User login
What to do if an employee tests positive for COVID-19
An increasingly common question I’m receiving is:
As always, it depends, but here is some general advice: The specifics will vary depending on state/local laws, or your particular situation.
First, you need to determine the level of exposure, and whether it requires action. According to the Centers for Disease Control and Prevention, actionable exposure occurs 2 days prior to the onset of illness, and lasts 10 days after onset.
If action is required, you’ll need to determine who needs to quarantine and who needs to be tested. Vaccinated employees who have been exposed to suspected or confirmed COVID-19 are not required to quarantine or be tested if they are fully vaccinated and have remained asymptomatic since the exposure. Those employees should, however, follow all the usual precautions (masks, social distancing, handwashing, etc.) with increased diligence. Remind them that no vaccine is 100% effective, and suggest they self-monitor for symptoms (fever, cough, shortness of breath, etc.)
All other exposed employees should be tested. A negative test means an individual was not infected at the time the sample was collected, but that does not mean an individual will not get sick later. Some providers are retesting on days 5 and 7 post exposure.
Some experts advise that you monitor exposed employees (vaccinated or not) yourself, with daily temperature readings and inquiries regarding symptoms, and perhaps a daily pulse oximetry check, for 14 days following exposure. Document these screenings in writing. Anyone testing positive or developing a fever or other symptoms should, of course, be sent home and seek medical treatment as necessary.
Employees who develop symptoms or test positive for COVID-19 should remain out of work until all CDC “return-to-work” criteria are met. At this writing, the basic criteria include:
- At least 10 days pass after symptoms first appeared
- At least 24 hours pass after last fever without the use of fever-reducing medications
- Cough, shortness of breath, and any other symptoms improve
Anyone who is significantly immunocompromised may need more time at home, and probably consultation with an infectious disease specialist.
Your facility should be thoroughly cleaned after the exposure. Close off all areas used by the sick individual, and clean and disinfect all areas such as offices, doorknobs, bathrooms, common areas, and shared electronic equipment. Of course, the cleaners should wear gowns, gloves, masks, and goggles. Some practices are hiring cleaning crews to professionally disinfect their offices. Once the area has been disinfected, it can be reopened for use. Workers without close contact with the person who is sick can return to work immediately after disinfection.
If the potential infected area is widespread and cannot be isolated to a room or rooms where doors can be shut, it may be prudent to temporarily close your office, send staff home, and divert patients to other locations if they cannot be rescheduled. Once your facility is cleaned and disinfected and staff have been cleared, your office may reopen.
Use enhanced precautions for any staff or patients who are immunocompromised, or otherwise fall into the high-risk category, to keep them out of the path of potential exposure areas and allow them to self-quarantine if they desire.
You should continue following existing leave policies (paid time off, vacation, sick, short-term disability, leave of absence, Family and Medical Leave Act, and Americans with Disabilities Act). If the employee was exposed at work, contact your workers’ compensation carrier regarding lost wages. Unless your state laws specify otherwise, you are under no obligation to pay beyond your policies, but you may do so if you choose.
Of course, you can take proactive steps to prevent unnecessary exposure and avoid closures in the first place; for example:
- Call patients prior to their visit, or question them upon arrival, regarding fever, shortness of breath, and other COVID-19 symptoms.
- Check employees’ temperatures every morning.
- Check patients’ temperatures as they enter the office.
- Require everyone, patients and employees alike, to wear face coverings.
- Ask patients to leave friends and family members at home.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
An increasingly common question I’m receiving is:
As always, it depends, but here is some general advice: The specifics will vary depending on state/local laws, or your particular situation.
First, you need to determine the level of exposure, and whether it requires action. According to the Centers for Disease Control and Prevention, actionable exposure occurs 2 days prior to the onset of illness, and lasts 10 days after onset.
If action is required, you’ll need to determine who needs to quarantine and who needs to be tested. Vaccinated employees who have been exposed to suspected or confirmed COVID-19 are not required to quarantine or be tested if they are fully vaccinated and have remained asymptomatic since the exposure. Those employees should, however, follow all the usual precautions (masks, social distancing, handwashing, etc.) with increased diligence. Remind them that no vaccine is 100% effective, and suggest they self-monitor for symptoms (fever, cough, shortness of breath, etc.)
All other exposed employees should be tested. A negative test means an individual was not infected at the time the sample was collected, but that does not mean an individual will not get sick later. Some providers are retesting on days 5 and 7 post exposure.
Some experts advise that you monitor exposed employees (vaccinated or not) yourself, with daily temperature readings and inquiries regarding symptoms, and perhaps a daily pulse oximetry check, for 14 days following exposure. Document these screenings in writing. Anyone testing positive or developing a fever or other symptoms should, of course, be sent home and seek medical treatment as necessary.
Employees who develop symptoms or test positive for COVID-19 should remain out of work until all CDC “return-to-work” criteria are met. At this writing, the basic criteria include:
- At least 10 days pass after symptoms first appeared
- At least 24 hours pass after last fever without the use of fever-reducing medications
- Cough, shortness of breath, and any other symptoms improve
Anyone who is significantly immunocompromised may need more time at home, and probably consultation with an infectious disease specialist.
Your facility should be thoroughly cleaned after the exposure. Close off all areas used by the sick individual, and clean and disinfect all areas such as offices, doorknobs, bathrooms, common areas, and shared electronic equipment. Of course, the cleaners should wear gowns, gloves, masks, and goggles. Some practices are hiring cleaning crews to professionally disinfect their offices. Once the area has been disinfected, it can be reopened for use. Workers without close contact with the person who is sick can return to work immediately after disinfection.
If the potential infected area is widespread and cannot be isolated to a room or rooms where doors can be shut, it may be prudent to temporarily close your office, send staff home, and divert patients to other locations if they cannot be rescheduled. Once your facility is cleaned and disinfected and staff have been cleared, your office may reopen.
Use enhanced precautions for any staff or patients who are immunocompromised, or otherwise fall into the high-risk category, to keep them out of the path of potential exposure areas and allow them to self-quarantine if they desire.
You should continue following existing leave policies (paid time off, vacation, sick, short-term disability, leave of absence, Family and Medical Leave Act, and Americans with Disabilities Act). If the employee was exposed at work, contact your workers’ compensation carrier regarding lost wages. Unless your state laws specify otherwise, you are under no obligation to pay beyond your policies, but you may do so if you choose.
Of course, you can take proactive steps to prevent unnecessary exposure and avoid closures in the first place; for example:
- Call patients prior to their visit, or question them upon arrival, regarding fever, shortness of breath, and other COVID-19 symptoms.
- Check employees’ temperatures every morning.
- Check patients’ temperatures as they enter the office.
- Require everyone, patients and employees alike, to wear face coverings.
- Ask patients to leave friends and family members at home.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
An increasingly common question I’m receiving is:
As always, it depends, but here is some general advice: The specifics will vary depending on state/local laws, or your particular situation.
First, you need to determine the level of exposure, and whether it requires action. According to the Centers for Disease Control and Prevention, actionable exposure occurs 2 days prior to the onset of illness, and lasts 10 days after onset.
If action is required, you’ll need to determine who needs to quarantine and who needs to be tested. Vaccinated employees who have been exposed to suspected or confirmed COVID-19 are not required to quarantine or be tested if they are fully vaccinated and have remained asymptomatic since the exposure. Those employees should, however, follow all the usual precautions (masks, social distancing, handwashing, etc.) with increased diligence. Remind them that no vaccine is 100% effective, and suggest they self-monitor for symptoms (fever, cough, shortness of breath, etc.)
All other exposed employees should be tested. A negative test means an individual was not infected at the time the sample was collected, but that does not mean an individual will not get sick later. Some providers are retesting on days 5 and 7 post exposure.
Some experts advise that you monitor exposed employees (vaccinated or not) yourself, with daily temperature readings and inquiries regarding symptoms, and perhaps a daily pulse oximetry check, for 14 days following exposure. Document these screenings in writing. Anyone testing positive or developing a fever or other symptoms should, of course, be sent home and seek medical treatment as necessary.
Employees who develop symptoms or test positive for COVID-19 should remain out of work until all CDC “return-to-work” criteria are met. At this writing, the basic criteria include:
- At least 10 days pass after symptoms first appeared
- At least 24 hours pass after last fever without the use of fever-reducing medications
- Cough, shortness of breath, and any other symptoms improve
Anyone who is significantly immunocompromised may need more time at home, and probably consultation with an infectious disease specialist.
Your facility should be thoroughly cleaned after the exposure. Close off all areas used by the sick individual, and clean and disinfect all areas such as offices, doorknobs, bathrooms, common areas, and shared electronic equipment. Of course, the cleaners should wear gowns, gloves, masks, and goggles. Some practices are hiring cleaning crews to professionally disinfect their offices. Once the area has been disinfected, it can be reopened for use. Workers without close contact with the person who is sick can return to work immediately after disinfection.
If the potential infected area is widespread and cannot be isolated to a room or rooms where doors can be shut, it may be prudent to temporarily close your office, send staff home, and divert patients to other locations if they cannot be rescheduled. Once your facility is cleaned and disinfected and staff have been cleared, your office may reopen.
Use enhanced precautions for any staff or patients who are immunocompromised, or otherwise fall into the high-risk category, to keep them out of the path of potential exposure areas and allow them to self-quarantine if they desire.
You should continue following existing leave policies (paid time off, vacation, sick, short-term disability, leave of absence, Family and Medical Leave Act, and Americans with Disabilities Act). If the employee was exposed at work, contact your workers’ compensation carrier regarding lost wages. Unless your state laws specify otherwise, you are under no obligation to pay beyond your policies, but you may do so if you choose.
Of course, you can take proactive steps to prevent unnecessary exposure and avoid closures in the first place; for example:
- Call patients prior to their visit, or question them upon arrival, regarding fever, shortness of breath, and other COVID-19 symptoms.
- Check employees’ temperatures every morning.
- Check patients’ temperatures as they enter the office.
- Require everyone, patients and employees alike, to wear face coverings.
- Ask patients to leave friends and family members at home.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Survey: Most patients support teledermatology
Many medical practices turned to telemedicine when the pandemic shut down the economy last spring, but what do dermatology patients think about the socially distant approach?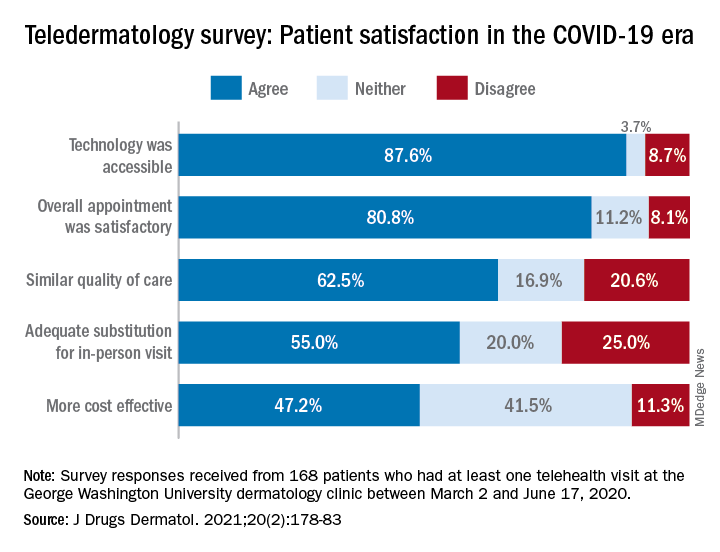
and 80% said that they would consider another such visit in the future, according to a survey conducted at George Washington University in Washington.
Although “telehealth is not without its drawbacks … it is clear from this study that the majority of patients feel positively towards teledermatology during the COVID-19 pandemic and [believe it] can be a suitable alternative for patients who are unable to meet with their providers in person,” Samuel Yeroushalmi, Sarah H. Millan, and associates at the university said in the Journal of Drugs in Dermatology.
When presented with a set of statements about the telehealth experience, the 168 survey respondents largely agreed that the overall appointment was satisfactory (80.8%), that minimal barriers were present (78.1%), and that the quality of care was similar to an in-person visit (62.5%), the investigators said.
Other factors, however, were not as well supported. Less than half (47.2%) of the respondents agreed that the telehealth appointments were more cost effective, and just over half (54.7%) agreed that they provided an adequate skin exam, they reported.
Of the set of 14 statements given to the patients – all of whom had at least one telehealth visit with the GW clinic between March 2 and June 17, 2020 – the one on the adequacy of the skin exam provided the largest share of disagreement at 27.1%, Mr. Yeroushalmi and Ms. Millan, medical students at the university and coauthors.
The lack of physical touch was mentioned most often (26.8%) when respondents were asked about their reasons for disliking telehealth visits, followed by the feeling that they had received an inadequate assessment (15.7%), they said.
Despite these drawbacks, “the convenience and efficacy of telehealth as well as its ability to maintain separation while social distancing recommendations are in place make it an effective way for dermatologists to continue to provide quality and safe care during the pandemics as well as during potential future public health crises,” the investigators concluded.
Many medical practices turned to telemedicine when the pandemic shut down the economy last spring, but what do dermatology patients think about the socially distant approach?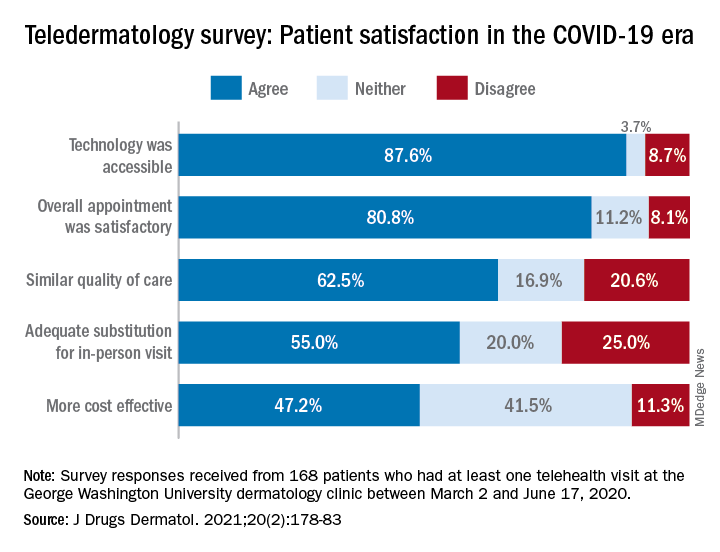
and 80% said that they would consider another such visit in the future, according to a survey conducted at George Washington University in Washington.
Although “telehealth is not without its drawbacks … it is clear from this study that the majority of patients feel positively towards teledermatology during the COVID-19 pandemic and [believe it] can be a suitable alternative for patients who are unable to meet with their providers in person,” Samuel Yeroushalmi, Sarah H. Millan, and associates at the university said in the Journal of Drugs in Dermatology.
When presented with a set of statements about the telehealth experience, the 168 survey respondents largely agreed that the overall appointment was satisfactory (80.8%), that minimal barriers were present (78.1%), and that the quality of care was similar to an in-person visit (62.5%), the investigators said.
Other factors, however, were not as well supported. Less than half (47.2%) of the respondents agreed that the telehealth appointments were more cost effective, and just over half (54.7%) agreed that they provided an adequate skin exam, they reported.
Of the set of 14 statements given to the patients – all of whom had at least one telehealth visit with the GW clinic between March 2 and June 17, 2020 – the one on the adequacy of the skin exam provided the largest share of disagreement at 27.1%, Mr. Yeroushalmi and Ms. Millan, medical students at the university and coauthors.
The lack of physical touch was mentioned most often (26.8%) when respondents were asked about their reasons for disliking telehealth visits, followed by the feeling that they had received an inadequate assessment (15.7%), they said.
Despite these drawbacks, “the convenience and efficacy of telehealth as well as its ability to maintain separation while social distancing recommendations are in place make it an effective way for dermatologists to continue to provide quality and safe care during the pandemics as well as during potential future public health crises,” the investigators concluded.
Many medical practices turned to telemedicine when the pandemic shut down the economy last spring, but what do dermatology patients think about the socially distant approach?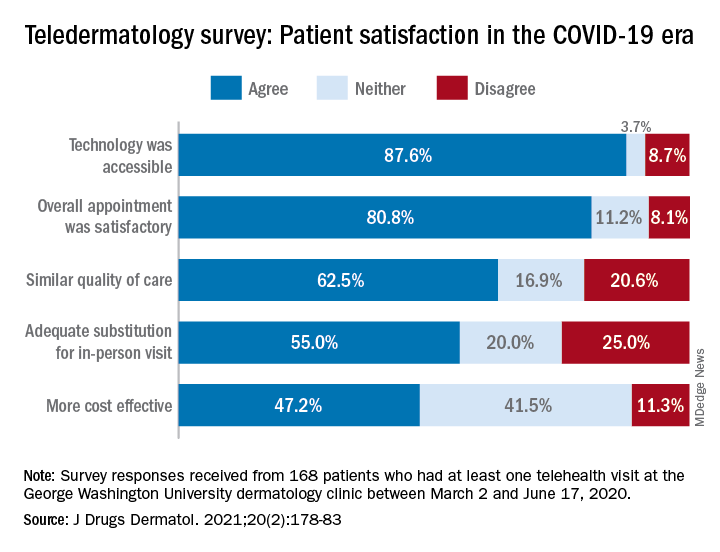
and 80% said that they would consider another such visit in the future, according to a survey conducted at George Washington University in Washington.
Although “telehealth is not without its drawbacks … it is clear from this study that the majority of patients feel positively towards teledermatology during the COVID-19 pandemic and [believe it] can be a suitable alternative for patients who are unable to meet with their providers in person,” Samuel Yeroushalmi, Sarah H. Millan, and associates at the university said in the Journal of Drugs in Dermatology.
When presented with a set of statements about the telehealth experience, the 168 survey respondents largely agreed that the overall appointment was satisfactory (80.8%), that minimal barriers were present (78.1%), and that the quality of care was similar to an in-person visit (62.5%), the investigators said.
Other factors, however, were not as well supported. Less than half (47.2%) of the respondents agreed that the telehealth appointments were more cost effective, and just over half (54.7%) agreed that they provided an adequate skin exam, they reported.
Of the set of 14 statements given to the patients – all of whom had at least one telehealth visit with the GW clinic between March 2 and June 17, 2020 – the one on the adequacy of the skin exam provided the largest share of disagreement at 27.1%, Mr. Yeroushalmi and Ms. Millan, medical students at the university and coauthors.
The lack of physical touch was mentioned most often (26.8%) when respondents were asked about their reasons for disliking telehealth visits, followed by the feeling that they had received an inadequate assessment (15.7%), they said.
Despite these drawbacks, “the convenience and efficacy of telehealth as well as its ability to maintain separation while social distancing recommendations are in place make it an effective way for dermatologists to continue to provide quality and safe care during the pandemics as well as during potential future public health crises,” the investigators concluded.
FROM JOURNAL OF DRUGS IN DERMATOLOGY
Lifestyle coaching for obesity associated with improved cardiometabolic numbers in study
Patients who received intensive lifestyle training by coaches in the primary care setting experienced improvement in several indicators of cardiometabolic health in a 2-year trial.
The 803 trial participants comprised a racially diverse, low-income population with obesity. In this study, primary care clinics were randomly assigned to provide weight-loss coaching or usual care. Patients at the intensive training clinics lost significantly more weight than the other patients, as reported in a paper published in September in the New England Journal of Medicine on the PROmoting Successful Weight Loss in Primary CarE in Louisiana (PROPEL) trial. The patients who received weight loss coaching also had significantly more improvement in HDL cholesterol levels, total to HDL cholesterol ratios, and metabolic syndrome severity score, said researchers in the new paper on the PROPEL trial, which was published in Circulation on February 8 .
“We believe that one reason for success of the program was the use of a health coach [who] was embedded in the primary care office,” said lead author Peter Katzmarzyk, PhD, associate executive director for population and public health sciences at the Pennington Biomedical Research Center, Baton Rouge, La. “This way, the patients could get their counseling in a familiar environment and did not have to go to a different setting. The coaches developed close relationships with the patients over the 2 years, and this helped develop a sense of responsibility in the patients as the coaches were helping the patients to set goals and kept them accountable.”
In the PROPEL study, 67% of patients were Black and had low health literacy scores that corresponded with less than a ninth-grade education level. The intensive lifestyle intervention program included weekly sessions with the trained health coaches over the first 6 months — 16 face-to-face and 6 over the phone — and then at least monthly for the last 18 months. The coaches had higher education degrees in nutrition, physical activity, or behavioral medicine. Before the program started, the coaches also received training in the management of obesity and related health issues, health literacy, and patient communication and education. The goal of the program was 10% weight loss, using personalized action plans on eating, dieting, and physical activity.
Those in the usual-care clinics continued receiving normal care and received newsletters on health topics, such as the importance of sleep and tips for limiting time spent sitting. The primary care physicians at those clinics also were given a presentation with Centers for Medicare & Medicaid Services (CMS) information on intensive lifestyle interventions for obesity.
Cholesterol changes in intervention vs. control group
HDL cholesterol improved significantly among the coached patients, compared with the other patients, with a mean difference of 4.1 mg/dL at 1 year and 4.6 mg/dL at 2 years (P less than .01 for both). The total cholesterol to HDL cholesterol ratio showed a similarly significant difference in decline, with a between-group difference of –0.29 at 1 year and –0.31 at 2 years (P less than .01 for both). Also, the difference in the change in metabolic severity scores were –0.40 at 1 year and –0.21 at 2 years (P less than .01 for both).
Fasting blood glucose had declined after the 1st year by a significantly greater degree in the clinics with coaching, compared with the others, but not after the second year, researchers found.
There were no significant differences seen in total cholesterol, LDL cholesterol, non-HDL cholesterol, or blood pressure. Dr. Katzmarzyk said the likely reason for no change in blood pressure was that it was already relatively well-controlled at baseline for all the patients.
Funding barriers to obesity treatment
The CMS currently cover intensive training for obesity if delivered directly by a primary care physician, according to the authors of the new paper. Dr. Katzmarzyk said he hopes that will change.
“We are hoping that the evidence provided in this study may change the way that CMS funds obesity treatment in the future by allowing an expansion of the care team,” he said.
John Flack, MD, chair of internal medicine at Southern Illinois University, Springfield, said that the main achievement of the study was that it showed that intensive weight-loss training in the primary-care setting could be accomplished in a racially diverse population with low health literacy.
“You can’t just automatically assume just because you’ve seen it in some other populations that you can replicate this in every population, so they’ve done a really good job,” he said.
That programs are eligible for reimbursement only if they’re run by primary-care physicians is an ongoing problem, he said.
“You don’t necessarily need to be a physician to do this,” Dr. Flack said.
For best results, payment for coaching should not be tied to office visits, Dr. Flack noted.
“If they’re de-tethered from the office visits and you’re paid for quality ... you’re going to build out your infrastructure differently to care for people,” he said.
Andrew Freeman, MD, associate professor of medicine at the University of Colorado, Denver, and cochair of the American College of Cardiology’s nutrition and lifestyle work group, said the findings dovetail with his experience.
“I’m a huge believer that when people need to make lifestyle changes, having someone hold their hand and guide them through the effort is incredibly rewarding and incredibly powerful,” said Dr. Freeman, who also oversees the intensive cardiac rehab program at National Jewish Health in Denver.
A program like this needs proper funding in order to work, Dr, Freeman noted. He added that, even with coaches being paid well, “if you are able to prevent just one readmission for, say, heart failure a month . . . you could be saving millions of dollars over just a couple of years.”
Dr. Katzmarzyk, Dr. Flack, and Dr. Freeman reported no relevant disclosures. Louisiana State University, Pennington Biomedical Research Center, and Montclair State University have interest in the intellectual property surrounding a weight graph used in the study. The other researchers reported grants and/or fees from Bayer, Boehringer Ingelheim, Gilead, Takeda, Novo Nordisk, and other companies.
Patients who received intensive lifestyle training by coaches in the primary care setting experienced improvement in several indicators of cardiometabolic health in a 2-year trial.
The 803 trial participants comprised a racially diverse, low-income population with obesity. In this study, primary care clinics were randomly assigned to provide weight-loss coaching or usual care. Patients at the intensive training clinics lost significantly more weight than the other patients, as reported in a paper published in September in the New England Journal of Medicine on the PROmoting Successful Weight Loss in Primary CarE in Louisiana (PROPEL) trial. The patients who received weight loss coaching also had significantly more improvement in HDL cholesterol levels, total to HDL cholesterol ratios, and metabolic syndrome severity score, said researchers in the new paper on the PROPEL trial, which was published in Circulation on February 8 .
“We believe that one reason for success of the program was the use of a health coach [who] was embedded in the primary care office,” said lead author Peter Katzmarzyk, PhD, associate executive director for population and public health sciences at the Pennington Biomedical Research Center, Baton Rouge, La. “This way, the patients could get their counseling in a familiar environment and did not have to go to a different setting. The coaches developed close relationships with the patients over the 2 years, and this helped develop a sense of responsibility in the patients as the coaches were helping the patients to set goals and kept them accountable.”
In the PROPEL study, 67% of patients were Black and had low health literacy scores that corresponded with less than a ninth-grade education level. The intensive lifestyle intervention program included weekly sessions with the trained health coaches over the first 6 months — 16 face-to-face and 6 over the phone — and then at least monthly for the last 18 months. The coaches had higher education degrees in nutrition, physical activity, or behavioral medicine. Before the program started, the coaches also received training in the management of obesity and related health issues, health literacy, and patient communication and education. The goal of the program was 10% weight loss, using personalized action plans on eating, dieting, and physical activity.
Those in the usual-care clinics continued receiving normal care and received newsletters on health topics, such as the importance of sleep and tips for limiting time spent sitting. The primary care physicians at those clinics also were given a presentation with Centers for Medicare & Medicaid Services (CMS) information on intensive lifestyle interventions for obesity.
Cholesterol changes in intervention vs. control group
HDL cholesterol improved significantly among the coached patients, compared with the other patients, with a mean difference of 4.1 mg/dL at 1 year and 4.6 mg/dL at 2 years (P less than .01 for both). The total cholesterol to HDL cholesterol ratio showed a similarly significant difference in decline, with a between-group difference of –0.29 at 1 year and –0.31 at 2 years (P less than .01 for both). Also, the difference in the change in metabolic severity scores were –0.40 at 1 year and –0.21 at 2 years (P less than .01 for both).
Fasting blood glucose had declined after the 1st year by a significantly greater degree in the clinics with coaching, compared with the others, but not after the second year, researchers found.
There were no significant differences seen in total cholesterol, LDL cholesterol, non-HDL cholesterol, or blood pressure. Dr. Katzmarzyk said the likely reason for no change in blood pressure was that it was already relatively well-controlled at baseline for all the patients.
Funding barriers to obesity treatment
The CMS currently cover intensive training for obesity if delivered directly by a primary care physician, according to the authors of the new paper. Dr. Katzmarzyk said he hopes that will change.
“We are hoping that the evidence provided in this study may change the way that CMS funds obesity treatment in the future by allowing an expansion of the care team,” he said.
John Flack, MD, chair of internal medicine at Southern Illinois University, Springfield, said that the main achievement of the study was that it showed that intensive weight-loss training in the primary-care setting could be accomplished in a racially diverse population with low health literacy.
“You can’t just automatically assume just because you’ve seen it in some other populations that you can replicate this in every population, so they’ve done a really good job,” he said.
That programs are eligible for reimbursement only if they’re run by primary-care physicians is an ongoing problem, he said.
“You don’t necessarily need to be a physician to do this,” Dr. Flack said.
For best results, payment for coaching should not be tied to office visits, Dr. Flack noted.
“If they’re de-tethered from the office visits and you’re paid for quality ... you’re going to build out your infrastructure differently to care for people,” he said.
Andrew Freeman, MD, associate professor of medicine at the University of Colorado, Denver, and cochair of the American College of Cardiology’s nutrition and lifestyle work group, said the findings dovetail with his experience.
“I’m a huge believer that when people need to make lifestyle changes, having someone hold their hand and guide them through the effort is incredibly rewarding and incredibly powerful,” said Dr. Freeman, who also oversees the intensive cardiac rehab program at National Jewish Health in Denver.
A program like this needs proper funding in order to work, Dr, Freeman noted. He added that, even with coaches being paid well, “if you are able to prevent just one readmission for, say, heart failure a month . . . you could be saving millions of dollars over just a couple of years.”
Dr. Katzmarzyk, Dr. Flack, and Dr. Freeman reported no relevant disclosures. Louisiana State University, Pennington Biomedical Research Center, and Montclair State University have interest in the intellectual property surrounding a weight graph used in the study. The other researchers reported grants and/or fees from Bayer, Boehringer Ingelheim, Gilead, Takeda, Novo Nordisk, and other companies.
Patients who received intensive lifestyle training by coaches in the primary care setting experienced improvement in several indicators of cardiometabolic health in a 2-year trial.
The 803 trial participants comprised a racially diverse, low-income population with obesity. In this study, primary care clinics were randomly assigned to provide weight-loss coaching or usual care. Patients at the intensive training clinics lost significantly more weight than the other patients, as reported in a paper published in September in the New England Journal of Medicine on the PROmoting Successful Weight Loss in Primary CarE in Louisiana (PROPEL) trial. The patients who received weight loss coaching also had significantly more improvement in HDL cholesterol levels, total to HDL cholesterol ratios, and metabolic syndrome severity score, said researchers in the new paper on the PROPEL trial, which was published in Circulation on February 8 .
“We believe that one reason for success of the program was the use of a health coach [who] was embedded in the primary care office,” said lead author Peter Katzmarzyk, PhD, associate executive director for population and public health sciences at the Pennington Biomedical Research Center, Baton Rouge, La. “This way, the patients could get their counseling in a familiar environment and did not have to go to a different setting. The coaches developed close relationships with the patients over the 2 years, and this helped develop a sense of responsibility in the patients as the coaches were helping the patients to set goals and kept them accountable.”
In the PROPEL study, 67% of patients were Black and had low health literacy scores that corresponded with less than a ninth-grade education level. The intensive lifestyle intervention program included weekly sessions with the trained health coaches over the first 6 months — 16 face-to-face and 6 over the phone — and then at least monthly for the last 18 months. The coaches had higher education degrees in nutrition, physical activity, or behavioral medicine. Before the program started, the coaches also received training in the management of obesity and related health issues, health literacy, and patient communication and education. The goal of the program was 10% weight loss, using personalized action plans on eating, dieting, and physical activity.
Those in the usual-care clinics continued receiving normal care and received newsletters on health topics, such as the importance of sleep and tips for limiting time spent sitting. The primary care physicians at those clinics also were given a presentation with Centers for Medicare & Medicaid Services (CMS) information on intensive lifestyle interventions for obesity.
Cholesterol changes in intervention vs. control group
HDL cholesterol improved significantly among the coached patients, compared with the other patients, with a mean difference of 4.1 mg/dL at 1 year and 4.6 mg/dL at 2 years (P less than .01 for both). The total cholesterol to HDL cholesterol ratio showed a similarly significant difference in decline, with a between-group difference of –0.29 at 1 year and –0.31 at 2 years (P less than .01 for both). Also, the difference in the change in metabolic severity scores were –0.40 at 1 year and –0.21 at 2 years (P less than .01 for both).
Fasting blood glucose had declined after the 1st year by a significantly greater degree in the clinics with coaching, compared with the others, but not after the second year, researchers found.
There were no significant differences seen in total cholesterol, LDL cholesterol, non-HDL cholesterol, or blood pressure. Dr. Katzmarzyk said the likely reason for no change in blood pressure was that it was already relatively well-controlled at baseline for all the patients.
Funding barriers to obesity treatment
The CMS currently cover intensive training for obesity if delivered directly by a primary care physician, according to the authors of the new paper. Dr. Katzmarzyk said he hopes that will change.
“We are hoping that the evidence provided in this study may change the way that CMS funds obesity treatment in the future by allowing an expansion of the care team,” he said.
John Flack, MD, chair of internal medicine at Southern Illinois University, Springfield, said that the main achievement of the study was that it showed that intensive weight-loss training in the primary-care setting could be accomplished in a racially diverse population with low health literacy.
“You can’t just automatically assume just because you’ve seen it in some other populations that you can replicate this in every population, so they’ve done a really good job,” he said.
That programs are eligible for reimbursement only if they’re run by primary-care physicians is an ongoing problem, he said.
“You don’t necessarily need to be a physician to do this,” Dr. Flack said.
For best results, payment for coaching should not be tied to office visits, Dr. Flack noted.
“If they’re de-tethered from the office visits and you’re paid for quality ... you’re going to build out your infrastructure differently to care for people,” he said.
Andrew Freeman, MD, associate professor of medicine at the University of Colorado, Denver, and cochair of the American College of Cardiology’s nutrition and lifestyle work group, said the findings dovetail with his experience.
“I’m a huge believer that when people need to make lifestyle changes, having someone hold their hand and guide them through the effort is incredibly rewarding and incredibly powerful,” said Dr. Freeman, who also oversees the intensive cardiac rehab program at National Jewish Health in Denver.
A program like this needs proper funding in order to work, Dr, Freeman noted. He added that, even with coaches being paid well, “if you are able to prevent just one readmission for, say, heart failure a month . . . you could be saving millions of dollars over just a couple of years.”
Dr. Katzmarzyk, Dr. Flack, and Dr. Freeman reported no relevant disclosures. Louisiana State University, Pennington Biomedical Research Center, and Montclair State University have interest in the intellectual property surrounding a weight graph used in the study. The other researchers reported grants and/or fees from Bayer, Boehringer Ingelheim, Gilead, Takeda, Novo Nordisk, and other companies.
COVID-19 studies funded by rheumatology foundation
Five lines of research related to COVID-19 and people with rheumatic diseases will be explored with $1.65 million awarded recently by the Rheumatology Research Foundation.
Investigators will explore topics ranging from respiratory health to telemedicine with the awards, given by the foundation that is the largest private funding source for rheumatology research and training in the United States. The projects are an attempt to deepen the understanding about how people with rheumatic illnesses are affected by COVID-19.
“Our current understanding of why there are differences in severity of COVID-19 illness among rheumatology patients is limited,” Foundation President S. Louis Bridges, MD, PhD, said. “Additionally, there are many other gaps in our knowledge of the clinical aspects of SARS-CoV-2 infection in patients with rheumatic diseases, and how the pandemic has changed health care delivery. There is an urgent need to acquire new knowledge on COVID-19 in patients with [rheumatic and musculoskeletal diseases].”
These are the research projects funded:
- Scientist Development Award: Respiratory complications of coronavirus disease (COVID-19) in rheumatic diseases, led by Kristin D’Silva, MD, of Massachusetts General Hospital in Boston (3-year, $225,000 grant)
- Scientist Development Award: COVID-19 in patients with inflammatory arthritis: A prospective study on the effects of immunomodulatory therapy on susceptibility and clinical outcomes, by Rebecca Haberman, MD, of New York University (3-year, $225,000 grant)
- Innovative Research Award: Antiphospholipid antibodies in COVID-19, led by Jason Knight, MD, PhD, of the University of Michigan, Ann Arbor (2-year, $400,000 grant);
- Innovative Research Award: Effectiveness of telerheumatology for delivering high-quality rheumatology care during the COVID-19 crisis, led by Maria Danila, MD, MSc, MSPH, of University of Alabama at Birmingham (2-year, $400,000 grant)
- Norman B. Gaylis, MD, Clinical Research Award: Telehealth-delivered health care to improve care (THRIVE) in community-practice rheumatology, led by Swamy Venuturupalli, MD, of Beverly Hills, Calif.–based Attune Health (2-year, $400,000 grant)
Dr. Bridges said the foundation accepted submissions in basic science, translational science, clinical science, health services research, and patient- and practice-centered research.
“What differentiates these studies from our existing awards portfolio is they all explore the relationships between rheumatic and musculoskeletal diseases and SARS-CoV-2,” he said. “Ultimately, the outcomes of these projects will contribute to a more comprehensive knowledge base and advance avenues of patient care in the COVID-19 pandemic.”
Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., said he was pleased that a telehealth project was chosen as the award given in his name.
“From a COVID point of view, this has been extremely valuable in allowing us to continue to help out patients, connect with our patients, provide them treatment, even if it’s not hands on, at least guide them in how to deal with their chronic rheumatic illnesses,” he said.
This line of research can also help explore the feasibility of telemedicine in helping meet the needs of rural communities facing shortages of rheumatologists.
“Can telemedicine provide a source of rheumatologic access for people who really don’t have a live provider in close proximity?” he said. “I think that’s really why this particular award is very, very timely.”
“It’s so difficult for clinicians to get funding for their research, for their ideas and for the discoveries they were making on a day-to-day basis while they were practicing in a clinical community environment,” he said. “So for me it was really something that inspired me to really create this award.”
Five lines of research related to COVID-19 and people with rheumatic diseases will be explored with $1.65 million awarded recently by the Rheumatology Research Foundation.
Investigators will explore topics ranging from respiratory health to telemedicine with the awards, given by the foundation that is the largest private funding source for rheumatology research and training in the United States. The projects are an attempt to deepen the understanding about how people with rheumatic illnesses are affected by COVID-19.
“Our current understanding of why there are differences in severity of COVID-19 illness among rheumatology patients is limited,” Foundation President S. Louis Bridges, MD, PhD, said. “Additionally, there are many other gaps in our knowledge of the clinical aspects of SARS-CoV-2 infection in patients with rheumatic diseases, and how the pandemic has changed health care delivery. There is an urgent need to acquire new knowledge on COVID-19 in patients with [rheumatic and musculoskeletal diseases].”
These are the research projects funded:
- Scientist Development Award: Respiratory complications of coronavirus disease (COVID-19) in rheumatic diseases, led by Kristin D’Silva, MD, of Massachusetts General Hospital in Boston (3-year, $225,000 grant)
- Scientist Development Award: COVID-19 in patients with inflammatory arthritis: A prospective study on the effects of immunomodulatory therapy on susceptibility and clinical outcomes, by Rebecca Haberman, MD, of New York University (3-year, $225,000 grant)
- Innovative Research Award: Antiphospholipid antibodies in COVID-19, led by Jason Knight, MD, PhD, of the University of Michigan, Ann Arbor (2-year, $400,000 grant);
- Innovative Research Award: Effectiveness of telerheumatology for delivering high-quality rheumatology care during the COVID-19 crisis, led by Maria Danila, MD, MSc, MSPH, of University of Alabama at Birmingham (2-year, $400,000 grant)
- Norman B. Gaylis, MD, Clinical Research Award: Telehealth-delivered health care to improve care (THRIVE) in community-practice rheumatology, led by Swamy Venuturupalli, MD, of Beverly Hills, Calif.–based Attune Health (2-year, $400,000 grant)
Dr. Bridges said the foundation accepted submissions in basic science, translational science, clinical science, health services research, and patient- and practice-centered research.
“What differentiates these studies from our existing awards portfolio is they all explore the relationships between rheumatic and musculoskeletal diseases and SARS-CoV-2,” he said. “Ultimately, the outcomes of these projects will contribute to a more comprehensive knowledge base and advance avenues of patient care in the COVID-19 pandemic.”
Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., said he was pleased that a telehealth project was chosen as the award given in his name.
“From a COVID point of view, this has been extremely valuable in allowing us to continue to help out patients, connect with our patients, provide them treatment, even if it’s not hands on, at least guide them in how to deal with their chronic rheumatic illnesses,” he said.
This line of research can also help explore the feasibility of telemedicine in helping meet the needs of rural communities facing shortages of rheumatologists.
“Can telemedicine provide a source of rheumatologic access for people who really don’t have a live provider in close proximity?” he said. “I think that’s really why this particular award is very, very timely.”
“It’s so difficult for clinicians to get funding for their research, for their ideas and for the discoveries they were making on a day-to-day basis while they were practicing in a clinical community environment,” he said. “So for me it was really something that inspired me to really create this award.”
Five lines of research related to COVID-19 and people with rheumatic diseases will be explored with $1.65 million awarded recently by the Rheumatology Research Foundation.
Investigators will explore topics ranging from respiratory health to telemedicine with the awards, given by the foundation that is the largest private funding source for rheumatology research and training in the United States. The projects are an attempt to deepen the understanding about how people with rheumatic illnesses are affected by COVID-19.
“Our current understanding of why there are differences in severity of COVID-19 illness among rheumatology patients is limited,” Foundation President S. Louis Bridges, MD, PhD, said. “Additionally, there are many other gaps in our knowledge of the clinical aspects of SARS-CoV-2 infection in patients with rheumatic diseases, and how the pandemic has changed health care delivery. There is an urgent need to acquire new knowledge on COVID-19 in patients with [rheumatic and musculoskeletal diseases].”
These are the research projects funded:
- Scientist Development Award: Respiratory complications of coronavirus disease (COVID-19) in rheumatic diseases, led by Kristin D’Silva, MD, of Massachusetts General Hospital in Boston (3-year, $225,000 grant)
- Scientist Development Award: COVID-19 in patients with inflammatory arthritis: A prospective study on the effects of immunomodulatory therapy on susceptibility and clinical outcomes, by Rebecca Haberman, MD, of New York University (3-year, $225,000 grant)
- Innovative Research Award: Antiphospholipid antibodies in COVID-19, led by Jason Knight, MD, PhD, of the University of Michigan, Ann Arbor (2-year, $400,000 grant);
- Innovative Research Award: Effectiveness of telerheumatology for delivering high-quality rheumatology care during the COVID-19 crisis, led by Maria Danila, MD, MSc, MSPH, of University of Alabama at Birmingham (2-year, $400,000 grant)
- Norman B. Gaylis, MD, Clinical Research Award: Telehealth-delivered health care to improve care (THRIVE) in community-practice rheumatology, led by Swamy Venuturupalli, MD, of Beverly Hills, Calif.–based Attune Health (2-year, $400,000 grant)
Dr. Bridges said the foundation accepted submissions in basic science, translational science, clinical science, health services research, and patient- and practice-centered research.
“What differentiates these studies from our existing awards portfolio is they all explore the relationships between rheumatic and musculoskeletal diseases and SARS-CoV-2,” he said. “Ultimately, the outcomes of these projects will contribute to a more comprehensive knowledge base and advance avenues of patient care in the COVID-19 pandemic.”
Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., said he was pleased that a telehealth project was chosen as the award given in his name.
“From a COVID point of view, this has been extremely valuable in allowing us to continue to help out patients, connect with our patients, provide them treatment, even if it’s not hands on, at least guide them in how to deal with their chronic rheumatic illnesses,” he said.
This line of research can also help explore the feasibility of telemedicine in helping meet the needs of rural communities facing shortages of rheumatologists.
“Can telemedicine provide a source of rheumatologic access for people who really don’t have a live provider in close proximity?” he said. “I think that’s really why this particular award is very, very timely.”
“It’s so difficult for clinicians to get funding for their research, for their ideas and for the discoveries they were making on a day-to-day basis while they were practicing in a clinical community environment,” he said. “So for me it was really something that inspired me to really create this award.”
Reminders of our mortality can come when physicians least expect it
This time of year I spend weekend afternoons in my hot tub, catching up on medical journals, CME, paperbacks, and generally anything worth reading that shows up in my mailbox.
One of those items was the alumni news from my medical school. As usual, I leafed through it, reading articles of interest and glancing at updates on any classmates that were featured.
Then I stopped.
There, in the back of the magazine, was an obituary on the first of my classmates to pass (that I’m aware of).
I reread it a few times in disbelief. Maybe it was on her taking a new job or being promoted, and was in the wrong section. Nope.
I put the magazine down. She was 1 year younger than me and had gone into internal medicine. Not someone I’d kept in touch with, but certainly was friendly with during those 4 years and frequently chatted with in hallways or between classes. I remember meeting her during the first week of school, when I got her name mixed up with another girl’s in our class. I saw her at parties, meetings, and I think even played doubles tennis with her once, though who we played against I have no idea anymore.
She was at our 20th reunion, and we’d talked for a few minutes. We caught up on our lives since graduation and, as people do at these things, moved on to chat with others.
No details were given as to her death, and it really doesn’t matter.
. For most of each day it’s a fact in the back of our minds, behind the daily activities of working, shopping, doing laundry, commuting, and cooking dinner. After all, it’s really what we do while here that matters, no matter how mundane it may seem.
But sometimes something will push that realization to the front, and make us remember how important every minute really is.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This time of year I spend weekend afternoons in my hot tub, catching up on medical journals, CME, paperbacks, and generally anything worth reading that shows up in my mailbox.
One of those items was the alumni news from my medical school. As usual, I leafed through it, reading articles of interest and glancing at updates on any classmates that were featured.
Then I stopped.
There, in the back of the magazine, was an obituary on the first of my classmates to pass (that I’m aware of).
I reread it a few times in disbelief. Maybe it was on her taking a new job or being promoted, and was in the wrong section. Nope.
I put the magazine down. She was 1 year younger than me and had gone into internal medicine. Not someone I’d kept in touch with, but certainly was friendly with during those 4 years and frequently chatted with in hallways or between classes. I remember meeting her during the first week of school, when I got her name mixed up with another girl’s in our class. I saw her at parties, meetings, and I think even played doubles tennis with her once, though who we played against I have no idea anymore.
She was at our 20th reunion, and we’d talked for a few minutes. We caught up on our lives since graduation and, as people do at these things, moved on to chat with others.
No details were given as to her death, and it really doesn’t matter.
. For most of each day it’s a fact in the back of our minds, behind the daily activities of working, shopping, doing laundry, commuting, and cooking dinner. After all, it’s really what we do while here that matters, no matter how mundane it may seem.
But sometimes something will push that realization to the front, and make us remember how important every minute really is.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This time of year I spend weekend afternoons in my hot tub, catching up on medical journals, CME, paperbacks, and generally anything worth reading that shows up in my mailbox.
One of those items was the alumni news from my medical school. As usual, I leafed through it, reading articles of interest and glancing at updates on any classmates that were featured.
Then I stopped.
There, in the back of the magazine, was an obituary on the first of my classmates to pass (that I’m aware of).
I reread it a few times in disbelief. Maybe it was on her taking a new job or being promoted, and was in the wrong section. Nope.
I put the magazine down. She was 1 year younger than me and had gone into internal medicine. Not someone I’d kept in touch with, but certainly was friendly with during those 4 years and frequently chatted with in hallways or between classes. I remember meeting her during the first week of school, when I got her name mixed up with another girl’s in our class. I saw her at parties, meetings, and I think even played doubles tennis with her once, though who we played against I have no idea anymore.
She was at our 20th reunion, and we’d talked for a few minutes. We caught up on our lives since graduation and, as people do at these things, moved on to chat with others.
No details were given as to her death, and it really doesn’t matter.
. For most of each day it’s a fact in the back of our minds, behind the daily activities of working, shopping, doing laundry, commuting, and cooking dinner. After all, it’s really what we do while here that matters, no matter how mundane it may seem.
But sometimes something will push that realization to the front, and make us remember how important every minute really is.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Psychiatrist alleges plagiarism by journal editor
A psychiatrist known for her expertise in gun violence prevention is alleging that the editor of a medical journal plagiarized her work and published it under his name after she withdrew her paper from the journal.
Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, is still waiting for the Journal of Health Service Psychology, published by Springer, to take action on what she says is blatant copying of an article she and colleague Rocco Pallin, MPH, wrote in response to an invitation from the managing editor, Gary VandenBos, PhD.
Out of frustration and sheer disbelief, Dr. Barnhorst, who is also director of the BulletPoints Project, said she took to Twitter to share her experience.
“I reached a new academic milestone last week when I read a published journal article about firearm suicide and realized it was my and my colleague’s writing! Except that the authors on the paper were these two other guys we don’t know,” Dr. Barnhorst tweeted. Barnhorst did not name the journal or its editor.
“I wasn’t mad so much as befuddled,” she said in an interview. She also wondered if other people had experienced anything similar.
The tweet thread was retweeted 7,800 times and liked by almost 40,000 people.
“I got so many messages and emails and comments from people saying, ‘This [also] happened to me,’ ” Barnhorst said.
In documents shared with this news organization,
The published paper also listed a coauthor, Michael O. Miller, a retired judge who trained as a psychologist, and who has largely written about juvenile delinquency.
Dr. Barnhorst said she became aware of the VandenBos paper when he notified her that it had been posted to the journal’s website. According to Dr. Barnhorst, he said: “Thought you two might be interested to see what we came up with.” When she viewed the article in full, she said she was speechless.
“It was really stunning,” said Dr. Barnhorst, noting that the bibliography, structure, vignette, and other elements were either similar or the same.
As soon as she saw the abstract, she said she became suspicious. Even the case vignette was extremely similar.
In the VandenBos paper, the case was Scott, a white 52-year-old divorced veteran struggling over the relatively recent death of his exwife. Dr. Barnhorst and Ms. Pallin’s vignette was about Robert, a white 55-year-old widower and veteran. In both papers, the patient had problems with alcohol.
Initially, she said, she and Ms. Pallin “were trying to rationalize it or justify it or make excuses for him because it just seemed so out there.” However, the women soon concluded that they were plagiarized.
Dr. Barnhorst said she emailed the journal’s editor-in-chief, Morgan Sammons, PhD, who is also the CEO of the National Register of Health Service Psychologists.
Initially, Dr. Sammons offered her and her colleague coauthorship on the paper, which she rejected. In a subsequent phone call, Dr. Sammons said he would investigate.
Publisher investigating
According to Dr. Barnhorst, Dr. Sammons later said he would retract the paper, but only after suggesting that she not go to “external parties” with her concerns. It was at that point that she emailed Springer.
“My colleague and I believe the evidence of plagiarism is plain and anticipate that you will so conclude,” she wrote in her email to the publishing company. “We are requesting that Springer take prompt remedial action in accordance with prevailing industry standards and your policy on publishing integrity.”
Dr. Barnhorst also told the company she and Ms. Pallin could not submit their original paper for publication elsewhere until Springer made a determination on the plagiarism allegation.
A Springer spokesperson told this news organization that the company is “extremely concerned” and “committed to fully investigating the concerns raised in line with COPE [Committee on Publication Ethics] guidelines, as a matter of urgency.”
On Feb. 1, Springer added an editor’s note to the paper, which has not been taken down or officially retracted. The note said: “Concerns have been raised with this article and are being investigated. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.”
The Springer spokesperson said the company was investigating and would “take further action as appropriate once our investigation is complete.”
Neither Dr. Sammons nor Dr. VandenBos responded to requests for comment.
Dr. Barnhorst has consulted her university’s general counsel but has not taken any legal action and is not currently exploring any, she said in an interview. “It’s not a tough question whether or not this was plagiarism. We just want this article pulled down and retracted.”
A version of this article first appeared on Medscape.com.
A psychiatrist known for her expertise in gun violence prevention is alleging that the editor of a medical journal plagiarized her work and published it under his name after she withdrew her paper from the journal.
Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, is still waiting for the Journal of Health Service Psychology, published by Springer, to take action on what she says is blatant copying of an article she and colleague Rocco Pallin, MPH, wrote in response to an invitation from the managing editor, Gary VandenBos, PhD.
Out of frustration and sheer disbelief, Dr. Barnhorst, who is also director of the BulletPoints Project, said she took to Twitter to share her experience.
“I reached a new academic milestone last week when I read a published journal article about firearm suicide and realized it was my and my colleague’s writing! Except that the authors on the paper were these two other guys we don’t know,” Dr. Barnhorst tweeted. Barnhorst did not name the journal or its editor.
“I wasn’t mad so much as befuddled,” she said in an interview. She also wondered if other people had experienced anything similar.
The tweet thread was retweeted 7,800 times and liked by almost 40,000 people.
“I got so many messages and emails and comments from people saying, ‘This [also] happened to me,’ ” Barnhorst said.
In documents shared with this news organization,
The published paper also listed a coauthor, Michael O. Miller, a retired judge who trained as a psychologist, and who has largely written about juvenile delinquency.
Dr. Barnhorst said she became aware of the VandenBos paper when he notified her that it had been posted to the journal’s website. According to Dr. Barnhorst, he said: “Thought you two might be interested to see what we came up with.” When she viewed the article in full, she said she was speechless.
“It was really stunning,” said Dr. Barnhorst, noting that the bibliography, structure, vignette, and other elements were either similar or the same.
As soon as she saw the abstract, she said she became suspicious. Even the case vignette was extremely similar.
In the VandenBos paper, the case was Scott, a white 52-year-old divorced veteran struggling over the relatively recent death of his exwife. Dr. Barnhorst and Ms. Pallin’s vignette was about Robert, a white 55-year-old widower and veteran. In both papers, the patient had problems with alcohol.
Initially, she said, she and Ms. Pallin “were trying to rationalize it or justify it or make excuses for him because it just seemed so out there.” However, the women soon concluded that they were plagiarized.
Dr. Barnhorst said she emailed the journal’s editor-in-chief, Morgan Sammons, PhD, who is also the CEO of the National Register of Health Service Psychologists.
Initially, Dr. Sammons offered her and her colleague coauthorship on the paper, which she rejected. In a subsequent phone call, Dr. Sammons said he would investigate.
Publisher investigating
According to Dr. Barnhorst, Dr. Sammons later said he would retract the paper, but only after suggesting that she not go to “external parties” with her concerns. It was at that point that she emailed Springer.
“My colleague and I believe the evidence of plagiarism is plain and anticipate that you will so conclude,” she wrote in her email to the publishing company. “We are requesting that Springer take prompt remedial action in accordance with prevailing industry standards and your policy on publishing integrity.”
Dr. Barnhorst also told the company she and Ms. Pallin could not submit their original paper for publication elsewhere until Springer made a determination on the plagiarism allegation.
A Springer spokesperson told this news organization that the company is “extremely concerned” and “committed to fully investigating the concerns raised in line with COPE [Committee on Publication Ethics] guidelines, as a matter of urgency.”
On Feb. 1, Springer added an editor’s note to the paper, which has not been taken down or officially retracted. The note said: “Concerns have been raised with this article and are being investigated. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.”
The Springer spokesperson said the company was investigating and would “take further action as appropriate once our investigation is complete.”
Neither Dr. Sammons nor Dr. VandenBos responded to requests for comment.
Dr. Barnhorst has consulted her university’s general counsel but has not taken any legal action and is not currently exploring any, she said in an interview. “It’s not a tough question whether or not this was plagiarism. We just want this article pulled down and retracted.”
A version of this article first appeared on Medscape.com.
A psychiatrist known for her expertise in gun violence prevention is alleging that the editor of a medical journal plagiarized her work and published it under his name after she withdrew her paper from the journal.
Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, is still waiting for the Journal of Health Service Psychology, published by Springer, to take action on what she says is blatant copying of an article she and colleague Rocco Pallin, MPH, wrote in response to an invitation from the managing editor, Gary VandenBos, PhD.
Out of frustration and sheer disbelief, Dr. Barnhorst, who is also director of the BulletPoints Project, said she took to Twitter to share her experience.
“I reached a new academic milestone last week when I read a published journal article about firearm suicide and realized it was my and my colleague’s writing! Except that the authors on the paper were these two other guys we don’t know,” Dr. Barnhorst tweeted. Barnhorst did not name the journal or its editor.
“I wasn’t mad so much as befuddled,” she said in an interview. She also wondered if other people had experienced anything similar.
The tweet thread was retweeted 7,800 times and liked by almost 40,000 people.
“I got so many messages and emails and comments from people saying, ‘This [also] happened to me,’ ” Barnhorst said.
In documents shared with this news organization,
The published paper also listed a coauthor, Michael O. Miller, a retired judge who trained as a psychologist, and who has largely written about juvenile delinquency.
Dr. Barnhorst said she became aware of the VandenBos paper when he notified her that it had been posted to the journal’s website. According to Dr. Barnhorst, he said: “Thought you two might be interested to see what we came up with.” When she viewed the article in full, she said she was speechless.
“It was really stunning,” said Dr. Barnhorst, noting that the bibliography, structure, vignette, and other elements were either similar or the same.
As soon as she saw the abstract, she said she became suspicious. Even the case vignette was extremely similar.
In the VandenBos paper, the case was Scott, a white 52-year-old divorced veteran struggling over the relatively recent death of his exwife. Dr. Barnhorst and Ms. Pallin’s vignette was about Robert, a white 55-year-old widower and veteran. In both papers, the patient had problems with alcohol.
Initially, she said, she and Ms. Pallin “were trying to rationalize it or justify it or make excuses for him because it just seemed so out there.” However, the women soon concluded that they were plagiarized.
Dr. Barnhorst said she emailed the journal’s editor-in-chief, Morgan Sammons, PhD, who is also the CEO of the National Register of Health Service Psychologists.
Initially, Dr. Sammons offered her and her colleague coauthorship on the paper, which she rejected. In a subsequent phone call, Dr. Sammons said he would investigate.
Publisher investigating
According to Dr. Barnhorst, Dr. Sammons later said he would retract the paper, but only after suggesting that she not go to “external parties” with her concerns. It was at that point that she emailed Springer.
“My colleague and I believe the evidence of plagiarism is plain and anticipate that you will so conclude,” she wrote in her email to the publishing company. “We are requesting that Springer take prompt remedial action in accordance with prevailing industry standards and your policy on publishing integrity.”
Dr. Barnhorst also told the company she and Ms. Pallin could not submit their original paper for publication elsewhere until Springer made a determination on the plagiarism allegation.
A Springer spokesperson told this news organization that the company is “extremely concerned” and “committed to fully investigating the concerns raised in line with COPE [Committee on Publication Ethics] guidelines, as a matter of urgency.”
On Feb. 1, Springer added an editor’s note to the paper, which has not been taken down or officially retracted. The note said: “Concerns have been raised with this article and are being investigated. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.”
The Springer spokesperson said the company was investigating and would “take further action as appropriate once our investigation is complete.”
Neither Dr. Sammons nor Dr. VandenBos responded to requests for comment.
Dr. Barnhorst has consulted her university’s general counsel but has not taken any legal action and is not currently exploring any, she said in an interview. “It’s not a tough question whether or not this was plagiarism. We just want this article pulled down and retracted.”
A version of this article first appeared on Medscape.com.
Views on ethical issues shifting in family, internal medicine
according to the Medscape Internal Medicine Ethics Report 2020 and the corresponding report for Family Medicine.
An example comes in an apparent loosening of attitudes about romantic/sexual relationships with former patients. Now, 31% of internists believe such a relationship is acceptable at least 6 months after the medical relationship has ended. That’s up from 22% in 2018. The number of family physicians this year who said 6 months later was acceptable also increased, but by a smaller margin – from 28% in 2018 to 33% in 2020.
“It’s acceptable as long as there is no undue influence,” David Fleming, MD, a member of the American Medical Association Council on Ethical and Judicial Affairs, said in an interview. “The important thing is that you don’t mix the two.”
Thoughts on upcoding
Views on billing are also shifting. Ten years ago, 17% of physicians overall thought upcoding was acceptable when submitting claims or getting prior authorization. Today just 8% of physicians overall said it was, as did 8% of family medicine (FM) physicians, according to responses.
The number of internal medicine (IM) physicians clearly opposed to upcoding declined a bit from 79% in 2018 to 75% this year, while the number saying “it depends” increased from 11% to 15%.
Many responders in both specialties said they would upgrade a code in the interest of patient advocacy.
An internist put it this way: “If the system is set up so that the only thing that would work for the patient’s condition can be obtained by an upcode, then I would consider this.”
More than a third say random drug checks needed
More than one-third of physicians in both specialties (34% in IM and 38% in FM) said physicians should be subjected to random alcohol and drug testing.
However, many say testing should only happen if abuse is suspected.
Some said specialty matters when it comes to random checks. An internist responded: “I think this is more important for procedure-based physicians.”
Some family physicians said that, if other health care workers were subjected to the same checks in the same circumstances, they would not object, but said doctors shouldn’t be singled out.
Vast majority would report an impaired peer
Nine out of 10 internists and family physicians say they would report a physician who occasionally seemed impaired but most (60% of IM respondents and 62% of FM respondents) said they would do so only after talking with the physician first.
Some noted their decision would depend on the setting.
“Big difference if they are on vacation and drink too much so they need a ride home versus being impaired at work or when on call,” one FM physician said.
About one-third of family physicians (34%) and internists (33%) now favor physician-assisted dying/suicide for incurable suffering. A substantial number (26%-28%) hesitated to make a clear decision in both specialties, responding “it depends.”
“Patient control over quality of life can be even more important than control over its quantity/duration,” one internist wrote.
The proportion of physicians who agreed physician-assisted dying/suicide should be legalized for the terminally ill was much larger, with 49% of family physicians and 52% of IM physicians saying it should.
Talking politics
Data in this survey were collected in summer months of 2020, before the U.S. presidential election, in a highly polarized climate. Some numbers reflect increasing distaste for such conversations with patients.
For example, the number of family physicians who said talking about politics with patients was ethical dropped from 31% in 2018 to 23% in the latest survey. The numbers remained nearly flat among IM physicians in the past 2 years – at 21% in 2018 and 23% this year.
Should a flu shot be mandatory?
Almost three-fourths of physicians overall – and 76% of IM physicians – say annual flu shots should be required for physicians who have patient contact. Agreement was somewhat lower among family physicians at 68%.
Some family physicians cited “freedom of choice” and that they would want to see a higher effectiveness rate before they were mandatory.
Data for this survey, with 5,130 respondents, were collected before COVID-19 vaccines became available.
A version of this article first appeared on Medscape.com.
according to the Medscape Internal Medicine Ethics Report 2020 and the corresponding report for Family Medicine.
An example comes in an apparent loosening of attitudes about romantic/sexual relationships with former patients. Now, 31% of internists believe such a relationship is acceptable at least 6 months after the medical relationship has ended. That’s up from 22% in 2018. The number of family physicians this year who said 6 months later was acceptable also increased, but by a smaller margin – from 28% in 2018 to 33% in 2020.
“It’s acceptable as long as there is no undue influence,” David Fleming, MD, a member of the American Medical Association Council on Ethical and Judicial Affairs, said in an interview. “The important thing is that you don’t mix the two.”
Thoughts on upcoding
Views on billing are also shifting. Ten years ago, 17% of physicians overall thought upcoding was acceptable when submitting claims or getting prior authorization. Today just 8% of physicians overall said it was, as did 8% of family medicine (FM) physicians, according to responses.
The number of internal medicine (IM) physicians clearly opposed to upcoding declined a bit from 79% in 2018 to 75% this year, while the number saying “it depends” increased from 11% to 15%.
Many responders in both specialties said they would upgrade a code in the interest of patient advocacy.
An internist put it this way: “If the system is set up so that the only thing that would work for the patient’s condition can be obtained by an upcode, then I would consider this.”
More than a third say random drug checks needed
More than one-third of physicians in both specialties (34% in IM and 38% in FM) said physicians should be subjected to random alcohol and drug testing.
However, many say testing should only happen if abuse is suspected.
Some said specialty matters when it comes to random checks. An internist responded: “I think this is more important for procedure-based physicians.”
Some family physicians said that, if other health care workers were subjected to the same checks in the same circumstances, they would not object, but said doctors shouldn’t be singled out.
Vast majority would report an impaired peer
Nine out of 10 internists and family physicians say they would report a physician who occasionally seemed impaired but most (60% of IM respondents and 62% of FM respondents) said they would do so only after talking with the physician first.
Some noted their decision would depend on the setting.
“Big difference if they are on vacation and drink too much so they need a ride home versus being impaired at work or when on call,” one FM physician said.
About one-third of family physicians (34%) and internists (33%) now favor physician-assisted dying/suicide for incurable suffering. A substantial number (26%-28%) hesitated to make a clear decision in both specialties, responding “it depends.”
“Patient control over quality of life can be even more important than control over its quantity/duration,” one internist wrote.
The proportion of physicians who agreed physician-assisted dying/suicide should be legalized for the terminally ill was much larger, with 49% of family physicians and 52% of IM physicians saying it should.
Talking politics
Data in this survey were collected in summer months of 2020, before the U.S. presidential election, in a highly polarized climate. Some numbers reflect increasing distaste for such conversations with patients.
For example, the number of family physicians who said talking about politics with patients was ethical dropped from 31% in 2018 to 23% in the latest survey. The numbers remained nearly flat among IM physicians in the past 2 years – at 21% in 2018 and 23% this year.
Should a flu shot be mandatory?
Almost three-fourths of physicians overall – and 76% of IM physicians – say annual flu shots should be required for physicians who have patient contact. Agreement was somewhat lower among family physicians at 68%.
Some family physicians cited “freedom of choice” and that they would want to see a higher effectiveness rate before they were mandatory.
Data for this survey, with 5,130 respondents, were collected before COVID-19 vaccines became available.
A version of this article first appeared on Medscape.com.
according to the Medscape Internal Medicine Ethics Report 2020 and the corresponding report for Family Medicine.
An example comes in an apparent loosening of attitudes about romantic/sexual relationships with former patients. Now, 31% of internists believe such a relationship is acceptable at least 6 months after the medical relationship has ended. That’s up from 22% in 2018. The number of family physicians this year who said 6 months later was acceptable also increased, but by a smaller margin – from 28% in 2018 to 33% in 2020.
“It’s acceptable as long as there is no undue influence,” David Fleming, MD, a member of the American Medical Association Council on Ethical and Judicial Affairs, said in an interview. “The important thing is that you don’t mix the two.”
Thoughts on upcoding
Views on billing are also shifting. Ten years ago, 17% of physicians overall thought upcoding was acceptable when submitting claims or getting prior authorization. Today just 8% of physicians overall said it was, as did 8% of family medicine (FM) physicians, according to responses.
The number of internal medicine (IM) physicians clearly opposed to upcoding declined a bit from 79% in 2018 to 75% this year, while the number saying “it depends” increased from 11% to 15%.
Many responders in both specialties said they would upgrade a code in the interest of patient advocacy.
An internist put it this way: “If the system is set up so that the only thing that would work for the patient’s condition can be obtained by an upcode, then I would consider this.”
More than a third say random drug checks needed
More than one-third of physicians in both specialties (34% in IM and 38% in FM) said physicians should be subjected to random alcohol and drug testing.
However, many say testing should only happen if abuse is suspected.
Some said specialty matters when it comes to random checks. An internist responded: “I think this is more important for procedure-based physicians.”
Some family physicians said that, if other health care workers were subjected to the same checks in the same circumstances, they would not object, but said doctors shouldn’t be singled out.
Vast majority would report an impaired peer
Nine out of 10 internists and family physicians say they would report a physician who occasionally seemed impaired but most (60% of IM respondents and 62% of FM respondents) said they would do so only after talking with the physician first.
Some noted their decision would depend on the setting.
“Big difference if they are on vacation and drink too much so they need a ride home versus being impaired at work or when on call,” one FM physician said.
About one-third of family physicians (34%) and internists (33%) now favor physician-assisted dying/suicide for incurable suffering. A substantial number (26%-28%) hesitated to make a clear decision in both specialties, responding “it depends.”
“Patient control over quality of life can be even more important than control over its quantity/duration,” one internist wrote.
The proportion of physicians who agreed physician-assisted dying/suicide should be legalized for the terminally ill was much larger, with 49% of family physicians and 52% of IM physicians saying it should.
Talking politics
Data in this survey were collected in summer months of 2020, before the U.S. presidential election, in a highly polarized climate. Some numbers reflect increasing distaste for such conversations with patients.
For example, the number of family physicians who said talking about politics with patients was ethical dropped from 31% in 2018 to 23% in the latest survey. The numbers remained nearly flat among IM physicians in the past 2 years – at 21% in 2018 and 23% this year.
Should a flu shot be mandatory?
Almost three-fourths of physicians overall – and 76% of IM physicians – say annual flu shots should be required for physicians who have patient contact. Agreement was somewhat lower among family physicians at 68%.
Some family physicians cited “freedom of choice” and that they would want to see a higher effectiveness rate before they were mandatory.
Data for this survey, with 5,130 respondents, were collected before COVID-19 vaccines became available.
A version of this article first appeared on Medscape.com.
The Match and COVID-19: Stolen interviews, swag bags, and stress
The final numbers won’t look much different, but the 2021 Match results will be unlike any before. As of mid-January, only 16 more institutions were confirmed to be participating in Match Day this year, resulting in about 800 more positions, said Donna Lamb, president and CEO of the National Resident Matching Program (NRMP). The Electronic Residency Application Service reported about 50,000 individual applicant submissions, a slight increase from prior years.
The stats may be similar, but the current residency application cycle may lead to wildly different results after the pandemic forced interviews to be conducted virtually and caused the cancellation of most away clinical rotations. Troy Amen, a fifth-year MD-MBA student at Harvard Medical School, Boston, and copresident of his student class, says the lack of on-campus, in-person experiences means students feel more in the dark than ever. The same is true for institutions. “The programs are also suffering because now they don’t know which students are a good ‘cultural fit’ for them,” he said.
Standing out has always been a concern for prospective residents, but Mr. Amen says fears are even higher this year. “[Institutions are] struggling to vet out 850 applicants, and they have no connection to us.”
Organizations have scrambled to keep the process as fair and informative as possible. “Everyone is trying to do the right thing here,” said Alison J. Whelan, MD, chief academic officer of the Association of American Medical Colleges (AAMC). She says that although the process has significantly changed, the heart of it remains the same. “The bottom line is directors really want to fill their intern class, and schools and students really want to match.”
Since the NRMP was established in 1952, it has never had to contend with a pandemic of this scale. The unprecedented circumstances have led to some much-feared and some unexpected changes, like top candidates “stealing” interview slots, “swag bags” sent to entice residents, beefed-up online profiles, as well as “Zoom fatigue,” a spike in home-field advantage for institutions, and massive anxiety for those students staking their future to a city they may have never seen in person.
What was lost and what was gained
“It’s really hard to get a real feel for the program when you’ve not been there in person,” said Christopher Smith, MD, director of the internal medicine residency program at Beth Israel Deaconess Medical Center in Boston. Dr. Smith recalled interviewing for residencies 25 years ago. His wife, a teacher, took time off to travel with him.
“She would ‘interview the town’ while I interviewed the program, and we compared notes at night,” he said. Because of COVID-19-related travel restrictions, just physically seeing the city in which they may live for years wasn’t an option for many. “I have a lot of sympathy for students applying right now,” Dr. Smith said.
For the residency class of 2021, the first shoe really dropped last March, when the AAMC issued guidance strongly recommending that programs pause clinical rotations away from their home schools. As established doctors know well, and as graduating medical students confirmed, these rotations are crucial to understanding a program’s culture and gaining experience that can boost candidacy. “I’m applying to orthopedic surgery, where away rotations are the gold standard for impressing attendees and residents at institutions away from home,” said Mr. Amen.
The pandemic completely cut off that key source of information to determine the right fit. It also meant applicants couldn’t have as diverse a portfolio of recommendation letters, something many worry may be detrimental to their soon-to-be-released Match rankings.
Unlike the loss of away rotations, the forced shift from in-person to virtual interviews had some meaningful benefits. Students no longer incurred expenses for airline flights, hotel rooms, and rental cars. Many organizations and programs have been trying for years to figure out how to lower the financial burden of interviews to make the process more equitable for those at economic or other disadvantage.
“The equity piece of this is huge – decreasing barriers and leveling the field a little bit is a really huge advantage,” said Kate Shaw, MD, residency program director and associate chair of education for the obstetrics and gynecology program at Stanford (Calif.) University. In some ways, this latest change is an extension of a strategy Dr. Shaw and others had already begun implementing.
“Over the last 5 to 10 years, we’ve been working to address the implicit bias in the application process, so we’ve gone to a holistic review of applicants, where we don’t have score cutoffs. We look at the whole person,” she said. “And we did that in an effort to increase diversity and equity.” Dr. Shaw and others hope that the accidental positive changes from COVID restrictions may be intentionally preserved long after the pandemic ends.
Home-field advantage vs. swag bags
Many medical students applying to residencies this year say they have given greater weight to their home programs than they might have without the pandemic. “I didn’t get a sense of anyone’s culture other than my home institution,” said Alex Skidmore, a fourth-year medical student at Washington University in St. Louis. “I definitely am ranking Wash-U higher.”
The desire to emphasize the known quality of a student’s home institution isn’t surprising to program directors. Dr. Shaw said she thinks this year’s Match could well end with a higher percentage of students matching either in their home programs or in programs close to loved ones. “The value of being close to family has come up in our conversations, where students are considering the right program for them but also the other life factors,” she said.
To overcome this home-field advantage, many programs have beefed up their websites, including providing video tours of their facilities. They also “upped their social media game” and encouraged residents to create online groups for prospective residents to share information about programs and life outside of work. Some residents even offered video tours of their personal apartments to applicants.
Without in-person access to facilities and staff, a program’s online presence became a deciding factor, applicants said. “If you have a bad website, it’s like having a dirty building to interview applicants in,” Mr. Skidmore said. For many prospective residents, an institution’s Internet presence was a “make or break” factor. “It’s the only thing I saw for many programs, and when we are doing the amount of research we are doing remotely, when I saw a program with a bad website, it made me not like the program as much,” he said.
Some programs, hoping to woo candidates as well as to provide them with more insight into what they and their cities have to offer, sent “swag bags” to candidates. These included things like gift cards for food delivery and offerings from local businesses. Washington University’s pediatrics residency program sent gooey butter cakes – a St. Louis staple – along with other treats from small businesses and copies of magazines that showcased the city’s dining and entertainment scene.
Other programs, even those at the same medical institution, felt quite strongly that those types of packages shouldn’t be sent. “We interviewed almost 500 applicants, so there was no way we could have afforded that,” said Dominique Cosco, MD, director of Washington University’s internal medicine residency program. “Our normal recruitment budget is almost $100,000 in a normal year, and that got cut because of COVID. For us, it was thinking about allocations of resources.”
Interview slot theft and zoom fatigue
Remote interviewing also meant that applicants could accept more interviews, something that raised a big concern. Without expenses or travel time, would top-tier candidates take more interviews than normal and thus take limited interview spots from other qualified candidates? Maybe so, says the AAMC’s Dr. Whelan.
“We didn’t have systematic data, but we heard from enough schools and programs ... that students who were maybe not the top-top ranked students in the class but in every way solid were receiving fewer interviews than previous years,” Dr. Whelan said. This is despite guidance that recommended programs add interview slots to serve as a counterbalance.
Some students say they accepted more interview slots in the beginning of the interview season, partly because they could, and partly because some thought of early interviews as “practice” for later interviews. However, as video interviews piled up, some of them described feeling “Zoom fatigue” and said they later canceled interviews with programs they didn’t anticipate joining.
More SOAP, less clarity
As for what comes next, the NRMP is preparing for a longer-than-normal Supplemental Offer and Acceptance Program (SOAP) than in years past. SOAP usually offers three rounds of matches after the initial Match Day; Ms. Lamb said things are different this year.
“SOAP will be the same number of days, but we’ve added an additional round on Thursday afternoon,” she said. Will it be unnecessary or not enough? Nobody knows. “How big SOAP actually is going to be is one of the things that we really don’t have a sense of right now and probably aren’t going to have a sense of until the Match.”
Uncertainty is the name of the game. More than any other Match before, programs and applicants won’t know how results from this pandemic year stack up for a few months at the very least. “I really want to see what this looks like on the other side,” Dr. Smith said. “Are applicants happy with the way it looks when they come here? Do they feel like they matched with the right place?”
Whether this unprecedented year will be remembered more for positive changes moving forward, including more flexibility on remote interviews, or for less-informed decisions that result in dissatisfied participants is also unclear.
“I think after the Match is over, we’ll be talking to everyone to get more perspective on what people who are applying now would tell the next class, and how programs can adjust,” said Kathy Diemer, MD, assistant dean for career counseling at Washington University. At the very least, those who are involved in this year after year can start thinking about what the future should look like.
“We’re going to need to do some kind of debriefing after this is over, both program directors and our students as well, so we can determine how to move forward next year and beyond.”
A version of this article first appeared on Medscape.com.
The final numbers won’t look much different, but the 2021 Match results will be unlike any before. As of mid-January, only 16 more institutions were confirmed to be participating in Match Day this year, resulting in about 800 more positions, said Donna Lamb, president and CEO of the National Resident Matching Program (NRMP). The Electronic Residency Application Service reported about 50,000 individual applicant submissions, a slight increase from prior years.
The stats may be similar, but the current residency application cycle may lead to wildly different results after the pandemic forced interviews to be conducted virtually and caused the cancellation of most away clinical rotations. Troy Amen, a fifth-year MD-MBA student at Harvard Medical School, Boston, and copresident of his student class, says the lack of on-campus, in-person experiences means students feel more in the dark than ever. The same is true for institutions. “The programs are also suffering because now they don’t know which students are a good ‘cultural fit’ for them,” he said.
Standing out has always been a concern for prospective residents, but Mr. Amen says fears are even higher this year. “[Institutions are] struggling to vet out 850 applicants, and they have no connection to us.”
Organizations have scrambled to keep the process as fair and informative as possible. “Everyone is trying to do the right thing here,” said Alison J. Whelan, MD, chief academic officer of the Association of American Medical Colleges (AAMC). She says that although the process has significantly changed, the heart of it remains the same. “The bottom line is directors really want to fill their intern class, and schools and students really want to match.”
Since the NRMP was established in 1952, it has never had to contend with a pandemic of this scale. The unprecedented circumstances have led to some much-feared and some unexpected changes, like top candidates “stealing” interview slots, “swag bags” sent to entice residents, beefed-up online profiles, as well as “Zoom fatigue,” a spike in home-field advantage for institutions, and massive anxiety for those students staking their future to a city they may have never seen in person.
What was lost and what was gained
“It’s really hard to get a real feel for the program when you’ve not been there in person,” said Christopher Smith, MD, director of the internal medicine residency program at Beth Israel Deaconess Medical Center in Boston. Dr. Smith recalled interviewing for residencies 25 years ago. His wife, a teacher, took time off to travel with him.
“She would ‘interview the town’ while I interviewed the program, and we compared notes at night,” he said. Because of COVID-19-related travel restrictions, just physically seeing the city in which they may live for years wasn’t an option for many. “I have a lot of sympathy for students applying right now,” Dr. Smith said.
For the residency class of 2021, the first shoe really dropped last March, when the AAMC issued guidance strongly recommending that programs pause clinical rotations away from their home schools. As established doctors know well, and as graduating medical students confirmed, these rotations are crucial to understanding a program’s culture and gaining experience that can boost candidacy. “I’m applying to orthopedic surgery, where away rotations are the gold standard for impressing attendees and residents at institutions away from home,” said Mr. Amen.
The pandemic completely cut off that key source of information to determine the right fit. It also meant applicants couldn’t have as diverse a portfolio of recommendation letters, something many worry may be detrimental to their soon-to-be-released Match rankings.
Unlike the loss of away rotations, the forced shift from in-person to virtual interviews had some meaningful benefits. Students no longer incurred expenses for airline flights, hotel rooms, and rental cars. Many organizations and programs have been trying for years to figure out how to lower the financial burden of interviews to make the process more equitable for those at economic or other disadvantage.
“The equity piece of this is huge – decreasing barriers and leveling the field a little bit is a really huge advantage,” said Kate Shaw, MD, residency program director and associate chair of education for the obstetrics and gynecology program at Stanford (Calif.) University. In some ways, this latest change is an extension of a strategy Dr. Shaw and others had already begun implementing.
“Over the last 5 to 10 years, we’ve been working to address the implicit bias in the application process, so we’ve gone to a holistic review of applicants, where we don’t have score cutoffs. We look at the whole person,” she said. “And we did that in an effort to increase diversity and equity.” Dr. Shaw and others hope that the accidental positive changes from COVID restrictions may be intentionally preserved long after the pandemic ends.
Home-field advantage vs. swag bags
Many medical students applying to residencies this year say they have given greater weight to their home programs than they might have without the pandemic. “I didn’t get a sense of anyone’s culture other than my home institution,” said Alex Skidmore, a fourth-year medical student at Washington University in St. Louis. “I definitely am ranking Wash-U higher.”
The desire to emphasize the known quality of a student’s home institution isn’t surprising to program directors. Dr. Shaw said she thinks this year’s Match could well end with a higher percentage of students matching either in their home programs or in programs close to loved ones. “The value of being close to family has come up in our conversations, where students are considering the right program for them but also the other life factors,” she said.
To overcome this home-field advantage, many programs have beefed up their websites, including providing video tours of their facilities. They also “upped their social media game” and encouraged residents to create online groups for prospective residents to share information about programs and life outside of work. Some residents even offered video tours of their personal apartments to applicants.
Without in-person access to facilities and staff, a program’s online presence became a deciding factor, applicants said. “If you have a bad website, it’s like having a dirty building to interview applicants in,” Mr. Skidmore said. For many prospective residents, an institution’s Internet presence was a “make or break” factor. “It’s the only thing I saw for many programs, and when we are doing the amount of research we are doing remotely, when I saw a program with a bad website, it made me not like the program as much,” he said.
Some programs, hoping to woo candidates as well as to provide them with more insight into what they and their cities have to offer, sent “swag bags” to candidates. These included things like gift cards for food delivery and offerings from local businesses. Washington University’s pediatrics residency program sent gooey butter cakes – a St. Louis staple – along with other treats from small businesses and copies of magazines that showcased the city’s dining and entertainment scene.
Other programs, even those at the same medical institution, felt quite strongly that those types of packages shouldn’t be sent. “We interviewed almost 500 applicants, so there was no way we could have afforded that,” said Dominique Cosco, MD, director of Washington University’s internal medicine residency program. “Our normal recruitment budget is almost $100,000 in a normal year, and that got cut because of COVID. For us, it was thinking about allocations of resources.”
Interview slot theft and zoom fatigue
Remote interviewing also meant that applicants could accept more interviews, something that raised a big concern. Without expenses or travel time, would top-tier candidates take more interviews than normal and thus take limited interview spots from other qualified candidates? Maybe so, says the AAMC’s Dr. Whelan.
“We didn’t have systematic data, but we heard from enough schools and programs ... that students who were maybe not the top-top ranked students in the class but in every way solid were receiving fewer interviews than previous years,” Dr. Whelan said. This is despite guidance that recommended programs add interview slots to serve as a counterbalance.
Some students say they accepted more interview slots in the beginning of the interview season, partly because they could, and partly because some thought of early interviews as “practice” for later interviews. However, as video interviews piled up, some of them described feeling “Zoom fatigue” and said they later canceled interviews with programs they didn’t anticipate joining.
More SOAP, less clarity
As for what comes next, the NRMP is preparing for a longer-than-normal Supplemental Offer and Acceptance Program (SOAP) than in years past. SOAP usually offers three rounds of matches after the initial Match Day; Ms. Lamb said things are different this year.
“SOAP will be the same number of days, but we’ve added an additional round on Thursday afternoon,” she said. Will it be unnecessary or not enough? Nobody knows. “How big SOAP actually is going to be is one of the things that we really don’t have a sense of right now and probably aren’t going to have a sense of until the Match.”
Uncertainty is the name of the game. More than any other Match before, programs and applicants won’t know how results from this pandemic year stack up for a few months at the very least. “I really want to see what this looks like on the other side,” Dr. Smith said. “Are applicants happy with the way it looks when they come here? Do they feel like they matched with the right place?”
Whether this unprecedented year will be remembered more for positive changes moving forward, including more flexibility on remote interviews, or for less-informed decisions that result in dissatisfied participants is also unclear.
“I think after the Match is over, we’ll be talking to everyone to get more perspective on what people who are applying now would tell the next class, and how programs can adjust,” said Kathy Diemer, MD, assistant dean for career counseling at Washington University. At the very least, those who are involved in this year after year can start thinking about what the future should look like.
“We’re going to need to do some kind of debriefing after this is over, both program directors and our students as well, so we can determine how to move forward next year and beyond.”
A version of this article first appeared on Medscape.com.
The final numbers won’t look much different, but the 2021 Match results will be unlike any before. As of mid-January, only 16 more institutions were confirmed to be participating in Match Day this year, resulting in about 800 more positions, said Donna Lamb, president and CEO of the National Resident Matching Program (NRMP). The Electronic Residency Application Service reported about 50,000 individual applicant submissions, a slight increase from prior years.
The stats may be similar, but the current residency application cycle may lead to wildly different results after the pandemic forced interviews to be conducted virtually and caused the cancellation of most away clinical rotations. Troy Amen, a fifth-year MD-MBA student at Harvard Medical School, Boston, and copresident of his student class, says the lack of on-campus, in-person experiences means students feel more in the dark than ever. The same is true for institutions. “The programs are also suffering because now they don’t know which students are a good ‘cultural fit’ for them,” he said.
Standing out has always been a concern for prospective residents, but Mr. Amen says fears are even higher this year. “[Institutions are] struggling to vet out 850 applicants, and they have no connection to us.”
Organizations have scrambled to keep the process as fair and informative as possible. “Everyone is trying to do the right thing here,” said Alison J. Whelan, MD, chief academic officer of the Association of American Medical Colleges (AAMC). She says that although the process has significantly changed, the heart of it remains the same. “The bottom line is directors really want to fill their intern class, and schools and students really want to match.”
Since the NRMP was established in 1952, it has never had to contend with a pandemic of this scale. The unprecedented circumstances have led to some much-feared and some unexpected changes, like top candidates “stealing” interview slots, “swag bags” sent to entice residents, beefed-up online profiles, as well as “Zoom fatigue,” a spike in home-field advantage for institutions, and massive anxiety for those students staking their future to a city they may have never seen in person.
What was lost and what was gained
“It’s really hard to get a real feel for the program when you’ve not been there in person,” said Christopher Smith, MD, director of the internal medicine residency program at Beth Israel Deaconess Medical Center in Boston. Dr. Smith recalled interviewing for residencies 25 years ago. His wife, a teacher, took time off to travel with him.
“She would ‘interview the town’ while I interviewed the program, and we compared notes at night,” he said. Because of COVID-19-related travel restrictions, just physically seeing the city in which they may live for years wasn’t an option for many. “I have a lot of sympathy for students applying right now,” Dr. Smith said.
For the residency class of 2021, the first shoe really dropped last March, when the AAMC issued guidance strongly recommending that programs pause clinical rotations away from their home schools. As established doctors know well, and as graduating medical students confirmed, these rotations are crucial to understanding a program’s culture and gaining experience that can boost candidacy. “I’m applying to orthopedic surgery, where away rotations are the gold standard for impressing attendees and residents at institutions away from home,” said Mr. Amen.
The pandemic completely cut off that key source of information to determine the right fit. It also meant applicants couldn’t have as diverse a portfolio of recommendation letters, something many worry may be detrimental to their soon-to-be-released Match rankings.
Unlike the loss of away rotations, the forced shift from in-person to virtual interviews had some meaningful benefits. Students no longer incurred expenses for airline flights, hotel rooms, and rental cars. Many organizations and programs have been trying for years to figure out how to lower the financial burden of interviews to make the process more equitable for those at economic or other disadvantage.
“The equity piece of this is huge – decreasing barriers and leveling the field a little bit is a really huge advantage,” said Kate Shaw, MD, residency program director and associate chair of education for the obstetrics and gynecology program at Stanford (Calif.) University. In some ways, this latest change is an extension of a strategy Dr. Shaw and others had already begun implementing.
“Over the last 5 to 10 years, we’ve been working to address the implicit bias in the application process, so we’ve gone to a holistic review of applicants, where we don’t have score cutoffs. We look at the whole person,” she said. “And we did that in an effort to increase diversity and equity.” Dr. Shaw and others hope that the accidental positive changes from COVID restrictions may be intentionally preserved long after the pandemic ends.
Home-field advantage vs. swag bags
Many medical students applying to residencies this year say they have given greater weight to their home programs than they might have without the pandemic. “I didn’t get a sense of anyone’s culture other than my home institution,” said Alex Skidmore, a fourth-year medical student at Washington University in St. Louis. “I definitely am ranking Wash-U higher.”
The desire to emphasize the known quality of a student’s home institution isn’t surprising to program directors. Dr. Shaw said she thinks this year’s Match could well end with a higher percentage of students matching either in their home programs or in programs close to loved ones. “The value of being close to family has come up in our conversations, where students are considering the right program for them but also the other life factors,” she said.
To overcome this home-field advantage, many programs have beefed up their websites, including providing video tours of their facilities. They also “upped their social media game” and encouraged residents to create online groups for prospective residents to share information about programs and life outside of work. Some residents even offered video tours of their personal apartments to applicants.
Without in-person access to facilities and staff, a program’s online presence became a deciding factor, applicants said. “If you have a bad website, it’s like having a dirty building to interview applicants in,” Mr. Skidmore said. For many prospective residents, an institution’s Internet presence was a “make or break” factor. “It’s the only thing I saw for many programs, and when we are doing the amount of research we are doing remotely, when I saw a program with a bad website, it made me not like the program as much,” he said.
Some programs, hoping to woo candidates as well as to provide them with more insight into what they and their cities have to offer, sent “swag bags” to candidates. These included things like gift cards for food delivery and offerings from local businesses. Washington University’s pediatrics residency program sent gooey butter cakes – a St. Louis staple – along with other treats from small businesses and copies of magazines that showcased the city’s dining and entertainment scene.
Other programs, even those at the same medical institution, felt quite strongly that those types of packages shouldn’t be sent. “We interviewed almost 500 applicants, so there was no way we could have afforded that,” said Dominique Cosco, MD, director of Washington University’s internal medicine residency program. “Our normal recruitment budget is almost $100,000 in a normal year, and that got cut because of COVID. For us, it was thinking about allocations of resources.”
Interview slot theft and zoom fatigue
Remote interviewing also meant that applicants could accept more interviews, something that raised a big concern. Without expenses or travel time, would top-tier candidates take more interviews than normal and thus take limited interview spots from other qualified candidates? Maybe so, says the AAMC’s Dr. Whelan.
“We didn’t have systematic data, but we heard from enough schools and programs ... that students who were maybe not the top-top ranked students in the class but in every way solid were receiving fewer interviews than previous years,” Dr. Whelan said. This is despite guidance that recommended programs add interview slots to serve as a counterbalance.
Some students say they accepted more interview slots in the beginning of the interview season, partly because they could, and partly because some thought of early interviews as “practice” for later interviews. However, as video interviews piled up, some of them described feeling “Zoom fatigue” and said they later canceled interviews with programs they didn’t anticipate joining.
More SOAP, less clarity
As for what comes next, the NRMP is preparing for a longer-than-normal Supplemental Offer and Acceptance Program (SOAP) than in years past. SOAP usually offers three rounds of matches after the initial Match Day; Ms. Lamb said things are different this year.
“SOAP will be the same number of days, but we’ve added an additional round on Thursday afternoon,” she said. Will it be unnecessary or not enough? Nobody knows. “How big SOAP actually is going to be is one of the things that we really don’t have a sense of right now and probably aren’t going to have a sense of until the Match.”
Uncertainty is the name of the game. More than any other Match before, programs and applicants won’t know how results from this pandemic year stack up for a few months at the very least. “I really want to see what this looks like on the other side,” Dr. Smith said. “Are applicants happy with the way it looks when they come here? Do they feel like they matched with the right place?”
Whether this unprecedented year will be remembered more for positive changes moving forward, including more flexibility on remote interviews, or for less-informed decisions that result in dissatisfied participants is also unclear.
“I think after the Match is over, we’ll be talking to everyone to get more perspective on what people who are applying now would tell the next class, and how programs can adjust,” said Kathy Diemer, MD, assistant dean for career counseling at Washington University. At the very least, those who are involved in this year after year can start thinking about what the future should look like.
“We’re going to need to do some kind of debriefing after this is over, both program directors and our students as well, so we can determine how to move forward next year and beyond.”
A version of this article first appeared on Medscape.com.
How to choose the best aesthetic devices when launching your career
When a new body contouring device hit the market a few years ago, Nazanin Saedi, MD, had an opportunity to become the first Philadelphia area dermatologist to add the technology to her practice.
“I thought about it, but it didn’t make sense because it wasn’t something important to my patient population,” Dr. Saedi, who directs the Jefferson Laser Surgery and Cosmetic Dermatology Center in Philadelphia, said during the Orlando Dermatology Aesthetic and Clinical Conference. “If I’m not going to have the patient demand and make money from it, then it just doesn’t make sense.”
That experience illustrates one of many pearls of advice that Dr. Saedi shared during . “Include additional questions in new patient intake forms or online forms to get a sense of what your patient population is interested in,” she advised. “It’s important to understand that before you start to offer new services. Don’t just depend on social media to inform you of the latest trends and what people are doing across the country, because if you purchase something that is very popular on social media for people in New York or L.A., that might not be the best for your practice.”
According to market trends from the American Society for Dermatologic Surgery, 3.5 million laser-, light-, and energy-based procedures were performed in 2018. The top five were for wrinkles (809,166), sun damage (786,856), facial redness (612,367), excess hair (385,466), and melasma (226,007). “Considering this data, when you start a practice, do you buy something for wrinkles or for sun damage right away?” Dr. Saedi asked. “Maybe, but you really need to gauge the market that you practice in. You also want to consider your own skill set and what other dermatologists in your area are offering. If you don’t want to do aggressive procedures, then purchasing a fractional CO2 laser might not be the best device to start off with. If you are not comfortable dealing with those patients, and potential infections and scarring, then that’s not the right treatment for you. You have to reflect on and identify what you’re comfortable learning and doing and managing.”
Taking time to investigate the services offered by dermatologists and med spas within a few miles of your practice can help you avoid redundancy. “Learn the techniques and the small nuances that will give you a little bit of finesse and make you an expert, to set you apart from other practices,” said Dr. Saedi, who coauthored a chapter in the book, “The Business of Dermatology” (New York: Thieme Medical Publishers, 2020). “I always recommend treating your staff and members of your family, to understand how you can tweak treatments to get the most out of them. Once you treat your staff, they are walking advertisements for what you do. They can also counsel patients, walking them through the healing process after a procedure, so they can know what to expect.”
Appropriate planning and preparation can help avoid acquiring the wrong device, she continued. This includes patient demand, scheduling availability, office space, overhead costs, and the level of staff training. She recommends buying one device at a time and clearing profitability from that device before purchasing another, “because it can be a burden on your practice to have multiple devices all at once,” she said. “You also have to think about the hidden costs – the maintenance and the service contracts. That can exceed $10,000 per year, so consider that when you’re looking to purchase a new device.”
Most people buy laser-, light-, and energy-based devices, but renting for a stretch can help you test the waters without a significant long-term investment. “It might not be the newest laser, but it can help you gauge how much of demand you have for that service to see if you have the patient base to make that larger step of purchasing the device,” she said. “If you buy a new device, make sure that it’s not a counterfeit and that you still have a company service contract. There are many third-party companies selling pre-owned laser aesthetics. Make sure you’re getting the authentic device and that there is some kind of a service contract with the actual manufacturer so they can help fix it when things break down.”
When Dr. Saedi counsels residents about purchasing devices, she typically recommends these five categories in order of preference: vascular, pigment, hair, resurfacing, and body contouring/skin tightening. “If you can cover vascular, pigment, and some kind of textural improvement, you can treat about 90% of aesthetic patients who come through your door,” she said. “Sure, there are some who may want skin tightening that you may not be able to offer with laser resurfacing, but you’re going to be able capture a high patient population by offering these services,” she added. That is why a lot of people end up getting a platform with attachable handpieces, “where you can have one system that is able to offer many different services right off the bat.”
She advised factoring in the amount of time it takes for a procedure and how much time it will take up in a certain room. “That will affect your revenue as well. Are you going to delegate this, or is this something you will do on your own? Take that into account.”
Above all, don’t rush your device purchase. “Some laser company sales representatives may pressure you at the end of a quarter by saying, ‘This is the best deal I’m going to offer you. You’re never going to get a deal like this ever again,’ ” she said. “I advise people to do multiple demos so you’re not just doing a demo for a day and seeing one or two patients. Treat the same patients again a month later. Do multiple demos so that you can feel comfortable. Talk to dermatologists who have the device, who have real experience with it, so you can have the most amount of information moving forward.”
Dr. Saedi reported that she has received equipment from Alma, Aerolase, Cartessa, and Cynosure. She is a consultant to and/or an advisory board member for those companies, as well as for Alastin.
When a new body contouring device hit the market a few years ago, Nazanin Saedi, MD, had an opportunity to become the first Philadelphia area dermatologist to add the technology to her practice.
“I thought about it, but it didn’t make sense because it wasn’t something important to my patient population,” Dr. Saedi, who directs the Jefferson Laser Surgery and Cosmetic Dermatology Center in Philadelphia, said during the Orlando Dermatology Aesthetic and Clinical Conference. “If I’m not going to have the patient demand and make money from it, then it just doesn’t make sense.”
That experience illustrates one of many pearls of advice that Dr. Saedi shared during . “Include additional questions in new patient intake forms or online forms to get a sense of what your patient population is interested in,” she advised. “It’s important to understand that before you start to offer new services. Don’t just depend on social media to inform you of the latest trends and what people are doing across the country, because if you purchase something that is very popular on social media for people in New York or L.A., that might not be the best for your practice.”
According to market trends from the American Society for Dermatologic Surgery, 3.5 million laser-, light-, and energy-based procedures were performed in 2018. The top five were for wrinkles (809,166), sun damage (786,856), facial redness (612,367), excess hair (385,466), and melasma (226,007). “Considering this data, when you start a practice, do you buy something for wrinkles or for sun damage right away?” Dr. Saedi asked. “Maybe, but you really need to gauge the market that you practice in. You also want to consider your own skill set and what other dermatologists in your area are offering. If you don’t want to do aggressive procedures, then purchasing a fractional CO2 laser might not be the best device to start off with. If you are not comfortable dealing with those patients, and potential infections and scarring, then that’s not the right treatment for you. You have to reflect on and identify what you’re comfortable learning and doing and managing.”
Taking time to investigate the services offered by dermatologists and med spas within a few miles of your practice can help you avoid redundancy. “Learn the techniques and the small nuances that will give you a little bit of finesse and make you an expert, to set you apart from other practices,” said Dr. Saedi, who coauthored a chapter in the book, “The Business of Dermatology” (New York: Thieme Medical Publishers, 2020). “I always recommend treating your staff and members of your family, to understand how you can tweak treatments to get the most out of them. Once you treat your staff, they are walking advertisements for what you do. They can also counsel patients, walking them through the healing process after a procedure, so they can know what to expect.”
Appropriate planning and preparation can help avoid acquiring the wrong device, she continued. This includes patient demand, scheduling availability, office space, overhead costs, and the level of staff training. She recommends buying one device at a time and clearing profitability from that device before purchasing another, “because it can be a burden on your practice to have multiple devices all at once,” she said. “You also have to think about the hidden costs – the maintenance and the service contracts. That can exceed $10,000 per year, so consider that when you’re looking to purchase a new device.”
Most people buy laser-, light-, and energy-based devices, but renting for a stretch can help you test the waters without a significant long-term investment. “It might not be the newest laser, but it can help you gauge how much of demand you have for that service to see if you have the patient base to make that larger step of purchasing the device,” she said. “If you buy a new device, make sure that it’s not a counterfeit and that you still have a company service contract. There are many third-party companies selling pre-owned laser aesthetics. Make sure you’re getting the authentic device and that there is some kind of a service contract with the actual manufacturer so they can help fix it when things break down.”
When Dr. Saedi counsels residents about purchasing devices, she typically recommends these five categories in order of preference: vascular, pigment, hair, resurfacing, and body contouring/skin tightening. “If you can cover vascular, pigment, and some kind of textural improvement, you can treat about 90% of aesthetic patients who come through your door,” she said. “Sure, there are some who may want skin tightening that you may not be able to offer with laser resurfacing, but you’re going to be able capture a high patient population by offering these services,” she added. That is why a lot of people end up getting a platform with attachable handpieces, “where you can have one system that is able to offer many different services right off the bat.”
She advised factoring in the amount of time it takes for a procedure and how much time it will take up in a certain room. “That will affect your revenue as well. Are you going to delegate this, or is this something you will do on your own? Take that into account.”
Above all, don’t rush your device purchase. “Some laser company sales representatives may pressure you at the end of a quarter by saying, ‘This is the best deal I’m going to offer you. You’re never going to get a deal like this ever again,’ ” she said. “I advise people to do multiple demos so you’re not just doing a demo for a day and seeing one or two patients. Treat the same patients again a month later. Do multiple demos so that you can feel comfortable. Talk to dermatologists who have the device, who have real experience with it, so you can have the most amount of information moving forward.”
Dr. Saedi reported that she has received equipment from Alma, Aerolase, Cartessa, and Cynosure. She is a consultant to and/or an advisory board member for those companies, as well as for Alastin.
When a new body contouring device hit the market a few years ago, Nazanin Saedi, MD, had an opportunity to become the first Philadelphia area dermatologist to add the technology to her practice.
“I thought about it, but it didn’t make sense because it wasn’t something important to my patient population,” Dr. Saedi, who directs the Jefferson Laser Surgery and Cosmetic Dermatology Center in Philadelphia, said during the Orlando Dermatology Aesthetic and Clinical Conference. “If I’m not going to have the patient demand and make money from it, then it just doesn’t make sense.”
That experience illustrates one of many pearls of advice that Dr. Saedi shared during . “Include additional questions in new patient intake forms or online forms to get a sense of what your patient population is interested in,” she advised. “It’s important to understand that before you start to offer new services. Don’t just depend on social media to inform you of the latest trends and what people are doing across the country, because if you purchase something that is very popular on social media for people in New York or L.A., that might not be the best for your practice.”
According to market trends from the American Society for Dermatologic Surgery, 3.5 million laser-, light-, and energy-based procedures were performed in 2018. The top five were for wrinkles (809,166), sun damage (786,856), facial redness (612,367), excess hair (385,466), and melasma (226,007). “Considering this data, when you start a practice, do you buy something for wrinkles or for sun damage right away?” Dr. Saedi asked. “Maybe, but you really need to gauge the market that you practice in. You also want to consider your own skill set and what other dermatologists in your area are offering. If you don’t want to do aggressive procedures, then purchasing a fractional CO2 laser might not be the best device to start off with. If you are not comfortable dealing with those patients, and potential infections and scarring, then that’s not the right treatment for you. You have to reflect on and identify what you’re comfortable learning and doing and managing.”
Taking time to investigate the services offered by dermatologists and med spas within a few miles of your practice can help you avoid redundancy. “Learn the techniques and the small nuances that will give you a little bit of finesse and make you an expert, to set you apart from other practices,” said Dr. Saedi, who coauthored a chapter in the book, “The Business of Dermatology” (New York: Thieme Medical Publishers, 2020). “I always recommend treating your staff and members of your family, to understand how you can tweak treatments to get the most out of them. Once you treat your staff, they are walking advertisements for what you do. They can also counsel patients, walking them through the healing process after a procedure, so they can know what to expect.”
Appropriate planning and preparation can help avoid acquiring the wrong device, she continued. This includes patient demand, scheduling availability, office space, overhead costs, and the level of staff training. She recommends buying one device at a time and clearing profitability from that device before purchasing another, “because it can be a burden on your practice to have multiple devices all at once,” she said. “You also have to think about the hidden costs – the maintenance and the service contracts. That can exceed $10,000 per year, so consider that when you’re looking to purchase a new device.”
Most people buy laser-, light-, and energy-based devices, but renting for a stretch can help you test the waters without a significant long-term investment. “It might not be the newest laser, but it can help you gauge how much of demand you have for that service to see if you have the patient base to make that larger step of purchasing the device,” she said. “If you buy a new device, make sure that it’s not a counterfeit and that you still have a company service contract. There are many third-party companies selling pre-owned laser aesthetics. Make sure you’re getting the authentic device and that there is some kind of a service contract with the actual manufacturer so they can help fix it when things break down.”
When Dr. Saedi counsels residents about purchasing devices, she typically recommends these five categories in order of preference: vascular, pigment, hair, resurfacing, and body contouring/skin tightening. “If you can cover vascular, pigment, and some kind of textural improvement, you can treat about 90% of aesthetic patients who come through your door,” she said. “Sure, there are some who may want skin tightening that you may not be able to offer with laser resurfacing, but you’re going to be able capture a high patient population by offering these services,” she added. That is why a lot of people end up getting a platform with attachable handpieces, “where you can have one system that is able to offer many different services right off the bat.”
She advised factoring in the amount of time it takes for a procedure and how much time it will take up in a certain room. “That will affect your revenue as well. Are you going to delegate this, or is this something you will do on your own? Take that into account.”
Above all, don’t rush your device purchase. “Some laser company sales representatives may pressure you at the end of a quarter by saying, ‘This is the best deal I’m going to offer you. You’re never going to get a deal like this ever again,’ ” she said. “I advise people to do multiple demos so you’re not just doing a demo for a day and seeing one or two patients. Treat the same patients again a month later. Do multiple demos so that you can feel comfortable. Talk to dermatologists who have the device, who have real experience with it, so you can have the most amount of information moving forward.”
Dr. Saedi reported that she has received equipment from Alma, Aerolase, Cartessa, and Cynosure. She is a consultant to and/or an advisory board member for those companies, as well as for Alastin.
FROM ODAC 2021
Biden administration nixes buprenorphine waiver, docs disappointed
The Biden administration has halted a Trump administration initiative that would have allowed more physicians to prescribe buprenorphine for opioid use disorder (OUD).
Under the Trump administration’s plan, many doctors would be exempt from taking a day’s training before they could prescribe buprenorphine for OUD.
On Jan. 25, 2021, citing anonymous sources, the Washington Post reported that this action by the Biden administration was likely. At the time, there were concerns about whether the Department of Health & Human Services had the legal authority to make this policy change, the Post reported. The Substance Abuse and Mental Health Services Administration subsequently announced the derailment of the buprenorphine proposal on its website.
In SAMHSA’s view, the proposal was made “prematurely.” The SAMHSA statement did not detail the reasons for abandoning the Jan. 14 proposal. It had been scheduled to take effect upon publication in the Federal Register.
Instead of finalizing it in this way, the HHS said it would work with other federal agencies to “increase access to buprenorphine, reduce overdose rates and save lives.”
The HHS decision to scupper the proposal disappointed many physician groups. In a letter dated Jan. 27, several physician groups called on the Biden administration to proceed with the Trump proposal.
Under current federal law, physicians who wish to prescribe buprenorphine outside of opioid treatment programs must take an 8-hour course and receive a waiver from the Drug Enforcement Administration, the letter noted. It was signed by the American College of Emergency Physicians, the American Medical Association, and other organizations.
Treatment barrier
After taking the training course, it can take 60-90 days for physicians to receive the waiver. The license application can then be submitted. Physician groups argue that this so-called X-waiver requirement creates a barrier to providing medication-assisted treatment.
“Due to the stigma, some clinicians are not willing to pursue this DEA license or even engage in treatment of patients with [OUD],” the letter said.
The Trump administration’s proposal would have limited most physicians to treating no more than 30 patients with buprenorphine for OUD at any one time. This cap would not have applied to hospital-based physicians, such as those practicing emergency medicine, the HHS noted in a statement. The policy would have applied to only physicians who already have registered with the DEA.
Patrice A. Harris, MD, the immediate past president of the AMA and chair of the organization’s Opioid Task Force, was among the many physicians who supported the Trump administration proposal.
“It is estimated that more than 2 million Americans need treatment for opioid use disorder, but only a small percentage actually receive treatment,” Dr. Harris said in statement. Dr. Harris also noted that overdose deaths have reportedly accelerated during the COVID-19 pandemic.
Centers for Disease Control and Prevention data show there were more than 83,000 drug overdose deaths in the United States in the 12 months ending in June 2020. That is the highest number of overdose deaths ever recorded in a 12-month period and is an increase of more than 21%, compared with the previous year.
A ‘disappointment’
On Jan. 28, Dr. Harris said the decision to drop the plan was a disappointment.
“We encourage the current administration to quickly develop a path forward that removes the burdensome waiver requirement, thus allowing more physicians to prescribe this lifesaving medication,” she said in a statement sent to this news organization.
In a Jan. 26 statement, the American Society of Addiction Medicine urged Congress to eliminate the X-waiver and called for more education and training in the treatment of patients who struggle with opioids.
In the 116th session of Congress, which ended on Jan. 3, there was bipartisan support for proposed legislation to ease requirements for buprenorphine prescribing. A House bill had more than 90 Democratic and 21 Republican sponsors. A companion Senate bill had three Democratic and three Republican Sponsors, including Sen. Maggie Hassan (D-N.H.). On Jan. 25, Dr. Hassan tweeted that she would be seeking an explanation from the Biden administration if it halted the plan to ease the waiver restriction.
“Medication-assisted treatment can save lives, and the buprenorphine waiver requirement should be eliminated so that physicians can more easily prescribe it to those who need it,” she said.
Many clinicians and policy experts turned to Twitter to urge an easing of buprenorphine prescribing, using the hashtag “Xthexwaiver.”
Among them was the official who put forward the Jan. 14 proposal, Brett Giroir, MD. He served as assistant secretary for health during the Trump administration.
Objections
In its Jan. 25 article, the Washington Post referred to an article in Alcoholism and Drug Abuse Weekly in which a top federal official in the Trump administration objected to Dr. Giroir’s plan.
Elinore F. McCance-Katz, MD, PhD, who served as the assistant secretary of HHS for SAMHSA, had earlier proposed raising the cap for addiction experts. Alcoholism and Drug Abuse Weekly quotes Dr. McCance-Katz as saying the Trump buprenorphine proposal was “unfair to the incoming administration.”
“The Biden administration has so much work to do to get their programs and policies into place, and to do something like this at the 11th hour that could get doctors into trouble – it’s heinous,” she said in the article.
Dr. McCance-Katz had resigned before the Trump administration proposal was unveiled. On Jan. 7, she issued a public notice announcing she would resign, citing concerns about the previous day’s attack on the U.S. Capitol.
“It had been my plan to stay until the change in administration occurred, but my plans abruptly changed last evening when, on my way back from visiting an excellent residential treatment program in New York, I saw the violent takeover of the Capitol building,” she said.
On Twitter, Roland Flores, MD, an anesthesiologist and pain specialist, urged his colleagues to consider the need for more education among clinicians who treat OUD. He jousted a bit with those favoring a swift drive to “XtheXwaiver” and questioned their arguments about the burden of the current rules.
“I think ‘all this red tape’ is a little bit of an exaggeration – it’s an 8-hour online course, and an application,” Dr. Flores tweeted in one exchange. “But #XtheXwaiver is fine – it’s probably rooted in stigma. It’s unlikely to make much difference tho. The waiver wasn’t the thing keeping docs from prescribing.”
A version of this article first appeared on Medscape.com.
The Biden administration has halted a Trump administration initiative that would have allowed more physicians to prescribe buprenorphine for opioid use disorder (OUD).
Under the Trump administration’s plan, many doctors would be exempt from taking a day’s training before they could prescribe buprenorphine for OUD.
On Jan. 25, 2021, citing anonymous sources, the Washington Post reported that this action by the Biden administration was likely. At the time, there were concerns about whether the Department of Health & Human Services had the legal authority to make this policy change, the Post reported. The Substance Abuse and Mental Health Services Administration subsequently announced the derailment of the buprenorphine proposal on its website.
In SAMHSA’s view, the proposal was made “prematurely.” The SAMHSA statement did not detail the reasons for abandoning the Jan. 14 proposal. It had been scheduled to take effect upon publication in the Federal Register.
Instead of finalizing it in this way, the HHS said it would work with other federal agencies to “increase access to buprenorphine, reduce overdose rates and save lives.”
The HHS decision to scupper the proposal disappointed many physician groups. In a letter dated Jan. 27, several physician groups called on the Biden administration to proceed with the Trump proposal.
Under current federal law, physicians who wish to prescribe buprenorphine outside of opioid treatment programs must take an 8-hour course and receive a waiver from the Drug Enforcement Administration, the letter noted. It was signed by the American College of Emergency Physicians, the American Medical Association, and other organizations.
Treatment barrier
After taking the training course, it can take 60-90 days for physicians to receive the waiver. The license application can then be submitted. Physician groups argue that this so-called X-waiver requirement creates a barrier to providing medication-assisted treatment.
“Due to the stigma, some clinicians are not willing to pursue this DEA license or even engage in treatment of patients with [OUD],” the letter said.
The Trump administration’s proposal would have limited most physicians to treating no more than 30 patients with buprenorphine for OUD at any one time. This cap would not have applied to hospital-based physicians, such as those practicing emergency medicine, the HHS noted in a statement. The policy would have applied to only physicians who already have registered with the DEA.
Patrice A. Harris, MD, the immediate past president of the AMA and chair of the organization’s Opioid Task Force, was among the many physicians who supported the Trump administration proposal.
“It is estimated that more than 2 million Americans need treatment for opioid use disorder, but only a small percentage actually receive treatment,” Dr. Harris said in statement. Dr. Harris also noted that overdose deaths have reportedly accelerated during the COVID-19 pandemic.
Centers for Disease Control and Prevention data show there were more than 83,000 drug overdose deaths in the United States in the 12 months ending in June 2020. That is the highest number of overdose deaths ever recorded in a 12-month period and is an increase of more than 21%, compared with the previous year.
A ‘disappointment’
On Jan. 28, Dr. Harris said the decision to drop the plan was a disappointment.
“We encourage the current administration to quickly develop a path forward that removes the burdensome waiver requirement, thus allowing more physicians to prescribe this lifesaving medication,” she said in a statement sent to this news organization.
In a Jan. 26 statement, the American Society of Addiction Medicine urged Congress to eliminate the X-waiver and called for more education and training in the treatment of patients who struggle with opioids.
In the 116th session of Congress, which ended on Jan. 3, there was bipartisan support for proposed legislation to ease requirements for buprenorphine prescribing. A House bill had more than 90 Democratic and 21 Republican sponsors. A companion Senate bill had three Democratic and three Republican Sponsors, including Sen. Maggie Hassan (D-N.H.). On Jan. 25, Dr. Hassan tweeted that she would be seeking an explanation from the Biden administration if it halted the plan to ease the waiver restriction.
“Medication-assisted treatment can save lives, and the buprenorphine waiver requirement should be eliminated so that physicians can more easily prescribe it to those who need it,” she said.
Many clinicians and policy experts turned to Twitter to urge an easing of buprenorphine prescribing, using the hashtag “Xthexwaiver.”
Among them was the official who put forward the Jan. 14 proposal, Brett Giroir, MD. He served as assistant secretary for health during the Trump administration.
Objections
In its Jan. 25 article, the Washington Post referred to an article in Alcoholism and Drug Abuse Weekly in which a top federal official in the Trump administration objected to Dr. Giroir’s plan.
Elinore F. McCance-Katz, MD, PhD, who served as the assistant secretary of HHS for SAMHSA, had earlier proposed raising the cap for addiction experts. Alcoholism and Drug Abuse Weekly quotes Dr. McCance-Katz as saying the Trump buprenorphine proposal was “unfair to the incoming administration.”
“The Biden administration has so much work to do to get their programs and policies into place, and to do something like this at the 11th hour that could get doctors into trouble – it’s heinous,” she said in the article.
Dr. McCance-Katz had resigned before the Trump administration proposal was unveiled. On Jan. 7, she issued a public notice announcing she would resign, citing concerns about the previous day’s attack on the U.S. Capitol.
“It had been my plan to stay until the change in administration occurred, but my plans abruptly changed last evening when, on my way back from visiting an excellent residential treatment program in New York, I saw the violent takeover of the Capitol building,” she said.
On Twitter, Roland Flores, MD, an anesthesiologist and pain specialist, urged his colleagues to consider the need for more education among clinicians who treat OUD. He jousted a bit with those favoring a swift drive to “XtheXwaiver” and questioned their arguments about the burden of the current rules.
“I think ‘all this red tape’ is a little bit of an exaggeration – it’s an 8-hour online course, and an application,” Dr. Flores tweeted in one exchange. “But #XtheXwaiver is fine – it’s probably rooted in stigma. It’s unlikely to make much difference tho. The waiver wasn’t the thing keeping docs from prescribing.”
A version of this article first appeared on Medscape.com.
The Biden administration has halted a Trump administration initiative that would have allowed more physicians to prescribe buprenorphine for opioid use disorder (OUD).
Under the Trump administration’s plan, many doctors would be exempt from taking a day’s training before they could prescribe buprenorphine for OUD.
On Jan. 25, 2021, citing anonymous sources, the Washington Post reported that this action by the Biden administration was likely. At the time, there were concerns about whether the Department of Health & Human Services had the legal authority to make this policy change, the Post reported. The Substance Abuse and Mental Health Services Administration subsequently announced the derailment of the buprenorphine proposal on its website.
In SAMHSA’s view, the proposal was made “prematurely.” The SAMHSA statement did not detail the reasons for abandoning the Jan. 14 proposal. It had been scheduled to take effect upon publication in the Federal Register.
Instead of finalizing it in this way, the HHS said it would work with other federal agencies to “increase access to buprenorphine, reduce overdose rates and save lives.”
The HHS decision to scupper the proposal disappointed many physician groups. In a letter dated Jan. 27, several physician groups called on the Biden administration to proceed with the Trump proposal.
Under current federal law, physicians who wish to prescribe buprenorphine outside of opioid treatment programs must take an 8-hour course and receive a waiver from the Drug Enforcement Administration, the letter noted. It was signed by the American College of Emergency Physicians, the American Medical Association, and other organizations.
Treatment barrier
After taking the training course, it can take 60-90 days for physicians to receive the waiver. The license application can then be submitted. Physician groups argue that this so-called X-waiver requirement creates a barrier to providing medication-assisted treatment.
“Due to the stigma, some clinicians are not willing to pursue this DEA license or even engage in treatment of patients with [OUD],” the letter said.
The Trump administration’s proposal would have limited most physicians to treating no more than 30 patients with buprenorphine for OUD at any one time. This cap would not have applied to hospital-based physicians, such as those practicing emergency medicine, the HHS noted in a statement. The policy would have applied to only physicians who already have registered with the DEA.
Patrice A. Harris, MD, the immediate past president of the AMA and chair of the organization’s Opioid Task Force, was among the many physicians who supported the Trump administration proposal.
“It is estimated that more than 2 million Americans need treatment for opioid use disorder, but only a small percentage actually receive treatment,” Dr. Harris said in statement. Dr. Harris also noted that overdose deaths have reportedly accelerated during the COVID-19 pandemic.
Centers for Disease Control and Prevention data show there were more than 83,000 drug overdose deaths in the United States in the 12 months ending in June 2020. That is the highest number of overdose deaths ever recorded in a 12-month period and is an increase of more than 21%, compared with the previous year.
A ‘disappointment’
On Jan. 28, Dr. Harris said the decision to drop the plan was a disappointment.
“We encourage the current administration to quickly develop a path forward that removes the burdensome waiver requirement, thus allowing more physicians to prescribe this lifesaving medication,” she said in a statement sent to this news organization.
In a Jan. 26 statement, the American Society of Addiction Medicine urged Congress to eliminate the X-waiver and called for more education and training in the treatment of patients who struggle with opioids.
In the 116th session of Congress, which ended on Jan. 3, there was bipartisan support for proposed legislation to ease requirements for buprenorphine prescribing. A House bill had more than 90 Democratic and 21 Republican sponsors. A companion Senate bill had three Democratic and three Republican Sponsors, including Sen. Maggie Hassan (D-N.H.). On Jan. 25, Dr. Hassan tweeted that she would be seeking an explanation from the Biden administration if it halted the plan to ease the waiver restriction.
“Medication-assisted treatment can save lives, and the buprenorphine waiver requirement should be eliminated so that physicians can more easily prescribe it to those who need it,” she said.
Many clinicians and policy experts turned to Twitter to urge an easing of buprenorphine prescribing, using the hashtag “Xthexwaiver.”
Among them was the official who put forward the Jan. 14 proposal, Brett Giroir, MD. He served as assistant secretary for health during the Trump administration.
Objections
In its Jan. 25 article, the Washington Post referred to an article in Alcoholism and Drug Abuse Weekly in which a top federal official in the Trump administration objected to Dr. Giroir’s plan.
Elinore F. McCance-Katz, MD, PhD, who served as the assistant secretary of HHS for SAMHSA, had earlier proposed raising the cap for addiction experts. Alcoholism and Drug Abuse Weekly quotes Dr. McCance-Katz as saying the Trump buprenorphine proposal was “unfair to the incoming administration.”
“The Biden administration has so much work to do to get their programs and policies into place, and to do something like this at the 11th hour that could get doctors into trouble – it’s heinous,” she said in the article.
Dr. McCance-Katz had resigned before the Trump administration proposal was unveiled. On Jan. 7, she issued a public notice announcing she would resign, citing concerns about the previous day’s attack on the U.S. Capitol.
“It had been my plan to stay until the change in administration occurred, but my plans abruptly changed last evening when, on my way back from visiting an excellent residential treatment program in New York, I saw the violent takeover of the Capitol building,” she said.
On Twitter, Roland Flores, MD, an anesthesiologist and pain specialist, urged his colleagues to consider the need for more education among clinicians who treat OUD. He jousted a bit with those favoring a swift drive to “XtheXwaiver” and questioned their arguments about the burden of the current rules.
“I think ‘all this red tape’ is a little bit of an exaggeration – it’s an 8-hour online course, and an application,” Dr. Flores tweeted in one exchange. “But #XtheXwaiver is fine – it’s probably rooted in stigma. It’s unlikely to make much difference tho. The waiver wasn’t the thing keeping docs from prescribing.”
A version of this article first appeared on Medscape.com.














