User login
Child abuse tied to persistent inflammation in later life
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data on worldwide mental health impact of COVID-19
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
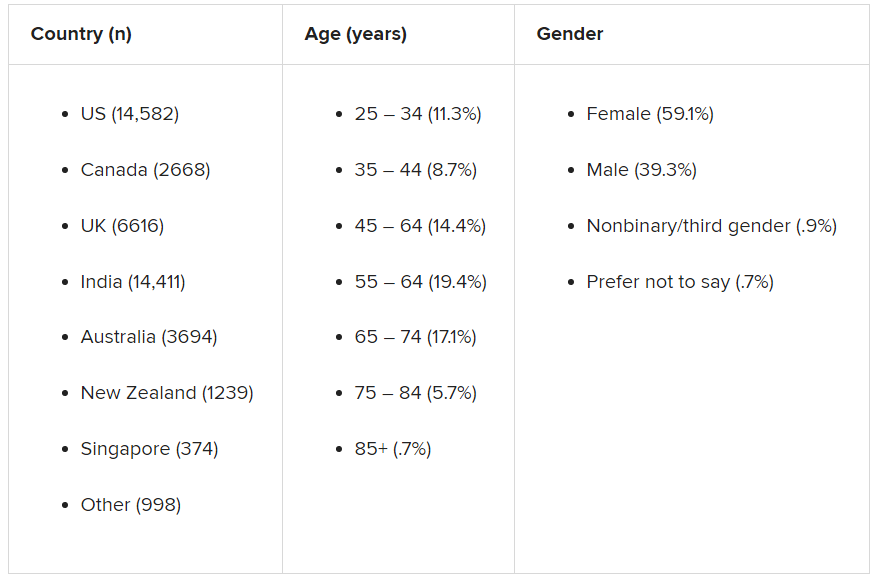
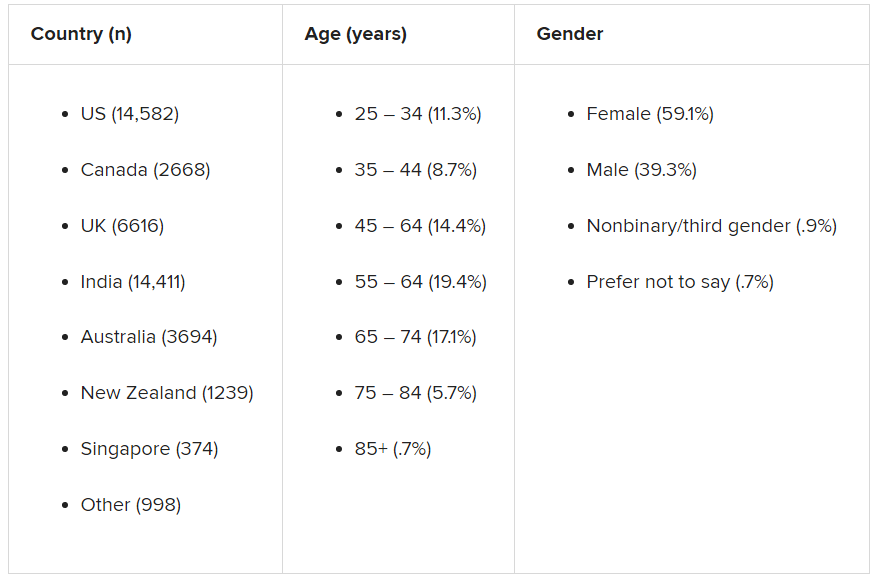
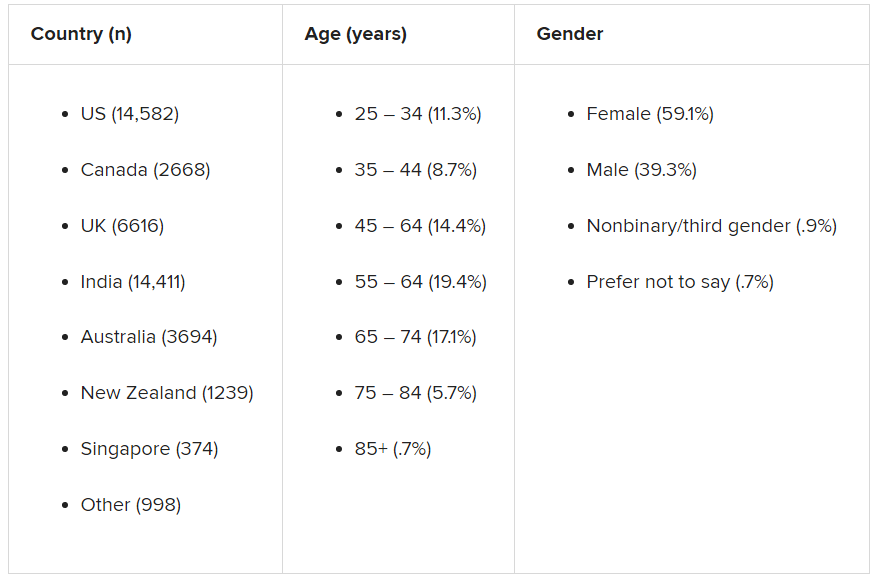
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Tips to share with patients feeling vaccine FOMO
COVID-19 has filled our lives with so many challenges, and now we are faced with a new one. For some of our patients, getting a vaccine appointment feels a lot like winning the lottery.
At first, it might have been easy to be joyful for others’ good fortune, but after weeks and now months of seeing others get vaccinated, patience can wear thin. It also creates an imbalance when one member of a “bubble” is vaccinated and others aren’t. It can be painful to be the one who continues to miss out on activities as those around resume pleasures such as seeing friends, dining out, shopping, and traveling.
So many of our patients are feeling worn down from the chronic stress and are not in the best shape to deal with another issue: the fear of missing out. Yet,
Here are some tips to share with patients who are feeling vaccine envy.
- Acknowledge your feelings. Sure, you want to be happy for those getting vaccinated but it does hurt to be left behind. These feelings are real and deserve space. Share them with a trusted friend or therapist. It is indeed quite upsetting to have to wait. In the United States, we are used to having speedy access to medical care. It is unfortunate that so many have to wait for such an important intervention. You have a right to be upset.
- Express your concern to the family member or friend who is vaccinated. Discuss how it could affect your relationship and activities.
- Focus on what you can control. Double down on efforts to not catch or spread COVID. Vaccines are only one very modern way out of the pandemic. Stick to the basics so you feel a sense of control over your health destiny.
- Take advantage of the remaining days or weeks of quarantine. What did you want to accomplish during your time of limited activity? Did you always want to play the piano? These last slower days or weeks might be a great time to try (over Zoom of course). Have you put off cleaning your closet and organizing your drawers? There is nothing like a deadline to kick us into gear.
- Take your best guess for when you will be vaccinated and start to plan. Start to make those plans for late summer and fall.
- Keep things in perspective. We are ALL so fortunate that several vaccines were developed so quickly. Even if the wait is a few more weeks, an end is in sight. One year ago, we had no idea what lay ahead and the uncertainty caused so much anxiety. Now we can feel hopeful that more “normal days” will be returning soon in a predictable time frame.
- Focus on the herd. By now we know that “we are all in this together.” Although we aren’t leaving at the exact same time, mere months will separate us. The more our friends and family get vaccinated, the safer we all are.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018).
COVID-19 has filled our lives with so many challenges, and now we are faced with a new one. For some of our patients, getting a vaccine appointment feels a lot like winning the lottery.
At first, it might have been easy to be joyful for others’ good fortune, but after weeks and now months of seeing others get vaccinated, patience can wear thin. It also creates an imbalance when one member of a “bubble” is vaccinated and others aren’t. It can be painful to be the one who continues to miss out on activities as those around resume pleasures such as seeing friends, dining out, shopping, and traveling.
So many of our patients are feeling worn down from the chronic stress and are not in the best shape to deal with another issue: the fear of missing out. Yet,
Here are some tips to share with patients who are feeling vaccine envy.
- Acknowledge your feelings. Sure, you want to be happy for those getting vaccinated but it does hurt to be left behind. These feelings are real and deserve space. Share them with a trusted friend or therapist. It is indeed quite upsetting to have to wait. In the United States, we are used to having speedy access to medical care. It is unfortunate that so many have to wait for such an important intervention. You have a right to be upset.
- Express your concern to the family member or friend who is vaccinated. Discuss how it could affect your relationship and activities.
- Focus on what you can control. Double down on efforts to not catch or spread COVID. Vaccines are only one very modern way out of the pandemic. Stick to the basics so you feel a sense of control over your health destiny.
- Take advantage of the remaining days or weeks of quarantine. What did you want to accomplish during your time of limited activity? Did you always want to play the piano? These last slower days or weeks might be a great time to try (over Zoom of course). Have you put off cleaning your closet and organizing your drawers? There is nothing like a deadline to kick us into gear.
- Take your best guess for when you will be vaccinated and start to plan. Start to make those plans for late summer and fall.
- Keep things in perspective. We are ALL so fortunate that several vaccines were developed so quickly. Even if the wait is a few more weeks, an end is in sight. One year ago, we had no idea what lay ahead and the uncertainty caused so much anxiety. Now we can feel hopeful that more “normal days” will be returning soon in a predictable time frame.
- Focus on the herd. By now we know that “we are all in this together.” Although we aren’t leaving at the exact same time, mere months will separate us. The more our friends and family get vaccinated, the safer we all are.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018).
COVID-19 has filled our lives with so many challenges, and now we are faced with a new one. For some of our patients, getting a vaccine appointment feels a lot like winning the lottery.
At first, it might have been easy to be joyful for others’ good fortune, but after weeks and now months of seeing others get vaccinated, patience can wear thin. It also creates an imbalance when one member of a “bubble” is vaccinated and others aren’t. It can be painful to be the one who continues to miss out on activities as those around resume pleasures such as seeing friends, dining out, shopping, and traveling.
So many of our patients are feeling worn down from the chronic stress and are not in the best shape to deal with another issue: the fear of missing out. Yet,
Here are some tips to share with patients who are feeling vaccine envy.
- Acknowledge your feelings. Sure, you want to be happy for those getting vaccinated but it does hurt to be left behind. These feelings are real and deserve space. Share them with a trusted friend or therapist. It is indeed quite upsetting to have to wait. In the United States, we are used to having speedy access to medical care. It is unfortunate that so many have to wait for such an important intervention. You have a right to be upset.
- Express your concern to the family member or friend who is vaccinated. Discuss how it could affect your relationship and activities.
- Focus on what you can control. Double down on efforts to not catch or spread COVID. Vaccines are only one very modern way out of the pandemic. Stick to the basics so you feel a sense of control over your health destiny.
- Take advantage of the remaining days or weeks of quarantine. What did you want to accomplish during your time of limited activity? Did you always want to play the piano? These last slower days or weeks might be a great time to try (over Zoom of course). Have you put off cleaning your closet and organizing your drawers? There is nothing like a deadline to kick us into gear.
- Take your best guess for when you will be vaccinated and start to plan. Start to make those plans for late summer and fall.
- Keep things in perspective. We are ALL so fortunate that several vaccines were developed so quickly. Even if the wait is a few more weeks, an end is in sight. One year ago, we had no idea what lay ahead and the uncertainty caused so much anxiety. Now we can feel hopeful that more “normal days” will be returning soon in a predictable time frame.
- Focus on the herd. By now we know that “we are all in this together.” Although we aren’t leaving at the exact same time, mere months will separate us. The more our friends and family get vaccinated, the safer we all are.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018).
Buprenorphine for OUD may also mitigate risk with concomitant benzo, Z-drug use
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Fauci worries about possible post–COVID-19 ‘mental health pandemic’
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Novel therapeutic target for depression identified
An antiseizure medication appears to reduce anhedonia in patients with depression via a novel mechanism that may offer a new therapeutic target for the disorder, new research suggests.
Results of a small, randomized trial show those who received ezogabine (Potiga) experienced a significant reduction in key measures of depression and anhedonia versus placebo.
Participants in the treatment group also showed a trend toward increased response to reward anticipation on functional MRI (fMRI), compared with those treated with placebo, although the effect did not reach statistical significance.
“Our study was the first randomized, placebo-controlled trial to show that a drug affecting this kind of ion channel in the brain can improve depression and anhedonia in patients,” senior investigator James Murrough, MD, PhD, associate professor of psychiatry and neuroscience at the Icahn School of Medicine at Mount Sinai, New York, said in a press release.
“Targeting this channel represents a completely different mechanism of action than any currently available antidepressant treatment,” said Dr. Murrough, who is also director of the Depression and Anxiety Center for Discovery and Treatment at Mount Sinai.
The study was published online March 3 in the American Journal of Psychiatry.
Need for a novel target
“One of the main issues in treating depression is that many of our current antidepressants have similar mechanisms of action,” Dr. Murrough said in an interview. “Once a patient hasn’t responded to currently available agents, it’s hard think of new medications to fill that need.”
This need for a novel target motivated Dr. Murrough and associates to research the KCNQ2/3 potassium channel, which has not been previously studied as a therapeutic target for depression.
The KCNQ2/3 channel controls brain cell excitability and function by controlling the flow of the electrical charge across the cell membrane in the form of potassium ions, Dr. Murrough explained.
Previous research using a chronic social defeat model of depression in mice showed changes in the KCNQ2/3 channel. “This was key to determining whether a mouse showed depressive behavior in the context of stress, or whether the mice were resistant or resilient to stress,” he said.
Mice resistant to stress showed increased markers in brain regions associated with reward, while the less resilient mice showed excessive excitability and dysfunction. Dysfunction in the brain’s reward system leads to anhedonia, a “core feature” of depressive disorders.
This inspired Dr. Murrough’s group to identify ezogabine, a drug that acts on this channel.
“ for addressing depressive symptoms,” Dr. Murrough said
Nonsignificant trend
The researchers studied 45 adults diagnosed with depression who exhibited significant anhedonia and at least moderate illness severity.
Participants were randomly assigned to receive either ezogabine (n = 21, mean age 44 years at enrollment, 28.3% male) or placebo (n = 24, mean age 39 years at enrollment, 50% male). At baseline and following treatment, participants completed the incentive flanker test under fMRI conditions to model brain activity during anticipation of a reward. In addition, clinical measures of depression and anhedonia were assessed at weekly visits.
The study groups did not differ significantly in performance accuracy during the fMRI task at baseline or following treatment. The table below summarizes the percentage of errors in each group, with standard deviation.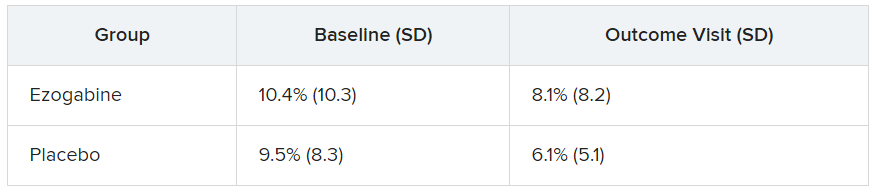
Participants in the ezogabine group showed a numerical increase in ventral striatum activation in response to reward anticipation, compared with participants in the placebo group, but this trend was not considered significant.
Heterogeneous condition
In contrast, there were notable improvements from baseline to the final outcome visit in clinical measures of depression and anhedonia in the ezogabine group, compared with the placebo group. Mean (SD) differences in depression scores, based on the MADRS (Montgomery-Åsberg Depression Rating Scale) from baseline to endpoint as follows: mean difference, –7.9 (3.0); effect size, 0.76; response rate, 61.9% (ezogabine) and 37.5% (placebo); remission rate: 38.1% (ezogabine) and 20.8% (placebo)
Compared with placebo, there were also large improvements in hedonic capacity, as measured by the Snaith-Hamilton Pleasure Scale and the anticipatory subscale of the Temporal Experience of Pleasure Scale (t, –4.1; df, 212; P < .001 and t, 3.4; df, 213; P < .001, respectively).
Compared with placebo, ezogabine was associated with “significant benefit” in global illness severity and improvement (Clinical Global Impression–Severity: t, –2.2; df, 214; P = .026 and CGI-Improvement: t, –2.9; d, 214; P = .004, respectively).
Ezogabine was well tolerated. Dizziness and headache were the most common adverse events.
Depression is a “heterogeneous condition” with a single diagnosis encompassing a “large, multifaceted” array of symptoms, Dr. Murrough noted. A growing body of research is focusing on specific components as potential treatment targets. “Our study looked specifically at patients with a diagnosis of depression but high scores on the anhedonia scale and we found that boosting the function of the KCNQ2/3 channel may have a beneficial antidepressant effect by improving anhedonia.”
Potential gain
In a comment, Alan Schatzberg, MD, professor in the department of psychiatry and behavioral sciences at Stanford (Calif.) University, said that “anytime there’s a new treatment with a new mechanism of action for a given condition, there’s a potential gain for the field.”
Dr. Schatzberg, who was not involved with the study, said that ezogabine, with its “potentially new mechanism of action, seems to have an effect and reasonable safety and could be important for patients who may not respond to traditional medications. It might also be important for all sorts of patients, depending on findings of later trials.”
Dr. Murrough said that ezogabine in still in “early stages” of research. “We hope that future studies will look at other agents that would also affect this channel,” he added.
This research was supported by the National Institute of Mental Health. Additional funding was provided by the Friedman Brain Institute at the Icahn School of Medicine at Mount Sinai and the Ehrenkranz Laboratory for Human Resilience, a component of the Depression and Anxiety Center for Discovery and Treatment at the Icahn School of Medicine at Mount Sinai. Dr. Murrough is an inventor of a pending patent application for the use of ezogabine and other KCNQ channel openers to treat depression and related disorders. Dr. Schatzberg disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An antiseizure medication appears to reduce anhedonia in patients with depression via a novel mechanism that may offer a new therapeutic target for the disorder, new research suggests.
Results of a small, randomized trial show those who received ezogabine (Potiga) experienced a significant reduction in key measures of depression and anhedonia versus placebo.
Participants in the treatment group also showed a trend toward increased response to reward anticipation on functional MRI (fMRI), compared with those treated with placebo, although the effect did not reach statistical significance.
“Our study was the first randomized, placebo-controlled trial to show that a drug affecting this kind of ion channel in the brain can improve depression and anhedonia in patients,” senior investigator James Murrough, MD, PhD, associate professor of psychiatry and neuroscience at the Icahn School of Medicine at Mount Sinai, New York, said in a press release.
“Targeting this channel represents a completely different mechanism of action than any currently available antidepressant treatment,” said Dr. Murrough, who is also director of the Depression and Anxiety Center for Discovery and Treatment at Mount Sinai.
The study was published online March 3 in the American Journal of Psychiatry.
Need for a novel target
“One of the main issues in treating depression is that many of our current antidepressants have similar mechanisms of action,” Dr. Murrough said in an interview. “Once a patient hasn’t responded to currently available agents, it’s hard think of new medications to fill that need.”
This need for a novel target motivated Dr. Murrough and associates to research the KCNQ2/3 potassium channel, which has not been previously studied as a therapeutic target for depression.
The KCNQ2/3 channel controls brain cell excitability and function by controlling the flow of the electrical charge across the cell membrane in the form of potassium ions, Dr. Murrough explained.
Previous research using a chronic social defeat model of depression in mice showed changes in the KCNQ2/3 channel. “This was key to determining whether a mouse showed depressive behavior in the context of stress, or whether the mice were resistant or resilient to stress,” he said.
Mice resistant to stress showed increased markers in brain regions associated with reward, while the less resilient mice showed excessive excitability and dysfunction. Dysfunction in the brain’s reward system leads to anhedonia, a “core feature” of depressive disorders.
This inspired Dr. Murrough’s group to identify ezogabine, a drug that acts on this channel.
“ for addressing depressive symptoms,” Dr. Murrough said
Nonsignificant trend
The researchers studied 45 adults diagnosed with depression who exhibited significant anhedonia and at least moderate illness severity.
Participants were randomly assigned to receive either ezogabine (n = 21, mean age 44 years at enrollment, 28.3% male) or placebo (n = 24, mean age 39 years at enrollment, 50% male). At baseline and following treatment, participants completed the incentive flanker test under fMRI conditions to model brain activity during anticipation of a reward. In addition, clinical measures of depression and anhedonia were assessed at weekly visits.
The study groups did not differ significantly in performance accuracy during the fMRI task at baseline or following treatment. The table below summarizes the percentage of errors in each group, with standard deviation.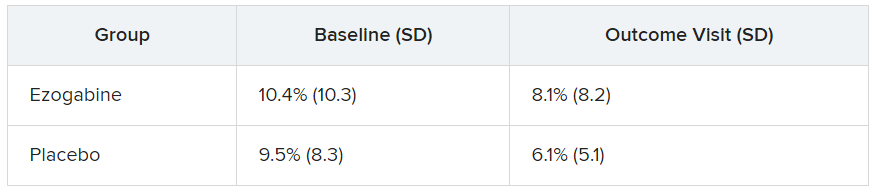
Participants in the ezogabine group showed a numerical increase in ventral striatum activation in response to reward anticipation, compared with participants in the placebo group, but this trend was not considered significant.
Heterogeneous condition
In contrast, there were notable improvements from baseline to the final outcome visit in clinical measures of depression and anhedonia in the ezogabine group, compared with the placebo group. Mean (SD) differences in depression scores, based on the MADRS (Montgomery-Åsberg Depression Rating Scale) from baseline to endpoint as follows: mean difference, –7.9 (3.0); effect size, 0.76; response rate, 61.9% (ezogabine) and 37.5% (placebo); remission rate: 38.1% (ezogabine) and 20.8% (placebo)
Compared with placebo, there were also large improvements in hedonic capacity, as measured by the Snaith-Hamilton Pleasure Scale and the anticipatory subscale of the Temporal Experience of Pleasure Scale (t, –4.1; df, 212; P < .001 and t, 3.4; df, 213; P < .001, respectively).
Compared with placebo, ezogabine was associated with “significant benefit” in global illness severity and improvement (Clinical Global Impression–Severity: t, –2.2; df, 214; P = .026 and CGI-Improvement: t, –2.9; d, 214; P = .004, respectively).
Ezogabine was well tolerated. Dizziness and headache were the most common adverse events.
Depression is a “heterogeneous condition” with a single diagnosis encompassing a “large, multifaceted” array of symptoms, Dr. Murrough noted. A growing body of research is focusing on specific components as potential treatment targets. “Our study looked specifically at patients with a diagnosis of depression but high scores on the anhedonia scale and we found that boosting the function of the KCNQ2/3 channel may have a beneficial antidepressant effect by improving anhedonia.”
Potential gain
In a comment, Alan Schatzberg, MD, professor in the department of psychiatry and behavioral sciences at Stanford (Calif.) University, said that “anytime there’s a new treatment with a new mechanism of action for a given condition, there’s a potential gain for the field.”
Dr. Schatzberg, who was not involved with the study, said that ezogabine, with its “potentially new mechanism of action, seems to have an effect and reasonable safety and could be important for patients who may not respond to traditional medications. It might also be important for all sorts of patients, depending on findings of later trials.”
Dr. Murrough said that ezogabine in still in “early stages” of research. “We hope that future studies will look at other agents that would also affect this channel,” he added.
This research was supported by the National Institute of Mental Health. Additional funding was provided by the Friedman Brain Institute at the Icahn School of Medicine at Mount Sinai and the Ehrenkranz Laboratory for Human Resilience, a component of the Depression and Anxiety Center for Discovery and Treatment at the Icahn School of Medicine at Mount Sinai. Dr. Murrough is an inventor of a pending patent application for the use of ezogabine and other KCNQ channel openers to treat depression and related disorders. Dr. Schatzberg disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An antiseizure medication appears to reduce anhedonia in patients with depression via a novel mechanism that may offer a new therapeutic target for the disorder, new research suggests.
Results of a small, randomized trial show those who received ezogabine (Potiga) experienced a significant reduction in key measures of depression and anhedonia versus placebo.
Participants in the treatment group also showed a trend toward increased response to reward anticipation on functional MRI (fMRI), compared with those treated with placebo, although the effect did not reach statistical significance.
“Our study was the first randomized, placebo-controlled trial to show that a drug affecting this kind of ion channel in the brain can improve depression and anhedonia in patients,” senior investigator James Murrough, MD, PhD, associate professor of psychiatry and neuroscience at the Icahn School of Medicine at Mount Sinai, New York, said in a press release.
“Targeting this channel represents a completely different mechanism of action than any currently available antidepressant treatment,” said Dr. Murrough, who is also director of the Depression and Anxiety Center for Discovery and Treatment at Mount Sinai.
The study was published online March 3 in the American Journal of Psychiatry.
Need for a novel target
“One of the main issues in treating depression is that many of our current antidepressants have similar mechanisms of action,” Dr. Murrough said in an interview. “Once a patient hasn’t responded to currently available agents, it’s hard think of new medications to fill that need.”
This need for a novel target motivated Dr. Murrough and associates to research the KCNQ2/3 potassium channel, which has not been previously studied as a therapeutic target for depression.
The KCNQ2/3 channel controls brain cell excitability and function by controlling the flow of the electrical charge across the cell membrane in the form of potassium ions, Dr. Murrough explained.
Previous research using a chronic social defeat model of depression in mice showed changes in the KCNQ2/3 channel. “This was key to determining whether a mouse showed depressive behavior in the context of stress, or whether the mice were resistant or resilient to stress,” he said.
Mice resistant to stress showed increased markers in brain regions associated with reward, while the less resilient mice showed excessive excitability and dysfunction. Dysfunction in the brain’s reward system leads to anhedonia, a “core feature” of depressive disorders.
This inspired Dr. Murrough’s group to identify ezogabine, a drug that acts on this channel.
“ for addressing depressive symptoms,” Dr. Murrough said
Nonsignificant trend
The researchers studied 45 adults diagnosed with depression who exhibited significant anhedonia and at least moderate illness severity.
Participants were randomly assigned to receive either ezogabine (n = 21, mean age 44 years at enrollment, 28.3% male) or placebo (n = 24, mean age 39 years at enrollment, 50% male). At baseline and following treatment, participants completed the incentive flanker test under fMRI conditions to model brain activity during anticipation of a reward. In addition, clinical measures of depression and anhedonia were assessed at weekly visits.
The study groups did not differ significantly in performance accuracy during the fMRI task at baseline or following treatment. The table below summarizes the percentage of errors in each group, with standard deviation.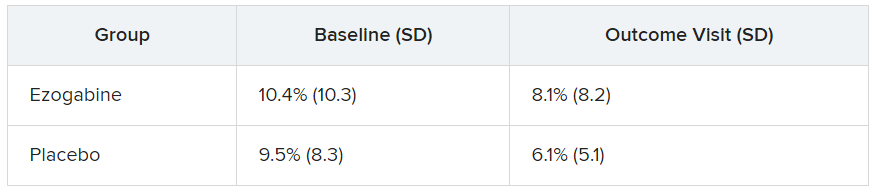
Participants in the ezogabine group showed a numerical increase in ventral striatum activation in response to reward anticipation, compared with participants in the placebo group, but this trend was not considered significant.
Heterogeneous condition
In contrast, there were notable improvements from baseline to the final outcome visit in clinical measures of depression and anhedonia in the ezogabine group, compared with the placebo group. Mean (SD) differences in depression scores, based on the MADRS (Montgomery-Åsberg Depression Rating Scale) from baseline to endpoint as follows: mean difference, –7.9 (3.0); effect size, 0.76; response rate, 61.9% (ezogabine) and 37.5% (placebo); remission rate: 38.1% (ezogabine) and 20.8% (placebo)
Compared with placebo, there were also large improvements in hedonic capacity, as measured by the Snaith-Hamilton Pleasure Scale and the anticipatory subscale of the Temporal Experience of Pleasure Scale (t, –4.1; df, 212; P < .001 and t, 3.4; df, 213; P < .001, respectively).
Compared with placebo, ezogabine was associated with “significant benefit” in global illness severity and improvement (Clinical Global Impression–Severity: t, –2.2; df, 214; P = .026 and CGI-Improvement: t, –2.9; d, 214; P = .004, respectively).
Ezogabine was well tolerated. Dizziness and headache were the most common adverse events.
Depression is a “heterogeneous condition” with a single diagnosis encompassing a “large, multifaceted” array of symptoms, Dr. Murrough noted. A growing body of research is focusing on specific components as potential treatment targets. “Our study looked specifically at patients with a diagnosis of depression but high scores on the anhedonia scale and we found that boosting the function of the KCNQ2/3 channel may have a beneficial antidepressant effect by improving anhedonia.”
Potential gain
In a comment, Alan Schatzberg, MD, professor in the department of psychiatry and behavioral sciences at Stanford (Calif.) University, said that “anytime there’s a new treatment with a new mechanism of action for a given condition, there’s a potential gain for the field.”
Dr. Schatzberg, who was not involved with the study, said that ezogabine, with its “potentially new mechanism of action, seems to have an effect and reasonable safety and could be important for patients who may not respond to traditional medications. It might also be important for all sorts of patients, depending on findings of later trials.”
Dr. Murrough said that ezogabine in still in “early stages” of research. “We hope that future studies will look at other agents that would also affect this channel,” he added.
This research was supported by the National Institute of Mental Health. Additional funding was provided by the Friedman Brain Institute at the Icahn School of Medicine at Mount Sinai and the Ehrenkranz Laboratory for Human Resilience, a component of the Depression and Anxiety Center for Discovery and Treatment at the Icahn School of Medicine at Mount Sinai. Dr. Murrough is an inventor of a pending patent application for the use of ezogabine and other KCNQ channel openers to treat depression and related disorders. Dr. Schatzberg disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How to make resident mental health care stigma free
Sarah Sofka, MD, FACP, noticed a pattern. As program director for the internal medicine (IM) residency at West Virginia University, Morgantown, she was informed when residents were sent to counseling because they were affected by burnout, depression, or anxiety. When trainees returned from these visits, many told her the same thing: They wished they had sought help sooner.
IM residents and their families had access to free counseling at WVU, but few used the resource, says Dr. Sofka. “So, we thought, let’s just schedule all of our residents for a therapy visit so they can go and see what it’s like,” she said. “This will hopefully decrease the stigma for seeking mental health care. If everybody’s going, it’s not a big deal.”
In July 2015, Dr. Sofka and her colleagues launched a universal well-being assessment program for the IM residents at WVU. The program leaders automatically scheduled first- and second-year residents for a visit to the faculty staff assistance program counselors. The visits were not mandatory, and residents could choose not to go; but if they did go, they received the entire day of their visit off from work.
Five and a half years after launching their program, Dr. Sofka and her colleagues conducted one of the first studies of the efficacy of an opt-out approach for resident mental wellness. They found that , suggesting that residents were seeking help proactively after having to at least consider it.
Opt-out counseling is a recent concept in residency programs – one that’s attracting interest from training programs across the country. Brown University, Providence, R.I.; the University of Colorado at Denver, Aurora; University of Pennsylvania, Philadelphia; and the University of California, San Francisco have at least one residency program that uses the approach.
Lisa Meeks, PhD, an assistant professor of family medicine at Michigan Medicine, in Ann Arbor, and other experts also believe opt-out counseling could decrease stigma and help normalize seeking care for mental health problems in the medical community while lowering the barriers for trainees who need help.
No time, no access, plenty of stigma
Burnout and mental health are known to be major concerns for health care workers, especially trainees. College graduates starting medical education have lower rates of burnout and depression, compared with demographically matched peers; however, once they’ve started training, medical students, residents, and fellows are more likely to be burned out and exhibit symptoms of depression. The ongoing COVID-19 pandemic is further fraying the well-being of overworked and traumatized health care professionals, and experts predict a mental health crisis will follow the viral crisis.
The Accreditation Council for Graduate Medical Education recently mandated that programs offer wellness services to trainees. Yet this doesn’t mean they are always used; well-known barriers stand between residents, medical students, and physicians and their receiving effective mental health treatment.
Two of the most obvious are access and time, given the grueling and often inflexible schedules of most trainees, says Jessica Gold, MD, a psychiatrist at Washington University, St. Louis, who specializes in treating medical professionals. Dr. Gold also points out that, to be done correctly, these programs require institutional support and investment – resources that aren’t always adequate.
“A lack of transparency and clear messaging around what is available, who provides the services, and how to access these services can be a major barrier,” says Erene Stergiopoulos, MD, a second-year psychiatry resident at the University of Toronto. In addition, there can be considerable lag between when a resident realizes they need help and when they manage to find a provider and schedule an appointment, says Dr. Meeks.
Even when these logistical barriers are overcome, trainees and physicians have to contend with the persistent stigma associated with mental health treatment in the culture of medicine, says Dr. Gold. A recent survey by the American College of Emergency Physicians found that 73% of surveyed physicians feel there is stigma in their workplace about seeking mental health treatment. Many state medical licensing boards still require physicians to disclose mental health treatment, which discourages many trainees and providers from seeking proactive care, says Mary Moffit, PhD, associate professor of psychiatry and director of the resident and faculty wellness program at Oregon Health & Science University, Portland.
How the opt-out approach works
“The idea is by making it opt-out, you really normalize it,” says Maneesh Batra, MD, MPH, associate director of the University of Washington, Seattle, Children’s Hospital residency program. Similar approaches have proven effective at shaping human behavior in other health care settings, including boosting testing rates for HIV and increasing immunization rates for childhood vaccines, Dr. Batra says.
In general, opt-out programs acknowledge that people are busy and won’t take that extra step or click that extra button if they don’t have to, says Oana Tomescu, MD, PhD, associate professor of clinical medicine and pediatrics at the University of Pennsylvania, Philadelphia.
In 2018, Dr. Sofka and her colleagues at WVU conducted a survey that showed that a majority of residents thought favorably of their opt-out program and said they would return to counseling for follow-up care. In their most recent study, published in the Journal of Graduate Medical Education in 2021, Dr. Sofka and her colleagues found that residents did just that – only 8 of 239 opted out of universally scheduled visits. Resident-initiated visits increased significantly from zero during the 2014-2015 academic year to 23 in 2018-2019. Between those periods, program-mandated visits decreased significantly from 12 to 3.
The initiative has succeeded in creating a culture of openness and caring at WVU, says 2nd-year internal medicine resident Nistha Modi, MD. “It sets the tone for the program – we talk about mental health openly,” says Dr. Modi.
Crucially, the counselors work out of a different building than the hospital where Dr. Modi and her fellow residents work and use a separate electronic medical record system to protect resident privacy. This is hugely important for medical trainees, note Dr. Tomescu, Dr. Gold, and many other experts. The therapists understand residency and medical education, and there is no limit to the number of visits a resident or fellow can make with the program counselors, says Dr. Modi.
Opt-out programs offer a counterbalance to many negative tendencies in residency, says Dr. Meeks. “We’ve normalized so many things that are not healthy and productive. ... We need to counterbalance that with normalizing help seeking. And it’s really difficult to normalize something that’s not part of a system.”
Costs, concerns, and systematic support
Providing unlimited, free counseling for trainees can be very beneficial, but it requires adequate funding and personnel resources. Offering unlimited access means that an institution has to follow through in making this degree of care available while also ensuring that the system doesn’t get overwhelmed or is unable to accommodate very sick individuals, says Dr. Gold.
Another concern that experts like Dr. Batra, Dr. Moffit, and Dr. Gold share is that residents who go to their scheduled appointments may not completely buy into the experience because it wasn’t their idea in the first place. Participation alone doesn’t necessarily indicate full acceptance. Program personnel don’t intend for these appointments to be thought of as mandatory, yet residents may still experience them that way. Several leading resident well-being programs instead emphasize outreach to trainees, institutional support, and accessible mental health resources that are – and feel – entirely voluntary.
“If I tell someone that they have to do something, it’s very different than if they arrive at that conclusion for themselves,” says Dr. Batra. “That’s how life works.”
When it comes to cost, a recent study published in Academic Medicine provides encouraging data. At the University of Colorado, an opt-out pilot program for IM and pediatrics interns during the 2017-2018 academic year cost just $940 total, equal to $11.75 per intern. As in West Virginia, the program in Colorado covered the cost of the visit, interns were provided a half day off (whether they attended their appointment or not), and the visits and surveys were entirely optional and confidential. During the 1-year pilot program, 29% of 80 interns attended the scheduled appointment, 56% opted out in advance, and 15% didn’t show up. The majority of interns who were surveyed (85%), however, thought the program should continue and that it had a positive effect on their wellness even if they didn’t attend their appointment.
In West Virginia, program costs are higher. The program has $20,000 in annual funding to cover the opt-out program and unlimited counseling visits for residents and fellows. With that funding, Dr. Sofka and her colleagues were also able to expand the program slightly last year to schedule all the critical care faculty for counseling visits. Cost is a barrier to expanding these services to the entire institution, which Dr. Sofka says she hopes to do one day.
Research in this area is still preliminary. The WVU and Colorado studies provide some of the first evidence in support of an opt-out approach. Eventually, it would be beneficial for multicenter studies and longitudinal research to track the effects of such programs over time, say Dr. Sofka and Ajay Major, MD, MBA, one of the study’s coauthors and a hematology/oncology fellow at the University of Chicago.
Whether a program goes with an opt-out approach or not, the systematic supports – protecting resident privacy, providing flexible scheduling, and more – are crucial.
As Dr. Tomescu notes, wellness shouldn’t be just something trainees have to do. “The key with really working on burnout at a huge level is for all programs and schools to recognize that it’s a shared responsibility.”
“I felt very fortunate that I was able to get some help throughout residency,” says Dr. Modi. “About how to be a better daughter. How to be content with things I have in life. How to be happy, and grateful. With the kind of job we have, I think we sometimes forget to be grateful.”
A version of this article first appeared on Medscape.com.
Sarah Sofka, MD, FACP, noticed a pattern. As program director for the internal medicine (IM) residency at West Virginia University, Morgantown, she was informed when residents were sent to counseling because they were affected by burnout, depression, or anxiety. When trainees returned from these visits, many told her the same thing: They wished they had sought help sooner.
IM residents and their families had access to free counseling at WVU, but few used the resource, says Dr. Sofka. “So, we thought, let’s just schedule all of our residents for a therapy visit so they can go and see what it’s like,” she said. “This will hopefully decrease the stigma for seeking mental health care. If everybody’s going, it’s not a big deal.”
In July 2015, Dr. Sofka and her colleagues launched a universal well-being assessment program for the IM residents at WVU. The program leaders automatically scheduled first- and second-year residents for a visit to the faculty staff assistance program counselors. The visits were not mandatory, and residents could choose not to go; but if they did go, they received the entire day of their visit off from work.
Five and a half years after launching their program, Dr. Sofka and her colleagues conducted one of the first studies of the efficacy of an opt-out approach for resident mental wellness. They found that , suggesting that residents were seeking help proactively after having to at least consider it.
Opt-out counseling is a recent concept in residency programs – one that’s attracting interest from training programs across the country. Brown University, Providence, R.I.; the University of Colorado at Denver, Aurora; University of Pennsylvania, Philadelphia; and the University of California, San Francisco have at least one residency program that uses the approach.
Lisa Meeks, PhD, an assistant professor of family medicine at Michigan Medicine, in Ann Arbor, and other experts also believe opt-out counseling could decrease stigma and help normalize seeking care for mental health problems in the medical community while lowering the barriers for trainees who need help.
No time, no access, plenty of stigma
Burnout and mental health are known to be major concerns for health care workers, especially trainees. College graduates starting medical education have lower rates of burnout and depression, compared with demographically matched peers; however, once they’ve started training, medical students, residents, and fellows are more likely to be burned out and exhibit symptoms of depression. The ongoing COVID-19 pandemic is further fraying the well-being of overworked and traumatized health care professionals, and experts predict a mental health crisis will follow the viral crisis.
The Accreditation Council for Graduate Medical Education recently mandated that programs offer wellness services to trainees. Yet this doesn’t mean they are always used; well-known barriers stand between residents, medical students, and physicians and their receiving effective mental health treatment.
Two of the most obvious are access and time, given the grueling and often inflexible schedules of most trainees, says Jessica Gold, MD, a psychiatrist at Washington University, St. Louis, who specializes in treating medical professionals. Dr. Gold also points out that, to be done correctly, these programs require institutional support and investment – resources that aren’t always adequate.
“A lack of transparency and clear messaging around what is available, who provides the services, and how to access these services can be a major barrier,” says Erene Stergiopoulos, MD, a second-year psychiatry resident at the University of Toronto. In addition, there can be considerable lag between when a resident realizes they need help and when they manage to find a provider and schedule an appointment, says Dr. Meeks.
Even when these logistical barriers are overcome, trainees and physicians have to contend with the persistent stigma associated with mental health treatment in the culture of medicine, says Dr. Gold. A recent survey by the American College of Emergency Physicians found that 73% of surveyed physicians feel there is stigma in their workplace about seeking mental health treatment. Many state medical licensing boards still require physicians to disclose mental health treatment, which discourages many trainees and providers from seeking proactive care, says Mary Moffit, PhD, associate professor of psychiatry and director of the resident and faculty wellness program at Oregon Health & Science University, Portland.
How the opt-out approach works
“The idea is by making it opt-out, you really normalize it,” says Maneesh Batra, MD, MPH, associate director of the University of Washington, Seattle, Children’s Hospital residency program. Similar approaches have proven effective at shaping human behavior in other health care settings, including boosting testing rates for HIV and increasing immunization rates for childhood vaccines, Dr. Batra says.
In general, opt-out programs acknowledge that people are busy and won’t take that extra step or click that extra button if they don’t have to, says Oana Tomescu, MD, PhD, associate professor of clinical medicine and pediatrics at the University of Pennsylvania, Philadelphia.
In 2018, Dr. Sofka and her colleagues at WVU conducted a survey that showed that a majority of residents thought favorably of their opt-out program and said they would return to counseling for follow-up care. In their most recent study, published in the Journal of Graduate Medical Education in 2021, Dr. Sofka and her colleagues found that residents did just that – only 8 of 239 opted out of universally scheduled visits. Resident-initiated visits increased significantly from zero during the 2014-2015 academic year to 23 in 2018-2019. Between those periods, program-mandated visits decreased significantly from 12 to 3.
The initiative has succeeded in creating a culture of openness and caring at WVU, says 2nd-year internal medicine resident Nistha Modi, MD. “It sets the tone for the program – we talk about mental health openly,” says Dr. Modi.
Crucially, the counselors work out of a different building than the hospital where Dr. Modi and her fellow residents work and use a separate electronic medical record system to protect resident privacy. This is hugely important for medical trainees, note Dr. Tomescu, Dr. Gold, and many other experts. The therapists understand residency and medical education, and there is no limit to the number of visits a resident or fellow can make with the program counselors, says Dr. Modi.
Opt-out programs offer a counterbalance to many negative tendencies in residency, says Dr. Meeks. “We’ve normalized so many things that are not healthy and productive. ... We need to counterbalance that with normalizing help seeking. And it’s really difficult to normalize something that’s not part of a system.”
Costs, concerns, and systematic support
Providing unlimited, free counseling for trainees can be very beneficial, but it requires adequate funding and personnel resources. Offering unlimited access means that an institution has to follow through in making this degree of care available while also ensuring that the system doesn’t get overwhelmed or is unable to accommodate very sick individuals, says Dr. Gold.
Another concern that experts like Dr. Batra, Dr. Moffit, and Dr. Gold share is that residents who go to their scheduled appointments may not completely buy into the experience because it wasn’t their idea in the first place. Participation alone doesn’t necessarily indicate full acceptance. Program personnel don’t intend for these appointments to be thought of as mandatory, yet residents may still experience them that way. Several leading resident well-being programs instead emphasize outreach to trainees, institutional support, and accessible mental health resources that are – and feel – entirely voluntary.
“If I tell someone that they have to do something, it’s very different than if they arrive at that conclusion for themselves,” says Dr. Batra. “That’s how life works.”
When it comes to cost, a recent study published in Academic Medicine provides encouraging data. At the University of Colorado, an opt-out pilot program for IM and pediatrics interns during the 2017-2018 academic year cost just $940 total, equal to $11.75 per intern. As in West Virginia, the program in Colorado covered the cost of the visit, interns were provided a half day off (whether they attended their appointment or not), and the visits and surveys were entirely optional and confidential. During the 1-year pilot program, 29% of 80 interns attended the scheduled appointment, 56% opted out in advance, and 15% didn’t show up. The majority of interns who were surveyed (85%), however, thought the program should continue and that it had a positive effect on their wellness even if they didn’t attend their appointment.
In West Virginia, program costs are higher. The program has $20,000 in annual funding to cover the opt-out program and unlimited counseling visits for residents and fellows. With that funding, Dr. Sofka and her colleagues were also able to expand the program slightly last year to schedule all the critical care faculty for counseling visits. Cost is a barrier to expanding these services to the entire institution, which Dr. Sofka says she hopes to do one day.
Research in this area is still preliminary. The WVU and Colorado studies provide some of the first evidence in support of an opt-out approach. Eventually, it would be beneficial for multicenter studies and longitudinal research to track the effects of such programs over time, say Dr. Sofka and Ajay Major, MD, MBA, one of the study’s coauthors and a hematology/oncology fellow at the University of Chicago.
Whether a program goes with an opt-out approach or not, the systematic supports – protecting resident privacy, providing flexible scheduling, and more – are crucial.
As Dr. Tomescu notes, wellness shouldn’t be just something trainees have to do. “The key with really working on burnout at a huge level is for all programs and schools to recognize that it’s a shared responsibility.”
“I felt very fortunate that I was able to get some help throughout residency,” says Dr. Modi. “About how to be a better daughter. How to be content with things I have in life. How to be happy, and grateful. With the kind of job we have, I think we sometimes forget to be grateful.”
A version of this article first appeared on Medscape.com.
Sarah Sofka, MD, FACP, noticed a pattern. As program director for the internal medicine (IM) residency at West Virginia University, Morgantown, she was informed when residents were sent to counseling because they were affected by burnout, depression, or anxiety. When trainees returned from these visits, many told her the same thing: They wished they had sought help sooner.
IM residents and their families had access to free counseling at WVU, but few used the resource, says Dr. Sofka. “So, we thought, let’s just schedule all of our residents for a therapy visit so they can go and see what it’s like,” she said. “This will hopefully decrease the stigma for seeking mental health care. If everybody’s going, it’s not a big deal.”
In July 2015, Dr. Sofka and her colleagues launched a universal well-being assessment program for the IM residents at WVU. The program leaders automatically scheduled first- and second-year residents for a visit to the faculty staff assistance program counselors. The visits were not mandatory, and residents could choose not to go; but if they did go, they received the entire day of their visit off from work.
Five and a half years after launching their program, Dr. Sofka and her colleagues conducted one of the first studies of the efficacy of an opt-out approach for resident mental wellness. They found that , suggesting that residents were seeking help proactively after having to at least consider it.
Opt-out counseling is a recent concept in residency programs – one that’s attracting interest from training programs across the country. Brown University, Providence, R.I.; the University of Colorado at Denver, Aurora; University of Pennsylvania, Philadelphia; and the University of California, San Francisco have at least one residency program that uses the approach.
Lisa Meeks, PhD, an assistant professor of family medicine at Michigan Medicine, in Ann Arbor, and other experts also believe opt-out counseling could decrease stigma and help normalize seeking care for mental health problems in the medical community while lowering the barriers for trainees who need help.
No time, no access, plenty of stigma
Burnout and mental health are known to be major concerns for health care workers, especially trainees. College graduates starting medical education have lower rates of burnout and depression, compared with demographically matched peers; however, once they’ve started training, medical students, residents, and fellows are more likely to be burned out and exhibit symptoms of depression. The ongoing COVID-19 pandemic is further fraying the well-being of overworked and traumatized health care professionals, and experts predict a mental health crisis will follow the viral crisis.
The Accreditation Council for Graduate Medical Education recently mandated that programs offer wellness services to trainees. Yet this doesn’t mean they are always used; well-known barriers stand between residents, medical students, and physicians and their receiving effective mental health treatment.
Two of the most obvious are access and time, given the grueling and often inflexible schedules of most trainees, says Jessica Gold, MD, a psychiatrist at Washington University, St. Louis, who specializes in treating medical professionals. Dr. Gold also points out that, to be done correctly, these programs require institutional support and investment – resources that aren’t always adequate.
“A lack of transparency and clear messaging around what is available, who provides the services, and how to access these services can be a major barrier,” says Erene Stergiopoulos, MD, a second-year psychiatry resident at the University of Toronto. In addition, there can be considerable lag between when a resident realizes they need help and when they manage to find a provider and schedule an appointment, says Dr. Meeks.
Even when these logistical barriers are overcome, trainees and physicians have to contend with the persistent stigma associated with mental health treatment in the culture of medicine, says Dr. Gold. A recent survey by the American College of Emergency Physicians found that 73% of surveyed physicians feel there is stigma in their workplace about seeking mental health treatment. Many state medical licensing boards still require physicians to disclose mental health treatment, which discourages many trainees and providers from seeking proactive care, says Mary Moffit, PhD, associate professor of psychiatry and director of the resident and faculty wellness program at Oregon Health & Science University, Portland.
How the opt-out approach works
“The idea is by making it opt-out, you really normalize it,” says Maneesh Batra, MD, MPH, associate director of the University of Washington, Seattle, Children’s Hospital residency program. Similar approaches have proven effective at shaping human behavior in other health care settings, including boosting testing rates for HIV and increasing immunization rates for childhood vaccines, Dr. Batra says.
In general, opt-out programs acknowledge that people are busy and won’t take that extra step or click that extra button if they don’t have to, says Oana Tomescu, MD, PhD, associate professor of clinical medicine and pediatrics at the University of Pennsylvania, Philadelphia.
In 2018, Dr. Sofka and her colleagues at WVU conducted a survey that showed that a majority of residents thought favorably of their opt-out program and said they would return to counseling for follow-up care. In their most recent study, published in the Journal of Graduate Medical Education in 2021, Dr. Sofka and her colleagues found that residents did just that – only 8 of 239 opted out of universally scheduled visits. Resident-initiated visits increased significantly from zero during the 2014-2015 academic year to 23 in 2018-2019. Between those periods, program-mandated visits decreased significantly from 12 to 3.
The initiative has succeeded in creating a culture of openness and caring at WVU, says 2nd-year internal medicine resident Nistha Modi, MD. “It sets the tone for the program – we talk about mental health openly,” says Dr. Modi.
Crucially, the counselors work out of a different building than the hospital where Dr. Modi and her fellow residents work and use a separate electronic medical record system to protect resident privacy. This is hugely important for medical trainees, note Dr. Tomescu, Dr. Gold, and many other experts. The therapists understand residency and medical education, and there is no limit to the number of visits a resident or fellow can make with the program counselors, says Dr. Modi.
Opt-out programs offer a counterbalance to many negative tendencies in residency, says Dr. Meeks. “We’ve normalized so many things that are not healthy and productive. ... We need to counterbalance that with normalizing help seeking. And it’s really difficult to normalize something that’s not part of a system.”
Costs, concerns, and systematic support
Providing unlimited, free counseling for trainees can be very beneficial, but it requires adequate funding and personnel resources. Offering unlimited access means that an institution has to follow through in making this degree of care available while also ensuring that the system doesn’t get overwhelmed or is unable to accommodate very sick individuals, says Dr. Gold.
Another concern that experts like Dr. Batra, Dr. Moffit, and Dr. Gold share is that residents who go to their scheduled appointments may not completely buy into the experience because it wasn’t their idea in the first place. Participation alone doesn’t necessarily indicate full acceptance. Program personnel don’t intend for these appointments to be thought of as mandatory, yet residents may still experience them that way. Several leading resident well-being programs instead emphasize outreach to trainees, institutional support, and accessible mental health resources that are – and feel – entirely voluntary.
“If I tell someone that they have to do something, it’s very different than if they arrive at that conclusion for themselves,” says Dr. Batra. “That’s how life works.”
When it comes to cost, a recent study published in Academic Medicine provides encouraging data. At the University of Colorado, an opt-out pilot program for IM and pediatrics interns during the 2017-2018 academic year cost just $940 total, equal to $11.75 per intern. As in West Virginia, the program in Colorado covered the cost of the visit, interns were provided a half day off (whether they attended their appointment or not), and the visits and surveys were entirely optional and confidential. During the 1-year pilot program, 29% of 80 interns attended the scheduled appointment, 56% opted out in advance, and 15% didn’t show up. The majority of interns who were surveyed (85%), however, thought the program should continue and that it had a positive effect on their wellness even if they didn’t attend their appointment.
In West Virginia, program costs are higher. The program has $20,000 in annual funding to cover the opt-out program and unlimited counseling visits for residents and fellows. With that funding, Dr. Sofka and her colleagues were also able to expand the program slightly last year to schedule all the critical care faculty for counseling visits. Cost is a barrier to expanding these services to the entire institution, which Dr. Sofka says she hopes to do one day.
Research in this area is still preliminary. The WVU and Colorado studies provide some of the first evidence in support of an opt-out approach. Eventually, it would be beneficial for multicenter studies and longitudinal research to track the effects of such programs over time, say Dr. Sofka and Ajay Major, MD, MBA, one of the study’s coauthors and a hematology/oncology fellow at the University of Chicago.
Whether a program goes with an opt-out approach or not, the systematic supports – protecting resident privacy, providing flexible scheduling, and more – are crucial.
As Dr. Tomescu notes, wellness shouldn’t be just something trainees have to do. “The key with really working on burnout at a huge level is for all programs and schools to recognize that it’s a shared responsibility.”
“I felt very fortunate that I was able to get some help throughout residency,” says Dr. Modi. “About how to be a better daughter. How to be content with things I have in life. How to be happy, and grateful. With the kind of job we have, I think we sometimes forget to be grateful.”
A version of this article first appeared on Medscape.com.
Fear, stigma can stymie the care of criminal justice-involved outpatients
One of the greatest challenges psychotherapists face when working with justice-involved outpatients is a lack of familiarity with the criminal legal system, according to Debra A. Pinals, MD.
“It’s certainly nothing we learned about in medical school or in our mental health training, per se,” said Dr. Pinals, director of the program in psychiatry, law, and ethics at the University of Michigan, Ann Arbor, during an annual psychopharmacology update held by the Nevada Psychiatric Association.
“Another challenge is a lack of comfort with some patient personality styles, particularly those with antisocial personality styles,” she said. “We may have countertransference issues that emerge in our work with this population. That can lead to concerns about our own safety, which may at times be reasonable but often because of stereotypes often becomes of mythical proportion. The population is a high-demand population with limited resources, usually tapping public mental health services. That becomes a challenge as well. And there can be burnout when the challenges of our patient population exceed our capacity.”
Despite such obstacles, Dr. Pinals described the outpatient treatment of individuals involved in the criminal justice system as exciting, interesting, and intellectually challenging. But she acknowledged the role that stigma and fear can play.
“Though there are some unique challenges, the benefits of working with criminal justice–involved persons with serious mental illness are often not discussed,” Dr. Pinals said. “There is a tendency to overvalue the risk they may present without really looking at the specific nuances that would be involved in conducting true risk assessments and understanding that not all of these patients will be as risky as we might believe due to stigma and fear.”
Separate from how patients with criminal histories may be perceived in clinical settings. There is much to learn about the role of mental illness in crime. In a 2014 study, researchers reviewed the records of criminal arrests in 143 people with mental illness and tried to discern whether the crime itself was completely independent or completely directly connected to the symptoms of mental illness the individual was experiencing. They found that 65% were completely independent of mental illness symptoms while 8% were directly related to mental illness symptoms.
“This means that as clinicians working with outpatients, we have to understand the whole person, and what might be going on in their lives that leads them down this criminal pathway,” said Dr. Pinals, who is also a clinical professor of psychiatry at the medical school.
According to the risk-need-responsivity (RNR) paradigm, eight criminogenic risk factors are associated with recurrent involvement in the criminal legal system (Crime & Delinquency. 2006;52:7-27). The big four include history of antisocial behavior, antisocial personality pattern, antisocial cognition, and antisocial attitudes. “These are the factors that certain cognitive-behavioral therapy approaches try to address, in an effort to reduce those antisocial cognitive tendencies,” Dr. Pinals said. The other four risk factors include family or marital discord, poor school and/or work performance, few leisure or recreation activities, and substance misuse.
“You’ll notice that mental illness is not listed,” she said. “ although it might be considered a responsivity factor within this RNR paradigm. This means it’s important to address it because it may help people better respond to criminal justice supervision and thereby have an indirect effect in reducing criminal recidivism. For example, if somebody has a social anxiety disorder or agoraphobia and therefore can’t make their probation appointment, probation won’t be able to help them adhere to the terms of their probation conditions. So, we do have to treat the illnesses underlying responsivity to how the criminal justice system operates.”
To optimally serve this population, Dr. Pinals recommends that psychotherapists become familiar with the Sequential Intercept Model, which was first published in 2006. “It takes the premise that individuals move through the criminal legal system in logical steps, and if we could identify those with mental health or substance use conditions and redirect them out of the criminal legal system and into treatment, we could reduce the overall penetration of those individuals from the criminal legal system,” she said. “We know that individuals with mental illness are overrepresented in the criminal legal system.”
By understanding what happens when a patient is arrested, mental health professionals can foster communication that could facilitate treatment for their patients.
“It’s important that we remember that these are people who are going through a challenging time,” Dr. Pinals said. “Maybe we don’t like what they did. Maybe we don’t like that they were accused of committing some kind of crime. However, it is important to realize that they are patients, and we want them to achieve the best outcome, whatever setting they’re in, that continuity of care and communication across systems might be beneficial. It might reduce their chance of returning to the criminal system and having other people victimized.”
Mental health services vary across jails and prisons, she continued, but they are generally required to be commensurate with community standards.
“Of course, that’s often fraught with complexity and may not be available in particular jurisdictions” she said. Prisons, unlike local county jails, tend to have more levels of outpatient care, including inpatient, outpatient, and residential services. “Persons with mental illness can be moved in and out of these levels of care as needed,” Dr. Pinals said. “However, persons with mental illness can be at more risk for disciplinary infractions, especially if they’re not able to follow directions or if they’re psychotic or manic.”
Reentry creates certain risks to be mindful of, including social isolation, recurrent symptoms, problems acquiring medications and housing, suicide, violence, and a return to substance use. A reentry approach she recommended is the APIC model, which stands for Assess, Plan, Identify, and Coordinate. “That means individuals approaching release should be screened and assessed for their needs with a plan to meet the needs, identify critical periods and needed policies, and coordinate across systems,” Dr. Pinals said. “So, if you get a call as an outpatient provider from the reentry coordinator at a local jail trying to help you coordinate a patient’s reentry, that’s something to pay attention to.”
When first meeting with patients after a criminal justice experience, Dr. Pinals recommends asking them to discuss their arrest and criminal justice experience, and to address any emerging psychiatric or clinical issues, including trauma and adjustment associated with the arrests, incarceration, and legal processes. “The risks of rearrest are higher for those who have already touched the criminal justice system, so we want to help minimize that risk of rearrest,” she said.
Some clinics won’t allow patients with a criminal record to return, “which means you have to help potentially find alternative places for them to be seen,” she noted. “You may want to consult a specialist if you have doubts about your capacity to work with the patient. You also want to support staff who might have concerns about how to continue to treat this patient and you want to advocate for the patient’s needs and help them return to a stable treatment setting.”
Dr. Pinals concluded her presentation by underscoring the importance of delivering treatment services that are trauma informed. “There are high levels of trauma for those receiving care in psychiatric settings and among those who have spent time in jails and prisons,” she said. “We want to be sensitive to the fact that any of our patients who were involved in the criminal legal system might have a strong trauma history. Help instill a sense of safety and community, and hold hope for positive change.”
She reported consulting to jurisdictions and attorneys pertaining to behavioral health and justice, and forensic psychiatry. She reported having no relevant commercial financial disclosures.
One of the greatest challenges psychotherapists face when working with justice-involved outpatients is a lack of familiarity with the criminal legal system, according to Debra A. Pinals, MD.
“It’s certainly nothing we learned about in medical school or in our mental health training, per se,” said Dr. Pinals, director of the program in psychiatry, law, and ethics at the University of Michigan, Ann Arbor, during an annual psychopharmacology update held by the Nevada Psychiatric Association.
“Another challenge is a lack of comfort with some patient personality styles, particularly those with antisocial personality styles,” she said. “We may have countertransference issues that emerge in our work with this population. That can lead to concerns about our own safety, which may at times be reasonable but often because of stereotypes often becomes of mythical proportion. The population is a high-demand population with limited resources, usually tapping public mental health services. That becomes a challenge as well. And there can be burnout when the challenges of our patient population exceed our capacity.”
Despite such obstacles, Dr. Pinals described the outpatient treatment of individuals involved in the criminal justice system as exciting, interesting, and intellectually challenging. But she acknowledged the role that stigma and fear can play.
“Though there are some unique challenges, the benefits of working with criminal justice–involved persons with serious mental illness are often not discussed,” Dr. Pinals said. “There is a tendency to overvalue the risk they may present without really looking at the specific nuances that would be involved in conducting true risk assessments and understanding that not all of these patients will be as risky as we might believe due to stigma and fear.”
Separate from how patients with criminal histories may be perceived in clinical settings. There is much to learn about the role of mental illness in crime. In a 2014 study, researchers reviewed the records of criminal arrests in 143 people with mental illness and tried to discern whether the crime itself was completely independent or completely directly connected to the symptoms of mental illness the individual was experiencing. They found that 65% were completely independent of mental illness symptoms while 8% were directly related to mental illness symptoms.
“This means that as clinicians working with outpatients, we have to understand the whole person, and what might be going on in their lives that leads them down this criminal pathway,” said Dr. Pinals, who is also a clinical professor of psychiatry at the medical school.
According to the risk-need-responsivity (RNR) paradigm, eight criminogenic risk factors are associated with recurrent involvement in the criminal legal system (Crime & Delinquency. 2006;52:7-27). The big four include history of antisocial behavior, antisocial personality pattern, antisocial cognition, and antisocial attitudes. “These are the factors that certain cognitive-behavioral therapy approaches try to address, in an effort to reduce those antisocial cognitive tendencies,” Dr. Pinals said. The other four risk factors include family or marital discord, poor school and/or work performance, few leisure or recreation activities, and substance misuse.
“You’ll notice that mental illness is not listed,” she said. “ although it might be considered a responsivity factor within this RNR paradigm. This means it’s important to address it because it may help people better respond to criminal justice supervision and thereby have an indirect effect in reducing criminal recidivism. For example, if somebody has a social anxiety disorder or agoraphobia and therefore can’t make their probation appointment, probation won’t be able to help them adhere to the terms of their probation conditions. So, we do have to treat the illnesses underlying responsivity to how the criminal justice system operates.”
To optimally serve this population, Dr. Pinals recommends that psychotherapists become familiar with the Sequential Intercept Model, which was first published in 2006. “It takes the premise that individuals move through the criminal legal system in logical steps, and if we could identify those with mental health or substance use conditions and redirect them out of the criminal legal system and into treatment, we could reduce the overall penetration of those individuals from the criminal legal system,” she said. “We know that individuals with mental illness are overrepresented in the criminal legal system.”
By understanding what happens when a patient is arrested, mental health professionals can foster communication that could facilitate treatment for their patients.
“It’s important that we remember that these are people who are going through a challenging time,” Dr. Pinals said. “Maybe we don’t like what they did. Maybe we don’t like that they were accused of committing some kind of crime. However, it is important to realize that they are patients, and we want them to achieve the best outcome, whatever setting they’re in, that continuity of care and communication across systems might be beneficial. It might reduce their chance of returning to the criminal system and having other people victimized.”
Mental health services vary across jails and prisons, she continued, but they are generally required to be commensurate with community standards.
“Of course, that’s often fraught with complexity and may not be available in particular jurisdictions” she said. Prisons, unlike local county jails, tend to have more levels of outpatient care, including inpatient, outpatient, and residential services. “Persons with mental illness can be moved in and out of these levels of care as needed,” Dr. Pinals said. “However, persons with mental illness can be at more risk for disciplinary infractions, especially if they’re not able to follow directions or if they’re psychotic or manic.”
Reentry creates certain risks to be mindful of, including social isolation, recurrent symptoms, problems acquiring medications and housing, suicide, violence, and a return to substance use. A reentry approach she recommended is the APIC model, which stands for Assess, Plan, Identify, and Coordinate. “That means individuals approaching release should be screened and assessed for their needs with a plan to meet the needs, identify critical periods and needed policies, and coordinate across systems,” Dr. Pinals said. “So, if you get a call as an outpatient provider from the reentry coordinator at a local jail trying to help you coordinate a patient’s reentry, that’s something to pay attention to.”
When first meeting with patients after a criminal justice experience, Dr. Pinals recommends asking them to discuss their arrest and criminal justice experience, and to address any emerging psychiatric or clinical issues, including trauma and adjustment associated with the arrests, incarceration, and legal processes. “The risks of rearrest are higher for those who have already touched the criminal justice system, so we want to help minimize that risk of rearrest,” she said.
Some clinics won’t allow patients with a criminal record to return, “which means you have to help potentially find alternative places for them to be seen,” she noted. “You may want to consult a specialist if you have doubts about your capacity to work with the patient. You also want to support staff who might have concerns about how to continue to treat this patient and you want to advocate for the patient’s needs and help them return to a stable treatment setting.”
Dr. Pinals concluded her presentation by underscoring the importance of delivering treatment services that are trauma informed. “There are high levels of trauma for those receiving care in psychiatric settings and among those who have spent time in jails and prisons,” she said. “We want to be sensitive to the fact that any of our patients who were involved in the criminal legal system might have a strong trauma history. Help instill a sense of safety and community, and hold hope for positive change.”
She reported consulting to jurisdictions and attorneys pertaining to behavioral health and justice, and forensic psychiatry. She reported having no relevant commercial financial disclosures.
One of the greatest challenges psychotherapists face when working with justice-involved outpatients is a lack of familiarity with the criminal legal system, according to Debra A. Pinals, MD.
“It’s certainly nothing we learned about in medical school or in our mental health training, per se,” said Dr. Pinals, director of the program in psychiatry, law, and ethics at the University of Michigan, Ann Arbor, during an annual psychopharmacology update held by the Nevada Psychiatric Association.
“Another challenge is a lack of comfort with some patient personality styles, particularly those with antisocial personality styles,” she said. “We may have countertransference issues that emerge in our work with this population. That can lead to concerns about our own safety, which may at times be reasonable but often because of stereotypes often becomes of mythical proportion. The population is a high-demand population with limited resources, usually tapping public mental health services. That becomes a challenge as well. And there can be burnout when the challenges of our patient population exceed our capacity.”
Despite such obstacles, Dr. Pinals described the outpatient treatment of individuals involved in the criminal justice system as exciting, interesting, and intellectually challenging. But she acknowledged the role that stigma and fear can play.
“Though there are some unique challenges, the benefits of working with criminal justice–involved persons with serious mental illness are often not discussed,” Dr. Pinals said. “There is a tendency to overvalue the risk they may present without really looking at the specific nuances that would be involved in conducting true risk assessments and understanding that not all of these patients will be as risky as we might believe due to stigma and fear.”
Separate from how patients with criminal histories may be perceived in clinical settings. There is much to learn about the role of mental illness in crime. In a 2014 study, researchers reviewed the records of criminal arrests in 143 people with mental illness and tried to discern whether the crime itself was completely independent or completely directly connected to the symptoms of mental illness the individual was experiencing. They found that 65% were completely independent of mental illness symptoms while 8% were directly related to mental illness symptoms.
“This means that as clinicians working with outpatients, we have to understand the whole person, and what might be going on in their lives that leads them down this criminal pathway,” said Dr. Pinals, who is also a clinical professor of psychiatry at the medical school.
According to the risk-need-responsivity (RNR) paradigm, eight criminogenic risk factors are associated with recurrent involvement in the criminal legal system (Crime & Delinquency. 2006;52:7-27). The big four include history of antisocial behavior, antisocial personality pattern, antisocial cognition, and antisocial attitudes. “These are the factors that certain cognitive-behavioral therapy approaches try to address, in an effort to reduce those antisocial cognitive tendencies,” Dr. Pinals said. The other four risk factors include family or marital discord, poor school and/or work performance, few leisure or recreation activities, and substance misuse.
“You’ll notice that mental illness is not listed,” she said. “ although it might be considered a responsivity factor within this RNR paradigm. This means it’s important to address it because it may help people better respond to criminal justice supervision and thereby have an indirect effect in reducing criminal recidivism. For example, if somebody has a social anxiety disorder or agoraphobia and therefore can’t make their probation appointment, probation won’t be able to help them adhere to the terms of their probation conditions. So, we do have to treat the illnesses underlying responsivity to how the criminal justice system operates.”
To optimally serve this population, Dr. Pinals recommends that psychotherapists become familiar with the Sequential Intercept Model, which was first published in 2006. “It takes the premise that individuals move through the criminal legal system in logical steps, and if we could identify those with mental health or substance use conditions and redirect them out of the criminal legal system and into treatment, we could reduce the overall penetration of those individuals from the criminal legal system,” she said. “We know that individuals with mental illness are overrepresented in the criminal legal system.”
By understanding what happens when a patient is arrested, mental health professionals can foster communication that could facilitate treatment for their patients.
“It’s important that we remember that these are people who are going through a challenging time,” Dr. Pinals said. “Maybe we don’t like what they did. Maybe we don’t like that they were accused of committing some kind of crime. However, it is important to realize that they are patients, and we want them to achieve the best outcome, whatever setting they’re in, that continuity of care and communication across systems might be beneficial. It might reduce their chance of returning to the criminal system and having other people victimized.”
Mental health services vary across jails and prisons, she continued, but they are generally required to be commensurate with community standards.
“Of course, that’s often fraught with complexity and may not be available in particular jurisdictions” she said. Prisons, unlike local county jails, tend to have more levels of outpatient care, including inpatient, outpatient, and residential services. “Persons with mental illness can be moved in and out of these levels of care as needed,” Dr. Pinals said. “However, persons with mental illness can be at more risk for disciplinary infractions, especially if they’re not able to follow directions or if they’re psychotic or manic.”
Reentry creates certain risks to be mindful of, including social isolation, recurrent symptoms, problems acquiring medications and housing, suicide, violence, and a return to substance use. A reentry approach she recommended is the APIC model, which stands for Assess, Plan, Identify, and Coordinate. “That means individuals approaching release should be screened and assessed for their needs with a plan to meet the needs, identify critical periods and needed policies, and coordinate across systems,” Dr. Pinals said. “So, if you get a call as an outpatient provider from the reentry coordinator at a local jail trying to help you coordinate a patient’s reentry, that’s something to pay attention to.”
When first meeting with patients after a criminal justice experience, Dr. Pinals recommends asking them to discuss their arrest and criminal justice experience, and to address any emerging psychiatric or clinical issues, including trauma and adjustment associated with the arrests, incarceration, and legal processes. “The risks of rearrest are higher for those who have already touched the criminal justice system, so we want to help minimize that risk of rearrest,” she said.
Some clinics won’t allow patients with a criminal record to return, “which means you have to help potentially find alternative places for them to be seen,” she noted. “You may want to consult a specialist if you have doubts about your capacity to work with the patient. You also want to support staff who might have concerns about how to continue to treat this patient and you want to advocate for the patient’s needs and help them return to a stable treatment setting.”
Dr. Pinals concluded her presentation by underscoring the importance of delivering treatment services that are trauma informed. “There are high levels of trauma for those receiving care in psychiatric settings and among those who have spent time in jails and prisons,” she said. “We want to be sensitive to the fact that any of our patients who were involved in the criminal legal system might have a strong trauma history. Help instill a sense of safety and community, and hold hope for positive change.”
She reported consulting to jurisdictions and attorneys pertaining to behavioral health and justice, and forensic psychiatry. She reported having no relevant commercial financial disclosures.
FROM NPA 2021
The Physician Support Line: One psychiatrist strives to make a difference
Have you ever had a really good idea about how to improve the delivery of mental health services? An idea that would help people, but that would require passion, innovation, and hard work to implement, and one that immediately is beset with a list of reasons why it can not be implemented?
Mona Masood, DO, had an idea. The Pennsylvania psychiatrist was asked to help moderate a Facebook group started by one of her infectious disease colleagues last winter – a private Facebook group for physicians working with COVID-19 patients.
“The group was getting posts from frontline workers about how depressed and hopeless they were feeling.” Dr. Masood said. “People were posting about how they were having escape fantasies and how they regretted becoming physicians. It became clear that there was a need for more support.”
psychiatrist volunteers would take calls from physicians who needed someone to talk to – the psychiatrist would provide a sympathetic ear and have a list of resources, but this would be support, not treatment. There would be no prescriptions, no treatment relationship, no reporting to licensing boards or employers. The calls would be anonymous.
She posted her idea on the Facebook group, and the response was immediate. “There were a lot of emails – 200 psychiatrists responded saying: “Sign me up.” A Zoom meeting was set up, and the process was set in motion.
Dr. Masood used a Google document for weekly sign-ups so the volunteer psychiatrists could choose times. “We had to pay for an upgraded Google suite package for that many users. Getting this up and running was like the saying about building a plane as you fly it,” Dr. Masood said. “It forced so much so quickly because there was this acknowledgment that the need was there.”
Initially, the support line launched with a telehealth platform, but there was a problem. “Many doctors don’t want to be seen; they worry about being recognized.” Dr. Masood researched hotline phone services and was able to get one for a reduced fee. The volunteers have an App on their smartphones that enables them to log in at the start of their shifts and log out at the end. In addition to the logistics of coordinating the volunteers – now numbering over 700 – the group found a health care law firm that provided pro bono services to review the policies and procedures.
Now that the support line is running, Dr. Masood is able to set up the day’s volunteers for the support line connection in a few minutes each morning, but the beginning was not easy. Her private practice transitioned to telemedicine, and her two children were home with one in virtual school. “At first, it was like another full-time job.” She still remains available for trouble-shooting during the day. It’s a project she has taken on with passion.
The support line began as a response to watching colleagues struggle with COVID. Since it launched, there have been approximately 2,000 calls. Calls typically last for 20 to 90 minutes, and no one has called with a suicidal crisis. It is now open to doctors and medical students looking for support for any reason. “Physicians call with all kinds of issues. In the first 3 months, it was COVID, but then they called with other concerns – there were doctors who called with election anxiety, really anything that affects the general public also affects us.”
The group has also offered Saturday didactic sessions for volunteers and weekly debriefing sessions. Dr. Masood has been approached by Vibrant Emotional Health, the administrator of the National Suicide Prevention Lifeline, about resources to help with funding – until now, this endeavor has had no financing – and she is hopeful that their financial support will allow the support line to sustain itself and grow. Future directions include advocating for systemic change in how physician mental health and wellness issues are addressed.
The Physician Support Line was one psychiatrist’s vision for how to address a problem. Like so many things related to this pandemic, it happened quickly and with surprising efficiency. Implementing this service, however, was not easy – it required hard work, innovative thinking, and passion. Those looking for someone to listen can call 1-888-409-0141 and psychiatrists who wish to volunteer can sign up at physiciansupportline.com/volunteer-info.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Have you ever had a really good idea about how to improve the delivery of mental health services? An idea that would help people, but that would require passion, innovation, and hard work to implement, and one that immediately is beset with a list of reasons why it can not be implemented?
Mona Masood, DO, had an idea. The Pennsylvania psychiatrist was asked to help moderate a Facebook group started by one of her infectious disease colleagues last winter – a private Facebook group for physicians working with COVID-19 patients.
“The group was getting posts from frontline workers about how depressed and hopeless they were feeling.” Dr. Masood said. “People were posting about how they were having escape fantasies and how they regretted becoming physicians. It became clear that there was a need for more support.”
psychiatrist volunteers would take calls from physicians who needed someone to talk to – the psychiatrist would provide a sympathetic ear and have a list of resources, but this would be support, not treatment. There would be no prescriptions, no treatment relationship, no reporting to licensing boards or employers. The calls would be anonymous.
She posted her idea on the Facebook group, and the response was immediate. “There were a lot of emails – 200 psychiatrists responded saying: “Sign me up.” A Zoom meeting was set up, and the process was set in motion.
Dr. Masood used a Google document for weekly sign-ups so the volunteer psychiatrists could choose times. “We had to pay for an upgraded Google suite package for that many users. Getting this up and running was like the saying about building a plane as you fly it,” Dr. Masood said. “It forced so much so quickly because there was this acknowledgment that the need was there.”
Initially, the support line launched with a telehealth platform, but there was a problem. “Many doctors don’t want to be seen; they worry about being recognized.” Dr. Masood researched hotline phone services and was able to get one for a reduced fee. The volunteers have an App on their smartphones that enables them to log in at the start of their shifts and log out at the end. In addition to the logistics of coordinating the volunteers – now numbering over 700 – the group found a health care law firm that provided pro bono services to review the policies and procedures.
Now that the support line is running, Dr. Masood is able to set up the day’s volunteers for the support line connection in a few minutes each morning, but the beginning was not easy. Her private practice transitioned to telemedicine, and her two children were home with one in virtual school. “At first, it was like another full-time job.” She still remains available for trouble-shooting during the day. It’s a project she has taken on with passion.
The support line began as a response to watching colleagues struggle with COVID. Since it launched, there have been approximately 2,000 calls. Calls typically last for 20 to 90 minutes, and no one has called with a suicidal crisis. It is now open to doctors and medical students looking for support for any reason. “Physicians call with all kinds of issues. In the first 3 months, it was COVID, but then they called with other concerns – there were doctors who called with election anxiety, really anything that affects the general public also affects us.”
The group has also offered Saturday didactic sessions for volunteers and weekly debriefing sessions. Dr. Masood has been approached by Vibrant Emotional Health, the administrator of the National Suicide Prevention Lifeline, about resources to help with funding – until now, this endeavor has had no financing – and she is hopeful that their financial support will allow the support line to sustain itself and grow. Future directions include advocating for systemic change in how physician mental health and wellness issues are addressed.
The Physician Support Line was one psychiatrist’s vision for how to address a problem. Like so many things related to this pandemic, it happened quickly and with surprising efficiency. Implementing this service, however, was not easy – it required hard work, innovative thinking, and passion. Those looking for someone to listen can call 1-888-409-0141 and psychiatrists who wish to volunteer can sign up at physiciansupportline.com/volunteer-info.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Have you ever had a really good idea about how to improve the delivery of mental health services? An idea that would help people, but that would require passion, innovation, and hard work to implement, and one that immediately is beset with a list of reasons why it can not be implemented?
Mona Masood, DO, had an idea. The Pennsylvania psychiatrist was asked to help moderate a Facebook group started by one of her infectious disease colleagues last winter – a private Facebook group for physicians working with COVID-19 patients.
“The group was getting posts from frontline workers about how depressed and hopeless they were feeling.” Dr. Masood said. “People were posting about how they were having escape fantasies and how they regretted becoming physicians. It became clear that there was a need for more support.”
psychiatrist volunteers would take calls from physicians who needed someone to talk to – the psychiatrist would provide a sympathetic ear and have a list of resources, but this would be support, not treatment. There would be no prescriptions, no treatment relationship, no reporting to licensing boards or employers. The calls would be anonymous.
She posted her idea on the Facebook group, and the response was immediate. “There were a lot of emails – 200 psychiatrists responded saying: “Sign me up.” A Zoom meeting was set up, and the process was set in motion.
Dr. Masood used a Google document for weekly sign-ups so the volunteer psychiatrists could choose times. “We had to pay for an upgraded Google suite package for that many users. Getting this up and running was like the saying about building a plane as you fly it,” Dr. Masood said. “It forced so much so quickly because there was this acknowledgment that the need was there.”
Initially, the support line launched with a telehealth platform, but there was a problem. “Many doctors don’t want to be seen; they worry about being recognized.” Dr. Masood researched hotline phone services and was able to get one for a reduced fee. The volunteers have an App on their smartphones that enables them to log in at the start of their shifts and log out at the end. In addition to the logistics of coordinating the volunteers – now numbering over 700 – the group found a health care law firm that provided pro bono services to review the policies and procedures.
Now that the support line is running, Dr. Masood is able to set up the day’s volunteers for the support line connection in a few minutes each morning, but the beginning was not easy. Her private practice transitioned to telemedicine, and her two children were home with one in virtual school. “At first, it was like another full-time job.” She still remains available for trouble-shooting during the day. It’s a project she has taken on with passion.
The support line began as a response to watching colleagues struggle with COVID. Since it launched, there have been approximately 2,000 calls. Calls typically last for 20 to 90 minutes, and no one has called with a suicidal crisis. It is now open to doctors and medical students looking for support for any reason. “Physicians call with all kinds of issues. In the first 3 months, it was COVID, but then they called with other concerns – there were doctors who called with election anxiety, really anything that affects the general public also affects us.”
The group has also offered Saturday didactic sessions for volunteers and weekly debriefing sessions. Dr. Masood has been approached by Vibrant Emotional Health, the administrator of the National Suicide Prevention Lifeline, about resources to help with funding – until now, this endeavor has had no financing – and she is hopeful that their financial support will allow the support line to sustain itself and grow. Future directions include advocating for systemic change in how physician mental health and wellness issues are addressed.
The Physician Support Line was one psychiatrist’s vision for how to address a problem. Like so many things related to this pandemic, it happened quickly and with surprising efficiency. Implementing this service, however, was not easy – it required hard work, innovative thinking, and passion. Those looking for someone to listen can call 1-888-409-0141 and psychiatrists who wish to volunteer can sign up at physiciansupportline.com/volunteer-info.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
The psychiatrist’s role in navigating a toxic news cycle
This transcript has been edited for clarity.
I’m Dr. Gregory Scott Brown, an Austin (Tex.)-based psychiatrist and an affiliate faculty member at the University of Texas Dell Medical School.
Recently, a patient of mine told me that, because of the political environment we find ourselves in, he’s avoiding conversations with some of his longtime friends. Because of this, he’s feeling even more isolated than before.
We’re all coming off the heels of a tough year, and many of us expected that when we entered 2021 we’d quickly turn the page and life would get a whole lot easier. Since the reality is that we’re still dealing with deep divisions, social injustices, and the politicization of evidence-based medicine, emotions are naturally running high.
In listening to my patients over the past few weeks, there’s definitely a sense of optimism about coronavirus vaccines and getting back to life as usual. But there’s also a lingering sense of uncertainty and fear, especially when it comes to the possibility of saying the wrong thing, offending our friends, or just having conversations with people we may disagree with. I’m hearing concerns from my patients that 2020 exposed a dormant hatred that was brewing in the underbelly of our society, in our politics, and in our institutions. Patients are telling me that these concerns are making them anxious and some are avoiding interacting with people they may disagree with altogether because they’re afraid of the difficult conversations that may follow.
Since, like many of my patients as well as many of you, I follow the news, including stories of COVID-related deaths, economic hardships, peaceful protests gone bad, and political vitriol, I’ve had to remind myself about the importance of intentional kindness for effective communication and for supporting mental health.
I was reminded of the paper “Hate in the Counter-Transference” by the well-known pediatrician and psychoanalyst Donald Winnicott. He focuses on how to manage and sort through the strong emotions that may be experienced even during an encounter between a therapist and a patient. Although some of what he has to say doesn’t translate well to modern times, his recommendation that we acknowledge and try to normalize some of our feelings does. And this is how I’ve been starting a conversation with my patients – just by normalizing things a bit.
The past year or so has brought with it a range of intense emotions, including frustration, exhaustion, and some degree of sadness for most of us. When we’re self-aware about our feelings, we can make sense of them early on so that they don’t evolve into maladaptive ones like unhinged anger or hatred. My patients and I actively discuss how our feelings don’t have to get in the way of our ability to live and to interact with each other as we’d like to.
Considering the basic tenets of kindness is a good place to start. I recently spoke with Kelli Harding, MD, a psychiatrist and author of The Rabbit Effect: Live Longer, Happier, and Healthier with the Groundbreaking Science of Kindness. She pointed to research suggesting that kindness can benefit multiple areas of our health, from reducing cardiovascular events to improving mood and anxiety. In her book, she notes that
I tell my patients that we can’t always change our environment, but we can definitely change how we respond to it. This doesn’t mean it’s always an easy process, but there are things we can do. First, we have to acknowledge that some degree of conflict or cordial disagreement is inevitable and it doesn’t have to disrupt our mood.
An interesting study on conflict management pointed out that healthy conflict is actually beneficial in some cases. For instance, in the work environment, conflict can help with team development and better group decision-making. But it’s rigid personality differences, poor communication, emotional stress, and lack of candor that may contribute to so-called high-tension events, and this is where conflict can go awry. These are the areas that we can all focus on improving, not only for performance benefits but for our overall health and well-being as well.
The authors also recommend an active style of engagement as a technique to manage conflict, but in a way that feels both natural and safe. Other authors agree that so-called engaged coping is associated with a higher sense of control and overall improved psychological well-being. What this means is that avoidance may be necessary in the short term, but over time it may lead to more emotional stress and anxiety.
Overcoming the tendency to avoid requires both motivation and self-awareness. We need to know about patterns in our own behavior and how the behavior of others can push our buttons and spiral a healthy disagreement into a heated argument.
I like to recommend the hunger, angry, lonely, tired (HALT) model, which is often used as a self-care gauge in addiction treatment and to reduce medication errors. But I think it’s also a useful way to assess personal readiness for having a difficult conversation. I tell my patients to ask themselves in this moment: “Am I hungry, angry, lonely, or tired?” And if they are, perhaps it’s not the best time for the conversation.
Because 2020 brought with it a new set of challenges, it also forced many of us to focus on things that we just didn’t pay as much attention to before, including checking in on our feelings and the feelings of those around us. It also taught us to pay attention to the way and manner in which we communicate. I think that kindness is much easier to carry into difficult conversations if we approach them with a sense of curiosity before judgment. Ultimately, kindness is one of the best tools for balancing the intense emotions that many of us are feeling right now.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Gregory Scott Brown, an Austin (Tex.)-based psychiatrist and an affiliate faculty member at the University of Texas Dell Medical School.
Recently, a patient of mine told me that, because of the political environment we find ourselves in, he’s avoiding conversations with some of his longtime friends. Because of this, he’s feeling even more isolated than before.
We’re all coming off the heels of a tough year, and many of us expected that when we entered 2021 we’d quickly turn the page and life would get a whole lot easier. Since the reality is that we’re still dealing with deep divisions, social injustices, and the politicization of evidence-based medicine, emotions are naturally running high.
In listening to my patients over the past few weeks, there’s definitely a sense of optimism about coronavirus vaccines and getting back to life as usual. But there’s also a lingering sense of uncertainty and fear, especially when it comes to the possibility of saying the wrong thing, offending our friends, or just having conversations with people we may disagree with. I’m hearing concerns from my patients that 2020 exposed a dormant hatred that was brewing in the underbelly of our society, in our politics, and in our institutions. Patients are telling me that these concerns are making them anxious and some are avoiding interacting with people they may disagree with altogether because they’re afraid of the difficult conversations that may follow.
Since, like many of my patients as well as many of you, I follow the news, including stories of COVID-related deaths, economic hardships, peaceful protests gone bad, and political vitriol, I’ve had to remind myself about the importance of intentional kindness for effective communication and for supporting mental health.
I was reminded of the paper “Hate in the Counter-Transference” by the well-known pediatrician and psychoanalyst Donald Winnicott. He focuses on how to manage and sort through the strong emotions that may be experienced even during an encounter between a therapist and a patient. Although some of what he has to say doesn’t translate well to modern times, his recommendation that we acknowledge and try to normalize some of our feelings does. And this is how I’ve been starting a conversation with my patients – just by normalizing things a bit.
The past year or so has brought with it a range of intense emotions, including frustration, exhaustion, and some degree of sadness for most of us. When we’re self-aware about our feelings, we can make sense of them early on so that they don’t evolve into maladaptive ones like unhinged anger or hatred. My patients and I actively discuss how our feelings don’t have to get in the way of our ability to live and to interact with each other as we’d like to.
Considering the basic tenets of kindness is a good place to start. I recently spoke with Kelli Harding, MD, a psychiatrist and author of The Rabbit Effect: Live Longer, Happier, and Healthier with the Groundbreaking Science of Kindness. She pointed to research suggesting that kindness can benefit multiple areas of our health, from reducing cardiovascular events to improving mood and anxiety. In her book, she notes that
I tell my patients that we can’t always change our environment, but we can definitely change how we respond to it. This doesn’t mean it’s always an easy process, but there are things we can do. First, we have to acknowledge that some degree of conflict or cordial disagreement is inevitable and it doesn’t have to disrupt our mood.
An interesting study on conflict management pointed out that healthy conflict is actually beneficial in some cases. For instance, in the work environment, conflict can help with team development and better group decision-making. But it’s rigid personality differences, poor communication, emotional stress, and lack of candor that may contribute to so-called high-tension events, and this is where conflict can go awry. These are the areas that we can all focus on improving, not only for performance benefits but for our overall health and well-being as well.
The authors also recommend an active style of engagement as a technique to manage conflict, but in a way that feels both natural and safe. Other authors agree that so-called engaged coping is associated with a higher sense of control and overall improved psychological well-being. What this means is that avoidance may be necessary in the short term, but over time it may lead to more emotional stress and anxiety.
Overcoming the tendency to avoid requires both motivation and self-awareness. We need to know about patterns in our own behavior and how the behavior of others can push our buttons and spiral a healthy disagreement into a heated argument.
I like to recommend the hunger, angry, lonely, tired (HALT) model, which is often used as a self-care gauge in addiction treatment and to reduce medication errors. But I think it’s also a useful way to assess personal readiness for having a difficult conversation. I tell my patients to ask themselves in this moment: “Am I hungry, angry, lonely, or tired?” And if they are, perhaps it’s not the best time for the conversation.
Because 2020 brought with it a new set of challenges, it also forced many of us to focus on things that we just didn’t pay as much attention to before, including checking in on our feelings and the feelings of those around us. It also taught us to pay attention to the way and manner in which we communicate. I think that kindness is much easier to carry into difficult conversations if we approach them with a sense of curiosity before judgment. Ultimately, kindness is one of the best tools for balancing the intense emotions that many of us are feeling right now.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Gregory Scott Brown, an Austin (Tex.)-based psychiatrist and an affiliate faculty member at the University of Texas Dell Medical School.
Recently, a patient of mine told me that, because of the political environment we find ourselves in, he’s avoiding conversations with some of his longtime friends. Because of this, he’s feeling even more isolated than before.
We’re all coming off the heels of a tough year, and many of us expected that when we entered 2021 we’d quickly turn the page and life would get a whole lot easier. Since the reality is that we’re still dealing with deep divisions, social injustices, and the politicization of evidence-based medicine, emotions are naturally running high.
In listening to my patients over the past few weeks, there’s definitely a sense of optimism about coronavirus vaccines and getting back to life as usual. But there’s also a lingering sense of uncertainty and fear, especially when it comes to the possibility of saying the wrong thing, offending our friends, or just having conversations with people we may disagree with. I’m hearing concerns from my patients that 2020 exposed a dormant hatred that was brewing in the underbelly of our society, in our politics, and in our institutions. Patients are telling me that these concerns are making them anxious and some are avoiding interacting with people they may disagree with altogether because they’re afraid of the difficult conversations that may follow.
Since, like many of my patients as well as many of you, I follow the news, including stories of COVID-related deaths, economic hardships, peaceful protests gone bad, and political vitriol, I’ve had to remind myself about the importance of intentional kindness for effective communication and for supporting mental health.
I was reminded of the paper “Hate in the Counter-Transference” by the well-known pediatrician and psychoanalyst Donald Winnicott. He focuses on how to manage and sort through the strong emotions that may be experienced even during an encounter between a therapist and a patient. Although some of what he has to say doesn’t translate well to modern times, his recommendation that we acknowledge and try to normalize some of our feelings does. And this is how I’ve been starting a conversation with my patients – just by normalizing things a bit.
The past year or so has brought with it a range of intense emotions, including frustration, exhaustion, and some degree of sadness for most of us. When we’re self-aware about our feelings, we can make sense of them early on so that they don’t evolve into maladaptive ones like unhinged anger or hatred. My patients and I actively discuss how our feelings don’t have to get in the way of our ability to live and to interact with each other as we’d like to.
Considering the basic tenets of kindness is a good place to start. I recently spoke with Kelli Harding, MD, a psychiatrist and author of The Rabbit Effect: Live Longer, Happier, and Healthier with the Groundbreaking Science of Kindness. She pointed to research suggesting that kindness can benefit multiple areas of our health, from reducing cardiovascular events to improving mood and anxiety. In her book, she notes that
I tell my patients that we can’t always change our environment, but we can definitely change how we respond to it. This doesn’t mean it’s always an easy process, but there are things we can do. First, we have to acknowledge that some degree of conflict or cordial disagreement is inevitable and it doesn’t have to disrupt our mood.
An interesting study on conflict management pointed out that healthy conflict is actually beneficial in some cases. For instance, in the work environment, conflict can help with team development and better group decision-making. But it’s rigid personality differences, poor communication, emotional stress, and lack of candor that may contribute to so-called high-tension events, and this is where conflict can go awry. These are the areas that we can all focus on improving, not only for performance benefits but for our overall health and well-being as well.
The authors also recommend an active style of engagement as a technique to manage conflict, but in a way that feels both natural and safe. Other authors agree that so-called engaged coping is associated with a higher sense of control and overall improved psychological well-being. What this means is that avoidance may be necessary in the short term, but over time it may lead to more emotional stress and anxiety.
Overcoming the tendency to avoid requires both motivation and self-awareness. We need to know about patterns in our own behavior and how the behavior of others can push our buttons and spiral a healthy disagreement into a heated argument.
I like to recommend the hunger, angry, lonely, tired (HALT) model, which is often used as a self-care gauge in addiction treatment and to reduce medication errors. But I think it’s also a useful way to assess personal readiness for having a difficult conversation. I tell my patients to ask themselves in this moment: “Am I hungry, angry, lonely, or tired?” And if they are, perhaps it’s not the best time for the conversation.
Because 2020 brought with it a new set of challenges, it also forced many of us to focus on things that we just didn’t pay as much attention to before, including checking in on our feelings and the feelings of those around us. It also taught us to pay attention to the way and manner in which we communicate. I think that kindness is much easier to carry into difficult conversations if we approach them with a sense of curiosity before judgment. Ultimately, kindness is one of the best tools for balancing the intense emotions that many of us are feeling right now.
A version of this article first appeared on Medscape.com.



























