User login
Time to revise your HIV testing routine
The CDC now recommends that clinicians:
- Do HIV testing in all health care settings after the patient is notified that testing will be performed (unless the patient declines).
- Test high-risk patients annually.
- Discontinue use of a separate written consent for HIV testing, if allowed by state law. General consent for medical care should be considered sufficient.
- Drop the requirement that prevention counseling be conducted with HIV testing.
- Include HIV testing in the routine panel of prenatal screening tests for all pregnant women.
- Perform a repeat test on women in their third trimester in regions with elevated rates of HIV infection among pregnant women.
Should all adults and adolescents be screened for HIV? Do all persons at high risk deserve annual screening? The Centers for Disease Control and Prevention thinks so, but the US Preventive Services Task Force takes a less aggressive stance. The 2 agencies looked at the evidence and interpreted it differently—and likewise we must each decide what is best for our own patients and community.
Routine screening is one of several recently revised recommendations from the CDC (at right).1 Though the CDC has historically taken a cautious approach to HIV testing, the winds appear to be changing. The reasons:
- Risk-based screening did not reduce incidence. The previous approach—targeted counseling and testing—has not led to a decline in HIV incidence—it has hovered at around 40,000 cases per year for over a decade.2
- An estimated one fourth of HIV-positive people in the US don’t know their status, and thus are at increased risk of transmitting the disease to others.
- Risk-based screening failed to detect many who are HIV-infected because patients either don’t appreciate—or don’t want to acknowledge—their risks.3,4
- Risk-based screening failed to detect many HIV-infected pregnant women, leading to preventable infection in newborns; routine opt-out testing has been more successful.5
- Highly active antiretroviral therapy has had marked success in reducing mortality from HIV infection. Chemoprophylaxis has proven benefits for preventing certain opportunistic infections.6,7
Removing barriers to testing
The CDC is also advising clinicians that requiring pretest counseling or a separate written consent is a barrier to testing. Clinicians still should inform patients that HIV testing is being conducted and that they have a right to refuse. There is evidence, though, that making the test routine reduces its stigma and increases acceptance.8-11
Evidence also indicates that preventive counseling is very effective in reducing risky behavior among those who are HIV-positive. It’s unclear, however, whether such counseling is effective among those who are HIV-negative.12
Thus, the CDC’s new approach stresses finding those who are infected, getting them medical care, and lowering their risk of transmitting infection to others.
If a pregnant women refuses HIV testing, ask why
The new CDC recommendations take an especially aggressive approach to screening pregnant women, stating that women who refuse testing should be questioned about their reasons for refusal and counseled about the benefits of the test.
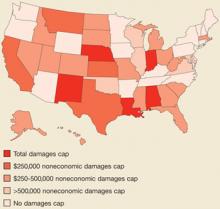
The CDC advises repeat testing in the third trimester, in areas of increased risk—which includes 20 states1—and for pregnant women with individual risk factors, as well as those who receive care in facilities with rates of infection of 1 per 1000 women screened. The CDC also urges rapid HIV testing during labor, in women who were not tested during pregnancy, and on newborns whose mothers were not tested during pregnancy or labor.
USPSTF is less aggressive
The USPSTF13 does not recommend for or against testing persons who are not at high risk (TABLE). Both the CDC and the USPSTF recognize that routine screening is probably warranted in populations with HIV prevalence of 1/1000 or greater. However, the CDC recommends routine screening in all settings until there is evidence that the site or population-specific prevalence is lower than this threshold, while the USPSTF simply states that routine screening may be warranted in populations with a prevalence above this level.
TABLE
USPSTF vs CDC recommendations on HIV testing
| GROUP | USPSTF | CDC |
|---|---|---|
| High-risk adolescents | Recommends testing, no frequency mentioned | Recommends annual testing and before starting a new sexual relationship |
| High-risk adults | Recommends testing, no frequency mentioned | Recommends annual testing as well as before starting a new sexual relationship |
| Adolescents not at high risk | No recommendation for or against | Recommends testing, no frequency mentioned, and testing before starting a new sexual relationship. |
| Adults not at high risk | No recommendation for or against | Recommends testing, no frequency mentioned. recommends testing before starting a new sexual relationship. |
| Pregnant women | Recommends testing | Recommends testing at first visit, repeat test in the third trimester in regions with high rates of HIV infection in pregnant women. |
| Written consent | Does not comment about | Recommends against |
The take-away message
It’s time to review both sets of guidelines and adopt HIV testing policies that are most appropriate for your clinical and community situation, and that meet state laws, many of which still require separate written consent and pretest counseling.
Correspondence
Doug Campos-outcalt, MD, MPA, 4001 N. Third Street #415, phoenix, AZ 85012. [email protected]
1. Branson BM, Handsfield HH, Lampe MA, et al. CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR Recomm Rep 2006;55(RR-14):1-17.Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm. Accessed on March 16, 2007.
2. CDC. US HIV and AIDS cases reported through December 2001. HIV/AIDS Surveillance Report 2001;13(2). Available at: www.cdc.gov/hiv/stats/hasr1302.htm. Accessed on March 13, 2007.
3. Institute of Medicine No Time to Lose: Getting More from HIV Prevention. Washington, DC: National Academy Press; 2001.
4. Peterman TA, Todd KA, Mupanduki I. Opportunities for targeting publicly funded human immunodeficiency virus counseling and testing. J Acquir Immune Defic Syndr Hum Retrovirol 1996;12:69-74.
5. CDC. HIV testing among pregnant women—US and Canada, 1998–2001. MMWR Morb Mortal Wkly Rep 2002;51:1013-1016.
6. McNaghten AD, Hanson DL, Jones JL, Dworkin MS, Ward JW. Effects of antiretroviral therapy and opportunistic illness primary chemoprophylaxis on survival after AIDS diagnosis. Adult/Adolescent Spectrum of Disease Group. AIDS 1999;13:1687-1695.
7. Palella FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338:853-860.
8. Irwin KL, Valdiserri RO, Holmberg SD. The acceptability of voluntary HIV antibody testing in the United States: a decade of lessons learned. AIDS 1996;10:1707-1717.
9. Hutchinson AB, Corbie-Smith G, Thomas SB, et al. Understanding the patient’s perspective on rapid and routine HIV testing in an inner-city urgent care center. AIDS Educ Prev 2004;16:101-114.
10. Spielberg F, Branson BM, Goldbaum GM, et al. Overcoming barriers to HIV testing: p for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr 2003;32:318-328.
11. Copenhaver MM, Fisher JD. Experts outline ways to decrease the decade-long yearly rate of 40,000 new HIV infections in the US. AIDS Behav 2006;10:105-114.
12. Weinhard LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a metanalytic review of published research 1985–1997. Am J Public Health 1999;89:1397-1405.
13. USPSTF. Recommendation statement: Screening for HIV. Available at: www.ahrq.gov/clinic/uspstf05/hiv/hivrs.htm#clinical. Accessed on March 13, 2007.
The CDC now recommends that clinicians:
- Do HIV testing in all health care settings after the patient is notified that testing will be performed (unless the patient declines).
- Test high-risk patients annually.
- Discontinue use of a separate written consent for HIV testing, if allowed by state law. General consent for medical care should be considered sufficient.
- Drop the requirement that prevention counseling be conducted with HIV testing.
- Include HIV testing in the routine panel of prenatal screening tests for all pregnant women.
- Perform a repeat test on women in their third trimester in regions with elevated rates of HIV infection among pregnant women.
Should all adults and adolescents be screened for HIV? Do all persons at high risk deserve annual screening? The Centers for Disease Control and Prevention thinks so, but the US Preventive Services Task Force takes a less aggressive stance. The 2 agencies looked at the evidence and interpreted it differently—and likewise we must each decide what is best for our own patients and community.
Routine screening is one of several recently revised recommendations from the CDC (at right).1 Though the CDC has historically taken a cautious approach to HIV testing, the winds appear to be changing. The reasons:
- Risk-based screening did not reduce incidence. The previous approach—targeted counseling and testing—has not led to a decline in HIV incidence—it has hovered at around 40,000 cases per year for over a decade.2
- An estimated one fourth of HIV-positive people in the US don’t know their status, and thus are at increased risk of transmitting the disease to others.
- Risk-based screening failed to detect many who are HIV-infected because patients either don’t appreciate—or don’t want to acknowledge—their risks.3,4
- Risk-based screening failed to detect many HIV-infected pregnant women, leading to preventable infection in newborns; routine opt-out testing has been more successful.5
- Highly active antiretroviral therapy has had marked success in reducing mortality from HIV infection. Chemoprophylaxis has proven benefits for preventing certain opportunistic infections.6,7
Removing barriers to testing
The CDC is also advising clinicians that requiring pretest counseling or a separate written consent is a barrier to testing. Clinicians still should inform patients that HIV testing is being conducted and that they have a right to refuse. There is evidence, though, that making the test routine reduces its stigma and increases acceptance.8-11
Evidence also indicates that preventive counseling is very effective in reducing risky behavior among those who are HIV-positive. It’s unclear, however, whether such counseling is effective among those who are HIV-negative.12
Thus, the CDC’s new approach stresses finding those who are infected, getting them medical care, and lowering their risk of transmitting infection to others.
If a pregnant women refuses HIV testing, ask why
The new CDC recommendations take an especially aggressive approach to screening pregnant women, stating that women who refuse testing should be questioned about their reasons for refusal and counseled about the benefits of the test.
The CDC advises repeat testing in the third trimester, in areas of increased risk—which includes 20 states1—and for pregnant women with individual risk factors, as well as those who receive care in facilities with rates of infection of 1 per 1000 women screened. The CDC also urges rapid HIV testing during labor, in women who were not tested during pregnancy, and on newborns whose mothers were not tested during pregnancy or labor.
USPSTF is less aggressive
The USPSTF13 does not recommend for or against testing persons who are not at high risk (TABLE). Both the CDC and the USPSTF recognize that routine screening is probably warranted in populations with HIV prevalence of 1/1000 or greater. However, the CDC recommends routine screening in all settings until there is evidence that the site or population-specific prevalence is lower than this threshold, while the USPSTF simply states that routine screening may be warranted in populations with a prevalence above this level.
TABLE
USPSTF vs CDC recommendations on HIV testing
| GROUP | USPSTF | CDC |
|---|---|---|
| High-risk adolescents | Recommends testing, no frequency mentioned | Recommends annual testing and before starting a new sexual relationship |
| High-risk adults | Recommends testing, no frequency mentioned | Recommends annual testing as well as before starting a new sexual relationship |
| Adolescents not at high risk | No recommendation for or against | Recommends testing, no frequency mentioned, and testing before starting a new sexual relationship. |
| Adults not at high risk | No recommendation for or against | Recommends testing, no frequency mentioned. recommends testing before starting a new sexual relationship. |
| Pregnant women | Recommends testing | Recommends testing at first visit, repeat test in the third trimester in regions with high rates of HIV infection in pregnant women. |
| Written consent | Does not comment about | Recommends against |
The take-away message
It’s time to review both sets of guidelines and adopt HIV testing policies that are most appropriate for your clinical and community situation, and that meet state laws, many of which still require separate written consent and pretest counseling.
Correspondence
Doug Campos-outcalt, MD, MPA, 4001 N. Third Street #415, phoenix, AZ 85012. [email protected]
The CDC now recommends that clinicians:
- Do HIV testing in all health care settings after the patient is notified that testing will be performed (unless the patient declines).
- Test high-risk patients annually.
- Discontinue use of a separate written consent for HIV testing, if allowed by state law. General consent for medical care should be considered sufficient.
- Drop the requirement that prevention counseling be conducted with HIV testing.
- Include HIV testing in the routine panel of prenatal screening tests for all pregnant women.
- Perform a repeat test on women in their third trimester in regions with elevated rates of HIV infection among pregnant women.
Should all adults and adolescents be screened for HIV? Do all persons at high risk deserve annual screening? The Centers for Disease Control and Prevention thinks so, but the US Preventive Services Task Force takes a less aggressive stance. The 2 agencies looked at the evidence and interpreted it differently—and likewise we must each decide what is best for our own patients and community.
Routine screening is one of several recently revised recommendations from the CDC (at right).1 Though the CDC has historically taken a cautious approach to HIV testing, the winds appear to be changing. The reasons:
- Risk-based screening did not reduce incidence. The previous approach—targeted counseling and testing—has not led to a decline in HIV incidence—it has hovered at around 40,000 cases per year for over a decade.2
- An estimated one fourth of HIV-positive people in the US don’t know their status, and thus are at increased risk of transmitting the disease to others.
- Risk-based screening failed to detect many who are HIV-infected because patients either don’t appreciate—or don’t want to acknowledge—their risks.3,4
- Risk-based screening failed to detect many HIV-infected pregnant women, leading to preventable infection in newborns; routine opt-out testing has been more successful.5
- Highly active antiretroviral therapy has had marked success in reducing mortality from HIV infection. Chemoprophylaxis has proven benefits for preventing certain opportunistic infections.6,7
Removing barriers to testing
The CDC is also advising clinicians that requiring pretest counseling or a separate written consent is a barrier to testing. Clinicians still should inform patients that HIV testing is being conducted and that they have a right to refuse. There is evidence, though, that making the test routine reduces its stigma and increases acceptance.8-11
Evidence also indicates that preventive counseling is very effective in reducing risky behavior among those who are HIV-positive. It’s unclear, however, whether such counseling is effective among those who are HIV-negative.12
Thus, the CDC’s new approach stresses finding those who are infected, getting them medical care, and lowering their risk of transmitting infection to others.
If a pregnant women refuses HIV testing, ask why
The new CDC recommendations take an especially aggressive approach to screening pregnant women, stating that women who refuse testing should be questioned about their reasons for refusal and counseled about the benefits of the test.
The CDC advises repeat testing in the third trimester, in areas of increased risk—which includes 20 states1—and for pregnant women with individual risk factors, as well as those who receive care in facilities with rates of infection of 1 per 1000 women screened. The CDC also urges rapid HIV testing during labor, in women who were not tested during pregnancy, and on newborns whose mothers were not tested during pregnancy or labor.
USPSTF is less aggressive
The USPSTF13 does not recommend for or against testing persons who are not at high risk (TABLE). Both the CDC and the USPSTF recognize that routine screening is probably warranted in populations with HIV prevalence of 1/1000 or greater. However, the CDC recommends routine screening in all settings until there is evidence that the site or population-specific prevalence is lower than this threshold, while the USPSTF simply states that routine screening may be warranted in populations with a prevalence above this level.
TABLE
USPSTF vs CDC recommendations on HIV testing
| GROUP | USPSTF | CDC |
|---|---|---|
| High-risk adolescents | Recommends testing, no frequency mentioned | Recommends annual testing and before starting a new sexual relationship |
| High-risk adults | Recommends testing, no frequency mentioned | Recommends annual testing as well as before starting a new sexual relationship |
| Adolescents not at high risk | No recommendation for or against | Recommends testing, no frequency mentioned, and testing before starting a new sexual relationship. |
| Adults not at high risk | No recommendation for or against | Recommends testing, no frequency mentioned. recommends testing before starting a new sexual relationship. |
| Pregnant women | Recommends testing | Recommends testing at first visit, repeat test in the third trimester in regions with high rates of HIV infection in pregnant women. |
| Written consent | Does not comment about | Recommends against |
The take-away message
It’s time to review both sets of guidelines and adopt HIV testing policies that are most appropriate for your clinical and community situation, and that meet state laws, many of which still require separate written consent and pretest counseling.
Correspondence
Doug Campos-outcalt, MD, MPA, 4001 N. Third Street #415, phoenix, AZ 85012. [email protected]
1. Branson BM, Handsfield HH, Lampe MA, et al. CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR Recomm Rep 2006;55(RR-14):1-17.Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm. Accessed on March 16, 2007.
2. CDC. US HIV and AIDS cases reported through December 2001. HIV/AIDS Surveillance Report 2001;13(2). Available at: www.cdc.gov/hiv/stats/hasr1302.htm. Accessed on March 13, 2007.
3. Institute of Medicine No Time to Lose: Getting More from HIV Prevention. Washington, DC: National Academy Press; 2001.
4. Peterman TA, Todd KA, Mupanduki I. Opportunities for targeting publicly funded human immunodeficiency virus counseling and testing. J Acquir Immune Defic Syndr Hum Retrovirol 1996;12:69-74.
5. CDC. HIV testing among pregnant women—US and Canada, 1998–2001. MMWR Morb Mortal Wkly Rep 2002;51:1013-1016.
6. McNaghten AD, Hanson DL, Jones JL, Dworkin MS, Ward JW. Effects of antiretroviral therapy and opportunistic illness primary chemoprophylaxis on survival after AIDS diagnosis. Adult/Adolescent Spectrum of Disease Group. AIDS 1999;13:1687-1695.
7. Palella FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338:853-860.
8. Irwin KL, Valdiserri RO, Holmberg SD. The acceptability of voluntary HIV antibody testing in the United States: a decade of lessons learned. AIDS 1996;10:1707-1717.
9. Hutchinson AB, Corbie-Smith G, Thomas SB, et al. Understanding the patient’s perspective on rapid and routine HIV testing in an inner-city urgent care center. AIDS Educ Prev 2004;16:101-114.
10. Spielberg F, Branson BM, Goldbaum GM, et al. Overcoming barriers to HIV testing: p for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr 2003;32:318-328.
11. Copenhaver MM, Fisher JD. Experts outline ways to decrease the decade-long yearly rate of 40,000 new HIV infections in the US. AIDS Behav 2006;10:105-114.
12. Weinhard LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a metanalytic review of published research 1985–1997. Am J Public Health 1999;89:1397-1405.
13. USPSTF. Recommendation statement: Screening for HIV. Available at: www.ahrq.gov/clinic/uspstf05/hiv/hivrs.htm#clinical. Accessed on March 13, 2007.
1. Branson BM, Handsfield HH, Lampe MA, et al. CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR Recomm Rep 2006;55(RR-14):1-17.Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm. Accessed on March 16, 2007.
2. CDC. US HIV and AIDS cases reported through December 2001. HIV/AIDS Surveillance Report 2001;13(2). Available at: www.cdc.gov/hiv/stats/hasr1302.htm. Accessed on March 13, 2007.
3. Institute of Medicine No Time to Lose: Getting More from HIV Prevention. Washington, DC: National Academy Press; 2001.
4. Peterman TA, Todd KA, Mupanduki I. Opportunities for targeting publicly funded human immunodeficiency virus counseling and testing. J Acquir Immune Defic Syndr Hum Retrovirol 1996;12:69-74.
5. CDC. HIV testing among pregnant women—US and Canada, 1998–2001. MMWR Morb Mortal Wkly Rep 2002;51:1013-1016.
6. McNaghten AD, Hanson DL, Jones JL, Dworkin MS, Ward JW. Effects of antiretroviral therapy and opportunistic illness primary chemoprophylaxis on survival after AIDS diagnosis. Adult/Adolescent Spectrum of Disease Group. AIDS 1999;13:1687-1695.
7. Palella FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338:853-860.
8. Irwin KL, Valdiserri RO, Holmberg SD. The acceptability of voluntary HIV antibody testing in the United States: a decade of lessons learned. AIDS 1996;10:1707-1717.
9. Hutchinson AB, Corbie-Smith G, Thomas SB, et al. Understanding the patient’s perspective on rapid and routine HIV testing in an inner-city urgent care center. AIDS Educ Prev 2004;16:101-114.
10. Spielberg F, Branson BM, Goldbaum GM, et al. Overcoming barriers to HIV testing: p for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr 2003;32:318-328.
11. Copenhaver MM, Fisher JD. Experts outline ways to decrease the decade-long yearly rate of 40,000 new HIV infections in the US. AIDS Behav 2006;10:105-114.
12. Weinhard LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a metanalytic review of published research 1985–1997. Am J Public Health 1999;89:1397-1405.
13. USPSTF. Recommendation statement: Screening for HIV. Available at: www.ahrq.gov/clinic/uspstf05/hiv/hivrs.htm#clinical. Accessed on March 13, 2007.
The preteen visit: An opportunity for prevention
All early adolescents should visit a physician at age 11 or 12 years to receive a set of recommended vaccines. Two vaccines are recommended for boys in this age group—quadrivalent meningococcal conjugate vaccine (MCV4) and tetanus toxoid, reduced diphtheria, and acellular pertussis vaccine (Tdap). Three vaccines are recommended for girls—MCV4, Tdap, and human papilloma virus (HPV) vaccine.
In addition, 2 doses of varicella vaccine are now recommended before age 5 years; both boys and girls at age 11 or 12 who have received only 1 dose should be given a second. TABLE 1 contains details on each recommended vaccine.
TABLE 1
Vaccines recommended for early adolescents
| VACCINE | ROUTE | SCHEDULE | CONTRAINDICATIONS* | PRECAUTIONS |
|---|---|---|---|---|
| MCV4 | IM | 1 dose | Moderate to severe illness | |
| Tdap | IM | 1 dose, may need other doses of Td to complete a tetanus and diphtheria series | Encephalopathy within 7 days of previous vaccine not attributed to other cause | Hypersensitivity with prior tetanus toxoid |
| Progressive neurological disorder | ||||
| Latex allergy | ||||
| Guillain-Barré syndrome within 6 weeks of a previous dose of tetanus toxoid | ||||
| Acute moderate to severe illness | ||||
| HPV | IM | 3 doses at months 0, 2, and 6 | History of hypersensitivity | Defer for moderate to severe illness to yeast |
| Varicella | SQ | 2 doses 3 months apart (1 month interval is acceptable) | Pregnancy | Moderate to severe illness |
| Severe suppression of cellular immunity | Receipt of antibody containing blood product in the preceding 11 months | |||
| Complete information for each vaccine can be located on the CDC web site at: www.cdc.gov/node.do/id/0900f3ec8005df1f. | ||||
| * All vaccines have as a contraindication a previous anaphylactic reaction to the vaccine or vaccine components. | ||||
| Details on contraindications can be found at: www.cdc.gov/nip/recs/contraindications_vacc.htm#var. | ||||
Meningococcal vaccine
Quadrivalent meningococcal conjugate vaccine (Menactra) contains antigens for 4 meningococcal groups (A, C, Y, W-135), and is licensed for ages 11 to 55 years. The Advisory Committee on Immunization Practices (ACIP) recommends that all preteens receive 1 dose at age 11 or 12. Unvaccinated older children should receive a dose before entering high school; unvaccinated college freshmen living in dorms should also be vaccinated.
Because of a shortage of vaccine, the Centers for Disease Control and Prevention (CDC) had recommended a delay in the implementation of routine vaccination at age 11 and 12. The supply situation has now corrected, and this recommendation has been rescinded.
There have been 17 cases of Guillain-Barré syndrome appearing in adolescents and young adults within 33 days of receiving MCV4. The possibility of a cause-and-effect relationship is under investigation. The CDC recommends that preadolescents and adolescents who have a history of Guillain-Barré should not receive MCV4 unless they are college freshmen who live in dorms.
Tetanus/diphtheria/pertussis vaccine
There are 2 Tdap products, one licensed for ages 10 to 18 years (Boostrix), the other for ages 11 to 64 (Adacel). The ACIP recommends a single dose of Tdap for those aged 11 to 18, preferably at age 11 or 12. The optimal interval from the last tetanus and diphtheria toxoid (TD or Td) is 5 years but a shorter interval is acceptable. Thereafter, Td boosters are recommended every 10 years. If an 11- or 12-year-old has not previously received a complete series of a tetanus toxoid, diphtheria product tetanus and diphtheria vaccines, they should be given the recommended number of doses—only one of which should be Tdap, the others Td. The number and timing of doses can be found at www.cdc.gov/mmwr/preview/mmwrhtml/rr55e223a5.htm.
Human papilloma virus vaccine
The HPV vaccine (Gardasil) is licensed only for females aged 9 to 26 years, and is the first vaccine for the prevention of cervical cancer. It protects against HPV types 6, 11, 16, and 18, which are the cause of approximately 80% of cervical cancers. The ACIP recommends routine administration for all females between ages 9 and 26, preferably before the onset of sexual activity. The vaccine requires 3 doses at months 0, 2, and 6; it can be administered concurrently with MCV4, Tdap, and Td.
Varicella vaccine
Two doses of varicella are now recommended for all children at ages 12 to 15 months and 4 to 6 years—the same as for the measles, mumps, and rubella vaccine (MMR). A new MMRV product (Proquad) could reduce the number of injections needed at these ages.
Adolescents and adults who are not immune to varicella should receive 2 doses of vaccine 3 months apart, or 1 dose if they have been vaccinated with a single dose of varicella vaccine. Immunity to varicella is defined as birth in the US prior to 1980, 2 doses of varicella vaccine, or having had a diagnosed case of chickenpox or shingles.
Other interventions
This expanding list of recommended vaccines should create an incentive for parents to bring their preteen children to visit a physician. The American College of Physicians (ACP) recommendations are built on the assumption that these vaccines should be part of a routine preventive visit at this age group.
If preteens do visit a physician more frequently, it will provide an opportunity for other health care maintenance interventions, such as measuring height, weight, and blood pressure and providing health education on diet, physical activity, and substance abuse. Unfortunately, the evidence base for the effectiveness of preventive interventions at this age is very weak.
TABLE 2 lists the interventions for the age group 11 to 12 years that have been evaluated by the US Preventive Services Task Force (USPSTF). This is not a comprehensive list of all possible preventive interventions for young adolescents, only those that have been evaluated by the USPSTF. Those with either an A (strongly recommend) or B (recommend) recommendation are screening tests related to risks involved with sexual activity and will not apply to all young adolescents. Some of those with a D recommendation (recommend against) will surprise many physicians, as they have historically been included in various screening guidelines.
TABLE 2
US Preventive Services Task Force recommendations on interventions for adolescents
Recommend for
|
Recommend Against
|
Insufficient Evidence to Recommend For or Against
|
Reports in Progress
|
For a listing of vaccine components and contraindications see: www.cdc.gov/nip/recs/contraindications.htm
Vaccine information statements are found at: www.cdc.gov/nip/publications/VIS/default.htm#hpv
For a useful chart with information on all vaccines go to: www.cdc.gov/nip/vaccine/vac-chart-hcp.htm
General information on immunizations is on the CDC web site: www.cdc.gov/mmwr/preview/mmwrhtml/rr5102a1.htm
The United States Preventive Services Task Force lists current recommendations, rationales, and clinical considerations at: www.ahrq.gov/clinic/uspstfix.htm
The bulk of the potential interventions are in the I category (insufficient evidence to recommend for or against) or are the subject of an ongoing evaluation. Many of these receive this rating not because the targeted behavior is in question but because it is unclear how effective physician counseling in a clinical encounter is in changing these behaviors—for example, avoidance of tobacco products and maintenance of ideal weight. Many providers will probably choose to provide young adolescents advice on these topics in spite of the meager evidence available.
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
All early adolescents should visit a physician at age 11 or 12 years to receive a set of recommended vaccines. Two vaccines are recommended for boys in this age group—quadrivalent meningococcal conjugate vaccine (MCV4) and tetanus toxoid, reduced diphtheria, and acellular pertussis vaccine (Tdap). Three vaccines are recommended for girls—MCV4, Tdap, and human papilloma virus (HPV) vaccine.
In addition, 2 doses of varicella vaccine are now recommended before age 5 years; both boys and girls at age 11 or 12 who have received only 1 dose should be given a second. TABLE 1 contains details on each recommended vaccine.
TABLE 1
Vaccines recommended for early adolescents
| VACCINE | ROUTE | SCHEDULE | CONTRAINDICATIONS* | PRECAUTIONS |
|---|---|---|---|---|
| MCV4 | IM | 1 dose | Moderate to severe illness | |
| Tdap | IM | 1 dose, may need other doses of Td to complete a tetanus and diphtheria series | Encephalopathy within 7 days of previous vaccine not attributed to other cause | Hypersensitivity with prior tetanus toxoid |
| Progressive neurological disorder | ||||
| Latex allergy | ||||
| Guillain-Barré syndrome within 6 weeks of a previous dose of tetanus toxoid | ||||
| Acute moderate to severe illness | ||||
| HPV | IM | 3 doses at months 0, 2, and 6 | History of hypersensitivity | Defer for moderate to severe illness to yeast |
| Varicella | SQ | 2 doses 3 months apart (1 month interval is acceptable) | Pregnancy | Moderate to severe illness |
| Severe suppression of cellular immunity | Receipt of antibody containing blood product in the preceding 11 months | |||
| Complete information for each vaccine can be located on the CDC web site at: www.cdc.gov/node.do/id/0900f3ec8005df1f. | ||||
| * All vaccines have as a contraindication a previous anaphylactic reaction to the vaccine or vaccine components. | ||||
| Details on contraindications can be found at: www.cdc.gov/nip/recs/contraindications_vacc.htm#var. | ||||
Meningococcal vaccine
Quadrivalent meningococcal conjugate vaccine (Menactra) contains antigens for 4 meningococcal groups (A, C, Y, W-135), and is licensed for ages 11 to 55 years. The Advisory Committee on Immunization Practices (ACIP) recommends that all preteens receive 1 dose at age 11 or 12. Unvaccinated older children should receive a dose before entering high school; unvaccinated college freshmen living in dorms should also be vaccinated.
Because of a shortage of vaccine, the Centers for Disease Control and Prevention (CDC) had recommended a delay in the implementation of routine vaccination at age 11 and 12. The supply situation has now corrected, and this recommendation has been rescinded.
There have been 17 cases of Guillain-Barré syndrome appearing in adolescents and young adults within 33 days of receiving MCV4. The possibility of a cause-and-effect relationship is under investigation. The CDC recommends that preadolescents and adolescents who have a history of Guillain-Barré should not receive MCV4 unless they are college freshmen who live in dorms.
Tetanus/diphtheria/pertussis vaccine
There are 2 Tdap products, one licensed for ages 10 to 18 years (Boostrix), the other for ages 11 to 64 (Adacel). The ACIP recommends a single dose of Tdap for those aged 11 to 18, preferably at age 11 or 12. The optimal interval from the last tetanus and diphtheria toxoid (TD or Td) is 5 years but a shorter interval is acceptable. Thereafter, Td boosters are recommended every 10 years. If an 11- or 12-year-old has not previously received a complete series of a tetanus toxoid, diphtheria product tetanus and diphtheria vaccines, they should be given the recommended number of doses—only one of which should be Tdap, the others Td. The number and timing of doses can be found at www.cdc.gov/mmwr/preview/mmwrhtml/rr55e223a5.htm.
Human papilloma virus vaccine
The HPV vaccine (Gardasil) is licensed only for females aged 9 to 26 years, and is the first vaccine for the prevention of cervical cancer. It protects against HPV types 6, 11, 16, and 18, which are the cause of approximately 80% of cervical cancers. The ACIP recommends routine administration for all females between ages 9 and 26, preferably before the onset of sexual activity. The vaccine requires 3 doses at months 0, 2, and 6; it can be administered concurrently with MCV4, Tdap, and Td.
Varicella vaccine
Two doses of varicella are now recommended for all children at ages 12 to 15 months and 4 to 6 years—the same as for the measles, mumps, and rubella vaccine (MMR). A new MMRV product (Proquad) could reduce the number of injections needed at these ages.
Adolescents and adults who are not immune to varicella should receive 2 doses of vaccine 3 months apart, or 1 dose if they have been vaccinated with a single dose of varicella vaccine. Immunity to varicella is defined as birth in the US prior to 1980, 2 doses of varicella vaccine, or having had a diagnosed case of chickenpox or shingles.
Other interventions
This expanding list of recommended vaccines should create an incentive for parents to bring their preteen children to visit a physician. The American College of Physicians (ACP) recommendations are built on the assumption that these vaccines should be part of a routine preventive visit at this age group.
If preteens do visit a physician more frequently, it will provide an opportunity for other health care maintenance interventions, such as measuring height, weight, and blood pressure and providing health education on diet, physical activity, and substance abuse. Unfortunately, the evidence base for the effectiveness of preventive interventions at this age is very weak.
TABLE 2 lists the interventions for the age group 11 to 12 years that have been evaluated by the US Preventive Services Task Force (USPSTF). This is not a comprehensive list of all possible preventive interventions for young adolescents, only those that have been evaluated by the USPSTF. Those with either an A (strongly recommend) or B (recommend) recommendation are screening tests related to risks involved with sexual activity and will not apply to all young adolescents. Some of those with a D recommendation (recommend against) will surprise many physicians, as they have historically been included in various screening guidelines.
TABLE 2
US Preventive Services Task Force recommendations on interventions for adolescents
Recommend for
|
Recommend Against
|
Insufficient Evidence to Recommend For or Against
|
Reports in Progress
|
For a listing of vaccine components and contraindications see: www.cdc.gov/nip/recs/contraindications.htm
Vaccine information statements are found at: www.cdc.gov/nip/publications/VIS/default.htm#hpv
For a useful chart with information on all vaccines go to: www.cdc.gov/nip/vaccine/vac-chart-hcp.htm
General information on immunizations is on the CDC web site: www.cdc.gov/mmwr/preview/mmwrhtml/rr5102a1.htm
The United States Preventive Services Task Force lists current recommendations, rationales, and clinical considerations at: www.ahrq.gov/clinic/uspstfix.htm
The bulk of the potential interventions are in the I category (insufficient evidence to recommend for or against) or are the subject of an ongoing evaluation. Many of these receive this rating not because the targeted behavior is in question but because it is unclear how effective physician counseling in a clinical encounter is in changing these behaviors—for example, avoidance of tobacco products and maintenance of ideal weight. Many providers will probably choose to provide young adolescents advice on these topics in spite of the meager evidence available.
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
All early adolescents should visit a physician at age 11 or 12 years to receive a set of recommended vaccines. Two vaccines are recommended for boys in this age group—quadrivalent meningococcal conjugate vaccine (MCV4) and tetanus toxoid, reduced diphtheria, and acellular pertussis vaccine (Tdap). Three vaccines are recommended for girls—MCV4, Tdap, and human papilloma virus (HPV) vaccine.
In addition, 2 doses of varicella vaccine are now recommended before age 5 years; both boys and girls at age 11 or 12 who have received only 1 dose should be given a second. TABLE 1 contains details on each recommended vaccine.
TABLE 1
Vaccines recommended for early adolescents
| VACCINE | ROUTE | SCHEDULE | CONTRAINDICATIONS* | PRECAUTIONS |
|---|---|---|---|---|
| MCV4 | IM | 1 dose | Moderate to severe illness | |
| Tdap | IM | 1 dose, may need other doses of Td to complete a tetanus and diphtheria series | Encephalopathy within 7 days of previous vaccine not attributed to other cause | Hypersensitivity with prior tetanus toxoid |
| Progressive neurological disorder | ||||
| Latex allergy | ||||
| Guillain-Barré syndrome within 6 weeks of a previous dose of tetanus toxoid | ||||
| Acute moderate to severe illness | ||||
| HPV | IM | 3 doses at months 0, 2, and 6 | History of hypersensitivity | Defer for moderate to severe illness to yeast |
| Varicella | SQ | 2 doses 3 months apart (1 month interval is acceptable) | Pregnancy | Moderate to severe illness |
| Severe suppression of cellular immunity | Receipt of antibody containing blood product in the preceding 11 months | |||
| Complete information for each vaccine can be located on the CDC web site at: www.cdc.gov/node.do/id/0900f3ec8005df1f. | ||||
| * All vaccines have as a contraindication a previous anaphylactic reaction to the vaccine or vaccine components. | ||||
| Details on contraindications can be found at: www.cdc.gov/nip/recs/contraindications_vacc.htm#var. | ||||
Meningococcal vaccine
Quadrivalent meningococcal conjugate vaccine (Menactra) contains antigens for 4 meningococcal groups (A, C, Y, W-135), and is licensed for ages 11 to 55 years. The Advisory Committee on Immunization Practices (ACIP) recommends that all preteens receive 1 dose at age 11 or 12. Unvaccinated older children should receive a dose before entering high school; unvaccinated college freshmen living in dorms should also be vaccinated.
Because of a shortage of vaccine, the Centers for Disease Control and Prevention (CDC) had recommended a delay in the implementation of routine vaccination at age 11 and 12. The supply situation has now corrected, and this recommendation has been rescinded.
There have been 17 cases of Guillain-Barré syndrome appearing in adolescents and young adults within 33 days of receiving MCV4. The possibility of a cause-and-effect relationship is under investigation. The CDC recommends that preadolescents and adolescents who have a history of Guillain-Barré should not receive MCV4 unless they are college freshmen who live in dorms.
Tetanus/diphtheria/pertussis vaccine
There are 2 Tdap products, one licensed for ages 10 to 18 years (Boostrix), the other for ages 11 to 64 (Adacel). The ACIP recommends a single dose of Tdap for those aged 11 to 18, preferably at age 11 or 12. The optimal interval from the last tetanus and diphtheria toxoid (TD or Td) is 5 years but a shorter interval is acceptable. Thereafter, Td boosters are recommended every 10 years. If an 11- or 12-year-old has not previously received a complete series of a tetanus toxoid, diphtheria product tetanus and diphtheria vaccines, they should be given the recommended number of doses—only one of which should be Tdap, the others Td. The number and timing of doses can be found at www.cdc.gov/mmwr/preview/mmwrhtml/rr55e223a5.htm.
Human papilloma virus vaccine
The HPV vaccine (Gardasil) is licensed only for females aged 9 to 26 years, and is the first vaccine for the prevention of cervical cancer. It protects against HPV types 6, 11, 16, and 18, which are the cause of approximately 80% of cervical cancers. The ACIP recommends routine administration for all females between ages 9 and 26, preferably before the onset of sexual activity. The vaccine requires 3 doses at months 0, 2, and 6; it can be administered concurrently with MCV4, Tdap, and Td.
Varicella vaccine
Two doses of varicella are now recommended for all children at ages 12 to 15 months and 4 to 6 years—the same as for the measles, mumps, and rubella vaccine (MMR). A new MMRV product (Proquad) could reduce the number of injections needed at these ages.
Adolescents and adults who are not immune to varicella should receive 2 doses of vaccine 3 months apart, or 1 dose if they have been vaccinated with a single dose of varicella vaccine. Immunity to varicella is defined as birth in the US prior to 1980, 2 doses of varicella vaccine, or having had a diagnosed case of chickenpox or shingles.
Other interventions
This expanding list of recommended vaccines should create an incentive for parents to bring their preteen children to visit a physician. The American College of Physicians (ACP) recommendations are built on the assumption that these vaccines should be part of a routine preventive visit at this age group.
If preteens do visit a physician more frequently, it will provide an opportunity for other health care maintenance interventions, such as measuring height, weight, and blood pressure and providing health education on diet, physical activity, and substance abuse. Unfortunately, the evidence base for the effectiveness of preventive interventions at this age is very weak.
TABLE 2 lists the interventions for the age group 11 to 12 years that have been evaluated by the US Preventive Services Task Force (USPSTF). This is not a comprehensive list of all possible preventive interventions for young adolescents, only those that have been evaluated by the USPSTF. Those with either an A (strongly recommend) or B (recommend) recommendation are screening tests related to risks involved with sexual activity and will not apply to all young adolescents. Some of those with a D recommendation (recommend against) will surprise many physicians, as they have historically been included in various screening guidelines.
TABLE 2
US Preventive Services Task Force recommendations on interventions for adolescents
Recommend for
|
Recommend Against
|
Insufficient Evidence to Recommend For or Against
|
Reports in Progress
|
For a listing of vaccine components and contraindications see: www.cdc.gov/nip/recs/contraindications.htm
Vaccine information statements are found at: www.cdc.gov/nip/publications/VIS/default.htm#hpv
For a useful chart with information on all vaccines go to: www.cdc.gov/nip/vaccine/vac-chart-hcp.htm
General information on immunizations is on the CDC web site: www.cdc.gov/mmwr/preview/mmwrhtml/rr5102a1.htm
The United States Preventive Services Task Force lists current recommendations, rationales, and clinical considerations at: www.ahrq.gov/clinic/uspstfix.htm
The bulk of the potential interventions are in the I category (insufficient evidence to recommend for or against) or are the subject of an ongoing evaluation. Many of these receive this rating not because the targeted behavior is in question but because it is unclear how effective physician counseling in a clinical encounter is in changing these behaviors—for example, avoidance of tobacco products and maintenance of ideal weight. Many providers will probably choose to provide young adolescents advice on these topics in spite of the meager evidence available.
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
Endarterectomy for carotid artery stenosis: Who qualifies?
What are the indications for carotid endarterectomy (CE) in the symptomatic patient?
How is symptomatic defined?
What are the indications for CE in the asymptomatic patient?
What is the role of aspirin therapy in these patients?
This guideline reviews the efficacy of carotid endarterectomy for stroke prevention in adults with symptomatic or asymptomatic internal carotid artery stenosis.
Symptomatic is defined as a cerebrovascular event in the carotid distribution (transient ischemic attack or nondisabling stroke) in the previous 6 months.
Indications for or against CE appear in the Practice Recommendations.
GRADE A RECOMMENDATIONS
- Carotid endarterectomy is effective for symptomatic patients with 70% to 99% stenosis. Carotid endarterectomy should not be considered for symptomatic patients with less than 50% stenosis—medical management is preferred. (50%–99% stenosis, Grade B)
- Carotid endarterectomy may be considered for patients between ages 40 to 75 years, with asymptomatic stenosis between 60% to 99%, if there is a 5-year life expectancy and surgical risk is <3%.
- Symptomatic and asymptomatic patients undergoing carotid endarterectomy should receive aspirin (81 or 325 mg) daily prior to surgery and for at least 3 months postoperatively. In the absence of contraindications, it should be continued indefinitely.
GRADE B RECOMMENDATIONS
- Carotid endarterectomy may be considered for symptomatic patients with 50% to 69% stenosis in patients with a 5-year life expectancy and surgical risk <6%.
GRADE C RECOMMENDATION
- Patients with hemispheric transient ischemic attack or cerebrovascular accident had greater benefit from carotid endarterectomy than those with retinal events.
- Patients with severe stenosis and a cerebrovascular event should have carotid endarterectomy within 2 weeks for greatest benefit.
- Contralateral occlusion reduces the benefit of carotid endarterectomy in asymptomatic patients.
- Data are insufficient to recommend other antiplatelet agents perioperatively.
The evidence categories are assessment of therapeutic effectiveness, prevention, and risk assessment. Study outcomes considered are: benefits of carotid endarterectomy for symptomatic patients, benefits for asymptomatic patients, the efficacy within 24 hours in patients with progressing stroke, clinical variables that impact the risk/benefit ratio, the most important radiologic factors impacting the risk/benefit ratio, the ideal dose of aspirin preoperatively, the evidence/practice gap, the likelihood that trial results can be achieved in practice, the benefit of carotid endarterectomy concurrent with or prior to coronary artery bypass grafting, and the optimal time after stroke to perform the surgery. The evidence rating is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Carotid endarterectomy has an important role in the prevention of stroke in patients with internal carotid artery stenosis, since the majority of strokes are ischemic. Strokes can be prevented if a high-grade internal carotid stenosis is corrected. More than 700,000 patients suffer a stroke each year in the US, with 80% related to ischemia (either thrombotic or embolic).2 Most strokes occur after the age of 65, and the risk doubles each decade after the age of 55. Stroke is the third leading cause of death, with only heart disease and cancer killing more people. Strokes cause more serious long-term disabilities than any other illness. The guideline was weakened by lack of cost analysis.
Guideline development and evidence review
A literature search was performed using Ovid Medline for relevant articles published from 1990 to 2001 using the keywords carotid endarterectomy, carotid stenosis, carotid artery diseases, and clinical trials. The Cochrane Library statements on carotid endarterectomy for symptomatic and asymptomatic stenosis from 2004 were reviewed to confirm that additional relevant citations from 2002 to 2004 were identified.
The initial search yielded 1462 citations. This list was reduced by excluding case reports, letters to the editor, review articles without primary data, studies addressing carotid endarterectomy technical issues, case series from a single surgeon, and articles not written in English. Case series from a single institution were included. This narrowed the pertinent list to 186 articles, which were reviewed independently by 2 committee members. The committee also agreed that if a pooled analysis of the major symptomatic carotid endarterectomy studies or if the results of the Asymptomatic Carotid Surgery Trial were published prior to the completion of the committee’s manuscript, these would subsequently be reviewed.
Source for this guideline
Chaturvedi S, Bruno A, Feasby T, Holloway R, Benavente O, Cohen SN, Cote R, Hess D, Saver J, Spence JD, Stern B, Wilterdink J. Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2005; 65:794–801 [27 refs]. Available at: www.neurology.org/cgi/reprint/65/6/794.pdf.
Other guidelines on surgical management of carotid stenosis and stroke
Life after stroke: New Zealand guideline for management of stroke
This comprehensive 2003 guideline is written for New Zealand health care delivery system. It summarizes recommendations for the assessment and management of stroke, transient ischemic attacks, and intracerebral hemorrhage in various locales. The utility of carotid endarterectomy for secondary prevention is reviewed. The recommendations are comparable to the American Academy of Neurology.
Source. New Zealand Guidelines Group. Life after stroke. New Zealand guideline for management of stroke. Wellington, NZ: New Zealand Guidelines Group; 2003: 84 pp [164 refs]. Available at: www.nzgg.org.nz/guidelines/0037/Stroke_Summary.pdf.
1. Ebell M, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-120.
2. National Institute of Neurological Disorders and Stroke. Stroke: Hope through research. 2006. Available at: www.ninds.nih.gov/disorders/stroke/detail_stroke.htm#56 051105. Accessed on March 21, 2006.
CORRESPONDENCE: Keith B. Holten, MD, 825 Locust Street, Wilmington, OH 45177. E-mail: [email protected]
What are the indications for carotid endarterectomy (CE) in the symptomatic patient?
How is symptomatic defined?
What are the indications for CE in the asymptomatic patient?
What is the role of aspirin therapy in these patients?
This guideline reviews the efficacy of carotid endarterectomy for stroke prevention in adults with symptomatic or asymptomatic internal carotid artery stenosis.
Symptomatic is defined as a cerebrovascular event in the carotid distribution (transient ischemic attack or nondisabling stroke) in the previous 6 months.
Indications for or against CE appear in the Practice Recommendations.
GRADE A RECOMMENDATIONS
- Carotid endarterectomy is effective for symptomatic patients with 70% to 99% stenosis. Carotid endarterectomy should not be considered for symptomatic patients with less than 50% stenosis—medical management is preferred. (50%–99% stenosis, Grade B)
- Carotid endarterectomy may be considered for patients between ages 40 to 75 years, with asymptomatic stenosis between 60% to 99%, if there is a 5-year life expectancy and surgical risk is <3%.
- Symptomatic and asymptomatic patients undergoing carotid endarterectomy should receive aspirin (81 or 325 mg) daily prior to surgery and for at least 3 months postoperatively. In the absence of contraindications, it should be continued indefinitely.
GRADE B RECOMMENDATIONS
- Carotid endarterectomy may be considered for symptomatic patients with 50% to 69% stenosis in patients with a 5-year life expectancy and surgical risk <6%.
GRADE C RECOMMENDATION
- Patients with hemispheric transient ischemic attack or cerebrovascular accident had greater benefit from carotid endarterectomy than those with retinal events.
- Patients with severe stenosis and a cerebrovascular event should have carotid endarterectomy within 2 weeks for greatest benefit.
- Contralateral occlusion reduces the benefit of carotid endarterectomy in asymptomatic patients.
- Data are insufficient to recommend other antiplatelet agents perioperatively.
The evidence categories are assessment of therapeutic effectiveness, prevention, and risk assessment. Study outcomes considered are: benefits of carotid endarterectomy for symptomatic patients, benefits for asymptomatic patients, the efficacy within 24 hours in patients with progressing stroke, clinical variables that impact the risk/benefit ratio, the most important radiologic factors impacting the risk/benefit ratio, the ideal dose of aspirin preoperatively, the evidence/practice gap, the likelihood that trial results can be achieved in practice, the benefit of carotid endarterectomy concurrent with or prior to coronary artery bypass grafting, and the optimal time after stroke to perform the surgery. The evidence rating is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Carotid endarterectomy has an important role in the prevention of stroke in patients with internal carotid artery stenosis, since the majority of strokes are ischemic. Strokes can be prevented if a high-grade internal carotid stenosis is corrected. More than 700,000 patients suffer a stroke each year in the US, with 80% related to ischemia (either thrombotic or embolic).2 Most strokes occur after the age of 65, and the risk doubles each decade after the age of 55. Stroke is the third leading cause of death, with only heart disease and cancer killing more people. Strokes cause more serious long-term disabilities than any other illness. The guideline was weakened by lack of cost analysis.
Guideline development and evidence review
A literature search was performed using Ovid Medline for relevant articles published from 1990 to 2001 using the keywords carotid endarterectomy, carotid stenosis, carotid artery diseases, and clinical trials. The Cochrane Library statements on carotid endarterectomy for symptomatic and asymptomatic stenosis from 2004 were reviewed to confirm that additional relevant citations from 2002 to 2004 were identified.
The initial search yielded 1462 citations. This list was reduced by excluding case reports, letters to the editor, review articles without primary data, studies addressing carotid endarterectomy technical issues, case series from a single surgeon, and articles not written in English. Case series from a single institution were included. This narrowed the pertinent list to 186 articles, which were reviewed independently by 2 committee members. The committee also agreed that if a pooled analysis of the major symptomatic carotid endarterectomy studies or if the results of the Asymptomatic Carotid Surgery Trial were published prior to the completion of the committee’s manuscript, these would subsequently be reviewed.
Source for this guideline
Chaturvedi S, Bruno A, Feasby T, Holloway R, Benavente O, Cohen SN, Cote R, Hess D, Saver J, Spence JD, Stern B, Wilterdink J. Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2005; 65:794–801 [27 refs]. Available at: www.neurology.org/cgi/reprint/65/6/794.pdf.
Other guidelines on surgical management of carotid stenosis and stroke
Life after stroke: New Zealand guideline for management of stroke
This comprehensive 2003 guideline is written for New Zealand health care delivery system. It summarizes recommendations for the assessment and management of stroke, transient ischemic attacks, and intracerebral hemorrhage in various locales. The utility of carotid endarterectomy for secondary prevention is reviewed. The recommendations are comparable to the American Academy of Neurology.
Source. New Zealand Guidelines Group. Life after stroke. New Zealand guideline for management of stroke. Wellington, NZ: New Zealand Guidelines Group; 2003: 84 pp [164 refs]. Available at: www.nzgg.org.nz/guidelines/0037/Stroke_Summary.pdf.
What are the indications for carotid endarterectomy (CE) in the symptomatic patient?
How is symptomatic defined?
What are the indications for CE in the asymptomatic patient?
What is the role of aspirin therapy in these patients?
This guideline reviews the efficacy of carotid endarterectomy for stroke prevention in adults with symptomatic or asymptomatic internal carotid artery stenosis.
Symptomatic is defined as a cerebrovascular event in the carotid distribution (transient ischemic attack or nondisabling stroke) in the previous 6 months.
Indications for or against CE appear in the Practice Recommendations.
GRADE A RECOMMENDATIONS
- Carotid endarterectomy is effective for symptomatic patients with 70% to 99% stenosis. Carotid endarterectomy should not be considered for symptomatic patients with less than 50% stenosis—medical management is preferred. (50%–99% stenosis, Grade B)
- Carotid endarterectomy may be considered for patients between ages 40 to 75 years, with asymptomatic stenosis between 60% to 99%, if there is a 5-year life expectancy and surgical risk is <3%.
- Symptomatic and asymptomatic patients undergoing carotid endarterectomy should receive aspirin (81 or 325 mg) daily prior to surgery and for at least 3 months postoperatively. In the absence of contraindications, it should be continued indefinitely.
GRADE B RECOMMENDATIONS
- Carotid endarterectomy may be considered for symptomatic patients with 50% to 69% stenosis in patients with a 5-year life expectancy and surgical risk <6%.
GRADE C RECOMMENDATION
- Patients with hemispheric transient ischemic attack or cerebrovascular accident had greater benefit from carotid endarterectomy than those with retinal events.
- Patients with severe stenosis and a cerebrovascular event should have carotid endarterectomy within 2 weeks for greatest benefit.
- Contralateral occlusion reduces the benefit of carotid endarterectomy in asymptomatic patients.
- Data are insufficient to recommend other antiplatelet agents perioperatively.
The evidence categories are assessment of therapeutic effectiveness, prevention, and risk assessment. Study outcomes considered are: benefits of carotid endarterectomy for symptomatic patients, benefits for asymptomatic patients, the efficacy within 24 hours in patients with progressing stroke, clinical variables that impact the risk/benefit ratio, the most important radiologic factors impacting the risk/benefit ratio, the ideal dose of aspirin preoperatively, the evidence/practice gap, the likelihood that trial results can be achieved in practice, the benefit of carotid endarterectomy concurrent with or prior to coronary artery bypass grafting, and the optimal time after stroke to perform the surgery. The evidence rating is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Carotid endarterectomy has an important role in the prevention of stroke in patients with internal carotid artery stenosis, since the majority of strokes are ischemic. Strokes can be prevented if a high-grade internal carotid stenosis is corrected. More than 700,000 patients suffer a stroke each year in the US, with 80% related to ischemia (either thrombotic or embolic).2 Most strokes occur after the age of 65, and the risk doubles each decade after the age of 55. Stroke is the third leading cause of death, with only heart disease and cancer killing more people. Strokes cause more serious long-term disabilities than any other illness. The guideline was weakened by lack of cost analysis.
Guideline development and evidence review
A literature search was performed using Ovid Medline for relevant articles published from 1990 to 2001 using the keywords carotid endarterectomy, carotid stenosis, carotid artery diseases, and clinical trials. The Cochrane Library statements on carotid endarterectomy for symptomatic and asymptomatic stenosis from 2004 were reviewed to confirm that additional relevant citations from 2002 to 2004 were identified.
The initial search yielded 1462 citations. This list was reduced by excluding case reports, letters to the editor, review articles without primary data, studies addressing carotid endarterectomy technical issues, case series from a single surgeon, and articles not written in English. Case series from a single institution were included. This narrowed the pertinent list to 186 articles, which were reviewed independently by 2 committee members. The committee also agreed that if a pooled analysis of the major symptomatic carotid endarterectomy studies or if the results of the Asymptomatic Carotid Surgery Trial were published prior to the completion of the committee’s manuscript, these would subsequently be reviewed.
Source for this guideline
Chaturvedi S, Bruno A, Feasby T, Holloway R, Benavente O, Cohen SN, Cote R, Hess D, Saver J, Spence JD, Stern B, Wilterdink J. Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2005; 65:794–801 [27 refs]. Available at: www.neurology.org/cgi/reprint/65/6/794.pdf.
Other guidelines on surgical management of carotid stenosis and stroke
Life after stroke: New Zealand guideline for management of stroke
This comprehensive 2003 guideline is written for New Zealand health care delivery system. It summarizes recommendations for the assessment and management of stroke, transient ischemic attacks, and intracerebral hemorrhage in various locales. The utility of carotid endarterectomy for secondary prevention is reviewed. The recommendations are comparable to the American Academy of Neurology.
Source. New Zealand Guidelines Group. Life after stroke. New Zealand guideline for management of stroke. Wellington, NZ: New Zealand Guidelines Group; 2003: 84 pp [164 refs]. Available at: www.nzgg.org.nz/guidelines/0037/Stroke_Summary.pdf.
1. Ebell M, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-120.
2. National Institute of Neurological Disorders and Stroke. Stroke: Hope through research. 2006. Available at: www.ninds.nih.gov/disorders/stroke/detail_stroke.htm#56 051105. Accessed on March 21, 2006.
CORRESPONDENCE: Keith B. Holten, MD, 825 Locust Street, Wilmington, OH 45177. E-mail: [email protected]
1. Ebell M, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-120.
2. National Institute of Neurological Disorders and Stroke. Stroke: Hope through research. 2006. Available at: www.ninds.nih.gov/disorders/stroke/detail_stroke.htm#56 051105. Accessed on March 21, 2006.
CORRESPONDENCE: Keith B. Holten, MD, 825 Locust Street, Wilmington, OH 45177. E-mail: [email protected]
The Journal of Family Practice ©2006 Dowden Health Media
Important questions before flu season
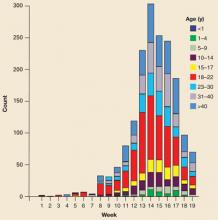
Influenza season is upon us. If this year is typical, 5% to 20 % of the US population will contract influenza. Of these, 200,000 people will be hospitalized and 36,000 will die. To minimize the effects of seasonal influenza, family physicians rely on annual influenza vaccine and antiviral therapy and prophylaxis. Every year at this time, we need to ask ourselves important questions as we prepare to provide maximum protection for our patients, our communities, and ourselves.
Who should receive an influenza vaccine?—an addition this year
The list of those who should receive an annual influenza vaccine (TABLE 1) is the same as last year, with 1 addition; children between ages 24 and 59 months and their household contacts and out-of-home caregivers.1-2 There are 2 types of vaccines available; trivalent inactivated influenza vaccine (TIA) and live attenuated influenza vaccine (LAIV). The TIA vaccine is administered intramuscularly, the LAIV by nasal spray. The vaccine products available and the ages for which they are licensed are listed in TABLE 2.3
The LAIV can be used for healthy people between the ages of 5 and 49 years; it should not be used for those who are pregnant, have a chronic illness, are caregivers to someone severely immune suppressed, are on chronic aspirin therapy, or have a history of Guillain-Barré syndrome. Neither vaccine should be used for anyone with an anaphylactic hypersensitivity to eggs or has had a severe allergic reaction to a previous vaccine. Vaccine should be postponed for anyone with a moderate-to-severe acute illness.
There are several other considerations for LAIV. Vaccination should be postponed for anyone with nasal congestion since it is not clear the vaccine can be administered correctly. Since LAIV is a live virus vaccine, it should be administered concurrently with, or 4 weeks after, any other live virus vaccines. It should also not be administered concurrently or within 2 weeks of receiving influenza antiviral agents. Finally, it needs to be stored at –15°C or below.
TABLE 1
Who should receive influenza vaccine
| People at high risk for complications from the flu, including: |
| Children aged 6–59 months |
| Pregnant women |
| People aged 50 years and older |
| People who live in nursing homes and other long-term care facilities |
People of any age with the following chronic medical conditions:
|
| People who live with or care for those at high risk for complications from flu, including: |
| Household contacts of persons at high risk for complications from the flu (see above) |
| Household contacts and out of home caregivers of children less than 6 months of age (these children are too young to be vaccinated) |
| Healthcare workers |
TABLE 2
Vaccine products available
| VACCINE | TRADE NAME (MANUFACTURER) | DOSE/PRESENTATION | THIMEROSAL MERCURY CONTENT (MCG/HG/0.5-ML DOSE) | AGE GROUP | NO. OF DOSES | ROUTE |
|---|---|---|---|---|---|---|
| Inactivated | ||||||
| TIV | Fluzone (Sanofi Pasteur) | 0.25-mL prefilled syringe | 0 | 6–35 mos | 1 or 2* | IM† |
| 0.5-mL prefilled syringe | 0 | ≥36 mos | 1 or 2* | IM† | ||
| 0.5-mL vial | 0 | ≥36 mos | 1 or 2* | IM† | ||
| 5.0-mL multidose vial | 25 | ≥6 mos | 1 or 2* | IM† | ||
| TIV | Fluvirin | 0.5-mL prefilled syringe | <1.0 | ≥4 years | 1 or 2* | IM† |
| 5.0-mL multidose vial | 24.5 | ≥4 years | 1 or 2* | IM† | ||
| TIV | FLUARIX (Glaxo-SmithKline) | 0.5-mL prefilled syringe | <1.25 | ≥18 years | 1 | IM† |
| Live, attenuated | ||||||
| LAIV | FluMist (Medimmune) | 0.5-mL sprayer | 0 | 5–49 years | 1 or 2‡ | Intranasal** |
| * Two doses administered at least 1 month apart are recommended for children aged 6 months to <9 years who are receiving influenza vaccine for the first time. | ||||||
| † For adults and older children, the recommended site of vaccination is the deltoid muscle. | ||||||
| The preferred site for infants and young children is the anterolateral aspect of the thigh. | ||||||
| ‡ Two doses administered at least 6 weeks apart are recommended for children aged 5 to <9 years who are receiving influenza vaccine for the first time. | ||||||
| ** One dose equals 0.5 mL, divided equally between each nostril. | ||||||
What issues are specific to ages 6 months to <9 years?
A child being immunized against influenza for the first time before his or her ninth birthday should receive 2 doses—4 weeks apart for TIV, 6 weeks apart for LAIV. The doses can be 2 of either TIV or LAIV or 1 of each. If a child received only 1 dose the prior year and it was their first time to receive the vaccine, they only need 1 dose the current year.
The supply of vaccine for this age group can be problematic, especially for age 3, for whom there is only 1 product licensed. Four of the products available for children contain trace amounts of thimerosal (TABLE 2), with the highest amounts being in multidose vials.3 There have been no proven harmful effects of these amounts of thimerosal, and both the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) continue to recommend these products. Some parents, however, may insist on a thimerosal-free product, and a few states have taken action to limit the use of thimerosal-containing vaccines.
When should we immunize?
Immunization of those at high risk should begin in September (if vaccine is available) or October. This is particularly important for children who need 2 doses for protection. Vaccination in nursing homes is best started in October—early enough to provide protection throughout the season but late enough to provide more assurance immunity will last throughout a late season. Vaccination of all those at risk should continue throughout the whole season, or as long as vaccine supplies last.
Will there be an adequate supply of vaccine?
There will be between 100 million and 120 million doses of vaccine available this year. Based on prior years, this should be an adequate supply.
Information is available on the American Academy of Family Physicians (AAFP) Web site on current vaccine supply issues and how to purchase influenza vaccine (available at: www.aafp.org/online/en/home/clinical/immunizations/flu06/ordering.html). The AAFP Web site will also contain information on vaccine prioritization should a shortage develop.
What is the role of antiviral medications?
The CDC currently recommends that the adamantanes (amantadine [Symmetrel] and rimantadine [Flumadine]) not be used for treatment or prophylaxis of influenza A because of a high rate of resistance documented last flu season. This situation could change as the current influenza season progresses. The remaining antivirals are both neuraminidase inhibitors; oseltamivir (Tamiflu—licensed for use in treatment and prophylaxis beginning at age 1 year) and zanamivir (Relenza—licensed for treatment beginning at age 5 years and prophylaxis at age 7 years).
Chemoprophylaxis is most useful in those whom the vaccine is contraindicated; in the 2 weeks after receipt of a vaccine, which is the time needed for it to be effective (2 weeks after the second dose in children receiving the vaccine for the first time); when the circulating virus does not match the vaccine; in those who are immune-suppressed and may have an inadequate response to the vaccine; and in nursing homes where there is an outbreak, when it should be used for everyone regardless of their vaccine status.
Treatment of those with influenza A can shorten the illness and reduce its severity if started within 2 days of symptoms. Details on antiviral recommendations and doses for treatment and prophylaxis can be found in the annual CDC influenza recommendations.3
Are rapid office lab tests useful?
The gold standard for laboratory confirmation of influenza is viral culture from a nasopharyngeal swab or washing. The time needed for this creates some difficulty initiating antiviral therapy within the two day window. Rapid, office-based tests are available and are listed in TABLE 3.5 Some of these tests are specific for influenza A, others for influenza B, and some are for both. The sensitivities and specificities for each product vary. A negative test in a highly suspicious patient should not rule out the disease, especially in a high prevalence situation. In a low prevalence situation a positive test is more likely to be a false positive than when the virus is causing an outbreak in the community.
TABLE 3
Rapid (<30-minute) laboratory tests available for influenza
| RAPID DIAGNOSTIC TESTS | INFLUENZA TYPE | APPLICATION METHODS |
|---|---|---|
| Directigen Flu A* (Becton-Dickinson) | A | NP swab, throat swab, nasal wash, nasal aspirate |
| Directigen Flu A+B* (Becton-Dickinson) | A and B† | NP swab, throat swab, nasal wash, nasal aspirate |
| Directigen EZ Flu A+B* (Becton-Dickinson) | A and B† | Throat swab, nasal wash, nasal aspirate |
| FLU OIA* (Thermo Electron) | A and B‡ | NP swab, throat swab, nasal aspirate, sputum |
| FLU OIA A/B* (Thermo Electron) | A and B† | NP swab, throat swab, nasal aspirate, sputum |
| XPECT Flu A&B* (Remel) | A and B† | Nasal wash, NP swab, throat swab |
| NOW Influenza A & B* (Binax) | A and B† | Nasal wash, NP swab |
| QuickVue Influenza Test** (Quidel) | A and B‡ | NP swab, nasal wash, nasal aspirate |
| QuickVue Influenza A+B Test** (Quidel) | A and B‡ | NP swab, nasal wash, nasal aspirate |
| SAS Influenza A Test* | A† | NP wash, NP aspirate |
| SAS Influenza B Test* | A† | NP wash, NP aspirate |
| ZstatFlu† (ZymeTx) | A and B‡ | Throat swab |
| Table may not include all test kits approved by the US Food and Drug Administration. | ||
| NP, nasopharyngeal | ||
| * Moderately complex test—requires specific laboratory certification. | ||
| † Distinguishes between influenza A and B virus infections. | ||
| ‡ Does not distinguish between influenza A and B virus infections. | ||
| ** CLIA-waived test. Can be used in any office setting. Requires a certificate of waiver or higher laboratory certification | ||
| Source: Centers for Disease Control and Prevention.5 | ||
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
RESOURCES
1. American Academy of Family Physicians Web site. Clinical Care & Research. Immunization resources. Available at: www.aafp.org/online/en/home/clinical/immunizations.html. Accessed on September 21, 2006. Current immunization recommendations, information on ordering influenza vaccine and steps to take should there be a vaccine shortage.
2. Centers for Disease Control and Prevention (CDC) Web site. Influenza (flu). Available at: www.cdc.gov/flu/. Accessed on September 21, 2006. Information for health professionals and consumers on all aspects of influenza.
3. CDC. Prevention and control of influenza. MMWR Recomm Rep 2006; 55:(RR-10):1-42. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5510a1.htm. Accessed on September 21, 2006. Annual update on recommendations for physicians on influenza diagnosis, treatment and prevention.
4. CDC Web site. Infection guidance for the prevention and control of influenza in acute care facilities. Available at: www.cdc.gov/flu/professionals/infectioncontrol/health-carefacilities.htm. Accessed on September 21, 2006. Information on how to protect staff and patients from the spread of influenza in the office setting.
5. CDC. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005; 54(RR-8):1-40. Available at: www.cdc.gov/flu/professionals/labdiagnosis.htm. Accessed on September 21, 2006.
Influenza season is upon us. If this year is typical, 5% to 20 % of the US population will contract influenza. Of these, 200,000 people will be hospitalized and 36,000 will die. To minimize the effects of seasonal influenza, family physicians rely on annual influenza vaccine and antiviral therapy and prophylaxis. Every year at this time, we need to ask ourselves important questions as we prepare to provide maximum protection for our patients, our communities, and ourselves.
Who should receive an influenza vaccine?—an addition this year
The list of those who should receive an annual influenza vaccine (TABLE 1) is the same as last year, with 1 addition; children between ages 24 and 59 months and their household contacts and out-of-home caregivers.1-2 There are 2 types of vaccines available; trivalent inactivated influenza vaccine (TIA) and live attenuated influenza vaccine (LAIV). The TIA vaccine is administered intramuscularly, the LAIV by nasal spray. The vaccine products available and the ages for which they are licensed are listed in TABLE 2.3
The LAIV can be used for healthy people between the ages of 5 and 49 years; it should not be used for those who are pregnant, have a chronic illness, are caregivers to someone severely immune suppressed, are on chronic aspirin therapy, or have a history of Guillain-Barré syndrome. Neither vaccine should be used for anyone with an anaphylactic hypersensitivity to eggs or has had a severe allergic reaction to a previous vaccine. Vaccine should be postponed for anyone with a moderate-to-severe acute illness.
There are several other considerations for LAIV. Vaccination should be postponed for anyone with nasal congestion since it is not clear the vaccine can be administered correctly. Since LAIV is a live virus vaccine, it should be administered concurrently with, or 4 weeks after, any other live virus vaccines. It should also not be administered concurrently or within 2 weeks of receiving influenza antiviral agents. Finally, it needs to be stored at –15°C or below.
TABLE 1
Who should receive influenza vaccine
| People at high risk for complications from the flu, including: |
| Children aged 6–59 months |
| Pregnant women |
| People aged 50 years and older |
| People who live in nursing homes and other long-term care facilities |
People of any age with the following chronic medical conditions:
|
| People who live with or care for those at high risk for complications from flu, including: |
| Household contacts of persons at high risk for complications from the flu (see above) |
| Household contacts and out of home caregivers of children less than 6 months of age (these children are too young to be vaccinated) |
| Healthcare workers |
TABLE 2
Vaccine products available
| VACCINE | TRADE NAME (MANUFACTURER) | DOSE/PRESENTATION | THIMEROSAL MERCURY CONTENT (MCG/HG/0.5-ML DOSE) | AGE GROUP | NO. OF DOSES | ROUTE |
|---|---|---|---|---|---|---|
| Inactivated | ||||||
| TIV | Fluzone (Sanofi Pasteur) | 0.25-mL prefilled syringe | 0 | 6–35 mos | 1 or 2* | IM† |
| 0.5-mL prefilled syringe | 0 | ≥36 mos | 1 or 2* | IM† | ||
| 0.5-mL vial | 0 | ≥36 mos | 1 or 2* | IM† | ||
| 5.0-mL multidose vial | 25 | ≥6 mos | 1 or 2* | IM† | ||
| TIV | Fluvirin | 0.5-mL prefilled syringe | <1.0 | ≥4 years | 1 or 2* | IM† |
| 5.0-mL multidose vial | 24.5 | ≥4 years | 1 or 2* | IM† | ||
| TIV | FLUARIX (Glaxo-SmithKline) | 0.5-mL prefilled syringe | <1.25 | ≥18 years | 1 | IM† |
| Live, attenuated | ||||||
| LAIV | FluMist (Medimmune) | 0.5-mL sprayer | 0 | 5–49 years | 1 or 2‡ | Intranasal** |
| * Two doses administered at least 1 month apart are recommended for children aged 6 months to <9 years who are receiving influenza vaccine for the first time. | ||||||
| † For adults and older children, the recommended site of vaccination is the deltoid muscle. | ||||||
| The preferred site for infants and young children is the anterolateral aspect of the thigh. | ||||||
| ‡ Two doses administered at least 6 weeks apart are recommended for children aged 5 to <9 years who are receiving influenza vaccine for the first time. | ||||||
| ** One dose equals 0.5 mL, divided equally between each nostril. | ||||||
What issues are specific to ages 6 months to <9 years?
A child being immunized against influenza for the first time before his or her ninth birthday should receive 2 doses—4 weeks apart for TIV, 6 weeks apart for LAIV. The doses can be 2 of either TIV or LAIV or 1 of each. If a child received only 1 dose the prior year and it was their first time to receive the vaccine, they only need 1 dose the current year.
The supply of vaccine for this age group can be problematic, especially for age 3, for whom there is only 1 product licensed. Four of the products available for children contain trace amounts of thimerosal (TABLE 2), with the highest amounts being in multidose vials.3 There have been no proven harmful effects of these amounts of thimerosal, and both the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) continue to recommend these products. Some parents, however, may insist on a thimerosal-free product, and a few states have taken action to limit the use of thimerosal-containing vaccines.
When should we immunize?
Immunization of those at high risk should begin in September (if vaccine is available) or October. This is particularly important for children who need 2 doses for protection. Vaccination in nursing homes is best started in October—early enough to provide protection throughout the season but late enough to provide more assurance immunity will last throughout a late season. Vaccination of all those at risk should continue throughout the whole season, or as long as vaccine supplies last.
Will there be an adequate supply of vaccine?
There will be between 100 million and 120 million doses of vaccine available this year. Based on prior years, this should be an adequate supply.
Information is available on the American Academy of Family Physicians (AAFP) Web site on current vaccine supply issues and how to purchase influenza vaccine (available at: www.aafp.org/online/en/home/clinical/immunizations/flu06/ordering.html). The AAFP Web site will also contain information on vaccine prioritization should a shortage develop.
What is the role of antiviral medications?
The CDC currently recommends that the adamantanes (amantadine [Symmetrel] and rimantadine [Flumadine]) not be used for treatment or prophylaxis of influenza A because of a high rate of resistance documented last flu season. This situation could change as the current influenza season progresses. The remaining antivirals are both neuraminidase inhibitors; oseltamivir (Tamiflu—licensed for use in treatment and prophylaxis beginning at age 1 year) and zanamivir (Relenza—licensed for treatment beginning at age 5 years and prophylaxis at age 7 years).
Chemoprophylaxis is most useful in those whom the vaccine is contraindicated; in the 2 weeks after receipt of a vaccine, which is the time needed for it to be effective (2 weeks after the second dose in children receiving the vaccine for the first time); when the circulating virus does not match the vaccine; in those who are immune-suppressed and may have an inadequate response to the vaccine; and in nursing homes where there is an outbreak, when it should be used for everyone regardless of their vaccine status.
Treatment of those with influenza A can shorten the illness and reduce its severity if started within 2 days of symptoms. Details on antiviral recommendations and doses for treatment and prophylaxis can be found in the annual CDC influenza recommendations.3
Are rapid office lab tests useful?
The gold standard for laboratory confirmation of influenza is viral culture from a nasopharyngeal swab or washing. The time needed for this creates some difficulty initiating antiviral therapy within the two day window. Rapid, office-based tests are available and are listed in TABLE 3.5 Some of these tests are specific for influenza A, others for influenza B, and some are for both. The sensitivities and specificities for each product vary. A negative test in a highly suspicious patient should not rule out the disease, especially in a high prevalence situation. In a low prevalence situation a positive test is more likely to be a false positive than when the virus is causing an outbreak in the community.
TABLE 3
Rapid (<30-minute) laboratory tests available for influenza
| RAPID DIAGNOSTIC TESTS | INFLUENZA TYPE | APPLICATION METHODS |
|---|---|---|
| Directigen Flu A* (Becton-Dickinson) | A | NP swab, throat swab, nasal wash, nasal aspirate |
| Directigen Flu A+B* (Becton-Dickinson) | A and B† | NP swab, throat swab, nasal wash, nasal aspirate |
| Directigen EZ Flu A+B* (Becton-Dickinson) | A and B† | Throat swab, nasal wash, nasal aspirate |
| FLU OIA* (Thermo Electron) | A and B‡ | NP swab, throat swab, nasal aspirate, sputum |
| FLU OIA A/B* (Thermo Electron) | A and B† | NP swab, throat swab, nasal aspirate, sputum |
| XPECT Flu A&B* (Remel) | A and B† | Nasal wash, NP swab, throat swab |
| NOW Influenza A & B* (Binax) | A and B† | Nasal wash, NP swab |
| QuickVue Influenza Test** (Quidel) | A and B‡ | NP swab, nasal wash, nasal aspirate |
| QuickVue Influenza A+B Test** (Quidel) | A and B‡ | NP swab, nasal wash, nasal aspirate |
| SAS Influenza A Test* | A† | NP wash, NP aspirate |
| SAS Influenza B Test* | A† | NP wash, NP aspirate |
| ZstatFlu† (ZymeTx) | A and B‡ | Throat swab |
| Table may not include all test kits approved by the US Food and Drug Administration. | ||
| NP, nasopharyngeal | ||
| * Moderately complex test—requires specific laboratory certification. | ||
| † Distinguishes between influenza A and B virus infections. | ||
| ‡ Does not distinguish between influenza A and B virus infections. | ||
| ** CLIA-waived test. Can be used in any office setting. Requires a certificate of waiver or higher laboratory certification | ||
| Source: Centers for Disease Control and Prevention.5 | ||
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
Influenza season is upon us. If this year is typical, 5% to 20 % of the US population will contract influenza. Of these, 200,000 people will be hospitalized and 36,000 will die. To minimize the effects of seasonal influenza, family physicians rely on annual influenza vaccine and antiviral therapy and prophylaxis. Every year at this time, we need to ask ourselves important questions as we prepare to provide maximum protection for our patients, our communities, and ourselves.
Who should receive an influenza vaccine?—an addition this year
The list of those who should receive an annual influenza vaccine (TABLE 1) is the same as last year, with 1 addition; children between ages 24 and 59 months and their household contacts and out-of-home caregivers.1-2 There are 2 types of vaccines available; trivalent inactivated influenza vaccine (TIA) and live attenuated influenza vaccine (LAIV). The TIA vaccine is administered intramuscularly, the LAIV by nasal spray. The vaccine products available and the ages for which they are licensed are listed in TABLE 2.3
The LAIV can be used for healthy people between the ages of 5 and 49 years; it should not be used for those who are pregnant, have a chronic illness, are caregivers to someone severely immune suppressed, are on chronic aspirin therapy, or have a history of Guillain-Barré syndrome. Neither vaccine should be used for anyone with an anaphylactic hypersensitivity to eggs or has had a severe allergic reaction to a previous vaccine. Vaccine should be postponed for anyone with a moderate-to-severe acute illness.
There are several other considerations for LAIV. Vaccination should be postponed for anyone with nasal congestion since it is not clear the vaccine can be administered correctly. Since LAIV is a live virus vaccine, it should be administered concurrently with, or 4 weeks after, any other live virus vaccines. It should also not be administered concurrently or within 2 weeks of receiving influenza antiviral agents. Finally, it needs to be stored at –15°C or below.
TABLE 1
Who should receive influenza vaccine
| People at high risk for complications from the flu, including: |
| Children aged 6–59 months |
| Pregnant women |
| People aged 50 years and older |
| People who live in nursing homes and other long-term care facilities |
People of any age with the following chronic medical conditions:
|
| People who live with or care for those at high risk for complications from flu, including: |
| Household contacts of persons at high risk for complications from the flu (see above) |
| Household contacts and out of home caregivers of children less than 6 months of age (these children are too young to be vaccinated) |
| Healthcare workers |
TABLE 2
Vaccine products available
| VACCINE | TRADE NAME (MANUFACTURER) | DOSE/PRESENTATION | THIMEROSAL MERCURY CONTENT (MCG/HG/0.5-ML DOSE) | AGE GROUP | NO. OF DOSES | ROUTE |
|---|---|---|---|---|---|---|
| Inactivated | ||||||
| TIV | Fluzone (Sanofi Pasteur) | 0.25-mL prefilled syringe | 0 | 6–35 mos | 1 or 2* | IM† |
| 0.5-mL prefilled syringe | 0 | ≥36 mos | 1 or 2* | IM† | ||
| 0.5-mL vial | 0 | ≥36 mos | 1 or 2* | IM† | ||
| 5.0-mL multidose vial | 25 | ≥6 mos | 1 or 2* | IM† | ||
| TIV | Fluvirin | 0.5-mL prefilled syringe | <1.0 | ≥4 years | 1 or 2* | IM† |
| 5.0-mL multidose vial | 24.5 | ≥4 years | 1 or 2* | IM† | ||
| TIV | FLUARIX (Glaxo-SmithKline) | 0.5-mL prefilled syringe | <1.25 | ≥18 years | 1 | IM† |
| Live, attenuated | ||||||
| LAIV | FluMist (Medimmune) | 0.5-mL sprayer | 0 | 5–49 years | 1 or 2‡ | Intranasal** |
| * Two doses administered at least 1 month apart are recommended for children aged 6 months to <9 years who are receiving influenza vaccine for the first time. | ||||||
| † For adults and older children, the recommended site of vaccination is the deltoid muscle. | ||||||
| The preferred site for infants and young children is the anterolateral aspect of the thigh. | ||||||
| ‡ Two doses administered at least 6 weeks apart are recommended for children aged 5 to <9 years who are receiving influenza vaccine for the first time. | ||||||
| ** One dose equals 0.5 mL, divided equally between each nostril. | ||||||
What issues are specific to ages 6 months to <9 years?
A child being immunized against influenza for the first time before his or her ninth birthday should receive 2 doses—4 weeks apart for TIV, 6 weeks apart for LAIV. The doses can be 2 of either TIV or LAIV or 1 of each. If a child received only 1 dose the prior year and it was their first time to receive the vaccine, they only need 1 dose the current year.
The supply of vaccine for this age group can be problematic, especially for age 3, for whom there is only 1 product licensed. Four of the products available for children contain trace amounts of thimerosal (TABLE 2), with the highest amounts being in multidose vials.3 There have been no proven harmful effects of these amounts of thimerosal, and both the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) continue to recommend these products. Some parents, however, may insist on a thimerosal-free product, and a few states have taken action to limit the use of thimerosal-containing vaccines.
When should we immunize?
Immunization of those at high risk should begin in September (if vaccine is available) or October. This is particularly important for children who need 2 doses for protection. Vaccination in nursing homes is best started in October—early enough to provide protection throughout the season but late enough to provide more assurance immunity will last throughout a late season. Vaccination of all those at risk should continue throughout the whole season, or as long as vaccine supplies last.
Will there be an adequate supply of vaccine?
There will be between 100 million and 120 million doses of vaccine available this year. Based on prior years, this should be an adequate supply.
Information is available on the American Academy of Family Physicians (AAFP) Web site on current vaccine supply issues and how to purchase influenza vaccine (available at: www.aafp.org/online/en/home/clinical/immunizations/flu06/ordering.html). The AAFP Web site will also contain information on vaccine prioritization should a shortage develop.
What is the role of antiviral medications?
The CDC currently recommends that the adamantanes (amantadine [Symmetrel] and rimantadine [Flumadine]) not be used for treatment or prophylaxis of influenza A because of a high rate of resistance documented last flu season. This situation could change as the current influenza season progresses. The remaining antivirals are both neuraminidase inhibitors; oseltamivir (Tamiflu—licensed for use in treatment and prophylaxis beginning at age 1 year) and zanamivir (Relenza—licensed for treatment beginning at age 5 years and prophylaxis at age 7 years).
Chemoprophylaxis is most useful in those whom the vaccine is contraindicated; in the 2 weeks after receipt of a vaccine, which is the time needed for it to be effective (2 weeks after the second dose in children receiving the vaccine for the first time); when the circulating virus does not match the vaccine; in those who are immune-suppressed and may have an inadequate response to the vaccine; and in nursing homes where there is an outbreak, when it should be used for everyone regardless of their vaccine status.
Treatment of those with influenza A can shorten the illness and reduce its severity if started within 2 days of symptoms. Details on antiviral recommendations and doses for treatment and prophylaxis can be found in the annual CDC influenza recommendations.3
Are rapid office lab tests useful?
The gold standard for laboratory confirmation of influenza is viral culture from a nasopharyngeal swab or washing. The time needed for this creates some difficulty initiating antiviral therapy within the two day window. Rapid, office-based tests are available and are listed in TABLE 3.5 Some of these tests are specific for influenza A, others for influenza B, and some are for both. The sensitivities and specificities for each product vary. A negative test in a highly suspicious patient should not rule out the disease, especially in a high prevalence situation. In a low prevalence situation a positive test is more likely to be a false positive than when the virus is causing an outbreak in the community.
TABLE 3
Rapid (<30-minute) laboratory tests available for influenza
| RAPID DIAGNOSTIC TESTS | INFLUENZA TYPE | APPLICATION METHODS |
|---|---|---|
| Directigen Flu A* (Becton-Dickinson) | A | NP swab, throat swab, nasal wash, nasal aspirate |
| Directigen Flu A+B* (Becton-Dickinson) | A and B† | NP swab, throat swab, nasal wash, nasal aspirate |
| Directigen EZ Flu A+B* (Becton-Dickinson) | A and B† | Throat swab, nasal wash, nasal aspirate |
| FLU OIA* (Thermo Electron) | A and B‡ | NP swab, throat swab, nasal aspirate, sputum |
| FLU OIA A/B* (Thermo Electron) | A and B† | NP swab, throat swab, nasal aspirate, sputum |
| XPECT Flu A&B* (Remel) | A and B† | Nasal wash, NP swab, throat swab |
| NOW Influenza A & B* (Binax) | A and B† | Nasal wash, NP swab |
| QuickVue Influenza Test** (Quidel) | A and B‡ | NP swab, nasal wash, nasal aspirate |
| QuickVue Influenza A+B Test** (Quidel) | A and B‡ | NP swab, nasal wash, nasal aspirate |
| SAS Influenza A Test* | A† | NP wash, NP aspirate |
| SAS Influenza B Test* | A† | NP wash, NP aspirate |
| ZstatFlu† (ZymeTx) | A and B‡ | Throat swab |
| Table may not include all test kits approved by the US Food and Drug Administration. | ||
| NP, nasopharyngeal | ||
| * Moderately complex test—requires specific laboratory certification. | ||
| † Distinguishes between influenza A and B virus infections. | ||
| ‡ Does not distinguish between influenza A and B virus infections. | ||
| ** CLIA-waived test. Can be used in any office setting. Requires a certificate of waiver or higher laboratory certification | ||
| Source: Centers for Disease Control and Prevention.5 | ||
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
RESOURCES
1. American Academy of Family Physicians Web site. Clinical Care & Research. Immunization resources. Available at: www.aafp.org/online/en/home/clinical/immunizations.html. Accessed on September 21, 2006. Current immunization recommendations, information on ordering influenza vaccine and steps to take should there be a vaccine shortage.
2. Centers for Disease Control and Prevention (CDC) Web site. Influenza (flu). Available at: www.cdc.gov/flu/. Accessed on September 21, 2006. Information for health professionals and consumers on all aspects of influenza.
3. CDC. Prevention and control of influenza. MMWR Recomm Rep 2006; 55:(RR-10):1-42. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5510a1.htm. Accessed on September 21, 2006. Annual update on recommendations for physicians on influenza diagnosis, treatment and prevention.
4. CDC Web site. Infection guidance for the prevention and control of influenza in acute care facilities. Available at: www.cdc.gov/flu/professionals/infectioncontrol/health-carefacilities.htm. Accessed on September 21, 2006. Information on how to protect staff and patients from the spread of influenza in the office setting.
5. CDC. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005; 54(RR-8):1-40. Available at: www.cdc.gov/flu/professionals/labdiagnosis.htm. Accessed on September 21, 2006.
RESOURCES
1. American Academy of Family Physicians Web site. Clinical Care & Research. Immunization resources. Available at: www.aafp.org/online/en/home/clinical/immunizations.html. Accessed on September 21, 2006. Current immunization recommendations, information on ordering influenza vaccine and steps to take should there be a vaccine shortage.
2. Centers for Disease Control and Prevention (CDC) Web site. Influenza (flu). Available at: www.cdc.gov/flu/. Accessed on September 21, 2006. Information for health professionals and consumers on all aspects of influenza.
3. CDC. Prevention and control of influenza. MMWR Recomm Rep 2006; 55:(RR-10):1-42. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5510a1.htm. Accessed on September 21, 2006. Annual update on recommendations for physicians on influenza diagnosis, treatment and prevention.
4. CDC Web site. Infection guidance for the prevention and control of influenza in acute care facilities. Available at: www.cdc.gov/flu/professionals/infectioncontrol/health-carefacilities.htm. Accessed on September 21, 2006. Information on how to protect staff and patients from the spread of influenza in the office setting.
5. CDC. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2005; 54(RR-8):1-40. Available at: www.cdc.gov/flu/professionals/labdiagnosis.htm. Accessed on September 21, 2006.
The Journal of Family Practice ©2006 Dowden Health Media
What hope is there for meaningful tort reform to stop another malpractice crisis?
A handful of papers published in the past few years have looked at different aspects of the current malpractice situation and have yielded some revelations (see page 775 in this issue) or data banks working on safety issues.
- Though it does a reasonable job at separating valid from invalid claims and compensating them accordingly, it often takes a tremendously long time to accomplish this and still has a 10% to 16% rate of false positive (payment with no error) and false negative (no payment with error) outcomes.
- The system is not overwhelmed with frivolous claims. Still, it costs a lot of money to manage, and less than half of this money goes to claimants.
- Hard caps on total damages or noneconomic damages, unlike other state tort reforms (Figure), appear to reduce claims payments, physician premiums, and total health costs,7 while increasing physician supply.
- Defensive medicine exists, though putting a valid dollar amount on its costs is difficult.
- Anecdotal evidence suggests that physicians are leaving practice or limiting their practice (eg, family physicians discontinuing deliveries) as a result of malpractice costs.
FIGURE
Tort reforms commonly adopted by states
AMA’s proposal for change
Malpractice reform has been at or near the top of the AMA’s political agenda for the past 4 or 5 years, with strong lobbying efforts at the national level as well as support for state chapter efforts. The AMA’s proposal is based on California’s liability reform law known as MICRA that was passed over 30 years ago and has been associated with significantly lower premium growth since then compared with the rest of the US.8 Key provisions:
- Unlimited economic damages (medical expenses, future earnings)
- Limits on noneconomic damages (pain and suffering)
- Punitive damages, if available, up to $250,000 or 2 times economic damages, whichever is greater
- Allocation of damage awards in proportion to fault
- Sliding scale for attorney contingency fees.
Dubious premises. The AMA literature on malpractice includes valid information on the costs of the tort system, the rise in claims payouts, and effects on physician premiums. But it also suggests that meritless lawsuits are increasing. This is untrue. And its implication that physicians are increasingly leaving practice is anecdotal. There is no good research on the extent of this problem.8
Too narrow a focus. More important, the AMA plan is focused on physician premium costs while ignoring the unfairness of the system (eg, time to resolve claims, lack of payment for many patients with legitimate claims) and the vast number of medical errors for which claims are never filed.
The MEDIC proposal
Senators Hillary Clinton (D-NY) and Barack Obama (D-IL) have proposed federal legislation to address the malpractice crisis. Their bill would create an Office of Patient Safety in the Department of Health and Human Services, and would establish the National Medical Error Disclosure and Compensation (MEDIC) program within that office.9
Apologies would not be actionable in court. The MEDIC program would provide grants to physicians, hospitals, and health systems for the creation of programs to disclose medical errors to patients and negotiate fair compensation. The law would preserve confidentiality so that any apology offered by a health care provider as part of those negotiations would be kept confidential and could not be used in a trial. Any savings achieved from lower administrative and legal costs would be used to reduce physician malpractice premiums and toward patient safety initiatives.
Federal mandating of caps unlikely, however. At the federal level, Democrats have firmly opposed mandating caps on malpractice claims settlements. They argue that caps are unfair to patients who have been victims of medical errors. Others say this opposition reflects financial contributions from trial lawyers. It seems time to get past this conflict. Without dramatic changes in the composition of the Senate, which seems unlikely, there is little or no chance that caps will pass at the national level. At the same time, physician groups have been successful at achieving caps in a number of states (total of 26 at last count).
Signs this program could succeed. The MEDIC proposal is an attempt to find another way out of the malpractice impasse in the Senate by linking the patient safety and tort reform issues. It is primarily based on a growing movement to have physicians more directly acknowledge medical errors to patients,10 and in some cases, link these apologies to immediate financial negotiations to settle any potential claim of injury. The University of Michigan is the best known academic institution pursuing these strategies, and they report a significant decrease in the number of claims and annual litigation costs. The Lexington, Kentucky, VA Hospital has a similar program that has reduced liability costs compared with other VA hospitals.
The MEDIC proposal is attractive in its attempt to tie doctor-patient communication, patient safety, and liability together. And the anecdotal reports of success with isolated programs of its type are encouraging. It also moves the argument at a national level away from a fight about caps, which puts many physicians in the uncomfortable position of opposing Democrats who support many of their other positions—eg, Title VII funding, preservation of the traditional Medicare program, expansion of the Medicare Part D program, and better funding of public health programs. Nonetheless, there is a big row to hoe in making physicians more comfortable with acknowledging their errors, convincing them this would not be held against them in court, and assuring both physicians and hospitals that such efforts will actually lead to lower malpractice costs.
Thorpe analyzed data from 1995–2001 collected by the National Association of Insurance Commissioners to see the relationship between state tort reforms and premium levels. Premiums in states with caps on awards were 17% lower than states without caps. There was no association between premium levels and other reforms, such as caps on attorney fees or collateral offset rules (decreasing awards by the amount the plaintiff receives from other sources). Some association was noted between decreased competition among insurers and higher premiums.1
Rodwin et al used data from AMA surveys of self-employed physicians (physicians in groups or solo practice who are not employees) from 1970 to 2000. They found that while premiums increased from 1970 to 1986 and from 1996 to 2000, they had only a small effect on physician income. Premiums made up a small percentage of total practice costs and had a negligible effect on practice income, arguing against a malpractice crisis. However, this study lacked more recent data on premium increases and practice expenses and did not take into account differences among states that might be due to tort reforms such as the institution of caps on awards.2
Studdert et al reviewed 1452 closed claims in 4 categories (obstetrics, surgery, missed or delayed diagnosis, and medication) from 5 liability insurers representing 4 regions of the US, and used objective criteria and independent reviewers to classify the merits of the claims. They found that 3% of the claims had no verifiable medical injury and 37% did not involve errors. About 73% of the claims not associated with errors or injuries resulted in no compensation, while 73% of those with errors did result in compensation. Further payment for claims not involving errors were lower than those that did involve errors. Looked at another way, of the 1452 claims reviewed, about 10% received payment but had no identifiable error, while about 17% had an identifiable error but no payment was made.3
This study demonstrated that: 1) the cost of defending claims involving no error was substantial but still only amounted to about 13% of direct system costs, meaning that contesting and paying for claims caused by errors accounts for most of the costs of the liability system, and 2) the malpractice system works reasonably well at separating claims without merit from those with merit.
Nonetheless, the study also demonstrated the unfairness of a system in which 1 in 6 valid claims received no payment (this in addition to the vast number of negligent injuries that never even lead to a claim as discussed in the 1999 IOM report). Then there is the frustration with a system wherein the average time between injury and claim resolution is 5 years and 54% of the payments are absorbed by defense costs and contingency fees. That 80% of expenses were incurred in resolving claims with errors suggests that steps to decrease frivolous litigation (claims without merit) will not lead to substantial savings and that steps to streamlining the system of handling claims will be more useful.
Blake et al looked at state-specific data from the National Practitioner Data Bank, which collects reports of all malpractice payments in the US on behalf of physicians, dentists, and nurses. They looked at the relationship between payments, physician premiums, and various state tort reforms. They found that mean payments were 26% lower in states with total damage caps ($196,000 vs $265,000) and 22% less in states with noneconomic (pain and suffering) damage caps ($212,000 vs $279,000). In addition, total damage caps were associated with lower mean annual premiums and hard, but not soft (caps with exceptions) noneconomic caps were associated with premium reductions. No other state tort reforms measured showed a significant association with payments or premiums.4
Studdert et al surveyed Pennsylvania physicians in high-risk specialties (obstetrics/gynecology, ortho, ER, surgery, neurosurgery) to ascertain self-report of defensive medicine practice. Almost all respondents reported practicing defensive medicine, the most common form (92%) being unnecessary ordering of tests and imaging studies and referring for consultation. In addition, 42% said they had restricted their practice by either decreasing the performance of more risky procedures (eg, trauma surgery) or avoiding complex cases or patients perceived as more likely to sue. Defensive medicine was highly correlated with physicians’ lack of confidence in their liability insurance or its cost.5
Kessler et al looked at physician supply from 1985–2001 and its correlates to state tort reforms during that time. Three years after States that adopted direct reforms (mainly caps on damage awards) showed an average physician growth rate within 3 years that was 3.3% greater than states not adopting such reforms. The authors controlled for a variety of factors that can influence physician supply including population growth and other state-level characteristics.6
Common Good proposal
Another approach is advocated by Common Good, a bipartisan legal reform coalition. This organization has funding from the RWJ Foundation to work with researchers from the Harvard School of Public Health to investigate the creation of special health courts to hear malpractice cases.11 Their ideas are incorporated into the Fair and Reliable Medical Justice Act introduced as S.1337 by Senators Mike Enzi (R-WY) Max Baucus (D-MT).11
How it would work. Health courts would have full-time judges, neutral medical experts, faster proceedings with legal fees held to 20%, and rulings that could be appealed to a new Medical Appellate Court. Like other administrative courts that handle tax disputes, workmen’s comp, and vaccine injury, there would be no juries. Judges would issue written rulings and establish legal precedents. Once a mistake was verified, recovery would be automatic. Patients would be reimbursed for all their medical expenses and lost income plus a fixed sum that would be determined from an expert derived schedule addressing specific types of injuries.
Strengths and weaknesses. This proposal has the support of a wide array of national medical and legal leaders but not any medical associations. It attempts to address some of the most egregious parts of the current system—the time it takes to get claims resolved, the many errors that go uncompensated, and the diversion of so many dollars to overhead and legal fees rather than to patients. On the other hand, the plan does not provide firm caps, which may make the AMA and other professional associations skeptical. And the proposed health courts would rely on select medical experts and judges, a system likely to be strongly opposed by trial lawyers and some consumer groups. It also does not directly address the prevention of patient errors.
Those who fail to learn from history…
The current malpractice crisis may be abating, leaving physicians with higher malpractice premiums but some state tort reforms. History, however, suggests that the insurance cycle will eventually lead to another crisis. There may be a window of opportunity now to come up with a completely different system to address the goals and problems with our current system, but it is likely to be a small window. Capitalizing on it will require a willingness for both sides in the current stand-off to get past their own self-interests in order to come up with something better for all.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
1. Thorpe K. The Medical malpractice “crisis”: Recent trends and the impact of state tort reforms. Health Affairs 2004 January 21;web-only.
2. Rodwin M, Chang H, Clausen J. Malpractice premiums and physicians’ income: Perceptions of a crisis conflict with empirical evidence. Health Affairs 2006;525:750-758.
3. Studdert D, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med 2006;354:2024-2033.
4. Guirguis-Blake J, Fryer GE, Phillips RL, Jr, Szabat R, Green LA. The US medical liability system: Evidence for legislative reform. Ann Fam Med 2006;4:240-246.
5. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005;293:2609-2617.
6. Kessler DP, Sage WM, Becker DJ, et al. Impact of malpractice reforms on the supply of physician services. JAMA 2005;293:2618-2625.
7. Hellinger F, Encinosa W. The impact of state laws limiting malpractice damage awards on health care expenditures. AJPH 2006;96:1375-1381.
8. American Medical Association. Medical liability talking points. Available at: www.ama-assn.org/ama1/pub/upload/mm/399/mlr_fastfacts.pdf. Accessed on August 15, 2006.
9. Clinton HR, Obama B. Making patient safety the centerpiece of medical liability reform. N Engl J Med 2006;354:2205-2208.
10. O’Reilly K. Harvard adopts a disclosure and apology policy. AMA News, June 12, 2006.
11. Common Good. What are health courts? Available at: cgood.org/f-healthcourtsinfo.html. Accessed on August 15, 2006.
A handful of papers published in the past few years have looked at different aspects of the current malpractice situation and have yielded some revelations (see page 775 in this issue) or data banks working on safety issues.
- Though it does a reasonable job at separating valid from invalid claims and compensating them accordingly, it often takes a tremendously long time to accomplish this and still has a 10% to 16% rate of false positive (payment with no error) and false negative (no payment with error) outcomes.
- The system is not overwhelmed with frivolous claims. Still, it costs a lot of money to manage, and less than half of this money goes to claimants.
- Hard caps on total damages or noneconomic damages, unlike other state tort reforms (Figure), appear to reduce claims payments, physician premiums, and total health costs,7 while increasing physician supply.
- Defensive medicine exists, though putting a valid dollar amount on its costs is difficult.
- Anecdotal evidence suggests that physicians are leaving practice or limiting their practice (eg, family physicians discontinuing deliveries) as a result of malpractice costs.
FIGURE
Tort reforms commonly adopted by states
AMA’s proposal for change
Malpractice reform has been at or near the top of the AMA’s political agenda for the past 4 or 5 years, with strong lobbying efforts at the national level as well as support for state chapter efforts. The AMA’s proposal is based on California’s liability reform law known as MICRA that was passed over 30 years ago and has been associated with significantly lower premium growth since then compared with the rest of the US.8 Key provisions:
- Unlimited economic damages (medical expenses, future earnings)
- Limits on noneconomic damages (pain and suffering)
- Punitive damages, if available, up to $250,000 or 2 times economic damages, whichever is greater
- Allocation of damage awards in proportion to fault
- Sliding scale for attorney contingency fees.
Dubious premises. The AMA literature on malpractice includes valid information on the costs of the tort system, the rise in claims payouts, and effects on physician premiums. But it also suggests that meritless lawsuits are increasing. This is untrue. And its implication that physicians are increasingly leaving practice is anecdotal. There is no good research on the extent of this problem.8
Too narrow a focus. More important, the AMA plan is focused on physician premium costs while ignoring the unfairness of the system (eg, time to resolve claims, lack of payment for many patients with legitimate claims) and the vast number of medical errors for which claims are never filed.
The MEDIC proposal
Senators Hillary Clinton (D-NY) and Barack Obama (D-IL) have proposed federal legislation to address the malpractice crisis. Their bill would create an Office of Patient Safety in the Department of Health and Human Services, and would establish the National Medical Error Disclosure and Compensation (MEDIC) program within that office.9
Apologies would not be actionable in court. The MEDIC program would provide grants to physicians, hospitals, and health systems for the creation of programs to disclose medical errors to patients and negotiate fair compensation. The law would preserve confidentiality so that any apology offered by a health care provider as part of those negotiations would be kept confidential and could not be used in a trial. Any savings achieved from lower administrative and legal costs would be used to reduce physician malpractice premiums and toward patient safety initiatives.
Federal mandating of caps unlikely, however. At the federal level, Democrats have firmly opposed mandating caps on malpractice claims settlements. They argue that caps are unfair to patients who have been victims of medical errors. Others say this opposition reflects financial contributions from trial lawyers. It seems time to get past this conflict. Without dramatic changes in the composition of the Senate, which seems unlikely, there is little or no chance that caps will pass at the national level. At the same time, physician groups have been successful at achieving caps in a number of states (total of 26 at last count).
Signs this program could succeed. The MEDIC proposal is an attempt to find another way out of the malpractice impasse in the Senate by linking the patient safety and tort reform issues. It is primarily based on a growing movement to have physicians more directly acknowledge medical errors to patients,10 and in some cases, link these apologies to immediate financial negotiations to settle any potential claim of injury. The University of Michigan is the best known academic institution pursuing these strategies, and they report a significant decrease in the number of claims and annual litigation costs. The Lexington, Kentucky, VA Hospital has a similar program that has reduced liability costs compared with other VA hospitals.
The MEDIC proposal is attractive in its attempt to tie doctor-patient communication, patient safety, and liability together. And the anecdotal reports of success with isolated programs of its type are encouraging. It also moves the argument at a national level away from a fight about caps, which puts many physicians in the uncomfortable position of opposing Democrats who support many of their other positions—eg, Title VII funding, preservation of the traditional Medicare program, expansion of the Medicare Part D program, and better funding of public health programs. Nonetheless, there is a big row to hoe in making physicians more comfortable with acknowledging their errors, convincing them this would not be held against them in court, and assuring both physicians and hospitals that such efforts will actually lead to lower malpractice costs.
Thorpe analyzed data from 1995–2001 collected by the National Association of Insurance Commissioners to see the relationship between state tort reforms and premium levels. Premiums in states with caps on awards were 17% lower than states without caps. There was no association between premium levels and other reforms, such as caps on attorney fees or collateral offset rules (decreasing awards by the amount the plaintiff receives from other sources). Some association was noted between decreased competition among insurers and higher premiums.1
Rodwin et al used data from AMA surveys of self-employed physicians (physicians in groups or solo practice who are not employees) from 1970 to 2000. They found that while premiums increased from 1970 to 1986 and from 1996 to 2000, they had only a small effect on physician income. Premiums made up a small percentage of total practice costs and had a negligible effect on practice income, arguing against a malpractice crisis. However, this study lacked more recent data on premium increases and practice expenses and did not take into account differences among states that might be due to tort reforms such as the institution of caps on awards.2
Studdert et al reviewed 1452 closed claims in 4 categories (obstetrics, surgery, missed or delayed diagnosis, and medication) from 5 liability insurers representing 4 regions of the US, and used objective criteria and independent reviewers to classify the merits of the claims. They found that 3% of the claims had no verifiable medical injury and 37% did not involve errors. About 73% of the claims not associated with errors or injuries resulted in no compensation, while 73% of those with errors did result in compensation. Further payment for claims not involving errors were lower than those that did involve errors. Looked at another way, of the 1452 claims reviewed, about 10% received payment but had no identifiable error, while about 17% had an identifiable error but no payment was made.3
This study demonstrated that: 1) the cost of defending claims involving no error was substantial but still only amounted to about 13% of direct system costs, meaning that contesting and paying for claims caused by errors accounts for most of the costs of the liability system, and 2) the malpractice system works reasonably well at separating claims without merit from those with merit.
Nonetheless, the study also demonstrated the unfairness of a system in which 1 in 6 valid claims received no payment (this in addition to the vast number of negligent injuries that never even lead to a claim as discussed in the 1999 IOM report). Then there is the frustration with a system wherein the average time between injury and claim resolution is 5 years and 54% of the payments are absorbed by defense costs and contingency fees. That 80% of expenses were incurred in resolving claims with errors suggests that steps to decrease frivolous litigation (claims without merit) will not lead to substantial savings and that steps to streamlining the system of handling claims will be more useful.
Blake et al looked at state-specific data from the National Practitioner Data Bank, which collects reports of all malpractice payments in the US on behalf of physicians, dentists, and nurses. They looked at the relationship between payments, physician premiums, and various state tort reforms. They found that mean payments were 26% lower in states with total damage caps ($196,000 vs $265,000) and 22% less in states with noneconomic (pain and suffering) damage caps ($212,000 vs $279,000). In addition, total damage caps were associated with lower mean annual premiums and hard, but not soft (caps with exceptions) noneconomic caps were associated with premium reductions. No other state tort reforms measured showed a significant association with payments or premiums.4
Studdert et al surveyed Pennsylvania physicians in high-risk specialties (obstetrics/gynecology, ortho, ER, surgery, neurosurgery) to ascertain self-report of defensive medicine practice. Almost all respondents reported practicing defensive medicine, the most common form (92%) being unnecessary ordering of tests and imaging studies and referring for consultation. In addition, 42% said they had restricted their practice by either decreasing the performance of more risky procedures (eg, trauma surgery) or avoiding complex cases or patients perceived as more likely to sue. Defensive medicine was highly correlated with physicians’ lack of confidence in their liability insurance or its cost.5
Kessler et al looked at physician supply from 1985–2001 and its correlates to state tort reforms during that time. Three years after States that adopted direct reforms (mainly caps on damage awards) showed an average physician growth rate within 3 years that was 3.3% greater than states not adopting such reforms. The authors controlled for a variety of factors that can influence physician supply including population growth and other state-level characteristics.6
Common Good proposal
Another approach is advocated by Common Good, a bipartisan legal reform coalition. This organization has funding from the RWJ Foundation to work with researchers from the Harvard School of Public Health to investigate the creation of special health courts to hear malpractice cases.11 Their ideas are incorporated into the Fair and Reliable Medical Justice Act introduced as S.1337 by Senators Mike Enzi (R-WY) Max Baucus (D-MT).11
How it would work. Health courts would have full-time judges, neutral medical experts, faster proceedings with legal fees held to 20%, and rulings that could be appealed to a new Medical Appellate Court. Like other administrative courts that handle tax disputes, workmen’s comp, and vaccine injury, there would be no juries. Judges would issue written rulings and establish legal precedents. Once a mistake was verified, recovery would be automatic. Patients would be reimbursed for all their medical expenses and lost income plus a fixed sum that would be determined from an expert derived schedule addressing specific types of injuries.
Strengths and weaknesses. This proposal has the support of a wide array of national medical and legal leaders but not any medical associations. It attempts to address some of the most egregious parts of the current system—the time it takes to get claims resolved, the many errors that go uncompensated, and the diversion of so many dollars to overhead and legal fees rather than to patients. On the other hand, the plan does not provide firm caps, which may make the AMA and other professional associations skeptical. And the proposed health courts would rely on select medical experts and judges, a system likely to be strongly opposed by trial lawyers and some consumer groups. It also does not directly address the prevention of patient errors.
Those who fail to learn from history…
The current malpractice crisis may be abating, leaving physicians with higher malpractice premiums but some state tort reforms. History, however, suggests that the insurance cycle will eventually lead to another crisis. There may be a window of opportunity now to come up with a completely different system to address the goals and problems with our current system, but it is likely to be a small window. Capitalizing on it will require a willingness for both sides in the current stand-off to get past their own self-interests in order to come up with something better for all.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
A handful of papers published in the past few years have looked at different aspects of the current malpractice situation and have yielded some revelations (see page 775 in this issue) or data banks working on safety issues.
- Though it does a reasonable job at separating valid from invalid claims and compensating them accordingly, it often takes a tremendously long time to accomplish this and still has a 10% to 16% rate of false positive (payment with no error) and false negative (no payment with error) outcomes.
- The system is not overwhelmed with frivolous claims. Still, it costs a lot of money to manage, and less than half of this money goes to claimants.
- Hard caps on total damages or noneconomic damages, unlike other state tort reforms (Figure), appear to reduce claims payments, physician premiums, and total health costs,7 while increasing physician supply.
- Defensive medicine exists, though putting a valid dollar amount on its costs is difficult.
- Anecdotal evidence suggests that physicians are leaving practice or limiting their practice (eg, family physicians discontinuing deliveries) as a result of malpractice costs.
FIGURE
Tort reforms commonly adopted by states
AMA’s proposal for change
Malpractice reform has been at or near the top of the AMA’s political agenda for the past 4 or 5 years, with strong lobbying efforts at the national level as well as support for state chapter efforts. The AMA’s proposal is based on California’s liability reform law known as MICRA that was passed over 30 years ago and has been associated with significantly lower premium growth since then compared with the rest of the US.8 Key provisions:
- Unlimited economic damages (medical expenses, future earnings)
- Limits on noneconomic damages (pain and suffering)
- Punitive damages, if available, up to $250,000 or 2 times economic damages, whichever is greater
- Allocation of damage awards in proportion to fault
- Sliding scale for attorney contingency fees.
Dubious premises. The AMA literature on malpractice includes valid information on the costs of the tort system, the rise in claims payouts, and effects on physician premiums. But it also suggests that meritless lawsuits are increasing. This is untrue. And its implication that physicians are increasingly leaving practice is anecdotal. There is no good research on the extent of this problem.8
Too narrow a focus. More important, the AMA plan is focused on physician premium costs while ignoring the unfairness of the system (eg, time to resolve claims, lack of payment for many patients with legitimate claims) and the vast number of medical errors for which claims are never filed.
The MEDIC proposal
Senators Hillary Clinton (D-NY) and Barack Obama (D-IL) have proposed federal legislation to address the malpractice crisis. Their bill would create an Office of Patient Safety in the Department of Health and Human Services, and would establish the National Medical Error Disclosure and Compensation (MEDIC) program within that office.9
Apologies would not be actionable in court. The MEDIC program would provide grants to physicians, hospitals, and health systems for the creation of programs to disclose medical errors to patients and negotiate fair compensation. The law would preserve confidentiality so that any apology offered by a health care provider as part of those negotiations would be kept confidential and could not be used in a trial. Any savings achieved from lower administrative and legal costs would be used to reduce physician malpractice premiums and toward patient safety initiatives.
Federal mandating of caps unlikely, however. At the federal level, Democrats have firmly opposed mandating caps on malpractice claims settlements. They argue that caps are unfair to patients who have been victims of medical errors. Others say this opposition reflects financial contributions from trial lawyers. It seems time to get past this conflict. Without dramatic changes in the composition of the Senate, which seems unlikely, there is little or no chance that caps will pass at the national level. At the same time, physician groups have been successful at achieving caps in a number of states (total of 26 at last count).
Signs this program could succeed. The MEDIC proposal is an attempt to find another way out of the malpractice impasse in the Senate by linking the patient safety and tort reform issues. It is primarily based on a growing movement to have physicians more directly acknowledge medical errors to patients,10 and in some cases, link these apologies to immediate financial negotiations to settle any potential claim of injury. The University of Michigan is the best known academic institution pursuing these strategies, and they report a significant decrease in the number of claims and annual litigation costs. The Lexington, Kentucky, VA Hospital has a similar program that has reduced liability costs compared with other VA hospitals.
The MEDIC proposal is attractive in its attempt to tie doctor-patient communication, patient safety, and liability together. And the anecdotal reports of success with isolated programs of its type are encouraging. It also moves the argument at a national level away from a fight about caps, which puts many physicians in the uncomfortable position of opposing Democrats who support many of their other positions—eg, Title VII funding, preservation of the traditional Medicare program, expansion of the Medicare Part D program, and better funding of public health programs. Nonetheless, there is a big row to hoe in making physicians more comfortable with acknowledging their errors, convincing them this would not be held against them in court, and assuring both physicians and hospitals that such efforts will actually lead to lower malpractice costs.
Thorpe analyzed data from 1995–2001 collected by the National Association of Insurance Commissioners to see the relationship between state tort reforms and premium levels. Premiums in states with caps on awards were 17% lower than states without caps. There was no association between premium levels and other reforms, such as caps on attorney fees or collateral offset rules (decreasing awards by the amount the plaintiff receives from other sources). Some association was noted between decreased competition among insurers and higher premiums.1
Rodwin et al used data from AMA surveys of self-employed physicians (physicians in groups or solo practice who are not employees) from 1970 to 2000. They found that while premiums increased from 1970 to 1986 and from 1996 to 2000, they had only a small effect on physician income. Premiums made up a small percentage of total practice costs and had a negligible effect on practice income, arguing against a malpractice crisis. However, this study lacked more recent data on premium increases and practice expenses and did not take into account differences among states that might be due to tort reforms such as the institution of caps on awards.2
Studdert et al reviewed 1452 closed claims in 4 categories (obstetrics, surgery, missed or delayed diagnosis, and medication) from 5 liability insurers representing 4 regions of the US, and used objective criteria and independent reviewers to classify the merits of the claims. They found that 3% of the claims had no verifiable medical injury and 37% did not involve errors. About 73% of the claims not associated with errors or injuries resulted in no compensation, while 73% of those with errors did result in compensation. Further payment for claims not involving errors were lower than those that did involve errors. Looked at another way, of the 1452 claims reviewed, about 10% received payment but had no identifiable error, while about 17% had an identifiable error but no payment was made.3
This study demonstrated that: 1) the cost of defending claims involving no error was substantial but still only amounted to about 13% of direct system costs, meaning that contesting and paying for claims caused by errors accounts for most of the costs of the liability system, and 2) the malpractice system works reasonably well at separating claims without merit from those with merit.
Nonetheless, the study also demonstrated the unfairness of a system in which 1 in 6 valid claims received no payment (this in addition to the vast number of negligent injuries that never even lead to a claim as discussed in the 1999 IOM report). Then there is the frustration with a system wherein the average time between injury and claim resolution is 5 years and 54% of the payments are absorbed by defense costs and contingency fees. That 80% of expenses were incurred in resolving claims with errors suggests that steps to decrease frivolous litigation (claims without merit) will not lead to substantial savings and that steps to streamlining the system of handling claims will be more useful.
Blake et al looked at state-specific data from the National Practitioner Data Bank, which collects reports of all malpractice payments in the US on behalf of physicians, dentists, and nurses. They looked at the relationship between payments, physician premiums, and various state tort reforms. They found that mean payments were 26% lower in states with total damage caps ($196,000 vs $265,000) and 22% less in states with noneconomic (pain and suffering) damage caps ($212,000 vs $279,000). In addition, total damage caps were associated with lower mean annual premiums and hard, but not soft (caps with exceptions) noneconomic caps were associated with premium reductions. No other state tort reforms measured showed a significant association with payments or premiums.4
Studdert et al surveyed Pennsylvania physicians in high-risk specialties (obstetrics/gynecology, ortho, ER, surgery, neurosurgery) to ascertain self-report of defensive medicine practice. Almost all respondents reported practicing defensive medicine, the most common form (92%) being unnecessary ordering of tests and imaging studies and referring for consultation. In addition, 42% said they had restricted their practice by either decreasing the performance of more risky procedures (eg, trauma surgery) or avoiding complex cases or patients perceived as more likely to sue. Defensive medicine was highly correlated with physicians’ lack of confidence in their liability insurance or its cost.5
Kessler et al looked at physician supply from 1985–2001 and its correlates to state tort reforms during that time. Three years after States that adopted direct reforms (mainly caps on damage awards) showed an average physician growth rate within 3 years that was 3.3% greater than states not adopting such reforms. The authors controlled for a variety of factors that can influence physician supply including population growth and other state-level characteristics.6
Common Good proposal
Another approach is advocated by Common Good, a bipartisan legal reform coalition. This organization has funding from the RWJ Foundation to work with researchers from the Harvard School of Public Health to investigate the creation of special health courts to hear malpractice cases.11 Their ideas are incorporated into the Fair and Reliable Medical Justice Act introduced as S.1337 by Senators Mike Enzi (R-WY) Max Baucus (D-MT).11
How it would work. Health courts would have full-time judges, neutral medical experts, faster proceedings with legal fees held to 20%, and rulings that could be appealed to a new Medical Appellate Court. Like other administrative courts that handle tax disputes, workmen’s comp, and vaccine injury, there would be no juries. Judges would issue written rulings and establish legal precedents. Once a mistake was verified, recovery would be automatic. Patients would be reimbursed for all their medical expenses and lost income plus a fixed sum that would be determined from an expert derived schedule addressing specific types of injuries.
Strengths and weaknesses. This proposal has the support of a wide array of national medical and legal leaders but not any medical associations. It attempts to address some of the most egregious parts of the current system—the time it takes to get claims resolved, the many errors that go uncompensated, and the diversion of so many dollars to overhead and legal fees rather than to patients. On the other hand, the plan does not provide firm caps, which may make the AMA and other professional associations skeptical. And the proposed health courts would rely on select medical experts and judges, a system likely to be strongly opposed by trial lawyers and some consumer groups. It also does not directly address the prevention of patient errors.
Those who fail to learn from history…
The current malpractice crisis may be abating, leaving physicians with higher malpractice premiums but some state tort reforms. History, however, suggests that the insurance cycle will eventually lead to another crisis. There may be a window of opportunity now to come up with a completely different system to address the goals and problems with our current system, but it is likely to be a small window. Capitalizing on it will require a willingness for both sides in the current stand-off to get past their own self-interests in order to come up with something better for all.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
1. Thorpe K. The Medical malpractice “crisis”: Recent trends and the impact of state tort reforms. Health Affairs 2004 January 21;web-only.
2. Rodwin M, Chang H, Clausen J. Malpractice premiums and physicians’ income: Perceptions of a crisis conflict with empirical evidence. Health Affairs 2006;525:750-758.
3. Studdert D, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med 2006;354:2024-2033.
4. Guirguis-Blake J, Fryer GE, Phillips RL, Jr, Szabat R, Green LA. The US medical liability system: Evidence for legislative reform. Ann Fam Med 2006;4:240-246.
5. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005;293:2609-2617.
6. Kessler DP, Sage WM, Becker DJ, et al. Impact of malpractice reforms on the supply of physician services. JAMA 2005;293:2618-2625.
7. Hellinger F, Encinosa W. The impact of state laws limiting malpractice damage awards on health care expenditures. AJPH 2006;96:1375-1381.
8. American Medical Association. Medical liability talking points. Available at: www.ama-assn.org/ama1/pub/upload/mm/399/mlr_fastfacts.pdf. Accessed on August 15, 2006.
9. Clinton HR, Obama B. Making patient safety the centerpiece of medical liability reform. N Engl J Med 2006;354:2205-2208.
10. O’Reilly K. Harvard adopts a disclosure and apology policy. AMA News, June 12, 2006.
11. Common Good. What are health courts? Available at: cgood.org/f-healthcourtsinfo.html. Accessed on August 15, 2006.
1. Thorpe K. The Medical malpractice “crisis”: Recent trends and the impact of state tort reforms. Health Affairs 2004 January 21;web-only.
2. Rodwin M, Chang H, Clausen J. Malpractice premiums and physicians’ income: Perceptions of a crisis conflict with empirical evidence. Health Affairs 2006;525:750-758.
3. Studdert D, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med 2006;354:2024-2033.
4. Guirguis-Blake J, Fryer GE, Phillips RL, Jr, Szabat R, Green LA. The US medical liability system: Evidence for legislative reform. Ann Fam Med 2006;4:240-246.
5. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005;293:2609-2617.
6. Kessler DP, Sage WM, Becker DJ, et al. Impact of malpractice reforms on the supply of physician services. JAMA 2005;293:2618-2625.
7. Hellinger F, Encinosa W. The impact of state laws limiting malpractice damage awards on health care expenditures. AJPH 2006;96:1375-1381.
8. American Medical Association. Medical liability talking points. Available at: www.ama-assn.org/ama1/pub/upload/mm/399/mlr_fastfacts.pdf. Accessed on August 15, 2006.
9. Clinton HR, Obama B. Making patient safety the centerpiece of medical liability reform. N Engl J Med 2006;354:2205-2208.
10. O’Reilly K. Harvard adopts a disclosure and apology policy. AMA News, June 12, 2006.
11. Common Good. What are health courts? Available at: cgood.org/f-healthcourtsinfo.html. Accessed on August 15, 2006.
The Journal of Family Practice ©2006 Dowden Health Media
Malpractice crisis: Causes of escalating insurance premiums, and implications for you
What has led to the current malpractice crisis? There are 2 main theories.
Physicians, insurers, and hospitals generally blame lawyers and the litigation system for increasing the number of claims filed (claim frequency) and the average payout on claims (claims severity).
Attorneys and consumer groups argue that malpractice insurance goes through natural cycles in costs and charges. For the rise in premiums in the current crisis, they particularly blame decreased investment returns and poor pricing decisions by insurers.
Who’s right?
Research suggests that neither argument alone is persuasive. For instance, a study of the National Practitioner Data Bank, which collects results of all malpractice claims payments, found that claims severity did increase since 1991, but not during the current malpractice crisis period when adjusted for inflation: 52% from 1991 to 2003 but only 6% from 2000 to 2003.1 The highest growth rate has been in medium-sized awards, not the large ones you often read about. And, as always, claims severity growth varies among states (FIGURE 1).1
In contrast, when adjusted for population changes, Data Bank studies showed no significant nationwide increase in the number of paid claims from 1991 to 2003. Data from individual states also bear this out.1
Furthermore, studies of the relationship between claims’ payments and premiums have shown only a weakly positive relationship, suggesting other factors are involved. The argument that decreased investment returns have led to large price increases probably has some merit but does not explain the magnitude of the changes or the variation across states.
FIGURE 1
Amount of average paid claim, 1991-2003
So, what’s the answer for physicians?
Most likely, a combination of several changes has led to the recent crisis—increased claims’ costs, poor pricing decisions or cost projections by insurers, and decreased investment income. Rather than seeing these issues as distinct, it may be more useful to see their intrinsic relationships in leading to rapid premium increases and a malpractice crisis.
In this article, the first of 2, I discuss recent events influencing insurance premiums, which may also suggest to you avenues to explore in optimizing your own coverage. In part 2, I will address our current tort system and concrete proposals for change being pursued.
How premiums are determined
Almost all physicians carry professional liability (malpractice) insurance, either by choice or legal requirement. Coverage is usually purchased individually or by group from a commercial company or a physician-owned mutual company. Hospitals may purchase insurance or be self-insured, and their physician employees may be covered through those policies.
In theory, a tort system to resolve malpractice claims is supposed to serve as a negative incentive to physicians to practice high quality medicine. But the 1999 Institute of Medicine report on the occurrence and ramifications of medical errors, To Err is Human,2 provided evidence that the malpractice system has failed to accomplish this goal.
Unlike auto insurance, malpractice premiums are mainly determined by the class of physician (including type of work) and geography, rather than by an individual’s practice experience. Auto insurance premiums are adjusted according to the insured’s driving record. This is difficult to accomplish with malpractice insurance because claims experience is too variable over short periods of time.
Insurers take the following into account when they set premiums: 1) anticipated payouts to a class of physicians and the uncertainty of their estimate; 2) expected administrative expenses to manage the insurance; 3) future investment income; and 4) desired amount of profit. Information on past losses and expenses is used but, clearly, much of the determination involves complicated predictions.
Another characteristic that makes rate setting difficult is the length of time from the occurrence of an event to the filing of a claim to the resolution of that claim. On average, this is 4 to 5 years. The difficulty in predicting the liability for claims that have not yet been filed adds to the problem in setting premiums accurately.
How does your state manage rate setting?
Although malpractice has been a political issue at the federal level in the past few years, the reality is that, like most insurance, it is mainly regulated by the states.
States with substantial restrictions (17 states in 2004) require insurers to file rate changes and gain approval before prices can change.
States with less restrictive environments require such prior approval only if rate increases exceed a certain amount (23 in 2004) or only require notification after rates are changed (9 in 2004).1
Whether these varying types of state regulation lead to higher or lower premiums is unclear.
In addition to these strategies, states have also implemented an array of tort reforms in an attempt to address the cost of physician malpractice policies. Caps have been the most popular reform, with 26 states instituting them (FIGURE 2).3
FIGURE 2
Caps on damages by state
Recent events influencing premiums
A number of changes in the past few years have occurred in the malpractice arena
- Increased numbers of physician-owned companies and fewer commercial carriers since the malpractice crisis of the 1970s. These companies often give physicians better rates and more control, but some have been undercapitalized and not survived.
- A rise in the cost of reinsurance since September 11. Reinsurance covers costs above a certain level and limits companies’ losses in a given year. Reinsurers suffered large losses from the terrorist attacks of September 11, 2001 and, subsequently, raised their prices significantly to all liability companies.
- More hospitals self-insuring to better control rates and their risk pool leading increasing numbers of physicians to obtain their malpractice coverage through hospitals. This lowers their costs in comparison to those who practice in small groups or solo settings.
- A shift in the type of insurance from occurrence (all incidents in the policy year are covered regardless of when the claim is filed) to claims-made policies (coverage is for claims filed in the policy year regardless of when the event occurred). With claims-made insurance, physicians have to purchase costly “tail” policies to cover the possibility of incidents during the years of coverage becoming future claims.
- The growth of state-mandated funds as insurers of last resort for physicians who cannot find any coverage. These funds are financed by surcharges on hospital and physician malpractice policies, which in turn increases those costs.
- A decrease in companies’ investment yields since 2000 (from 5.2% in 2000 to4.3% in 2002), in spite of the fact that insurers’ portfolios are quite conservative as required by state law. While some companies saw their investment income drop by 50% in these years, this amount is still only a small part of insurers’ total income.
Options to explore
- Check with your state’s division of insurance website to see if there is a list of carriers, and information about their experience.
- Rather than a claims-made policy, consider getting an occurrence policy that will eliminate the worry and cost of purchasing “tail” insurance. If you work for a group practice, inquire about whether occurrence insurance is an option. If occurrence insurance is not available or seems too costly, ask your agent about what a typical tail policy would cost.
- You may want to inquire about purchasing insurance through a local hospital, which could yield cost savings.
- Don’t skimp on coverage amounts. Consider getting risk-management training to learn what you can do to minimize the risk of being sued.
A malpractice crisis, according to the AMA, occurs when “patients lose access to care as a result of a broken medical liability system… that causes physicians’ insurance premiums to skyrocket forcing them to restrict their practice.” An alternate description would be when insurers’ financial situation deteriorates resulting in higher than average increases in premiums or decrease in the supply of insurance. The existence and severity of a crisis varies from state to state (see map at right).4
Insurance becomes relatively unaffordable when premiums increase rapidly, as occurred in the second malpractice crisis in the mid-1980s and also in the current crisis, which has seen increasing premiums since 1999 and some moderation since 2004. Increases in premiums may differ across states, within states, and among specialties.
How providers feel about premium increases depends on both the size and rapidity of the increases and by their ability to collect more for their services to pay for increases. In the current crisis, providers have had more difficulty maintaining a balance between cost increases and income as discounted fee contracts and lack of growth in Medicare and Medicaid payments have constrained growth in practice revenue.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
1. Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood) 2005 Jan-Jun; Suppl Web Exclusives:W5-240-W5-249. Available at: content.healthaffairs.org/cgi/content/abstract/hlthaff.w5.240. Accessed on July 18, 2006.
2. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
3. Mello MM. Medical malpractice: Impact of crisis and effect of state tort reforms. The Synthesis Project Policy Brief #10, May 2006. Available at: www.rwjf.org/publications/synthesis/reports_and_briefs/charts/no10_pb_fig2.jpg. Accessed on July 18, 2006.
4. Medical liability crisis map. AMA News and Information [website]. Available at: www.amaassn.org/ama/noindex/category/11871.html. Accessed on July 18. 2006.
What has led to the current malpractice crisis? There are 2 main theories.
Physicians, insurers, and hospitals generally blame lawyers and the litigation system for increasing the number of claims filed (claim frequency) and the average payout on claims (claims severity).
Attorneys and consumer groups argue that malpractice insurance goes through natural cycles in costs and charges. For the rise in premiums in the current crisis, they particularly blame decreased investment returns and poor pricing decisions by insurers.
Who’s right?
Research suggests that neither argument alone is persuasive. For instance, a study of the National Practitioner Data Bank, which collects results of all malpractice claims payments, found that claims severity did increase since 1991, but not during the current malpractice crisis period when adjusted for inflation: 52% from 1991 to 2003 but only 6% from 2000 to 2003.1 The highest growth rate has been in medium-sized awards, not the large ones you often read about. And, as always, claims severity growth varies among states (FIGURE 1).1
In contrast, when adjusted for population changes, Data Bank studies showed no significant nationwide increase in the number of paid claims from 1991 to 2003. Data from individual states also bear this out.1
Furthermore, studies of the relationship between claims’ payments and premiums have shown only a weakly positive relationship, suggesting other factors are involved. The argument that decreased investment returns have led to large price increases probably has some merit but does not explain the magnitude of the changes or the variation across states.
FIGURE 1
Amount of average paid claim, 1991-2003
So, what’s the answer for physicians?
Most likely, a combination of several changes has led to the recent crisis—increased claims’ costs, poor pricing decisions or cost projections by insurers, and decreased investment income. Rather than seeing these issues as distinct, it may be more useful to see their intrinsic relationships in leading to rapid premium increases and a malpractice crisis.
In this article, the first of 2, I discuss recent events influencing insurance premiums, which may also suggest to you avenues to explore in optimizing your own coverage. In part 2, I will address our current tort system and concrete proposals for change being pursued.
How premiums are determined
Almost all physicians carry professional liability (malpractice) insurance, either by choice or legal requirement. Coverage is usually purchased individually or by group from a commercial company or a physician-owned mutual company. Hospitals may purchase insurance or be self-insured, and their physician employees may be covered through those policies.
In theory, a tort system to resolve malpractice claims is supposed to serve as a negative incentive to physicians to practice high quality medicine. But the 1999 Institute of Medicine report on the occurrence and ramifications of medical errors, To Err is Human,2 provided evidence that the malpractice system has failed to accomplish this goal.
Unlike auto insurance, malpractice premiums are mainly determined by the class of physician (including type of work) and geography, rather than by an individual’s practice experience. Auto insurance premiums are adjusted according to the insured’s driving record. This is difficult to accomplish with malpractice insurance because claims experience is too variable over short periods of time.
Insurers take the following into account when they set premiums: 1) anticipated payouts to a class of physicians and the uncertainty of their estimate; 2) expected administrative expenses to manage the insurance; 3) future investment income; and 4) desired amount of profit. Information on past losses and expenses is used but, clearly, much of the determination involves complicated predictions.
Another characteristic that makes rate setting difficult is the length of time from the occurrence of an event to the filing of a claim to the resolution of that claim. On average, this is 4 to 5 years. The difficulty in predicting the liability for claims that have not yet been filed adds to the problem in setting premiums accurately.
How does your state manage rate setting?
Although malpractice has been a political issue at the federal level in the past few years, the reality is that, like most insurance, it is mainly regulated by the states.
States with substantial restrictions (17 states in 2004) require insurers to file rate changes and gain approval before prices can change.
States with less restrictive environments require such prior approval only if rate increases exceed a certain amount (23 in 2004) or only require notification after rates are changed (9 in 2004).1
Whether these varying types of state regulation lead to higher or lower premiums is unclear.
In addition to these strategies, states have also implemented an array of tort reforms in an attempt to address the cost of physician malpractice policies. Caps have been the most popular reform, with 26 states instituting them (FIGURE 2).3
FIGURE 2
Caps on damages by state
Recent events influencing premiums
A number of changes in the past few years have occurred in the malpractice arena
- Increased numbers of physician-owned companies and fewer commercial carriers since the malpractice crisis of the 1970s. These companies often give physicians better rates and more control, but some have been undercapitalized and not survived.
- A rise in the cost of reinsurance since September 11. Reinsurance covers costs above a certain level and limits companies’ losses in a given year. Reinsurers suffered large losses from the terrorist attacks of September 11, 2001 and, subsequently, raised their prices significantly to all liability companies.
- More hospitals self-insuring to better control rates and their risk pool leading increasing numbers of physicians to obtain their malpractice coverage through hospitals. This lowers their costs in comparison to those who practice in small groups or solo settings.
- A shift in the type of insurance from occurrence (all incidents in the policy year are covered regardless of when the claim is filed) to claims-made policies (coverage is for claims filed in the policy year regardless of when the event occurred). With claims-made insurance, physicians have to purchase costly “tail” policies to cover the possibility of incidents during the years of coverage becoming future claims.
- The growth of state-mandated funds as insurers of last resort for physicians who cannot find any coverage. These funds are financed by surcharges on hospital and physician malpractice policies, which in turn increases those costs.
- A decrease in companies’ investment yields since 2000 (from 5.2% in 2000 to4.3% in 2002), in spite of the fact that insurers’ portfolios are quite conservative as required by state law. While some companies saw their investment income drop by 50% in these years, this amount is still only a small part of insurers’ total income.
Options to explore
- Check with your state’s division of insurance website to see if there is a list of carriers, and information about their experience.
- Rather than a claims-made policy, consider getting an occurrence policy that will eliminate the worry and cost of purchasing “tail” insurance. If you work for a group practice, inquire about whether occurrence insurance is an option. If occurrence insurance is not available or seems too costly, ask your agent about what a typical tail policy would cost.
- You may want to inquire about purchasing insurance through a local hospital, which could yield cost savings.
- Don’t skimp on coverage amounts. Consider getting risk-management training to learn what you can do to minimize the risk of being sued.
A malpractice crisis, according to the AMA, occurs when “patients lose access to care as a result of a broken medical liability system… that causes physicians’ insurance premiums to skyrocket forcing them to restrict their practice.” An alternate description would be when insurers’ financial situation deteriorates resulting in higher than average increases in premiums or decrease in the supply of insurance. The existence and severity of a crisis varies from state to state (see map at right).4
Insurance becomes relatively unaffordable when premiums increase rapidly, as occurred in the second malpractice crisis in the mid-1980s and also in the current crisis, which has seen increasing premiums since 1999 and some moderation since 2004. Increases in premiums may differ across states, within states, and among specialties.
How providers feel about premium increases depends on both the size and rapidity of the increases and by their ability to collect more for their services to pay for increases. In the current crisis, providers have had more difficulty maintaining a balance between cost increases and income as discounted fee contracts and lack of growth in Medicare and Medicaid payments have constrained growth in practice revenue.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
What has led to the current malpractice crisis? There are 2 main theories.
Physicians, insurers, and hospitals generally blame lawyers and the litigation system for increasing the number of claims filed (claim frequency) and the average payout on claims (claims severity).
Attorneys and consumer groups argue that malpractice insurance goes through natural cycles in costs and charges. For the rise in premiums in the current crisis, they particularly blame decreased investment returns and poor pricing decisions by insurers.
Who’s right?
Research suggests that neither argument alone is persuasive. For instance, a study of the National Practitioner Data Bank, which collects results of all malpractice claims payments, found that claims severity did increase since 1991, but not during the current malpractice crisis period when adjusted for inflation: 52% from 1991 to 2003 but only 6% from 2000 to 2003.1 The highest growth rate has been in medium-sized awards, not the large ones you often read about. And, as always, claims severity growth varies among states (FIGURE 1).1
In contrast, when adjusted for population changes, Data Bank studies showed no significant nationwide increase in the number of paid claims from 1991 to 2003. Data from individual states also bear this out.1
Furthermore, studies of the relationship between claims’ payments and premiums have shown only a weakly positive relationship, suggesting other factors are involved. The argument that decreased investment returns have led to large price increases probably has some merit but does not explain the magnitude of the changes or the variation across states.
FIGURE 1
Amount of average paid claim, 1991-2003
So, what’s the answer for physicians?
Most likely, a combination of several changes has led to the recent crisis—increased claims’ costs, poor pricing decisions or cost projections by insurers, and decreased investment income. Rather than seeing these issues as distinct, it may be more useful to see their intrinsic relationships in leading to rapid premium increases and a malpractice crisis.
In this article, the first of 2, I discuss recent events influencing insurance premiums, which may also suggest to you avenues to explore in optimizing your own coverage. In part 2, I will address our current tort system and concrete proposals for change being pursued.
How premiums are determined
Almost all physicians carry professional liability (malpractice) insurance, either by choice or legal requirement. Coverage is usually purchased individually or by group from a commercial company or a physician-owned mutual company. Hospitals may purchase insurance or be self-insured, and their physician employees may be covered through those policies.
In theory, a tort system to resolve malpractice claims is supposed to serve as a negative incentive to physicians to practice high quality medicine. But the 1999 Institute of Medicine report on the occurrence and ramifications of medical errors, To Err is Human,2 provided evidence that the malpractice system has failed to accomplish this goal.
Unlike auto insurance, malpractice premiums are mainly determined by the class of physician (including type of work) and geography, rather than by an individual’s practice experience. Auto insurance premiums are adjusted according to the insured’s driving record. This is difficult to accomplish with malpractice insurance because claims experience is too variable over short periods of time.
Insurers take the following into account when they set premiums: 1) anticipated payouts to a class of physicians and the uncertainty of their estimate; 2) expected administrative expenses to manage the insurance; 3) future investment income; and 4) desired amount of profit. Information on past losses and expenses is used but, clearly, much of the determination involves complicated predictions.
Another characteristic that makes rate setting difficult is the length of time from the occurrence of an event to the filing of a claim to the resolution of that claim. On average, this is 4 to 5 years. The difficulty in predicting the liability for claims that have not yet been filed adds to the problem in setting premiums accurately.
How does your state manage rate setting?
Although malpractice has been a political issue at the federal level in the past few years, the reality is that, like most insurance, it is mainly regulated by the states.
States with substantial restrictions (17 states in 2004) require insurers to file rate changes and gain approval before prices can change.
States with less restrictive environments require such prior approval only if rate increases exceed a certain amount (23 in 2004) or only require notification after rates are changed (9 in 2004).1
Whether these varying types of state regulation lead to higher or lower premiums is unclear.
In addition to these strategies, states have also implemented an array of tort reforms in an attempt to address the cost of physician malpractice policies. Caps have been the most popular reform, with 26 states instituting them (FIGURE 2).3
FIGURE 2
Caps on damages by state
Recent events influencing premiums
A number of changes in the past few years have occurred in the malpractice arena
- Increased numbers of physician-owned companies and fewer commercial carriers since the malpractice crisis of the 1970s. These companies often give physicians better rates and more control, but some have been undercapitalized and not survived.
- A rise in the cost of reinsurance since September 11. Reinsurance covers costs above a certain level and limits companies’ losses in a given year. Reinsurers suffered large losses from the terrorist attacks of September 11, 2001 and, subsequently, raised their prices significantly to all liability companies.
- More hospitals self-insuring to better control rates and their risk pool leading increasing numbers of physicians to obtain their malpractice coverage through hospitals. This lowers their costs in comparison to those who practice in small groups or solo settings.
- A shift in the type of insurance from occurrence (all incidents in the policy year are covered regardless of when the claim is filed) to claims-made policies (coverage is for claims filed in the policy year regardless of when the event occurred). With claims-made insurance, physicians have to purchase costly “tail” policies to cover the possibility of incidents during the years of coverage becoming future claims.
- The growth of state-mandated funds as insurers of last resort for physicians who cannot find any coverage. These funds are financed by surcharges on hospital and physician malpractice policies, which in turn increases those costs.
- A decrease in companies’ investment yields since 2000 (from 5.2% in 2000 to4.3% in 2002), in spite of the fact that insurers’ portfolios are quite conservative as required by state law. While some companies saw their investment income drop by 50% in these years, this amount is still only a small part of insurers’ total income.
Options to explore
- Check with your state’s division of insurance website to see if there is a list of carriers, and information about their experience.
- Rather than a claims-made policy, consider getting an occurrence policy that will eliminate the worry and cost of purchasing “tail” insurance. If you work for a group practice, inquire about whether occurrence insurance is an option. If occurrence insurance is not available or seems too costly, ask your agent about what a typical tail policy would cost.
- You may want to inquire about purchasing insurance through a local hospital, which could yield cost savings.
- Don’t skimp on coverage amounts. Consider getting risk-management training to learn what you can do to minimize the risk of being sued.
A malpractice crisis, according to the AMA, occurs when “patients lose access to care as a result of a broken medical liability system… that causes physicians’ insurance premiums to skyrocket forcing them to restrict their practice.” An alternate description would be when insurers’ financial situation deteriorates resulting in higher than average increases in premiums or decrease in the supply of insurance. The existence and severity of a crisis varies from state to state (see map at right).4
Insurance becomes relatively unaffordable when premiums increase rapidly, as occurred in the second malpractice crisis in the mid-1980s and also in the current crisis, which has seen increasing premiums since 1999 and some moderation since 2004. Increases in premiums may differ across states, within states, and among specialties.
How providers feel about premium increases depends on both the size and rapidity of the increases and by their ability to collect more for their services to pay for increases. In the current crisis, providers have had more difficulty maintaining a balance between cost increases and income as discounted fee contracts and lack of growth in Medicare and Medicaid payments have constrained growth in practice revenue.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
1. Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood) 2005 Jan-Jun; Suppl Web Exclusives:W5-240-W5-249. Available at: content.healthaffairs.org/cgi/content/abstract/hlthaff.w5.240. Accessed on July 18, 2006.
2. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
3. Mello MM. Medical malpractice: Impact of crisis and effect of state tort reforms. The Synthesis Project Policy Brief #10, May 2006. Available at: www.rwjf.org/publications/synthesis/reports_and_briefs/charts/no10_pb_fig2.jpg. Accessed on July 18, 2006.
4. Medical liability crisis map. AMA News and Information [website]. Available at: www.amaassn.org/ama/noindex/category/11871.html. Accessed on July 18. 2006.
1. Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood) 2005 Jan-Jun; Suppl Web Exclusives:W5-240-W5-249. Available at: content.healthaffairs.org/cgi/content/abstract/hlthaff.w5.240. Accessed on July 18, 2006.
2. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
3. Mello MM. Medical malpractice: Impact of crisis and effect of state tort reforms. The Synthesis Project Policy Brief #10, May 2006. Available at: www.rwjf.org/publications/synthesis/reports_and_briefs/charts/no10_pb_fig2.jpg. Accessed on July 18, 2006.
4. Medical liability crisis map. AMA News and Information [website]. Available at: www.amaassn.org/ama/noindex/category/11871.html. Accessed on July 18. 2006.
HIV postexposure prophylaxis: Who should get it?
One of your office personnel receives a superficial stick from a needle while putting it into a sharps disposal container. Is postexposure prophylaxis (PEP) for HIV warranted?
Another health care worker receives a major blood splash into her eye after dropping a blood tube taken from a source of unknown HIV status. Is PEP called for in this instance?
A child who was rifling through a trash bin accidentally poked himself with an improperly disposed hypodermic needle. Should he be given PEP?
In most cases, HIV PEP is given only to healthcare workers if the settings make exposure to HIV-infected persons likely. Otherwise, it is usually deemed unnecessary. However, a decision for or against PEP is complicated.
Occupational and nonoccupational exposure to HIV can produce fear, anxiety, and stress. Information on the exposure risk is frequently incomplete, the risk of infection is usually low, the degree of protection offered by PEP is not fully defined, and the potential for side effects from the medications is significant.
This article distills the Centers for Disease Control and Prevention’s most recent guidance on HIV PEP.
HIV on the rise again
Antiretroviral therapy has markedly reduced mortality from HIV/AIDS, but the incidence of new cases, after declining in the 1990s, has gradually increased since 2000.1 As described in a previous article in the Journal of Family Practice,2 efforts to control HIV now focus on increased testing of those persons at risk, behavior modification to reduce the chances of infected persons exposing others, and treating HIV-positive pregnant women and providing postnatal prophylaxis to their newly born infants.
Exposure to HIV can occur occupationally, during a sexual assault, or from the failure of barrier protection during sex. Though these types of exposure are not major contributors to HIV incidence, and postexposure prophylaxis is not expected to play a major role in reducing the incidence of disease, it is available to persons potentially exposed to HIV, and it is beneficial to know when it is and is not indicated. Evidence for possible effectiveness of PEP comes from studies of postnatal prophylaxis, animal studies, case control studies and case reports.3
The Centers for Disease Control and Prevention (CDC) has developed 2 sets of recommendations for PEP that take into consideration the type and severity of the exposure and characteristics of the source of the exposure (TABLE 1).3,4
TABLE 1
Recommended HIV postexposure prophylaxis for percutanous injuries and membrane/nonintact skin exposures
| For percutaneous injuries | |||||
| EXPOSURE TYPE | INFECTION STATUS OF SOURCE | ||||
| HIV-POSITIVE, CLASS 1* | HIV-POSITIVE, CLASS 2* | SOURCE OF UNKNOWN HIV STATUS† | UNKNOWN SOURCE‡ | HIV-NEGATIVE | |
| Less severe (eg, solid needle or supercficial injury) | Recommend basic 2-drug PEP | Recommend expanded ≥3-drug PEP | Generally, no PEP warranted however, consider basic 2-drug PEP¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV-infected persons is likely | No PEP warranted |
| More severe (large-bore hollow needle, deep puncture wound, blood on device, needle used in artery/vein) | Recommend expanded ≥3-drug PEP | Recommend expanded ≥3-drug PEP | Generally, no PEP warranted; however, consider basic 2-drug¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV infected persons is likely | No PEP warranted |
| For mucous membrane and nonintact skin exposures†† | |||||
| Small volume (eg, a few drops) | Consider basic 2-drug PEP¶ | Recommend basic 2-drug PEP | Generally, no PEP warranted** | Generally, no PEP warranted | No PEP warranted |
| Large volume (eg, a major blood splash) | Recommend basic 2-drug PEP | Recommend expended ≥3-drug PEP | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV-infected persons is likely | No PEP warranted |
| *HIV-positive, class 1—asymptomatic HIV infection or known low viral load (eg, <1500 ribonucleic acid copies/mL). HIV-positive, class 2—symptomatic HIV infection, AIDS, acute seroconversion, or known high viral load. If drug resistance is a concern, obtain expert consultation. Initiation of PEP should not be delayed pending expert consultation, and, because expert consultation alone cannot substitute for face-to-face counseling, resources should be available to provide immediate evaluation and follow-up care for all exposures. | |||||
| †For example, deceased source person with no samples available for HIV testing. | |||||
| ‡For example, a needle from a sharps container or splash from inappropriately disposed blood. | |||||
| ¶The recommendation “consider PEP” indicates that PEP is optional; a decision to initiate PEP should be based on a discussion between the exposed person and the treating clinician regarding the risks versus benefits of PEP. | |||||
| **If PEP is offered and administered and the source is later determined to be HIV-negative, PEP should be discontinued. | |||||
| ††For skin exposures, follow-up is indicated only if evidence exists of compromised skin integrity (eg, dermatitis, abrasion, or open wound). | |||||
| Source: Centers for Disease Control and Prevention 2005.4 | |||||
Occupational exposures to HIV
Occupational exposure to HIV can result from a needlestick injury, cut with a sharp object, or contact with potentially infectious body fluids to mucous membranes or skin that is not intact (chapped, cut, abraded, inflamed). Body fluids that are considered potentially infectious are listed in TABLE 2, along with fluids not considered to be infectious.
The risk of contracting HIV from an occupational exposure is determined by several factors, but is generally low. The risk of infection after a needle-stick injury with exposure to infected blood is estimated at 0.3%; after a mucous membrane exposure, 0.09%. The risk after exposure to nonintact skin is probably even lower. Risk increases with the quantity of blood exposed to, a needle-stick injury directly into a vein or artery, and deep injuries.
TABLE 2
Which body fluids are infectious?
| BODY FLUIDS POTENTIALLY INFECTIOUS FOR HIV | |
|
|
| BODY FLUIDS NOT CONSIDERED TO BE INFECTIOUS UNLESS THEY ARE VISIBLY BLOODY | |
|
|
Who should and should not receive PEP
TABLE 1 details recommended treatment responses to specific types of exposure (eg, puncture wound) and the status of the exposure source.4 In situations unlikely to result in disease transmission (superficial injury and source patient with unknown HIV status), no PEP is generally warranted due to the low risk of infection and potential toxicity of antiretrovirals.
Treatment particulars
Start postexposure prophylaxis, when indicated, as soon as possible following exposure and continue it for 4 weeks. Obtain baseline test results for HIV at the time of exposure and periodically for 6 months. The CDC recommends testing at 6 weeks, 12 weeks, and 6 months, whether or not PEP is provided.
Testing and monitoring for hepatitis B and C may also be indicated.
Advise patients on PEP to use precautions in avoiding the possibility of secondary transmission, especially in the first 3 months following exposure. Monitor for drug toxicity every week or 2 while giving PEP. Because of the complexity of potential PEP regimens and the risk for drug toxicity, you may want to take advantage of several national sources of consultation, such as the PEPline (www.ucsf.edu/hivcntr/Hotlines/PEPline or 888-448-4911) or the HIV/AIDS Treatment Information Service (aidsinfo.nih.gov)—especially with questions about potential drug resistance or if the exposed person is pregnant.
When risk is real but low, 2-drug PEP is recommended (TABLE 1), usually 2 nucleoside reverse transcriptase inhibitors (NRTI) or 1 NRTI and 1 nucleotide reverse transcriptase inhibitor (NtRTI).
For those at higher risk, 3 or more antiviral regimens are recommended, achieved by adding a protease inhibitor to one of the recommended 2-drug regimens. The potential antiviral combinations in the basic 2-drug and expanded PEP regimens, along with potential side effects and toxicities of antiviral medications are described in TABLE W1, available online at www.jfponline.com.4
Nonoccupational exposures rarely require PEP
There are many unresolved questions regarding PEP for nonoccupational exposures. The lack of definitive evidence of its effectiveness, its unknown influence on risk-taking behavior, and the potential to aggravate viral resistance have led CDC to recommend that PEP be used only infrequently and not continuously for those whose behavior results in frequent exposures.3 Those who continue to participate in high risk activities should be referred for risk-reduction behavioral counseling.
The risk of HIV transmission varies by route and source of exposure (TABLE 3). The CDC has developed an algorithm based on these variables (FIGURE) to help you decide whether to initiate PEP. Two situations that cause concerns but pose little known risk of infection are bites and needlestick injuries from discarded needles; PEP is rarely indicated for either.
As with occupational exposure PEP, those receiving nonoccupational PEP should be evaluated at baseline for HIV infection. In addition, consider evaluating them for other STD’s and pregnancy.
As with occupational exposure, start nonoccupational PEP as soon as possible and continue it for 28 days. Nonoccupational PEP is not recommended if time after exposure is more than 72 hours. A 3-drug regimen is recommended by the CDC for nonoccupational exposures, even though evidence is lacking that it provides superior benefit over 2 drugs (see TABLE W1 at www.jfponline.com).
Follow-up recommendations for those provided nonoccupational PEP are the same as for occupational PEP, and testing for other STDs and hepatitis B and C is also recommended (TABLE 4).
FIGURE
Evaluation and treatment of possible nonoccupational HIV exposures
Source: Centers for Disease Control and Prevention 2005.3
TABLE 3
Estimated per-act risk for acquisition of HIV, by exposure route*
| EXPOSURE ROUTE | RISK PER 10,000 EXPOSURES TO AN INFECTED SOURCE |
|---|---|
| Blood transfusion | 9000 |
| Needle-sharing injection-drug use | 67 |
| Receptive anal intercourse | 50 |
| Percutaneous needle stick | 30 |
| Receptive penile-vaginal intercourse | 10 |
| Insertive anal intercourse | 6.5 |
| Insertive penile-vaginal intercourse | 5 |
| Receptive oral intercourse† | 1 |
| Insertive oral intercourse† | 0.5 |
| *Estimates of risk for transmission from sexual exposures assume no condom use. | |
| †Source refers to oral intercourse performed on a man. | |
| Source: Centers for Disease Control and Prevention 2005.3 | |
TABLE 4
Recommended laboratory evaluation for nonoccupational postexposure prophylaxis of HIV infection
| TEST | BASELINE | DURING PEP* | 4 TO 6 WEEKS AFTER EXPOSURE | 3 MONTHS AFTER EXPOSURE | 6 MONTHS AFTER EXPOSURE |
|---|---|---|---|---|---|
| HIV antibody testing | E, S† | E | E | E | |
| Complete blood count with differential | E | E | |||
| Serum liver enzymes | E | E | |||
| Blood urea nitrogen/creatinine | E | E | |||
| Sexually transmitted diseases screen (gonorrhea, chlamydia, syphilis) | E, S | E‡ | E‡ | ||
| Hepatitis B serology | E, S | E‡ | E‡ | ||
| Hepatitis C serology | E, S | E | E | ||
| Pregnancy test (for women of reproductive age) | E | E‡ | E‡ | ||
| HIV viral load | S | E§ | E§ | E§ | |
| HIV resistance testing | S | E§ | E§ | E§ | |
| CD4+T lymphocyte count | S | E§ | E§ | E§ | |
| PEP, postexposure prophylaxis; E, exposed patient; S, source. | |||||
| *Other specific tests might be indicated dependent on the antiretrovirals prescribed. Literature pertaining to individual agents should be consulted. | |||||
| †HIV antibody testing of the source patient is indicated for sources of unknown serostatus. | |||||
| ‡Additional testing for pregnancy, sexually transmitted diseases, and hepatitis B should be performed as clinically indicated. | |||||
| §If determined to be HIV infected on follow-up testing; perform as clinically indicated once diagnosed. | |||||
Conclusion
When there is uncertainty whether PEP is recommended, start patients on a PEP regimen while the situation is sorted out. Fortunately, joint patient-physician decision making can be assisted by the physician consultation resources mentioned previously. Keep in mind that, depending on the circumstances of the exposure, HIV transmission is only one concern among others, including infectious diseases, pregnancy, and emotional/psychological aspects resulting from the incident.
CORRESPONDENCE
Doug Campos-Outcalt, MD,MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
REFERENCE
1. Centers for Disease Control and Prevention (CDC). Trends in HIV/AIDS Diagnoses—33 States, 2001-2004. MMWR Morb Mortal Wkly Rep 2005;54:1149-1153.Available at: www.cdc.gov/mmwr/preview/mmwrhtml/mm5445a1.htm. Accessed on June 8, 2006.
2. Campos-Outcalt D. HIV prevention enters a new era. J Fam Pract 2004;53:563-566.
3. CDC. Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposures to HIV in the United States. MMWR Recomm Rep 2005;54(RR-2).-Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm. Accessed on June 8, 2006.
4. CDC. Updated U.S. public health service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep 2005;54(RR-9).-Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm. Accessed on June 8, 2006.
5. US Department of Health and Human Services. Guideline for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents. October 29, 2004 revision. Available at: aidsinfo.nih.gov/guidelines.default_db2,asp?id+50. Accessed on June 8, 2006.
One of your office personnel receives a superficial stick from a needle while putting it into a sharps disposal container. Is postexposure prophylaxis (PEP) for HIV warranted?
Another health care worker receives a major blood splash into her eye after dropping a blood tube taken from a source of unknown HIV status. Is PEP called for in this instance?
A child who was rifling through a trash bin accidentally poked himself with an improperly disposed hypodermic needle. Should he be given PEP?
In most cases, HIV PEP is given only to healthcare workers if the settings make exposure to HIV-infected persons likely. Otherwise, it is usually deemed unnecessary. However, a decision for or against PEP is complicated.
Occupational and nonoccupational exposure to HIV can produce fear, anxiety, and stress. Information on the exposure risk is frequently incomplete, the risk of infection is usually low, the degree of protection offered by PEP is not fully defined, and the potential for side effects from the medications is significant.
This article distills the Centers for Disease Control and Prevention’s most recent guidance on HIV PEP.
HIV on the rise again
Antiretroviral therapy has markedly reduced mortality from HIV/AIDS, but the incidence of new cases, after declining in the 1990s, has gradually increased since 2000.1 As described in a previous article in the Journal of Family Practice,2 efforts to control HIV now focus on increased testing of those persons at risk, behavior modification to reduce the chances of infected persons exposing others, and treating HIV-positive pregnant women and providing postnatal prophylaxis to their newly born infants.
Exposure to HIV can occur occupationally, during a sexual assault, or from the failure of barrier protection during sex. Though these types of exposure are not major contributors to HIV incidence, and postexposure prophylaxis is not expected to play a major role in reducing the incidence of disease, it is available to persons potentially exposed to HIV, and it is beneficial to know when it is and is not indicated. Evidence for possible effectiveness of PEP comes from studies of postnatal prophylaxis, animal studies, case control studies and case reports.3
The Centers for Disease Control and Prevention (CDC) has developed 2 sets of recommendations for PEP that take into consideration the type and severity of the exposure and characteristics of the source of the exposure (TABLE 1).3,4
TABLE 1
Recommended HIV postexposure prophylaxis for percutanous injuries and membrane/nonintact skin exposures
| For percutaneous injuries | |||||
| EXPOSURE TYPE | INFECTION STATUS OF SOURCE | ||||
| HIV-POSITIVE, CLASS 1* | HIV-POSITIVE, CLASS 2* | SOURCE OF UNKNOWN HIV STATUS† | UNKNOWN SOURCE‡ | HIV-NEGATIVE | |
| Less severe (eg, solid needle or supercficial injury) | Recommend basic 2-drug PEP | Recommend expanded ≥3-drug PEP | Generally, no PEP warranted however, consider basic 2-drug PEP¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV-infected persons is likely | No PEP warranted |
| More severe (large-bore hollow needle, deep puncture wound, blood on device, needle used in artery/vein) | Recommend expanded ≥3-drug PEP | Recommend expanded ≥3-drug PEP | Generally, no PEP warranted; however, consider basic 2-drug¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV infected persons is likely | No PEP warranted |
| For mucous membrane and nonintact skin exposures†† | |||||
| Small volume (eg, a few drops) | Consider basic 2-drug PEP¶ | Recommend basic 2-drug PEP | Generally, no PEP warranted** | Generally, no PEP warranted | No PEP warranted |
| Large volume (eg, a major blood splash) | Recommend basic 2-drug PEP | Recommend expended ≥3-drug PEP | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV-infected persons is likely | No PEP warranted |
| *HIV-positive, class 1—asymptomatic HIV infection or known low viral load (eg, <1500 ribonucleic acid copies/mL). HIV-positive, class 2—symptomatic HIV infection, AIDS, acute seroconversion, or known high viral load. If drug resistance is a concern, obtain expert consultation. Initiation of PEP should not be delayed pending expert consultation, and, because expert consultation alone cannot substitute for face-to-face counseling, resources should be available to provide immediate evaluation and follow-up care for all exposures. | |||||
| †For example, deceased source person with no samples available for HIV testing. | |||||
| ‡For example, a needle from a sharps container or splash from inappropriately disposed blood. | |||||
| ¶The recommendation “consider PEP” indicates that PEP is optional; a decision to initiate PEP should be based on a discussion between the exposed person and the treating clinician regarding the risks versus benefits of PEP. | |||||
| **If PEP is offered and administered and the source is later determined to be HIV-negative, PEP should be discontinued. | |||||
| ††For skin exposures, follow-up is indicated only if evidence exists of compromised skin integrity (eg, dermatitis, abrasion, or open wound). | |||||
| Source: Centers for Disease Control and Prevention 2005.4 | |||||
Occupational exposures to HIV
Occupational exposure to HIV can result from a needlestick injury, cut with a sharp object, or contact with potentially infectious body fluids to mucous membranes or skin that is not intact (chapped, cut, abraded, inflamed). Body fluids that are considered potentially infectious are listed in TABLE 2, along with fluids not considered to be infectious.
The risk of contracting HIV from an occupational exposure is determined by several factors, but is generally low. The risk of infection after a needle-stick injury with exposure to infected blood is estimated at 0.3%; after a mucous membrane exposure, 0.09%. The risk after exposure to nonintact skin is probably even lower. Risk increases with the quantity of blood exposed to, a needle-stick injury directly into a vein or artery, and deep injuries.
TABLE 2
Which body fluids are infectious?
| BODY FLUIDS POTENTIALLY INFECTIOUS FOR HIV | |
|
|
| BODY FLUIDS NOT CONSIDERED TO BE INFECTIOUS UNLESS THEY ARE VISIBLY BLOODY | |
|
|
Who should and should not receive PEP
TABLE 1 details recommended treatment responses to specific types of exposure (eg, puncture wound) and the status of the exposure source.4 In situations unlikely to result in disease transmission (superficial injury and source patient with unknown HIV status), no PEP is generally warranted due to the low risk of infection and potential toxicity of antiretrovirals.
Treatment particulars
Start postexposure prophylaxis, when indicated, as soon as possible following exposure and continue it for 4 weeks. Obtain baseline test results for HIV at the time of exposure and periodically for 6 months. The CDC recommends testing at 6 weeks, 12 weeks, and 6 months, whether or not PEP is provided.
Testing and monitoring for hepatitis B and C may also be indicated.
Advise patients on PEP to use precautions in avoiding the possibility of secondary transmission, especially in the first 3 months following exposure. Monitor for drug toxicity every week or 2 while giving PEP. Because of the complexity of potential PEP regimens and the risk for drug toxicity, you may want to take advantage of several national sources of consultation, such as the PEPline (www.ucsf.edu/hivcntr/Hotlines/PEPline or 888-448-4911) or the HIV/AIDS Treatment Information Service (aidsinfo.nih.gov)—especially with questions about potential drug resistance or if the exposed person is pregnant.
When risk is real but low, 2-drug PEP is recommended (TABLE 1), usually 2 nucleoside reverse transcriptase inhibitors (NRTI) or 1 NRTI and 1 nucleotide reverse transcriptase inhibitor (NtRTI).
For those at higher risk, 3 or more antiviral regimens are recommended, achieved by adding a protease inhibitor to one of the recommended 2-drug regimens. The potential antiviral combinations in the basic 2-drug and expanded PEP regimens, along with potential side effects and toxicities of antiviral medications are described in TABLE W1, available online at www.jfponline.com.4
Nonoccupational exposures rarely require PEP
There are many unresolved questions regarding PEP for nonoccupational exposures. The lack of definitive evidence of its effectiveness, its unknown influence on risk-taking behavior, and the potential to aggravate viral resistance have led CDC to recommend that PEP be used only infrequently and not continuously for those whose behavior results in frequent exposures.3 Those who continue to participate in high risk activities should be referred for risk-reduction behavioral counseling.
The risk of HIV transmission varies by route and source of exposure (TABLE 3). The CDC has developed an algorithm based on these variables (FIGURE) to help you decide whether to initiate PEP. Two situations that cause concerns but pose little known risk of infection are bites and needlestick injuries from discarded needles; PEP is rarely indicated for either.
As with occupational exposure PEP, those receiving nonoccupational PEP should be evaluated at baseline for HIV infection. In addition, consider evaluating them for other STD’s and pregnancy.
As with occupational exposure, start nonoccupational PEP as soon as possible and continue it for 28 days. Nonoccupational PEP is not recommended if time after exposure is more than 72 hours. A 3-drug regimen is recommended by the CDC for nonoccupational exposures, even though evidence is lacking that it provides superior benefit over 2 drugs (see TABLE W1 at www.jfponline.com).
Follow-up recommendations for those provided nonoccupational PEP are the same as for occupational PEP, and testing for other STDs and hepatitis B and C is also recommended (TABLE 4).
FIGURE
Evaluation and treatment of possible nonoccupational HIV exposures
Source: Centers for Disease Control and Prevention 2005.3
TABLE 3
Estimated per-act risk for acquisition of HIV, by exposure route*
| EXPOSURE ROUTE | RISK PER 10,000 EXPOSURES TO AN INFECTED SOURCE |
|---|---|
| Blood transfusion | 9000 |
| Needle-sharing injection-drug use | 67 |
| Receptive anal intercourse | 50 |
| Percutaneous needle stick | 30 |
| Receptive penile-vaginal intercourse | 10 |
| Insertive anal intercourse | 6.5 |
| Insertive penile-vaginal intercourse | 5 |
| Receptive oral intercourse† | 1 |
| Insertive oral intercourse† | 0.5 |
| *Estimates of risk for transmission from sexual exposures assume no condom use. | |
| †Source refers to oral intercourse performed on a man. | |
| Source: Centers for Disease Control and Prevention 2005.3 | |
TABLE 4
Recommended laboratory evaluation for nonoccupational postexposure prophylaxis of HIV infection
| TEST | BASELINE | DURING PEP* | 4 TO 6 WEEKS AFTER EXPOSURE | 3 MONTHS AFTER EXPOSURE | 6 MONTHS AFTER EXPOSURE |
|---|---|---|---|---|---|
| HIV antibody testing | E, S† | E | E | E | |
| Complete blood count with differential | E | E | |||
| Serum liver enzymes | E | E | |||
| Blood urea nitrogen/creatinine | E | E | |||
| Sexually transmitted diseases screen (gonorrhea, chlamydia, syphilis) | E, S | E‡ | E‡ | ||
| Hepatitis B serology | E, S | E‡ | E‡ | ||
| Hepatitis C serology | E, S | E | E | ||
| Pregnancy test (for women of reproductive age) | E | E‡ | E‡ | ||
| HIV viral load | S | E§ | E§ | E§ | |
| HIV resistance testing | S | E§ | E§ | E§ | |
| CD4+T lymphocyte count | S | E§ | E§ | E§ | |
| PEP, postexposure prophylaxis; E, exposed patient; S, source. | |||||
| *Other specific tests might be indicated dependent on the antiretrovirals prescribed. Literature pertaining to individual agents should be consulted. | |||||
| †HIV antibody testing of the source patient is indicated for sources of unknown serostatus. | |||||
| ‡Additional testing for pregnancy, sexually transmitted diseases, and hepatitis B should be performed as clinically indicated. | |||||
| §If determined to be HIV infected on follow-up testing; perform as clinically indicated once diagnosed. | |||||
Conclusion
When there is uncertainty whether PEP is recommended, start patients on a PEP regimen while the situation is sorted out. Fortunately, joint patient-physician decision making can be assisted by the physician consultation resources mentioned previously. Keep in mind that, depending on the circumstances of the exposure, HIV transmission is only one concern among others, including infectious diseases, pregnancy, and emotional/psychological aspects resulting from the incident.
CORRESPONDENCE
Doug Campos-Outcalt, MD,MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
One of your office personnel receives a superficial stick from a needle while putting it into a sharps disposal container. Is postexposure prophylaxis (PEP) for HIV warranted?
Another health care worker receives a major blood splash into her eye after dropping a blood tube taken from a source of unknown HIV status. Is PEP called for in this instance?
A child who was rifling through a trash bin accidentally poked himself with an improperly disposed hypodermic needle. Should he be given PEP?
In most cases, HIV PEP is given only to healthcare workers if the settings make exposure to HIV-infected persons likely. Otherwise, it is usually deemed unnecessary. However, a decision for or against PEP is complicated.
Occupational and nonoccupational exposure to HIV can produce fear, anxiety, and stress. Information on the exposure risk is frequently incomplete, the risk of infection is usually low, the degree of protection offered by PEP is not fully defined, and the potential for side effects from the medications is significant.
This article distills the Centers for Disease Control and Prevention’s most recent guidance on HIV PEP.
HIV on the rise again
Antiretroviral therapy has markedly reduced mortality from HIV/AIDS, but the incidence of new cases, after declining in the 1990s, has gradually increased since 2000.1 As described in a previous article in the Journal of Family Practice,2 efforts to control HIV now focus on increased testing of those persons at risk, behavior modification to reduce the chances of infected persons exposing others, and treating HIV-positive pregnant women and providing postnatal prophylaxis to their newly born infants.
Exposure to HIV can occur occupationally, during a sexual assault, or from the failure of barrier protection during sex. Though these types of exposure are not major contributors to HIV incidence, and postexposure prophylaxis is not expected to play a major role in reducing the incidence of disease, it is available to persons potentially exposed to HIV, and it is beneficial to know when it is and is not indicated. Evidence for possible effectiveness of PEP comes from studies of postnatal prophylaxis, animal studies, case control studies and case reports.3
The Centers for Disease Control and Prevention (CDC) has developed 2 sets of recommendations for PEP that take into consideration the type and severity of the exposure and characteristics of the source of the exposure (TABLE 1).3,4
TABLE 1
Recommended HIV postexposure prophylaxis for percutanous injuries and membrane/nonintact skin exposures
| For percutaneous injuries | |||||
| EXPOSURE TYPE | INFECTION STATUS OF SOURCE | ||||
| HIV-POSITIVE, CLASS 1* | HIV-POSITIVE, CLASS 2* | SOURCE OF UNKNOWN HIV STATUS† | UNKNOWN SOURCE‡ | HIV-NEGATIVE | |
| Less severe (eg, solid needle or supercficial injury) | Recommend basic 2-drug PEP | Recommend expanded ≥3-drug PEP | Generally, no PEP warranted however, consider basic 2-drug PEP¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV-infected persons is likely | No PEP warranted |
| More severe (large-bore hollow needle, deep puncture wound, blood on device, needle used in artery/vein) | Recommend expanded ≥3-drug PEP | Recommend expanded ≥3-drug PEP | Generally, no PEP warranted; however, consider basic 2-drug¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV infected persons is likely | No PEP warranted |
| For mucous membrane and nonintact skin exposures†† | |||||
| Small volume (eg, a few drops) | Consider basic 2-drug PEP¶ | Recommend basic 2-drug PEP | Generally, no PEP warranted** | Generally, no PEP warranted | No PEP warranted |
| Large volume (eg, a major blood splash) | Recommend basic 2-drug PEP | Recommend expended ≥3-drug PEP | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ for source with HIV risk factors** | Generally, no PEP warranted; however, consider basic 2-drug PEP¶ in settings in which exposure to HIV-infected persons is likely | No PEP warranted |
| *HIV-positive, class 1—asymptomatic HIV infection or known low viral load (eg, <1500 ribonucleic acid copies/mL). HIV-positive, class 2—symptomatic HIV infection, AIDS, acute seroconversion, or known high viral load. If drug resistance is a concern, obtain expert consultation. Initiation of PEP should not be delayed pending expert consultation, and, because expert consultation alone cannot substitute for face-to-face counseling, resources should be available to provide immediate evaluation and follow-up care for all exposures. | |||||
| †For example, deceased source person with no samples available for HIV testing. | |||||
| ‡For example, a needle from a sharps container or splash from inappropriately disposed blood. | |||||
| ¶The recommendation “consider PEP” indicates that PEP is optional; a decision to initiate PEP should be based on a discussion between the exposed person and the treating clinician regarding the risks versus benefits of PEP. | |||||
| **If PEP is offered and administered and the source is later determined to be HIV-negative, PEP should be discontinued. | |||||
| ††For skin exposures, follow-up is indicated only if evidence exists of compromised skin integrity (eg, dermatitis, abrasion, or open wound). | |||||
| Source: Centers for Disease Control and Prevention 2005.4 | |||||
Occupational exposures to HIV
Occupational exposure to HIV can result from a needlestick injury, cut with a sharp object, or contact with potentially infectious body fluids to mucous membranes or skin that is not intact (chapped, cut, abraded, inflamed). Body fluids that are considered potentially infectious are listed in TABLE 2, along with fluids not considered to be infectious.
The risk of contracting HIV from an occupational exposure is determined by several factors, but is generally low. The risk of infection after a needle-stick injury with exposure to infected blood is estimated at 0.3%; after a mucous membrane exposure, 0.09%. The risk after exposure to nonintact skin is probably even lower. Risk increases with the quantity of blood exposed to, a needle-stick injury directly into a vein or artery, and deep injuries.
TABLE 2
Which body fluids are infectious?
| BODY FLUIDS POTENTIALLY INFECTIOUS FOR HIV | |
|
|
| BODY FLUIDS NOT CONSIDERED TO BE INFECTIOUS UNLESS THEY ARE VISIBLY BLOODY | |
|
|
Who should and should not receive PEP
TABLE 1 details recommended treatment responses to specific types of exposure (eg, puncture wound) and the status of the exposure source.4 In situations unlikely to result in disease transmission (superficial injury and source patient with unknown HIV status), no PEP is generally warranted due to the low risk of infection and potential toxicity of antiretrovirals.
Treatment particulars
Start postexposure prophylaxis, when indicated, as soon as possible following exposure and continue it for 4 weeks. Obtain baseline test results for HIV at the time of exposure and periodically for 6 months. The CDC recommends testing at 6 weeks, 12 weeks, and 6 months, whether or not PEP is provided.
Testing and monitoring for hepatitis B and C may also be indicated.
Advise patients on PEP to use precautions in avoiding the possibility of secondary transmission, especially in the first 3 months following exposure. Monitor for drug toxicity every week or 2 while giving PEP. Because of the complexity of potential PEP regimens and the risk for drug toxicity, you may want to take advantage of several national sources of consultation, such as the PEPline (www.ucsf.edu/hivcntr/Hotlines/PEPline or 888-448-4911) or the HIV/AIDS Treatment Information Service (aidsinfo.nih.gov)—especially with questions about potential drug resistance or if the exposed person is pregnant.
When risk is real but low, 2-drug PEP is recommended (TABLE 1), usually 2 nucleoside reverse transcriptase inhibitors (NRTI) or 1 NRTI and 1 nucleotide reverse transcriptase inhibitor (NtRTI).
For those at higher risk, 3 or more antiviral regimens are recommended, achieved by adding a protease inhibitor to one of the recommended 2-drug regimens. The potential antiviral combinations in the basic 2-drug and expanded PEP regimens, along with potential side effects and toxicities of antiviral medications are described in TABLE W1, available online at www.jfponline.com.4
Nonoccupational exposures rarely require PEP
There are many unresolved questions regarding PEP for nonoccupational exposures. The lack of definitive evidence of its effectiveness, its unknown influence on risk-taking behavior, and the potential to aggravate viral resistance have led CDC to recommend that PEP be used only infrequently and not continuously for those whose behavior results in frequent exposures.3 Those who continue to participate in high risk activities should be referred for risk-reduction behavioral counseling.
The risk of HIV transmission varies by route and source of exposure (TABLE 3). The CDC has developed an algorithm based on these variables (FIGURE) to help you decide whether to initiate PEP. Two situations that cause concerns but pose little known risk of infection are bites and needlestick injuries from discarded needles; PEP is rarely indicated for either.
As with occupational exposure PEP, those receiving nonoccupational PEP should be evaluated at baseline for HIV infection. In addition, consider evaluating them for other STD’s and pregnancy.
As with occupational exposure, start nonoccupational PEP as soon as possible and continue it for 28 days. Nonoccupational PEP is not recommended if time after exposure is more than 72 hours. A 3-drug regimen is recommended by the CDC for nonoccupational exposures, even though evidence is lacking that it provides superior benefit over 2 drugs (see TABLE W1 at www.jfponline.com).
Follow-up recommendations for those provided nonoccupational PEP are the same as for occupational PEP, and testing for other STDs and hepatitis B and C is also recommended (TABLE 4).
FIGURE
Evaluation and treatment of possible nonoccupational HIV exposures
Source: Centers for Disease Control and Prevention 2005.3
TABLE 3
Estimated per-act risk for acquisition of HIV, by exposure route*
| EXPOSURE ROUTE | RISK PER 10,000 EXPOSURES TO AN INFECTED SOURCE |
|---|---|
| Blood transfusion | 9000 |
| Needle-sharing injection-drug use | 67 |
| Receptive anal intercourse | 50 |
| Percutaneous needle stick | 30 |
| Receptive penile-vaginal intercourse | 10 |
| Insertive anal intercourse | 6.5 |
| Insertive penile-vaginal intercourse | 5 |
| Receptive oral intercourse† | 1 |
| Insertive oral intercourse† | 0.5 |
| *Estimates of risk for transmission from sexual exposures assume no condom use. | |
| †Source refers to oral intercourse performed on a man. | |
| Source: Centers for Disease Control and Prevention 2005.3 | |
TABLE 4
Recommended laboratory evaluation for nonoccupational postexposure prophylaxis of HIV infection
| TEST | BASELINE | DURING PEP* | 4 TO 6 WEEKS AFTER EXPOSURE | 3 MONTHS AFTER EXPOSURE | 6 MONTHS AFTER EXPOSURE |
|---|---|---|---|---|---|
| HIV antibody testing | E, S† | E | E | E | |
| Complete blood count with differential | E | E | |||
| Serum liver enzymes | E | E | |||
| Blood urea nitrogen/creatinine | E | E | |||
| Sexually transmitted diseases screen (gonorrhea, chlamydia, syphilis) | E, S | E‡ | E‡ | ||
| Hepatitis B serology | E, S | E‡ | E‡ | ||
| Hepatitis C serology | E, S | E | E | ||
| Pregnancy test (for women of reproductive age) | E | E‡ | E‡ | ||
| HIV viral load | S | E§ | E§ | E§ | |
| HIV resistance testing | S | E§ | E§ | E§ | |
| CD4+T lymphocyte count | S | E§ | E§ | E§ | |
| PEP, postexposure prophylaxis; E, exposed patient; S, source. | |||||
| *Other specific tests might be indicated dependent on the antiretrovirals prescribed. Literature pertaining to individual agents should be consulted. | |||||
| †HIV antibody testing of the source patient is indicated for sources of unknown serostatus. | |||||
| ‡Additional testing for pregnancy, sexually transmitted diseases, and hepatitis B should be performed as clinically indicated. | |||||
| §If determined to be HIV infected on follow-up testing; perform as clinically indicated once diagnosed. | |||||
Conclusion
When there is uncertainty whether PEP is recommended, start patients on a PEP regimen while the situation is sorted out. Fortunately, joint patient-physician decision making can be assisted by the physician consultation resources mentioned previously. Keep in mind that, depending on the circumstances of the exposure, HIV transmission is only one concern among others, including infectious diseases, pregnancy, and emotional/psychological aspects resulting from the incident.
CORRESPONDENCE
Doug Campos-Outcalt, MD,MPA, 4001 North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
REFERENCE
1. Centers for Disease Control and Prevention (CDC). Trends in HIV/AIDS Diagnoses—33 States, 2001-2004. MMWR Morb Mortal Wkly Rep 2005;54:1149-1153.Available at: www.cdc.gov/mmwr/preview/mmwrhtml/mm5445a1.htm. Accessed on June 8, 2006.
2. Campos-Outcalt D. HIV prevention enters a new era. J Fam Pract 2004;53:563-566.
3. CDC. Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposures to HIV in the United States. MMWR Recomm Rep 2005;54(RR-2).-Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm. Accessed on June 8, 2006.
4. CDC. Updated U.S. public health service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep 2005;54(RR-9).-Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm. Accessed on June 8, 2006.
5. US Department of Health and Human Services. Guideline for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents. October 29, 2004 revision. Available at: aidsinfo.nih.gov/guidelines.default_db2,asp?id+50. Accessed on June 8, 2006.
REFERENCE
1. Centers for Disease Control and Prevention (CDC). Trends in HIV/AIDS Diagnoses—33 States, 2001-2004. MMWR Morb Mortal Wkly Rep 2005;54:1149-1153.Available at: www.cdc.gov/mmwr/preview/mmwrhtml/mm5445a1.htm. Accessed on June 8, 2006.
2. Campos-Outcalt D. HIV prevention enters a new era. J Fam Pract 2004;53:563-566.
3. CDC. Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposures to HIV in the United States. MMWR Recomm Rep 2005;54(RR-2).-Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm. Accessed on June 8, 2006.
4. CDC. Updated U.S. public health service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep 2005;54(RR-9).-Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5409a1.htm. Accessed on June 8, 2006.
5. US Department of Health and Human Services. Guideline for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents. October 29, 2004 revision. Available at: aidsinfo.nih.gov/guidelines.default_db2,asp?id+50. Accessed on June 8, 2006.
Mumps epidemic in 2006: Are you prepared to detect and prevent it?
The ongoing mumps epidemic in the Midwestern US is a stark reminder of how fast and easily an epidemic can still occur. It serves as a warning that we need to remain vigilant in maintaining high immunization levels among our patients. The morbidity and mortality resulting from this outbreak will depend on the soundness and response of the public health infrastructure.
We family physicians need to be prepared to detect and prevent mumps among our patients and staff. While it may not be immediately apparent, if we fulfill our roles competently the outbreak will be less severe.
The start of an epidemic
As of May 15, 1765 cases of mumps had been reported to the Iowa Department of Public Health.1 The median age of those infected was 22 years, with more than one third of cases occurring in those aged 16 to 22 years (FIGURE). College students accounted for 20% of cases.
By the middle of April, at least 8 other states were also investigating possible mumps cases. More states will likely become involved: 2 people who were probably infectious traveled on 9 commercial airline flights in a 1-week period in late March.2 The number of fellow travelers infected is under investigation.
In Iowa, investigation has shown that 5% of those infected reported no history of mumps immunization, 13% reported only 1 MMR vaccine, and in 30% the vaccine status was unknown. A majority of cases (51%) had received the recommended 2 MMR vaccines.1 These numbers are consistent with what would be expected with a vaccine that has 90% to 95% effectiveness in a highly immunized population. In such conditions, most cases occur among the vaccinated even though their rate of infection is far lower than the unvaccinated.
The strain of mumps virus isolated in this outbreak is the same one responsible for a recent large outbreak in Great Britain, where there have been more than 70,000 cases in the past 3 years.3 In contrast to measles—which has resulted in few secondary cases and practically no prolonged transmission in the US after importation from abroad4 —this introduction of mumps has resulted in more cases and multiple generations. Given that mumps and measles vaccine are usally given together in MMR, the reasons for this difference are not clear and include several possibilities:
- The mumps vaccine appears to be less effective than measles vaccine. The mumps vaccine is reported to be 80% effective after the first dose and 90% after the second,3 where measles vaccine effectiveness approaches 98% after 2 doses.
- The number of persons with atypical or asymptomatic mumps presentations is significant and complicates control efforts.
- There is possibly a lower level of immunity to mumps in older age groups. The pre-vaccine epidemiology of measles and mumps were different, with virtually everyone born before 1957 having contracted measles naturally. This artificial cutoff date has also been used to set an age limit for mumps vaccine, although those born before 1957 may not be universally immune to mumps from natural infection.
- Later adoption of routine mumps immunization (1970s) vs routine measles immunization (1960s).
FIGURE
Age distribution of mumps cases in Iowa
Source: Data from the Iowa Department of Public Health website.1
The public health response: Controlling the outbreak
Mumps vaccine is not effective until 2 to 4 weeks after it is administered, so it is not useful as postexposure prophylaxis. However, it is effective in stopping population-based outbreaks after 1 or 2 generations. MMR vaccine should be given to all who cannot provide evidence of immunity, which includes laboratory evidence of prior mumps infection, birth before 1957, or history of 1 dose of mumps-containing vaccine. Health care workers and students (including college students) should receive a second dose of vaccine.
At schools with documented cases, students and staff without proof of mumps immunity should be excluded until they receive a mumps vaccine (MMR) or provide proof of immunity. Exclusion should be until 25 days after the onset of parotitis in the last person with mumps at the institution. Anyone with mumps should be isolated until 9 days after onset of symptoms.
Laboratory confirmation of mumps involves positive mumps immunoglobulin M (IgM), a 4-fold rise in mumps IgG titers between acute and 2-week convalescent serum, or detection of virus by culture or polymerase chain reaction (PCR) in urine or throat swab specimens. Laboratory results can be confusing in those previously vaccinated; mumps IgM titers may not be detectable, a 4-fold rise in IgG titers my not occur, and the acute IgG titer may be high. False-positive IgM results can occur because of infection with parainfluenza viruses.7
Transmission of the mumps virus occurs through the saliva or respiratory droplets of an infected person. The incubation period is usually 16 to 18 days but can range from 12 to 25 days. A person is infectious up to 2 days before symptoms begin and until 9 days after. Symptoms include myalgia, malaise, fever, and headache followed by tender swelling of parotid or other salivary glands (sublingual, submaxillary). Up to 50% of those infected can present atypically and 20% can be asymptomatic, which compicates disease control efforts.
Compications of mumps caninclude orchitis (in 20% of postpubertal males), oophoritis, mastitis (30% of postpubertal females), pancreatitis (4%), deafness (5/100,000), encephalitis (2/10,000), and spontaneous abortion 25% of first-trimester pregnancies.5,6
How can you help bring this outbreak under control?
Appropriate steps can be grouped into office infection control practices, diagnosis and reporting, and community infection control measures (TABLE).
Office infection control. Office infection control (subject of a Practice Alert8) is critical so that health care settings do not become a major source of disease transmission. Make sure you and your staff have immunity to mumps. Health care workers should receive 2 doses of MMR vaccine at least a month apart. If mumps occurs in your area, consider requiring proof of immunity, even for those born before 1957.
Make sure that tissues and hand sanitizers are available for patients in the waiting areas, and that signs are posted advising respiratory hygiene. Instruct your front-office staff to ask patients to cover their mouths and noses when they cough and sneeze. Make masks available to any patient who is unable or unwilling to comply; surgical masks are sufficient. Health care staff should be familiar with and use recommended hand sanitation practices.
Don’t let patients with parotid gland swelling sit in the waiting area—place them in an examination room and ask them to wear a mask.
Diagnosis and reporting. When you suspect mumps, collect any specimens requested by the local health department. This probably includes an immediate serum sample for IgM or IgG and possibly a convalescent serum for IgG; it may include a throat swab or urine sample for viral isolation. You should know the phone number of the local health department or have access to their Web site so that current recommendations for specimen collection and analysis can be obtained quickly.
Community infection control. If you suspect a patient has mumps, report it to the local health department and instruct the patient to remain in isolation for 9 days after the start of symptoms. Family members and close contacts should be assisted in assuring they are immune to mumps.
Review with each patient their immunization status; encourage those without documented immunity to mumps to receive the vaccine, if they have no contraindications.
TABLE
Family physicians’ role in controlling mumps
| OFFICE INFECTION CONTROL |
| Post respiratory hygiene notices |
| Make readily available for patients and staff tissues, tissue disposal containers, and hand sanitizers |
| Instruct office staff to request patients use respiratory hygiene |
| Have masks available for those who cannot or refuse to comply with respiratory hygiene |
| Train staff to place patients suspected to have mumps in an examine room immediately and to provide them a mask |
| Instruct staff to use recommended hand sanitation methods |
| Insure that staff are immunized |
| DIAGNOSING AND REPORTING |
| Maintain a high index of suspicion for mumps |
| Collect recommended laboratory specimens |
| COMMUNITY INFECTION CONTROL |
| Report suspected mumps cases to the local public health department |
| Advise those infected to remain in isolation until 9 days after the start of symptoms |
| Help insure families and close contacts of those infected are immunized against mumps |
| Check mumps immunization status of all patients |
1. Iowa mumps update. Available at: www.idph.state.ia.us/adper/common/pdf/mumps/mumps_update_051606.pdf. Accessed on May 16, 2006.
2. Centers for Disease Control and Prevention (CDC). Exposure to mumps during air travel—United States, April 2006. MMWR 2006;55:401-402.
3. CDC Health Advisory. Multi-state mumps outbreak. Available at: www.phppo.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00243. Accessed on May 16, 2006.
4. CDC. Measles history. Available at: www.cdc.gov/nip/diseases/measles/history.htm. Accessed on May 16, 2006.
5. Heyman DL. Control of Communicable Diseases Manual 18th ed. Washington, DC: American Public Health Association; 2004.
6. Zimmerman L, Reef S, Wharton M. Mumps. Chapter 7 in Manual for the Surveillance of Vaccine-Preventable Diseases. 3rd ed. Washington, DC: National Immunization Program; 2002. Available at: www.cdc.gov/nip/publications/surv-manual/chpt07_mumps.pdf. Accessed on May 16, 2006.
7. CDC. Laboratory testing for mumps infection. Available at: www.cdc.gov/nip/diseases/mumps/lab-test-faqs.htm. Accessed on May 16, 2006.
8. Campos-Outcalt D. Infection control in the outpatient settings. J Fam Pract 2004;53:485-488.
The ongoing mumps epidemic in the Midwestern US is a stark reminder of how fast and easily an epidemic can still occur. It serves as a warning that we need to remain vigilant in maintaining high immunization levels among our patients. The morbidity and mortality resulting from this outbreak will depend on the soundness and response of the public health infrastructure.
We family physicians need to be prepared to detect and prevent mumps among our patients and staff. While it may not be immediately apparent, if we fulfill our roles competently the outbreak will be less severe.
The start of an epidemic
As of May 15, 1765 cases of mumps had been reported to the Iowa Department of Public Health.1 The median age of those infected was 22 years, with more than one third of cases occurring in those aged 16 to 22 years (FIGURE). College students accounted for 20% of cases.
By the middle of April, at least 8 other states were also investigating possible mumps cases. More states will likely become involved: 2 people who were probably infectious traveled on 9 commercial airline flights in a 1-week period in late March.2 The number of fellow travelers infected is under investigation.
In Iowa, investigation has shown that 5% of those infected reported no history of mumps immunization, 13% reported only 1 MMR vaccine, and in 30% the vaccine status was unknown. A majority of cases (51%) had received the recommended 2 MMR vaccines.1 These numbers are consistent with what would be expected with a vaccine that has 90% to 95% effectiveness in a highly immunized population. In such conditions, most cases occur among the vaccinated even though their rate of infection is far lower than the unvaccinated.
The strain of mumps virus isolated in this outbreak is the same one responsible for a recent large outbreak in Great Britain, where there have been more than 70,000 cases in the past 3 years.3 In contrast to measles—which has resulted in few secondary cases and practically no prolonged transmission in the US after importation from abroad4 —this introduction of mumps has resulted in more cases and multiple generations. Given that mumps and measles vaccine are usally given together in MMR, the reasons for this difference are not clear and include several possibilities:
- The mumps vaccine appears to be less effective than measles vaccine. The mumps vaccine is reported to be 80% effective after the first dose and 90% after the second,3 where measles vaccine effectiveness approaches 98% after 2 doses.
- The number of persons with atypical or asymptomatic mumps presentations is significant and complicates control efforts.
- There is possibly a lower level of immunity to mumps in older age groups. The pre-vaccine epidemiology of measles and mumps were different, with virtually everyone born before 1957 having contracted measles naturally. This artificial cutoff date has also been used to set an age limit for mumps vaccine, although those born before 1957 may not be universally immune to mumps from natural infection.
- Later adoption of routine mumps immunization (1970s) vs routine measles immunization (1960s).
FIGURE
Age distribution of mumps cases in Iowa
Source: Data from the Iowa Department of Public Health website.1
The public health response: Controlling the outbreak
Mumps vaccine is not effective until 2 to 4 weeks after it is administered, so it is not useful as postexposure prophylaxis. However, it is effective in stopping population-based outbreaks after 1 or 2 generations. MMR vaccine should be given to all who cannot provide evidence of immunity, which includes laboratory evidence of prior mumps infection, birth before 1957, or history of 1 dose of mumps-containing vaccine. Health care workers and students (including college students) should receive a second dose of vaccine.
At schools with documented cases, students and staff without proof of mumps immunity should be excluded until they receive a mumps vaccine (MMR) or provide proof of immunity. Exclusion should be until 25 days after the onset of parotitis in the last person with mumps at the institution. Anyone with mumps should be isolated until 9 days after onset of symptoms.
Laboratory confirmation of mumps involves positive mumps immunoglobulin M (IgM), a 4-fold rise in mumps IgG titers between acute and 2-week convalescent serum, or detection of virus by culture or polymerase chain reaction (PCR) in urine or throat swab specimens. Laboratory results can be confusing in those previously vaccinated; mumps IgM titers may not be detectable, a 4-fold rise in IgG titers my not occur, and the acute IgG titer may be high. False-positive IgM results can occur because of infection with parainfluenza viruses.7
Transmission of the mumps virus occurs through the saliva or respiratory droplets of an infected person. The incubation period is usually 16 to 18 days but can range from 12 to 25 days. A person is infectious up to 2 days before symptoms begin and until 9 days after. Symptoms include myalgia, malaise, fever, and headache followed by tender swelling of parotid or other salivary glands (sublingual, submaxillary). Up to 50% of those infected can present atypically and 20% can be asymptomatic, which compicates disease control efforts.
Compications of mumps caninclude orchitis (in 20% of postpubertal males), oophoritis, mastitis (30% of postpubertal females), pancreatitis (4%), deafness (5/100,000), encephalitis (2/10,000), and spontaneous abortion 25% of first-trimester pregnancies.5,6
How can you help bring this outbreak under control?
Appropriate steps can be grouped into office infection control practices, diagnosis and reporting, and community infection control measures (TABLE).
Office infection control. Office infection control (subject of a Practice Alert8) is critical so that health care settings do not become a major source of disease transmission. Make sure you and your staff have immunity to mumps. Health care workers should receive 2 doses of MMR vaccine at least a month apart. If mumps occurs in your area, consider requiring proof of immunity, even for those born before 1957.
Make sure that tissues and hand sanitizers are available for patients in the waiting areas, and that signs are posted advising respiratory hygiene. Instruct your front-office staff to ask patients to cover their mouths and noses when they cough and sneeze. Make masks available to any patient who is unable or unwilling to comply; surgical masks are sufficient. Health care staff should be familiar with and use recommended hand sanitation practices.
Don’t let patients with parotid gland swelling sit in the waiting area—place them in an examination room and ask them to wear a mask.
Diagnosis and reporting. When you suspect mumps, collect any specimens requested by the local health department. This probably includes an immediate serum sample for IgM or IgG and possibly a convalescent serum for IgG; it may include a throat swab or urine sample for viral isolation. You should know the phone number of the local health department or have access to their Web site so that current recommendations for specimen collection and analysis can be obtained quickly.
Community infection control. If you suspect a patient has mumps, report it to the local health department and instruct the patient to remain in isolation for 9 days after the start of symptoms. Family members and close contacts should be assisted in assuring they are immune to mumps.
Review with each patient their immunization status; encourage those without documented immunity to mumps to receive the vaccine, if they have no contraindications.
TABLE
Family physicians’ role in controlling mumps
| OFFICE INFECTION CONTROL |
| Post respiratory hygiene notices |
| Make readily available for patients and staff tissues, tissue disposal containers, and hand sanitizers |
| Instruct office staff to request patients use respiratory hygiene |
| Have masks available for those who cannot or refuse to comply with respiratory hygiene |
| Train staff to place patients suspected to have mumps in an examine room immediately and to provide them a mask |
| Instruct staff to use recommended hand sanitation methods |
| Insure that staff are immunized |
| DIAGNOSING AND REPORTING |
| Maintain a high index of suspicion for mumps |
| Collect recommended laboratory specimens |
| COMMUNITY INFECTION CONTROL |
| Report suspected mumps cases to the local public health department |
| Advise those infected to remain in isolation until 9 days after the start of symptoms |
| Help insure families and close contacts of those infected are immunized against mumps |
| Check mumps immunization status of all patients |
The ongoing mumps epidemic in the Midwestern US is a stark reminder of how fast and easily an epidemic can still occur. It serves as a warning that we need to remain vigilant in maintaining high immunization levels among our patients. The morbidity and mortality resulting from this outbreak will depend on the soundness and response of the public health infrastructure.
We family physicians need to be prepared to detect and prevent mumps among our patients and staff. While it may not be immediately apparent, if we fulfill our roles competently the outbreak will be less severe.
The start of an epidemic
As of May 15, 1765 cases of mumps had been reported to the Iowa Department of Public Health.1 The median age of those infected was 22 years, with more than one third of cases occurring in those aged 16 to 22 years (FIGURE). College students accounted for 20% of cases.
By the middle of April, at least 8 other states were also investigating possible mumps cases. More states will likely become involved: 2 people who were probably infectious traveled on 9 commercial airline flights in a 1-week period in late March.2 The number of fellow travelers infected is under investigation.
In Iowa, investigation has shown that 5% of those infected reported no history of mumps immunization, 13% reported only 1 MMR vaccine, and in 30% the vaccine status was unknown. A majority of cases (51%) had received the recommended 2 MMR vaccines.1 These numbers are consistent with what would be expected with a vaccine that has 90% to 95% effectiveness in a highly immunized population. In such conditions, most cases occur among the vaccinated even though their rate of infection is far lower than the unvaccinated.
The strain of mumps virus isolated in this outbreak is the same one responsible for a recent large outbreak in Great Britain, where there have been more than 70,000 cases in the past 3 years.3 In contrast to measles—which has resulted in few secondary cases and practically no prolonged transmission in the US after importation from abroad4 —this introduction of mumps has resulted in more cases and multiple generations. Given that mumps and measles vaccine are usally given together in MMR, the reasons for this difference are not clear and include several possibilities:
- The mumps vaccine appears to be less effective than measles vaccine. The mumps vaccine is reported to be 80% effective after the first dose and 90% after the second,3 where measles vaccine effectiveness approaches 98% after 2 doses.
- The number of persons with atypical or asymptomatic mumps presentations is significant and complicates control efforts.
- There is possibly a lower level of immunity to mumps in older age groups. The pre-vaccine epidemiology of measles and mumps were different, with virtually everyone born before 1957 having contracted measles naturally. This artificial cutoff date has also been used to set an age limit for mumps vaccine, although those born before 1957 may not be universally immune to mumps from natural infection.
- Later adoption of routine mumps immunization (1970s) vs routine measles immunization (1960s).
FIGURE
Age distribution of mumps cases in Iowa
Source: Data from the Iowa Department of Public Health website.1
The public health response: Controlling the outbreak
Mumps vaccine is not effective until 2 to 4 weeks after it is administered, so it is not useful as postexposure prophylaxis. However, it is effective in stopping population-based outbreaks after 1 or 2 generations. MMR vaccine should be given to all who cannot provide evidence of immunity, which includes laboratory evidence of prior mumps infection, birth before 1957, or history of 1 dose of mumps-containing vaccine. Health care workers and students (including college students) should receive a second dose of vaccine.
At schools with documented cases, students and staff without proof of mumps immunity should be excluded until they receive a mumps vaccine (MMR) or provide proof of immunity. Exclusion should be until 25 days after the onset of parotitis in the last person with mumps at the institution. Anyone with mumps should be isolated until 9 days after onset of symptoms.
Laboratory confirmation of mumps involves positive mumps immunoglobulin M (IgM), a 4-fold rise in mumps IgG titers between acute and 2-week convalescent serum, or detection of virus by culture or polymerase chain reaction (PCR) in urine or throat swab specimens. Laboratory results can be confusing in those previously vaccinated; mumps IgM titers may not be detectable, a 4-fold rise in IgG titers my not occur, and the acute IgG titer may be high. False-positive IgM results can occur because of infection with parainfluenza viruses.7
Transmission of the mumps virus occurs through the saliva or respiratory droplets of an infected person. The incubation period is usually 16 to 18 days but can range from 12 to 25 days. A person is infectious up to 2 days before symptoms begin and until 9 days after. Symptoms include myalgia, malaise, fever, and headache followed by tender swelling of parotid or other salivary glands (sublingual, submaxillary). Up to 50% of those infected can present atypically and 20% can be asymptomatic, which compicates disease control efforts.
Compications of mumps caninclude orchitis (in 20% of postpubertal males), oophoritis, mastitis (30% of postpubertal females), pancreatitis (4%), deafness (5/100,000), encephalitis (2/10,000), and spontaneous abortion 25% of first-trimester pregnancies.5,6
How can you help bring this outbreak under control?
Appropriate steps can be grouped into office infection control practices, diagnosis and reporting, and community infection control measures (TABLE).
Office infection control. Office infection control (subject of a Practice Alert8) is critical so that health care settings do not become a major source of disease transmission. Make sure you and your staff have immunity to mumps. Health care workers should receive 2 doses of MMR vaccine at least a month apart. If mumps occurs in your area, consider requiring proof of immunity, even for those born before 1957.
Make sure that tissues and hand sanitizers are available for patients in the waiting areas, and that signs are posted advising respiratory hygiene. Instruct your front-office staff to ask patients to cover their mouths and noses when they cough and sneeze. Make masks available to any patient who is unable or unwilling to comply; surgical masks are sufficient. Health care staff should be familiar with and use recommended hand sanitation practices.
Don’t let patients with parotid gland swelling sit in the waiting area—place them in an examination room and ask them to wear a mask.
Diagnosis and reporting. When you suspect mumps, collect any specimens requested by the local health department. This probably includes an immediate serum sample for IgM or IgG and possibly a convalescent serum for IgG; it may include a throat swab or urine sample for viral isolation. You should know the phone number of the local health department or have access to their Web site so that current recommendations for specimen collection and analysis can be obtained quickly.
Community infection control. If you suspect a patient has mumps, report it to the local health department and instruct the patient to remain in isolation for 9 days after the start of symptoms. Family members and close contacts should be assisted in assuring they are immune to mumps.
Review with each patient their immunization status; encourage those without documented immunity to mumps to receive the vaccine, if they have no contraindications.
TABLE
Family physicians’ role in controlling mumps
| OFFICE INFECTION CONTROL |
| Post respiratory hygiene notices |
| Make readily available for patients and staff tissues, tissue disposal containers, and hand sanitizers |
| Instruct office staff to request patients use respiratory hygiene |
| Have masks available for those who cannot or refuse to comply with respiratory hygiene |
| Train staff to place patients suspected to have mumps in an examine room immediately and to provide them a mask |
| Instruct staff to use recommended hand sanitation methods |
| Insure that staff are immunized |
| DIAGNOSING AND REPORTING |
| Maintain a high index of suspicion for mumps |
| Collect recommended laboratory specimens |
| COMMUNITY INFECTION CONTROL |
| Report suspected mumps cases to the local public health department |
| Advise those infected to remain in isolation until 9 days after the start of symptoms |
| Help insure families and close contacts of those infected are immunized against mumps |
| Check mumps immunization status of all patients |
1. Iowa mumps update. Available at: www.idph.state.ia.us/adper/common/pdf/mumps/mumps_update_051606.pdf. Accessed on May 16, 2006.
2. Centers for Disease Control and Prevention (CDC). Exposure to mumps during air travel—United States, April 2006. MMWR 2006;55:401-402.
3. CDC Health Advisory. Multi-state mumps outbreak. Available at: www.phppo.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00243. Accessed on May 16, 2006.
4. CDC. Measles history. Available at: www.cdc.gov/nip/diseases/measles/history.htm. Accessed on May 16, 2006.
5. Heyman DL. Control of Communicable Diseases Manual 18th ed. Washington, DC: American Public Health Association; 2004.
6. Zimmerman L, Reef S, Wharton M. Mumps. Chapter 7 in Manual for the Surveillance of Vaccine-Preventable Diseases. 3rd ed. Washington, DC: National Immunization Program; 2002. Available at: www.cdc.gov/nip/publications/surv-manual/chpt07_mumps.pdf. Accessed on May 16, 2006.
7. CDC. Laboratory testing for mumps infection. Available at: www.cdc.gov/nip/diseases/mumps/lab-test-faqs.htm. Accessed on May 16, 2006.
8. Campos-Outcalt D. Infection control in the outpatient settings. J Fam Pract 2004;53:485-488.
1. Iowa mumps update. Available at: www.idph.state.ia.us/adper/common/pdf/mumps/mumps_update_051606.pdf. Accessed on May 16, 2006.
2. Centers for Disease Control and Prevention (CDC). Exposure to mumps during air travel—United States, April 2006. MMWR 2006;55:401-402.
3. CDC Health Advisory. Multi-state mumps outbreak. Available at: www.phppo.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00243. Accessed on May 16, 2006.
4. CDC. Measles history. Available at: www.cdc.gov/nip/diseases/measles/history.htm. Accessed on May 16, 2006.
5. Heyman DL. Control of Communicable Diseases Manual 18th ed. Washington, DC: American Public Health Association; 2004.
6. Zimmerman L, Reef S, Wharton M. Mumps. Chapter 7 in Manual for the Surveillance of Vaccine-Preventable Diseases. 3rd ed. Washington, DC: National Immunization Program; 2002. Available at: www.cdc.gov/nip/publications/surv-manual/chpt07_mumps.pdf. Accessed on May 16, 2006.
7. CDC. Laboratory testing for mumps infection. Available at: www.cdc.gov/nip/diseases/mumps/lab-test-faqs.htm. Accessed on May 16, 2006.
8. Campos-Outcalt D. Infection control in the outpatient settings. J Fam Pract 2004;53:485-488.
Clarifying the US Preventive Services Task Force’s 2005 recommendations
The United States Preventive Services Task Force (USPSTF) is the most evidence-based and authoritative organization making recommendations on preventive services in the US. During 2005, 20 recommendations were made on a total of 10 conditions. TABLE 1 lists the recommendations made in 2005. TABLE 2 describes the criteria for the recommendations coming from the task force.
Several of these recommendations deserve elaboration.
TABLE 1
USPSTF recommendations made in 2005
| A RECOMMENDATION (STRONGLY RECOMMENDS) |
|
| B RECOMMENDATION (RECOMMENDS) |
|
| C RECOMMENDATION (NO RECOMMENDATION FOR OR AGAINST) |
|
| D RECOMMENDATION (RECOMMENDS AGAINST) |
|
| I RECOMMENDATION (INSUFFICIENT EVIDENCE TO RECOMMEND FOR OR AGAINST) |
|
TABLE 2
Meaning of recommendations by the USPSTF
| A RECOMMENDATION: STRONGLY RECOMMENDS |
| The USPSTF found good evidence that the service improves important health outcomes and concludes that benefits substantially outweigh harms. |
| B RECOMMENDATION: RECOMMENDS |
| The USPSTF found at least fair evidence that the service improves important health outcomes and concludes that benefits outweigh harms. |
| C RECOMMENDATION: NO RECOMMENDATION FOR OR AGAINST |
| The USPSTF found at least fair evidence that the service can improve health outcomes but concludes that the balance of the benefits and harms is too close to justify a general recommendation. |
| D RECOMMENDATION: RECOMMENDS AGAINST |
| The USPSTF found at least fair evidence that the service is ineffective or that harms outweigh benefits. |
| I RECOMMENDATION: INSUFFICIENT EVIDENCE TO RECOMMEND FOR OR AGAINST |
| Evidence that the service is effective is lacking, of poor quality, or conflicting and the balance of benefits and harms cannot be determined. |
Sexually transmitted infections
Among the conditions studied in 2005 were gonorrhea, herpes simplex virus (HSV), and human immunodefeciency virus (HIV). The recommendations were different for each. The task force strongly recommends (A recommendation) screening all pregnant women and all high-risk adolescents and adults for HIV. No recommendation is made regarding HIV screening in adolescents and adults who are not at high risk.
The task force recommends (B recommendation) screening high-risk women for gonorrhea, including those who are pregnant.
It recommends against (D recommendation) screening for gonorrhea in men and women at low risk and believes there is insufficient evidence (I recommendation) to advocate for or against screening men at high risk and pregnant women at low risk. It recommends against screening for HSV during pregnancy and among asymptomatic adolescents and adults.
The Task Force defines high risk a little differently for gonorrhea and HIV. These definitions are listed in TABLE 3.
What the C and I recommendations do and do not mean. Keep several points in mind regarding these recommendations. When no recommendation is made for or against (C recommendation), it signifies there is evidence of some benefit but not clear enough to outweigh harms. An I recommendation means that there is not enough quality evidence to make a recommendation. These 2 recommendations are often misinterpreted as a recommendation against the service, which they are not.
Don’t confuse screening with diagnosis. Screening, by definition, means looking for a condition among asymptomatic persons. Diagnostic tests performed to clarify the cause of symptoms or to improve clinical care are not screening tests. Screening recommendations therefore do not apply in these latter instances. In addition, the task force recognizes that screening recommendations need to be interpreted in light of local epidemiology. In areas of high STD prevalence, more widespread screening might well be justified.
TABLE 3
USPSTF definitions of risk for HIV and gonorrhea
| HIV RISK |
|
| GONORRHEA RISK |
|
Abdominal aortic aneurysms
The rationale behind these recommendations was discussed in a previous Practice Alert.1 The take-home message for physicians is that any male who has ever smoked can possibly benefit from a one-time abdominal ultrasound.
Women’s health conditions
Two sets of recommendations pertain to hormone replacement therapy (HRT) and screening for breast and ovarian cancer.
When to avoid HRT. The task force recommends against using combined estrogen and progestin in postmenopausal women, and against using estrogen to prevent chronic health conditions in postmenopausal women who have had a hysterectomy.
Estrogen and progestin combinations reduce the risk for fractures and colorectal cancer but have no beneficial effect on (and may increase the risk of) coronary heart disease. Other documented harms include increased risk for breast cancer, venous thromboembolism, stroke, cholecystitis, dementia, and lower global cognitive function. Unopposed estrogen reduces the risk for fractures but increases risk for venous thromboembolism, stroke, dementia, and lower global cognitive functioning, and it has no beneficial effect on coronary heart disease.
When to investigate possible BRCA1 or BRCA2 gene mutations. For women with family histories suggestive of mutations of BRCA1 or BRCA2 genes—which place women at markedly higher lifetime risk of breast and ovarian cancer—the task force recommends referral for counseling and possible genetic testing. While the task force acknowledges the unresolved ethical, social, and legal issues, as well as the unknown benefits of chemoprevention and intensive screening, they believe the potential of prophylactic surgery to prevent breast and ovarian cancer is sufficient to make the recommendation.
Note that the recommendation is for referral for genetic counseling in which genetic testing may be considered. It is not a recommendation for testing by itself.
The following elements of a family history place a woman at risk:
- 2 first-degree relatives with breast cancer, 1 of whom received the diagnosis at age 50 years or younger
- A combination of 3 or more first- or second-degree relatives with breast cancer regardless of age at diagnosis
- A combination of both breast and ovarian cancer among first- and second-degree relatives
- A first-degree relative with bilateral breast cancer
- A combination of 2 or more first-or second-degree relatives with ovarian cancer regardless of age at diagnosis
- A first- or second-degree relative with both breast and ovarian cancer at any age
- A history of breast cancer in a male relative.
For Ashkenazi Jewish women, an increased-risk family history includes any first-degree relative (or 2 second-degree relatives on the same side of the family) with breast or ovarian cancer.
For women without a high-risk family history, the task force believes that counseling or routine testing will lead to more harms than benefits and they recommend against it.
Overweight in children and adolescents
The task force acknowledges the increasing prevalence of overweight and obesity in children and adolescents and the consequent adverse health outcomes caused by this condition. As with many unhealthy conditions or habits, however, it is not known whether screening and counseling in the primary care setting reduce child and adolescent obesity.
Remember that the task force is not recommending for or against measuring height, weight, and body-mass index in the office or talking to young patients about their weight. They are simply summarizing the state of the science, which is unclear about whether such efforts by physicians have any effect.
Resources
The complete set of current USPSTF recommendations along with clinical considerations and links to evidence reports can be found on the USPSTF web site, www.ahrq.gov/clinic/uspstfix.htm.
CORRESPONDENCE
Doug Campos-Outcalt, MD,MPA, 4001North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
REFERENCE
1. Campos-Outcalt D. US Preventive Services Task Force: The gold standard of evidence-based prevention. J Fam Pract 2005;54:517-519.
The United States Preventive Services Task Force (USPSTF) is the most evidence-based and authoritative organization making recommendations on preventive services in the US. During 2005, 20 recommendations were made on a total of 10 conditions. TABLE 1 lists the recommendations made in 2005. TABLE 2 describes the criteria for the recommendations coming from the task force.
Several of these recommendations deserve elaboration.
TABLE 1
USPSTF recommendations made in 2005
| A RECOMMENDATION (STRONGLY RECOMMENDS) |
|
| B RECOMMENDATION (RECOMMENDS) |
|
| C RECOMMENDATION (NO RECOMMENDATION FOR OR AGAINST) |
|
| D RECOMMENDATION (RECOMMENDS AGAINST) |
|
| I RECOMMENDATION (INSUFFICIENT EVIDENCE TO RECOMMEND FOR OR AGAINST) |
|
TABLE 2
Meaning of recommendations by the USPSTF
| A RECOMMENDATION: STRONGLY RECOMMENDS |
| The USPSTF found good evidence that the service improves important health outcomes and concludes that benefits substantially outweigh harms. |
| B RECOMMENDATION: RECOMMENDS |
| The USPSTF found at least fair evidence that the service improves important health outcomes and concludes that benefits outweigh harms. |
| C RECOMMENDATION: NO RECOMMENDATION FOR OR AGAINST |
| The USPSTF found at least fair evidence that the service can improve health outcomes but concludes that the balance of the benefits and harms is too close to justify a general recommendation. |
| D RECOMMENDATION: RECOMMENDS AGAINST |
| The USPSTF found at least fair evidence that the service is ineffective or that harms outweigh benefits. |
| I RECOMMENDATION: INSUFFICIENT EVIDENCE TO RECOMMEND FOR OR AGAINST |
| Evidence that the service is effective is lacking, of poor quality, or conflicting and the balance of benefits and harms cannot be determined. |
Sexually transmitted infections
Among the conditions studied in 2005 were gonorrhea, herpes simplex virus (HSV), and human immunodefeciency virus (HIV). The recommendations were different for each. The task force strongly recommends (A recommendation) screening all pregnant women and all high-risk adolescents and adults for HIV. No recommendation is made regarding HIV screening in adolescents and adults who are not at high risk.
The task force recommends (B recommendation) screening high-risk women for gonorrhea, including those who are pregnant.
It recommends against (D recommendation) screening for gonorrhea in men and women at low risk and believes there is insufficient evidence (I recommendation) to advocate for or against screening men at high risk and pregnant women at low risk. It recommends against screening for HSV during pregnancy and among asymptomatic adolescents and adults.
The Task Force defines high risk a little differently for gonorrhea and HIV. These definitions are listed in TABLE 3.
What the C and I recommendations do and do not mean. Keep several points in mind regarding these recommendations. When no recommendation is made for or against (C recommendation), it signifies there is evidence of some benefit but not clear enough to outweigh harms. An I recommendation means that there is not enough quality evidence to make a recommendation. These 2 recommendations are often misinterpreted as a recommendation against the service, which they are not.
Don’t confuse screening with diagnosis. Screening, by definition, means looking for a condition among asymptomatic persons. Diagnostic tests performed to clarify the cause of symptoms or to improve clinical care are not screening tests. Screening recommendations therefore do not apply in these latter instances. In addition, the task force recognizes that screening recommendations need to be interpreted in light of local epidemiology. In areas of high STD prevalence, more widespread screening might well be justified.
TABLE 3
USPSTF definitions of risk for HIV and gonorrhea
| HIV RISK |
|
| GONORRHEA RISK |
|
Abdominal aortic aneurysms
The rationale behind these recommendations was discussed in a previous Practice Alert.1 The take-home message for physicians is that any male who has ever smoked can possibly benefit from a one-time abdominal ultrasound.
Women’s health conditions
Two sets of recommendations pertain to hormone replacement therapy (HRT) and screening for breast and ovarian cancer.
When to avoid HRT. The task force recommends against using combined estrogen and progestin in postmenopausal women, and against using estrogen to prevent chronic health conditions in postmenopausal women who have had a hysterectomy.
Estrogen and progestin combinations reduce the risk for fractures and colorectal cancer but have no beneficial effect on (and may increase the risk of) coronary heart disease. Other documented harms include increased risk for breast cancer, venous thromboembolism, stroke, cholecystitis, dementia, and lower global cognitive function. Unopposed estrogen reduces the risk for fractures but increases risk for venous thromboembolism, stroke, dementia, and lower global cognitive functioning, and it has no beneficial effect on coronary heart disease.
When to investigate possible BRCA1 or BRCA2 gene mutations. For women with family histories suggestive of mutations of BRCA1 or BRCA2 genes—which place women at markedly higher lifetime risk of breast and ovarian cancer—the task force recommends referral for counseling and possible genetic testing. While the task force acknowledges the unresolved ethical, social, and legal issues, as well as the unknown benefits of chemoprevention and intensive screening, they believe the potential of prophylactic surgery to prevent breast and ovarian cancer is sufficient to make the recommendation.
Note that the recommendation is for referral for genetic counseling in which genetic testing may be considered. It is not a recommendation for testing by itself.
The following elements of a family history place a woman at risk:
- 2 first-degree relatives with breast cancer, 1 of whom received the diagnosis at age 50 years or younger
- A combination of 3 or more first- or second-degree relatives with breast cancer regardless of age at diagnosis
- A combination of both breast and ovarian cancer among first- and second-degree relatives
- A first-degree relative with bilateral breast cancer
- A combination of 2 or more first-or second-degree relatives with ovarian cancer regardless of age at diagnosis
- A first- or second-degree relative with both breast and ovarian cancer at any age
- A history of breast cancer in a male relative.
For Ashkenazi Jewish women, an increased-risk family history includes any first-degree relative (or 2 second-degree relatives on the same side of the family) with breast or ovarian cancer.
For women without a high-risk family history, the task force believes that counseling or routine testing will lead to more harms than benefits and they recommend against it.
Overweight in children and adolescents
The task force acknowledges the increasing prevalence of overweight and obesity in children and adolescents and the consequent adverse health outcomes caused by this condition. As with many unhealthy conditions or habits, however, it is not known whether screening and counseling in the primary care setting reduce child and adolescent obesity.
Remember that the task force is not recommending for or against measuring height, weight, and body-mass index in the office or talking to young patients about their weight. They are simply summarizing the state of the science, which is unclear about whether such efforts by physicians have any effect.
Resources
The complete set of current USPSTF recommendations along with clinical considerations and links to evidence reports can be found on the USPSTF web site, www.ahrq.gov/clinic/uspstfix.htm.
CORRESPONDENCE
Doug Campos-Outcalt, MD,MPA, 4001North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
The United States Preventive Services Task Force (USPSTF) is the most evidence-based and authoritative organization making recommendations on preventive services in the US. During 2005, 20 recommendations were made on a total of 10 conditions. TABLE 1 lists the recommendations made in 2005. TABLE 2 describes the criteria for the recommendations coming from the task force.
Several of these recommendations deserve elaboration.
TABLE 1
USPSTF recommendations made in 2005
| A RECOMMENDATION (STRONGLY RECOMMENDS) |
|
| B RECOMMENDATION (RECOMMENDS) |
|
| C RECOMMENDATION (NO RECOMMENDATION FOR OR AGAINST) |
|
| D RECOMMENDATION (RECOMMENDS AGAINST) |
|
| I RECOMMENDATION (INSUFFICIENT EVIDENCE TO RECOMMEND FOR OR AGAINST) |
|
TABLE 2
Meaning of recommendations by the USPSTF
| A RECOMMENDATION: STRONGLY RECOMMENDS |
| The USPSTF found good evidence that the service improves important health outcomes and concludes that benefits substantially outweigh harms. |
| B RECOMMENDATION: RECOMMENDS |
| The USPSTF found at least fair evidence that the service improves important health outcomes and concludes that benefits outweigh harms. |
| C RECOMMENDATION: NO RECOMMENDATION FOR OR AGAINST |
| The USPSTF found at least fair evidence that the service can improve health outcomes but concludes that the balance of the benefits and harms is too close to justify a general recommendation. |
| D RECOMMENDATION: RECOMMENDS AGAINST |
| The USPSTF found at least fair evidence that the service is ineffective or that harms outweigh benefits. |
| I RECOMMENDATION: INSUFFICIENT EVIDENCE TO RECOMMEND FOR OR AGAINST |
| Evidence that the service is effective is lacking, of poor quality, or conflicting and the balance of benefits and harms cannot be determined. |
Sexually transmitted infections
Among the conditions studied in 2005 were gonorrhea, herpes simplex virus (HSV), and human immunodefeciency virus (HIV). The recommendations were different for each. The task force strongly recommends (A recommendation) screening all pregnant women and all high-risk adolescents and adults for HIV. No recommendation is made regarding HIV screening in adolescents and adults who are not at high risk.
The task force recommends (B recommendation) screening high-risk women for gonorrhea, including those who are pregnant.
It recommends against (D recommendation) screening for gonorrhea in men and women at low risk and believes there is insufficient evidence (I recommendation) to advocate for or against screening men at high risk and pregnant women at low risk. It recommends against screening for HSV during pregnancy and among asymptomatic adolescents and adults.
The Task Force defines high risk a little differently for gonorrhea and HIV. These definitions are listed in TABLE 3.
What the C and I recommendations do and do not mean. Keep several points in mind regarding these recommendations. When no recommendation is made for or against (C recommendation), it signifies there is evidence of some benefit but not clear enough to outweigh harms. An I recommendation means that there is not enough quality evidence to make a recommendation. These 2 recommendations are often misinterpreted as a recommendation against the service, which they are not.
Don’t confuse screening with diagnosis. Screening, by definition, means looking for a condition among asymptomatic persons. Diagnostic tests performed to clarify the cause of symptoms or to improve clinical care are not screening tests. Screening recommendations therefore do not apply in these latter instances. In addition, the task force recognizes that screening recommendations need to be interpreted in light of local epidemiology. In areas of high STD prevalence, more widespread screening might well be justified.
TABLE 3
USPSTF definitions of risk for HIV and gonorrhea
| HIV RISK |
|
| GONORRHEA RISK |
|
Abdominal aortic aneurysms
The rationale behind these recommendations was discussed in a previous Practice Alert.1 The take-home message for physicians is that any male who has ever smoked can possibly benefit from a one-time abdominal ultrasound.
Women’s health conditions
Two sets of recommendations pertain to hormone replacement therapy (HRT) and screening for breast and ovarian cancer.
When to avoid HRT. The task force recommends against using combined estrogen and progestin in postmenopausal women, and against using estrogen to prevent chronic health conditions in postmenopausal women who have had a hysterectomy.
Estrogen and progestin combinations reduce the risk for fractures and colorectal cancer but have no beneficial effect on (and may increase the risk of) coronary heart disease. Other documented harms include increased risk for breast cancer, venous thromboembolism, stroke, cholecystitis, dementia, and lower global cognitive function. Unopposed estrogen reduces the risk for fractures but increases risk for venous thromboembolism, stroke, dementia, and lower global cognitive functioning, and it has no beneficial effect on coronary heart disease.
When to investigate possible BRCA1 or BRCA2 gene mutations. For women with family histories suggestive of mutations of BRCA1 or BRCA2 genes—which place women at markedly higher lifetime risk of breast and ovarian cancer—the task force recommends referral for counseling and possible genetic testing. While the task force acknowledges the unresolved ethical, social, and legal issues, as well as the unknown benefits of chemoprevention and intensive screening, they believe the potential of prophylactic surgery to prevent breast and ovarian cancer is sufficient to make the recommendation.
Note that the recommendation is for referral for genetic counseling in which genetic testing may be considered. It is not a recommendation for testing by itself.
The following elements of a family history place a woman at risk:
- 2 first-degree relatives with breast cancer, 1 of whom received the diagnosis at age 50 years or younger
- A combination of 3 or more first- or second-degree relatives with breast cancer regardless of age at diagnosis
- A combination of both breast and ovarian cancer among first- and second-degree relatives
- A first-degree relative with bilateral breast cancer
- A combination of 2 or more first-or second-degree relatives with ovarian cancer regardless of age at diagnosis
- A first- or second-degree relative with both breast and ovarian cancer at any age
- A history of breast cancer in a male relative.
For Ashkenazi Jewish women, an increased-risk family history includes any first-degree relative (or 2 second-degree relatives on the same side of the family) with breast or ovarian cancer.
For women without a high-risk family history, the task force believes that counseling or routine testing will lead to more harms than benefits and they recommend against it.
Overweight in children and adolescents
The task force acknowledges the increasing prevalence of overweight and obesity in children and adolescents and the consequent adverse health outcomes caused by this condition. As with many unhealthy conditions or habits, however, it is not known whether screening and counseling in the primary care setting reduce child and adolescent obesity.
Remember that the task force is not recommending for or against measuring height, weight, and body-mass index in the office or talking to young patients about their weight. They are simply summarizing the state of the science, which is unclear about whether such efforts by physicians have any effect.
Resources
The complete set of current USPSTF recommendations along with clinical considerations and links to evidence reports can be found on the USPSTF web site, www.ahrq.gov/clinic/uspstfix.htm.
CORRESPONDENCE
Doug Campos-Outcalt, MD,MPA, 4001North Third Street #415, Phoenix, AZ 85012. E-mail: [email protected]
REFERENCE
1. Campos-Outcalt D. US Preventive Services Task Force: The gold standard of evidence-based prevention. J Fam Pract 2005;54:517-519.
REFERENCE
1. Campos-Outcalt D. US Preventive Services Task Force: The gold standard of evidence-based prevention. J Fam Pract 2005;54:517-519.
Trouble at the FDA: Can we fix the problems affecting you and your patients?
While often held in high esteem, the FDA has seen its reputation tarnished in recent years by adverse drug regulation experiences, apparent conflicts of interest, and problems with consistent agency leadership.
Examples of problems at the FDA
- The COX-2 inhibitor disaster that led to the withdrawal of rofecoxib (Vioxx) from the market due its association with adverse cardiovascular effects; a problem the company may have hidden from physicians and the public through manipulation of research reports.2
- The recent addition of black box warnings on selective serotonin reuptake inhibitor (SSRI) labels to warn of a potential association with suicidal behavior in adolescents after publicity that some FDA scientists were prevented from presenting this information to review panels.
- A plea bargain agreement in which Pfizer agreed to pay $430 million to resolve charges that Warner-Lambert, a company it took over, paid doctors to prescribe gabapentin (Neurontin) for off-label uses including bipolar disorder, attention deficit/hyperactivity disorder, and alcohol withdrawal seizures. Although physicians can prescribe drugs for whatever reason they choose, pharmaceutical companies are prohibited from promoting drugs for unapproved uses.3
- A lack of strong leadership with acting commissioners leading the agency 3 of the past 5 years. The last permanent commissioner resigned in September 2005 after 2 months in the position amidst accusations that he or his family had financial interests in some of the companies regulated by the agency.4
Given these and other negative events in conjunction with the dramatic increase in prescription drug use by Americans—up 60% in the past decade to 3.1 billion prescriptions in 2004 with reports of 375,000 adverse events—it’s not surprising that a recent survey showed the public wants a stronger FDA. In fact, two thirds support the creation of an independent oversight panel, 70% want the FDA to improve its gathering and reporting on possible harms of drugs and medical devices after their approval, and many believe that industry has too much influence over agency decisions.5
How the FDA performs its job matters very much to physicians, the public, and business. In recent months, outside experts and the FDA itself have proposed changes in how the agency handles new drug approvals that will affect all its stakeholders. Before reviewing those proposals, it’s worth understanding how the approval process works.
The Food and Drug Administration (FDA) is responsible for protecting the public health by assuring the safety and efficacy of human and veterinary drugs, biological products, medical devices, our nation’s food supply, cosmetics, and products that emit radiation—a list that accounts for at least 20% of consumer spending. It does this on a budget of about $1.7 billion and 10,000 employees. In comparison, the Department of Agriculture has a budget 50 times larger and a workforce 10 times larger.1
Speeding approval of new drugs
In the early 1990s, Congress responded to complaints about the FDA’s slow drug approval process, particularly regarding HIV drugs, by passing the Prescription Drug User Fee Act (PDUFA). The law mandated that pharmaceutical companies pay fees to the FDA that were then used by the agency to speed up the approval process by hiring more staff and adhering to a strict timetable for review. The PDUFA accomplished its goal; for instance, priority review drugs had their time to approval drop from a median of 14.9 months in 1993 to 6.7 months in 2003, and standard review drugs went from 27.2 months to 23.1 months during the same period.6 Ironically, in spite of the quicker approval process, in 2005, pharmaceutical companies had a record low number of FDA drug approvals—only 20 as opposed to 36 in 2004.7
As quality improvement experts say, however, you often get exactly the results your system was built for. Thus, it is not surprising that in recent years some FDA scientists have complained of increasing time pressures to perform reviews, increased pressure to approve drugs, and inability to communicate directly with the companies about the drugs they were reviewing so as to clarify study designs and data analyses.8
In addition, many observers believe that having the industry support the FDA budget (about $300 million/year) presents a potential conflict of interest for the agency, particularly in the current pro-business climate of the Bush administration.
Given these reports as well as the adverse drug safety events that have occurred recently, Congress and independent scientists are now calling for more attention to safety and less focus on the approval timetable.
How the drug approval process works
Companies obtain FDA approval for human trials after promising results from animal trials. Human trials begin with phase 1 trials, which are small studies looking at safety issues in healthy volunteers. Phase 2 studies are trials of safety and efficacy (how well the drug works) in patients with the target condition. If these prove successful, phase 3 studies are undertaken, which include at least 2 large randomized control trials of safety and efficacy. After these studies, which may involve 2000 to 5000 patients at most, the FDA can grant approval for the drug to be sold to the public.
The agency may require a company to conduct additional post-marketing studies as a condition of drug approval. These so-called phase 4 studies are often designed to identify uncommon adverse events or further investigate a drug’s effectiveness. Unfortunately, completion of many of these studies is either significantly delayed or never happens. For instance, as of September 2005, the FDA reported that 65% of the 1231 “post-marketing” studies that companies had pledged to carry out were still pending and that many of these had not even been started.9
After the drug is released, the agency may collect post-marketing data on adverse events and ask the companies to participate in this effort. But no further studies can be required of the company.
Major complaints about phase 3 studies are 1) they are relatively small and often study patients who differ in terms of demographics and extent of disease from those who end up using the medicine; 2) they are placebo-controlled trials rather than comparison trials between the new drug and the current standard therapy; and 3) the FDA increasingly uses surrogate endpoints to judge efficacy, such as tumor shrinkage for cancer drugs or LDL cholesterol decrease for lipid therapy, instead of definitive outcomes like morbidity and mortality. To the extent these surrogate endpoints strongly correlate with major outcomes, this can appropriately speed up the approval process, but the value of surrogate markers is not always clear. These characteristics of phase 3 studies often lead to approval of many “me-too” drugs without the information necessary to decide whether they are better than current standard therapy.
Deficiencies in using surrogate markers
A particular problem with surrogate markers occurs with the review of higher-priority drugs. For these, the FDA may grant provisional approval on the basis of a surrogate measure of clinical benefit shown in a single, uncontrolled trial as long as the treatment addresses an unmet need for a serious medical illness. In return, the FDA requires the company to complete confirmatory trials in the post-approval period, and may withdraw approval of the drug if no benefit is shown in these phase 4 trials.
However, between 1996 and 2003, only 6 of 23 cancer drugs have gone through such post-marketing trials, and the FDA has not withdrawn approval for any of the 23 drugs. Furthermore, many of these drugs cost thousands of dollars per treatment and have low response rates, yet the FDA has not required companies to better define the target populations for their use.10
The problem with using surrogate endpoints in short trials has been demonstrated in cardiovascular medicine with the experience using antiarrhythmics to prevent premature ventricular contractions (later discovered to lead to increased mortality), inotropics to improve ejection fraction (no long-term benefit) and, most recently, with nesiritide (Natrecor) for heart failure. The latter drug was approved based on improved pulmonarycapillary wedge pressure and self-reported improvement in dyspnea. Subsequent research and analyses have shown increased rates of renal failure and death but only after hundreds of millions of dollars worth of treatments.11
Recommendations to make the system work
Given the controversy surrounding the release and marketing of medications that later have shown to cause problems, and given the array of real and perceived conflicts of interest in the approval process, the FDA has proposed establishing a Drug Safety Oversight Board that will include outside experts to review safety issues arising with new applications. Others have argued that such a board should be completely independent of the FDA so as to minimize conflicts of interest and potential agency interference with obtaining necessary information from the companies.
The FDA also recently announced a new rule to overhaul prescription drug labeling, information in package inserts, and some drug reference books. The labels are full of information but much of it is inconsequential or difficult to use for prescribing, and most physicians don’t read them. The new labels will list safety warnings, advise how to use the drug and dose it, and advise physicians on what patients should be told about the medication. The goal is to give physicians more useful information to make decisions about drug indications and dosing. While the new rule will not change the patient drug information sheets that pharmacists hand out, it may force consumer advertising to make clearer statements about medication risks. Finally, the rule will preempt state liability statutes, which upsets some trial lawyers and politicians.12
Outside experts have proposed additional ideas to improve the FDA’s work: eliminating the current drug company fees that support new drug reviews to minimize conflicts of interest, mandating post-approval studies to look for uncommon adverse events (phase 4 studies), providing more information on relative efficacy of new drugs compared with current medication treatment and attention to real clinical outcome end points, and prohibiting direct-to-consumer advertising in the first 3 years after a new drug is released.13
Considering the turmoil surrounding the FDA’s performance right now, it is very possible we will see some of these proposed changes come to pass. Given the importance of prescription medications, these changes will be very relevant to the practices of family physicians and their patients’ health.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
1. Slater E. Today’s FDA. N Engl J Med 2005;352:293-297.
2. Curfman GD, Morrissey S, Drazen JM. Expression of concern: Bombardier et al., “Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis,” N Engl J Med 2000; 343:1520-8. Editorial. N Engl J Med 2005;353:2813-2814.
3. Harris G. Pfizer to pay $420 million in illegal marketing case. New York Times, May 14, 2004.
4. Markel H. Why America needs a strong FDA. JAMA 2005;294:2489-2491.
5. Kaiser Daily Health Policy Report. March 3, 2005. Available at: www.kaisernetwork.org/daily_reports/rep_index.cfm?hint=3&DR_ID=28455. Accessed on March 10, 2006.
6. Okie S. What ails the FDA. N Engl J Med 2005;352:1063-1066.
7. Berenson A. Drugs in ’05: Much promise, little payoff; just 20 new products are approved despite biotechnology’s hope. New York Times, Jan 11, 2006.
8. FDA’s review process for new drug applications. Office of Inspector General. March 2003. Available at: www.oig.hhs.gov/oei/reports/oei-01-01-00590.pdf. Accessed on March 10, 2006.
9. 65% of promised drug studies pending. Washington Post, March 4, 2006 (AP report)
10. Roberts T, Chabner B. Beyond fast track for drug approvals. N Engl J Med 2004;351:501-505.
11. Topol E. Nesiritide—not verified. N Engl J Med 2005;353:113-116.
12. Harris G. New drug label rule is intended to reduce medical errors. New York Times, January 19, 2006.
13. Ray W, Stein CM. Reform of drug regulation—beyond an independent drug-safety board. N Engl J Med 2006;354:194-201.
While often held in high esteem, the FDA has seen its reputation tarnished in recent years by adverse drug regulation experiences, apparent conflicts of interest, and problems with consistent agency leadership.
Examples of problems at the FDA
- The COX-2 inhibitor disaster that led to the withdrawal of rofecoxib (Vioxx) from the market due its association with adverse cardiovascular effects; a problem the company may have hidden from physicians and the public through manipulation of research reports.2
- The recent addition of black box warnings on selective serotonin reuptake inhibitor (SSRI) labels to warn of a potential association with suicidal behavior in adolescents after publicity that some FDA scientists were prevented from presenting this information to review panels.
- A plea bargain agreement in which Pfizer agreed to pay $430 million to resolve charges that Warner-Lambert, a company it took over, paid doctors to prescribe gabapentin (Neurontin) for off-label uses including bipolar disorder, attention deficit/hyperactivity disorder, and alcohol withdrawal seizures. Although physicians can prescribe drugs for whatever reason they choose, pharmaceutical companies are prohibited from promoting drugs for unapproved uses.3
- A lack of strong leadership with acting commissioners leading the agency 3 of the past 5 years. The last permanent commissioner resigned in September 2005 after 2 months in the position amidst accusations that he or his family had financial interests in some of the companies regulated by the agency.4
Given these and other negative events in conjunction with the dramatic increase in prescription drug use by Americans—up 60% in the past decade to 3.1 billion prescriptions in 2004 with reports of 375,000 adverse events—it’s not surprising that a recent survey showed the public wants a stronger FDA. In fact, two thirds support the creation of an independent oversight panel, 70% want the FDA to improve its gathering and reporting on possible harms of drugs and medical devices after their approval, and many believe that industry has too much influence over agency decisions.5
How the FDA performs its job matters very much to physicians, the public, and business. In recent months, outside experts and the FDA itself have proposed changes in how the agency handles new drug approvals that will affect all its stakeholders. Before reviewing those proposals, it’s worth understanding how the approval process works.
The Food and Drug Administration (FDA) is responsible for protecting the public health by assuring the safety and efficacy of human and veterinary drugs, biological products, medical devices, our nation’s food supply, cosmetics, and products that emit radiation—a list that accounts for at least 20% of consumer spending. It does this on a budget of about $1.7 billion and 10,000 employees. In comparison, the Department of Agriculture has a budget 50 times larger and a workforce 10 times larger.1
Speeding approval of new drugs
In the early 1990s, Congress responded to complaints about the FDA’s slow drug approval process, particularly regarding HIV drugs, by passing the Prescription Drug User Fee Act (PDUFA). The law mandated that pharmaceutical companies pay fees to the FDA that were then used by the agency to speed up the approval process by hiring more staff and adhering to a strict timetable for review. The PDUFA accomplished its goal; for instance, priority review drugs had their time to approval drop from a median of 14.9 months in 1993 to 6.7 months in 2003, and standard review drugs went from 27.2 months to 23.1 months during the same period.6 Ironically, in spite of the quicker approval process, in 2005, pharmaceutical companies had a record low number of FDA drug approvals—only 20 as opposed to 36 in 2004.7
As quality improvement experts say, however, you often get exactly the results your system was built for. Thus, it is not surprising that in recent years some FDA scientists have complained of increasing time pressures to perform reviews, increased pressure to approve drugs, and inability to communicate directly with the companies about the drugs they were reviewing so as to clarify study designs and data analyses.8
In addition, many observers believe that having the industry support the FDA budget (about $300 million/year) presents a potential conflict of interest for the agency, particularly in the current pro-business climate of the Bush administration.
Given these reports as well as the adverse drug safety events that have occurred recently, Congress and independent scientists are now calling for more attention to safety and less focus on the approval timetable.
How the drug approval process works
Companies obtain FDA approval for human trials after promising results from animal trials. Human trials begin with phase 1 trials, which are small studies looking at safety issues in healthy volunteers. Phase 2 studies are trials of safety and efficacy (how well the drug works) in patients with the target condition. If these prove successful, phase 3 studies are undertaken, which include at least 2 large randomized control trials of safety and efficacy. After these studies, which may involve 2000 to 5000 patients at most, the FDA can grant approval for the drug to be sold to the public.
The agency may require a company to conduct additional post-marketing studies as a condition of drug approval. These so-called phase 4 studies are often designed to identify uncommon adverse events or further investigate a drug’s effectiveness. Unfortunately, completion of many of these studies is either significantly delayed or never happens. For instance, as of September 2005, the FDA reported that 65% of the 1231 “post-marketing” studies that companies had pledged to carry out were still pending and that many of these had not even been started.9
After the drug is released, the agency may collect post-marketing data on adverse events and ask the companies to participate in this effort. But no further studies can be required of the company.
Major complaints about phase 3 studies are 1) they are relatively small and often study patients who differ in terms of demographics and extent of disease from those who end up using the medicine; 2) they are placebo-controlled trials rather than comparison trials between the new drug and the current standard therapy; and 3) the FDA increasingly uses surrogate endpoints to judge efficacy, such as tumor shrinkage for cancer drugs or LDL cholesterol decrease for lipid therapy, instead of definitive outcomes like morbidity and mortality. To the extent these surrogate endpoints strongly correlate with major outcomes, this can appropriately speed up the approval process, but the value of surrogate markers is not always clear. These characteristics of phase 3 studies often lead to approval of many “me-too” drugs without the information necessary to decide whether they are better than current standard therapy.
Deficiencies in using surrogate markers
A particular problem with surrogate markers occurs with the review of higher-priority drugs. For these, the FDA may grant provisional approval on the basis of a surrogate measure of clinical benefit shown in a single, uncontrolled trial as long as the treatment addresses an unmet need for a serious medical illness. In return, the FDA requires the company to complete confirmatory trials in the post-approval period, and may withdraw approval of the drug if no benefit is shown in these phase 4 trials.
However, between 1996 and 2003, only 6 of 23 cancer drugs have gone through such post-marketing trials, and the FDA has not withdrawn approval for any of the 23 drugs. Furthermore, many of these drugs cost thousands of dollars per treatment and have low response rates, yet the FDA has not required companies to better define the target populations for their use.10
The problem with using surrogate endpoints in short trials has been demonstrated in cardiovascular medicine with the experience using antiarrhythmics to prevent premature ventricular contractions (later discovered to lead to increased mortality), inotropics to improve ejection fraction (no long-term benefit) and, most recently, with nesiritide (Natrecor) for heart failure. The latter drug was approved based on improved pulmonarycapillary wedge pressure and self-reported improvement in dyspnea. Subsequent research and analyses have shown increased rates of renal failure and death but only after hundreds of millions of dollars worth of treatments.11
Recommendations to make the system work
Given the controversy surrounding the release and marketing of medications that later have shown to cause problems, and given the array of real and perceived conflicts of interest in the approval process, the FDA has proposed establishing a Drug Safety Oversight Board that will include outside experts to review safety issues arising with new applications. Others have argued that such a board should be completely independent of the FDA so as to minimize conflicts of interest and potential agency interference with obtaining necessary information from the companies.
The FDA also recently announced a new rule to overhaul prescription drug labeling, information in package inserts, and some drug reference books. The labels are full of information but much of it is inconsequential or difficult to use for prescribing, and most physicians don’t read them. The new labels will list safety warnings, advise how to use the drug and dose it, and advise physicians on what patients should be told about the medication. The goal is to give physicians more useful information to make decisions about drug indications and dosing. While the new rule will not change the patient drug information sheets that pharmacists hand out, it may force consumer advertising to make clearer statements about medication risks. Finally, the rule will preempt state liability statutes, which upsets some trial lawyers and politicians.12
Outside experts have proposed additional ideas to improve the FDA’s work: eliminating the current drug company fees that support new drug reviews to minimize conflicts of interest, mandating post-approval studies to look for uncommon adverse events (phase 4 studies), providing more information on relative efficacy of new drugs compared with current medication treatment and attention to real clinical outcome end points, and prohibiting direct-to-consumer advertising in the first 3 years after a new drug is released.13
Considering the turmoil surrounding the FDA’s performance right now, it is very possible we will see some of these proposed changes come to pass. Given the importance of prescription medications, these changes will be very relevant to the practices of family physicians and their patients’ health.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
While often held in high esteem, the FDA has seen its reputation tarnished in recent years by adverse drug regulation experiences, apparent conflicts of interest, and problems with consistent agency leadership.
Examples of problems at the FDA
- The COX-2 inhibitor disaster that led to the withdrawal of rofecoxib (Vioxx) from the market due its association with adverse cardiovascular effects; a problem the company may have hidden from physicians and the public through manipulation of research reports.2
- The recent addition of black box warnings on selective serotonin reuptake inhibitor (SSRI) labels to warn of a potential association with suicidal behavior in adolescents after publicity that some FDA scientists were prevented from presenting this information to review panels.
- A plea bargain agreement in which Pfizer agreed to pay $430 million to resolve charges that Warner-Lambert, a company it took over, paid doctors to prescribe gabapentin (Neurontin) for off-label uses including bipolar disorder, attention deficit/hyperactivity disorder, and alcohol withdrawal seizures. Although physicians can prescribe drugs for whatever reason they choose, pharmaceutical companies are prohibited from promoting drugs for unapproved uses.3
- A lack of strong leadership with acting commissioners leading the agency 3 of the past 5 years. The last permanent commissioner resigned in September 2005 after 2 months in the position amidst accusations that he or his family had financial interests in some of the companies regulated by the agency.4
Given these and other negative events in conjunction with the dramatic increase in prescription drug use by Americans—up 60% in the past decade to 3.1 billion prescriptions in 2004 with reports of 375,000 adverse events—it’s not surprising that a recent survey showed the public wants a stronger FDA. In fact, two thirds support the creation of an independent oversight panel, 70% want the FDA to improve its gathering and reporting on possible harms of drugs and medical devices after their approval, and many believe that industry has too much influence over agency decisions.5
How the FDA performs its job matters very much to physicians, the public, and business. In recent months, outside experts and the FDA itself have proposed changes in how the agency handles new drug approvals that will affect all its stakeholders. Before reviewing those proposals, it’s worth understanding how the approval process works.
The Food and Drug Administration (FDA) is responsible for protecting the public health by assuring the safety and efficacy of human and veterinary drugs, biological products, medical devices, our nation’s food supply, cosmetics, and products that emit radiation—a list that accounts for at least 20% of consumer spending. It does this on a budget of about $1.7 billion and 10,000 employees. In comparison, the Department of Agriculture has a budget 50 times larger and a workforce 10 times larger.1
Speeding approval of new drugs
In the early 1990s, Congress responded to complaints about the FDA’s slow drug approval process, particularly regarding HIV drugs, by passing the Prescription Drug User Fee Act (PDUFA). The law mandated that pharmaceutical companies pay fees to the FDA that were then used by the agency to speed up the approval process by hiring more staff and adhering to a strict timetable for review. The PDUFA accomplished its goal; for instance, priority review drugs had their time to approval drop from a median of 14.9 months in 1993 to 6.7 months in 2003, and standard review drugs went from 27.2 months to 23.1 months during the same period.6 Ironically, in spite of the quicker approval process, in 2005, pharmaceutical companies had a record low number of FDA drug approvals—only 20 as opposed to 36 in 2004.7
As quality improvement experts say, however, you often get exactly the results your system was built for. Thus, it is not surprising that in recent years some FDA scientists have complained of increasing time pressures to perform reviews, increased pressure to approve drugs, and inability to communicate directly with the companies about the drugs they were reviewing so as to clarify study designs and data analyses.8
In addition, many observers believe that having the industry support the FDA budget (about $300 million/year) presents a potential conflict of interest for the agency, particularly in the current pro-business climate of the Bush administration.
Given these reports as well as the adverse drug safety events that have occurred recently, Congress and independent scientists are now calling for more attention to safety and less focus on the approval timetable.
How the drug approval process works
Companies obtain FDA approval for human trials after promising results from animal trials. Human trials begin with phase 1 trials, which are small studies looking at safety issues in healthy volunteers. Phase 2 studies are trials of safety and efficacy (how well the drug works) in patients with the target condition. If these prove successful, phase 3 studies are undertaken, which include at least 2 large randomized control trials of safety and efficacy. After these studies, which may involve 2000 to 5000 patients at most, the FDA can grant approval for the drug to be sold to the public.
The agency may require a company to conduct additional post-marketing studies as a condition of drug approval. These so-called phase 4 studies are often designed to identify uncommon adverse events or further investigate a drug’s effectiveness. Unfortunately, completion of many of these studies is either significantly delayed or never happens. For instance, as of September 2005, the FDA reported that 65% of the 1231 “post-marketing” studies that companies had pledged to carry out were still pending and that many of these had not even been started.9
After the drug is released, the agency may collect post-marketing data on adverse events and ask the companies to participate in this effort. But no further studies can be required of the company.
Major complaints about phase 3 studies are 1) they are relatively small and often study patients who differ in terms of demographics and extent of disease from those who end up using the medicine; 2) they are placebo-controlled trials rather than comparison trials between the new drug and the current standard therapy; and 3) the FDA increasingly uses surrogate endpoints to judge efficacy, such as tumor shrinkage for cancer drugs or LDL cholesterol decrease for lipid therapy, instead of definitive outcomes like morbidity and mortality. To the extent these surrogate endpoints strongly correlate with major outcomes, this can appropriately speed up the approval process, but the value of surrogate markers is not always clear. These characteristics of phase 3 studies often lead to approval of many “me-too” drugs without the information necessary to decide whether they are better than current standard therapy.
Deficiencies in using surrogate markers
A particular problem with surrogate markers occurs with the review of higher-priority drugs. For these, the FDA may grant provisional approval on the basis of a surrogate measure of clinical benefit shown in a single, uncontrolled trial as long as the treatment addresses an unmet need for a serious medical illness. In return, the FDA requires the company to complete confirmatory trials in the post-approval period, and may withdraw approval of the drug if no benefit is shown in these phase 4 trials.
However, between 1996 and 2003, only 6 of 23 cancer drugs have gone through such post-marketing trials, and the FDA has not withdrawn approval for any of the 23 drugs. Furthermore, many of these drugs cost thousands of dollars per treatment and have low response rates, yet the FDA has not required companies to better define the target populations for their use.10
The problem with using surrogate endpoints in short trials has been demonstrated in cardiovascular medicine with the experience using antiarrhythmics to prevent premature ventricular contractions (later discovered to lead to increased mortality), inotropics to improve ejection fraction (no long-term benefit) and, most recently, with nesiritide (Natrecor) for heart failure. The latter drug was approved based on improved pulmonarycapillary wedge pressure and self-reported improvement in dyspnea. Subsequent research and analyses have shown increased rates of renal failure and death but only after hundreds of millions of dollars worth of treatments.11
Recommendations to make the system work
Given the controversy surrounding the release and marketing of medications that later have shown to cause problems, and given the array of real and perceived conflicts of interest in the approval process, the FDA has proposed establishing a Drug Safety Oversight Board that will include outside experts to review safety issues arising with new applications. Others have argued that such a board should be completely independent of the FDA so as to minimize conflicts of interest and potential agency interference with obtaining necessary information from the companies.
The FDA also recently announced a new rule to overhaul prescription drug labeling, information in package inserts, and some drug reference books. The labels are full of information but much of it is inconsequential or difficult to use for prescribing, and most physicians don’t read them. The new labels will list safety warnings, advise how to use the drug and dose it, and advise physicians on what patients should be told about the medication. The goal is to give physicians more useful information to make decisions about drug indications and dosing. While the new rule will not change the patient drug information sheets that pharmacists hand out, it may force consumer advertising to make clearer statements about medication risks. Finally, the rule will preempt state liability statutes, which upsets some trial lawyers and politicians.12
Outside experts have proposed additional ideas to improve the FDA’s work: eliminating the current drug company fees that support new drug reviews to minimize conflicts of interest, mandating post-approval studies to look for uncommon adverse events (phase 4 studies), providing more information on relative efficacy of new drugs compared with current medication treatment and attention to real clinical outcome end points, and prohibiting direct-to-consumer advertising in the first 3 years after a new drug is released.13
Considering the turmoil surrounding the FDA’s performance right now, it is very possible we will see some of these proposed changes come to pass. Given the importance of prescription medications, these changes will be very relevant to the practices of family physicians and their patients’ health.
CORRESPONDENCE
Eric A. Henley, MD, MPH, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, 1601 Parkview Avenue, Rockford, IL 61107-1897. E-mail: [email protected]
1. Slater E. Today’s FDA. N Engl J Med 2005;352:293-297.
2. Curfman GD, Morrissey S, Drazen JM. Expression of concern: Bombardier et al., “Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis,” N Engl J Med 2000; 343:1520-8. Editorial. N Engl J Med 2005;353:2813-2814.
3. Harris G. Pfizer to pay $420 million in illegal marketing case. New York Times, May 14, 2004.
4. Markel H. Why America needs a strong FDA. JAMA 2005;294:2489-2491.
5. Kaiser Daily Health Policy Report. March 3, 2005. Available at: www.kaisernetwork.org/daily_reports/rep_index.cfm?hint=3&DR_ID=28455. Accessed on March 10, 2006.
6. Okie S. What ails the FDA. N Engl J Med 2005;352:1063-1066.
7. Berenson A. Drugs in ’05: Much promise, little payoff; just 20 new products are approved despite biotechnology’s hope. New York Times, Jan 11, 2006.
8. FDA’s review process for new drug applications. Office of Inspector General. March 2003. Available at: www.oig.hhs.gov/oei/reports/oei-01-01-00590.pdf. Accessed on March 10, 2006.
9. 65% of promised drug studies pending. Washington Post, March 4, 2006 (AP report)
10. Roberts T, Chabner B. Beyond fast track for drug approvals. N Engl J Med 2004;351:501-505.
11. Topol E. Nesiritide—not verified. N Engl J Med 2005;353:113-116.
12. Harris G. New drug label rule is intended to reduce medical errors. New York Times, January 19, 2006.
13. Ray W, Stein CM. Reform of drug regulation—beyond an independent drug-safety board. N Engl J Med 2006;354:194-201.
1. Slater E. Today’s FDA. N Engl J Med 2005;352:293-297.
2. Curfman GD, Morrissey S, Drazen JM. Expression of concern: Bombardier et al., “Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis,” N Engl J Med 2000; 343:1520-8. Editorial. N Engl J Med 2005;353:2813-2814.
3. Harris G. Pfizer to pay $420 million in illegal marketing case. New York Times, May 14, 2004.
4. Markel H. Why America needs a strong FDA. JAMA 2005;294:2489-2491.
5. Kaiser Daily Health Policy Report. March 3, 2005. Available at: www.kaisernetwork.org/daily_reports/rep_index.cfm?hint=3&DR_ID=28455. Accessed on March 10, 2006.
6. Okie S. What ails the FDA. N Engl J Med 2005;352:1063-1066.
7. Berenson A. Drugs in ’05: Much promise, little payoff; just 20 new products are approved despite biotechnology’s hope. New York Times, Jan 11, 2006.
8. FDA’s review process for new drug applications. Office of Inspector General. March 2003. Available at: www.oig.hhs.gov/oei/reports/oei-01-01-00590.pdf. Accessed on March 10, 2006.
9. 65% of promised drug studies pending. Washington Post, March 4, 2006 (AP report)
10. Roberts T, Chabner B. Beyond fast track for drug approvals. N Engl J Med 2004;351:501-505.
11. Topol E. Nesiritide—not verified. N Engl J Med 2005;353:113-116.
12. Harris G. New drug label rule is intended to reduce medical errors. New York Times, January 19, 2006.
13. Ray W, Stein CM. Reform of drug regulation—beyond an independent drug-safety board. N Engl J Med 2006;354:194-201.