User login
Lower thyroid hormone levels a red flag for elevated suicide risk?
Patients with comorbid anxiety and mood disorders who have reduced, albeit “normal” serum levels of thyroid-stimulating hormone (TSH) may be at increased risk for suicidal ideation, new research suggests.
In a cross-sectional study, clinical data on diagnosis, medication use, and symptom scores were gathered, along with assessments of blood levels of thyroid axis hormones, in patients with both anxiety and mood disorders.
After investigators accounted for age, gender, symptoms, medication use, and other potential confounders, patients with suicidal ideation were 54% less likely to have higher TSH levels. There was no association found with other thyroid hormones.
Based on the results, the assessment of thyroid hormone levels “may be important for suicide prevention and might allow clinicians to evaluate the potential of the suicidal ideation risk in individuals with [anxiety and mood disorders],” co-investigator Vilma Liaugaudaite, PhD student, Neuroscience Institute of the Lithuanian University of Health Sciences, Palanga, and colleagues note.
The findings were presented at the 34th European College of Neuropsychopharmacology (ECNP) Congress.
‘Complex mechanism’
Ms. Liaugaudaite told this news organization that thyroid hormones are known to have a “profound” effect on mood and behavior.
Recent studies show “various degrees of hypothalamic-pituitary-thyroid axis dysregulation are associated with suicidal behavior” in patients with depression, she added.
Noting that disturbances in the serotonin system “constitute the most common biochemical abnormality associated with suicidal behavior,” Ms. Liaugaudaite said it is thought thyroid hormones “are involved in a complex compensatory mechanism to correct reduced central 5-hydroxytryptamine activity” via lower TSH levels.
In addition, hypersecretion of thyrotropin-releasing hormone, which stimulates the release of TSH, “has been considered a compensatory mechanism to maintain normal thyroid hormone secretion and normalize serotonin activity in depressed patients,” she said.
To investigate associations between thyroid axis hormones and suicidality in individuals with comorbid anxiety and mood disorders, the researchers assessed consecutive patients attending a stress disorders clinic.
Sociodemographic and clinical information was gathered, and patients completed the Mini International Neuropsychiatric Interview, the Patient Health Questionnaire-9 (PHQ-9), and the General Anxiety Disorder-7 (GAD-7) scale.
Fasting blood samples were also tested for free thyroxine (FT4), free triiodothyronine (FT3), and TSH levels.
Significant association
Suicidal ideation was identified in 42 participants. Serum FT4, FT3, and TSH levels were within the normal range.
There were no significant differences between patients with and without suicidal ideation in terms of age, gender, education, obesity, smoking, and medication use.
Suicidal ideation was associated with higher scores on the PHQ-9 (15.5 vs. 13.3; P = .085), and with lower TSH levels (1.54 IU/L vs. 2.04 IU/L; P = .092).
The association between serum TSH levels and suicidal ideation was significant after multivariate logistic regression analysis accounted for age, gender, PHQ-9 and GAD-7 scores, education, body mass index, smoking, and use of antidepressants, tranquilizers, mood stabilizers, and neuroleptics.
Specifically, patients with suicidal ideation were significantly less likely to have higher TSH levels than those without, at an odds ratio of 0.46 (P = .027).
There were no significant associations between serum FT4 and FT3 levels and suicidal ideation.
Interesting, but preliminary
Commenting on the findings, Sanjeev Sockalingam, MD, vice chair and professor of psychiatry at the University of Toronto, said it is an “interesting study” because the literature on trying to identify individuals at risk for suicidal ideation or behaviors is “quite mixed, in terms of the results.”
However, it was a cross-sectional study with a relatively small sample size, and studies of this nature typically include patients with hypothyroidism “who end up having suicidal thoughts,” said Dr. Sockalingam, who was not involved with the research.
“I do wonder, given the sample size and patient population, if there may be other factors that may have been related to this,” he added.
Dr. Sockalingam noted that he would like to see more data on the medications the patients were taking, and he underlined that the thyroid levels were in the normal range, “so it’s a bit difficult to untangle what that means in terms of these subtle changes in thyroid levels.”
Robert Levitan, MD, Cameron Wilson Chair in Depression Research at the Centre for Addiction and Mental Health, Toronto, also emphasized that the thyroid levels were in the normal range.
He commented that it therefore “seems unlikely that there’s going to be some biological effect that’s going to affect the brain in a significant enough way” to influence suicidal ideation.
Dr. Levitan continued, “What’s probably happening is there’s some other clinical issue here that they just haven’t picked up on that’s leading in one direction to the suicidal ideation and perhaps affecting the TSH to some extent.”
Although the study is, therefore, “preliminary,” the findings are nevertheless “interesting,” he concluded.
The study received no funding. Ms. Liaugaudaite, Dr. Sockalingam, and Dr. Levitan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with comorbid anxiety and mood disorders who have reduced, albeit “normal” serum levels of thyroid-stimulating hormone (TSH) may be at increased risk for suicidal ideation, new research suggests.
In a cross-sectional study, clinical data on diagnosis, medication use, and symptom scores were gathered, along with assessments of blood levels of thyroid axis hormones, in patients with both anxiety and mood disorders.
After investigators accounted for age, gender, symptoms, medication use, and other potential confounders, patients with suicidal ideation were 54% less likely to have higher TSH levels. There was no association found with other thyroid hormones.
Based on the results, the assessment of thyroid hormone levels “may be important for suicide prevention and might allow clinicians to evaluate the potential of the suicidal ideation risk in individuals with [anxiety and mood disorders],” co-investigator Vilma Liaugaudaite, PhD student, Neuroscience Institute of the Lithuanian University of Health Sciences, Palanga, and colleagues note.
The findings were presented at the 34th European College of Neuropsychopharmacology (ECNP) Congress.
‘Complex mechanism’
Ms. Liaugaudaite told this news organization that thyroid hormones are known to have a “profound” effect on mood and behavior.
Recent studies show “various degrees of hypothalamic-pituitary-thyroid axis dysregulation are associated with suicidal behavior” in patients with depression, she added.
Noting that disturbances in the serotonin system “constitute the most common biochemical abnormality associated with suicidal behavior,” Ms. Liaugaudaite said it is thought thyroid hormones “are involved in a complex compensatory mechanism to correct reduced central 5-hydroxytryptamine activity” via lower TSH levels.
In addition, hypersecretion of thyrotropin-releasing hormone, which stimulates the release of TSH, “has been considered a compensatory mechanism to maintain normal thyroid hormone secretion and normalize serotonin activity in depressed patients,” she said.
To investigate associations between thyroid axis hormones and suicidality in individuals with comorbid anxiety and mood disorders, the researchers assessed consecutive patients attending a stress disorders clinic.
Sociodemographic and clinical information was gathered, and patients completed the Mini International Neuropsychiatric Interview, the Patient Health Questionnaire-9 (PHQ-9), and the General Anxiety Disorder-7 (GAD-7) scale.
Fasting blood samples were also tested for free thyroxine (FT4), free triiodothyronine (FT3), and TSH levels.
Significant association
Suicidal ideation was identified in 42 participants. Serum FT4, FT3, and TSH levels were within the normal range.
There were no significant differences between patients with and without suicidal ideation in terms of age, gender, education, obesity, smoking, and medication use.
Suicidal ideation was associated with higher scores on the PHQ-9 (15.5 vs. 13.3; P = .085), and with lower TSH levels (1.54 IU/L vs. 2.04 IU/L; P = .092).
The association between serum TSH levels and suicidal ideation was significant after multivariate logistic regression analysis accounted for age, gender, PHQ-9 and GAD-7 scores, education, body mass index, smoking, and use of antidepressants, tranquilizers, mood stabilizers, and neuroleptics.
Specifically, patients with suicidal ideation were significantly less likely to have higher TSH levels than those without, at an odds ratio of 0.46 (P = .027).
There were no significant associations between serum FT4 and FT3 levels and suicidal ideation.
Interesting, but preliminary
Commenting on the findings, Sanjeev Sockalingam, MD, vice chair and professor of psychiatry at the University of Toronto, said it is an “interesting study” because the literature on trying to identify individuals at risk for suicidal ideation or behaviors is “quite mixed, in terms of the results.”
However, it was a cross-sectional study with a relatively small sample size, and studies of this nature typically include patients with hypothyroidism “who end up having suicidal thoughts,” said Dr. Sockalingam, who was not involved with the research.
“I do wonder, given the sample size and patient population, if there may be other factors that may have been related to this,” he added.
Dr. Sockalingam noted that he would like to see more data on the medications the patients were taking, and he underlined that the thyroid levels were in the normal range, “so it’s a bit difficult to untangle what that means in terms of these subtle changes in thyroid levels.”
Robert Levitan, MD, Cameron Wilson Chair in Depression Research at the Centre for Addiction and Mental Health, Toronto, also emphasized that the thyroid levels were in the normal range.
He commented that it therefore “seems unlikely that there’s going to be some biological effect that’s going to affect the brain in a significant enough way” to influence suicidal ideation.
Dr. Levitan continued, “What’s probably happening is there’s some other clinical issue here that they just haven’t picked up on that’s leading in one direction to the suicidal ideation and perhaps affecting the TSH to some extent.”
Although the study is, therefore, “preliminary,” the findings are nevertheless “interesting,” he concluded.
The study received no funding. Ms. Liaugaudaite, Dr. Sockalingam, and Dr. Levitan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with comorbid anxiety and mood disorders who have reduced, albeit “normal” serum levels of thyroid-stimulating hormone (TSH) may be at increased risk for suicidal ideation, new research suggests.
In a cross-sectional study, clinical data on diagnosis, medication use, and symptom scores were gathered, along with assessments of blood levels of thyroid axis hormones, in patients with both anxiety and mood disorders.
After investigators accounted for age, gender, symptoms, medication use, and other potential confounders, patients with suicidal ideation were 54% less likely to have higher TSH levels. There was no association found with other thyroid hormones.
Based on the results, the assessment of thyroid hormone levels “may be important for suicide prevention and might allow clinicians to evaluate the potential of the suicidal ideation risk in individuals with [anxiety and mood disorders],” co-investigator Vilma Liaugaudaite, PhD student, Neuroscience Institute of the Lithuanian University of Health Sciences, Palanga, and colleagues note.
The findings were presented at the 34th European College of Neuropsychopharmacology (ECNP) Congress.
‘Complex mechanism’
Ms. Liaugaudaite told this news organization that thyroid hormones are known to have a “profound” effect on mood and behavior.
Recent studies show “various degrees of hypothalamic-pituitary-thyroid axis dysregulation are associated with suicidal behavior” in patients with depression, she added.
Noting that disturbances in the serotonin system “constitute the most common biochemical abnormality associated with suicidal behavior,” Ms. Liaugaudaite said it is thought thyroid hormones “are involved in a complex compensatory mechanism to correct reduced central 5-hydroxytryptamine activity” via lower TSH levels.
In addition, hypersecretion of thyrotropin-releasing hormone, which stimulates the release of TSH, “has been considered a compensatory mechanism to maintain normal thyroid hormone secretion and normalize serotonin activity in depressed patients,” she said.
To investigate associations between thyroid axis hormones and suicidality in individuals with comorbid anxiety and mood disorders, the researchers assessed consecutive patients attending a stress disorders clinic.
Sociodemographic and clinical information was gathered, and patients completed the Mini International Neuropsychiatric Interview, the Patient Health Questionnaire-9 (PHQ-9), and the General Anxiety Disorder-7 (GAD-7) scale.
Fasting blood samples were also tested for free thyroxine (FT4), free triiodothyronine (FT3), and TSH levels.
Significant association
Suicidal ideation was identified in 42 participants. Serum FT4, FT3, and TSH levels were within the normal range.
There were no significant differences between patients with and without suicidal ideation in terms of age, gender, education, obesity, smoking, and medication use.
Suicidal ideation was associated with higher scores on the PHQ-9 (15.5 vs. 13.3; P = .085), and with lower TSH levels (1.54 IU/L vs. 2.04 IU/L; P = .092).
The association between serum TSH levels and suicidal ideation was significant after multivariate logistic regression analysis accounted for age, gender, PHQ-9 and GAD-7 scores, education, body mass index, smoking, and use of antidepressants, tranquilizers, mood stabilizers, and neuroleptics.
Specifically, patients with suicidal ideation were significantly less likely to have higher TSH levels than those without, at an odds ratio of 0.46 (P = .027).
There were no significant associations between serum FT4 and FT3 levels and suicidal ideation.
Interesting, but preliminary
Commenting on the findings, Sanjeev Sockalingam, MD, vice chair and professor of psychiatry at the University of Toronto, said it is an “interesting study” because the literature on trying to identify individuals at risk for suicidal ideation or behaviors is “quite mixed, in terms of the results.”
However, it was a cross-sectional study with a relatively small sample size, and studies of this nature typically include patients with hypothyroidism “who end up having suicidal thoughts,” said Dr. Sockalingam, who was not involved with the research.
“I do wonder, given the sample size and patient population, if there may be other factors that may have been related to this,” he added.
Dr. Sockalingam noted that he would like to see more data on the medications the patients were taking, and he underlined that the thyroid levels were in the normal range, “so it’s a bit difficult to untangle what that means in terms of these subtle changes in thyroid levels.”
Robert Levitan, MD, Cameron Wilson Chair in Depression Research at the Centre for Addiction and Mental Health, Toronto, also emphasized that the thyroid levels were in the normal range.
He commented that it therefore “seems unlikely that there’s going to be some biological effect that’s going to affect the brain in a significant enough way” to influence suicidal ideation.
Dr. Levitan continued, “What’s probably happening is there’s some other clinical issue here that they just haven’t picked up on that’s leading in one direction to the suicidal ideation and perhaps affecting the TSH to some extent.”
Although the study is, therefore, “preliminary,” the findings are nevertheless “interesting,” he concluded.
The study received no funding. Ms. Liaugaudaite, Dr. Sockalingam, and Dr. Levitan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ECNP 2021
COVID-19: Greater mortality among psych patients remains a mystery
Antipsychotics are not responsible for the increased COVID-related death rate among patients with serious mental illness (SMI), new research shows.
The significant increase in COVID-19 mortality that continues to be reported among those with schizophrenia and schizoaffective disorder “underscores the importance of protective interventions for this group, including priority vaccination,” study investigator Katlyn Nemani, MD, research assistant professor, department of psychiatry, New York University, told this news organization.
The study was published online September 22 in JAMA Psychiatry.
Threefold increase in death
Previous research has linked a diagnosis of a schizophrenia spectrum disorder, which includes schizophrenia and schizoaffective disorder, to an almost threefold increase in mortality among patients with COVID-19.
Some population-based research has also reported a link between antipsychotic medication use and increased risk for COVID-related mortality, but these studies did not take psychiatric diagnoses into account.
“This raised the question of whether the increased risk observed in this population is related to underlying psychiatric illness or its treatment,” said Dr. Nemani.
The retrospective cohort study included 464 adults (mean age, 53 years) who were diagnosed with COVID-19 between March 3, 2020, and Feb. 17, 2021, and who had previously been diagnosed with schizophrenia spectrum disorder or bipolar disorder. Of these, 42.2% were treated with an antipsychotic medication.
The primary endpoint was death within 60 days of COVID-19 diagnosis. Covariates included sociodemographic characteristics, such as patient-reported race and ethnicity, age, and insurance type, a psychiatric diagnosis, medical comorbidities, and smoking status.
Of the total, 41 patients (8.8%) died. The 60-day fatality rate was 13.7% among patients with a schizophrenia spectrum disorder (n = 182) and 5.7% among patients with bipolar disorder (n = 282).
Antipsychotic treatment was not significantly associated with mortality (odds ratio, 1.00; 95% confidence interval, 0.48-2.08; P = .99).
“This suggests that antipsychotic medication is unlikely to be responsible for the increased risk we’ve observed in this population, although this finding needs to be replicated,” said Dr. Nemani.
Surprise finding
A diagnosis of a schizophrenia spectrum disorder was associated with an almost threefold increased risk for mortality compared with bipolar disorder (OR, 2.88; 95% CI, 1.36-6.11; P = .006).
“This was a surprising finding,” said Dr. Nemani.
She noted that there is evidence suggesting the immune system may play a role in the pathogenesis of schizophrenia, and research has shown that pneumonia and infection are among the leading causes of premature mortality in this population.
As well, several potential risk factors disproportionately affect people with serious mental illness, including an increase in the prevalence of medical comorbidities such as cardiovascular disease and diabetes, socioeconomic disadvantages, and barriers to accessing timely care. Prior studies have also found that people with SMI are less likely to receive preventive care interventions, including vaccination, said Dr. Nemani.
However, these factors are unlikely to fully account for the increased risk found in the study, she said.
“Our study population was limited to people who had received treatment within the NYU Langone Health System. We took a comprehensive list of sociodemographic and medical risk factors into account, and our research was conducted prior to the availability of COVID-19 vaccines,” she said.
Further research is necessary to understand what underlies the increase in susceptibility to severe infection among patients with schizophrenia and to identify interventions that may mitigate risk, said Dr. Nemani.
“This includes evaluating systems-level factors, such as access to preventive interventions and treatment, as well as investigating underlying immune mechanisms that may contribute to severe and fatal infection,” she said.
The researchers could not validate psychiatric diagnoses or capture deaths not documented in the electronic health record. In addition, the limited sample size precluded analysis of the use of individual antipsychotic medications, which may differ in their associated effects.
“It’s possible individual antipsychotic medications may be associated with harmful or protective effects,” said Dr. Nemani.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Antipsychotics are not responsible for the increased COVID-related death rate among patients with serious mental illness (SMI), new research shows.
The significant increase in COVID-19 mortality that continues to be reported among those with schizophrenia and schizoaffective disorder “underscores the importance of protective interventions for this group, including priority vaccination,” study investigator Katlyn Nemani, MD, research assistant professor, department of psychiatry, New York University, told this news organization.
The study was published online September 22 in JAMA Psychiatry.
Threefold increase in death
Previous research has linked a diagnosis of a schizophrenia spectrum disorder, which includes schizophrenia and schizoaffective disorder, to an almost threefold increase in mortality among patients with COVID-19.
Some population-based research has also reported a link between antipsychotic medication use and increased risk for COVID-related mortality, but these studies did not take psychiatric diagnoses into account.
“This raised the question of whether the increased risk observed in this population is related to underlying psychiatric illness or its treatment,” said Dr. Nemani.
The retrospective cohort study included 464 adults (mean age, 53 years) who were diagnosed with COVID-19 between March 3, 2020, and Feb. 17, 2021, and who had previously been diagnosed with schizophrenia spectrum disorder or bipolar disorder. Of these, 42.2% were treated with an antipsychotic medication.
The primary endpoint was death within 60 days of COVID-19 diagnosis. Covariates included sociodemographic characteristics, such as patient-reported race and ethnicity, age, and insurance type, a psychiatric diagnosis, medical comorbidities, and smoking status.
Of the total, 41 patients (8.8%) died. The 60-day fatality rate was 13.7% among patients with a schizophrenia spectrum disorder (n = 182) and 5.7% among patients with bipolar disorder (n = 282).
Antipsychotic treatment was not significantly associated with mortality (odds ratio, 1.00; 95% confidence interval, 0.48-2.08; P = .99).
“This suggests that antipsychotic medication is unlikely to be responsible for the increased risk we’ve observed in this population, although this finding needs to be replicated,” said Dr. Nemani.
Surprise finding
A diagnosis of a schizophrenia spectrum disorder was associated with an almost threefold increased risk for mortality compared with bipolar disorder (OR, 2.88; 95% CI, 1.36-6.11; P = .006).
“This was a surprising finding,” said Dr. Nemani.
She noted that there is evidence suggesting the immune system may play a role in the pathogenesis of schizophrenia, and research has shown that pneumonia and infection are among the leading causes of premature mortality in this population.
As well, several potential risk factors disproportionately affect people with serious mental illness, including an increase in the prevalence of medical comorbidities such as cardiovascular disease and diabetes, socioeconomic disadvantages, and barriers to accessing timely care. Prior studies have also found that people with SMI are less likely to receive preventive care interventions, including vaccination, said Dr. Nemani.
However, these factors are unlikely to fully account for the increased risk found in the study, she said.
“Our study population was limited to people who had received treatment within the NYU Langone Health System. We took a comprehensive list of sociodemographic and medical risk factors into account, and our research was conducted prior to the availability of COVID-19 vaccines,” she said.
Further research is necessary to understand what underlies the increase in susceptibility to severe infection among patients with schizophrenia and to identify interventions that may mitigate risk, said Dr. Nemani.
“This includes evaluating systems-level factors, such as access to preventive interventions and treatment, as well as investigating underlying immune mechanisms that may contribute to severe and fatal infection,” she said.
The researchers could not validate psychiatric diagnoses or capture deaths not documented in the electronic health record. In addition, the limited sample size precluded analysis of the use of individual antipsychotic medications, which may differ in their associated effects.
“It’s possible individual antipsychotic medications may be associated with harmful or protective effects,” said Dr. Nemani.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Antipsychotics are not responsible for the increased COVID-related death rate among patients with serious mental illness (SMI), new research shows.
The significant increase in COVID-19 mortality that continues to be reported among those with schizophrenia and schizoaffective disorder “underscores the importance of protective interventions for this group, including priority vaccination,” study investigator Katlyn Nemani, MD, research assistant professor, department of psychiatry, New York University, told this news organization.
The study was published online September 22 in JAMA Psychiatry.
Threefold increase in death
Previous research has linked a diagnosis of a schizophrenia spectrum disorder, which includes schizophrenia and schizoaffective disorder, to an almost threefold increase in mortality among patients with COVID-19.
Some population-based research has also reported a link between antipsychotic medication use and increased risk for COVID-related mortality, but these studies did not take psychiatric diagnoses into account.
“This raised the question of whether the increased risk observed in this population is related to underlying psychiatric illness or its treatment,” said Dr. Nemani.
The retrospective cohort study included 464 adults (mean age, 53 years) who were diagnosed with COVID-19 between March 3, 2020, and Feb. 17, 2021, and who had previously been diagnosed with schizophrenia spectrum disorder or bipolar disorder. Of these, 42.2% were treated with an antipsychotic medication.
The primary endpoint was death within 60 days of COVID-19 diagnosis. Covariates included sociodemographic characteristics, such as patient-reported race and ethnicity, age, and insurance type, a psychiatric diagnosis, medical comorbidities, and smoking status.
Of the total, 41 patients (8.8%) died. The 60-day fatality rate was 13.7% among patients with a schizophrenia spectrum disorder (n = 182) and 5.7% among patients with bipolar disorder (n = 282).
Antipsychotic treatment was not significantly associated with mortality (odds ratio, 1.00; 95% confidence interval, 0.48-2.08; P = .99).
“This suggests that antipsychotic medication is unlikely to be responsible for the increased risk we’ve observed in this population, although this finding needs to be replicated,” said Dr. Nemani.
Surprise finding
A diagnosis of a schizophrenia spectrum disorder was associated with an almost threefold increased risk for mortality compared with bipolar disorder (OR, 2.88; 95% CI, 1.36-6.11; P = .006).
“This was a surprising finding,” said Dr. Nemani.
She noted that there is evidence suggesting the immune system may play a role in the pathogenesis of schizophrenia, and research has shown that pneumonia and infection are among the leading causes of premature mortality in this population.
As well, several potential risk factors disproportionately affect people with serious mental illness, including an increase in the prevalence of medical comorbidities such as cardiovascular disease and diabetes, socioeconomic disadvantages, and barriers to accessing timely care. Prior studies have also found that people with SMI are less likely to receive preventive care interventions, including vaccination, said Dr. Nemani.
However, these factors are unlikely to fully account for the increased risk found in the study, she said.
“Our study population was limited to people who had received treatment within the NYU Langone Health System. We took a comprehensive list of sociodemographic and medical risk factors into account, and our research was conducted prior to the availability of COVID-19 vaccines,” she said.
Further research is necessary to understand what underlies the increase in susceptibility to severe infection among patients with schizophrenia and to identify interventions that may mitigate risk, said Dr. Nemani.
“This includes evaluating systems-level factors, such as access to preventive interventions and treatment, as well as investigating underlying immune mechanisms that may contribute to severe and fatal infection,” she said.
The researchers could not validate psychiatric diagnoses or capture deaths not documented in the electronic health record. In addition, the limited sample size precluded analysis of the use of individual antipsychotic medications, which may differ in their associated effects.
“It’s possible individual antipsychotic medications may be associated with harmful or protective effects,” said Dr. Nemani.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Antipsychotic effective for bipolar depression in phase 3 trial
Results of a phase 3 study show that treatment with lumateperone (Caplyta) significantly improved depressive symptoms for patients with major depressive episodes associated with both bipolar I and bipolar II disorders.
“Bipolar depression represents the most prevalent and debilitating presentation of bipolar disorder. There is a critical need for more treatments that are effective and have favorable safety profiles,” study investigator Gary S. Sachs, MD, associate clinical professor in psychiatry, Harvard Medical School, Boston, said in a company news release.
“The strong efficacy and impressive safety results reported in this trial for a broad patient population position lumateperone as a potentially important advancement in the treatment of this disorder,” said Dr. Sachs, who is also founding director of the Bipolar Clinic and Research Program at Massachusetts General Hospital, Boston.
The findings were published online September 23 in the American Journal of Psychiatry.
First-in-class antipsychotic
Lumateperone is a first-in-class antipsychotic that acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
It was approved by the U.S. Food and Drug Administration in late 2019 for the treatment of adults with schizophrenia, as reported at the time by this news organization.
All were randomly allocated in a 1:1 ratio to receive 6 weeks of lumateperone monotherapy at 42 mg/d or matching placebo.
At day 43, lumateperone treatment was associated with significantly greater improvement from baseline in Montgomery-Åsberg Depression Rating Scale (MADRS) score in comparison with placebo (drug-placebo difference, -4.6 points; P < .0001; effect size = -0.56), which met the study’s primary endpoint.
The study drug led to significant improvement in MADRS total score as early as the first week, which was the first time point measured. Improvement continued throughout the study.
Treatment with lumateperone also led to significantly greater improvement in the key secondary endpoints of total score on the severity scale of the Clinical Global Impressions Scale–Bipolar Version (CGI-BP-S) (P < .0001; effect size = -0.46) and the CGI-BP-S depression score (P < .001; effect size = -50).
In addition, it was superior to placebo both for patients with bipolar I disorder and those with bipolar II disorder.
Somnolence and nausea were the most commonly reported adverse events associated with lumateperone. Minimal changes were observed in weight and vital signs and in results of metabolic or endocrine assessments. These findings are in line with previous studies involving patients with schizophrenia.
The incidence of extrapyramidal symptom–related events was low and was similar to those with placebo.
The company has submitted a supplemental new drug application for lumateperone for the treatment of bipolar depression, which is currently under review with the FDA. The target action date is December 17.
A version of this article first appeared on Medscape.com.
Results of a phase 3 study show that treatment with lumateperone (Caplyta) significantly improved depressive symptoms for patients with major depressive episodes associated with both bipolar I and bipolar II disorders.
“Bipolar depression represents the most prevalent and debilitating presentation of bipolar disorder. There is a critical need for more treatments that are effective and have favorable safety profiles,” study investigator Gary S. Sachs, MD, associate clinical professor in psychiatry, Harvard Medical School, Boston, said in a company news release.
“The strong efficacy and impressive safety results reported in this trial for a broad patient population position lumateperone as a potentially important advancement in the treatment of this disorder,” said Dr. Sachs, who is also founding director of the Bipolar Clinic and Research Program at Massachusetts General Hospital, Boston.
The findings were published online September 23 in the American Journal of Psychiatry.
First-in-class antipsychotic
Lumateperone is a first-in-class antipsychotic that acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
It was approved by the U.S. Food and Drug Administration in late 2019 for the treatment of adults with schizophrenia, as reported at the time by this news organization.
All were randomly allocated in a 1:1 ratio to receive 6 weeks of lumateperone monotherapy at 42 mg/d or matching placebo.
At day 43, lumateperone treatment was associated with significantly greater improvement from baseline in Montgomery-Åsberg Depression Rating Scale (MADRS) score in comparison with placebo (drug-placebo difference, -4.6 points; P < .0001; effect size = -0.56), which met the study’s primary endpoint.
The study drug led to significant improvement in MADRS total score as early as the first week, which was the first time point measured. Improvement continued throughout the study.
Treatment with lumateperone also led to significantly greater improvement in the key secondary endpoints of total score on the severity scale of the Clinical Global Impressions Scale–Bipolar Version (CGI-BP-S) (P < .0001; effect size = -0.46) and the CGI-BP-S depression score (P < .001; effect size = -50).
In addition, it was superior to placebo both for patients with bipolar I disorder and those with bipolar II disorder.
Somnolence and nausea were the most commonly reported adverse events associated with lumateperone. Minimal changes were observed in weight and vital signs and in results of metabolic or endocrine assessments. These findings are in line with previous studies involving patients with schizophrenia.
The incidence of extrapyramidal symptom–related events was low and was similar to those with placebo.
The company has submitted a supplemental new drug application for lumateperone for the treatment of bipolar depression, which is currently under review with the FDA. The target action date is December 17.
A version of this article first appeared on Medscape.com.
Results of a phase 3 study show that treatment with lumateperone (Caplyta) significantly improved depressive symptoms for patients with major depressive episodes associated with both bipolar I and bipolar II disorders.
“Bipolar depression represents the most prevalent and debilitating presentation of bipolar disorder. There is a critical need for more treatments that are effective and have favorable safety profiles,” study investigator Gary S. Sachs, MD, associate clinical professor in psychiatry, Harvard Medical School, Boston, said in a company news release.
“The strong efficacy and impressive safety results reported in this trial for a broad patient population position lumateperone as a potentially important advancement in the treatment of this disorder,” said Dr. Sachs, who is also founding director of the Bipolar Clinic and Research Program at Massachusetts General Hospital, Boston.
The findings were published online September 23 in the American Journal of Psychiatry.
First-in-class antipsychotic
Lumateperone is a first-in-class antipsychotic that acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
It was approved by the U.S. Food and Drug Administration in late 2019 for the treatment of adults with schizophrenia, as reported at the time by this news organization.
All were randomly allocated in a 1:1 ratio to receive 6 weeks of lumateperone monotherapy at 42 mg/d or matching placebo.
At day 43, lumateperone treatment was associated with significantly greater improvement from baseline in Montgomery-Åsberg Depression Rating Scale (MADRS) score in comparison with placebo (drug-placebo difference, -4.6 points; P < .0001; effect size = -0.56), which met the study’s primary endpoint.
The study drug led to significant improvement in MADRS total score as early as the first week, which was the first time point measured. Improvement continued throughout the study.
Treatment with lumateperone also led to significantly greater improvement in the key secondary endpoints of total score on the severity scale of the Clinical Global Impressions Scale–Bipolar Version (CGI-BP-S) (P < .0001; effect size = -0.46) and the CGI-BP-S depression score (P < .001; effect size = -50).
In addition, it was superior to placebo both for patients with bipolar I disorder and those with bipolar II disorder.
Somnolence and nausea were the most commonly reported adverse events associated with lumateperone. Minimal changes were observed in weight and vital signs and in results of metabolic or endocrine assessments. These findings are in line with previous studies involving patients with schizophrenia.
The incidence of extrapyramidal symptom–related events was low and was similar to those with placebo.
The company has submitted a supplemental new drug application for lumateperone for the treatment of bipolar depression, which is currently under review with the FDA. The target action date is December 17.
A version of this article first appeared on Medscape.com.
Gut health ‘vitally important’ for mental health
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Residency programs need greater focus on BPD treatment
Borderline personality disorder (BPD) has suffered from underdiagnosis, in part because not enough clinicians know how to handle patients with BPD. “They don’t have the tools to know how to manage these situations effectively,” Lois W. Choi-Kain, MEd, MD, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass., said in an interview.
As a result, the clinician avoids the BPD patient, who feels demeaned and never finds the capacity to get better.
Psychiatry training in residency tends to emphasize biomedical treatments and does not focus enough on learning psychotherapy and other psychosocial treatments, according to Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass.
“This is where I see the need for a greater psychotherapy teaching focus in residency, along with teaching of general principles for working with patients with BPD,” said Dr. Plakun.
In his last phase of his career, BPD pioneer John G. Gunderson, MD, worked with Dr. Choi-Kain to train clinicians on general psychiatric management (GPM), which employs a sensitive, nonattacking approach to diffuse and calm situations with BPD patients.
As interest grows in combining GPM with manual treatments, GPM alone offers a more accessible approach for therapist and patient, said Dr. Choi-Kain, who has been trying to promote its use and do research on its techniques.
“It’s trying to boil it down to make it simple,” she said. As much as evidence-based, manualized approaches have advanced the field, they’re just not that widely available, she said.
Orchestrating treatments such as dialectical behavior therapy and mentalization-based therapy takes a lot of specialization, noted Dr. Choi-Kain. “And because of the amount of work that it involves for both the clinician and the patient, it decreases the capacity that clinicians and systems have to offer treatment to a wider number of patients.”
Learning a manualized treatment for BPD is asking a lot from residents, agreed Dr. Plakun. “Those who want more immersion in treating these patients can pursue further training in residency electives, in postresidency graduate medical education programs or through psychoanalytic training.”
Borderline personality disorder (BPD) has suffered from underdiagnosis, in part because not enough clinicians know how to handle patients with BPD. “They don’t have the tools to know how to manage these situations effectively,” Lois W. Choi-Kain, MEd, MD, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass., said in an interview.
As a result, the clinician avoids the BPD patient, who feels demeaned and never finds the capacity to get better.
Psychiatry training in residency tends to emphasize biomedical treatments and does not focus enough on learning psychotherapy and other psychosocial treatments, according to Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass.
“This is where I see the need for a greater psychotherapy teaching focus in residency, along with teaching of general principles for working with patients with BPD,” said Dr. Plakun.
In his last phase of his career, BPD pioneer John G. Gunderson, MD, worked with Dr. Choi-Kain to train clinicians on general psychiatric management (GPM), which employs a sensitive, nonattacking approach to diffuse and calm situations with BPD patients.
As interest grows in combining GPM with manual treatments, GPM alone offers a more accessible approach for therapist and patient, said Dr. Choi-Kain, who has been trying to promote its use and do research on its techniques.
“It’s trying to boil it down to make it simple,” she said. As much as evidence-based, manualized approaches have advanced the field, they’re just not that widely available, she said.
Orchestrating treatments such as dialectical behavior therapy and mentalization-based therapy takes a lot of specialization, noted Dr. Choi-Kain. “And because of the amount of work that it involves for both the clinician and the patient, it decreases the capacity that clinicians and systems have to offer treatment to a wider number of patients.”
Learning a manualized treatment for BPD is asking a lot from residents, agreed Dr. Plakun. “Those who want more immersion in treating these patients can pursue further training in residency electives, in postresidency graduate medical education programs or through psychoanalytic training.”
Borderline personality disorder (BPD) has suffered from underdiagnosis, in part because not enough clinicians know how to handle patients with BPD. “They don’t have the tools to know how to manage these situations effectively,” Lois W. Choi-Kain, MEd, MD, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass., said in an interview.
As a result, the clinician avoids the BPD patient, who feels demeaned and never finds the capacity to get better.
Psychiatry training in residency tends to emphasize biomedical treatments and does not focus enough on learning psychotherapy and other psychosocial treatments, according to Eric M. Plakun, MD, DLFAPA, FACPsych, medical director/CEO of the Austen Riggs Center in Stockbridge, Mass.
“This is where I see the need for a greater psychotherapy teaching focus in residency, along with teaching of general principles for working with patients with BPD,” said Dr. Plakun.
In his last phase of his career, BPD pioneer John G. Gunderson, MD, worked with Dr. Choi-Kain to train clinicians on general psychiatric management (GPM), which employs a sensitive, nonattacking approach to diffuse and calm situations with BPD patients.
As interest grows in combining GPM with manual treatments, GPM alone offers a more accessible approach for therapist and patient, said Dr. Choi-Kain, who has been trying to promote its use and do research on its techniques.
“It’s trying to boil it down to make it simple,” she said. As much as evidence-based, manualized approaches have advanced the field, they’re just not that widely available, she said.
Orchestrating treatments such as dialectical behavior therapy and mentalization-based therapy takes a lot of specialization, noted Dr. Choi-Kain. “And because of the amount of work that it involves for both the clinician and the patient, it decreases the capacity that clinicians and systems have to offer treatment to a wider number of patients.”
Learning a manualized treatment for BPD is asking a lot from residents, agreed Dr. Plakun. “Those who want more immersion in treating these patients can pursue further training in residency electives, in postresidency graduate medical education programs or through psychoanalytic training.”
A new name for BPD?
Michael A. Cummings, MD, has never liked the term “borderline personality disorder” (BPD). In his view, it’s a misnomer and needs to be changed.
“What is it bordering on? It’s not bordering on something, it’s a disorder on its own,” said Dr. Cummings of the department of psychiatry at the University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD grew out of the concept that patients were bordering on something, perhaps becoming bipolar. “In many ways, I don’t think it is even a personality disorder. It appears to be an inherent temperament that evolves into an inability to regulate mood.”
In his view, this puts it in the category of a mood dysregulation disorder.
Changing the label would not necessarily improve treatment, he added. However, transitioning from a pejorative to a more neutral label could make it easier for people to say, “this is just a type of mood disorder. It’s not necessarily easy, but it’s workable,” said Dr. Cummings.
Others in the field contend that the term fits the condition. BPD “describes how it encompasses a lot of complex psychological difficulties, undermining functioning of patients in a specific way,” said Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass. The disorder was identified because of its relationship with other known psychiatric disorders, said Dr. Choi-Kain. “There’s an element of BPD that borders on mood disorders because moods are so unstable with BPD. It also borders on trauma-related disorders. It borders on psychotic disorders because there’s sometimes stress-induced experiences of losing contact with realistic thinking.”
If anything needs to change, it’s the attitude toward the disorder, not the name. “I don’t think the term itself is pejorative. But I think that associations with the term have been very stigmatizing. For a long time, there was an attitude that these patients could not be treated or had negative therapeutic reactions.”
Data suggest that these patients are highly prevalent in clinical settings. “And I interpret that as them seeking the care that they need rather than resisting care or not responding to care,” said Dr. Choi-Kain.
Michael A. Cummings, MD, has never liked the term “borderline personality disorder” (BPD). In his view, it’s a misnomer and needs to be changed.
“What is it bordering on? It’s not bordering on something, it’s a disorder on its own,” said Dr. Cummings of the department of psychiatry at the University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD grew out of the concept that patients were bordering on something, perhaps becoming bipolar. “In many ways, I don’t think it is even a personality disorder. It appears to be an inherent temperament that evolves into an inability to regulate mood.”
In his view, this puts it in the category of a mood dysregulation disorder.
Changing the label would not necessarily improve treatment, he added. However, transitioning from a pejorative to a more neutral label could make it easier for people to say, “this is just a type of mood disorder. It’s not necessarily easy, but it’s workable,” said Dr. Cummings.
Others in the field contend that the term fits the condition. BPD “describes how it encompasses a lot of complex psychological difficulties, undermining functioning of patients in a specific way,” said Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass. The disorder was identified because of its relationship with other known psychiatric disorders, said Dr. Choi-Kain. “There’s an element of BPD that borders on mood disorders because moods are so unstable with BPD. It also borders on trauma-related disorders. It borders on psychotic disorders because there’s sometimes stress-induced experiences of losing contact with realistic thinking.”
If anything needs to change, it’s the attitude toward the disorder, not the name. “I don’t think the term itself is pejorative. But I think that associations with the term have been very stigmatizing. For a long time, there was an attitude that these patients could not be treated or had negative therapeutic reactions.”
Data suggest that these patients are highly prevalent in clinical settings. “And I interpret that as them seeking the care that they need rather than resisting care or not responding to care,” said Dr. Choi-Kain.
Michael A. Cummings, MD, has never liked the term “borderline personality disorder” (BPD). In his view, it’s a misnomer and needs to be changed.
“What is it bordering on? It’s not bordering on something, it’s a disorder on its own,” said Dr. Cummings of the department of psychiatry at the University of California, Riverside, and a psychopharmacology consultant with the California Department of State Hospitals’ Psychopharmacology Resource Network.
BPD grew out of the concept that patients were bordering on something, perhaps becoming bipolar. “In many ways, I don’t think it is even a personality disorder. It appears to be an inherent temperament that evolves into an inability to regulate mood.”
In his view, this puts it in the category of a mood dysregulation disorder.
Changing the label would not necessarily improve treatment, he added. However, transitioning from a pejorative to a more neutral label could make it easier for people to say, “this is just a type of mood disorder. It’s not necessarily easy, but it’s workable,” said Dr. Cummings.
Others in the field contend that the term fits the condition. BPD “describes how it encompasses a lot of complex psychological difficulties, undermining functioning of patients in a specific way,” said Lois W. Choi-Kain, MD, MEd, director of the Gunderson Personality Disorders Institute, McLean Hospital, Belmont, Mass. The disorder was identified because of its relationship with other known psychiatric disorders, said Dr. Choi-Kain. “There’s an element of BPD that borders on mood disorders because moods are so unstable with BPD. It also borders on trauma-related disorders. It borders on psychotic disorders because there’s sometimes stress-induced experiences of losing contact with realistic thinking.”
If anything needs to change, it’s the attitude toward the disorder, not the name. “I don’t think the term itself is pejorative. But I think that associations with the term have been very stigmatizing. For a long time, there was an attitude that these patients could not be treated or had negative therapeutic reactions.”
Data suggest that these patients are highly prevalent in clinical settings. “And I interpret that as them seeking the care that they need rather than resisting care or not responding to care,” said Dr. Choi-Kain.
The role of probiotics in mental health
In 1950, at Staten Island’s Sea View Hospital, a group of patients with terminal tuberculosis were given a new antibiotic called isoniazid, which caused some unexpected side effects. The patients reported euphoria, mental stimulation, and improved sleep, and even began socializing with more vigor. The press was all over the case, writing about the sick “dancing in the halls tho’ they had holes in their lungs.” Soon doctors started prescribing isoniazid as the first-ever antidepressant.
The Sea View Hospital experiment was an early hint that changing the composition of the gut microbiome – in this case, via antibiotics – might affect our mental health. Yet only in the last 2 decades has research into connections between what we ingest and psychiatric disorders really taken off. In 2004, a landmark study showed that germ-free mice (born in such sterile conditions that they lacked a microbiome) had an exaggerated stress response. The effects were reversed, however, if the mice were fed a bacterial strain, Bifidobacterium infantis, a probiotic. This sparked academic interest, and thousands of research papers followed.
According to Stephen Ilardi, PhD, a clinical psychologist at the University of Kansas, Lawrence, focusing on the etiology and treatment of depression, now is the “time of exciting discovery” in the field of probiotics and psychiatric disorders, although, admittedly, a lot still remains unknown.
Gut microbiome profiles in mental health disorders
We humans have about 100 trillion microbes residing in our guts. Some of these are archaea, some fungi, some protozoans and even viruses, but most are bacteria. Things like diet, sleep, and stress can all impact the composition of our gut microbiome. When the microbiome differs considerably from the typical, doctors and researchers describe it as dysbiosis, or imbalance. Studies have uncovered dysbiosis in patients with depression, anxiety, schizophrenia, and bipolar disorder.
“I think there is now pretty good evidence that the gut microbiome is actually an important factor in a number of psychiatric disorders,” says Allan Young, MBChB, clinical psychiatrist at King’s College London. The gut microbiome composition does seem to differ between psychiatric patients and the healthy. In depression, for example, a recent review of nine studies found an increase on the genus level in Streptococcus and Oscillibacter and low abundance of Lactobacillus and Coprococcus, among others. In generalized anxiety disorder, meanwhile, there appears to be an increase in Fusobacteria and Escherichia/Shigella .
For Dr. Ilardi, the next important question is whether there are plausible mechanisms that could explain how gut microbiota may influence brain function. And, it appears there are.
“The microbes in the gut can release neurotransmitters into blood that cross into the brain and influence brain function. They can release hormones into the blood that again cross into the brain. They’ve got a lot of tricks up their sleeve,” he says.
One particularly important pathway runs through the vagus nerve – the longest nerve that emerges directly from the brain, connecting it to the gut. Another is the immune pathway. Gut bacteria can interact with immune cells and reduce cytokine production, which in turn can reduce systemic inflammation. Inflammatory processes have been implicated in both depression and bipolar disorder. What’s more, gut microbes can upregulate the expression of a protein called BDNF – brain-derived neurotrophic factor – which helps the development and survival of nerve cells in the brain.
Probiotics’ promise varies for different conditions
As the pathways by which gut dysbiosis may influence psychiatric disorders become clearer, the next logical step is to try to influence the composition of the microbiome to prevent and treat depression, anxiety, or schizophrenia. That’s where probiotics come in.
The evidence for the effects of probiotics – live microorganisms which, when ingested in adequate amounts, confer a health benefit – so far is the strongest for depression, says Viktoriya Nikolova, MRes, MSc, a PhD student and researcher at King’s College London. In their 2021 meta-analysis of seven trials, Mr. Nikolova and colleagues revealed that probiotics can significantly reduce depressive symptoms after just 8 weeks. There was a caveat, however – the probiotics only worked when used in addition to an approved antidepressant. Another meta-analysis, published in 2018, also showed that probiotics, when compared with placebo, improve mood in people with depressive symptoms (here, no antidepressant treatment was necessary).
Roumen Milev, MD, PhD, a neuroscientist at Queen’s University, Kingston, Ont., and coauthor of a review on probiotics and depression published in the Annals of General Psychiatry, warns, however, that the research is still in its infancy. “,” he says.
When it comes to using probiotics to relieve anxiety, “the evidence in the animal literature is really compelling,” says Dr. Ilardi. Human studies are less convincing, however, which Dr. Dr. Ilardi showed in his 2018 review and meta-analysis involving 743 animals and 1,527 humans. “Studies are small for the most part, and some of them aren’t terribly well conducted, and they often use very low doses of probiotics,” he says. One of the larger double-blind and placebo-controlled trials showed that supplementation with Lactobacillus plantarum helps reduce stress and anxiety, while the levels of proinflammatory cytokines go down. Another meta-analysis, published in June, revealed that, when it comes to reducing stress and anxiety in youth, the results are mixed.
Evidence of probiotics’ efficiency in schizophrenia is emerging, yet also limited. A 2019 review concluded that currently available results only “hint” at a possibility that probiotics could make a difference in schizophrenia. Similarly, a 2020 review summed up that the role of probiotics in bipolar disorder “remains unclear and underexplored.”
Better studies, remaining questions
Apart from small samples, one issue with research on probiotics is that they generally tend to use varied doses of different strains of bacteria, or even multistrain mixtures, making it tough to compare results. Although there are hundreds of species of bacteria in the human gut, only a few have been evaluated for their antidepressant or antianxiety effects.
“To make it even worse, it’s almost certainly the case that depending on a person’s actual genetics or maybe their epigenetics, a strain that is helpful for one person may not be helpful for another. There is almost certainly no one-size-fits-all probiotic formulation,” says Dr. Ilardi.
Another critical question that remains to be answered is that of potential side effects.
“Probiotics are often seen as food supplements, so they don’t follow under the same regulations as drugs would,” says Mr. Nikolova. “They don’t necessarily have to follow the pattern of drug trials in many countries, which means that the monitoring of side effects is not the requirement.”
That’s something that worries King’s College psychiatrist Young too. “If you are giving it to modulate how the brain works, you could potentially induce psychiatric symptoms or a psychiatric disorder. There could be allergic reactions. There could be lots of different things,” he says.
When you search the web for “probiotics,” chances are you will come across sites boasting amazing effects that such products can have on cardiovascular heath, the immune system, and yes, mental well-being. Many also sell various probiotic supplements “formulated” for your gut health or improved moods. However, many such commercially available strains have never been actually tested in clinical trials. What’s more, according to Kathrin Cohen Kadosh, PhD, a neuroscientist at University of Surrey (England), “it is not always clear whether the different strains actually reach the gut intact.”
For now, considering the limited research evidence, a safer bet is to try to improve gut health through consumption of fermented foods that naturally contain probiotics, such as miso, kefir, or sauerkraut. Alternatively, you could reach for prebiotics, such as foods containing fiber (prebiotics enhance the growth of beneficial gut microbes). This, Dr. Kadosh says, could be “a gentler way of improving gut health” than popping a pill. Whether an improved mental well-being might follow still remains to be seen.
A version of this article first appeared on Medscape.com.
In 1950, at Staten Island’s Sea View Hospital, a group of patients with terminal tuberculosis were given a new antibiotic called isoniazid, which caused some unexpected side effects. The patients reported euphoria, mental stimulation, and improved sleep, and even began socializing with more vigor. The press was all over the case, writing about the sick “dancing in the halls tho’ they had holes in their lungs.” Soon doctors started prescribing isoniazid as the first-ever antidepressant.
The Sea View Hospital experiment was an early hint that changing the composition of the gut microbiome – in this case, via antibiotics – might affect our mental health. Yet only in the last 2 decades has research into connections between what we ingest and psychiatric disorders really taken off. In 2004, a landmark study showed that germ-free mice (born in such sterile conditions that they lacked a microbiome) had an exaggerated stress response. The effects were reversed, however, if the mice were fed a bacterial strain, Bifidobacterium infantis, a probiotic. This sparked academic interest, and thousands of research papers followed.
According to Stephen Ilardi, PhD, a clinical psychologist at the University of Kansas, Lawrence, focusing on the etiology and treatment of depression, now is the “time of exciting discovery” in the field of probiotics and psychiatric disorders, although, admittedly, a lot still remains unknown.
Gut microbiome profiles in mental health disorders
We humans have about 100 trillion microbes residing in our guts. Some of these are archaea, some fungi, some protozoans and even viruses, but most are bacteria. Things like diet, sleep, and stress can all impact the composition of our gut microbiome. When the microbiome differs considerably from the typical, doctors and researchers describe it as dysbiosis, or imbalance. Studies have uncovered dysbiosis in patients with depression, anxiety, schizophrenia, and bipolar disorder.
“I think there is now pretty good evidence that the gut microbiome is actually an important factor in a number of psychiatric disorders,” says Allan Young, MBChB, clinical psychiatrist at King’s College London. The gut microbiome composition does seem to differ between psychiatric patients and the healthy. In depression, for example, a recent review of nine studies found an increase on the genus level in Streptococcus and Oscillibacter and low abundance of Lactobacillus and Coprococcus, among others. In generalized anxiety disorder, meanwhile, there appears to be an increase in Fusobacteria and Escherichia/Shigella .
For Dr. Ilardi, the next important question is whether there are plausible mechanisms that could explain how gut microbiota may influence brain function. And, it appears there are.
“The microbes in the gut can release neurotransmitters into blood that cross into the brain and influence brain function. They can release hormones into the blood that again cross into the brain. They’ve got a lot of tricks up their sleeve,” he says.
One particularly important pathway runs through the vagus nerve – the longest nerve that emerges directly from the brain, connecting it to the gut. Another is the immune pathway. Gut bacteria can interact with immune cells and reduce cytokine production, which in turn can reduce systemic inflammation. Inflammatory processes have been implicated in both depression and bipolar disorder. What’s more, gut microbes can upregulate the expression of a protein called BDNF – brain-derived neurotrophic factor – which helps the development and survival of nerve cells in the brain.
Probiotics’ promise varies for different conditions
As the pathways by which gut dysbiosis may influence psychiatric disorders become clearer, the next logical step is to try to influence the composition of the microbiome to prevent and treat depression, anxiety, or schizophrenia. That’s where probiotics come in.
The evidence for the effects of probiotics – live microorganisms which, when ingested in adequate amounts, confer a health benefit – so far is the strongest for depression, says Viktoriya Nikolova, MRes, MSc, a PhD student and researcher at King’s College London. In their 2021 meta-analysis of seven trials, Mr. Nikolova and colleagues revealed that probiotics can significantly reduce depressive symptoms after just 8 weeks. There was a caveat, however – the probiotics only worked when used in addition to an approved antidepressant. Another meta-analysis, published in 2018, also showed that probiotics, when compared with placebo, improve mood in people with depressive symptoms (here, no antidepressant treatment was necessary).
Roumen Milev, MD, PhD, a neuroscientist at Queen’s University, Kingston, Ont., and coauthor of a review on probiotics and depression published in the Annals of General Psychiatry, warns, however, that the research is still in its infancy. “,” he says.
When it comes to using probiotics to relieve anxiety, “the evidence in the animal literature is really compelling,” says Dr. Ilardi. Human studies are less convincing, however, which Dr. Dr. Ilardi showed in his 2018 review and meta-analysis involving 743 animals and 1,527 humans. “Studies are small for the most part, and some of them aren’t terribly well conducted, and they often use very low doses of probiotics,” he says. One of the larger double-blind and placebo-controlled trials showed that supplementation with Lactobacillus plantarum helps reduce stress and anxiety, while the levels of proinflammatory cytokines go down. Another meta-analysis, published in June, revealed that, when it comes to reducing stress and anxiety in youth, the results are mixed.
Evidence of probiotics’ efficiency in schizophrenia is emerging, yet also limited. A 2019 review concluded that currently available results only “hint” at a possibility that probiotics could make a difference in schizophrenia. Similarly, a 2020 review summed up that the role of probiotics in bipolar disorder “remains unclear and underexplored.”
Better studies, remaining questions
Apart from small samples, one issue with research on probiotics is that they generally tend to use varied doses of different strains of bacteria, or even multistrain mixtures, making it tough to compare results. Although there are hundreds of species of bacteria in the human gut, only a few have been evaluated for their antidepressant or antianxiety effects.
“To make it even worse, it’s almost certainly the case that depending on a person’s actual genetics or maybe their epigenetics, a strain that is helpful for one person may not be helpful for another. There is almost certainly no one-size-fits-all probiotic formulation,” says Dr. Ilardi.
Another critical question that remains to be answered is that of potential side effects.
“Probiotics are often seen as food supplements, so they don’t follow under the same regulations as drugs would,” says Mr. Nikolova. “They don’t necessarily have to follow the pattern of drug trials in many countries, which means that the monitoring of side effects is not the requirement.”
That’s something that worries King’s College psychiatrist Young too. “If you are giving it to modulate how the brain works, you could potentially induce psychiatric symptoms or a psychiatric disorder. There could be allergic reactions. There could be lots of different things,” he says.
When you search the web for “probiotics,” chances are you will come across sites boasting amazing effects that such products can have on cardiovascular heath, the immune system, and yes, mental well-being. Many also sell various probiotic supplements “formulated” for your gut health or improved moods. However, many such commercially available strains have never been actually tested in clinical trials. What’s more, according to Kathrin Cohen Kadosh, PhD, a neuroscientist at University of Surrey (England), “it is not always clear whether the different strains actually reach the gut intact.”
For now, considering the limited research evidence, a safer bet is to try to improve gut health through consumption of fermented foods that naturally contain probiotics, such as miso, kefir, or sauerkraut. Alternatively, you could reach for prebiotics, such as foods containing fiber (prebiotics enhance the growth of beneficial gut microbes). This, Dr. Kadosh says, could be “a gentler way of improving gut health” than popping a pill. Whether an improved mental well-being might follow still remains to be seen.
A version of this article first appeared on Medscape.com.
In 1950, at Staten Island’s Sea View Hospital, a group of patients with terminal tuberculosis were given a new antibiotic called isoniazid, which caused some unexpected side effects. The patients reported euphoria, mental stimulation, and improved sleep, and even began socializing with more vigor. The press was all over the case, writing about the sick “dancing in the halls tho’ they had holes in their lungs.” Soon doctors started prescribing isoniazid as the first-ever antidepressant.
The Sea View Hospital experiment was an early hint that changing the composition of the gut microbiome – in this case, via antibiotics – might affect our mental health. Yet only in the last 2 decades has research into connections between what we ingest and psychiatric disorders really taken off. In 2004, a landmark study showed that germ-free mice (born in such sterile conditions that they lacked a microbiome) had an exaggerated stress response. The effects were reversed, however, if the mice were fed a bacterial strain, Bifidobacterium infantis, a probiotic. This sparked academic interest, and thousands of research papers followed.
According to Stephen Ilardi, PhD, a clinical psychologist at the University of Kansas, Lawrence, focusing on the etiology and treatment of depression, now is the “time of exciting discovery” in the field of probiotics and psychiatric disorders, although, admittedly, a lot still remains unknown.
Gut microbiome profiles in mental health disorders
We humans have about 100 trillion microbes residing in our guts. Some of these are archaea, some fungi, some protozoans and even viruses, but most are bacteria. Things like diet, sleep, and stress can all impact the composition of our gut microbiome. When the microbiome differs considerably from the typical, doctors and researchers describe it as dysbiosis, or imbalance. Studies have uncovered dysbiosis in patients with depression, anxiety, schizophrenia, and bipolar disorder.
“I think there is now pretty good evidence that the gut microbiome is actually an important factor in a number of psychiatric disorders,” says Allan Young, MBChB, clinical psychiatrist at King’s College London. The gut microbiome composition does seem to differ between psychiatric patients and the healthy. In depression, for example, a recent review of nine studies found an increase on the genus level in Streptococcus and Oscillibacter and low abundance of Lactobacillus and Coprococcus, among others. In generalized anxiety disorder, meanwhile, there appears to be an increase in Fusobacteria and Escherichia/Shigella .
For Dr. Ilardi, the next important question is whether there are plausible mechanisms that could explain how gut microbiota may influence brain function. And, it appears there are.
“The microbes in the gut can release neurotransmitters into blood that cross into the brain and influence brain function. They can release hormones into the blood that again cross into the brain. They’ve got a lot of tricks up their sleeve,” he says.
One particularly important pathway runs through the vagus nerve – the longest nerve that emerges directly from the brain, connecting it to the gut. Another is the immune pathway. Gut bacteria can interact with immune cells and reduce cytokine production, which in turn can reduce systemic inflammation. Inflammatory processes have been implicated in both depression and bipolar disorder. What’s more, gut microbes can upregulate the expression of a protein called BDNF – brain-derived neurotrophic factor – which helps the development and survival of nerve cells in the brain.
Probiotics’ promise varies for different conditions
As the pathways by which gut dysbiosis may influence psychiatric disorders become clearer, the next logical step is to try to influence the composition of the microbiome to prevent and treat depression, anxiety, or schizophrenia. That’s where probiotics come in.
The evidence for the effects of probiotics – live microorganisms which, when ingested in adequate amounts, confer a health benefit – so far is the strongest for depression, says Viktoriya Nikolova, MRes, MSc, a PhD student and researcher at King’s College London. In their 2021 meta-analysis of seven trials, Mr. Nikolova and colleagues revealed that probiotics can significantly reduce depressive symptoms after just 8 weeks. There was a caveat, however – the probiotics only worked when used in addition to an approved antidepressant. Another meta-analysis, published in 2018, also showed that probiotics, when compared with placebo, improve mood in people with depressive symptoms (here, no antidepressant treatment was necessary).
Roumen Milev, MD, PhD, a neuroscientist at Queen’s University, Kingston, Ont., and coauthor of a review on probiotics and depression published in the Annals of General Psychiatry, warns, however, that the research is still in its infancy. “,” he says.
When it comes to using probiotics to relieve anxiety, “the evidence in the animal literature is really compelling,” says Dr. Ilardi. Human studies are less convincing, however, which Dr. Dr. Ilardi showed in his 2018 review and meta-analysis involving 743 animals and 1,527 humans. “Studies are small for the most part, and some of them aren’t terribly well conducted, and they often use very low doses of probiotics,” he says. One of the larger double-blind and placebo-controlled trials showed that supplementation with Lactobacillus plantarum helps reduce stress and anxiety, while the levels of proinflammatory cytokines go down. Another meta-analysis, published in June, revealed that, when it comes to reducing stress and anxiety in youth, the results are mixed.
Evidence of probiotics’ efficiency in schizophrenia is emerging, yet also limited. A 2019 review concluded that currently available results only “hint” at a possibility that probiotics could make a difference in schizophrenia. Similarly, a 2020 review summed up that the role of probiotics in bipolar disorder “remains unclear and underexplored.”
Better studies, remaining questions
Apart from small samples, one issue with research on probiotics is that they generally tend to use varied doses of different strains of bacteria, or even multistrain mixtures, making it tough to compare results. Although there are hundreds of species of bacteria in the human gut, only a few have been evaluated for their antidepressant or antianxiety effects.
“To make it even worse, it’s almost certainly the case that depending on a person’s actual genetics or maybe their epigenetics, a strain that is helpful for one person may not be helpful for another. There is almost certainly no one-size-fits-all probiotic formulation,” says Dr. Ilardi.
Another critical question that remains to be answered is that of potential side effects.
“Probiotics are often seen as food supplements, so they don’t follow under the same regulations as drugs would,” says Mr. Nikolova. “They don’t necessarily have to follow the pattern of drug trials in many countries, which means that the monitoring of side effects is not the requirement.”
That’s something that worries King’s College psychiatrist Young too. “If you are giving it to modulate how the brain works, you could potentially induce psychiatric symptoms or a psychiatric disorder. There could be allergic reactions. There could be lots of different things,” he says.
When you search the web for “probiotics,” chances are you will come across sites boasting amazing effects that such products can have on cardiovascular heath, the immune system, and yes, mental well-being. Many also sell various probiotic supplements “formulated” for your gut health or improved moods. However, many such commercially available strains have never been actually tested in clinical trials. What’s more, according to Kathrin Cohen Kadosh, PhD, a neuroscientist at University of Surrey (England), “it is not always clear whether the different strains actually reach the gut intact.”
For now, considering the limited research evidence, a safer bet is to try to improve gut health through consumption of fermented foods that naturally contain probiotics, such as miso, kefir, or sauerkraut. Alternatively, you could reach for prebiotics, such as foods containing fiber (prebiotics enhance the growth of beneficial gut microbes). This, Dr. Kadosh says, could be “a gentler way of improving gut health” than popping a pill. Whether an improved mental well-being might follow still remains to be seen.
A version of this article first appeared on Medscape.com.
Teleintegrated versus telereferral care for complex psychiatric disorders
Two models for treating patients with complex psychiatric disorders in primary care are equally effective, new research suggests.
Results from a pragmatic, randomized comparative effectiveness study involving more than 1,000 patients showed that both integrated telepsychiatry collaborative care (TCC) and telepsychiatry/telepsychology enhanced referral (TER) provided “significantly and substantially” improved clinical outcomes, researchers noted.
However, the referral model required substantially more mental health specialist time than does the integrated model.
Therefore, ,” lead author John Fortney, PhD, department of psychiatry and behavioral sciences, University of Washington, Seattle, told this news organization.
The findings were published online Aug. 25 in JAMA Psychiatry.
Clinically meaningful improvement
The Study to Promote Innovation in Rural Integrated Telepsychiatry (SPIRIT) trial included 1,004 adults with untreated posttraumatic stress disorder and/or bipolar disorder. The participants were from 24 primary care clinics in rural and underserved areas in which there were no on-site psychiatrists or psychologists.
In SPIRIT, 508 patients were randomly allocated to TCC, and 496 were assigned to TER.
With TCC, an on-site behavioral health care manager and an off-site telepsychiatrist consultant support the primary care clinician in prescribing medications. With TER, an off-site telepsychiatrist prescribes medication, and an off-site telepsychologist delivers therapy.
The primary outcome was mental health functioning at 12 months, as measured by the Veterans RAND 12-item Health Survey Mental Component Summary (MCS) score. MSC scores range from 0 to 100.
Baseline MCS scores for the study participants were two standard deviations below the national average. The mean MCS scores were 39.7 and 41.2 in the TCC and TER groups, respectively.
There was no significant difference between TCC and TER in 12-month MCS score (beta = 1.0; 95% confidence interval, –0.8 to 2.8; P = .28). In addition, no significant differences in treatment effects were identified.
Patients in both groups experienced “large and clinically meaningful” improvements in MCS scores from baseline to 12 months (Cohen d = 0.81 and 0.90 for TCC and TER, respectively), the researchers report.
‘Bit of a surprise’
The comparative effectiveness of both models in this study was “a bit of a surprise,” Dr. Fortney noted.
“We hypothesized that TCC would have better outcomes than TER because we thought patients would be more likely to engage in treatment,” he said.
In collaborative care, the familiar primary care practitioner is the prescriber. The local care manager’s job is to keep patients engaged in care, said Dr. Fortney.
“However, because the medical school telemental health providers were privileged and credentialed to practice in the primary care clinic, the referral process to the telepsychiatrist and telepsychologist was much more successful than it usually is. So engagement was the same in both groups, and thus outcomes were equally as good,” Dr. Fortney said.
He noted that the referral model is used more than the collaborative care model “because it is similar to the more traditional approach to managing complex psychiatric disorders. I would say this is true both before and after COVID-19, but more so after.”
From a health care system perspective, “clinical leadership should implement whichever approach is most sustainable,” the investigators concluded.
Good news for clinics
Commenting on the study, Adam C. Powell, PhD, president of Payer+Provider Syndicate, said the “similar efficacy” of teleintegrated care and telereferral care for delivering behavioral health services in primary care is “good news for clinics,” because it suggests that clinicians may pick between the two modes of delivery and achieve similar outcomes.
“The resources available within a clinic may determine which of these approaches is most viable. The teleintegrated care approach requires the clinic to have more extensive resources locally,” Dr. Powell noted.
However, he pointed out that the study did not report relative costs of the two approaches, which may also be a factor in determining which one clinics choose to implement.
“Overall, the study shows that advances in telemedicine are making it possible for patients to access telepsychiatry and to achieve improvements in their mental health. Given the lack of access that many patients face, telepsychiatry offers one potential solution,” Dr. Powell concluded.
The SPIRIT study was funded by a grant from the Patient-Centered Outcomes Research Institute. Dr. Fortney and Dr. Powell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two models for treating patients with complex psychiatric disorders in primary care are equally effective, new research suggests.
Results from a pragmatic, randomized comparative effectiveness study involving more than 1,000 patients showed that both integrated telepsychiatry collaborative care (TCC) and telepsychiatry/telepsychology enhanced referral (TER) provided “significantly and substantially” improved clinical outcomes, researchers noted.
However, the referral model required substantially more mental health specialist time than does the integrated model.
Therefore, ,” lead author John Fortney, PhD, department of psychiatry and behavioral sciences, University of Washington, Seattle, told this news organization.
The findings were published online Aug. 25 in JAMA Psychiatry.
Clinically meaningful improvement
The Study to Promote Innovation in Rural Integrated Telepsychiatry (SPIRIT) trial included 1,004 adults with untreated posttraumatic stress disorder and/or bipolar disorder. The participants were from 24 primary care clinics in rural and underserved areas in which there were no on-site psychiatrists or psychologists.
In SPIRIT, 508 patients were randomly allocated to TCC, and 496 were assigned to TER.
With TCC, an on-site behavioral health care manager and an off-site telepsychiatrist consultant support the primary care clinician in prescribing medications. With TER, an off-site telepsychiatrist prescribes medication, and an off-site telepsychologist delivers therapy.
The primary outcome was mental health functioning at 12 months, as measured by the Veterans RAND 12-item Health Survey Mental Component Summary (MCS) score. MSC scores range from 0 to 100.
Baseline MCS scores for the study participants were two standard deviations below the national average. The mean MCS scores were 39.7 and 41.2 in the TCC and TER groups, respectively.
There was no significant difference between TCC and TER in 12-month MCS score (beta = 1.0; 95% confidence interval, –0.8 to 2.8; P = .28). In addition, no significant differences in treatment effects were identified.
Patients in both groups experienced “large and clinically meaningful” improvements in MCS scores from baseline to 12 months (Cohen d = 0.81 and 0.90 for TCC and TER, respectively), the researchers report.
‘Bit of a surprise’
The comparative effectiveness of both models in this study was “a bit of a surprise,” Dr. Fortney noted.
“We hypothesized that TCC would have better outcomes than TER because we thought patients would be more likely to engage in treatment,” he said.
In collaborative care, the familiar primary care practitioner is the prescriber. The local care manager’s job is to keep patients engaged in care, said Dr. Fortney.
“However, because the medical school telemental health providers were privileged and credentialed to practice in the primary care clinic, the referral process to the telepsychiatrist and telepsychologist was much more successful than it usually is. So engagement was the same in both groups, and thus outcomes were equally as good,” Dr. Fortney said.
He noted that the referral model is used more than the collaborative care model “because it is similar to the more traditional approach to managing complex psychiatric disorders. I would say this is true both before and after COVID-19, but more so after.”
From a health care system perspective, “clinical leadership should implement whichever approach is most sustainable,” the investigators concluded.
Good news for clinics
Commenting on the study, Adam C. Powell, PhD, president of Payer+Provider Syndicate, said the “similar efficacy” of teleintegrated care and telereferral care for delivering behavioral health services in primary care is “good news for clinics,” because it suggests that clinicians may pick between the two modes of delivery and achieve similar outcomes.
“The resources available within a clinic may determine which of these approaches is most viable. The teleintegrated care approach requires the clinic to have more extensive resources locally,” Dr. Powell noted.
However, he pointed out that the study did not report relative costs of the two approaches, which may also be a factor in determining which one clinics choose to implement.
“Overall, the study shows that advances in telemedicine are making it possible for patients to access telepsychiatry and to achieve improvements in their mental health. Given the lack of access that many patients face, telepsychiatry offers one potential solution,” Dr. Powell concluded.
The SPIRIT study was funded by a grant from the Patient-Centered Outcomes Research Institute. Dr. Fortney and Dr. Powell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two models for treating patients with complex psychiatric disorders in primary care are equally effective, new research suggests.
Results from a pragmatic, randomized comparative effectiveness study involving more than 1,000 patients showed that both integrated telepsychiatry collaborative care (TCC) and telepsychiatry/telepsychology enhanced referral (TER) provided “significantly and substantially” improved clinical outcomes, researchers noted.
However, the referral model required substantially more mental health specialist time than does the integrated model.
Therefore, ,” lead author John Fortney, PhD, department of psychiatry and behavioral sciences, University of Washington, Seattle, told this news organization.
The findings were published online Aug. 25 in JAMA Psychiatry.
Clinically meaningful improvement
The Study to Promote Innovation in Rural Integrated Telepsychiatry (SPIRIT) trial included 1,004 adults with untreated posttraumatic stress disorder and/or bipolar disorder. The participants were from 24 primary care clinics in rural and underserved areas in which there were no on-site psychiatrists or psychologists.
In SPIRIT, 508 patients were randomly allocated to TCC, and 496 were assigned to TER.
With TCC, an on-site behavioral health care manager and an off-site telepsychiatrist consultant support the primary care clinician in prescribing medications. With TER, an off-site telepsychiatrist prescribes medication, and an off-site telepsychologist delivers therapy.
The primary outcome was mental health functioning at 12 months, as measured by the Veterans RAND 12-item Health Survey Mental Component Summary (MCS) score. MSC scores range from 0 to 100.
Baseline MCS scores for the study participants were two standard deviations below the national average. The mean MCS scores were 39.7 and 41.2 in the TCC and TER groups, respectively.
There was no significant difference between TCC and TER in 12-month MCS score (beta = 1.0; 95% confidence interval, –0.8 to 2.8; P = .28). In addition, no significant differences in treatment effects were identified.
Patients in both groups experienced “large and clinically meaningful” improvements in MCS scores from baseline to 12 months (Cohen d = 0.81 and 0.90 for TCC and TER, respectively), the researchers report.
‘Bit of a surprise’
The comparative effectiveness of both models in this study was “a bit of a surprise,” Dr. Fortney noted.
“We hypothesized that TCC would have better outcomes than TER because we thought patients would be more likely to engage in treatment,” he said.
In collaborative care, the familiar primary care practitioner is the prescriber. The local care manager’s job is to keep patients engaged in care, said Dr. Fortney.
“However, because the medical school telemental health providers were privileged and credentialed to practice in the primary care clinic, the referral process to the telepsychiatrist and telepsychologist was much more successful than it usually is. So engagement was the same in both groups, and thus outcomes were equally as good,” Dr. Fortney said.
He noted that the referral model is used more than the collaborative care model “because it is similar to the more traditional approach to managing complex psychiatric disorders. I would say this is true both before and after COVID-19, but more so after.”
From a health care system perspective, “clinical leadership should implement whichever approach is most sustainable,” the investigators concluded.
Good news for clinics
Commenting on the study, Adam C. Powell, PhD, president of Payer+Provider Syndicate, said the “similar efficacy” of teleintegrated care and telereferral care for delivering behavioral health services in primary care is “good news for clinics,” because it suggests that clinicians may pick between the two modes of delivery and achieve similar outcomes.
“The resources available within a clinic may determine which of these approaches is most viable. The teleintegrated care approach requires the clinic to have more extensive resources locally,” Dr. Powell noted.
However, he pointed out that the study did not report relative costs of the two approaches, which may also be a factor in determining which one clinics choose to implement.
“Overall, the study shows that advances in telemedicine are making it possible for patients to access telepsychiatry and to achieve improvements in their mental health. Given the lack of access that many patients face, telepsychiatry offers one potential solution,” Dr. Powell concluded.
The SPIRIT study was funded by a grant from the Patient-Centered Outcomes Research Institute. Dr. Fortney and Dr. Powell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Beyond DSM symptoms: Behavioral clues to diagnosing bipolar II disorder
The diagnosis of bipolar II disorder is one of the most common challenges in psychiatric practice. Bipolar II disorder is frequently misdiagnosed as major depressive disorder (MDD) because symptoms of transient hypomanic episodes are either insufficiently probed or are rather vague. However, there are many valuable biographical clues that can expedite the diagnosis of bipolar II disorder.
The late Hagop S. Akiskal, MD, who passed away in January 2021, was an internationally recognized expert in mood disorders, and a dear friend for decades. He was a keen observer of human behavior who delved into the “life stories” of patients seeking help for depression. By thinking “outside the DSM box,” Dr. Akiskal was the first to recognize and codify a variety of behavioral and biographical clues for the bipolar spectrum (of which he was a pioneer) in patients presenting with a chief complaint of depression. He proposed a colorful set of behavioral stigmata in most patients with bipolar II disorder by carefully canvassing the life experiences of the patients he treated in the mood disorder clinic he established in the 1970s, which is believed to have been the first mood specialty clinic in the country.
Based on a review of >1,000 patients in his clinic who presented with depressive symptoms and were ultimately diagnosed as bipolar II disorder, Dr. Akiskal highlighted what he labeled as “behavioral activation, flamboyance and extravagance” among those patients. He referred to the cluster of those behaviors as “the soft spectrum” of bipolar disorder, which manifests in a set of distinctive behaviors in addition to depressive symptoms. He found that research tools such as the DSM-based Structured Clinical Interview often fail and frequently lead to a misdiagnosis of bipolar II disorder as MDD. This often condemns the patient to multiple failed trials of antidepressant monotherapy, and a delay in improvement, thus increasing the risk of job loss, disrupted relationships, and even suicide.
Over 3 decades, Dr. Akiskal developed the Mood Clinic Data Questionnaire (MCDQ) to systematize unstructured observations of patients presenting with a chief complaint of depression. His tool expedites the diagnosis of bipolar II disorder by understanding the patient as an individual, revealing personal and behavioral features consistent with what he labeled as episodic “hyperthymia” within the context of recurrent depression. This “social and behavioral phenotype,” as Dr. Akiskal called it, is rarely observed among patients with MDD.
By examining many patients with bipolar II disorder, Dr. Akiskal identified several “triads” of behavioral traits in the patients’ biographical history and in some of their close blood relatives as well. He also noticed that temperamentally, patients with bipolar II disorder thrive on “activity” and lovingly referred to themselves as “activity junkies.” Some of them may qualify as workaholics.
Biographical features that suggest bipolar II disorder
Here is a summary of the unique biographical features of patients with bipolar II disorder that Dr. Akiskal described:
Multilingual. Speaking ≥3 languages is unusual among individuals born in the United States, but often encountered among those with bipolar II disorder.
Continue to: Eminence
Eminence. Patients with bipolar II disorder, as well as their family members, tend to have leadership roles and prominence in journalism, media, and entertainment, fields that require interpersonal charm and eloquence. Those are common features of the “hyperthymic” temperament.
Creativity. Artists, poets, painters, and musicians who experience depression are more likely to have bipolar II disorder than MDD.
Biographical instability and/or excess. This is exemplified by going to 3 colleges and not necessarily obtaining a degree, or by frequently changing one’s line of work or city of residence. A classic example is a professor of medicine who also practices law and regularly sings in the opera, or a physician who is board-certified in 3 distinct specialties.
Activity junkies. Examples include a person with boundless energy, such as a novelist who writes 3 books a year or a professional who regularly works 12 hours a day without getting exhausted but seeks treatment for depressive episodes.
Multiple substances of abuse, such as nicotine, alcohol, stimulants, and opiates.
Continue to: Multiple psychiatric comorbidities
Multiple psychiatric comorbidities, such as having 3 types of anxiety (panic attacks, social phobia, and obsessive-compulsive disorder) or bulimia, seasonal depression, and anxiety.
Multiple pleasure-seeking or “outrageous” behaviors, such as compulsive gambling, sexual addiction, car racing, or skydiving. Another example is having a history of shoplifting, paraphilia, or arrest for participating in a riot, all of which are suggestive of antisocial traits in a patient seeking help for depression.
Sexual excesses, such as dating or having sex with ≥3 individuals concurrently, sometimes on the same day, or demanding sexual intercourse from a partner several times a day. Dr. Akiskal suggested that “sexual prowess” may represent an evolutionary advantage for the perpetuation of bipolar II disorder.
Marital history, such as a history of ≥3 marriages, or maintaining ≥2 families in different cities without being married.
Flamboyance and/or ornamentation. Examples might include wearing loud, colorful clothing (especially red), wearing ≥3 rings, or having piercings in ≥3 different body parts (tongue, nipples, navel, genitalia). Having elaborate tattoos across the body is no longer unique to “hyperthymic” persons with bipolar II disorder because tattoos have become far more common in the general population than they were in the 1970s. However, some take their tattoos to extremes.
Continue to: The above behaviors...
The above behaviors are condensed in a list that Dr. Akiskal called “the rule of 3” in patients with depression (Table1). Not all patients with bipolar II disorder will meet all the criteria of the rule of 3, but the first item in the mental status exam (appearance) alone may reflect the “soft bipolar spectrum,” such as garish clothing, red sneakers, multiple rings, bizarre hair coloring, and multiple piercings. This might prompt the clinician to ask further questions about hypomanic episodes as well as other personal behaviors related to the rule of 3.
Dr. Akiskal’s contributions to psychiatry are legendary in their originality, creativity, and clinical relevance. The rule of 3 is but one of his clinical concepts that may help identify many individuals with bipolar II disorder who are misdiagnosed as having MDD and prescribed a treatment that does not help or may exacerbate their illness course and worsen their outcome.
Based on the referrals of patients who are “treatment-resistant” to our Resident Mood Clinic, there are numerous persons in the country with bipolar II disorder (possibly millions) who are mislabeled with MDD and receiving the wrong treatments, to which they failed to respond. Their lifestyles and behaviors can provide valuable clinical insights into their true psychopathology, and that will lead to developing the right treatment plan.
1. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: the “red sign,” the “rule of three” and other biographic signs of temperamental extravagance, activation and hypomania. J Affect Disord. 2005;84(2-3):279-290.
The diagnosis of bipolar II disorder is one of the most common challenges in psychiatric practice. Bipolar II disorder is frequently misdiagnosed as major depressive disorder (MDD) because symptoms of transient hypomanic episodes are either insufficiently probed or are rather vague. However, there are many valuable biographical clues that can expedite the diagnosis of bipolar II disorder.
The late Hagop S. Akiskal, MD, who passed away in January 2021, was an internationally recognized expert in mood disorders, and a dear friend for decades. He was a keen observer of human behavior who delved into the “life stories” of patients seeking help for depression. By thinking “outside the DSM box,” Dr. Akiskal was the first to recognize and codify a variety of behavioral and biographical clues for the bipolar spectrum (of which he was a pioneer) in patients presenting with a chief complaint of depression. He proposed a colorful set of behavioral stigmata in most patients with bipolar II disorder by carefully canvassing the life experiences of the patients he treated in the mood disorder clinic he established in the 1970s, which is believed to have been the first mood specialty clinic in the country.
Based on a review of >1,000 patients in his clinic who presented with depressive symptoms and were ultimately diagnosed as bipolar II disorder, Dr. Akiskal highlighted what he labeled as “behavioral activation, flamboyance and extravagance” among those patients. He referred to the cluster of those behaviors as “the soft spectrum” of bipolar disorder, which manifests in a set of distinctive behaviors in addition to depressive symptoms. He found that research tools such as the DSM-based Structured Clinical Interview often fail and frequently lead to a misdiagnosis of bipolar II disorder as MDD. This often condemns the patient to multiple failed trials of antidepressant monotherapy, and a delay in improvement, thus increasing the risk of job loss, disrupted relationships, and even suicide.
Over 3 decades, Dr. Akiskal developed the Mood Clinic Data Questionnaire (MCDQ) to systematize unstructured observations of patients presenting with a chief complaint of depression. His tool expedites the diagnosis of bipolar II disorder by understanding the patient as an individual, revealing personal and behavioral features consistent with what he labeled as episodic “hyperthymia” within the context of recurrent depression. This “social and behavioral phenotype,” as Dr. Akiskal called it, is rarely observed among patients with MDD.
By examining many patients with bipolar II disorder, Dr. Akiskal identified several “triads” of behavioral traits in the patients’ biographical history and in some of their close blood relatives as well. He also noticed that temperamentally, patients with bipolar II disorder thrive on “activity” and lovingly referred to themselves as “activity junkies.” Some of them may qualify as workaholics.
Biographical features that suggest bipolar II disorder
Here is a summary of the unique biographical features of patients with bipolar II disorder that Dr. Akiskal described:
Multilingual. Speaking ≥3 languages is unusual among individuals born in the United States, but often encountered among those with bipolar II disorder.
Continue to: Eminence
Eminence. Patients with bipolar II disorder, as well as their family members, tend to have leadership roles and prominence in journalism, media, and entertainment, fields that require interpersonal charm and eloquence. Those are common features of the “hyperthymic” temperament.
Creativity. Artists, poets, painters, and musicians who experience depression are more likely to have bipolar II disorder than MDD.
Biographical instability and/or excess. This is exemplified by going to 3 colleges and not necessarily obtaining a degree, or by frequently changing one’s line of work or city of residence. A classic example is a professor of medicine who also practices law and regularly sings in the opera, or a physician who is board-certified in 3 distinct specialties.
Activity junkies. Examples include a person with boundless energy, such as a novelist who writes 3 books a year or a professional who regularly works 12 hours a day without getting exhausted but seeks treatment for depressive episodes.
Multiple substances of abuse, such as nicotine, alcohol, stimulants, and opiates.
Continue to: Multiple psychiatric comorbidities
Multiple psychiatric comorbidities, such as having 3 types of anxiety (panic attacks, social phobia, and obsessive-compulsive disorder) or bulimia, seasonal depression, and anxiety.
Multiple pleasure-seeking or “outrageous” behaviors, such as compulsive gambling, sexual addiction, car racing, or skydiving. Another example is having a history of shoplifting, paraphilia, or arrest for participating in a riot, all of which are suggestive of antisocial traits in a patient seeking help for depression.
Sexual excesses, such as dating or having sex with ≥3 individuals concurrently, sometimes on the same day, or demanding sexual intercourse from a partner several times a day. Dr. Akiskal suggested that “sexual prowess” may represent an evolutionary advantage for the perpetuation of bipolar II disorder.
Marital history, such as a history of ≥3 marriages, or maintaining ≥2 families in different cities without being married.
Flamboyance and/or ornamentation. Examples might include wearing loud, colorful clothing (especially red), wearing ≥3 rings, or having piercings in ≥3 different body parts (tongue, nipples, navel, genitalia). Having elaborate tattoos across the body is no longer unique to “hyperthymic” persons with bipolar II disorder because tattoos have become far more common in the general population than they were in the 1970s. However, some take their tattoos to extremes.
Continue to: The above behaviors...
The above behaviors are condensed in a list that Dr. Akiskal called “the rule of 3” in patients with depression (Table1). Not all patients with bipolar II disorder will meet all the criteria of the rule of 3, but the first item in the mental status exam (appearance) alone may reflect the “soft bipolar spectrum,” such as garish clothing, red sneakers, multiple rings, bizarre hair coloring, and multiple piercings. This might prompt the clinician to ask further questions about hypomanic episodes as well as other personal behaviors related to the rule of 3.
Dr. Akiskal’s contributions to psychiatry are legendary in their originality, creativity, and clinical relevance. The rule of 3 is but one of his clinical concepts that may help identify many individuals with bipolar II disorder who are misdiagnosed as having MDD and prescribed a treatment that does not help or may exacerbate their illness course and worsen their outcome.
Based on the referrals of patients who are “treatment-resistant” to our Resident Mood Clinic, there are numerous persons in the country with bipolar II disorder (possibly millions) who are mislabeled with MDD and receiving the wrong treatments, to which they failed to respond. Their lifestyles and behaviors can provide valuable clinical insights into their true psychopathology, and that will lead to developing the right treatment plan.
The diagnosis of bipolar II disorder is one of the most common challenges in psychiatric practice. Bipolar II disorder is frequently misdiagnosed as major depressive disorder (MDD) because symptoms of transient hypomanic episodes are either insufficiently probed or are rather vague. However, there are many valuable biographical clues that can expedite the diagnosis of bipolar II disorder.
The late Hagop S. Akiskal, MD, who passed away in January 2021, was an internationally recognized expert in mood disorders, and a dear friend for decades. He was a keen observer of human behavior who delved into the “life stories” of patients seeking help for depression. By thinking “outside the DSM box,” Dr. Akiskal was the first to recognize and codify a variety of behavioral and biographical clues for the bipolar spectrum (of which he was a pioneer) in patients presenting with a chief complaint of depression. He proposed a colorful set of behavioral stigmata in most patients with bipolar II disorder by carefully canvassing the life experiences of the patients he treated in the mood disorder clinic he established in the 1970s, which is believed to have been the first mood specialty clinic in the country.
Based on a review of >1,000 patients in his clinic who presented with depressive symptoms and were ultimately diagnosed as bipolar II disorder, Dr. Akiskal highlighted what he labeled as “behavioral activation, flamboyance and extravagance” among those patients. He referred to the cluster of those behaviors as “the soft spectrum” of bipolar disorder, which manifests in a set of distinctive behaviors in addition to depressive symptoms. He found that research tools such as the DSM-based Structured Clinical Interview often fail and frequently lead to a misdiagnosis of bipolar II disorder as MDD. This often condemns the patient to multiple failed trials of antidepressant monotherapy, and a delay in improvement, thus increasing the risk of job loss, disrupted relationships, and even suicide.
Over 3 decades, Dr. Akiskal developed the Mood Clinic Data Questionnaire (MCDQ) to systematize unstructured observations of patients presenting with a chief complaint of depression. His tool expedites the diagnosis of bipolar II disorder by understanding the patient as an individual, revealing personal and behavioral features consistent with what he labeled as episodic “hyperthymia” within the context of recurrent depression. This “social and behavioral phenotype,” as Dr. Akiskal called it, is rarely observed among patients with MDD.
By examining many patients with bipolar II disorder, Dr. Akiskal identified several “triads” of behavioral traits in the patients’ biographical history and in some of their close blood relatives as well. He also noticed that temperamentally, patients with bipolar II disorder thrive on “activity” and lovingly referred to themselves as “activity junkies.” Some of them may qualify as workaholics.
Biographical features that suggest bipolar II disorder
Here is a summary of the unique biographical features of patients with bipolar II disorder that Dr. Akiskal described:
Multilingual. Speaking ≥3 languages is unusual among individuals born in the United States, but often encountered among those with bipolar II disorder.
Continue to: Eminence
Eminence. Patients with bipolar II disorder, as well as their family members, tend to have leadership roles and prominence in journalism, media, and entertainment, fields that require interpersonal charm and eloquence. Those are common features of the “hyperthymic” temperament.
Creativity. Artists, poets, painters, and musicians who experience depression are more likely to have bipolar II disorder than MDD.
Biographical instability and/or excess. This is exemplified by going to 3 colleges and not necessarily obtaining a degree, or by frequently changing one’s line of work or city of residence. A classic example is a professor of medicine who also practices law and regularly sings in the opera, or a physician who is board-certified in 3 distinct specialties.
Activity junkies. Examples include a person with boundless energy, such as a novelist who writes 3 books a year or a professional who regularly works 12 hours a day without getting exhausted but seeks treatment for depressive episodes.
Multiple substances of abuse, such as nicotine, alcohol, stimulants, and opiates.
Continue to: Multiple psychiatric comorbidities
Multiple psychiatric comorbidities, such as having 3 types of anxiety (panic attacks, social phobia, and obsessive-compulsive disorder) or bulimia, seasonal depression, and anxiety.
Multiple pleasure-seeking or “outrageous” behaviors, such as compulsive gambling, sexual addiction, car racing, or skydiving. Another example is having a history of shoplifting, paraphilia, or arrest for participating in a riot, all of which are suggestive of antisocial traits in a patient seeking help for depression.
Sexual excesses, such as dating or having sex with ≥3 individuals concurrently, sometimes on the same day, or demanding sexual intercourse from a partner several times a day. Dr. Akiskal suggested that “sexual prowess” may represent an evolutionary advantage for the perpetuation of bipolar II disorder.
Marital history, such as a history of ≥3 marriages, or maintaining ≥2 families in different cities without being married.
Flamboyance and/or ornamentation. Examples might include wearing loud, colorful clothing (especially red), wearing ≥3 rings, or having piercings in ≥3 different body parts (tongue, nipples, navel, genitalia). Having elaborate tattoos across the body is no longer unique to “hyperthymic” persons with bipolar II disorder because tattoos have become far more common in the general population than they were in the 1970s. However, some take their tattoos to extremes.
Continue to: The above behaviors...
The above behaviors are condensed in a list that Dr. Akiskal called “the rule of 3” in patients with depression (Table1). Not all patients with bipolar II disorder will meet all the criteria of the rule of 3, but the first item in the mental status exam (appearance) alone may reflect the “soft bipolar spectrum,” such as garish clothing, red sneakers, multiple rings, bizarre hair coloring, and multiple piercings. This might prompt the clinician to ask further questions about hypomanic episodes as well as other personal behaviors related to the rule of 3.
Dr. Akiskal’s contributions to psychiatry are legendary in their originality, creativity, and clinical relevance. The rule of 3 is but one of his clinical concepts that may help identify many individuals with bipolar II disorder who are misdiagnosed as having MDD and prescribed a treatment that does not help or may exacerbate their illness course and worsen their outcome.
Based on the referrals of patients who are “treatment-resistant” to our Resident Mood Clinic, there are numerous persons in the country with bipolar II disorder (possibly millions) who are mislabeled with MDD and receiving the wrong treatments, to which they failed to respond. Their lifestyles and behaviors can provide valuable clinical insights into their true psychopathology, and that will lead to developing the right treatment plan.
1. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: the “red sign,” the “rule of three” and other biographic signs of temperamental extravagance, activation and hypomania. J Affect Disord. 2005;84(2-3):279-290.
1. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: the “red sign,” the “rule of three” and other biographic signs of temperamental extravagance, activation and hypomania. J Affect Disord. 2005;84(2-3):279-290.
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.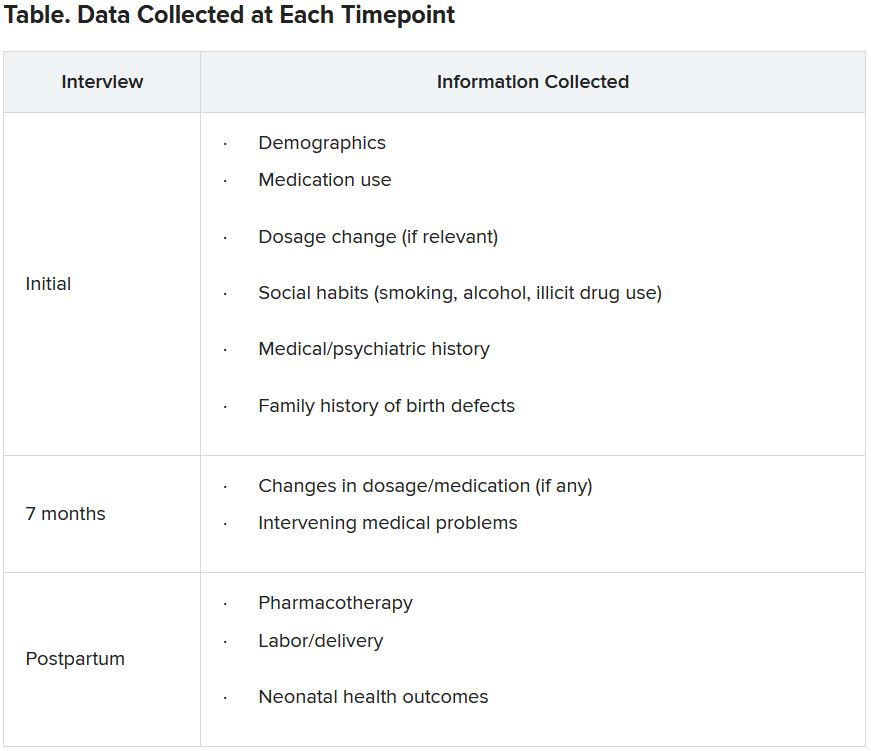
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.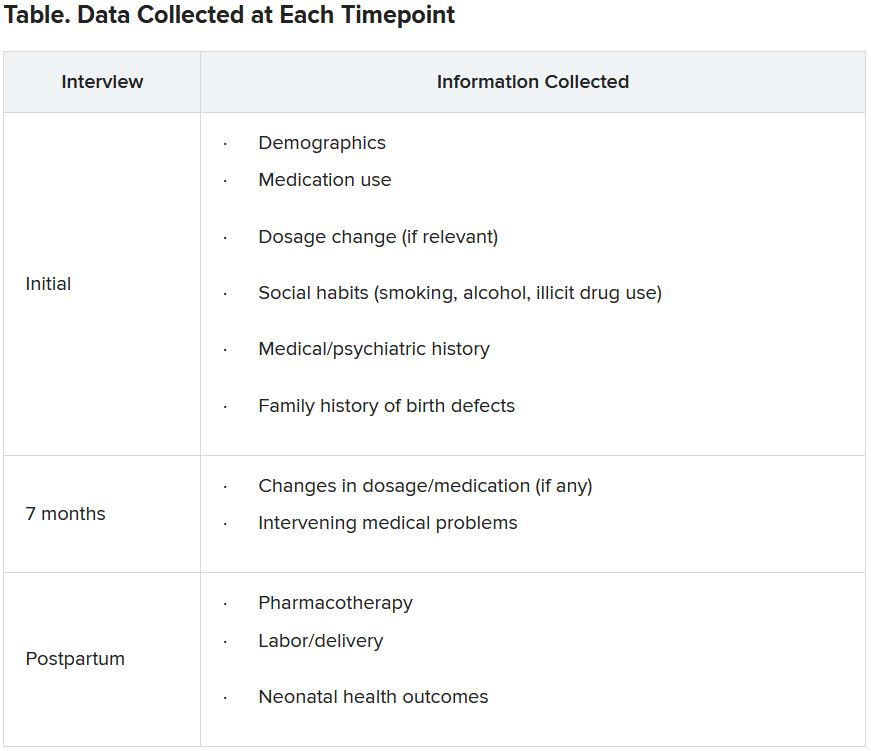
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.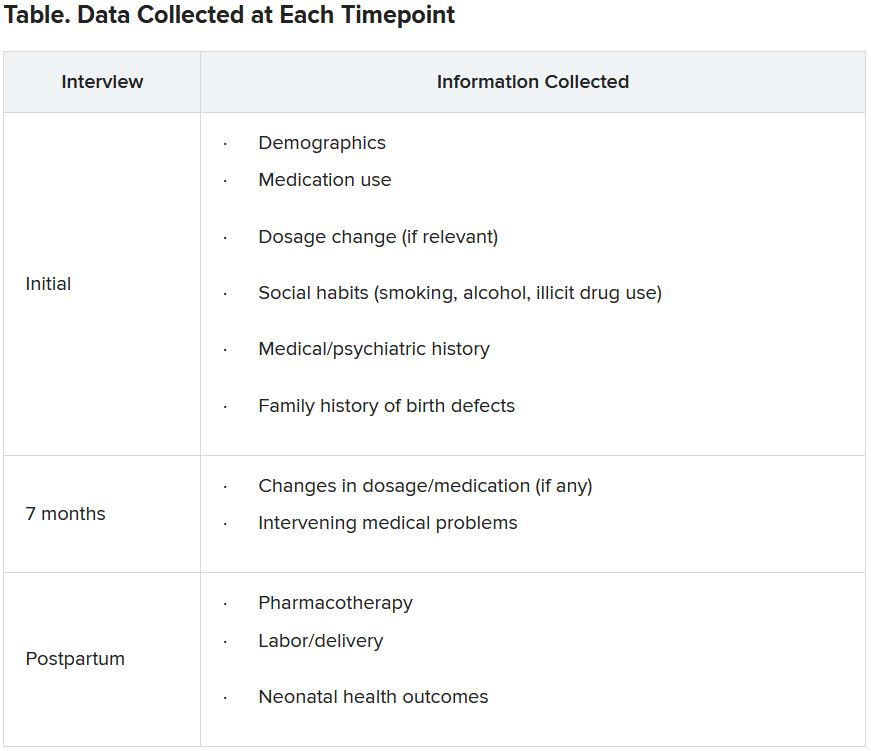
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.