User login
Experimental drug holds promise for the treatment of thyroid eye disease
LOS ANGELES – researchers reported at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
“For the first time, there appears to be a medicine that can be given during the active phase of the disease and can actually reverse not just the eyelid swelling and the clinical activity score, but also reduce the eye bulging and double vision and [improve] the [patient’s] quality of life. It could be a watershed moment in the treatment of the disease,” said ophthalmologist Raymond Douglas, MD, PhD, professor of surgery at Cedar-Sinai Medical Center Los Angeles and the study’s coprincipal investigator, in an interview at the meeting.
According to Dr. Douglas, thyroid eye disease, which is also known as Graves’ eye disease, is a severely disabling condition that causes swelling, pain, discomfort, and blindness. “The burden really is quite significant,” he said, with an impact that’s been compared with that of breast cancer in quality-of-life studies.
“Current treatments for thyroid eye disease are rather limited,” he said. “They really encompass just reducing the swelling and the short-term manifestations of the disease. Treatments such as IV steroids and radiation have been shown to not have any effect on long-term manifestations such as eye bulging and double vision.”
Teprotumumab is a fully human monoclonal antibody that targets the insulinlike growth factor I receptor (IGF-IR). It seems to downregulate thyroid eye disease, Dr. Douglas said.
Researchers studied the drug in a randomized, placebo-controlled study: 41 patients were designated to receive eight intravenous infusions of the drug over 21 weeks (10 mg/kg for the first infusion, then 20 mg/kg thereafter). At week 24, 83% of the study group (34 of 41 patients) reached the endpoint of a reduction of eye bulging by at least 2 mm, compared with 10% of patients (4 of 42) in the placebo group, which received infusions of saline solution.
Two millimeters is significant, Dr. Douglas said. “If you noticed someone’s eye was bulging 2 millimeters, you’d say, ‘Hey, I think something is wrong with your eye.’ ”
Initial study results were released in February 2019. New data about secondary endpoints were released at the AACE meeting: Researchers reported that the average reduction in proptosis (eye bulging) was 2.82 mm in the study group, compared with 0.54 mm in the placebo group (P less than .001).
Dr. Douglas said he can “achieve 3 mm of reduction through surgery to drill out the bone between the eye and the brain. [The patients in the study group] were able to achieve almost 3 millimeters of reduction by the drug alone. It’s a rather significant improvement.”
The new data also provided some insight into the timing of clinical improvements. According to Dr. Douglas, “most of the endpoints were met as early as 6 weeks or [after] two infusions of this drug.”
The adverse effects were relatively mild and included muscle spasms, said Dr. Douglas. The side effects seem to be “well tolerated,” he noted, and none led to cessation of therapy.
Participants with potential for motherhood or fatherhood during the trial had to agree to take precautions to avoid becoming pregnant or impregnating a partner.
Dr. Douglas didn’t provide cost information about the drug. However, it seems likely to be expensive. A writer with Seeking Alpha, a stock market analysis site, estimated that the cost could reach “$250,000 or $300,000 per patient per year, which translates to a $3.7 billion to $6 billion market in the United States alone (based on the estimated patient population in the 15,000-20,000 range).”
The drug’s manufacturer, Horizon Therapeutics, expects to apply to the Food and Drug Administration later this year for approval of the drug.
If it is approved, endocrinologists will have an opportunity to partner with eye surgeons to treat thyroid eye disease, Dr. Douglas said. “The crux will be the comanagement with the endocrinologist helping to control the thyroid function and manage some of the side effects of this medication, and the oculoplastic surgeon [working on] diagnosis, appropriate use, and management.”
Horizon Therapeutics funded the study. Dr. Douglas disclosed that he is a consultant with the company.
LOS ANGELES – researchers reported at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
“For the first time, there appears to be a medicine that can be given during the active phase of the disease and can actually reverse not just the eyelid swelling and the clinical activity score, but also reduce the eye bulging and double vision and [improve] the [patient’s] quality of life. It could be a watershed moment in the treatment of the disease,” said ophthalmologist Raymond Douglas, MD, PhD, professor of surgery at Cedar-Sinai Medical Center Los Angeles and the study’s coprincipal investigator, in an interview at the meeting.
According to Dr. Douglas, thyroid eye disease, which is also known as Graves’ eye disease, is a severely disabling condition that causes swelling, pain, discomfort, and blindness. “The burden really is quite significant,” he said, with an impact that’s been compared with that of breast cancer in quality-of-life studies.
“Current treatments for thyroid eye disease are rather limited,” he said. “They really encompass just reducing the swelling and the short-term manifestations of the disease. Treatments such as IV steroids and radiation have been shown to not have any effect on long-term manifestations such as eye bulging and double vision.”
Teprotumumab is a fully human monoclonal antibody that targets the insulinlike growth factor I receptor (IGF-IR). It seems to downregulate thyroid eye disease, Dr. Douglas said.
Researchers studied the drug in a randomized, placebo-controlled study: 41 patients were designated to receive eight intravenous infusions of the drug over 21 weeks (10 mg/kg for the first infusion, then 20 mg/kg thereafter). At week 24, 83% of the study group (34 of 41 patients) reached the endpoint of a reduction of eye bulging by at least 2 mm, compared with 10% of patients (4 of 42) in the placebo group, which received infusions of saline solution.
Two millimeters is significant, Dr. Douglas said. “If you noticed someone’s eye was bulging 2 millimeters, you’d say, ‘Hey, I think something is wrong with your eye.’ ”
Initial study results were released in February 2019. New data about secondary endpoints were released at the AACE meeting: Researchers reported that the average reduction in proptosis (eye bulging) was 2.82 mm in the study group, compared with 0.54 mm in the placebo group (P less than .001).
Dr. Douglas said he can “achieve 3 mm of reduction through surgery to drill out the bone between the eye and the brain. [The patients in the study group] were able to achieve almost 3 millimeters of reduction by the drug alone. It’s a rather significant improvement.”
The new data also provided some insight into the timing of clinical improvements. According to Dr. Douglas, “most of the endpoints were met as early as 6 weeks or [after] two infusions of this drug.”
The adverse effects were relatively mild and included muscle spasms, said Dr. Douglas. The side effects seem to be “well tolerated,” he noted, and none led to cessation of therapy.
Participants with potential for motherhood or fatherhood during the trial had to agree to take precautions to avoid becoming pregnant or impregnating a partner.
Dr. Douglas didn’t provide cost information about the drug. However, it seems likely to be expensive. A writer with Seeking Alpha, a stock market analysis site, estimated that the cost could reach “$250,000 or $300,000 per patient per year, which translates to a $3.7 billion to $6 billion market in the United States alone (based on the estimated patient population in the 15,000-20,000 range).”
The drug’s manufacturer, Horizon Therapeutics, expects to apply to the Food and Drug Administration later this year for approval of the drug.
If it is approved, endocrinologists will have an opportunity to partner with eye surgeons to treat thyroid eye disease, Dr. Douglas said. “The crux will be the comanagement with the endocrinologist helping to control the thyroid function and manage some of the side effects of this medication, and the oculoplastic surgeon [working on] diagnosis, appropriate use, and management.”
Horizon Therapeutics funded the study. Dr. Douglas disclosed that he is a consultant with the company.
LOS ANGELES – researchers reported at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
“For the first time, there appears to be a medicine that can be given during the active phase of the disease and can actually reverse not just the eyelid swelling and the clinical activity score, but also reduce the eye bulging and double vision and [improve] the [patient’s] quality of life. It could be a watershed moment in the treatment of the disease,” said ophthalmologist Raymond Douglas, MD, PhD, professor of surgery at Cedar-Sinai Medical Center Los Angeles and the study’s coprincipal investigator, in an interview at the meeting.
According to Dr. Douglas, thyroid eye disease, which is also known as Graves’ eye disease, is a severely disabling condition that causes swelling, pain, discomfort, and blindness. “The burden really is quite significant,” he said, with an impact that’s been compared with that of breast cancer in quality-of-life studies.
“Current treatments for thyroid eye disease are rather limited,” he said. “They really encompass just reducing the swelling and the short-term manifestations of the disease. Treatments such as IV steroids and radiation have been shown to not have any effect on long-term manifestations such as eye bulging and double vision.”
Teprotumumab is a fully human monoclonal antibody that targets the insulinlike growth factor I receptor (IGF-IR). It seems to downregulate thyroid eye disease, Dr. Douglas said.
Researchers studied the drug in a randomized, placebo-controlled study: 41 patients were designated to receive eight intravenous infusions of the drug over 21 weeks (10 mg/kg for the first infusion, then 20 mg/kg thereafter). At week 24, 83% of the study group (34 of 41 patients) reached the endpoint of a reduction of eye bulging by at least 2 mm, compared with 10% of patients (4 of 42) in the placebo group, which received infusions of saline solution.
Two millimeters is significant, Dr. Douglas said. “If you noticed someone’s eye was bulging 2 millimeters, you’d say, ‘Hey, I think something is wrong with your eye.’ ”
Initial study results were released in February 2019. New data about secondary endpoints were released at the AACE meeting: Researchers reported that the average reduction in proptosis (eye bulging) was 2.82 mm in the study group, compared with 0.54 mm in the placebo group (P less than .001).
Dr. Douglas said he can “achieve 3 mm of reduction through surgery to drill out the bone between the eye and the brain. [The patients in the study group] were able to achieve almost 3 millimeters of reduction by the drug alone. It’s a rather significant improvement.”
The new data also provided some insight into the timing of clinical improvements. According to Dr. Douglas, “most of the endpoints were met as early as 6 weeks or [after] two infusions of this drug.”
The adverse effects were relatively mild and included muscle spasms, said Dr. Douglas. The side effects seem to be “well tolerated,” he noted, and none led to cessation of therapy.
Participants with potential for motherhood or fatherhood during the trial had to agree to take precautions to avoid becoming pregnant or impregnating a partner.
Dr. Douglas didn’t provide cost information about the drug. However, it seems likely to be expensive. A writer with Seeking Alpha, a stock market analysis site, estimated that the cost could reach “$250,000 or $300,000 per patient per year, which translates to a $3.7 billion to $6 billion market in the United States alone (based on the estimated patient population in the 15,000-20,000 range).”
The drug’s manufacturer, Horizon Therapeutics, expects to apply to the Food and Drug Administration later this year for approval of the drug.
If it is approved, endocrinologists will have an opportunity to partner with eye surgeons to treat thyroid eye disease, Dr. Douglas said. “The crux will be the comanagement with the endocrinologist helping to control the thyroid function and manage some of the side effects of this medication, and the oculoplastic surgeon [working on] diagnosis, appropriate use, and management.”
Horizon Therapeutics funded the study. Dr. Douglas disclosed that he is a consultant with the company.
REPORTING FROM AACE 2019
Renal denervation boosts effectiveness of AFib catheter ablation
SAN FRANCISCO – Adding renal denervation when performing catheter ablation of paroxysmal atrial fibrillation in hypertensive patients substantially reduced their arrhythmia recurrence rate during the subsequent year in a multicenter, randomized trial with 302 patients.
The findings established renal denervation (RDN) as a “reasonable” tool to increase the success of atrial fibrillation (AFib) catheter ablation, Jonathan S. Steinberg, MD, said at the annual scientific sessions of the Heart Rhythm Society.
“The RDN procedure seems remarkably safe and seems to be reliably accomplished when an electrophysiologist does it,” said Dr. Steinberg, director of the Arrhythmia Center of the Summit Medical Group in Montclair, N.J. Given the evidence he reported that performing RDN simultaneously with AFib catheter ablation by pulmonary vein isolation significantly improved freedom from arrhythmia recurrence, this approach “is ready for clinical use at institutions that could mount this kind of program,” he declared.
The rate of freedom from arrhythmia recurrence while off antiarrhythmic drugs during the year following treatment was 57% among 138 patients treated with pulmonary vein isolation only, and 72% in 145 who underwent both pulmonary vein isolation and renal denervation. That’s “a pretty big difference in outcome” with no increased risk and with about 20 added minutes of procedure time, Dr. Steinberg said in a video interview. He acknowledged that, currently, no catheter is approved for U.S. marketing that is specifically designed for renal denervation, but the operators in the study he reported all used conventional radiofrequency ablation catheters with an irrigated tip, a design with U.S. availability.
The ERADICATE-AF (Renal Artery Denervation in Addition to Catheter Ablation to Eliminate Atrial Fibrillation) study randomized 302 patients with paroxysmal AFib and hypertension uncontrolled by medication at three centers in Russia, one in Germany, and one in Poland. Enrolled patients averaged about 60 years of age, about 60% were men, and their average blood pressure was roughly 150/90 mm Hg while on treatment with a median of two antihypertensive drugs, including 100% on either an ACE inhibitor or angiotensin receptor blocker. The study operators performed RDN by placing an average of six lesions in a spiral pattern in each of the patient’s two renal arteries.
The investigators screened for arrhythmia recurrence with 7-day Holter monitoring at 3, 6, 9, and 12 months, with full 12-month follow-up available for 283 patients. After 12 months, blood pressures had declined by an average of 16/11 mm Hg among the patients who underwent RDN, with essentially no change in the patients who had pulmonary vein isolation only. Dr. Steinberg attributed the high success of the renal denervation procedures to the familiarity of the participating electrophysiologist operators with catheter-tip ablations.
“We have gone from treating patients with resistant hypertension to now treating patients with less severe hypertension,” Dr. Steinberg noted, and the next study he is planning will take this approach into patients with paroxysmal AFib but without hypertension, using RDN “solely as an anti-arrhythmic intervention,” he explained.
ERADICATE-AF did not receive commercial funding. Dr. Steinberg has been a consultant to Allergan, AtriCure, Biosense Webster, Corfigo, Medtronic, and Omron. He owns stock in AliveCor and receives salary from National Cardiac and G Medical.
ERADICATE-AF was a well-performed, informative, and provocative study that produced exciting results. I was very impressed that, despite the added complexity of performing an extra procedure, there appeared to be virtually no added risk to patients, with essentially identical complication rates in the two arms of the study. The 15.6% absolute difference in the rate of arrhythmia recurrences means that about six patients need to have renal denervation added to their catheter ablation to prevent one arrhythmia recurrence during 12 months, a pretty remarkable number-needed-to-treat.
Despite the successful outcome, adding renal denervation is not a panacea. These patients still had a 28% rate of recurrent atrial fibrillation during follow-up, and on average they also remained above their goal blood pressure despite the pressure reduction that renal denervation produced. The 43% arrhythmia recurrence rate among the patients who underwent only pulmonary vein isolation was consistent with prior reports on the efficacy of this treatment.
The findings raise the question of whether this approach would also work in AFib patients who are not hypertensive, and we must be cautious about the longer-term safety and durability of this treatment.
Cara N. Pellegrini, MD , is director of cardiac electrophysiology at the San Francisco VA Medical Center. She had no disclosures. She made these comments as designated discussant for ERADICATE-AF.
ERADICATE-AF was a well-performed, informative, and provocative study that produced exciting results. I was very impressed that, despite the added complexity of performing an extra procedure, there appeared to be virtually no added risk to patients, with essentially identical complication rates in the two arms of the study. The 15.6% absolute difference in the rate of arrhythmia recurrences means that about six patients need to have renal denervation added to their catheter ablation to prevent one arrhythmia recurrence during 12 months, a pretty remarkable number-needed-to-treat.
Despite the successful outcome, adding renal denervation is not a panacea. These patients still had a 28% rate of recurrent atrial fibrillation during follow-up, and on average they also remained above their goal blood pressure despite the pressure reduction that renal denervation produced. The 43% arrhythmia recurrence rate among the patients who underwent only pulmonary vein isolation was consistent with prior reports on the efficacy of this treatment.
The findings raise the question of whether this approach would also work in AFib patients who are not hypertensive, and we must be cautious about the longer-term safety and durability of this treatment.
Cara N. Pellegrini, MD , is director of cardiac electrophysiology at the San Francisco VA Medical Center. She had no disclosures. She made these comments as designated discussant for ERADICATE-AF.
ERADICATE-AF was a well-performed, informative, and provocative study that produced exciting results. I was very impressed that, despite the added complexity of performing an extra procedure, there appeared to be virtually no added risk to patients, with essentially identical complication rates in the two arms of the study. The 15.6% absolute difference in the rate of arrhythmia recurrences means that about six patients need to have renal denervation added to their catheter ablation to prevent one arrhythmia recurrence during 12 months, a pretty remarkable number-needed-to-treat.
Despite the successful outcome, adding renal denervation is not a panacea. These patients still had a 28% rate of recurrent atrial fibrillation during follow-up, and on average they also remained above their goal blood pressure despite the pressure reduction that renal denervation produced. The 43% arrhythmia recurrence rate among the patients who underwent only pulmonary vein isolation was consistent with prior reports on the efficacy of this treatment.
The findings raise the question of whether this approach would also work in AFib patients who are not hypertensive, and we must be cautious about the longer-term safety and durability of this treatment.
Cara N. Pellegrini, MD , is director of cardiac electrophysiology at the San Francisco VA Medical Center. She had no disclosures. She made these comments as designated discussant for ERADICATE-AF.
SAN FRANCISCO – Adding renal denervation when performing catheter ablation of paroxysmal atrial fibrillation in hypertensive patients substantially reduced their arrhythmia recurrence rate during the subsequent year in a multicenter, randomized trial with 302 patients.
The findings established renal denervation (RDN) as a “reasonable” tool to increase the success of atrial fibrillation (AFib) catheter ablation, Jonathan S. Steinberg, MD, said at the annual scientific sessions of the Heart Rhythm Society.
“The RDN procedure seems remarkably safe and seems to be reliably accomplished when an electrophysiologist does it,” said Dr. Steinberg, director of the Arrhythmia Center of the Summit Medical Group in Montclair, N.J. Given the evidence he reported that performing RDN simultaneously with AFib catheter ablation by pulmonary vein isolation significantly improved freedom from arrhythmia recurrence, this approach “is ready for clinical use at institutions that could mount this kind of program,” he declared.
The rate of freedom from arrhythmia recurrence while off antiarrhythmic drugs during the year following treatment was 57% among 138 patients treated with pulmonary vein isolation only, and 72% in 145 who underwent both pulmonary vein isolation and renal denervation. That’s “a pretty big difference in outcome” with no increased risk and with about 20 added minutes of procedure time, Dr. Steinberg said in a video interview. He acknowledged that, currently, no catheter is approved for U.S. marketing that is specifically designed for renal denervation, but the operators in the study he reported all used conventional radiofrequency ablation catheters with an irrigated tip, a design with U.S. availability.
The ERADICATE-AF (Renal Artery Denervation in Addition to Catheter Ablation to Eliminate Atrial Fibrillation) study randomized 302 patients with paroxysmal AFib and hypertension uncontrolled by medication at three centers in Russia, one in Germany, and one in Poland. Enrolled patients averaged about 60 years of age, about 60% were men, and their average blood pressure was roughly 150/90 mm Hg while on treatment with a median of two antihypertensive drugs, including 100% on either an ACE inhibitor or angiotensin receptor blocker. The study operators performed RDN by placing an average of six lesions in a spiral pattern in each of the patient’s two renal arteries.
The investigators screened for arrhythmia recurrence with 7-day Holter monitoring at 3, 6, 9, and 12 months, with full 12-month follow-up available for 283 patients. After 12 months, blood pressures had declined by an average of 16/11 mm Hg among the patients who underwent RDN, with essentially no change in the patients who had pulmonary vein isolation only. Dr. Steinberg attributed the high success of the renal denervation procedures to the familiarity of the participating electrophysiologist operators with catheter-tip ablations.
“We have gone from treating patients with resistant hypertension to now treating patients with less severe hypertension,” Dr. Steinberg noted, and the next study he is planning will take this approach into patients with paroxysmal AFib but without hypertension, using RDN “solely as an anti-arrhythmic intervention,” he explained.
ERADICATE-AF did not receive commercial funding. Dr. Steinberg has been a consultant to Allergan, AtriCure, Biosense Webster, Corfigo, Medtronic, and Omron. He owns stock in AliveCor and receives salary from National Cardiac and G Medical.
SAN FRANCISCO – Adding renal denervation when performing catheter ablation of paroxysmal atrial fibrillation in hypertensive patients substantially reduced their arrhythmia recurrence rate during the subsequent year in a multicenter, randomized trial with 302 patients.
The findings established renal denervation (RDN) as a “reasonable” tool to increase the success of atrial fibrillation (AFib) catheter ablation, Jonathan S. Steinberg, MD, said at the annual scientific sessions of the Heart Rhythm Society.
“The RDN procedure seems remarkably safe and seems to be reliably accomplished when an electrophysiologist does it,” said Dr. Steinberg, director of the Arrhythmia Center of the Summit Medical Group in Montclair, N.J. Given the evidence he reported that performing RDN simultaneously with AFib catheter ablation by pulmonary vein isolation significantly improved freedom from arrhythmia recurrence, this approach “is ready for clinical use at institutions that could mount this kind of program,” he declared.
The rate of freedom from arrhythmia recurrence while off antiarrhythmic drugs during the year following treatment was 57% among 138 patients treated with pulmonary vein isolation only, and 72% in 145 who underwent both pulmonary vein isolation and renal denervation. That’s “a pretty big difference in outcome” with no increased risk and with about 20 added minutes of procedure time, Dr. Steinberg said in a video interview. He acknowledged that, currently, no catheter is approved for U.S. marketing that is specifically designed for renal denervation, but the operators in the study he reported all used conventional radiofrequency ablation catheters with an irrigated tip, a design with U.S. availability.
The ERADICATE-AF (Renal Artery Denervation in Addition to Catheter Ablation to Eliminate Atrial Fibrillation) study randomized 302 patients with paroxysmal AFib and hypertension uncontrolled by medication at three centers in Russia, one in Germany, and one in Poland. Enrolled patients averaged about 60 years of age, about 60% were men, and their average blood pressure was roughly 150/90 mm Hg while on treatment with a median of two antihypertensive drugs, including 100% on either an ACE inhibitor or angiotensin receptor blocker. The study operators performed RDN by placing an average of six lesions in a spiral pattern in each of the patient’s two renal arteries.
The investigators screened for arrhythmia recurrence with 7-day Holter monitoring at 3, 6, 9, and 12 months, with full 12-month follow-up available for 283 patients. After 12 months, blood pressures had declined by an average of 16/11 mm Hg among the patients who underwent RDN, with essentially no change in the patients who had pulmonary vein isolation only. Dr. Steinberg attributed the high success of the renal denervation procedures to the familiarity of the participating electrophysiologist operators with catheter-tip ablations.
“We have gone from treating patients with resistant hypertension to now treating patients with less severe hypertension,” Dr. Steinberg noted, and the next study he is planning will take this approach into patients with paroxysmal AFib but without hypertension, using RDN “solely as an anti-arrhythmic intervention,” he explained.
ERADICATE-AF did not receive commercial funding. Dr. Steinberg has been a consultant to Allergan, AtriCure, Biosense Webster, Corfigo, Medtronic, and Omron. He owns stock in AliveCor and receives salary from National Cardiac and G Medical.
REPORTING FROM HEART RHYTHM 2019
Higher AFib ablation volumes linked with better outcomes
SAN FRANCISCO – The number of atrial fibrillation (Afib) catheter ablations a hospital did a year had a substantial, independent effect on patient outcomes in a study of more than 54,000 U.S. catheter ablations performed during 2010-2014.
The results showed that the roughly one-third of studied hospitals with the lowest annual volume of catheter ablations performed, 20 or fewer, had twice the acute complication rate and twice the 30-day in-hospital mortality rate, compared with the hospitals that did 53 or more such procedures annually in patients with atrial fibrillation, Jim W. Cheung, MD, said while presenting a poster at the annual scientific sessions of the Heart Rhythm Society.
The data, taken from 1,738 U.S. hospitals during 2010-2014 and captured in the Nationwide Readmissions Database, also showed that 79% of these hospitals performed 20 or fewer catheter ablations for atrial fibrillation (AFib) annually, with 63% doing 10 or fewer cases per year during the 5 years studied.
The findings raise the question of whether U.S. guidelines for catheter ablation of AFib should specify a minimum case volume for hospital programs, and if so, how high the minimum should be. Volume thresholds are “something to think about,” or a system to designate centers of excellence, Dr. Cheung suggested in a video interview. But interest in setting volume thresholds to better insure competence is often counterbalanced by concerns about patient access, he noted.
The prevailing U.S. guidelines for catheter ablation of AFib are in a 2017 statement from the Heart Rhythm Society and several collaborating groups (J Arrhythm. 2017 Oct;33[5]:369-409). The statement focused on operator volume rather than hospital volume and said that each operator should perform “several” AFib ablation procedures each month, which is generally understood to mean at least 2 per month or at least about 25 annually, commented Hugh Calkins, MD, chair of the panel that wrote the statement and professor of medicine at Johns Hopkins Medicine in Baltimore. The major rationale for setting a suggested minimum of about 25 cases/year came largely from a 2013 report that is cited as the first study to document a volume-outcome relationship for catheter ablation of AFib (Circulation. 2013 Nov 5;128[19]:2104-12), Dr. Calkins noted. “Volume does matter,” he agreed in an interview, but no society or organization monitors hospital or operator volumes, nor takes any steps when volumes are low.
The Nationwide Readmissions Database included 54,599 patients who underwent AFib catheter ablation during 2010-2014. Dr. Cheung and his associates divided these patients into rough tertiles based on the annual procedure volumes of the hospitals that performed these ablations. The 36% of patients treated at hospitals that did 20 or fewer procedures annually were on average older and had more comorbidities than the 31% treated at hospitals in the highest-volume tertile, which performed at least 53 ablations annually. In an analysis that adjusted for these demographic and clinical differences, patients ablated at the lower-volume hospitals had a statistically significant 2.06-fold higher rate of any complication and a 2.24-fold increased rate of in-hospital mortality, either during the index hospitalization or during a 30-day hospital readmission, reported Dr. Cheung, director of clinical electrophysiology research at Weill Cornell Medical College in New York. The increased rate of complications was driven by a fivefold increased rate of cardiac perforations, a greater than doubled periprocedural stroke rate, and a roughly 50% increased rate of vascular complications, compared with the highest-volume hospitals and after adjustment for baseline differences.
Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. Dr. Calkins disclosed ties to Abbott, Altathera, AtriCure, Boehringer Ingelheim, Boston Scientific, Medtronic, St. Jude, and MRI Interventions.
SOURCE: Cheung JW. HRS 2019, Abstract S-P001-123.
SAN FRANCISCO – The number of atrial fibrillation (Afib) catheter ablations a hospital did a year had a substantial, independent effect on patient outcomes in a study of more than 54,000 U.S. catheter ablations performed during 2010-2014.
The results showed that the roughly one-third of studied hospitals with the lowest annual volume of catheter ablations performed, 20 or fewer, had twice the acute complication rate and twice the 30-day in-hospital mortality rate, compared with the hospitals that did 53 or more such procedures annually in patients with atrial fibrillation, Jim W. Cheung, MD, said while presenting a poster at the annual scientific sessions of the Heart Rhythm Society.
The data, taken from 1,738 U.S. hospitals during 2010-2014 and captured in the Nationwide Readmissions Database, also showed that 79% of these hospitals performed 20 or fewer catheter ablations for atrial fibrillation (AFib) annually, with 63% doing 10 or fewer cases per year during the 5 years studied.
The findings raise the question of whether U.S. guidelines for catheter ablation of AFib should specify a minimum case volume for hospital programs, and if so, how high the minimum should be. Volume thresholds are “something to think about,” or a system to designate centers of excellence, Dr. Cheung suggested in a video interview. But interest in setting volume thresholds to better insure competence is often counterbalanced by concerns about patient access, he noted.
The prevailing U.S. guidelines for catheter ablation of AFib are in a 2017 statement from the Heart Rhythm Society and several collaborating groups (J Arrhythm. 2017 Oct;33[5]:369-409). The statement focused on operator volume rather than hospital volume and said that each operator should perform “several” AFib ablation procedures each month, which is generally understood to mean at least 2 per month or at least about 25 annually, commented Hugh Calkins, MD, chair of the panel that wrote the statement and professor of medicine at Johns Hopkins Medicine in Baltimore. The major rationale for setting a suggested minimum of about 25 cases/year came largely from a 2013 report that is cited as the first study to document a volume-outcome relationship for catheter ablation of AFib (Circulation. 2013 Nov 5;128[19]:2104-12), Dr. Calkins noted. “Volume does matter,” he agreed in an interview, but no society or organization monitors hospital or operator volumes, nor takes any steps when volumes are low.
The Nationwide Readmissions Database included 54,599 patients who underwent AFib catheter ablation during 2010-2014. Dr. Cheung and his associates divided these patients into rough tertiles based on the annual procedure volumes of the hospitals that performed these ablations. The 36% of patients treated at hospitals that did 20 or fewer procedures annually were on average older and had more comorbidities than the 31% treated at hospitals in the highest-volume tertile, which performed at least 53 ablations annually. In an analysis that adjusted for these demographic and clinical differences, patients ablated at the lower-volume hospitals had a statistically significant 2.06-fold higher rate of any complication and a 2.24-fold increased rate of in-hospital mortality, either during the index hospitalization or during a 30-day hospital readmission, reported Dr. Cheung, director of clinical electrophysiology research at Weill Cornell Medical College in New York. The increased rate of complications was driven by a fivefold increased rate of cardiac perforations, a greater than doubled periprocedural stroke rate, and a roughly 50% increased rate of vascular complications, compared with the highest-volume hospitals and after adjustment for baseline differences.
Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. Dr. Calkins disclosed ties to Abbott, Altathera, AtriCure, Boehringer Ingelheim, Boston Scientific, Medtronic, St. Jude, and MRI Interventions.
SOURCE: Cheung JW. HRS 2019, Abstract S-P001-123.
SAN FRANCISCO – The number of atrial fibrillation (Afib) catheter ablations a hospital did a year had a substantial, independent effect on patient outcomes in a study of more than 54,000 U.S. catheter ablations performed during 2010-2014.
The results showed that the roughly one-third of studied hospitals with the lowest annual volume of catheter ablations performed, 20 or fewer, had twice the acute complication rate and twice the 30-day in-hospital mortality rate, compared with the hospitals that did 53 or more such procedures annually in patients with atrial fibrillation, Jim W. Cheung, MD, said while presenting a poster at the annual scientific sessions of the Heart Rhythm Society.
The data, taken from 1,738 U.S. hospitals during 2010-2014 and captured in the Nationwide Readmissions Database, also showed that 79% of these hospitals performed 20 or fewer catheter ablations for atrial fibrillation (AFib) annually, with 63% doing 10 or fewer cases per year during the 5 years studied.
The findings raise the question of whether U.S. guidelines for catheter ablation of AFib should specify a minimum case volume for hospital programs, and if so, how high the minimum should be. Volume thresholds are “something to think about,” or a system to designate centers of excellence, Dr. Cheung suggested in a video interview. But interest in setting volume thresholds to better insure competence is often counterbalanced by concerns about patient access, he noted.
The prevailing U.S. guidelines for catheter ablation of AFib are in a 2017 statement from the Heart Rhythm Society and several collaborating groups (J Arrhythm. 2017 Oct;33[5]:369-409). The statement focused on operator volume rather than hospital volume and said that each operator should perform “several” AFib ablation procedures each month, which is generally understood to mean at least 2 per month or at least about 25 annually, commented Hugh Calkins, MD, chair of the panel that wrote the statement and professor of medicine at Johns Hopkins Medicine in Baltimore. The major rationale for setting a suggested minimum of about 25 cases/year came largely from a 2013 report that is cited as the first study to document a volume-outcome relationship for catheter ablation of AFib (Circulation. 2013 Nov 5;128[19]:2104-12), Dr. Calkins noted. “Volume does matter,” he agreed in an interview, but no society or organization monitors hospital or operator volumes, nor takes any steps when volumes are low.
The Nationwide Readmissions Database included 54,599 patients who underwent AFib catheter ablation during 2010-2014. Dr. Cheung and his associates divided these patients into rough tertiles based on the annual procedure volumes of the hospitals that performed these ablations. The 36% of patients treated at hospitals that did 20 or fewer procedures annually were on average older and had more comorbidities than the 31% treated at hospitals in the highest-volume tertile, which performed at least 53 ablations annually. In an analysis that adjusted for these demographic and clinical differences, patients ablated at the lower-volume hospitals had a statistically significant 2.06-fold higher rate of any complication and a 2.24-fold increased rate of in-hospital mortality, either during the index hospitalization or during a 30-day hospital readmission, reported Dr. Cheung, director of clinical electrophysiology research at Weill Cornell Medical College in New York. The increased rate of complications was driven by a fivefold increased rate of cardiac perforations, a greater than doubled periprocedural stroke rate, and a roughly 50% increased rate of vascular complications, compared with the highest-volume hospitals and after adjustment for baseline differences.
Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. Dr. Calkins disclosed ties to Abbott, Altathera, AtriCure, Boehringer Ingelheim, Boston Scientific, Medtronic, St. Jude, and MRI Interventions.
SOURCE: Cheung JW. HRS 2019, Abstract S-P001-123.
REPORTING FROM HEART RHYTHM 2019
Key clinical point: .
Major finding: Hospitals performing 20 or fewer catheter ablations annually had twice as many acute complications as hospitals doing at least 53.
Study details: Analysis of 54,599 atrial fibrillation patients who underwent catheter ablation in the Nationwide Readmissions Database.
Disclosures: Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude.
Source: Cheung JW et al. Heart Rhythm 2019, Abstract S-P001-123.
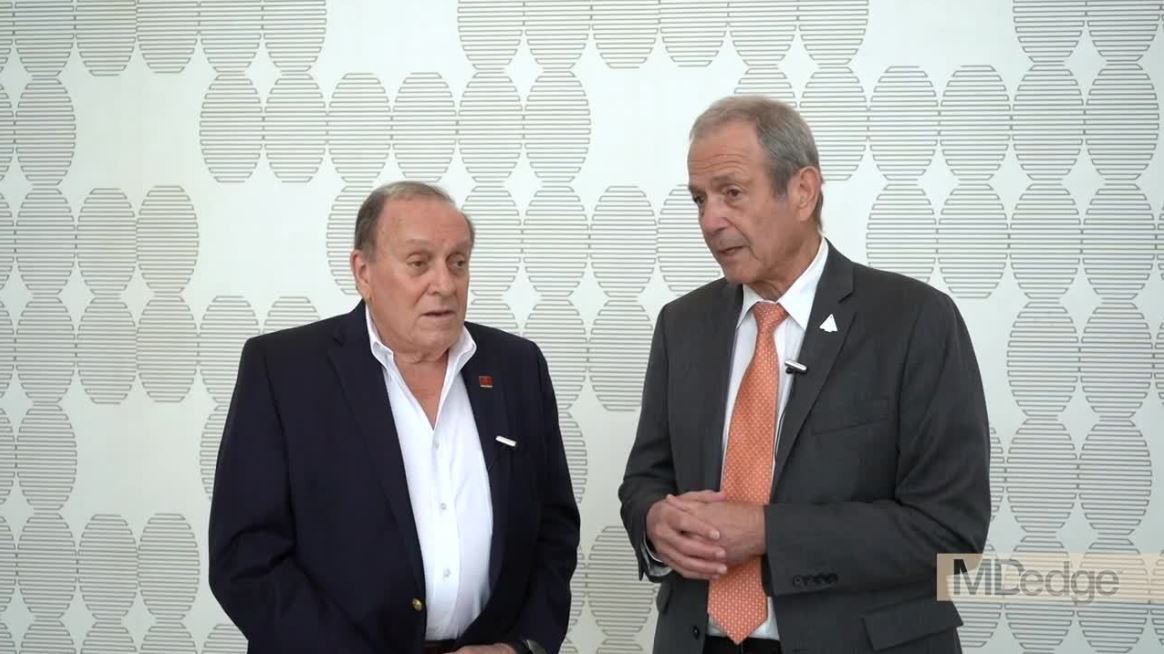
Experts discuss what’s new in migraine treatment
PHILADELPHIA – At the annual meeting of the American Academy of Neurology, Alan M. Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, sat down with Stewart J. Tepper, MD, professor of neurology at the Geisel School of Medicine at Dartmouth, Hanover, N.H., to discuss in a video some of the new data presented at the meeting regarding the CGRP monoclonal antibodies, the small molecule receptor antagonists (gepants), and what Dr. Tepper described as “a real shift in paradigm and a watershed moment in migraine.”
The three gepants that are farthest along in clinical trials are ubrogepant, rimegepant, and atogepant. “Reassuring data” was presented, Dr. Tepper said, regarding liver toxicity, which has been a concern with earlier generations of the gepants. The Food and Drug Administration had mandated a close look at liver function with the use of these drugs, which are metabolized in the liver, and, to date, no safety signals have emerged.
The three CGRP monoclonal antibodies that are currently on the market are erenumab (Aimovig), fremanezumab (Ajovy), and galcanezumab (Emgality). Data from numerous open-label extension studies were presented. In general, it seems that “the monoclonal antibodies accumulate greater efficacy over time,” Dr. Tepper said. No safety concerns have emerged from 5 years of clinical trial data. With 250,000 patients on these drugs worldwide, that is “very reassuring,” Dr. Tepper said.
New data also show that the majority of patients with chronic migraine who are taking monoclonal antibodies convert from chronic migraine to episodic migraine. Additionally, new data show that use of monoclonal antibodies “dramatically reduce all migraine medication use,” Dr. Tepper said.
PHILADELPHIA – At the annual meeting of the American Academy of Neurology, Alan M. Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, sat down with Stewart J. Tepper, MD, professor of neurology at the Geisel School of Medicine at Dartmouth, Hanover, N.H., to discuss in a video some of the new data presented at the meeting regarding the CGRP monoclonal antibodies, the small molecule receptor antagonists (gepants), and what Dr. Tepper described as “a real shift in paradigm and a watershed moment in migraine.”
The three gepants that are farthest along in clinical trials are ubrogepant, rimegepant, and atogepant. “Reassuring data” was presented, Dr. Tepper said, regarding liver toxicity, which has been a concern with earlier generations of the gepants. The Food and Drug Administration had mandated a close look at liver function with the use of these drugs, which are metabolized in the liver, and, to date, no safety signals have emerged.
The three CGRP monoclonal antibodies that are currently on the market are erenumab (Aimovig), fremanezumab (Ajovy), and galcanezumab (Emgality). Data from numerous open-label extension studies were presented. In general, it seems that “the monoclonal antibodies accumulate greater efficacy over time,” Dr. Tepper said. No safety concerns have emerged from 5 years of clinical trial data. With 250,000 patients on these drugs worldwide, that is “very reassuring,” Dr. Tepper said.
New data also show that the majority of patients with chronic migraine who are taking monoclonal antibodies convert from chronic migraine to episodic migraine. Additionally, new data show that use of monoclonal antibodies “dramatically reduce all migraine medication use,” Dr. Tepper said.
PHILADELPHIA – At the annual meeting of the American Academy of Neurology, Alan M. Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, sat down with Stewart J. Tepper, MD, professor of neurology at the Geisel School of Medicine at Dartmouth, Hanover, N.H., to discuss in a video some of the new data presented at the meeting regarding the CGRP monoclonal antibodies, the small molecule receptor antagonists (gepants), and what Dr. Tepper described as “a real shift in paradigm and a watershed moment in migraine.”
The three gepants that are farthest along in clinical trials are ubrogepant, rimegepant, and atogepant. “Reassuring data” was presented, Dr. Tepper said, regarding liver toxicity, which has been a concern with earlier generations of the gepants. The Food and Drug Administration had mandated a close look at liver function with the use of these drugs, which are metabolized in the liver, and, to date, no safety signals have emerged.
The three CGRP monoclonal antibodies that are currently on the market are erenumab (Aimovig), fremanezumab (Ajovy), and galcanezumab (Emgality). Data from numerous open-label extension studies were presented. In general, it seems that “the monoclonal antibodies accumulate greater efficacy over time,” Dr. Tepper said. No safety concerns have emerged from 5 years of clinical trial data. With 250,000 patients on these drugs worldwide, that is “very reassuring,” Dr. Tepper said.
New data also show that the majority of patients with chronic migraine who are taking monoclonal antibodies convert from chronic migraine to episodic migraine. Additionally, new data show that use of monoclonal antibodies “dramatically reduce all migraine medication use,” Dr. Tepper said.
EXPERT ANALYSIS FROM AAN 2019
2019 Update: Contraceptives and unintended pregnancy rates
NASHVILLE, TENN. – The unintended pregnancy rate is declining after years of hovering at close to 50%.
While the rates among women of color remain high – currently at 58 and 79 per 1,000 women aged 15-44 years for Hispanic and black women, respectively – they have declined from 79 and 92 per 1,000 Hispanic and black women in that age group in 2008, and the overall rate is now at about 45%, Eve Espey, MD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“Considering the scope and number of women affected by unplanned pregnancy, this is actually a huge public health achievement,” said Dr. Espey, professor and chair of the department of obstetrics & gynecology at the University of New Mexico, Albuquerque.
she noted, adding that “another enormous determinant of this decrease in unintended pregnancy is the use of long-acting reversible contraception [LARC].” About 2% of women used contraceptives in 2002, and now, based on the latest cycle of data from 2015-2017, 16% of women use contraceptives.
In this video interview, Dr. Espey discusses the main points of her talk entitled “Contraceptives: What you need to know in 2019,” including:
- The importance of “following reproductive justice–based principles and counseling” when it comes to prescribing contraceptives.
- The latest data showing that certain LARC methods remain safe and effective beyond their approved duration of use.
- Trends with respect to tubal ligation and salpingectomy.
- The value of the Centers for Disease Control and Prevention’s U.S. Medical Eligibility Criteria (MEC) for evidence-based guidance on selecting contraceptives based on patients’ individual needs.
“[MEC] is something every ob.gyn. should consider using,” she said, noting that access is available through a free app. “As our patients are more complex and have more comorbidities, it’s particularly helpful for matching up patients and their conditions with recommendations for specific contraceptive methods.”
Dr. Espey reported having no financial disclosures.
NASHVILLE, TENN. – The unintended pregnancy rate is declining after years of hovering at close to 50%.
While the rates among women of color remain high – currently at 58 and 79 per 1,000 women aged 15-44 years for Hispanic and black women, respectively – they have declined from 79 and 92 per 1,000 Hispanic and black women in that age group in 2008, and the overall rate is now at about 45%, Eve Espey, MD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“Considering the scope and number of women affected by unplanned pregnancy, this is actually a huge public health achievement,” said Dr. Espey, professor and chair of the department of obstetrics & gynecology at the University of New Mexico, Albuquerque.
she noted, adding that “another enormous determinant of this decrease in unintended pregnancy is the use of long-acting reversible contraception [LARC].” About 2% of women used contraceptives in 2002, and now, based on the latest cycle of data from 2015-2017, 16% of women use contraceptives.
In this video interview, Dr. Espey discusses the main points of her talk entitled “Contraceptives: What you need to know in 2019,” including:
- The importance of “following reproductive justice–based principles and counseling” when it comes to prescribing contraceptives.
- The latest data showing that certain LARC methods remain safe and effective beyond their approved duration of use.
- Trends with respect to tubal ligation and salpingectomy.
- The value of the Centers for Disease Control and Prevention’s U.S. Medical Eligibility Criteria (MEC) for evidence-based guidance on selecting contraceptives based on patients’ individual needs.
“[MEC] is something every ob.gyn. should consider using,” she said, noting that access is available through a free app. “As our patients are more complex and have more comorbidities, it’s particularly helpful for matching up patients and their conditions with recommendations for specific contraceptive methods.”
Dr. Espey reported having no financial disclosures.
NASHVILLE, TENN. – The unintended pregnancy rate is declining after years of hovering at close to 50%.
While the rates among women of color remain high – currently at 58 and 79 per 1,000 women aged 15-44 years for Hispanic and black women, respectively – they have declined from 79 and 92 per 1,000 Hispanic and black women in that age group in 2008, and the overall rate is now at about 45%, Eve Espey, MD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“Considering the scope and number of women affected by unplanned pregnancy, this is actually a huge public health achievement,” said Dr. Espey, professor and chair of the department of obstetrics & gynecology at the University of New Mexico, Albuquerque.
she noted, adding that “another enormous determinant of this decrease in unintended pregnancy is the use of long-acting reversible contraception [LARC].” About 2% of women used contraceptives in 2002, and now, based on the latest cycle of data from 2015-2017, 16% of women use contraceptives.
In this video interview, Dr. Espey discusses the main points of her talk entitled “Contraceptives: What you need to know in 2019,” including:
- The importance of “following reproductive justice–based principles and counseling” when it comes to prescribing contraceptives.
- The latest data showing that certain LARC methods remain safe and effective beyond their approved duration of use.
- Trends with respect to tubal ligation and salpingectomy.
- The value of the Centers for Disease Control and Prevention’s U.S. Medical Eligibility Criteria (MEC) for evidence-based guidance on selecting contraceptives based on patients’ individual needs.
“[MEC] is something every ob.gyn. should consider using,” she said, noting that access is available through a free app. “As our patients are more complex and have more comorbidities, it’s particularly helpful for matching up patients and their conditions with recommendations for specific contraceptive methods.”
Dr. Espey reported having no financial disclosures.
EXPERT ANALYSIS FROM ACOG 2019
Consider varying generational needs, preferences in the workplace and with patients
NASHVILLE, TENN. – By 2020, millennials will comprise more than a third of individuals in the workplace, and that has important implications for employment, communication, and education, according to Patrice M. Weiss, MD.
Each generation brings a unique set of experiences and expectations. Millennials – or members of “Generation Y,” who comprised 18% of the workforce in 2018 and 0% in 2008 – tend to prefer flexible work hours and communication via technology, she said during a session on navigating generational differences in the workplace during the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
They, along with members of “Generation X” (generally those born between 1962 and 1981) and “Generation Z” (generally those born from 1987 on), tend to be technology savvy, whereas the “Silent Generation” (generally those born between 1925 and 1942) and older members of the “Baby Boomer Generation” (generally those born between 1943 and 1961), may prefer printed communication and phone calls, said Dr. Weiss, chief medical officer at the Carilion Clinic in Roanoke, Va.
“It’s not good, it’s not bad – it’s just the way things are changing,” she said, adding that it’s important to look at the strengths that each generation brings to the workplace.
Importantly, the she said.
In this video interview, she further discusses how generational differences should be considered in medical practice, and how clinicians can adapt to the changing expectations and different needs of patients from different generations.
“Gen Ys want to communicate with us through technology. They don’t want to pick up the phone and schedule an appointment, they want to be able to go online ... through an app and self-schedule an appointment,” she said. “And they want health care when they want it.
“We as health care providers and health care organizations, we need to meet the needs of each generation ... so what we need to do is really identify what are the needs of all the generations as patients.”
During her presentation, Dr. Weiss further noted that these generational differences present a major challenge with respect to teaching, learning, and communicating.
“Rather than becoming frustrated ... let’s hope that we can ... reach across generations, identify what their strengths are, capitalize on those, and then, as health care providers, be more user and consumer friendly to the generations, particularly the millennials [so] that they have access to us and to information.”
Dr. Weiss said she had no relevant financial disclosures.
NASHVILLE, TENN. – By 2020, millennials will comprise more than a third of individuals in the workplace, and that has important implications for employment, communication, and education, according to Patrice M. Weiss, MD.
Each generation brings a unique set of experiences and expectations. Millennials – or members of “Generation Y,” who comprised 18% of the workforce in 2018 and 0% in 2008 – tend to prefer flexible work hours and communication via technology, she said during a session on navigating generational differences in the workplace during the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
They, along with members of “Generation X” (generally those born between 1962 and 1981) and “Generation Z” (generally those born from 1987 on), tend to be technology savvy, whereas the “Silent Generation” (generally those born between 1925 and 1942) and older members of the “Baby Boomer Generation” (generally those born between 1943 and 1961), may prefer printed communication and phone calls, said Dr. Weiss, chief medical officer at the Carilion Clinic in Roanoke, Va.
“It’s not good, it’s not bad – it’s just the way things are changing,” she said, adding that it’s important to look at the strengths that each generation brings to the workplace.
Importantly, the she said.
In this video interview, she further discusses how generational differences should be considered in medical practice, and how clinicians can adapt to the changing expectations and different needs of patients from different generations.
“Gen Ys want to communicate with us through technology. They don’t want to pick up the phone and schedule an appointment, they want to be able to go online ... through an app and self-schedule an appointment,” she said. “And they want health care when they want it.
“We as health care providers and health care organizations, we need to meet the needs of each generation ... so what we need to do is really identify what are the needs of all the generations as patients.”
During her presentation, Dr. Weiss further noted that these generational differences present a major challenge with respect to teaching, learning, and communicating.
“Rather than becoming frustrated ... let’s hope that we can ... reach across generations, identify what their strengths are, capitalize on those, and then, as health care providers, be more user and consumer friendly to the generations, particularly the millennials [so] that they have access to us and to information.”
Dr. Weiss said she had no relevant financial disclosures.
NASHVILLE, TENN. – By 2020, millennials will comprise more than a third of individuals in the workplace, and that has important implications for employment, communication, and education, according to Patrice M. Weiss, MD.
Each generation brings a unique set of experiences and expectations. Millennials – or members of “Generation Y,” who comprised 18% of the workforce in 2018 and 0% in 2008 – tend to prefer flexible work hours and communication via technology, she said during a session on navigating generational differences in the workplace during the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
They, along with members of “Generation X” (generally those born between 1962 and 1981) and “Generation Z” (generally those born from 1987 on), tend to be technology savvy, whereas the “Silent Generation” (generally those born between 1925 and 1942) and older members of the “Baby Boomer Generation” (generally those born between 1943 and 1961), may prefer printed communication and phone calls, said Dr. Weiss, chief medical officer at the Carilion Clinic in Roanoke, Va.
“It’s not good, it’s not bad – it’s just the way things are changing,” she said, adding that it’s important to look at the strengths that each generation brings to the workplace.
Importantly, the she said.
In this video interview, she further discusses how generational differences should be considered in medical practice, and how clinicians can adapt to the changing expectations and different needs of patients from different generations.
“Gen Ys want to communicate with us through technology. They don’t want to pick up the phone and schedule an appointment, they want to be able to go online ... through an app and self-schedule an appointment,” she said. “And they want health care when they want it.
“We as health care providers and health care organizations, we need to meet the needs of each generation ... so what we need to do is really identify what are the needs of all the generations as patients.”
During her presentation, Dr. Weiss further noted that these generational differences present a major challenge with respect to teaching, learning, and communicating.
“Rather than becoming frustrated ... let’s hope that we can ... reach across generations, identify what their strengths are, capitalize on those, and then, as health care providers, be more user and consumer friendly to the generations, particularly the millennials [so] that they have access to us and to information.”
Dr. Weiss said she had no relevant financial disclosures.
EXPERT ANALYSIS FROM ACOG 2019
Researchers propose new risk groups for NK-AML
NEWPORT BEACH, CALIF. – New research suggests patients with normal karyotype acute myeloid leukemia (NK-AML) can be divided into four risk groups associated with overall survival.
Investigators used machine learning algorithms to study the association between mutations and overall survival in 1,352 patients with NK-AML. The analysis revealed combinations of mutations that could be used to classify NK-AML patients into favorable, intermediate-1, intermediate-2, and unfavorable risk groups.
For example, patients who had NPM1 mutations but wild-type FLT3-ITD and DNMT3A, had a median overall survival of 99.1 months and could be classified as favorable risk. Conversely, patients who had NPM1, FLT3-ITD, and DNMT3A mutations, had a median overall survival of 13.4 months and could be classified as unfavorable risk.
Aziz Nazha, MD, of the Cleveland Clinic, and his colleagues conducted this research and presented the findings at the Acute Leukemia Forum of Hemedicus.
The investigators looked at genomic and clinical data from 1,352 patients with NK-AML. The patients were a median age of 55 years and had a median white blood cell count of 21.3 x 109/L, a median hemoglobin of 9.1 g/dL, and a median platelet count of 61 x 109/L. More than half of patients (57.3%) were male.
The patients were screened for 35 genes that are commonly mutated in AML and other myeloid malignancies. The investigators used machine learning algorithms, including random survival forest and recommender system algorithms, to study the association between mutations and overall survival in an “unbiased” way.
Dr. Nazha said there were a median of three mutations per patient sample, and “there are some competing interests between those mutations to impact the prognosis of the patient.”
The investigators used the mutations and their associations with overall survival to classify patients into the risk groups outlined in the table below.
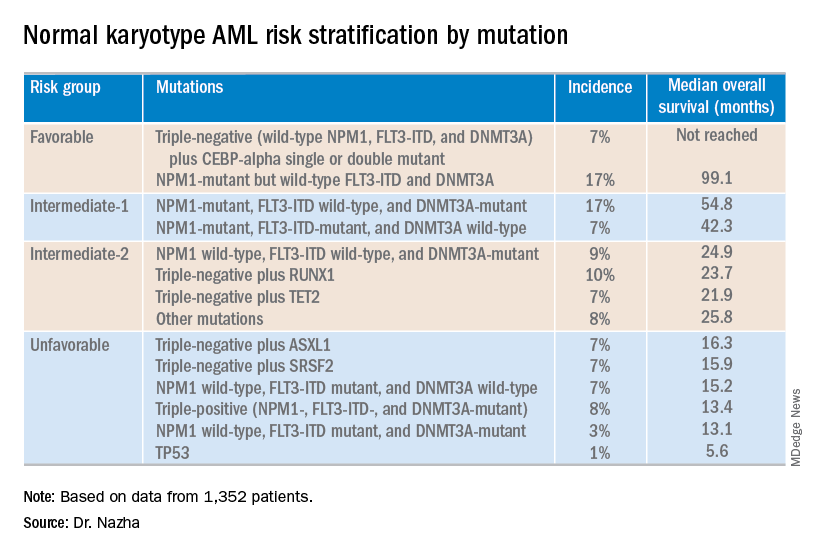
These findings can improve the risk stratification of NK-AML and may aid physicians in making treatment decisions, according to Dr. Nazha and his colleagues. To move this work forward, the investigators are attempting to develop a personalized model that can make predictions specific to an individual patient based on that patient’s mutation information.
Dr. Nazha reported having no financial disclosures relevant to this research. Other investigators reported relationships with the Munich Leukemia Laboratory.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – New research suggests patients with normal karyotype acute myeloid leukemia (NK-AML) can be divided into four risk groups associated with overall survival.
Investigators used machine learning algorithms to study the association between mutations and overall survival in 1,352 patients with NK-AML. The analysis revealed combinations of mutations that could be used to classify NK-AML patients into favorable, intermediate-1, intermediate-2, and unfavorable risk groups.
For example, patients who had NPM1 mutations but wild-type FLT3-ITD and DNMT3A, had a median overall survival of 99.1 months and could be classified as favorable risk. Conversely, patients who had NPM1, FLT3-ITD, and DNMT3A mutations, had a median overall survival of 13.4 months and could be classified as unfavorable risk.
Aziz Nazha, MD, of the Cleveland Clinic, and his colleagues conducted this research and presented the findings at the Acute Leukemia Forum of Hemedicus.
The investigators looked at genomic and clinical data from 1,352 patients with NK-AML. The patients were a median age of 55 years and had a median white blood cell count of 21.3 x 109/L, a median hemoglobin of 9.1 g/dL, and a median platelet count of 61 x 109/L. More than half of patients (57.3%) were male.
The patients were screened for 35 genes that are commonly mutated in AML and other myeloid malignancies. The investigators used machine learning algorithms, including random survival forest and recommender system algorithms, to study the association between mutations and overall survival in an “unbiased” way.
Dr. Nazha said there were a median of three mutations per patient sample, and “there are some competing interests between those mutations to impact the prognosis of the patient.”
The investigators used the mutations and their associations with overall survival to classify patients into the risk groups outlined in the table below.
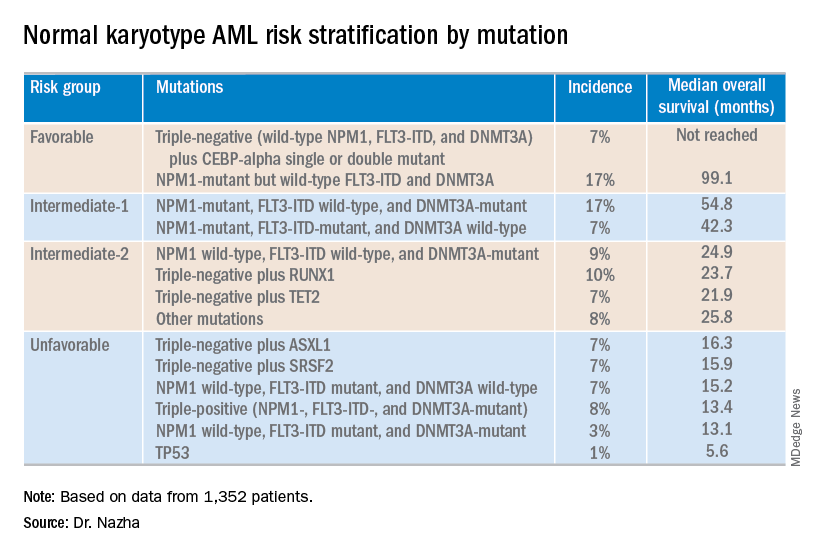
These findings can improve the risk stratification of NK-AML and may aid physicians in making treatment decisions, according to Dr. Nazha and his colleagues. To move this work forward, the investigators are attempting to develop a personalized model that can make predictions specific to an individual patient based on that patient’s mutation information.
Dr. Nazha reported having no financial disclosures relevant to this research. Other investigators reported relationships with the Munich Leukemia Laboratory.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – New research suggests patients with normal karyotype acute myeloid leukemia (NK-AML) can be divided into four risk groups associated with overall survival.
Investigators used machine learning algorithms to study the association between mutations and overall survival in 1,352 patients with NK-AML. The analysis revealed combinations of mutations that could be used to classify NK-AML patients into favorable, intermediate-1, intermediate-2, and unfavorable risk groups.
For example, patients who had NPM1 mutations but wild-type FLT3-ITD and DNMT3A, had a median overall survival of 99.1 months and could be classified as favorable risk. Conversely, patients who had NPM1, FLT3-ITD, and DNMT3A mutations, had a median overall survival of 13.4 months and could be classified as unfavorable risk.
Aziz Nazha, MD, of the Cleveland Clinic, and his colleagues conducted this research and presented the findings at the Acute Leukemia Forum of Hemedicus.
The investigators looked at genomic and clinical data from 1,352 patients with NK-AML. The patients were a median age of 55 years and had a median white blood cell count of 21.3 x 109/L, a median hemoglobin of 9.1 g/dL, and a median platelet count of 61 x 109/L. More than half of patients (57.3%) were male.
The patients were screened for 35 genes that are commonly mutated in AML and other myeloid malignancies. The investigators used machine learning algorithms, including random survival forest and recommender system algorithms, to study the association between mutations and overall survival in an “unbiased” way.
Dr. Nazha said there were a median of three mutations per patient sample, and “there are some competing interests between those mutations to impact the prognosis of the patient.”
The investigators used the mutations and their associations with overall survival to classify patients into the risk groups outlined in the table below.
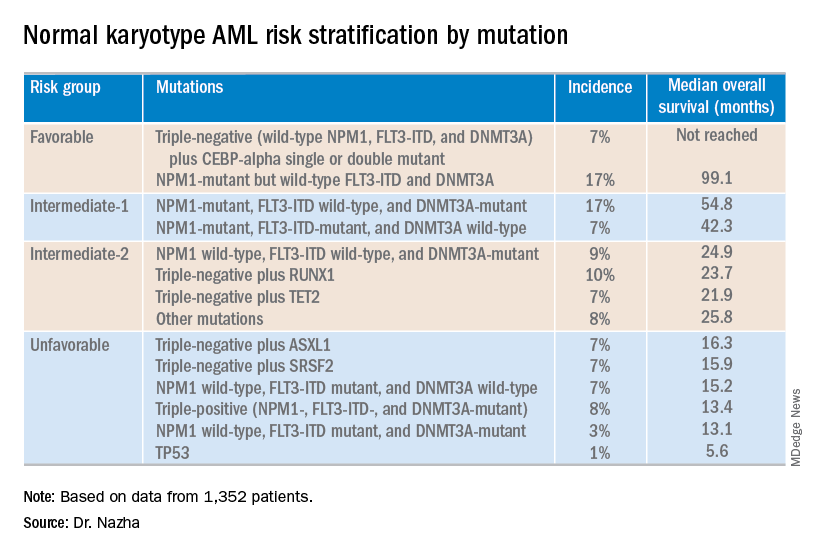
These findings can improve the risk stratification of NK-AML and may aid physicians in making treatment decisions, according to Dr. Nazha and his colleagues. To move this work forward, the investigators are attempting to develop a personalized model that can make predictions specific to an individual patient based on that patient’s mutation information.
Dr. Nazha reported having no financial disclosures relevant to this research. Other investigators reported relationships with the Munich Leukemia Laboratory.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
REPORTING FROM ALF 2019
AACE 2019: Top takeaways from Yehuda Handelsman and Paul Jellinger
in a video interview at the meeting.
Dr. Handelsman, medical director of the Metabolic Institute of America, in Tarzana, Calif., summarized the top take-home messages from a premeeting symposium he chaired on diabetes, cardiovascular disease (CVD), and lipid management in high-risk patients. Dr. Jellinger, professor of clinical medicine on the voluntary faculty at the University of Miami Miller School of Medicine, looked at management aspects and therapy goals based on a comparison of the lipid guideline from the American College of Cardiology and the American Heart Association with that from the AACE. Other highlights from the symposium included expert analysis of the CREDENCE trial results on canagliflozin for improving renal outcomes in patients with type 2 diabetes, advice on the management of heart failure in diabetes, and recommendations on managing hyperglycemia.
Dr. Jellinger and Dr. Handelsman, who are members of the editorial advisory board of Clinical Endocrinology News, highlighted the emergence of anabolic treatments for osteoporosis, in particular the sclerostin-neutralizing monoclonal antibody, romosozumab. The therapy was recently approved for the treatment of postmenopausal osteoporosis and is unique in that it both promotes bone formation and reduces resorption. They also noted the switch away from previous practice to now using an anabolic drug first, then going to an antiresorptive therapy, rather than the other way around.
They discussed the keynote address by social media guru, Kevin Pho, MD; a debate that centered on the merits of the American Diabetes Association’s guideline for treating diabetes versus that from the AACE; a presentation on sustained remission of type 2 diabetes with a very low calorie diet; and a report on encouraging findings with an experimental drug for Graves eye disease.
in a video interview at the meeting.
Dr. Handelsman, medical director of the Metabolic Institute of America, in Tarzana, Calif., summarized the top take-home messages from a premeeting symposium he chaired on diabetes, cardiovascular disease (CVD), and lipid management in high-risk patients. Dr. Jellinger, professor of clinical medicine on the voluntary faculty at the University of Miami Miller School of Medicine, looked at management aspects and therapy goals based on a comparison of the lipid guideline from the American College of Cardiology and the American Heart Association with that from the AACE. Other highlights from the symposium included expert analysis of the CREDENCE trial results on canagliflozin for improving renal outcomes in patients with type 2 diabetes, advice on the management of heart failure in diabetes, and recommendations on managing hyperglycemia.
Dr. Jellinger and Dr. Handelsman, who are members of the editorial advisory board of Clinical Endocrinology News, highlighted the emergence of anabolic treatments for osteoporosis, in particular the sclerostin-neutralizing monoclonal antibody, romosozumab. The therapy was recently approved for the treatment of postmenopausal osteoporosis and is unique in that it both promotes bone formation and reduces resorption. They also noted the switch away from previous practice to now using an anabolic drug first, then going to an antiresorptive therapy, rather than the other way around.
They discussed the keynote address by social media guru, Kevin Pho, MD; a debate that centered on the merits of the American Diabetes Association’s guideline for treating diabetes versus that from the AACE; a presentation on sustained remission of type 2 diabetes with a very low calorie diet; and a report on encouraging findings with an experimental drug for Graves eye disease.
in a video interview at the meeting.
Dr. Handelsman, medical director of the Metabolic Institute of America, in Tarzana, Calif., summarized the top take-home messages from a premeeting symposium he chaired on diabetes, cardiovascular disease (CVD), and lipid management in high-risk patients. Dr. Jellinger, professor of clinical medicine on the voluntary faculty at the University of Miami Miller School of Medicine, looked at management aspects and therapy goals based on a comparison of the lipid guideline from the American College of Cardiology and the American Heart Association with that from the AACE. Other highlights from the symposium included expert analysis of the CREDENCE trial results on canagliflozin for improving renal outcomes in patients with type 2 diabetes, advice on the management of heart failure in diabetes, and recommendations on managing hyperglycemia.
Dr. Jellinger and Dr. Handelsman, who are members of the editorial advisory board of Clinical Endocrinology News, highlighted the emergence of anabolic treatments for osteoporosis, in particular the sclerostin-neutralizing monoclonal antibody, romosozumab. The therapy was recently approved for the treatment of postmenopausal osteoporosis and is unique in that it both promotes bone formation and reduces resorption. They also noted the switch away from previous practice to now using an anabolic drug first, then going to an antiresorptive therapy, rather than the other way around.
They discussed the keynote address by social media guru, Kevin Pho, MD; a debate that centered on the merits of the American Diabetes Association’s guideline for treating diabetes versus that from the AACE; a presentation on sustained remission of type 2 diabetes with a very low calorie diet; and a report on encouraging findings with an experimental drug for Graves eye disease.
REPORTING FROM AACE 2019
Patients describe significant impact of epilepsy on their lives
PHILADELPHIA – said Jacqueline French, MD, a professor at the Comprehensive Epilepsy Center at New York University.
“This underscores the need to consider these experiences, and potentially the stage of disease, when developing patient-reported outcome measures,” she said at the annual meeting of the American Academy of Neurology.
To describe the patient’s experience of living with epilepsy, including the occurrence of disease-related signs and symptoms and impact on daily life at different disease stages, Dr. French conducted qualitative, semistructured interviews with adults with focal epilepsy at the following stages: early (1 year or less since diagnosis), middle (1-5 years since diagnosis), and late (more than 5 years since diagnosis). The patients had varying seizure frequency and treatment experiences. They were asked to describe the symptoms and functional impact they had experienced related to epilepsy, and then to rate the degree to which each symptom and impact “bothered” them, using a disturbance rating scale from 0 (not at all) to 10 (extremely).
A total of 62 patients who were aged 18-60 years (mean age, 37 years; 73% female) were interviewed. In all, 19 of the patients had early-stage disease, 17 had middle-stage, and 26 had late-stage disease. Symptoms reported with the highest frequency and highest average disturbance (AD) ratings across all cohorts included twitching/tremors (80% of patients; AD, 5.3), confusion (78%; AD, 7.8), difficulty talking (75%; AD, 8.1), impaired/loss of consciousness (70%; AD, 6.8), stiffening (65%; AD, 5.4), déjà vu (62%; AD, 5.1), difficulty remembering (60%; AD, 8.5), and dizziness/light-headedness (58%; AD, 6.4).
The high-frequency/high-disturbance daily impact of epilepsy included the inability to drive (74%; AD, 7.1), limited ability to work and/or go to school (61%; AD, 6.7), limitations on leisure and social activities (58%; AD, 6.3), and memory loss (47%; AD, 8.4).
Dr French noted that, although disease experiences were similar among the cohorts, some heterogeneity across patient subgroups was observed.
Eisai sponsored the study.
PHILADELPHIA – said Jacqueline French, MD, a professor at the Comprehensive Epilepsy Center at New York University.
“This underscores the need to consider these experiences, and potentially the stage of disease, when developing patient-reported outcome measures,” she said at the annual meeting of the American Academy of Neurology.
To describe the patient’s experience of living with epilepsy, including the occurrence of disease-related signs and symptoms and impact on daily life at different disease stages, Dr. French conducted qualitative, semistructured interviews with adults with focal epilepsy at the following stages: early (1 year or less since diagnosis), middle (1-5 years since diagnosis), and late (more than 5 years since diagnosis). The patients had varying seizure frequency and treatment experiences. They were asked to describe the symptoms and functional impact they had experienced related to epilepsy, and then to rate the degree to which each symptom and impact “bothered” them, using a disturbance rating scale from 0 (not at all) to 10 (extremely).
A total of 62 patients who were aged 18-60 years (mean age, 37 years; 73% female) were interviewed. In all, 19 of the patients had early-stage disease, 17 had middle-stage, and 26 had late-stage disease. Symptoms reported with the highest frequency and highest average disturbance (AD) ratings across all cohorts included twitching/tremors (80% of patients; AD, 5.3), confusion (78%; AD, 7.8), difficulty talking (75%; AD, 8.1), impaired/loss of consciousness (70%; AD, 6.8), stiffening (65%; AD, 5.4), déjà vu (62%; AD, 5.1), difficulty remembering (60%; AD, 8.5), and dizziness/light-headedness (58%; AD, 6.4).
The high-frequency/high-disturbance daily impact of epilepsy included the inability to drive (74%; AD, 7.1), limited ability to work and/or go to school (61%; AD, 6.7), limitations on leisure and social activities (58%; AD, 6.3), and memory loss (47%; AD, 8.4).
Dr French noted that, although disease experiences were similar among the cohorts, some heterogeneity across patient subgroups was observed.
Eisai sponsored the study.
PHILADELPHIA – said Jacqueline French, MD, a professor at the Comprehensive Epilepsy Center at New York University.
“This underscores the need to consider these experiences, and potentially the stage of disease, when developing patient-reported outcome measures,” she said at the annual meeting of the American Academy of Neurology.
To describe the patient’s experience of living with epilepsy, including the occurrence of disease-related signs and symptoms and impact on daily life at different disease stages, Dr. French conducted qualitative, semistructured interviews with adults with focal epilepsy at the following stages: early (1 year or less since diagnosis), middle (1-5 years since diagnosis), and late (more than 5 years since diagnosis). The patients had varying seizure frequency and treatment experiences. They were asked to describe the symptoms and functional impact they had experienced related to epilepsy, and then to rate the degree to which each symptom and impact “bothered” them, using a disturbance rating scale from 0 (not at all) to 10 (extremely).
A total of 62 patients who were aged 18-60 years (mean age, 37 years; 73% female) were interviewed. In all, 19 of the patients had early-stage disease, 17 had middle-stage, and 26 had late-stage disease. Symptoms reported with the highest frequency and highest average disturbance (AD) ratings across all cohorts included twitching/tremors (80% of patients; AD, 5.3), confusion (78%; AD, 7.8), difficulty talking (75%; AD, 8.1), impaired/loss of consciousness (70%; AD, 6.8), stiffening (65%; AD, 5.4), déjà vu (62%; AD, 5.1), difficulty remembering (60%; AD, 8.5), and dizziness/light-headedness (58%; AD, 6.4).
The high-frequency/high-disturbance daily impact of epilepsy included the inability to drive (74%; AD, 7.1), limited ability to work and/or go to school (61%; AD, 6.7), limitations on leisure and social activities (58%; AD, 6.3), and memory loss (47%; AD, 8.4).
Dr French noted that, although disease experiences were similar among the cohorts, some heterogeneity across patient subgroups was observed.
Eisai sponsored the study.
REPORTING FROM AAN 2019
Key clinical point: Adults with focal epilepsy report a range of high-disturbance symptoms and impacts on daily life.
Major finding: The high-frequency/high-disturbance daily impact of epilepsy included the inability to drive (reported by 74% of respondents), limited ability to work and/or go to school (61%), limitations on leisure and social activities (58%), and memory loss (47%).
Study details: Qualitative, semistructured interviews with 62 adults with focal epilepsy at different stages of illness: early, middle, and late.
Disclosures: Eisai sponsored the study.
Physical activity slows cognitive decline in patients with Parkinson’s disease
PHILADELPHIA – according to Sneha Mantri, MD, of Duke University in Durham, N.C., and colleagues, who presented the results of their study at the annual meeting of the American Academy of Neurology.
Physical activity is an important component of the management of Parkinson’s disease and is shown to mitigate cognitive decline among patients with moderate disease, said Dr. Mantri and colleagues. “Exercise levels in de novo and early disease may influence risk of future cognitive decline; early disease also presents an opportunity for early intervention and possible disease modification,” Dr. Mantri said.
Physical activity levels in early disease are known to be low, but the effects of activity on cognition are currently unclear. To assess the relationship between physical activity and cognition, Dr. Mantri and colleagues examined patients with Parkinson’s disease who were enrolled in the prospective Parkinson’s Progression Markers Initiative (PPMI) cohort. At annual study visits, participants completed the Physical Activity Scale for the Elderly (PASE), a validated self-reported questionnaire assessing household, leisure, and work activities over the previous 7 days. The researchers used a linear mixed-effects model to compare rates of change in the Montreal Cognitive Assessment (MoCA) according to PASE scores; covariates included age, sex, Unified Parkinson’s Disease Rating Scale (UPDRS) part III score, and baseline MoCA.
A total of 379 patients completed at least one PASE questionnaire over the course of the study. PASE scores in this cohort have been previously described (Mantri S et al. J Park Dis. 2018;8[1]:107-11). Although overall rates of cognitive decline are known to be modest in this early cohort, PASE over time has a significant effect on MoCA during follow-up (P = 0.02) which suggest that higher levels of activity throughout disease are associated with better cognitive performance.
Dr. Mantri had nothing to disclose. Among her coauthors, Dr. Tropea received personal compensation from Genzyme and Medtronics and research support from Sanofi. Dr. Morley had nothing to disclose.
SOURCE: Mantri S et al. AAN 2019, Abstract P2.8-021.
PHILADELPHIA – according to Sneha Mantri, MD, of Duke University in Durham, N.C., and colleagues, who presented the results of their study at the annual meeting of the American Academy of Neurology.
Physical activity is an important component of the management of Parkinson’s disease and is shown to mitigate cognitive decline among patients with moderate disease, said Dr. Mantri and colleagues. “Exercise levels in de novo and early disease may influence risk of future cognitive decline; early disease also presents an opportunity for early intervention and possible disease modification,” Dr. Mantri said.
Physical activity levels in early disease are known to be low, but the effects of activity on cognition are currently unclear. To assess the relationship between physical activity and cognition, Dr. Mantri and colleagues examined patients with Parkinson’s disease who were enrolled in the prospective Parkinson’s Progression Markers Initiative (PPMI) cohort. At annual study visits, participants completed the Physical Activity Scale for the Elderly (PASE), a validated self-reported questionnaire assessing household, leisure, and work activities over the previous 7 days. The researchers used a linear mixed-effects model to compare rates of change in the Montreal Cognitive Assessment (MoCA) according to PASE scores; covariates included age, sex, Unified Parkinson’s Disease Rating Scale (UPDRS) part III score, and baseline MoCA.
A total of 379 patients completed at least one PASE questionnaire over the course of the study. PASE scores in this cohort have been previously described (Mantri S et al. J Park Dis. 2018;8[1]:107-11). Although overall rates of cognitive decline are known to be modest in this early cohort, PASE over time has a significant effect on MoCA during follow-up (P = 0.02) which suggest that higher levels of activity throughout disease are associated with better cognitive performance.
Dr. Mantri had nothing to disclose. Among her coauthors, Dr. Tropea received personal compensation from Genzyme and Medtronics and research support from Sanofi. Dr. Morley had nothing to disclose.
SOURCE: Mantri S et al. AAN 2019, Abstract P2.8-021.
PHILADELPHIA – according to Sneha Mantri, MD, of Duke University in Durham, N.C., and colleagues, who presented the results of their study at the annual meeting of the American Academy of Neurology.
Physical activity is an important component of the management of Parkinson’s disease and is shown to mitigate cognitive decline among patients with moderate disease, said Dr. Mantri and colleagues. “Exercise levels in de novo and early disease may influence risk of future cognitive decline; early disease also presents an opportunity for early intervention and possible disease modification,” Dr. Mantri said.
Physical activity levels in early disease are known to be low, but the effects of activity on cognition are currently unclear. To assess the relationship between physical activity and cognition, Dr. Mantri and colleagues examined patients with Parkinson’s disease who were enrolled in the prospective Parkinson’s Progression Markers Initiative (PPMI) cohort. At annual study visits, participants completed the Physical Activity Scale for the Elderly (PASE), a validated self-reported questionnaire assessing household, leisure, and work activities over the previous 7 days. The researchers used a linear mixed-effects model to compare rates of change in the Montreal Cognitive Assessment (MoCA) according to PASE scores; covariates included age, sex, Unified Parkinson’s Disease Rating Scale (UPDRS) part III score, and baseline MoCA.
A total of 379 patients completed at least one PASE questionnaire over the course of the study. PASE scores in this cohort have been previously described (Mantri S et al. J Park Dis. 2018;8[1]:107-11). Although overall rates of cognitive decline are known to be modest in this early cohort, PASE over time has a significant effect on MoCA during follow-up (P = 0.02) which suggest that higher levels of activity throughout disease are associated with better cognitive performance.
Dr. Mantri had nothing to disclose. Among her coauthors, Dr. Tropea received personal compensation from Genzyme and Medtronics and research support from Sanofi. Dr. Morley had nothing to disclose.
SOURCE: Mantri S et al. AAN 2019, Abstract P2.8-021.
REPORTING FROM AAN 2019
Key clinical point: Physical activity is associated with slower cognitive decline in patients with de novo Parkinson’s disease.
Major finding: Higher scores on the Physical Activity Scale for the Elderly over time had a significant effect on cognitive function.
Study details: A prospective study of 379 patients enrolled in the Parkinson’s Progression Markers Initiative.
Disclosures: Dr. Mantri had no relevant financial disclosures. Among her coauthors, Dr. Tropea received personal compensation from Genzyme and Medtronics and research support from Sanofi. Dr. Morley had nothing to disclose.
Source: Mantri S et al. AAN 2019, Abstract P2.8-021.