User login
COVID cuts internists’ happiness in life outside work
Before the pandemic, a large majority of internists reported that they were generally happy with life outside of work, although by specialty, they were near the bottom in happiness.
But this year’s Medscape Internist Lifestyle, Happiness & Burnout Report 2021 shows a sharp drop, with just 55% of respondents saying they are somewhat or very happy in life outside work, compared with 78% last year.
Internists were not alone among the more than 12,000 physicians who responded to the survey. The contrast from last year’s report was clear for physicians in general and reflects COVID-19’s substantial toll on clinicians.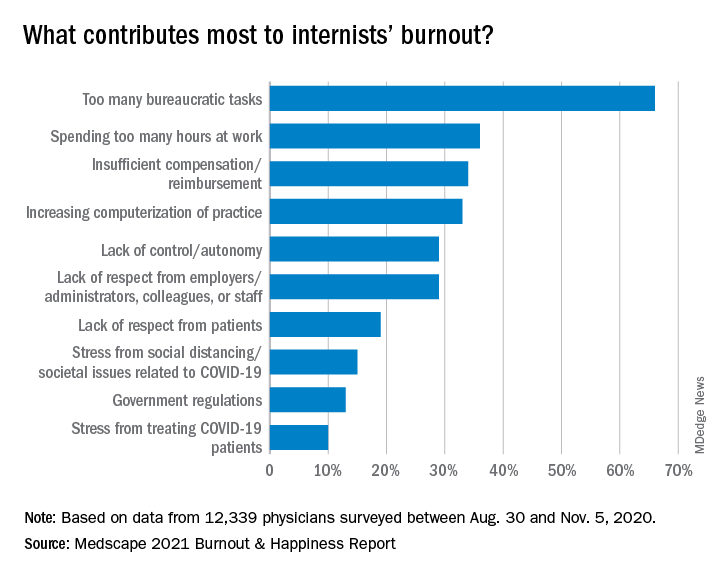
Just 58% of physicians overall reported happy lives outside work, down from 82% last year.
Perhaps not surprising, given the particular demands on certain specialties, physicians in infectious disease were the least happy, at 45%, followed by pulmonologists (47%) and rheumatologists and intensivists, at 49%.
The highest happiness level was reported by those in diabetes and endocrinology, at 73% this year, but that proportion was also substantially lower than the 89% from last year.
Burnout has ‘strong impact on lives’
The percentage of internists who reported burnout or depression, however, has stayed fairly consistent.
More than half (52%) said that burnout had a strong or severe impact on their lives, and nearly 1 in 10 said it was severe enough that they are considering leaving medicine.
One percent of the internists who responded to the survey said they had attempted suicide, and 12% said they had thoughts of suicide but had not attempted it.
Most of those reporting burnout (82%) said it started before the COVID-19 pandemic, but 18% said it began with the pandemic.
Notably, though, physicians ranked problems related to stress from COVID-19 near the bottom among burnout drivers. The top factor, by far, again, was “too many bureaucratic tasks.”
A large majority (78%) of internists work online for up to 10 hours a week, a number that could grow as telemedicine grows.
Exercise is top coping method
Responses gave a peek into how physicians are coping with burnout. Among internists, 49% put exercise at the top. Isolating themselves from others was the next most popular choice, at 45%. Eating junk food and drinking alcohol were further down the list, at 34% and 24%, respectively.
Few internists said they drink alcohol daily, a finding consistent with past years. In fact, 29% said they don’t drink at all, and 26% said they have fewer than one alcoholic drink per week. Only 7% said they had seven or more drinks per week.
The National Institute on Alcohol Abuse and Alcoholism advises that men not have more than 14 alcoholic drinks per week and that women not have more than 7.
Work-life balance topped list of concerns
By far, internists said work-life balance was their top workplace concern. Nearly half (48%) chose that answer, more than twice the percentage who said compensation was the biggest concern (21%).
Asked whether they would take a salary cut for more work-life balance, a similar proportion (46%) said yes.
Forty-three percent of internists manage to take 3-4 weeks of vacation, and 10% take at least 5 weeks, similar to reported vacation time in last year’s survey.
The vast majority are in committed relationships, with 79% reporting that they are married, and 5% reporting that they are living with a partner. Of those who are married, 48% described the marriage as very good; 32%, good; 16%, fair; 2%, poor; and 1%, very poor; 1% preferred not to answer.
One in five internists said their spouse was a physician, and 24% said their spouse worked in the health care field but not as a physician.
Pandemic has increased burnout
Douglas S. Paauw, MD, and Eileen Barrett, MD, two members of the Internal Medicine News editorial advisory board, said they were not surprised by the survey findings.
“There is more burnout since the pandemic,” said Dr. Paauw, professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and third-year medical student clerkship director at the University of Washington. “People may be working more hours, higher stress, but also, some may be working less hours, are socially isolated, taking on a new role of helping their kids in virtual education, andn living in cramped quarters with family that they may not be accustomed to spending so much time with.”
“Also, most physicians love travel, to detress, get back in balance, and that has by and large been taken away by the pandemic,” Dr. Paauw noted. “Unfortunately, bureaucracy did not go away during the pandemic!
Dr. Barrett, an internal medicine hospitalist, said, “It is most concerning to me today that 12% have had thoughts of suicide, and yet 39% are too busy to seek care for depression or burnout, and 17% aren’t seeking due to fear it will be disclosed,”
“Credentialing, medical license applications, and malpractice insurance applications can and must be changed posthaste to support physicians and stop stigmatizing mental health diagnoses and mental health care,” she said. “Removing application questions about physician mental health will be consistent with recommendations from the Federation of State Medical Boards, medical professional societies, and the Americans with Disabilities Act, and is something actionable and achievable for every organization to do in 2021.” “From a public policy perspective, I am deeply concerned about the physician workforce and how patients will be able to receive care from exhausted, burned out physicians who may be reducing their clinical hours to restore their personal happiness – understandably so,” added Dr. Barrett, who is associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
She pointed out that there are mental health resources available for physicians that don’t go through their employers or insurance such as www.emotionalppe.org/.
A version of this article first appeared on Medscape.com.
Katie Lennon contributed to this report.
Before the pandemic, a large majority of internists reported that they were generally happy with life outside of work, although by specialty, they were near the bottom in happiness.
But this year’s Medscape Internist Lifestyle, Happiness & Burnout Report 2021 shows a sharp drop, with just 55% of respondents saying they are somewhat or very happy in life outside work, compared with 78% last year.
Internists were not alone among the more than 12,000 physicians who responded to the survey. The contrast from last year’s report was clear for physicians in general and reflects COVID-19’s substantial toll on clinicians.
Just 58% of physicians overall reported happy lives outside work, down from 82% last year.
Perhaps not surprising, given the particular demands on certain specialties, physicians in infectious disease were the least happy, at 45%, followed by pulmonologists (47%) and rheumatologists and intensivists, at 49%.
The highest happiness level was reported by those in diabetes and endocrinology, at 73% this year, but that proportion was also substantially lower than the 89% from last year.
Burnout has ‘strong impact on lives’
The percentage of internists who reported burnout or depression, however, has stayed fairly consistent.
More than half (52%) said that burnout had a strong or severe impact on their lives, and nearly 1 in 10 said it was severe enough that they are considering leaving medicine.
One percent of the internists who responded to the survey said they had attempted suicide, and 12% said they had thoughts of suicide but had not attempted it.
Most of those reporting burnout (82%) said it started before the COVID-19 pandemic, but 18% said it began with the pandemic.
Notably, though, physicians ranked problems related to stress from COVID-19 near the bottom among burnout drivers. The top factor, by far, again, was “too many bureaucratic tasks.”
A large majority (78%) of internists work online for up to 10 hours a week, a number that could grow as telemedicine grows.
Exercise is top coping method
Responses gave a peek into how physicians are coping with burnout. Among internists, 49% put exercise at the top. Isolating themselves from others was the next most popular choice, at 45%. Eating junk food and drinking alcohol were further down the list, at 34% and 24%, respectively.
Few internists said they drink alcohol daily, a finding consistent with past years. In fact, 29% said they don’t drink at all, and 26% said they have fewer than one alcoholic drink per week. Only 7% said they had seven or more drinks per week.
The National Institute on Alcohol Abuse and Alcoholism advises that men not have more than 14 alcoholic drinks per week and that women not have more than 7.
Work-life balance topped list of concerns
By far, internists said work-life balance was their top workplace concern. Nearly half (48%) chose that answer, more than twice the percentage who said compensation was the biggest concern (21%).
Asked whether they would take a salary cut for more work-life balance, a similar proportion (46%) said yes.
Forty-three percent of internists manage to take 3-4 weeks of vacation, and 10% take at least 5 weeks, similar to reported vacation time in last year’s survey.
The vast majority are in committed relationships, with 79% reporting that they are married, and 5% reporting that they are living with a partner. Of those who are married, 48% described the marriage as very good; 32%, good; 16%, fair; 2%, poor; and 1%, very poor; 1% preferred not to answer.
One in five internists said their spouse was a physician, and 24% said their spouse worked in the health care field but not as a physician.
Pandemic has increased burnout
Douglas S. Paauw, MD, and Eileen Barrett, MD, two members of the Internal Medicine News editorial advisory board, said they were not surprised by the survey findings.
“There is more burnout since the pandemic,” said Dr. Paauw, professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and third-year medical student clerkship director at the University of Washington. “People may be working more hours, higher stress, but also, some may be working less hours, are socially isolated, taking on a new role of helping their kids in virtual education, andn living in cramped quarters with family that they may not be accustomed to spending so much time with.”
“Also, most physicians love travel, to detress, get back in balance, and that has by and large been taken away by the pandemic,” Dr. Paauw noted. “Unfortunately, bureaucracy did not go away during the pandemic!
Dr. Barrett, an internal medicine hospitalist, said, “It is most concerning to me today that 12% have had thoughts of suicide, and yet 39% are too busy to seek care for depression or burnout, and 17% aren’t seeking due to fear it will be disclosed,”
“Credentialing, medical license applications, and malpractice insurance applications can and must be changed posthaste to support physicians and stop stigmatizing mental health diagnoses and mental health care,” she said. “Removing application questions about physician mental health will be consistent with recommendations from the Federation of State Medical Boards, medical professional societies, and the Americans with Disabilities Act, and is something actionable and achievable for every organization to do in 2021.” “From a public policy perspective, I am deeply concerned about the physician workforce and how patients will be able to receive care from exhausted, burned out physicians who may be reducing their clinical hours to restore their personal happiness – understandably so,” added Dr. Barrett, who is associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
She pointed out that there are mental health resources available for physicians that don’t go through their employers or insurance such as www.emotionalppe.org/.
A version of this article first appeared on Medscape.com.
Katie Lennon contributed to this report.
Before the pandemic, a large majority of internists reported that they were generally happy with life outside of work, although by specialty, they were near the bottom in happiness.
But this year’s Medscape Internist Lifestyle, Happiness & Burnout Report 2021 shows a sharp drop, with just 55% of respondents saying they are somewhat or very happy in life outside work, compared with 78% last year.
Internists were not alone among the more than 12,000 physicians who responded to the survey. The contrast from last year’s report was clear for physicians in general and reflects COVID-19’s substantial toll on clinicians.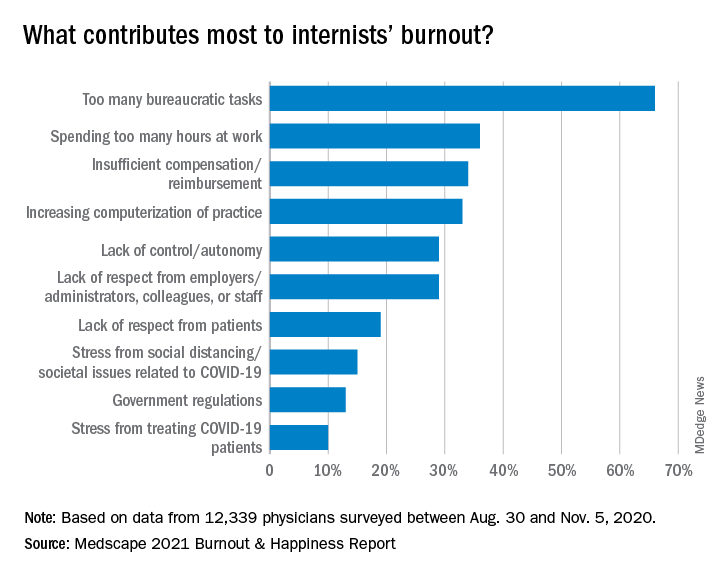
Just 58% of physicians overall reported happy lives outside work, down from 82% last year.
Perhaps not surprising, given the particular demands on certain specialties, physicians in infectious disease were the least happy, at 45%, followed by pulmonologists (47%) and rheumatologists and intensivists, at 49%.
The highest happiness level was reported by those in diabetes and endocrinology, at 73% this year, but that proportion was also substantially lower than the 89% from last year.
Burnout has ‘strong impact on lives’
The percentage of internists who reported burnout or depression, however, has stayed fairly consistent.
More than half (52%) said that burnout had a strong or severe impact on their lives, and nearly 1 in 10 said it was severe enough that they are considering leaving medicine.
One percent of the internists who responded to the survey said they had attempted suicide, and 12% said they had thoughts of suicide but had not attempted it.
Most of those reporting burnout (82%) said it started before the COVID-19 pandemic, but 18% said it began with the pandemic.
Notably, though, physicians ranked problems related to stress from COVID-19 near the bottom among burnout drivers. The top factor, by far, again, was “too many bureaucratic tasks.”
A large majority (78%) of internists work online for up to 10 hours a week, a number that could grow as telemedicine grows.
Exercise is top coping method
Responses gave a peek into how physicians are coping with burnout. Among internists, 49% put exercise at the top. Isolating themselves from others was the next most popular choice, at 45%. Eating junk food and drinking alcohol were further down the list, at 34% and 24%, respectively.
Few internists said they drink alcohol daily, a finding consistent with past years. In fact, 29% said they don’t drink at all, and 26% said they have fewer than one alcoholic drink per week. Only 7% said they had seven or more drinks per week.
The National Institute on Alcohol Abuse and Alcoholism advises that men not have more than 14 alcoholic drinks per week and that women not have more than 7.
Work-life balance topped list of concerns
By far, internists said work-life balance was their top workplace concern. Nearly half (48%) chose that answer, more than twice the percentage who said compensation was the biggest concern (21%).
Asked whether they would take a salary cut for more work-life balance, a similar proportion (46%) said yes.
Forty-three percent of internists manage to take 3-4 weeks of vacation, and 10% take at least 5 weeks, similar to reported vacation time in last year’s survey.
The vast majority are in committed relationships, with 79% reporting that they are married, and 5% reporting that they are living with a partner. Of those who are married, 48% described the marriage as very good; 32%, good; 16%, fair; 2%, poor; and 1%, very poor; 1% preferred not to answer.
One in five internists said their spouse was a physician, and 24% said their spouse worked in the health care field but not as a physician.
Pandemic has increased burnout
Douglas S. Paauw, MD, and Eileen Barrett, MD, two members of the Internal Medicine News editorial advisory board, said they were not surprised by the survey findings.
“There is more burnout since the pandemic,” said Dr. Paauw, professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and third-year medical student clerkship director at the University of Washington. “People may be working more hours, higher stress, but also, some may be working less hours, are socially isolated, taking on a new role of helping their kids in virtual education, andn living in cramped quarters with family that they may not be accustomed to spending so much time with.”
“Also, most physicians love travel, to detress, get back in balance, and that has by and large been taken away by the pandemic,” Dr. Paauw noted. “Unfortunately, bureaucracy did not go away during the pandemic!
Dr. Barrett, an internal medicine hospitalist, said, “It is most concerning to me today that 12% have had thoughts of suicide, and yet 39% are too busy to seek care for depression or burnout, and 17% aren’t seeking due to fear it will be disclosed,”
“Credentialing, medical license applications, and malpractice insurance applications can and must be changed posthaste to support physicians and stop stigmatizing mental health diagnoses and mental health care,” she said. “Removing application questions about physician mental health will be consistent with recommendations from the Federation of State Medical Boards, medical professional societies, and the Americans with Disabilities Act, and is something actionable and achievable for every organization to do in 2021.” “From a public policy perspective, I am deeply concerned about the physician workforce and how patients will be able to receive care from exhausted, burned out physicians who may be reducing their clinical hours to restore their personal happiness – understandably so,” added Dr. Barrett, who is associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
She pointed out that there are mental health resources available for physicians that don’t go through their employers or insurance such as www.emotionalppe.org/.
A version of this article first appeared on Medscape.com.
Katie Lennon contributed to this report.
One in 10 family docs with burnout consider quitting medicine
and 1 in 10 said it was serious enough to make them consider leaving medicine.
Yet, responses to the Medscape Family Medicine Physician Lifestyle, Happiness & Burnout Report 2021 also indicate that family physicians are in the middle of the pack again this year in rankings by specialty of physician happiness outside work. Overall, more than 12,000 physicians from more than 29 specialties responded to this year’s survey, conducted between Aug. 30 and Nov. 5, 2020.
Happiness levels sink for physicians
In light of the COVID-19 pandemic, happiness levels took a sharp drop among physicians across the board. Last year, for instance, the happiness level was highest for physicians practicing in diabetes and endocrinology, at 89%. They remain the happiest this year, but the proportion saying they were happy dropped to 73%. Infectious disease physicians were the least happy outside work both last year and this year, with the proportion reporting they were happy dropping from 69% to 45%.
For family physicians, happiness levels outside work plunged from 79% last year to 57% this year.
Burnout and depression levels, however, remained steady. The portion saying they were either burned out or burned out and depressed was up only 1 percentage point, rising to 47%.
Fifteen percent of family physicians have had thoughts of suicide, and 1% said they had attempted it, according to the survey responses.
The most common strategy for coping with burnout, reported by 48% of family physicians, is talking with family members and close friends, followed closely by exercise, reported by 46%.
Sixty-eight percent of family physicians say they exercise at least twice a week, and 12% exercise every day.
However, not all coping strategies were as positive: Forty-five percent said they cope by isolating themselves from others; 40% turned to junk food; and 23%-24% said they drank alcohol or were binge-eating to cope. Respondents could choose more than one answer.
Among family physicians, 75% expressed anxiety about their futures, given the pandemic, which is similar to the proportion among physicians overall (77%) who had the same worries.
Work-life balance biggest worry
The survey also asked what workplace issues concern family physicians the most. The biggest concern, by far, was work-life balance, chosen by 51%. Next highest was compensation, at 19%, followed by combining parenthood and work (9%) and relationships with colleagues/staff (6%).
More than half (52%) of family doctors said they would take a cut in pay to have better work-life balance.
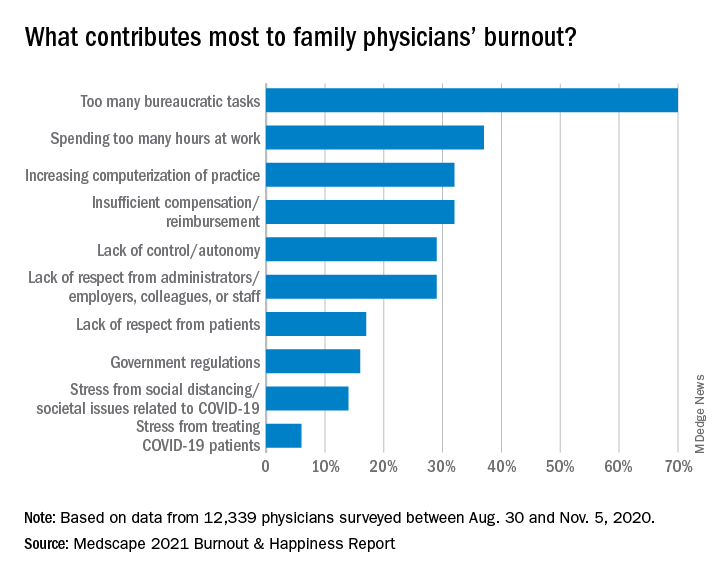
A little more than a third (36%) of family physicians – about the same percentage as physicians overall – said they always or most of the time spend enough time on their own health and wellness. One in five said they rarely or never do.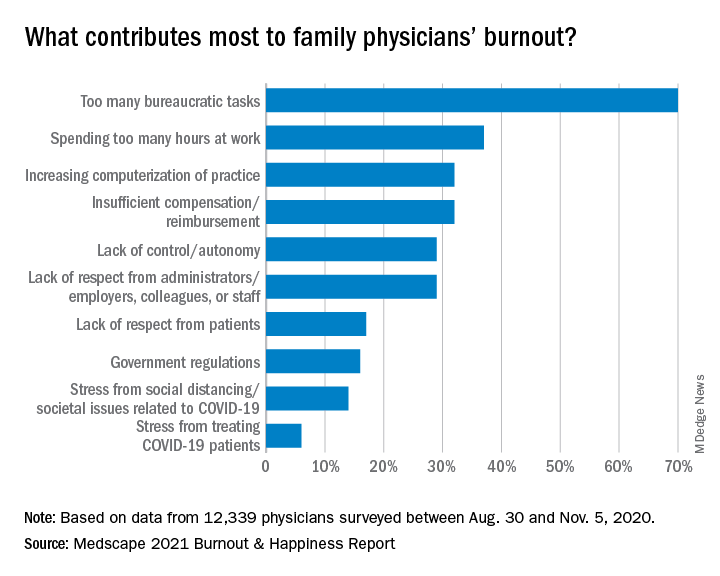
The amount of work required beyond the bedside continues to frustrate family physicians.
Again this year, the top cause of burnout, chosen by 70% of family physicians, was “too many bureaucratic tasks.” That was followed by “spending too many hours at work” (37%) and “increasing computerization of practice” (32%).
A large majority (82%) of family doctors report that they work online up to 10 hours a week, a number that could increase with the rise of telemedicine; 64% are personally online up to 10 hours a week. But even with combined personal and professional Internet time, family doctors don’t come close to the average time spent online among all Internet users, which Hootsuite and We Are Social report is an average of 7 hours per day.
Most in committed, satisfying relationships
Most family medicine physicians are juggling committed relationships with work life. In this survey, 78% said they were married, and another 5% said they were living with a partner.
A little more than half of married family doctors described their marriages as very good (51%). The rest were good (32%); fair (13%); poor (2%); and very poor (2%). Some (15%) had spouses who were also physicians, and 25% said their spouses worked in the health care field but were not physicians.
Almost all family physicians were able to take some vacation time during this reporting period – 43% took 3-4 weeks; 35% took 1-2 weeks; 10% took less than 1 week; 9% took 5-6 weeks; and 4% took more than 6 weeks.
If they drove to vacation destinations, they were likely to be in their favorite make of vehicle, which for family physicians were Toyotas (22%), Hondas (14%) and Fords (11%), according to the survey responses. Physicians overall favored Toyotas, Hondas, and BMWs.
A version of this article first appeared on Medscape.com.
and 1 in 10 said it was serious enough to make them consider leaving medicine.
Yet, responses to the Medscape Family Medicine Physician Lifestyle, Happiness & Burnout Report 2021 also indicate that family physicians are in the middle of the pack again this year in rankings by specialty of physician happiness outside work. Overall, more than 12,000 physicians from more than 29 specialties responded to this year’s survey, conducted between Aug. 30 and Nov. 5, 2020.
Happiness levels sink for physicians
In light of the COVID-19 pandemic, happiness levels took a sharp drop among physicians across the board. Last year, for instance, the happiness level was highest for physicians practicing in diabetes and endocrinology, at 89%. They remain the happiest this year, but the proportion saying they were happy dropped to 73%. Infectious disease physicians were the least happy outside work both last year and this year, with the proportion reporting they were happy dropping from 69% to 45%.
For family physicians, happiness levels outside work plunged from 79% last year to 57% this year.
Burnout and depression levels, however, remained steady. The portion saying they were either burned out or burned out and depressed was up only 1 percentage point, rising to 47%.
Fifteen percent of family physicians have had thoughts of suicide, and 1% said they had attempted it, according to the survey responses.
The most common strategy for coping with burnout, reported by 48% of family physicians, is talking with family members and close friends, followed closely by exercise, reported by 46%.
Sixty-eight percent of family physicians say they exercise at least twice a week, and 12% exercise every day.
However, not all coping strategies were as positive: Forty-five percent said they cope by isolating themselves from others; 40% turned to junk food; and 23%-24% said they drank alcohol or were binge-eating to cope. Respondents could choose more than one answer.
Among family physicians, 75% expressed anxiety about their futures, given the pandemic, which is similar to the proportion among physicians overall (77%) who had the same worries.
Work-life balance biggest worry
The survey also asked what workplace issues concern family physicians the most. The biggest concern, by far, was work-life balance, chosen by 51%. Next highest was compensation, at 19%, followed by combining parenthood and work (9%) and relationships with colleagues/staff (6%).
More than half (52%) of family doctors said they would take a cut in pay to have better work-life balance.
A little more than a third (36%) of family physicians – about the same percentage as physicians overall – said they always or most of the time spend enough time on their own health and wellness. One in five said they rarely or never do.
The amount of work required beyond the bedside continues to frustrate family physicians.
Again this year, the top cause of burnout, chosen by 70% of family physicians, was “too many bureaucratic tasks.” That was followed by “spending too many hours at work” (37%) and “increasing computerization of practice” (32%).
A large majority (82%) of family doctors report that they work online up to 10 hours a week, a number that could increase with the rise of telemedicine; 64% are personally online up to 10 hours a week. But even with combined personal and professional Internet time, family doctors don’t come close to the average time spent online among all Internet users, which Hootsuite and We Are Social report is an average of 7 hours per day.
Most in committed, satisfying relationships
Most family medicine physicians are juggling committed relationships with work life. In this survey, 78% said they were married, and another 5% said they were living with a partner.
A little more than half of married family doctors described their marriages as very good (51%). The rest were good (32%); fair (13%); poor (2%); and very poor (2%). Some (15%) had spouses who were also physicians, and 25% said their spouses worked in the health care field but were not physicians.
Almost all family physicians were able to take some vacation time during this reporting period – 43% took 3-4 weeks; 35% took 1-2 weeks; 10% took less than 1 week; 9% took 5-6 weeks; and 4% took more than 6 weeks.
If they drove to vacation destinations, they were likely to be in their favorite make of vehicle, which for family physicians were Toyotas (22%), Hondas (14%) and Fords (11%), according to the survey responses. Physicians overall favored Toyotas, Hondas, and BMWs.
A version of this article first appeared on Medscape.com.
and 1 in 10 said it was serious enough to make them consider leaving medicine.
Yet, responses to the Medscape Family Medicine Physician Lifestyle, Happiness & Burnout Report 2021 also indicate that family physicians are in the middle of the pack again this year in rankings by specialty of physician happiness outside work. Overall, more than 12,000 physicians from more than 29 specialties responded to this year’s survey, conducted between Aug. 30 and Nov. 5, 2020.
Happiness levels sink for physicians
In light of the COVID-19 pandemic, happiness levels took a sharp drop among physicians across the board. Last year, for instance, the happiness level was highest for physicians practicing in diabetes and endocrinology, at 89%. They remain the happiest this year, but the proportion saying they were happy dropped to 73%. Infectious disease physicians were the least happy outside work both last year and this year, with the proportion reporting they were happy dropping from 69% to 45%.
For family physicians, happiness levels outside work plunged from 79% last year to 57% this year.
Burnout and depression levels, however, remained steady. The portion saying they were either burned out or burned out and depressed was up only 1 percentage point, rising to 47%.
Fifteen percent of family physicians have had thoughts of suicide, and 1% said they had attempted it, according to the survey responses.
The most common strategy for coping with burnout, reported by 48% of family physicians, is talking with family members and close friends, followed closely by exercise, reported by 46%.
Sixty-eight percent of family physicians say they exercise at least twice a week, and 12% exercise every day.
However, not all coping strategies were as positive: Forty-five percent said they cope by isolating themselves from others; 40% turned to junk food; and 23%-24% said they drank alcohol or were binge-eating to cope. Respondents could choose more than one answer.
Among family physicians, 75% expressed anxiety about their futures, given the pandemic, which is similar to the proportion among physicians overall (77%) who had the same worries.
Work-life balance biggest worry
The survey also asked what workplace issues concern family physicians the most. The biggest concern, by far, was work-life balance, chosen by 51%. Next highest was compensation, at 19%, followed by combining parenthood and work (9%) and relationships with colleagues/staff (6%).
More than half (52%) of family doctors said they would take a cut in pay to have better work-life balance.
A little more than a third (36%) of family physicians – about the same percentage as physicians overall – said they always or most of the time spend enough time on their own health and wellness. One in five said they rarely or never do.
The amount of work required beyond the bedside continues to frustrate family physicians.
Again this year, the top cause of burnout, chosen by 70% of family physicians, was “too many bureaucratic tasks.” That was followed by “spending too many hours at work” (37%) and “increasing computerization of practice” (32%).
A large majority (82%) of family doctors report that they work online up to 10 hours a week, a number that could increase with the rise of telemedicine; 64% are personally online up to 10 hours a week. But even with combined personal and professional Internet time, family doctors don’t come close to the average time spent online among all Internet users, which Hootsuite and We Are Social report is an average of 7 hours per day.
Most in committed, satisfying relationships
Most family medicine physicians are juggling committed relationships with work life. In this survey, 78% said they were married, and another 5% said they were living with a partner.
A little more than half of married family doctors described their marriages as very good (51%). The rest were good (32%); fair (13%); poor (2%); and very poor (2%). Some (15%) had spouses who were also physicians, and 25% said their spouses worked in the health care field but were not physicians.
Almost all family physicians were able to take some vacation time during this reporting period – 43% took 3-4 weeks; 35% took 1-2 weeks; 10% took less than 1 week; 9% took 5-6 weeks; and 4% took more than 6 weeks.
If they drove to vacation destinations, they were likely to be in their favorite make of vehicle, which for family physicians were Toyotas (22%), Hondas (14%) and Fords (11%), according to the survey responses. Physicians overall favored Toyotas, Hondas, and BMWs.
A version of this article first appeared on Medscape.com.
Roots of physician burnout: It’s the work load
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
FROM THE JOINT COMMISSION JOURNAL ON QUALITY AND PATIENT SAFETY
Family medicine has grown; its composition has evolved
and the men and women who practice it are no exception.
The family medicine workforce of 2021 is not the workforce of 1971. Not even close. Although we would like to give a huge shout-out to anyone who can claim to be a member of both.
Today’s FP workforce is, first of all, much larger than it was in 1971, although we can’t actually prove it because the American Medical Association’s data for that year are “only available in books that are locked away at the empty AMA headquarters,” according to a member of the AMA media relations staff who is, like so many people these days, working at home because of the pandemic.
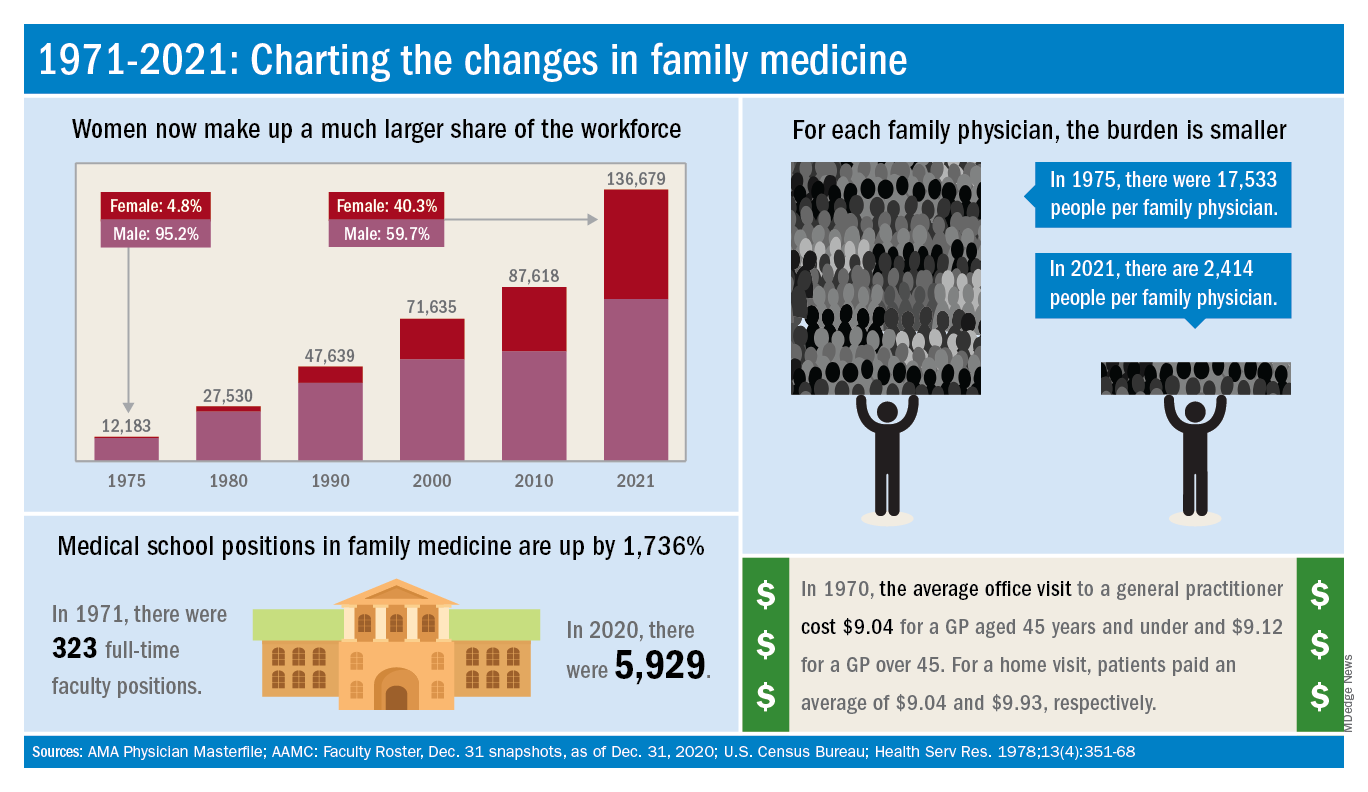
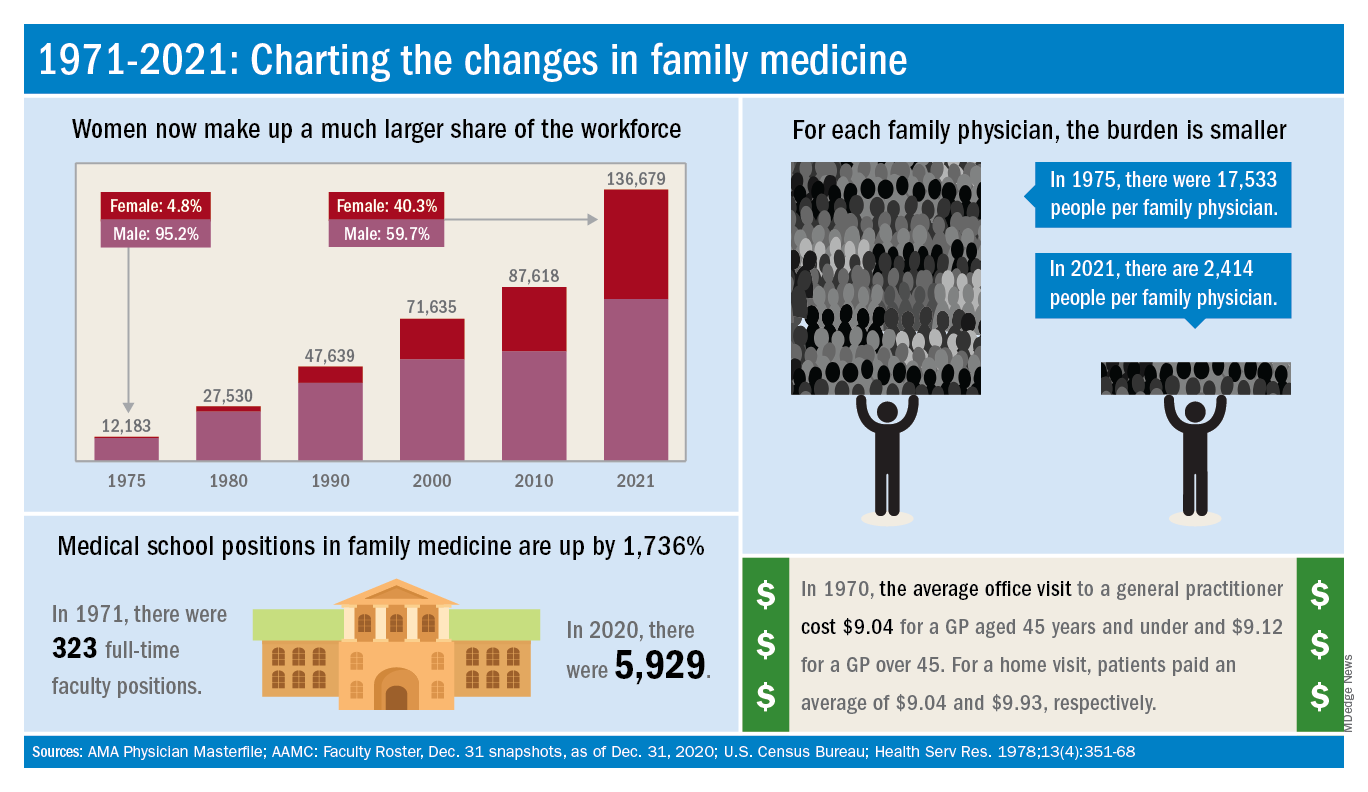
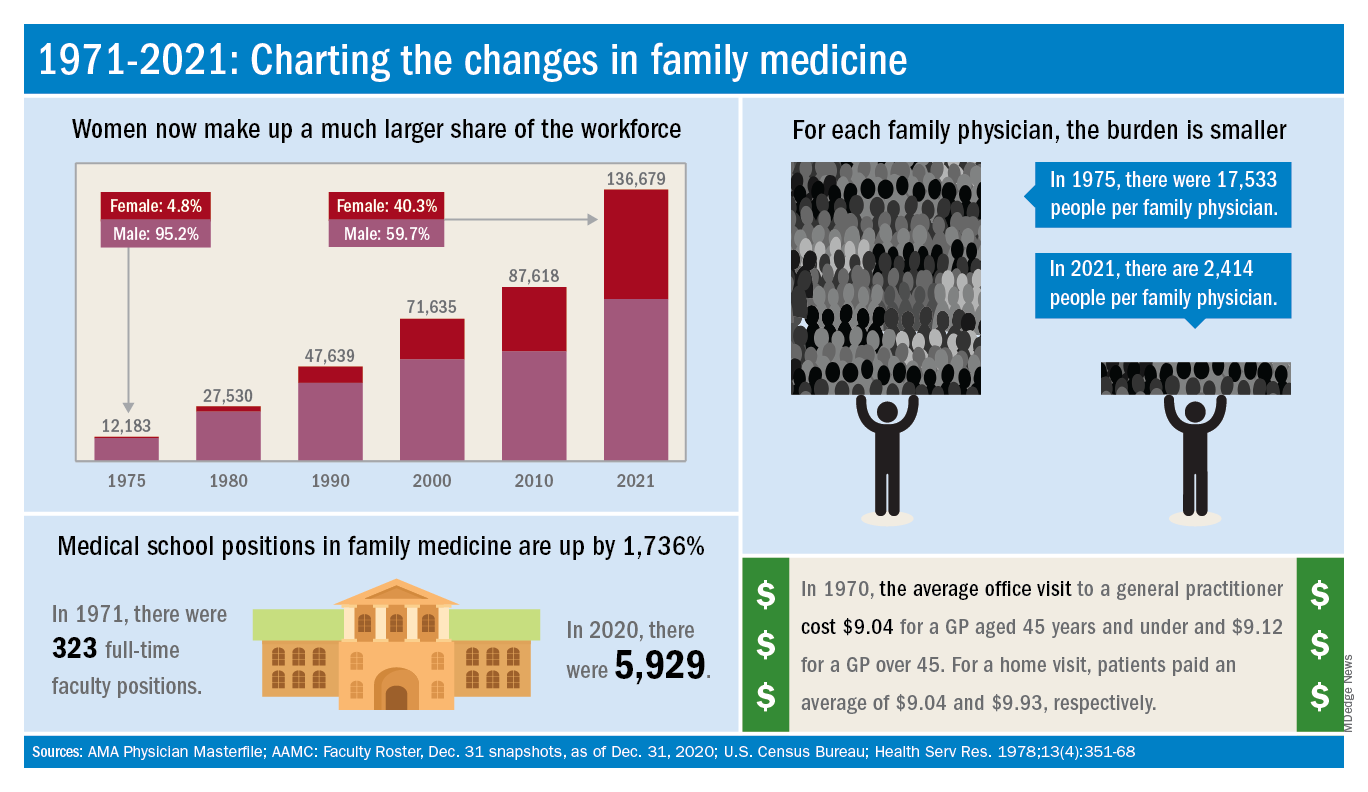
The face of family medicine in 1975 vs. today
Today’s workforce is much larger than it was in 1975, when there were just over 12,000 family physicians in the United States. As of January 2021, the total was approaching 137,000, including all “physicians and residents in patient care, research, administration, teaching, retired, inactive, etc.,” the AMA explained.
Family physicians as a group are much more diverse than they were in 1975. That year, 8.3% of FPs were international medical graduates (IMGs). By 2010, IMGs made up almost 23% of the workforce, and in the 2020 resident match, 37% of the 4,662 available family medicine slots were filled by IMGs.
Women have made even greater inroads into the family physician ranks over the last 5 decades. In 1975, less than 5% of all FPs were females, but by 2021 the proportion of females in the specialty was just over 40%.
In the first 5 years of the family practice era, 1969-1973, only 12 women and 31 IMGs graduated from FP residency programs, those numbers representing 3.2% and 8.3%, respectively, of the total of 372, according to a 1996 study in JAMA. By 1990-1993, women made up 33% and IMGs 14% of the 9,400 graduates.
Another group that increased its presence in family medicine is doctors of osteopathy, who went from zero residency graduates in 1969-1973 to over 1,100 (11.8%) in 1990-1993, the JAMA report noted. By 2020, almost 1,400 osteopathic physicians entered family medicine residencies, filling 30% of all slots available, according to the National Resident Matching Program.
The medical schools producing all these new residents have raised their games since 1971: the number of full-time faculty in family medicine departments rose from 323 to 5,929 in 2020, based on data from the Association of American Medical Colleges (Faculty Roster, Dec. 31 snapshots, as of Dec. 31, 2020).
A shortage or a surplus of FPs?
It has been suggested, however, that all is not well in primary care land. A study conducted by the American Academy of Family Physicians in 2016 – a year after 2,463 graduates of MD- and DO-granting medical schools entered family medicine residencies – concluded “that the current medical school system is failing, collectively, to produce the primary care workforce that is needed to achieve optimal health.”
Warnings about physician shortages are nothing new, but how about the other side of the coin? The Jan. 15, 1981, issue of Family Practice News covered a somewhat controversial report from the Graduate Medical Education National Advisory Committee, which projected a surplus of 3,000 FPs, and as many as 70,000 physicians overall, by the year 1990.
Just a few months later, in the June 15, 1981, issue of FPN, an AAFP officer predicted that “the flood of new physicians in the next decade may affect family practice more than any other specialty.”
Mostly, though, the issue is shortages. In 2002, a status report on family practice from the Robert Graham Center acknowledged that “many centers of academic medicine continue to resist the development of family practice and primary care. ... Family medicine remains a true counterculture in these environments, and students may continue to face significant discouragement in response to interest they may express in becoming a family physician.”
and the men and women who practice it are no exception.
The family medicine workforce of 2021 is not the workforce of 1971. Not even close. Although we would like to give a huge shout-out to anyone who can claim to be a member of both.
Today’s FP workforce is, first of all, much larger than it was in 1971, although we can’t actually prove it because the American Medical Association’s data for that year are “only available in books that are locked away at the empty AMA headquarters,” according to a member of the AMA media relations staff who is, like so many people these days, working at home because of the pandemic.
The face of family medicine in 1975 vs. today
Today’s workforce is much larger than it was in 1975, when there were just over 12,000 family physicians in the United States. As of January 2021, the total was approaching 137,000, including all “physicians and residents in patient care, research, administration, teaching, retired, inactive, etc.,” the AMA explained.
Family physicians as a group are much more diverse than they were in 1975. That year, 8.3% of FPs were international medical graduates (IMGs). By 2010, IMGs made up almost 23% of the workforce, and in the 2020 resident match, 37% of the 4,662 available family medicine slots were filled by IMGs.
Women have made even greater inroads into the family physician ranks over the last 5 decades. In 1975, less than 5% of all FPs were females, but by 2021 the proportion of females in the specialty was just over 40%.
In the first 5 years of the family practice era, 1969-1973, only 12 women and 31 IMGs graduated from FP residency programs, those numbers representing 3.2% and 8.3%, respectively, of the total of 372, according to a 1996 study in JAMA. By 1990-1993, women made up 33% and IMGs 14% of the 9,400 graduates.
Another group that increased its presence in family medicine is doctors of osteopathy, who went from zero residency graduates in 1969-1973 to over 1,100 (11.8%) in 1990-1993, the JAMA report noted. By 2020, almost 1,400 osteopathic physicians entered family medicine residencies, filling 30% of all slots available, according to the National Resident Matching Program.
The medical schools producing all these new residents have raised their games since 1971: the number of full-time faculty in family medicine departments rose from 323 to 5,929 in 2020, based on data from the Association of American Medical Colleges (Faculty Roster, Dec. 31 snapshots, as of Dec. 31, 2020).
A shortage or a surplus of FPs?
It has been suggested, however, that all is not well in primary care land. A study conducted by the American Academy of Family Physicians in 2016 – a year after 2,463 graduates of MD- and DO-granting medical schools entered family medicine residencies – concluded “that the current medical school system is failing, collectively, to produce the primary care workforce that is needed to achieve optimal health.”
Warnings about physician shortages are nothing new, but how about the other side of the coin? The Jan. 15, 1981, issue of Family Practice News covered a somewhat controversial report from the Graduate Medical Education National Advisory Committee, which projected a surplus of 3,000 FPs, and as many as 70,000 physicians overall, by the year 1990.
Just a few months later, in the June 15, 1981, issue of FPN, an AAFP officer predicted that “the flood of new physicians in the next decade may affect family practice more than any other specialty.”
Mostly, though, the issue is shortages. In 2002, a status report on family practice from the Robert Graham Center acknowledged that “many centers of academic medicine continue to resist the development of family practice and primary care. ... Family medicine remains a true counterculture in these environments, and students may continue to face significant discouragement in response to interest they may express in becoming a family physician.”
and the men and women who practice it are no exception.
The family medicine workforce of 2021 is not the workforce of 1971. Not even close. Although we would like to give a huge shout-out to anyone who can claim to be a member of both.
Today’s FP workforce is, first of all, much larger than it was in 1971, although we can’t actually prove it because the American Medical Association’s data for that year are “only available in books that are locked away at the empty AMA headquarters,” according to a member of the AMA media relations staff who is, like so many people these days, working at home because of the pandemic.
The face of family medicine in 1975 vs. today
Today’s workforce is much larger than it was in 1975, when there were just over 12,000 family physicians in the United States. As of January 2021, the total was approaching 137,000, including all “physicians and residents in patient care, research, administration, teaching, retired, inactive, etc.,” the AMA explained.
Family physicians as a group are much more diverse than they were in 1975. That year, 8.3% of FPs were international medical graduates (IMGs). By 2010, IMGs made up almost 23% of the workforce, and in the 2020 resident match, 37% of the 4,662 available family medicine slots were filled by IMGs.
Women have made even greater inroads into the family physician ranks over the last 5 decades. In 1975, less than 5% of all FPs were females, but by 2021 the proportion of females in the specialty was just over 40%.
In the first 5 years of the family practice era, 1969-1973, only 12 women and 31 IMGs graduated from FP residency programs, those numbers representing 3.2% and 8.3%, respectively, of the total of 372, according to a 1996 study in JAMA. By 1990-1993, women made up 33% and IMGs 14% of the 9,400 graduates.
Another group that increased its presence in family medicine is doctors of osteopathy, who went from zero residency graduates in 1969-1973 to over 1,100 (11.8%) in 1990-1993, the JAMA report noted. By 2020, almost 1,400 osteopathic physicians entered family medicine residencies, filling 30% of all slots available, according to the National Resident Matching Program.
The medical schools producing all these new residents have raised their games since 1971: the number of full-time faculty in family medicine departments rose from 323 to 5,929 in 2020, based on data from the Association of American Medical Colleges (Faculty Roster, Dec. 31 snapshots, as of Dec. 31, 2020).
A shortage or a surplus of FPs?
It has been suggested, however, that all is not well in primary care land. A study conducted by the American Academy of Family Physicians in 2016 – a year after 2,463 graduates of MD- and DO-granting medical schools entered family medicine residencies – concluded “that the current medical school system is failing, collectively, to produce the primary care workforce that is needed to achieve optimal health.”
Warnings about physician shortages are nothing new, but how about the other side of the coin? The Jan. 15, 1981, issue of Family Practice News covered a somewhat controversial report from the Graduate Medical Education National Advisory Committee, which projected a surplus of 3,000 FPs, and as many as 70,000 physicians overall, by the year 1990.
Just a few months later, in the June 15, 1981, issue of FPN, an AAFP officer predicted that “the flood of new physicians in the next decade may affect family practice more than any other specialty.”
Mostly, though, the issue is shortages. In 2002, a status report on family practice from the Robert Graham Center acknowledged that “many centers of academic medicine continue to resist the development of family practice and primary care. ... Family medicine remains a true counterculture in these environments, and students may continue to face significant discouragement in response to interest they may express in becoming a family physician.”
Medicaid and access to dermatologists
Recently, an interview titled “Dermatology a bellwether of health inequities during COVID-19,” was published by the AMA. In my opinion, the interview was largely accurate, but I took issue with the following statement in the article: “Dermatology is a lucrative specialty, and many dermatologists do not accept Medicaid.”
To me, this implies that physicians are to blame for poor health care access, which drives me insane. Dermatology is not a particularly lucrative specialty; it ranked 13th in a recent survey from the professional medical network Doximity. Furthermore, if payment for practice expense is removed, dermatology drops much further down, close to primary care.
There is a fundamental misunderstanding by the public and legislators about physician incomes. The reimbursements that are reported by Medicare for example, include the practice expense cost, which for dermatology is about 60% of the total remitted to the doctor, as I wrote in a 2015 column.
That is, the cost of providing the facility, supplies, staff, rent, and utilities are included in “reimbursement,” though this is money that goes out the door to pay the bills as quickly as it comes in. This is for overhead, nothing here for the practitioner’s time and work.
Even when dermatologists perform hospital consults, they usually bring their own supply kit from their office for skin biopsies, or other procedures since these are impossible to find in a hospital.
I also pointed out in my earlier column that most other specialties do not provide the majority of their procedures in the office, but instead, use the hospital, which provides supplies and staff for procedures. These other specialists are to be lauded for providing their services at charity rates, or for no pay at all, but at least they do not have to pay for the building, equipment, supplies, and staff out of pocket. Dermatologists do, since in a sense, they run their own “hospitals” as almost all of their procedures are based out of their offices.
The economics of a patient visit
I do not dispute that it is more difficult for a Medicaid patient to get an appointment with a dermatologist than it is for a patient with private insurance, but this is because Medicaid often pays less than the cost of supplies to see them. It is also easier to get an appointment for a cosmetic procedure than a rash because reimbursements in general are artificially suppressed, even for Medicare (which is also the benchmark for private insurers) by the federal government. Medicare reimbursements have not kept pace with inflation and are about 53% less than they were in 1992.
Let’s look at a skin biopsy. The supplies and equipment to perform a skin biopsy cost over $50. In Ohio, Medicare pays $96.19 for a skin biopsy. Medicaid pays $47.20. That’s correct: less than the cost of supplies and overhead. So, a private practitioner not only provides the service for free, but loses money on every visit that involves a skin biopsy. When I talk to legislators, I liken this to my standing in front of my office and handing out $5 bills. In Ohio, Medicare pays $105.04 for a level 3 office visit. Medicaid pays $57.76. Medicare overhead on a level 3 office visit is again about 50%, so the office visit is about a break-even proposition, if you donate your time.
Academic medical centers can charge additional facility fees, and some receive subsidies from the city and county to treat indigent patients, and are often obligated to see all. Most hospitals with high Medicaid and indigent patient loads pay their surgical specialists to take call at their emergency rooms and often subsidize their emergency room doctors as well.
I agree that dermatology is an important specialty to have access to in the COVID-19 pandemic. I agree that patients of color may be disproportionately impacted because they may be covered by Medicaid more often, or have no insurance at all. The finger of blame, however, should be squarely pointed at politicians who have woefully underfunded Medicaid reimbursement rates, as well as payments for physicians under the Affordable Care Act, while thumping their chests and boasting how they have provided health care to millions. I think this was eloquently demonstrated when as part of the “deal” Congress made with the AMA to get the ACA passed, Congress agreed to pay primary care physicians (but only primary care) Medicare rates for Medicaid patients for 2 years.
Some states have continued to pay enhanced Medicaid rates and have fewer Medicaid patient access issues.
Most convincing, perhaps, are the states that pay Medicare rates or better for their Medicaid enrollees, for example Alaska and Montana. In these states, you will not have access to care issues beyond the actual human shortage of physicians in remote areas.
So, in conclusion, I maintain that dermatology is not a particularly lucrative specialty, once the overhead expense payments are removed, and further argue, that even if it were, why does that obligate us to provide care to insurance plans at a loss? Medicaid access to dermatologists is a government economic issue, not a physician ethical one. Most Americans get to pick the charities they choose to donate to.
The federal government would love to force all physicians into a plan where you must see patients at their chosen rates or see no patients at all. Look no further than our Canadian neighbors, where long wait times to see specialists are legendary. It has been reported that there are only six to seven hundred dermatologists in all of Canada to serve 30 million people.
So, when the topic of poor patient access to care for the Medicaid enrollee or indigent comes up, stand tall and point your finger to your state capital. That is where the blame lies.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Recently, an interview titled “Dermatology a bellwether of health inequities during COVID-19,” was published by the AMA. In my opinion, the interview was largely accurate, but I took issue with the following statement in the article: “Dermatology is a lucrative specialty, and many dermatologists do not accept Medicaid.”
To me, this implies that physicians are to blame for poor health care access, which drives me insane. Dermatology is not a particularly lucrative specialty; it ranked 13th in a recent survey from the professional medical network Doximity. Furthermore, if payment for practice expense is removed, dermatology drops much further down, close to primary care.
There is a fundamental misunderstanding by the public and legislators about physician incomes. The reimbursements that are reported by Medicare for example, include the practice expense cost, which for dermatology is about 60% of the total remitted to the doctor, as I wrote in a 2015 column.
That is, the cost of providing the facility, supplies, staff, rent, and utilities are included in “reimbursement,” though this is money that goes out the door to pay the bills as quickly as it comes in. This is for overhead, nothing here for the practitioner’s time and work.
Even when dermatologists perform hospital consults, they usually bring their own supply kit from their office for skin biopsies, or other procedures since these are impossible to find in a hospital.
I also pointed out in my earlier column that most other specialties do not provide the majority of their procedures in the office, but instead, use the hospital, which provides supplies and staff for procedures. These other specialists are to be lauded for providing their services at charity rates, or for no pay at all, but at least they do not have to pay for the building, equipment, supplies, and staff out of pocket. Dermatologists do, since in a sense, they run their own “hospitals” as almost all of their procedures are based out of their offices.
The economics of a patient visit
I do not dispute that it is more difficult for a Medicaid patient to get an appointment with a dermatologist than it is for a patient with private insurance, but this is because Medicaid often pays less than the cost of supplies to see them. It is also easier to get an appointment for a cosmetic procedure than a rash because reimbursements in general are artificially suppressed, even for Medicare (which is also the benchmark for private insurers) by the federal government. Medicare reimbursements have not kept pace with inflation and are about 53% less than they were in 1992.
Let’s look at a skin biopsy. The supplies and equipment to perform a skin biopsy cost over $50. In Ohio, Medicare pays $96.19 for a skin biopsy. Medicaid pays $47.20. That’s correct: less than the cost of supplies and overhead. So, a private practitioner not only provides the service for free, but loses money on every visit that involves a skin biopsy. When I talk to legislators, I liken this to my standing in front of my office and handing out $5 bills. In Ohio, Medicare pays $105.04 for a level 3 office visit. Medicaid pays $57.76. Medicare overhead on a level 3 office visit is again about 50%, so the office visit is about a break-even proposition, if you donate your time.
Academic medical centers can charge additional facility fees, and some receive subsidies from the city and county to treat indigent patients, and are often obligated to see all. Most hospitals with high Medicaid and indigent patient loads pay their surgical specialists to take call at their emergency rooms and often subsidize their emergency room doctors as well.
I agree that dermatology is an important specialty to have access to in the COVID-19 pandemic. I agree that patients of color may be disproportionately impacted because they may be covered by Medicaid more often, or have no insurance at all. The finger of blame, however, should be squarely pointed at politicians who have woefully underfunded Medicaid reimbursement rates, as well as payments for physicians under the Affordable Care Act, while thumping their chests and boasting how they have provided health care to millions. I think this was eloquently demonstrated when as part of the “deal” Congress made with the AMA to get the ACA passed, Congress agreed to pay primary care physicians (but only primary care) Medicare rates for Medicaid patients for 2 years.
Some states have continued to pay enhanced Medicaid rates and have fewer Medicaid patient access issues.
Most convincing, perhaps, are the states that pay Medicare rates or better for their Medicaid enrollees, for example Alaska and Montana. In these states, you will not have access to care issues beyond the actual human shortage of physicians in remote areas.
So, in conclusion, I maintain that dermatology is not a particularly lucrative specialty, once the overhead expense payments are removed, and further argue, that even if it were, why does that obligate us to provide care to insurance plans at a loss? Medicaid access to dermatologists is a government economic issue, not a physician ethical one. Most Americans get to pick the charities they choose to donate to.
The federal government would love to force all physicians into a plan where you must see patients at their chosen rates or see no patients at all. Look no further than our Canadian neighbors, where long wait times to see specialists are legendary. It has been reported that there are only six to seven hundred dermatologists in all of Canada to serve 30 million people.
So, when the topic of poor patient access to care for the Medicaid enrollee or indigent comes up, stand tall and point your finger to your state capital. That is where the blame lies.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Recently, an interview titled “Dermatology a bellwether of health inequities during COVID-19,” was published by the AMA. In my opinion, the interview was largely accurate, but I took issue with the following statement in the article: “Dermatology is a lucrative specialty, and many dermatologists do not accept Medicaid.”
To me, this implies that physicians are to blame for poor health care access, which drives me insane. Dermatology is not a particularly lucrative specialty; it ranked 13th in a recent survey from the professional medical network Doximity. Furthermore, if payment for practice expense is removed, dermatology drops much further down, close to primary care.
There is a fundamental misunderstanding by the public and legislators about physician incomes. The reimbursements that are reported by Medicare for example, include the practice expense cost, which for dermatology is about 60% of the total remitted to the doctor, as I wrote in a 2015 column.
That is, the cost of providing the facility, supplies, staff, rent, and utilities are included in “reimbursement,” though this is money that goes out the door to pay the bills as quickly as it comes in. This is for overhead, nothing here for the practitioner’s time and work.
Even when dermatologists perform hospital consults, they usually bring their own supply kit from their office for skin biopsies, or other procedures since these are impossible to find in a hospital.
I also pointed out in my earlier column that most other specialties do not provide the majority of their procedures in the office, but instead, use the hospital, which provides supplies and staff for procedures. These other specialists are to be lauded for providing their services at charity rates, or for no pay at all, but at least they do not have to pay for the building, equipment, supplies, and staff out of pocket. Dermatologists do, since in a sense, they run their own “hospitals” as almost all of their procedures are based out of their offices.
The economics of a patient visit
I do not dispute that it is more difficult for a Medicaid patient to get an appointment with a dermatologist than it is for a patient with private insurance, but this is because Medicaid often pays less than the cost of supplies to see them. It is also easier to get an appointment for a cosmetic procedure than a rash because reimbursements in general are artificially suppressed, even for Medicare (which is also the benchmark for private insurers) by the federal government. Medicare reimbursements have not kept pace with inflation and are about 53% less than they were in 1992.
Let’s look at a skin biopsy. The supplies and equipment to perform a skin biopsy cost over $50. In Ohio, Medicare pays $96.19 for a skin biopsy. Medicaid pays $47.20. That’s correct: less than the cost of supplies and overhead. So, a private practitioner not only provides the service for free, but loses money on every visit that involves a skin biopsy. When I talk to legislators, I liken this to my standing in front of my office and handing out $5 bills. In Ohio, Medicare pays $105.04 for a level 3 office visit. Medicaid pays $57.76. Medicare overhead on a level 3 office visit is again about 50%, so the office visit is about a break-even proposition, if you donate your time.
Academic medical centers can charge additional facility fees, and some receive subsidies from the city and county to treat indigent patients, and are often obligated to see all. Most hospitals with high Medicaid and indigent patient loads pay their surgical specialists to take call at their emergency rooms and often subsidize their emergency room doctors as well.
I agree that dermatology is an important specialty to have access to in the COVID-19 pandemic. I agree that patients of color may be disproportionately impacted because they may be covered by Medicaid more often, or have no insurance at all. The finger of blame, however, should be squarely pointed at politicians who have woefully underfunded Medicaid reimbursement rates, as well as payments for physicians under the Affordable Care Act, while thumping their chests and boasting how they have provided health care to millions. I think this was eloquently demonstrated when as part of the “deal” Congress made with the AMA to get the ACA passed, Congress agreed to pay primary care physicians (but only primary care) Medicare rates for Medicaid patients for 2 years.
Some states have continued to pay enhanced Medicaid rates and have fewer Medicaid patient access issues.
Most convincing, perhaps, are the states that pay Medicare rates or better for their Medicaid enrollees, for example Alaska and Montana. In these states, you will not have access to care issues beyond the actual human shortage of physicians in remote areas.
So, in conclusion, I maintain that dermatology is not a particularly lucrative specialty, once the overhead expense payments are removed, and further argue, that even if it were, why does that obligate us to provide care to insurance plans at a loss? Medicaid access to dermatologists is a government economic issue, not a physician ethical one. Most Americans get to pick the charities they choose to donate to.
The federal government would love to force all physicians into a plan where you must see patients at their chosen rates or see no patients at all. Look no further than our Canadian neighbors, where long wait times to see specialists are legendary. It has been reported that there are only six to seven hundred dermatologists in all of Canada to serve 30 million people.
So, when the topic of poor patient access to care for the Medicaid enrollee or indigent comes up, stand tall and point your finger to your state capital. That is where the blame lies.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Cardiovascular trials lose more women than men
A new analysis of 11 phase 3/4 cardiovascular clinical trials conducted by the Thrombolysis in Myocardial Infarction (TIMI) group shows that women are more likely than men to discontinue study medications, and to withdraw from trials. The differences could not be explained by different frequencies of reporting adverse events, or by baseline differences.
The findings are significant, since cardiovascular drugs are routinely prescribed to women based on clinical trials that are populated largely by men, according to lead study author Emily Lau, MD, who is an advanced cardiology fellow at Massachusetts General Hospital, Boston. “It highlights an important disparity in clinical research in cardiology, because if women are already not represented well in clinical trials, and if once in clinical trials they don’t complete the study, it’s very hard to extrapolate the clinical trial findings to our female population in an accurate way,” Dr. Lau said in an interview. She also noted that sex-specific and reproductive factors are increasingly recognized as being important in the development and progression of cardiovascular disease.
The study was published in the journal Circulation.
The study refutes previously advanced explanations for higher withdrawal among women, including sex difference and comorbidities, according to an accompanying editorial by Sofia Sederholm Lawesson, MD, PhD, Eva Swahn, MD, PhD, and Joakim Alfredsson, MD, PhD, of Linköping University, Sweden. They also pointed out that the study found a larger between-sex difference in failure to adhere to study drug in North America (odds ratio, 1.35; 95% confidence interval, 1.30-1.41), but a more moderate difference among participants in Europe/Middle East/Africa (OR, 1.13; 95% CI, 1.09-1.17) and Asia/Pacific (OR, 1.13; 95% CI, 1.03-1.23) regions. And there were no sex differences at all among South/Central American populations.
They noted that high rates of nonadherence increase the chances of a false negative finding and overestimation of drug safety. “We know the associations between nonadherence and clinical outcomes. The next step should be to better understand the underlying reasons for, as well as consistent reporting of, nonadherence, and discontinuation in RCTs,” the editorial authors wrote.
Dr. Lau suggested a simple method to better understand reasons for withdrawal: Addition of questions to the case report form that asks about reasons for drug discontinuation or study withdrawal. “Was it an adverse event? Was it because I’m a mother of three and I can’t get to the clinical trial site after work and also pick up my kids? Are there societal barriers for women, or was it the experience of the clinical trial that was maybe less favorable for women compared to men? Or maybe there are medical reasons we simply don’t know. Something as simple as asking those questions can help us better understand the barriers to female retention,” said Dr. Lau.
The analysis included data from 135,879 men (72%) and 51,812 women (28%) enrolled in the trials. After adjustment for baseline differences, women were more likely than were men to permanently discontinue study drug (adjusted odds ratio [aOR], 1.22: P < .001), which did not vary by study duration. The finding was consistent regardless of the type of drug studied, as well as across placebo and active study arms.
Women also were more likely to prematurely discontinue study drug (trial-adjusted OR, 1.18; P < .001). The rate of drug discontinuation due to adverse event was identical in both men and women, at 36%.
Women were more likely to withdraw consent than were men in a meta-analysis and when individual patient-level results were pooled (aOR, 1.26; P < .001 for both).
Dr. Lau received funding from the National Institutes of Health and has no relevant financial disclosures. The editorial authors had various disclosures, including lecture fees from Bayer, Pfizer, and Boehringer Ingelheim, and they served on advisory boards for AstraZeneca and MSD.
A new analysis of 11 phase 3/4 cardiovascular clinical trials conducted by the Thrombolysis in Myocardial Infarction (TIMI) group shows that women are more likely than men to discontinue study medications, and to withdraw from trials. The differences could not be explained by different frequencies of reporting adverse events, or by baseline differences.
The findings are significant, since cardiovascular drugs are routinely prescribed to women based on clinical trials that are populated largely by men, according to lead study author Emily Lau, MD, who is an advanced cardiology fellow at Massachusetts General Hospital, Boston. “It highlights an important disparity in clinical research in cardiology, because if women are already not represented well in clinical trials, and if once in clinical trials they don’t complete the study, it’s very hard to extrapolate the clinical trial findings to our female population in an accurate way,” Dr. Lau said in an interview. She also noted that sex-specific and reproductive factors are increasingly recognized as being important in the development and progression of cardiovascular disease.
The study was published in the journal Circulation.
The study refutes previously advanced explanations for higher withdrawal among women, including sex difference and comorbidities, according to an accompanying editorial by Sofia Sederholm Lawesson, MD, PhD, Eva Swahn, MD, PhD, and Joakim Alfredsson, MD, PhD, of Linköping University, Sweden. They also pointed out that the study found a larger between-sex difference in failure to adhere to study drug in North America (odds ratio, 1.35; 95% confidence interval, 1.30-1.41), but a more moderate difference among participants in Europe/Middle East/Africa (OR, 1.13; 95% CI, 1.09-1.17) and Asia/Pacific (OR, 1.13; 95% CI, 1.03-1.23) regions. And there were no sex differences at all among South/Central American populations.
They noted that high rates of nonadherence increase the chances of a false negative finding and overestimation of drug safety. “We know the associations between nonadherence and clinical outcomes. The next step should be to better understand the underlying reasons for, as well as consistent reporting of, nonadherence, and discontinuation in RCTs,” the editorial authors wrote.
Dr. Lau suggested a simple method to better understand reasons for withdrawal: Addition of questions to the case report form that asks about reasons for drug discontinuation or study withdrawal. “Was it an adverse event? Was it because I’m a mother of three and I can’t get to the clinical trial site after work and also pick up my kids? Are there societal barriers for women, or was it the experience of the clinical trial that was maybe less favorable for women compared to men? Or maybe there are medical reasons we simply don’t know. Something as simple as asking those questions can help us better understand the barriers to female retention,” said Dr. Lau.
The analysis included data from 135,879 men (72%) and 51,812 women (28%) enrolled in the trials. After adjustment for baseline differences, women were more likely than were men to permanently discontinue study drug (adjusted odds ratio [aOR], 1.22: P < .001), which did not vary by study duration. The finding was consistent regardless of the type of drug studied, as well as across placebo and active study arms.
Women also were more likely to prematurely discontinue study drug (trial-adjusted OR, 1.18; P < .001). The rate of drug discontinuation due to adverse event was identical in both men and women, at 36%.
Women were more likely to withdraw consent than were men in a meta-analysis and when individual patient-level results were pooled (aOR, 1.26; P < .001 for both).
Dr. Lau received funding from the National Institutes of Health and has no relevant financial disclosures. The editorial authors had various disclosures, including lecture fees from Bayer, Pfizer, and Boehringer Ingelheim, and they served on advisory boards for AstraZeneca and MSD.
A new analysis of 11 phase 3/4 cardiovascular clinical trials conducted by the Thrombolysis in Myocardial Infarction (TIMI) group shows that women are more likely than men to discontinue study medications, and to withdraw from trials. The differences could not be explained by different frequencies of reporting adverse events, or by baseline differences.
The findings are significant, since cardiovascular drugs are routinely prescribed to women based on clinical trials that are populated largely by men, according to lead study author Emily Lau, MD, who is an advanced cardiology fellow at Massachusetts General Hospital, Boston. “It highlights an important disparity in clinical research in cardiology, because if women are already not represented well in clinical trials, and if once in clinical trials they don’t complete the study, it’s very hard to extrapolate the clinical trial findings to our female population in an accurate way,” Dr. Lau said in an interview. She also noted that sex-specific and reproductive factors are increasingly recognized as being important in the development and progression of cardiovascular disease.
The study was published in the journal Circulation.
The study refutes previously advanced explanations for higher withdrawal among women, including sex difference and comorbidities, according to an accompanying editorial by Sofia Sederholm Lawesson, MD, PhD, Eva Swahn, MD, PhD, and Joakim Alfredsson, MD, PhD, of Linköping University, Sweden. They also pointed out that the study found a larger between-sex difference in failure to adhere to study drug in North America (odds ratio, 1.35; 95% confidence interval, 1.30-1.41), but a more moderate difference among participants in Europe/Middle East/Africa (OR, 1.13; 95% CI, 1.09-1.17) and Asia/Pacific (OR, 1.13; 95% CI, 1.03-1.23) regions. And there were no sex differences at all among South/Central American populations.
They noted that high rates of nonadherence increase the chances of a false negative finding and overestimation of drug safety. “We know the associations between nonadherence and clinical outcomes. The next step should be to better understand the underlying reasons for, as well as consistent reporting of, nonadherence, and discontinuation in RCTs,” the editorial authors wrote.
Dr. Lau suggested a simple method to better understand reasons for withdrawal: Addition of questions to the case report form that asks about reasons for drug discontinuation or study withdrawal. “Was it an adverse event? Was it because I’m a mother of three and I can’t get to the clinical trial site after work and also pick up my kids? Are there societal barriers for women, or was it the experience of the clinical trial that was maybe less favorable for women compared to men? Or maybe there are medical reasons we simply don’t know. Something as simple as asking those questions can help us better understand the barriers to female retention,” said Dr. Lau.
The analysis included data from 135,879 men (72%) and 51,812 women (28%) enrolled in the trials. After adjustment for baseline differences, women were more likely than were men to permanently discontinue study drug (adjusted odds ratio [aOR], 1.22: P < .001), which did not vary by study duration. The finding was consistent regardless of the type of drug studied, as well as across placebo and active study arms.
Women also were more likely to prematurely discontinue study drug (trial-adjusted OR, 1.18; P < .001). The rate of drug discontinuation due to adverse event was identical in both men and women, at 36%.
Women were more likely to withdraw consent than were men in a meta-analysis and when individual patient-level results were pooled (aOR, 1.26; P < .001 for both).
Dr. Lau received funding from the National Institutes of Health and has no relevant financial disclosures. The editorial authors had various disclosures, including lecture fees from Bayer, Pfizer, and Boehringer Ingelheim, and they served on advisory boards for AstraZeneca and MSD.
FROM CIRCULATION
What Tom Brady and Patrick Mahomes can teach us about physicians
Warning: This article will be about Tom Brady. If you love Tom Brady, hate Tom Brady, previously loved and now hate Tom Brady, I’m just warning you so you’ll be in the right frame of mind to continue. (If you don’t know who Tom Brady is, he’s Gisele’s husband).
Brady, who plays for the Tampa Bay Buccaneers, has played in the NFL for 21 seasons, an unbelievable number given the average career for a quarterback is 3 years. He’s 43 years old and was the oldest player in a Super Bowl, ever. He faced Patrick Mahomes, the quarterback for the opposing Kansas City Chiefs. Mahomes is one of the most athletic and talented quarterbacks of all time, and Mahomes is nearly 20 years younger than Brady. Yet, in a shot heard around the NFL world, Brady won.
But, was a Brady victory so shocking? Hot-shot residents may have a lot of moxie and talent, but experienced doctors often prevail by simply making sound decisions and avoiding mistakes. In our department, we’ve been discussing this lately: We’re hiring two dermatologists and we’re fortunate to have some amazing candidates apply. Some, like Mahomes, are young all-stars with outstanding ability and potential, right out of residency. Others, Brady-like, have been in practice for years and are ready to move to a new franchise.
Our medical group’s experiences are probably similar to many practices: New physicians out of residency often bring energy, inspiration, and ease with the latest therapies, devices, and surgical techniques. Yet, they sometimes struggle with efficiency and unforced errors. Experienced physicians might not know what’s hot, but they can often see where the best course of action lies, understanding not only the physiology but also the patient in ways that only experience can teach you. Fortunately, for those like me who’ve crossed midlife, there doesn’t seem to be an upper limit to experience – it is possible to keep getting better. Yes, I’m just like Tom Brady. (I wrote this article just to print that line.)
Some of the best doctors I’ve ever seen in action were emeritus physicians. In medical school at Wake Forest University, one of my professors was Dr. Eben Alexander. A retired neurosurgeon, he taught a case-based critical thinking skills class. I recall his brilliant insight and coaching, working through cases that had nothing to do with the brain or with surgery. He used his vast experience and wisdom to teach us how to practice medicine. He was, at that time, nearly 90 years old. Despite having been retired for decades, he was still writing articles and editing journals. He was inspiring. For a minute, he had me thinking I’d like to be a neurosurgeon, so I could be just like Eben Alexander. I did not, but I learned things from him that still impact my practice as a dermatologist today.
I’m sure you’ve had similar experiences of older colleagues or mentors who were the best doctor in the clinic or the O.R. They are the Dr. Anthony Faucis, not just practicing, but leading while in their 8th or 9th decade. We are all so fortunate that they keep playing.
We’ve not made our final choices on whom to hire, but with two positions, I expect we’ll choose both a young doctor and an experienced one to add to our team. It will be fun to watch and learn from them. Just like it will be fun to watch Tom Brady in the Super Bowl again next year.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Warning: This article will be about Tom Brady. If you love Tom Brady, hate Tom Brady, previously loved and now hate Tom Brady, I’m just warning you so you’ll be in the right frame of mind to continue. (If you don’t know who Tom Brady is, he’s Gisele’s husband).
Brady, who plays for the Tampa Bay Buccaneers, has played in the NFL for 21 seasons, an unbelievable number given the average career for a quarterback is 3 years. He’s 43 years old and was the oldest player in a Super Bowl, ever. He faced Patrick Mahomes, the quarterback for the opposing Kansas City Chiefs. Mahomes is one of the most athletic and talented quarterbacks of all time, and Mahomes is nearly 20 years younger than Brady. Yet, in a shot heard around the NFL world, Brady won.
But, was a Brady victory so shocking? Hot-shot residents may have a lot of moxie and talent, but experienced doctors often prevail by simply making sound decisions and avoiding mistakes. In our department, we’ve been discussing this lately: We’re hiring two dermatologists and we’re fortunate to have some amazing candidates apply. Some, like Mahomes, are young all-stars with outstanding ability and potential, right out of residency. Others, Brady-like, have been in practice for years and are ready to move to a new franchise.
Our medical group’s experiences are probably similar to many practices: New physicians out of residency often bring energy, inspiration, and ease with the latest therapies, devices, and surgical techniques. Yet, they sometimes struggle with efficiency and unforced errors. Experienced physicians might not know what’s hot, but they can often see where the best course of action lies, understanding not only the physiology but also the patient in ways that only experience can teach you. Fortunately, for those like me who’ve crossed midlife, there doesn’t seem to be an upper limit to experience – it is possible to keep getting better. Yes, I’m just like Tom Brady. (I wrote this article just to print that line.)
Some of the best doctors I’ve ever seen in action were emeritus physicians. In medical school at Wake Forest University, one of my professors was Dr. Eben Alexander. A retired neurosurgeon, he taught a case-based critical thinking skills class. I recall his brilliant insight and coaching, working through cases that had nothing to do with the brain or with surgery. He used his vast experience and wisdom to teach us how to practice medicine. He was, at that time, nearly 90 years old. Despite having been retired for decades, he was still writing articles and editing journals. He was inspiring. For a minute, he had me thinking I’d like to be a neurosurgeon, so I could be just like Eben Alexander. I did not, but I learned things from him that still impact my practice as a dermatologist today.
I’m sure you’ve had similar experiences of older colleagues or mentors who were the best doctor in the clinic or the O.R. They are the Dr. Anthony Faucis, not just practicing, but leading while in their 8th or 9th decade. We are all so fortunate that they keep playing.
We’ve not made our final choices on whom to hire, but with two positions, I expect we’ll choose both a young doctor and an experienced one to add to our team. It will be fun to watch and learn from them. Just like it will be fun to watch Tom Brady in the Super Bowl again next year.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Warning: This article will be about Tom Brady. If you love Tom Brady, hate Tom Brady, previously loved and now hate Tom Brady, I’m just warning you so you’ll be in the right frame of mind to continue. (If you don’t know who Tom Brady is, he’s Gisele’s husband).
Brady, who plays for the Tampa Bay Buccaneers, has played in the NFL for 21 seasons, an unbelievable number given the average career for a quarterback is 3 years. He’s 43 years old and was the oldest player in a Super Bowl, ever. He faced Patrick Mahomes, the quarterback for the opposing Kansas City Chiefs. Mahomes is one of the most athletic and talented quarterbacks of all time, and Mahomes is nearly 20 years younger than Brady. Yet, in a shot heard around the NFL world, Brady won.
But, was a Brady victory so shocking? Hot-shot residents may have a lot of moxie and talent, but experienced doctors often prevail by simply making sound decisions and avoiding mistakes. In our department, we’ve been discussing this lately: We’re hiring two dermatologists and we’re fortunate to have some amazing candidates apply. Some, like Mahomes, are young all-stars with outstanding ability and potential, right out of residency. Others, Brady-like, have been in practice for years and are ready to move to a new franchise.
Our medical group’s experiences are probably similar to many practices: New physicians out of residency often bring energy, inspiration, and ease with the latest therapies, devices, and surgical techniques. Yet, they sometimes struggle with efficiency and unforced errors. Experienced physicians might not know what’s hot, but they can often see where the best course of action lies, understanding not only the physiology but also the patient in ways that only experience can teach you. Fortunately, for those like me who’ve crossed midlife, there doesn’t seem to be an upper limit to experience – it is possible to keep getting better. Yes, I’m just like Tom Brady. (I wrote this article just to print that line.)
Some of the best doctors I’ve ever seen in action were emeritus physicians. In medical school at Wake Forest University, one of my professors was Dr. Eben Alexander. A retired neurosurgeon, he taught a case-based critical thinking skills class. I recall his brilliant insight and coaching, working through cases that had nothing to do with the brain or with surgery. He used his vast experience and wisdom to teach us how to practice medicine. He was, at that time, nearly 90 years old. Despite having been retired for decades, he was still writing articles and editing journals. He was inspiring. For a minute, he had me thinking I’d like to be a neurosurgeon, so I could be just like Eben Alexander. I did not, but I learned things from him that still impact my practice as a dermatologist today.
I’m sure you’ve had similar experiences of older colleagues or mentors who were the best doctor in the clinic or the O.R. They are the Dr. Anthony Faucis, not just practicing, but leading while in their 8th or 9th decade. We are all so fortunate that they keep playing.
We’ve not made our final choices on whom to hire, but with two positions, I expect we’ll choose both a young doctor and an experienced one to add to our team. It will be fun to watch and learn from them. Just like it will be fun to watch Tom Brady in the Super Bowl again next year.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Family medicine: Who cares for the children?
according to new research.
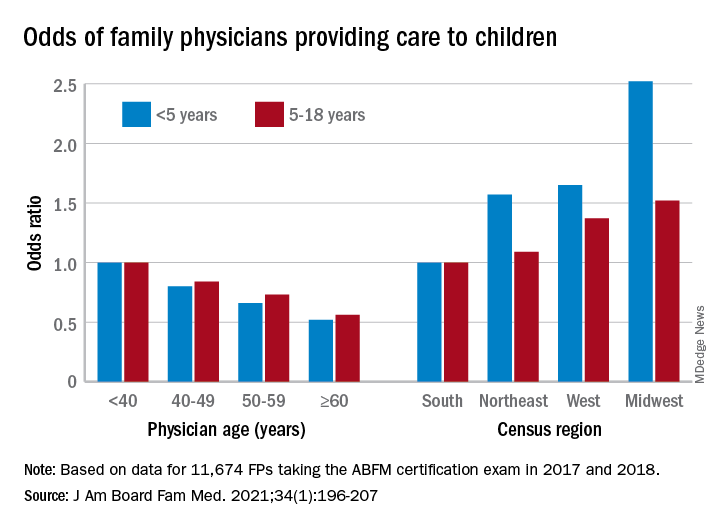
This the latest sign of a long-term decline, and it “poses a broader concern for a specialty that defines itself by its comprehensive scope of practice,” said the study investigators of the Robert Graham Center in Washington, D.C., in a written statement. “This is consistent with previous Robert Graham Center research that reported a similar steady decline from 1992 to 2002.”
Self-reported data from family physicians indicate that 84.3% cared for children aged 18 years and under in 2017, compared with 83.0% in 2018, based on a cross-sectional analysis of data gathered from 11,674 family physicians who completed the practice demographic questionnaire attached to the American Board of Family Medicine’s certification exam in 2017 and 2018.
“This current trend is unsettling, because family physicians provide the majority of pediatric care in rural and pediatrically underserved areas of the United States,” study author Anuradha Jetty, MPH, and coauthors said in the statement.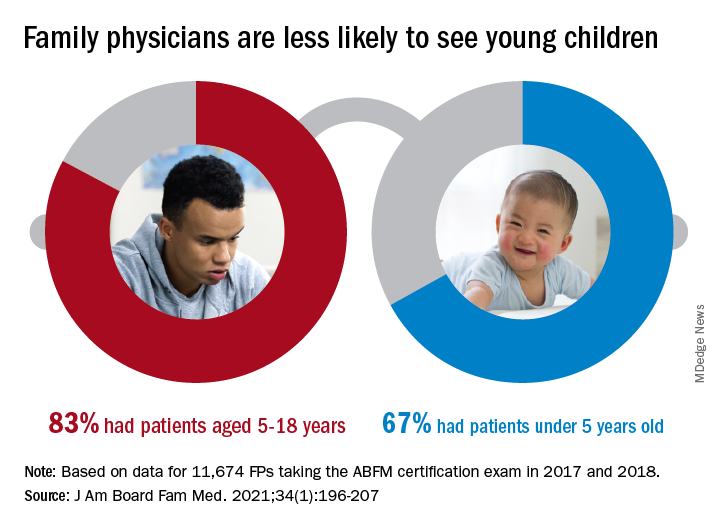
The analysis also offers a snapshot of the current state of pediatric care offered by family physicians. In 2017 and 2018, FPs were more likely to see patients aged 5-18 years than those under age 5 (83.0% vs. 67.0%), with variation by age, location, and race/ethnicity, said Ms. Jetty and colleagues, in their new paper.
FPs aged 60 years and older were much less likely to see pediatric patients, compared with those under age 40: odds ratios were 0.52 for children under 5 and 0.56 for children 5-18. Regional variation was even more pronounced: Compared with their colleagues in the Southern states, Midwestern FPs were 1.52 times as likely to treat children aged 5-18 and 2.52 times as likely to treat children under age 5, the investigators reported.
Non-Hispanic Asian and Hispanic family physicians had significantly lower odds of seeing pediatric patients, relative to non-Hispanic White family physicians, as did FPs who were international medical graduates (OR, 0.74), compared with those who trained in the United States, they said.
“Female gender was associated with seeing pediatric patients in a prior study using 2006-2009 [American Board of Family Medicine] data; however, we found no such association in 2017-2018,” Ms. Jetty and associates noted.
“Many diverse drivers likely influence the findings we observed, including organizational, personal, social, and economic factors,” they wrote, suggesting that the policies of some HMOs “may limit scope of practice for employed physicians,” while those who practice in areas of low pediatrician density might “capitalize on a market opportunity ... more than physicians in pediatrician-saturated areas with greater competition for young patients.”
The overall shortage of primary pediatric care may be a matter of debate, the investigators said, but “there is undoubtedly significant variability in the regional supply of pediatric primary care physicians and thus areas where family physicians are needed to meet current pediatric workforce demand.”
The authors reported no conflicts.
according to new research.
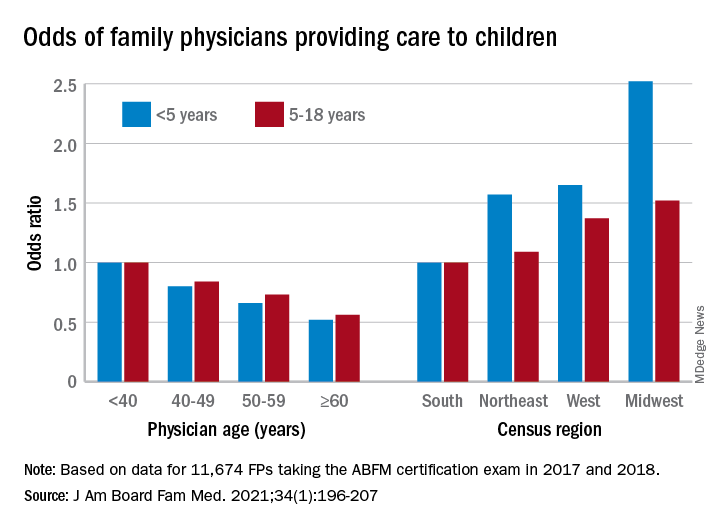
This the latest sign of a long-term decline, and it “poses a broader concern for a specialty that defines itself by its comprehensive scope of practice,” said the study investigators of the Robert Graham Center in Washington, D.C., in a written statement. “This is consistent with previous Robert Graham Center research that reported a similar steady decline from 1992 to 2002.”
Self-reported data from family physicians indicate that 84.3% cared for children aged 18 years and under in 2017, compared with 83.0% in 2018, based on a cross-sectional analysis of data gathered from 11,674 family physicians who completed the practice demographic questionnaire attached to the American Board of Family Medicine’s certification exam in 2017 and 2018.
“This current trend is unsettling, because family physicians provide the majority of pediatric care in rural and pediatrically underserved areas of the United States,” study author Anuradha Jetty, MPH, and coauthors said in the statement.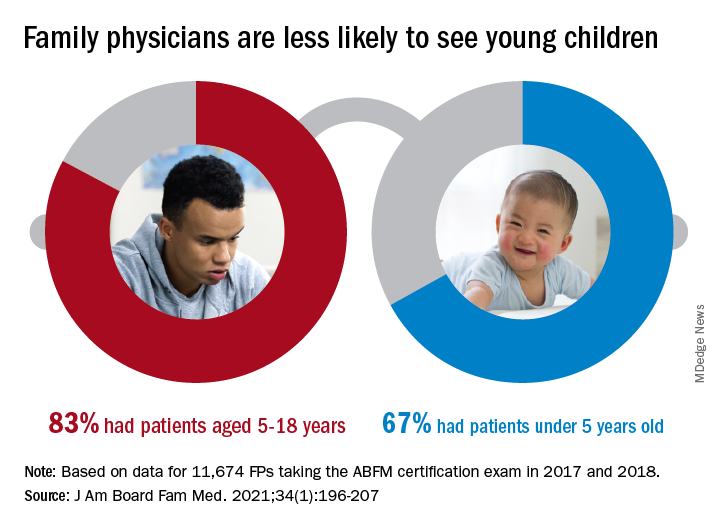
The analysis also offers a snapshot of the current state of pediatric care offered by family physicians. In 2017 and 2018, FPs were more likely to see patients aged 5-18 years than those under age 5 (83.0% vs. 67.0%), with variation by age, location, and race/ethnicity, said Ms. Jetty and colleagues, in their new paper.
FPs aged 60 years and older were much less likely to see pediatric patients, compared with those under age 40: odds ratios were 0.52 for children under 5 and 0.56 for children 5-18. Regional variation was even more pronounced: Compared with their colleagues in the Southern states, Midwestern FPs were 1.52 times as likely to treat children aged 5-18 and 2.52 times as likely to treat children under age 5, the investigators reported.
Non-Hispanic Asian and Hispanic family physicians had significantly lower odds of seeing pediatric patients, relative to non-Hispanic White family physicians, as did FPs who were international medical graduates (OR, 0.74), compared with those who trained in the United States, they said.
“Female gender was associated with seeing pediatric patients in a prior study using 2006-2009 [American Board of Family Medicine] data; however, we found no such association in 2017-2018,” Ms. Jetty and associates noted.
“Many diverse drivers likely influence the findings we observed, including organizational, personal, social, and economic factors,” they wrote, suggesting that the policies of some HMOs “may limit scope of practice for employed physicians,” while those who practice in areas of low pediatrician density might “capitalize on a market opportunity ... more than physicians in pediatrician-saturated areas with greater competition for young patients.”
The overall shortage of primary pediatric care may be a matter of debate, the investigators said, but “there is undoubtedly significant variability in the regional supply of pediatric primary care physicians and thus areas where family physicians are needed to meet current pediatric workforce demand.”
The authors reported no conflicts.
according to new research.
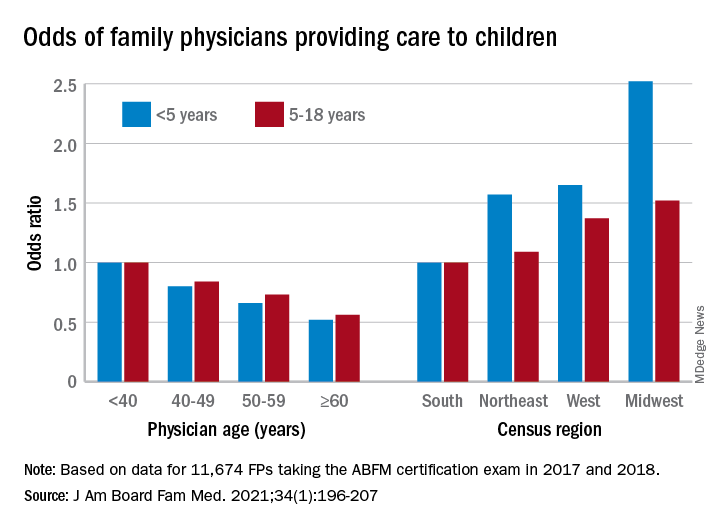
This the latest sign of a long-term decline, and it “poses a broader concern for a specialty that defines itself by its comprehensive scope of practice,” said the study investigators of the Robert Graham Center in Washington, D.C., in a written statement. “This is consistent with previous Robert Graham Center research that reported a similar steady decline from 1992 to 2002.”
Self-reported data from family physicians indicate that 84.3% cared for children aged 18 years and under in 2017, compared with 83.0% in 2018, based on a cross-sectional analysis of data gathered from 11,674 family physicians who completed the practice demographic questionnaire attached to the American Board of Family Medicine’s certification exam in 2017 and 2018.
“This current trend is unsettling, because family physicians provide the majority of pediatric care in rural and pediatrically underserved areas of the United States,” study author Anuradha Jetty, MPH, and coauthors said in the statement.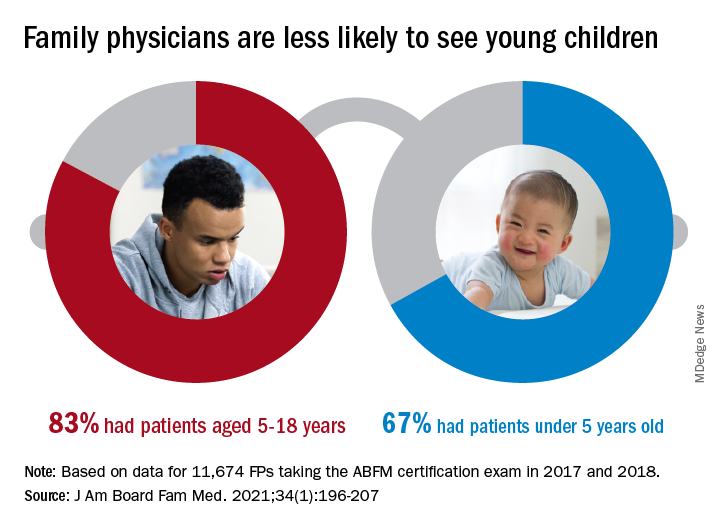
The analysis also offers a snapshot of the current state of pediatric care offered by family physicians. In 2017 and 2018, FPs were more likely to see patients aged 5-18 years than those under age 5 (83.0% vs. 67.0%), with variation by age, location, and race/ethnicity, said Ms. Jetty and colleagues, in their new paper.
FPs aged 60 years and older were much less likely to see pediatric patients, compared with those under age 40: odds ratios were 0.52 for children under 5 and 0.56 for children 5-18. Regional variation was even more pronounced: Compared with their colleagues in the Southern states, Midwestern FPs were 1.52 times as likely to treat children aged 5-18 and 2.52 times as likely to treat children under age 5, the investigators reported.
Non-Hispanic Asian and Hispanic family physicians had significantly lower odds of seeing pediatric patients, relative to non-Hispanic White family physicians, as did FPs who were international medical graduates (OR, 0.74), compared with those who trained in the United States, they said.
“Female gender was associated with seeing pediatric patients in a prior study using 2006-2009 [American Board of Family Medicine] data; however, we found no such association in 2017-2018,” Ms. Jetty and associates noted.
“Many diverse drivers likely influence the findings we observed, including organizational, personal, social, and economic factors,” they wrote, suggesting that the policies of some HMOs “may limit scope of practice for employed physicians,” while those who practice in areas of low pediatrician density might “capitalize on a market opportunity ... more than physicians in pediatrician-saturated areas with greater competition for young patients.”
The overall shortage of primary pediatric care may be a matter of debate, the investigators said, but “there is undoubtedly significant variability in the regional supply of pediatric primary care physicians and thus areas where family physicians are needed to meet current pediatric workforce demand.”
The authors reported no conflicts.
FROM THE JOURNAL OF THE AMERICAN BOARD OF FAMILY MEDICINE
AAD announces diversity initiatives
not only within the academy itself, but also in the profession of dermatology overall.
“Last year’s events surrounding social justice issues and the disproportionate impact of COVID-19 on minority communities underscored an urgent need for the academy to outline a strategy to address gaps in diversity, equity, and inclusion across the academy’s programs, provide better access to dermatologic care, and expand the pipeline for prospective dermatologists,” according to an AAD statement introducing the plan.
“The AAD has long recognized the importance of fostering diversity in the dermatology specialty and increasing dermatologic services to underserved populations as a key strategic goal,” Kanya Ferguson, MD, chair of the AAD’s diversity committee, said in an interview.
“The importance and urgency of furthering these goals have been underscored by the social justice events of 2020 and the disproportionate impact that COVID-19 has had, specifically on Black and Latino communities,” added Dr. Ferguson, of the department of dermatology, at the University of Iowa, Iowa City. “The 3-year plan comprehensively expands current diversity, equity, and inclusion initiatives in an effort to accelerate the Academy’s progress toward its strategic goals.”
“Numerous barriers persist that contribute to the narrowing pipeline in medicine and ultimately in dermatology,” Dr. Ferguson noted. “The AAD’s diversity, equity, and inclusion initiatives, toolkits, and resources aim to address some of these barriers through early exposure, pipeline programming, and mentorship.”
As for the next steps, “the diversity committee will be working hard over the next few years to coordinate the integration and adoption of initiatives throughout the Academy’s activities,” she added. “This work will take a significant amount of collaboration and the committee is excited to move this forward in a meaningful and sustainable way.”
The AAD’s diversity committee headed the development of the plan, unanimously approved by the AAD’s board of directors, which outlines four key goals for the next 3 years, presented in the Diversity in Dermatology plan as follows:
“Promote and facilitate diversity, equity, and inclusion within the AAD.” Steps toward this goal include facilitating diverse representation on AAD committees, councils, and task forces, increasing representation of skin of color session speakers and lecture topics at Academy meetings, and ensuring equity in the selection process for awards including the Leadership Forum, Academic Dermatology Leadership Program, Advanced Leadership Forum, Journal of the AAD Editorial Mentorship Program, and other leadership activities.
- “Ensure dermatologic education and research encompasses health disparities and skin of color, and advocate for Black and Latino patient representation in research.” Steps toward this goal include increasing use of images reflecting the full spectrum of skin types, ensuring that skin of color populations receive information about dermatologic diseases, and supporting underrepresented minority (URM) dermatology physician scientists in leadership and professional development.
- “Expand Academy’s Advocacy Priorities to prioritize addressing health inequities.” Steps toward this goal include prioritizing issues that affect minority and marginalized populations, establishing relationships with relevant congressional leadership, and advocating for patient support groups for diseases that disproportionately impact skin of color patients.
- “Increase the number of practicing dermatologists who are underrepresented minorities and provide leadership and professional development programming.” Steps toward this goal include expanding the AAD mentorship program to include physician scientists, expanding diversity champion programs, expanding outreach to URM college students in STEM majors, and launching an AAD Summer Diversity & Inclusion camp for younger students to promote interest in a medical career.
The AAD diversity committee also has assembled a toolkit of resources designed to help its members learn how to talk about race, be an effective ally, and achieve cultural competency. Additional updated resources include guidelines on mentorship and outreach.
not only within the academy itself, but also in the profession of dermatology overall.
“Last year’s events surrounding social justice issues and the disproportionate impact of COVID-19 on minority communities underscored an urgent need for the academy to outline a strategy to address gaps in diversity, equity, and inclusion across the academy’s programs, provide better access to dermatologic care, and expand the pipeline for prospective dermatologists,” according to an AAD statement introducing the plan.
“The AAD has long recognized the importance of fostering diversity in the dermatology specialty and increasing dermatologic services to underserved populations as a key strategic goal,” Kanya Ferguson, MD, chair of the AAD’s diversity committee, said in an interview.
“The importance and urgency of furthering these goals have been underscored by the social justice events of 2020 and the disproportionate impact that COVID-19 has had, specifically on Black and Latino communities,” added Dr. Ferguson, of the department of dermatology, at the University of Iowa, Iowa City. “The 3-year plan comprehensively expands current diversity, equity, and inclusion initiatives in an effort to accelerate the Academy’s progress toward its strategic goals.”
“Numerous barriers persist that contribute to the narrowing pipeline in medicine and ultimately in dermatology,” Dr. Ferguson noted. “The AAD’s diversity, equity, and inclusion initiatives, toolkits, and resources aim to address some of these barriers through early exposure, pipeline programming, and mentorship.”
As for the next steps, “the diversity committee will be working hard over the next few years to coordinate the integration and adoption of initiatives throughout the Academy’s activities,” she added. “This work will take a significant amount of collaboration and the committee is excited to move this forward in a meaningful and sustainable way.”
The AAD’s diversity committee headed the development of the plan, unanimously approved by the AAD’s board of directors, which outlines four key goals for the next 3 years, presented in the Diversity in Dermatology plan as follows:
“Promote and facilitate diversity, equity, and inclusion within the AAD.” Steps toward this goal include facilitating diverse representation on AAD committees, councils, and task forces, increasing representation of skin of color session speakers and lecture topics at Academy meetings, and ensuring equity in the selection process for awards including the Leadership Forum, Academic Dermatology Leadership Program, Advanced Leadership Forum, Journal of the AAD Editorial Mentorship Program, and other leadership activities.
- “Ensure dermatologic education and research encompasses health disparities and skin of color, and advocate for Black and Latino patient representation in research.” Steps toward this goal include increasing use of images reflecting the full spectrum of skin types, ensuring that skin of color populations receive information about dermatologic diseases, and supporting underrepresented minority (URM) dermatology physician scientists in leadership and professional development.
- “Expand Academy’s Advocacy Priorities to prioritize addressing health inequities.” Steps toward this goal include prioritizing issues that affect minority and marginalized populations, establishing relationships with relevant congressional leadership, and advocating for patient support groups for diseases that disproportionately impact skin of color patients.
- “Increase the number of practicing dermatologists who are underrepresented minorities and provide leadership and professional development programming.” Steps toward this goal include expanding the AAD mentorship program to include physician scientists, expanding diversity champion programs, expanding outreach to URM college students in STEM majors, and launching an AAD Summer Diversity & Inclusion camp for younger students to promote interest in a medical career.
The AAD diversity committee also has assembled a toolkit of resources designed to help its members learn how to talk about race, be an effective ally, and achieve cultural competency. Additional updated resources include guidelines on mentorship and outreach.
not only within the academy itself, but also in the profession of dermatology overall.
“Last year’s events surrounding social justice issues and the disproportionate impact of COVID-19 on minority communities underscored an urgent need for the academy to outline a strategy to address gaps in diversity, equity, and inclusion across the academy’s programs, provide better access to dermatologic care, and expand the pipeline for prospective dermatologists,” according to an AAD statement introducing the plan.
“The AAD has long recognized the importance of fostering diversity in the dermatology specialty and increasing dermatologic services to underserved populations as a key strategic goal,” Kanya Ferguson, MD, chair of the AAD’s diversity committee, said in an interview.
“The importance and urgency of furthering these goals have been underscored by the social justice events of 2020 and the disproportionate impact that COVID-19 has had, specifically on Black and Latino communities,” added Dr. Ferguson, of the department of dermatology, at the University of Iowa, Iowa City. “The 3-year plan comprehensively expands current diversity, equity, and inclusion initiatives in an effort to accelerate the Academy’s progress toward its strategic goals.”
“Numerous barriers persist that contribute to the narrowing pipeline in medicine and ultimately in dermatology,” Dr. Ferguson noted. “The AAD’s diversity, equity, and inclusion initiatives, toolkits, and resources aim to address some of these barriers through early exposure, pipeline programming, and mentorship.”
As for the next steps, “the diversity committee will be working hard over the next few years to coordinate the integration and adoption of initiatives throughout the Academy’s activities,” she added. “This work will take a significant amount of collaboration and the committee is excited to move this forward in a meaningful and sustainable way.”
The AAD’s diversity committee headed the development of the plan, unanimously approved by the AAD’s board of directors, which outlines four key goals for the next 3 years, presented in the Diversity in Dermatology plan as follows:
“Promote and facilitate diversity, equity, and inclusion within the AAD.” Steps toward this goal include facilitating diverse representation on AAD committees, councils, and task forces, increasing representation of skin of color session speakers and lecture topics at Academy meetings, and ensuring equity in the selection process for awards including the Leadership Forum, Academic Dermatology Leadership Program, Advanced Leadership Forum, Journal of the AAD Editorial Mentorship Program, and other leadership activities.
- “Ensure dermatologic education and research encompasses health disparities and skin of color, and advocate for Black and Latino patient representation in research.” Steps toward this goal include increasing use of images reflecting the full spectrum of skin types, ensuring that skin of color populations receive information about dermatologic diseases, and supporting underrepresented minority (URM) dermatology physician scientists in leadership and professional development.
- “Expand Academy’s Advocacy Priorities to prioritize addressing health inequities.” Steps toward this goal include prioritizing issues that affect minority and marginalized populations, establishing relationships with relevant congressional leadership, and advocating for patient support groups for diseases that disproportionately impact skin of color patients.
- “Increase the number of practicing dermatologists who are underrepresented minorities and provide leadership and professional development programming.” Steps toward this goal include expanding the AAD mentorship program to include physician scientists, expanding diversity champion programs, expanding outreach to URM college students in STEM majors, and launching an AAD Summer Diversity & Inclusion camp for younger students to promote interest in a medical career.
The AAD diversity committee also has assembled a toolkit of resources designed to help its members learn how to talk about race, be an effective ally, and achieve cultural competency. Additional updated resources include guidelines on mentorship and outreach.
Don’t fear patients reading their clinical notes: Opinion
Doctors are learning about new rules coming this April that encourage open and transparent communication among patients, families, and clinicians. The rules, putting into effect the bipartisan 21st Century Cures Act, mandate offering patients access to notes (“open notes”) written by clinicians in electronic medical records.
A recent article from this news organization noted that for many doctors this represents both a sudden and troubling change in practice. For others, the rules codify what they have been doing as a matter of routine for a decade. Spurred by the OpenNotes movement, at least 55 million Americans are already offered access to their clinical notes, including, since 2013, more than 9 million veterans with access to the Blue Button function in Veterans Affairs practices and hospitals.
The practice is spreading beyond the United States to other countries, including Canada, Sweden, Norway, Estonia, and the United Kingdom.
In this commentary, we review what patients, clinicians, and policymakers have been learning about open notes.
The patient experience
What do patients experience? In a survey of more than 22,000 patients who read notes in three diverse health systems, more than 90% reported having a good grasp of what their doctors and other clinicians had written, and very few (3%) reported being very confused by what they read. About two-thirds described reading their notes as very important for taking care of their health, remembering details of their visits and their care plans, and understanding why a medication was prescribed.
Indeed, in a clinically exciting finding, 14% of survey respondents reported that reading their notes made them more likely to take their medications as their doctors wished. With about half of Americans with chronic illness failing to take their medicines as prescribed, which sometimes leads to compromised outcomes and associated unnecessary costs (estimated at $300 billion annually), these reports of increased adherence should be taken very seriously.
Some doctors anticipate that open notes will erode patient communication. A growing body of research reveals just the opposite. In multiple surveys, patients describe open notes as “extending the visit,” strengthening collaboration and teamwork with their doctor. Quite possibly, the invitation to read notes may in itself increase trust. Such benefits appear especially pronounced among patients who are older, less educated, are persons of color or Hispanic, or who do not speak English at home.
And in several studies, more than a third of patients also report sharing their notes with others, with older and chronically ill patients in particular sharing access with family and friends who are their care partners.
On the other hand, a small minority of patients (5%) do report being more worried by what they read. It’s unknown whether this is because they are better informed about their care or because baseline anxiety levels increase. Doctors expect also that some patients, particularly those with cancer or serious mental illness, will be upset by their notes. So far, evidence does not support that specific concern.
Conversely, withholding, delaying, or blocking notes may be a source of anxiety or even stigmatization. When clinicians find themselves worried about sharing notes, we suggest that they discuss with their patients the benefits and risks. Recall also that transparency facilitates freedom of choice; patients make their own decision, and quite a few choose to leave notes unread.
Finding mistakes early and preventing harm are important goals for health care, and open notes can make care safer. Inevitably, medical records contain errors, omissions, and inaccuracies. In a large patient survey, 21% reported finding an error in their notes, and 42% perceived the error to be serious.
Moreover, 25% of doctors with more than a year’s experience with open notes reported patients finding errors that they (the doctors) considered “serious.” In 2015, the National Academy of Medicine cited open notes as a mechanism for improving diagnostic accuracy. In regard to possible legal action from patients, most attorneys, patients, and doctors agree that more transparent communication will build trust overall and, if anything, diminish litigation. We know of no instances so far of lawsuits deriving from open notes.
The physician experience
Doctors may worry that open notes will impede workflow, that they will be compelled to “dumb down” their documentation to avoid causing offense or anxiety, and that patients will demand changes to what is written. Here, extensive survey research should allay such fears and expectations. In a survey of more than 1,600 clinicians with at least 1 year of experience with open notes, reports of disruption to workflow were uncommon.
Most doctors (84%) reported that patients contacted them with questions about their notes “less than monthly or never.” Approximately two-thirds (62%) reported spending the same amount of time writing visit notes.
After implementing open notes, many doctors do report being more mindful about their documentation. For example, 41% reported changing how they used language such as “patient denies” or “noncompliant,” and 18% reported changing their use of medical jargon or abbreviations. Might these changes undermine the utility of medical notes? A majority of doctors surveyed (78%) said no, reporting that, after implementing open notes, the value of their documentation was the same or better.
Innovations spotlight difficult and often longstanding challenges. Open notes highlight the complex role of medical records in preserving privacy, especially in the spectrum of abuse, whether domestic or involving elders, children or sexual transgressions. For families with adolescents, issues concerning confidentiality can become a two-way street, and federal and state rules at times provide conflicting and idiosyncratic guidance. It is important to emphasize that the new rules permit information blocking if there is clear evidence that doing so “will substantially reduce the risk of harm” to patients or to other third parties.
Perhaps think of open notes as a new medicine designed to help the vast majority of those who use it but with side effects and even contraindications for a few. Doctors can step in to minimize risks to vulnerable individuals, and imaginative and creative solutions to complex issues may emerge. In a growing number of practices serving adolescents, clinicians can now create two notes, with some elements of care visible on a patient portal and others held privately or visible only to the adolescent.
The shared experience
Overall, when it comes to documenting sensitive social information, open notes may act as a useful catalyst prompting deeper discussion about personal details clinically important to record, as opposed to those perhaps best left unwritten.
The implementation of open notes nationwide calls for exciting explorations. How can transparent systems maximize benefits for targeted populations in diverse settings? For patients with mental illness, can notes become part of the therapy? Given that care partners often report more benefit from reading notes than do patients themselves, how can they be mobilized to maximize their contributions to those acutely ill on hospital floors, or to family members with Alzheimer’s or in long-term care facilities?
How can we harness emerging technologies to translate notes and medical records into other languages or support lower literacy levels, while preserving the clinical detail in the notes? Should patients contribute to their own notes, cogenerating them with their clinicians? Experiments for “OurNotes” interventions are underway, and early reports from both patients and doctors hold considerable promise.
Ownership of medical records is evolving. Once firmly held by clinicians, electronic technologies have rapidly led to what may best be viewed currently as joint ownership by clinicians and patients. As apps evolve further and issues with interoperability of records diminish, it is likely that patients will eventually take control. Then it will be up to patients what to carry in their records. Clinicians will advise, but patients will decide.
The new rules herald clear changes in the fabric of care, and after a decade of study we anticipate that the benefits well outweigh the harms. But in the short run, it’s wrong to predict an avalanche. Two decades ago, when patient portals first revealed laboratory test findings to patients, doctors expected cataclysmic change in their practices. It did not occur. The vast majority of patients who registered on portals benefited and few disturbed their doctors.
Similarly, after notes were first unblinded by the OpenNotes research teams, the question we were asked most commonly by the primary care doctors who volunteered was whether the computers were actually displaying their notes. Even though many patients read them carefully, the doctors heard little from them. Clinicians have now reported the same experience in several subsequent studies.
Patients are resourceful, turning quickly to friends or the Internet for answers to their questions. They know how busy doctors are and don’t want to bother them if at all possible. When notes do trigger questions, the time taken to respond is probably offset by silence from other patients finding answers to their own questions in notes they read.
We believe that clinicians should embrace the spirit of the rules and also view them as HIPAA catching up with a computerized universe. As the new practice takes hold, ambiguities will diminish as further experience and research evolve. Warner V. Slack, MD, the first doctor to ask patients to talk to computers, opined that patients are the “largest and least utilized resource in health care.” Open and transparent communication through electronic medical records may mobilize patients (and their families) far more effectively. Patients will almost certainly benefit. Remembering Dr. Slack’s prophecy, we believe that clinicians will too.
A version of this article first appeared on Medscape.com.
Doctors are learning about new rules coming this April that encourage open and transparent communication among patients, families, and clinicians. The rules, putting into effect the bipartisan 21st Century Cures Act, mandate offering patients access to notes (“open notes”) written by clinicians in electronic medical records.
A recent article from this news organization noted that for many doctors this represents both a sudden and troubling change in practice. For others, the rules codify what they have been doing as a matter of routine for a decade. Spurred by the OpenNotes movement, at least 55 million Americans are already offered access to their clinical notes, including, since 2013, more than 9 million veterans with access to the Blue Button function in Veterans Affairs practices and hospitals.
The practice is spreading beyond the United States to other countries, including Canada, Sweden, Norway, Estonia, and the United Kingdom.
In this commentary, we review what patients, clinicians, and policymakers have been learning about open notes.
The patient experience
What do patients experience? In a survey of more than 22,000 patients who read notes in three diverse health systems, more than 90% reported having a good grasp of what their doctors and other clinicians had written, and very few (3%) reported being very confused by what they read. About two-thirds described reading their notes as very important for taking care of their health, remembering details of their visits and their care plans, and understanding why a medication was prescribed.
Indeed, in a clinically exciting finding, 14% of survey respondents reported that reading their notes made them more likely to take their medications as their doctors wished. With about half of Americans with chronic illness failing to take their medicines as prescribed, which sometimes leads to compromised outcomes and associated unnecessary costs (estimated at $300 billion annually), these reports of increased adherence should be taken very seriously.
Some doctors anticipate that open notes will erode patient communication. A growing body of research reveals just the opposite. In multiple surveys, patients describe open notes as “extending the visit,” strengthening collaboration and teamwork with their doctor. Quite possibly, the invitation to read notes may in itself increase trust. Such benefits appear especially pronounced among patients who are older, less educated, are persons of color or Hispanic, or who do not speak English at home.
And in several studies, more than a third of patients also report sharing their notes with others, with older and chronically ill patients in particular sharing access with family and friends who are their care partners.
On the other hand, a small minority of patients (5%) do report being more worried by what they read. It’s unknown whether this is because they are better informed about their care or because baseline anxiety levels increase. Doctors expect also that some patients, particularly those with cancer or serious mental illness, will be upset by their notes. So far, evidence does not support that specific concern.
Conversely, withholding, delaying, or blocking notes may be a source of anxiety or even stigmatization. When clinicians find themselves worried about sharing notes, we suggest that they discuss with their patients the benefits and risks. Recall also that transparency facilitates freedom of choice; patients make their own decision, and quite a few choose to leave notes unread.
Finding mistakes early and preventing harm are important goals for health care, and open notes can make care safer. Inevitably, medical records contain errors, omissions, and inaccuracies. In a large patient survey, 21% reported finding an error in their notes, and 42% perceived the error to be serious.
Moreover, 25% of doctors with more than a year’s experience with open notes reported patients finding errors that they (the doctors) considered “serious.” In 2015, the National Academy of Medicine cited open notes as a mechanism for improving diagnostic accuracy. In regard to possible legal action from patients, most attorneys, patients, and doctors agree that more transparent communication will build trust overall and, if anything, diminish litigation. We know of no instances so far of lawsuits deriving from open notes.
The physician experience
Doctors may worry that open notes will impede workflow, that they will be compelled to “dumb down” their documentation to avoid causing offense or anxiety, and that patients will demand changes to what is written. Here, extensive survey research should allay such fears and expectations. In a survey of more than 1,600 clinicians with at least 1 year of experience with open notes, reports of disruption to workflow were uncommon.
Most doctors (84%) reported that patients contacted them with questions about their notes “less than monthly or never.” Approximately two-thirds (62%) reported spending the same amount of time writing visit notes.
After implementing open notes, many doctors do report being more mindful about their documentation. For example, 41% reported changing how they used language such as “patient denies” or “noncompliant,” and 18% reported changing their use of medical jargon or abbreviations. Might these changes undermine the utility of medical notes? A majority of doctors surveyed (78%) said no, reporting that, after implementing open notes, the value of their documentation was the same or better.
Innovations spotlight difficult and often longstanding challenges. Open notes highlight the complex role of medical records in preserving privacy, especially in the spectrum of abuse, whether domestic or involving elders, children or sexual transgressions. For families with adolescents, issues concerning confidentiality can become a two-way street, and federal and state rules at times provide conflicting and idiosyncratic guidance. It is important to emphasize that the new rules permit information blocking if there is clear evidence that doing so “will substantially reduce the risk of harm” to patients or to other third parties.
Perhaps think of open notes as a new medicine designed to help the vast majority of those who use it but with side effects and even contraindications for a few. Doctors can step in to minimize risks to vulnerable individuals, and imaginative and creative solutions to complex issues may emerge. In a growing number of practices serving adolescents, clinicians can now create two notes, with some elements of care visible on a patient portal and others held privately or visible only to the adolescent.
The shared experience
Overall, when it comes to documenting sensitive social information, open notes may act as a useful catalyst prompting deeper discussion about personal details clinically important to record, as opposed to those perhaps best left unwritten.
The implementation of open notes nationwide calls for exciting explorations. How can transparent systems maximize benefits for targeted populations in diverse settings? For patients with mental illness, can notes become part of the therapy? Given that care partners often report more benefit from reading notes than do patients themselves, how can they be mobilized to maximize their contributions to those acutely ill on hospital floors, or to family members with Alzheimer’s or in long-term care facilities?
How can we harness emerging technologies to translate notes and medical records into other languages or support lower literacy levels, while preserving the clinical detail in the notes? Should patients contribute to their own notes, cogenerating them with their clinicians? Experiments for “OurNotes” interventions are underway, and early reports from both patients and doctors hold considerable promise.
Ownership of medical records is evolving. Once firmly held by clinicians, electronic technologies have rapidly led to what may best be viewed currently as joint ownership by clinicians and patients. As apps evolve further and issues with interoperability of records diminish, it is likely that patients will eventually take control. Then it will be up to patients what to carry in their records. Clinicians will advise, but patients will decide.
The new rules herald clear changes in the fabric of care, and after a decade of study we anticipate that the benefits well outweigh the harms. But in the short run, it’s wrong to predict an avalanche. Two decades ago, when patient portals first revealed laboratory test findings to patients, doctors expected cataclysmic change in their practices. It did not occur. The vast majority of patients who registered on portals benefited and few disturbed their doctors.
Similarly, after notes were first unblinded by the OpenNotes research teams, the question we were asked most commonly by the primary care doctors who volunteered was whether the computers were actually displaying their notes. Even though many patients read them carefully, the doctors heard little from them. Clinicians have now reported the same experience in several subsequent studies.
Patients are resourceful, turning quickly to friends or the Internet for answers to their questions. They know how busy doctors are and don’t want to bother them if at all possible. When notes do trigger questions, the time taken to respond is probably offset by silence from other patients finding answers to their own questions in notes they read.
We believe that clinicians should embrace the spirit of the rules and also view them as HIPAA catching up with a computerized universe. As the new practice takes hold, ambiguities will diminish as further experience and research evolve. Warner V. Slack, MD, the first doctor to ask patients to talk to computers, opined that patients are the “largest and least utilized resource in health care.” Open and transparent communication through electronic medical records may mobilize patients (and their families) far more effectively. Patients will almost certainly benefit. Remembering Dr. Slack’s prophecy, we believe that clinicians will too.
A version of this article first appeared on Medscape.com.
Doctors are learning about new rules coming this April that encourage open and transparent communication among patients, families, and clinicians. The rules, putting into effect the bipartisan 21st Century Cures Act, mandate offering patients access to notes (“open notes”) written by clinicians in electronic medical records.
A recent article from this news organization noted that for many doctors this represents both a sudden and troubling change in practice. For others, the rules codify what they have been doing as a matter of routine for a decade. Spurred by the OpenNotes movement, at least 55 million Americans are already offered access to their clinical notes, including, since 2013, more than 9 million veterans with access to the Blue Button function in Veterans Affairs practices and hospitals.
The practice is spreading beyond the United States to other countries, including Canada, Sweden, Norway, Estonia, and the United Kingdom.
In this commentary, we review what patients, clinicians, and policymakers have been learning about open notes.
The patient experience
What do patients experience? In a survey of more than 22,000 patients who read notes in three diverse health systems, more than 90% reported having a good grasp of what their doctors and other clinicians had written, and very few (3%) reported being very confused by what they read. About two-thirds described reading their notes as very important for taking care of their health, remembering details of their visits and their care plans, and understanding why a medication was prescribed.
Indeed, in a clinically exciting finding, 14% of survey respondents reported that reading their notes made them more likely to take their medications as their doctors wished. With about half of Americans with chronic illness failing to take their medicines as prescribed, which sometimes leads to compromised outcomes and associated unnecessary costs (estimated at $300 billion annually), these reports of increased adherence should be taken very seriously.
Some doctors anticipate that open notes will erode patient communication. A growing body of research reveals just the opposite. In multiple surveys, patients describe open notes as “extending the visit,” strengthening collaboration and teamwork with their doctor. Quite possibly, the invitation to read notes may in itself increase trust. Such benefits appear especially pronounced among patients who are older, less educated, are persons of color or Hispanic, or who do not speak English at home.
And in several studies, more than a third of patients also report sharing their notes with others, with older and chronically ill patients in particular sharing access with family and friends who are their care partners.
On the other hand, a small minority of patients (5%) do report being more worried by what they read. It’s unknown whether this is because they are better informed about their care or because baseline anxiety levels increase. Doctors expect also that some patients, particularly those with cancer or serious mental illness, will be upset by their notes. So far, evidence does not support that specific concern.
Conversely, withholding, delaying, or blocking notes may be a source of anxiety or even stigmatization. When clinicians find themselves worried about sharing notes, we suggest that they discuss with their patients the benefits and risks. Recall also that transparency facilitates freedom of choice; patients make their own decision, and quite a few choose to leave notes unread.
Finding mistakes early and preventing harm are important goals for health care, and open notes can make care safer. Inevitably, medical records contain errors, omissions, and inaccuracies. In a large patient survey, 21% reported finding an error in their notes, and 42% perceived the error to be serious.
Moreover, 25% of doctors with more than a year’s experience with open notes reported patients finding errors that they (the doctors) considered “serious.” In 2015, the National Academy of Medicine cited open notes as a mechanism for improving diagnostic accuracy. In regard to possible legal action from patients, most attorneys, patients, and doctors agree that more transparent communication will build trust overall and, if anything, diminish litigation. We know of no instances so far of lawsuits deriving from open notes.
The physician experience
Doctors may worry that open notes will impede workflow, that they will be compelled to “dumb down” their documentation to avoid causing offense or anxiety, and that patients will demand changes to what is written. Here, extensive survey research should allay such fears and expectations. In a survey of more than 1,600 clinicians with at least 1 year of experience with open notes, reports of disruption to workflow were uncommon.
Most doctors (84%) reported that patients contacted them with questions about their notes “less than monthly or never.” Approximately two-thirds (62%) reported spending the same amount of time writing visit notes.
After implementing open notes, many doctors do report being more mindful about their documentation. For example, 41% reported changing how they used language such as “patient denies” or “noncompliant,” and 18% reported changing their use of medical jargon or abbreviations. Might these changes undermine the utility of medical notes? A majority of doctors surveyed (78%) said no, reporting that, after implementing open notes, the value of their documentation was the same or better.
Innovations spotlight difficult and often longstanding challenges. Open notes highlight the complex role of medical records in preserving privacy, especially in the spectrum of abuse, whether domestic or involving elders, children or sexual transgressions. For families with adolescents, issues concerning confidentiality can become a two-way street, and federal and state rules at times provide conflicting and idiosyncratic guidance. It is important to emphasize that the new rules permit information blocking if there is clear evidence that doing so “will substantially reduce the risk of harm” to patients or to other third parties.
Perhaps think of open notes as a new medicine designed to help the vast majority of those who use it but with side effects and even contraindications for a few. Doctors can step in to minimize risks to vulnerable individuals, and imaginative and creative solutions to complex issues may emerge. In a growing number of practices serving adolescents, clinicians can now create two notes, with some elements of care visible on a patient portal and others held privately or visible only to the adolescent.
The shared experience
Overall, when it comes to documenting sensitive social information, open notes may act as a useful catalyst prompting deeper discussion about personal details clinically important to record, as opposed to those perhaps best left unwritten.
The implementation of open notes nationwide calls for exciting explorations. How can transparent systems maximize benefits for targeted populations in diverse settings? For patients with mental illness, can notes become part of the therapy? Given that care partners often report more benefit from reading notes than do patients themselves, how can they be mobilized to maximize their contributions to those acutely ill on hospital floors, or to family members with Alzheimer’s or in long-term care facilities?
How can we harness emerging technologies to translate notes and medical records into other languages or support lower literacy levels, while preserving the clinical detail in the notes? Should patients contribute to their own notes, cogenerating them with their clinicians? Experiments for “OurNotes” interventions are underway, and early reports from both patients and doctors hold considerable promise.
Ownership of medical records is evolving. Once firmly held by clinicians, electronic technologies have rapidly led to what may best be viewed currently as joint ownership by clinicians and patients. As apps evolve further and issues with interoperability of records diminish, it is likely that patients will eventually take control. Then it will be up to patients what to carry in their records. Clinicians will advise, but patients will decide.
The new rules herald clear changes in the fabric of care, and after a decade of study we anticipate that the benefits well outweigh the harms. But in the short run, it’s wrong to predict an avalanche. Two decades ago, when patient portals first revealed laboratory test findings to patients, doctors expected cataclysmic change in their practices. It did not occur. The vast majority of patients who registered on portals benefited and few disturbed their doctors.
Similarly, after notes were first unblinded by the OpenNotes research teams, the question we were asked most commonly by the primary care doctors who volunteered was whether the computers were actually displaying their notes. Even though many patients read them carefully, the doctors heard little from them. Clinicians have now reported the same experience in several subsequent studies.
Patients are resourceful, turning quickly to friends or the Internet for answers to their questions. They know how busy doctors are and don’t want to bother them if at all possible. When notes do trigger questions, the time taken to respond is probably offset by silence from other patients finding answers to their own questions in notes they read.
We believe that clinicians should embrace the spirit of the rules and also view them as HIPAA catching up with a computerized universe. As the new practice takes hold, ambiguities will diminish as further experience and research evolve. Warner V. Slack, MD, the first doctor to ask patients to talk to computers, opined that patients are the “largest and least utilized resource in health care.” Open and transparent communication through electronic medical records may mobilize patients (and their families) far more effectively. Patients will almost certainly benefit. Remembering Dr. Slack’s prophecy, we believe that clinicians will too.
A version of this article first appeared on Medscape.com.