User login
Times change, but children still come first
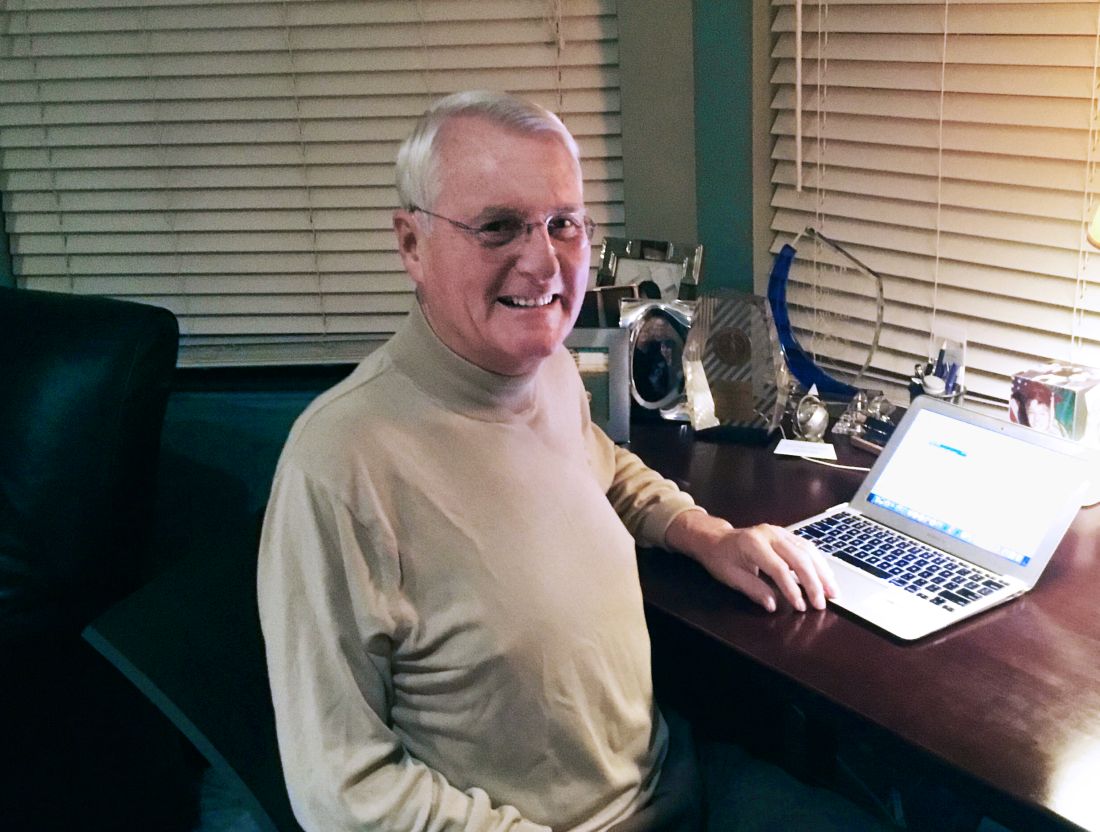
After decades of pediatric practice, Thomas K. McInerny, MD, still accentuates the positive. “I decided to become a pediatrician in my third year of medical school after my pediatrics rotation. I loved working with the children and their families so full of joy and hope,” he said. “I still feel that pediatrics is the greatest profession despite some frustrations with rules, regulations, and computer work.”
Many childhood diseases, including birth defects and forms of cancer that were fatal 50 years ago, now can be treated successfully, he noted. “However, there are more children with emotional, behavioral, and school problems, which pediatricians are now treating as there is a great shortage of mental health professionals for children.”
Although the dedication of pediatricians to their specialty has remained strong over the past 50 years, their work environment has evolved in many ways.
David T. Tayloe Jr., MD, also a past president of the AAP, currently practices in Goldsboro, N.C. When he established a solo community practice in 1977, he was one of a few pediatricians in the area, and he was busy. “I was the only pediatrician who could take care of really sick newborns and hospital patients, so I basically was available 24-7 for those first 2 years; there were two older pediatricians in town, and they took routine night call with me, giving me some time with my family,” he said. “With 1,500 deliveries a year at our hospital, there were always sick babies who needed my services. My office hours were 9 a.m. until 5 p.m. but often, in the cooler months, we saw patients until 8 p.m.” These days, Dr. Tayloe said he works 3-4 days in the office, and “my practice is largely behavioral health, school problems, obesity, asthma, and well-baby/child care.”
“In the last 20 years, my typical work day has changed in many ways,” said Julia Richerson, MD, who practices at the Family Health Center Iroquois office in South Louisville, Ky.
“I use electronic resources to find patient education, to look up current treatments, and research complicated diagnosis,” she noted.
“I feel that having the computer in the room isn’t a barrier to communication with my patients and families. Using the EHR doesn’t take me more time to see a patient,” she said. “However, the review of consult and ER records is harder and takes longer to complete. Consult, ER, and other outside records are much larger with the key clinical data more disorganized and harder to find among the pages and pages of nonrelevant content. This makes the workday much longer.”
The conditions that take up most of a pediatric office visit have changed as well, and include more complex medical, behavioral, and social issues, Dr. Richerson observed. “Obesity, ADHD, autism, complications of prematurity, behavioral health issues, developmental delays, and asthma are commonly seen in practice now. One in five children nationally have a chronic illness or special health care need. And we strive to help ease the challenges for families struggling with economic insecurity, and children growing up experiencing significant adversities.”
The office and the EHR
EHRs are a fact of life in all specialties today, but should not get in the way of interacting with patients, Dr. McInerny said. Many pediatricians complete their medical records after hours at home because they don’t have time to complete them in the office.
“I would advise the younger pediatricians to be sure to look at and interact with their families as much as possible while working on the computer, and showing the families entries and graphs from the computer. We were able to interact with families much more easily when writing out notes with pen and paper,” he said.
In his early years of practice, Dr. Tayloe recalled, “I spent less time with each patient; my focus was infectious disease, and I treated many patients with what today are vaccine-preventable diseases. I could see patients much faster with paper charts, but my documentation left much to be desired,” he said. “With the electronic record, I spend more time with each patient, but I type really fast and finish my charts in the exam rooms with the patients.”
“EHRs have made daily practice easier and more complicated for pediatricians,” said Dr. Richerson. “In the moment-to-moment use of EHRs while seeing patients, we can fairly quickly document the information we need to for patient care.” However, she said, “It takes some additional time to document all the data points required for quality- and value-based reimbursement programs, and it takes a significant amount of additional time in most EHRs to retrieve relevant information because you cannot query the system for clinical content on a patient. Also, reviewing incoming records is difficult because the information is voluminous and poorly organized,” she noted. “There are so many opportunities for improvement, and hopefully 20 years from now we will have EHRs that significantly improve quality and safety of patient care.”
Money and malpractice
The Vaccines for Children program led to an increase in incomes for pediatricians in the United States after 1994, according to Dr. Tayloe. “We began to be paid by insurance companies for most of what we do during the mid-90s and that boosted revenues,” he said. However, “On the flip side, we are now at the mercy of private payers, and must participate in all their very burdensome quality improvement/assurance programs if we are to be paid fairly. Our incomes were pretty flat over the last 5-10 years, especially for practices that participate fully in Medicaid/CHIP.”
Over the past 50 years, malpractice claims against pediatricians have remained consistently among the lowest for any medical specialty, according to Paul Greve, JD, a registered professional liability underwriter and executive vice president and senior consultant at Willis Towers Watson Health Care Practice.
The impact of EHRs on pediatric practice from a legal standpoint depends on the format of the EHR itself, Mr. Greve said. “Many of the EHRs that are designed for physicians, particularly the ones used in acute care settings, don’t allow the doctor to really highlight their thinking as they work through the diagnostic process, and that is very important in the defense of a malpractice case against a pediatrician,” he said.
“The pediatrician doesn’t have to be correct all the time, but it is important for the lawyers defending the case to see what the pediatrician’s thought process was. If the EHR allows for capturing the doctor’s thought process, that’s a well-designed EHR, and that’s critical,” he emphasized.
Diagnostic error is one of the most entrenched problems in medical malpractice, said Mr. Greve. Failure to diagnose and delay in diagnosis remain the most common allegations against pediatricians, he noted. Also, being aware of the environment is important to risk management in the office.
“The American Academy of Pediatrics has excellent publications on safety and risk management that all pediatricians should be aware of,” he said.
Inspiration and intangibles
“I think the changes that we are starting to see will continue to evolve over the next 50 years,” said Dr. Richerson. “Increased medical and social complexity of patients, changes in health technology, EHRs, personal health data monitoring, and continued changes in value based payment methods will be key.
“I hope that we gain, as a health delivery system, an appreciation of the impact of child health on adult health. Long-term adult health outcomes depend on improved child health outcomes. Investing in diseases like childhood obesity, mental health, and developmental issues, to name a few, will have a bigger impact on adult disease than any adult interventions,” she said. And really dealing with the impact of childhood adversity in health care and in the community and nationally in general is critical. This requires grassroots interventions to support families as well as local, state, and national policy. It also requires payment for health care services for the needed interventions in the office and hospital. Providing comprehensive medical care and addressing the medical and social complexities of child health in an effective, compassionate, and family-centered way takes time. It’s not easy, but it’s not impossible. But it requires more resources than are currently given to child health care. Adult medicine is accustomed to paying for disease managers for diabetes or care coordinators for heart failure. This is not the current state of delivery for children’s care and it should be. These are some of the major issues confronting pediatricians.
What has remained the same in pediatrics is the love the doctors have for their work, and the reflections of veteran clinicians on the intangible rewards of the practice may inspire the next generation.
Dr. Tayloe said that he chose pediatrics because “I was really intrigued by the skills necessary to care for sick newborns, including premature babies. I wanted to practice in a remote location where I could use all the skills I developed during residency, and be of significant value to the community.” Two of his four adult children were similarly inspired and followed in his footsteps.
“For pediatricians, helping families raise healthy children is a real privilege and very satisfying,” Dr. McInerny said.
After decades of pediatric practice, Thomas K. McInerny, MD, still accentuates the positive. “I decided to become a pediatrician in my third year of medical school after my pediatrics rotation. I loved working with the children and their families so full of joy and hope,” he said. “I still feel that pediatrics is the greatest profession despite some frustrations with rules, regulations, and computer work.”
Many childhood diseases, including birth defects and forms of cancer that were fatal 50 years ago, now can be treated successfully, he noted. “However, there are more children with emotional, behavioral, and school problems, which pediatricians are now treating as there is a great shortage of mental health professionals for children.”
Although the dedication of pediatricians to their specialty has remained strong over the past 50 years, their work environment has evolved in many ways.
David T. Tayloe Jr., MD, also a past president of the AAP, currently practices in Goldsboro, N.C. When he established a solo community practice in 1977, he was one of a few pediatricians in the area, and he was busy. “I was the only pediatrician who could take care of really sick newborns and hospital patients, so I basically was available 24-7 for those first 2 years; there were two older pediatricians in town, and they took routine night call with me, giving me some time with my family,” he said. “With 1,500 deliveries a year at our hospital, there were always sick babies who needed my services. My office hours were 9 a.m. until 5 p.m. but often, in the cooler months, we saw patients until 8 p.m.” These days, Dr. Tayloe said he works 3-4 days in the office, and “my practice is largely behavioral health, school problems, obesity, asthma, and well-baby/child care.”
“In the last 20 years, my typical work day has changed in many ways,” said Julia Richerson, MD, who practices at the Family Health Center Iroquois office in South Louisville, Ky.
“I use electronic resources to find patient education, to look up current treatments, and research complicated diagnosis,” she noted.
“I feel that having the computer in the room isn’t a barrier to communication with my patients and families. Using the EHR doesn’t take me more time to see a patient,” she said. “However, the review of consult and ER records is harder and takes longer to complete. Consult, ER, and other outside records are much larger with the key clinical data more disorganized and harder to find among the pages and pages of nonrelevant content. This makes the workday much longer.”
The conditions that take up most of a pediatric office visit have changed as well, and include more complex medical, behavioral, and social issues, Dr. Richerson observed. “Obesity, ADHD, autism, complications of prematurity, behavioral health issues, developmental delays, and asthma are commonly seen in practice now. One in five children nationally have a chronic illness or special health care need. And we strive to help ease the challenges for families struggling with economic insecurity, and children growing up experiencing significant adversities.”
The office and the EHR
EHRs are a fact of life in all specialties today, but should not get in the way of interacting with patients, Dr. McInerny said. Many pediatricians complete their medical records after hours at home because they don’t have time to complete them in the office.
“I would advise the younger pediatricians to be sure to look at and interact with their families as much as possible while working on the computer, and showing the families entries and graphs from the computer. We were able to interact with families much more easily when writing out notes with pen and paper,” he said.
In his early years of practice, Dr. Tayloe recalled, “I spent less time with each patient; my focus was infectious disease, and I treated many patients with what today are vaccine-preventable diseases. I could see patients much faster with paper charts, but my documentation left much to be desired,” he said. “With the electronic record, I spend more time with each patient, but I type really fast and finish my charts in the exam rooms with the patients.”
“EHRs have made daily practice easier and more complicated for pediatricians,” said Dr. Richerson. “In the moment-to-moment use of EHRs while seeing patients, we can fairly quickly document the information we need to for patient care.” However, she said, “It takes some additional time to document all the data points required for quality- and value-based reimbursement programs, and it takes a significant amount of additional time in most EHRs to retrieve relevant information because you cannot query the system for clinical content on a patient. Also, reviewing incoming records is difficult because the information is voluminous and poorly organized,” she noted. “There are so many opportunities for improvement, and hopefully 20 years from now we will have EHRs that significantly improve quality and safety of patient care.”
Money and malpractice
The Vaccines for Children program led to an increase in incomes for pediatricians in the United States after 1994, according to Dr. Tayloe. “We began to be paid by insurance companies for most of what we do during the mid-90s and that boosted revenues,” he said. However, “On the flip side, we are now at the mercy of private payers, and must participate in all their very burdensome quality improvement/assurance programs if we are to be paid fairly. Our incomes were pretty flat over the last 5-10 years, especially for practices that participate fully in Medicaid/CHIP.”
Over the past 50 years, malpractice claims against pediatricians have remained consistently among the lowest for any medical specialty, according to Paul Greve, JD, a registered professional liability underwriter and executive vice president and senior consultant at Willis Towers Watson Health Care Practice.
The impact of EHRs on pediatric practice from a legal standpoint depends on the format of the EHR itself, Mr. Greve said. “Many of the EHRs that are designed for physicians, particularly the ones used in acute care settings, don’t allow the doctor to really highlight their thinking as they work through the diagnostic process, and that is very important in the defense of a malpractice case against a pediatrician,” he said.
“The pediatrician doesn’t have to be correct all the time, but it is important for the lawyers defending the case to see what the pediatrician’s thought process was. If the EHR allows for capturing the doctor’s thought process, that’s a well-designed EHR, and that’s critical,” he emphasized.
Diagnostic error is one of the most entrenched problems in medical malpractice, said Mr. Greve. Failure to diagnose and delay in diagnosis remain the most common allegations against pediatricians, he noted. Also, being aware of the environment is important to risk management in the office.
“The American Academy of Pediatrics has excellent publications on safety and risk management that all pediatricians should be aware of,” he said.
Inspiration and intangibles
“I think the changes that we are starting to see will continue to evolve over the next 50 years,” said Dr. Richerson. “Increased medical and social complexity of patients, changes in health technology, EHRs, personal health data monitoring, and continued changes in value based payment methods will be key.
“I hope that we gain, as a health delivery system, an appreciation of the impact of child health on adult health. Long-term adult health outcomes depend on improved child health outcomes. Investing in diseases like childhood obesity, mental health, and developmental issues, to name a few, will have a bigger impact on adult disease than any adult interventions,” she said. And really dealing with the impact of childhood adversity in health care and in the community and nationally in general is critical. This requires grassroots interventions to support families as well as local, state, and national policy. It also requires payment for health care services for the needed interventions in the office and hospital. Providing comprehensive medical care and addressing the medical and social complexities of child health in an effective, compassionate, and family-centered way takes time. It’s not easy, but it’s not impossible. But it requires more resources than are currently given to child health care. Adult medicine is accustomed to paying for disease managers for diabetes or care coordinators for heart failure. This is not the current state of delivery for children’s care and it should be. These are some of the major issues confronting pediatricians.
What has remained the same in pediatrics is the love the doctors have for their work, and the reflections of veteran clinicians on the intangible rewards of the practice may inspire the next generation.
Dr. Tayloe said that he chose pediatrics because “I was really intrigued by the skills necessary to care for sick newborns, including premature babies. I wanted to practice in a remote location where I could use all the skills I developed during residency, and be of significant value to the community.” Two of his four adult children were similarly inspired and followed in his footsteps.
“For pediatricians, helping families raise healthy children is a real privilege and very satisfying,” Dr. McInerny said.
After decades of pediatric practice, Thomas K. McInerny, MD, still accentuates the positive. “I decided to become a pediatrician in my third year of medical school after my pediatrics rotation. I loved working with the children and their families so full of joy and hope,” he said. “I still feel that pediatrics is the greatest profession despite some frustrations with rules, regulations, and computer work.”
Many childhood diseases, including birth defects and forms of cancer that were fatal 50 years ago, now can be treated successfully, he noted. “However, there are more children with emotional, behavioral, and school problems, which pediatricians are now treating as there is a great shortage of mental health professionals for children.”
Although the dedication of pediatricians to their specialty has remained strong over the past 50 years, their work environment has evolved in many ways.
David T. Tayloe Jr., MD, also a past president of the AAP, currently practices in Goldsboro, N.C. When he established a solo community practice in 1977, he was one of a few pediatricians in the area, and he was busy. “I was the only pediatrician who could take care of really sick newborns and hospital patients, so I basically was available 24-7 for those first 2 years; there were two older pediatricians in town, and they took routine night call with me, giving me some time with my family,” he said. “With 1,500 deliveries a year at our hospital, there were always sick babies who needed my services. My office hours were 9 a.m. until 5 p.m. but often, in the cooler months, we saw patients until 8 p.m.” These days, Dr. Tayloe said he works 3-4 days in the office, and “my practice is largely behavioral health, school problems, obesity, asthma, and well-baby/child care.”
“In the last 20 years, my typical work day has changed in many ways,” said Julia Richerson, MD, who practices at the Family Health Center Iroquois office in South Louisville, Ky.
“I use electronic resources to find patient education, to look up current treatments, and research complicated diagnosis,” she noted.
“I feel that having the computer in the room isn’t a barrier to communication with my patients and families. Using the EHR doesn’t take me more time to see a patient,” she said. “However, the review of consult and ER records is harder and takes longer to complete. Consult, ER, and other outside records are much larger with the key clinical data more disorganized and harder to find among the pages and pages of nonrelevant content. This makes the workday much longer.”
The conditions that take up most of a pediatric office visit have changed as well, and include more complex medical, behavioral, and social issues, Dr. Richerson observed. “Obesity, ADHD, autism, complications of prematurity, behavioral health issues, developmental delays, and asthma are commonly seen in practice now. One in five children nationally have a chronic illness or special health care need. And we strive to help ease the challenges for families struggling with economic insecurity, and children growing up experiencing significant adversities.”
The office and the EHR
EHRs are a fact of life in all specialties today, but should not get in the way of interacting with patients, Dr. McInerny said. Many pediatricians complete their medical records after hours at home because they don’t have time to complete them in the office.
“I would advise the younger pediatricians to be sure to look at and interact with their families as much as possible while working on the computer, and showing the families entries and graphs from the computer. We were able to interact with families much more easily when writing out notes with pen and paper,” he said.
In his early years of practice, Dr. Tayloe recalled, “I spent less time with each patient; my focus was infectious disease, and I treated many patients with what today are vaccine-preventable diseases. I could see patients much faster with paper charts, but my documentation left much to be desired,” he said. “With the electronic record, I spend more time with each patient, but I type really fast and finish my charts in the exam rooms with the patients.”
“EHRs have made daily practice easier and more complicated for pediatricians,” said Dr. Richerson. “In the moment-to-moment use of EHRs while seeing patients, we can fairly quickly document the information we need to for patient care.” However, she said, “It takes some additional time to document all the data points required for quality- and value-based reimbursement programs, and it takes a significant amount of additional time in most EHRs to retrieve relevant information because you cannot query the system for clinical content on a patient. Also, reviewing incoming records is difficult because the information is voluminous and poorly organized,” she noted. “There are so many opportunities for improvement, and hopefully 20 years from now we will have EHRs that significantly improve quality and safety of patient care.”
Money and malpractice
The Vaccines for Children program led to an increase in incomes for pediatricians in the United States after 1994, according to Dr. Tayloe. “We began to be paid by insurance companies for most of what we do during the mid-90s and that boosted revenues,” he said. However, “On the flip side, we are now at the mercy of private payers, and must participate in all their very burdensome quality improvement/assurance programs if we are to be paid fairly. Our incomes were pretty flat over the last 5-10 years, especially for practices that participate fully in Medicaid/CHIP.”
Over the past 50 years, malpractice claims against pediatricians have remained consistently among the lowest for any medical specialty, according to Paul Greve, JD, a registered professional liability underwriter and executive vice president and senior consultant at Willis Towers Watson Health Care Practice.
The impact of EHRs on pediatric practice from a legal standpoint depends on the format of the EHR itself, Mr. Greve said. “Many of the EHRs that are designed for physicians, particularly the ones used in acute care settings, don’t allow the doctor to really highlight their thinking as they work through the diagnostic process, and that is very important in the defense of a malpractice case against a pediatrician,” he said.
“The pediatrician doesn’t have to be correct all the time, but it is important for the lawyers defending the case to see what the pediatrician’s thought process was. If the EHR allows for capturing the doctor’s thought process, that’s a well-designed EHR, and that’s critical,” he emphasized.
Diagnostic error is one of the most entrenched problems in medical malpractice, said Mr. Greve. Failure to diagnose and delay in diagnosis remain the most common allegations against pediatricians, he noted. Also, being aware of the environment is important to risk management in the office.
“The American Academy of Pediatrics has excellent publications on safety and risk management that all pediatricians should be aware of,” he said.
Inspiration and intangibles
“I think the changes that we are starting to see will continue to evolve over the next 50 years,” said Dr. Richerson. “Increased medical and social complexity of patients, changes in health technology, EHRs, personal health data monitoring, and continued changes in value based payment methods will be key.
“I hope that we gain, as a health delivery system, an appreciation of the impact of child health on adult health. Long-term adult health outcomes depend on improved child health outcomes. Investing in diseases like childhood obesity, mental health, and developmental issues, to name a few, will have a bigger impact on adult disease than any adult interventions,” she said. And really dealing with the impact of childhood adversity in health care and in the community and nationally in general is critical. This requires grassroots interventions to support families as well as local, state, and national policy. It also requires payment for health care services for the needed interventions in the office and hospital. Providing comprehensive medical care and addressing the medical and social complexities of child health in an effective, compassionate, and family-centered way takes time. It’s not easy, but it’s not impossible. But it requires more resources than are currently given to child health care. Adult medicine is accustomed to paying for disease managers for diabetes or care coordinators for heart failure. This is not the current state of delivery for children’s care and it should be. These are some of the major issues confronting pediatricians.
What has remained the same in pediatrics is the love the doctors have for their work, and the reflections of veteran clinicians on the intangible rewards of the practice may inspire the next generation.
Dr. Tayloe said that he chose pediatrics because “I was really intrigued by the skills necessary to care for sick newborns, including premature babies. I wanted to practice in a remote location where I could use all the skills I developed during residency, and be of significant value to the community.” Two of his four adult children were similarly inspired and followed in his footsteps.
“For pediatricians, helping families raise healthy children is a real privilege and very satisfying,” Dr. McInerny said.
Group B streptococcus
It once was a very a common scenario. A baby born at term looks fine for the first 24 hours of life. Without much warning, the infant develops grunting, tachypnea, and tachycardia. Sepsis is suspected, and within a few hours, group B streptococcus (GBS) is isolated from a blood culture.
According to the CDC, a woman colonized with Group B strep at the time of delivery has a 1 in 200 chance of delivering a baby who will develop GBS disease. Antibiotics during labor drop that risk to 1 in 4,000. It’s not perfect – there are still about 1,000 cases annually in the United States – but is has been a major step forward. In recent years, the incidence of early-onset GBS disease has fallen to just under 0.3 cases per 1,000 live births, and some experts think rates could go even lower with improved adherence to current guidelines.
Reducing late-onset GBS disease requires a different strategy. Efforts to develop a GBS vaccine that could be given to pregnant women continue, and recent phase 2 trials of a trivalent polysaccharide-protein conjugate vaccine looked promising. Fingers crossed that we won’t have to wait until we celebrate the 75th anniversary of Pediatric News to tout the impact of maternal immunization on reducing GBS disease in infants.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
It once was a very a common scenario. A baby born at term looks fine for the first 24 hours of life. Without much warning, the infant develops grunting, tachypnea, and tachycardia. Sepsis is suspected, and within a few hours, group B streptococcus (GBS) is isolated from a blood culture.
According to the CDC, a woman colonized with Group B strep at the time of delivery has a 1 in 200 chance of delivering a baby who will develop GBS disease. Antibiotics during labor drop that risk to 1 in 4,000. It’s not perfect – there are still about 1,000 cases annually in the United States – but is has been a major step forward. In recent years, the incidence of early-onset GBS disease has fallen to just under 0.3 cases per 1,000 live births, and some experts think rates could go even lower with improved adherence to current guidelines.
Reducing late-onset GBS disease requires a different strategy. Efforts to develop a GBS vaccine that could be given to pregnant women continue, and recent phase 2 trials of a trivalent polysaccharide-protein conjugate vaccine looked promising. Fingers crossed that we won’t have to wait until we celebrate the 75th anniversary of Pediatric News to tout the impact of maternal immunization on reducing GBS disease in infants.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
It once was a very a common scenario. A baby born at term looks fine for the first 24 hours of life. Without much warning, the infant develops grunting, tachypnea, and tachycardia. Sepsis is suspected, and within a few hours, group B streptococcus (GBS) is isolated from a blood culture.
According to the CDC, a woman colonized with Group B strep at the time of delivery has a 1 in 200 chance of delivering a baby who will develop GBS disease. Antibiotics during labor drop that risk to 1 in 4,000. It’s not perfect – there are still about 1,000 cases annually in the United States – but is has been a major step forward. In recent years, the incidence of early-onset GBS disease has fallen to just under 0.3 cases per 1,000 live births, and some experts think rates could go even lower with improved adherence to current guidelines.
Reducing late-onset GBS disease requires a different strategy. Efforts to develop a GBS vaccine that could be given to pregnant women continue, and recent phase 2 trials of a trivalent polysaccharide-protein conjugate vaccine looked promising. Fingers crossed that we won’t have to wait until we celebrate the 75th anniversary of Pediatric News to tout the impact of maternal immunization on reducing GBS disease in infants.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
Vaccine renaissance
In 1967, pediatric patients were vaccinated routinely against eight diseases with 10 vaccines: smallpox; diphtheria; tetanus and pertussis; polio serotypes 1, 2, and 3; measles; rubella; and mumps. Then in 1989, vaccine discovery took a dramatic upward trend. For the physicians and scientists involved in vaccine discovery, the driving force may have been a passion for scientific discovery and a humanitarian motivation, but what drove this major change in pediatric infectious diseases was economics.
I believe The hiatus of more than 20 years between the introduction of the mumps vaccine in 1967 and that of the Hib vaccine in 1989 in my view was because the economic incentives to develop vaccines were absent. In fact, in the 1970s and early 1980s, vaccine manufacturers were drawing back from making vaccines because they were losing money selling them at a few dollars per dose.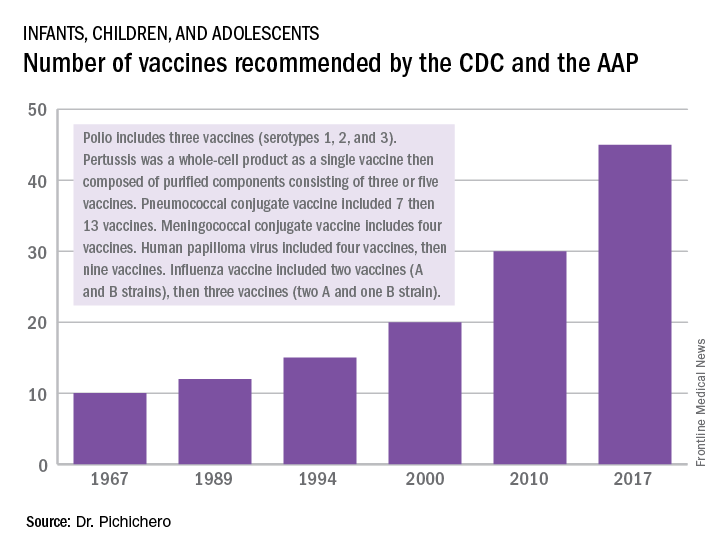
A trailblazing path had been created, and more and more vaccines have been discovered and come to market since then. Combination vaccines and vaccines for adolescents and adults have followed. The biggest blockbuster is Prevnar13 (actually 13 vaccines contained in a single combination), now with annual sales in excess of $7 billion worldwide and growing. Other vaccines with sales of a billion dollars or more are also on the market; anything in excess of $1 billion is considered a blockbuster in the pharmaceutical industry and gets the attention of CEOs (and investors) in a big way.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute at Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. He has received funding awarded to his institution for vaccine research from GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. Email him at [email protected].
In 1967, pediatric patients were vaccinated routinely against eight diseases with 10 vaccines: smallpox; diphtheria; tetanus and pertussis; polio serotypes 1, 2, and 3; measles; rubella; and mumps. Then in 1989, vaccine discovery took a dramatic upward trend. For the physicians and scientists involved in vaccine discovery, the driving force may have been a passion for scientific discovery and a humanitarian motivation, but what drove this major change in pediatric infectious diseases was economics.
I believe The hiatus of more than 20 years between the introduction of the mumps vaccine in 1967 and that of the Hib vaccine in 1989 in my view was because the economic incentives to develop vaccines were absent. In fact, in the 1970s and early 1980s, vaccine manufacturers were drawing back from making vaccines because they were losing money selling them at a few dollars per dose.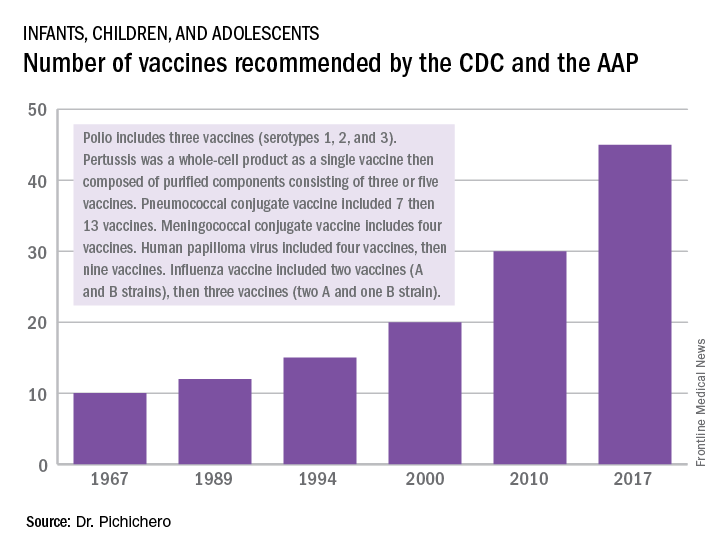
A trailblazing path had been created, and more and more vaccines have been discovered and come to market since then. Combination vaccines and vaccines for adolescents and adults have followed. The biggest blockbuster is Prevnar13 (actually 13 vaccines contained in a single combination), now with annual sales in excess of $7 billion worldwide and growing. Other vaccines with sales of a billion dollars or more are also on the market; anything in excess of $1 billion is considered a blockbuster in the pharmaceutical industry and gets the attention of CEOs (and investors) in a big way.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute at Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. He has received funding awarded to his institution for vaccine research from GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. Email him at [email protected].
In 1967, pediatric patients were vaccinated routinely against eight diseases with 10 vaccines: smallpox; diphtheria; tetanus and pertussis; polio serotypes 1, 2, and 3; measles; rubella; and mumps. Then in 1989, vaccine discovery took a dramatic upward trend. For the physicians and scientists involved in vaccine discovery, the driving force may have been a passion for scientific discovery and a humanitarian motivation, but what drove this major change in pediatric infectious diseases was economics.
I believe The hiatus of more than 20 years between the introduction of the mumps vaccine in 1967 and that of the Hib vaccine in 1989 in my view was because the economic incentives to develop vaccines were absent. In fact, in the 1970s and early 1980s, vaccine manufacturers were drawing back from making vaccines because they were losing money selling them at a few dollars per dose.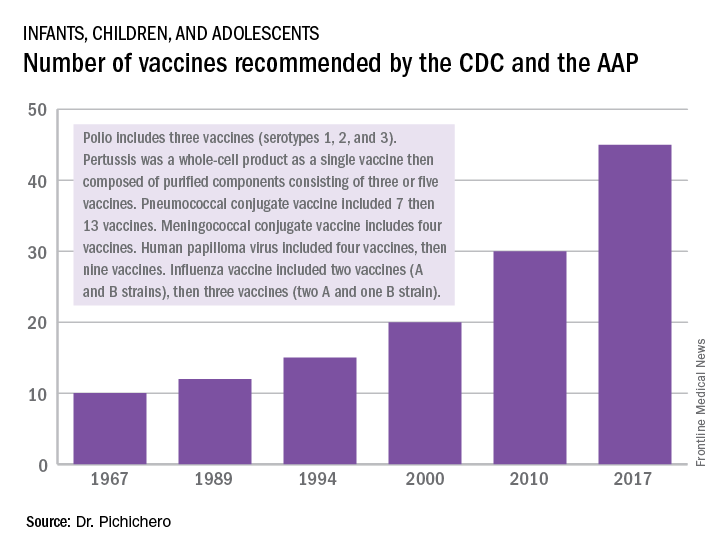
A trailblazing path had been created, and more and more vaccines have been discovered and come to market since then. Combination vaccines and vaccines for adolescents and adults have followed. The biggest blockbuster is Prevnar13 (actually 13 vaccines contained in a single combination), now with annual sales in excess of $7 billion worldwide and growing. Other vaccines with sales of a billion dollars or more are also on the market; anything in excess of $1 billion is considered a blockbuster in the pharmaceutical industry and gets the attention of CEOs (and investors) in a big way.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute at Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. He has received funding awarded to his institution for vaccine research from GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. Email him at [email protected].
Artemisinin: Its global impact on the treatment of malaria
Malaria remains a major international public health concern. In 2015, the World Health Organization estimated that 212 million individuals were infected and that there were 429,000 deaths. This represents a 21% decline in incidence globally and a 29% decline in global mortality between 2010 and 2015. In 2016, malaria was endemic in 91 countries and territories, down from 108 in 2000. Although malaria has been eliminated from the United States since the early 1950s, approximately 1,700 cases are reported annually, most of which occur in returned travelers, according to the Centers for Disease Control and Prevention.
Five species of Plasmodium (P. falciparum, P. vivax, P. malariae, P. ovale, and, more recently, P. knowelsi) account for most of the infections in humans and are transmitted by the bite of an infected female Anopheles mosquito. The disease is rarely acquired by blood transfusion, by needle sharing, by organ transplantation, or congenitally. Once diagnosed, malaria can be treated; however, delay in initiating therapy can lead to both serious and fatal outcomes.
Treatment
Historically, drug development was driven by the need to protect the military. While quinine was isolated from the bark of the cinchona tree in 1820, chloroquine, proguanil, mefloquine, and atovaquone each were developed during or after a military conflict during 1945-1985. Tetracycline/doxycycline and clindamycin also have antimalarial activity. Use of any of these agents as monotherapy has led to drug resistance and treatment failure.
Artemisinin
Artemisinin (also known as qinghao su) and its derivatives are a new class of antimalarials derived from the sweet wormwood plant Artemisia annua. Initially developed in China in the 1970s, this class gained global attention in the 1990s. and have the fastest parasite clearance time, rapid resolution of symptoms, and an excellent safety profile. They have activity against all Plasmodium species.
Because of artemisinins’ rapid elimination, they are used in combination with an agent that also kills blood parasites but has a slower elimination rate and a different mechanism of action. The goal is to prevent and delay the development of resistance and reduce recrudescence. The superiority of artemisinin-based combination therapy (ACT) over monotherapies has been documented.
Resistance, always a concern, has remained limited to specific areas in Southeast Asia since reported in 2008. Monitoring drug efficacy, safety, quality of antimalarials is ongoing, as is discouraging monotherapy use of these agents. Globally, artemisinins are the mainstay of treatment. Spread of resistance would be a major setback for both malaria control and elimination.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
Malaria remains a major international public health concern. In 2015, the World Health Organization estimated that 212 million individuals were infected and that there were 429,000 deaths. This represents a 21% decline in incidence globally and a 29% decline in global mortality between 2010 and 2015. In 2016, malaria was endemic in 91 countries and territories, down from 108 in 2000. Although malaria has been eliminated from the United States since the early 1950s, approximately 1,700 cases are reported annually, most of which occur in returned travelers, according to the Centers for Disease Control and Prevention.
Five species of Plasmodium (P. falciparum, P. vivax, P. malariae, P. ovale, and, more recently, P. knowelsi) account for most of the infections in humans and are transmitted by the bite of an infected female Anopheles mosquito. The disease is rarely acquired by blood transfusion, by needle sharing, by organ transplantation, or congenitally. Once diagnosed, malaria can be treated; however, delay in initiating therapy can lead to both serious and fatal outcomes.
Treatment
Historically, drug development was driven by the need to protect the military. While quinine was isolated from the bark of the cinchona tree in 1820, chloroquine, proguanil, mefloquine, and atovaquone each were developed during or after a military conflict during 1945-1985. Tetracycline/doxycycline and clindamycin also have antimalarial activity. Use of any of these agents as monotherapy has led to drug resistance and treatment failure.
Artemisinin
Artemisinin (also known as qinghao su) and its derivatives are a new class of antimalarials derived from the sweet wormwood plant Artemisia annua. Initially developed in China in the 1970s, this class gained global attention in the 1990s. and have the fastest parasite clearance time, rapid resolution of symptoms, and an excellent safety profile. They have activity against all Plasmodium species.
Because of artemisinins’ rapid elimination, they are used in combination with an agent that also kills blood parasites but has a slower elimination rate and a different mechanism of action. The goal is to prevent and delay the development of resistance and reduce recrudescence. The superiority of artemisinin-based combination therapy (ACT) over monotherapies has been documented.
Resistance, always a concern, has remained limited to specific areas in Southeast Asia since reported in 2008. Monitoring drug efficacy, safety, quality of antimalarials is ongoing, as is discouraging monotherapy use of these agents. Globally, artemisinins are the mainstay of treatment. Spread of resistance would be a major setback for both malaria control and elimination.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
Malaria remains a major international public health concern. In 2015, the World Health Organization estimated that 212 million individuals were infected and that there were 429,000 deaths. This represents a 21% decline in incidence globally and a 29% decline in global mortality between 2010 and 2015. In 2016, malaria was endemic in 91 countries and territories, down from 108 in 2000. Although malaria has been eliminated from the United States since the early 1950s, approximately 1,700 cases are reported annually, most of which occur in returned travelers, according to the Centers for Disease Control and Prevention.
Five species of Plasmodium (P. falciparum, P. vivax, P. malariae, P. ovale, and, more recently, P. knowelsi) account for most of the infections in humans and are transmitted by the bite of an infected female Anopheles mosquito. The disease is rarely acquired by blood transfusion, by needle sharing, by organ transplantation, or congenitally. Once diagnosed, malaria can be treated; however, delay in initiating therapy can lead to both serious and fatal outcomes.
Treatment
Historically, drug development was driven by the need to protect the military. While quinine was isolated from the bark of the cinchona tree in 1820, chloroquine, proguanil, mefloquine, and atovaquone each were developed during or after a military conflict during 1945-1985. Tetracycline/doxycycline and clindamycin also have antimalarial activity. Use of any of these agents as monotherapy has led to drug resistance and treatment failure.
Artemisinin
Artemisinin (also known as qinghao su) and its derivatives are a new class of antimalarials derived from the sweet wormwood plant Artemisia annua. Initially developed in China in the 1970s, this class gained global attention in the 1990s. and have the fastest parasite clearance time, rapid resolution of symptoms, and an excellent safety profile. They have activity against all Plasmodium species.
Because of artemisinins’ rapid elimination, they are used in combination with an agent that also kills blood parasites but has a slower elimination rate and a different mechanism of action. The goal is to prevent and delay the development of resistance and reduce recrudescence. The superiority of artemisinin-based combination therapy (ACT) over monotherapies has been documented.
Resistance, always a concern, has remained limited to specific areas in Southeast Asia since reported in 2008. Monitoring drug efficacy, safety, quality of antimalarials is ongoing, as is discouraging monotherapy use of these agents. Globally, artemisinins are the mainstay of treatment. Spread of resistance would be a major setback for both malaria control and elimination.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
A ‘game changer’ for pediatric HIV
In memory of Anne Marie Regan, CPNP, senior research coordinator, Pediatric HIV Program, Boston City Hospital
Our first child with perinatal HIV presented in 1985 at age 4 weeks with failure to thrive, vomiting, diarrhea, and thrush. Over the next several years, the number of HIV-infected infants grew exponentially, and by 1991, we were caring for more than 50 infants and children at Boston City Hospital.
Antiretrovirals were marginally effective for HIV-infected infants and children at this time. Subsequently, we embarked on a national effort to prevent vertical transmission. We participated first in the study of pharmacokinetics of zidovudine (AZT) in newborns. We enrolled patients in ACTG 076 to test the hypothesis that treatment with AZT during pregnancy and labor, and in the infant, would reduce the risk of vertical transmission. Fifty U.S. and nine French sites enrolled 473 women between April 1991 and December 20, 1993. The results were spectacular; 8 of 100 infants in the AZT treatment group, compared with 25 out of 100 infants in the control group, developed HIV. By 1995, HIV testing was offered to all women at Boston Medical Center (formerly Boston City Hospital), and the promise of prevention of vertical transmission was reaching fruition. Between 1996 and 2016, approximately 500 HIV-infected women delivered at Boston Medical Center with vertical transmission identified in only 6 (1.2%) infants; without ACTG 076, we would have expected 125! In 2013, the Centers for Disease Control and Prevention reported that 70% of pregnant HIV-infected women received the complete 076 regimen, and 93% of mothers or infants received some part of the regimen. In 1992, 900 HIV-infected infants were diagnosed in the United States, and as many as 2,000 newborns were estimated to have been born infected with HIV; in 2015, 86 vertical transmissions were identified. This was, and remains, a remarkable accomplishment.
Dr. Pelton is chief of pediatric infectious diseases and coordinator of the maternal-child HIV program at Boston Medical Center. Ms. Moloney is a certified pediatric nurse practitioner in the division of pediatric infectious diseases. Dr. Pelton said he had no relevant financial disclosures, and Ms. Moloney is a speaker (on vaccines) for Sanofi Pasteur. Email them at [email protected].
In memory of Anne Marie Regan, CPNP, senior research coordinator, Pediatric HIV Program, Boston City Hospital
Our first child with perinatal HIV presented in 1985 at age 4 weeks with failure to thrive, vomiting, diarrhea, and thrush. Over the next several years, the number of HIV-infected infants grew exponentially, and by 1991, we were caring for more than 50 infants and children at Boston City Hospital.
Antiretrovirals were marginally effective for HIV-infected infants and children at this time. Subsequently, we embarked on a national effort to prevent vertical transmission. We participated first in the study of pharmacokinetics of zidovudine (AZT) in newborns. We enrolled patients in ACTG 076 to test the hypothesis that treatment with AZT during pregnancy and labor, and in the infant, would reduce the risk of vertical transmission. Fifty U.S. and nine French sites enrolled 473 women between April 1991 and December 20, 1993. The results were spectacular; 8 of 100 infants in the AZT treatment group, compared with 25 out of 100 infants in the control group, developed HIV. By 1995, HIV testing was offered to all women at Boston Medical Center (formerly Boston City Hospital), and the promise of prevention of vertical transmission was reaching fruition. Between 1996 and 2016, approximately 500 HIV-infected women delivered at Boston Medical Center with vertical transmission identified in only 6 (1.2%) infants; without ACTG 076, we would have expected 125! In 2013, the Centers for Disease Control and Prevention reported that 70% of pregnant HIV-infected women received the complete 076 regimen, and 93% of mothers or infants received some part of the regimen. In 1992, 900 HIV-infected infants were diagnosed in the United States, and as many as 2,000 newborns were estimated to have been born infected with HIV; in 2015, 86 vertical transmissions were identified. This was, and remains, a remarkable accomplishment.
Dr. Pelton is chief of pediatric infectious diseases and coordinator of the maternal-child HIV program at Boston Medical Center. Ms. Moloney is a certified pediatric nurse practitioner in the division of pediatric infectious diseases. Dr. Pelton said he had no relevant financial disclosures, and Ms. Moloney is a speaker (on vaccines) for Sanofi Pasteur. Email them at [email protected].
In memory of Anne Marie Regan, CPNP, senior research coordinator, Pediatric HIV Program, Boston City Hospital
Our first child with perinatal HIV presented in 1985 at age 4 weeks with failure to thrive, vomiting, diarrhea, and thrush. Over the next several years, the number of HIV-infected infants grew exponentially, and by 1991, we were caring for more than 50 infants and children at Boston City Hospital.
Antiretrovirals were marginally effective for HIV-infected infants and children at this time. Subsequently, we embarked on a national effort to prevent vertical transmission. We participated first in the study of pharmacokinetics of zidovudine (AZT) in newborns. We enrolled patients in ACTG 076 to test the hypothesis that treatment with AZT during pregnancy and labor, and in the infant, would reduce the risk of vertical transmission. Fifty U.S. and nine French sites enrolled 473 women between April 1991 and December 20, 1993. The results were spectacular; 8 of 100 infants in the AZT treatment group, compared with 25 out of 100 infants in the control group, developed HIV. By 1995, HIV testing was offered to all women at Boston Medical Center (formerly Boston City Hospital), and the promise of prevention of vertical transmission was reaching fruition. Between 1996 and 2016, approximately 500 HIV-infected women delivered at Boston Medical Center with vertical transmission identified in only 6 (1.2%) infants; without ACTG 076, we would have expected 125! In 2013, the Centers for Disease Control and Prevention reported that 70% of pregnant HIV-infected women received the complete 076 regimen, and 93% of mothers or infants received some part of the regimen. In 1992, 900 HIV-infected infants were diagnosed in the United States, and as many as 2,000 newborns were estimated to have been born infected with HIV; in 2015, 86 vertical transmissions were identified. This was, and remains, a remarkable accomplishment.
Dr. Pelton is chief of pediatric infectious diseases and coordinator of the maternal-child HIV program at Boston Medical Center. Ms. Moloney is a certified pediatric nurse practitioner in the division of pediatric infectious diseases. Dr. Pelton said he had no relevant financial disclosures, and Ms. Moloney is a speaker (on vaccines) for Sanofi Pasteur. Email them at [email protected].
50 years of pediatric dermatology
The world in pediatric dermatology has changed in incredible ways since 1967. In fact, pediatric dermatology was not an organized specialty until years later! This article will look back at some of the history of pediatric dermatology, exploring how different the field was 50 years ago, and how it has evolved into the vibrant field that it is. By looking at some disease states, and differences in practice in relation to the care of dermatologic conditions in children both by pediatricians and dermatologists, we can see the tremendous evolution in our understanding and management of pediatric skin conditions, and perhaps gain insight into the future.
Pediatric dermatology was fairly “neonatal” 50 years ago, with only a few practitioners in the field. Recognizing that up to 30% of pediatric primary care visits include a skin-related problem, and that there was limited training about skin diseases among primary care practitioners and inconsistent training amongst dermatologists, there was a clinical need for establishing the subspecialty of pediatric dermatology. The first international symposium was held in Mexico City in October 1972, and with this meeting the International Society of Pediatric Dermatology was founded. The Society for Pediatric Dermatology (SPD) began in 1973, with Alvin Jacobs, MD, Samuel Weinberg, MD, Nancy Esterly, MD, Sidney Hurwitz, MD, William Weston, MD, and Coleman Jacobson, MD, as some of the initial “founding mothers and fathers.” The journal Pediatric Dermatology released its first issue in 1982 (35 years ago), and the American Academy of Pediatrics did not have a section of dermatology until 1986.
Pediatrics and dermatology: The interface
Many of the first generation of pediatric dermatologists trained as pediatricians prior to pursuing their dermatology work, with some being “assigned” dermatology as pediatric experts, while others did formal residencies in dermatology. This history is important, as pediatric dermatology was, and remains, integrated with pediatrics, even while training in dermatology residencies became standard practice. An important part of the development of the field has been the education of pediatricians and dermatologists by pediatric dermatologists, with a strong sensibility that improved training for both generalists and specialists about pediatric skin disease would yield better care for patients and families.
Initially, there were very few pediatric or dermatology programs in the United States that had pediatric dermatologists. Over the succeeding decades, this is now less common, although even now there are still dermatology and pediatric residency programs that do not have a pediatric dermatologist for either training or to serve their patients. The founding leaders of the SPD set a tone of collaboration nationally and internationally, reaching out to pediatric colleagues and dermatology associates from around the world, and establishing superb educational programs for the exchange of ideas, presentation of challenging cases, and promoting state of the art knowledge of the field. Through annual meetings of the SPD, conferences immediately preceding the American Academy of Dermatology annual meetings, the World Congress of Pediatric Dermatology, and other regional and international meetings, the field developed as the number of practitioners grew, and as the specialized published literature reflected new knowledge in diagnosis and therapy.
Building upon the history of collaboration and reflecting the maturation of the field with a desire to influence the breadth and quantity of research in pediatric dermatology, the Pediatric Dermatology Research Alliance (PeDRA) was formed in 2012. This organization was formed to promote and facilitate high quality collaborative clinical, translational, educational, and basic science research in pediatric dermatology with a vision to create sustainable, collaborative networks to better understand, prevent, treat, and cure dermatologic diseases in children. This network is now composed of over 230 members representing over 68 institutions from the United States and Canada, but including involvement globally from Mexico, Europe, and the Middle East.
Examples of changing perspectives: hemangiomas
A good way to look at evolution of the field is take a look at some of the similarities and differences in clinical practice in relation to common and uncommon disease states.
A great example is hemangiomas. Some of the first natural history studies on hemangiomas were done in the early 1960s, establishing that many lesions had a typical clinical course of fairly rapid growth, plateau, and involution over time. Of course, the identification of hemangiomas of infancy (or “HOI” in the trade), was confused with vascular malformations, and no one had recognized variant tumors that were distinct, such as rapidly involuting and noninvoluting congenital hemangiomas (RICHs or NICHs), tufted angiomas, and hemangioendotheliomas. PHACE syndrome (posterior fossa brain malformations) had yet to be described (that was done in 1996 by Ilona Frieden and her colleagues). For a time period, hemangiomas were treated with X-rays, before the negative impact of such radiation was acknowledged. For many years after that, even deforming and functionally significant lesions were “followed clinically” for natural involution, presumably a backlash from the radiation therapy interventions.
This story also reflects how organized research efforts helped with the evolution of knowledge and clinical care. The Hemangioma of Infancy Group was formed to take a collaborative approach to characterize and study hemangiomas and related tumors. Beginning with energetic, insightful pediatric dermatologists, and little funding, they changed our knowledge base of how hemangiomas present, the risk factors for their development and the characteristics and multiple organ findings associated with PHACE and other syndromic hemangiomas.
Procedural pediatric dermatology: Tremendous revolution in surgery and laser
The first generation of pediatric dermatologists were considered medical dermatologist specialists. And how important this specialty work was! Acne, atopic dermatitis, psoriasis, diaper and seborrheic dermatitis, and rare genetic syndromes, these conditions were a major part of the work of early pediatric dermatologists (and remain so now). What was not common was for pediatric dermatologists to have procedural or surgical practices, while this now is routinely part of the work of specialists in the field. How did this shift occur?
The fundamental shift began to occur with the introduction of the pulsed dye laser in 1989 and the publication of a seminal article in the New England Journal of Medicine (1989 Feb 16;320[7]:416-21) on its utility in treating port-wine stains in children with minimal scarring. Vascular lesions including port-wine stains were common, and pediatric dermatologists managed these patients for both diagnosis and medical management. Also, dermatology residencies at this time offered training in cutaneous surgery, excisions (including Mohs surgery) and repairs, and trainees in pediatric dermatology were “trained up” to high levels of expertise. As lasers were incorporated into dermatology residency work and practices, pediatric dermatologists had the exposure and skill to do this work. An added advantage was having the pediatric knowledge of how to handle children and adolescents in an age appropriate manner, and consideration of methods to minimize the pain and anxiety of procedures. Within a few years, pediatric dermatologists were at the forefront of the use of topical anesthetics (EMLA and liposomal lidocaine) and had general anesthesia privileges for laser and excisional surgery.
So while pediatric dermatologists still do “small procedures” every hour in most practices (cryotherapy for warts, cantharidin for molluscum, shave and punch biopsies), a subset now have extensive procedural practices, which in recent years has extended to pigment lesion lasers (to treat nevus of Ota), hair lasers (to treat perineal areas to prevent pilonidal cyst recurrence or to treat hirsutism), and combinations of lasers to treat hypertrophic, constrictive, and/or deforming scars).
Inflammatory skin disorders: Bread and butter ... and peanut butter?
The care of pediatric inflammatory skin disorders has evolved, but more slowly for some diseases than others. Acne vulgaris now is recognized as much more common under age 12 years than previously, presumably reflecting earlier pubertal changes in our preteens. Over the past 30 years, therapy has evolved with the use of topical retinoids (still underused by pediatricians, considered a “practice gap”), hormonal therapy with combined oral contraceptives, and oral isotretinoin, a powerful but highly effective systemic agent for severe and refractory acne. Specific pediatric guidelines came much later. Pediatric acne expert recommendations were formulated by the American Acne and Rosacea Society and endorsed by the American Academy of Pediatrics in 2013 (Pediatrics. 2013;131:S163-86). Over the past few years, there is a push by experts for more judicious use of antibiotics for acne (oral and topical) to minimize the emergence of bacterial resistance.
Psoriasis has been a condition that has been “behind the revolution,” in that no biologic agent was approved for pediatric psoriasis in the United States until several months ago, lagging behind Europe and elsewhere in the world by almost a decade. Adult psoriasis has been recognized to be associated with a broad set of comorbidities, including obesity and early heart disease, and there is now research on how children are at risk as well, and new recommendations on how to screen children with psoriasis. Moderate to severe psoriasis in adults is now tremendously controllable with biologic agents targeting TNF-alpha, IL 12/23, and IL-17. Etanercept has been approved for children with psoriasis aged 4 years and older, and other biologic agents are under study.
Atopic dermatitis now is ready for its revolution! AD has increased in prevalence from around 5% of the pediatric population 30-plus years ago to 10%-15%. Treatment of most individuals has remained the same over the decades: Good skin care, frequent moisturizers, topical corticosteroids for flares, management of infection if noted. The topical calcineurin inhibitors (TCIs) broadened the therapeutic approach when introduced in 2000 and 2001, but the boxed warning resulted in some practitioners minimizing their utilization of these useful agents.

It has been recognized for years that children with AD have higher risk of developing food allergies than children without AD. A changing understanding of how early food exposure may induce tolerance is changing the world of allergy and influencing the care of children with AD. This is where the peanut butter (or other processed peanut, such as “Bamba”) may be life saving. New guidelines have come from the National Institute of Allergy and Infectious Diseases recommending that infants with severe eczema (or egg allergy, or both) have introduction of age-appropriate peanut-containing food as early as 4-6 months of age to reduce the risk of development of peanut allergy. It is recommended that these infants undergo early evaluation for possible sensitization to peanut protein, with referral to allergists for skin prick tests or serum IgE screens (though if positive, referral to allergists is appropriate), and assess the safety of going ahead with early feeding. It is hoped that following these new guidelines can minimize the development of peanut allergy.
The future
Where will pediatric skin disease, or more importantly, skin health over a lifetime be in 50 years? Can we cure or prevent the consequences of our lethal and life altering genetic diseases such as epidermolysis bullosa or our neurocutaneous disorders? Will our new insights into birthmarks (they are mostly somatic mutations) allow us to form specific, personalized therapies to minimize their impact? Will we be using computers equipped with imaging devices and algorithms to assess our patients’ moles, papules, and nodules? Will our vaccines have wiped out warts, molluscum, and perhaps, acne? Will we have cured our inflammatory skin disorders, or perhaps prevented them by interventions in the neonatal period? No predictions will be offered here, other than that we can look forward to incredible changes for our future generations of health care practitioners, patients, and families.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego and professor of dermatology and pediatrics at the University of California, San Diego. Dr. Eichenfield has served as a consultant for Anacor/Pfizer and Regeneron/Sanofi. Email him at [email protected].
The world in pediatric dermatology has changed in incredible ways since 1967. In fact, pediatric dermatology was not an organized specialty until years later! This article will look back at some of the history of pediatric dermatology, exploring how different the field was 50 years ago, and how it has evolved into the vibrant field that it is. By looking at some disease states, and differences in practice in relation to the care of dermatologic conditions in children both by pediatricians and dermatologists, we can see the tremendous evolution in our understanding and management of pediatric skin conditions, and perhaps gain insight into the future.
Pediatric dermatology was fairly “neonatal” 50 years ago, with only a few practitioners in the field. Recognizing that up to 30% of pediatric primary care visits include a skin-related problem, and that there was limited training about skin diseases among primary care practitioners and inconsistent training amongst dermatologists, there was a clinical need for establishing the subspecialty of pediatric dermatology. The first international symposium was held in Mexico City in October 1972, and with this meeting the International Society of Pediatric Dermatology was founded. The Society for Pediatric Dermatology (SPD) began in 1973, with Alvin Jacobs, MD, Samuel Weinberg, MD, Nancy Esterly, MD, Sidney Hurwitz, MD, William Weston, MD, and Coleman Jacobson, MD, as some of the initial “founding mothers and fathers.” The journal Pediatric Dermatology released its first issue in 1982 (35 years ago), and the American Academy of Pediatrics did not have a section of dermatology until 1986.
Pediatrics and dermatology: The interface
Many of the first generation of pediatric dermatologists trained as pediatricians prior to pursuing their dermatology work, with some being “assigned” dermatology as pediatric experts, while others did formal residencies in dermatology. This history is important, as pediatric dermatology was, and remains, integrated with pediatrics, even while training in dermatology residencies became standard practice. An important part of the development of the field has been the education of pediatricians and dermatologists by pediatric dermatologists, with a strong sensibility that improved training for both generalists and specialists about pediatric skin disease would yield better care for patients and families.
Initially, there were very few pediatric or dermatology programs in the United States that had pediatric dermatologists. Over the succeeding decades, this is now less common, although even now there are still dermatology and pediatric residency programs that do not have a pediatric dermatologist for either training or to serve their patients. The founding leaders of the SPD set a tone of collaboration nationally and internationally, reaching out to pediatric colleagues and dermatology associates from around the world, and establishing superb educational programs for the exchange of ideas, presentation of challenging cases, and promoting state of the art knowledge of the field. Through annual meetings of the SPD, conferences immediately preceding the American Academy of Dermatology annual meetings, the World Congress of Pediatric Dermatology, and other regional and international meetings, the field developed as the number of practitioners grew, and as the specialized published literature reflected new knowledge in diagnosis and therapy.
Building upon the history of collaboration and reflecting the maturation of the field with a desire to influence the breadth and quantity of research in pediatric dermatology, the Pediatric Dermatology Research Alliance (PeDRA) was formed in 2012. This organization was formed to promote and facilitate high quality collaborative clinical, translational, educational, and basic science research in pediatric dermatology with a vision to create sustainable, collaborative networks to better understand, prevent, treat, and cure dermatologic diseases in children. This network is now composed of over 230 members representing over 68 institutions from the United States and Canada, but including involvement globally from Mexico, Europe, and the Middle East.
Examples of changing perspectives: hemangiomas
A good way to look at evolution of the field is take a look at some of the similarities and differences in clinical practice in relation to common and uncommon disease states.
A great example is hemangiomas. Some of the first natural history studies on hemangiomas were done in the early 1960s, establishing that many lesions had a typical clinical course of fairly rapid growth, plateau, and involution over time. Of course, the identification of hemangiomas of infancy (or “HOI” in the trade), was confused with vascular malformations, and no one had recognized variant tumors that were distinct, such as rapidly involuting and noninvoluting congenital hemangiomas (RICHs or NICHs), tufted angiomas, and hemangioendotheliomas. PHACE syndrome (posterior fossa brain malformations) had yet to be described (that was done in 1996 by Ilona Frieden and her colleagues). For a time period, hemangiomas were treated with X-rays, before the negative impact of such radiation was acknowledged. For many years after that, even deforming and functionally significant lesions were “followed clinically” for natural involution, presumably a backlash from the radiation therapy interventions.
This story also reflects how organized research efforts helped with the evolution of knowledge and clinical care. The Hemangioma of Infancy Group was formed to take a collaborative approach to characterize and study hemangiomas and related tumors. Beginning with energetic, insightful pediatric dermatologists, and little funding, they changed our knowledge base of how hemangiomas present, the risk factors for their development and the characteristics and multiple organ findings associated with PHACE and other syndromic hemangiomas.
Procedural pediatric dermatology: Tremendous revolution in surgery and laser
The first generation of pediatric dermatologists were considered medical dermatologist specialists. And how important this specialty work was! Acne, atopic dermatitis, psoriasis, diaper and seborrheic dermatitis, and rare genetic syndromes, these conditions were a major part of the work of early pediatric dermatologists (and remain so now). What was not common was for pediatric dermatologists to have procedural or surgical practices, while this now is routinely part of the work of specialists in the field. How did this shift occur?
The fundamental shift began to occur with the introduction of the pulsed dye laser in 1989 and the publication of a seminal article in the New England Journal of Medicine (1989 Feb 16;320[7]:416-21) on its utility in treating port-wine stains in children with minimal scarring. Vascular lesions including port-wine stains were common, and pediatric dermatologists managed these patients for both diagnosis and medical management. Also, dermatology residencies at this time offered training in cutaneous surgery, excisions (including Mohs surgery) and repairs, and trainees in pediatric dermatology were “trained up” to high levels of expertise. As lasers were incorporated into dermatology residency work and practices, pediatric dermatologists had the exposure and skill to do this work. An added advantage was having the pediatric knowledge of how to handle children and adolescents in an age appropriate manner, and consideration of methods to minimize the pain and anxiety of procedures. Within a few years, pediatric dermatologists were at the forefront of the use of topical anesthetics (EMLA and liposomal lidocaine) and had general anesthesia privileges for laser and excisional surgery.
So while pediatric dermatologists still do “small procedures” every hour in most practices (cryotherapy for warts, cantharidin for molluscum, shave and punch biopsies), a subset now have extensive procedural practices, which in recent years has extended to pigment lesion lasers (to treat nevus of Ota), hair lasers (to treat perineal areas to prevent pilonidal cyst recurrence or to treat hirsutism), and combinations of lasers to treat hypertrophic, constrictive, and/or deforming scars).
Inflammatory skin disorders: Bread and butter ... and peanut butter?
The care of pediatric inflammatory skin disorders has evolved, but more slowly for some diseases than others. Acne vulgaris now is recognized as much more common under age 12 years than previously, presumably reflecting earlier pubertal changes in our preteens. Over the past 30 years, therapy has evolved with the use of topical retinoids (still underused by pediatricians, considered a “practice gap”), hormonal therapy with combined oral contraceptives, and oral isotretinoin, a powerful but highly effective systemic agent for severe and refractory acne. Specific pediatric guidelines came much later. Pediatric acne expert recommendations were formulated by the American Acne and Rosacea Society and endorsed by the American Academy of Pediatrics in 2013 (Pediatrics. 2013;131:S163-86). Over the past few years, there is a push by experts for more judicious use of antibiotics for acne (oral and topical) to minimize the emergence of bacterial resistance.
Psoriasis has been a condition that has been “behind the revolution,” in that no biologic agent was approved for pediatric psoriasis in the United States until several months ago, lagging behind Europe and elsewhere in the world by almost a decade. Adult psoriasis has been recognized to be associated with a broad set of comorbidities, including obesity and early heart disease, and there is now research on how children are at risk as well, and new recommendations on how to screen children with psoriasis. Moderate to severe psoriasis in adults is now tremendously controllable with biologic agents targeting TNF-alpha, IL 12/23, and IL-17. Etanercept has been approved for children with psoriasis aged 4 years and older, and other biologic agents are under study.
Atopic dermatitis now is ready for its revolution! AD has increased in prevalence from around 5% of the pediatric population 30-plus years ago to 10%-15%. Treatment of most individuals has remained the same over the decades: Good skin care, frequent moisturizers, topical corticosteroids for flares, management of infection if noted. The topical calcineurin inhibitors (TCIs) broadened the therapeutic approach when introduced in 2000 and 2001, but the boxed warning resulted in some practitioners minimizing their utilization of these useful agents.

It has been recognized for years that children with AD have higher risk of developing food allergies than children without AD. A changing understanding of how early food exposure may induce tolerance is changing the world of allergy and influencing the care of children with AD. This is where the peanut butter (or other processed peanut, such as “Bamba”) may be life saving. New guidelines have come from the National Institute of Allergy and Infectious Diseases recommending that infants with severe eczema (or egg allergy, or both) have introduction of age-appropriate peanut-containing food as early as 4-6 months of age to reduce the risk of development of peanut allergy. It is recommended that these infants undergo early evaluation for possible sensitization to peanut protein, with referral to allergists for skin prick tests or serum IgE screens (though if positive, referral to allergists is appropriate), and assess the safety of going ahead with early feeding. It is hoped that following these new guidelines can minimize the development of peanut allergy.
The future
Where will pediatric skin disease, or more importantly, skin health over a lifetime be in 50 years? Can we cure or prevent the consequences of our lethal and life altering genetic diseases such as epidermolysis bullosa or our neurocutaneous disorders? Will our new insights into birthmarks (they are mostly somatic mutations) allow us to form specific, personalized therapies to minimize their impact? Will we be using computers equipped with imaging devices and algorithms to assess our patients’ moles, papules, and nodules? Will our vaccines have wiped out warts, molluscum, and perhaps, acne? Will we have cured our inflammatory skin disorders, or perhaps prevented them by interventions in the neonatal period? No predictions will be offered here, other than that we can look forward to incredible changes for our future generations of health care practitioners, patients, and families.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego and professor of dermatology and pediatrics at the University of California, San Diego. Dr. Eichenfield has served as a consultant for Anacor/Pfizer and Regeneron/Sanofi. Email him at [email protected].
The world in pediatric dermatology has changed in incredible ways since 1967. In fact, pediatric dermatology was not an organized specialty until years later! This article will look back at some of the history of pediatric dermatology, exploring how different the field was 50 years ago, and how it has evolved into the vibrant field that it is. By looking at some disease states, and differences in practice in relation to the care of dermatologic conditions in children both by pediatricians and dermatologists, we can see the tremendous evolution in our understanding and management of pediatric skin conditions, and perhaps gain insight into the future.
Pediatric dermatology was fairly “neonatal” 50 years ago, with only a few practitioners in the field. Recognizing that up to 30% of pediatric primary care visits include a skin-related problem, and that there was limited training about skin diseases among primary care practitioners and inconsistent training amongst dermatologists, there was a clinical need for establishing the subspecialty of pediatric dermatology. The first international symposium was held in Mexico City in October 1972, and with this meeting the International Society of Pediatric Dermatology was founded. The Society for Pediatric Dermatology (SPD) began in 1973, with Alvin Jacobs, MD, Samuel Weinberg, MD, Nancy Esterly, MD, Sidney Hurwitz, MD, William Weston, MD, and Coleman Jacobson, MD, as some of the initial “founding mothers and fathers.” The journal Pediatric Dermatology released its first issue in 1982 (35 years ago), and the American Academy of Pediatrics did not have a section of dermatology until 1986.
Pediatrics and dermatology: The interface
Many of the first generation of pediatric dermatologists trained as pediatricians prior to pursuing their dermatology work, with some being “assigned” dermatology as pediatric experts, while others did formal residencies in dermatology. This history is important, as pediatric dermatology was, and remains, integrated with pediatrics, even while training in dermatology residencies became standard practice. An important part of the development of the field has been the education of pediatricians and dermatologists by pediatric dermatologists, with a strong sensibility that improved training for both generalists and specialists about pediatric skin disease would yield better care for patients and families.
Initially, there were very few pediatric or dermatology programs in the United States that had pediatric dermatologists. Over the succeeding decades, this is now less common, although even now there are still dermatology and pediatric residency programs that do not have a pediatric dermatologist for either training or to serve their patients. The founding leaders of the SPD set a tone of collaboration nationally and internationally, reaching out to pediatric colleagues and dermatology associates from around the world, and establishing superb educational programs for the exchange of ideas, presentation of challenging cases, and promoting state of the art knowledge of the field. Through annual meetings of the SPD, conferences immediately preceding the American Academy of Dermatology annual meetings, the World Congress of Pediatric Dermatology, and other regional and international meetings, the field developed as the number of practitioners grew, and as the specialized published literature reflected new knowledge in diagnosis and therapy.
Building upon the history of collaboration and reflecting the maturation of the field with a desire to influence the breadth and quantity of research in pediatric dermatology, the Pediatric Dermatology Research Alliance (PeDRA) was formed in 2012. This organization was formed to promote and facilitate high quality collaborative clinical, translational, educational, and basic science research in pediatric dermatology with a vision to create sustainable, collaborative networks to better understand, prevent, treat, and cure dermatologic diseases in children. This network is now composed of over 230 members representing over 68 institutions from the United States and Canada, but including involvement globally from Mexico, Europe, and the Middle East.
Examples of changing perspectives: hemangiomas
A good way to look at evolution of the field is take a look at some of the similarities and differences in clinical practice in relation to common and uncommon disease states.
A great example is hemangiomas. Some of the first natural history studies on hemangiomas were done in the early 1960s, establishing that many lesions had a typical clinical course of fairly rapid growth, plateau, and involution over time. Of course, the identification of hemangiomas of infancy (or “HOI” in the trade), was confused with vascular malformations, and no one had recognized variant tumors that were distinct, such as rapidly involuting and noninvoluting congenital hemangiomas (RICHs or NICHs), tufted angiomas, and hemangioendotheliomas. PHACE syndrome (posterior fossa brain malformations) had yet to be described (that was done in 1996 by Ilona Frieden and her colleagues). For a time period, hemangiomas were treated with X-rays, before the negative impact of such radiation was acknowledged. For many years after that, even deforming and functionally significant lesions were “followed clinically” for natural involution, presumably a backlash from the radiation therapy interventions.
This story also reflects how organized research efforts helped with the evolution of knowledge and clinical care. The Hemangioma of Infancy Group was formed to take a collaborative approach to characterize and study hemangiomas and related tumors. Beginning with energetic, insightful pediatric dermatologists, and little funding, they changed our knowledge base of how hemangiomas present, the risk factors for their development and the characteristics and multiple organ findings associated with PHACE and other syndromic hemangiomas.
Procedural pediatric dermatology: Tremendous revolution in surgery and laser
The first generation of pediatric dermatologists were considered medical dermatologist specialists. And how important this specialty work was! Acne, atopic dermatitis, psoriasis, diaper and seborrheic dermatitis, and rare genetic syndromes, these conditions were a major part of the work of early pediatric dermatologists (and remain so now). What was not common was for pediatric dermatologists to have procedural or surgical practices, while this now is routinely part of the work of specialists in the field. How did this shift occur?
The fundamental shift began to occur with the introduction of the pulsed dye laser in 1989 and the publication of a seminal article in the New England Journal of Medicine (1989 Feb 16;320[7]:416-21) on its utility in treating port-wine stains in children with minimal scarring. Vascular lesions including port-wine stains were common, and pediatric dermatologists managed these patients for both diagnosis and medical management. Also, dermatology residencies at this time offered training in cutaneous surgery, excisions (including Mohs surgery) and repairs, and trainees in pediatric dermatology were “trained up” to high levels of expertise. As lasers were incorporated into dermatology residency work and practices, pediatric dermatologists had the exposure and skill to do this work. An added advantage was having the pediatric knowledge of how to handle children and adolescents in an age appropriate manner, and consideration of methods to minimize the pain and anxiety of procedures. Within a few years, pediatric dermatologists were at the forefront of the use of topical anesthetics (EMLA and liposomal lidocaine) and had general anesthesia privileges for laser and excisional surgery.
So while pediatric dermatologists still do “small procedures” every hour in most practices (cryotherapy for warts, cantharidin for molluscum, shave and punch biopsies), a subset now have extensive procedural practices, which in recent years has extended to pigment lesion lasers (to treat nevus of Ota), hair lasers (to treat perineal areas to prevent pilonidal cyst recurrence or to treat hirsutism), and combinations of lasers to treat hypertrophic, constrictive, and/or deforming scars).
Inflammatory skin disorders: Bread and butter ... and peanut butter?
The care of pediatric inflammatory skin disorders has evolved, but more slowly for some diseases than others. Acne vulgaris now is recognized as much more common under age 12 years than previously, presumably reflecting earlier pubertal changes in our preteens. Over the past 30 years, therapy has evolved with the use of topical retinoids (still underused by pediatricians, considered a “practice gap”), hormonal therapy with combined oral contraceptives, and oral isotretinoin, a powerful but highly effective systemic agent for severe and refractory acne. Specific pediatric guidelines came much later. Pediatric acne expert recommendations were formulated by the American Acne and Rosacea Society and endorsed by the American Academy of Pediatrics in 2013 (Pediatrics. 2013;131:S163-86). Over the past few years, there is a push by experts for more judicious use of antibiotics for acne (oral and topical) to minimize the emergence of bacterial resistance.
Psoriasis has been a condition that has been “behind the revolution,” in that no biologic agent was approved for pediatric psoriasis in the United States until several months ago, lagging behind Europe and elsewhere in the world by almost a decade. Adult psoriasis has been recognized to be associated with a broad set of comorbidities, including obesity and early heart disease, and there is now research on how children are at risk as well, and new recommendations on how to screen children with psoriasis. Moderate to severe psoriasis in adults is now tremendously controllable with biologic agents targeting TNF-alpha, IL 12/23, and IL-17. Etanercept has been approved for children with psoriasis aged 4 years and older, and other biologic agents are under study.
Atopic dermatitis now is ready for its revolution! AD has increased in prevalence from around 5% of the pediatric population 30-plus years ago to 10%-15%. Treatment of most individuals has remained the same over the decades: Good skin care, frequent moisturizers, topical corticosteroids for flares, management of infection if noted. The topical calcineurin inhibitors (TCIs) broadened the therapeutic approach when introduced in 2000 and 2001, but the boxed warning resulted in some practitioners minimizing their utilization of these useful agents.

It has been recognized for years that children with AD have higher risk of developing food allergies than children without AD. A changing understanding of how early food exposure may induce tolerance is changing the world of allergy and influencing the care of children with AD. This is where the peanut butter (or other processed peanut, such as “Bamba”) may be life saving. New guidelines have come from the National Institute of Allergy and Infectious Diseases recommending that infants with severe eczema (or egg allergy, or both) have introduction of age-appropriate peanut-containing food as early as 4-6 months of age to reduce the risk of development of peanut allergy. It is recommended that these infants undergo early evaluation for possible sensitization to peanut protein, with referral to allergists for skin prick tests or serum IgE screens (though if positive, referral to allergists is appropriate), and assess the safety of going ahead with early feeding. It is hoped that following these new guidelines can minimize the development of peanut allergy.
The future
Where will pediatric skin disease, or more importantly, skin health over a lifetime be in 50 years? Can we cure or prevent the consequences of our lethal and life altering genetic diseases such as epidermolysis bullosa or our neurocutaneous disorders? Will our new insights into birthmarks (they are mostly somatic mutations) allow us to form specific, personalized therapies to minimize their impact? Will we be using computers equipped with imaging devices and algorithms to assess our patients’ moles, papules, and nodules? Will our vaccines have wiped out warts, molluscum, and perhaps, acne? Will we have cured our inflammatory skin disorders, or perhaps prevented them by interventions in the neonatal period? No predictions will be offered here, other than that we can look forward to incredible changes for our future generations of health care practitioners, patients, and families.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego and professor of dermatology and pediatrics at the University of California, San Diego. Dr. Eichenfield has served as a consultant for Anacor/Pfizer and Regeneron/Sanofi. Email him at [email protected].
50 years of pediatrics: What has changed for female pediatricians?
In the last 50 years, the field of pediatrics has vastly changed, particularly for female physicians.
For starters, the number of female pediatricians has rapidly grown over the last few decades. In 1970, 21% of pediatricians were women, compared with 59% in 2013, according to the American Medical Association physician characteristics and distribution data 2015 edition. The overall pediatric workforce also has increased: A total of 18,332 pediatricians were practicing in 1970, and 84,559 pediatricians were in practice in 2013.
Along with numbers, the field of pediatrics has seen significant changes in practice size, technology, clinical responsibilities, and record keeping, to name a few. However, longtime pediatricians say there are also many ways that the specialty has stayed the same.
Dr. Bennett’s story
When Jean L. Bennett, MD, opened her solo pediatric practice in 1963, she initially had no nurses or team of assistants to help carry out clinical duties. With one receptionist answering phones and Dr. Bennett in the exam room, the Clearwater, Fla., practice opened for business. There was no shortage of patients, Dr. Bennett recalls.
“There was no such thing as neonatology. As a pediatrician, one took care of well and sick newborns and of course, saw a variety of infectious diseases in the office,” Dr. Bennett said in an interview. “We started our own IVs, we did our own lumbar punctures, we did subdural taps, we did exchange transfusions. We did all of those ourselves.”
Dr. Bennett was no stranger to being the lone woman on the job. She was the first woman to graduate from the University of Florida College of Medicine in Gainesville, the first woman to serve as chief of staff at Morton F. Plant Hospital in Clearwater, and the first woman to chair the hospital’s department of pediatrics. Despite being the first in many cases, Dr. Bennett does not remember facing discrimination from colleagues or community members, nor experiencing prejudice against her gender as a medical student or young resident
“My experience was different, of course, than other people graduating at that time, but I can truly say that I always felt the playing field was level,” Dr. Bennett said. “Nobody gave me anything for being a woman, and nobody took anything away.”
Compared with concerns that physicians have today, such as electronic medical records and increasing regulations, Dr. Bennett remembers a relatively worry-free career. She recalls some concern over the medical malpractice crisis in the 1970s and 1980s, but said the majority of her tenure was spent with a clear mind and positive attitude.
“In the 60s, I was naive enough not to worry a whole lot,” she said. “I was in the process of getting my practice started, and I was raising in a family at the same time. I would struggle to tell you the things I spent time worrying about. I went to work every day with a joyful attitude, grateful that I was in a community where I could serve.”
Two of the most significant changes Dr. Bennett witnessed during her career were the development of pediatric subspecialists and the establishment of children’s hospitals. Both markedly altered the field of pediatrics and the way in which children were cared for, she said.
“Early in medicine, children were thought of as the stepchildren of medicine, if you will,” she said. “All the attention research-wise and provision-wise was for adults. During my tenure, I saw that attitude change. The attitude that children were just little adults certainly changed, and the development of specialty hospitals for children, that was a real plus.”
Dr. Bennett spent 27 years in solo practice before hiring additional doctors at what is now Myrtle Avenue Pediatrics, a group practice in Clearwater. She retired in 2003 after a career spanning 40 years. The best advice she would offer young pediatricians is to treat their staff well, especially the front office staff who answer phones and make appointments. Pay them well, train them, and treat them right in order to retain loyal employees and reduce turnover.
In addition, Dr. Bennett stresses that young women who want to be pediatricians should not focus on their gender. “I would remind them that they are physicians who happen to be women,” and they should not think of themselves as female physicians, she said. “Personally I believe becoming a physician is a calling, and I don’t think it is gender oriented. I think males and females can have that calling. I see no difference.”
Dr. Eaton’s story
In the 1960s, when most young pediatricians were opening practices or joining small groups, Antoinette P. Eaton, MD, chose an different path. A passion for serving undeserved families led her to back to what is now Nationwide Children’s Hospital in Columbus, Ohio, where she had completed her residency. In the early 60s, Dr. Eaton served as assistant medical director at the hospital, and in 1965 she become director of the hospital’s birth defect center.
Back then, insurers operated much differently, Dr. Eaton recalled. Insurance companies would not pay for outpatient care, and so children with developmental or congenital disorders would have to be admitted to the hospital for treatment. “It was a complete reversal of what it is like now,” she said.
“We all saw each patient, and then we would get together and conference on the patient and decide on the best approach,” Dr. Eaton said in an interview. “I would definitely say it was unique. It certainly ingrained in me how valuable the team approach to medicine was then and is now. It’s become a very popular approach, and I’m happy to see that, but that was my approach way back in the mid-60s and mid-70s.”
Like female pediatricians of today, Dr. Eaton worked to juggle her career and her role as a mother to four children. She found balance by working part time when necessary and getting off early when her children were school-aged. “Being a mother and being a physician, especially in leadership, there’s always going to be pressure for allocating your time appropriately between all of those demands, but I can tell you I always made being a mother my top priority, and I don’t think I sacrificed my professional duties as a result,” she said. “I think it was possible to combine them, although it’s certainly challenging at times.”
Dr. Eaton went on to become director for maternal health at the Ohio Department of Health and later served as president for the AAP Ohio Chapter and as AAP president from 1990 to 1991.
Her most important achievement however, was being a strong voice for children, she said. “My biggest accomplishment, I hope, was standing up for children and speaking out for children and assuming leadership roles in organizations like AAP to underscore that important role as an advocate.”
[email protected]
On Twitter @legal_med
In the last 50 years, the field of pediatrics has vastly changed, particularly for female physicians.
For starters, the number of female pediatricians has rapidly grown over the last few decades. In 1970, 21% of pediatricians were women, compared with 59% in 2013, according to the American Medical Association physician characteristics and distribution data 2015 edition. The overall pediatric workforce also has increased: A total of 18,332 pediatricians were practicing in 1970, and 84,559 pediatricians were in practice in 2013.
Along with numbers, the field of pediatrics has seen significant changes in practice size, technology, clinical responsibilities, and record keeping, to name a few. However, longtime pediatricians say there are also many ways that the specialty has stayed the same.
Dr. Bennett’s story
When Jean L. Bennett, MD, opened her solo pediatric practice in 1963, she initially had no nurses or team of assistants to help carry out clinical duties. With one receptionist answering phones and Dr. Bennett in the exam room, the Clearwater, Fla., practice opened for business. There was no shortage of patients, Dr. Bennett recalls.
“There was no such thing as neonatology. As a pediatrician, one took care of well and sick newborns and of course, saw a variety of infectious diseases in the office,” Dr. Bennett said in an interview. “We started our own IVs, we did our own lumbar punctures, we did subdural taps, we did exchange transfusions. We did all of those ourselves.”
Dr. Bennett was no stranger to being the lone woman on the job. She was the first woman to graduate from the University of Florida College of Medicine in Gainesville, the first woman to serve as chief of staff at Morton F. Plant Hospital in Clearwater, and the first woman to chair the hospital’s department of pediatrics. Despite being the first in many cases, Dr. Bennett does not remember facing discrimination from colleagues or community members, nor experiencing prejudice against her gender as a medical student or young resident
“My experience was different, of course, than other people graduating at that time, but I can truly say that I always felt the playing field was level,” Dr. Bennett said. “Nobody gave me anything for being a woman, and nobody took anything away.”
Compared with concerns that physicians have today, such as electronic medical records and increasing regulations, Dr. Bennett remembers a relatively worry-free career. She recalls some concern over the medical malpractice crisis in the 1970s and 1980s, but said the majority of her tenure was spent with a clear mind and positive attitude.
“In the 60s, I was naive enough not to worry a whole lot,” she said. “I was in the process of getting my practice started, and I was raising in a family at the same time. I would struggle to tell you the things I spent time worrying about. I went to work every day with a joyful attitude, grateful that I was in a community where I could serve.”
Two of the most significant changes Dr. Bennett witnessed during her career were the development of pediatric subspecialists and the establishment of children’s hospitals. Both markedly altered the field of pediatrics and the way in which children were cared for, she said.
“Early in medicine, children were thought of as the stepchildren of medicine, if you will,” she said. “All the attention research-wise and provision-wise was for adults. During my tenure, I saw that attitude change. The attitude that children were just little adults certainly changed, and the development of specialty hospitals for children, that was a real plus.”
Dr. Bennett spent 27 years in solo practice before hiring additional doctors at what is now Myrtle Avenue Pediatrics, a group practice in Clearwater. She retired in 2003 after a career spanning 40 years. The best advice she would offer young pediatricians is to treat their staff well, especially the front office staff who answer phones and make appointments. Pay them well, train them, and treat them right in order to retain loyal employees and reduce turnover.
In addition, Dr. Bennett stresses that young women who want to be pediatricians should not focus on their gender. “I would remind them that they are physicians who happen to be women,” and they should not think of themselves as female physicians, she said. “Personally I believe becoming a physician is a calling, and I don’t think it is gender oriented. I think males and females can have that calling. I see no difference.”
Dr. Eaton’s story
In the 1960s, when most young pediatricians were opening practices or joining small groups, Antoinette P. Eaton, MD, chose an different path. A passion for serving undeserved families led her to back to what is now Nationwide Children’s Hospital in Columbus, Ohio, where she had completed her residency. In the early 60s, Dr. Eaton served as assistant medical director at the hospital, and in 1965 she become director of the hospital’s birth defect center.
Back then, insurers operated much differently, Dr. Eaton recalled. Insurance companies would not pay for outpatient care, and so children with developmental or congenital disorders would have to be admitted to the hospital for treatment. “It was a complete reversal of what it is like now,” she said.
“We all saw each patient, and then we would get together and conference on the patient and decide on the best approach,” Dr. Eaton said in an interview. “I would definitely say it was unique. It certainly ingrained in me how valuable the team approach to medicine was then and is now. It’s become a very popular approach, and I’m happy to see that, but that was my approach way back in the mid-60s and mid-70s.”
Like female pediatricians of today, Dr. Eaton worked to juggle her career and her role as a mother to four children. She found balance by working part time when necessary and getting off early when her children were school-aged. “Being a mother and being a physician, especially in leadership, there’s always going to be pressure for allocating your time appropriately between all of those demands, but I can tell you I always made being a mother my top priority, and I don’t think I sacrificed my professional duties as a result,” she said. “I think it was possible to combine them, although it’s certainly challenging at times.”
Dr. Eaton went on to become director for maternal health at the Ohio Department of Health and later served as president for the AAP Ohio Chapter and as AAP president from 1990 to 1991.
Her most important achievement however, was being a strong voice for children, she said. “My biggest accomplishment, I hope, was standing up for children and speaking out for children and assuming leadership roles in organizations like AAP to underscore that important role as an advocate.”
[email protected]
On Twitter @legal_med
In the last 50 years, the field of pediatrics has vastly changed, particularly for female physicians.
For starters, the number of female pediatricians has rapidly grown over the last few decades. In 1970, 21% of pediatricians were women, compared with 59% in 2013, according to the American Medical Association physician characteristics and distribution data 2015 edition. The overall pediatric workforce also has increased: A total of 18,332 pediatricians were practicing in 1970, and 84,559 pediatricians were in practice in 2013.
Along with numbers, the field of pediatrics has seen significant changes in practice size, technology, clinical responsibilities, and record keeping, to name a few. However, longtime pediatricians say there are also many ways that the specialty has stayed the same.
Dr. Bennett’s story
When Jean L. Bennett, MD, opened her solo pediatric practice in 1963, she initially had no nurses or team of assistants to help carry out clinical duties. With one receptionist answering phones and Dr. Bennett in the exam room, the Clearwater, Fla., practice opened for business. There was no shortage of patients, Dr. Bennett recalls.
“There was no such thing as neonatology. As a pediatrician, one took care of well and sick newborns and of course, saw a variety of infectious diseases in the office,” Dr. Bennett said in an interview. “We started our own IVs, we did our own lumbar punctures, we did subdural taps, we did exchange transfusions. We did all of those ourselves.”
Dr. Bennett was no stranger to being the lone woman on the job. She was the first woman to graduate from the University of Florida College of Medicine in Gainesville, the first woman to serve as chief of staff at Morton F. Plant Hospital in Clearwater, and the first woman to chair the hospital’s department of pediatrics. Despite being the first in many cases, Dr. Bennett does not remember facing discrimination from colleagues or community members, nor experiencing prejudice against her gender as a medical student or young resident
“My experience was different, of course, than other people graduating at that time, but I can truly say that I always felt the playing field was level,” Dr. Bennett said. “Nobody gave me anything for being a woman, and nobody took anything away.”
Compared with concerns that physicians have today, such as electronic medical records and increasing regulations, Dr. Bennett remembers a relatively worry-free career. She recalls some concern over the medical malpractice crisis in the 1970s and 1980s, but said the majority of her tenure was spent with a clear mind and positive attitude.
“In the 60s, I was naive enough not to worry a whole lot,” she said. “I was in the process of getting my practice started, and I was raising in a family at the same time. I would struggle to tell you the things I spent time worrying about. I went to work every day with a joyful attitude, grateful that I was in a community where I could serve.”
Two of the most significant changes Dr. Bennett witnessed during her career were the development of pediatric subspecialists and the establishment of children’s hospitals. Both markedly altered the field of pediatrics and the way in which children were cared for, she said.
“Early in medicine, children were thought of as the stepchildren of medicine, if you will,” she said. “All the attention research-wise and provision-wise was for adults. During my tenure, I saw that attitude change. The attitude that children were just little adults certainly changed, and the development of specialty hospitals for children, that was a real plus.”
Dr. Bennett spent 27 years in solo practice before hiring additional doctors at what is now Myrtle Avenue Pediatrics, a group practice in Clearwater. She retired in 2003 after a career spanning 40 years. The best advice she would offer young pediatricians is to treat their staff well, especially the front office staff who answer phones and make appointments. Pay them well, train them, and treat them right in order to retain loyal employees and reduce turnover.
In addition, Dr. Bennett stresses that young women who want to be pediatricians should not focus on their gender. “I would remind them that they are physicians who happen to be women,” and they should not think of themselves as female physicians, she said. “Personally I believe becoming a physician is a calling, and I don’t think it is gender oriented. I think males and females can have that calling. I see no difference.”
Dr. Eaton’s story
In the 1960s, when most young pediatricians were opening practices or joining small groups, Antoinette P. Eaton, MD, chose an different path. A passion for serving undeserved families led her to back to what is now Nationwide Children’s Hospital in Columbus, Ohio, where she had completed her residency. In the early 60s, Dr. Eaton served as assistant medical director at the hospital, and in 1965 she become director of the hospital’s birth defect center.
Back then, insurers operated much differently, Dr. Eaton recalled. Insurance companies would not pay for outpatient care, and so children with developmental or congenital disorders would have to be admitted to the hospital for treatment. “It was a complete reversal of what it is like now,” she said.
“We all saw each patient, and then we would get together and conference on the patient and decide on the best approach,” Dr. Eaton said in an interview. “I would definitely say it was unique. It certainly ingrained in me how valuable the team approach to medicine was then and is now. It’s become a very popular approach, and I’m happy to see that, but that was my approach way back in the mid-60s and mid-70s.”
Like female pediatricians of today, Dr. Eaton worked to juggle her career and her role as a mother to four children. She found balance by working part time when necessary and getting off early when her children were school-aged. “Being a mother and being a physician, especially in leadership, there’s always going to be pressure for allocating your time appropriately between all of those demands, but I can tell you I always made being a mother my top priority, and I don’t think I sacrificed my professional duties as a result,” she said. “I think it was possible to combine them, although it’s certainly challenging at times.”
Dr. Eaton went on to become director for maternal health at the Ohio Department of Health and later served as president for the AAP Ohio Chapter and as AAP president from 1990 to 1991.
Her most important achievement however, was being a strong voice for children, she said. “My biggest accomplishment, I hope, was standing up for children and speaking out for children and assuming leadership roles in organizations like AAP to underscore that important role as an advocate.”
[email protected]
On Twitter @legal_med
Fifty-year retrospective by Dr. William G. Wilkoff
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
Changing ethics of pediatric health care: The last 50 years
The ethics of pediatric health care have changed radically in the past 50 years. “History,” they say, “is written by the victors.” So, if you are not careful, you will only get part of the story. Clinical ethicists learn to seek out, involve, and empower the voices of all stakeholders. To fully appreciate how much things have changed, you must learn more than one side of the story. Indeed, piecing together the history of medical ethics reminds me of the Indian story of five blind men describing an elephant, in which each can only describe a part of an ultimately much bigger animal.
If you ask philosophers about the history of medical ethics, they will point to events 50 years ago as the beginning of the modern era. In the 1960s, physicians tended to be paternalistic authoritarians. Some considered it best not to even tell a patient that he had cancer. There was minimal patient education provided. Medications were prescribed as orders for the patient to follow. Medical research had harmed volunteers, and new protections were needed.
In 1995, the American Academy of Pediatrics Section on Bioethics emphasized the importance of obtaining the child’s assent in addition to the parent’s consent.2 Most states have passed laws permitting minors to give consent for treatment for pregnancy, sexually transmitted diseases, drug addiction, and mental health care.
Technology alters ethics
At the same time, technology has been changing medicine. New life sustaining technologies in the 1960s – such as dialysis and ventilators – created new issues of extreme financial cost, allocation of scarce resources, and even the existential question of when life ends. In 1968, an ad hoc committee at Harvard created criteria for what is colloquially called “brain death.”3 Many landmark legal cases further developed the ethics of end-of-life care.
The boundaries were even less clear at the beginning of life. Technological advances in ventilators, improvements in nursing care by neonatal intensive care unit nurses, and the whole new subspecialty of neonatology progressively lowered the gestational age for survival. The distinction between clinical care and experimental care was again blurry as neonatologists sought to overcome previously unknown complications, like retinopathy of prematurity resulting from too much oxygen and bronchopulmonary dysplasia from the ventilator. Many babies survived with profound physical and neurological compromise. The ethical dilemmas were continuously present.
Change in the status of children
There is more to the story than philosophy, law, and technology. Pediatric ethics has been profoundly impacted by a change in the status of the children. One change from 50 years ago has been the social response to child abuse.4 Norms changed. Before, fathers pretty much could raise their children any way they saw fit, including corporal punishment. Neighbors didn’t intervene. The proverb was “spare the rod and spoil the child,” but abuse was not motivated by discipline. It was cruel, authoritarian, and demeaning. The landmark article describing the Battered Child Syndrome was published in 1962.5 By 1967, the local Society for the Prevention of Cruelty to Children had become nearly obsolete, but understaffed local government agencies were just beginning to respond. In 1974, federal action produced the Child Abuse Prevention and Treatment Act.6 Medical personnel became mandatory reporters, developed expertise, and, in 2009, child abuse became a boarded subspecialty in pediatrics.
Then, in 1971, a documentary “Who Should Survive?” explored the ethical decision making for babies with birth defects.7 The harms of institutionalization became recognized. The benefits of early intervention and special education have been established. Support for an Individual Education Plan has progressed through successive laws beginning in 1975 until the Individuals with Disabilities Education Improvement Act of 2004.
This is just another example of how ethics develops from a philosophical ideal to a change in social status, followed by consciousness raising, civil rights legislation, enabling legislation, funding, and program development and implementation.
It takes a village of philosophers, activists, lawyers, legislators, physicians, and other experts to implement ethics. There are also countervailing forces. The mainstreaming of children with disabilities is one factor in the movement of children into private schools and the pressure for a voucher system, as advocated by the new Secretary of Education, Betty DeVos.
There also has been a change in the status of children as future providers. Historically, children were relied upon to provide for the parents in their old age. With decreases in infant mortality, the availability of birth control, and legalized abortions, smaller families became the social norm. Worldwide, there has been a marked drop in fertility rates in developed nations. Governmental programs such as Social Security, particularly with the introduction of Medicare in 1965, meant that the elderly were less dependent on their descendants. China found that acceptance of the One Child policy was heavily dependent on convincing parents that the State would provide for them in their old age. The modern political state has assumed duties previously performed by the family.
More recent changes
Pediatric health care is strongly impacted by public health measures. Infant mortality has been reduced by improved nutrition and public health, not medication and surgery. Mass immunization programs were viewed as an appropriate function of civic government.
The introduction of polio vaccine in the 1950s made a large impact. Families lined up at any opportunity to get the vaccine. Polio went from hundreds of thousands of cases of paralysis each summer down to zero cases of wild polio transmitted within the western hemisphere. Measles cases went from 450,000 cases a year in the early 1960s down to zero, until a fraudulent link to autism led to a significant number of parents not immunizing their children. Vaccine refusal, previously a rare ethical issue related to religious liberty, became corrupted by efforts at boutique medicine and alternative facts. In modern America, the ethics of individualism and personal rights have eclipsed civic responsibility. With herd immunity compromised, a blip up to 100 cases of measles per year was histrionically described as a huge epidemic. That spin shows ignorance of the historical record, but the risk was enough for the liberal state of California in 2015 to ban philosophical exemptions to vaccination with one of the strictest state laws in the nation.
Ethics is about values. So, as I look at the changes over 50 years, the areas that have failed to make progress are illuminating. Mental health care for children has not made the same progress achieved with vaccines and cancer therapy. My most recent clinical ethics case involved a teenager who had made a suicidal gesture by taking a handful of pills. The nurses were caught between caring for their patient and meeting the demands of an upset, authoritarian parent in a world where customer satisfaction is critical. I spent much of the night exploring hospital policy and state law. I solicited and listened to widely disparate interpretations of law, medical ethics, and hospital policy from the floor nurse, the nursing supervisor, the nursing staff on the adult inpatient psychiatric unit, three ED docs, a social worker, a government agency, and a judge’s representative. The physician of 1967 was captain of the ship and would not recognize the chaotic teamwork of modern medicine. The exercise showed me how little progress we have made in mental health care for adolescents during my 25 years of practice.
It also reminded me that I have the luxury to debate ethical minutia like vaccine hesitancy and adolescent consent in a world with Syrian refugee camps and starvation in South Sudan. Mahatma Gandhi said, “There are people in the world so hungry that God cannot appear to them except in the form of bread.” That, unfortunately, has not changed in 50 years.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
References
1. www.hhs.gov/ohrp/regulations-and-policy/belmont-report/
2. Pediatrics 1995;95:314-7.
3. JAMA. 1968;205(6):337-40.
4. Family Law Quarterly. 2008 Fall;42(3):449-63.
5. JAMA. 1962;181(1):17-24.
6. National Child Abuse and Neglect Training and Publications Project (2014). The Child Abuse Prevention and Treatment Act: 40 years of safeguarding America’s children. Washington: U.S. Department of Health and Human Services, Children’s Bureau.
7. Kennedy Inst Ethics J. 2006 Sep;16(3):205-24.
The ethics of pediatric health care have changed radically in the past 50 years. “History,” they say, “is written by the victors.” So, if you are not careful, you will only get part of the story. Clinical ethicists learn to seek out, involve, and empower the voices of all stakeholders. To fully appreciate how much things have changed, you must learn more than one side of the story. Indeed, piecing together the history of medical ethics reminds me of the Indian story of five blind men describing an elephant, in which each can only describe a part of an ultimately much bigger animal.
If you ask philosophers about the history of medical ethics, they will point to events 50 years ago as the beginning of the modern era. In the 1960s, physicians tended to be paternalistic authoritarians. Some considered it best not to even tell a patient that he had cancer. There was minimal patient education provided. Medications were prescribed as orders for the patient to follow. Medical research had harmed volunteers, and new protections were needed.
In 1995, the American Academy of Pediatrics Section on Bioethics emphasized the importance of obtaining the child’s assent in addition to the parent’s consent.2 Most states have passed laws permitting minors to give consent for treatment for pregnancy, sexually transmitted diseases, drug addiction, and mental health care.
Technology alters ethics
At the same time, technology has been changing medicine. New life sustaining technologies in the 1960s – such as dialysis and ventilators – created new issues of extreme financial cost, allocation of scarce resources, and even the existential question of when life ends. In 1968, an ad hoc committee at Harvard created criteria for what is colloquially called “brain death.”3 Many landmark legal cases further developed the ethics of end-of-life care.
The boundaries were even less clear at the beginning of life. Technological advances in ventilators, improvements in nursing care by neonatal intensive care unit nurses, and the whole new subspecialty of neonatology progressively lowered the gestational age for survival. The distinction between clinical care and experimental care was again blurry as neonatologists sought to overcome previously unknown complications, like retinopathy of prematurity resulting from too much oxygen and bronchopulmonary dysplasia from the ventilator. Many babies survived with profound physical and neurological compromise. The ethical dilemmas were continuously present.
Change in the status of children
There is more to the story than philosophy, law, and technology. Pediatric ethics has been profoundly impacted by a change in the status of the children. One change from 50 years ago has been the social response to child abuse.4 Norms changed. Before, fathers pretty much could raise their children any way they saw fit, including corporal punishment. Neighbors didn’t intervene. The proverb was “spare the rod and spoil the child,” but abuse was not motivated by discipline. It was cruel, authoritarian, and demeaning. The landmark article describing the Battered Child Syndrome was published in 1962.5 By 1967, the local Society for the Prevention of Cruelty to Children had become nearly obsolete, but understaffed local government agencies were just beginning to respond. In 1974, federal action produced the Child Abuse Prevention and Treatment Act.6 Medical personnel became mandatory reporters, developed expertise, and, in 2009, child abuse became a boarded subspecialty in pediatrics.
Then, in 1971, a documentary “Who Should Survive?” explored the ethical decision making for babies with birth defects.7 The harms of institutionalization became recognized. The benefits of early intervention and special education have been established. Support for an Individual Education Plan has progressed through successive laws beginning in 1975 until the Individuals with Disabilities Education Improvement Act of 2004.
This is just another example of how ethics develops from a philosophical ideal to a change in social status, followed by consciousness raising, civil rights legislation, enabling legislation, funding, and program development and implementation.
It takes a village of philosophers, activists, lawyers, legislators, physicians, and other experts to implement ethics. There are also countervailing forces. The mainstreaming of children with disabilities is one factor in the movement of children into private schools and the pressure for a voucher system, as advocated by the new Secretary of Education, Betty DeVos.
There also has been a change in the status of children as future providers. Historically, children were relied upon to provide for the parents in their old age. With decreases in infant mortality, the availability of birth control, and legalized abortions, smaller families became the social norm. Worldwide, there has been a marked drop in fertility rates in developed nations. Governmental programs such as Social Security, particularly with the introduction of Medicare in 1965, meant that the elderly were less dependent on their descendants. China found that acceptance of the One Child policy was heavily dependent on convincing parents that the State would provide for them in their old age. The modern political state has assumed duties previously performed by the family.
More recent changes
Pediatric health care is strongly impacted by public health measures. Infant mortality has been reduced by improved nutrition and public health, not medication and surgery. Mass immunization programs were viewed as an appropriate function of civic government.
The introduction of polio vaccine in the 1950s made a large impact. Families lined up at any opportunity to get the vaccine. Polio went from hundreds of thousands of cases of paralysis each summer down to zero cases of wild polio transmitted within the western hemisphere. Measles cases went from 450,000 cases a year in the early 1960s down to zero, until a fraudulent link to autism led to a significant number of parents not immunizing their children. Vaccine refusal, previously a rare ethical issue related to religious liberty, became corrupted by efforts at boutique medicine and alternative facts. In modern America, the ethics of individualism and personal rights have eclipsed civic responsibility. With herd immunity compromised, a blip up to 100 cases of measles per year was histrionically described as a huge epidemic. That spin shows ignorance of the historical record, but the risk was enough for the liberal state of California in 2015 to ban philosophical exemptions to vaccination with one of the strictest state laws in the nation.
Ethics is about values. So, as I look at the changes over 50 years, the areas that have failed to make progress are illuminating. Mental health care for children has not made the same progress achieved with vaccines and cancer therapy. My most recent clinical ethics case involved a teenager who had made a suicidal gesture by taking a handful of pills. The nurses were caught between caring for their patient and meeting the demands of an upset, authoritarian parent in a world where customer satisfaction is critical. I spent much of the night exploring hospital policy and state law. I solicited and listened to widely disparate interpretations of law, medical ethics, and hospital policy from the floor nurse, the nursing supervisor, the nursing staff on the adult inpatient psychiatric unit, three ED docs, a social worker, a government agency, and a judge’s representative. The physician of 1967 was captain of the ship and would not recognize the chaotic teamwork of modern medicine. The exercise showed me how little progress we have made in mental health care for adolescents during my 25 years of practice.
It also reminded me that I have the luxury to debate ethical minutia like vaccine hesitancy and adolescent consent in a world with Syrian refugee camps and starvation in South Sudan. Mahatma Gandhi said, “There are people in the world so hungry that God cannot appear to them except in the form of bread.” That, unfortunately, has not changed in 50 years.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
References
1. www.hhs.gov/ohrp/regulations-and-policy/belmont-report/
2. Pediatrics 1995;95:314-7.
3. JAMA. 1968;205(6):337-40.
4. Family Law Quarterly. 2008 Fall;42(3):449-63.
5. JAMA. 1962;181(1):17-24.
6. National Child Abuse and Neglect Training and Publications Project (2014). The Child Abuse Prevention and Treatment Act: 40 years of safeguarding America’s children. Washington: U.S. Department of Health and Human Services, Children’s Bureau.
7. Kennedy Inst Ethics J. 2006 Sep;16(3):205-24.
The ethics of pediatric health care have changed radically in the past 50 years. “History,” they say, “is written by the victors.” So, if you are not careful, you will only get part of the story. Clinical ethicists learn to seek out, involve, and empower the voices of all stakeholders. To fully appreciate how much things have changed, you must learn more than one side of the story. Indeed, piecing together the history of medical ethics reminds me of the Indian story of five blind men describing an elephant, in which each can only describe a part of an ultimately much bigger animal.
If you ask philosophers about the history of medical ethics, they will point to events 50 years ago as the beginning of the modern era. In the 1960s, physicians tended to be paternalistic authoritarians. Some considered it best not to even tell a patient that he had cancer. There was minimal patient education provided. Medications were prescribed as orders for the patient to follow. Medical research had harmed volunteers, and new protections were needed.
In 1995, the American Academy of Pediatrics Section on Bioethics emphasized the importance of obtaining the child’s assent in addition to the parent’s consent.2 Most states have passed laws permitting minors to give consent for treatment for pregnancy, sexually transmitted diseases, drug addiction, and mental health care.
Technology alters ethics
At the same time, technology has been changing medicine. New life sustaining technologies in the 1960s – such as dialysis and ventilators – created new issues of extreme financial cost, allocation of scarce resources, and even the existential question of when life ends. In 1968, an ad hoc committee at Harvard created criteria for what is colloquially called “brain death.”3 Many landmark legal cases further developed the ethics of end-of-life care.
The boundaries were even less clear at the beginning of life. Technological advances in ventilators, improvements in nursing care by neonatal intensive care unit nurses, and the whole new subspecialty of neonatology progressively lowered the gestational age for survival. The distinction between clinical care and experimental care was again blurry as neonatologists sought to overcome previously unknown complications, like retinopathy of prematurity resulting from too much oxygen and bronchopulmonary dysplasia from the ventilator. Many babies survived with profound physical and neurological compromise. The ethical dilemmas were continuously present.
Change in the status of children
There is more to the story than philosophy, law, and technology. Pediatric ethics has been profoundly impacted by a change in the status of the children. One change from 50 years ago has been the social response to child abuse.4 Norms changed. Before, fathers pretty much could raise their children any way they saw fit, including corporal punishment. Neighbors didn’t intervene. The proverb was “spare the rod and spoil the child,” but abuse was not motivated by discipline. It was cruel, authoritarian, and demeaning. The landmark article describing the Battered Child Syndrome was published in 1962.5 By 1967, the local Society for the Prevention of Cruelty to Children had become nearly obsolete, but understaffed local government agencies were just beginning to respond. In 1974, federal action produced the Child Abuse Prevention and Treatment Act.6 Medical personnel became mandatory reporters, developed expertise, and, in 2009, child abuse became a boarded subspecialty in pediatrics.
Then, in 1971, a documentary “Who Should Survive?” explored the ethical decision making for babies with birth defects.7 The harms of institutionalization became recognized. The benefits of early intervention and special education have been established. Support for an Individual Education Plan has progressed through successive laws beginning in 1975 until the Individuals with Disabilities Education Improvement Act of 2004.
This is just another example of how ethics develops from a philosophical ideal to a change in social status, followed by consciousness raising, civil rights legislation, enabling legislation, funding, and program development and implementation.
It takes a village of philosophers, activists, lawyers, legislators, physicians, and other experts to implement ethics. There are also countervailing forces. The mainstreaming of children with disabilities is one factor in the movement of children into private schools and the pressure for a voucher system, as advocated by the new Secretary of Education, Betty DeVos.
There also has been a change in the status of children as future providers. Historically, children were relied upon to provide for the parents in their old age. With decreases in infant mortality, the availability of birth control, and legalized abortions, smaller families became the social norm. Worldwide, there has been a marked drop in fertility rates in developed nations. Governmental programs such as Social Security, particularly with the introduction of Medicare in 1965, meant that the elderly were less dependent on their descendants. China found that acceptance of the One Child policy was heavily dependent on convincing parents that the State would provide for them in their old age. The modern political state has assumed duties previously performed by the family.
More recent changes
Pediatric health care is strongly impacted by public health measures. Infant mortality has been reduced by improved nutrition and public health, not medication and surgery. Mass immunization programs were viewed as an appropriate function of civic government.
The introduction of polio vaccine in the 1950s made a large impact. Families lined up at any opportunity to get the vaccine. Polio went from hundreds of thousands of cases of paralysis each summer down to zero cases of wild polio transmitted within the western hemisphere. Measles cases went from 450,000 cases a year in the early 1960s down to zero, until a fraudulent link to autism led to a significant number of parents not immunizing their children. Vaccine refusal, previously a rare ethical issue related to religious liberty, became corrupted by efforts at boutique medicine and alternative facts. In modern America, the ethics of individualism and personal rights have eclipsed civic responsibility. With herd immunity compromised, a blip up to 100 cases of measles per year was histrionically described as a huge epidemic. That spin shows ignorance of the historical record, but the risk was enough for the liberal state of California in 2015 to ban philosophical exemptions to vaccination with one of the strictest state laws in the nation.
Ethics is about values. So, as I look at the changes over 50 years, the areas that have failed to make progress are illuminating. Mental health care for children has not made the same progress achieved with vaccines and cancer therapy. My most recent clinical ethics case involved a teenager who had made a suicidal gesture by taking a handful of pills. The nurses were caught between caring for their patient and meeting the demands of an upset, authoritarian parent in a world where customer satisfaction is critical. I spent much of the night exploring hospital policy and state law. I solicited and listened to widely disparate interpretations of law, medical ethics, and hospital policy from the floor nurse, the nursing supervisor, the nursing staff on the adult inpatient psychiatric unit, three ED docs, a social worker, a government agency, and a judge’s representative. The physician of 1967 was captain of the ship and would not recognize the chaotic teamwork of modern medicine. The exercise showed me how little progress we have made in mental health care for adolescents during my 25 years of practice.
It also reminded me that I have the luxury to debate ethical minutia like vaccine hesitancy and adolescent consent in a world with Syrian refugee camps and starvation in South Sudan. Mahatma Gandhi said, “There are people in the world so hungry that God cannot appear to them except in the form of bread.” That, unfortunately, has not changed in 50 years.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
References
1. www.hhs.gov/ohrp/regulations-and-policy/belmont-report/
2. Pediatrics 1995;95:314-7.
3. JAMA. 1968;205(6):337-40.
4. Family Law Quarterly. 2008 Fall;42(3):449-63.
5. JAMA. 1962;181(1):17-24.
6. National Child Abuse and Neglect Training and Publications Project (2014). The Child Abuse Prevention and Treatment Act: 40 years of safeguarding America’s children. Washington: U.S. Department of Health and Human Services, Children’s Bureau.
7. Kennedy Inst Ethics J. 2006 Sep;16(3):205-24.