User login
Consider risk for Barrett’s esophagus after bariatric surgery
Barrett’s esophagus occurred in nearly 12% of patients who underwent esophagogastroduodenoscopy after sleeve gastrectomy, but it was not associated with postoperative gastroesophageal reflux disease (GERD), based on data from 10 studies that totaled 680 adult patients.
Sleeve gastrectomy has become more popular in recent years as an effective strategy for patients with severe obesity, wrote Bashar J. Qumseya, MD, of the University of Florida, Gainesville, and colleagues. However, GERD is a common concern for patients undergoing sleeve gastrectomy and is the major risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus in the sleeve gastrectomy population has not been examined.
In a meta-analysis published in Gastrointestinal Endoscopy, the researchers reviewed 10 studies that totaled 680 patients who underwent esophagogastroduodenoscopy 6 months to 10 years after a sleeve gastrectomy procedure. The primary outcome was Barrett’s esophagus prevalence in sleeve gastrectomy patients, with the prevalence of erosive esophagitis and GERD at follow-up as secondary outcomes.
Overall, 54 patients developed Barrett’s esophagus, for a pooled prevalence of 11.6%, and all cases were nondysplastic and de novo. There was no significant association between Barrett’s esophagus and the presence of postoperative GERD, the researchers said (odds ratio, 1.74; P = .37).
However, the rate of erosive esophagitis increased by 86% in five studies with long-term follow-up and by 35% in two studies with short-term follow-up, which suggests an increased risk of 13% each year after sleeve gastrectomy, the researchers noted.
Besides the risk of Barrett’s esophagus after sleeve gastrectomy, “the risk of [erosive esophagitis] is also of significant interest and shares the same pathophysiology with [Barrett’s esophagus] and GERD,” they emphasized.
The study findings were limited by several factors including the small sample size and the focus on Barrett’s esophagus rather than erosive esophagitis or GERD as the primary outcome, the researchers noted. However, the results indicate that sleeve gastrectomy patients are at increased risk for Barrett’s esophagus, and larger studies are needed to better understand the pathophysiology. Furthermore, although there is some debate regarding the risk of GERD and erosive esophagitis after sleeve gastrectomy, the authors wrote that the data from their study showed a “consistent and substantial trend” toward more erosive esophagitis after sleeve gastrectomy.
“Gastroenterologists, primary care providers, and bariatric surgeons should be aware” of the data and should discuss the risks of sleeve gastrectomy with patients before the procedure, including the risks and benefits of postprocedure screening for Barrett’s esophagus, they concluded.
Consider surveillance for Barrett’s
The study is important because of the increased rates of GERD and potentially Barrett’s esophagus that have been noted after sleeve gastrectomy, Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Many of these studies have been small, and the findings of meta-analyses have been limited by high heterogeneity,” he noted. “With the rise in popularity of sleeve gastrectomy, it is important to accurately assess potential long-term complications.”
Dr. Ketwaroo said he was not surprised by the study findings given several reports of increased GERD after sleeve gastrectomy. “Given the accepted pathophysiology of Barrett’s esophagus, I anticipated increased risk of Barrett’s esophagus after sleeve gastrectomy as well.
“Clinicians should consider surveillance for Barrett’s esophagus after sleeve gastrectomy, and possible early proton pump inhibitor use for both GERD/erosive esophagitis and Barrett’s esophagus chemoprophylaxis. Patients with longer-segment or dysplastic Barrett’s esophagus prior to sleeve gastrectomy may have to be monitored more closely after surgery,” he said.
Dr. Ketwaroo noted that the study was limited by the small sample size, “with only approximately 50 patients with Barrett’s esophagus after surgery among 680 overall.” He emphasized that “we will need a much larger prospective study to confirm this finding. Additionally, I would want to explore if sleeve gastrectomy increases rate of progression of dysplasia in those who develop Barrett’s esophagus.”
The study received no outside funding. Lead author Dr. Qumseya had no financial conflicts to disclose. Dr. Ketwaroo serves on the GI & Hepatology News editorial advisory board.
Barrett’s esophagus occurred in nearly 12% of patients who underwent esophagogastroduodenoscopy after sleeve gastrectomy, but it was not associated with postoperative gastroesophageal reflux disease (GERD), based on data from 10 studies that totaled 680 adult patients.
Sleeve gastrectomy has become more popular in recent years as an effective strategy for patients with severe obesity, wrote Bashar J. Qumseya, MD, of the University of Florida, Gainesville, and colleagues. However, GERD is a common concern for patients undergoing sleeve gastrectomy and is the major risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus in the sleeve gastrectomy population has not been examined.
In a meta-analysis published in Gastrointestinal Endoscopy, the researchers reviewed 10 studies that totaled 680 patients who underwent esophagogastroduodenoscopy 6 months to 10 years after a sleeve gastrectomy procedure. The primary outcome was Barrett’s esophagus prevalence in sleeve gastrectomy patients, with the prevalence of erosive esophagitis and GERD at follow-up as secondary outcomes.
Overall, 54 patients developed Barrett’s esophagus, for a pooled prevalence of 11.6%, and all cases were nondysplastic and de novo. There was no significant association between Barrett’s esophagus and the presence of postoperative GERD, the researchers said (odds ratio, 1.74; P = .37).
However, the rate of erosive esophagitis increased by 86% in five studies with long-term follow-up and by 35% in two studies with short-term follow-up, which suggests an increased risk of 13% each year after sleeve gastrectomy, the researchers noted.
Besides the risk of Barrett’s esophagus after sleeve gastrectomy, “the risk of [erosive esophagitis] is also of significant interest and shares the same pathophysiology with [Barrett’s esophagus] and GERD,” they emphasized.
The study findings were limited by several factors including the small sample size and the focus on Barrett’s esophagus rather than erosive esophagitis or GERD as the primary outcome, the researchers noted. However, the results indicate that sleeve gastrectomy patients are at increased risk for Barrett’s esophagus, and larger studies are needed to better understand the pathophysiology. Furthermore, although there is some debate regarding the risk of GERD and erosive esophagitis after sleeve gastrectomy, the authors wrote that the data from their study showed a “consistent and substantial trend” toward more erosive esophagitis after sleeve gastrectomy.
“Gastroenterologists, primary care providers, and bariatric surgeons should be aware” of the data and should discuss the risks of sleeve gastrectomy with patients before the procedure, including the risks and benefits of postprocedure screening for Barrett’s esophagus, they concluded.
Consider surveillance for Barrett’s
The study is important because of the increased rates of GERD and potentially Barrett’s esophagus that have been noted after sleeve gastrectomy, Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Many of these studies have been small, and the findings of meta-analyses have been limited by high heterogeneity,” he noted. “With the rise in popularity of sleeve gastrectomy, it is important to accurately assess potential long-term complications.”
Dr. Ketwaroo said he was not surprised by the study findings given several reports of increased GERD after sleeve gastrectomy. “Given the accepted pathophysiology of Barrett’s esophagus, I anticipated increased risk of Barrett’s esophagus after sleeve gastrectomy as well.
“Clinicians should consider surveillance for Barrett’s esophagus after sleeve gastrectomy, and possible early proton pump inhibitor use for both GERD/erosive esophagitis and Barrett’s esophagus chemoprophylaxis. Patients with longer-segment or dysplastic Barrett’s esophagus prior to sleeve gastrectomy may have to be monitored more closely after surgery,” he said.
Dr. Ketwaroo noted that the study was limited by the small sample size, “with only approximately 50 patients with Barrett’s esophagus after surgery among 680 overall.” He emphasized that “we will need a much larger prospective study to confirm this finding. Additionally, I would want to explore if sleeve gastrectomy increases rate of progression of dysplasia in those who develop Barrett’s esophagus.”
The study received no outside funding. Lead author Dr. Qumseya had no financial conflicts to disclose. Dr. Ketwaroo serves on the GI & Hepatology News editorial advisory board.
Barrett’s esophagus occurred in nearly 12% of patients who underwent esophagogastroduodenoscopy after sleeve gastrectomy, but it was not associated with postoperative gastroesophageal reflux disease (GERD), based on data from 10 studies that totaled 680 adult patients.
Sleeve gastrectomy has become more popular in recent years as an effective strategy for patients with severe obesity, wrote Bashar J. Qumseya, MD, of the University of Florida, Gainesville, and colleagues. However, GERD is a common concern for patients undergoing sleeve gastrectomy and is the major risk factor for Barrett’s esophagus. However, the prevalence of Barrett’s esophagus in the sleeve gastrectomy population has not been examined.
In a meta-analysis published in Gastrointestinal Endoscopy, the researchers reviewed 10 studies that totaled 680 patients who underwent esophagogastroduodenoscopy 6 months to 10 years after a sleeve gastrectomy procedure. The primary outcome was Barrett’s esophagus prevalence in sleeve gastrectomy patients, with the prevalence of erosive esophagitis and GERD at follow-up as secondary outcomes.
Overall, 54 patients developed Barrett’s esophagus, for a pooled prevalence of 11.6%, and all cases were nondysplastic and de novo. There was no significant association between Barrett’s esophagus and the presence of postoperative GERD, the researchers said (odds ratio, 1.74; P = .37).
However, the rate of erosive esophagitis increased by 86% in five studies with long-term follow-up and by 35% in two studies with short-term follow-up, which suggests an increased risk of 13% each year after sleeve gastrectomy, the researchers noted.
Besides the risk of Barrett’s esophagus after sleeve gastrectomy, “the risk of [erosive esophagitis] is also of significant interest and shares the same pathophysiology with [Barrett’s esophagus] and GERD,” they emphasized.
The study findings were limited by several factors including the small sample size and the focus on Barrett’s esophagus rather than erosive esophagitis or GERD as the primary outcome, the researchers noted. However, the results indicate that sleeve gastrectomy patients are at increased risk for Barrett’s esophagus, and larger studies are needed to better understand the pathophysiology. Furthermore, although there is some debate regarding the risk of GERD and erosive esophagitis after sleeve gastrectomy, the authors wrote that the data from their study showed a “consistent and substantial trend” toward more erosive esophagitis after sleeve gastrectomy.
“Gastroenterologists, primary care providers, and bariatric surgeons should be aware” of the data and should discuss the risks of sleeve gastrectomy with patients before the procedure, including the risks and benefits of postprocedure screening for Barrett’s esophagus, they concluded.
Consider surveillance for Barrett’s
The study is important because of the increased rates of GERD and potentially Barrett’s esophagus that have been noted after sleeve gastrectomy, Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Many of these studies have been small, and the findings of meta-analyses have been limited by high heterogeneity,” he noted. “With the rise in popularity of sleeve gastrectomy, it is important to accurately assess potential long-term complications.”
Dr. Ketwaroo said he was not surprised by the study findings given several reports of increased GERD after sleeve gastrectomy. “Given the accepted pathophysiology of Barrett’s esophagus, I anticipated increased risk of Barrett’s esophagus after sleeve gastrectomy as well.
“Clinicians should consider surveillance for Barrett’s esophagus after sleeve gastrectomy, and possible early proton pump inhibitor use for both GERD/erosive esophagitis and Barrett’s esophagus chemoprophylaxis. Patients with longer-segment or dysplastic Barrett’s esophagus prior to sleeve gastrectomy may have to be monitored more closely after surgery,” he said.
Dr. Ketwaroo noted that the study was limited by the small sample size, “with only approximately 50 patients with Barrett’s esophagus after surgery among 680 overall.” He emphasized that “we will need a much larger prospective study to confirm this finding. Additionally, I would want to explore if sleeve gastrectomy increases rate of progression of dysplasia in those who develop Barrett’s esophagus.”
The study received no outside funding. Lead author Dr. Qumseya had no financial conflicts to disclose. Dr. Ketwaroo serves on the GI & Hepatology News editorial advisory board.
FROM GASTROINTESTINAL ENDOSCOPY
Bariatric surgery gives 10-year cure for some advanced diabetes
A small, single-center randomized trial of patients with obesity and advanced type 2 diabetes, defined as diabetes for ≥ 5 years and A1c ≥ 7%, found that a quarter to a half of patients who had metabolic surgery had diabetes remission (cure) that lasted 5-9 years.
That is, of the 60 randomized patients, 50% who had biliopancreatic diversion and 25% who had Roux-en-Y gastric bypass – but none who had received current medical therapy – still had diabetes remission a decade later.
Until now, there had only been 5-year follow-up data from this and similar trials, Geltrude Mingrone, MD, PhD, and colleagues noted in the study published online Jan. 23 in The Lancet.
These results provide “the most robust scientific evidence yet that full-blown type 2 diabetes is a curable disease, not inevitably progressive, and irreversible,” senior author Francesco Rubino, MD, chair of bariatric and metabolic surgery at King’s College London, said in a statement from his institution.
“The results of this trial will make a noticeable difference in the field and convince even the most skeptical of clinicians about the role of metabolic surgery as part of optimal care for their patients with difficult to control type 2 diabetes,” predicted two editorialists.
Alexander D. Miras, PhD, section of metabolism, digestion, and reproduction, Imperial College London, and Carel le Roux, MBChB, PhD, of the Diabetes Complications Research Centre, University College Dublin, penned the accompanying commentary.
Patients who had metabolic surgery also had greater weight loss, reduced medication use, lower cardiovascular risk, better quality of life, and a lower incidence of diabetes-related complications compared with those who received medical therapy.
“Clinicians and policymakers should ensure that metabolic surgery is appropriately considered in the management of patients with obesity and type 2 diabetes,” advised Dr. Mingrone of King’s College London and the Catholic University of Rome, and colleagues.
“Reassuring results, will make a difference in the field”
“It is reassuring that we now have 10-year data showing greater efficacy of metabolic surgery than conventional medical therapy,” Dr. Miras and Dr. le Roux wrote in their commentary.
There were no unexpected risks associated with surgery, they noted, and the findings are consistent with those of 12 other randomized controlled trials in the past 12 years.
“New generations of diabetologists are now more open to the use of metabolic surgery for patients with suboptimal responses to medical treatments,” they wrote, rather than endlessly intensifying insulin and blaming poor response on poor compliance.
And Dr. Miras and Dr. le Roux “eagerly await” 10-year data from the 150-patient STAMPEDE trial – which is examining sleeve gastrectomy, currently the most widely performed bariatric procedure, as well as Roux-en-Y gastric bypass and medical therapy – following the 5-year results published in 2017.
Diabetes for at least 5 years, mid 40s, half on insulin
Dr. Mingrone and colleagues previously reported 5-year findings from the 60 patients with obesity and advanced diabetes who were seen in a single center in Rome and randomized to three treatments (20 in each group) in 2009-2011.
Biliopancreatic diversion “remains infrequently performed but is still considered the best operation for glycemic control,” the researchers noted.
The primary endpoint was diabetes remission at 2 years (fasting plasma glucose < 100 mg/dL [5.6 mmol/L] and A1c < 6.5%) without the need for ongoing pharmacological treatment for at least 1 year.
Patients were a mean age of 44 years and had a mean body mass index of 44 kg/m2. About half were men. They had diabetes for a mean of 5.8 years and an average A1c of 8.6%. About half were taking insulin.
Patient retention rate was high (95%) and trial outcomes were assessed by nonsurgeons.
At 10 years, patients’ mean A1c had dropped to 6.4%, 6.7%, and 7.6%, in the biliopancreatic diversion, Roux-en-Y gastric bypass, and medical therapy groups, respectively; only 2.5% of patients in the surgery groups, versus 53% in the medical therapy group, required insulin.
At study end, patients in the surgery groups had lost about 29% of their initial weight versus a weight loss of 4.2% in the medical therapy group.
First 2 years after surgery is key
“We also learnt that patients who do not go into remission after 2 years are very unlikely to ever do so,” Dr. Miras and Dr. le Roux observed, which “might help us to intensify modern and potent glucose-lowering therapies like SGLT2 inhibitors and GLP-1 receptor agonists earlier after metabolic surgery.”
Ten of 19 patients (53%) in the biliopancreatic diversion group and 10 of 15 patients (67%) in the Roux-en-Y gastric bypass group who had diabetes remission at 2 years had a diabetes relapse, but at 10 years, they all had adequate glycemic control (mean A1c 6.7%), despite drastically reduced use of diabetes medications.
The two patients who crossed over to surgery from the medical therapy group had postoperative diabetes remission, which was maintained at 10 years in one patient.
Better risk-to-benefit ratio with Roux-en-y gastric bypass
No patient in the medical therapy group had a serious adverse event, but one patient in each surgery group had deep vein thrombosis or pulmonary embolism, and one patient in the biliopancreatic diversion group had an episode of atrial fibrillation. There were no late surgical complications.
Iron deficiency and mild osteopenia occurred in both surgical groups, but were more common in the biliopancreatic diversion group. And osteoporosis, transient nyctalopia (night blindness) due to vitamin A deficiency, and kidney stones were observed only with biliopancreatic diversion.
This suggests that despite the greater antidiabetic potential of biliopancreatic diversion, Roux-en-Y gastric bypass might have a more favorable risk-to-benefit profile as a standard surgical option for the treatment of type 2 diabetes, Dr. Mingrone and colleagues concluded.
The authors and Dr. Miras have reported no relevant financial relationships. Dr. le Roux has reported receiving funding from the Science Foundation Ireland, the Health Research Board, and the Irish Research Council for type 2 diabetes research, and serves on several advisory boards outside of the scope of the current study.
A version of this article first appeared on Medscape.com.
A small, single-center randomized trial of patients with obesity and advanced type 2 diabetes, defined as diabetes for ≥ 5 years and A1c ≥ 7%, found that a quarter to a half of patients who had metabolic surgery had diabetes remission (cure) that lasted 5-9 years.
That is, of the 60 randomized patients, 50% who had biliopancreatic diversion and 25% who had Roux-en-Y gastric bypass – but none who had received current medical therapy – still had diabetes remission a decade later.
Until now, there had only been 5-year follow-up data from this and similar trials, Geltrude Mingrone, MD, PhD, and colleagues noted in the study published online Jan. 23 in The Lancet.
These results provide “the most robust scientific evidence yet that full-blown type 2 diabetes is a curable disease, not inevitably progressive, and irreversible,” senior author Francesco Rubino, MD, chair of bariatric and metabolic surgery at King’s College London, said in a statement from his institution.
“The results of this trial will make a noticeable difference in the field and convince even the most skeptical of clinicians about the role of metabolic surgery as part of optimal care for their patients with difficult to control type 2 diabetes,” predicted two editorialists.
Alexander D. Miras, PhD, section of metabolism, digestion, and reproduction, Imperial College London, and Carel le Roux, MBChB, PhD, of the Diabetes Complications Research Centre, University College Dublin, penned the accompanying commentary.
Patients who had metabolic surgery also had greater weight loss, reduced medication use, lower cardiovascular risk, better quality of life, and a lower incidence of diabetes-related complications compared with those who received medical therapy.
“Clinicians and policymakers should ensure that metabolic surgery is appropriately considered in the management of patients with obesity and type 2 diabetes,” advised Dr. Mingrone of King’s College London and the Catholic University of Rome, and colleagues.
“Reassuring results, will make a difference in the field”
“It is reassuring that we now have 10-year data showing greater efficacy of metabolic surgery than conventional medical therapy,” Dr. Miras and Dr. le Roux wrote in their commentary.
There were no unexpected risks associated with surgery, they noted, and the findings are consistent with those of 12 other randomized controlled trials in the past 12 years.
“New generations of diabetologists are now more open to the use of metabolic surgery for patients with suboptimal responses to medical treatments,” they wrote, rather than endlessly intensifying insulin and blaming poor response on poor compliance.
And Dr. Miras and Dr. le Roux “eagerly await” 10-year data from the 150-patient STAMPEDE trial – which is examining sleeve gastrectomy, currently the most widely performed bariatric procedure, as well as Roux-en-Y gastric bypass and medical therapy – following the 5-year results published in 2017.
Diabetes for at least 5 years, mid 40s, half on insulin
Dr. Mingrone and colleagues previously reported 5-year findings from the 60 patients with obesity and advanced diabetes who were seen in a single center in Rome and randomized to three treatments (20 in each group) in 2009-2011.
Biliopancreatic diversion “remains infrequently performed but is still considered the best operation for glycemic control,” the researchers noted.
The primary endpoint was diabetes remission at 2 years (fasting plasma glucose < 100 mg/dL [5.6 mmol/L] and A1c < 6.5%) without the need for ongoing pharmacological treatment for at least 1 year.
Patients were a mean age of 44 years and had a mean body mass index of 44 kg/m2. About half were men. They had diabetes for a mean of 5.8 years and an average A1c of 8.6%. About half were taking insulin.
Patient retention rate was high (95%) and trial outcomes were assessed by nonsurgeons.
At 10 years, patients’ mean A1c had dropped to 6.4%, 6.7%, and 7.6%, in the biliopancreatic diversion, Roux-en-Y gastric bypass, and medical therapy groups, respectively; only 2.5% of patients in the surgery groups, versus 53% in the medical therapy group, required insulin.
At study end, patients in the surgery groups had lost about 29% of their initial weight versus a weight loss of 4.2% in the medical therapy group.
First 2 years after surgery is key
“We also learnt that patients who do not go into remission after 2 years are very unlikely to ever do so,” Dr. Miras and Dr. le Roux observed, which “might help us to intensify modern and potent glucose-lowering therapies like SGLT2 inhibitors and GLP-1 receptor agonists earlier after metabolic surgery.”
Ten of 19 patients (53%) in the biliopancreatic diversion group and 10 of 15 patients (67%) in the Roux-en-Y gastric bypass group who had diabetes remission at 2 years had a diabetes relapse, but at 10 years, they all had adequate glycemic control (mean A1c 6.7%), despite drastically reduced use of diabetes medications.
The two patients who crossed over to surgery from the medical therapy group had postoperative diabetes remission, which was maintained at 10 years in one patient.
Better risk-to-benefit ratio with Roux-en-y gastric bypass
No patient in the medical therapy group had a serious adverse event, but one patient in each surgery group had deep vein thrombosis or pulmonary embolism, and one patient in the biliopancreatic diversion group had an episode of atrial fibrillation. There were no late surgical complications.
Iron deficiency and mild osteopenia occurred in both surgical groups, but were more common in the biliopancreatic diversion group. And osteoporosis, transient nyctalopia (night blindness) due to vitamin A deficiency, and kidney stones were observed only with biliopancreatic diversion.
This suggests that despite the greater antidiabetic potential of biliopancreatic diversion, Roux-en-Y gastric bypass might have a more favorable risk-to-benefit profile as a standard surgical option for the treatment of type 2 diabetes, Dr. Mingrone and colleagues concluded.
The authors and Dr. Miras have reported no relevant financial relationships. Dr. le Roux has reported receiving funding from the Science Foundation Ireland, the Health Research Board, and the Irish Research Council for type 2 diabetes research, and serves on several advisory boards outside of the scope of the current study.
A version of this article first appeared on Medscape.com.
A small, single-center randomized trial of patients with obesity and advanced type 2 diabetes, defined as diabetes for ≥ 5 years and A1c ≥ 7%, found that a quarter to a half of patients who had metabolic surgery had diabetes remission (cure) that lasted 5-9 years.
That is, of the 60 randomized patients, 50% who had biliopancreatic diversion and 25% who had Roux-en-Y gastric bypass – but none who had received current medical therapy – still had diabetes remission a decade later.
Until now, there had only been 5-year follow-up data from this and similar trials, Geltrude Mingrone, MD, PhD, and colleagues noted in the study published online Jan. 23 in The Lancet.
These results provide “the most robust scientific evidence yet that full-blown type 2 diabetes is a curable disease, not inevitably progressive, and irreversible,” senior author Francesco Rubino, MD, chair of bariatric and metabolic surgery at King’s College London, said in a statement from his institution.
“The results of this trial will make a noticeable difference in the field and convince even the most skeptical of clinicians about the role of metabolic surgery as part of optimal care for their patients with difficult to control type 2 diabetes,” predicted two editorialists.
Alexander D. Miras, PhD, section of metabolism, digestion, and reproduction, Imperial College London, and Carel le Roux, MBChB, PhD, of the Diabetes Complications Research Centre, University College Dublin, penned the accompanying commentary.
Patients who had metabolic surgery also had greater weight loss, reduced medication use, lower cardiovascular risk, better quality of life, and a lower incidence of diabetes-related complications compared with those who received medical therapy.
“Clinicians and policymakers should ensure that metabolic surgery is appropriately considered in the management of patients with obesity and type 2 diabetes,” advised Dr. Mingrone of King’s College London and the Catholic University of Rome, and colleagues.
“Reassuring results, will make a difference in the field”
“It is reassuring that we now have 10-year data showing greater efficacy of metabolic surgery than conventional medical therapy,” Dr. Miras and Dr. le Roux wrote in their commentary.
There were no unexpected risks associated with surgery, they noted, and the findings are consistent with those of 12 other randomized controlled trials in the past 12 years.
“New generations of diabetologists are now more open to the use of metabolic surgery for patients with suboptimal responses to medical treatments,” they wrote, rather than endlessly intensifying insulin and blaming poor response on poor compliance.
And Dr. Miras and Dr. le Roux “eagerly await” 10-year data from the 150-patient STAMPEDE trial – which is examining sleeve gastrectomy, currently the most widely performed bariatric procedure, as well as Roux-en-Y gastric bypass and medical therapy – following the 5-year results published in 2017.
Diabetes for at least 5 years, mid 40s, half on insulin
Dr. Mingrone and colleagues previously reported 5-year findings from the 60 patients with obesity and advanced diabetes who were seen in a single center in Rome and randomized to three treatments (20 in each group) in 2009-2011.
Biliopancreatic diversion “remains infrequently performed but is still considered the best operation for glycemic control,” the researchers noted.
The primary endpoint was diabetes remission at 2 years (fasting plasma glucose < 100 mg/dL [5.6 mmol/L] and A1c < 6.5%) without the need for ongoing pharmacological treatment for at least 1 year.
Patients were a mean age of 44 years and had a mean body mass index of 44 kg/m2. About half were men. They had diabetes for a mean of 5.8 years and an average A1c of 8.6%. About half were taking insulin.
Patient retention rate was high (95%) and trial outcomes were assessed by nonsurgeons.
At 10 years, patients’ mean A1c had dropped to 6.4%, 6.7%, and 7.6%, in the biliopancreatic diversion, Roux-en-Y gastric bypass, and medical therapy groups, respectively; only 2.5% of patients in the surgery groups, versus 53% in the medical therapy group, required insulin.
At study end, patients in the surgery groups had lost about 29% of their initial weight versus a weight loss of 4.2% in the medical therapy group.
First 2 years after surgery is key
“We also learnt that patients who do not go into remission after 2 years are very unlikely to ever do so,” Dr. Miras and Dr. le Roux observed, which “might help us to intensify modern and potent glucose-lowering therapies like SGLT2 inhibitors and GLP-1 receptor agonists earlier after metabolic surgery.”
Ten of 19 patients (53%) in the biliopancreatic diversion group and 10 of 15 patients (67%) in the Roux-en-Y gastric bypass group who had diabetes remission at 2 years had a diabetes relapse, but at 10 years, they all had adequate glycemic control (mean A1c 6.7%), despite drastically reduced use of diabetes medications.
The two patients who crossed over to surgery from the medical therapy group had postoperative diabetes remission, which was maintained at 10 years in one patient.
Better risk-to-benefit ratio with Roux-en-y gastric bypass
No patient in the medical therapy group had a serious adverse event, but one patient in each surgery group had deep vein thrombosis or pulmonary embolism, and one patient in the biliopancreatic diversion group had an episode of atrial fibrillation. There were no late surgical complications.
Iron deficiency and mild osteopenia occurred in both surgical groups, but were more common in the biliopancreatic diversion group. And osteoporosis, transient nyctalopia (night blindness) due to vitamin A deficiency, and kidney stones were observed only with biliopancreatic diversion.
This suggests that despite the greater antidiabetic potential of biliopancreatic diversion, Roux-en-Y gastric bypass might have a more favorable risk-to-benefit profile as a standard surgical option for the treatment of type 2 diabetes, Dr. Mingrone and colleagues concluded.
The authors and Dr. Miras have reported no relevant financial relationships. Dr. le Roux has reported receiving funding from the Science Foundation Ireland, the Health Research Board, and the Irish Research Council for type 2 diabetes research, and serves on several advisory boards outside of the scope of the current study.
A version of this article first appeared on Medscape.com.
Bariatric surgery might reduce severity of COVID-19 infection
and the disease was less severe than among COVID patients with obesity who had not undergone the surgery, a new retrospective analysis shows.
The research was published in Surgery for Obesity and Related Diseases.
Because obesity is a well-known risk factor for poor COVID-19 outcomes, Ali Aminian, MD, Bariatric and Metabolic Institute, Cleveland Clinic, and colleagues decided to study whether weight-loss surgery had a bearing on outcomes of patients with COVID-19.
They matched 33 COVID-19 patients who had undergone metabolic surgery with 330 control patients with obesity who were infected with the virus during the first wave of the pandemic.
Surgery was associated with a 69% reduction in the risk of being hospitalized as a result of COVID-19. None of the surgery patients required intensive care, mechanical ventilation, or dialysis, and none died.
“Patients after bariatric surgery become significantly healthier and can fight the virus better,” said Dr. Aminian in a statement from his institution. “If confirmed by future studies, this can be added to the long list of health benefits of bariatric surgery.”
COVID-19 is a wake-up call for the consequences of obesity
Dr. Aminian said in an interview that COVID-19 is a “wake-up call to show the public and health care professionals that obesity is a major health problem and has multiple health consequences.”
More than 300 articles in the literature show that obesity is a major risk factor for poor outcomes following COVID-19 infection. Dr. Aminian said the pandemic has “improved public awareness about the consequences of obesity.”
Compared with last year at his institution, the intake of new patients “who would like to join a program to have surgery or have some tools to help them to lose weight is almost double,” he noted.
Furthermore, referrals to their unit from primary care physicians, as well as from endocrinologists and cardiologists, for bariatric surgery nearly doubled in recent months.
Although the unit had to stop all bariatric surgeries for around 6 weeks in April because of COVID-19, it has performed the same number of procedures this year as in 2019 and 2018.
Because of the recent surge in COVID cases in Ohio, bariatric procedures are once again on hold. “Elective operations that require hospital beds after surgery have been paused to provide beds for patients who have COVID-19,” he explained.
Small sample size, study should be repeated
For their study, Dr. Aminian and colleagues examined the records of 4,365 patients at the Cleveland Clinic Health System who tested positive for the virus between March 8 and July 22, 2020.
Of these, 1,003 had a body mass index of at least 35 mg/kg2; 482 had a BMI of at least 40. The team identified 33 patients who had previously undergone metabolic surgery, comprising 20 sleeve gastrectomies and 13 Roux-en-Y gastric bypasses.
The surgical patients were propensity matched in a 1:10 ratio with nonsurgical control patients with a BMI of at least 40. The patients were matched on the basis of age, sex, ethnicity, location, smoking status, and history of chronic obstructive pulmonary disease.
The mean BMI of surgical patients was 49.1 before their procedure. It fell to 37.2 by the time they tested positive for COVID-19. This compares with an average of 46.7 in the control group at the time they tested positive for the virus.
The team found that 18.2% of metabolic surgery patients were admitted to hospital versus 42.1% of control patients (P = .013).
Moreover, metabolic surgery patients did not require admission to the intensive care unit, nor did they require mechanical ventilation or dialysis, and none died. This compares with 13.0% (P = .021), 6.7% (P = .24), 1.5%, and 2.4%, respectively, of patients in the control group.
Multivariate analysis indicated that prior metabolic surgery was associated with lower hospital admission, at an odds ratio of 0.31 (P = .028), in comparison with control patients with obesity.
Acknowledging the limited sample size of their study, the team wrote: “As this study reflects findings early in the course of the pandemic, it will be of interest to repeat this study with larger data sets and later in the course of the pandemic.”
Continue as many aspects of obesity management as possible during pandemic
Dr. Aminian underlined that, for him, the take-home message from the study is that health care professionals should “ideally” continue all aspects of obesity management during the pandemic, including “medical management, behavioral therapy, lifestyle changes, and access to bariatric surgery.”
This is despite the fact that insurance coverage for bariatric surgery has “always been a challenge for many patients, since many insurance plans do not cover” bariatric procedures, he noted.
In July, the American Society for Metabolic and Bariatric Surgery issued a statement declaring that obesity surgery should not be considered an elective procedure and should be resumed as soon as it’s safe to do so during any resurgence of the COVID-19 pandemic.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and the disease was less severe than among COVID patients with obesity who had not undergone the surgery, a new retrospective analysis shows.
The research was published in Surgery for Obesity and Related Diseases.
Because obesity is a well-known risk factor for poor COVID-19 outcomes, Ali Aminian, MD, Bariatric and Metabolic Institute, Cleveland Clinic, and colleagues decided to study whether weight-loss surgery had a bearing on outcomes of patients with COVID-19.
They matched 33 COVID-19 patients who had undergone metabolic surgery with 330 control patients with obesity who were infected with the virus during the first wave of the pandemic.
Surgery was associated with a 69% reduction in the risk of being hospitalized as a result of COVID-19. None of the surgery patients required intensive care, mechanical ventilation, or dialysis, and none died.
“Patients after bariatric surgery become significantly healthier and can fight the virus better,” said Dr. Aminian in a statement from his institution. “If confirmed by future studies, this can be added to the long list of health benefits of bariatric surgery.”
COVID-19 is a wake-up call for the consequences of obesity
Dr. Aminian said in an interview that COVID-19 is a “wake-up call to show the public and health care professionals that obesity is a major health problem and has multiple health consequences.”
More than 300 articles in the literature show that obesity is a major risk factor for poor outcomes following COVID-19 infection. Dr. Aminian said the pandemic has “improved public awareness about the consequences of obesity.”
Compared with last year at his institution, the intake of new patients “who would like to join a program to have surgery or have some tools to help them to lose weight is almost double,” he noted.
Furthermore, referrals to their unit from primary care physicians, as well as from endocrinologists and cardiologists, for bariatric surgery nearly doubled in recent months.
Although the unit had to stop all bariatric surgeries for around 6 weeks in April because of COVID-19, it has performed the same number of procedures this year as in 2019 and 2018.
Because of the recent surge in COVID cases in Ohio, bariatric procedures are once again on hold. “Elective operations that require hospital beds after surgery have been paused to provide beds for patients who have COVID-19,” he explained.
Small sample size, study should be repeated
For their study, Dr. Aminian and colleagues examined the records of 4,365 patients at the Cleveland Clinic Health System who tested positive for the virus between March 8 and July 22, 2020.
Of these, 1,003 had a body mass index of at least 35 mg/kg2; 482 had a BMI of at least 40. The team identified 33 patients who had previously undergone metabolic surgery, comprising 20 sleeve gastrectomies and 13 Roux-en-Y gastric bypasses.
The surgical patients were propensity matched in a 1:10 ratio with nonsurgical control patients with a BMI of at least 40. The patients were matched on the basis of age, sex, ethnicity, location, smoking status, and history of chronic obstructive pulmonary disease.
The mean BMI of surgical patients was 49.1 before their procedure. It fell to 37.2 by the time they tested positive for COVID-19. This compares with an average of 46.7 in the control group at the time they tested positive for the virus.
The team found that 18.2% of metabolic surgery patients were admitted to hospital versus 42.1% of control patients (P = .013).
Moreover, metabolic surgery patients did not require admission to the intensive care unit, nor did they require mechanical ventilation or dialysis, and none died. This compares with 13.0% (P = .021), 6.7% (P = .24), 1.5%, and 2.4%, respectively, of patients in the control group.
Multivariate analysis indicated that prior metabolic surgery was associated with lower hospital admission, at an odds ratio of 0.31 (P = .028), in comparison with control patients with obesity.
Acknowledging the limited sample size of their study, the team wrote: “As this study reflects findings early in the course of the pandemic, it will be of interest to repeat this study with larger data sets and later in the course of the pandemic.”
Continue as many aspects of obesity management as possible during pandemic
Dr. Aminian underlined that, for him, the take-home message from the study is that health care professionals should “ideally” continue all aspects of obesity management during the pandemic, including “medical management, behavioral therapy, lifestyle changes, and access to bariatric surgery.”
This is despite the fact that insurance coverage for bariatric surgery has “always been a challenge for many patients, since many insurance plans do not cover” bariatric procedures, he noted.
In July, the American Society for Metabolic and Bariatric Surgery issued a statement declaring that obesity surgery should not be considered an elective procedure and should be resumed as soon as it’s safe to do so during any resurgence of the COVID-19 pandemic.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and the disease was less severe than among COVID patients with obesity who had not undergone the surgery, a new retrospective analysis shows.
The research was published in Surgery for Obesity and Related Diseases.
Because obesity is a well-known risk factor for poor COVID-19 outcomes, Ali Aminian, MD, Bariatric and Metabolic Institute, Cleveland Clinic, and colleagues decided to study whether weight-loss surgery had a bearing on outcomes of patients with COVID-19.
They matched 33 COVID-19 patients who had undergone metabolic surgery with 330 control patients with obesity who were infected with the virus during the first wave of the pandemic.
Surgery was associated with a 69% reduction in the risk of being hospitalized as a result of COVID-19. None of the surgery patients required intensive care, mechanical ventilation, or dialysis, and none died.
“Patients after bariatric surgery become significantly healthier and can fight the virus better,” said Dr. Aminian in a statement from his institution. “If confirmed by future studies, this can be added to the long list of health benefits of bariatric surgery.”
COVID-19 is a wake-up call for the consequences of obesity
Dr. Aminian said in an interview that COVID-19 is a “wake-up call to show the public and health care professionals that obesity is a major health problem and has multiple health consequences.”
More than 300 articles in the literature show that obesity is a major risk factor for poor outcomes following COVID-19 infection. Dr. Aminian said the pandemic has “improved public awareness about the consequences of obesity.”
Compared with last year at his institution, the intake of new patients “who would like to join a program to have surgery or have some tools to help them to lose weight is almost double,” he noted.
Furthermore, referrals to their unit from primary care physicians, as well as from endocrinologists and cardiologists, for bariatric surgery nearly doubled in recent months.
Although the unit had to stop all bariatric surgeries for around 6 weeks in April because of COVID-19, it has performed the same number of procedures this year as in 2019 and 2018.
Because of the recent surge in COVID cases in Ohio, bariatric procedures are once again on hold. “Elective operations that require hospital beds after surgery have been paused to provide beds for patients who have COVID-19,” he explained.
Small sample size, study should be repeated
For their study, Dr. Aminian and colleagues examined the records of 4,365 patients at the Cleveland Clinic Health System who tested positive for the virus between March 8 and July 22, 2020.
Of these, 1,003 had a body mass index of at least 35 mg/kg2; 482 had a BMI of at least 40. The team identified 33 patients who had previously undergone metabolic surgery, comprising 20 sleeve gastrectomies and 13 Roux-en-Y gastric bypasses.
The surgical patients were propensity matched in a 1:10 ratio with nonsurgical control patients with a BMI of at least 40. The patients were matched on the basis of age, sex, ethnicity, location, smoking status, and history of chronic obstructive pulmonary disease.
The mean BMI of surgical patients was 49.1 before their procedure. It fell to 37.2 by the time they tested positive for COVID-19. This compares with an average of 46.7 in the control group at the time they tested positive for the virus.
The team found that 18.2% of metabolic surgery patients were admitted to hospital versus 42.1% of control patients (P = .013).
Moreover, metabolic surgery patients did not require admission to the intensive care unit, nor did they require mechanical ventilation or dialysis, and none died. This compares with 13.0% (P = .021), 6.7% (P = .24), 1.5%, and 2.4%, respectively, of patients in the control group.
Multivariate analysis indicated that prior metabolic surgery was associated with lower hospital admission, at an odds ratio of 0.31 (P = .028), in comparison with control patients with obesity.
Acknowledging the limited sample size of their study, the team wrote: “As this study reflects findings early in the course of the pandemic, it will be of interest to repeat this study with larger data sets and later in the course of the pandemic.”
Continue as many aspects of obesity management as possible during pandemic
Dr. Aminian underlined that, for him, the take-home message from the study is that health care professionals should “ideally” continue all aspects of obesity management during the pandemic, including “medical management, behavioral therapy, lifestyle changes, and access to bariatric surgery.”
This is despite the fact that insurance coverage for bariatric surgery has “always been a challenge for many patients, since many insurance plans do not cover” bariatric procedures, he noted.
In July, the American Society for Metabolic and Bariatric Surgery issued a statement declaring that obesity surgery should not be considered an elective procedure and should be resumed as soon as it’s safe to do so during any resurgence of the COVID-19 pandemic.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Disordered eating’ drops after teens undergo bariatric surgery
Kristina M. Decker, PhD, a postdoctoral fellow at Cincinnati Children’s Hospital Medical Center, presented these findings during the virtual ObesityWeek 2020.
Dr. Decker and associates examined rates of disordered eating in more than 200 adolescents (aged 13-18 years) who were severely obese, of whom 141 underwent bariatric surgery and the remainder did not.
At baseline (presurgery), the teens in both groups had rates of disordered eating ranging from 11% to 50%, with higher rates in those who went on to have bariatric surgery.
Six years later, rates of disordered eating were much lower in those who had bariatric surgery.
The data nevertheless “underscore that young adults with persistent severe obesity are at high risk for poor health and well-being,” Dr. Decker said in an interview.
“This means disordered eating behaviors should be closely monitored” in all such patients, both those who undergo surgery and those who don’t, she stressed.
Robust findings because of long follow-up and controls
The findings are not unexpected, based on adult bariatric literature, but are “novel because of the age of the patients,” senior author Margaret H. Zeller, PhD, Cincinnati Children’s Hospital Medical Center and professor at the University of Cincinnati, added.
In a comment comment, psychologist Kajsa Järvholm, PhD, of the Childhood Obesity Unit at Skåne University Hospital, Malmö̈, Sweden, who has published related work, said that this is “a needed study.”
Notably, it had “long-term follow-up and a control group,” and it “confirms that adolescents are in better control of their eating after surgery.”
However, an important additional takeaway for clinicians is that “disordered eating is associated with other mental health problems and self-worth. Clinicians treating obesity must address problems related to eating disorders to improve outcomes and well-being,” she stressed.
How does bariatric surgery impact overeating, binge eating, in teens?
“For teens with severe obesity, metabolic and bariatric surgery is the most effective treatment for improved cardiometabolic functioning, weight loss, and improved quality of life,” Dr. Decker stressed.
However, pre- and postsurgical disordered eating behaviors have been associated with a lower percentage change in body mass index (BMI), although this has not been well studied.
To investigate how disordered eating is affected by bariatric surgery in adolescents with severe obesity, researchers used data from Teen-LABS, which enrolled 242 participants aged 19 years and under who mainly underwent Roux-en-Y gastric bypass (67%) or sleeve gastrectomy (28%) from 2007 to 2012 at five adolescent bariatric surgery centers.
The current analysis examined data from 141 participants in Teen-LABS who underwent bariatric surgery at a mean age of 16.8 years. Mean BMI was 51.5, most were girls (80%), and they had diverse race/ethnicity (66% were White).
Researchers also identified a control group of 83 adolescents of a similar age and gender who had diverse race/ethnicity (54% White) and a mean BMI of 46.9.
At year 6, data were available for 123 young adults in the surgery group (who by then had a mean BMI of 39.7) and 63 young adults in the nonsurgery group (who had a mean BMI of 52.6).
At baseline and year 6, participants replied to questionnaires that identified three eating disorders: continuous eating (eating in an unplanned and repetitious way between meals and snacks), objective overeating (eating a “large” amount of food without loss of control), and objective binge eating (eating a “large” amount of food with loss of control).
At baseline, rates of continuous eating, overeating, and binge eating were higher in the surgical group (50%, 40%, and 30%, respectively) than the nonsurgical group (40%, 22%, and 11%, respectively).
Six years later, when participants were aged 19-24 years, rates of continuous eating, overeating, and binge eating had declined in the surgical group (to 17%, 5%, and 1%, respectively). In the nonsurgical group, only continuous eating and overeating declined (to 24% and 7%, respectively), and binge eating increased slightly (to 13%).
Disordered eating associated with low self-worth, anxiety, and depression
In young adulthood in both groups, disordered eating was associated with lower self-worth. In the surgical group, it was also associated with lower weight-related quality of life, and in the nonsurgical group, it was also associated with anxiety and/or depression.
“The current findings cannot tell us whether disordered eating is a direct result or caused by anxiety, depression, low self-worth, or poor quality of life,” Dr. Decker said.
“These findings do give us insight about what other areas of clinical concern might present together [in] young adults (e.g., disordered eating, low self-esteem).”
Bariatric surgery affects the amount of food people can eat at one time, she noted in reply to a question from the audience. If people eat too much at a time they can experience vomiting, dumping syndrome (where certain food is “dumped” into the small intestine without being digested, causing nausea and vomiting), and plugging (a sense of food becoming stuck).
The home environment and transition to adulthood might impact disordered eating in young adults, she said in reply to another question, but these issues were not examined in this study.
A version of this article originally appeared on Medscape.com.
Kristina M. Decker, PhD, a postdoctoral fellow at Cincinnati Children’s Hospital Medical Center, presented these findings during the virtual ObesityWeek 2020.
Dr. Decker and associates examined rates of disordered eating in more than 200 adolescents (aged 13-18 years) who were severely obese, of whom 141 underwent bariatric surgery and the remainder did not.
At baseline (presurgery), the teens in both groups had rates of disordered eating ranging from 11% to 50%, with higher rates in those who went on to have bariatric surgery.
Six years later, rates of disordered eating were much lower in those who had bariatric surgery.
The data nevertheless “underscore that young adults with persistent severe obesity are at high risk for poor health and well-being,” Dr. Decker said in an interview.
“This means disordered eating behaviors should be closely monitored” in all such patients, both those who undergo surgery and those who don’t, she stressed.
Robust findings because of long follow-up and controls
The findings are not unexpected, based on adult bariatric literature, but are “novel because of the age of the patients,” senior author Margaret H. Zeller, PhD, Cincinnati Children’s Hospital Medical Center and professor at the University of Cincinnati, added.
In a comment comment, psychologist Kajsa Järvholm, PhD, of the Childhood Obesity Unit at Skåne University Hospital, Malmö̈, Sweden, who has published related work, said that this is “a needed study.”
Notably, it had “long-term follow-up and a control group,” and it “confirms that adolescents are in better control of their eating after surgery.”
However, an important additional takeaway for clinicians is that “disordered eating is associated with other mental health problems and self-worth. Clinicians treating obesity must address problems related to eating disorders to improve outcomes and well-being,” she stressed.
How does bariatric surgery impact overeating, binge eating, in teens?
“For teens with severe obesity, metabolic and bariatric surgery is the most effective treatment for improved cardiometabolic functioning, weight loss, and improved quality of life,” Dr. Decker stressed.
However, pre- and postsurgical disordered eating behaviors have been associated with a lower percentage change in body mass index (BMI), although this has not been well studied.
To investigate how disordered eating is affected by bariatric surgery in adolescents with severe obesity, researchers used data from Teen-LABS, which enrolled 242 participants aged 19 years and under who mainly underwent Roux-en-Y gastric bypass (67%) or sleeve gastrectomy (28%) from 2007 to 2012 at five adolescent bariatric surgery centers.
The current analysis examined data from 141 participants in Teen-LABS who underwent bariatric surgery at a mean age of 16.8 years. Mean BMI was 51.5, most were girls (80%), and they had diverse race/ethnicity (66% were White).
Researchers also identified a control group of 83 adolescents of a similar age and gender who had diverse race/ethnicity (54% White) and a mean BMI of 46.9.
At year 6, data were available for 123 young adults in the surgery group (who by then had a mean BMI of 39.7) and 63 young adults in the nonsurgery group (who had a mean BMI of 52.6).
At baseline and year 6, participants replied to questionnaires that identified three eating disorders: continuous eating (eating in an unplanned and repetitious way between meals and snacks), objective overeating (eating a “large” amount of food without loss of control), and objective binge eating (eating a “large” amount of food with loss of control).
At baseline, rates of continuous eating, overeating, and binge eating were higher in the surgical group (50%, 40%, and 30%, respectively) than the nonsurgical group (40%, 22%, and 11%, respectively).
Six years later, when participants were aged 19-24 years, rates of continuous eating, overeating, and binge eating had declined in the surgical group (to 17%, 5%, and 1%, respectively). In the nonsurgical group, only continuous eating and overeating declined (to 24% and 7%, respectively), and binge eating increased slightly (to 13%).
Disordered eating associated with low self-worth, anxiety, and depression
In young adulthood in both groups, disordered eating was associated with lower self-worth. In the surgical group, it was also associated with lower weight-related quality of life, and in the nonsurgical group, it was also associated with anxiety and/or depression.
“The current findings cannot tell us whether disordered eating is a direct result or caused by anxiety, depression, low self-worth, or poor quality of life,” Dr. Decker said.
“These findings do give us insight about what other areas of clinical concern might present together [in] young adults (e.g., disordered eating, low self-esteem).”
Bariatric surgery affects the amount of food people can eat at one time, she noted in reply to a question from the audience. If people eat too much at a time they can experience vomiting, dumping syndrome (where certain food is “dumped” into the small intestine without being digested, causing nausea and vomiting), and plugging (a sense of food becoming stuck).
The home environment and transition to adulthood might impact disordered eating in young adults, she said in reply to another question, but these issues were not examined in this study.
A version of this article originally appeared on Medscape.com.
Kristina M. Decker, PhD, a postdoctoral fellow at Cincinnati Children’s Hospital Medical Center, presented these findings during the virtual ObesityWeek 2020.
Dr. Decker and associates examined rates of disordered eating in more than 200 adolescents (aged 13-18 years) who were severely obese, of whom 141 underwent bariatric surgery and the remainder did not.
At baseline (presurgery), the teens in both groups had rates of disordered eating ranging from 11% to 50%, with higher rates in those who went on to have bariatric surgery.
Six years later, rates of disordered eating were much lower in those who had bariatric surgery.
The data nevertheless “underscore that young adults with persistent severe obesity are at high risk for poor health and well-being,” Dr. Decker said in an interview.
“This means disordered eating behaviors should be closely monitored” in all such patients, both those who undergo surgery and those who don’t, she stressed.
Robust findings because of long follow-up and controls
The findings are not unexpected, based on adult bariatric literature, but are “novel because of the age of the patients,” senior author Margaret H. Zeller, PhD, Cincinnati Children’s Hospital Medical Center and professor at the University of Cincinnati, added.
In a comment comment, psychologist Kajsa Järvholm, PhD, of the Childhood Obesity Unit at Skåne University Hospital, Malmö̈, Sweden, who has published related work, said that this is “a needed study.”
Notably, it had “long-term follow-up and a control group,” and it “confirms that adolescents are in better control of their eating after surgery.”
However, an important additional takeaway for clinicians is that “disordered eating is associated with other mental health problems and self-worth. Clinicians treating obesity must address problems related to eating disorders to improve outcomes and well-being,” she stressed.
How does bariatric surgery impact overeating, binge eating, in teens?
“For teens with severe obesity, metabolic and bariatric surgery is the most effective treatment for improved cardiometabolic functioning, weight loss, and improved quality of life,” Dr. Decker stressed.
However, pre- and postsurgical disordered eating behaviors have been associated with a lower percentage change in body mass index (BMI), although this has not been well studied.
To investigate how disordered eating is affected by bariatric surgery in adolescents with severe obesity, researchers used data from Teen-LABS, which enrolled 242 participants aged 19 years and under who mainly underwent Roux-en-Y gastric bypass (67%) or sleeve gastrectomy (28%) from 2007 to 2012 at five adolescent bariatric surgery centers.
The current analysis examined data from 141 participants in Teen-LABS who underwent bariatric surgery at a mean age of 16.8 years. Mean BMI was 51.5, most were girls (80%), and they had diverse race/ethnicity (66% were White).
Researchers also identified a control group of 83 adolescents of a similar age and gender who had diverse race/ethnicity (54% White) and a mean BMI of 46.9.
At year 6, data were available for 123 young adults in the surgery group (who by then had a mean BMI of 39.7) and 63 young adults in the nonsurgery group (who had a mean BMI of 52.6).
At baseline and year 6, participants replied to questionnaires that identified three eating disorders: continuous eating (eating in an unplanned and repetitious way between meals and snacks), objective overeating (eating a “large” amount of food without loss of control), and objective binge eating (eating a “large” amount of food with loss of control).
At baseline, rates of continuous eating, overeating, and binge eating were higher in the surgical group (50%, 40%, and 30%, respectively) than the nonsurgical group (40%, 22%, and 11%, respectively).
Six years later, when participants were aged 19-24 years, rates of continuous eating, overeating, and binge eating had declined in the surgical group (to 17%, 5%, and 1%, respectively). In the nonsurgical group, only continuous eating and overeating declined (to 24% and 7%, respectively), and binge eating increased slightly (to 13%).
Disordered eating associated with low self-worth, anxiety, and depression
In young adulthood in both groups, disordered eating was associated with lower self-worth. In the surgical group, it was also associated with lower weight-related quality of life, and in the nonsurgical group, it was also associated with anxiety and/or depression.
“The current findings cannot tell us whether disordered eating is a direct result or caused by anxiety, depression, low self-worth, or poor quality of life,” Dr. Decker said.
“These findings do give us insight about what other areas of clinical concern might present together [in] young adults (e.g., disordered eating, low self-esteem).”
Bariatric surgery affects the amount of food people can eat at one time, she noted in reply to a question from the audience. If people eat too much at a time they can experience vomiting, dumping syndrome (where certain food is “dumped” into the small intestine without being digested, causing nausea and vomiting), and plugging (a sense of food becoming stuck).
The home environment and transition to adulthood might impact disordered eating in young adults, she said in reply to another question, but these issues were not examined in this study.
A version of this article originally appeared on Medscape.com.
Bariatric surgery tied to lower aortic dissection risk
The finding is the latest in a series of benefits researchers have linked to the surgery, not all of which appear to directly result from weight loss.
“It has an incredible impact on hyperlipidemia and hypertension,” said Luis Felipe Okida, MD, from Cleveland Clinic Florida, Weston. “Those are the main risk factors for aortic dissection.”
He presented the finding at the virtual American Congress of Surgeons Clinical Congress 2020. The study was also published online in the Journal of the American College of Surgeons.
Although uncommon, acute aortic dissection proves fatal to half the people it strikes if patients do not receive treatment within 72 hours, Dr. Okida said in an interview.
To learn whether there is an association between bariatric surgery and risk for aortic dissection, Dr. Okida and colleagues analyzed data from the National Inpatient Sample (NIS) database from 2010 to 2015. The NIS comprises about 20% of hospital inpatient admissions in the United States.
Among the patients in the sample, 296,041 adults had undergone bariatric surgery, and 2,004,804 adults had obesity (body mass index ≥35 kg/m2) but had never undergone bariatric surgery. This latter group represented the control group.
Among the control group, 1,411 patients (.070%) experienced aortic dissection; among the bariatric surgery group, 94 patients (0.032%) experienced aortic dissection. This was a statistically significant difference (P < .0001).
The groups differed significantly in many ways. The mean age of the patients in the control group was 54.4 years, which was a mean of 2.5 years older than the bariatric surgery group. Additionally, the control group included a higher percentage of women and a lower percentage of White persons.
Those in the control group were also more likely to have a history of tobacco use, hypertension (64.2% vs. 48.9% in the surgery group), hyperlipidemia (32.7% vs. 18.3%), diabetes, aortic aneurysm (20.6% vs. 12.0%), and bicuspid aortic valves but were less likely to have Marfan/Ehlers-Danlos syndrome.
A multivariate analysis showed that gender, age, history of tobacco use, hypertension, hyperlipidemia, and Marfan/Ehlers-Danlos syndrome were associated with an increased risk for aortic dissection. Diabetes was associated with a lower risk. All of these findings had previously been reported in the literature, Dr. Okida said, but the reasons for the negative association with diabetes is not well understood.
The association between the surgery and aortic dissection applied to younger patients as well as older ones.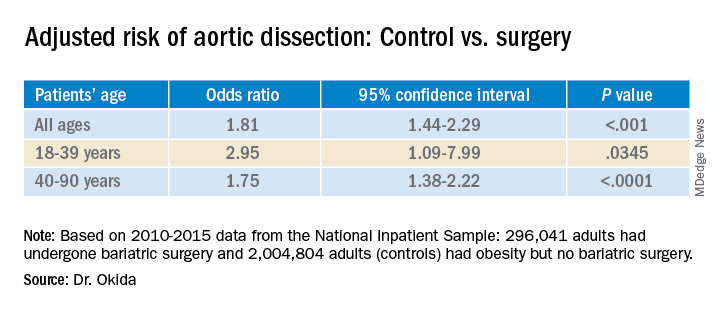
“In elderly patients, the main risk factor for aortic dissection is hypertension, and in younger patients, below 40 years old, the main risk factors are diseases of the collagen and diseases of the aorta,” said Dr. Okida during his presentation. “But these younger patients still have a high prevalence of hypertension, and that’s why bariatric surgery is beneficial.”
Although the finding regarding risk for aortic dissection supports the value of bariatric surgery, it does not in itself provide justification for undergoing the procedure. “It’s not even one of the comorbidities that insurance companies would recognize as key in approving this procedure,” said senior author Emanuele Lo Menzo, MD, PhD, also from the Cleveland Clinic Florida.
“I don’t think a physician would ever recommend this procedure specifically to avoid aortic dissection,” he said in an interview. “It’s sort of an extended benefit.”
The study raises interesting questions about the effects of the surgery, said Shanu Kothari, MD, president-elect of the American Society for Metabolic and Bariatric Surgery.
“We’ve known for a long time that patients with chronic obesity who undergo weight-loss surgery live longer than those who don’t,” he said in an interview. “They have less cardiovascular disease and cancer. Is this one more reason that they live longer?”
Bariatric surgery produces benefits for people with diabetes the day after the surgery, long before patients lose weight as a result of the procedure, Dr. Kothari said.
The effects on metabolism are complex, he added. Besides caloric restriction, they include changes in bile salt absorption and the gut microbiome, which in turn can affect hormones and inflammation.
A key question is how long after the surgery the risk for aortic dissection starts to decline, said Dr. Kothari.
The study could not answer such questions, and Dr. Okida could not find any previous studies that explored the association. He also couldn’t find any study that examined whether weight loss by other means might also reduce the risk for aortic dissection.
Dr. Okida, Dr. Lo Menzo, and Dr. Kothari disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The finding is the latest in a series of benefits researchers have linked to the surgery, not all of which appear to directly result from weight loss.
“It has an incredible impact on hyperlipidemia and hypertension,” said Luis Felipe Okida, MD, from Cleveland Clinic Florida, Weston. “Those are the main risk factors for aortic dissection.”
He presented the finding at the virtual American Congress of Surgeons Clinical Congress 2020. The study was also published online in the Journal of the American College of Surgeons.
Although uncommon, acute aortic dissection proves fatal to half the people it strikes if patients do not receive treatment within 72 hours, Dr. Okida said in an interview.
To learn whether there is an association between bariatric surgery and risk for aortic dissection, Dr. Okida and colleagues analyzed data from the National Inpatient Sample (NIS) database from 2010 to 2015. The NIS comprises about 20% of hospital inpatient admissions in the United States.
Among the patients in the sample, 296,041 adults had undergone bariatric surgery, and 2,004,804 adults had obesity (body mass index ≥35 kg/m2) but had never undergone bariatric surgery. This latter group represented the control group.
Among the control group, 1,411 patients (.070%) experienced aortic dissection; among the bariatric surgery group, 94 patients (0.032%) experienced aortic dissection. This was a statistically significant difference (P < .0001).
The groups differed significantly in many ways. The mean age of the patients in the control group was 54.4 years, which was a mean of 2.5 years older than the bariatric surgery group. Additionally, the control group included a higher percentage of women and a lower percentage of White persons.
Those in the control group were also more likely to have a history of tobacco use, hypertension (64.2% vs. 48.9% in the surgery group), hyperlipidemia (32.7% vs. 18.3%), diabetes, aortic aneurysm (20.6% vs. 12.0%), and bicuspid aortic valves but were less likely to have Marfan/Ehlers-Danlos syndrome.
A multivariate analysis showed that gender, age, history of tobacco use, hypertension, hyperlipidemia, and Marfan/Ehlers-Danlos syndrome were associated with an increased risk for aortic dissection. Diabetes was associated with a lower risk. All of these findings had previously been reported in the literature, Dr. Okida said, but the reasons for the negative association with diabetes is not well understood.
The association between the surgery and aortic dissection applied to younger patients as well as older ones.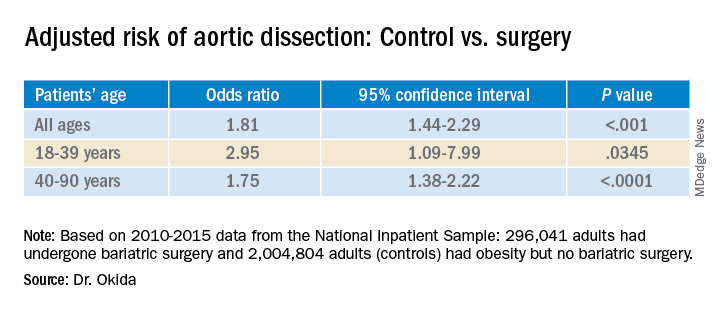
“In elderly patients, the main risk factor for aortic dissection is hypertension, and in younger patients, below 40 years old, the main risk factors are diseases of the collagen and diseases of the aorta,” said Dr. Okida during his presentation. “But these younger patients still have a high prevalence of hypertension, and that’s why bariatric surgery is beneficial.”
Although the finding regarding risk for aortic dissection supports the value of bariatric surgery, it does not in itself provide justification for undergoing the procedure. “It’s not even one of the comorbidities that insurance companies would recognize as key in approving this procedure,” said senior author Emanuele Lo Menzo, MD, PhD, also from the Cleveland Clinic Florida.
“I don’t think a physician would ever recommend this procedure specifically to avoid aortic dissection,” he said in an interview. “It’s sort of an extended benefit.”
The study raises interesting questions about the effects of the surgery, said Shanu Kothari, MD, president-elect of the American Society for Metabolic and Bariatric Surgery.
“We’ve known for a long time that patients with chronic obesity who undergo weight-loss surgery live longer than those who don’t,” he said in an interview. “They have less cardiovascular disease and cancer. Is this one more reason that they live longer?”
Bariatric surgery produces benefits for people with diabetes the day after the surgery, long before patients lose weight as a result of the procedure, Dr. Kothari said.
The effects on metabolism are complex, he added. Besides caloric restriction, they include changes in bile salt absorption and the gut microbiome, which in turn can affect hormones and inflammation.
A key question is how long after the surgery the risk for aortic dissection starts to decline, said Dr. Kothari.
The study could not answer such questions, and Dr. Okida could not find any previous studies that explored the association. He also couldn’t find any study that examined whether weight loss by other means might also reduce the risk for aortic dissection.
Dr. Okida, Dr. Lo Menzo, and Dr. Kothari disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The finding is the latest in a series of benefits researchers have linked to the surgery, not all of which appear to directly result from weight loss.
“It has an incredible impact on hyperlipidemia and hypertension,” said Luis Felipe Okida, MD, from Cleveland Clinic Florida, Weston. “Those are the main risk factors for aortic dissection.”
He presented the finding at the virtual American Congress of Surgeons Clinical Congress 2020. The study was also published online in the Journal of the American College of Surgeons.
Although uncommon, acute aortic dissection proves fatal to half the people it strikes if patients do not receive treatment within 72 hours, Dr. Okida said in an interview.
To learn whether there is an association between bariatric surgery and risk for aortic dissection, Dr. Okida and colleagues analyzed data from the National Inpatient Sample (NIS) database from 2010 to 2015. The NIS comprises about 20% of hospital inpatient admissions in the United States.
Among the patients in the sample, 296,041 adults had undergone bariatric surgery, and 2,004,804 adults had obesity (body mass index ≥35 kg/m2) but had never undergone bariatric surgery. This latter group represented the control group.
Among the control group, 1,411 patients (.070%) experienced aortic dissection; among the bariatric surgery group, 94 patients (0.032%) experienced aortic dissection. This was a statistically significant difference (P < .0001).
The groups differed significantly in many ways. The mean age of the patients in the control group was 54.4 years, which was a mean of 2.5 years older than the bariatric surgery group. Additionally, the control group included a higher percentage of women and a lower percentage of White persons.
Those in the control group were also more likely to have a history of tobacco use, hypertension (64.2% vs. 48.9% in the surgery group), hyperlipidemia (32.7% vs. 18.3%), diabetes, aortic aneurysm (20.6% vs. 12.0%), and bicuspid aortic valves but were less likely to have Marfan/Ehlers-Danlos syndrome.
A multivariate analysis showed that gender, age, history of tobacco use, hypertension, hyperlipidemia, and Marfan/Ehlers-Danlos syndrome were associated with an increased risk for aortic dissection. Diabetes was associated with a lower risk. All of these findings had previously been reported in the literature, Dr. Okida said, but the reasons for the negative association with diabetes is not well understood.
The association between the surgery and aortic dissection applied to younger patients as well as older ones.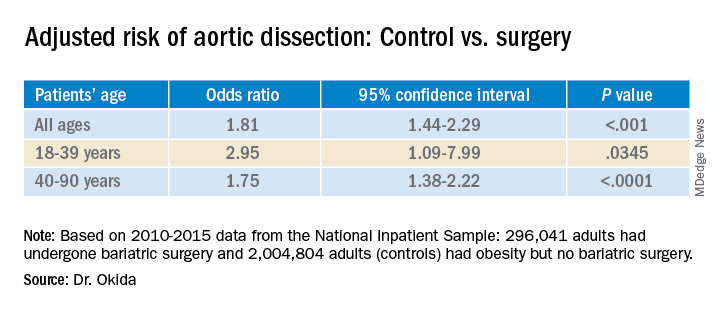
“In elderly patients, the main risk factor for aortic dissection is hypertension, and in younger patients, below 40 years old, the main risk factors are diseases of the collagen and diseases of the aorta,” said Dr. Okida during his presentation. “But these younger patients still have a high prevalence of hypertension, and that’s why bariatric surgery is beneficial.”
Although the finding regarding risk for aortic dissection supports the value of bariatric surgery, it does not in itself provide justification for undergoing the procedure. “It’s not even one of the comorbidities that insurance companies would recognize as key in approving this procedure,” said senior author Emanuele Lo Menzo, MD, PhD, also from the Cleveland Clinic Florida.
“I don’t think a physician would ever recommend this procedure specifically to avoid aortic dissection,” he said in an interview. “It’s sort of an extended benefit.”
The study raises interesting questions about the effects of the surgery, said Shanu Kothari, MD, president-elect of the American Society for Metabolic and Bariatric Surgery.
“We’ve known for a long time that patients with chronic obesity who undergo weight-loss surgery live longer than those who don’t,” he said in an interview. “They have less cardiovascular disease and cancer. Is this one more reason that they live longer?”
Bariatric surgery produces benefits for people with diabetes the day after the surgery, long before patients lose weight as a result of the procedure, Dr. Kothari said.
The effects on metabolism are complex, he added. Besides caloric restriction, they include changes in bile salt absorption and the gut microbiome, which in turn can affect hormones and inflammation.
A key question is how long after the surgery the risk for aortic dissection starts to decline, said Dr. Kothari.
The study could not answer such questions, and Dr. Okida could not find any previous studies that explored the association. He also couldn’t find any study that examined whether weight loss by other means might also reduce the risk for aortic dissection.
Dr. Okida, Dr. Lo Menzo, and Dr. Kothari disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Screening algorithm safely selects patients for OSA treatment before bariatric surgery
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
REPORTING FROM SLEEP 2020
Bariatric surgery achieved long-term resolution of NASH without worsening fibrosis
Bariatric surgery resolved nonalcoholic steatohepatitis (NASH) without worsening fibrosis in 84% of patients with evaluable biopsies, according to the findings of a prospective study.
The study included 180 severely or morbidly obese adults (body mass index >35 kg/m2) with NASH who underwent bariatric surgery at a center in France. Among 94 patients evaluated 5 years later, 68% had follow-up liver biopsies, of whom 84% (95% confidence interval, 73.1%-92.2%) met the primary endpoint of resolution of NASH without worsening of fibrosis. All histologic aspects of NASH had improved, median nonalcoholic fatty liver disease scores (NAS) fell from 5 (interquartile range, 4 to 5) to 1 (IQR, 0-2; P < .001), and 90% of patients achieved at least a 2-point NAS improvement. Hepatocellular ballooning also improved in 87.5% of patients. Baseline severity of NASH did not affect the chances of it resolving at 5 years. “The reduction of fibrosis [was] progressive, beginning during the first year and continuing through 5 years,” Guillaume Lassailly, MD, and associates wrote in Gastroenterology.
NASH is a priority for clinical research because of the substantial risk for subsequent cirrhosis, added Dr. Lassailly of CHU Lille (France). For NASH to resolve, most patients need to lose at least 7%-10% of their body weight, but “only 10% of patients reach this objective with lifestyle therapy at 1 year, and less than half maintain the weight loss 5 years later.” Despite ongoing drug development efforts, no medications have been approved for treating NASH. Although weight loss after bariatric surgery has been reported to resolve NASH in approximately 80% of patients at 1 year, longer-term data have been unavailable, and it has remained unclear whether bariatric surgery can slow or halt fibrosis progression.
All patients in this study had biopsy-confirmed NASH and at least a 5-year history of severe or morbid obesity as well as at least one comorbidity, such as diabetes mellitus or arterial hypertension. Patients were not heavy drinkers, and none had detectable markers of chronic liver disease.
Bariatric surgery produced a median 12-kg/m2 drop in body mass index. At 5-year follow-up, 93% of patients meeting or exceeding this threshold who had biopsies performed showed resolution of NASH without worsening of fibrosis. Furthermore, 56% of patients (95% CI, 42.4%-69.3%) had no histologic evidence of fibrosis, including 45.5% of patients who had bridging fibrosis at baseline.
Participants in this study received intensive preoperative support, including evaluations by numerous specialists, a nutrition plan, and a 6- to 12-month therapeutic education program. Bariatric surgery techniques included Roux-en-Y gastric bypass, gastric banding, and sleeve gastrectomy. A subgroup analysis linked gastric bypass to a significantly higher probability of meeting the primary endpoint, compared with gastric banding. Refusal was the most common reason for not having a follow-up biopsy, the researchers said. “Patients without liver biopsy after bariatric surgery were not significantly different from those with a histological follow-up except for a lower BMI at 1 year. Baseline fibrosis did not influence the probability of undergoing histological reevaluation at 5 years.”
Two study participants died from surgical complications within 1 month after surgery, and one patient died from cardiac dysfunction 4 years later. No fatality was deemed liver related.
The study was funded by the French Ministry of Health, Conseil Régional Nord-Pas de Calais, National de la Recherche, and the European commission (FEDER). The researchers reported having no conflicts of interest.
SOURCE: Lassailly G et al. Gastroenterology. 2020 Jun 15. doi: 10.1053/j.gastro.2020.06.006.
As obesity prevalence increases at an alarming pace, nonalcoholic steatohepatitis (NASH) has become the most common indication for liver transplantation in women and the second most common in men in the United States. Impeding the inflammation and reversing the resultant fibrosis prior to the development of end-stage liver disease and needing liver transplantation are essential goals in NASH management. The lack of Food and Drug Administration–approved pharmacotherapy triggered interest in the effect of weight loss on NASH and short-term benefits were noted.
In this article, Lassailly et al. demonstrated long-term benefits of bariatric surgery in patients with NASH. They prospectively enrolled 180 patients and histologically followed 64 patients at 1 year and 5 years postoperatively. NASH resolved in 84% of patients and fibrosis regressed in >70%. Importantly, advanced fibrosis (F3) regressed in 15/19 patients. Cirrhosis regressed to F3 in two-thirds of patients. No liver-related mortality or decompensation was observed.
These favorable outcomes embolden the practice of referring NASH patients with morbid obesity to bariatric surgery before liver disease severity becomes prohibitive of this approach. NASH pharmacotherapy may become available in the future. However, we must not forget that cardiovascular disease remains a common cause of morbidity and mortality in NASH patients.
With these study findings and previously established benefits of bariatric surgery on mitigating cardiovascular risk and treating relevant metabolic derangements (e.g., diabetes mellitus), pursuing bariatric surgery in NASH patients may be the seed that, if planted early on, can later flourish with resolution of NASH, prevention of cardiovascular disease, metabolic optimization, and potentially longer and healthier life.
Manhal J. Izzy, MD, is assistant professor of medicine, Vanderbilt Digestive Disease Center, Vanderbilt University, Nashville, Tenn.
As obesity prevalence increases at an alarming pace, nonalcoholic steatohepatitis (NASH) has become the most common indication for liver transplantation in women and the second most common in men in the United States. Impeding the inflammation and reversing the resultant fibrosis prior to the development of end-stage liver disease and needing liver transplantation are essential goals in NASH management. The lack of Food and Drug Administration–approved pharmacotherapy triggered interest in the effect of weight loss on NASH and short-term benefits were noted.
In this article, Lassailly et al. demonstrated long-term benefits of bariatric surgery in patients with NASH. They prospectively enrolled 180 patients and histologically followed 64 patients at 1 year and 5 years postoperatively. NASH resolved in 84% of patients and fibrosis regressed in >70%. Importantly, advanced fibrosis (F3) regressed in 15/19 patients. Cirrhosis regressed to F3 in two-thirds of patients. No liver-related mortality or decompensation was observed.
These favorable outcomes embolden the practice of referring NASH patients with morbid obesity to bariatric surgery before liver disease severity becomes prohibitive of this approach. NASH pharmacotherapy may become available in the future. However, we must not forget that cardiovascular disease remains a common cause of morbidity and mortality in NASH patients.
With these study findings and previously established benefits of bariatric surgery on mitigating cardiovascular risk and treating relevant metabolic derangements (e.g., diabetes mellitus), pursuing bariatric surgery in NASH patients may be the seed that, if planted early on, can later flourish with resolution of NASH, prevention of cardiovascular disease, metabolic optimization, and potentially longer and healthier life.
Manhal J. Izzy, MD, is assistant professor of medicine, Vanderbilt Digestive Disease Center, Vanderbilt University, Nashville, Tenn.
As obesity prevalence increases at an alarming pace, nonalcoholic steatohepatitis (NASH) has become the most common indication for liver transplantation in women and the second most common in men in the United States. Impeding the inflammation and reversing the resultant fibrosis prior to the development of end-stage liver disease and needing liver transplantation are essential goals in NASH management. The lack of Food and Drug Administration–approved pharmacotherapy triggered interest in the effect of weight loss on NASH and short-term benefits were noted.
In this article, Lassailly et al. demonstrated long-term benefits of bariatric surgery in patients with NASH. They prospectively enrolled 180 patients and histologically followed 64 patients at 1 year and 5 years postoperatively. NASH resolved in 84% of patients and fibrosis regressed in >70%. Importantly, advanced fibrosis (F3) regressed in 15/19 patients. Cirrhosis regressed to F3 in two-thirds of patients. No liver-related mortality or decompensation was observed.
These favorable outcomes embolden the practice of referring NASH patients with morbid obesity to bariatric surgery before liver disease severity becomes prohibitive of this approach. NASH pharmacotherapy may become available in the future. However, we must not forget that cardiovascular disease remains a common cause of morbidity and mortality in NASH patients.
With these study findings and previously established benefits of bariatric surgery on mitigating cardiovascular risk and treating relevant metabolic derangements (e.g., diabetes mellitus), pursuing bariatric surgery in NASH patients may be the seed that, if planted early on, can later flourish with resolution of NASH, prevention of cardiovascular disease, metabolic optimization, and potentially longer and healthier life.
Manhal J. Izzy, MD, is assistant professor of medicine, Vanderbilt Digestive Disease Center, Vanderbilt University, Nashville, Tenn.
Bariatric surgery resolved nonalcoholic steatohepatitis (NASH) without worsening fibrosis in 84% of patients with evaluable biopsies, according to the findings of a prospective study.
The study included 180 severely or morbidly obese adults (body mass index >35 kg/m2) with NASH who underwent bariatric surgery at a center in France. Among 94 patients evaluated 5 years later, 68% had follow-up liver biopsies, of whom 84% (95% confidence interval, 73.1%-92.2%) met the primary endpoint of resolution of NASH without worsening of fibrosis. All histologic aspects of NASH had improved, median nonalcoholic fatty liver disease scores (NAS) fell from 5 (interquartile range, 4 to 5) to 1 (IQR, 0-2; P < .001), and 90% of patients achieved at least a 2-point NAS improvement. Hepatocellular ballooning also improved in 87.5% of patients. Baseline severity of NASH did not affect the chances of it resolving at 5 years. “The reduction of fibrosis [was] progressive, beginning during the first year and continuing through 5 years,” Guillaume Lassailly, MD, and associates wrote in Gastroenterology.
NASH is a priority for clinical research because of the substantial risk for subsequent cirrhosis, added Dr. Lassailly of CHU Lille (France). For NASH to resolve, most patients need to lose at least 7%-10% of their body weight, but “only 10% of patients reach this objective with lifestyle therapy at 1 year, and less than half maintain the weight loss 5 years later.” Despite ongoing drug development efforts, no medications have been approved for treating NASH. Although weight loss after bariatric surgery has been reported to resolve NASH in approximately 80% of patients at 1 year, longer-term data have been unavailable, and it has remained unclear whether bariatric surgery can slow or halt fibrosis progression.
All patients in this study had biopsy-confirmed NASH and at least a 5-year history of severe or morbid obesity as well as at least one comorbidity, such as diabetes mellitus or arterial hypertension. Patients were not heavy drinkers, and none had detectable markers of chronic liver disease.
Bariatric surgery produced a median 12-kg/m2 drop in body mass index. At 5-year follow-up, 93% of patients meeting or exceeding this threshold who had biopsies performed showed resolution of NASH without worsening of fibrosis. Furthermore, 56% of patients (95% CI, 42.4%-69.3%) had no histologic evidence of fibrosis, including 45.5% of patients who had bridging fibrosis at baseline.
Participants in this study received intensive preoperative support, including evaluations by numerous specialists, a nutrition plan, and a 6- to 12-month therapeutic education program. Bariatric surgery techniques included Roux-en-Y gastric bypass, gastric banding, and sleeve gastrectomy. A subgroup analysis linked gastric bypass to a significantly higher probability of meeting the primary endpoint, compared with gastric banding. Refusal was the most common reason for not having a follow-up biopsy, the researchers said. “Patients without liver biopsy after bariatric surgery were not significantly different from those with a histological follow-up except for a lower BMI at 1 year. Baseline fibrosis did not influence the probability of undergoing histological reevaluation at 5 years.”
Two study participants died from surgical complications within 1 month after surgery, and one patient died from cardiac dysfunction 4 years later. No fatality was deemed liver related.
The study was funded by the French Ministry of Health, Conseil Régional Nord-Pas de Calais, National de la Recherche, and the European commission (FEDER). The researchers reported having no conflicts of interest.
SOURCE: Lassailly G et al. Gastroenterology. 2020 Jun 15. doi: 10.1053/j.gastro.2020.06.006.
Bariatric surgery resolved nonalcoholic steatohepatitis (NASH) without worsening fibrosis in 84% of patients with evaluable biopsies, according to the findings of a prospective study.
The study included 180 severely or morbidly obese adults (body mass index >35 kg/m2) with NASH who underwent bariatric surgery at a center in France. Among 94 patients evaluated 5 years later, 68% had follow-up liver biopsies, of whom 84% (95% confidence interval, 73.1%-92.2%) met the primary endpoint of resolution of NASH without worsening of fibrosis. All histologic aspects of NASH had improved, median nonalcoholic fatty liver disease scores (NAS) fell from 5 (interquartile range, 4 to 5) to 1 (IQR, 0-2; P < .001), and 90% of patients achieved at least a 2-point NAS improvement. Hepatocellular ballooning also improved in 87.5% of patients. Baseline severity of NASH did not affect the chances of it resolving at 5 years. “The reduction of fibrosis [was] progressive, beginning during the first year and continuing through 5 years,” Guillaume Lassailly, MD, and associates wrote in Gastroenterology.
NASH is a priority for clinical research because of the substantial risk for subsequent cirrhosis, added Dr. Lassailly of CHU Lille (France). For NASH to resolve, most patients need to lose at least 7%-10% of their body weight, but “only 10% of patients reach this objective with lifestyle therapy at 1 year, and less than half maintain the weight loss 5 years later.” Despite ongoing drug development efforts, no medications have been approved for treating NASH. Although weight loss after bariatric surgery has been reported to resolve NASH in approximately 80% of patients at 1 year, longer-term data have been unavailable, and it has remained unclear whether bariatric surgery can slow or halt fibrosis progression.
All patients in this study had biopsy-confirmed NASH and at least a 5-year history of severe or morbid obesity as well as at least one comorbidity, such as diabetes mellitus or arterial hypertension. Patients were not heavy drinkers, and none had detectable markers of chronic liver disease.
Bariatric surgery produced a median 12-kg/m2 drop in body mass index. At 5-year follow-up, 93% of patients meeting or exceeding this threshold who had biopsies performed showed resolution of NASH without worsening of fibrosis. Furthermore, 56% of patients (95% CI, 42.4%-69.3%) had no histologic evidence of fibrosis, including 45.5% of patients who had bridging fibrosis at baseline.
Participants in this study received intensive preoperative support, including evaluations by numerous specialists, a nutrition plan, and a 6- to 12-month therapeutic education program. Bariatric surgery techniques included Roux-en-Y gastric bypass, gastric banding, and sleeve gastrectomy. A subgroup analysis linked gastric bypass to a significantly higher probability of meeting the primary endpoint, compared with gastric banding. Refusal was the most common reason for not having a follow-up biopsy, the researchers said. “Patients without liver biopsy after bariatric surgery were not significantly different from those with a histological follow-up except for a lower BMI at 1 year. Baseline fibrosis did not influence the probability of undergoing histological reevaluation at 5 years.”
Two study participants died from surgical complications within 1 month after surgery, and one patient died from cardiac dysfunction 4 years later. No fatality was deemed liver related.
The study was funded by the French Ministry of Health, Conseil Régional Nord-Pas de Calais, National de la Recherche, and the European commission (FEDER). The researchers reported having no conflicts of interest.
SOURCE: Lassailly G et al. Gastroenterology. 2020 Jun 15. doi: 10.1053/j.gastro.2020.06.006.
FROM GASTROENTEROLOGY
Obesity-related hypoventilation increased morbidity risk after bariatric surgery
Patients with obesity-associated sleep hypoventilation had a heightened risk of postoperative morbidities after bariatric surgery, according to a retrospective study.
Reena Mehra, MD, director of sleep disorders research for the Sleep Disorders Center at the Cleveland Clinic, led the team and the findings were presented at the virtual annual meeting of the Associated Professional Sleep Societies. Her research team examined the outcomes of 1,665 patients who underwent polysomnography prior to bariatric surgery performed at the Cleveland Clinic from 2011 to 2018.
More than two-thirds – 68.5% – had obesity-associated sleep hypoventilation as defined by body mass index (BMI) of ≥30 kg/m2 and either polysomnography-based end-tidal CO2 ≥45 mm Hg or serum bicarbonate ≥27 mEq/L.
These patients represent “a subset, if you will, of obesity hypoventilation syndrome – a subset that we were able to capture from our sleep studies … [because] we do CO2 monitoring during sleep studies uniformly,” Dr. Mehra said in an interview after the meeting.
Pornprapa Chindamporn, MD, a former fellow at the center and first author on the abstract, presented the findings. Patients in the study had a mean age of 45.2 ± 12.0 years and a BMI of 48.7 ± 9.0. Approximately 20% were male and 63.6% were White.
Those with obesity-associated sleep hypoventilation were more likely to be male and have a higher BMI and higher hemoglobin A1c than those without the condition. They also had a significantly higher apnea-hypopnea index (17.0 vs. 13.8) in those without the condition, she reported.
A number of outcomes (ICU stay, intubation, tracheostomy, discharge disposition, and 30-day readmission) were compared individually and as a composite outcome between those with and without obesity-associated sleep hypoventilation. While some of these postoperative morbidities were more common in patients with the condition, the differences between those with and without OHS were not statistically significant for intubation (1.5% vs. 1.3%, P = .81) and 30-day readmission (13.8% vs. 11.3%, P = .16). However, the composite outcome was significantly higher: 18.9% vs. 14.3% (P = .021), including in multivariable analysis that considered age, gender, BMI, Apnea Hypopnea Index, and diabetes.
All-cause mortality was not significantly different between the groups, likely because of its low overall rate (hazard ratio, 1.39; 95% confidence interval, 0.56-3.42).
“In this largest sample to date of systematically phenotyped obesity-associated sleep hypoventilation in patients undergoing bariatric surgery, we identified increased postoperative morbidity,” said Dr. Chindamporn, now a pulmonologist and sleep specialist practicing in Bangkok.
Dr. Mehra said in the interview that patients considering bariatric surgery are typically assessed for obstructive sleep apnea, but “not so much obesity hypoventilation syndrome or obesity-associated sleep-related hypoventilation syndrome.” The findings, “support the notion that we should be closely examining sleep-related hypoventilation in these patients.”
At the Cleveland Clinic, “clinically, we make sure we’re identifying these individuals and communicating the findings to bariatric surgery colleagues and to anesthesia,” said Dr. Mehra, also professor of medicine at Case Western Reserve University, Cleveland.
OHS is defined, according to the 2019 American Thoracic Society clinical practice guideline on evaluation and management of OHS, by the combination of obesity, sleep-disordered breathing, and awake daytime hypercapnia, after excluding other causes for hypoventilation (Am J Respir Crit Care Med. 2019;200[3]:e6-24).
A European Respiratory Society task force has proposed severity grading for OHS, with early stages defined by sleep-related hypoventilation and the highest grade of severity defined by morbidity-associated daytime hypercapnia (Eur Respir Rev. 2019;28:180097). However, Dr. Mehra said she is “not sure that we know enough [from long-term studies of OHS] to say definitively that there’s such an evolution.”
Certainly, she said, future research on OHS should consider its heterogeneity. It is possible that a subset of patients with OHS, “maybe these individuals with sleep-related hypoventilation,” are most likely to have adverse postsurgical outcomes.
Atul Malhotra, MD, professor of medicine at the University of California, San Diego, who was asked to comment on the study, said that OHS is understudied in general and particularly in the perioperative setting. “With the obesity pandemic, issues around OHS are likely to be [increasingly] important. And with increasing [use of] bariatric surgery, strategies to minimize risks are clearly needed,” he said, adding that the potential risks of nonbariatric surgery in patients with OHS require further study.
He noted that mortality rates in good hospitals “have become quite low for many elective surgeries, making it hard to show mortality benefit to most interventions.”
The ATS guideline on OHS states that it is the most severe form of obesity-induced respiratory compromise and leads to serious sequelae, including increased rates of mortality, chronic heart failure, pulmonary hypertension, and hospitalization caused by acute-on-chronic hypercapnic respiratory failure.
Dr. Chindamporn said in her presentation that she had no disclosures. Dr. Mehra’s research program is funded by the National Institute of Health, but she has also procured funding from the American College of Chest Physicians, American Heart Association, Clinical Translational Science Collaborative, and Central Society of Clinical Research. Dr. Malhotra disclosed that he is funded by the NIH and has received income from Merck and LIvanova related to medical education.
CORRECTION 9/15/2020: The original story misstated the presenter of the study. Dr. Chindamporn presented the findings.
Patients with obesity-associated sleep hypoventilation had a heightened risk of postoperative morbidities after bariatric surgery, according to a retrospective study.
Reena Mehra, MD, director of sleep disorders research for the Sleep Disorders Center at the Cleveland Clinic, led the team and the findings were presented at the virtual annual meeting of the Associated Professional Sleep Societies. Her research team examined the outcomes of 1,665 patients who underwent polysomnography prior to bariatric surgery performed at the Cleveland Clinic from 2011 to 2018.
More than two-thirds – 68.5% – had obesity-associated sleep hypoventilation as defined by body mass index (BMI) of ≥30 kg/m2 and either polysomnography-based end-tidal CO2 ≥45 mm Hg or serum bicarbonate ≥27 mEq/L.
These patients represent “a subset, if you will, of obesity hypoventilation syndrome – a subset that we were able to capture from our sleep studies … [because] we do CO2 monitoring during sleep studies uniformly,” Dr. Mehra said in an interview after the meeting.
Pornprapa Chindamporn, MD, a former fellow at the center and first author on the abstract, presented the findings. Patients in the study had a mean age of 45.2 ± 12.0 years and a BMI of 48.7 ± 9.0. Approximately 20% were male and 63.6% were White.
Those with obesity-associated sleep hypoventilation were more likely to be male and have a higher BMI and higher hemoglobin A1c than those without the condition. They also had a significantly higher apnea-hypopnea index (17.0 vs. 13.8) in those without the condition, she reported.
A number of outcomes (ICU stay, intubation, tracheostomy, discharge disposition, and 30-day readmission) were compared individually and as a composite outcome between those with and without obesity-associated sleep hypoventilation. While some of these postoperative morbidities were more common in patients with the condition, the differences between those with and without OHS were not statistically significant for intubation (1.5% vs. 1.3%, P = .81) and 30-day readmission (13.8% vs. 11.3%, P = .16). However, the composite outcome was significantly higher: 18.9% vs. 14.3% (P = .021), including in multivariable analysis that considered age, gender, BMI, Apnea Hypopnea Index, and diabetes.
All-cause mortality was not significantly different between the groups, likely because of its low overall rate (hazard ratio, 1.39; 95% confidence interval, 0.56-3.42).
“In this largest sample to date of systematically phenotyped obesity-associated sleep hypoventilation in patients undergoing bariatric surgery, we identified increased postoperative morbidity,” said Dr. Chindamporn, now a pulmonologist and sleep specialist practicing in Bangkok.
Dr. Mehra said in the interview that patients considering bariatric surgery are typically assessed for obstructive sleep apnea, but “not so much obesity hypoventilation syndrome or obesity-associated sleep-related hypoventilation syndrome.” The findings, “support the notion that we should be closely examining sleep-related hypoventilation in these patients.”
At the Cleveland Clinic, “clinically, we make sure we’re identifying these individuals and communicating the findings to bariatric surgery colleagues and to anesthesia,” said Dr. Mehra, also professor of medicine at Case Western Reserve University, Cleveland.
OHS is defined, according to the 2019 American Thoracic Society clinical practice guideline on evaluation and management of OHS, by the combination of obesity, sleep-disordered breathing, and awake daytime hypercapnia, after excluding other causes for hypoventilation (Am J Respir Crit Care Med. 2019;200[3]:e6-24).
A European Respiratory Society task force has proposed severity grading for OHS, with early stages defined by sleep-related hypoventilation and the highest grade of severity defined by morbidity-associated daytime hypercapnia (Eur Respir Rev. 2019;28:180097). However, Dr. Mehra said she is “not sure that we know enough [from long-term studies of OHS] to say definitively that there’s such an evolution.”
Certainly, she said, future research on OHS should consider its heterogeneity. It is possible that a subset of patients with OHS, “maybe these individuals with sleep-related hypoventilation,” are most likely to have adverse postsurgical outcomes.
Atul Malhotra, MD, professor of medicine at the University of California, San Diego, who was asked to comment on the study, said that OHS is understudied in general and particularly in the perioperative setting. “With the obesity pandemic, issues around OHS are likely to be [increasingly] important. And with increasing [use of] bariatric surgery, strategies to minimize risks are clearly needed,” he said, adding that the potential risks of nonbariatric surgery in patients with OHS require further study.
He noted that mortality rates in good hospitals “have become quite low for many elective surgeries, making it hard to show mortality benefit to most interventions.”
The ATS guideline on OHS states that it is the most severe form of obesity-induced respiratory compromise and leads to serious sequelae, including increased rates of mortality, chronic heart failure, pulmonary hypertension, and hospitalization caused by acute-on-chronic hypercapnic respiratory failure.
Dr. Chindamporn said in her presentation that she had no disclosures. Dr. Mehra’s research program is funded by the National Institute of Health, but she has also procured funding from the American College of Chest Physicians, American Heart Association, Clinical Translational Science Collaborative, and Central Society of Clinical Research. Dr. Malhotra disclosed that he is funded by the NIH and has received income from Merck and LIvanova related to medical education.
CORRECTION 9/15/2020: The original story misstated the presenter of the study. Dr. Chindamporn presented the findings.
Patients with obesity-associated sleep hypoventilation had a heightened risk of postoperative morbidities after bariatric surgery, according to a retrospective study.
Reena Mehra, MD, director of sleep disorders research for the Sleep Disorders Center at the Cleveland Clinic, led the team and the findings were presented at the virtual annual meeting of the Associated Professional Sleep Societies. Her research team examined the outcomes of 1,665 patients who underwent polysomnography prior to bariatric surgery performed at the Cleveland Clinic from 2011 to 2018.
More than two-thirds – 68.5% – had obesity-associated sleep hypoventilation as defined by body mass index (BMI) of ≥30 kg/m2 and either polysomnography-based end-tidal CO2 ≥45 mm Hg or serum bicarbonate ≥27 mEq/L.
These patients represent “a subset, if you will, of obesity hypoventilation syndrome – a subset that we were able to capture from our sleep studies … [because] we do CO2 monitoring during sleep studies uniformly,” Dr. Mehra said in an interview after the meeting.
Pornprapa Chindamporn, MD, a former fellow at the center and first author on the abstract, presented the findings. Patients in the study had a mean age of 45.2 ± 12.0 years and a BMI of 48.7 ± 9.0. Approximately 20% were male and 63.6% were White.
Those with obesity-associated sleep hypoventilation were more likely to be male and have a higher BMI and higher hemoglobin A1c than those without the condition. They also had a significantly higher apnea-hypopnea index (17.0 vs. 13.8) in those without the condition, she reported.
A number of outcomes (ICU stay, intubation, tracheostomy, discharge disposition, and 30-day readmission) were compared individually and as a composite outcome between those with and without obesity-associated sleep hypoventilation. While some of these postoperative morbidities were more common in patients with the condition, the differences between those with and without OHS were not statistically significant for intubation (1.5% vs. 1.3%, P = .81) and 30-day readmission (13.8% vs. 11.3%, P = .16). However, the composite outcome was significantly higher: 18.9% vs. 14.3% (P = .021), including in multivariable analysis that considered age, gender, BMI, Apnea Hypopnea Index, and diabetes.
All-cause mortality was not significantly different between the groups, likely because of its low overall rate (hazard ratio, 1.39; 95% confidence interval, 0.56-3.42).
“In this largest sample to date of systematically phenotyped obesity-associated sleep hypoventilation in patients undergoing bariatric surgery, we identified increased postoperative morbidity,” said Dr. Chindamporn, now a pulmonologist and sleep specialist practicing in Bangkok.
Dr. Mehra said in the interview that patients considering bariatric surgery are typically assessed for obstructive sleep apnea, but “not so much obesity hypoventilation syndrome or obesity-associated sleep-related hypoventilation syndrome.” The findings, “support the notion that we should be closely examining sleep-related hypoventilation in these patients.”
At the Cleveland Clinic, “clinically, we make sure we’re identifying these individuals and communicating the findings to bariatric surgery colleagues and to anesthesia,” said Dr. Mehra, also professor of medicine at Case Western Reserve University, Cleveland.
OHS is defined, according to the 2019 American Thoracic Society clinical practice guideline on evaluation and management of OHS, by the combination of obesity, sleep-disordered breathing, and awake daytime hypercapnia, after excluding other causes for hypoventilation (Am J Respir Crit Care Med. 2019;200[3]:e6-24).
A European Respiratory Society task force has proposed severity grading for OHS, with early stages defined by sleep-related hypoventilation and the highest grade of severity defined by morbidity-associated daytime hypercapnia (Eur Respir Rev. 2019;28:180097). However, Dr. Mehra said she is “not sure that we know enough [from long-term studies of OHS] to say definitively that there’s such an evolution.”
Certainly, she said, future research on OHS should consider its heterogeneity. It is possible that a subset of patients with OHS, “maybe these individuals with sleep-related hypoventilation,” are most likely to have adverse postsurgical outcomes.
Atul Malhotra, MD, professor of medicine at the University of California, San Diego, who was asked to comment on the study, said that OHS is understudied in general and particularly in the perioperative setting. “With the obesity pandemic, issues around OHS are likely to be [increasingly] important. And with increasing [use of] bariatric surgery, strategies to minimize risks are clearly needed,” he said, adding that the potential risks of nonbariatric surgery in patients with OHS require further study.
He noted that mortality rates in good hospitals “have become quite low for many elective surgeries, making it hard to show mortality benefit to most interventions.”
The ATS guideline on OHS states that it is the most severe form of obesity-induced respiratory compromise and leads to serious sequelae, including increased rates of mortality, chronic heart failure, pulmonary hypertension, and hospitalization caused by acute-on-chronic hypercapnic respiratory failure.
Dr. Chindamporn said in her presentation that she had no disclosures. Dr. Mehra’s research program is funded by the National Institute of Health, but she has also procured funding from the American College of Chest Physicians, American Heart Association, Clinical Translational Science Collaborative, and Central Society of Clinical Research. Dr. Malhotra disclosed that he is funded by the NIH and has received income from Merck and LIvanova related to medical education.
CORRECTION 9/15/2020: The original story misstated the presenter of the study. Dr. Chindamporn presented the findings.
FROM SLEEP 2020
How high a priority is bariatric surgery during COVID-19?
The ASMBS statement, “Safer Through Surgery,” was published online in Surgery for Obesity and Related Diseases by the ASMBS executive committee.
It is a reaction to the fact that some U.S. states have placed metabolic and bariatric surgery in the same low-priority category as cosmetic surgery as examples of “elective” procedures that should be among the last to be restarted when pandemic restrictions are eased.
Rather, ASMBS argues, although obesity surgery must be postponed along with other nonemergency procedures when surges in the novel coronavirus make them unsafe, such operations should be resumed as soon as possible along with other medically necessary procedures.
“Metabolic and bariatric surgery is NOT elective. Metabolic and bariatric surgery is medically necessary and the best treatment for those with the life-threatening and life-limiting disease of severe obesity,” the statement says.
And obesity itself is a major risk factor for worse COVID-19 outcomes, ASMBS President Matt Hutter, MD, told Medscape Medical News, noting that individuals with obesity are “more likely to be in [intensive care units].”
“Mortality rates are higher, even in young patients. And [obesity] ... is associated with other comorbidities including diabetes and heart disease...We know the clock is ticking for some folks. For those with early diabetes, the sooner the [bariatric] surgery the more likely it is [for diabetes] to go into remission.”
Because the pandemic may be around for a while, “If we can make people [with obesity] safer ... because they’ve had surgery ... they may be better off,” should they get COVID-19 later, he pointed out.
Hutter noted that the ASMBS recorded a series of webinars, archived on the society’s website, with panels discussing in-depth issues to consider in prioritizing patients when restarting metabolic and bariatric surgery.
There are some differences of opinion, such as whether the sickest patients should be the first to have the surgeries upon reopening, or whether those individuals might be worse off if they contract COVID-19 in the perioperative setting.
“I don’t think there’s a right or wrong answer, but I think we have to figure out what’s right for the individual patient, considering their specific risks of having versus not having surgery, of waiting 1 month, 2 months, or 6 months. One thing we do know is that obesity is a significant disease.”
‘Before, during, and after COVID, obesity itself remains an epidemic’
Asked to comment on the ASMBS stance, Obesity Society president Lee M. Kaplan, MD, PhD, sent Medscape Medical News a statement.
“We do not fully understand which aspects of obesity pathophysiology ... are most responsible for the adverse COVID-19 outcomes, nor do we know the degree to which reduced access to care, social isolation, and other social and environmental determinants of health disproportionately affect COVID-19 patients with obesity,” he noted.
“At this early stage, we have not yet determined the impact of weight loss and various types of antiobesity therapies on these risks.”
Nonetheless, Kaplan said, “the extended COVID-19 pandemic underscores the importance of increasing, not diminishing, our commitment to understanding and treating obesity, using all available, evidence-based therapies, including lifestyle modification, antiobesity medications, bariatric surgery, and combinations thereof.”
As all health care delivery is being reorganized around the pandemic, Kaplan added: “Rethinking and changing our approach to obesity needs to be a central feature of this process.
“Before, during, and after COVID, obesity itself remains an epidemic. Its high global prevalence, increasing severity, and profound impact on all aspects of health and disease require that it be addressed more universally within the health care system, with the same commitment afforded to other chronic diseases.”
Obesity treatment isn’t generally considered an emergency, he noted, “because obesity is a chronic disease, whose adverse health effects often accumulate slowly and insidiously. Its generally slow progression allows for careful and coordinated care planning, and advanced scheduling of therapeutic interventions, including surgery. These characteristics, however, should not lead us to infer that treating obesity itself is optional.”
Hutter has reported receiving honoraria from Ethicon and Medtronic, and is a consultant for Vicarious Surgical and Sigilon Therapeutics. Kaplan has reported consulting for Boehringer Ingelheim, Fractyl, Gelesis, GI Dynamics, Johnson & Johnson, Novo Nordisk, Pfizer, Rhythm Pharmaceuticals, the National Institutes of Health, and the Department of State.
This article first appeared on Medscape.com.
The ASMBS statement, “Safer Through Surgery,” was published online in Surgery for Obesity and Related Diseases by the ASMBS executive committee.
It is a reaction to the fact that some U.S. states have placed metabolic and bariatric surgery in the same low-priority category as cosmetic surgery as examples of “elective” procedures that should be among the last to be restarted when pandemic restrictions are eased.
Rather, ASMBS argues, although obesity surgery must be postponed along with other nonemergency procedures when surges in the novel coronavirus make them unsafe, such operations should be resumed as soon as possible along with other medically necessary procedures.
“Metabolic and bariatric surgery is NOT elective. Metabolic and bariatric surgery is medically necessary and the best treatment for those with the life-threatening and life-limiting disease of severe obesity,” the statement says.
And obesity itself is a major risk factor for worse COVID-19 outcomes, ASMBS President Matt Hutter, MD, told Medscape Medical News, noting that individuals with obesity are “more likely to be in [intensive care units].”
“Mortality rates are higher, even in young patients. And [obesity] ... is associated with other comorbidities including diabetes and heart disease...We know the clock is ticking for some folks. For those with early diabetes, the sooner the [bariatric] surgery the more likely it is [for diabetes] to go into remission.”
Because the pandemic may be around for a while, “If we can make people [with obesity] safer ... because they’ve had surgery ... they may be better off,” should they get COVID-19 later, he pointed out.
Hutter noted that the ASMBS recorded a series of webinars, archived on the society’s website, with panels discussing in-depth issues to consider in prioritizing patients when restarting metabolic and bariatric surgery.
There are some differences of opinion, such as whether the sickest patients should be the first to have the surgeries upon reopening, or whether those individuals might be worse off if they contract COVID-19 in the perioperative setting.
“I don’t think there’s a right or wrong answer, but I think we have to figure out what’s right for the individual patient, considering their specific risks of having versus not having surgery, of waiting 1 month, 2 months, or 6 months. One thing we do know is that obesity is a significant disease.”
‘Before, during, and after COVID, obesity itself remains an epidemic’
Asked to comment on the ASMBS stance, Obesity Society president Lee M. Kaplan, MD, PhD, sent Medscape Medical News a statement.
“We do not fully understand which aspects of obesity pathophysiology ... are most responsible for the adverse COVID-19 outcomes, nor do we know the degree to which reduced access to care, social isolation, and other social and environmental determinants of health disproportionately affect COVID-19 patients with obesity,” he noted.
“At this early stage, we have not yet determined the impact of weight loss and various types of antiobesity therapies on these risks.”
Nonetheless, Kaplan said, “the extended COVID-19 pandemic underscores the importance of increasing, not diminishing, our commitment to understanding and treating obesity, using all available, evidence-based therapies, including lifestyle modification, antiobesity medications, bariatric surgery, and combinations thereof.”
As all health care delivery is being reorganized around the pandemic, Kaplan added: “Rethinking and changing our approach to obesity needs to be a central feature of this process.
“Before, during, and after COVID, obesity itself remains an epidemic. Its high global prevalence, increasing severity, and profound impact on all aspects of health and disease require that it be addressed more universally within the health care system, with the same commitment afforded to other chronic diseases.”
Obesity treatment isn’t generally considered an emergency, he noted, “because obesity is a chronic disease, whose adverse health effects often accumulate slowly and insidiously. Its generally slow progression allows for careful and coordinated care planning, and advanced scheduling of therapeutic interventions, including surgery. These characteristics, however, should not lead us to infer that treating obesity itself is optional.”
Hutter has reported receiving honoraria from Ethicon and Medtronic, and is a consultant for Vicarious Surgical and Sigilon Therapeutics. Kaplan has reported consulting for Boehringer Ingelheim, Fractyl, Gelesis, GI Dynamics, Johnson & Johnson, Novo Nordisk, Pfizer, Rhythm Pharmaceuticals, the National Institutes of Health, and the Department of State.
This article first appeared on Medscape.com.
The ASMBS statement, “Safer Through Surgery,” was published online in Surgery for Obesity and Related Diseases by the ASMBS executive committee.
It is a reaction to the fact that some U.S. states have placed metabolic and bariatric surgery in the same low-priority category as cosmetic surgery as examples of “elective” procedures that should be among the last to be restarted when pandemic restrictions are eased.
Rather, ASMBS argues, although obesity surgery must be postponed along with other nonemergency procedures when surges in the novel coronavirus make them unsafe, such operations should be resumed as soon as possible along with other medically necessary procedures.
“Metabolic and bariatric surgery is NOT elective. Metabolic and bariatric surgery is medically necessary and the best treatment for those with the life-threatening and life-limiting disease of severe obesity,” the statement says.
And obesity itself is a major risk factor for worse COVID-19 outcomes, ASMBS President Matt Hutter, MD, told Medscape Medical News, noting that individuals with obesity are “more likely to be in [intensive care units].”
“Mortality rates are higher, even in young patients. And [obesity] ... is associated with other comorbidities including diabetes and heart disease...We know the clock is ticking for some folks. For those with early diabetes, the sooner the [bariatric] surgery the more likely it is [for diabetes] to go into remission.”
Because the pandemic may be around for a while, “If we can make people [with obesity] safer ... because they’ve had surgery ... they may be better off,” should they get COVID-19 later, he pointed out.
Hutter noted that the ASMBS recorded a series of webinars, archived on the society’s website, with panels discussing in-depth issues to consider in prioritizing patients when restarting metabolic and bariatric surgery.
There are some differences of opinion, such as whether the sickest patients should be the first to have the surgeries upon reopening, or whether those individuals might be worse off if they contract COVID-19 in the perioperative setting.
“I don’t think there’s a right or wrong answer, but I think we have to figure out what’s right for the individual patient, considering their specific risks of having versus not having surgery, of waiting 1 month, 2 months, or 6 months. One thing we do know is that obesity is a significant disease.”
‘Before, during, and after COVID, obesity itself remains an epidemic’
Asked to comment on the ASMBS stance, Obesity Society president Lee M. Kaplan, MD, PhD, sent Medscape Medical News a statement.
“We do not fully understand which aspects of obesity pathophysiology ... are most responsible for the adverse COVID-19 outcomes, nor do we know the degree to which reduced access to care, social isolation, and other social and environmental determinants of health disproportionately affect COVID-19 patients with obesity,” he noted.
“At this early stage, we have not yet determined the impact of weight loss and various types of antiobesity therapies on these risks.”
Nonetheless, Kaplan said, “the extended COVID-19 pandemic underscores the importance of increasing, not diminishing, our commitment to understanding and treating obesity, using all available, evidence-based therapies, including lifestyle modification, antiobesity medications, bariatric surgery, and combinations thereof.”
As all health care delivery is being reorganized around the pandemic, Kaplan added: “Rethinking and changing our approach to obesity needs to be a central feature of this process.
“Before, during, and after COVID, obesity itself remains an epidemic. Its high global prevalence, increasing severity, and profound impact on all aspects of health and disease require that it be addressed more universally within the health care system, with the same commitment afforded to other chronic diseases.”
Obesity treatment isn’t generally considered an emergency, he noted, “because obesity is a chronic disease, whose adverse health effects often accumulate slowly and insidiously. Its generally slow progression allows for careful and coordinated care planning, and advanced scheduling of therapeutic interventions, including surgery. These characteristics, however, should not lead us to infer that treating obesity itself is optional.”
Hutter has reported receiving honoraria from Ethicon and Medtronic, and is a consultant for Vicarious Surgical and Sigilon Therapeutics. Kaplan has reported consulting for Boehringer Ingelheim, Fractyl, Gelesis, GI Dynamics, Johnson & Johnson, Novo Nordisk, Pfizer, Rhythm Pharmaceuticals, the National Institutes of Health, and the Department of State.
This article first appeared on Medscape.com.
Daily Recap: Hospitalized COVID patients need MRIs; Americans vote for face masks
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Three stages to COVID-19 brain damage, new review suggests
A new review outlined a three-stage classification of the impact of COVID-19 on the central nervous system and recommended all hospitalized patients with the virus undergo MRI to flag potential neurologic damage and inform postdischarge monitoring.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” said lead author Majid Fotuhi, MD, PhD. The review was published online in the Journal of Alzheimer’s Disease. Read more.
Topline results for novel intranasal med to treat opioid overdose
Topline results show positive results for the experimental intranasal nalmefene product OX125 for opioid overdose reversal, Orexo, the drug’s manufacturer, announced.
A crossover, comparative bioavailability study was conducted in healthy volunteers to assess nalmefene absorption of three development formulations of OX125. Preliminary results showed “extensive and rapid absorption” across all three formulations versus an intramuscular injection of nalmefene, Orexo reported.
“As the U.S. heroin crisis has developed to a fentanyl crisis, the medical need for novel and more powerful opioid rescue medications is vast,” Nikolaj Sørensen, president and CEO of Orexo, said in a press release. Read more.
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
Regarding regular testing, 66% of Republicans and those leaning Republican said that such testing was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Read more.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders.
Of gastric band patients, “almost 20% did not think they made the right decision,” he said. As for RYGP patients, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.

