User login
Technology for primary care — terrific, terrifying, or both?
We have all been using technology in our primary care practices for a long time but newer formats have been emerging so fast that our minds, much less our staff’s minds, may be spinning.
Our old friend the telephone, a time-soaking nemesis for scheduling, checking coverage, questions calls, prescribing, quick consults, and follow-up is being replaced by EHR portals and SMS for messaging (e.g. DoctorConnect, SimplePractice), drop-in televisits and patient education links on our websites (e.g. Schmitt Pediatric Care, Remedy Connect), and chatbots for scheduling (e.g. CHEC-UP). While time is saved, what is lost may be hearing the subtext of anxiety or misperceptions in parents’ voices that would change our advice and the empathetic human connection in conversations with our patients. A hybrid approach may be better.
The paper appointment book has been replaced by scheduling systems sometimes lacking in flexibility for double booking, sibling visits, and variable length or extremely valuable multi-professional visits. Allowing patients to book their own visits may place complex problems in inappropriate slots, so only allowing online requests for visits is safer. On the other hand, many of us can now squeeze in “same day” televisits (e.g. Blueberry Pediatrics), sometimes from outside our practice (e.g., zocdoc), to increase payments and even entice new patients to enroll.
Amazing advances in technology are being made in specialty care such as genetic modifications (CRISPR), immunotherapies (mRNA vaccines and AI drug design), robot-assisted surgery, and 3-D printing of body parts and prosthetics. Technology as treatment such as transcranial magnetic stimulation and vagal stimulation are finding value in psychiatry.
But beside being aware of and able to order such specialty technologies, innovations are now extending our senses in primary care such as amplified or visual stethoscopes, bedside ultrasound (e.g. Butterfly), remote visualization (oto-, endo-)scopes, photographic vision screens (e.g. iScreen) for skin lesion (VisualDx) and genetic syndrome facial recognition. We need to be sure that technologies are tested and calibrated for children and different racial groups and genders to provide safe and equitable care. Early adoption may not always be the best approach. Costs of technology, as usual, may limit access to these advanced care aids especially, as usual, in practices serving low income and rural communities.
Patients, especially younger parents and youth, now expect to participate and can directly benefit from technology as part of their health care. Validated parent or self-report screens (e.g. EHRs, Phreesia) can detect important issues early for more effective intervention. Such questionnaires typically provide a pass/fail result or score, but other delivery systems (e.g. CHADIS) include interpretation, assist patients/parents in setting visit priorities and health goals, and even chain results of one questionnaire to secondary screens to hone in on problems, sometimes obviating a time-consuming second visit. Patient-completed comprehensive questionnaires (e.g. Well Visit Planner, CHADIS) allow us time to use our skills to focus on concerns, education, and management rather than asking myriad routine questions. Some (e.g. CHADIS) even create visit documentation reducing our “pajama time” write ups (and burnout); automate repeated online measures to track progress; and use questionnaire results to trigger related patient-specific education and resources rather than the often-ignored generic EHR handouts.
Digital therapeutics such as apps for anxiety (e.g. Calm), depression (e.g. SparkRx, Cass), weight control (e.g. Noom, Lose it), fitness, or sleep tracking (e.g. Whoop) help educate and, in some cases, provide real-time feedback to personalize discovery of contributing factors in order to maintain motivation for positive health behavior change. Some video games improve ADHD symptoms (e.g. EndeavorRX). Virtual reality scenarios have been shown to desensitize those with PTSD and social anxiety or teach social skills to children with autism.
Systems that trigger resource listings (including apps) from screen results can help, but now with over 10,000 apps for mental health, knowing what to recommend for what conditions is a challenge for which ratings (e.g. MINDapps.org) can help. With few product reps visiting to tell us what’s new, we need to read critically about innovations, search the web, subscribe to the AAP SOAPM LISTSERV, visit exhibitors at professional meetings, and talk with peers.
All the digital data collected from health care technology, if assembled with privacy constraints and analyzed with advanced statistical methods, have the possibility, with or without inclusion of genomic data, to allow for more accurate diagnostic and treatment decision support. While AI can search widely for patterns, it needs to be “trained” on appropriate data to make correct conclusions. We are all aware that the history determines 85% of both diagnosis and treatment decisions, particularly in primary care where x-rays or lab tests are not often needed.
But history in EHR notes is often idiosyncratic, entered hours after the visit by the clinician, and does not include the information needed to define diagnostic or guideline criteria, even if the clinician knows and considered those criteria. EHR templates are presented blank and are onerous and time consuming for clinicians. In addition, individual patient barriers to care, preferences, and environmental or subjective concerns are infrequently documented even though they may make the biggest difference to adherence and/or outcomes.
Notes made from voice to text digital AI translation of the encounter (e.g. Nuance DAX) are even less likely to include diagnostic criteria as it would be inappropriate to speak these. To use EHR history data to train AI and to test efficacy of care using variations of guidelines, guideline-related data is needed from online patient entries in questionnaires that are transformed to fill in templates along with some structured choices for clinician entries forming visit notes (e.g. CHADIS). New apps to facilitate clinician documentation of guidelines (e.g. AvoMD) could streamline visits as well as help document guideline criteria. The resulting combination of guideline-relevant patient histories and objective data to test and iteratively refine guidelines will allow a process known as a “Learning Health System.”
Technology to collect this kind of data can allow for the aspirational American Academy of Pediatrics CHILD Registry to approach this goal. Population-level data can provide surveillance for illness, toxins, effects of climate change, social drivers of health, and even effects of technologies themselves such as social media and remote learning so that we can attempt to make the best choices for the future.
Clinicians, staff, and patients will need to develop trust in technology as it infiltrates all aspects of health care. Professionals need both evidence and experience to trust a technology, which takes time and effort. Disinformation in the media may reduce trust or evoke unwarranted trust, as we have all seen regarding vaccines. Clear and coherent public health messaging can help but is no longer a panacea for developing trust in health care. Our nonjudgmental listening and informed opinions are needed more than ever.
The biggest issues for new technology are likely to be the need for workflow adjustments, changing our habit patterns, training, and cost/benefit analyses. With today’s high staff churn, confusion and even chaos can ensue when adopting new technology.
Staff need to be part of the selection process, if at all possible, and discuss how roles and flow will need to change. Having one staff member be a champion and expert for new tech can move adoption to a shared process rather than imposing “one more thing.” It is crucial to discuss the benefits for patients and staff even if the change is required. Sometimes cost savings can include a bonus for staff or free group lunches. Providing a certificate of achievement or title promotion for mastering new tech may be appropriate. Giving some time off from other tasks to learn new workflows can reduce resistance rather than just adding it on to a regular workload. Office “huddles” going forward can include examples of benefits staff have observed or heard about from the adoption. There are quality improvement processes that engage the team — some that earn MOC-4 or CEU credits — that apply to making workflow changes and measuring them iteratively.
If technology takes over important aspects of the work of medical professionals, even if it is faster and/or more accurate, it may degrade clinical observational, interactional, and decision-making skills through lack of use. It may also remove the sense of self-efficacy that motivates professionals to endure onerous training and desire to enter the field. Using technology may reduce empathetic interactions that are basic to humanistic motivation, work satisfaction, and even community respect. Moral injury is already rampant in medicine from restrictions on freedom to do what we see as important for our patients. Technology has great potential and already is enhancing our ability to provide the best care for patients but the risks need to be watched for and ameliorated.
When technology automates comprehensive visit documentation that highlights priority and risk areas from patient input and individualizes decision support, it can facilitate the personalized care that we and our patients want to experience. We must not be so awed, intrigued, or wary of new technology to miss its benefits nor give up our good clinical judgment about the technology or about our patients.
Dr. Howard is assistant professor of pediatrics at The Johns Hopkins University School of Medicine, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
We have all been using technology in our primary care practices for a long time but newer formats have been emerging so fast that our minds, much less our staff’s minds, may be spinning.
Our old friend the telephone, a time-soaking nemesis for scheduling, checking coverage, questions calls, prescribing, quick consults, and follow-up is being replaced by EHR portals and SMS for messaging (e.g. DoctorConnect, SimplePractice), drop-in televisits and patient education links on our websites (e.g. Schmitt Pediatric Care, Remedy Connect), and chatbots for scheduling (e.g. CHEC-UP). While time is saved, what is lost may be hearing the subtext of anxiety or misperceptions in parents’ voices that would change our advice and the empathetic human connection in conversations with our patients. A hybrid approach may be better.
The paper appointment book has been replaced by scheduling systems sometimes lacking in flexibility for double booking, sibling visits, and variable length or extremely valuable multi-professional visits. Allowing patients to book their own visits may place complex problems in inappropriate slots, so only allowing online requests for visits is safer. On the other hand, many of us can now squeeze in “same day” televisits (e.g. Blueberry Pediatrics), sometimes from outside our practice (e.g., zocdoc), to increase payments and even entice new patients to enroll.
Amazing advances in technology are being made in specialty care such as genetic modifications (CRISPR), immunotherapies (mRNA vaccines and AI drug design), robot-assisted surgery, and 3-D printing of body parts and prosthetics. Technology as treatment such as transcranial magnetic stimulation and vagal stimulation are finding value in psychiatry.
But beside being aware of and able to order such specialty technologies, innovations are now extending our senses in primary care such as amplified or visual stethoscopes, bedside ultrasound (e.g. Butterfly), remote visualization (oto-, endo-)scopes, photographic vision screens (e.g. iScreen) for skin lesion (VisualDx) and genetic syndrome facial recognition. We need to be sure that technologies are tested and calibrated for children and different racial groups and genders to provide safe and equitable care. Early adoption may not always be the best approach. Costs of technology, as usual, may limit access to these advanced care aids especially, as usual, in practices serving low income and rural communities.
Patients, especially younger parents and youth, now expect to participate and can directly benefit from technology as part of their health care. Validated parent or self-report screens (e.g. EHRs, Phreesia) can detect important issues early for more effective intervention. Such questionnaires typically provide a pass/fail result or score, but other delivery systems (e.g. CHADIS) include interpretation, assist patients/parents in setting visit priorities and health goals, and even chain results of one questionnaire to secondary screens to hone in on problems, sometimes obviating a time-consuming second visit. Patient-completed comprehensive questionnaires (e.g. Well Visit Planner, CHADIS) allow us time to use our skills to focus on concerns, education, and management rather than asking myriad routine questions. Some (e.g. CHADIS) even create visit documentation reducing our “pajama time” write ups (and burnout); automate repeated online measures to track progress; and use questionnaire results to trigger related patient-specific education and resources rather than the often-ignored generic EHR handouts.
Digital therapeutics such as apps for anxiety (e.g. Calm), depression (e.g. SparkRx, Cass), weight control (e.g. Noom, Lose it), fitness, or sleep tracking (e.g. Whoop) help educate and, in some cases, provide real-time feedback to personalize discovery of contributing factors in order to maintain motivation for positive health behavior change. Some video games improve ADHD symptoms (e.g. EndeavorRX). Virtual reality scenarios have been shown to desensitize those with PTSD and social anxiety or teach social skills to children with autism.
Systems that trigger resource listings (including apps) from screen results can help, but now with over 10,000 apps for mental health, knowing what to recommend for what conditions is a challenge for which ratings (e.g. MINDapps.org) can help. With few product reps visiting to tell us what’s new, we need to read critically about innovations, search the web, subscribe to the AAP SOAPM LISTSERV, visit exhibitors at professional meetings, and talk with peers.
All the digital data collected from health care technology, if assembled with privacy constraints and analyzed with advanced statistical methods, have the possibility, with or without inclusion of genomic data, to allow for more accurate diagnostic and treatment decision support. While AI can search widely for patterns, it needs to be “trained” on appropriate data to make correct conclusions. We are all aware that the history determines 85% of both diagnosis and treatment decisions, particularly in primary care where x-rays or lab tests are not often needed.
But history in EHR notes is often idiosyncratic, entered hours after the visit by the clinician, and does not include the information needed to define diagnostic or guideline criteria, even if the clinician knows and considered those criteria. EHR templates are presented blank and are onerous and time consuming for clinicians. In addition, individual patient barriers to care, preferences, and environmental or subjective concerns are infrequently documented even though they may make the biggest difference to adherence and/or outcomes.
Notes made from voice to text digital AI translation of the encounter (e.g. Nuance DAX) are even less likely to include diagnostic criteria as it would be inappropriate to speak these. To use EHR history data to train AI and to test efficacy of care using variations of guidelines, guideline-related data is needed from online patient entries in questionnaires that are transformed to fill in templates along with some structured choices for clinician entries forming visit notes (e.g. CHADIS). New apps to facilitate clinician documentation of guidelines (e.g. AvoMD) could streamline visits as well as help document guideline criteria. The resulting combination of guideline-relevant patient histories and objective data to test and iteratively refine guidelines will allow a process known as a “Learning Health System.”
Technology to collect this kind of data can allow for the aspirational American Academy of Pediatrics CHILD Registry to approach this goal. Population-level data can provide surveillance for illness, toxins, effects of climate change, social drivers of health, and even effects of technologies themselves such as social media and remote learning so that we can attempt to make the best choices for the future.
Clinicians, staff, and patients will need to develop trust in technology as it infiltrates all aspects of health care. Professionals need both evidence and experience to trust a technology, which takes time and effort. Disinformation in the media may reduce trust or evoke unwarranted trust, as we have all seen regarding vaccines. Clear and coherent public health messaging can help but is no longer a panacea for developing trust in health care. Our nonjudgmental listening and informed opinions are needed more than ever.
The biggest issues for new technology are likely to be the need for workflow adjustments, changing our habit patterns, training, and cost/benefit analyses. With today’s high staff churn, confusion and even chaos can ensue when adopting new technology.
Staff need to be part of the selection process, if at all possible, and discuss how roles and flow will need to change. Having one staff member be a champion and expert for new tech can move adoption to a shared process rather than imposing “one more thing.” It is crucial to discuss the benefits for patients and staff even if the change is required. Sometimes cost savings can include a bonus for staff or free group lunches. Providing a certificate of achievement or title promotion for mastering new tech may be appropriate. Giving some time off from other tasks to learn new workflows can reduce resistance rather than just adding it on to a regular workload. Office “huddles” going forward can include examples of benefits staff have observed or heard about from the adoption. There are quality improvement processes that engage the team — some that earn MOC-4 or CEU credits — that apply to making workflow changes and measuring them iteratively.
If technology takes over important aspects of the work of medical professionals, even if it is faster and/or more accurate, it may degrade clinical observational, interactional, and decision-making skills through lack of use. It may also remove the sense of self-efficacy that motivates professionals to endure onerous training and desire to enter the field. Using technology may reduce empathetic interactions that are basic to humanistic motivation, work satisfaction, and even community respect. Moral injury is already rampant in medicine from restrictions on freedom to do what we see as important for our patients. Technology has great potential and already is enhancing our ability to provide the best care for patients but the risks need to be watched for and ameliorated.
When technology automates comprehensive visit documentation that highlights priority and risk areas from patient input and individualizes decision support, it can facilitate the personalized care that we and our patients want to experience. We must not be so awed, intrigued, or wary of new technology to miss its benefits nor give up our good clinical judgment about the technology or about our patients.
Dr. Howard is assistant professor of pediatrics at The Johns Hopkins University School of Medicine, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
We have all been using technology in our primary care practices for a long time but newer formats have been emerging so fast that our minds, much less our staff’s minds, may be spinning.
Our old friend the telephone, a time-soaking nemesis for scheduling, checking coverage, questions calls, prescribing, quick consults, and follow-up is being replaced by EHR portals and SMS for messaging (e.g. DoctorConnect, SimplePractice), drop-in televisits and patient education links on our websites (e.g. Schmitt Pediatric Care, Remedy Connect), and chatbots for scheduling (e.g. CHEC-UP). While time is saved, what is lost may be hearing the subtext of anxiety or misperceptions in parents’ voices that would change our advice and the empathetic human connection in conversations with our patients. A hybrid approach may be better.
The paper appointment book has been replaced by scheduling systems sometimes lacking in flexibility for double booking, sibling visits, and variable length or extremely valuable multi-professional visits. Allowing patients to book their own visits may place complex problems in inappropriate slots, so only allowing online requests for visits is safer. On the other hand, many of us can now squeeze in “same day” televisits (e.g. Blueberry Pediatrics), sometimes from outside our practice (e.g., zocdoc), to increase payments and even entice new patients to enroll.
Amazing advances in technology are being made in specialty care such as genetic modifications (CRISPR), immunotherapies (mRNA vaccines and AI drug design), robot-assisted surgery, and 3-D printing of body parts and prosthetics. Technology as treatment such as transcranial magnetic stimulation and vagal stimulation are finding value in psychiatry.
But beside being aware of and able to order such specialty technologies, innovations are now extending our senses in primary care such as amplified or visual stethoscopes, bedside ultrasound (e.g. Butterfly), remote visualization (oto-, endo-)scopes, photographic vision screens (e.g. iScreen) for skin lesion (VisualDx) and genetic syndrome facial recognition. We need to be sure that technologies are tested and calibrated for children and different racial groups and genders to provide safe and equitable care. Early adoption may not always be the best approach. Costs of technology, as usual, may limit access to these advanced care aids especially, as usual, in practices serving low income and rural communities.
Patients, especially younger parents and youth, now expect to participate and can directly benefit from technology as part of their health care. Validated parent or self-report screens (e.g. EHRs, Phreesia) can detect important issues early for more effective intervention. Such questionnaires typically provide a pass/fail result or score, but other delivery systems (e.g. CHADIS) include interpretation, assist patients/parents in setting visit priorities and health goals, and even chain results of one questionnaire to secondary screens to hone in on problems, sometimes obviating a time-consuming second visit. Patient-completed comprehensive questionnaires (e.g. Well Visit Planner, CHADIS) allow us time to use our skills to focus on concerns, education, and management rather than asking myriad routine questions. Some (e.g. CHADIS) even create visit documentation reducing our “pajama time” write ups (and burnout); automate repeated online measures to track progress; and use questionnaire results to trigger related patient-specific education and resources rather than the often-ignored generic EHR handouts.
Digital therapeutics such as apps for anxiety (e.g. Calm), depression (e.g. SparkRx, Cass), weight control (e.g. Noom, Lose it), fitness, or sleep tracking (e.g. Whoop) help educate and, in some cases, provide real-time feedback to personalize discovery of contributing factors in order to maintain motivation for positive health behavior change. Some video games improve ADHD symptoms (e.g. EndeavorRX). Virtual reality scenarios have been shown to desensitize those with PTSD and social anxiety or teach social skills to children with autism.
Systems that trigger resource listings (including apps) from screen results can help, but now with over 10,000 apps for mental health, knowing what to recommend for what conditions is a challenge for which ratings (e.g. MINDapps.org) can help. With few product reps visiting to tell us what’s new, we need to read critically about innovations, search the web, subscribe to the AAP SOAPM LISTSERV, visit exhibitors at professional meetings, and talk with peers.
All the digital data collected from health care technology, if assembled with privacy constraints and analyzed with advanced statistical methods, have the possibility, with or without inclusion of genomic data, to allow for more accurate diagnostic and treatment decision support. While AI can search widely for patterns, it needs to be “trained” on appropriate data to make correct conclusions. We are all aware that the history determines 85% of both diagnosis and treatment decisions, particularly in primary care where x-rays or lab tests are not often needed.
But history in EHR notes is often idiosyncratic, entered hours after the visit by the clinician, and does not include the information needed to define diagnostic or guideline criteria, even if the clinician knows and considered those criteria. EHR templates are presented blank and are onerous and time consuming for clinicians. In addition, individual patient barriers to care, preferences, and environmental or subjective concerns are infrequently documented even though they may make the biggest difference to adherence and/or outcomes.
Notes made from voice to text digital AI translation of the encounter (e.g. Nuance DAX) are even less likely to include diagnostic criteria as it would be inappropriate to speak these. To use EHR history data to train AI and to test efficacy of care using variations of guidelines, guideline-related data is needed from online patient entries in questionnaires that are transformed to fill in templates along with some structured choices for clinician entries forming visit notes (e.g. CHADIS). New apps to facilitate clinician documentation of guidelines (e.g. AvoMD) could streamline visits as well as help document guideline criteria. The resulting combination of guideline-relevant patient histories and objective data to test and iteratively refine guidelines will allow a process known as a “Learning Health System.”
Technology to collect this kind of data can allow for the aspirational American Academy of Pediatrics CHILD Registry to approach this goal. Population-level data can provide surveillance for illness, toxins, effects of climate change, social drivers of health, and even effects of technologies themselves such as social media and remote learning so that we can attempt to make the best choices for the future.
Clinicians, staff, and patients will need to develop trust in technology as it infiltrates all aspects of health care. Professionals need both evidence and experience to trust a technology, which takes time and effort. Disinformation in the media may reduce trust or evoke unwarranted trust, as we have all seen regarding vaccines. Clear and coherent public health messaging can help but is no longer a panacea for developing trust in health care. Our nonjudgmental listening and informed opinions are needed more than ever.
The biggest issues for new technology are likely to be the need for workflow adjustments, changing our habit patterns, training, and cost/benefit analyses. With today’s high staff churn, confusion and even chaos can ensue when adopting new technology.
Staff need to be part of the selection process, if at all possible, and discuss how roles and flow will need to change. Having one staff member be a champion and expert for new tech can move adoption to a shared process rather than imposing “one more thing.” It is crucial to discuss the benefits for patients and staff even if the change is required. Sometimes cost savings can include a bonus for staff or free group lunches. Providing a certificate of achievement or title promotion for mastering new tech may be appropriate. Giving some time off from other tasks to learn new workflows can reduce resistance rather than just adding it on to a regular workload. Office “huddles” going forward can include examples of benefits staff have observed or heard about from the adoption. There are quality improvement processes that engage the team — some that earn MOC-4 or CEU credits — that apply to making workflow changes and measuring them iteratively.
If technology takes over important aspects of the work of medical professionals, even if it is faster and/or more accurate, it may degrade clinical observational, interactional, and decision-making skills through lack of use. It may also remove the sense of self-efficacy that motivates professionals to endure onerous training and desire to enter the field. Using technology may reduce empathetic interactions that are basic to humanistic motivation, work satisfaction, and even community respect. Moral injury is already rampant in medicine from restrictions on freedom to do what we see as important for our patients. Technology has great potential and already is enhancing our ability to provide the best care for patients but the risks need to be watched for and ameliorated.
When technology automates comprehensive visit documentation that highlights priority and risk areas from patient input and individualizes decision support, it can facilitate the personalized care that we and our patients want to experience. We must not be so awed, intrigued, or wary of new technology to miss its benefits nor give up our good clinical judgment about the technology or about our patients.
Dr. Howard is assistant professor of pediatrics at The Johns Hopkins University School of Medicine, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Can AI enhance mental health treatment?
Three questions for clinicians
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Three questions for clinicians
Three questions for clinicians
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
New cardiology certification board: What’s the plan?
The proposal by the major cardiovascular societies in the US to form a new board of cardiovascular medicine to manage initial and ongoing certification of cardiologists represents something of a revolution in the field of continuing medical education and assessment of competency.
Five US cardiovascular societies — the American College of Cardiology (ACC), the American Heart Association (AHA), the Heart Failure Society of America (HFSA), the Heart Rhythm Society (HRS), and the Society for Cardiovascular Angiography & Interventions (SCAI) — have now joined forces to propose a new professional certification board for cardiovascular medicine, to be known as the American Board of Cardiovascular Medicine (ABCVM).
The ABCVM would be independent of the American Board of Internal Medicine (ABIM), the current organization providing maintenance of certification for cardiologists as well as many other internal medicine subspecialties. The ABIM’s maintenance of certification process has been widely criticized for many years and has been described as “needlessly burdensome and expensive.”
, according to Jeffrey Kuvin, MD, a trustee of the ACC, who has been heading up the working group to develop this plan.
Dr. Kuvin, who is chair of the cardiology at Northwell Health, Manhasset, New York, a large academic healthcare system, explained that maintenance of certification has been a topic of discussion across the cardiovascular community for many years, and the ACC has a working group focused on the next steps for evaluation of competency, which he chairs.
“The topic of evaluation of competence has been on the mind of the ACC for many years and hence a work group was developed to focus on this,” Dr. Kuvin noted. “A lot of evolution of the concepts and next steps have been drawn out of this working group. And now other cardiovascular societies have joined to show unification across the house of cardiology and that this is indeed the way that the cardiovascular profession should move.”
“Time to Separate from Internal Medicine”
The general concept behind the new cardiology board is to separate cardiology from the ABIM.
“This is rooted from the concept that cardiology has evolved so much over the last few decades into such a large multidimensional specialty that it really does demarcate itself from internal medicine, and as such, it deserves a separate board governed by cardiologists with collaboration across the entirely of cardiology,” Dr. Kuvin said.
Cardiology has had significant growth and expansion of technology, tools, medications, and the approach to patients in many specialities and subspecialties, he added. “We have defined training programs in many different areas within cardiology; we have our own guidelines, our own competency statements, and in many cases, cardiology exists as its own department outside of medicine in many institutions. It’s just time to separate cardiology from the umbrella of internal medicine.”
The new cardiology board would be separate from, and not report to, the ABIM; rather, it would report directly to the American Board of Medical Specialties (ABMS), the only recognized medical certification body in the US.
What Are the Proposed Changes
Under the present system, managed by the ABIM, clinicians must undergo two stages of certification to be a cardiologist. First, they have to pass the initial certification exam in general cardiology, and then exams in one of four subspecialties if they plan to enter one of these, including interventional cardiology, electrophysiology, advanced heart failure or adult congenital heart disease.
Next, clinicians enter the maintenance of certification phase, which can take three different forms: 1) taking another recertification exam every 10 years; 2) the collaborative maintenance pathway — a collaboration between ACC and ABIM, which includes evaluation, learning and a certified exam each year; or 3) longitudinal knowledge and assessment — in which the program interacts with the clinician on an ongoing basis, sending secured questions regularly.
All three of these pathways for maintenance of certification involve high stakes questions and a set bar for passing or failing.
Under the proposed new cardiology board, an initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured, with the new approach taking the form of continuous learning and assessment of competency.
“This is an iterative process, but we envision with a new American Board of Cardiovascular Medicine, we will pick up where the ABIM left off,” Dr. Kuvin notes. “That includes an initial certifying examination for the five areas that already exist under the ABIM system but with the opportunities to expand that to further specialties as well.”
He points out that there are several areas in cardiology that are currently not represented by these five areas that warrant some discussion, including multimodality imaging, vascular heart disease, and cardio-oncology.
“At present, everybody has to pass the general cardiology exam and then some may wish to further train and get certified in one of the other four other specific areas. But one topic that has been discussed over many years is how do we maintain competency in the areas in which clinicians practice over their lifetime as a cardiologist,” Dr. Kuvin commented.
He said the proposed cardiology board would like to adhere to some basic principles that are fundamental to the practice of medicine.
“We want to make sure that we are practicing medicine so that our patients derive the most benefit from seeing a cardiologist,” he said. “We also want to make sure, however, that this is a supportive process, supporting cardiologists to learn what they know and more importantly what they don’t know; to identify knowledge gaps in specific area; to help the cardiologist fill those knowledge gaps; to acknowledge those gaps have been filled; and then move on to another area of interest. This will be the focus of this new and improved model of continuous competency.”
The proposed new board also says it wants to make sure this is appropriate to the area in which the clinician is practicing.
“To take a closed book certified exam every 10 years on the world of cardiology as happens at the current time – or the assessments conducted in the other two pathways – is often meaningless to the cardiologist,” Dr. Kuvin says. “All three current pathways involve high stakes questions that are often irrelevant to one’s clinical practice.”
Lifelong Learning
“The crux of the changes we are proposing will be away from the focus of passing a test towards a model of helping the individual with their competency, with continuous learning and evaluation of competency to help the clinician fill in their knowledge gaps,” he explains.
He described the new approach as “lifelong learning,” adding that, instead of it being “a punitive pass/fail environment with no feedback, which causes a lot of discontent among clinicians,” it will be a supportive process, where a clinician will be helped in filling their knowledge gaps.
“I think this would be a welcome change not just for cardiology but across medical specialties,” Dr. Kuvin said.
He also pointed out the ABMS itself is considering a continuous competency approach, and the proposed new cardiology board aims to work with the ABMS to make sure that their goals of continuous competency assessment are matched.
“The world has changed. The ability to access information has changed. It is no longer imperative for a clinician to have every piece of knowledge in their brain, but rather to know how to get knowledge and to incorporate that knowledge into clinical practice,” Dr. Kuvin noted. “Competency should not involve knowledge alone as in a closed book exam. It is more about understanding the world that we live in, how to synthesize information, where we need to improve knowledge and how to do that.”
Dr. Kuvin acknowledged that asking clinicians questions is a very helpful tool to identify their knowledge base and their knowledge gaps. “But we believe the clinician needs to be given resources — that could be a conference, an article, a simulation — to fill that knowledge gap. Then we could ask clinicians some different questions and if they get those right then we have provided a service.”
Tactile skills for cardiologists needing to perform procedures – such as interventionalists or electrophysiologists may be incorporated by simulation in a technology-based scenario.
On how often these assessments would take place, Dr. Kuvin said that hadn’t been decided for sure.
“We certainly do not think an assessment every 10 years is appropriate. We envision, instead of an episodic model, it will be rather a lifelong journey of education and competency. This will involve frequent contact and making sure knowledge gaps are being filled. There are criteria being set out by the ABMS that there should be a certain number of touch points with individuals on an annual as well as a 5-year basis to make sure cardiologists are staying within specific guardrails. The exact nature of these is yet to be determined,” he said.
Dr. Kuvin added that it was not known yet what sort of hours would be required but added that “this will not be a significant time burden.”
What is the Timeframe?
The application to the ABMS for a separate cardiology board is still ongoing and has not yet received formal acceptance. Representatives from the five US cardiovascular societies are in the initial stages of formulating a transition board.
“The submission to the ABMS will take time for them to review. This could take up to a year or so,” Dr. Kuvin estimates.
This is the first time the ABMS has entertained the concept of a new board in many years, he noted. “It will be a paradigm shift for the whole country. I think that cardiology is really at the forefront and in a position where we can actually do this. If cardiovascular medicine is granted a new board, I think this will help change the approach of how physicians are assessed in terms of continuous competency not just in cardiology but across all specialties of medicine.”
He added: “We are confident that we can work within the construct of the ABMS guidelines that have been revised to be much more holistic in the approach of continuous competence across the board. This includes thinking beyond rote medical knowledge and thinking about the clinician as a whole and their abilities to communicate, act professionally, work within a complex medical system, utilize medical resources effectively. These all have to be part of continuous competence.”
How Much Will This Cost?
Noting that the ABIM has received criticism over the costs of the certification process, Dr. Kuvin said they intend to make this “as lean a machine as possible with the focus on reducing the financial [burden] as well as the time burden for cardiologists. It is very important that this is not cumbersome, that it is woven into clinical practice, and that it is not costly.”
But he pointed out that building a new board will have significant costs.
“We have to think about developing initial board certification examinations as well as changing the paradigm on continuous certification,” he said. “This will take some up-front costs, and our society partners have decided that they are willing to provide some start-up funds for this. We anticipate the initial certification will remain somewhat similar in price, but the cost of ongoing continuous competency assessment will be significantly reduced compared to today’s models.”
Dr. Kuvin said the collaboration of the five participating US cardiovascular societies was unprecedented. But he noted that while the transition board is beginning with representatives of these individual societies, it will ultimately be independent from these societies and have its own board of directors.
He suggested that other societies representing other parts of cardiology are also interested. “Cardiology has recognized how important this is,” he said. “Everybody is excited about this.”
A version of this article appeared on Medscape.com.
The proposal by the major cardiovascular societies in the US to form a new board of cardiovascular medicine to manage initial and ongoing certification of cardiologists represents something of a revolution in the field of continuing medical education and assessment of competency.
Five US cardiovascular societies — the American College of Cardiology (ACC), the American Heart Association (AHA), the Heart Failure Society of America (HFSA), the Heart Rhythm Society (HRS), and the Society for Cardiovascular Angiography & Interventions (SCAI) — have now joined forces to propose a new professional certification board for cardiovascular medicine, to be known as the American Board of Cardiovascular Medicine (ABCVM).
The ABCVM would be independent of the American Board of Internal Medicine (ABIM), the current organization providing maintenance of certification for cardiologists as well as many other internal medicine subspecialties. The ABIM’s maintenance of certification process has been widely criticized for many years and has been described as “needlessly burdensome and expensive.”
, according to Jeffrey Kuvin, MD, a trustee of the ACC, who has been heading up the working group to develop this plan.
Dr. Kuvin, who is chair of the cardiology at Northwell Health, Manhasset, New York, a large academic healthcare system, explained that maintenance of certification has been a topic of discussion across the cardiovascular community for many years, and the ACC has a working group focused on the next steps for evaluation of competency, which he chairs.
“The topic of evaluation of competence has been on the mind of the ACC for many years and hence a work group was developed to focus on this,” Dr. Kuvin noted. “A lot of evolution of the concepts and next steps have been drawn out of this working group. And now other cardiovascular societies have joined to show unification across the house of cardiology and that this is indeed the way that the cardiovascular profession should move.”
“Time to Separate from Internal Medicine”
The general concept behind the new cardiology board is to separate cardiology from the ABIM.
“This is rooted from the concept that cardiology has evolved so much over the last few decades into such a large multidimensional specialty that it really does demarcate itself from internal medicine, and as such, it deserves a separate board governed by cardiologists with collaboration across the entirely of cardiology,” Dr. Kuvin said.
Cardiology has had significant growth and expansion of technology, tools, medications, and the approach to patients in many specialities and subspecialties, he added. “We have defined training programs in many different areas within cardiology; we have our own guidelines, our own competency statements, and in many cases, cardiology exists as its own department outside of medicine in many institutions. It’s just time to separate cardiology from the umbrella of internal medicine.”
The new cardiology board would be separate from, and not report to, the ABIM; rather, it would report directly to the American Board of Medical Specialties (ABMS), the only recognized medical certification body in the US.
What Are the Proposed Changes
Under the present system, managed by the ABIM, clinicians must undergo two stages of certification to be a cardiologist. First, they have to pass the initial certification exam in general cardiology, and then exams in one of four subspecialties if they plan to enter one of these, including interventional cardiology, electrophysiology, advanced heart failure or adult congenital heart disease.
Next, clinicians enter the maintenance of certification phase, which can take three different forms: 1) taking another recertification exam every 10 years; 2) the collaborative maintenance pathway — a collaboration between ACC and ABIM, which includes evaluation, learning and a certified exam each year; or 3) longitudinal knowledge and assessment — in which the program interacts with the clinician on an ongoing basis, sending secured questions regularly.
All three of these pathways for maintenance of certification involve high stakes questions and a set bar for passing or failing.
Under the proposed new cardiology board, an initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured, with the new approach taking the form of continuous learning and assessment of competency.
“This is an iterative process, but we envision with a new American Board of Cardiovascular Medicine, we will pick up where the ABIM left off,” Dr. Kuvin notes. “That includes an initial certifying examination for the five areas that already exist under the ABIM system but with the opportunities to expand that to further specialties as well.”
He points out that there are several areas in cardiology that are currently not represented by these five areas that warrant some discussion, including multimodality imaging, vascular heart disease, and cardio-oncology.
“At present, everybody has to pass the general cardiology exam and then some may wish to further train and get certified in one of the other four other specific areas. But one topic that has been discussed over many years is how do we maintain competency in the areas in which clinicians practice over their lifetime as a cardiologist,” Dr. Kuvin commented.
He said the proposed cardiology board would like to adhere to some basic principles that are fundamental to the practice of medicine.
“We want to make sure that we are practicing medicine so that our patients derive the most benefit from seeing a cardiologist,” he said. “We also want to make sure, however, that this is a supportive process, supporting cardiologists to learn what they know and more importantly what they don’t know; to identify knowledge gaps in specific area; to help the cardiologist fill those knowledge gaps; to acknowledge those gaps have been filled; and then move on to another area of interest. This will be the focus of this new and improved model of continuous competency.”
The proposed new board also says it wants to make sure this is appropriate to the area in which the clinician is practicing.
“To take a closed book certified exam every 10 years on the world of cardiology as happens at the current time – or the assessments conducted in the other two pathways – is often meaningless to the cardiologist,” Dr. Kuvin says. “All three current pathways involve high stakes questions that are often irrelevant to one’s clinical practice.”
Lifelong Learning
“The crux of the changes we are proposing will be away from the focus of passing a test towards a model of helping the individual with their competency, with continuous learning and evaluation of competency to help the clinician fill in their knowledge gaps,” he explains.
He described the new approach as “lifelong learning,” adding that, instead of it being “a punitive pass/fail environment with no feedback, which causes a lot of discontent among clinicians,” it will be a supportive process, where a clinician will be helped in filling their knowledge gaps.
“I think this would be a welcome change not just for cardiology but across medical specialties,” Dr. Kuvin said.
He also pointed out the ABMS itself is considering a continuous competency approach, and the proposed new cardiology board aims to work with the ABMS to make sure that their goals of continuous competency assessment are matched.
“The world has changed. The ability to access information has changed. It is no longer imperative for a clinician to have every piece of knowledge in their brain, but rather to know how to get knowledge and to incorporate that knowledge into clinical practice,” Dr. Kuvin noted. “Competency should not involve knowledge alone as in a closed book exam. It is more about understanding the world that we live in, how to synthesize information, where we need to improve knowledge and how to do that.”
Dr. Kuvin acknowledged that asking clinicians questions is a very helpful tool to identify their knowledge base and their knowledge gaps. “But we believe the clinician needs to be given resources — that could be a conference, an article, a simulation — to fill that knowledge gap. Then we could ask clinicians some different questions and if they get those right then we have provided a service.”
Tactile skills for cardiologists needing to perform procedures – such as interventionalists or electrophysiologists may be incorporated by simulation in a technology-based scenario.
On how often these assessments would take place, Dr. Kuvin said that hadn’t been decided for sure.
“We certainly do not think an assessment every 10 years is appropriate. We envision, instead of an episodic model, it will be rather a lifelong journey of education and competency. This will involve frequent contact and making sure knowledge gaps are being filled. There are criteria being set out by the ABMS that there should be a certain number of touch points with individuals on an annual as well as a 5-year basis to make sure cardiologists are staying within specific guardrails. The exact nature of these is yet to be determined,” he said.
Dr. Kuvin added that it was not known yet what sort of hours would be required but added that “this will not be a significant time burden.”
What is the Timeframe?
The application to the ABMS for a separate cardiology board is still ongoing and has not yet received formal acceptance. Representatives from the five US cardiovascular societies are in the initial stages of formulating a transition board.
“The submission to the ABMS will take time for them to review. This could take up to a year or so,” Dr. Kuvin estimates.
This is the first time the ABMS has entertained the concept of a new board in many years, he noted. “It will be a paradigm shift for the whole country. I think that cardiology is really at the forefront and in a position where we can actually do this. If cardiovascular medicine is granted a new board, I think this will help change the approach of how physicians are assessed in terms of continuous competency not just in cardiology but across all specialties of medicine.”
He added: “We are confident that we can work within the construct of the ABMS guidelines that have been revised to be much more holistic in the approach of continuous competence across the board. This includes thinking beyond rote medical knowledge and thinking about the clinician as a whole and their abilities to communicate, act professionally, work within a complex medical system, utilize medical resources effectively. These all have to be part of continuous competence.”
How Much Will This Cost?
Noting that the ABIM has received criticism over the costs of the certification process, Dr. Kuvin said they intend to make this “as lean a machine as possible with the focus on reducing the financial [burden] as well as the time burden for cardiologists. It is very important that this is not cumbersome, that it is woven into clinical practice, and that it is not costly.”
But he pointed out that building a new board will have significant costs.
“We have to think about developing initial board certification examinations as well as changing the paradigm on continuous certification,” he said. “This will take some up-front costs, and our society partners have decided that they are willing to provide some start-up funds for this. We anticipate the initial certification will remain somewhat similar in price, but the cost of ongoing continuous competency assessment will be significantly reduced compared to today’s models.”
Dr. Kuvin said the collaboration of the five participating US cardiovascular societies was unprecedented. But he noted that while the transition board is beginning with representatives of these individual societies, it will ultimately be independent from these societies and have its own board of directors.
He suggested that other societies representing other parts of cardiology are also interested. “Cardiology has recognized how important this is,” he said. “Everybody is excited about this.”
A version of this article appeared on Medscape.com.
The proposal by the major cardiovascular societies in the US to form a new board of cardiovascular medicine to manage initial and ongoing certification of cardiologists represents something of a revolution in the field of continuing medical education and assessment of competency.
Five US cardiovascular societies — the American College of Cardiology (ACC), the American Heart Association (AHA), the Heart Failure Society of America (HFSA), the Heart Rhythm Society (HRS), and the Society for Cardiovascular Angiography & Interventions (SCAI) — have now joined forces to propose a new professional certification board for cardiovascular medicine, to be known as the American Board of Cardiovascular Medicine (ABCVM).
The ABCVM would be independent of the American Board of Internal Medicine (ABIM), the current organization providing maintenance of certification for cardiologists as well as many other internal medicine subspecialties. The ABIM’s maintenance of certification process has been widely criticized for many years and has been described as “needlessly burdensome and expensive.”
, according to Jeffrey Kuvin, MD, a trustee of the ACC, who has been heading up the working group to develop this plan.
Dr. Kuvin, who is chair of the cardiology at Northwell Health, Manhasset, New York, a large academic healthcare system, explained that maintenance of certification has been a topic of discussion across the cardiovascular community for many years, and the ACC has a working group focused on the next steps for evaluation of competency, which he chairs.
“The topic of evaluation of competence has been on the mind of the ACC for many years and hence a work group was developed to focus on this,” Dr. Kuvin noted. “A lot of evolution of the concepts and next steps have been drawn out of this working group. And now other cardiovascular societies have joined to show unification across the house of cardiology and that this is indeed the way that the cardiovascular profession should move.”
“Time to Separate from Internal Medicine”
The general concept behind the new cardiology board is to separate cardiology from the ABIM.
“This is rooted from the concept that cardiology has evolved so much over the last few decades into such a large multidimensional specialty that it really does demarcate itself from internal medicine, and as such, it deserves a separate board governed by cardiologists with collaboration across the entirely of cardiology,” Dr. Kuvin said.
Cardiology has had significant growth and expansion of technology, tools, medications, and the approach to patients in many specialities and subspecialties, he added. “We have defined training programs in many different areas within cardiology; we have our own guidelines, our own competency statements, and in many cases, cardiology exists as its own department outside of medicine in many institutions. It’s just time to separate cardiology from the umbrella of internal medicine.”
The new cardiology board would be separate from, and not report to, the ABIM; rather, it would report directly to the American Board of Medical Specialties (ABMS), the only recognized medical certification body in the US.
What Are the Proposed Changes
Under the present system, managed by the ABIM, clinicians must undergo two stages of certification to be a cardiologist. First, they have to pass the initial certification exam in general cardiology, and then exams in one of four subspecialties if they plan to enter one of these, including interventional cardiology, electrophysiology, advanced heart failure or adult congenital heart disease.
Next, clinicians enter the maintenance of certification phase, which can take three different forms: 1) taking another recertification exam every 10 years; 2) the collaborative maintenance pathway — a collaboration between ACC and ABIM, which includes evaluation, learning and a certified exam each year; or 3) longitudinal knowledge and assessment — in which the program interacts with the clinician on an ongoing basis, sending secured questions regularly.
All three of these pathways for maintenance of certification involve high stakes questions and a set bar for passing or failing.
Under the proposed new cardiology board, an initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured, with the new approach taking the form of continuous learning and assessment of competency.
“This is an iterative process, but we envision with a new American Board of Cardiovascular Medicine, we will pick up where the ABIM left off,” Dr. Kuvin notes. “That includes an initial certifying examination for the five areas that already exist under the ABIM system but with the opportunities to expand that to further specialties as well.”
He points out that there are several areas in cardiology that are currently not represented by these five areas that warrant some discussion, including multimodality imaging, vascular heart disease, and cardio-oncology.
“At present, everybody has to pass the general cardiology exam and then some may wish to further train and get certified in one of the other four other specific areas. But one topic that has been discussed over many years is how do we maintain competency in the areas in which clinicians practice over their lifetime as a cardiologist,” Dr. Kuvin commented.
He said the proposed cardiology board would like to adhere to some basic principles that are fundamental to the practice of medicine.
“We want to make sure that we are practicing medicine so that our patients derive the most benefit from seeing a cardiologist,” he said. “We also want to make sure, however, that this is a supportive process, supporting cardiologists to learn what they know and more importantly what they don’t know; to identify knowledge gaps in specific area; to help the cardiologist fill those knowledge gaps; to acknowledge those gaps have been filled; and then move on to another area of interest. This will be the focus of this new and improved model of continuous competency.”
The proposed new board also says it wants to make sure this is appropriate to the area in which the clinician is practicing.
“To take a closed book certified exam every 10 years on the world of cardiology as happens at the current time – or the assessments conducted in the other two pathways – is often meaningless to the cardiologist,” Dr. Kuvin says. “All three current pathways involve high stakes questions that are often irrelevant to one’s clinical practice.”
Lifelong Learning
“The crux of the changes we are proposing will be away from the focus of passing a test towards a model of helping the individual with their competency, with continuous learning and evaluation of competency to help the clinician fill in their knowledge gaps,” he explains.
He described the new approach as “lifelong learning,” adding that, instead of it being “a punitive pass/fail environment with no feedback, which causes a lot of discontent among clinicians,” it will be a supportive process, where a clinician will be helped in filling their knowledge gaps.
“I think this would be a welcome change not just for cardiology but across medical specialties,” Dr. Kuvin said.
He also pointed out the ABMS itself is considering a continuous competency approach, and the proposed new cardiology board aims to work with the ABMS to make sure that their goals of continuous competency assessment are matched.
“The world has changed. The ability to access information has changed. It is no longer imperative for a clinician to have every piece of knowledge in their brain, but rather to know how to get knowledge and to incorporate that knowledge into clinical practice,” Dr. Kuvin noted. “Competency should not involve knowledge alone as in a closed book exam. It is more about understanding the world that we live in, how to synthesize information, where we need to improve knowledge and how to do that.”
Dr. Kuvin acknowledged that asking clinicians questions is a very helpful tool to identify their knowledge base and their knowledge gaps. “But we believe the clinician needs to be given resources — that could be a conference, an article, a simulation — to fill that knowledge gap. Then we could ask clinicians some different questions and if they get those right then we have provided a service.”
Tactile skills for cardiologists needing to perform procedures – such as interventionalists or electrophysiologists may be incorporated by simulation in a technology-based scenario.
On how often these assessments would take place, Dr. Kuvin said that hadn’t been decided for sure.
“We certainly do not think an assessment every 10 years is appropriate. We envision, instead of an episodic model, it will be rather a lifelong journey of education and competency. This will involve frequent contact and making sure knowledge gaps are being filled. There are criteria being set out by the ABMS that there should be a certain number of touch points with individuals on an annual as well as a 5-year basis to make sure cardiologists are staying within specific guardrails. The exact nature of these is yet to be determined,” he said.
Dr. Kuvin added that it was not known yet what sort of hours would be required but added that “this will not be a significant time burden.”
What is the Timeframe?
The application to the ABMS for a separate cardiology board is still ongoing and has not yet received formal acceptance. Representatives from the five US cardiovascular societies are in the initial stages of formulating a transition board.
“The submission to the ABMS will take time for them to review. This could take up to a year or so,” Dr. Kuvin estimates.
This is the first time the ABMS has entertained the concept of a new board in many years, he noted. “It will be a paradigm shift for the whole country. I think that cardiology is really at the forefront and in a position where we can actually do this. If cardiovascular medicine is granted a new board, I think this will help change the approach of how physicians are assessed in terms of continuous competency not just in cardiology but across all specialties of medicine.”
He added: “We are confident that we can work within the construct of the ABMS guidelines that have been revised to be much more holistic in the approach of continuous competence across the board. This includes thinking beyond rote medical knowledge and thinking about the clinician as a whole and their abilities to communicate, act professionally, work within a complex medical system, utilize medical resources effectively. These all have to be part of continuous competence.”
How Much Will This Cost?
Noting that the ABIM has received criticism over the costs of the certification process, Dr. Kuvin said they intend to make this “as lean a machine as possible with the focus on reducing the financial [burden] as well as the time burden for cardiologists. It is very important that this is not cumbersome, that it is woven into clinical practice, and that it is not costly.”
But he pointed out that building a new board will have significant costs.
“We have to think about developing initial board certification examinations as well as changing the paradigm on continuous certification,” he said. “This will take some up-front costs, and our society partners have decided that they are willing to provide some start-up funds for this. We anticipate the initial certification will remain somewhat similar in price, but the cost of ongoing continuous competency assessment will be significantly reduced compared to today’s models.”
Dr. Kuvin said the collaboration of the five participating US cardiovascular societies was unprecedented. But he noted that while the transition board is beginning with representatives of these individual societies, it will ultimately be independent from these societies and have its own board of directors.
He suggested that other societies representing other parts of cardiology are also interested. “Cardiology has recognized how important this is,” he said. “Everybody is excited about this.”
A version of this article appeared on Medscape.com.
Clinician responsibilities during times of geopolitical conflict
In the realm of clinical psychology and psychiatry, our primary duty and commitment is (and should be) to the well-being of our patients. Yet, as we find ourselves in an era marked by escalating geopolitical conflict, such as the Israel-Hamas war, probably more aptly titled the Israeli-Hamas-Hezbollah-Houthi war (a clarification that elucidates a later point), clinicians are increasingly confronted with ethical dilemmas that extend far beyond what is outlined in our code of ethics.
These challenges are not only impacting us on a personal level but are also spilling over into our professional lives, creating a divisive and non-collegial environment within the healthcare community. We commit to “do no harm” when delivering care and yet we are doing harm to one another as colleagues.
We are no strangers to the complexities of human behavior and the intricate tapestry of emotions that are involved with our professional work. However, the current geopolitical landscape has added an extra layer of difficulty to our already taxing professional lives. We are, after all, human first with unconscious drives that govern how we negotiate cognitive dissonance and our need for the illusion of absolute justice as Yuval Noah Harari explains in a recent podcast.
Humans are notoriously bad at holding the multiplicity of experience in mind and various (often competing narratives) that impede the capacity for nuanced thinking. We would like to believe we are better and more capable than the average person in doing so, but divisiveness in our profession has become disturbingly pronounced, making it essential for us to carve out reflective space, more than ever.
The personal and professional divide
Geopolitical conflicts like the current war have a unique capacity to ignite strong emotions and deeply held convictions. It’s not hard to quickly become embroiled in passionate and engaged debate.
While discussion and discourse are healthy, these are bleeding into professional spheres, creating rifts within our clinical communities and contributing to a culture where not everyone feels safe. Look at any professional listserv in medicine or psychology and you will find the evidence. It should be an immediate call to action that we need to be fostering a different type of environment.
The impact of divisiveness is profound, hindering opportunities for collaboration, mentorship, and the free exchange of ideas among clinicians. It may lead to misunderstandings, mistrust, and an erosion of the support systems we rely on, ultimately diverting energy away from the pursuit of providing quality patient-care.
Balancing obligations and limits
Because of the inherent power differential that accompanies being in a provider role (physician and psychologist alike), we have a social and moral responsibility to be mindful of what we share – for the sake of humanity. There is an implicit assumption that a provider’s guidance should be adhered to and respected. In other words, words carry tremendous weight and deeply matter, and people in the general public ascribe significant meaning to messages put out by professionals.
When providers steer from their lanes of professional expertise to provide the general public with opinions or recommendations on nonmedical topics, problematic precedents can be set. We may be doing people a disservice.
Unfortunately, I have heard several anecdotes about clinicians who spend their patient’s time in session pushing their own ideological agendas. The patient-provider relationship is founded on principles of trust, empathy, and collaboration, with the primary goal of improving overall well-being and addressing a specific presenting problem. Of course, issues emerge that need to be addressed outside of the initial scope of treatment, an inherent part of the process. However, a grave concern emerges when clinicians initiate dialogue that is not meaningful to a patient, disclose and discuss their personal ideologies, or put pressure on patients to explain their beliefs in an attempt to change the patients’ minds.
Clinicians pushing their own agenda during patient sessions is antithetical to the objectives of psychotherapy and compromises the therapeutic alliance by diverting the focus of care in a way that serves the clinician rather than the client. It is quite the opposite of the patient-centered care that we strive for in training and practice.
Even within one’s theoretical professional scope of competence, I have seen the impact of emotions running high during this conflict, and have witnessed trained professionals making light of, or even mocking, hostages and their behavior upon release. These are care providers who could elucidate the complexities of captor-captive dynamics and the impact of trauma for the general public, yet they are contributing to dangerous perceptions and divisiveness.
I have also seen providers justify sexual violence, diminishing survivor and witness testimony due to ideological differences and strong personal beliefs. This is harmful to those impacted and does a disservice to our profession at large. In a helping profession we should strive to support and advocate for anyone who has been maltreated or experienced any form of victimization, violence, or abuse. This should be a professional standard.
As clinicians, we have an ethical obligation to uphold the well-being, autonomy, and dignity of our patients — and humanity. It is crucial to recognize the limits of our expertise and the ethical concerns that can arise in light of geopolitical conflict. How can we balance our duty to provide psychological support while also being cautious about delving into the realms of political analysis, foreign policy, or international relations?
The pitfalls of well-intentioned speaking out
In the age of social media and instant communication, a critical aspect to consider is the role of speaking out. The point I made above, in naming all partaking in the current conflict, speaks to this issue.
As providers and programs, we must be mindful of the inadvertent harm that can arise from making brief, underdeveloped, uninformed, or emotionally charged statements. Expressing opinions without a solid understanding of the historical, cultural, and political nuances of a conflict can contribute to misinformation and further polarization.
Anecdotally, there appears to be some significant degree of bias emerging within professional fields (e.g., psychology, medicine) and an innate calling for providers to “weigh in” as the war continues. Obviously, physicians and psychologists are trained to provide care and to be humanistic and empathic, but the majority do not have expertise in geopolitics or a nuanced awareness of the complexities of the conflict in the Middle East.
While hearts may be in the right place, issuing statements on complicated humanitarian/political situations can inadvertently have unintended and harmful consequences (in terms of antisemitism and islamophobia, increased incidence of hate crimes, and colleagues not feeling safe within professional societies or member organizations).
Unsophisticated, overly simplistic, and reductionistic statements that do not adequately convey nuance will not reflect the range of experience reflected by providers in the field (or the patients we treat). It is essential for clinicians and institutions putting out public statements to engage in deep reflection and utilize discernment. We must recognize that our words carry weight, given our position of influence as treatment providers. To minimize harm, we should seek to provide information that is fair, vetted, and balanced, and encourage open, respectful dialogue rather than asserting definitive positions.
Ultimately, as providers we must strive to seek unity and inclusivity amidst the current challenges. It is important for us to embody a spirit of collaboration during a time demarcated by deep fragmentation.
By acknowledging our limitations, promoting informed discussion, and avoiding the pitfalls of uninformed advocacy, we can contribute to a more compassionate and understanding world, even in the face of the most divisive geopolitical conflicts. We have an obligation to uphold when it comes to ourselves as professionals, and we need to foster healthy, respectful dialogue while maintaining an awareness of our blind spots.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She is an affiliate of Baptist West Kendall Hospital/FIU Family Medicine Residency Program and serves as president on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. The opinions expressed by Dr. Feldman are her own and do not represent the institutions with which she is affiliated. She has no disclosures.
In the realm of clinical psychology and psychiatry, our primary duty and commitment is (and should be) to the well-being of our patients. Yet, as we find ourselves in an era marked by escalating geopolitical conflict, such as the Israel-Hamas war, probably more aptly titled the Israeli-Hamas-Hezbollah-Houthi war (a clarification that elucidates a later point), clinicians are increasingly confronted with ethical dilemmas that extend far beyond what is outlined in our code of ethics.
These challenges are not only impacting us on a personal level but are also spilling over into our professional lives, creating a divisive and non-collegial environment within the healthcare community. We commit to “do no harm” when delivering care and yet we are doing harm to one another as colleagues.
We are no strangers to the complexities of human behavior and the intricate tapestry of emotions that are involved with our professional work. However, the current geopolitical landscape has added an extra layer of difficulty to our already taxing professional lives. We are, after all, human first with unconscious drives that govern how we negotiate cognitive dissonance and our need for the illusion of absolute justice as Yuval Noah Harari explains in a recent podcast.
Humans are notoriously bad at holding the multiplicity of experience in mind and various (often competing narratives) that impede the capacity for nuanced thinking. We would like to believe we are better and more capable than the average person in doing so, but divisiveness in our profession has become disturbingly pronounced, making it essential for us to carve out reflective space, more than ever.
The personal and professional divide
Geopolitical conflicts like the current war have a unique capacity to ignite strong emotions and deeply held convictions. It’s not hard to quickly become embroiled in passionate and engaged debate.
While discussion and discourse are healthy, these are bleeding into professional spheres, creating rifts within our clinical communities and contributing to a culture where not everyone feels safe. Look at any professional listserv in medicine or psychology and you will find the evidence. It should be an immediate call to action that we need to be fostering a different type of environment.
The impact of divisiveness is profound, hindering opportunities for collaboration, mentorship, and the free exchange of ideas among clinicians. It may lead to misunderstandings, mistrust, and an erosion of the support systems we rely on, ultimately diverting energy away from the pursuit of providing quality patient-care.
Balancing obligations and limits
Because of the inherent power differential that accompanies being in a provider role (physician and psychologist alike), we have a social and moral responsibility to be mindful of what we share – for the sake of humanity. There is an implicit assumption that a provider’s guidance should be adhered to and respected. In other words, words carry tremendous weight and deeply matter, and people in the general public ascribe significant meaning to messages put out by professionals.
When providers steer from their lanes of professional expertise to provide the general public with opinions or recommendations on nonmedical topics, problematic precedents can be set. We may be doing people a disservice.
Unfortunately, I have heard several anecdotes about clinicians who spend their patient’s time in session pushing their own ideological agendas. The patient-provider relationship is founded on principles of trust, empathy, and collaboration, with the primary goal of improving overall well-being and addressing a specific presenting problem. Of course, issues emerge that need to be addressed outside of the initial scope of treatment, an inherent part of the process. However, a grave concern emerges when clinicians initiate dialogue that is not meaningful to a patient, disclose and discuss their personal ideologies, or put pressure on patients to explain their beliefs in an attempt to change the patients’ minds.
Clinicians pushing their own agenda during patient sessions is antithetical to the objectives of psychotherapy and compromises the therapeutic alliance by diverting the focus of care in a way that serves the clinician rather than the client. It is quite the opposite of the patient-centered care that we strive for in training and practice.
Even within one’s theoretical professional scope of competence, I have seen the impact of emotions running high during this conflict, and have witnessed trained professionals making light of, or even mocking, hostages and their behavior upon release. These are care providers who could elucidate the complexities of captor-captive dynamics and the impact of trauma for the general public, yet they are contributing to dangerous perceptions and divisiveness.
I have also seen providers justify sexual violence, diminishing survivor and witness testimony due to ideological differences and strong personal beliefs. This is harmful to those impacted and does a disservice to our profession at large. In a helping profession we should strive to support and advocate for anyone who has been maltreated or experienced any form of victimization, violence, or abuse. This should be a professional standard.
As clinicians, we have an ethical obligation to uphold the well-being, autonomy, and dignity of our patients — and humanity. It is crucial to recognize the limits of our expertise and the ethical concerns that can arise in light of geopolitical conflict. How can we balance our duty to provide psychological support while also being cautious about delving into the realms of political analysis, foreign policy, or international relations?
The pitfalls of well-intentioned speaking out
In the age of social media and instant communication, a critical aspect to consider is the role of speaking out. The point I made above, in naming all partaking in the current conflict, speaks to this issue.
As providers and programs, we must be mindful of the inadvertent harm that can arise from making brief, underdeveloped, uninformed, or emotionally charged statements. Expressing opinions without a solid understanding of the historical, cultural, and political nuances of a conflict can contribute to misinformation and further polarization.
Anecdotally, there appears to be some significant degree of bias emerging within professional fields (e.g., psychology, medicine) and an innate calling for providers to “weigh in” as the war continues. Obviously, physicians and psychologists are trained to provide care and to be humanistic and empathic, but the majority do not have expertise in geopolitics or a nuanced awareness of the complexities of the conflict in the Middle East.
While hearts may be in the right place, issuing statements on complicated humanitarian/political situations can inadvertently have unintended and harmful consequences (in terms of antisemitism and islamophobia, increased incidence of hate crimes, and colleagues not feeling safe within professional societies or member organizations).
Unsophisticated, overly simplistic, and reductionistic statements that do not adequately convey nuance will not reflect the range of experience reflected by providers in the field (or the patients we treat). It is essential for clinicians and institutions putting out public statements to engage in deep reflection and utilize discernment. We must recognize that our words carry weight, given our position of influence as treatment providers. To minimize harm, we should seek to provide information that is fair, vetted, and balanced, and encourage open, respectful dialogue rather than asserting definitive positions.
Ultimately, as providers we must strive to seek unity and inclusivity amidst the current challenges. It is important for us to embody a spirit of collaboration during a time demarcated by deep fragmentation.
By acknowledging our limitations, promoting informed discussion, and avoiding the pitfalls of uninformed advocacy, we can contribute to a more compassionate and understanding world, even in the face of the most divisive geopolitical conflicts. We have an obligation to uphold when it comes to ourselves as professionals, and we need to foster healthy, respectful dialogue while maintaining an awareness of our blind spots.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She is an affiliate of Baptist West Kendall Hospital/FIU Family Medicine Residency Program and serves as president on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. The opinions expressed by Dr. Feldman are her own and do not represent the institutions with which she is affiliated. She has no disclosures.
In the realm of clinical psychology and psychiatry, our primary duty and commitment is (and should be) to the well-being of our patients. Yet, as we find ourselves in an era marked by escalating geopolitical conflict, such as the Israel-Hamas war, probably more aptly titled the Israeli-Hamas-Hezbollah-Houthi war (a clarification that elucidates a later point), clinicians are increasingly confronted with ethical dilemmas that extend far beyond what is outlined in our code of ethics.
These challenges are not only impacting us on a personal level but are also spilling over into our professional lives, creating a divisive and non-collegial environment within the healthcare community. We commit to “do no harm” when delivering care and yet we are doing harm to one another as colleagues.
We are no strangers to the complexities of human behavior and the intricate tapestry of emotions that are involved with our professional work. However, the current geopolitical landscape has added an extra layer of difficulty to our already taxing professional lives. We are, after all, human first with unconscious drives that govern how we negotiate cognitive dissonance and our need for the illusion of absolute justice as Yuval Noah Harari explains in a recent podcast.
Humans are notoriously bad at holding the multiplicity of experience in mind and various (often competing narratives) that impede the capacity for nuanced thinking. We would like to believe we are better and more capable than the average person in doing so, but divisiveness in our profession has become disturbingly pronounced, making it essential for us to carve out reflective space, more than ever.
The personal and professional divide
Geopolitical conflicts like the current war have a unique capacity to ignite strong emotions and deeply held convictions. It’s not hard to quickly become embroiled in passionate and engaged debate.
While discussion and discourse are healthy, these are bleeding into professional spheres, creating rifts within our clinical communities and contributing to a culture where not everyone feels safe. Look at any professional listserv in medicine or psychology and you will find the evidence. It should be an immediate call to action that we need to be fostering a different type of environment.
The impact of divisiveness is profound, hindering opportunities for collaboration, mentorship, and the free exchange of ideas among clinicians. It may lead to misunderstandings, mistrust, and an erosion of the support systems we rely on, ultimately diverting energy away from the pursuit of providing quality patient-care.
Balancing obligations and limits
Because of the inherent power differential that accompanies being in a provider role (physician and psychologist alike), we have a social and moral responsibility to be mindful of what we share – for the sake of humanity. There is an implicit assumption that a provider’s guidance should be adhered to and respected. In other words, words carry tremendous weight and deeply matter, and people in the general public ascribe significant meaning to messages put out by professionals.
When providers steer from their lanes of professional expertise to provide the general public with opinions or recommendations on nonmedical topics, problematic precedents can be set. We may be doing people a disservice.
Unfortunately, I have heard several anecdotes about clinicians who spend their patient’s time in session pushing their own ideological agendas. The patient-provider relationship is founded on principles of trust, empathy, and collaboration, with the primary goal of improving overall well-being and addressing a specific presenting problem. Of course, issues emerge that need to be addressed outside of the initial scope of treatment, an inherent part of the process. However, a grave concern emerges when clinicians initiate dialogue that is not meaningful to a patient, disclose and discuss their personal ideologies, or put pressure on patients to explain their beliefs in an attempt to change the patients’ minds.
Clinicians pushing their own agenda during patient sessions is antithetical to the objectives of psychotherapy and compromises the therapeutic alliance by diverting the focus of care in a way that serves the clinician rather than the client. It is quite the opposite of the patient-centered care that we strive for in training and practice.
Even within one’s theoretical professional scope of competence, I have seen the impact of emotions running high during this conflict, and have witnessed trained professionals making light of, or even mocking, hostages and their behavior upon release. These are care providers who could elucidate the complexities of captor-captive dynamics and the impact of trauma for the general public, yet they are contributing to dangerous perceptions and divisiveness.
I have also seen providers justify sexual violence, diminishing survivor and witness testimony due to ideological differences and strong personal beliefs. This is harmful to those impacted and does a disservice to our profession at large. In a helping profession we should strive to support and advocate for anyone who has been maltreated or experienced any form of victimization, violence, or abuse. This should be a professional standard.
As clinicians, we have an ethical obligation to uphold the well-being, autonomy, and dignity of our patients — and humanity. It is crucial to recognize the limits of our expertise and the ethical concerns that can arise in light of geopolitical conflict. How can we balance our duty to provide psychological support while also being cautious about delving into the realms of political analysis, foreign policy, or international relations?
The pitfalls of well-intentioned speaking out
In the age of social media and instant communication, a critical aspect to consider is the role of speaking out. The point I made above, in naming all partaking in the current conflict, speaks to this issue.
As providers and programs, we must be mindful of the inadvertent harm that can arise from making brief, underdeveloped, uninformed, or emotionally charged statements. Expressing opinions without a solid understanding of the historical, cultural, and political nuances of a conflict can contribute to misinformation and further polarization.
Anecdotally, there appears to be some significant degree of bias emerging within professional fields (e.g., psychology, medicine) and an innate calling for providers to “weigh in” as the war continues. Obviously, physicians and psychologists are trained to provide care and to be humanistic and empathic, but the majority do not have expertise in geopolitics or a nuanced awareness of the complexities of the conflict in the Middle East.
While hearts may be in the right place, issuing statements on complicated humanitarian/political situations can inadvertently have unintended and harmful consequences (in terms of antisemitism and islamophobia, increased incidence of hate crimes, and colleagues not feeling safe within professional societies or member organizations).
Unsophisticated, overly simplistic, and reductionistic statements that do not adequately convey nuance will not reflect the range of experience reflected by providers in the field (or the patients we treat). It is essential for clinicians and institutions putting out public statements to engage in deep reflection and utilize discernment. We must recognize that our words carry weight, given our position of influence as treatment providers. To minimize harm, we should seek to provide information that is fair, vetted, and balanced, and encourage open, respectful dialogue rather than asserting definitive positions.
Ultimately, as providers we must strive to seek unity and inclusivity amidst the current challenges. It is important for us to embody a spirit of collaboration during a time demarcated by deep fragmentation.
By acknowledging our limitations, promoting informed discussion, and avoiding the pitfalls of uninformed advocacy, we can contribute to a more compassionate and understanding world, even in the face of the most divisive geopolitical conflicts. We have an obligation to uphold when it comes to ourselves as professionals, and we need to foster healthy, respectful dialogue while maintaining an awareness of our blind spots.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She is an affiliate of Baptist West Kendall Hospital/FIU Family Medicine Residency Program and serves as president on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. The opinions expressed by Dr. Feldman are her own and do not represent the institutions with which she is affiliated. She has no disclosures.
EMRs: gumming up the works
I don’t like EMR systems, with all their requirements, click boxes, endless cut & paste abuse, and 20-page notes that say nothing.
But I am a fan of what computers have brought to medical charts.
When I started out in 2000, I had no patients, hence no charts. I had the advantage of being able to start from scratch — there was nothing to convert to digital. So, from the beginning, that’s how I went. Back then, of course, everything came to the office as paper. It had to be scanned in, then named, then placed in the right computer file.
But it was still easier than amassing paper records. At that time I subleased from a doc who’d been in practice for 15 years. His charts were all paper. Charts were neatly filed on shelves, everything was initialed, hole-punched, and put in the right section (which involved pulling out other stuff and putting it back). A few times a year, his staff would comb through the charts in front, and anyone who hadn’t been seen in 2 years would have their chart moved to a storage room in the back. Once a year they’d pull the charts of anyone not seen in 7 years and a company would come in and shred those records.
After 23 years, I still have it all. The whole thing takes up a little over 50 gigabytes on a hard drive, which realistically is nothing these days. Electrons don’t take up much space.
The majority of the charts — those that are more than 7 years old — I’ll probably never need to access, but it still happens sometimes. People call in and say they’ve moved back to Phoenix, or need to see a neurologist again, or need the records for insurance reasons, or whatever. My staff is also spared from moving charts to a storage room, then to shredding. Since they don’t take up any physical space, it’s no effort to keep everything.
And they aren’t just at my office. They’re at home, on my phone, wherever I am. If I get called from an ER, I can pull them up quickly. If I travel, they’re with me. My memory is good, but not that good, and I’d rather be able to look things up than guess.
This, at least to me, is the advantage of computers. Their data storage and retrieval advantages far exceed that of paper. In my opinion EMRs, while well-intentioned, have taken these benefits and twisted them into something cumbersome, geared more to meet nonmedical requirements and billing purposes.
In the process they’ve lost sight of our age-old job of caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t like EMR systems, with all their requirements, click boxes, endless cut & paste abuse, and 20-page notes that say nothing.
But I am a fan of what computers have brought to medical charts.
When I started out in 2000, I had no patients, hence no charts. I had the advantage of being able to start from scratch — there was nothing to convert to digital. So, from the beginning, that’s how I went. Back then, of course, everything came to the office as paper. It had to be scanned in, then named, then placed in the right computer file.
But it was still easier than amassing paper records. At that time I subleased from a doc who’d been in practice for 15 years. His charts were all paper. Charts were neatly filed on shelves, everything was initialed, hole-punched, and put in the right section (which involved pulling out other stuff and putting it back). A few times a year, his staff would comb through the charts in front, and anyone who hadn’t been seen in 2 years would have their chart moved to a storage room in the back. Once a year they’d pull the charts of anyone not seen in 7 years and a company would come in and shred those records.
After 23 years, I still have it all. The whole thing takes up a little over 50 gigabytes on a hard drive, which realistically is nothing these days. Electrons don’t take up much space.
The majority of the charts — those that are more than 7 years old — I’ll probably never need to access, but it still happens sometimes. People call in and say they’ve moved back to Phoenix, or need to see a neurologist again, or need the records for insurance reasons, or whatever. My staff is also spared from moving charts to a storage room, then to shredding. Since they don’t take up any physical space, it’s no effort to keep everything.
And they aren’t just at my office. They’re at home, on my phone, wherever I am. If I get called from an ER, I can pull them up quickly. If I travel, they’re with me. My memory is good, but not that good, and I’d rather be able to look things up than guess.
This, at least to me, is the advantage of computers. Their data storage and retrieval advantages far exceed that of paper. In my opinion EMRs, while well-intentioned, have taken these benefits and twisted them into something cumbersome, geared more to meet nonmedical requirements and billing purposes.
In the process they’ve lost sight of our age-old job of caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t like EMR systems, with all their requirements, click boxes, endless cut & paste abuse, and 20-page notes that say nothing.
But I am a fan of what computers have brought to medical charts.
When I started out in 2000, I had no patients, hence no charts. I had the advantage of being able to start from scratch — there was nothing to convert to digital. So, from the beginning, that’s how I went. Back then, of course, everything came to the office as paper. It had to be scanned in, then named, then placed in the right computer file.
But it was still easier than amassing paper records. At that time I subleased from a doc who’d been in practice for 15 years. His charts were all paper. Charts were neatly filed on shelves, everything was initialed, hole-punched, and put in the right section (which involved pulling out other stuff and putting it back). A few times a year, his staff would comb through the charts in front, and anyone who hadn’t been seen in 2 years would have their chart moved to a storage room in the back. Once a year they’d pull the charts of anyone not seen in 7 years and a company would come in and shred those records.
After 23 years, I still have it all. The whole thing takes up a little over 50 gigabytes on a hard drive, which realistically is nothing these days. Electrons don’t take up much space.
The majority of the charts — those that are more than 7 years old — I’ll probably never need to access, but it still happens sometimes. People call in and say they’ve moved back to Phoenix, or need to see a neurologist again, or need the records for insurance reasons, or whatever. My staff is also spared from moving charts to a storage room, then to shredding. Since they don’t take up any physical space, it’s no effort to keep everything.
And they aren’t just at my office. They’re at home, on my phone, wherever I am. If I get called from an ER, I can pull them up quickly. If I travel, they’re with me. My memory is good, but not that good, and I’d rather be able to look things up than guess.
This, at least to me, is the advantage of computers. Their data storage and retrieval advantages far exceed that of paper. In my opinion EMRs, while well-intentioned, have taken these benefits and twisted them into something cumbersome, geared more to meet nonmedical requirements and billing purposes.
In the process they’ve lost sight of our age-old job of caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
An alternative to walking out
Organized labor seems to be experiencing a rebirth of sorts. In October 2022 a strike by railroad workers was averted when a tentative agreement about wages, working conditions, health insurance, and medical leave was hammered out. This past fall, strikes by auto workers that threatened to paralyze the big three manufacturers have now been resolved with agreements that meet many of the workers’ demands. The President even made an appearance on a picket line. Baristas at coffee shops, screenwriters, and actors have all been involved in work actions around the country.
While the health care industry has been relatively immune to threatened work stoppages, there are a growing number of hospitals and clinics where nurses and physicians are exploring the possibility of organizing to give themselves a stronger voice in how health care is being delivered. The realities that come when you transition from owner to employee are finally beginning to sink in for physicians, whether they are specialists or primary care providers.
One of the most significant efforts toward unionization recently occurred in Minnesota and Wisconsin. About 400 physicians and 150 physician’s assistants and nurse practitioners employed at Allina Health System voted to unionize and join the Doctors Council.
In an interview with Jacobin, a publication that offers a socialist perspective, three of the providers involved in the process that led to the vote shared their observations. The physicians claim that the first steps toward unionization came after multiple efforts to work with the Allina’s administration were rebuffed. As primary care physicians, their initial demands focused on getting help with hiring staffing and getting support with paperwork and administrative obligations.
The organizers complained that while Medicare hoped to bolster primary care by paying the providers more, the funds went to the companies, who then distributed them in a way that often did little to help the overworked providers. In addition to achieving a more equitable distribution of the monies, one of the organizers sees unionization as a way to provide a layer of protection when providers feel they must speak out about situations which clearly put quality of care at risk.
The organizers say the idea of unionization has been particularly appealing to the younger providers who are feeling threatened by burnout. When these new physicians look to their older coworkers for advice, they often find that the seasoned employees are as stressed as they are. Realizing that things aren’t going to improve with time, acting now to strengthen their voices sounds appealing.
With the vote for unionization behind them, the organizers are now ready to formulate a prioritized list of demands. Those of you who are regular readers of Letters from Maine know that I have been urging primary care physicians to find their voices. Unfortunately, unionization seems to be becoming a more common fall-back strategy when other avenues have failed to reach a sympathetic ear in the corporate boardrooms.
As more unions form, it will be interesting to see how the organizers structure their demands and job actions. While walkouts and strikes can certainly be effective in gaining attention, that attention can carry a risk of counter productivity sometimes by alienating patients, who should become allies.
Since an unsustainable burden of paperwork and administrative demands seems to be at the top of everyone’s priority list, it might make sense to adopt this message as a scaffolding on which to built a work action. Instead of walking off the job or marching on a picket line, why not stay in the hospital and continue to see patients but only for part of the work day. The remainder of the day would be spent doing all the clerical work that has become so onerous.
Providers would agree to see patients in the mornings, saving up the clerical work and administrative obligations for the afternoon. The definition of “morning” could vary depending on local conditions.
The important message to the public and the patients would be that the providers were not abandoning them by walking out. The patients’ access to face-to-face care was being limited not because the doctors didn’t want to see them but because the providers were being forced to accept other responsibilities by the administration. The physicians would always be on site in case of a crisis, but until reasonable demands for support from the company were met, a certain portion of the providers’ day would be spent doing things not directly related to face-to-face patient care. This burden of meaningless work is the reality as it stands already. Why not organize it in a way that makes it startlingly visible to the patients and the public.
There would be no video clips of physicians walking the picket lines carrying signs. Any images released to the media would be of empty waiting rooms while providers sat hunched over their computers or talking on the phone to insurance companies.
The strategy needs a catchy phrase like “a paperwork-in” but I’m still struggling with a name. Let me know if you have a better one or even a better strategy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Organized labor seems to be experiencing a rebirth of sorts. In October 2022 a strike by railroad workers was averted when a tentative agreement about wages, working conditions, health insurance, and medical leave was hammered out. This past fall, strikes by auto workers that threatened to paralyze the big three manufacturers have now been resolved with agreements that meet many of the workers’ demands. The President even made an appearance on a picket line. Baristas at coffee shops, screenwriters, and actors have all been involved in work actions around the country.
While the health care industry has been relatively immune to threatened work stoppages, there are a growing number of hospitals and clinics where nurses and physicians are exploring the possibility of organizing to give themselves a stronger voice in how health care is being delivered. The realities that come when you transition from owner to employee are finally beginning to sink in for physicians, whether they are specialists or primary care providers.
One of the most significant efforts toward unionization recently occurred in Minnesota and Wisconsin. About 400 physicians and 150 physician’s assistants and nurse practitioners employed at Allina Health System voted to unionize and join the Doctors Council.
In an interview with Jacobin, a publication that offers a socialist perspective, three of the providers involved in the process that led to the vote shared their observations. The physicians claim that the first steps toward unionization came after multiple efforts to work with the Allina’s administration were rebuffed. As primary care physicians, their initial demands focused on getting help with hiring staffing and getting support with paperwork and administrative obligations.
The organizers complained that while Medicare hoped to bolster primary care by paying the providers more, the funds went to the companies, who then distributed them in a way that often did little to help the overworked providers. In addition to achieving a more equitable distribution of the monies, one of the organizers sees unionization as a way to provide a layer of protection when providers feel they must speak out about situations which clearly put quality of care at risk.
The organizers say the idea of unionization has been particularly appealing to the younger providers who are feeling threatened by burnout. When these new physicians look to their older coworkers for advice, they often find that the seasoned employees are as stressed as they are. Realizing that things aren’t going to improve with time, acting now to strengthen their voices sounds appealing.
With the vote for unionization behind them, the organizers are now ready to formulate a prioritized list of demands. Those of you who are regular readers of Letters from Maine know that I have been urging primary care physicians to find their voices. Unfortunately, unionization seems to be becoming a more common fall-back strategy when other avenues have failed to reach a sympathetic ear in the corporate boardrooms.
As more unions form, it will be interesting to see how the organizers structure their demands and job actions. While walkouts and strikes can certainly be effective in gaining attention, that attention can carry a risk of counter productivity sometimes by alienating patients, who should become allies.
Since an unsustainable burden of paperwork and administrative demands seems to be at the top of everyone’s priority list, it might make sense to adopt this message as a scaffolding on which to built a work action. Instead of walking off the job or marching on a picket line, why not stay in the hospital and continue to see patients but only for part of the work day. The remainder of the day would be spent doing all the clerical work that has become so onerous.
Providers would agree to see patients in the mornings, saving up the clerical work and administrative obligations for the afternoon. The definition of “morning” could vary depending on local conditions.
The important message to the public and the patients would be that the providers were not abandoning them by walking out. The patients’ access to face-to-face care was being limited not because the doctors didn’t want to see them but because the providers were being forced to accept other responsibilities by the administration. The physicians would always be on site in case of a crisis, but until reasonable demands for support from the company were met, a certain portion of the providers’ day would be spent doing things not directly related to face-to-face patient care. This burden of meaningless work is the reality as it stands already. Why not organize it in a way that makes it startlingly visible to the patients and the public.
There would be no video clips of physicians walking the picket lines carrying signs. Any images released to the media would be of empty waiting rooms while providers sat hunched over their computers or talking on the phone to insurance companies.
The strategy needs a catchy phrase like “a paperwork-in” but I’m still struggling with a name. Let me know if you have a better one or even a better strategy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Organized labor seems to be experiencing a rebirth of sorts. In October 2022 a strike by railroad workers was averted when a tentative agreement about wages, working conditions, health insurance, and medical leave was hammered out. This past fall, strikes by auto workers that threatened to paralyze the big three manufacturers have now been resolved with agreements that meet many of the workers’ demands. The President even made an appearance on a picket line. Baristas at coffee shops, screenwriters, and actors have all been involved in work actions around the country.
While the health care industry has been relatively immune to threatened work stoppages, there are a growing number of hospitals and clinics where nurses and physicians are exploring the possibility of organizing to give themselves a stronger voice in how health care is being delivered. The realities that come when you transition from owner to employee are finally beginning to sink in for physicians, whether they are specialists or primary care providers.
One of the most significant efforts toward unionization recently occurred in Minnesota and Wisconsin. About 400 physicians and 150 physician’s assistants and nurse practitioners employed at Allina Health System voted to unionize and join the Doctors Council.
In an interview with Jacobin, a publication that offers a socialist perspective, three of the providers involved in the process that led to the vote shared their observations. The physicians claim that the first steps toward unionization came after multiple efforts to work with the Allina’s administration were rebuffed. As primary care physicians, their initial demands focused on getting help with hiring staffing and getting support with paperwork and administrative obligations.
The organizers complained that while Medicare hoped to bolster primary care by paying the providers more, the funds went to the companies, who then distributed them in a way that often did little to help the overworked providers. In addition to achieving a more equitable distribution of the monies, one of the organizers sees unionization as a way to provide a layer of protection when providers feel they must speak out about situations which clearly put quality of care at risk.
The organizers say the idea of unionization has been particularly appealing to the younger providers who are feeling threatened by burnout. When these new physicians look to their older coworkers for advice, they often find that the seasoned employees are as stressed as they are. Realizing that things aren’t going to improve with time, acting now to strengthen their voices sounds appealing.
With the vote for unionization behind them, the organizers are now ready to formulate a prioritized list of demands. Those of you who are regular readers of Letters from Maine know that I have been urging primary care physicians to find their voices. Unfortunately, unionization seems to be becoming a more common fall-back strategy when other avenues have failed to reach a sympathetic ear in the corporate boardrooms.
As more unions form, it will be interesting to see how the organizers structure their demands and job actions. While walkouts and strikes can certainly be effective in gaining attention, that attention can carry a risk of counter productivity sometimes by alienating patients, who should become allies.
Since an unsustainable burden of paperwork and administrative demands seems to be at the top of everyone’s priority list, it might make sense to adopt this message as a scaffolding on which to built a work action. Instead of walking off the job or marching on a picket line, why not stay in the hospital and continue to see patients but only for part of the work day. The remainder of the day would be spent doing all the clerical work that has become so onerous.
Providers would agree to see patients in the mornings, saving up the clerical work and administrative obligations for the afternoon. The definition of “morning” could vary depending on local conditions.
The important message to the public and the patients would be that the providers were not abandoning them by walking out. The patients’ access to face-to-face care was being limited not because the doctors didn’t want to see them but because the providers were being forced to accept other responsibilities by the administration. The physicians would always be on site in case of a crisis, but until reasonable demands for support from the company were met, a certain portion of the providers’ day would be spent doing things not directly related to face-to-face patient care. This burden of meaningless work is the reality as it stands already. Why not organize it in a way that makes it startlingly visible to the patients and the public.
There would be no video clips of physicians walking the picket lines carrying signs. Any images released to the media would be of empty waiting rooms while providers sat hunched over their computers or talking on the phone to insurance companies.
The strategy needs a catchy phrase like “a paperwork-in” but I’m still struggling with a name. Let me know if you have a better one or even a better strategy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Are you sure your patient is alive?
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.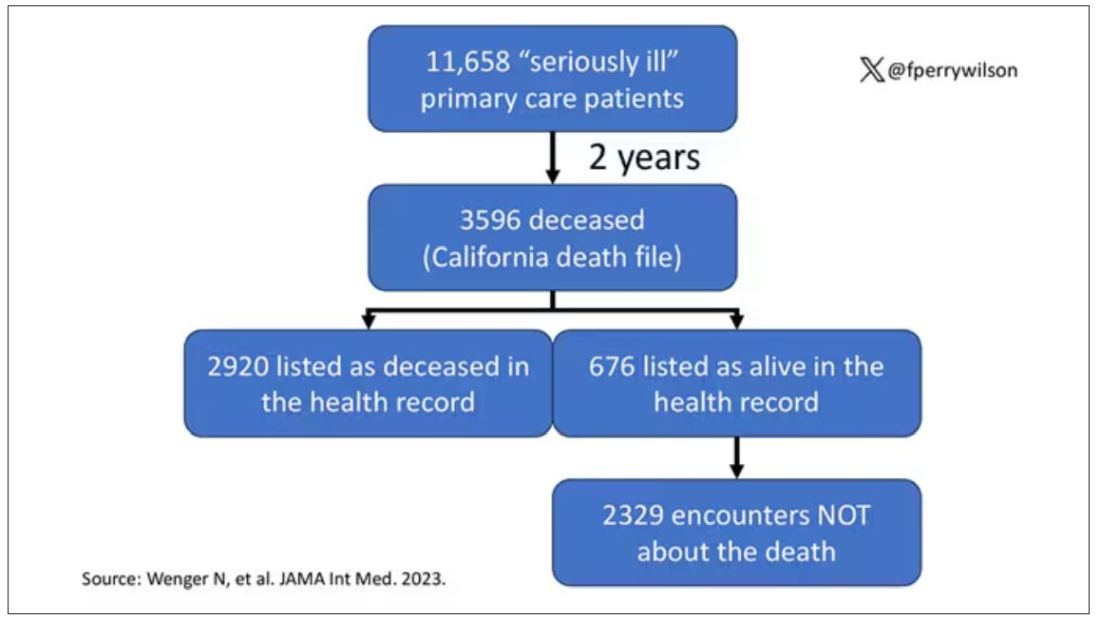
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.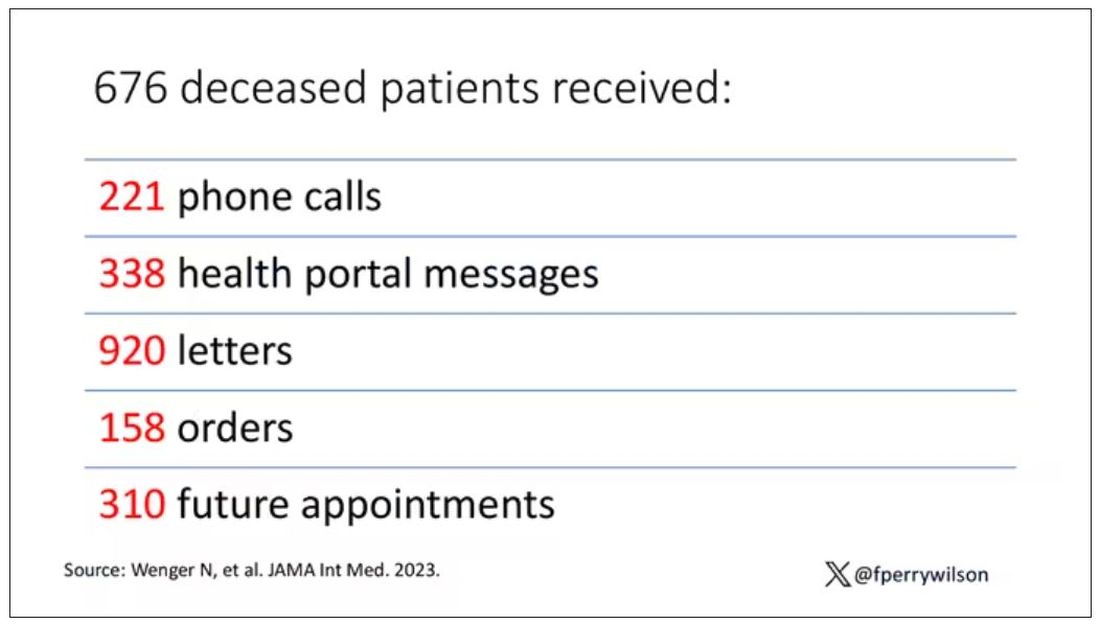
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.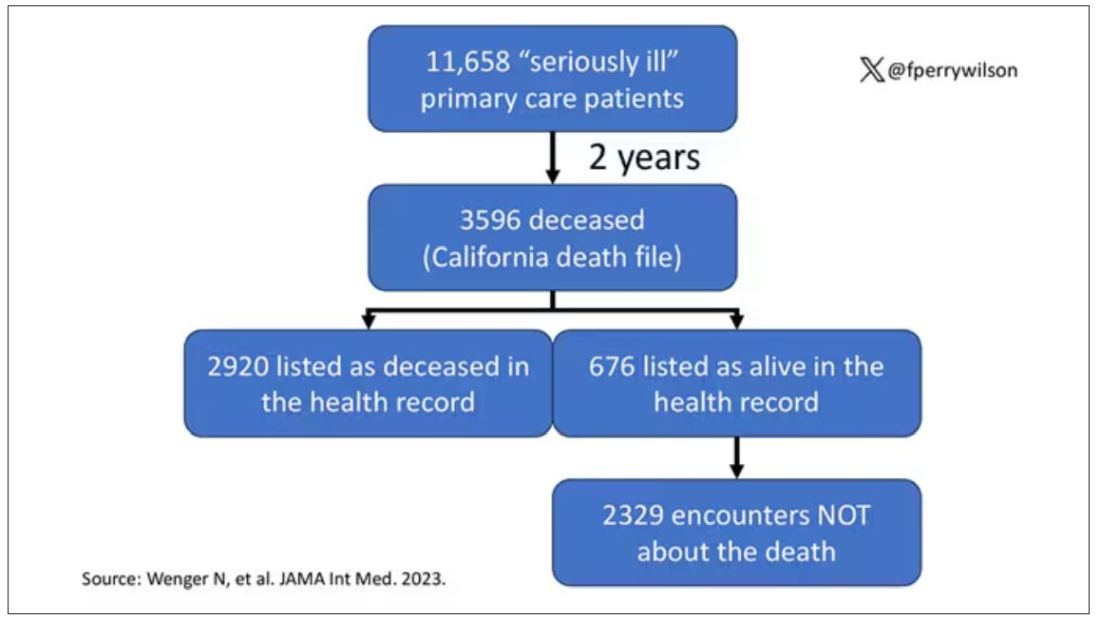
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.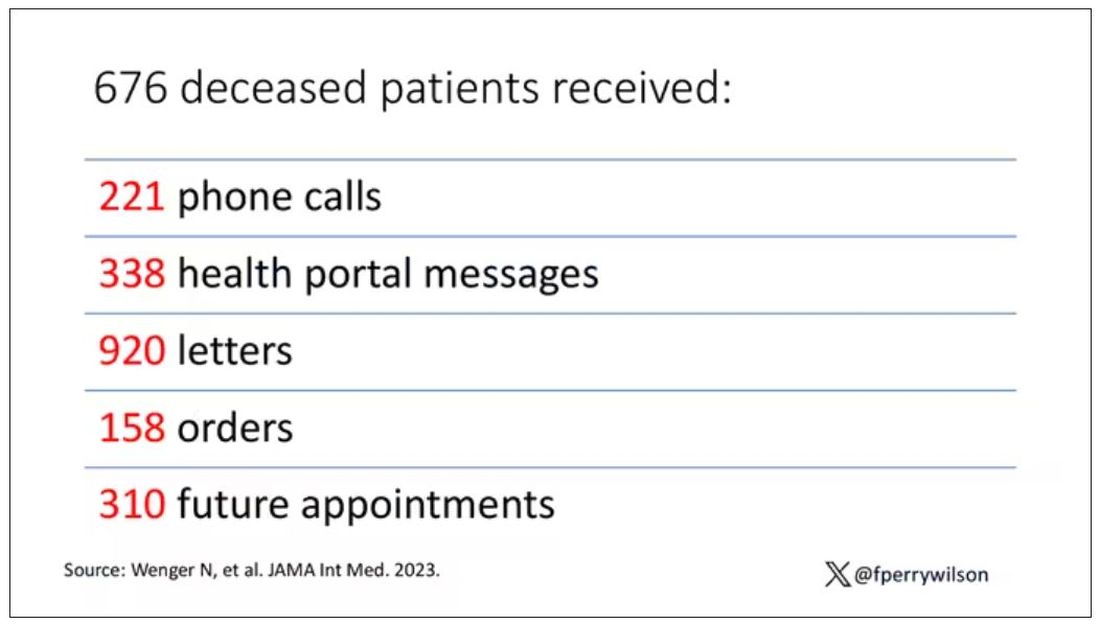
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.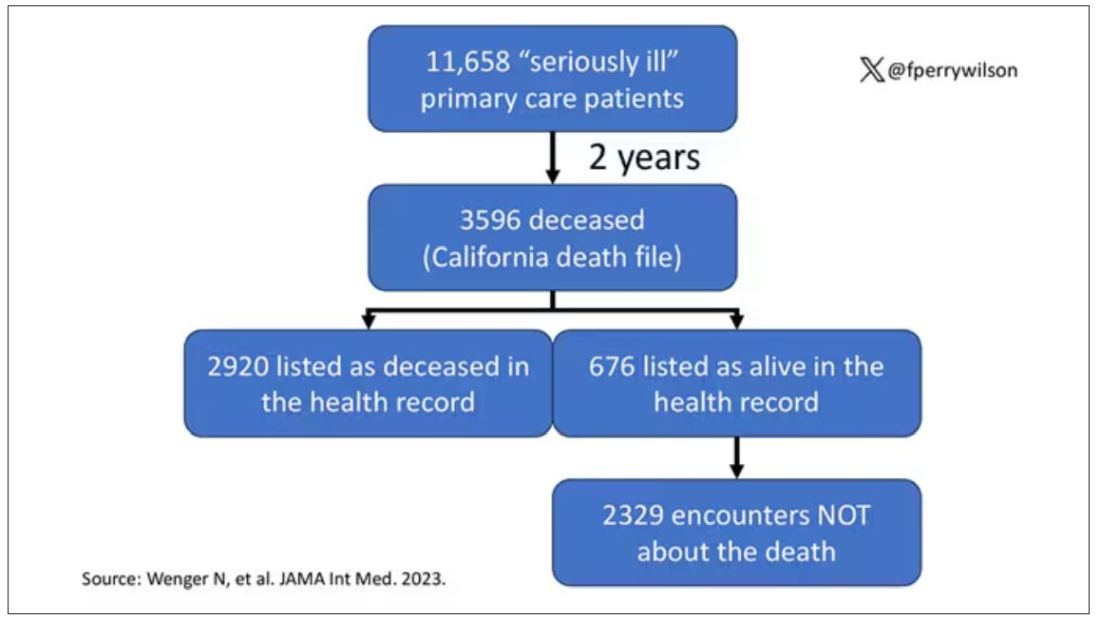
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.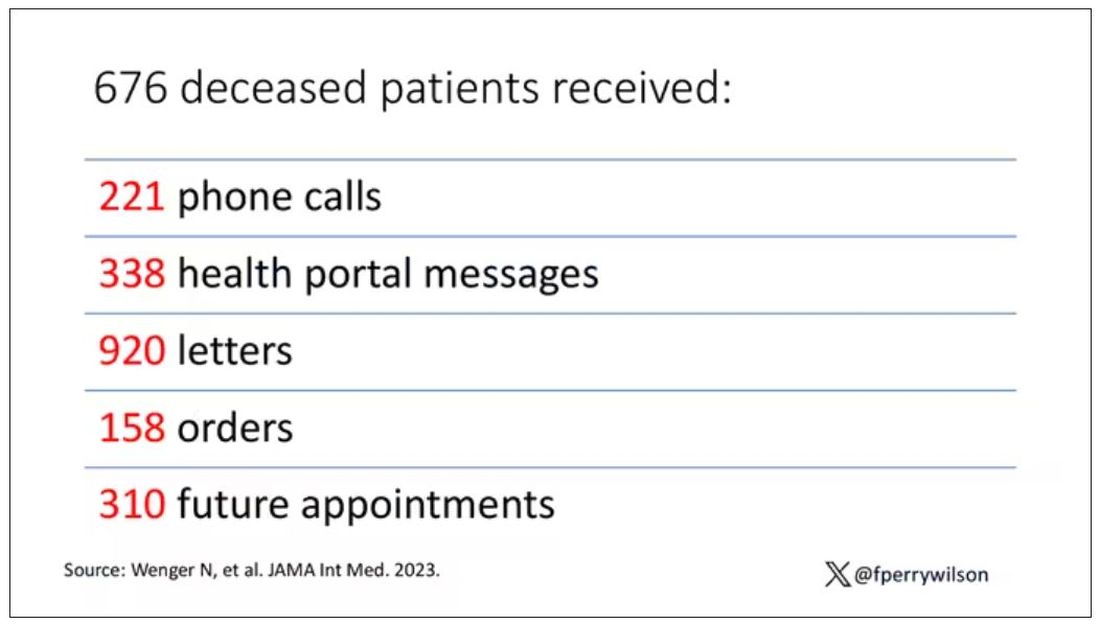
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
Eight wealth tips just for doctors
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
Patients exposed to HIV, hepatitis at Massachusetts hospital
The negligent administration of intravenous medications during endoscopy procedures performed between June 14, 2021, and April 19, 2023, at Salem Hospital, located about 20 miles northeast of Boston, has caused a “heightened risk of exposure to these harmful life-altering and life-threatening infections,” according to the lawsuit filed at Suffolk County Superior Court in Boston by Keches Law Group on behalf of plaintiff Melinda Cashman and others.
Although patients were notified in early November of their potential exposure, it could take months or even years to determine if infection has occurred. Attorneys for Ms. Cashman claim that the plaintiff “suffered and will continue to suffer severe emotional distress and anguish” as a result of the associated risks.
The lawyers argue that Ms. Cashman and others like her may “suffer permanent injuries,” along with “extreme anxiety and decreased quality of life.” They are seeking monetary damages to offset disruptions to relationships, increased medical bills, and any mental health therapy required.
Outreach to potentially affected patients began after the hospital was made aware, earlier this year, of an “isolated practice” that could have led to viral transmission, according to a statement from Mass General Brigham, but there is no evidence to date of any infections resulting from this incident. “We sincerely apologize to those who have been impacted and we remain committed to delivering high-quality, compassionate healthcare to our community.”
Hepatitis B and C are both treatable with antiviral mediations, and hepatitis C is curable in 95% of cases, according to the Centers for Disease Control and Prevention. HIV, although not curable, can be managed with antiretroviral therapy.
Mass General Brigham is working with the Massachusetts Department of Public Health, which will conduct an onsite investigation into quality-control practices. Affected patients can reach out to a clinician-staffed hotline with questions and receive free screening for the viruses, hospital officials report.
A version of this article appeared on Medscape.com.
The negligent administration of intravenous medications during endoscopy procedures performed between June 14, 2021, and April 19, 2023, at Salem Hospital, located about 20 miles northeast of Boston, has caused a “heightened risk of exposure to these harmful life-altering and life-threatening infections,” according to the lawsuit filed at Suffolk County Superior Court in Boston by Keches Law Group on behalf of plaintiff Melinda Cashman and others.
Although patients were notified in early November of their potential exposure, it could take months or even years to determine if infection has occurred. Attorneys for Ms. Cashman claim that the plaintiff “suffered and will continue to suffer severe emotional distress and anguish” as a result of the associated risks.
The lawyers argue that Ms. Cashman and others like her may “suffer permanent injuries,” along with “extreme anxiety and decreased quality of life.” They are seeking monetary damages to offset disruptions to relationships, increased medical bills, and any mental health therapy required.
Outreach to potentially affected patients began after the hospital was made aware, earlier this year, of an “isolated practice” that could have led to viral transmission, according to a statement from Mass General Brigham, but there is no evidence to date of any infections resulting from this incident. “We sincerely apologize to those who have been impacted and we remain committed to delivering high-quality, compassionate healthcare to our community.”
Hepatitis B and C are both treatable with antiviral mediations, and hepatitis C is curable in 95% of cases, according to the Centers for Disease Control and Prevention. HIV, although not curable, can be managed with antiretroviral therapy.
Mass General Brigham is working with the Massachusetts Department of Public Health, which will conduct an onsite investigation into quality-control practices. Affected patients can reach out to a clinician-staffed hotline with questions and receive free screening for the viruses, hospital officials report.
A version of this article appeared on Medscape.com.
The negligent administration of intravenous medications during endoscopy procedures performed between June 14, 2021, and April 19, 2023, at Salem Hospital, located about 20 miles northeast of Boston, has caused a “heightened risk of exposure to these harmful life-altering and life-threatening infections,” according to the lawsuit filed at Suffolk County Superior Court in Boston by Keches Law Group on behalf of plaintiff Melinda Cashman and others.
Although patients were notified in early November of their potential exposure, it could take months or even years to determine if infection has occurred. Attorneys for Ms. Cashman claim that the plaintiff “suffered and will continue to suffer severe emotional distress and anguish” as a result of the associated risks.
The lawyers argue that Ms. Cashman and others like her may “suffer permanent injuries,” along with “extreme anxiety and decreased quality of life.” They are seeking monetary damages to offset disruptions to relationships, increased medical bills, and any mental health therapy required.
Outreach to potentially affected patients began after the hospital was made aware, earlier this year, of an “isolated practice” that could have led to viral transmission, according to a statement from Mass General Brigham, but there is no evidence to date of any infections resulting from this incident. “We sincerely apologize to those who have been impacted and we remain committed to delivering high-quality, compassionate healthcare to our community.”
Hepatitis B and C are both treatable with antiviral mediations, and hepatitis C is curable in 95% of cases, according to the Centers for Disease Control and Prevention. HIV, although not curable, can be managed with antiretroviral therapy.
Mass General Brigham is working with the Massachusetts Department of Public Health, which will conduct an onsite investigation into quality-control practices. Affected patients can reach out to a clinician-staffed hotline with questions and receive free screening for the viruses, hospital officials report.
A version of this article appeared on Medscape.com.
Rx for resilience: Five prescriptions for physician burnout
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.









