User login
Questions about optimal dosing of isotretinoin persist, expert says
Although the to this day, according to Diane M. Thiboutot, MD.
These include, what is the ideal daily dose of isotretinoin? What is the ideal cumulative dose of isotretinoin to minimize relapse of acne? What is the ideal duration of isotretinoin therapy? How do you define relapse?
“Initially, it was recommended as 1–mg/kg per day dosing,” Dr. Thiboutot, professor of dermatology at Penn State University, Hershey, said during the Orlando Dermatology Aesthetic and Clinical Conference. “As time went on and we became familiar with flares that some patients can have on that dose, it was recommended to start treatment at a dose of 0.5 mg/kg per day. Then there were trends for low dosing, intermittent dosing, and some of the more recent medical literature is talking about high dosing.”
Clinical studies
A multicenter study of 150 patients published in 1984 found that rates of relapse (retreatment needed) were 42% of patients of patients treated with 0.1 mg/kg daily, 20% in patients treated with 0.5 mg/kg daily, and 10% in patients treated with 1.0 mg/kg daily.
In a later study, researchers who followed 299 patients for 5 years post isotretinoin treatment found that there were more relapses in the 0.5-mg/kg group versus those treated with 1.0 mg/kg. Factors that contributed to the need for more treatment courses included lower-dose regimens (0.1 mg/kg and 0.5 mg/kg), having severe acne, being a female over the age of 25 at the onset of therapy, and having a prolonged history of acne.
More recently, investigators who conducted a single-center study of 1,453 patients treated with isotretinoin defined relapse as the need for a second course of isotretinoin. “They found that neither daily nor cumulative dosages influenced relapse of acne vulgaris in patients treated with varying doses of isotretinoin as long as treatment was continued for 2 or more months after the acne had completely resolved,” said Dr. Thiboutot, a past president of the American Acne and Rosacea Society.
“The current evidence underpinning the 120-150 mg/kg cumulative threshold–dosing regimen is equivocal and is based on two low-grade studies,” she noted. “Cumulative doses required for clearance appear lower for acne of mild to moderate severity and higher for more severe acne. Future investigations should use clinically relevant endpoints as end of treatment criteria and define treatment success in acne accurately.”
Other studies have looked at whether higher doses of isotretinoin could reduce treatment failures in patients with acne, Dr. Thiboutot said. In a retrospective chart review of 102 patients with acne who had been treated with isotretinoin for at least 4 consecutive months and followed for over a year, 45.1% required further treatment and 15.7% received a second course of isotretinoin. Cumulative dose (mg/kg), follow-up period, duration of treatment, and daily dose during the last month of treatment were not significantly different between those who relapsed and those who did not relapse.
However, “while the cumulative dose of isotretinoin did not significantly impact acne relapse, patients who received a higher cumulative dose were less likely to require a second course of treatment,” the authors wrote, adding that “female patients had a higher risk of needing retrial regardless of their cumulative dose.” They commented that “prescribing a higher dose per weight may result in less severe acne recurrences and the need for further isotretinoin therapy.”
Another study evaluated 116 patients who were treated to clearance with dosing at the discretion of the provider and defined relapse as subsequent treatment with an oral or topical agent. In the lower-dose treatment (less than 220 mg/kg; mean of 170 mg/kg) group, the relapse rate was 47.4%, compared with 26.9% in the higher-dose (greater than 220 mg/kg) group (P = .03). Cheilitis and xerosis during treatment was reported in nearly all patients in both treatment groups, but retinoid dermatitis was significantly more common among those in the higher-dose group (53.8% vs. 31.6%; P = .02). There were no significant differences in other adverse events between the two groups.
According to Dr. Thiboutot, variables to consider in selection of a daily dose include the presence of intense inflammation, cysts, nodules, potential difference in side-effect profiles with ethnicity, and an individual’s degree of side effects and their level of comfort. “What are some of the concerns with higher doses? Those of us who have treated a lot of acne patients have had the unfortunate occurrence where you start someone on isotretinoin and their acne explodes, as do their cysts and nodules. Once that happens it’s a bad situation and it takes you a while to get past it.”
Acne fulminans
Dr. Thiboutot was part of a panel of experts who assembled guidelines on the classification, management, and prevention of acne fulminans, published in 2017. “Acne fulminans can be induced by isotretinoin or it can occur on its own. If you have someone who has a lot of inflammation, a lot of cysts and nodules, it’s probably best to start them on a lower dose with or without prednisone,” she said.
Age at treatment is another variable that can affect the duration of response to isotretinoin. “If the patient is very young when they need isotretinoin, it’s highly likely that they will need it again,” Dr. Thiboutot said. “Also, adult females often need a repeat dose of isotretinoin. The cumulative dose is important, and the presence of truncal acne is a factor affecting duration of response. Truncal acne takes longer to clear, and it oftentimes needs a longer treatment course.”
Data from the iPledge database indicate that 37% of 10- to 11-year-olds needed a repeat course of isotretinoin, “and as you get older, the need for retreatment is less,” she said.
High-dose versus low-dose isotretinoin
A slow, low-dose approach to the use of isotretinoin in practice can minimize side effects and cystic flares, according to Dr. Thiboutot. “The cons are that you could have a longer treatment duration, you might need more patient visits, and it creates more prolonged drug exposure in patients who can become pregnant,” she said.
“The pros of a high-dose strategy include a shorter treatment duration and potential costs savings. The cons are that there is an increased risk of side effects and a risk of cystic flare. It seems that the general agreement is to treat until clearance and then treat for another 2 months. A clear definition of acne relapse is needed as well as prospective studies to optimize dosing.”
Dr. Thiboutot disclosed that she is a consultant Galderma and Novartis. She has also performed clinical trials for Galderma, Cassiopea, and Foamix.
Commentary by Robert Sidbury, MD, MPH
Isotretinoin has been around for a long time – 40-plus years, to be exact. Despite this cumulative experience, ideal dosing and duration remain uncertain. Many providers have evolved from a “one size fits all” approach (for example, 1 mg/kg of body weight per day for 4-6 months) to a more tailored and nuanced strategy. Dr. Thiboutot validates the need to individualize therapy and helps identify patients at higher risk for relapse. Younger patients are at greater risk for repeat courses of isotretinoin – Dr. Thiboutot cites a study showing 37% of 10- to 11-year-olds required a second course of isotretinoin. This could simply be a proxy for severity, which also augurs a more protracted course. Adult women and those with truncal acne also trend toward longer courses. Knowing these risk factors will help practitioners counsel proper expectations, tailor treatment courses, and thread the always challenging isotretinoin needle: Should one dose “low and slow” and court a longer risk window, or higher and faster, sometimes leading to a dryer disaster?
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
This article was updated 6/10/22.
Although the to this day, according to Diane M. Thiboutot, MD.
These include, what is the ideal daily dose of isotretinoin? What is the ideal cumulative dose of isotretinoin to minimize relapse of acne? What is the ideal duration of isotretinoin therapy? How do you define relapse?
“Initially, it was recommended as 1–mg/kg per day dosing,” Dr. Thiboutot, professor of dermatology at Penn State University, Hershey, said during the Orlando Dermatology Aesthetic and Clinical Conference. “As time went on and we became familiar with flares that some patients can have on that dose, it was recommended to start treatment at a dose of 0.5 mg/kg per day. Then there were trends for low dosing, intermittent dosing, and some of the more recent medical literature is talking about high dosing.”
Clinical studies
A multicenter study of 150 patients published in 1984 found that rates of relapse (retreatment needed) were 42% of patients of patients treated with 0.1 mg/kg daily, 20% in patients treated with 0.5 mg/kg daily, and 10% in patients treated with 1.0 mg/kg daily.
In a later study, researchers who followed 299 patients for 5 years post isotretinoin treatment found that there were more relapses in the 0.5-mg/kg group versus those treated with 1.0 mg/kg. Factors that contributed to the need for more treatment courses included lower-dose regimens (0.1 mg/kg and 0.5 mg/kg), having severe acne, being a female over the age of 25 at the onset of therapy, and having a prolonged history of acne.
More recently, investigators who conducted a single-center study of 1,453 patients treated with isotretinoin defined relapse as the need for a second course of isotretinoin. “They found that neither daily nor cumulative dosages influenced relapse of acne vulgaris in patients treated with varying doses of isotretinoin as long as treatment was continued for 2 or more months after the acne had completely resolved,” said Dr. Thiboutot, a past president of the American Acne and Rosacea Society.
“The current evidence underpinning the 120-150 mg/kg cumulative threshold–dosing regimen is equivocal and is based on two low-grade studies,” she noted. “Cumulative doses required for clearance appear lower for acne of mild to moderate severity and higher for more severe acne. Future investigations should use clinically relevant endpoints as end of treatment criteria and define treatment success in acne accurately.”
Other studies have looked at whether higher doses of isotretinoin could reduce treatment failures in patients with acne, Dr. Thiboutot said. In a retrospective chart review of 102 patients with acne who had been treated with isotretinoin for at least 4 consecutive months and followed for over a year, 45.1% required further treatment and 15.7% received a second course of isotretinoin. Cumulative dose (mg/kg), follow-up period, duration of treatment, and daily dose during the last month of treatment were not significantly different between those who relapsed and those who did not relapse.
However, “while the cumulative dose of isotretinoin did not significantly impact acne relapse, patients who received a higher cumulative dose were less likely to require a second course of treatment,” the authors wrote, adding that “female patients had a higher risk of needing retrial regardless of their cumulative dose.” They commented that “prescribing a higher dose per weight may result in less severe acne recurrences and the need for further isotretinoin therapy.”
Another study evaluated 116 patients who were treated to clearance with dosing at the discretion of the provider and defined relapse as subsequent treatment with an oral or topical agent. In the lower-dose treatment (less than 220 mg/kg; mean of 170 mg/kg) group, the relapse rate was 47.4%, compared with 26.9% in the higher-dose (greater than 220 mg/kg) group (P = .03). Cheilitis and xerosis during treatment was reported in nearly all patients in both treatment groups, but retinoid dermatitis was significantly more common among those in the higher-dose group (53.8% vs. 31.6%; P = .02). There were no significant differences in other adverse events between the two groups.
According to Dr. Thiboutot, variables to consider in selection of a daily dose include the presence of intense inflammation, cysts, nodules, potential difference in side-effect profiles with ethnicity, and an individual’s degree of side effects and their level of comfort. “What are some of the concerns with higher doses? Those of us who have treated a lot of acne patients have had the unfortunate occurrence where you start someone on isotretinoin and their acne explodes, as do their cysts and nodules. Once that happens it’s a bad situation and it takes you a while to get past it.”
Acne fulminans
Dr. Thiboutot was part of a panel of experts who assembled guidelines on the classification, management, and prevention of acne fulminans, published in 2017. “Acne fulminans can be induced by isotretinoin or it can occur on its own. If you have someone who has a lot of inflammation, a lot of cysts and nodules, it’s probably best to start them on a lower dose with or without prednisone,” she said.
Age at treatment is another variable that can affect the duration of response to isotretinoin. “If the patient is very young when they need isotretinoin, it’s highly likely that they will need it again,” Dr. Thiboutot said. “Also, adult females often need a repeat dose of isotretinoin. The cumulative dose is important, and the presence of truncal acne is a factor affecting duration of response. Truncal acne takes longer to clear, and it oftentimes needs a longer treatment course.”
Data from the iPledge database indicate that 37% of 10- to 11-year-olds needed a repeat course of isotretinoin, “and as you get older, the need for retreatment is less,” she said.
High-dose versus low-dose isotretinoin
A slow, low-dose approach to the use of isotretinoin in practice can minimize side effects and cystic flares, according to Dr. Thiboutot. “The cons are that you could have a longer treatment duration, you might need more patient visits, and it creates more prolonged drug exposure in patients who can become pregnant,” she said.
“The pros of a high-dose strategy include a shorter treatment duration and potential costs savings. The cons are that there is an increased risk of side effects and a risk of cystic flare. It seems that the general agreement is to treat until clearance and then treat for another 2 months. A clear definition of acne relapse is needed as well as prospective studies to optimize dosing.”
Dr. Thiboutot disclosed that she is a consultant Galderma and Novartis. She has also performed clinical trials for Galderma, Cassiopea, and Foamix.
Commentary by Robert Sidbury, MD, MPH
Isotretinoin has been around for a long time – 40-plus years, to be exact. Despite this cumulative experience, ideal dosing and duration remain uncertain. Many providers have evolved from a “one size fits all” approach (for example, 1 mg/kg of body weight per day for 4-6 months) to a more tailored and nuanced strategy. Dr. Thiboutot validates the need to individualize therapy and helps identify patients at higher risk for relapse. Younger patients are at greater risk for repeat courses of isotretinoin – Dr. Thiboutot cites a study showing 37% of 10- to 11-year-olds required a second course of isotretinoin. This could simply be a proxy for severity, which also augurs a more protracted course. Adult women and those with truncal acne also trend toward longer courses. Knowing these risk factors will help practitioners counsel proper expectations, tailor treatment courses, and thread the always challenging isotretinoin needle: Should one dose “low and slow” and court a longer risk window, or higher and faster, sometimes leading to a dryer disaster?
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
This article was updated 6/10/22.
Although the to this day, according to Diane M. Thiboutot, MD.
These include, what is the ideal daily dose of isotretinoin? What is the ideal cumulative dose of isotretinoin to minimize relapse of acne? What is the ideal duration of isotretinoin therapy? How do you define relapse?
“Initially, it was recommended as 1–mg/kg per day dosing,” Dr. Thiboutot, professor of dermatology at Penn State University, Hershey, said during the Orlando Dermatology Aesthetic and Clinical Conference. “As time went on and we became familiar with flares that some patients can have on that dose, it was recommended to start treatment at a dose of 0.5 mg/kg per day. Then there were trends for low dosing, intermittent dosing, and some of the more recent medical literature is talking about high dosing.”
Clinical studies
A multicenter study of 150 patients published in 1984 found that rates of relapse (retreatment needed) were 42% of patients of patients treated with 0.1 mg/kg daily, 20% in patients treated with 0.5 mg/kg daily, and 10% in patients treated with 1.0 mg/kg daily.
In a later study, researchers who followed 299 patients for 5 years post isotretinoin treatment found that there were more relapses in the 0.5-mg/kg group versus those treated with 1.0 mg/kg. Factors that contributed to the need for more treatment courses included lower-dose regimens (0.1 mg/kg and 0.5 mg/kg), having severe acne, being a female over the age of 25 at the onset of therapy, and having a prolonged history of acne.
More recently, investigators who conducted a single-center study of 1,453 patients treated with isotretinoin defined relapse as the need for a second course of isotretinoin. “They found that neither daily nor cumulative dosages influenced relapse of acne vulgaris in patients treated with varying doses of isotretinoin as long as treatment was continued for 2 or more months after the acne had completely resolved,” said Dr. Thiboutot, a past president of the American Acne and Rosacea Society.
“The current evidence underpinning the 120-150 mg/kg cumulative threshold–dosing regimen is equivocal and is based on two low-grade studies,” she noted. “Cumulative doses required for clearance appear lower for acne of mild to moderate severity and higher for more severe acne. Future investigations should use clinically relevant endpoints as end of treatment criteria and define treatment success in acne accurately.”
Other studies have looked at whether higher doses of isotretinoin could reduce treatment failures in patients with acne, Dr. Thiboutot said. In a retrospective chart review of 102 patients with acne who had been treated with isotretinoin for at least 4 consecutive months and followed for over a year, 45.1% required further treatment and 15.7% received a second course of isotretinoin. Cumulative dose (mg/kg), follow-up period, duration of treatment, and daily dose during the last month of treatment were not significantly different between those who relapsed and those who did not relapse.
However, “while the cumulative dose of isotretinoin did not significantly impact acne relapse, patients who received a higher cumulative dose were less likely to require a second course of treatment,” the authors wrote, adding that “female patients had a higher risk of needing retrial regardless of their cumulative dose.” They commented that “prescribing a higher dose per weight may result in less severe acne recurrences and the need for further isotretinoin therapy.”
Another study evaluated 116 patients who were treated to clearance with dosing at the discretion of the provider and defined relapse as subsequent treatment with an oral or topical agent. In the lower-dose treatment (less than 220 mg/kg; mean of 170 mg/kg) group, the relapse rate was 47.4%, compared with 26.9% in the higher-dose (greater than 220 mg/kg) group (P = .03). Cheilitis and xerosis during treatment was reported in nearly all patients in both treatment groups, but retinoid dermatitis was significantly more common among those in the higher-dose group (53.8% vs. 31.6%; P = .02). There were no significant differences in other adverse events between the two groups.
According to Dr. Thiboutot, variables to consider in selection of a daily dose include the presence of intense inflammation, cysts, nodules, potential difference in side-effect profiles with ethnicity, and an individual’s degree of side effects and their level of comfort. “What are some of the concerns with higher doses? Those of us who have treated a lot of acne patients have had the unfortunate occurrence where you start someone on isotretinoin and their acne explodes, as do their cysts and nodules. Once that happens it’s a bad situation and it takes you a while to get past it.”
Acne fulminans
Dr. Thiboutot was part of a panel of experts who assembled guidelines on the classification, management, and prevention of acne fulminans, published in 2017. “Acne fulminans can be induced by isotretinoin or it can occur on its own. If you have someone who has a lot of inflammation, a lot of cysts and nodules, it’s probably best to start them on a lower dose with or without prednisone,” she said.
Age at treatment is another variable that can affect the duration of response to isotretinoin. “If the patient is very young when they need isotretinoin, it’s highly likely that they will need it again,” Dr. Thiboutot said. “Also, adult females often need a repeat dose of isotretinoin. The cumulative dose is important, and the presence of truncal acne is a factor affecting duration of response. Truncal acne takes longer to clear, and it oftentimes needs a longer treatment course.”
Data from the iPledge database indicate that 37% of 10- to 11-year-olds needed a repeat course of isotretinoin, “and as you get older, the need for retreatment is less,” she said.
High-dose versus low-dose isotretinoin
A slow, low-dose approach to the use of isotretinoin in practice can minimize side effects and cystic flares, according to Dr. Thiboutot. “The cons are that you could have a longer treatment duration, you might need more patient visits, and it creates more prolonged drug exposure in patients who can become pregnant,” she said.
“The pros of a high-dose strategy include a shorter treatment duration and potential costs savings. The cons are that there is an increased risk of side effects and a risk of cystic flare. It seems that the general agreement is to treat until clearance and then treat for another 2 months. A clear definition of acne relapse is needed as well as prospective studies to optimize dosing.”
Dr. Thiboutot disclosed that she is a consultant Galderma and Novartis. She has also performed clinical trials for Galderma, Cassiopea, and Foamix.
Commentary by Robert Sidbury, MD, MPH
Isotretinoin has been around for a long time – 40-plus years, to be exact. Despite this cumulative experience, ideal dosing and duration remain uncertain. Many providers have evolved from a “one size fits all” approach (for example, 1 mg/kg of body weight per day for 4-6 months) to a more tailored and nuanced strategy. Dr. Thiboutot validates the need to individualize therapy and helps identify patients at higher risk for relapse. Younger patients are at greater risk for repeat courses of isotretinoin – Dr. Thiboutot cites a study showing 37% of 10- to 11-year-olds required a second course of isotretinoin. This could simply be a proxy for severity, which also augurs a more protracted course. Adult women and those with truncal acne also trend toward longer courses. Knowing these risk factors will help practitioners counsel proper expectations, tailor treatment courses, and thread the always challenging isotretinoin needle: Should one dose “low and slow” and court a longer risk window, or higher and faster, sometimes leading to a dryer disaster?
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
This article was updated 6/10/22.
FROM ODAC 2022
A test for cannabis-caused impairment
You have a 16-year-old patient who has been doing poorly in school. He has withdrawn from his social group and quit the sports in which he excelled. He admits to using marijuana “maybe once or twice a week.” But you and his parents suspect that it is much more often and contributing to the change in his behavior and school performance.
They would prefer he not use marijuana at all but could maybe be comfortable with some arrangement in which their son could demonstrate that his usage was indeed limited to once or twice on the weekends. They ask for your help with crafting a contract that might include “some urine or blood test” that would allow them to be sure their son was adhering to the contract.
You explain to them that there are hazards associated with setting up contracts such as the one they are proposing. One revolving around the issue of trust. Another being that he may be addicted to the point that a compromise that includes scaling back his usage is unlikely to succeed. And, finally, you tell them that because of marijuana’s pharmacokinetics, their son’s urine tests will always be positive and not reflective of the how much he is using or whether he is intoxicated.
Scenarios similar to this are increasingly common for those of us living in states that have legalized recreational cannabis use. The absence of a laboratory test that can determine when a person is impaired by marijuana has made life difficult for law enforcement officers accustomed to relying on breath and blood tests for alcohol to confirm their suspicion that a driver is under the influence.
In addition, because marijuana is still detectable days after it is used, many well-paying jobs go unfilled when potential applicants are hesitant to submit to a required drug test. The quirky pharmacokinetics of cannabis are well-known to the recreational users and they see no reason to risk failing a urine test regardless of how good the job may be.
This lack of a reliable indicator of cannabis intoxication has not gone unnoticed, and in a recent study published in the journal Neuropharmacology, researchers at Massachusetts General Hospital in Boston report some hopeful results using fNIRS brain scanning. The investigators observed an increase in the level of oxygenated hemoglobin concentration (HbO), which is a type of neural activity signature, in the prefrontal cortex region of the volunteers who reported being impaired.
While a brain scan may sound like an unwieldy tool to use on roadside sobriety stops, the researchers report that portable scanners – some using skull cap sensors – could be easily adapted for use by law enforcement in the field. This technology also could be used by employers on the job site to test truck drivers and heavy machine operators at the beginning of each shift, thereby allaying the fears of responsible cannabis users.
This technology might be helpful to you in advising the parents of the 16-year-old you suspect of heavy usage. It would certainly help in confirming the suspicion that he is using more often than he claims. However, the contract the parents propose still may not work. If this young man demonstrates on multiple attempts that his word can’t be trusted, technology isn’t going to be the answer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
You have a 16-year-old patient who has been doing poorly in school. He has withdrawn from his social group and quit the sports in which he excelled. He admits to using marijuana “maybe once or twice a week.” But you and his parents suspect that it is much more often and contributing to the change in his behavior and school performance.
They would prefer he not use marijuana at all but could maybe be comfortable with some arrangement in which their son could demonstrate that his usage was indeed limited to once or twice on the weekends. They ask for your help with crafting a contract that might include “some urine or blood test” that would allow them to be sure their son was adhering to the contract.
You explain to them that there are hazards associated with setting up contracts such as the one they are proposing. One revolving around the issue of trust. Another being that he may be addicted to the point that a compromise that includes scaling back his usage is unlikely to succeed. And, finally, you tell them that because of marijuana’s pharmacokinetics, their son’s urine tests will always be positive and not reflective of the how much he is using or whether he is intoxicated.
Scenarios similar to this are increasingly common for those of us living in states that have legalized recreational cannabis use. The absence of a laboratory test that can determine when a person is impaired by marijuana has made life difficult for law enforcement officers accustomed to relying on breath and blood tests for alcohol to confirm their suspicion that a driver is under the influence.
In addition, because marijuana is still detectable days after it is used, many well-paying jobs go unfilled when potential applicants are hesitant to submit to a required drug test. The quirky pharmacokinetics of cannabis are well-known to the recreational users and they see no reason to risk failing a urine test regardless of how good the job may be.
This lack of a reliable indicator of cannabis intoxication has not gone unnoticed, and in a recent study published in the journal Neuropharmacology, researchers at Massachusetts General Hospital in Boston report some hopeful results using fNIRS brain scanning. The investigators observed an increase in the level of oxygenated hemoglobin concentration (HbO), which is a type of neural activity signature, in the prefrontal cortex region of the volunteers who reported being impaired.
While a brain scan may sound like an unwieldy tool to use on roadside sobriety stops, the researchers report that portable scanners – some using skull cap sensors – could be easily adapted for use by law enforcement in the field. This technology also could be used by employers on the job site to test truck drivers and heavy machine operators at the beginning of each shift, thereby allaying the fears of responsible cannabis users.
This technology might be helpful to you in advising the parents of the 16-year-old you suspect of heavy usage. It would certainly help in confirming the suspicion that he is using more often than he claims. However, the contract the parents propose still may not work. If this young man demonstrates on multiple attempts that his word can’t be trusted, technology isn’t going to be the answer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
You have a 16-year-old patient who has been doing poorly in school. He has withdrawn from his social group and quit the sports in which he excelled. He admits to using marijuana “maybe once or twice a week.” But you and his parents suspect that it is much more often and contributing to the change in his behavior and school performance.
They would prefer he not use marijuana at all but could maybe be comfortable with some arrangement in which their son could demonstrate that his usage was indeed limited to once or twice on the weekends. They ask for your help with crafting a contract that might include “some urine or blood test” that would allow them to be sure their son was adhering to the contract.
You explain to them that there are hazards associated with setting up contracts such as the one they are proposing. One revolving around the issue of trust. Another being that he may be addicted to the point that a compromise that includes scaling back his usage is unlikely to succeed. And, finally, you tell them that because of marijuana’s pharmacokinetics, their son’s urine tests will always be positive and not reflective of the how much he is using or whether he is intoxicated.
Scenarios similar to this are increasingly common for those of us living in states that have legalized recreational cannabis use. The absence of a laboratory test that can determine when a person is impaired by marijuana has made life difficult for law enforcement officers accustomed to relying on breath and blood tests for alcohol to confirm their suspicion that a driver is under the influence.
In addition, because marijuana is still detectable days after it is used, many well-paying jobs go unfilled when potential applicants are hesitant to submit to a required drug test. The quirky pharmacokinetics of cannabis are well-known to the recreational users and they see no reason to risk failing a urine test regardless of how good the job may be.
This lack of a reliable indicator of cannabis intoxication has not gone unnoticed, and in a recent study published in the journal Neuropharmacology, researchers at Massachusetts General Hospital in Boston report some hopeful results using fNIRS brain scanning. The investigators observed an increase in the level of oxygenated hemoglobin concentration (HbO), which is a type of neural activity signature, in the prefrontal cortex region of the volunteers who reported being impaired.
While a brain scan may sound like an unwieldy tool to use on roadside sobriety stops, the researchers report that portable scanners – some using skull cap sensors – could be easily adapted for use by law enforcement in the field. This technology also could be used by employers on the job site to test truck drivers and heavy machine operators at the beginning of each shift, thereby allaying the fears of responsible cannabis users.
This technology might be helpful to you in advising the parents of the 16-year-old you suspect of heavy usage. It would certainly help in confirming the suspicion that he is using more often than he claims. However, the contract the parents propose still may not work. If this young man demonstrates on multiple attempts that his word can’t be trusted, technology isn’t going to be the answer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
‘We just have to keep them alive’: Transitioning youth with type 1 diabetes
“No one has asked young people what they want,” said Tabitha Randell, MBChB, an endocrinologist with Nottingham (England) University Hospitals NHS Trust, who specializes in treating teenagers with type 1 diabetes as they transition to adult care.
Dr. Randell, who has set up a very successful specialist service in her hospital for such patients, said: “We consistently have the best, or the second best, outcomes in this country for our diabetes patients.” She believes this is one of the most important issues in modern endocrinology today.
Speaking at the Diabetes Professional Care conference in London at the end of 2021, and sharing her thoughts afterward with this news organization, she noted that in general there are “virtually no published outcomes” on how best to transition a patient with type 1 diabetes from pediatric to adult care.
“If you actually get them to transition – because some just drop out and disengage and there’s nothing you can do – none of them get lost. Some of them disengage in the adult clinic, but if you’re in the young diabetes service [in England] the rules are that if you miss a diabetes appointment you do not get discharged, as compared with the adult clinic, where if you miss an appointment, you are discharged.”
In the young diabetes clinic, doctors will “carry on trying to contact you, and get you back,” she explained. “And the patients do eventually come back in – it might be a year or 2, but they do come back. We’ve just got to keep them alive in the meantime!”
This issue needs tackling all over the world. Dr. Randell said she’s not aware of any one country – although there may be “pockets” of good care within a given country – that is doing this perfectly.
Across the pond, Grazia Aleppo, MD, division of endocrinology at Northwestern University, Chicago, agreed that transitioning pediatric patients with type 1 diabetes to adult care presents “unique challenges.”
Challenges when transitioning from pediatric to adult care
During childhood, type 1 diabetes management is largely supervised by patients’ parents and members of the pediatric diabetes care team, which may include diabetes educators, psychologists, or social workers, as well as pediatric endocrinologists.
When the patient with type 1 diabetes becomes a young adult and takes over management of their own health, Dr. Aleppo said, the care team may diminish along with the time spent in provider visits.
The adult endocrinology setting focuses more on self-management and autonomous functioning of the individual with diabetes.
Adult appointments are typically shorter, and the patient is usually expected to follow doctors’ suggestions independently, she noted. They are also expected to manage the practical aspects of their diabetes care, including prescriptions, diabetes supplies, laboratory tests, scheduling, and keeping appointments.
At the same time that the emerging adult needs to start asserting independence over their health care, they will also be going through a myriad of other important lifestyle changes, such as attending college, living on their own for the first time, and starting a career.
“With these fundamental differences and challenges, competing priorities, such as college, work and relationships, medical care may become of secondary importance and patients may become disengaged,” Dr. Aleppo explained.
As Dr. Randell has said, loss to follow-up is a big problem with this patient population, with disengagement from specialist services and worsening A1c across the transition, Dr. Aleppo noted. This makes addressing these patients’ specific needs extremely important.
Engage with kid, not disease; don’t palm them off on new recruits
“The really key thing these kids say is, ‘I do not want to be a disease,’” Dr. Randell said. “They want you to know that they are a person. Engage these kids!” she suggested. “Ask them: ‘How is your exam revision going?’ Find something positive to say, even if it’s just: ‘I’m glad you came today.’ ”
“If the first thing that you do is tell them off [for poor diabetes care], you are never going to see them again,” she cautioned.
Dr. Randell also said that role models with type 1 diabetes, such as Lila Moss – daughter of British supermodel Kate Moss – who was recently pictured wearing an insulin pump on her leg on the catwalk, are helping youngsters not feel so self-conscious about their diabetes.
“Let them know it’s not the end of the world, having [type 1] diabetes,” she emphasized.
And Partha Kar, MBBS, OBE, national specialty advisor, diabetes with NHS England, agreed wholeheartedly with Dr. Randall.
Reminiscing about his early days as a newly qualified endocrinologist, Dr. Kar, who works at Portsmouth (England) Hospital NHS Trust, noted that as a new member of staff he was given the youth with type 1 diabetes – those getting ready to transition to adult care – to look after.
But this is the exact opposite of what should be happening, he emphasized. “If you don’t think transition care is important, you shouldn’t be treating type 1 diabetes.”
He believes that every diabetes center “must have a young-adult team lead” and this job must not be given to the least experienced member of staff.
This lead “doesn’t need to be a doctor,” Dr. Kar stressed. “It can be a psychologist, or a diabetes nurse, or a pharmacist, or a dietician.”
In short, it must be someone experienced who loves working with this age group.
Dr. Randell agreed: “Make sure the team is interested in young people. It shouldn’t be the last person in who gets the job no one else wants.” Teens “are my favorite group to work with. They don’t take any nonsense.”
And she explained: “Young people like to get to know the person who’s going to take care of them. So, stay with them for their young adult years.” This can be “quite a fluid period,” with it normally extending to age 25, but in some cases, “it can be up to 32 years old.”
Preparing for the transition
To ease pediatric patients into the transition to adult care, Dr. Aleppo recommended that the pediatric diabetes team provide enough time so that any concerns the patient and their family may have can be addressed.
This should also include transferring management responsibilities to the young adult rather than their parent.
The pediatric provider should discuss with the patient available potential adult colleagues, personalizing these options to their needs, she said.
And the adult and pediatric clinicians should collaborate and provide important information beyond medical records or health summaries.
Adult providers should guide young adults on how to navigate the new practices, from scheduling follow-up appointments to policies regarding medication refills or supplies, to providing information about urgent numbers or email addresses for after-hours communications.
Dr. Kar reiterated that there are too few published outcomes in this patient group to guide the establishment of good transition services.
“Without data, we are dead on the ground. Without data, it’s all conjecture, anecdotes,” he said.
What he does know is that, in the latest national type 1 diabetes audit for England, “Diabetic ketoacidosis admissions ... are up in this age group,” which suggests these patients are not receiving adequate care.
Be a guide, not a gatekeeper
Dr. Kar stressed that, of the 8,760 hours in a year, the average patient with type 1 diabetes in the United Kingdom gets just “1-2 hours with you as a clinician, based on four appointments per year of 30 minutes each.”
“So you spend 0.02% of their time with individuals with type 1 diabetes. So, what’s the one thing you can do with that minimal contact? Be nice!”
Dr. Kar said he always has his email open to his adult patients and they are very respectful of his time. “They don’t email you at 1 a.m. That means every one of my patients has got support [from me]. Don’t be a barrier.”
“We have to fundamentally change the narrative. Doctors must have more empathy,” he said, stating that the one thing adolescents have constantly given feedback on has been, “Why don’t appointments start with: ‘How are you?’
“For a teenager, if you throw type 1 diabetes into the loop, it’s not easy,” he stressed. “Talk to them about something else. As a clinician, be a guide, not a gatekeeper. Give people the tools to self-manage better.”
Adult providers can meet these young adult patients “at their level,” Dr. Aleppo agreed.
“Pay attention to their immediate needs and focus on their present circumstances – whether how to get through their next semester in college, navigating job interviews, or handling having diabetes in the workplace.”
Paying attention to the mental health needs of these young patients is equally “paramount,” Dr. Aleppo said.
While access to mental health professionals may be challenging in the adult setting, providers should bring it up with their patients and offer counseling referrals.
“Diabetes impacts everything, and office appointments and conversations carry weight on these patients’ lives as a whole, not just on their diabetes,” she stressed. “A patient told me recently: ‘We’re learning to be adults,’ which can be hard enough, and with diabetes it can be even more challenging. Adult providers need to be aware of the patient’s ‘diabetes language’ in that often it is not what a patient is saying, rather how they are saying it that gives us information on what they truly need.
“As adult providers, we need to also train and teach our young patients to advocate for themselves on where to find resources that can help them navigate adulthood with diabetes,” she added.
One particularly helpful resource in the United States is the College Diabetes Network, a not-for-profit organization whose mission is to equip young adults with type 1 diabetes to successfully manage the challenging transition to independence at college and beyond.
“The sweetest thing that can happen to us as adult diabetes providers is when a patient – seen as an emerging adult during college – returns to your practice 10 years later after moving back and seeks you out for their diabetes care because of the relationship and trust you developed in those transitioning years,” Dr. Aleppo said.
Another resource is a freely available comic book series cocreated by Dr. Kar and colleague Mayank Patel, MBBS, an endocrinologist from University Hospital Southampton NHS Foundation Trust.
As detailed by this news organization in 2021, the series consists of three volumes: the first, Type 1: Origins, focuses on actual experiences of patients who have type 1 diabetes; the second, Type 1: Attack of the Ketones, is aimed at professionals who may provide care but have limited understanding of type 1 diabetes; and the third, Type 1 Mission 3: S.T.I.G.M.A., addresses the stigmas and misconceptions that patients with type 1 diabetes may face.
The idea for the first comic was inspired by a patient who compared having diabetes to being like the Marvel character The Hulk, said Dr. Kar, and has been expanded to include the additional volumes.
Dr. Kar and Dr. Patel have also just launched the fourth comic in the series, Type 1: Generations, to mark the 100-year anniversary since insulin was first given to a human.
“This is high priority”
Dr. Kar said the NHS in England has just appointed a national lead for type 1 diabetes in youth, Fulya Mehta, MD, of Alder Hey Children’s NHS Foundation Trust, Liverpool, England.
“If you have a plan, bring it to us,” he told the audience at the DPC conference, and “tell us, what is the one thing you would change? This is not a session we are doing just to tick a box. This is high priority.
“Encourage your colleagues to think about transition services. This is an absolute priority. We will be asking every center [in England] who is your transitioning lead?”
And he once again stressed that “a lead of transition service does not have to be a medic. This should be a multidisciplinary team. But they do need to be comfortable in that space. To that teenager, your job title means nothing. Give them time and space.”
Dr. Randell summed it up: “If we can work together, it’s only going to result in better outcomes. We need to blaze the trail for young people.”
Dr. Aleppo has reported serving as a consultant to Dexcom and Insulet and receiving support to Northwestern University from AstraZeneca, Dexcom, Eli Lilly, Fractyl Health, Insulet, and Novo Nordisk. Dr. Randell and Dr. Kar have no conflicts of interest.
A version of this article first appeared on Medscape.com.
“No one has asked young people what they want,” said Tabitha Randell, MBChB, an endocrinologist with Nottingham (England) University Hospitals NHS Trust, who specializes in treating teenagers with type 1 diabetes as they transition to adult care.
Dr. Randell, who has set up a very successful specialist service in her hospital for such patients, said: “We consistently have the best, or the second best, outcomes in this country for our diabetes patients.” She believes this is one of the most important issues in modern endocrinology today.
Speaking at the Diabetes Professional Care conference in London at the end of 2021, and sharing her thoughts afterward with this news organization, she noted that in general there are “virtually no published outcomes” on how best to transition a patient with type 1 diabetes from pediatric to adult care.
“If you actually get them to transition – because some just drop out and disengage and there’s nothing you can do – none of them get lost. Some of them disengage in the adult clinic, but if you’re in the young diabetes service [in England] the rules are that if you miss a diabetes appointment you do not get discharged, as compared with the adult clinic, where if you miss an appointment, you are discharged.”
In the young diabetes clinic, doctors will “carry on trying to contact you, and get you back,” she explained. “And the patients do eventually come back in – it might be a year or 2, but they do come back. We’ve just got to keep them alive in the meantime!”
This issue needs tackling all over the world. Dr. Randell said she’s not aware of any one country – although there may be “pockets” of good care within a given country – that is doing this perfectly.
Across the pond, Grazia Aleppo, MD, division of endocrinology at Northwestern University, Chicago, agreed that transitioning pediatric patients with type 1 diabetes to adult care presents “unique challenges.”
Challenges when transitioning from pediatric to adult care
During childhood, type 1 diabetes management is largely supervised by patients’ parents and members of the pediatric diabetes care team, which may include diabetes educators, psychologists, or social workers, as well as pediatric endocrinologists.
When the patient with type 1 diabetes becomes a young adult and takes over management of their own health, Dr. Aleppo said, the care team may diminish along with the time spent in provider visits.
The adult endocrinology setting focuses more on self-management and autonomous functioning of the individual with diabetes.
Adult appointments are typically shorter, and the patient is usually expected to follow doctors’ suggestions independently, she noted. They are also expected to manage the practical aspects of their diabetes care, including prescriptions, diabetes supplies, laboratory tests, scheduling, and keeping appointments.
At the same time that the emerging adult needs to start asserting independence over their health care, they will also be going through a myriad of other important lifestyle changes, such as attending college, living on their own for the first time, and starting a career.
“With these fundamental differences and challenges, competing priorities, such as college, work and relationships, medical care may become of secondary importance and patients may become disengaged,” Dr. Aleppo explained.
As Dr. Randell has said, loss to follow-up is a big problem with this patient population, with disengagement from specialist services and worsening A1c across the transition, Dr. Aleppo noted. This makes addressing these patients’ specific needs extremely important.
Engage with kid, not disease; don’t palm them off on new recruits
“The really key thing these kids say is, ‘I do not want to be a disease,’” Dr. Randell said. “They want you to know that they are a person. Engage these kids!” she suggested. “Ask them: ‘How is your exam revision going?’ Find something positive to say, even if it’s just: ‘I’m glad you came today.’ ”
“If the first thing that you do is tell them off [for poor diabetes care], you are never going to see them again,” she cautioned.
Dr. Randell also said that role models with type 1 diabetes, such as Lila Moss – daughter of British supermodel Kate Moss – who was recently pictured wearing an insulin pump on her leg on the catwalk, are helping youngsters not feel so self-conscious about their diabetes.
“Let them know it’s not the end of the world, having [type 1] diabetes,” she emphasized.
And Partha Kar, MBBS, OBE, national specialty advisor, diabetes with NHS England, agreed wholeheartedly with Dr. Randall.
Reminiscing about his early days as a newly qualified endocrinologist, Dr. Kar, who works at Portsmouth (England) Hospital NHS Trust, noted that as a new member of staff he was given the youth with type 1 diabetes – those getting ready to transition to adult care – to look after.
But this is the exact opposite of what should be happening, he emphasized. “If you don’t think transition care is important, you shouldn’t be treating type 1 diabetes.”
He believes that every diabetes center “must have a young-adult team lead” and this job must not be given to the least experienced member of staff.
This lead “doesn’t need to be a doctor,” Dr. Kar stressed. “It can be a psychologist, or a diabetes nurse, or a pharmacist, or a dietician.”
In short, it must be someone experienced who loves working with this age group.
Dr. Randell agreed: “Make sure the team is interested in young people. It shouldn’t be the last person in who gets the job no one else wants.” Teens “are my favorite group to work with. They don’t take any nonsense.”
And she explained: “Young people like to get to know the person who’s going to take care of them. So, stay with them for their young adult years.” This can be “quite a fluid period,” with it normally extending to age 25, but in some cases, “it can be up to 32 years old.”
Preparing for the transition
To ease pediatric patients into the transition to adult care, Dr. Aleppo recommended that the pediatric diabetes team provide enough time so that any concerns the patient and their family may have can be addressed.
This should also include transferring management responsibilities to the young adult rather than their parent.
The pediatric provider should discuss with the patient available potential adult colleagues, personalizing these options to their needs, she said.
And the adult and pediatric clinicians should collaborate and provide important information beyond medical records or health summaries.
Adult providers should guide young adults on how to navigate the new practices, from scheduling follow-up appointments to policies regarding medication refills or supplies, to providing information about urgent numbers or email addresses for after-hours communications.
Dr. Kar reiterated that there are too few published outcomes in this patient group to guide the establishment of good transition services.
“Without data, we are dead on the ground. Without data, it’s all conjecture, anecdotes,” he said.
What he does know is that, in the latest national type 1 diabetes audit for England, “Diabetic ketoacidosis admissions ... are up in this age group,” which suggests these patients are not receiving adequate care.
Be a guide, not a gatekeeper
Dr. Kar stressed that, of the 8,760 hours in a year, the average patient with type 1 diabetes in the United Kingdom gets just “1-2 hours with you as a clinician, based on four appointments per year of 30 minutes each.”
“So you spend 0.02% of their time with individuals with type 1 diabetes. So, what’s the one thing you can do with that minimal contact? Be nice!”
Dr. Kar said he always has his email open to his adult patients and they are very respectful of his time. “They don’t email you at 1 a.m. That means every one of my patients has got support [from me]. Don’t be a barrier.”
“We have to fundamentally change the narrative. Doctors must have more empathy,” he said, stating that the one thing adolescents have constantly given feedback on has been, “Why don’t appointments start with: ‘How are you?’
“For a teenager, if you throw type 1 diabetes into the loop, it’s not easy,” he stressed. “Talk to them about something else. As a clinician, be a guide, not a gatekeeper. Give people the tools to self-manage better.”
Adult providers can meet these young adult patients “at their level,” Dr. Aleppo agreed.
“Pay attention to their immediate needs and focus on their present circumstances – whether how to get through their next semester in college, navigating job interviews, or handling having diabetes in the workplace.”
Paying attention to the mental health needs of these young patients is equally “paramount,” Dr. Aleppo said.
While access to mental health professionals may be challenging in the adult setting, providers should bring it up with their patients and offer counseling referrals.
“Diabetes impacts everything, and office appointments and conversations carry weight on these patients’ lives as a whole, not just on their diabetes,” she stressed. “A patient told me recently: ‘We’re learning to be adults,’ which can be hard enough, and with diabetes it can be even more challenging. Adult providers need to be aware of the patient’s ‘diabetes language’ in that often it is not what a patient is saying, rather how they are saying it that gives us information on what they truly need.
“As adult providers, we need to also train and teach our young patients to advocate for themselves on where to find resources that can help them navigate adulthood with diabetes,” she added.
One particularly helpful resource in the United States is the College Diabetes Network, a not-for-profit organization whose mission is to equip young adults with type 1 diabetes to successfully manage the challenging transition to independence at college and beyond.
“The sweetest thing that can happen to us as adult diabetes providers is when a patient – seen as an emerging adult during college – returns to your practice 10 years later after moving back and seeks you out for their diabetes care because of the relationship and trust you developed in those transitioning years,” Dr. Aleppo said.
Another resource is a freely available comic book series cocreated by Dr. Kar and colleague Mayank Patel, MBBS, an endocrinologist from University Hospital Southampton NHS Foundation Trust.
As detailed by this news organization in 2021, the series consists of three volumes: the first, Type 1: Origins, focuses on actual experiences of patients who have type 1 diabetes; the second, Type 1: Attack of the Ketones, is aimed at professionals who may provide care but have limited understanding of type 1 diabetes; and the third, Type 1 Mission 3: S.T.I.G.M.A., addresses the stigmas and misconceptions that patients with type 1 diabetes may face.
The idea for the first comic was inspired by a patient who compared having diabetes to being like the Marvel character The Hulk, said Dr. Kar, and has been expanded to include the additional volumes.
Dr. Kar and Dr. Patel have also just launched the fourth comic in the series, Type 1: Generations, to mark the 100-year anniversary since insulin was first given to a human.
“This is high priority”
Dr. Kar said the NHS in England has just appointed a national lead for type 1 diabetes in youth, Fulya Mehta, MD, of Alder Hey Children’s NHS Foundation Trust, Liverpool, England.
“If you have a plan, bring it to us,” he told the audience at the DPC conference, and “tell us, what is the one thing you would change? This is not a session we are doing just to tick a box. This is high priority.
“Encourage your colleagues to think about transition services. This is an absolute priority. We will be asking every center [in England] who is your transitioning lead?”
And he once again stressed that “a lead of transition service does not have to be a medic. This should be a multidisciplinary team. But they do need to be comfortable in that space. To that teenager, your job title means nothing. Give them time and space.”
Dr. Randell summed it up: “If we can work together, it’s only going to result in better outcomes. We need to blaze the trail for young people.”
Dr. Aleppo has reported serving as a consultant to Dexcom and Insulet and receiving support to Northwestern University from AstraZeneca, Dexcom, Eli Lilly, Fractyl Health, Insulet, and Novo Nordisk. Dr. Randell and Dr. Kar have no conflicts of interest.
A version of this article first appeared on Medscape.com.
“No one has asked young people what they want,” said Tabitha Randell, MBChB, an endocrinologist with Nottingham (England) University Hospitals NHS Trust, who specializes in treating teenagers with type 1 diabetes as they transition to adult care.
Dr. Randell, who has set up a very successful specialist service in her hospital for such patients, said: “We consistently have the best, or the second best, outcomes in this country for our diabetes patients.” She believes this is one of the most important issues in modern endocrinology today.
Speaking at the Diabetes Professional Care conference in London at the end of 2021, and sharing her thoughts afterward with this news organization, she noted that in general there are “virtually no published outcomes” on how best to transition a patient with type 1 diabetes from pediatric to adult care.
“If you actually get them to transition – because some just drop out and disengage and there’s nothing you can do – none of them get lost. Some of them disengage in the adult clinic, but if you’re in the young diabetes service [in England] the rules are that if you miss a diabetes appointment you do not get discharged, as compared with the adult clinic, where if you miss an appointment, you are discharged.”
In the young diabetes clinic, doctors will “carry on trying to contact you, and get you back,” she explained. “And the patients do eventually come back in – it might be a year or 2, but they do come back. We’ve just got to keep them alive in the meantime!”
This issue needs tackling all over the world. Dr. Randell said she’s not aware of any one country – although there may be “pockets” of good care within a given country – that is doing this perfectly.
Across the pond, Grazia Aleppo, MD, division of endocrinology at Northwestern University, Chicago, agreed that transitioning pediatric patients with type 1 diabetes to adult care presents “unique challenges.”
Challenges when transitioning from pediatric to adult care
During childhood, type 1 diabetes management is largely supervised by patients’ parents and members of the pediatric diabetes care team, which may include diabetes educators, psychologists, or social workers, as well as pediatric endocrinologists.
When the patient with type 1 diabetes becomes a young adult and takes over management of their own health, Dr. Aleppo said, the care team may diminish along with the time spent in provider visits.
The adult endocrinology setting focuses more on self-management and autonomous functioning of the individual with diabetes.
Adult appointments are typically shorter, and the patient is usually expected to follow doctors’ suggestions independently, she noted. They are also expected to manage the practical aspects of their diabetes care, including prescriptions, diabetes supplies, laboratory tests, scheduling, and keeping appointments.
At the same time that the emerging adult needs to start asserting independence over their health care, they will also be going through a myriad of other important lifestyle changes, such as attending college, living on their own for the first time, and starting a career.
“With these fundamental differences and challenges, competing priorities, such as college, work and relationships, medical care may become of secondary importance and patients may become disengaged,” Dr. Aleppo explained.
As Dr. Randell has said, loss to follow-up is a big problem with this patient population, with disengagement from specialist services and worsening A1c across the transition, Dr. Aleppo noted. This makes addressing these patients’ specific needs extremely important.
Engage with kid, not disease; don’t palm them off on new recruits
“The really key thing these kids say is, ‘I do not want to be a disease,’” Dr. Randell said. “They want you to know that they are a person. Engage these kids!” she suggested. “Ask them: ‘How is your exam revision going?’ Find something positive to say, even if it’s just: ‘I’m glad you came today.’ ”
“If the first thing that you do is tell them off [for poor diabetes care], you are never going to see them again,” she cautioned.
Dr. Randell also said that role models with type 1 diabetes, such as Lila Moss – daughter of British supermodel Kate Moss – who was recently pictured wearing an insulin pump on her leg on the catwalk, are helping youngsters not feel so self-conscious about their diabetes.
“Let them know it’s not the end of the world, having [type 1] diabetes,” she emphasized.
And Partha Kar, MBBS, OBE, national specialty advisor, diabetes with NHS England, agreed wholeheartedly with Dr. Randall.
Reminiscing about his early days as a newly qualified endocrinologist, Dr. Kar, who works at Portsmouth (England) Hospital NHS Trust, noted that as a new member of staff he was given the youth with type 1 diabetes – those getting ready to transition to adult care – to look after.
But this is the exact opposite of what should be happening, he emphasized. “If you don’t think transition care is important, you shouldn’t be treating type 1 diabetes.”
He believes that every diabetes center “must have a young-adult team lead” and this job must not be given to the least experienced member of staff.
This lead “doesn’t need to be a doctor,” Dr. Kar stressed. “It can be a psychologist, or a diabetes nurse, or a pharmacist, or a dietician.”
In short, it must be someone experienced who loves working with this age group.
Dr. Randell agreed: “Make sure the team is interested in young people. It shouldn’t be the last person in who gets the job no one else wants.” Teens “are my favorite group to work with. They don’t take any nonsense.”
And she explained: “Young people like to get to know the person who’s going to take care of them. So, stay with them for their young adult years.” This can be “quite a fluid period,” with it normally extending to age 25, but in some cases, “it can be up to 32 years old.”
Preparing for the transition
To ease pediatric patients into the transition to adult care, Dr. Aleppo recommended that the pediatric diabetes team provide enough time so that any concerns the patient and their family may have can be addressed.
This should also include transferring management responsibilities to the young adult rather than their parent.
The pediatric provider should discuss with the patient available potential adult colleagues, personalizing these options to their needs, she said.
And the adult and pediatric clinicians should collaborate and provide important information beyond medical records or health summaries.
Adult providers should guide young adults on how to navigate the new practices, from scheduling follow-up appointments to policies regarding medication refills or supplies, to providing information about urgent numbers or email addresses for after-hours communications.
Dr. Kar reiterated that there are too few published outcomes in this patient group to guide the establishment of good transition services.
“Without data, we are dead on the ground. Without data, it’s all conjecture, anecdotes,” he said.
What he does know is that, in the latest national type 1 diabetes audit for England, “Diabetic ketoacidosis admissions ... are up in this age group,” which suggests these patients are not receiving adequate care.
Be a guide, not a gatekeeper
Dr. Kar stressed that, of the 8,760 hours in a year, the average patient with type 1 diabetes in the United Kingdom gets just “1-2 hours with you as a clinician, based on four appointments per year of 30 minutes each.”
“So you spend 0.02% of their time with individuals with type 1 diabetes. So, what’s the one thing you can do with that minimal contact? Be nice!”
Dr. Kar said he always has his email open to his adult patients and they are very respectful of his time. “They don’t email you at 1 a.m. That means every one of my patients has got support [from me]. Don’t be a barrier.”
“We have to fundamentally change the narrative. Doctors must have more empathy,” he said, stating that the one thing adolescents have constantly given feedback on has been, “Why don’t appointments start with: ‘How are you?’
“For a teenager, if you throw type 1 diabetes into the loop, it’s not easy,” he stressed. “Talk to them about something else. As a clinician, be a guide, not a gatekeeper. Give people the tools to self-manage better.”
Adult providers can meet these young adult patients “at their level,” Dr. Aleppo agreed.
“Pay attention to their immediate needs and focus on their present circumstances – whether how to get through their next semester in college, navigating job interviews, or handling having diabetes in the workplace.”
Paying attention to the mental health needs of these young patients is equally “paramount,” Dr. Aleppo said.
While access to mental health professionals may be challenging in the adult setting, providers should bring it up with their patients and offer counseling referrals.
“Diabetes impacts everything, and office appointments and conversations carry weight on these patients’ lives as a whole, not just on their diabetes,” she stressed. “A patient told me recently: ‘We’re learning to be adults,’ which can be hard enough, and with diabetes it can be even more challenging. Adult providers need to be aware of the patient’s ‘diabetes language’ in that often it is not what a patient is saying, rather how they are saying it that gives us information on what they truly need.
“As adult providers, we need to also train and teach our young patients to advocate for themselves on where to find resources that can help them navigate adulthood with diabetes,” she added.
One particularly helpful resource in the United States is the College Diabetes Network, a not-for-profit organization whose mission is to equip young adults with type 1 diabetes to successfully manage the challenging transition to independence at college and beyond.
“The sweetest thing that can happen to us as adult diabetes providers is when a patient – seen as an emerging adult during college – returns to your practice 10 years later after moving back and seeks you out for their diabetes care because of the relationship and trust you developed in those transitioning years,” Dr. Aleppo said.
Another resource is a freely available comic book series cocreated by Dr. Kar and colleague Mayank Patel, MBBS, an endocrinologist from University Hospital Southampton NHS Foundation Trust.
As detailed by this news organization in 2021, the series consists of three volumes: the first, Type 1: Origins, focuses on actual experiences of patients who have type 1 diabetes; the second, Type 1: Attack of the Ketones, is aimed at professionals who may provide care but have limited understanding of type 1 diabetes; and the third, Type 1 Mission 3: S.T.I.G.M.A., addresses the stigmas and misconceptions that patients with type 1 diabetes may face.
The idea for the first comic was inspired by a patient who compared having diabetes to being like the Marvel character The Hulk, said Dr. Kar, and has been expanded to include the additional volumes.
Dr. Kar and Dr. Patel have also just launched the fourth comic in the series, Type 1: Generations, to mark the 100-year anniversary since insulin was first given to a human.
“This is high priority”
Dr. Kar said the NHS in England has just appointed a national lead for type 1 diabetes in youth, Fulya Mehta, MD, of Alder Hey Children’s NHS Foundation Trust, Liverpool, England.
“If you have a plan, bring it to us,” he told the audience at the DPC conference, and “tell us, what is the one thing you would change? This is not a session we are doing just to tick a box. This is high priority.
“Encourage your colleagues to think about transition services. This is an absolute priority. We will be asking every center [in England] who is your transitioning lead?”
And he once again stressed that “a lead of transition service does not have to be a medic. This should be a multidisciplinary team. But they do need to be comfortable in that space. To that teenager, your job title means nothing. Give them time and space.”
Dr. Randell summed it up: “If we can work together, it’s only going to result in better outcomes. We need to blaze the trail for young people.”
Dr. Aleppo has reported serving as a consultant to Dexcom and Insulet and receiving support to Northwestern University from AstraZeneca, Dexcom, Eli Lilly, Fractyl Health, Insulet, and Novo Nordisk. Dr. Randell and Dr. Kar have no conflicts of interest.
A version of this article first appeared on Medscape.com.
More than a month after launch, iPLEDGE glitches persist
which mandates the program to prevent fetal exposure to the teratogenic effects of isotretinoin, and by the American Academy of Dermatology Association, whose members have repeatedly asked the FDA for meetings to discuss solutions. The AADA is the legislative and advocacy arm of AAD.
When the new program launched Dec. 13, 2021, the website crashed repeatedly, with physicians and patients complaining they got locked out or bounced off the platform when they tried to follow instructions to enter information. Hold times to talk to a live person stretched to hours.
The latest improvement attempt, announced Jan. 14 by the FDA, is a tool created by the Isotretinoin Products Manufacturers Group, the manufacturers responsible for the FDA-mandated REMS program. It is meant to allow prescribers and designees to send log-in links directly to patients’ email accounts through the iPLEDGE REMS portal, bypassing the troublesome call center.
And it’s not the answer, dermatologists said.
“The new tool does not solve issues such as prescribers or pharmacies not being able to access the site, unacceptably long call center wait times, inefficiencies caused by frequent attestation requirements for those who cannot become pregnant, patients becoming ‘locked out’ because they missed a window period through no fault of their own, among others,” said John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital and instructor in dermatology at Harvard Medical School, both in Boston.
The day after the FDA update about the new tool, Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., tweeted: “Lip service and empty words.” He noted that the situation has been “disastrous from the start” as the new platform launched.
Under the iPLEDGE program in place for the acne drug, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The aim of the new gender-neutral approach to the risk mitigation program is to make the experience more inclusive for transgender patients. The previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) are now reduced to just two (those capable of getting pregnant and those not capable of getting pregnant).
The problem is the execution of the new platform. The transition from the old website to the new was done quickly. By most accounts, the Dec. 13 rollout was chaotic, a failure, and disastrous, triggering numerous expressions of frustration on Twitter and other social media, with some calling for the program to be halted until the bugs could be worked out.
“While the new gender-neutral categories are a welcome improvement to the system, the new categorization approach was not the underlying reason for the new platform and its failed rollout, which was instead due to a change in vendor,” Dr. Barbieri told this news organization.
AADA: More recent efforts to improve the system
“We have a letter to the FDA asking for a stakeholders meeting to include us, the IPMG, and pharmacists because there are ongoing problems, though there have been some improvement in terms of certain elements,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE Workgroup and professor of dermatology at the University of California, San Francisco, said in an interview shortly after the FDA posted the update on the new tool. “That said, there are many patients who have not gotten isotretinoin during the 1 month since the roll-out of the new platform.”
What still needs to be fixed? “We have ongoing concerns about the lack of transparency of the IPMG, about call center wait times, actual number of prescriptions on the hands of patients compared to the previous month, and those patients who can get pregnant who – despite complying with all of the REMS requirements – are being locked out because of the lack of timely attestation to their negative pregnancy status due to the website, not the patients themselves,” Dr. Frieden told this news organization.
“We are continuing to advocate to have decreased attestation requirements for individuals who cannot become pregnant – because this will improve the efficiency of the system for those patients for whom the REMS program goals are truly intended – those who can become pregnant, since the primary aim of the REMS program is to minimize fetal exposure.”
An AADA spokesperson said that the IPMG has invited the AADA to a joint stakeholders meeting on Jan. 26, along with representatives from the FDA and pharmacy industry.
Spotty progress
“The iPLEDGE situation is as frustrating as ever,” said Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, after the FDA’s Jan. 14 update was released. “It’s like they never tested the new website before deploying it.”
Among the issues he has experienced in his practice, he said, is an instance in which iPLEDGE swapped the first names of a mother and daughter, so it was impossible to fill the prescription. “It happened twice in the same day,” Dr. Goldberg said. The patient had to call iPLEDGE to fix this, but the call center wasn’t taking calls.
In today’s technology environment, he said, it’s hard to believe that “we have to put up with this.”
Some have seen success. ‘’The tool is working fine on our end,” said Mitesh Patel, PharmD, pharmacy manager at Sunshine Pharmacy in White Plains, N.Y. However, he added that some doctors and patients are still having issues. He encourages dermatologists still having issues with the system to reach out to independent pharmacies that have processed iPLEDGE prescriptions and ‘’lean on them to assist.”
This news organization contacted CVS and Walgreens about how the system is working at their locations, but has not yet received a response.
Dr. Goldberg, Dr. Frieden, Dr. Barbieri, and Dr. Peebles have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This story was updated on 1/24/22.
which mandates the program to prevent fetal exposure to the teratogenic effects of isotretinoin, and by the American Academy of Dermatology Association, whose members have repeatedly asked the FDA for meetings to discuss solutions. The AADA is the legislative and advocacy arm of AAD.
When the new program launched Dec. 13, 2021, the website crashed repeatedly, with physicians and patients complaining they got locked out or bounced off the platform when they tried to follow instructions to enter information. Hold times to talk to a live person stretched to hours.
The latest improvement attempt, announced Jan. 14 by the FDA, is a tool created by the Isotretinoin Products Manufacturers Group, the manufacturers responsible for the FDA-mandated REMS program. It is meant to allow prescribers and designees to send log-in links directly to patients’ email accounts through the iPLEDGE REMS portal, bypassing the troublesome call center.
And it’s not the answer, dermatologists said.
“The new tool does not solve issues such as prescribers or pharmacies not being able to access the site, unacceptably long call center wait times, inefficiencies caused by frequent attestation requirements for those who cannot become pregnant, patients becoming ‘locked out’ because they missed a window period through no fault of their own, among others,” said John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital and instructor in dermatology at Harvard Medical School, both in Boston.
The day after the FDA update about the new tool, Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., tweeted: “Lip service and empty words.” He noted that the situation has been “disastrous from the start” as the new platform launched.
Under the iPLEDGE program in place for the acne drug, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The aim of the new gender-neutral approach to the risk mitigation program is to make the experience more inclusive for transgender patients. The previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) are now reduced to just two (those capable of getting pregnant and those not capable of getting pregnant).
The problem is the execution of the new platform. The transition from the old website to the new was done quickly. By most accounts, the Dec. 13 rollout was chaotic, a failure, and disastrous, triggering numerous expressions of frustration on Twitter and other social media, with some calling for the program to be halted until the bugs could be worked out.
“While the new gender-neutral categories are a welcome improvement to the system, the new categorization approach was not the underlying reason for the new platform and its failed rollout, which was instead due to a change in vendor,” Dr. Barbieri told this news organization.
AADA: More recent efforts to improve the system
“We have a letter to the FDA asking for a stakeholders meeting to include us, the IPMG, and pharmacists because there are ongoing problems, though there have been some improvement in terms of certain elements,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE Workgroup and professor of dermatology at the University of California, San Francisco, said in an interview shortly after the FDA posted the update on the new tool. “That said, there are many patients who have not gotten isotretinoin during the 1 month since the roll-out of the new platform.”
What still needs to be fixed? “We have ongoing concerns about the lack of transparency of the IPMG, about call center wait times, actual number of prescriptions on the hands of patients compared to the previous month, and those patients who can get pregnant who – despite complying with all of the REMS requirements – are being locked out because of the lack of timely attestation to their negative pregnancy status due to the website, not the patients themselves,” Dr. Frieden told this news organization.
“We are continuing to advocate to have decreased attestation requirements for individuals who cannot become pregnant – because this will improve the efficiency of the system for those patients for whom the REMS program goals are truly intended – those who can become pregnant, since the primary aim of the REMS program is to minimize fetal exposure.”
An AADA spokesperson said that the IPMG has invited the AADA to a joint stakeholders meeting on Jan. 26, along with representatives from the FDA and pharmacy industry.
Spotty progress
“The iPLEDGE situation is as frustrating as ever,” said Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, after the FDA’s Jan. 14 update was released. “It’s like they never tested the new website before deploying it.”
Among the issues he has experienced in his practice, he said, is an instance in which iPLEDGE swapped the first names of a mother and daughter, so it was impossible to fill the prescription. “It happened twice in the same day,” Dr. Goldberg said. The patient had to call iPLEDGE to fix this, but the call center wasn’t taking calls.
In today’s technology environment, he said, it’s hard to believe that “we have to put up with this.”
Some have seen success. ‘’The tool is working fine on our end,” said Mitesh Patel, PharmD, pharmacy manager at Sunshine Pharmacy in White Plains, N.Y. However, he added that some doctors and patients are still having issues. He encourages dermatologists still having issues with the system to reach out to independent pharmacies that have processed iPLEDGE prescriptions and ‘’lean on them to assist.”
This news organization contacted CVS and Walgreens about how the system is working at their locations, but has not yet received a response.
Dr. Goldberg, Dr. Frieden, Dr. Barbieri, and Dr. Peebles have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This story was updated on 1/24/22.
which mandates the program to prevent fetal exposure to the teratogenic effects of isotretinoin, and by the American Academy of Dermatology Association, whose members have repeatedly asked the FDA for meetings to discuss solutions. The AADA is the legislative and advocacy arm of AAD.
When the new program launched Dec. 13, 2021, the website crashed repeatedly, with physicians and patients complaining they got locked out or bounced off the platform when they tried to follow instructions to enter information. Hold times to talk to a live person stretched to hours.
The latest improvement attempt, announced Jan. 14 by the FDA, is a tool created by the Isotretinoin Products Manufacturers Group, the manufacturers responsible for the FDA-mandated REMS program. It is meant to allow prescribers and designees to send log-in links directly to patients’ email accounts through the iPLEDGE REMS portal, bypassing the troublesome call center.
And it’s not the answer, dermatologists said.
“The new tool does not solve issues such as prescribers or pharmacies not being able to access the site, unacceptably long call center wait times, inefficiencies caused by frequent attestation requirements for those who cannot become pregnant, patients becoming ‘locked out’ because they missed a window period through no fault of their own, among others,” said John Barbieri, MD, MBA, director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital and instructor in dermatology at Harvard Medical School, both in Boston.
The day after the FDA update about the new tool, Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., tweeted: “Lip service and empty words.” He noted that the situation has been “disastrous from the start” as the new platform launched.
Under the iPLEDGE program in place for the acne drug, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The aim of the new gender-neutral approach to the risk mitigation program is to make the experience more inclusive for transgender patients. The previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) are now reduced to just two (those capable of getting pregnant and those not capable of getting pregnant).
The problem is the execution of the new platform. The transition from the old website to the new was done quickly. By most accounts, the Dec. 13 rollout was chaotic, a failure, and disastrous, triggering numerous expressions of frustration on Twitter and other social media, with some calling for the program to be halted until the bugs could be worked out.
“While the new gender-neutral categories are a welcome improvement to the system, the new categorization approach was not the underlying reason for the new platform and its failed rollout, which was instead due to a change in vendor,” Dr. Barbieri told this news organization.
AADA: More recent efforts to improve the system
“We have a letter to the FDA asking for a stakeholders meeting to include us, the IPMG, and pharmacists because there are ongoing problems, though there have been some improvement in terms of certain elements,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE Workgroup and professor of dermatology at the University of California, San Francisco, said in an interview shortly after the FDA posted the update on the new tool. “That said, there are many patients who have not gotten isotretinoin during the 1 month since the roll-out of the new platform.”
What still needs to be fixed? “We have ongoing concerns about the lack of transparency of the IPMG, about call center wait times, actual number of prescriptions on the hands of patients compared to the previous month, and those patients who can get pregnant who – despite complying with all of the REMS requirements – are being locked out because of the lack of timely attestation to their negative pregnancy status due to the website, not the patients themselves,” Dr. Frieden told this news organization.
“We are continuing to advocate to have decreased attestation requirements for individuals who cannot become pregnant – because this will improve the efficiency of the system for those patients for whom the REMS program goals are truly intended – those who can become pregnant, since the primary aim of the REMS program is to minimize fetal exposure.”
An AADA spokesperson said that the IPMG has invited the AADA to a joint stakeholders meeting on Jan. 26, along with representatives from the FDA and pharmacy industry.
Spotty progress
“The iPLEDGE situation is as frustrating as ever,” said Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, after the FDA’s Jan. 14 update was released. “It’s like they never tested the new website before deploying it.”
Among the issues he has experienced in his practice, he said, is an instance in which iPLEDGE swapped the first names of a mother and daughter, so it was impossible to fill the prescription. “It happened twice in the same day,” Dr. Goldberg said. The patient had to call iPLEDGE to fix this, but the call center wasn’t taking calls.
In today’s technology environment, he said, it’s hard to believe that “we have to put up with this.”
Some have seen success. ‘’The tool is working fine on our end,” said Mitesh Patel, PharmD, pharmacy manager at Sunshine Pharmacy in White Plains, N.Y. However, he added that some doctors and patients are still having issues. He encourages dermatologists still having issues with the system to reach out to independent pharmacies that have processed iPLEDGE prescriptions and ‘’lean on them to assist.”
This news organization contacted CVS and Walgreens about how the system is working at their locations, but has not yet received a response.
Dr. Goldberg, Dr. Frieden, Dr. Barbieri, and Dr. Peebles have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This story was updated on 1/24/22.
Antidepressants: Is less more?
When it comes to antidepressant prescribing, less may be more, new research suggests.
A new review suggests antidepressants are overprescribed and that the efficacy of these agents is questionable, leading researchers to recommend that, when physicians prescribe these medications, it should be for shorter periods.
“Antidepressants have never been shown to have a clinically significant difference from placebo in the treatment of depression,” study co\investigator Mark Horowitz, GDPsych, PhD, division of psychiatry, University College London, said in an interview.
He added antidepressants “exert profound adverse effects on the body and brain” and can be difficult to stop because of physical dependence that occurs when the brain adapts to them.
“The best way to take people off these drugs is to do so gradually enough that the unpleasant effects are minimized and in a way that means the reductions in dose get smaller and smaller as the total dose gets lower,” Dr. Horowitz said.
However, at least one expert urged caution in interpreting the review’s findings.
“The reality is that millions of people do benefit from these medications, and this review minimizes those benefits,” Philip Muskin, MD, chief of consultation-liaison for psychiatry and professor of psychiatry, Columbia University Medical Center and New York–Presbyterian Hospital, said when approached for comment.
The findings were published online Dec. 20, 2021, in the Drug and Therapeutics Bulletin.
Personal experience
Prescribing of newer-generation antidepressants, such as SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs), is increasing, with an estimated one in six adults in the United Kingdom receiving at least one prescription in 2019-2020, the investigators noted.
Dr. Horowitz noted a personal motivation for conducting the review. “As well as being an academic psychiatrist, I’m also a patient who has been prescribed antidepressants since age 21, when my mood was poor, due to life circumstances.”
The antidepressant “didn’t have particularly helpful effects,” but Dr. Horowitz continued taking it for 18 years. “I was told it was helpful and internalized that message. I came to understand that much of the information around antidepressants came from the drug companies that manufactured them or from academics paid by these companies.”
Dr. Horowitz is currently discontinuing his medication – a tapering process now in its third year. He said he has come to realize, in retrospect, that symptoms not initially attributed to the drug, such as fatigue, impaired concentration, and impaired memory, have improved since reducing the medication.
“That experience sensitized me to look for these symptoms in my patients and I see them; but most of my patients were told by their doctors that the cause of those problems was the depression or anxiety itself and not the drug,” he said.
Dr. Horowitz collaborated with Michael Wilcock, DTB, Pharmacy, Royal Cornwall Hospitals, NHS Trust, Truro, England, in conducting the review “to provide an independent assessment of benefits and harms of antidepressants.”
“Much of the evidence of the efficacy of antidepressants comes from randomized placebo-controlled trials,” Dr. Horowitz said. Several meta-analyses of these studies showed a difference of about two points between the agent and the placebo on the Hamilton Depression Rating Scale (HAM-D).
“Although this might be statistically significant, it does not meet the threshold for a clinical significance – those aren’t the same thing,” Dr. Horowitz said. Some analyses suggest that a “minimally clinically important difference” on the HAM-D would range from 3 to 6 points.
The findings in adolescents and children are “even less convincing,” the investigators noted, citing a Cochrane review.
“This is especially concerning because the number of children and adolescents being treated with antidepressants is rapidly increasing,” Dr. Horowitz said.
Additionally, the short duration of most trials, typically 6-12 weeks, is “largely uninformative for the clinical treatment of depression.”
Relapse or withdrawal?
The researchers reviewed the adverse effects of long-term antidepressant use, including daytime sleepiness, dry mouth, profuse sweating, weight gain, sexual dysfunction, restlessness, and feeling “foggy or detached.”
“Antidepressants have toxic effects on the brain and cause brain damage when they artificially increase serotonin and modify brain chemistry, which is why people become sick for years after stopping,” Dr. Horowitz said. “When the drug is reduced or stopped, the brain has difficulty dealing with the sudden drop in neurotransmitters, and withdrawal symptoms result, similar to stopping caffeine, nicotine, or opioids.”
He added it is not necessarily the original condition of depression or anxiety that is recurring but rather withdrawal, which can last for months or even years after medication discontinuation.
“Unfortunately, doctors have been taught that there are minimal withdrawal symptoms, euphemized as ‘discontinuation symptoms,’ and so when patients have reported withdrawal symptoms, they have been told it is a return of their underlying condition,” Dr. Horowitz said.
“This has led to many patients being incorrectly told that they need to get back on their antidepressants,” he added.
He likened this approach to “telling people that the need to continue smoking because when they stop, they get more anxiety.” Rather, the “correct response would be that they simply need to taper off the antidepressant more carefully,” he said.
Helpful in the short term
Patients should be informed prior to initiation of antidepressant treatment about the risk of withdrawal effects if they stop the drug, the investigators advise. They reference the Royal College of Psychiatrists’ updated guidance, which recommends slow tapering over a period long enough to mitigate withdrawal symptoms to “tolerable levels.”
The guidance suggests that patients start with a small “test reduction.” Withdrawal symptoms should be monitored for the following 2-4 weeks, using a symptom checklist such as the Discontinuation Emergent Signs and Symptoms Scale, with subsequent reductions based on the tolerability of the process.
Gradual dose reductions and very small final doses may necessitate the use of formulations of medication other than those commonly available in tablet forms, the researchers noted. During the tapering process, patients may benefit from increased psychosocial support.
Dr. Horowitz noted that antidepressants can be helpful on a short-term basis, and likened their use to the use of a cast to stabilize a broken arm.
“It’s useful for a short period. But if you leave someone in a plastic cast permanently, their arm will shrivel and you will disable them. These drugs should be prescribed minimally, and for the shortest possible period of time,” he said.
Dr. Horowitz recommended the recent draft National Institute for Health and Care Excellence depression guidance that recommends multiple other options beyond antidepressants, including cognitive-behavioral therapy, problem solving, counseling, and exercise.
Lack of balance
Dr. Muskin commented that the review is helpful in guiding clinicians on how to approach tapering of antidepressants and making patients aware of discontinuation symptoms.
However, “a lot of people will read this who need treatment, but they won’t get treated because they’ll take away the message that ‘drugs don’t work,’ ” he said.
“As it is, there is already stigma and prejudice toward psychiatric illness and using medications for treatment,” said Dr. Muskin, who was not involved with the research.
The current review “isn’t balanced, in terms of the efficacy of these drugs – both for the spectrum of depressive disorders and for panic or anxiety disorder. And there is nowhere that the authors say these drugs help people,” he added.
Moreover, the investigators’ assertion that long-term use of antidepressants causes harm is incorrect, he said.
“Yes, there are ongoing side effects that impose a burden, but that’s not the same as harm. And while the side effects are sometimes burdensome, ongoing depression is also terribly burdensome,” Dr. Muskin concluded.
Dr. Horowitz, Dr. Wilcock, and Dr. Muskin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When it comes to antidepressant prescribing, less may be more, new research suggests.
A new review suggests antidepressants are overprescribed and that the efficacy of these agents is questionable, leading researchers to recommend that, when physicians prescribe these medications, it should be for shorter periods.
“Antidepressants have never been shown to have a clinically significant difference from placebo in the treatment of depression,” study co\investigator Mark Horowitz, GDPsych, PhD, division of psychiatry, University College London, said in an interview.
He added antidepressants “exert profound adverse effects on the body and brain” and can be difficult to stop because of physical dependence that occurs when the brain adapts to them.
“The best way to take people off these drugs is to do so gradually enough that the unpleasant effects are minimized and in a way that means the reductions in dose get smaller and smaller as the total dose gets lower,” Dr. Horowitz said.
However, at least one expert urged caution in interpreting the review’s findings.
“The reality is that millions of people do benefit from these medications, and this review minimizes those benefits,” Philip Muskin, MD, chief of consultation-liaison for psychiatry and professor of psychiatry, Columbia University Medical Center and New York–Presbyterian Hospital, said when approached for comment.
The findings were published online Dec. 20, 2021, in the Drug and Therapeutics Bulletin.
Personal experience
Prescribing of newer-generation antidepressants, such as SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs), is increasing, with an estimated one in six adults in the United Kingdom receiving at least one prescription in 2019-2020, the investigators noted.
Dr. Horowitz noted a personal motivation for conducting the review. “As well as being an academic psychiatrist, I’m also a patient who has been prescribed antidepressants since age 21, when my mood was poor, due to life circumstances.”
The antidepressant “didn’t have particularly helpful effects,” but Dr. Horowitz continued taking it for 18 years. “I was told it was helpful and internalized that message. I came to understand that much of the information around antidepressants came from the drug companies that manufactured them or from academics paid by these companies.”
Dr. Horowitz is currently discontinuing his medication – a tapering process now in its third year. He said he has come to realize, in retrospect, that symptoms not initially attributed to the drug, such as fatigue, impaired concentration, and impaired memory, have improved since reducing the medication.
“That experience sensitized me to look for these symptoms in my patients and I see them; but most of my patients were told by their doctors that the cause of those problems was the depression or anxiety itself and not the drug,” he said.
Dr. Horowitz collaborated with Michael Wilcock, DTB, Pharmacy, Royal Cornwall Hospitals, NHS Trust, Truro, England, in conducting the review “to provide an independent assessment of benefits and harms of antidepressants.”
“Much of the evidence of the efficacy of antidepressants comes from randomized placebo-controlled trials,” Dr. Horowitz said. Several meta-analyses of these studies showed a difference of about two points between the agent and the placebo on the Hamilton Depression Rating Scale (HAM-D).
“Although this might be statistically significant, it does not meet the threshold for a clinical significance – those aren’t the same thing,” Dr. Horowitz said. Some analyses suggest that a “minimally clinically important difference” on the HAM-D would range from 3 to 6 points.
The findings in adolescents and children are “even less convincing,” the investigators noted, citing a Cochrane review.
“This is especially concerning because the number of children and adolescents being treated with antidepressants is rapidly increasing,” Dr. Horowitz said.
Additionally, the short duration of most trials, typically 6-12 weeks, is “largely uninformative for the clinical treatment of depression.”
Relapse or withdrawal?
The researchers reviewed the adverse effects of long-term antidepressant use, including daytime sleepiness, dry mouth, profuse sweating, weight gain, sexual dysfunction, restlessness, and feeling “foggy or detached.”
“Antidepressants have toxic effects on the brain and cause brain damage when they artificially increase serotonin and modify brain chemistry, which is why people become sick for years after stopping,” Dr. Horowitz said. “When the drug is reduced or stopped, the brain has difficulty dealing with the sudden drop in neurotransmitters, and withdrawal symptoms result, similar to stopping caffeine, nicotine, or opioids.”
He added it is not necessarily the original condition of depression or anxiety that is recurring but rather withdrawal, which can last for months or even years after medication discontinuation.
“Unfortunately, doctors have been taught that there are minimal withdrawal symptoms, euphemized as ‘discontinuation symptoms,’ and so when patients have reported withdrawal symptoms, they have been told it is a return of their underlying condition,” Dr. Horowitz said.
“This has led to many patients being incorrectly told that they need to get back on their antidepressants,” he added.
He likened this approach to “telling people that the need to continue smoking because when they stop, they get more anxiety.” Rather, the “correct response would be that they simply need to taper off the antidepressant more carefully,” he said.
Helpful in the short term
Patients should be informed prior to initiation of antidepressant treatment about the risk of withdrawal effects if they stop the drug, the investigators advise. They reference the Royal College of Psychiatrists’ updated guidance, which recommends slow tapering over a period long enough to mitigate withdrawal symptoms to “tolerable levels.”
The guidance suggests that patients start with a small “test reduction.” Withdrawal symptoms should be monitored for the following 2-4 weeks, using a symptom checklist such as the Discontinuation Emergent Signs and Symptoms Scale, with subsequent reductions based on the tolerability of the process.
Gradual dose reductions and very small final doses may necessitate the use of formulations of medication other than those commonly available in tablet forms, the researchers noted. During the tapering process, patients may benefit from increased psychosocial support.
Dr. Horowitz noted that antidepressants can be helpful on a short-term basis, and likened their use to the use of a cast to stabilize a broken arm.
“It’s useful for a short period. But if you leave someone in a plastic cast permanently, their arm will shrivel and you will disable them. These drugs should be prescribed minimally, and for the shortest possible period of time,” he said.
Dr. Horowitz recommended the recent draft National Institute for Health and Care Excellence depression guidance that recommends multiple other options beyond antidepressants, including cognitive-behavioral therapy, problem solving, counseling, and exercise.
Lack of balance
Dr. Muskin commented that the review is helpful in guiding clinicians on how to approach tapering of antidepressants and making patients aware of discontinuation symptoms.
However, “a lot of people will read this who need treatment, but they won’t get treated because they’ll take away the message that ‘drugs don’t work,’ ” he said.
“As it is, there is already stigma and prejudice toward psychiatric illness and using medications for treatment,” said Dr. Muskin, who was not involved with the research.
The current review “isn’t balanced, in terms of the efficacy of these drugs – both for the spectrum of depressive disorders and for panic or anxiety disorder. And there is nowhere that the authors say these drugs help people,” he added.
Moreover, the investigators’ assertion that long-term use of antidepressants causes harm is incorrect, he said.
“Yes, there are ongoing side effects that impose a burden, but that’s not the same as harm. And while the side effects are sometimes burdensome, ongoing depression is also terribly burdensome,” Dr. Muskin concluded.
Dr. Horowitz, Dr. Wilcock, and Dr. Muskin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When it comes to antidepressant prescribing, less may be more, new research suggests.
A new review suggests antidepressants are overprescribed and that the efficacy of these agents is questionable, leading researchers to recommend that, when physicians prescribe these medications, it should be for shorter periods.
“Antidepressants have never been shown to have a clinically significant difference from placebo in the treatment of depression,” study co\investigator Mark Horowitz, GDPsych, PhD, division of psychiatry, University College London, said in an interview.
He added antidepressants “exert profound adverse effects on the body and brain” and can be difficult to stop because of physical dependence that occurs when the brain adapts to them.
“The best way to take people off these drugs is to do so gradually enough that the unpleasant effects are minimized and in a way that means the reductions in dose get smaller and smaller as the total dose gets lower,” Dr. Horowitz said.
However, at least one expert urged caution in interpreting the review’s findings.
“The reality is that millions of people do benefit from these medications, and this review minimizes those benefits,” Philip Muskin, MD, chief of consultation-liaison for psychiatry and professor of psychiatry, Columbia University Medical Center and New York–Presbyterian Hospital, said when approached for comment.
The findings were published online Dec. 20, 2021, in the Drug and Therapeutics Bulletin.
Personal experience
Prescribing of newer-generation antidepressants, such as SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs), is increasing, with an estimated one in six adults in the United Kingdom receiving at least one prescription in 2019-2020, the investigators noted.
Dr. Horowitz noted a personal motivation for conducting the review. “As well as being an academic psychiatrist, I’m also a patient who has been prescribed antidepressants since age 21, when my mood was poor, due to life circumstances.”
The antidepressant “didn’t have particularly helpful effects,” but Dr. Horowitz continued taking it for 18 years. “I was told it was helpful and internalized that message. I came to understand that much of the information around antidepressants came from the drug companies that manufactured them or from academics paid by these companies.”
Dr. Horowitz is currently discontinuing his medication – a tapering process now in its third year. He said he has come to realize, in retrospect, that symptoms not initially attributed to the drug, such as fatigue, impaired concentration, and impaired memory, have improved since reducing the medication.
“That experience sensitized me to look for these symptoms in my patients and I see them; but most of my patients were told by their doctors that the cause of those problems was the depression or anxiety itself and not the drug,” he said.
Dr. Horowitz collaborated with Michael Wilcock, DTB, Pharmacy, Royal Cornwall Hospitals, NHS Trust, Truro, England, in conducting the review “to provide an independent assessment of benefits and harms of antidepressants.”
“Much of the evidence of the efficacy of antidepressants comes from randomized placebo-controlled trials,” Dr. Horowitz said. Several meta-analyses of these studies showed a difference of about two points between the agent and the placebo on the Hamilton Depression Rating Scale (HAM-D).
“Although this might be statistically significant, it does not meet the threshold for a clinical significance – those aren’t the same thing,” Dr. Horowitz said. Some analyses suggest that a “minimally clinically important difference” on the HAM-D would range from 3 to 6 points.
The findings in adolescents and children are “even less convincing,” the investigators noted, citing a Cochrane review.
“This is especially concerning because the number of children and adolescents being treated with antidepressants is rapidly increasing,” Dr. Horowitz said.
Additionally, the short duration of most trials, typically 6-12 weeks, is “largely uninformative for the clinical treatment of depression.”
Relapse or withdrawal?
The researchers reviewed the adverse effects of long-term antidepressant use, including daytime sleepiness, dry mouth, profuse sweating, weight gain, sexual dysfunction, restlessness, and feeling “foggy or detached.”
“Antidepressants have toxic effects on the brain and cause brain damage when they artificially increase serotonin and modify brain chemistry, which is why people become sick for years after stopping,” Dr. Horowitz said. “When the drug is reduced or stopped, the brain has difficulty dealing with the sudden drop in neurotransmitters, and withdrawal symptoms result, similar to stopping caffeine, nicotine, or opioids.”
He added it is not necessarily the original condition of depression or anxiety that is recurring but rather withdrawal, which can last for months or even years after medication discontinuation.
“Unfortunately, doctors have been taught that there are minimal withdrawal symptoms, euphemized as ‘discontinuation symptoms,’ and so when patients have reported withdrawal symptoms, they have been told it is a return of their underlying condition,” Dr. Horowitz said.
“This has led to many patients being incorrectly told that they need to get back on their antidepressants,” he added.
He likened this approach to “telling people that the need to continue smoking because when they stop, they get more anxiety.” Rather, the “correct response would be that they simply need to taper off the antidepressant more carefully,” he said.
Helpful in the short term
Patients should be informed prior to initiation of antidepressant treatment about the risk of withdrawal effects if they stop the drug, the investigators advise. They reference the Royal College of Psychiatrists’ updated guidance, which recommends slow tapering over a period long enough to mitigate withdrawal symptoms to “tolerable levels.”
The guidance suggests that patients start with a small “test reduction.” Withdrawal symptoms should be monitored for the following 2-4 weeks, using a symptom checklist such as the Discontinuation Emergent Signs and Symptoms Scale, with subsequent reductions based on the tolerability of the process.
Gradual dose reductions and very small final doses may necessitate the use of formulations of medication other than those commonly available in tablet forms, the researchers noted. During the tapering process, patients may benefit from increased psychosocial support.
Dr. Horowitz noted that antidepressants can be helpful on a short-term basis, and likened their use to the use of a cast to stabilize a broken arm.
“It’s useful for a short period. But if you leave someone in a plastic cast permanently, their arm will shrivel and you will disable them. These drugs should be prescribed minimally, and for the shortest possible period of time,” he said.
Dr. Horowitz recommended the recent draft National Institute for Health and Care Excellence depression guidance that recommends multiple other options beyond antidepressants, including cognitive-behavioral therapy, problem solving, counseling, and exercise.
Lack of balance
Dr. Muskin commented that the review is helpful in guiding clinicians on how to approach tapering of antidepressants and making patients aware of discontinuation symptoms.
However, “a lot of people will read this who need treatment, but they won’t get treated because they’ll take away the message that ‘drugs don’t work,’ ” he said.
“As it is, there is already stigma and prejudice toward psychiatric illness and using medications for treatment,” said Dr. Muskin, who was not involved with the research.
The current review “isn’t balanced, in terms of the efficacy of these drugs – both for the spectrum of depressive disorders and for panic or anxiety disorder. And there is nowhere that the authors say these drugs help people,” he added.
Moreover, the investigators’ assertion that long-term use of antidepressants causes harm is incorrect, he said.
“Yes, there are ongoing side effects that impose a burden, but that’s not the same as harm. And while the side effects are sometimes burdensome, ongoing depression is also terribly burdensome,” Dr. Muskin concluded.
Dr. Horowitz, Dr. Wilcock, and Dr. Muskin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE DRUG AND THERAPEUTICS BULLETIN
FDA updates status of iPLEDGE access problems
The, one month after a modified program was launched, the Food and Drug Administration announced on Jan. 14.
The IPMG has “created a new tool within the system to help resolve account access for some user groups without using the call center. This tool is intended to allow prescribers and designees to send login links directly to their patients’ desired email address through the Manage Patients page of the iPLEDGE REMS portal,” the FDA statement said.
“Prescribers can also send login links to their designees still having difficulty accessing their iPLEDGE account,” and users should check their emails for messages from iPLEDGE, including spam folders, the FDA advises. The iPLEDGE strategy is designed to prevent fetal exposure to isotretinoin, which is highly teratogenic.
Days after the new, gender-neutral approach to the isotretinoin risk mitigation program was launched on Dec. 13, the FDA convened an emergency meeting with representatives from the American Academy of Dermatology Association (AADA) to discuss the problematic rollout of the program, which was described as disastrous, chaotic, and a failure, with dermatologists on Twitter and elsewhere expressing anger and frustration over not being able to access the program or reach the call center.
A statement by the FDA on Dec. 23 followed, urging manufacturers to develop solutions for the website and to work with the AADA and pharmacy organizations to find solutions that would minimize treatment interruptions during the transition.
The modified REMS, launched on Dec. 13, is designed to make it more inclusive for transgender patients prescribed isotretinoin. Instead of three risk categories (females of reproductive potential, females not of reproductive potential, and males), patients who are prescribed isotretinoin for acne are assigned to one of two risk categories: those who can get pregnant and those who cannot get pregnant.
In the Jan. 14 statement, the FDA notes that the agency is continuing to work with the IPMG regarding the problems clinicians, pharmacists, and patients have had with accessing iPLEDGE over the last month.
“Although there has been progress, there is a significant amount of work still to be done,” the FDA acknowledged. “While we consider potential steps within the scope of FDA’s authorities, we will continue to meet with the IPMG for updates on the status of the problems with the iPLEDGE REMS and their progress towards having the system work as intended for all users.”
The, one month after a modified program was launched, the Food and Drug Administration announced on Jan. 14.
The IPMG has “created a new tool within the system to help resolve account access for some user groups without using the call center. This tool is intended to allow prescribers and designees to send login links directly to their patients’ desired email address through the Manage Patients page of the iPLEDGE REMS portal,” the FDA statement said.
“Prescribers can also send login links to their designees still having difficulty accessing their iPLEDGE account,” and users should check their emails for messages from iPLEDGE, including spam folders, the FDA advises. The iPLEDGE strategy is designed to prevent fetal exposure to isotretinoin, which is highly teratogenic.
Days after the new, gender-neutral approach to the isotretinoin risk mitigation program was launched on Dec. 13, the FDA convened an emergency meeting with representatives from the American Academy of Dermatology Association (AADA) to discuss the problematic rollout of the program, which was described as disastrous, chaotic, and a failure, with dermatologists on Twitter and elsewhere expressing anger and frustration over not being able to access the program or reach the call center.
A statement by the FDA on Dec. 23 followed, urging manufacturers to develop solutions for the website and to work with the AADA and pharmacy organizations to find solutions that would minimize treatment interruptions during the transition.
The modified REMS, launched on Dec. 13, is designed to make it more inclusive for transgender patients prescribed isotretinoin. Instead of three risk categories (females of reproductive potential, females not of reproductive potential, and males), patients who are prescribed isotretinoin for acne are assigned to one of two risk categories: those who can get pregnant and those who cannot get pregnant.
In the Jan. 14 statement, the FDA notes that the agency is continuing to work with the IPMG regarding the problems clinicians, pharmacists, and patients have had with accessing iPLEDGE over the last month.
“Although there has been progress, there is a significant amount of work still to be done,” the FDA acknowledged. “While we consider potential steps within the scope of FDA’s authorities, we will continue to meet with the IPMG for updates on the status of the problems with the iPLEDGE REMS and their progress towards having the system work as intended for all users.”
The, one month after a modified program was launched, the Food and Drug Administration announced on Jan. 14.
The IPMG has “created a new tool within the system to help resolve account access for some user groups without using the call center. This tool is intended to allow prescribers and designees to send login links directly to their patients’ desired email address through the Manage Patients page of the iPLEDGE REMS portal,” the FDA statement said.
“Prescribers can also send login links to their designees still having difficulty accessing their iPLEDGE account,” and users should check their emails for messages from iPLEDGE, including spam folders, the FDA advises. The iPLEDGE strategy is designed to prevent fetal exposure to isotretinoin, which is highly teratogenic.
Days after the new, gender-neutral approach to the isotretinoin risk mitigation program was launched on Dec. 13, the FDA convened an emergency meeting with representatives from the American Academy of Dermatology Association (AADA) to discuss the problematic rollout of the program, which was described as disastrous, chaotic, and a failure, with dermatologists on Twitter and elsewhere expressing anger and frustration over not being able to access the program or reach the call center.
A statement by the FDA on Dec. 23 followed, urging manufacturers to develop solutions for the website and to work with the AADA and pharmacy organizations to find solutions that would minimize treatment interruptions during the transition.
The modified REMS, launched on Dec. 13, is designed to make it more inclusive for transgender patients prescribed isotretinoin. Instead of three risk categories (females of reproductive potential, females not of reproductive potential, and males), patients who are prescribed isotretinoin for acne are assigned to one of two risk categories: those who can get pregnant and those who cannot get pregnant.
In the Jan. 14 statement, the FDA notes that the agency is continuing to work with the IPMG regarding the problems clinicians, pharmacists, and patients have had with accessing iPLEDGE over the last month.
“Although there has been progress, there is a significant amount of work still to be done,” the FDA acknowledged. “While we consider potential steps within the scope of FDA’s authorities, we will continue to meet with the IPMG for updates on the status of the problems with the iPLEDGE REMS and their progress towards having the system work as intended for all users.”
Parent group warns of social media/eating disorders link
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
Pediatric depression and parents
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
Increased electronic media use and youth suicidality: What can clinicians do?
Pediatric suicide was an emerging public health crisis prior to COVID-19, and recent data indicate that pediatric suicide attempts continued to increase during the pandemic.1 In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for pediatric mental health because of a surge in youth suicide attempts.2 Isolation mediated by the degradation of community and exacerbated by the pandemic, has been identified as a contributor to increasing pediatric suicidality.
It is impossible to understand this current public health crisis and to seek solutions without recognizing the ways in which the degradation of community and consequent social isolation play a central role. While the degradation of community and the isolation epidemic that preceded COVID-19 have been mediated by multiple factors, one factor associated with mental health problems in youth is electronic media use.3 During COVID-19, when physical distancing and virtual learning have been necessary to curb the spread, electronic media use has increased exponentially in the pediatric demographic. Some of this increase in screen time has been attributable to virtual schooling, but electronic devices also have become the only means by which kids can stay in contact with one another. While electronic communication has been viewed as an antidote to isolation, disturbing consequences associated with electronic media use have also been noted in our pediatric population.
In the health care system where I (P.L.L.) work as a pediatrician and a child and adolescent psychiatrist, electronic media use has been implicated in more than 90% of our inpatient admissions for suicidal ideation. Use of electronic devices has contributed to suicidal thoughts and attempts in most patients admitted to our acute crisis stabilization unit over the past year. During the pandemic, and in the absence of meaningful interpersonal interactions, many in our pediatric population have become even more dependent on electronic devices to cope with isolation. This has created an often-devastating irony, where the very devices already associated with mental health problems in youth are now being endorsed as “necessary” by mental health professionals.
So how does electronic media use relate to isolation and the continued degradation of community, and why might electronic media use be exacerbating pediatric suicide? One way we have coped with the deterioration of our communities has been the creation of the synthetic community-substitutes found on electronic devices. Unfortunately, our electronic devices create only an illusion of community, where interpersonal interaction occurs by way of inanimate objects, and by electronic text and ideograms. These become substitutes for genuine intimacy, personal contact, and reciprocity. Instead of engaging with one another, our youth are spending hours daily in isolation engaging with a piece of plastic. The mirage generated by pixels on a plastic screen creates an illusion of connectivity, but in reality, this only increases the isolation of our youth.
Human evolution and connection
Intimate social connectivity, woven together in our communities, was a fundamental mechanism for human survival. Historically, for our hunter-gatherer ancestors, the community provided access to our fundamental needs, such as safety from predators and access to substantive nutrition.4 Community allowed our ancestors to survive and procreate, and facilitated their triumph over predation and disease.5 Our distinction as the dominant species on Earth has been afforded by our social connectivity. Unfortunately, in the virtual worlds of our electronic devices the intimate social connectivity of community is absent. Our children wander in isolation, left to navigate age-old evolutionary pressures in the absence of the fundamental advantage for our survival as a species.
Unlike the living, breathing bears and wolves that threatened our ancestors, in the virtual world of the electronic device children are stalked by invisible predators seeking sexual or monetary exploitation. Children are being consumed by digital advertising and social media platforms that perpetually reinforce the requirement of perfection, and they fall prey to cyberbullies who mercilessly disparage their imperfections. In their virtual worlds, where their value is predicated upon anonymous others’ opinions, they succumb to the idea that they will never be enough.6 Their fundamental needs of competence and relatedness go unmet, and they lose their sense of purpose, belonging, and often their will to live. More importantly, absent from their children’s virtual worlds, and preoccupied within their own, parents cannot protect their children from online predators, deflect the vicious attacks of cyberbullies, or reframe their children’s imperfections as distinctive or empowering. They are unable to provide their children with the substantive interpersonal contact necessary for resilience and that bolsters their self-worth.
Human beings are inherently social creatures, who regardless of era require community to meet their fundamental needs. As the duration of daily screen time steadily increases, our youth are spending more and more of their waking hours living in isolation in an electronic world. Without the protective social connectivity of community, they are hunted by online predators, and they are consumed by the predatory culture of perfectionism that is contradictory to the reciprocal caretaking necessary to support their healthy development. Evolutionary biology informs us that, when children are isolated, they are susceptible to predation and disease. And in the socialized isolation of their electronic worlds, they are succumbing to predation and to the depressive diseases that are exacerbating the pediatric mental health crisis.
Creating and building community amid a pandemic has been challenging at best. However, now that we have better tools to fight COVID, it is important to encourage our young patients to reduce their nonacademic screen time, and to get outside and engage with others. Their mental health depends on it.
Dr. Loper is a pediatrician and child and adolescent psychiatrist at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. Dr. Loper has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
References
1. MMWR. 2021 Jun 18;70(24):888-94.
2. Ray G. “Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health.” Childrenshospitals.org. 2021 Oct 19.
3. JAMA Netw Open. 2020(8):e2011381.
4. Am J Phys Anthropol. 2018 April:165(4):777-800.
5. The influence of predation on primate and early human evolution: Impetus for cooperation, in “Origins of Altruism and Cooperation. Developments in Primatology: Progress and Prospects.” (Basingstoke, England: Springer Nature, 2011, pp. 19-40).
6. Media Psychology. 2020;23(1):52-78.
Pediatric suicide was an emerging public health crisis prior to COVID-19, and recent data indicate that pediatric suicide attempts continued to increase during the pandemic.1 In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for pediatric mental health because of a surge in youth suicide attempts.2 Isolation mediated by the degradation of community and exacerbated by the pandemic, has been identified as a contributor to increasing pediatric suicidality.
It is impossible to understand this current public health crisis and to seek solutions without recognizing the ways in which the degradation of community and consequent social isolation play a central role. While the degradation of community and the isolation epidemic that preceded COVID-19 have been mediated by multiple factors, one factor associated with mental health problems in youth is electronic media use.3 During COVID-19, when physical distancing and virtual learning have been necessary to curb the spread, electronic media use has increased exponentially in the pediatric demographic. Some of this increase in screen time has been attributable to virtual schooling, but electronic devices also have become the only means by which kids can stay in contact with one another. While electronic communication has been viewed as an antidote to isolation, disturbing consequences associated with electronic media use have also been noted in our pediatric population.
In the health care system where I (P.L.L.) work as a pediatrician and a child and adolescent psychiatrist, electronic media use has been implicated in more than 90% of our inpatient admissions for suicidal ideation. Use of electronic devices has contributed to suicidal thoughts and attempts in most patients admitted to our acute crisis stabilization unit over the past year. During the pandemic, and in the absence of meaningful interpersonal interactions, many in our pediatric population have become even more dependent on electronic devices to cope with isolation. This has created an often-devastating irony, where the very devices already associated with mental health problems in youth are now being endorsed as “necessary” by mental health professionals.
So how does electronic media use relate to isolation and the continued degradation of community, and why might electronic media use be exacerbating pediatric suicide? One way we have coped with the deterioration of our communities has been the creation of the synthetic community-substitutes found on electronic devices. Unfortunately, our electronic devices create only an illusion of community, where interpersonal interaction occurs by way of inanimate objects, and by electronic text and ideograms. These become substitutes for genuine intimacy, personal contact, and reciprocity. Instead of engaging with one another, our youth are spending hours daily in isolation engaging with a piece of plastic. The mirage generated by pixels on a plastic screen creates an illusion of connectivity, but in reality, this only increases the isolation of our youth.
Human evolution and connection
Intimate social connectivity, woven together in our communities, was a fundamental mechanism for human survival. Historically, for our hunter-gatherer ancestors, the community provided access to our fundamental needs, such as safety from predators and access to substantive nutrition.4 Community allowed our ancestors to survive and procreate, and facilitated their triumph over predation and disease.5 Our distinction as the dominant species on Earth has been afforded by our social connectivity. Unfortunately, in the virtual worlds of our electronic devices the intimate social connectivity of community is absent. Our children wander in isolation, left to navigate age-old evolutionary pressures in the absence of the fundamental advantage for our survival as a species.
Unlike the living, breathing bears and wolves that threatened our ancestors, in the virtual world of the electronic device children are stalked by invisible predators seeking sexual or monetary exploitation. Children are being consumed by digital advertising and social media platforms that perpetually reinforce the requirement of perfection, and they fall prey to cyberbullies who mercilessly disparage their imperfections. In their virtual worlds, where their value is predicated upon anonymous others’ opinions, they succumb to the idea that they will never be enough.6 Their fundamental needs of competence and relatedness go unmet, and they lose their sense of purpose, belonging, and often their will to live. More importantly, absent from their children’s virtual worlds, and preoccupied within their own, parents cannot protect their children from online predators, deflect the vicious attacks of cyberbullies, or reframe their children’s imperfections as distinctive or empowering. They are unable to provide their children with the substantive interpersonal contact necessary for resilience and that bolsters their self-worth.
Human beings are inherently social creatures, who regardless of era require community to meet their fundamental needs. As the duration of daily screen time steadily increases, our youth are spending more and more of their waking hours living in isolation in an electronic world. Without the protective social connectivity of community, they are hunted by online predators, and they are consumed by the predatory culture of perfectionism that is contradictory to the reciprocal caretaking necessary to support their healthy development. Evolutionary biology informs us that, when children are isolated, they are susceptible to predation and disease. And in the socialized isolation of their electronic worlds, they are succumbing to predation and to the depressive diseases that are exacerbating the pediatric mental health crisis.
Creating and building community amid a pandemic has been challenging at best. However, now that we have better tools to fight COVID, it is important to encourage our young patients to reduce their nonacademic screen time, and to get outside and engage with others. Their mental health depends on it.
Dr. Loper is a pediatrician and child and adolescent psychiatrist at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. Dr. Loper has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
References
1. MMWR. 2021 Jun 18;70(24):888-94.
2. Ray G. “Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health.” Childrenshospitals.org. 2021 Oct 19.
3. JAMA Netw Open. 2020(8):e2011381.
4. Am J Phys Anthropol. 2018 April:165(4):777-800.
5. The influence of predation on primate and early human evolution: Impetus for cooperation, in “Origins of Altruism and Cooperation. Developments in Primatology: Progress and Prospects.” (Basingstoke, England: Springer Nature, 2011, pp. 19-40).
6. Media Psychology. 2020;23(1):52-78.
Pediatric suicide was an emerging public health crisis prior to COVID-19, and recent data indicate that pediatric suicide attempts continued to increase during the pandemic.1 In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for pediatric mental health because of a surge in youth suicide attempts.2 Isolation mediated by the degradation of community and exacerbated by the pandemic, has been identified as a contributor to increasing pediatric suicidality.
It is impossible to understand this current public health crisis and to seek solutions without recognizing the ways in which the degradation of community and consequent social isolation play a central role. While the degradation of community and the isolation epidemic that preceded COVID-19 have been mediated by multiple factors, one factor associated with mental health problems in youth is electronic media use.3 During COVID-19, when physical distancing and virtual learning have been necessary to curb the spread, electronic media use has increased exponentially in the pediatric demographic. Some of this increase in screen time has been attributable to virtual schooling, but electronic devices also have become the only means by which kids can stay in contact with one another. While electronic communication has been viewed as an antidote to isolation, disturbing consequences associated with electronic media use have also been noted in our pediatric population.
In the health care system where I (P.L.L.) work as a pediatrician and a child and adolescent psychiatrist, electronic media use has been implicated in more than 90% of our inpatient admissions for suicidal ideation. Use of electronic devices has contributed to suicidal thoughts and attempts in most patients admitted to our acute crisis stabilization unit over the past year. During the pandemic, and in the absence of meaningful interpersonal interactions, many in our pediatric population have become even more dependent on electronic devices to cope with isolation. This has created an often-devastating irony, where the very devices already associated with mental health problems in youth are now being endorsed as “necessary” by mental health professionals.
So how does electronic media use relate to isolation and the continued degradation of community, and why might electronic media use be exacerbating pediatric suicide? One way we have coped with the deterioration of our communities has been the creation of the synthetic community-substitutes found on electronic devices. Unfortunately, our electronic devices create only an illusion of community, where interpersonal interaction occurs by way of inanimate objects, and by electronic text and ideograms. These become substitutes for genuine intimacy, personal contact, and reciprocity. Instead of engaging with one another, our youth are spending hours daily in isolation engaging with a piece of plastic. The mirage generated by pixels on a plastic screen creates an illusion of connectivity, but in reality, this only increases the isolation of our youth.
Human evolution and connection
Intimate social connectivity, woven together in our communities, was a fundamental mechanism for human survival. Historically, for our hunter-gatherer ancestors, the community provided access to our fundamental needs, such as safety from predators and access to substantive nutrition.4 Community allowed our ancestors to survive and procreate, and facilitated their triumph over predation and disease.5 Our distinction as the dominant species on Earth has been afforded by our social connectivity. Unfortunately, in the virtual worlds of our electronic devices the intimate social connectivity of community is absent. Our children wander in isolation, left to navigate age-old evolutionary pressures in the absence of the fundamental advantage for our survival as a species.
Unlike the living, breathing bears and wolves that threatened our ancestors, in the virtual world of the electronic device children are stalked by invisible predators seeking sexual or monetary exploitation. Children are being consumed by digital advertising and social media platforms that perpetually reinforce the requirement of perfection, and they fall prey to cyberbullies who mercilessly disparage their imperfections. In their virtual worlds, where their value is predicated upon anonymous others’ opinions, they succumb to the idea that they will never be enough.6 Their fundamental needs of competence and relatedness go unmet, and they lose their sense of purpose, belonging, and often their will to live. More importantly, absent from their children’s virtual worlds, and preoccupied within their own, parents cannot protect their children from online predators, deflect the vicious attacks of cyberbullies, or reframe their children’s imperfections as distinctive or empowering. They are unable to provide their children with the substantive interpersonal contact necessary for resilience and that bolsters their self-worth.
Human beings are inherently social creatures, who regardless of era require community to meet their fundamental needs. As the duration of daily screen time steadily increases, our youth are spending more and more of their waking hours living in isolation in an electronic world. Without the protective social connectivity of community, they are hunted by online predators, and they are consumed by the predatory culture of perfectionism that is contradictory to the reciprocal caretaking necessary to support their healthy development. Evolutionary biology informs us that, when children are isolated, they are susceptible to predation and disease. And in the socialized isolation of their electronic worlds, they are succumbing to predation and to the depressive diseases that are exacerbating the pediatric mental health crisis.
Creating and building community amid a pandemic has been challenging at best. However, now that we have better tools to fight COVID, it is important to encourage our young patients to reduce their nonacademic screen time, and to get outside and engage with others. Their mental health depends on it.
Dr. Loper is a pediatrician and child and adolescent psychiatrist at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. Dr. Loper has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
References
1. MMWR. 2021 Jun 18;70(24):888-94.
2. Ray G. “Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health.” Childrenshospitals.org. 2021 Oct 19.
3. JAMA Netw Open. 2020(8):e2011381.
4. Am J Phys Anthropol. 2018 April:165(4):777-800.
5. The influence of predation on primate and early human evolution: Impetus for cooperation, in “Origins of Altruism and Cooperation. Developments in Primatology: Progress and Prospects.” (Basingstoke, England: Springer Nature, 2011, pp. 19-40).
6. Media Psychology. 2020;23(1):52-78.
Changing terminology in LGBTQ+ spaces: How to keep up with the lingo
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
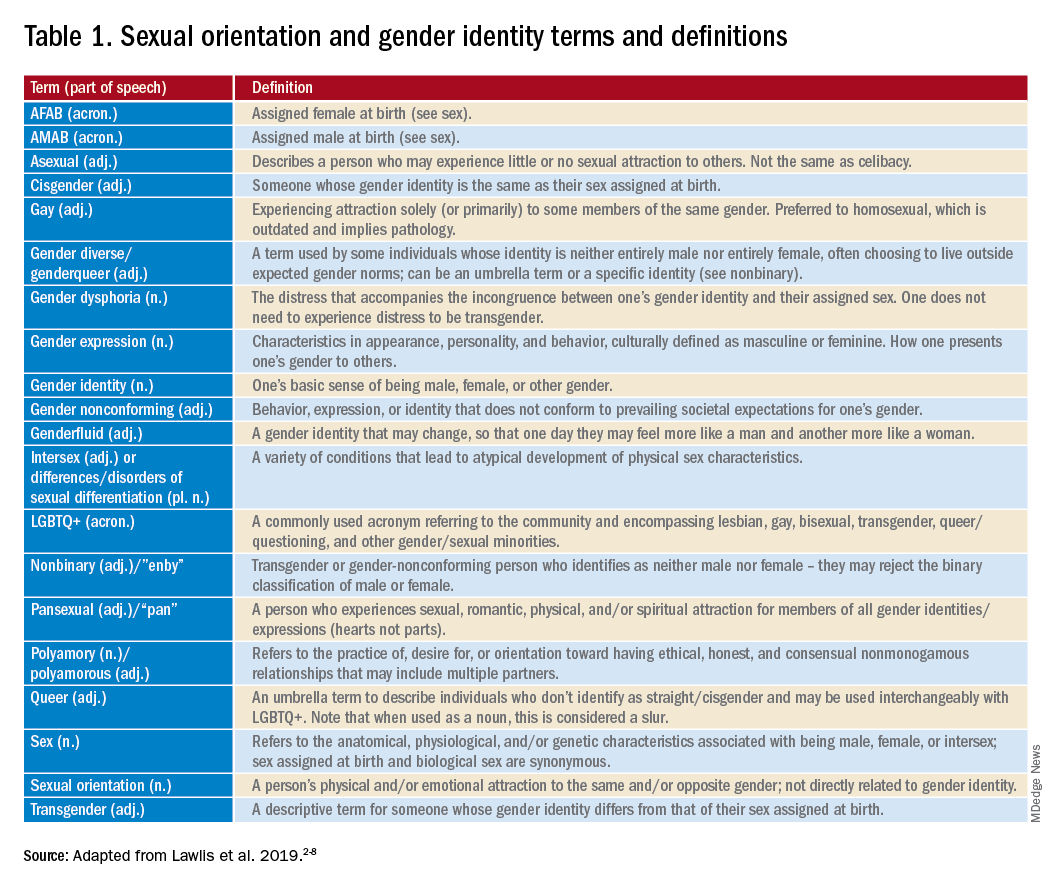
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
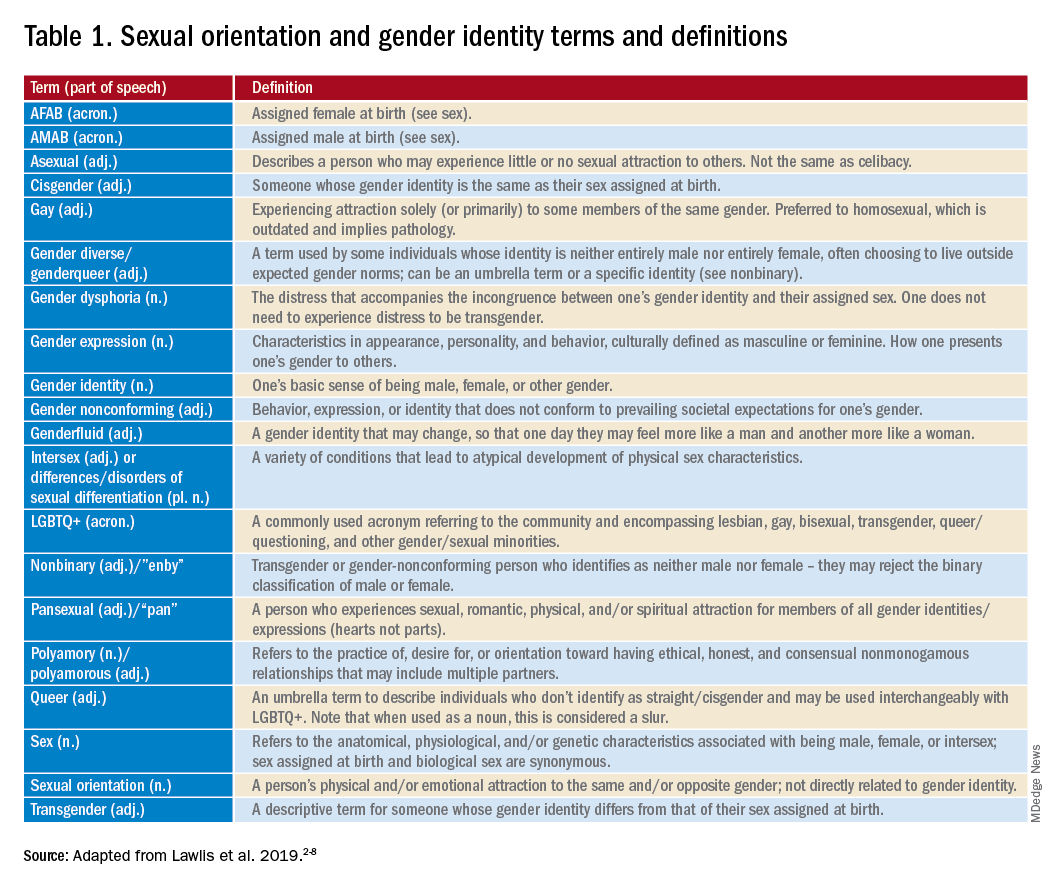
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
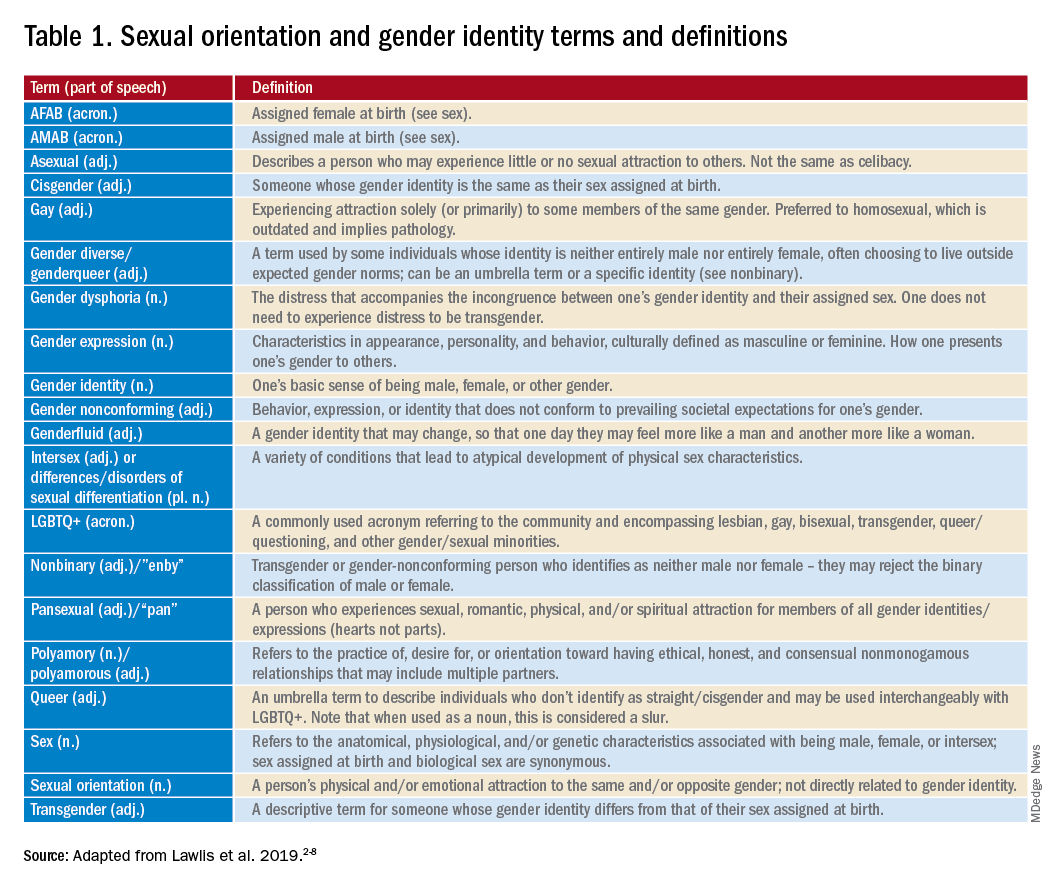
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.

















