User login
Polydoctoring: The case against fragmented psychiatric care
How many providers does it take to depersonalize a patient? Nine? 1. A psychiatrist for transcranial magnetic stimulation (TMS). 2. A psychiatrist for ketamine. 3. A psychiatrist who specializes in substance use disorder medication. 4. A psychiatrist for the rest of the psychotropic medication. 5. An alternative medicine provider who prescribes supplements. 6. A therapist for depression who uses cognitive-behavioral therapy. 7. A therapist for posttraumatic stress disorder who uses eye movement desensitization and reprocessing. 8. An addiction counselor. 9. An equine therapist.
This doesn’t include other providers and professionals who likely contribute to one’s mental well-being, including yoga instructors and personal trainers. In addition, any one of those psychiatrists may have one or more nurse practitioners who routinely step in to attend to appointments.
In our uncertain and lonely times, the value of human contact and interaction has become exponentially more precious. I long to see my patients in my private practice office. I am now much more aware of their grounding effect on my life, and I suspect I had a similar grounding effect on theirs. Few things provide me more comfort than sitting on my lounge chair with a curious gaze waiting for the patient to start the visit. I often wonder what makes a patient choose to go see a private practice physician. Yet a common reason offered is, “Wait! You do everything? Therapy and meds if I need them? You’ll see me every week?”
While I am realistic about the need and use of split-care, I have never been enamored with the concept. I think that few medical students choose psychiatry with the goal of referring all psychotherapeutic needs and intervention to “allied mental health providers” as my prior managed care organization liked to refer to psychologists, social workers, marriage and family therapists, and other counselors. I remember particularly as a chief resident being bombarded by complaints of therapists complaining about psychiatry residents. All of their patients’ symptoms allegedly required medication adjustment and residents were supposedly dismissing them. In return, residents would complain that the therapists did not address the psychological manifestations of the patient’s ailments. Herein lies my problem with split-care, it encourages psychotherapy to be about medication management, and medication management to be about psychotherapy.
However, this is not an article against split-treatment. Psychiatrists, for a variety of reasons, are not suited to perform psychotherapy in most management care models. The main reason being that psychiatrists’ time is too expensive to justify the expense, and psychiatrists are (for the most part), the only ones able to prescribe medications for which the wait-list is already long enough. This article is about the absurd levels at which we have fragmented care of certain patients. Split-treatment is relevant in that its negative side effects, we are almost all familiar with, exemplify the problem of the fragmentation of modern psychiatry. In many ways this fragmentation of care is similar to polypharmacy – the premise for each psychotropic intervention may be sound, but the end result is often incoherent.
My main concern with the fragmentation of modern psychiatry stems from my belief that the most important facet of our work is our relationship with our patients. It is the duty we owe them, the attention we give them, the unique nature of interactions. Who among the nine providers is responsible for writing a discharge summary? Who is responsible for calling an emergency contact in a critical situation? Who communicates with the new provider when someone is taken off an insurance panel? Who makes the patient feel cared for? I am often confronted by this situation when TMS or ketamine providers say, “I just give the procedure/medication that was ordered by the referring psychiatrist.” This response disturbs me in that I could not imagine myself being so hands off in the care of a patient. There is an implication of projected immunity and lack of responsibility that bothers me.
But my concerns are also practical. From my forensic experience, I am well aware that the larger the number of providers treating a patient, the larger the number of inconsistent diagnoses, the more likely medication reconciliations are not kept up to date or incorrect, and the more likely intervention recommendations are contrary to one another. A disengaged ketamine provider may not realize that the patient was more recently enrolled in a substance use disorder program, a potential contraindication for ketamine, if not well-abreast of the patient’s continued evolution. A substance use disorder psychiatric specialist may be at odds with a substance use disorder counselor who worries about the message of treating psychiatric symptoms with chemical substances if they don’t communicate.
As with polypharmacy, “polydoctoring” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to specialize, patients still desire and benefit from an intimate and close relationship with one provider who is warm, concerned, and hopeful. Those traits can theoretically be provided by anyone and there is not something inherently wrong with having more than one provider. However, psychiatry would be wise to recognize this concerning trend, especially at a time when we all feel lonely, disconnected, and depersonalized.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
How many providers does it take to depersonalize a patient? Nine? 1. A psychiatrist for transcranial magnetic stimulation (TMS). 2. A psychiatrist for ketamine. 3. A psychiatrist who specializes in substance use disorder medication. 4. A psychiatrist for the rest of the psychotropic medication. 5. An alternative medicine provider who prescribes supplements. 6. A therapist for depression who uses cognitive-behavioral therapy. 7. A therapist for posttraumatic stress disorder who uses eye movement desensitization and reprocessing. 8. An addiction counselor. 9. An equine therapist.
This doesn’t include other providers and professionals who likely contribute to one’s mental well-being, including yoga instructors and personal trainers. In addition, any one of those psychiatrists may have one or more nurse practitioners who routinely step in to attend to appointments.
In our uncertain and lonely times, the value of human contact and interaction has become exponentially more precious. I long to see my patients in my private practice office. I am now much more aware of their grounding effect on my life, and I suspect I had a similar grounding effect on theirs. Few things provide me more comfort than sitting on my lounge chair with a curious gaze waiting for the patient to start the visit. I often wonder what makes a patient choose to go see a private practice physician. Yet a common reason offered is, “Wait! You do everything? Therapy and meds if I need them? You’ll see me every week?”
While I am realistic about the need and use of split-care, I have never been enamored with the concept. I think that few medical students choose psychiatry with the goal of referring all psychotherapeutic needs and intervention to “allied mental health providers” as my prior managed care organization liked to refer to psychologists, social workers, marriage and family therapists, and other counselors. I remember particularly as a chief resident being bombarded by complaints of therapists complaining about psychiatry residents. All of their patients’ symptoms allegedly required medication adjustment and residents were supposedly dismissing them. In return, residents would complain that the therapists did not address the psychological manifestations of the patient’s ailments. Herein lies my problem with split-care, it encourages psychotherapy to be about medication management, and medication management to be about psychotherapy.
However, this is not an article against split-treatment. Psychiatrists, for a variety of reasons, are not suited to perform psychotherapy in most management care models. The main reason being that psychiatrists’ time is too expensive to justify the expense, and psychiatrists are (for the most part), the only ones able to prescribe medications for which the wait-list is already long enough. This article is about the absurd levels at which we have fragmented care of certain patients. Split-treatment is relevant in that its negative side effects, we are almost all familiar with, exemplify the problem of the fragmentation of modern psychiatry. In many ways this fragmentation of care is similar to polypharmacy – the premise for each psychotropic intervention may be sound, but the end result is often incoherent.
My main concern with the fragmentation of modern psychiatry stems from my belief that the most important facet of our work is our relationship with our patients. It is the duty we owe them, the attention we give them, the unique nature of interactions. Who among the nine providers is responsible for writing a discharge summary? Who is responsible for calling an emergency contact in a critical situation? Who communicates with the new provider when someone is taken off an insurance panel? Who makes the patient feel cared for? I am often confronted by this situation when TMS or ketamine providers say, “I just give the procedure/medication that was ordered by the referring psychiatrist.” This response disturbs me in that I could not imagine myself being so hands off in the care of a patient. There is an implication of projected immunity and lack of responsibility that bothers me.
But my concerns are also practical. From my forensic experience, I am well aware that the larger the number of providers treating a patient, the larger the number of inconsistent diagnoses, the more likely medication reconciliations are not kept up to date or incorrect, and the more likely intervention recommendations are contrary to one another. A disengaged ketamine provider may not realize that the patient was more recently enrolled in a substance use disorder program, a potential contraindication for ketamine, if not well-abreast of the patient’s continued evolution. A substance use disorder psychiatric specialist may be at odds with a substance use disorder counselor who worries about the message of treating psychiatric symptoms with chemical substances if they don’t communicate.
As with polypharmacy, “polydoctoring” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to specialize, patients still desire and benefit from an intimate and close relationship with one provider who is warm, concerned, and hopeful. Those traits can theoretically be provided by anyone and there is not something inherently wrong with having more than one provider. However, psychiatry would be wise to recognize this concerning trend, especially at a time when we all feel lonely, disconnected, and depersonalized.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
How many providers does it take to depersonalize a patient? Nine? 1. A psychiatrist for transcranial magnetic stimulation (TMS). 2. A psychiatrist for ketamine. 3. A psychiatrist who specializes in substance use disorder medication. 4. A psychiatrist for the rest of the psychotropic medication. 5. An alternative medicine provider who prescribes supplements. 6. A therapist for depression who uses cognitive-behavioral therapy. 7. A therapist for posttraumatic stress disorder who uses eye movement desensitization and reprocessing. 8. An addiction counselor. 9. An equine therapist.
This doesn’t include other providers and professionals who likely contribute to one’s mental well-being, including yoga instructors and personal trainers. In addition, any one of those psychiatrists may have one or more nurse practitioners who routinely step in to attend to appointments.
In our uncertain and lonely times, the value of human contact and interaction has become exponentially more precious. I long to see my patients in my private practice office. I am now much more aware of their grounding effect on my life, and I suspect I had a similar grounding effect on theirs. Few things provide me more comfort than sitting on my lounge chair with a curious gaze waiting for the patient to start the visit. I often wonder what makes a patient choose to go see a private practice physician. Yet a common reason offered is, “Wait! You do everything? Therapy and meds if I need them? You’ll see me every week?”
While I am realistic about the need and use of split-care, I have never been enamored with the concept. I think that few medical students choose psychiatry with the goal of referring all psychotherapeutic needs and intervention to “allied mental health providers” as my prior managed care organization liked to refer to psychologists, social workers, marriage and family therapists, and other counselors. I remember particularly as a chief resident being bombarded by complaints of therapists complaining about psychiatry residents. All of their patients’ symptoms allegedly required medication adjustment and residents were supposedly dismissing them. In return, residents would complain that the therapists did not address the psychological manifestations of the patient’s ailments. Herein lies my problem with split-care, it encourages psychotherapy to be about medication management, and medication management to be about psychotherapy.
However, this is not an article against split-treatment. Psychiatrists, for a variety of reasons, are not suited to perform psychotherapy in most management care models. The main reason being that psychiatrists’ time is too expensive to justify the expense, and psychiatrists are (for the most part), the only ones able to prescribe medications for which the wait-list is already long enough. This article is about the absurd levels at which we have fragmented care of certain patients. Split-treatment is relevant in that its negative side effects, we are almost all familiar with, exemplify the problem of the fragmentation of modern psychiatry. In many ways this fragmentation of care is similar to polypharmacy – the premise for each psychotropic intervention may be sound, but the end result is often incoherent.
My main concern with the fragmentation of modern psychiatry stems from my belief that the most important facet of our work is our relationship with our patients. It is the duty we owe them, the attention we give them, the unique nature of interactions. Who among the nine providers is responsible for writing a discharge summary? Who is responsible for calling an emergency contact in a critical situation? Who communicates with the new provider when someone is taken off an insurance panel? Who makes the patient feel cared for? I am often confronted by this situation when TMS or ketamine providers say, “I just give the procedure/medication that was ordered by the referring psychiatrist.” This response disturbs me in that I could not imagine myself being so hands off in the care of a patient. There is an implication of projected immunity and lack of responsibility that bothers me.
But my concerns are also practical. From my forensic experience, I am well aware that the larger the number of providers treating a patient, the larger the number of inconsistent diagnoses, the more likely medication reconciliations are not kept up to date or incorrect, and the more likely intervention recommendations are contrary to one another. A disengaged ketamine provider may not realize that the patient was more recently enrolled in a substance use disorder program, a potential contraindication for ketamine, if not well-abreast of the patient’s continued evolution. A substance use disorder psychiatric specialist may be at odds with a substance use disorder counselor who worries about the message of treating psychiatric symptoms with chemical substances if they don’t communicate.
As with polypharmacy, “polydoctoring” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to specialize, patients still desire and benefit from an intimate and close relationship with one provider who is warm, concerned, and hopeful. Those traits can theoretically be provided by anyone and there is not something inherently wrong with having more than one provider. However, psychiatry would be wise to recognize this concerning trend, especially at a time when we all feel lonely, disconnected, and depersonalized.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Pandemic packed a year of distress into 1 month
The first month of the coronavirus pandemic created almost as much psychological distress among American adults as they had experienced in the year before February 2019, according to the results of two representative surveys.
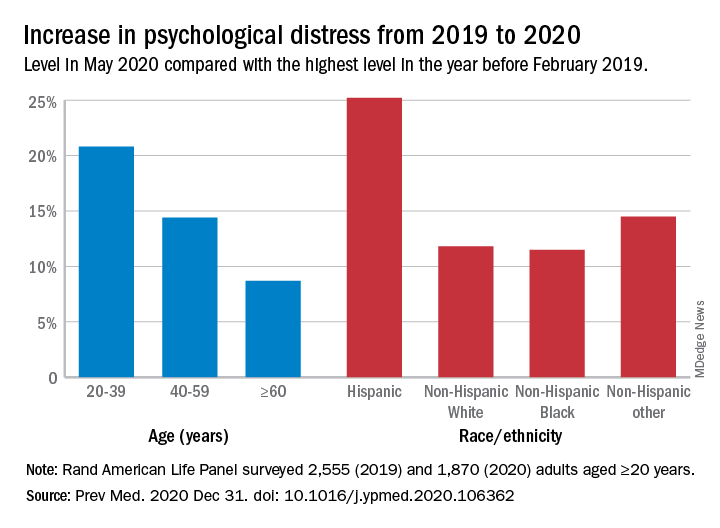
“The 30-day prevalence of SD [serious distress] in May 2020 did not differ from the past-year prevalence of SD assessed with the same instrument [the Kessler-6 distress scale] in February 2019. In other words, equal numbers of people experienced SD in 30-days during the pandemic as experienced SD over an entire year prior to the pandemic,” Joshua Breslau, PhD, and associates at the Rand Corporation wrote in Preventive Medicine.
In May of 2020, the prevalence of SD was 10.1% in the previous month among 1,870 adults aged 20 years and older who had participated in the two Rand American Life Panel surveys, the first occurring in February 2019. In that earlier poll, 10.9% of the 2,555 respondents said that they experienced SD in the worst month of the previous year, the investigators said.
The prevalence of overall psychological distress increased by 12.8% from February 2019 to May 2020, with increases higher among women (17.7%) than men (10.6%); adults under age 60 years, compared with those over 60 (see graph); and Hispanics, compared with other races/ethnicities. Disparities also were seen among income groups: Distress rose 10.2% for those earning over $100,000, compared with 15.4% for those making less than $35,000 and 18.2% for Americans earning between $35,000 and $60,000, the researchers reported.
A high level of stress in the prepandemic survey strongly predicted serious distress during the pandemic. “Risk for SD during the pandemic among those with SD during a year before the pandemic was almost 3 times higher than among those reporting mild/moderate distress and 15 times higher than among those reporting no/low distress during the prepandemic year,” they noted.
Distress levels often return to normal after a disaster, Dr. Breslau and associates pointed out, but “the pandemic’s influence on economic stressors, disruption of usual activities and subsequent effects on population health may continue for an extended period and affect different regions of the country at different points in time.”
SOURCE: Breslau J et al. Prev Med. 2020 Dec 31. doi: 10.1016/j.ypmed.2020.106362.
The first month of the coronavirus pandemic created almost as much psychological distress among American adults as they had experienced in the year before February 2019, according to the results of two representative surveys.
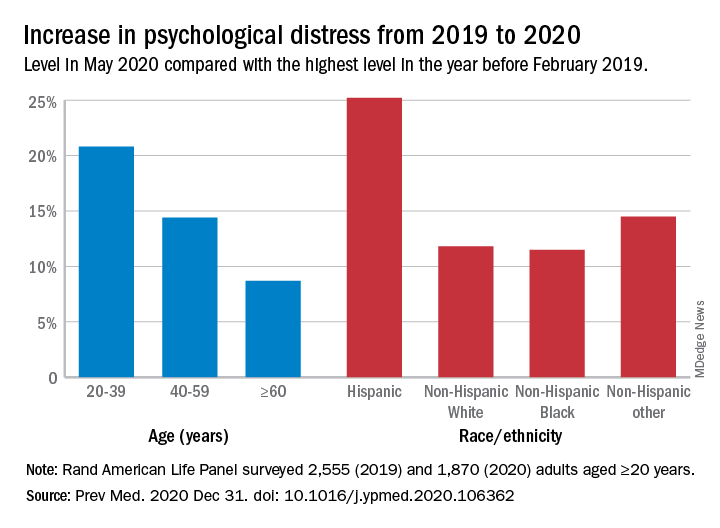
“The 30-day prevalence of SD [serious distress] in May 2020 did not differ from the past-year prevalence of SD assessed with the same instrument [the Kessler-6 distress scale] in February 2019. In other words, equal numbers of people experienced SD in 30-days during the pandemic as experienced SD over an entire year prior to the pandemic,” Joshua Breslau, PhD, and associates at the Rand Corporation wrote in Preventive Medicine.
In May of 2020, the prevalence of SD was 10.1% in the previous month among 1,870 adults aged 20 years and older who had participated in the two Rand American Life Panel surveys, the first occurring in February 2019. In that earlier poll, 10.9% of the 2,555 respondents said that they experienced SD in the worst month of the previous year, the investigators said.
The prevalence of overall psychological distress increased by 12.8% from February 2019 to May 2020, with increases higher among women (17.7%) than men (10.6%); adults under age 60 years, compared with those over 60 (see graph); and Hispanics, compared with other races/ethnicities. Disparities also were seen among income groups: Distress rose 10.2% for those earning over $100,000, compared with 15.4% for those making less than $35,000 and 18.2% for Americans earning between $35,000 and $60,000, the researchers reported.
A high level of stress in the prepandemic survey strongly predicted serious distress during the pandemic. “Risk for SD during the pandemic among those with SD during a year before the pandemic was almost 3 times higher than among those reporting mild/moderate distress and 15 times higher than among those reporting no/low distress during the prepandemic year,” they noted.
Distress levels often return to normal after a disaster, Dr. Breslau and associates pointed out, but “the pandemic’s influence on economic stressors, disruption of usual activities and subsequent effects on population health may continue for an extended period and affect different regions of the country at different points in time.”
SOURCE: Breslau J et al. Prev Med. 2020 Dec 31. doi: 10.1016/j.ypmed.2020.106362.
The first month of the coronavirus pandemic created almost as much psychological distress among American adults as they had experienced in the year before February 2019, according to the results of two representative surveys.
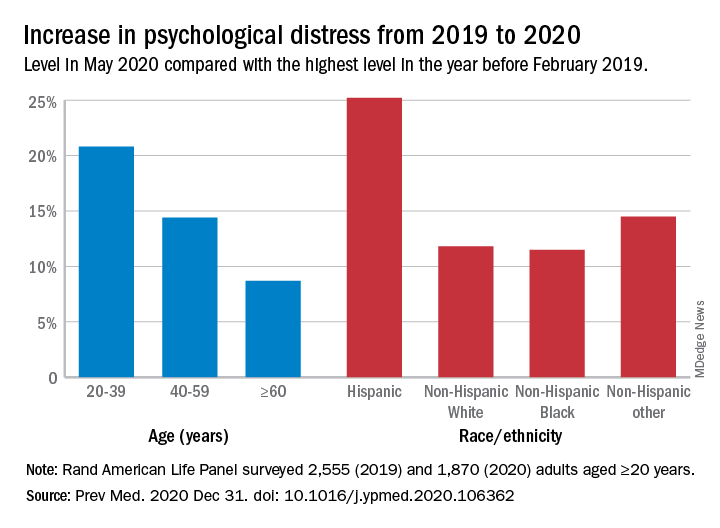
“The 30-day prevalence of SD [serious distress] in May 2020 did not differ from the past-year prevalence of SD assessed with the same instrument [the Kessler-6 distress scale] in February 2019. In other words, equal numbers of people experienced SD in 30-days during the pandemic as experienced SD over an entire year prior to the pandemic,” Joshua Breslau, PhD, and associates at the Rand Corporation wrote in Preventive Medicine.
In May of 2020, the prevalence of SD was 10.1% in the previous month among 1,870 adults aged 20 years and older who had participated in the two Rand American Life Panel surveys, the first occurring in February 2019. In that earlier poll, 10.9% of the 2,555 respondents said that they experienced SD in the worst month of the previous year, the investigators said.
The prevalence of overall psychological distress increased by 12.8% from February 2019 to May 2020, with increases higher among women (17.7%) than men (10.6%); adults under age 60 years, compared with those over 60 (see graph); and Hispanics, compared with other races/ethnicities. Disparities also were seen among income groups: Distress rose 10.2% for those earning over $100,000, compared with 15.4% for those making less than $35,000 and 18.2% for Americans earning between $35,000 and $60,000, the researchers reported.
A high level of stress in the prepandemic survey strongly predicted serious distress during the pandemic. “Risk for SD during the pandemic among those with SD during a year before the pandemic was almost 3 times higher than among those reporting mild/moderate distress and 15 times higher than among those reporting no/low distress during the prepandemic year,” they noted.
Distress levels often return to normal after a disaster, Dr. Breslau and associates pointed out, but “the pandemic’s influence on economic stressors, disruption of usual activities and subsequent effects on population health may continue for an extended period and affect different regions of the country at different points in time.”
SOURCE: Breslau J et al. Prev Med. 2020 Dec 31. doi: 10.1016/j.ypmed.2020.106362.
FROM PREVENTIVE MEDICINE
Collective trauma could lead to posttraumatic growth
Reflections for 2021
When we went to medical school, how many of us thought we would practice through a pandemic? For most of us, 2020 was the most challenging professional year of our lives. As a psychiatrist, I found it particularly odd to be struggling with the same issues as all of my patients and to have all my patients in crisis at the same time. I was repeatedly asked by friends, “How are your patients doing?” My reply, “About the same as the rest of us.” After a period of adapting, I felt truly blessed to be able to practice online. I know many of my colleagues did not have that luxury, and the stress you endured is hard to fathom.
Yet, as Friedrich Nietzsche said in so many words, “What doesn’t kill you, makes you stronger,” and here we are in a new year. As we enter 2021, we know so much more about COVID-19 than we did mere months ago, and many of us have been fortunate enough to be vaccinated already.
We should be very proud of our medical and scientific community, which has worked so hard to prevent and treat COVID-19. It is indeed a miracle of modern medicine that two vaccines made their way through development to distribution in under a year. It is a great relief that health care workers are first in line: Of the 4 million vaccine doses given worldwide, 2 million were to U.S. medical personnel. We can now track the number of people vaccinated around the globe.
Yet, “the darkest hour is just before the dawn.” We are currently in the riskiest part of the pandemic, and we must continue to work hard.
As 2021 progresses, we can expect to begin the long recovery process. We know we are innately wired to adapt to adversity and are therefore resilient. The key is to tap into this wiring by developing behaviors, habits, and strategies that support us.
Posttraumatic growth (PTG) is a theory in mental health that explains a kind of transformation following trauma. It was developed by psychologists Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, in the mid-1990s. They studied how people experienced positive growth following adversity. Dr. Tedeschi has said: “People develop new understandings of themselves, the world they live in, how to relate to other people, the kind of future they might have and a better understanding of how to live life.” One-half to two-thirds of individuals experiencing trauma will experience PTG. Given that our entire profession has gone through this collective trauma, far better times may indeed be ahead.
Resilience expert Eva Selhub, MD, suggests cultivating these six pillars:
- Physical vitality: The toll of 2020 has been enormous. If we are to rebound, we must care for ourselves. In our training, we were taught to put our health aside and work grueling hours. But to recover from trauma, we must attend to our own needs. Even after we are vaccinated, we must keep our nutritional status and immunity functioning at optimal levels. Let’s not get COVID-19 complacency. Clearly, health matters most. Ours included!
- Mental toughness: We made it through an incredibly grueling year, and we had to “build it as we sailed.” We figured out how to save as many lives as we could and simultaneously keep ourselves and our families safe. We have seen things previously unimaginable. We have adjusted to telemedicine. We have lived with far fewer pleasures. We have cultivated multiple ways to tame our anxieties. The year 2020 is one we can be proud of for ourselves and our colleagues. We have come a long way in a short time.
- Emotional balance: Anxiety and depression were easy to fall into in 2020. But as the pandemic subsides, the pendulum will swing the other way. The 1918 pandemic gave rise to the Roaring Twenties. What will the next chapter in our civilization bring?
- Loving and strong connections. Our relationships are what give depth and meaning to our lives, and these relationships are crucial now so we can heal. How can we nourish our connections? What toll has the pandemic taken on those closest to you? Did some friends or family step up and help? Can we move out of our caretaker role and allow others to care for us?
- Spiritual connection: Facing so much grief and suffering, we have had an opportunity to look at our own lives from a different perspective. It has been an important year for reflection. How can we cultivate a deeper appreciation recognizing that every day is truly a gift? Did you find more purpose in your work last year? What sustained you in your time of need?
- Inspiring leadership: As health care professionals, we must set an example. We must show our patients and our families how resilient we can be. Let’s grow from trauma and avoid succumbing to depression, self-destructive tendencies, and divisiveness. We must continue to care for ourselves, our patients, and our community and work together to ensure a brighter and safer future for all.
Wishing you a safe, happy and healthy 2021.
“I am not what happened to me, I am what I choose to become.”
– Carl Jung, PhD
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Mimosa Publishing, 2018). She has no conflicts of interest.
Reflections for 2021
Reflections for 2021
When we went to medical school, how many of us thought we would practice through a pandemic? For most of us, 2020 was the most challenging professional year of our lives. As a psychiatrist, I found it particularly odd to be struggling with the same issues as all of my patients and to have all my patients in crisis at the same time. I was repeatedly asked by friends, “How are your patients doing?” My reply, “About the same as the rest of us.” After a period of adapting, I felt truly blessed to be able to practice online. I know many of my colleagues did not have that luxury, and the stress you endured is hard to fathom.
Yet, as Friedrich Nietzsche said in so many words, “What doesn’t kill you, makes you stronger,” and here we are in a new year. As we enter 2021, we know so much more about COVID-19 than we did mere months ago, and many of us have been fortunate enough to be vaccinated already.
We should be very proud of our medical and scientific community, which has worked so hard to prevent and treat COVID-19. It is indeed a miracle of modern medicine that two vaccines made their way through development to distribution in under a year. It is a great relief that health care workers are first in line: Of the 4 million vaccine doses given worldwide, 2 million were to U.S. medical personnel. We can now track the number of people vaccinated around the globe.
Yet, “the darkest hour is just before the dawn.” We are currently in the riskiest part of the pandemic, and we must continue to work hard.
As 2021 progresses, we can expect to begin the long recovery process. We know we are innately wired to adapt to adversity and are therefore resilient. The key is to tap into this wiring by developing behaviors, habits, and strategies that support us.
Posttraumatic growth (PTG) is a theory in mental health that explains a kind of transformation following trauma. It was developed by psychologists Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, in the mid-1990s. They studied how people experienced positive growth following adversity. Dr. Tedeschi has said: “People develop new understandings of themselves, the world they live in, how to relate to other people, the kind of future they might have and a better understanding of how to live life.” One-half to two-thirds of individuals experiencing trauma will experience PTG. Given that our entire profession has gone through this collective trauma, far better times may indeed be ahead.
Resilience expert Eva Selhub, MD, suggests cultivating these six pillars:
- Physical vitality: The toll of 2020 has been enormous. If we are to rebound, we must care for ourselves. In our training, we were taught to put our health aside and work grueling hours. But to recover from trauma, we must attend to our own needs. Even after we are vaccinated, we must keep our nutritional status and immunity functioning at optimal levels. Let’s not get COVID-19 complacency. Clearly, health matters most. Ours included!
- Mental toughness: We made it through an incredibly grueling year, and we had to “build it as we sailed.” We figured out how to save as many lives as we could and simultaneously keep ourselves and our families safe. We have seen things previously unimaginable. We have adjusted to telemedicine. We have lived with far fewer pleasures. We have cultivated multiple ways to tame our anxieties. The year 2020 is one we can be proud of for ourselves and our colleagues. We have come a long way in a short time.
- Emotional balance: Anxiety and depression were easy to fall into in 2020. But as the pandemic subsides, the pendulum will swing the other way. The 1918 pandemic gave rise to the Roaring Twenties. What will the next chapter in our civilization bring?
- Loving and strong connections. Our relationships are what give depth and meaning to our lives, and these relationships are crucial now so we can heal. How can we nourish our connections? What toll has the pandemic taken on those closest to you? Did some friends or family step up and help? Can we move out of our caretaker role and allow others to care for us?
- Spiritual connection: Facing so much grief and suffering, we have had an opportunity to look at our own lives from a different perspective. It has been an important year for reflection. How can we cultivate a deeper appreciation recognizing that every day is truly a gift? Did you find more purpose in your work last year? What sustained you in your time of need?
- Inspiring leadership: As health care professionals, we must set an example. We must show our patients and our families how resilient we can be. Let’s grow from trauma and avoid succumbing to depression, self-destructive tendencies, and divisiveness. We must continue to care for ourselves, our patients, and our community and work together to ensure a brighter and safer future for all.
Wishing you a safe, happy and healthy 2021.
“I am not what happened to me, I am what I choose to become.”
– Carl Jung, PhD
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Mimosa Publishing, 2018). She has no conflicts of interest.
When we went to medical school, how many of us thought we would practice through a pandemic? For most of us, 2020 was the most challenging professional year of our lives. As a psychiatrist, I found it particularly odd to be struggling with the same issues as all of my patients and to have all my patients in crisis at the same time. I was repeatedly asked by friends, “How are your patients doing?” My reply, “About the same as the rest of us.” After a period of adapting, I felt truly blessed to be able to practice online. I know many of my colleagues did not have that luxury, and the stress you endured is hard to fathom.
Yet, as Friedrich Nietzsche said in so many words, “What doesn’t kill you, makes you stronger,” and here we are in a new year. As we enter 2021, we know so much more about COVID-19 than we did mere months ago, and many of us have been fortunate enough to be vaccinated already.
We should be very proud of our medical and scientific community, which has worked so hard to prevent and treat COVID-19. It is indeed a miracle of modern medicine that two vaccines made their way through development to distribution in under a year. It is a great relief that health care workers are first in line: Of the 4 million vaccine doses given worldwide, 2 million were to U.S. medical personnel. We can now track the number of people vaccinated around the globe.
Yet, “the darkest hour is just before the dawn.” We are currently in the riskiest part of the pandemic, and we must continue to work hard.
As 2021 progresses, we can expect to begin the long recovery process. We know we are innately wired to adapt to adversity and are therefore resilient. The key is to tap into this wiring by developing behaviors, habits, and strategies that support us.
Posttraumatic growth (PTG) is a theory in mental health that explains a kind of transformation following trauma. It was developed by psychologists Richard Tedeschi, PhD, and Lawrence Calhoun, PhD, in the mid-1990s. They studied how people experienced positive growth following adversity. Dr. Tedeschi has said: “People develop new understandings of themselves, the world they live in, how to relate to other people, the kind of future they might have and a better understanding of how to live life.” One-half to two-thirds of individuals experiencing trauma will experience PTG. Given that our entire profession has gone through this collective trauma, far better times may indeed be ahead.
Resilience expert Eva Selhub, MD, suggests cultivating these six pillars:
- Physical vitality: The toll of 2020 has been enormous. If we are to rebound, we must care for ourselves. In our training, we were taught to put our health aside and work grueling hours. But to recover from trauma, we must attend to our own needs. Even after we are vaccinated, we must keep our nutritional status and immunity functioning at optimal levels. Let’s not get COVID-19 complacency. Clearly, health matters most. Ours included!
- Mental toughness: We made it through an incredibly grueling year, and we had to “build it as we sailed.” We figured out how to save as many lives as we could and simultaneously keep ourselves and our families safe. We have seen things previously unimaginable. We have adjusted to telemedicine. We have lived with far fewer pleasures. We have cultivated multiple ways to tame our anxieties. The year 2020 is one we can be proud of for ourselves and our colleagues. We have come a long way in a short time.
- Emotional balance: Anxiety and depression were easy to fall into in 2020. But as the pandemic subsides, the pendulum will swing the other way. The 1918 pandemic gave rise to the Roaring Twenties. What will the next chapter in our civilization bring?
- Loving and strong connections. Our relationships are what give depth and meaning to our lives, and these relationships are crucial now so we can heal. How can we nourish our connections? What toll has the pandemic taken on those closest to you? Did some friends or family step up and help? Can we move out of our caretaker role and allow others to care for us?
- Spiritual connection: Facing so much grief and suffering, we have had an opportunity to look at our own lives from a different perspective. It has been an important year for reflection. How can we cultivate a deeper appreciation recognizing that every day is truly a gift? Did you find more purpose in your work last year? What sustained you in your time of need?
- Inspiring leadership: As health care professionals, we must set an example. We must show our patients and our families how resilient we can be. Let’s grow from trauma and avoid succumbing to depression, self-destructive tendencies, and divisiveness. We must continue to care for ourselves, our patients, and our community and work together to ensure a brighter and safer future for all.
Wishing you a safe, happy and healthy 2021.
“I am not what happened to me, I am what I choose to become.”
– Carl Jung, PhD
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Mimosa Publishing, 2018). She has no conflicts of interest.
Zoom Zoom Zoom: An end-of-year update from a virtual psychiatrist
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
In mid-April, a month into pandemic life with a stay-at-home order, I wrote about my experiences as a virtual outpatient psychiatrist in private practice. It’s been 10 months now and with this tragic year drawing to a close, it seems like a good time for an update.
In that April column, I describe how I created a makeshift home office. This entailed pushing my son’s baseball card collection and dusty sports trophies to the side of the room, bringing in a desk and a rug, a house plant, and a statue of a Buddha. I enjoyed watching out the window behind my computer screen as the neighbors and their dogs walked by, and I loved seeing the tree out the window blossom into gorgeous flowers.
With time, my physical space has changed. The remnants of my son’s childhood have all been moved to a closet, artwork has been added to the wall behind me, and the space is now clearly an office, though my laptop remains propped on a pile of books so that no one is looking up my nose. The room, with four large windows facing north and west, has issues with temperature control. In an old house, the heat works all too well in the adjacent bedroom (while the rest of the occupants in other rooms freeze), but the office itself has no heat: I have added both a fan and a space heater, and there are some very cold days where I’ve propped open one of the windows. And with the shortened days, large windows on two walls have presented a challenge as the sun changes positions throughout the day – there are times when the sun’s rays streak across my face in such a way that I look rather ethereal, and between sessions I have lowered, raised, and adjusted the blinds to avoid this. I finally pulled off the thin metal venetian blinds and took them to Lowe’s, where a partially masked young woman cut me new blinds with larger slats. An ergonomic office chair has replaced the wicker Ikea chair I was using, and between all these machinations, I am now physically comfortable most of the time. I believe I am still a bit too pixelated on the screen, but my patients are not complaining, and when the natural lighting fades at 4:30 p.m., the overhead lighting is all wrong again. These all are things I never considered – or long ago addressed – in my real-life practice of psychiatry in a office I have loved for years.
With time, I’ve grown more comfortable working from home on a screen and there are things about this life I’ve grown to like. My husband no longer travels, my daughter – my gift of the pandemic – returned home from New York City where she was in her final months of graduate school, and these unexpected months with her (and her cat) have been a pleasure. There is something nice about being trapped at home with people I love, even if we are all in our respective places, in front of our separate screens. There has been time for long walks, trips to the beach, and long bike rides. And as my daughter now prepares to move to Denver, I have been heartened by the hope of vaccines, and the knowledge that I will likely be able to see her again in the coming months. The people are not the only ones who have benefited from this time at home together – I have no idea how we would have managed with our elderly dog if we were not home to care for him.
My life has become more efficient. I used to find myself aggravated when patients forgot their appointments, a not-infrequent occurrence. People no longer get caught in traffic, they come on time, and they don’t complain about my crowded parking lot. When there is down time, I use it more efficiently at home – a load of laundry gets done, I get a chance to turn on the news or exercise, or make dinner early. And because I have two other family members working from home, I am not the only one mixing work with chores or exercise.
While my medical colleagues who work in settings where they must see patients in person have struggled or functioned in some state of denial, I have felt safe and protected, a bit cocooned with my family in a house big enough to give us all space, in a neighborhood with sidewalks and places to walk, and to protect my sanity, I am lucky to have a patio that has now been equipped with lights, patio heaters, a fire pit, and socially distanced tables so that I can still see friends outside.
Telemedicine has added a new dimension to treatment. I’ve had family sessions with multiple people joining a zoom link from different locations – so much easier than coordinating a time when everyone can travel to my office. I’ve had patients call in from cars and from closets in search of privacy, and from their gardens and poolsides. I’ve met spouses, children, many a dog and cat, plus the more unusual of pets and farm animals, including a goat, ferret, lizard, African grey parrot, and guinea pigs.
These are the good things, and while I wish I could say it was all good, so much of what remains is laden with anxiety. My son lives nearby, but he has shared a house with a hospital worker for much of the past year and there were COVID scares, months at a time without so much as a hug, and my husband has not seen his parents or brother for a year now. There are the awkward waves or salutes with friends I once gave carefree hugs, the constant thoughts of how far away is that person standing, and each person’s “beliefs” about what is safe when we still don’t fully understand how this virus spreads. I worry for myself, I worry for my family and friends, and I worry for my patients when they tell me about behaviors that clearly are not safe.
At first, I found my work as a telepsychiatrist to be exhausting, and I assumed it was because my patients were now just faces, inches from my own eyes, and no longer diffused by a visual field that included my whole office and the opportunity to break eye contact while I still listened with full attention. This has gotten much better – I’ve adjusted to my on-screen relationships, but what has not gotten better is both the acuity, and sometimes the boredom.
Patients are struggling; they are sad, lonely, and missing the richness of their former lives. They miss friends, meeting new people, cultural experiences, diversity in how they spend their time, and travel. They have all the same human experiences of loss, illness, and grief, but with the added burden of struggling alone or within the confines of pandemic life that has destroyed our ability to mark events with social and religious customs that guide healing. People who had done well for years are now needing more, and those who were not doing well are doing worse. It makes for long days.
I mentioned boredom: With less time spent with other people, so many sessions are about COVID – who has it, who might have it, what people are doing to avoid it, and still, how they get their groceries. The second most popular psychotherapy topic includes what they are watching on Netflix, and as human beings trudging through this together, I have appreciated my patients’ suggestions as much as they have appreciated mine.* Life for all of us has come to be more about survival, and less about self-discovery and striving. Many sessions have started to feel the same from 1 hour to the next, in ways they never did before.
There are other aspects to telepsychiatry that I have found difficult. The site I have used most – Doxy.me – works well with some patients, but with others there are technical problems. Sessions freeze, the sound goes in or out, and we end up switching to another platform, which may or may not work better. Sometimes patients have the camera at odd angles, or they bounce a laptop on their knees to the point that I get seasick. One of my family members has said that I can sometimes be overheard, so I now have a radio playing classical music outside my door, and I often use earbuds so that the patient can’t be overheard and I speak more softly with them – this has all been good in terms of improving privacy, but after a while I find that it’s stressful to have people talking to me inside my own ears! These are little kinks, but when you do it for hours a day, they add up to a sense of being stressed in ways that in-person psychiatry does not lend itself to.
Finally, three seasons into my work-at-home life, I still have not found a new rhythm for some of the logistical aspects of private practice that came so easily in my office. My mail still goes to the office, the plants there still need water, my files and computer are there, but tasks that were once a seamless part of my work day now spill into my time off and I go into the office each week to file, log medications, and attend to the business of my practice. My smartphone, with its ability to e-prescribe, invoice, and fax, has made it possible for me to manage and certainly, outpatient psychiatrists are very lucky that we have the option to continue our work with patients remotely during such difficult times.
I have sent people for virtual intensive substance treatment, and to virtual couples’ counseling, and these remote treatments have been useful. The one treatment that has been very difficult for patients to negotiate has been outpatient electroconvulsive therapy – this requires coordination with another person to drive the patient to treatments (and to wait outside in the parking lot), and also for separate weekly COVID testing. Transcranial magnetic stimulation, which also is still being done in person, has not been any different – patients can drive themselves and the one center I referred to has not required preprocedure COVID testing.
What does the future hold? Will we ever go back to practicing the way we did? While some of my patients miss real-life therapy, most do not; they too like the added efficiency, getting treatment from the comfort of their home without the stress of finding the time to travel. I’ve taken on new patients during this time, and while I anticipated that it would be difficult, it has gone surprisingly well – people I have never met in real life talk to me with ease, and both psychotherapy and medication management have gone well. The one area that I have found most difficult is assessing tremors and dyskinesias, and one patient mentioned she has gained nearly 50 pounds over the past year – something I certainly would have noticed and attended to sooner in real life. I have mixed feelings about returning to a completely live practice. I think I would like a combination where I see all my patients in person once in a while, but would like to be able to offer some times where I see people virtually from home at least one day a week.
Time will tell how that plays out with insurers. My best guess is that, with the lowered no-show rates that everyone is seeing and the higher levels of depression and anxiety that people are having, this may have been a costly time for mental health care. At the same time, inpatient psychiatric units have decreased their capacity, and perhaps more efficient delivery of outpatient care has lowered the overall cost. I suppose we will wait to hear, but for many, the transition to virtual care has allowed many people to get treatment who would have otherwise gone without care.
In my April article, I mentioned that I was having daily Facetime check-in visits with a distressed patient who was on a COVID unit with pneumonia. Since then, I have had several more patients contract COVID, and many of my patients have had family members who have tested positive or become symptomatic with COVID. It has been nice to have sessions with people during this time, and thankfully, I have not had any more patients who have required hospitalization for the virus.
I still catch myself thinking that, of all the things I have worried about over the years, “pandemic” was never on my list. It seems so strange that I left my office on a Friday with no idea that I would not be returning to work the following Monday, or that life would change in such a radical way. As we leave this awful year behind and greet the new one with the hope that vaccines and a new administration might offer solutions, I’d like to wish my readers the best for a healthy, safe, and gentle New Year.
*My top viewing picks for now are “The Queen’s Gambit” (Netflix), and “A Place to Call Home” (Acorn).
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
New resilience center targets traumatized health care workers
A physician assistant participating in a virtual workshop began to cry, confessing that she felt overwhelmed with guilt because New Yorkers were hailing her as a frontline hero in the pandemic. That was when Joe Ciavarro knew he was in the right place.
“She was saying all the things I could not verbalize because I, too, didn’t feel like I deserved all this praise and thousands of people cheering for us every evening when people were losing jobs, didn’t have money for food, and their loved ones were dying without family at their side,” says Mr. Ciavarro, a PA at Mount Sinai Medical Center in New York.
Mr. Ciavarro, who also manages 170 other PAs on two of Mount Sinai’s campuses in Manhattan, has been on the front lines since COVID-19 first hit; he lost a colleague and friend to suicide in September.
The mental anguish from his job prompted him to sign up for the resilience workshop offered by Mount Sinai’s Center for Stress, Resilience, and Personal Growth. The center – the first of its kind in North America – was launched in June to help health care workers like him cope with the intense psychological pressures they were facing. The weekly workshops became a safe place where Mr. Ciavarro and other staff members could share their darkest fears and learn ways to help them deal with their situation.
“It’s been grueling but we learned how to take care of ourselves so we can take care of our patients,” said Mr. Ciavarro. “This has become like a guided group therapy session on ways to manage and develop resilience. And I feel like my emotions are validated, knowing that others feel the same way.”
Caring for their own
Medical professionals treating patients with COVID-19 are in similar predicaments, and the psychological fallout is enormous: They’re exhausted by the seemingly never-ending patient load and staffing shortages, and haunted by fears for their own safety and that of their families. Studies in China, Canada, and Italy have revealed that a significant number of doctors and nurses in the early days of the pandemic experienced high levels of distress, depression, anxiety, nightmares, and insomnia.
after witnessing the deaths of so many patients who were alone, without family.
But the resilience workshop that Mr. Ciavarro attended offers some hope and is part of a multifaceted program that aims to be a model for other institutions and communities. The Mount Sinai health system already had some programs in place, including centers for 9/11 responders, for spirituality and health, and a wellness program to aid burned-out doctors. But the leadership at Mount Sinai, which includes psychiatrist Dennis Charney, MD, dean of the medical school and a leading expert on PTSD, knew early in the pandemic that emotional and psychological distress would plague health care workers, according to Deborah Marin, MD, director of the new center.
“We decided to quickly put in place a program that we could do virtually, with workshops and apps, that would give access to several services above and beyond what was already going on,” says Dr. Marin, a professor of psychiatry at the Icahn School of Medicine at Mount Sinai, New York, who also directs their center for spirituality and health.
The key components include a comprehensive screening tool that helps doctors at the center identify which potential participants are most at risk. Participants build personal inventories that detail the intensity of work-related exposures, personal or family stressors that have arisen because of the pandemic, or any mental health conditions or substance abuse problems that may make staff members more vulnerable.
The weekly workshops led by trained staff are designed to give participants the tools to foster resilience and process their experiences. Online apps provide feedback on their progress and engage them with video and other resources around meditation, relaxation, and resilience techniques.
In addition, all 40,000 members of the Mount Sinai staff are eligible for up to 14 one-on-one sessions with psychologists and psychiatrists who specialize in treating trauma.
“That’s highly unusual – to offer this at no cost to everyone,” said Dr. Marin. “We also have a treatment service that is specifically focused on behavioral health care, so people can learn better coping strategies, and we also have social workers to provide coaching.”
While the center doesn’t have specific numbers on how many nurses, physicians, and other staff have participated in treatment, they have trained over 70 peer leaders for their five workshops that home in on the most important factors of resilience.
“We’ve gotten enthusiastic responses from PAs and nurses,” said Craig Katz, MD, an expert in disaster psychiatry at Mount Sinai and a workshop moderator. Physicians have been slower to get on board. “Doctors are a tough nut to crack – it’s largely a culture where they may burn out but don’t want to talk about it. And asking for help is a hard transition for physicians to make.”
How to protect in midst of trauma
In formulating the program’s platform, Mount Sinai experts drew upon their extensive experience aiding 9/11 responders at the World Trade Center (WTC), as well as their system-wide wellness program that aids demoralized and burned-out physicians. While the reach of the pandemic is much broader than 9/11, experts see some commonalities in conditions that emerge after traumatic events, and they also discovered what can help.
“We learned from our WTC experience about what are protective factors – what are the social supports that buffer against depression, anxiety, and PTSD,” said Jonathan DePierro, PhD, clinical director of CSRPG and a psychologist at the Mount Sinai WTC Mental Health Program. “We also learned that people who have more prolonged exposures are at greater risk of developing mental health difficulties.”
The program itself reflects these lessons – and that’s why it’s open to all employees, not just medical professionals. Housekeepers, security staffers, even construction workers are also dealing with their lives being in danger. “That wasn’t in their job description,” said Dr. DePierro. “These people tend to have fewer social and economic resources, make less money and have fewer structural supports, which makes them even more vulnerable.”
Dr. Charney’s strategies on building resilience became a bible of sorts for the workshops, according to Dr. Katz, who authored the training curriculum. Sessions deal with how to build up reservoirs of realistic optimism, keep gratitude journals, find spiritual meaning in their lives, maintain physical wellness and create networks of social support. The workshops are meant to help participants create action plans, to reach out for support in their social networks, and keep the focus on the positives.
The goal is to give demoralized health care workers a renewed sense of competence. “The resilience workshop is a launching point to get people to show up and talk,” said Dr. Katz. “And if we do that, we’ve accomplished a lot just getting people in the door.”
The center will also have a research component to identify what works and what doesn’t so their platform can provide a template for other institutions; Dr. Marin said they’ve gotten inquiries about the program from major hospital systems in Michigan and California. They’ll also conduct longitudinal research to determine what lingering problems persist among healthcare workers over time.
Since the center opened its virtual doors, the curriculum has also been altered in response to feedback from the support staff, many of whom live in the community that surrounds Mount Sinai in northern Manhattan, which is largely lower-income Latinx and Black individuals. Workshop materials have been translated into Spanish and now feature people who reflect a more diverse set of experiences.
“Many of our employees and the population we serve identify as non-White so we’ve been doing outreach with a lot of the local unions,” said Dr. Marin. “Our next step is to take what we’re doing and work with local community organizations.”
A version of this article first appeared on Medscape.com.
A physician assistant participating in a virtual workshop began to cry, confessing that she felt overwhelmed with guilt because New Yorkers were hailing her as a frontline hero in the pandemic. That was when Joe Ciavarro knew he was in the right place.
“She was saying all the things I could not verbalize because I, too, didn’t feel like I deserved all this praise and thousands of people cheering for us every evening when people were losing jobs, didn’t have money for food, and their loved ones were dying without family at their side,” says Mr. Ciavarro, a PA at Mount Sinai Medical Center in New York.
Mr. Ciavarro, who also manages 170 other PAs on two of Mount Sinai’s campuses in Manhattan, has been on the front lines since COVID-19 first hit; he lost a colleague and friend to suicide in September.
The mental anguish from his job prompted him to sign up for the resilience workshop offered by Mount Sinai’s Center for Stress, Resilience, and Personal Growth. The center – the first of its kind in North America – was launched in June to help health care workers like him cope with the intense psychological pressures they were facing. The weekly workshops became a safe place where Mr. Ciavarro and other staff members could share their darkest fears and learn ways to help them deal with their situation.
“It’s been grueling but we learned how to take care of ourselves so we can take care of our patients,” said Mr. Ciavarro. “This has become like a guided group therapy session on ways to manage and develop resilience. And I feel like my emotions are validated, knowing that others feel the same way.”
Caring for their own
Medical professionals treating patients with COVID-19 are in similar predicaments, and the psychological fallout is enormous: They’re exhausted by the seemingly never-ending patient load and staffing shortages, and haunted by fears for their own safety and that of their families. Studies in China, Canada, and Italy have revealed that a significant number of doctors and nurses in the early days of the pandemic experienced high levels of distress, depression, anxiety, nightmares, and insomnia.
after witnessing the deaths of so many patients who were alone, without family.
But the resilience workshop that Mr. Ciavarro attended offers some hope and is part of a multifaceted program that aims to be a model for other institutions and communities. The Mount Sinai health system already had some programs in place, including centers for 9/11 responders, for spirituality and health, and a wellness program to aid burned-out doctors. But the leadership at Mount Sinai, which includes psychiatrist Dennis Charney, MD, dean of the medical school and a leading expert on PTSD, knew early in the pandemic that emotional and psychological distress would plague health care workers, according to Deborah Marin, MD, director of the new center.
“We decided to quickly put in place a program that we could do virtually, with workshops and apps, that would give access to several services above and beyond what was already going on,” says Dr. Marin, a professor of psychiatry at the Icahn School of Medicine at Mount Sinai, New York, who also directs their center for spirituality and health.
The key components include a comprehensive screening tool that helps doctors at the center identify which potential participants are most at risk. Participants build personal inventories that detail the intensity of work-related exposures, personal or family stressors that have arisen because of the pandemic, or any mental health conditions or substance abuse problems that may make staff members more vulnerable.
The weekly workshops led by trained staff are designed to give participants the tools to foster resilience and process their experiences. Online apps provide feedback on their progress and engage them with video and other resources around meditation, relaxation, and resilience techniques.
In addition, all 40,000 members of the Mount Sinai staff are eligible for up to 14 one-on-one sessions with psychologists and psychiatrists who specialize in treating trauma.
“That’s highly unusual – to offer this at no cost to everyone,” said Dr. Marin. “We also have a treatment service that is specifically focused on behavioral health care, so people can learn better coping strategies, and we also have social workers to provide coaching.”
While the center doesn’t have specific numbers on how many nurses, physicians, and other staff have participated in treatment, they have trained over 70 peer leaders for their five workshops that home in on the most important factors of resilience.
“We’ve gotten enthusiastic responses from PAs and nurses,” said Craig Katz, MD, an expert in disaster psychiatry at Mount Sinai and a workshop moderator. Physicians have been slower to get on board. “Doctors are a tough nut to crack – it’s largely a culture where they may burn out but don’t want to talk about it. And asking for help is a hard transition for physicians to make.”
How to protect in midst of trauma
In formulating the program’s platform, Mount Sinai experts drew upon their extensive experience aiding 9/11 responders at the World Trade Center (WTC), as well as their system-wide wellness program that aids demoralized and burned-out physicians. While the reach of the pandemic is much broader than 9/11, experts see some commonalities in conditions that emerge after traumatic events, and they also discovered what can help.
“We learned from our WTC experience about what are protective factors – what are the social supports that buffer against depression, anxiety, and PTSD,” said Jonathan DePierro, PhD, clinical director of CSRPG and a psychologist at the Mount Sinai WTC Mental Health Program. “We also learned that people who have more prolonged exposures are at greater risk of developing mental health difficulties.”
The program itself reflects these lessons – and that’s why it’s open to all employees, not just medical professionals. Housekeepers, security staffers, even construction workers are also dealing with their lives being in danger. “That wasn’t in their job description,” said Dr. DePierro. “These people tend to have fewer social and economic resources, make less money and have fewer structural supports, which makes them even more vulnerable.”
Dr. Charney’s strategies on building resilience became a bible of sorts for the workshops, according to Dr. Katz, who authored the training curriculum. Sessions deal with how to build up reservoirs of realistic optimism, keep gratitude journals, find spiritual meaning in their lives, maintain physical wellness and create networks of social support. The workshops are meant to help participants create action plans, to reach out for support in their social networks, and keep the focus on the positives.
The goal is to give demoralized health care workers a renewed sense of competence. “The resilience workshop is a launching point to get people to show up and talk,” said Dr. Katz. “And if we do that, we’ve accomplished a lot just getting people in the door.”
The center will also have a research component to identify what works and what doesn’t so their platform can provide a template for other institutions; Dr. Marin said they’ve gotten inquiries about the program from major hospital systems in Michigan and California. They’ll also conduct longitudinal research to determine what lingering problems persist among healthcare workers over time.
Since the center opened its virtual doors, the curriculum has also been altered in response to feedback from the support staff, many of whom live in the community that surrounds Mount Sinai in northern Manhattan, which is largely lower-income Latinx and Black individuals. Workshop materials have been translated into Spanish and now feature people who reflect a more diverse set of experiences.
“Many of our employees and the population we serve identify as non-White so we’ve been doing outreach with a lot of the local unions,” said Dr. Marin. “Our next step is to take what we’re doing and work with local community organizations.”
A version of this article first appeared on Medscape.com.
A physician assistant participating in a virtual workshop began to cry, confessing that she felt overwhelmed with guilt because New Yorkers were hailing her as a frontline hero in the pandemic. That was when Joe Ciavarro knew he was in the right place.
“She was saying all the things I could not verbalize because I, too, didn’t feel like I deserved all this praise and thousands of people cheering for us every evening when people were losing jobs, didn’t have money for food, and their loved ones were dying without family at their side,” says Mr. Ciavarro, a PA at Mount Sinai Medical Center in New York.
Mr. Ciavarro, who also manages 170 other PAs on two of Mount Sinai’s campuses in Manhattan, has been on the front lines since COVID-19 first hit; he lost a colleague and friend to suicide in September.
The mental anguish from his job prompted him to sign up for the resilience workshop offered by Mount Sinai’s Center for Stress, Resilience, and Personal Growth. The center – the first of its kind in North America – was launched in June to help health care workers like him cope with the intense psychological pressures they were facing. The weekly workshops became a safe place where Mr. Ciavarro and other staff members could share their darkest fears and learn ways to help them deal with their situation.
“It’s been grueling but we learned how to take care of ourselves so we can take care of our patients,” said Mr. Ciavarro. “This has become like a guided group therapy session on ways to manage and develop resilience. And I feel like my emotions are validated, knowing that others feel the same way.”
Caring for their own
Medical professionals treating patients with COVID-19 are in similar predicaments, and the psychological fallout is enormous: They’re exhausted by the seemingly never-ending patient load and staffing shortages, and haunted by fears for their own safety and that of their families. Studies in China, Canada, and Italy have revealed that a significant number of doctors and nurses in the early days of the pandemic experienced high levels of distress, depression, anxiety, nightmares, and insomnia.
after witnessing the deaths of so many patients who were alone, without family.
But the resilience workshop that Mr. Ciavarro attended offers some hope and is part of a multifaceted program that aims to be a model for other institutions and communities. The Mount Sinai health system already had some programs in place, including centers for 9/11 responders, for spirituality and health, and a wellness program to aid burned-out doctors. But the leadership at Mount Sinai, which includes psychiatrist Dennis Charney, MD, dean of the medical school and a leading expert on PTSD, knew early in the pandemic that emotional and psychological distress would plague health care workers, according to Deborah Marin, MD, director of the new center.
“We decided to quickly put in place a program that we could do virtually, with workshops and apps, that would give access to several services above and beyond what was already going on,” says Dr. Marin, a professor of psychiatry at the Icahn School of Medicine at Mount Sinai, New York, who also directs their center for spirituality and health.
The key components include a comprehensive screening tool that helps doctors at the center identify which potential participants are most at risk. Participants build personal inventories that detail the intensity of work-related exposures, personal or family stressors that have arisen because of the pandemic, or any mental health conditions or substance abuse problems that may make staff members more vulnerable.
The weekly workshops led by trained staff are designed to give participants the tools to foster resilience and process their experiences. Online apps provide feedback on their progress and engage them with video and other resources around meditation, relaxation, and resilience techniques.
In addition, all 40,000 members of the Mount Sinai staff are eligible for up to 14 one-on-one sessions with psychologists and psychiatrists who specialize in treating trauma.
“That’s highly unusual – to offer this at no cost to everyone,” said Dr. Marin. “We also have a treatment service that is specifically focused on behavioral health care, so people can learn better coping strategies, and we also have social workers to provide coaching.”
While the center doesn’t have specific numbers on how many nurses, physicians, and other staff have participated in treatment, they have trained over 70 peer leaders for their five workshops that home in on the most important factors of resilience.
“We’ve gotten enthusiastic responses from PAs and nurses,” said Craig Katz, MD, an expert in disaster psychiatry at Mount Sinai and a workshop moderator. Physicians have been slower to get on board. “Doctors are a tough nut to crack – it’s largely a culture where they may burn out but don’t want to talk about it. And asking for help is a hard transition for physicians to make.”
How to protect in midst of trauma
In formulating the program’s platform, Mount Sinai experts drew upon their extensive experience aiding 9/11 responders at the World Trade Center (WTC), as well as their system-wide wellness program that aids demoralized and burned-out physicians. While the reach of the pandemic is much broader than 9/11, experts see some commonalities in conditions that emerge after traumatic events, and they also discovered what can help.
“We learned from our WTC experience about what are protective factors – what are the social supports that buffer against depression, anxiety, and PTSD,” said Jonathan DePierro, PhD, clinical director of CSRPG and a psychologist at the Mount Sinai WTC Mental Health Program. “We also learned that people who have more prolonged exposures are at greater risk of developing mental health difficulties.”
The program itself reflects these lessons – and that’s why it’s open to all employees, not just medical professionals. Housekeepers, security staffers, even construction workers are also dealing with their lives being in danger. “That wasn’t in their job description,” said Dr. DePierro. “These people tend to have fewer social and economic resources, make less money and have fewer structural supports, which makes them even more vulnerable.”
Dr. Charney’s strategies on building resilience became a bible of sorts for the workshops, according to Dr. Katz, who authored the training curriculum. Sessions deal with how to build up reservoirs of realistic optimism, keep gratitude journals, find spiritual meaning in their lives, maintain physical wellness and create networks of social support. The workshops are meant to help participants create action plans, to reach out for support in their social networks, and keep the focus on the positives.
The goal is to give demoralized health care workers a renewed sense of competence. “The resilience workshop is a launching point to get people to show up and talk,” said Dr. Katz. “And if we do that, we’ve accomplished a lot just getting people in the door.”
The center will also have a research component to identify what works and what doesn’t so their platform can provide a template for other institutions; Dr. Marin said they’ve gotten inquiries about the program from major hospital systems in Michigan and California. They’ll also conduct longitudinal research to determine what lingering problems persist among healthcare workers over time.
Since the center opened its virtual doors, the curriculum has also been altered in response to feedback from the support staff, many of whom live in the community that surrounds Mount Sinai in northern Manhattan, which is largely lower-income Latinx and Black individuals. Workshop materials have been translated into Spanish and now feature people who reflect a more diverse set of experiences.
“Many of our employees and the population we serve identify as non-White so we’ve been doing outreach with a lot of the local unions,” said Dr. Marin. “Our next step is to take what we’re doing and work with local community organizations.”
A version of this article first appeared on Medscape.com.
The rebirth of psychedelic psychiatry
Mr. P, age 65, has a history of major depressive disorder (MDD), generalized anxiety disorder, and social phobia. Mr. P’s personality is high in neuroticism and he has often responded to new situations with feelings of impending doom. For him, fear, anxious rumination, helplessness, and catastrophizing are familiar mental processes.
When he was in his 30s, Mr. P had a severe major depressive episode with suicidal ideation and sought care from a psychiatrist. He began a treatment program of psychotherapy and concomitant psychopharmacotherapy with consecutive trials of fluoxetine, sertraline, and amitriptyline, each of an adequate dose and duration. With each medication, Mr. P experienced new adverse effects, including nausea, constipation, tremors, and headache. His psychiatrist transitioned him to bupropion, which helped Mr. P most. For the next several decades, Mr. P continued to experience low-grade depressive symptoms with intermittent exacerbation to mild-to-moderate major depressive episodes, but he remained adherent to his medication and continued psychotherapy.
Shortly after his 65th birthday, Mr. P experiences progressively worsening nausea and abdominal pain. Initially, he assumes the symptoms are secondary to anxiety. Taking his psychiatrist’s advice, Mr. P visits his primary care physician. A work-up reveals that Mr. P has advanced pancreatic cancer, and an oncologist estimates Mr. P has 6 months of life remaining.
Following his cancer diagnosis, Mr. P quickly develops symptoms of MDD despite continuing to take bupropion. Within a week he becomes withdrawn and hopeless, and thinks about ending his life “before God does.” His psychiatrist urges Mr. P to contact the local academic medical center because it is conducting a trial of a “new” drug, psilocybin, to treat anxiety and depression in patients with terminal illness.
Beginning in the 1940s, a growing body of scientific evidence suggested that psychedelic compounds such as lysergic acid diethylamide (LSD) could benefit individuals with various psychiatric maladies. Research interest in LSD and substances with similar effects persisted until the late 1960s. In response to the growing counterculture movement in the United States and the efforts of Harvard researchers Timothy Leary and Richard Alpert to popularize psychedelic drug use in the general population, in 1970 President Richard M. Nixon signed the Controlled Substances Act (CSA) into law. The CSA categorized LSD as a Schedule I drug, rendering its manufacture and distribution illegal. Research into the potential therapeutic benefits of LSD was effectively halted.1 In recent decades, however, there has been a quiet but growing renaissance of scientific interest in the effects of psychedelics on a variety of conditions, including terminal illness–related anxiety and depression, treatment-resistant depression, and substance use disorders (SUDs). One example is psilocybin, which is currently undergoing Phase 2 and 3 clinical trials in North America and Europe for treatment-resistant depression.
As researchers have once again picked up the torch in the pursuit of psychedelic therapeutics, jurisdictions in the United States are also relaxing their stance on these drugs. In 2019 and early 2020, Denver, Oakland, and Santa Cruz became the first 3 cities in the United States to decriminalize the possession of various psychedelic substances.2-4 With the passage of Measure 109 in November 2020, Oregon became the first state to decriminalize the use of psychedelic mushrooms in therapeutic settings.5 The combined forces of increased research and relaxed political concern related to psychedelics might make it possible for the FDA to approve their use for psychiatric conditions. Therefore, it is critical for psychiatrists to understand the psychopharmacology, range of effects, and potential risks and benefits of these agents. In this article, I describe what psychedelics are and how they work, summarize a few research findings about psilocybin, and offer a framework for psychedelic psychiatric practice in the years to come.
What are psychedelics?
Psychiatrist Humphry Osmond first coined the term “psychedelic” in 1957 at a meeting of the New York Academy of Sciences, where he was discussing his research on the effect of LSD on patients at the Weyburn Mental Hospital in Saskatchewan, Canada.6 Prior to 1957, LSD had been described as a “psychotomimetic” drug because it was believed to induce a state of psychosis similar to that experienced in schizophrenia. But LSD does not generally induce frank auditory hallucinations or clearly defined delusional beliefs. Osmond’s new term—derived from the Greek words psyche, meaning “mind,” and delos, meaning “to show”—referred to the “mind-manifesting” capacities of LSD and related drugs.6 Psychedelic drugs can cause an array of changes to an individual’s conscious experience, from relatively mild changes in visual perception to profound derangements in sense of self and reality.
Continue to: Before describing the effects...
Classic psychedelics vs other compounds
Before describing the effects of psychedelic drugs and how they may relate to their therapeutic potential, it is useful to define which compounds are considered “classic psychedelics.”
The classic psychedelics are substances that operate primarily through activation of the serotonin 5-hydroxytryptamine receptor 2A receptor (5-HT2A) (Table 17). Many psychedelic drugs are derived from natural sources, including plants, fungi, and animals. For example, N, N-dimethyltryptamine (DMT), which is one of the most potent psychedelic compounds, is found in various plant species and can be imbibed in a tea known as ayahuasca, most commonly in the context of spiritual ceremonies.
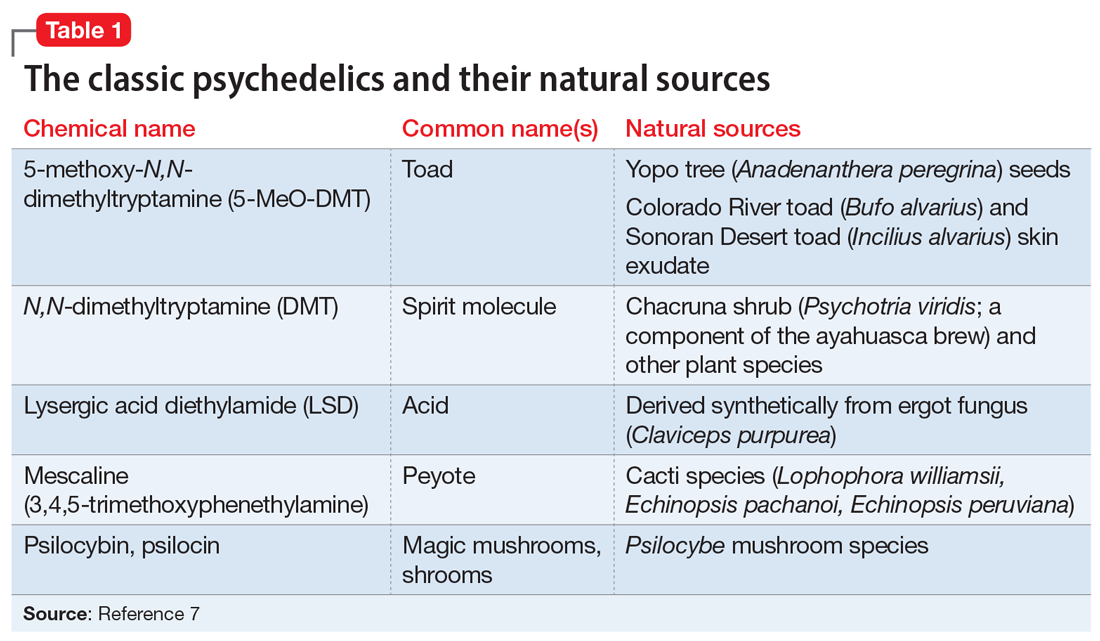
Other compounds. Some researchers continue to classify other compounds as “psychedelics,” although the mechanisms of action and effects of these compounds may vary greatly from those of the classic psychedelics. These include the dissociative anesthetics ketamine and phencyclidine (PCP), which exert their effects via N-methyl-
The DSM-58 does not differentiate between classic psychedelics and related compounds. In its chapter on Substance-Related and Addictive Disorders, the section Hallucinogen-Related Disorders provides criteria for the diagnoses of phencyclidine use disorder and other hallucinogen use disorder. Researchers generally have abandoned the term “hallucinogen” because psychedelics typically do not induce frank hallucinations. Furthermore, lumping psychedelics and compounds such as MDMA and ketamine into the category of “other hallucinogen” fails to address important distinctions between them, including diagnostically relevant issues. For example, psychedelics do not cause symptoms of physiologic dependence such as craving or a withdrawal syndrome, whereas MDMA can.9 The DSM-5 also contains a diagnosis called hallucinogen persisting perception disorder (HPPD), referring to residual distortions of visual perception that remain following psychedelic intoxication. Although the text notes the estimated prevalence of HPPD in individuals who use psychedelics is 4.2%, the condition is thought to occur infrequently in both therapeutic and recreational users.10
How psychedelics work
Psychedelics can induce a spectrum of effects that are not necessarily dose-dependent. Mild effects of intoxication include altered sensory perception in visual, auditory, proprioceptive, and somatosensory spheres, including synesthesia. Progressively more severe changes include a distorted or eliminated perception or awareness of space, time, body, and self, resulting in derealization and depersonalization. Some of the most extreme alterations of consciousness reported by users include mystical or transcendent experiences of birth, giving birth, death, exchanging bodies with a nonhuman species, and meeting otherworldly beings.11 In terms of neurophysiology, psychedelics cause altered cerebral blood flow and metabolism, increased connectivity between brain regions that do not typically communicate, and a reduction in the activity of a group of cortical structures called the default mode network (DMN).12
Continue to: Researchers hypothesize that...
Researchers hypothesize that the disruption of DMN activity may be a key mechanism accounting for psychedelics’ therapeutic effects in mental illness. The DMN is a group of structures that includes the posterior cingulate cortex, the medial prefrontal cortex, the angular gyrus, and other cortical areas that are active when an individual is not engaged in a particular mental task (for example, during mind wandering). It is thought to underlie introspection and to serve as an “orchestrator” of global brain function.13 Theoretically, then, by temporarily disrupting the neural circuits responsible for maintaining ingrained, negative thought and behavioral patterns, as observed in patients with depression or SUDs, psychedelics can help patients develop greater emotional and cognitive flexibility and identify new ways to view the world and to solve problems.
Evaluating psychedelics as therapeutic agents
The renaissance of research into psychedelics as therapeutic agents during the last 2 decades has produced some promising preliminary findings. In 2020, the American Psychiatric Association’s Work Group on Biomarkers and Novel Treatments published a review of the best evidence on the topic.14 Psilocybin is the most studied drug because compared with LSD, it carries less of a stigma and has a shorter duration of action. Psilocybin has been studied as a potential treatment for several psychiatric disorders, including terminal illness–related depression and anxiety, and SUDs.
Griffiths et al.15 In a double-blind randomized crossover study at Johns Hopkins School of Medicine, Griffiths et al15 administered a high dose (22 or 30 mg/70 kg) and a very low, placebo-like dose (1 or 3 mg/70 kg) of psilocybin at 2 separate sessions to 51 patients with terminal cancer and associated depressive and anxiety disorders. After 5 weeks, the participants assigned to one condition crossed over to the other condition. High-dose psilocybin had a significant effect on depression and anxiety symptoms within 5 weeks that persisted over 6 months of follow-up. At 6 months, 78% of participants experienced a response in depressive symptoms (≥50% decrease in GRID-Hamilton Depression Rating Scale [HAM-D-17] baseline scores) and 65% remitted (GRID-HAM-D-17 score ≤7). At 6 months, 83% of participants had a response in anxiety symptoms (≥50% decrease in Hamilton Rating Scale for Anxiety [HAM-A] baseline scores) and 57% remitted (HAM-A ≤7).
Johnson et al.16,17 In an open-label pilot study16 and ≥12-month follow-up study,17 Johnson et al administered a moderate (20 mg/70 kg) and high (30 mg/70 kg) dose of psilocybin to 15 participants enrolled in a 15-week smoking session program. The psilocybin sessions were scheduled at Weeks 5 and 7, with an optional psilocybin session at Week 13. The sessions included nondirective support from program staff, but not smoking cessation content. Relying on laboratory-verified exhaled carbon monoxide and urine cotinine measures, researchers found an 80% abstinence rate at 6 months, a 67% abstinence rate at 12 months, and a 75% abstinence rate at 2.5 years.16,17
Bogenschutz et al18 conducted a study of 10 patients who met DSM-IV criteria for alcohol dependence and had at least 2 heavy drinking days in the previous 30 days. They found that a 14-session treatment program that included 2 psilocybin-assisted psychotherapy sessions with dosages of 0.4 mg/kg resulted in a significant increase in self-reported alcohol abstinence at 4 weeks that persisted for 36 weeks.18
Although these studies were small, open-label, and had other methodologic flaws, their pilot work has led to larger-scale projects assessing psilocybin’s therapeutic potential. Psilocybin has also been studied for treatment-resistant depression and obsessive-compulsive disorder. Other clinical trials underway are investigating psilocybin for the treatment of cocaine and opioid use disorder, anorexia nervosa, and depression in Alzheimer’s disease.14 Although psilocybin is currently the best-studied psychedelic, there is some research demonstrating that LSD can also induce a persistent reduction in anxiety symptoms associated with terminal illness19 and that ayahuasca causes a rapid reduction in depressive symptoms that persists over 21 days.20
Continue to: The future of psychedelic psychiatry...
The future of psychedelic psychiatry
If psychedelic compounds become approved for the treatment of psychiatric conditions, psychiatrists will likely be responsible for prescribing them and managing patients who receive them.21Table 211,21-24 summarizes practical considerations for psychiatrists who may someday be prescribing psychedelic drugs. Areas of psychedelic treatment in which psychiatric expertise is necessary include:
- screening for patients at increased risk for a challenging or adverse experience or “bad trip”
- conducting a thorough informed consent process in which the risks are discussed and the patient’s wishes regarding potential situations are elicited
- managing acute medical and psychiatric complications, including agitation and violent behavior
- ensuring the use of trained guides during sessions.
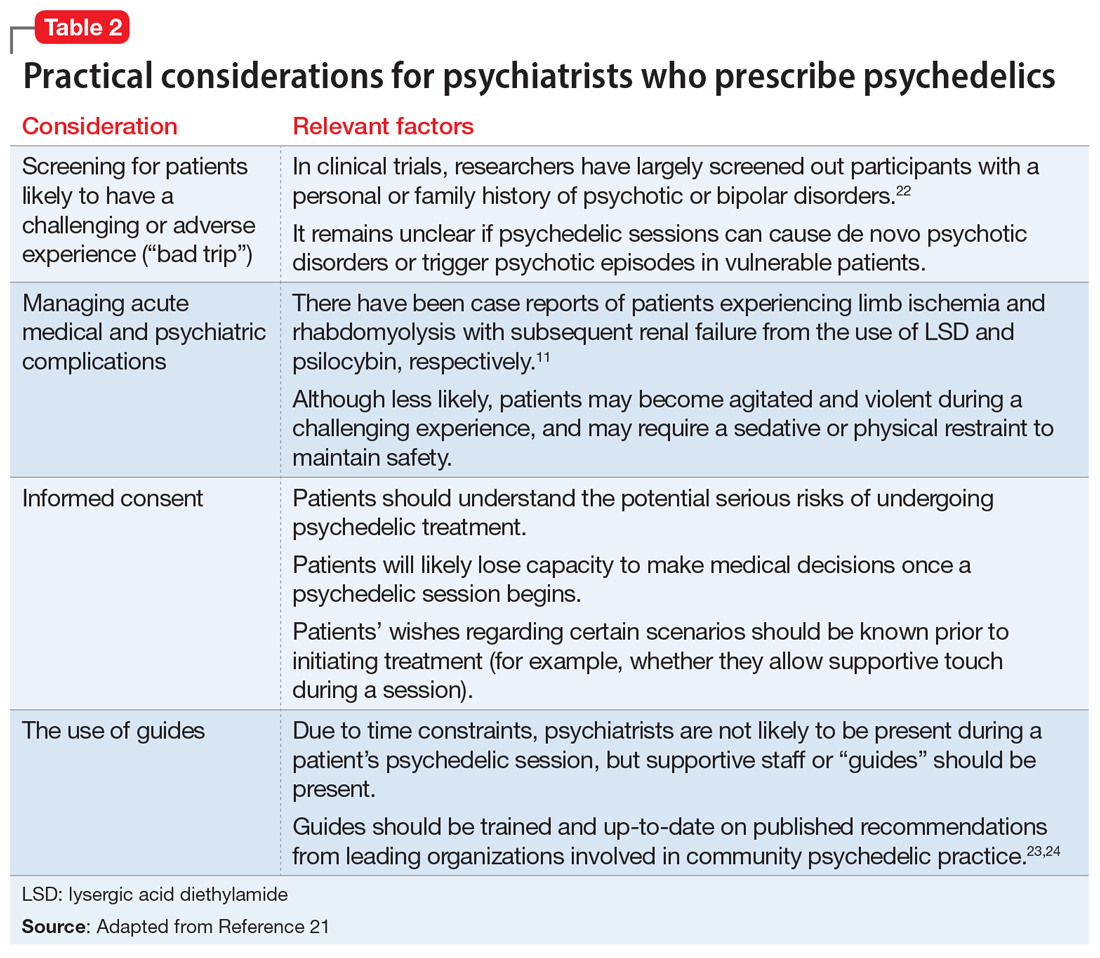
Psychiatrists who are interested in providing psychedelic-assisted therapy should understand the concept of “set and setting,” which was defined by Timothy Leary in the 1960s and is thought to play an important role in determining the types of experiences that arise during a psychedelic session.25 “Set” refers to an individual’s mindset going into a session, and “setting” refers to the environment in which the session occurs. Typical elements of each are summarized in Table 3.7 Psychiatrists will play a critical role in assessing and preparing the “set” by screening patients appropriately, assessing patient goals, and providing a thorough informed consent procedure. Psychiatrists should also be mindful of the “setting,” providing a comfortable, safe, familiar environment and access to appropriate music and eyeshades, if desired. Due to time restraints, psychiatrists are not likely to be responsible for guiding patients through sessions, and should educate themselves about ethical practices of psychedelic guides,if they are in the position to hire guides.23,24
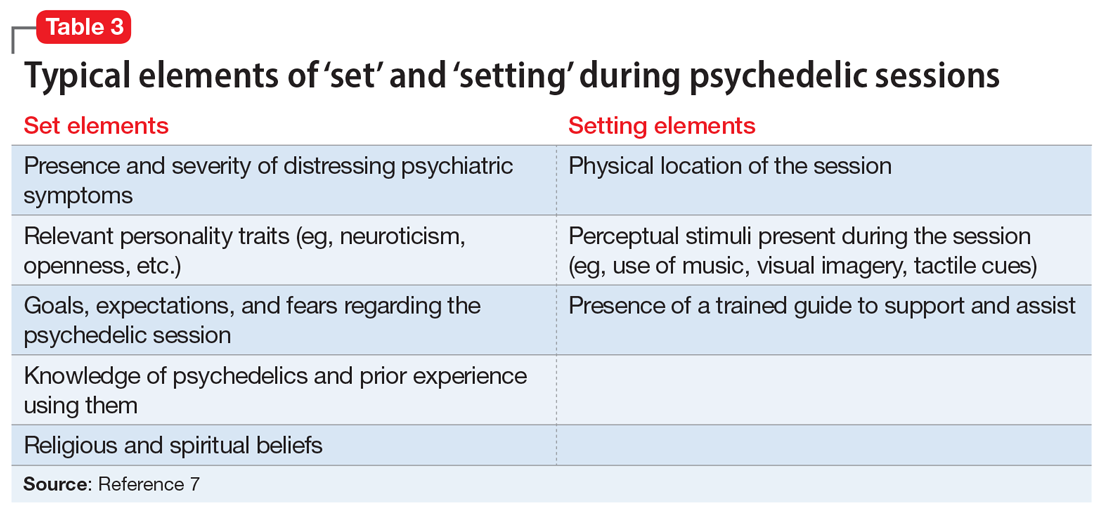
Psychiatrists may also play a role in providing psychotherapy to patients receiving treatment with psychedelics. These substances can induce both transcendent and terrifying experiences. Patients therefore require “integration” therapy sessions to assist with processing the content of their psychedelic treatment and incorporating the experiences into day-to-day life. In an online survey of nearly 2,000 individuals who used psilocybin recreationally, 7.6% reported that they had to seek treatment for enduring psychological symptoms that they attributed to their psilocybin use, including persistent anxiety, fear, paranoia, and depression.26 Integrative psychotherapy sessions may help reduce the risk of persistent negative effects from therapeutic psychedelics, as well as enhance their beneficial effects.
CASE CONTINUED
Mr. P is enrolled in the academic medical center study assessing the effect of psilocybin on terminal illness-related anxiety and depression. During a 5-hour, 30-mg psilocybin session, he initially experiences distorted visual cues, with vivid, colorful geometric patterns collapsing into each other. He then loses the concepts and experience of time, space, and his body, as his visual distortions convert to darkness. After what seems like a decade within the darkness, he sees himself lying in a hospital bed with loved ones surrounding him. He watches himself take his last breaths and his family members weep as he dies. As he regains his senses, Mr. P feels that he is being reborn.
In the therapy sessions that follow the psychedelic session, Mr. P reports feeling “finally freed” from the fear, sadness, and anger that he has felt throughout his life. He comes to accept his impending death with gratitude and peace. In his final days, he no longer experiences depression or anxiety. Mr. P’s friends and family members comment that he seems to be the best version of himself in the months that lead up to his death.
Related Resources
• Nutt D. Psychedelic drugs-a new era in psychiatry? Dialogues Clin Neurosci. 2019;21(2):139-147.
• Garcia-Romeu A, Kersgaard B, Addy PH. Clinical applications of hallucinogens: a review. Exp Clin Psychopharmacol. 2016; 24(4):229-268.
Drug Brand Names
Amitriptyline • Amitril, Elavil
Bupropion • Wellbutrin
Fluoxetine • Prozac
Sertraline • Zoloft
Bottom Line
Psychedelics are a class of consciousness-altering agents that have become a potentially promising source of new treatments for psychiatric illness. Although more evidence is needed, compounds such as psilocybin may one day become FDAapproved for conditions such as terminal illness–related depression and anxiety, and substance use disorders. When this occurs, psychiatrists should be responsible for prescribing psychedelics and managing patients who receive treatment.
1. Smith DE, Raswyck GE, Davidson LD. From Hofmann to the Haight Ashbury, and into the future: the past and potential of lysergic acid diethylamide. J Psychoactive Drugs. 2014;46(1):3-10.
2. Siegel M. Threading Denver’s magic mushrooms needle: promising as medicine, risky as recreation. USA Today. Published May 13, 2019. Accessed December 4, 2020. https://www.usatoday.com/story/opinion/2019/05/13/denver-magic-mushrooms-promising-medicine-reckless-recreation-column/1182543001
3. Epstein, K. Oakland decriminalizes ‘magic mushrooms’ and other natural psychedelics. The Washington Post. Published June 5, 2019. Accessed December 4, 2020. https://www.washingtonpost.com/nation/2019/06/05/oakland-decriminalizes-magic-mushrooms-other-natural-psychedelics
4. York JA. Santa Cruz decriminalizes natural psychedelics. Santa Cruz Sentinel. Published January 30, 2020. Accessed December 4, 2020. https://www.santacruzsentinel.com/2020/01/29/santa-cruz-decriminalizes-natural-psychedelics
5. Acker L. Oregon becomes first state to legalize psychedelic mushrooms. The Oregonian/Oregon Live. Published November 4, 2020. Accessed December 4, 2020. https://www.oregonlive.com/politics/2020/11/oregon-becomes-first-state-to-legalize-psychedelic-mushrooms.html
6. Dyck E. Flashback: psychiatric experimentation with LSD in historical perspective. Can J Psychiatry. 2005;50(7):381-388.
7. Holoyda BJ. The psychedelic renaissance and its forensic implications. J Am Acad Psychiatry Law. 2020;48(1):87-97.
8. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
9. Davis AK, Rosenberg H. The prevalence, intensity, and assessment of craving for MDMA/ecstasy in recreational users. J Psychoactive Drugs. 2014;46(2):154-151.
10. Halpern JH, Lerner AG, Passie T. A review of hallucinogen persisting perception disorder (HPPD) and an exploratory study of subjects claiming symptoms of HPPD. Curr Top Behav Neurosci. 2018;36:333-360.
11. Nichols DE. Psychedelics. Pharmacol Rev. 2016;68(2):264-355.
12. Nichols DE. Hallucinogens. Pharmacol Ther. 2004;101(2):131-181.
13. Carhart-Harris RL, Leech R, Hellyer PJ, et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci. 2014;8:20.
14. Reiff CM, Richman EE, Nemeroff CB, et al. Psychedelics and psychedelic-assisted psychotherapy. Am J Psychiatry. 2020;177(5):391-410.
15. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197.
16. Johnson MW, Garcia-Romeu A, Cosimano MP, et al. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J Psychopharmacol. 2014;28(11):983-992.
17. Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43(1):55-60.
18. Bogenschutz MP, Forcehimes AA, Pommy JA, et al. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. J Psychopharmacol. 2015;29(3):1182-1190.
19. Gasser P, Holstein D, Michel Y, et al. Safety and efficacy of lysergic acid diethylamide-assisted psychotherapy for anxiety associated with life-threatening diseases. J Nerv Ment Dis. 2014;202(7):531-520.
20. Osório F de L, Sanches RF, Macedo LR, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a preliminary report. Braz J Psychiatry. 2015;37(1):13-20.
21. Holoyda B. Psychedelic psychiatry: preparing for novel treatments involving altered states of consciousness. Psych Serv. 2020;71(12):1297-1299.
22. Johnson MW, Richards W, Griffiths RR. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008;22(6):603-620.
23. Council on Spiritual Practices. Code of ethics for spiritual Guides. Published August 10, 2001. Accessed November 25, 2020. https://csp.org/docs/code-of-ethics-for-spiritual-guides
24. Multidisciplinary Association for Psychedelic Studies. Zendo psychedelic harm reduction training manual. Published 2017. Accessed November 25, 2020. https://zendoproject.org/wp-content/uploads/2017/06/Zendo-Manual-2017.pdf
25. Zinberg NE. Drug, set, and setting: the basis for controlled intoxicant use. Yale University Press; 1984.
26. Carbonaro TM, Bradstreet MP, Barrett FS, et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: acute and enduring positive and negative consequences. J Psychopharmacol. 2016;30(12):1268-1278.
Mr. P, age 65, has a history of major depressive disorder (MDD), generalized anxiety disorder, and social phobia. Mr. P’s personality is high in neuroticism and he has often responded to new situations with feelings of impending doom. For him, fear, anxious rumination, helplessness, and catastrophizing are familiar mental processes.
When he was in his 30s, Mr. P had a severe major depressive episode with suicidal ideation and sought care from a psychiatrist. He began a treatment program of psychotherapy and concomitant psychopharmacotherapy with consecutive trials of fluoxetine, sertraline, and amitriptyline, each of an adequate dose and duration. With each medication, Mr. P experienced new adverse effects, including nausea, constipation, tremors, and headache. His psychiatrist transitioned him to bupropion, which helped Mr. P most. For the next several decades, Mr. P continued to experience low-grade depressive symptoms with intermittent exacerbation to mild-to-moderate major depressive episodes, but he remained adherent to his medication and continued psychotherapy.
Shortly after his 65th birthday, Mr. P experiences progressively worsening nausea and abdominal pain. Initially, he assumes the symptoms are secondary to anxiety. Taking his psychiatrist’s advice, Mr. P visits his primary care physician. A work-up reveals that Mr. P has advanced pancreatic cancer, and an oncologist estimates Mr. P has 6 months of life remaining.
Following his cancer diagnosis, Mr. P quickly develops symptoms of MDD despite continuing to take bupropion. Within a week he becomes withdrawn and hopeless, and thinks about ending his life “before God does.” His psychiatrist urges Mr. P to contact the local academic medical center because it is conducting a trial of a “new” drug, psilocybin, to treat anxiety and depression in patients with terminal illness.
Beginning in the 1940s, a growing body of scientific evidence suggested that psychedelic compounds such as lysergic acid diethylamide (LSD) could benefit individuals with various psychiatric maladies. Research interest in LSD and substances with similar effects persisted until the late 1960s. In response to the growing counterculture movement in the United States and the efforts of Harvard researchers Timothy Leary and Richard Alpert to popularize psychedelic drug use in the general population, in 1970 President Richard M. Nixon signed the Controlled Substances Act (CSA) into law. The CSA categorized LSD as a Schedule I drug, rendering its manufacture and distribution illegal. Research into the potential therapeutic benefits of LSD was effectively halted.1 In recent decades, however, there has been a quiet but growing renaissance of scientific interest in the effects of psychedelics on a variety of conditions, including terminal illness–related anxiety and depression, treatment-resistant depression, and substance use disorders (SUDs). One example is psilocybin, which is currently undergoing Phase 2 and 3 clinical trials in North America and Europe for treatment-resistant depression.
As researchers have once again picked up the torch in the pursuit of psychedelic therapeutics, jurisdictions in the United States are also relaxing their stance on these drugs. In 2019 and early 2020, Denver, Oakland, and Santa Cruz became the first 3 cities in the United States to decriminalize the possession of various psychedelic substances.2-4 With the passage of Measure 109 in November 2020, Oregon became the first state to decriminalize the use of psychedelic mushrooms in therapeutic settings.5 The combined forces of increased research and relaxed political concern related to psychedelics might make it possible for the FDA to approve their use for psychiatric conditions. Therefore, it is critical for psychiatrists to understand the psychopharmacology, range of effects, and potential risks and benefits of these agents. In this article, I describe what psychedelics are and how they work, summarize a few research findings about psilocybin, and offer a framework for psychedelic psychiatric practice in the years to come.
What are psychedelics?
Psychiatrist Humphry Osmond first coined the term “psychedelic” in 1957 at a meeting of the New York Academy of Sciences, where he was discussing his research on the effect of LSD on patients at the Weyburn Mental Hospital in Saskatchewan, Canada.6 Prior to 1957, LSD had been described as a “psychotomimetic” drug because it was believed to induce a state of psychosis similar to that experienced in schizophrenia. But LSD does not generally induce frank auditory hallucinations or clearly defined delusional beliefs. Osmond’s new term—derived from the Greek words psyche, meaning “mind,” and delos, meaning “to show”—referred to the “mind-manifesting” capacities of LSD and related drugs.6 Psychedelic drugs can cause an array of changes to an individual’s conscious experience, from relatively mild changes in visual perception to profound derangements in sense of self and reality.
Continue to: Before describing the effects...
Classic psychedelics vs other compounds
Before describing the effects of psychedelic drugs and how they may relate to their therapeutic potential, it is useful to define which compounds are considered “classic psychedelics.”
The classic psychedelics are substances that operate primarily through activation of the serotonin 5-hydroxytryptamine receptor 2A receptor (5-HT2A) (Table 17). Many psychedelic drugs are derived from natural sources, including plants, fungi, and animals. For example, N, N-dimethyltryptamine (DMT), which is one of the most potent psychedelic compounds, is found in various plant species and can be imbibed in a tea known as ayahuasca, most commonly in the context of spiritual ceremonies.
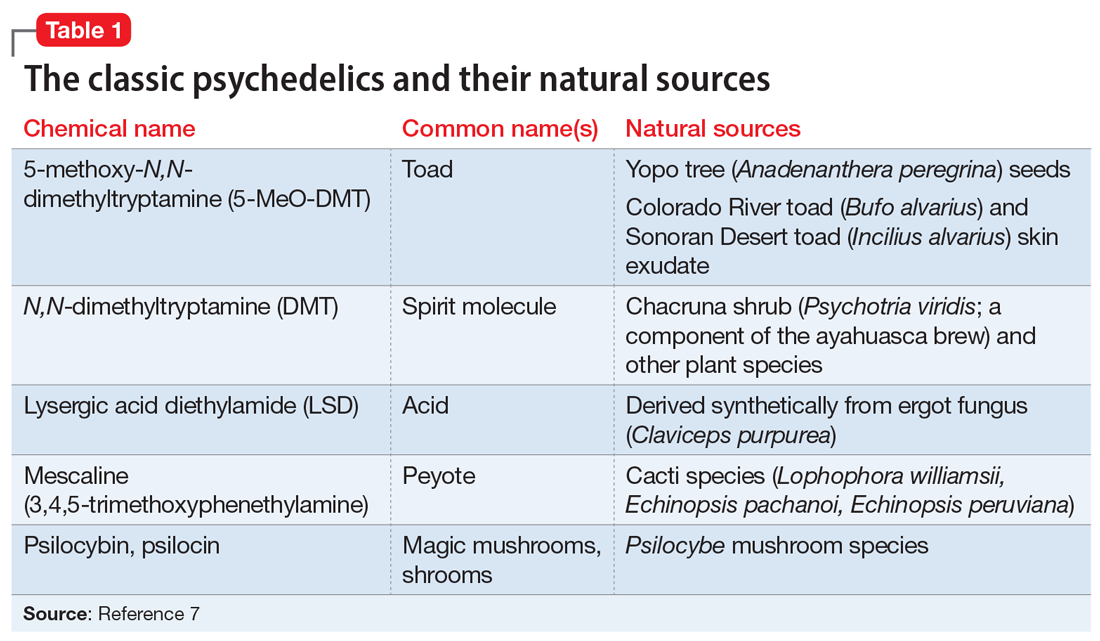
Other compounds. Some researchers continue to classify other compounds as “psychedelics,” although the mechanisms of action and effects of these compounds may vary greatly from those of the classic psychedelics. These include the dissociative anesthetics ketamine and phencyclidine (PCP), which exert their effects via N-methyl-
The DSM-58 does not differentiate between classic psychedelics and related compounds. In its chapter on Substance-Related and Addictive Disorders, the section Hallucinogen-Related Disorders provides criteria for the diagnoses of phencyclidine use disorder and other hallucinogen use disorder. Researchers generally have abandoned the term “hallucinogen” because psychedelics typically do not induce frank hallucinations. Furthermore, lumping psychedelics and compounds such as MDMA and ketamine into the category of “other hallucinogen” fails to address important distinctions between them, including diagnostically relevant issues. For example, psychedelics do not cause symptoms of physiologic dependence such as craving or a withdrawal syndrome, whereas MDMA can.9 The DSM-5 also contains a diagnosis called hallucinogen persisting perception disorder (HPPD), referring to residual distortions of visual perception that remain following psychedelic intoxication. Although the text notes the estimated prevalence of HPPD in individuals who use psychedelics is 4.2%, the condition is thought to occur infrequently in both therapeutic and recreational users.10
How psychedelics work
Psychedelics can induce a spectrum of effects that are not necessarily dose-dependent. Mild effects of intoxication include altered sensory perception in visual, auditory, proprioceptive, and somatosensory spheres, including synesthesia. Progressively more severe changes include a distorted or eliminated perception or awareness of space, time, body, and self, resulting in derealization and depersonalization. Some of the most extreme alterations of consciousness reported by users include mystical or transcendent experiences of birth, giving birth, death, exchanging bodies with a nonhuman species, and meeting otherworldly beings.11 In terms of neurophysiology, psychedelics cause altered cerebral blood flow and metabolism, increased connectivity between brain regions that do not typically communicate, and a reduction in the activity of a group of cortical structures called the default mode network (DMN).12
Continue to: Researchers hypothesize that...
Researchers hypothesize that the disruption of DMN activity may be a key mechanism accounting for psychedelics’ therapeutic effects in mental illness. The DMN is a group of structures that includes the posterior cingulate cortex, the medial prefrontal cortex, the angular gyrus, and other cortical areas that are active when an individual is not engaged in a particular mental task (for example, during mind wandering). It is thought to underlie introspection and to serve as an “orchestrator” of global brain function.13 Theoretically, then, by temporarily disrupting the neural circuits responsible for maintaining ingrained, negative thought and behavioral patterns, as observed in patients with depression or SUDs, psychedelics can help patients develop greater emotional and cognitive flexibility and identify new ways to view the world and to solve problems.
Evaluating psychedelics as therapeutic agents
The renaissance of research into psychedelics as therapeutic agents during the last 2 decades has produced some promising preliminary findings. In 2020, the American Psychiatric Association’s Work Group on Biomarkers and Novel Treatments published a review of the best evidence on the topic.14 Psilocybin is the most studied drug because compared with LSD, it carries less of a stigma and has a shorter duration of action. Psilocybin has been studied as a potential treatment for several psychiatric disorders, including terminal illness–related depression and anxiety, and SUDs.
Griffiths et al.15 In a double-blind randomized crossover study at Johns Hopkins School of Medicine, Griffiths et al15 administered a high dose (22 or 30 mg/70 kg) and a very low, placebo-like dose (1 or 3 mg/70 kg) of psilocybin at 2 separate sessions to 51 patients with terminal cancer and associated depressive and anxiety disorders. After 5 weeks, the participants assigned to one condition crossed over to the other condition. High-dose psilocybin had a significant effect on depression and anxiety symptoms within 5 weeks that persisted over 6 months of follow-up. At 6 months, 78% of participants experienced a response in depressive symptoms (≥50% decrease in GRID-Hamilton Depression Rating Scale [HAM-D-17] baseline scores) and 65% remitted (GRID-HAM-D-17 score ≤7). At 6 months, 83% of participants had a response in anxiety symptoms (≥50% decrease in Hamilton Rating Scale for Anxiety [HAM-A] baseline scores) and 57% remitted (HAM-A ≤7).
Johnson et al.16,17 In an open-label pilot study16 and ≥12-month follow-up study,17 Johnson et al administered a moderate (20 mg/70 kg) and high (30 mg/70 kg) dose of psilocybin to 15 participants enrolled in a 15-week smoking session program. The psilocybin sessions were scheduled at Weeks 5 and 7, with an optional psilocybin session at Week 13. The sessions included nondirective support from program staff, but not smoking cessation content. Relying on laboratory-verified exhaled carbon monoxide and urine cotinine measures, researchers found an 80% abstinence rate at 6 months, a 67% abstinence rate at 12 months, and a 75% abstinence rate at 2.5 years.16,17
Bogenschutz et al18 conducted a study of 10 patients who met DSM-IV criteria for alcohol dependence and had at least 2 heavy drinking days in the previous 30 days. They found that a 14-session treatment program that included 2 psilocybin-assisted psychotherapy sessions with dosages of 0.4 mg/kg resulted in a significant increase in self-reported alcohol abstinence at 4 weeks that persisted for 36 weeks.18
Although these studies were small, open-label, and had other methodologic flaws, their pilot work has led to larger-scale projects assessing psilocybin’s therapeutic potential. Psilocybin has also been studied for treatment-resistant depression and obsessive-compulsive disorder. Other clinical trials underway are investigating psilocybin for the treatment of cocaine and opioid use disorder, anorexia nervosa, and depression in Alzheimer’s disease.14 Although psilocybin is currently the best-studied psychedelic, there is some research demonstrating that LSD can also induce a persistent reduction in anxiety symptoms associated with terminal illness19 and that ayahuasca causes a rapid reduction in depressive symptoms that persists over 21 days.20
Continue to: The future of psychedelic psychiatry...
The future of psychedelic psychiatry
If psychedelic compounds become approved for the treatment of psychiatric conditions, psychiatrists will likely be responsible for prescribing them and managing patients who receive them.21Table 211,21-24 summarizes practical considerations for psychiatrists who may someday be prescribing psychedelic drugs. Areas of psychedelic treatment in which psychiatric expertise is necessary include:
- screening for patients at increased risk for a challenging or adverse experience or “bad trip”
- conducting a thorough informed consent process in which the risks are discussed and the patient’s wishes regarding potential situations are elicited
- managing acute medical and psychiatric complications, including agitation and violent behavior
- ensuring the use of trained guides during sessions.
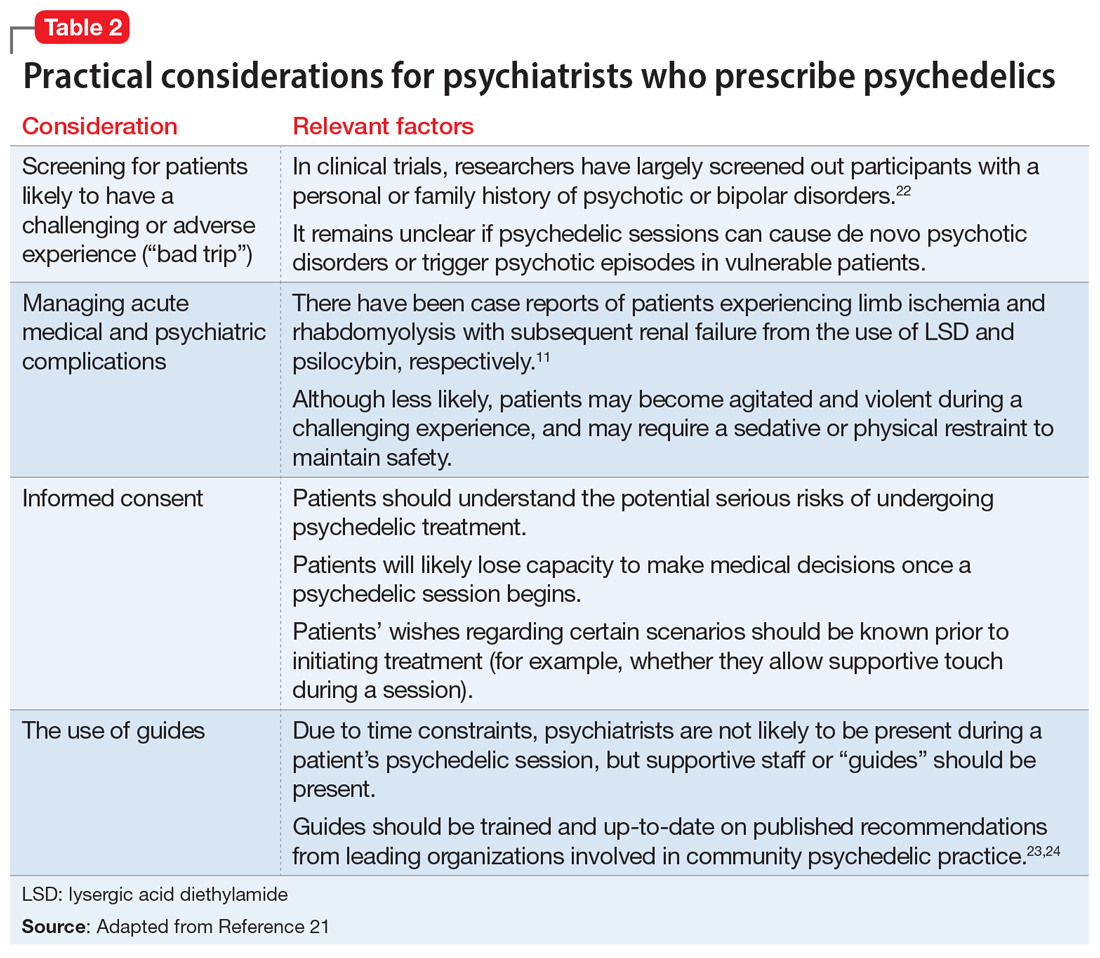
Psychiatrists who are interested in providing psychedelic-assisted therapy should understand the concept of “set and setting,” which was defined by Timothy Leary in the 1960s and is thought to play an important role in determining the types of experiences that arise during a psychedelic session.25 “Set” refers to an individual’s mindset going into a session, and “setting” refers to the environment in which the session occurs. Typical elements of each are summarized in Table 3.7 Psychiatrists will play a critical role in assessing and preparing the “set” by screening patients appropriately, assessing patient goals, and providing a thorough informed consent procedure. Psychiatrists should also be mindful of the “setting,” providing a comfortable, safe, familiar environment and access to appropriate music and eyeshades, if desired. Due to time restraints, psychiatrists are not likely to be responsible for guiding patients through sessions, and should educate themselves about ethical practices of psychedelic guides,if they are in the position to hire guides.23,24
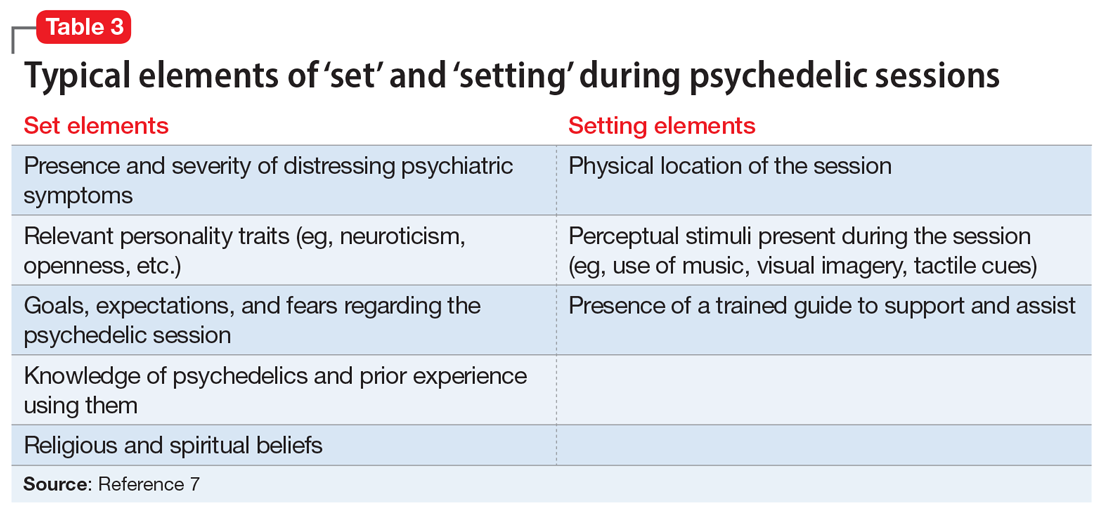
Psychiatrists may also play a role in providing psychotherapy to patients receiving treatment with psychedelics. These substances can induce both transcendent and terrifying experiences. Patients therefore require “integration” therapy sessions to assist with processing the content of their psychedelic treatment and incorporating the experiences into day-to-day life. In an online survey of nearly 2,000 individuals who used psilocybin recreationally, 7.6% reported that they had to seek treatment for enduring psychological symptoms that they attributed to their psilocybin use, including persistent anxiety, fear, paranoia, and depression.26 Integrative psychotherapy sessions may help reduce the risk of persistent negative effects from therapeutic psychedelics, as well as enhance their beneficial effects.
CASE CONTINUED
Mr. P is enrolled in the academic medical center study assessing the effect of psilocybin on terminal illness-related anxiety and depression. During a 5-hour, 30-mg psilocybin session, he initially experiences distorted visual cues, with vivid, colorful geometric patterns collapsing into each other. He then loses the concepts and experience of time, space, and his body, as his visual distortions convert to darkness. After what seems like a decade within the darkness, he sees himself lying in a hospital bed with loved ones surrounding him. He watches himself take his last breaths and his family members weep as he dies. As he regains his senses, Mr. P feels that he is being reborn.
In the therapy sessions that follow the psychedelic session, Mr. P reports feeling “finally freed” from the fear, sadness, and anger that he has felt throughout his life. He comes to accept his impending death with gratitude and peace. In his final days, he no longer experiences depression or anxiety. Mr. P’s friends and family members comment that he seems to be the best version of himself in the months that lead up to his death.
Related Resources
• Nutt D. Psychedelic drugs-a new era in psychiatry? Dialogues Clin Neurosci. 2019;21(2):139-147.
• Garcia-Romeu A, Kersgaard B, Addy PH. Clinical applications of hallucinogens: a review. Exp Clin Psychopharmacol. 2016; 24(4):229-268.
Drug Brand Names
Amitriptyline • Amitril, Elavil
Bupropion • Wellbutrin
Fluoxetine • Prozac
Sertraline • Zoloft
Bottom Line
Psychedelics are a class of consciousness-altering agents that have become a potentially promising source of new treatments for psychiatric illness. Although more evidence is needed, compounds such as psilocybin may one day become FDAapproved for conditions such as terminal illness–related depression and anxiety, and substance use disorders. When this occurs, psychiatrists should be responsible for prescribing psychedelics and managing patients who receive treatment.
Mr. P, age 65, has a history of major depressive disorder (MDD), generalized anxiety disorder, and social phobia. Mr. P’s personality is high in neuroticism and he has often responded to new situations with feelings of impending doom. For him, fear, anxious rumination, helplessness, and catastrophizing are familiar mental processes.
When he was in his 30s, Mr. P had a severe major depressive episode with suicidal ideation and sought care from a psychiatrist. He began a treatment program of psychotherapy and concomitant psychopharmacotherapy with consecutive trials of fluoxetine, sertraline, and amitriptyline, each of an adequate dose and duration. With each medication, Mr. P experienced new adverse effects, including nausea, constipation, tremors, and headache. His psychiatrist transitioned him to bupropion, which helped Mr. P most. For the next several decades, Mr. P continued to experience low-grade depressive symptoms with intermittent exacerbation to mild-to-moderate major depressive episodes, but he remained adherent to his medication and continued psychotherapy.
Shortly after his 65th birthday, Mr. P experiences progressively worsening nausea and abdominal pain. Initially, he assumes the symptoms are secondary to anxiety. Taking his psychiatrist’s advice, Mr. P visits his primary care physician. A work-up reveals that Mr. P has advanced pancreatic cancer, and an oncologist estimates Mr. P has 6 months of life remaining.
Following his cancer diagnosis, Mr. P quickly develops symptoms of MDD despite continuing to take bupropion. Within a week he becomes withdrawn and hopeless, and thinks about ending his life “before God does.” His psychiatrist urges Mr. P to contact the local academic medical center because it is conducting a trial of a “new” drug, psilocybin, to treat anxiety and depression in patients with terminal illness.
Beginning in the 1940s, a growing body of scientific evidence suggested that psychedelic compounds such as lysergic acid diethylamide (LSD) could benefit individuals with various psychiatric maladies. Research interest in LSD and substances with similar effects persisted until the late 1960s. In response to the growing counterculture movement in the United States and the efforts of Harvard researchers Timothy Leary and Richard Alpert to popularize psychedelic drug use in the general population, in 1970 President Richard M. Nixon signed the Controlled Substances Act (CSA) into law. The CSA categorized LSD as a Schedule I drug, rendering its manufacture and distribution illegal. Research into the potential therapeutic benefits of LSD was effectively halted.1 In recent decades, however, there has been a quiet but growing renaissance of scientific interest in the effects of psychedelics on a variety of conditions, including terminal illness–related anxiety and depression, treatment-resistant depression, and substance use disorders (SUDs). One example is psilocybin, which is currently undergoing Phase 2 and 3 clinical trials in North America and Europe for treatment-resistant depression.
As researchers have once again picked up the torch in the pursuit of psychedelic therapeutics, jurisdictions in the United States are also relaxing their stance on these drugs. In 2019 and early 2020, Denver, Oakland, and Santa Cruz became the first 3 cities in the United States to decriminalize the possession of various psychedelic substances.2-4 With the passage of Measure 109 in November 2020, Oregon became the first state to decriminalize the use of psychedelic mushrooms in therapeutic settings.5 The combined forces of increased research and relaxed political concern related to psychedelics might make it possible for the FDA to approve their use for psychiatric conditions. Therefore, it is critical for psychiatrists to understand the psychopharmacology, range of effects, and potential risks and benefits of these agents. In this article, I describe what psychedelics are and how they work, summarize a few research findings about psilocybin, and offer a framework for psychedelic psychiatric practice in the years to come.
What are psychedelics?
Psychiatrist Humphry Osmond first coined the term “psychedelic” in 1957 at a meeting of the New York Academy of Sciences, where he was discussing his research on the effect of LSD on patients at the Weyburn Mental Hospital in Saskatchewan, Canada.6 Prior to 1957, LSD had been described as a “psychotomimetic” drug because it was believed to induce a state of psychosis similar to that experienced in schizophrenia. But LSD does not generally induce frank auditory hallucinations or clearly defined delusional beliefs. Osmond’s new term—derived from the Greek words psyche, meaning “mind,” and delos, meaning “to show”—referred to the “mind-manifesting” capacities of LSD and related drugs.6 Psychedelic drugs can cause an array of changes to an individual’s conscious experience, from relatively mild changes in visual perception to profound derangements in sense of self and reality.
Continue to: Before describing the effects...
Classic psychedelics vs other compounds
Before describing the effects of psychedelic drugs and how they may relate to their therapeutic potential, it is useful to define which compounds are considered “classic psychedelics.”
The classic psychedelics are substances that operate primarily through activation of the serotonin 5-hydroxytryptamine receptor 2A receptor (5-HT2A) (Table 17). Many psychedelic drugs are derived from natural sources, including plants, fungi, and animals. For example, N, N-dimethyltryptamine (DMT), which is one of the most potent psychedelic compounds, is found in various plant species and can be imbibed in a tea known as ayahuasca, most commonly in the context of spiritual ceremonies.
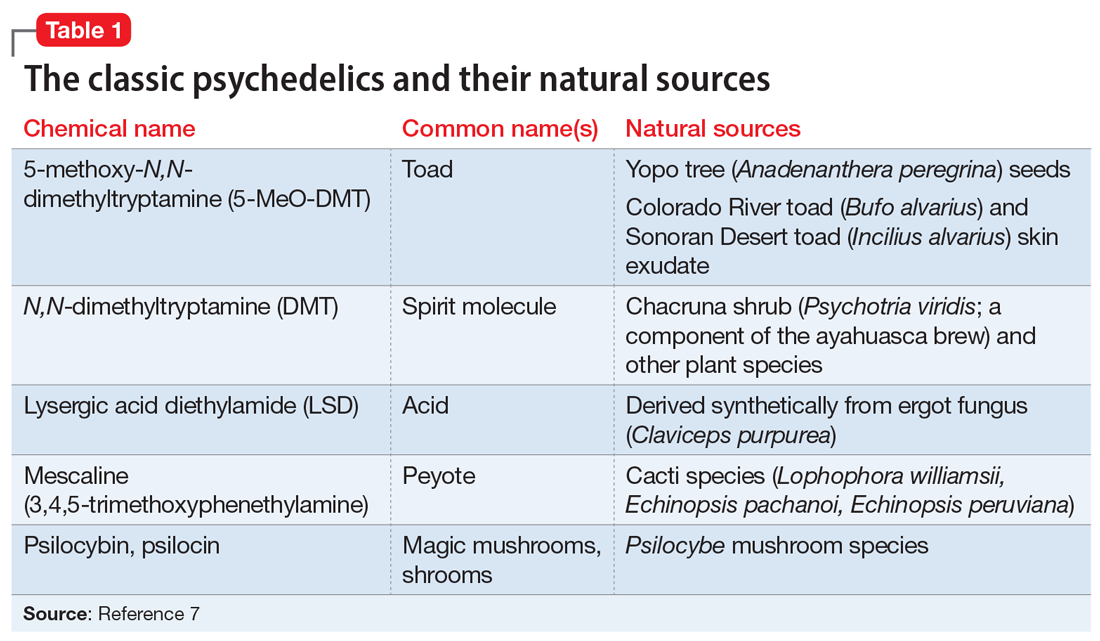
Other compounds. Some researchers continue to classify other compounds as “psychedelics,” although the mechanisms of action and effects of these compounds may vary greatly from those of the classic psychedelics. These include the dissociative anesthetics ketamine and phencyclidine (PCP), which exert their effects via N-methyl-
The DSM-58 does not differentiate between classic psychedelics and related compounds. In its chapter on Substance-Related and Addictive Disorders, the section Hallucinogen-Related Disorders provides criteria for the diagnoses of phencyclidine use disorder and other hallucinogen use disorder. Researchers generally have abandoned the term “hallucinogen” because psychedelics typically do not induce frank hallucinations. Furthermore, lumping psychedelics and compounds such as MDMA and ketamine into the category of “other hallucinogen” fails to address important distinctions between them, including diagnostically relevant issues. For example, psychedelics do not cause symptoms of physiologic dependence such as craving or a withdrawal syndrome, whereas MDMA can.9 The DSM-5 also contains a diagnosis called hallucinogen persisting perception disorder (HPPD), referring to residual distortions of visual perception that remain following psychedelic intoxication. Although the text notes the estimated prevalence of HPPD in individuals who use psychedelics is 4.2%, the condition is thought to occur infrequently in both therapeutic and recreational users.10
How psychedelics work
Psychedelics can induce a spectrum of effects that are not necessarily dose-dependent. Mild effects of intoxication include altered sensory perception in visual, auditory, proprioceptive, and somatosensory spheres, including synesthesia. Progressively more severe changes include a distorted or eliminated perception or awareness of space, time, body, and self, resulting in derealization and depersonalization. Some of the most extreme alterations of consciousness reported by users include mystical or transcendent experiences of birth, giving birth, death, exchanging bodies with a nonhuman species, and meeting otherworldly beings.11 In terms of neurophysiology, psychedelics cause altered cerebral blood flow and metabolism, increased connectivity between brain regions that do not typically communicate, and a reduction in the activity of a group of cortical structures called the default mode network (DMN).12
Continue to: Researchers hypothesize that...
Researchers hypothesize that the disruption of DMN activity may be a key mechanism accounting for psychedelics’ therapeutic effects in mental illness. The DMN is a group of structures that includes the posterior cingulate cortex, the medial prefrontal cortex, the angular gyrus, and other cortical areas that are active when an individual is not engaged in a particular mental task (for example, during mind wandering). It is thought to underlie introspection and to serve as an “orchestrator” of global brain function.13 Theoretically, then, by temporarily disrupting the neural circuits responsible for maintaining ingrained, negative thought and behavioral patterns, as observed in patients with depression or SUDs, psychedelics can help patients develop greater emotional and cognitive flexibility and identify new ways to view the world and to solve problems.
Evaluating psychedelics as therapeutic agents
The renaissance of research into psychedelics as therapeutic agents during the last 2 decades has produced some promising preliminary findings. In 2020, the American Psychiatric Association’s Work Group on Biomarkers and Novel Treatments published a review of the best evidence on the topic.14 Psilocybin is the most studied drug because compared with LSD, it carries less of a stigma and has a shorter duration of action. Psilocybin has been studied as a potential treatment for several psychiatric disorders, including terminal illness–related depression and anxiety, and SUDs.
Griffiths et al.15 In a double-blind randomized crossover study at Johns Hopkins School of Medicine, Griffiths et al15 administered a high dose (22 or 30 mg/70 kg) and a very low, placebo-like dose (1 or 3 mg/70 kg) of psilocybin at 2 separate sessions to 51 patients with terminal cancer and associated depressive and anxiety disorders. After 5 weeks, the participants assigned to one condition crossed over to the other condition. High-dose psilocybin had a significant effect on depression and anxiety symptoms within 5 weeks that persisted over 6 months of follow-up. At 6 months, 78% of participants experienced a response in depressive symptoms (≥50% decrease in GRID-Hamilton Depression Rating Scale [HAM-D-17] baseline scores) and 65% remitted (GRID-HAM-D-17 score ≤7). At 6 months, 83% of participants had a response in anxiety symptoms (≥50% decrease in Hamilton Rating Scale for Anxiety [HAM-A] baseline scores) and 57% remitted (HAM-A ≤7).
Johnson et al.16,17 In an open-label pilot study16 and ≥12-month follow-up study,17 Johnson et al administered a moderate (20 mg/70 kg) and high (30 mg/70 kg) dose of psilocybin to 15 participants enrolled in a 15-week smoking session program. The psilocybin sessions were scheduled at Weeks 5 and 7, with an optional psilocybin session at Week 13. The sessions included nondirective support from program staff, but not smoking cessation content. Relying on laboratory-verified exhaled carbon monoxide and urine cotinine measures, researchers found an 80% abstinence rate at 6 months, a 67% abstinence rate at 12 months, and a 75% abstinence rate at 2.5 years.16,17
Bogenschutz et al18 conducted a study of 10 patients who met DSM-IV criteria for alcohol dependence and had at least 2 heavy drinking days in the previous 30 days. They found that a 14-session treatment program that included 2 psilocybin-assisted psychotherapy sessions with dosages of 0.4 mg/kg resulted in a significant increase in self-reported alcohol abstinence at 4 weeks that persisted for 36 weeks.18
Although these studies were small, open-label, and had other methodologic flaws, their pilot work has led to larger-scale projects assessing psilocybin’s therapeutic potential. Psilocybin has also been studied for treatment-resistant depression and obsessive-compulsive disorder. Other clinical trials underway are investigating psilocybin for the treatment of cocaine and opioid use disorder, anorexia nervosa, and depression in Alzheimer’s disease.14 Although psilocybin is currently the best-studied psychedelic, there is some research demonstrating that LSD can also induce a persistent reduction in anxiety symptoms associated with terminal illness19 and that ayahuasca causes a rapid reduction in depressive symptoms that persists over 21 days.20
Continue to: The future of psychedelic psychiatry...
The future of psychedelic psychiatry
If psychedelic compounds become approved for the treatment of psychiatric conditions, psychiatrists will likely be responsible for prescribing them and managing patients who receive them.21Table 211,21-24 summarizes practical considerations for psychiatrists who may someday be prescribing psychedelic drugs. Areas of psychedelic treatment in which psychiatric expertise is necessary include:
- screening for patients at increased risk for a challenging or adverse experience or “bad trip”
- conducting a thorough informed consent process in which the risks are discussed and the patient’s wishes regarding potential situations are elicited
- managing acute medical and psychiatric complications, including agitation and violent behavior
- ensuring the use of trained guides during sessions.
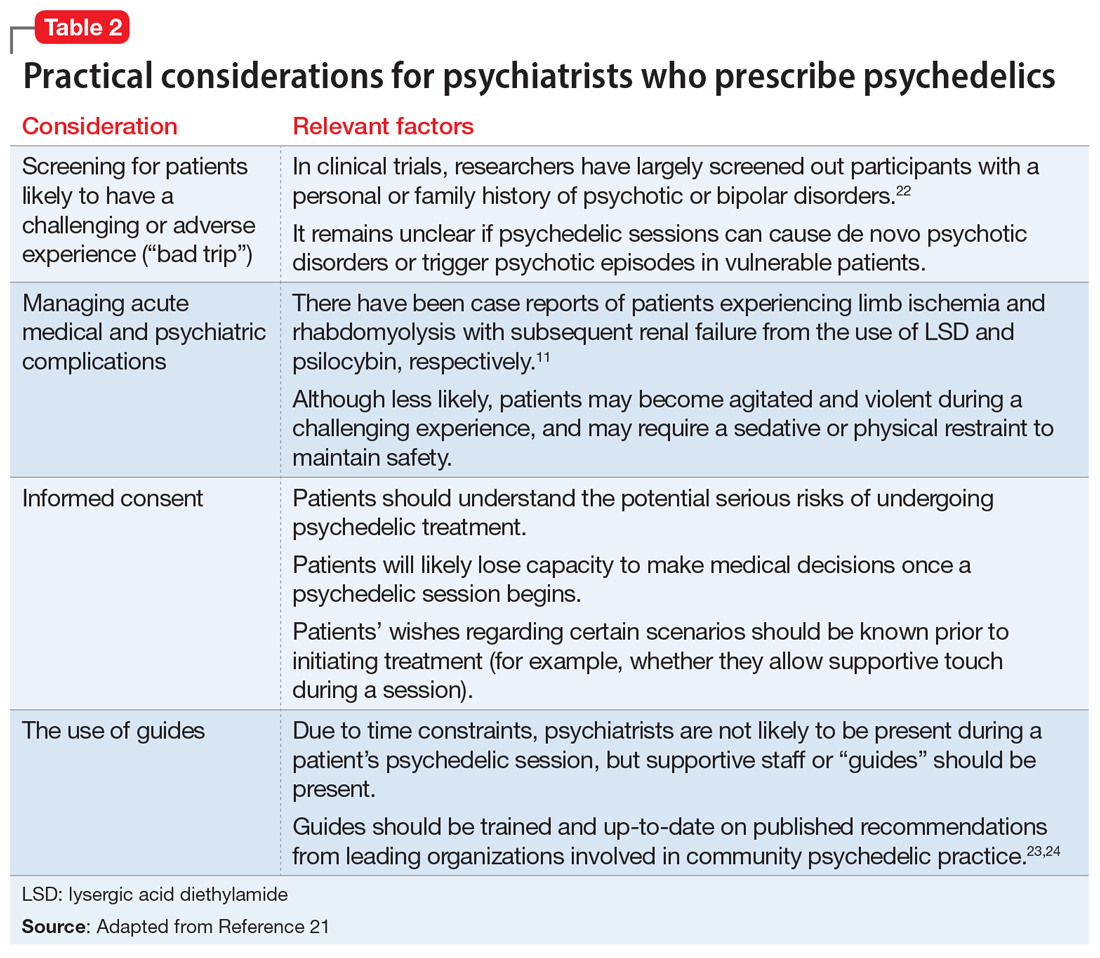
Psychiatrists who are interested in providing psychedelic-assisted therapy should understand the concept of “set and setting,” which was defined by Timothy Leary in the 1960s and is thought to play an important role in determining the types of experiences that arise during a psychedelic session.25 “Set” refers to an individual’s mindset going into a session, and “setting” refers to the environment in which the session occurs. Typical elements of each are summarized in Table 3.7 Psychiatrists will play a critical role in assessing and preparing the “set” by screening patients appropriately, assessing patient goals, and providing a thorough informed consent procedure. Psychiatrists should also be mindful of the “setting,” providing a comfortable, safe, familiar environment and access to appropriate music and eyeshades, if desired. Due to time restraints, psychiatrists are not likely to be responsible for guiding patients through sessions, and should educate themselves about ethical practices of psychedelic guides,if they are in the position to hire guides.23,24
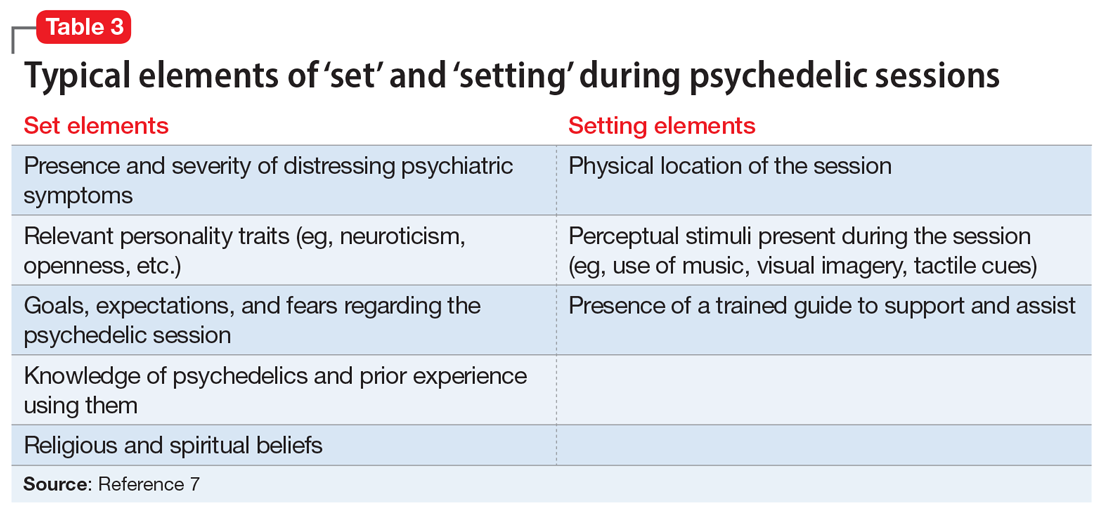
Psychiatrists may also play a role in providing psychotherapy to patients receiving treatment with psychedelics. These substances can induce both transcendent and terrifying experiences. Patients therefore require “integration” therapy sessions to assist with processing the content of their psychedelic treatment and incorporating the experiences into day-to-day life. In an online survey of nearly 2,000 individuals who used psilocybin recreationally, 7.6% reported that they had to seek treatment for enduring psychological symptoms that they attributed to their psilocybin use, including persistent anxiety, fear, paranoia, and depression.26 Integrative psychotherapy sessions may help reduce the risk of persistent negative effects from therapeutic psychedelics, as well as enhance their beneficial effects.
CASE CONTINUED
Mr. P is enrolled in the academic medical center study assessing the effect of psilocybin on terminal illness-related anxiety and depression. During a 5-hour, 30-mg psilocybin session, he initially experiences distorted visual cues, with vivid, colorful geometric patterns collapsing into each other. He then loses the concepts and experience of time, space, and his body, as his visual distortions convert to darkness. After what seems like a decade within the darkness, he sees himself lying in a hospital bed with loved ones surrounding him. He watches himself take his last breaths and his family members weep as he dies. As he regains his senses, Mr. P feels that he is being reborn.
In the therapy sessions that follow the psychedelic session, Mr. P reports feeling “finally freed” from the fear, sadness, and anger that he has felt throughout his life. He comes to accept his impending death with gratitude and peace. In his final days, he no longer experiences depression or anxiety. Mr. P’s friends and family members comment that he seems to be the best version of himself in the months that lead up to his death.
Related Resources
• Nutt D. Psychedelic drugs-a new era in psychiatry? Dialogues Clin Neurosci. 2019;21(2):139-147.
• Garcia-Romeu A, Kersgaard B, Addy PH. Clinical applications of hallucinogens: a review. Exp Clin Psychopharmacol. 2016; 24(4):229-268.
Drug Brand Names
Amitriptyline • Amitril, Elavil
Bupropion • Wellbutrin
Fluoxetine • Prozac
Sertraline • Zoloft
Bottom Line
Psychedelics are a class of consciousness-altering agents that have become a potentially promising source of new treatments for psychiatric illness. Although more evidence is needed, compounds such as psilocybin may one day become FDAapproved for conditions such as terminal illness–related depression and anxiety, and substance use disorders. When this occurs, psychiatrists should be responsible for prescribing psychedelics and managing patients who receive treatment.
1. Smith DE, Raswyck GE, Davidson LD. From Hofmann to the Haight Ashbury, and into the future: the past and potential of lysergic acid diethylamide. J Psychoactive Drugs. 2014;46(1):3-10.
2. Siegel M. Threading Denver’s magic mushrooms needle: promising as medicine, risky as recreation. USA Today. Published May 13, 2019. Accessed December 4, 2020. https://www.usatoday.com/story/opinion/2019/05/13/denver-magic-mushrooms-promising-medicine-reckless-recreation-column/1182543001
3. Epstein, K. Oakland decriminalizes ‘magic mushrooms’ and other natural psychedelics. The Washington Post. Published June 5, 2019. Accessed December 4, 2020. https://www.washingtonpost.com/nation/2019/06/05/oakland-decriminalizes-magic-mushrooms-other-natural-psychedelics
4. York JA. Santa Cruz decriminalizes natural psychedelics. Santa Cruz Sentinel. Published January 30, 2020. Accessed December 4, 2020. https://www.santacruzsentinel.com/2020/01/29/santa-cruz-decriminalizes-natural-psychedelics
5. Acker L. Oregon becomes first state to legalize psychedelic mushrooms. The Oregonian/Oregon Live. Published November 4, 2020. Accessed December 4, 2020. https://www.oregonlive.com/politics/2020/11/oregon-becomes-first-state-to-legalize-psychedelic-mushrooms.html
6. Dyck E. Flashback: psychiatric experimentation with LSD in historical perspective. Can J Psychiatry. 2005;50(7):381-388.
7. Holoyda BJ. The psychedelic renaissance and its forensic implications. J Am Acad Psychiatry Law. 2020;48(1):87-97.
8. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
9. Davis AK, Rosenberg H. The prevalence, intensity, and assessment of craving for MDMA/ecstasy in recreational users. J Psychoactive Drugs. 2014;46(2):154-151.
10. Halpern JH, Lerner AG, Passie T. A review of hallucinogen persisting perception disorder (HPPD) and an exploratory study of subjects claiming symptoms of HPPD. Curr Top Behav Neurosci. 2018;36:333-360.
11. Nichols DE. Psychedelics. Pharmacol Rev. 2016;68(2):264-355.
12. Nichols DE. Hallucinogens. Pharmacol Ther. 2004;101(2):131-181.
13. Carhart-Harris RL, Leech R, Hellyer PJ, et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci. 2014;8:20.
14. Reiff CM, Richman EE, Nemeroff CB, et al. Psychedelics and psychedelic-assisted psychotherapy. Am J Psychiatry. 2020;177(5):391-410.
15. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197.
16. Johnson MW, Garcia-Romeu A, Cosimano MP, et al. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J Psychopharmacol. 2014;28(11):983-992.
17. Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43(1):55-60.
18. Bogenschutz MP, Forcehimes AA, Pommy JA, et al. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. J Psychopharmacol. 2015;29(3):1182-1190.
19. Gasser P, Holstein D, Michel Y, et al. Safety and efficacy of lysergic acid diethylamide-assisted psychotherapy for anxiety associated with life-threatening diseases. J Nerv Ment Dis. 2014;202(7):531-520.
20. Osório F de L, Sanches RF, Macedo LR, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a preliminary report. Braz J Psychiatry. 2015;37(1):13-20.
21. Holoyda B. Psychedelic psychiatry: preparing for novel treatments involving altered states of consciousness. Psych Serv. 2020;71(12):1297-1299.
22. Johnson MW, Richards W, Griffiths RR. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008;22(6):603-620.
23. Council on Spiritual Practices. Code of ethics for spiritual Guides. Published August 10, 2001. Accessed November 25, 2020. https://csp.org/docs/code-of-ethics-for-spiritual-guides
24. Multidisciplinary Association for Psychedelic Studies. Zendo psychedelic harm reduction training manual. Published 2017. Accessed November 25, 2020. https://zendoproject.org/wp-content/uploads/2017/06/Zendo-Manual-2017.pdf
25. Zinberg NE. Drug, set, and setting: the basis for controlled intoxicant use. Yale University Press; 1984.
26. Carbonaro TM, Bradstreet MP, Barrett FS, et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: acute and enduring positive and negative consequences. J Psychopharmacol. 2016;30(12):1268-1278.
1. Smith DE, Raswyck GE, Davidson LD. From Hofmann to the Haight Ashbury, and into the future: the past and potential of lysergic acid diethylamide. J Psychoactive Drugs. 2014;46(1):3-10.
2. Siegel M. Threading Denver’s magic mushrooms needle: promising as medicine, risky as recreation. USA Today. Published May 13, 2019. Accessed December 4, 2020. https://www.usatoday.com/story/opinion/2019/05/13/denver-magic-mushrooms-promising-medicine-reckless-recreation-column/1182543001
3. Epstein, K. Oakland decriminalizes ‘magic mushrooms’ and other natural psychedelics. The Washington Post. Published June 5, 2019. Accessed December 4, 2020. https://www.washingtonpost.com/nation/2019/06/05/oakland-decriminalizes-magic-mushrooms-other-natural-psychedelics
4. York JA. Santa Cruz decriminalizes natural psychedelics. Santa Cruz Sentinel. Published January 30, 2020. Accessed December 4, 2020. https://www.santacruzsentinel.com/2020/01/29/santa-cruz-decriminalizes-natural-psychedelics
5. Acker L. Oregon becomes first state to legalize psychedelic mushrooms. The Oregonian/Oregon Live. Published November 4, 2020. Accessed December 4, 2020. https://www.oregonlive.com/politics/2020/11/oregon-becomes-first-state-to-legalize-psychedelic-mushrooms.html
6. Dyck E. Flashback: psychiatric experimentation with LSD in historical perspective. Can J Psychiatry. 2005;50(7):381-388.
7. Holoyda BJ. The psychedelic renaissance and its forensic implications. J Am Acad Psychiatry Law. 2020;48(1):87-97.
8. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
9. Davis AK, Rosenberg H. The prevalence, intensity, and assessment of craving for MDMA/ecstasy in recreational users. J Psychoactive Drugs. 2014;46(2):154-151.
10. Halpern JH, Lerner AG, Passie T. A review of hallucinogen persisting perception disorder (HPPD) and an exploratory study of subjects claiming symptoms of HPPD. Curr Top Behav Neurosci. 2018;36:333-360.
11. Nichols DE. Psychedelics. Pharmacol Rev. 2016;68(2):264-355.
12. Nichols DE. Hallucinogens. Pharmacol Ther. 2004;101(2):131-181.
13. Carhart-Harris RL, Leech R, Hellyer PJ, et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci. 2014;8:20.
14. Reiff CM, Richman EE, Nemeroff CB, et al. Psychedelics and psychedelic-assisted psychotherapy. Am J Psychiatry. 2020;177(5):391-410.
15. Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197.
16. Johnson MW, Garcia-Romeu A, Cosimano MP, et al. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J Psychopharmacol. 2014;28(11):983-992.
17. Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43(1):55-60.
18. Bogenschutz MP, Forcehimes AA, Pommy JA, et al. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. J Psychopharmacol. 2015;29(3):1182-1190.
19. Gasser P, Holstein D, Michel Y, et al. Safety and efficacy of lysergic acid diethylamide-assisted psychotherapy for anxiety associated with life-threatening diseases. J Nerv Ment Dis. 2014;202(7):531-520.
20. Osório F de L, Sanches RF, Macedo LR, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a preliminary report. Braz J Psychiatry. 2015;37(1):13-20.
21. Holoyda B. Psychedelic psychiatry: preparing for novel treatments involving altered states of consciousness. Psych Serv. 2020;71(12):1297-1299.
22. Johnson MW, Richards W, Griffiths RR. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008;22(6):603-620.
23. Council on Spiritual Practices. Code of ethics for spiritual Guides. Published August 10, 2001. Accessed November 25, 2020. https://csp.org/docs/code-of-ethics-for-spiritual-guides
24. Multidisciplinary Association for Psychedelic Studies. Zendo psychedelic harm reduction training manual. Published 2017. Accessed November 25, 2020. https://zendoproject.org/wp-content/uploads/2017/06/Zendo-Manual-2017.pdf
25. Zinberg NE. Drug, set, and setting: the basis for controlled intoxicant use. Yale University Press; 1984.
26. Carbonaro TM, Bradstreet MP, Barrett FS, et al. Survey study of challenging experiences after ingesting psilocybin mushrooms: acute and enduring positive and negative consequences. J Psychopharmacol. 2016;30(12):1268-1278.
Kennedy, NIMH demand urgent action on COVID-19 mental health toll
A public-private partnership, led by mental health advocate Patrick Kennedy and the head of the National Institute of Mental Health, Joshua Gordon, MD, PhD, want urgent action to address the wave of mental illness and suicide caused by COVID-19.
“Our country is in serious denial about the full impact of mental health in this country and certainly as part of this pandemic,” said former congressman Mr. Kennedy, cochair of the Action Alliance’s Mental Health & Suicide Prevention National Response to COVID-19, at a briefing unveiling the group’s new six-priority Action Plan.
“That’s reinforced when all we hear from is Dr. Fauci,” and only about the physical effects of the disease, said Mr. Kennedy, the founder of the Kennedy Forum, a nonprofit dedicated to changing the health system’s approach to mental health and substance use disorders.
“ he said. Mr. Kennedy noted the huge effort to speed therapeutics and vaccines to the American public. “We need to bring that same sense of urgency to these deaths of despair hiding in plain sight.”
Dr. Gordon, NIMH’s director and a cochair of the National Response group, was also at the briefing.
“We know many people report experiencing symptoms of distress, including anxiety, sleep problems, depression, substance use, and suicidal thoughts at rates two to three times higher than we might expect in times before the pandemic. Just as the country has come together to mitigate the physical impacts of pandemic, we also have to identify how to mitigate the mental health impacts,” said Dr. Gordon.
Plan of action
Mr. Kennedy emphasized that it is crucial that federal lawmakers and regulators find a way to increase parity between mental and physical health.
Paramount in that effort would be ensuring stronger enforcement of the Mental Health Parity and Addiction Equity Act, he said.
That 1996 law requires health plans to ensure that benefits for physical and mental health were equivalent, but it has frequently been ignored. In 2019, a U.S. federal court found that one of the nation’s largest behavioral health insurers, United Behavioral Health, had been violating the law. Mr. Kennedy said he expects this decision to continue to have a positive impact on achieving parity.
In November, United was ordered by a federal judge to reprocess 67,000 claims that it illegally denied.
The Alliance’s Action Plan has six priorities:
- Change the national conversation about mental health and suicide.
- Increase access to evidence-based treatments for substance use and mental health disorders in specialty and primary care, and include better reimbursement for services and make permanent reimbursement for telehealth services.
- Increase the use of nonpunitive and supportive crisis intervention services, including keeping people out of the criminal justice system.
- Establish near real-time data collection systems to promptly identify changes in rates of suicide, overdose, and other key events, and of clusters or spikes.
- Ensure the equitable delivery of comprehensive and effective suicide prevention and mental health services for Black Americans, Latin Americans, American Indian/Alaskan Natives, LGBTQ individuals, and others disproportionately impacted by the pandemic.
- Invest in prevention and early intervention approaches that treat the root causes of suicide and mental health problems.
Uptick in distress
Dr. Gordon noted that recent data indicate that, although ED visits for children are still down in 2020, compared with previous years, mental health ED visits are back to prepandemic levels.
A September survey showed an increase in suicidal thoughts and attempts, anxiety, and depression pandemic in youth because of the pandemic. Almost one-quarter of those surveyed said they knew a peer who developed suicidal thoughts since the start of the pandemic and 5% reported making a suicide attempt themselves.
In early December, research reported in JAMA Psychiatry showed the overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends in 2018 and 2019, and that all overdose-related incidents were about 17% above baseline in 2020.
COVID-19 also appears to be striking individuals who are living in behavioral health facilities, and some of those facilities are reducing inpatient care and other programs because they don’t have enough personal protective equipment, testing supplies, or staff to cope with the disease.
The facilities are not required to report infections to the federal government. Sen. Elizabeth Warren (D-Mass.), Rep. Carolyn Maloney (D-N.Y.), and Rep. Katie Porter (D-Calif.) issued a report based on their own offices’ survey of 10 large behavioral health program operators.
Eight of those operators – covering 376 facilities and more than 100,000 patients in 40 states and Puerto Rico – provided substantive responses.
More than half had at least one COVID case and 14% had large outbreaks of 10 or more cases. The infection rate for patients was in line with that of the general public.
A version of this article originally appeared on Medscape.com.
A public-private partnership, led by mental health advocate Patrick Kennedy and the head of the National Institute of Mental Health, Joshua Gordon, MD, PhD, want urgent action to address the wave of mental illness and suicide caused by COVID-19.
“Our country is in serious denial about the full impact of mental health in this country and certainly as part of this pandemic,” said former congressman Mr. Kennedy, cochair of the Action Alliance’s Mental Health & Suicide Prevention National Response to COVID-19, at a briefing unveiling the group’s new six-priority Action Plan.
“That’s reinforced when all we hear from is Dr. Fauci,” and only about the physical effects of the disease, said Mr. Kennedy, the founder of the Kennedy Forum, a nonprofit dedicated to changing the health system’s approach to mental health and substance use disorders.
“ he said. Mr. Kennedy noted the huge effort to speed therapeutics and vaccines to the American public. “We need to bring that same sense of urgency to these deaths of despair hiding in plain sight.”
Dr. Gordon, NIMH’s director and a cochair of the National Response group, was also at the briefing.
“We know many people report experiencing symptoms of distress, including anxiety, sleep problems, depression, substance use, and suicidal thoughts at rates two to three times higher than we might expect in times before the pandemic. Just as the country has come together to mitigate the physical impacts of pandemic, we also have to identify how to mitigate the mental health impacts,” said Dr. Gordon.
Plan of action
Mr. Kennedy emphasized that it is crucial that federal lawmakers and regulators find a way to increase parity between mental and physical health.
Paramount in that effort would be ensuring stronger enforcement of the Mental Health Parity and Addiction Equity Act, he said.
That 1996 law requires health plans to ensure that benefits for physical and mental health were equivalent, but it has frequently been ignored. In 2019, a U.S. federal court found that one of the nation’s largest behavioral health insurers, United Behavioral Health, had been violating the law. Mr. Kennedy said he expects this decision to continue to have a positive impact on achieving parity.
In November, United was ordered by a federal judge to reprocess 67,000 claims that it illegally denied.
The Alliance’s Action Plan has six priorities:
- Change the national conversation about mental health and suicide.
- Increase access to evidence-based treatments for substance use and mental health disorders in specialty and primary care, and include better reimbursement for services and make permanent reimbursement for telehealth services.
- Increase the use of nonpunitive and supportive crisis intervention services, including keeping people out of the criminal justice system.
- Establish near real-time data collection systems to promptly identify changes in rates of suicide, overdose, and other key events, and of clusters or spikes.
- Ensure the equitable delivery of comprehensive and effective suicide prevention and mental health services for Black Americans, Latin Americans, American Indian/Alaskan Natives, LGBTQ individuals, and others disproportionately impacted by the pandemic.
- Invest in prevention and early intervention approaches that treat the root causes of suicide and mental health problems.
Uptick in distress
Dr. Gordon noted that recent data indicate that, although ED visits for children are still down in 2020, compared with previous years, mental health ED visits are back to prepandemic levels.
A September survey showed an increase in suicidal thoughts and attempts, anxiety, and depression pandemic in youth because of the pandemic. Almost one-quarter of those surveyed said they knew a peer who developed suicidal thoughts since the start of the pandemic and 5% reported making a suicide attempt themselves.
In early December, research reported in JAMA Psychiatry showed the overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends in 2018 and 2019, and that all overdose-related incidents were about 17% above baseline in 2020.
COVID-19 also appears to be striking individuals who are living in behavioral health facilities, and some of those facilities are reducing inpatient care and other programs because they don’t have enough personal protective equipment, testing supplies, or staff to cope with the disease.
The facilities are not required to report infections to the federal government. Sen. Elizabeth Warren (D-Mass.), Rep. Carolyn Maloney (D-N.Y.), and Rep. Katie Porter (D-Calif.) issued a report based on their own offices’ survey of 10 large behavioral health program operators.
Eight of those operators – covering 376 facilities and more than 100,000 patients in 40 states and Puerto Rico – provided substantive responses.
More than half had at least one COVID case and 14% had large outbreaks of 10 or more cases. The infection rate for patients was in line with that of the general public.
A version of this article originally appeared on Medscape.com.
A public-private partnership, led by mental health advocate Patrick Kennedy and the head of the National Institute of Mental Health, Joshua Gordon, MD, PhD, want urgent action to address the wave of mental illness and suicide caused by COVID-19.
“Our country is in serious denial about the full impact of mental health in this country and certainly as part of this pandemic,” said former congressman Mr. Kennedy, cochair of the Action Alliance’s Mental Health & Suicide Prevention National Response to COVID-19, at a briefing unveiling the group’s new six-priority Action Plan.
“That’s reinforced when all we hear from is Dr. Fauci,” and only about the physical effects of the disease, said Mr. Kennedy, the founder of the Kennedy Forum, a nonprofit dedicated to changing the health system’s approach to mental health and substance use disorders.
“ he said. Mr. Kennedy noted the huge effort to speed therapeutics and vaccines to the American public. “We need to bring that same sense of urgency to these deaths of despair hiding in plain sight.”
Dr. Gordon, NIMH’s director and a cochair of the National Response group, was also at the briefing.
“We know many people report experiencing symptoms of distress, including anxiety, sleep problems, depression, substance use, and suicidal thoughts at rates two to three times higher than we might expect in times before the pandemic. Just as the country has come together to mitigate the physical impacts of pandemic, we also have to identify how to mitigate the mental health impacts,” said Dr. Gordon.
Plan of action
Mr. Kennedy emphasized that it is crucial that federal lawmakers and regulators find a way to increase parity between mental and physical health.
Paramount in that effort would be ensuring stronger enforcement of the Mental Health Parity and Addiction Equity Act, he said.
That 1996 law requires health plans to ensure that benefits for physical and mental health were equivalent, but it has frequently been ignored. In 2019, a U.S. federal court found that one of the nation’s largest behavioral health insurers, United Behavioral Health, had been violating the law. Mr. Kennedy said he expects this decision to continue to have a positive impact on achieving parity.
In November, United was ordered by a federal judge to reprocess 67,000 claims that it illegally denied.
The Alliance’s Action Plan has six priorities:
- Change the national conversation about mental health and suicide.
- Increase access to evidence-based treatments for substance use and mental health disorders in specialty and primary care, and include better reimbursement for services and make permanent reimbursement for telehealth services.
- Increase the use of nonpunitive and supportive crisis intervention services, including keeping people out of the criminal justice system.
- Establish near real-time data collection systems to promptly identify changes in rates of suicide, overdose, and other key events, and of clusters or spikes.
- Ensure the equitable delivery of comprehensive and effective suicide prevention and mental health services for Black Americans, Latin Americans, American Indian/Alaskan Natives, LGBTQ individuals, and others disproportionately impacted by the pandemic.
- Invest in prevention and early intervention approaches that treat the root causes of suicide and mental health problems.
Uptick in distress
Dr. Gordon noted that recent data indicate that, although ED visits for children are still down in 2020, compared with previous years, mental health ED visits are back to prepandemic levels.
A September survey showed an increase in suicidal thoughts and attempts, anxiety, and depression pandemic in youth because of the pandemic. Almost one-quarter of those surveyed said they knew a peer who developed suicidal thoughts since the start of the pandemic and 5% reported making a suicide attempt themselves.
In early December, research reported in JAMA Psychiatry showed the overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends in 2018 and 2019, and that all overdose-related incidents were about 17% above baseline in 2020.
COVID-19 also appears to be striking individuals who are living in behavioral health facilities, and some of those facilities are reducing inpatient care and other programs because they don’t have enough personal protective equipment, testing supplies, or staff to cope with the disease.
The facilities are not required to report infections to the federal government. Sen. Elizabeth Warren (D-Mass.), Rep. Carolyn Maloney (D-N.Y.), and Rep. Katie Porter (D-Calif.) issued a report based on their own offices’ survey of 10 large behavioral health program operators.
Eight of those operators – covering 376 facilities and more than 100,000 patients in 40 states and Puerto Rico – provided substantive responses.
More than half had at least one COVID case and 14% had large outbreaks of 10 or more cases. The infection rate for patients was in line with that of the general public.
A version of this article originally appeared on Medscape.com.
Rap music mention of mental health topics more than doubles
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
FROM JAMA PEDIATRICS
COVID-19 fuels surge in overdose-related cardiac arrests
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Treating insomnia, anxiety in a pandemic
Since the start of the pandemic, we have been conducting an extra hour of Virtual Rounds at the Center for Women’s Mental Health. Virtual Rounds has been an opportunity to discuss cases around a spectrum of clinical management issues with respect to depression, bipolar disorder, and a spectrum of anxiety disorders like obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder. How to apply the calculus of risk-benefit decision-making around management of psychiatric disorder during pregnancy and the postpartum period has been the cornerstone of the work at our center for over 2 decades.
When we went virtual at our center in the early Spring, we decided to keep the format of our faculty rounds the way they have been for years and to sustain cohesiveness of our program during the pandemic. But we thought the needs of pregnant and postpartum women warranted being addressed in a context more specific to COVID-19, and also that reproductive psychiatrists and other clinicians could learn from each other about novel issues coming up for this group of patients during the pandemic. With that backdrop, Marlene Freeman, MD, and I founded “Virtual Rounds at the Center” to respond to queries from our colleagues across the country; we do this just after our own rounds on Wednesdays at 2:00 p.m.
As the pandemic has progressed, Virtual Rounds has blossomed into a virtual community on the Zoom platform, where social workers, psychologists, nurse prescribers, psychiatrists, and obstetricians discuss the needs of pregnant and postpartum women specific to COVID-19. Frequently, our discussions involve a review of the risks and benefits of treatment before, during, and after pregnancy.
Seemingly, week to week, more and more colleagues raise questions about the treatment of anxiety and insomnia during pregnancy and the postpartum period. I’ve spoken in previous columns about the enhanced use of telemedicine. Telemedicine not only facilitates efforts like Virtual Rounds and our ability to reach out to colleagues across the country and share cases, but also has allowed us to keep even closer tabs on the emotional well-being of our pregnant and postpartum women during COVID-19.
The question is not just about the effects of a medicine that a woman might take to treat anxiety or insomnia during pregnancy, but the experience of the pandemic per se, which we are measuring in multiple studies now using a variety of psychological instruments that patients complete. The pandemic is unequivocally taking a still unquantified toll on the mental health of Americans and potentially on the next generation to come.
Midcycle awakening during pregnancy
Complaints of insomnia and midcycle awakening during pregnancy are not new – it is the rule, rather than the exception for many pregnant women, particularly later in pregnancy. We have unequivocally seen a worsening of complaints of sleep disruption including insomnia and midcycle awakening during the pandemic that is greater than what we have seen previously. Both patients and colleagues have asked us the safest ways to manage it. One of the first things we consider when we hear about insomnia is whether it is part of an underlying mood disorder. While we see primary insomnia clinically, it really is important to remember that insomnia can be part and parcel of an underlying mood disorder.
With that in mind, what are the options? During the pandemic, we’ve seen an increased use of digital cognitive behavioral therapy for insomnia (CBT-I) for patients who cannot initiate sleep, which has a very strong evidence base for effectiveness as a first-line intervention for many.
If a patient has an incomplete response to CBT-I, what might be pursued next? In our center, we have a low threshold for using low doses of benzodiazepines, such as lorazepam or clonazepam, because the majority of data do not support an increased risk of major congenital malformations even when used in the first trimester. It is quite common to see medicines such as newer nonbenzodiazepine sedative hypnotics such as Ambien CR (zolpidem) or Lunesta (eszopiclone) used by our colleagues in ob.gyn. The reproductive safety data on those medicines are particularly sparse, and they may have greater risk of cognitive side effects the next day, so we tend to avoid them.
Another sometimes-forgotten option to consider is using low doses of tricyclic antidepressants (i.e., 10-25 mg of nortriptyline at bedtime), with tricyclics having a 40-year history and at least one pooled analysis showing the absence of increased risk for major congenital malformations when used. This may be a very easy way of managing insomnia, with low-dose tricyclics having an anxiolytic effect as well.
Anxiety during pregnancy
The most common rise in symptoms during COVID-19 for women who are pregnant or post partum has been an increase in anxiety. Women present with a spectrum of concerns leading to anxiety symptoms in the context of the pandemic. Earlier on in the pandemic, concerns focused mostly on how to stay healthy, and how to mitigate risk and not catch SARS-CoV-2 during pregnancy, as well as the very complex issues that were playing out in real time as hospital systems were figuring out how to manage pregnant women in labor and to keep both them and staff safe. Over time, anxiety has shifted to still staying safe during the pandemic and the potential impact of SARS-CoV-2 infection on pregnancy outcomes. The No. 1 concern is what the implications of COVID-19 disease are on mother and child. New mothers also are anxious about how they will practically navigate life with a newborn in the postpartum setting.
Early on in the pandemic, some hospital systems severely limited who was in the room with a woman during labor, potentially impeding the wishes of women during delivery who would have wanted their loved ones and/or a doula present, as an example. With enhanced testing available now, protocols have since relaxed in many hospitals to allow partners – but not a team – to remain in the hospital during the labor process. Still, the prospect of delivering during a pandemic is undoubtedly a source of anxiety for some women.
This sort of anxiety, particularly in patients with preexisting anxiety disorders, can be particularly challenging. Fortunately, there has been a rapid increase over the last several years of digital apps to mitigate anxiety. While many of them have not been systematically studied, the data on biobehavioral intervention for anxiety is enormous, and this should be used as first-line treatment for patients with mild to moderate symptoms; so many women would prefer to avoid pharmacological intervention during pregnancy, if possible, to avoid fetal drug exposure. For patients who meet criteria for frank anxiety disorder, other nonpharmacologic interventions such as CBT have been shown to be effective.
Frequently, we see women who are experiencing levels of anxiety where nonpharmacological interventions have an incomplete response, and colleagues have asked about the safest way to treat these patients. As has been discussed in multiple previous columns, selective serotonin reuptake inhibitors (SSRIs) should be thought of sooner rather than later, particularly with medicines with good reproductive safety data such as sertraline, citalopram, or fluoxetine.
We also reported over 15 years ago that at least 30%-40% of women presenting with histories of recurrent major depression at the beginning of pregnancy had comorbid anxiety disorders, and that the use of benzodiazepines in that population in addition to SSRIs was exceedingly common, with doses of approximately 0.5-1.5 mg of clonazepam or lorazepam being standard fare. Again, this is very appropriate treatment to mitigate anxiety symptoms because now have enough data as a field that support the existence of adverse outcomes associated with untreated anxiety during pregnancy in terms of both adverse obstetric and neonatal outcomes, higher rates of preterm birth, and other obstetric complications. Hence, managing anxiety during pregnancy should be considered like managing a toxic exposure – the same way that one would be concerned about anything else that a pregnant woman could be exposed to.
Lastly, although no atypical antipsychotic has been approved for the treatment of anxiety, its use off label is extremely common. More and more data support the absence of a signal of teratogenicity across the family of molecules including atypical antipsychotics. Beyond potential use of atypical antipsychotics, at Virtual Rounds last week, a colleague asked about the use of gabapentin in a patient who was diagnosed with substance use disorder and who had inadvertently conceived on gabapentin, which was being used to treat both anxiety and insomnia. We have typically avoided the use of gabapentin during pregnancy because prospective data have been limited to relatively small case series and one report, with a total of exposures in roughly the 300 range.
However, our colleagues at the Harvard School of Public Health have recently published an article that looked at the United States Medicaid Analytic eXtract (MAX) dataset, which has been used to publish other articles addressing atypical antipsychotics, SSRIs, lithium, and pharmacovigilance investigations among other important topics. In this study, the database was used to look specifically at 4,642 pregnancies with gabapentin exposure relative to 1,744,447 unexposed pregnancies, without a significant finding for increased risk for major congenital malformations.
The question of an increased risk of cardiac malformations and of increased risk for obstetric complications are difficult to untangle from anxiety and depression, as they also are associated with those same outcomes. With that said, the analysis is a welcome addition to our knowledge base for a medicine used more widely to treat symptoms such as anxiety and insomnia in the general population, with a question mark around where it may fit into the algorithm during pregnancy.
In our center, gabapentin still would not be used as a first-line treatment for the management of anxiety or insomnia during pregnancy. But these new data still are reassuring for patients who come in, frequently with unplanned pregnancies. It is an important reminder to those of us taking care of patients during the pandemic to review use of contraception, because although data are unavailable specific to the period of the pandemic, what is clear is that, even prior to COVID-19, 50% of pregnancies in America were unplanned. Addressing issues of reliable use of contraception, particularly during the pandemic, is that much more important.
In this particular case, our clinician colleague in Virtual Rounds decided to continue gabapentin across pregnancy in the context of these reassuring data, but others may choose to discontinue or pursue some of the other treatment options noted above.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Since the start of the pandemic, we have been conducting an extra hour of Virtual Rounds at the Center for Women’s Mental Health. Virtual Rounds has been an opportunity to discuss cases around a spectrum of clinical management issues with respect to depression, bipolar disorder, and a spectrum of anxiety disorders like obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder. How to apply the calculus of risk-benefit decision-making around management of psychiatric disorder during pregnancy and the postpartum period has been the cornerstone of the work at our center for over 2 decades.
When we went virtual at our center in the early Spring, we decided to keep the format of our faculty rounds the way they have been for years and to sustain cohesiveness of our program during the pandemic. But we thought the needs of pregnant and postpartum women warranted being addressed in a context more specific to COVID-19, and also that reproductive psychiatrists and other clinicians could learn from each other about novel issues coming up for this group of patients during the pandemic. With that backdrop, Marlene Freeman, MD, and I founded “Virtual Rounds at the Center” to respond to queries from our colleagues across the country; we do this just after our own rounds on Wednesdays at 2:00 p.m.
As the pandemic has progressed, Virtual Rounds has blossomed into a virtual community on the Zoom platform, where social workers, psychologists, nurse prescribers, psychiatrists, and obstetricians discuss the needs of pregnant and postpartum women specific to COVID-19. Frequently, our discussions involve a review of the risks and benefits of treatment before, during, and after pregnancy.
Seemingly, week to week, more and more colleagues raise questions about the treatment of anxiety and insomnia during pregnancy and the postpartum period. I’ve spoken in previous columns about the enhanced use of telemedicine. Telemedicine not only facilitates efforts like Virtual Rounds and our ability to reach out to colleagues across the country and share cases, but also has allowed us to keep even closer tabs on the emotional well-being of our pregnant and postpartum women during COVID-19.
The question is not just about the effects of a medicine that a woman might take to treat anxiety or insomnia during pregnancy, but the experience of the pandemic per se, which we are measuring in multiple studies now using a variety of psychological instruments that patients complete. The pandemic is unequivocally taking a still unquantified toll on the mental health of Americans and potentially on the next generation to come.
Midcycle awakening during pregnancy
Complaints of insomnia and midcycle awakening during pregnancy are not new – it is the rule, rather than the exception for many pregnant women, particularly later in pregnancy. We have unequivocally seen a worsening of complaints of sleep disruption including insomnia and midcycle awakening during the pandemic that is greater than what we have seen previously. Both patients and colleagues have asked us the safest ways to manage it. One of the first things we consider when we hear about insomnia is whether it is part of an underlying mood disorder. While we see primary insomnia clinically, it really is important to remember that insomnia can be part and parcel of an underlying mood disorder.
With that in mind, what are the options? During the pandemic, we’ve seen an increased use of digital cognitive behavioral therapy for insomnia (CBT-I) for patients who cannot initiate sleep, which has a very strong evidence base for effectiveness as a first-line intervention for many.
If a patient has an incomplete response to CBT-I, what might be pursued next? In our center, we have a low threshold for using low doses of benzodiazepines, such as lorazepam or clonazepam, because the majority of data do not support an increased risk of major congenital malformations even when used in the first trimester. It is quite common to see medicines such as newer nonbenzodiazepine sedative hypnotics such as Ambien CR (zolpidem) or Lunesta (eszopiclone) used by our colleagues in ob.gyn. The reproductive safety data on those medicines are particularly sparse, and they may have greater risk of cognitive side effects the next day, so we tend to avoid them.
Another sometimes-forgotten option to consider is using low doses of tricyclic antidepressants (i.e., 10-25 mg of nortriptyline at bedtime), with tricyclics having a 40-year history and at least one pooled analysis showing the absence of increased risk for major congenital malformations when used. This may be a very easy way of managing insomnia, with low-dose tricyclics having an anxiolytic effect as well.
Anxiety during pregnancy
The most common rise in symptoms during COVID-19 for women who are pregnant or post partum has been an increase in anxiety. Women present with a spectrum of concerns leading to anxiety symptoms in the context of the pandemic. Earlier on in the pandemic, concerns focused mostly on how to stay healthy, and how to mitigate risk and not catch SARS-CoV-2 during pregnancy, as well as the very complex issues that were playing out in real time as hospital systems were figuring out how to manage pregnant women in labor and to keep both them and staff safe. Over time, anxiety has shifted to still staying safe during the pandemic and the potential impact of SARS-CoV-2 infection on pregnancy outcomes. The No. 1 concern is what the implications of COVID-19 disease are on mother and child. New mothers also are anxious about how they will practically navigate life with a newborn in the postpartum setting.
Early on in the pandemic, some hospital systems severely limited who was in the room with a woman during labor, potentially impeding the wishes of women during delivery who would have wanted their loved ones and/or a doula present, as an example. With enhanced testing available now, protocols have since relaxed in many hospitals to allow partners – but not a team – to remain in the hospital during the labor process. Still, the prospect of delivering during a pandemic is undoubtedly a source of anxiety for some women.
This sort of anxiety, particularly in patients with preexisting anxiety disorders, can be particularly challenging. Fortunately, there has been a rapid increase over the last several years of digital apps to mitigate anxiety. While many of them have not been systematically studied, the data on biobehavioral intervention for anxiety is enormous, and this should be used as first-line treatment for patients with mild to moderate symptoms; so many women would prefer to avoid pharmacological intervention during pregnancy, if possible, to avoid fetal drug exposure. For patients who meet criteria for frank anxiety disorder, other nonpharmacologic interventions such as CBT have been shown to be effective.
Frequently, we see women who are experiencing levels of anxiety where nonpharmacological interventions have an incomplete response, and colleagues have asked about the safest way to treat these patients. As has been discussed in multiple previous columns, selective serotonin reuptake inhibitors (SSRIs) should be thought of sooner rather than later, particularly with medicines with good reproductive safety data such as sertraline, citalopram, or fluoxetine.
We also reported over 15 years ago that at least 30%-40% of women presenting with histories of recurrent major depression at the beginning of pregnancy had comorbid anxiety disorders, and that the use of benzodiazepines in that population in addition to SSRIs was exceedingly common, with doses of approximately 0.5-1.5 mg of clonazepam or lorazepam being standard fare. Again, this is very appropriate treatment to mitigate anxiety symptoms because now have enough data as a field that support the existence of adverse outcomes associated with untreated anxiety during pregnancy in terms of both adverse obstetric and neonatal outcomes, higher rates of preterm birth, and other obstetric complications. Hence, managing anxiety during pregnancy should be considered like managing a toxic exposure – the same way that one would be concerned about anything else that a pregnant woman could be exposed to.
Lastly, although no atypical antipsychotic has been approved for the treatment of anxiety, its use off label is extremely common. More and more data support the absence of a signal of teratogenicity across the family of molecules including atypical antipsychotics. Beyond potential use of atypical antipsychotics, at Virtual Rounds last week, a colleague asked about the use of gabapentin in a patient who was diagnosed with substance use disorder and who had inadvertently conceived on gabapentin, which was being used to treat both anxiety and insomnia. We have typically avoided the use of gabapentin during pregnancy because prospective data have been limited to relatively small case series and one report, with a total of exposures in roughly the 300 range.
However, our colleagues at the Harvard School of Public Health have recently published an article that looked at the United States Medicaid Analytic eXtract (MAX) dataset, which has been used to publish other articles addressing atypical antipsychotics, SSRIs, lithium, and pharmacovigilance investigations among other important topics. In this study, the database was used to look specifically at 4,642 pregnancies with gabapentin exposure relative to 1,744,447 unexposed pregnancies, without a significant finding for increased risk for major congenital malformations.
The question of an increased risk of cardiac malformations and of increased risk for obstetric complications are difficult to untangle from anxiety and depression, as they also are associated with those same outcomes. With that said, the analysis is a welcome addition to our knowledge base for a medicine used more widely to treat symptoms such as anxiety and insomnia in the general population, with a question mark around where it may fit into the algorithm during pregnancy.
In our center, gabapentin still would not be used as a first-line treatment for the management of anxiety or insomnia during pregnancy. But these new data still are reassuring for patients who come in, frequently with unplanned pregnancies. It is an important reminder to those of us taking care of patients during the pandemic to review use of contraception, because although data are unavailable specific to the period of the pandemic, what is clear is that, even prior to COVID-19, 50% of pregnancies in America were unplanned. Addressing issues of reliable use of contraception, particularly during the pandemic, is that much more important.
In this particular case, our clinician colleague in Virtual Rounds decided to continue gabapentin across pregnancy in the context of these reassuring data, but others may choose to discontinue or pursue some of the other treatment options noted above.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Since the start of the pandemic, we have been conducting an extra hour of Virtual Rounds at the Center for Women’s Mental Health. Virtual Rounds has been an opportunity to discuss cases around a spectrum of clinical management issues with respect to depression, bipolar disorder, and a spectrum of anxiety disorders like obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder. How to apply the calculus of risk-benefit decision-making around management of psychiatric disorder during pregnancy and the postpartum period has been the cornerstone of the work at our center for over 2 decades.
When we went virtual at our center in the early Spring, we decided to keep the format of our faculty rounds the way they have been for years and to sustain cohesiveness of our program during the pandemic. But we thought the needs of pregnant and postpartum women warranted being addressed in a context more specific to COVID-19, and also that reproductive psychiatrists and other clinicians could learn from each other about novel issues coming up for this group of patients during the pandemic. With that backdrop, Marlene Freeman, MD, and I founded “Virtual Rounds at the Center” to respond to queries from our colleagues across the country; we do this just after our own rounds on Wednesdays at 2:00 p.m.
As the pandemic has progressed, Virtual Rounds has blossomed into a virtual community on the Zoom platform, where social workers, psychologists, nurse prescribers, psychiatrists, and obstetricians discuss the needs of pregnant and postpartum women specific to COVID-19. Frequently, our discussions involve a review of the risks and benefits of treatment before, during, and after pregnancy.
Seemingly, week to week, more and more colleagues raise questions about the treatment of anxiety and insomnia during pregnancy and the postpartum period. I’ve spoken in previous columns about the enhanced use of telemedicine. Telemedicine not only facilitates efforts like Virtual Rounds and our ability to reach out to colleagues across the country and share cases, but also has allowed us to keep even closer tabs on the emotional well-being of our pregnant and postpartum women during COVID-19.
The question is not just about the effects of a medicine that a woman might take to treat anxiety or insomnia during pregnancy, but the experience of the pandemic per se, which we are measuring in multiple studies now using a variety of psychological instruments that patients complete. The pandemic is unequivocally taking a still unquantified toll on the mental health of Americans and potentially on the next generation to come.
Midcycle awakening during pregnancy
Complaints of insomnia and midcycle awakening during pregnancy are not new – it is the rule, rather than the exception for many pregnant women, particularly later in pregnancy. We have unequivocally seen a worsening of complaints of sleep disruption including insomnia and midcycle awakening during the pandemic that is greater than what we have seen previously. Both patients and colleagues have asked us the safest ways to manage it. One of the first things we consider when we hear about insomnia is whether it is part of an underlying mood disorder. While we see primary insomnia clinically, it really is important to remember that insomnia can be part and parcel of an underlying mood disorder.
With that in mind, what are the options? During the pandemic, we’ve seen an increased use of digital cognitive behavioral therapy for insomnia (CBT-I) for patients who cannot initiate sleep, which has a very strong evidence base for effectiveness as a first-line intervention for many.
If a patient has an incomplete response to CBT-I, what might be pursued next? In our center, we have a low threshold for using low doses of benzodiazepines, such as lorazepam or clonazepam, because the majority of data do not support an increased risk of major congenital malformations even when used in the first trimester. It is quite common to see medicines such as newer nonbenzodiazepine sedative hypnotics such as Ambien CR (zolpidem) or Lunesta (eszopiclone) used by our colleagues in ob.gyn. The reproductive safety data on those medicines are particularly sparse, and they may have greater risk of cognitive side effects the next day, so we tend to avoid them.
Another sometimes-forgotten option to consider is using low doses of tricyclic antidepressants (i.e., 10-25 mg of nortriptyline at bedtime), with tricyclics having a 40-year history and at least one pooled analysis showing the absence of increased risk for major congenital malformations when used. This may be a very easy way of managing insomnia, with low-dose tricyclics having an anxiolytic effect as well.
Anxiety during pregnancy
The most common rise in symptoms during COVID-19 for women who are pregnant or post partum has been an increase in anxiety. Women present with a spectrum of concerns leading to anxiety symptoms in the context of the pandemic. Earlier on in the pandemic, concerns focused mostly on how to stay healthy, and how to mitigate risk and not catch SARS-CoV-2 during pregnancy, as well as the very complex issues that were playing out in real time as hospital systems were figuring out how to manage pregnant women in labor and to keep both them and staff safe. Over time, anxiety has shifted to still staying safe during the pandemic and the potential impact of SARS-CoV-2 infection on pregnancy outcomes. The No. 1 concern is what the implications of COVID-19 disease are on mother and child. New mothers also are anxious about how they will practically navigate life with a newborn in the postpartum setting.
Early on in the pandemic, some hospital systems severely limited who was in the room with a woman during labor, potentially impeding the wishes of women during delivery who would have wanted their loved ones and/or a doula present, as an example. With enhanced testing available now, protocols have since relaxed in many hospitals to allow partners – but not a team – to remain in the hospital during the labor process. Still, the prospect of delivering during a pandemic is undoubtedly a source of anxiety for some women.
This sort of anxiety, particularly in patients with preexisting anxiety disorders, can be particularly challenging. Fortunately, there has been a rapid increase over the last several years of digital apps to mitigate anxiety. While many of them have not been systematically studied, the data on biobehavioral intervention for anxiety is enormous, and this should be used as first-line treatment for patients with mild to moderate symptoms; so many women would prefer to avoid pharmacological intervention during pregnancy, if possible, to avoid fetal drug exposure. For patients who meet criteria for frank anxiety disorder, other nonpharmacologic interventions such as CBT have been shown to be effective.
Frequently, we see women who are experiencing levels of anxiety where nonpharmacological interventions have an incomplete response, and colleagues have asked about the safest way to treat these patients. As has been discussed in multiple previous columns, selective serotonin reuptake inhibitors (SSRIs) should be thought of sooner rather than later, particularly with medicines with good reproductive safety data such as sertraline, citalopram, or fluoxetine.
We also reported over 15 years ago that at least 30%-40% of women presenting with histories of recurrent major depression at the beginning of pregnancy had comorbid anxiety disorders, and that the use of benzodiazepines in that population in addition to SSRIs was exceedingly common, with doses of approximately 0.5-1.5 mg of clonazepam or lorazepam being standard fare. Again, this is very appropriate treatment to mitigate anxiety symptoms because now have enough data as a field that support the existence of adverse outcomes associated with untreated anxiety during pregnancy in terms of both adverse obstetric and neonatal outcomes, higher rates of preterm birth, and other obstetric complications. Hence, managing anxiety during pregnancy should be considered like managing a toxic exposure – the same way that one would be concerned about anything else that a pregnant woman could be exposed to.
Lastly, although no atypical antipsychotic has been approved for the treatment of anxiety, its use off label is extremely common. More and more data support the absence of a signal of teratogenicity across the family of molecules including atypical antipsychotics. Beyond potential use of atypical antipsychotics, at Virtual Rounds last week, a colleague asked about the use of gabapentin in a patient who was diagnosed with substance use disorder and who had inadvertently conceived on gabapentin, which was being used to treat both anxiety and insomnia. We have typically avoided the use of gabapentin during pregnancy because prospective data have been limited to relatively small case series and one report, with a total of exposures in roughly the 300 range.
However, our colleagues at the Harvard School of Public Health have recently published an article that looked at the United States Medicaid Analytic eXtract (MAX) dataset, which has been used to publish other articles addressing atypical antipsychotics, SSRIs, lithium, and pharmacovigilance investigations among other important topics. In this study, the database was used to look specifically at 4,642 pregnancies with gabapentin exposure relative to 1,744,447 unexposed pregnancies, without a significant finding for increased risk for major congenital malformations.
The question of an increased risk of cardiac malformations and of increased risk for obstetric complications are difficult to untangle from anxiety and depression, as they also are associated with those same outcomes. With that said, the analysis is a welcome addition to our knowledge base for a medicine used more widely to treat symptoms such as anxiety and insomnia in the general population, with a question mark around where it may fit into the algorithm during pregnancy.
In our center, gabapentin still would not be used as a first-line treatment for the management of anxiety or insomnia during pregnancy. But these new data still are reassuring for patients who come in, frequently with unplanned pregnancies. It is an important reminder to those of us taking care of patients during the pandemic to review use of contraception, because although data are unavailable specific to the period of the pandemic, what is clear is that, even prior to COVID-19, 50% of pregnancies in America were unplanned. Addressing issues of reliable use of contraception, particularly during the pandemic, is that much more important.
In this particular case, our clinician colleague in Virtual Rounds decided to continue gabapentin across pregnancy in the context of these reassuring data, but others may choose to discontinue or pursue some of the other treatment options noted above.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].