’s Letter. July 2012.
3. Mitchell JF. Oral dosage forms that should not be crushed. http://www.ismp. org/tools/donotcrush.pdf. Updated January 2014. Accessed March 13, 2014.
Many patients experience difficulty swallowing pills, for various reasons:
• discomfort (particularly pediatric and geriatric patients)
• postsurgical need for an alternate route of enteral intake (nasogastric tube, gastrostomy, jejunostomy)
• dysphagia due to a neurologic disorder (multiple sclerosis, impaired gag reflex, dementing processes)
• odynophagia (pain upon swallowing) due to gastroesophageal reflux or a structural abnormality
• a structural abnormality of the head or neck that impairs swallowing.1
If these difficulties are not addressed, they can interfere with medication adherence. In those instances, using an alternative dosage form or manipulating an available formulation might be required.
Crushing guidelines
There are limited data on crushed-form products and their impact on efficacy. Therefore, when patients have difficulty taking pills, switching to liquid solution or orally disintegrating forms is recommended. However, most psychotropics are available only as tablets or capsules. Patients can crush their pills immediately before administration for easier intake. The following are some general guidelines for doing so:2
• Scored tablets typically can be crushed.
• Crushing sublingual and buccal tablets can alter their effectiveness.
• Crushing sustained-release medications can eliminate the sustained-release action.3
• Enteric-coated medications should not be crushed, because this can alter drug absorption.
• Capsules can generally be opened to administer powdered contents, unless the capsule has time-release properties or an enteric coating.
The accompanying Table, organized by drug class, indicates whether a drug can be crushed to a powdered form, which usually is mixed with food or liquid for easier intake. The Table also lists liquid and orally disintegrating forms available, and other routes, including injectable immediate and long-acting formulations. Helping patients find a medication formulation that suits their needs strengthens adherence and the therapeutic relationship.
Many patients experience difficulty swallowing pills, for various reasons:
• discomfort (particularly pediatric and geriatric patients)
• postsurgical need for an alternate route of enteral intake (nasogastric tube, gastrostomy, jejunostomy)
• dysphagia due to a neurologic disorder (multiple sclerosis, impaired gag reflex, dementing processes)
• odynophagia (pain upon swallowing) due to gastroesophageal reflux or a structural abnormality
• a structural abnormality of the head or neck that impairs swallowing.1
If these difficulties are not addressed, they can interfere with medication adherence. In those instances, using an alternative dosage form or manipulating an available formulation might be required.
Crushing guidelines
There are limited data on crushed-form products and their impact on efficacy. Therefore, when patients have difficulty taking pills, switching to liquid solution or orally disintegrating forms is recommended. However, most psychotropics are available only as tablets or capsules. Patients can crush their pills immediately before administration for easier intake. The following are some general guidelines for doing so:2
• Scored tablets typically can be crushed.
• Crushing sublingual and buccal tablets can alter their effectiveness.
• Crushing sustained-release medications can eliminate the sustained-release action.3
• Enteric-coated medications should not be crushed, because this can alter drug absorption.
• Capsules can generally be opened to administer powdered contents, unless the capsule has time-release properties or an enteric coating.
The accompanying Table, organized by drug class, indicates whether a drug can be crushed to a powdered form, which usually is mixed with food or liquid for easier intake. The Table also lists liquid and orally disintegrating forms available, and other routes, including injectable immediate and long-acting formulations. Helping patients find a medication formulation that suits their needs strengthens adherence and the therapeutic relationship.
1. Schiele JT, Quinzler R, Klimm HD, et al. Difficulties swallowing solid oral dosage forms in a general practice population: prevalence, causes, and relationship to dosage forms. Eur J Clin Pharmacol. 2013;69(4): 937-948.
2. PL Detail-Document, Meds That Should Not Be Crushed. Pharmacist’s Letter/Prescriber’s Letter. July 2012.
3. Mitchell JF. Oral dosage forms that should not be crushed. http://www.ismp. org/tools/donotcrush.pdf. Updated January 2014. Accessed March 13, 2014.
1. Schiele JT, Quinzler R, Klimm HD, et al. Difficulties swallowing solid oral dosage forms in a general practice population: prevalence, causes, and relationship to dosage forms. Eur J Clin Pharmacol. 2013;69(4): 937-948.
2. PL Detail-Document, Meds That Should Not Be Crushed. Pharmacist’s Letter/Prescriber’s Letter. July 2012.
3. Mitchell JF. Oral dosage forms that should not be crushed. http://www.ismp. org/tools/donotcrush.pdf. Updated January 2014. Accessed March 13, 2014.