User login
Inflation will be the end of medicine
Inflation is the senility of democracies.
–Sylvia Townsend Warner
Electronic medical records? No, all of these are minor annoyances in the face of the practice killer, inflation.
Physicians live in a closed box where medical reimbursements are fixed, directly or by contract proxy to the government (Medicare) pay rate. Inflation is projected to be between 5% and 10% this year. We cannot increase our rates to increase the salaries of our employees, cover our increased medical disposable costs, and pay more for our state licensures and DEA registrations. No, we must try to find savings in our budget, which we have been squeezing for years.
Currently, medicine is facing a 9.75% cut in Medicare reimbursements, which will reset most private insurance rates, based on a percentage of Medicare. The temporary 3.75% conversion factor (CF) increase for all services is expiring. Also expiring is the 2% sequester from the Budget Control Act of 2011 (BCA), signed into law in August 2011. This was originally scheduled to sunset in 2021, but is going to continue to 2030.
A 4% statutory pay-as-you-go (PAYGO) sequester resulting from passage of the American Rescue Plan Act is being imposed. Statutory PAYGO is a policy written into law (it can be changed only through new legislation) that requires deficit neutrality overall in the laws (other than annual appropriations) enacted by Congress and imposes automatic spending reductions at the end of the year if such laws increase the deficit when they are added together.
There is a statutory freeze on Medicare Physician Fee Schedule (PFS) updates until 2026, at which time an annual increase of 0.25%, which is lower than inflation, will be enacted. This adds up to a 9.75% cut in Medicare pay until at least 2026. Recall that almost all of your private insurance contracts are tied to Medicare (some more, some less) and that this cut to the physician is doubled if your overhead is fixed at the typical 50% for most practices. This means an almost 20% cut in take-home pay for most physicians.
Now, when considering the most recent inflation number, which projects 5%-10% inflation for this year and at least 2% annually in the future, which compounds yearly (the Fed target), you are looking at catastrophic numbers.
The conversion factor – the pool of money doled out to physicians – has failed to keep pace with inflation – even at 2%-3% a year – and reimbursement is only 50% of what it was when created in 1998, despite small increases by Congress along the way. A recent Wall Street Journal guest editorial claimed that Medicare payments benefited from cost of living adjustments, same as Social Security. I do not agree, hence the 50% pay gap since 1998.
In addition, the costs of running a practice have increased by 37% between 2001 and 2020, 1.7% per year, according to the Medicare Economic Index.
Some of this may include general inflation, but certainly new OSHA rules, electronic medical records, Medicare quality improvement measures, and assorted other costs do not. So based on my own conservative estimate, on top of the 50% decline in the payment pool, physicians’ noninflationary operating costs increased by at least another 10% over the last 20 odd years. This is a 60% decline in reimbursements!
Medicare payments have been under pressure from the Centers for Medicare & Medicaid Services (CMS) anti-inflationary payment policies for more than 20 years. While physician services represent a very modest portion of the overall growth in health care costs, they are an easy target for cuts when policymakers seek to limit spending. Although we avoided direct cuts to reimbursements caused by the Medicare sustainable growth rate formula (SGR) – which was enacted in 1997 and repealed in 2015 – Medicare provider payments have remained constrained by a budget-neutral financing system.
There used to be ways out of the box. Physicians could go to work for hospitals or have their practices acquired by them, resulting in much better hospital-based reimbursement. This has been eliminated by site-neutral payments, which while instituted by President Trump, are unopposed by President Biden. You could also join larger groups with some loss of autonomy, which could presumably negotiate better rates with private insurers as another way out, but these rates are almost always based on a percentage of Medicare as noted above.
There may be a bit of good news, with price transparency being instituted, which again is unopposed by the Biden administration. At least private practice physicians may be able to show their services are a bargain compared to hospitals.
One could also take the low road, and sell out to private equity, but I suspect these deals will become much less attractive since some of these entities are going broke and all will feel the bite of lower reimbursements.
Physicians and patients should rise up and demand better reimbursements for physicians, or there will be no physicians to see. This is not greed, a bigger house, or a newer car, this is becoming a matter of practice survival. And seniors are not greedy, they have paid hundreds of thousands of dollars into Medicare in taxes for health insurance in retirement.
Physicians and retirees should contact their federal legislators and let them know a 9.75% cut is untenable and ask for Medicare rates to be fixed to the cost of living, just as Social Security is. Before we fund trillions of dollars in new government programs, perhaps we should look to the solvency of the existing ones we have.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Inflation is the senility of democracies.
–Sylvia Townsend Warner
Electronic medical records? No, all of these are minor annoyances in the face of the practice killer, inflation.
Physicians live in a closed box where medical reimbursements are fixed, directly or by contract proxy to the government (Medicare) pay rate. Inflation is projected to be between 5% and 10% this year. We cannot increase our rates to increase the salaries of our employees, cover our increased medical disposable costs, and pay more for our state licensures and DEA registrations. No, we must try to find savings in our budget, which we have been squeezing for years.
Currently, medicine is facing a 9.75% cut in Medicare reimbursements, which will reset most private insurance rates, based on a percentage of Medicare. The temporary 3.75% conversion factor (CF) increase for all services is expiring. Also expiring is the 2% sequester from the Budget Control Act of 2011 (BCA), signed into law in August 2011. This was originally scheduled to sunset in 2021, but is going to continue to 2030.
A 4% statutory pay-as-you-go (PAYGO) sequester resulting from passage of the American Rescue Plan Act is being imposed. Statutory PAYGO is a policy written into law (it can be changed only through new legislation) that requires deficit neutrality overall in the laws (other than annual appropriations) enacted by Congress and imposes automatic spending reductions at the end of the year if such laws increase the deficit when they are added together.
There is a statutory freeze on Medicare Physician Fee Schedule (PFS) updates until 2026, at which time an annual increase of 0.25%, which is lower than inflation, will be enacted. This adds up to a 9.75% cut in Medicare pay until at least 2026. Recall that almost all of your private insurance contracts are tied to Medicare (some more, some less) and that this cut to the physician is doubled if your overhead is fixed at the typical 50% for most practices. This means an almost 20% cut in take-home pay for most physicians.
Now, when considering the most recent inflation number, which projects 5%-10% inflation for this year and at least 2% annually in the future, which compounds yearly (the Fed target), you are looking at catastrophic numbers.
The conversion factor – the pool of money doled out to physicians – has failed to keep pace with inflation – even at 2%-3% a year – and reimbursement is only 50% of what it was when created in 1998, despite small increases by Congress along the way. A recent Wall Street Journal guest editorial claimed that Medicare payments benefited from cost of living adjustments, same as Social Security. I do not agree, hence the 50% pay gap since 1998.
In addition, the costs of running a practice have increased by 37% between 2001 and 2020, 1.7% per year, according to the Medicare Economic Index.
Some of this may include general inflation, but certainly new OSHA rules, electronic medical records, Medicare quality improvement measures, and assorted other costs do not. So based on my own conservative estimate, on top of the 50% decline in the payment pool, physicians’ noninflationary operating costs increased by at least another 10% over the last 20 odd years. This is a 60% decline in reimbursements!
Medicare payments have been under pressure from the Centers for Medicare & Medicaid Services (CMS) anti-inflationary payment policies for more than 20 years. While physician services represent a very modest portion of the overall growth in health care costs, they are an easy target for cuts when policymakers seek to limit spending. Although we avoided direct cuts to reimbursements caused by the Medicare sustainable growth rate formula (SGR) – which was enacted in 1997 and repealed in 2015 – Medicare provider payments have remained constrained by a budget-neutral financing system.
There used to be ways out of the box. Physicians could go to work for hospitals or have their practices acquired by them, resulting in much better hospital-based reimbursement. This has been eliminated by site-neutral payments, which while instituted by President Trump, are unopposed by President Biden. You could also join larger groups with some loss of autonomy, which could presumably negotiate better rates with private insurers as another way out, but these rates are almost always based on a percentage of Medicare as noted above.
There may be a bit of good news, with price transparency being instituted, which again is unopposed by the Biden administration. At least private practice physicians may be able to show their services are a bargain compared to hospitals.
One could also take the low road, and sell out to private equity, but I suspect these deals will become much less attractive since some of these entities are going broke and all will feel the bite of lower reimbursements.
Physicians and patients should rise up and demand better reimbursements for physicians, or there will be no physicians to see. This is not greed, a bigger house, or a newer car, this is becoming a matter of practice survival. And seniors are not greedy, they have paid hundreds of thousands of dollars into Medicare in taxes for health insurance in retirement.
Physicians and retirees should contact their federal legislators and let them know a 9.75% cut is untenable and ask for Medicare rates to be fixed to the cost of living, just as Social Security is. Before we fund trillions of dollars in new government programs, perhaps we should look to the solvency of the existing ones we have.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Inflation is the senility of democracies.
–Sylvia Townsend Warner
Electronic medical records? No, all of these are minor annoyances in the face of the practice killer, inflation.
Physicians live in a closed box where medical reimbursements are fixed, directly or by contract proxy to the government (Medicare) pay rate. Inflation is projected to be between 5% and 10% this year. We cannot increase our rates to increase the salaries of our employees, cover our increased medical disposable costs, and pay more for our state licensures and DEA registrations. No, we must try to find savings in our budget, which we have been squeezing for years.
Currently, medicine is facing a 9.75% cut in Medicare reimbursements, which will reset most private insurance rates, based on a percentage of Medicare. The temporary 3.75% conversion factor (CF) increase for all services is expiring. Also expiring is the 2% sequester from the Budget Control Act of 2011 (BCA), signed into law in August 2011. This was originally scheduled to sunset in 2021, but is going to continue to 2030.
A 4% statutory pay-as-you-go (PAYGO) sequester resulting from passage of the American Rescue Plan Act is being imposed. Statutory PAYGO is a policy written into law (it can be changed only through new legislation) that requires deficit neutrality overall in the laws (other than annual appropriations) enacted by Congress and imposes automatic spending reductions at the end of the year if such laws increase the deficit when they are added together.
There is a statutory freeze on Medicare Physician Fee Schedule (PFS) updates until 2026, at which time an annual increase of 0.25%, which is lower than inflation, will be enacted. This adds up to a 9.75% cut in Medicare pay until at least 2026. Recall that almost all of your private insurance contracts are tied to Medicare (some more, some less) and that this cut to the physician is doubled if your overhead is fixed at the typical 50% for most practices. This means an almost 20% cut in take-home pay for most physicians.
Now, when considering the most recent inflation number, which projects 5%-10% inflation for this year and at least 2% annually in the future, which compounds yearly (the Fed target), you are looking at catastrophic numbers.
The conversion factor – the pool of money doled out to physicians – has failed to keep pace with inflation – even at 2%-3% a year – and reimbursement is only 50% of what it was when created in 1998, despite small increases by Congress along the way. A recent Wall Street Journal guest editorial claimed that Medicare payments benefited from cost of living adjustments, same as Social Security. I do not agree, hence the 50% pay gap since 1998.
In addition, the costs of running a practice have increased by 37% between 2001 and 2020, 1.7% per year, according to the Medicare Economic Index.
Some of this may include general inflation, but certainly new OSHA rules, electronic medical records, Medicare quality improvement measures, and assorted other costs do not. So based on my own conservative estimate, on top of the 50% decline in the payment pool, physicians’ noninflationary operating costs increased by at least another 10% over the last 20 odd years. This is a 60% decline in reimbursements!
Medicare payments have been under pressure from the Centers for Medicare & Medicaid Services (CMS) anti-inflationary payment policies for more than 20 years. While physician services represent a very modest portion of the overall growth in health care costs, they are an easy target for cuts when policymakers seek to limit spending. Although we avoided direct cuts to reimbursements caused by the Medicare sustainable growth rate formula (SGR) – which was enacted in 1997 and repealed in 2015 – Medicare provider payments have remained constrained by a budget-neutral financing system.
There used to be ways out of the box. Physicians could go to work for hospitals or have their practices acquired by them, resulting in much better hospital-based reimbursement. This has been eliminated by site-neutral payments, which while instituted by President Trump, are unopposed by President Biden. You could also join larger groups with some loss of autonomy, which could presumably negotiate better rates with private insurers as another way out, but these rates are almost always based on a percentage of Medicare as noted above.
There may be a bit of good news, with price transparency being instituted, which again is unopposed by the Biden administration. At least private practice physicians may be able to show their services are a bargain compared to hospitals.
One could also take the low road, and sell out to private equity, but I suspect these deals will become much less attractive since some of these entities are going broke and all will feel the bite of lower reimbursements.
Physicians and patients should rise up and demand better reimbursements for physicians, or there will be no physicians to see. This is not greed, a bigger house, or a newer car, this is becoming a matter of practice survival. And seniors are not greedy, they have paid hundreds of thousands of dollars into Medicare in taxes for health insurance in retirement.
Physicians and retirees should contact their federal legislators and let them know a 9.75% cut is untenable and ask for Medicare rates to be fixed to the cost of living, just as Social Security is. Before we fund trillions of dollars in new government programs, perhaps we should look to the solvency of the existing ones we have.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Connecticut chapter of ACC at center of Twitter dustup
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Doctor wins restraining order against CVS after prescription ban
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
Medicinal liquor and edited mosquitoes
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
Drink to your health?
Whether you drink or not, most of us can agree that liquor is not the first thing that comes to mind when looking to make health improvements. But researchers have found a small exception in something traditional.
We’ve added buckwheat to pancakes, bread, and other baked goodies we made during the height of quarantine, but it’s also used to create a traditional liquor in some East Asian countries, where it is used medicinally.
Investigators have found that extracts in the Tartary buckwheat used to make the liquor induce autophagy, a process cells go through to remove proteins that are damaged or not needed anymore – sort of like a cellular spring cleaning.
To test this, the researchers treated liver and skin cells with Tartary buckwheat extract and looked to see how the cells responded with fluorescent markers. The results were clear.
“Treating cells with the extract stimulated the formation of autophagosomes, specialized cellular structures that carry out autophagy, and altered the location of proteins involved in regulating autophagy,” said senior author Takeshi Noda of Osaka (Japan) University.
Looking deeper, the researchers found that quercetin, a component of the buckwheat extract, had the same autophagic effect. And both the buckwheat and the quercetin gave the green light for liver cells to induce aggrephagy, the process of cleaning up protein aggregates.
Those protein aggregates in liver cells are closely linked to alcoholic liver disease, suggesting that quercetin could be a game changer in its treatment. In other words, liquor could help fix the problem that liquor started. Go figure.
From hospital bills to X-rated
Ralph Puglisi was an accounting manager for the University Medical Service Association (UMSA), a nonprofit that supports the massive University of South Florida health system. The association took in over $300 million in revenue in the 2019-2020 fiscal year, which is a rather large sum of money, but we’ll glide over the ethics of a “nonprofit” making a few hundred million for now.
Mr. Puglisi was in very close proximity to the money, generated from patient care, and he pled guilty to stealing it using UMSA credit cards. Now, that wouldn’t be LOTME worthy on its own, but what elevates this above garden-variety embezzlement is how the intrepid Mr. Puglisi chose to spend the millions he stole from the university health system: Adult entertainment.
And before you ask, he didn’t spend $11.5 million on something most people so inclined can find for free with judicious Google searches. What Mr. Puglisi actually did was invest in a website providing adult content through individual user profiles, one of which is believed to belong to his stepson’s fiancée, which brings a whole new level of sleaze to this enterprise. Over the course of 2 years, he visited her profile 2,800 times, an amount some might view as excessive.
While the vast majority of the embezzled money went to the adult website, Mr. Puglisi also used thousands of UMSA dollars to pay for travel, household improvements, rent, the works. Almost $44,000 was spent at a resort sometimes known as the happiest place on earth.
Then there’s Mr. Puglisi’s wife. Oh yes, this guy is married. He poured over $600,000 into a company he and his wife owned, which is a lot, but how much do you think went to the woman he married? Probably quite a bit. Go ahead, try to think of a number. It’s not like it was his money.
Did you guess $100 went into his wife’s PayPal account? No? Clearly you don’t understand the criminal mind. His stepson’s fiancée got millions, and his wife got a hundred. Now there are some priorities.
Step 1: Sit at desk. Step 2: Get in shape
Being a physician is not really a desk job, but doctors must spend a fair share of their time sitting, yes? Dealing with recalcitrant EHRs or talking on the phone to insurers or PBMs? If you are one of these physicians, or if you have patients who spend a lot of time sitting at their desks and might need to get a bit of exercise, then we’ve got a multitasking tip for you.
It came to us via one of our favorite websites, Sad and Useless. It’s the site that declares itself “the most depressive humor site on the Internet” and they’re offering up the “12 Best Exercises To Do At Your Desk.” It may not sound like much, but we think that the gang at Dunder-Mifflin would approve. And besides, who couldn’t stand to burn a few calories without having to leave the chair?
We won’t spoil your fun by going through all 12 – each one comes with step-by-step instructions and a helpful illustration or GIF – but here are just a few:
- Bending over backwards: “Agree to do something you don’t want to do. Spend twice as long as expected doing that thing. Hate yourself.”
- Fake laughter: “Hear a joke that isn’t even remotely funny. Open your mouth and make laughing sounds.”
- Bang your head: Feel the “pointlessness of your job overwhelm you” and then “bring your head forcefully down to your desk.”
Now, we here at LOTME are, of course [Bang!], highly skilled, professional wordsmithing humorists [Bang!], so when we tell you that this is a great workout [Bang!] … that this is a great workout [Bang!] … it’s great … uggh.
Wooooo. Feel the burn.
One order of mosquitoes, extra Crispr
What would it be like to have a barbecue in your backyard on a humid summer night and not get eaten alive by mosquitoes? If you’re like us, you probably thought you’d never see that day.
Mosquitoes cause itchy bites, but, more importantly, they can carry dengue, malaria, yellow fever, and Zika virus. New research shows that protection from these diseases may be possible with use of the Crispr-Cas9 gene-editing tool, which could make humans invisible to mosquitoes by taking away their light-sensing abilities and, thus, their ability to find us.
“The better we understand how they sense the human, the better we can control the mosquito in an eco-friendly manner,” Yinpeng Zhan, a postdoctoral researcher at the University of California, Santa Barbara, and the study’s lead author, told the New York Times.
After studying the mosquitoes and figuring out their hunting patterns, the researchers found that mosquitoes are attracted to dark spots more than white spots and used this to their advantage. After knocking out two of the proteins that mosquitoes need for vision – via Crispr – the little suckers could not distinguish the difference between the white and dark spots.
We’re sure mosquitoes don’t mean any harm – they’re just trying to survive and reproduce like any other species – but thanks to this new tool, gone might be the days of having to douse yourself in bug spray that smells like a mix of chemicals and melon.
The hateful patient
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Psychiatrists’ income, wealth gain ground despite COVID-19 challenges
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Outstanding medical bills: Dealing with deadbeats
Since the COVID-19 pandemic began, I have received a growing number of inquiries about collection issues. For a variety of reasons, many patients seem increasingly reluctant to pay their medical bills. I’ve written many columns on keeping credit card numbers on file, and other techniques for keeping your accounts receivable in check; but despite your best efforts, there will always be a few deadbeats that you will need to pursue.
For the record, I am not speaking about patients who lost income due to the pandemic and are now struggling with debts, or otherwise have fallen on hard times and are unable to pay.
The worst kinds of deadbeats are the ones who rob you twice; they accept payments from insurance companies and keep them. Such crooks must be pursued aggressively, with all the means at your disposal; but to reiterate the point I’ve tried to drive home repeatedly, the best cure is prevention.
You already know that you should collect as many fees as possible at the time of service. For cosmetic procedures you should require a substantial deposit in advance, with the balance due at the time of service. When that is impossible, maximize the chances you will be paid by making sure all available payment mechanisms are in place.
With my credit-card-on-file system that I’ve described many times, patients who fail to pay their credit card bill are the credit card company’s problem, not yours. In cases where you suspect fees might exceed credit card limits, you can arrange a realistic payment schedule in advance and have the patient fill out a credit application. You can find forms for this online at formswift.com, templates.office.com, and many other websites.
In some cases, it may be worth the trouble to run a background check. There are easy and affordable ways to do this. Dunn & Bradstreet, for example, will furnish a report containing payment records and details of any lawsuits, liens, and other legal actions for a nominal fee. The more financial information you have on file, the more leverage you have if a patient later balks at paying his or her balance.
For cosmetic work, always take before and after photos, and have all patients sign a written consent giving permission for the procedure, assuming full financial responsibility, and acknowledging that no guarantees have been given or implied. This defuses the common deadbeat tactics of claiming ignorance of personal financial obligations and professing dissatisfaction with the results.
Despite all your precautions, a deadbeat will inevitably slip through on occasion; but even then, you have options for extracting payment. Collection agencies are the traditional first line of attack for most medical practices. Ideally, your agency should specialize in handling medical accounts, so it will know exactly how much pressure to exert to avoid charges of harassment. Delinquent accounts should be submitted earlier rather than later to maximize the chances of success; my manager never allows an account to age more than 90 days, and if circumstances dictate, she refers them sooner than that.
When collection agencies fail, think about small claims court. You will need to learn the rules in your state, but in most states there is a small filing fee and a limit of $5,000 or so on claims. No attorneys are involved. If your paperwork is in order, the court will nearly always rule in your favor, but it will not provide the means for actual collection. In other words, you will still have to persuade the deadbeat to pay up. However, in many states a court order will give you the authority to attach a lien to property, or garnish wages, which often provides enough leverage to force payment.
What about those double-deadbeats who keep the insurance checks for themselves? First, check your third-party contract; sometimes the insurance company or HMO will be compelled to pay you directly and then go after the patient to get back its money. (They won’t volunteer this service, however – you’ll have to ask for it.)
If that’s not an option, consider reporting the misdirected payment to the Internal Revenue Service as income to the patient, by submitting a 1099 Miscellaneous Income form. Be sure to notify the deadbeat that you will be doing this. Sometimes the threat of such action will convince the individual to pay up; if not, at least you’ll have the satisfaction of knowing he or she will have to pay taxes on the money.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Since the COVID-19 pandemic began, I have received a growing number of inquiries about collection issues. For a variety of reasons, many patients seem increasingly reluctant to pay their medical bills. I’ve written many columns on keeping credit card numbers on file, and other techniques for keeping your accounts receivable in check; but despite your best efforts, there will always be a few deadbeats that you will need to pursue.
For the record, I am not speaking about patients who lost income due to the pandemic and are now struggling with debts, or otherwise have fallen on hard times and are unable to pay.
The worst kinds of deadbeats are the ones who rob you twice; they accept payments from insurance companies and keep them. Such crooks must be pursued aggressively, with all the means at your disposal; but to reiterate the point I’ve tried to drive home repeatedly, the best cure is prevention.
You already know that you should collect as many fees as possible at the time of service. For cosmetic procedures you should require a substantial deposit in advance, with the balance due at the time of service. When that is impossible, maximize the chances you will be paid by making sure all available payment mechanisms are in place.
With my credit-card-on-file system that I’ve described many times, patients who fail to pay their credit card bill are the credit card company’s problem, not yours. In cases where you suspect fees might exceed credit card limits, you can arrange a realistic payment schedule in advance and have the patient fill out a credit application. You can find forms for this online at formswift.com, templates.office.com, and many other websites.
In some cases, it may be worth the trouble to run a background check. There are easy and affordable ways to do this. Dunn & Bradstreet, for example, will furnish a report containing payment records and details of any lawsuits, liens, and other legal actions for a nominal fee. The more financial information you have on file, the more leverage you have if a patient later balks at paying his or her balance.
For cosmetic work, always take before and after photos, and have all patients sign a written consent giving permission for the procedure, assuming full financial responsibility, and acknowledging that no guarantees have been given or implied. This defuses the common deadbeat tactics of claiming ignorance of personal financial obligations and professing dissatisfaction with the results.
Despite all your precautions, a deadbeat will inevitably slip through on occasion; but even then, you have options for extracting payment. Collection agencies are the traditional first line of attack for most medical practices. Ideally, your agency should specialize in handling medical accounts, so it will know exactly how much pressure to exert to avoid charges of harassment. Delinquent accounts should be submitted earlier rather than later to maximize the chances of success; my manager never allows an account to age more than 90 days, and if circumstances dictate, she refers them sooner than that.
When collection agencies fail, think about small claims court. You will need to learn the rules in your state, but in most states there is a small filing fee and a limit of $5,000 or so on claims. No attorneys are involved. If your paperwork is in order, the court will nearly always rule in your favor, but it will not provide the means for actual collection. In other words, you will still have to persuade the deadbeat to pay up. However, in many states a court order will give you the authority to attach a lien to property, or garnish wages, which often provides enough leverage to force payment.
What about those double-deadbeats who keep the insurance checks for themselves? First, check your third-party contract; sometimes the insurance company or HMO will be compelled to pay you directly and then go after the patient to get back its money. (They won’t volunteer this service, however – you’ll have to ask for it.)
If that’s not an option, consider reporting the misdirected payment to the Internal Revenue Service as income to the patient, by submitting a 1099 Miscellaneous Income form. Be sure to notify the deadbeat that you will be doing this. Sometimes the threat of such action will convince the individual to pay up; if not, at least you’ll have the satisfaction of knowing he or she will have to pay taxes on the money.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Since the COVID-19 pandemic began, I have received a growing number of inquiries about collection issues. For a variety of reasons, many patients seem increasingly reluctant to pay their medical bills. I’ve written many columns on keeping credit card numbers on file, and other techniques for keeping your accounts receivable in check; but despite your best efforts, there will always be a few deadbeats that you will need to pursue.
For the record, I am not speaking about patients who lost income due to the pandemic and are now struggling with debts, or otherwise have fallen on hard times and are unable to pay.
The worst kinds of deadbeats are the ones who rob you twice; they accept payments from insurance companies and keep them. Such crooks must be pursued aggressively, with all the means at your disposal; but to reiterate the point I’ve tried to drive home repeatedly, the best cure is prevention.
You already know that you should collect as many fees as possible at the time of service. For cosmetic procedures you should require a substantial deposit in advance, with the balance due at the time of service. When that is impossible, maximize the chances you will be paid by making sure all available payment mechanisms are in place.
With my credit-card-on-file system that I’ve described many times, patients who fail to pay their credit card bill are the credit card company’s problem, not yours. In cases where you suspect fees might exceed credit card limits, you can arrange a realistic payment schedule in advance and have the patient fill out a credit application. You can find forms for this online at formswift.com, templates.office.com, and many other websites.
In some cases, it may be worth the trouble to run a background check. There are easy and affordable ways to do this. Dunn & Bradstreet, for example, will furnish a report containing payment records and details of any lawsuits, liens, and other legal actions for a nominal fee. The more financial information you have on file, the more leverage you have if a patient later balks at paying his or her balance.
For cosmetic work, always take before and after photos, and have all patients sign a written consent giving permission for the procedure, assuming full financial responsibility, and acknowledging that no guarantees have been given or implied. This defuses the common deadbeat tactics of claiming ignorance of personal financial obligations and professing dissatisfaction with the results.
Despite all your precautions, a deadbeat will inevitably slip through on occasion; but even then, you have options for extracting payment. Collection agencies are the traditional first line of attack for most medical practices. Ideally, your agency should specialize in handling medical accounts, so it will know exactly how much pressure to exert to avoid charges of harassment. Delinquent accounts should be submitted earlier rather than later to maximize the chances of success; my manager never allows an account to age more than 90 days, and if circumstances dictate, she refers them sooner than that.
When collection agencies fail, think about small claims court. You will need to learn the rules in your state, but in most states there is a small filing fee and a limit of $5,000 or so on claims. No attorneys are involved. If your paperwork is in order, the court will nearly always rule in your favor, but it will not provide the means for actual collection. In other words, you will still have to persuade the deadbeat to pay up. However, in many states a court order will give you the authority to attach a lien to property, or garnish wages, which often provides enough leverage to force payment.
What about those double-deadbeats who keep the insurance checks for themselves? First, check your third-party contract; sometimes the insurance company or HMO will be compelled to pay you directly and then go after the patient to get back its money. (They won’t volunteer this service, however – you’ll have to ask for it.)
If that’s not an option, consider reporting the misdirected payment to the Internal Revenue Service as income to the patient, by submitting a 1099 Miscellaneous Income form. Be sure to notify the deadbeat that you will be doing this. Sometimes the threat of such action will convince the individual to pay up; if not, at least you’ll have the satisfaction of knowing he or she will have to pay taxes on the money.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Walking through time
In the Phoenix summer days of 1998 I did a lot of walking. It wasn’t for exercise, though it was pretty good for that, I guess.
I had privileges at three hospitals, and used their staff directories to make a map of every medical office building in the area I was trying to start my practice in. I was 32, idealistic, married for a year, a child on the way, and we’d just bought our first house. So I had a lot of incentive.
The Phoenix summer isn’t conducive to walking, especially in standard medical office attire (I didn’t give that up until 2006). But I did it. I went into one office after another, introduced myself, gave them my CV, some business cards, and my pager number (yeah, I had a pager). I cooled off and drank water in my car as I drove to the next building – wash, rinse, repeat.
Occasionally the doctors I met would have a few minutes to meet me, which I appreciated. One of them, who’d been in the same boat a few years earlier himself, invited me back to his office, and we chatted for maybe 10 minutes.
We got along, and worked well together for several years. We tended to round at the same times of day and so ran into each other a lot. He sent me patients, I sent him patients, and when we met on rounds we’d talk about nothing in particular for a few minutes.
After I cut back on my hospital work I didn’t see him as much, though we still referred patients back and forth and occasionally crossed paths while covering weekends.
I found out that he retired recently.
It gave me an odd pause. I thought of our first encounter 23 years ago, me trying to get started in my profession, him established, but close enough to recall what it was like to be starting out that he spared a few minutes for me. Remembering that, I still try to make an effort to meet new physicians who come by for the same reason. Hell, they might end up taking care of me someday. Assuming a medical career is 30-40 years, I’m past the halfway point.
Not today, not tomorrow, but in the years to come my generation of physicians will start to retire, walking away from a role that has defined both our personal and professional lives.
I both am and am not looking forward to it. This was just another reminder that .
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the Phoenix summer days of 1998 I did a lot of walking. It wasn’t for exercise, though it was pretty good for that, I guess.
I had privileges at three hospitals, and used their staff directories to make a map of every medical office building in the area I was trying to start my practice in. I was 32, idealistic, married for a year, a child on the way, and we’d just bought our first house. So I had a lot of incentive.
The Phoenix summer isn’t conducive to walking, especially in standard medical office attire (I didn’t give that up until 2006). But I did it. I went into one office after another, introduced myself, gave them my CV, some business cards, and my pager number (yeah, I had a pager). I cooled off and drank water in my car as I drove to the next building – wash, rinse, repeat.
Occasionally the doctors I met would have a few minutes to meet me, which I appreciated. One of them, who’d been in the same boat a few years earlier himself, invited me back to his office, and we chatted for maybe 10 minutes.
We got along, and worked well together for several years. We tended to round at the same times of day and so ran into each other a lot. He sent me patients, I sent him patients, and when we met on rounds we’d talk about nothing in particular for a few minutes.
After I cut back on my hospital work I didn’t see him as much, though we still referred patients back and forth and occasionally crossed paths while covering weekends.
I found out that he retired recently.
It gave me an odd pause. I thought of our first encounter 23 years ago, me trying to get started in my profession, him established, but close enough to recall what it was like to be starting out that he spared a few minutes for me. Remembering that, I still try to make an effort to meet new physicians who come by for the same reason. Hell, they might end up taking care of me someday. Assuming a medical career is 30-40 years, I’m past the halfway point.
Not today, not tomorrow, but in the years to come my generation of physicians will start to retire, walking away from a role that has defined both our personal and professional lives.
I both am and am not looking forward to it. This was just another reminder that .
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the Phoenix summer days of 1998 I did a lot of walking. It wasn’t for exercise, though it was pretty good for that, I guess.
I had privileges at three hospitals, and used their staff directories to make a map of every medical office building in the area I was trying to start my practice in. I was 32, idealistic, married for a year, a child on the way, and we’d just bought our first house. So I had a lot of incentive.
The Phoenix summer isn’t conducive to walking, especially in standard medical office attire (I didn’t give that up until 2006). But I did it. I went into one office after another, introduced myself, gave them my CV, some business cards, and my pager number (yeah, I had a pager). I cooled off and drank water in my car as I drove to the next building – wash, rinse, repeat.
Occasionally the doctors I met would have a few minutes to meet me, which I appreciated. One of them, who’d been in the same boat a few years earlier himself, invited me back to his office, and we chatted for maybe 10 minutes.
We got along, and worked well together for several years. We tended to round at the same times of day and so ran into each other a lot. He sent me patients, I sent him patients, and when we met on rounds we’d talk about nothing in particular for a few minutes.
After I cut back on my hospital work I didn’t see him as much, though we still referred patients back and forth and occasionally crossed paths while covering weekends.
I found out that he retired recently.
It gave me an odd pause. I thought of our first encounter 23 years ago, me trying to get started in my profession, him established, but close enough to recall what it was like to be starting out that he spared a few minutes for me. Remembering that, I still try to make an effort to meet new physicians who come by for the same reason. Hell, they might end up taking care of me someday. Assuming a medical career is 30-40 years, I’m past the halfway point.
Not today, not tomorrow, but in the years to come my generation of physicians will start to retire, walking away from a role that has defined both our personal and professional lives.
I both am and am not looking forward to it. This was just another reminder that .
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Endocrinologists’ wealth remains steady, despite pandemic
Despite ongoing pandemic-related economic challenges, endocrinologists report stability in their overall wealth in the past year, with more than a third of the specialists having a net worth between $1 million and $5 million, according to the Medscape Endocrinologist Wealth & Debt Report 2021.
The findings regarding wealth and debt among endocrinologists, along with 28 other specialties, were reported as part of Medscape’s Physician Compensation Report 2021, which included nearly 18,000 physicians.
According to the report, endocrinologists had an upswing in their income, compared with the prior year, with average annual earnings of $245,000 versus $236,000 in 2020. The earnings tie them with infectious disease specialists at fourth from the bottom of the list of specialties.
In the latest report, 38% reported a net worth between $1 million and $5 million, down 1% from 39% in last year’s report.
Nine percent of endocrinologists had a net worth of over $5 million, matching last year’s rate.
That puts endocrinologists and rheumatologists near the middle of specialists earning more than $5 million. Dermatologists rank the highest, with 28% worth over $5 million. Allergy and immunology specialists are at the bottom of the list, with just 2%.
Joel Greenwald, MD, a wealth management advisor to physicians based in St. Louis Park, Minn., said the reasons for the stability in wealth are multifactorial.
“The rise in home prices is certainly a factor,” he said. “Definitely the rise in the stock market played a large role; the S&P 500 finished the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth,” Dr. Greenwald added. “They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on [during lockdowns].”
The percentage of endocrinologists reporting a net worth below $500,000 decreased from 37% in 2020 to 31% for the current report, placing them fifth from the top of the list of specialists with a net worth below $500,000. Family medicine was at the top of the list, at 40%.
Gender disparities in net worth are striking
The gender disparities in net worth among endocrinologists are substantial. Although only 15% of male endocrinologists have a net worth of less than $500,000, that rate is nearly three times higher – 44% – for female endocrinologists.
Twenty-seven percent of male endocrinologists have a net worth between $1 million and $2 million, compared with just 13% among women. Although 14% of men have a net worth of more than $5 million, only 4% of female endocrinologists fall in that category.
Of note, 61% of those who responded to the poll were men; 36% were women.
Expenses, savings
Only 6% of endocrinologists reported being unable to pay their mortgage as a result of the pandemic; 8% said they were unable to pay other bills because of COVID-19.
The vast majority, however – 91% – said the pandemic did not affect their ability to pay bills or their mortgage. U.S. Census Bureau data from last July show that about a quarter of adults (25.3%) missed a mortgage or rent payment because of challenges related to COVID-19.
Approximately three-quarters of endocrinologists (72%) reported having not made any changes to reduce major expenses in 2020, despite the pandemic. About 25% took significant measures to reduce expenses, including refinancing their house or moving to a different home.
Seventeen percent say they are still paying off their school loans, similar to the rate last year.
The report notes that, according to the Association of American Medical Colleges, the average medical school debt for students who graduated in 2019 was $201,490, compared with an average student loan debt for all graduating students in the same year of $28,950.
Although 65% of endocrinologists said they added the same amount to their 401(k) plan in the past year, 28% put less into their fund, and although 53% put the same amount into their taxable savings account, 23% reported not using the taxable savings accounts at all.
Although earnings were steady in the past year, 12% of endocrinologists report having losses from practice problems, compared with 5% the previous year. COVID-19 was the most common cause. The proportion reporting no financial losses declined to 65%, versus 75% in the last report.
A version of this article first appeared on Medscape.com.
Despite ongoing pandemic-related economic challenges, endocrinologists report stability in their overall wealth in the past year, with more than a third of the specialists having a net worth between $1 million and $5 million, according to the Medscape Endocrinologist Wealth & Debt Report 2021.
The findings regarding wealth and debt among endocrinologists, along with 28 other specialties, were reported as part of Medscape’s Physician Compensation Report 2021, which included nearly 18,000 physicians.
According to the report, endocrinologists had an upswing in their income, compared with the prior year, with average annual earnings of $245,000 versus $236,000 in 2020. The earnings tie them with infectious disease specialists at fourth from the bottom of the list of specialties.
In the latest report, 38% reported a net worth between $1 million and $5 million, down 1% from 39% in last year’s report.
Nine percent of endocrinologists had a net worth of over $5 million, matching last year’s rate.
That puts endocrinologists and rheumatologists near the middle of specialists earning more than $5 million. Dermatologists rank the highest, with 28% worth over $5 million. Allergy and immunology specialists are at the bottom of the list, with just 2%.
Joel Greenwald, MD, a wealth management advisor to physicians based in St. Louis Park, Minn., said the reasons for the stability in wealth are multifactorial.
“The rise in home prices is certainly a factor,” he said. “Definitely the rise in the stock market played a large role; the S&P 500 finished the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth,” Dr. Greenwald added. “They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on [during lockdowns].”
The percentage of endocrinologists reporting a net worth below $500,000 decreased from 37% in 2020 to 31% for the current report, placing them fifth from the top of the list of specialists with a net worth below $500,000. Family medicine was at the top of the list, at 40%.
Gender disparities in net worth are striking
The gender disparities in net worth among endocrinologists are substantial. Although only 15% of male endocrinologists have a net worth of less than $500,000, that rate is nearly three times higher – 44% – for female endocrinologists.
Twenty-seven percent of male endocrinologists have a net worth between $1 million and $2 million, compared with just 13% among women. Although 14% of men have a net worth of more than $5 million, only 4% of female endocrinologists fall in that category.
Of note, 61% of those who responded to the poll were men; 36% were women.
Expenses, savings
Only 6% of endocrinologists reported being unable to pay their mortgage as a result of the pandemic; 8% said they were unable to pay other bills because of COVID-19.
The vast majority, however – 91% – said the pandemic did not affect their ability to pay bills or their mortgage. U.S. Census Bureau data from last July show that about a quarter of adults (25.3%) missed a mortgage or rent payment because of challenges related to COVID-19.
Approximately three-quarters of endocrinologists (72%) reported having not made any changes to reduce major expenses in 2020, despite the pandemic. About 25% took significant measures to reduce expenses, including refinancing their house or moving to a different home.
Seventeen percent say they are still paying off their school loans, similar to the rate last year.
The report notes that, according to the Association of American Medical Colleges, the average medical school debt for students who graduated in 2019 was $201,490, compared with an average student loan debt for all graduating students in the same year of $28,950.
Although 65% of endocrinologists said they added the same amount to their 401(k) plan in the past year, 28% put less into their fund, and although 53% put the same amount into their taxable savings account, 23% reported not using the taxable savings accounts at all.
Although earnings were steady in the past year, 12% of endocrinologists report having losses from practice problems, compared with 5% the previous year. COVID-19 was the most common cause. The proportion reporting no financial losses declined to 65%, versus 75% in the last report.
A version of this article first appeared on Medscape.com.
Despite ongoing pandemic-related economic challenges, endocrinologists report stability in their overall wealth in the past year, with more than a third of the specialists having a net worth between $1 million and $5 million, according to the Medscape Endocrinologist Wealth & Debt Report 2021.
The findings regarding wealth and debt among endocrinologists, along with 28 other specialties, were reported as part of Medscape’s Physician Compensation Report 2021, which included nearly 18,000 physicians.
According to the report, endocrinologists had an upswing in their income, compared with the prior year, with average annual earnings of $245,000 versus $236,000 in 2020. The earnings tie them with infectious disease specialists at fourth from the bottom of the list of specialties.
In the latest report, 38% reported a net worth between $1 million and $5 million, down 1% from 39% in last year’s report.
Nine percent of endocrinologists had a net worth of over $5 million, matching last year’s rate.
That puts endocrinologists and rheumatologists near the middle of specialists earning more than $5 million. Dermatologists rank the highest, with 28% worth over $5 million. Allergy and immunology specialists are at the bottom of the list, with just 2%.
Joel Greenwald, MD, a wealth management advisor to physicians based in St. Louis Park, Minn., said the reasons for the stability in wealth are multifactorial.
“The rise in home prices is certainly a factor,” he said. “Definitely the rise in the stock market played a large role; the S&P 500 finished the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth,” Dr. Greenwald added. “They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on [during lockdowns].”
The percentage of endocrinologists reporting a net worth below $500,000 decreased from 37% in 2020 to 31% for the current report, placing them fifth from the top of the list of specialists with a net worth below $500,000. Family medicine was at the top of the list, at 40%.
Gender disparities in net worth are striking
The gender disparities in net worth among endocrinologists are substantial. Although only 15% of male endocrinologists have a net worth of less than $500,000, that rate is nearly three times higher – 44% – for female endocrinologists.
Twenty-seven percent of male endocrinologists have a net worth between $1 million and $2 million, compared with just 13% among women. Although 14% of men have a net worth of more than $5 million, only 4% of female endocrinologists fall in that category.
Of note, 61% of those who responded to the poll were men; 36% were women.
Expenses, savings
Only 6% of endocrinologists reported being unable to pay their mortgage as a result of the pandemic; 8% said they were unable to pay other bills because of COVID-19.
The vast majority, however – 91% – said the pandemic did not affect their ability to pay bills or their mortgage. U.S. Census Bureau data from last July show that about a quarter of adults (25.3%) missed a mortgage or rent payment because of challenges related to COVID-19.
Approximately three-quarters of endocrinologists (72%) reported having not made any changes to reduce major expenses in 2020, despite the pandemic. About 25% took significant measures to reduce expenses, including refinancing their house or moving to a different home.
Seventeen percent say they are still paying off their school loans, similar to the rate last year.
The report notes that, according to the Association of American Medical Colleges, the average medical school debt for students who graduated in 2019 was $201,490, compared with an average student loan debt for all graduating students in the same year of $28,950.
Although 65% of endocrinologists said they added the same amount to their 401(k) plan in the past year, 28% put less into their fund, and although 53% put the same amount into their taxable savings account, 23% reported not using the taxable savings accounts at all.
Although earnings were steady in the past year, 12% of endocrinologists report having losses from practice problems, compared with 5% the previous year. COVID-19 was the most common cause. The proportion reporting no financial losses declined to 65%, versus 75% in the last report.
A version of this article first appeared on Medscape.com.
Survey: Family medicine adds wealth, but higher net worth skews male
.
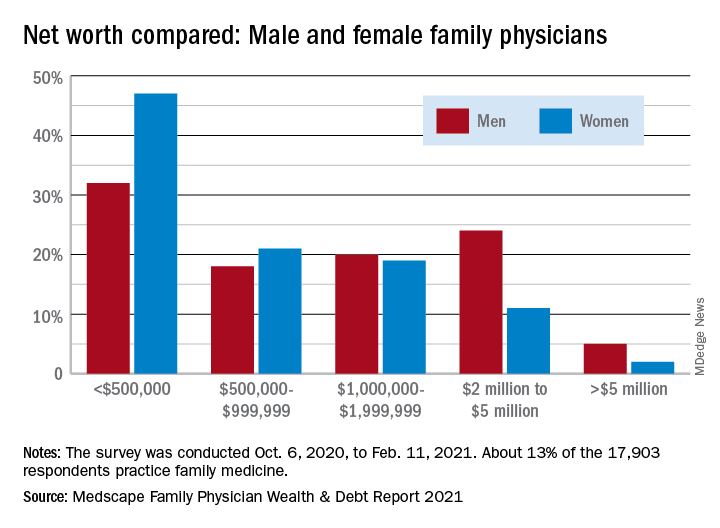
In early 2020, in a survey done before the pandemic, family physicians reported average earnings of $234,000. In 2021, with months of pandemic behind them, survey data show that family physicians averaged $236,000 in earnings.
“Although many medical offices were closed for a period of time in 2020, some physicians made use of the Paycheck Protection Program; others cut staff, renegotiated leases, switched to telephysician visits, and made other cost-cutting changes that kept earnings on par,” Medscape’s Christine Lehman wrote.
Their net worth – total wealth accounting for all financial assets and debts – did even better in 2021. More family physicians are worth $1 million to $5 million in 2021, compared with last year (38% vs. 33%), more are worth over $5 million (4% vs. 3%), and fewer FPs are worth less than $1 million (60% vs. 65%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely, the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male, female family physicians
The wealth disparities that exist among family physicians get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: Five percent of male FPs are worth over $5 million versus 2% of females, and 24% of men are worth $2 million to $5 million versus 11% of women, based on data from the 13% of survey respondents (n = 17,903) who practice family medicine.
Zooming out from the world of family practice to the universe of all physicians shows that FPs are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, family medicine at 4%, and dermatology at 28%. Meanwhile, family physicians’ 40% share of those worth under $500,000 is at the high end of a range in which oncologists are lowest at 16%.
Medical school and other debt
Another area where FPs find themselves looking down on most specialties is medical school debt. Only emergency medicine has more physicians (33%) paying off their school loans than family medicine (31%), while infectious disease has the fewest (12%), according to the Medscape survey, which was conducted Oct. 6, 2020, to Feb. 11, 2021.
Larger proportions of family physicians are paying off credit card debt (30%), car loans (44%), and mortgages on primary residences (67%), while 10% said that they are not paying off debts. Nonpayment of those debts was an issue for 9% of FPs who said that they missed payments on mortgages or other bills because of the COVID-19 pandemic. Almost all FPs said that they live either within (48%) or below (46%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-month emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
.
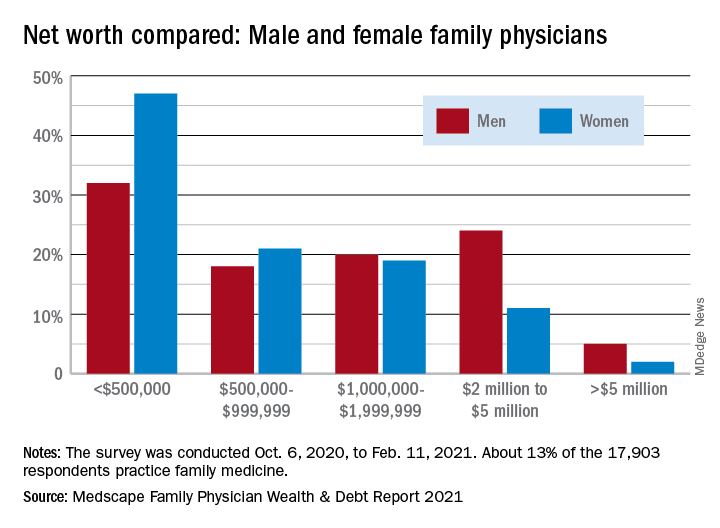
In early 2020, in a survey done before the pandemic, family physicians reported average earnings of $234,000. In 2021, with months of pandemic behind them, survey data show that family physicians averaged $236,000 in earnings.
“Although many medical offices were closed for a period of time in 2020, some physicians made use of the Paycheck Protection Program; others cut staff, renegotiated leases, switched to telephysician visits, and made other cost-cutting changes that kept earnings on par,” Medscape’s Christine Lehman wrote.
Their net worth – total wealth accounting for all financial assets and debts – did even better in 2021. More family physicians are worth $1 million to $5 million in 2021, compared with last year (38% vs. 33%), more are worth over $5 million (4% vs. 3%), and fewer FPs are worth less than $1 million (60% vs. 65%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely, the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male, female family physicians
The wealth disparities that exist among family physicians get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: Five percent of male FPs are worth over $5 million versus 2% of females, and 24% of men are worth $2 million to $5 million versus 11% of women, based on data from the 13% of survey respondents (n = 17,903) who practice family medicine.
Zooming out from the world of family practice to the universe of all physicians shows that FPs are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, family medicine at 4%, and dermatology at 28%. Meanwhile, family physicians’ 40% share of those worth under $500,000 is at the high end of a range in which oncologists are lowest at 16%.
Medical school and other debt
Another area where FPs find themselves looking down on most specialties is medical school debt. Only emergency medicine has more physicians (33%) paying off their school loans than family medicine (31%), while infectious disease has the fewest (12%), according to the Medscape survey, which was conducted Oct. 6, 2020, to Feb. 11, 2021.
Larger proportions of family physicians are paying off credit card debt (30%), car loans (44%), and mortgages on primary residences (67%), while 10% said that they are not paying off debts. Nonpayment of those debts was an issue for 9% of FPs who said that they missed payments on mortgages or other bills because of the COVID-19 pandemic. Almost all FPs said that they live either within (48%) or below (46%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-month emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”
.
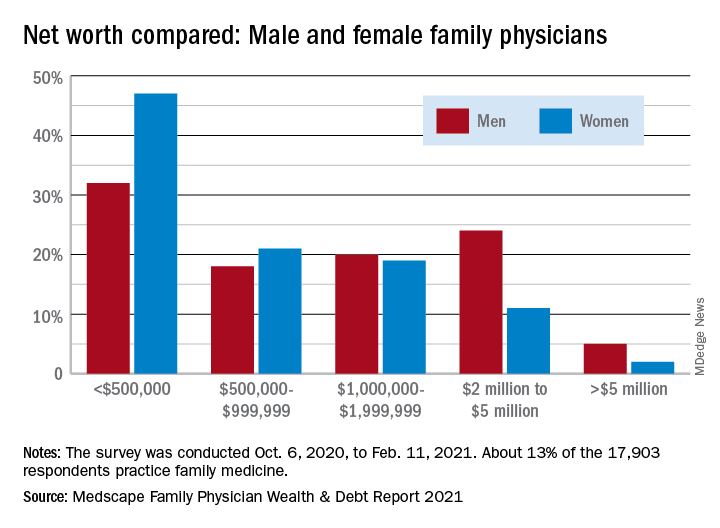
In early 2020, in a survey done before the pandemic, family physicians reported average earnings of $234,000. In 2021, with months of pandemic behind them, survey data show that family physicians averaged $236,000 in earnings.
“Although many medical offices were closed for a period of time in 2020, some physicians made use of the Paycheck Protection Program; others cut staff, renegotiated leases, switched to telephysician visits, and made other cost-cutting changes that kept earnings on par,” Medscape’s Christine Lehman wrote.
Their net worth – total wealth accounting for all financial assets and debts – did even better in 2021. More family physicians are worth $1 million to $5 million in 2021, compared with last year (38% vs. 33%), more are worth over $5 million (4% vs. 3%), and fewer FPs are worth less than $1 million (60% vs. 65%), according to Medscape’s annual wealth and debt report.
“The rise in home prices is certainly a factor,” Joel Greenwald, MD, CFP, a wealth management adviser for physicians, said in an interview.
“Definitely, the rise in the stock market played a large role; the S&P 500 finished the year up over 18%. Finally, I’ve seen clients ... cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” said Dr. Greenwald of St. Louis Park, Minn.
Wealth disparities between male, female family physicians
The wealth disparities that exist among family physicians get somewhat realigned, however, when viewed through the lens of physician gender. The higher-worth segments of the specialty skew rather heavily male: Five percent of male FPs are worth over $5 million versus 2% of females, and 24% of men are worth $2 million to $5 million versus 11% of women, based on data from the 13% of survey respondents (n = 17,903) who practice family medicine.
Zooming out from the world of family practice to the universe of all physicians shows that FPs are closer to allergists and immunologists than to dermatologists when it comes to share of practitioners with net worth over $5 million. That macro view puts allergy/immunology at 2%, family medicine at 4%, and dermatology at 28%. Meanwhile, family physicians’ 40% share of those worth under $500,000 is at the high end of a range in which oncologists are lowest at 16%.
Medical school and other debt
Another area where FPs find themselves looking down on most specialties is medical school debt. Only emergency medicine has more physicians (33%) paying off their school loans than family medicine (31%), while infectious disease has the fewest (12%), according to the Medscape survey, which was conducted Oct. 6, 2020, to Feb. 11, 2021.
Larger proportions of family physicians are paying off credit card debt (30%), car loans (44%), and mortgages on primary residences (67%), while 10% said that they are not paying off debts. Nonpayment of those debts was an issue for 9% of FPs who said that they missed payments on mortgages or other bills because of the COVID-19 pandemic. Almost all FPs said that they live either within (48%) or below (46%) their means, Medscape reported.
“There are certainly folks who believe that as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said. “I would say that living within one’s means is having a 3- to 6-month emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip.”

















