User login
VA Stops Rollout of Cerner EHR To Reset Amid Continued Problems
The painful paused and repaused rollout of the new Cerner electronic health record (EHR) system at the US Department of Veterans Affairs (VA) is now halted as the VA announces a “reset.” The decision applies to all planned deployments. An exception is the Captain James A. Lovell Federal Health Care Center in Chicago, the only fully integrated VA and US Department of Defense (DoD) health care system, which is expected go live in March 2024 as planned. The DoD rollout of its Cerner EHR is further along and expected to be completed in 2024.
The new plan is to redirect resources and “prioritize improvements” at the 5 sites currently using the new EHR: Spokane VA Health Care System, VA Walla Walla Health Care, Roseburg VA Health Care System, VA Southern Oregon Health Care, and VA Central Ohio Health Care System. Additional deployments will not be scheduled, the VA says, until it is confident that the new EHR is highly functioning at the current sites and ready to deliver at future sites, as demonstrated by “clear improvements” in the clinician and veteran experience, sustained high performance and high reliability.
“For the past few years, we’ve tried to fix this plane while flying it—and that hasn’t delivered the results that veterans or our staff deserve,” said Neil Evans, MD, acting program executive director at the Electronic Health Record Modernization Integration Office. “This reset changes that. We are going to take the time necessary to get this right for veterans and VA clinicians alike, and that means focusing our resources solely on improving the EHR at the sites where it is currently in use, and improving its fit for VA more broadly. In doing so, we will enhance the EHR for both current and future users, paving the way for successful future deployments.”
The various EHR rollouts around the country have been bumpy from the beginning, operating by fits and starts as new problems surfaced and were addressed. To be fair, the whole implementation process only started in 2020 (and deployed at the first VA hospital during the COVID-19 pandemic), but in that time, the VA has had to, in its own words, “revise the timeline” again and again. The Boise VA Medical Center, for instance, was originally scheduled to go live June 25, 2022, then a month later—then 2023.
The VA Office of the Inspector General published 3 reports last year that found significant issues, including improperly routed clinical orders. VA Secretary Denis McDonough announced last July that the VA would delay EHR deployments until January 2023 to ensure that the system’s issues had been resolved. “During VA’s subsequent investigation at our current sites,” he said, “several additional technical and system issues were identified—including challenges with performance, such as latency and slowness, problems with patient scheduling, referrals, medication management, and other types of medical orders.”
In February, Ken Glueck, executive vice president of Oracle, wrote a blog post that was both apologia and explanation. Modernization, he said, “doesn’t come with a magic wand and there’s no easy button.”
After the DoD moved to Cerner for a new EHR system, the VA decided to follow suit. The goal was to create a “seamless, longitudinal record”—and that was the beginning of the largest health IT modernization project in history, Glueck said. And, although he didn’t mention it, the beginning of one of the VA’s biggest headaches. The problem, Glueck wrote, was that the new project involved “standardizing procedures and workflows that may have been different across 130 VistA implementations at largely autonomous VA medical centers.”
In June 2022—a significant month in the whole rollout process—Cerner was acquired by Oracle. By Glueck’s lights, that meant the VA “now has essentially 2 vendors for the price of one—one with extensive clinical expertise and one with extensive engineering expertise.”
Oracle, he said, “is hard at work to stabilize and improve performance; make fixes to functionality and design issues; improve training and build a better user experience.” He noted that significant improvements to the system’s capacity and performance have included reducing the most severe outage incidents by 67%.
In a recent statement, House VA Committee Chairman Mike Bost (R-IL) and Technology Modernization Subcommittee Chairman Matt Rosendale (R-MT) said, “We support Secretary McDonough’s decision in the strongest possible terms. The best way to get out of a hole is to stop digging, and we’re encouraged that VA and Oracle Cerner have finally realized that.”
VA and Oracle Cerner are currently working toward an amended contract that will "increase Oracle Cerner’s accountability to deliver a high-functioning, high-reliability, world-class EHR system,” the VA says. As part of the re-set, the VA also will work with Congress on resource requirements. The VA estimates FY 2023 costs will be reduced by $400 million.
The painful paused and repaused rollout of the new Cerner electronic health record (EHR) system at the US Department of Veterans Affairs (VA) is now halted as the VA announces a “reset.” The decision applies to all planned deployments. An exception is the Captain James A. Lovell Federal Health Care Center in Chicago, the only fully integrated VA and US Department of Defense (DoD) health care system, which is expected go live in March 2024 as planned. The DoD rollout of its Cerner EHR is further along and expected to be completed in 2024.
The new plan is to redirect resources and “prioritize improvements” at the 5 sites currently using the new EHR: Spokane VA Health Care System, VA Walla Walla Health Care, Roseburg VA Health Care System, VA Southern Oregon Health Care, and VA Central Ohio Health Care System. Additional deployments will not be scheduled, the VA says, until it is confident that the new EHR is highly functioning at the current sites and ready to deliver at future sites, as demonstrated by “clear improvements” in the clinician and veteran experience, sustained high performance and high reliability.
“For the past few years, we’ve tried to fix this plane while flying it—and that hasn’t delivered the results that veterans or our staff deserve,” said Neil Evans, MD, acting program executive director at the Electronic Health Record Modernization Integration Office. “This reset changes that. We are going to take the time necessary to get this right for veterans and VA clinicians alike, and that means focusing our resources solely on improving the EHR at the sites where it is currently in use, and improving its fit for VA more broadly. In doing so, we will enhance the EHR for both current and future users, paving the way for successful future deployments.”
The various EHR rollouts around the country have been bumpy from the beginning, operating by fits and starts as new problems surfaced and were addressed. To be fair, the whole implementation process only started in 2020 (and deployed at the first VA hospital during the COVID-19 pandemic), but in that time, the VA has had to, in its own words, “revise the timeline” again and again. The Boise VA Medical Center, for instance, was originally scheduled to go live June 25, 2022, then a month later—then 2023.
The VA Office of the Inspector General published 3 reports last year that found significant issues, including improperly routed clinical orders. VA Secretary Denis McDonough announced last July that the VA would delay EHR deployments until January 2023 to ensure that the system’s issues had been resolved. “During VA’s subsequent investigation at our current sites,” he said, “several additional technical and system issues were identified—including challenges with performance, such as latency and slowness, problems with patient scheduling, referrals, medication management, and other types of medical orders.”
In February, Ken Glueck, executive vice president of Oracle, wrote a blog post that was both apologia and explanation. Modernization, he said, “doesn’t come with a magic wand and there’s no easy button.”
After the DoD moved to Cerner for a new EHR system, the VA decided to follow suit. The goal was to create a “seamless, longitudinal record”—and that was the beginning of the largest health IT modernization project in history, Glueck said. And, although he didn’t mention it, the beginning of one of the VA’s biggest headaches. The problem, Glueck wrote, was that the new project involved “standardizing procedures and workflows that may have been different across 130 VistA implementations at largely autonomous VA medical centers.”
In June 2022—a significant month in the whole rollout process—Cerner was acquired by Oracle. By Glueck’s lights, that meant the VA “now has essentially 2 vendors for the price of one—one with extensive clinical expertise and one with extensive engineering expertise.”
Oracle, he said, “is hard at work to stabilize and improve performance; make fixes to functionality and design issues; improve training and build a better user experience.” He noted that significant improvements to the system’s capacity and performance have included reducing the most severe outage incidents by 67%.
In a recent statement, House VA Committee Chairman Mike Bost (R-IL) and Technology Modernization Subcommittee Chairman Matt Rosendale (R-MT) said, “We support Secretary McDonough’s decision in the strongest possible terms. The best way to get out of a hole is to stop digging, and we’re encouraged that VA and Oracle Cerner have finally realized that.”
VA and Oracle Cerner are currently working toward an amended contract that will "increase Oracle Cerner’s accountability to deliver a high-functioning, high-reliability, world-class EHR system,” the VA says. As part of the re-set, the VA also will work with Congress on resource requirements. The VA estimates FY 2023 costs will be reduced by $400 million.
The painful paused and repaused rollout of the new Cerner electronic health record (EHR) system at the US Department of Veterans Affairs (VA) is now halted as the VA announces a “reset.” The decision applies to all planned deployments. An exception is the Captain James A. Lovell Federal Health Care Center in Chicago, the only fully integrated VA and US Department of Defense (DoD) health care system, which is expected go live in March 2024 as planned. The DoD rollout of its Cerner EHR is further along and expected to be completed in 2024.
The new plan is to redirect resources and “prioritize improvements” at the 5 sites currently using the new EHR: Spokane VA Health Care System, VA Walla Walla Health Care, Roseburg VA Health Care System, VA Southern Oregon Health Care, and VA Central Ohio Health Care System. Additional deployments will not be scheduled, the VA says, until it is confident that the new EHR is highly functioning at the current sites and ready to deliver at future sites, as demonstrated by “clear improvements” in the clinician and veteran experience, sustained high performance and high reliability.
“For the past few years, we’ve tried to fix this plane while flying it—and that hasn’t delivered the results that veterans or our staff deserve,” said Neil Evans, MD, acting program executive director at the Electronic Health Record Modernization Integration Office. “This reset changes that. We are going to take the time necessary to get this right for veterans and VA clinicians alike, and that means focusing our resources solely on improving the EHR at the sites where it is currently in use, and improving its fit for VA more broadly. In doing so, we will enhance the EHR for both current and future users, paving the way for successful future deployments.”
The various EHR rollouts around the country have been bumpy from the beginning, operating by fits and starts as new problems surfaced and were addressed. To be fair, the whole implementation process only started in 2020 (and deployed at the first VA hospital during the COVID-19 pandemic), but in that time, the VA has had to, in its own words, “revise the timeline” again and again. The Boise VA Medical Center, for instance, was originally scheduled to go live June 25, 2022, then a month later—then 2023.
The VA Office of the Inspector General published 3 reports last year that found significant issues, including improperly routed clinical orders. VA Secretary Denis McDonough announced last July that the VA would delay EHR deployments until January 2023 to ensure that the system’s issues had been resolved. “During VA’s subsequent investigation at our current sites,” he said, “several additional technical and system issues were identified—including challenges with performance, such as latency and slowness, problems with patient scheduling, referrals, medication management, and other types of medical orders.”
In February, Ken Glueck, executive vice president of Oracle, wrote a blog post that was both apologia and explanation. Modernization, he said, “doesn’t come with a magic wand and there’s no easy button.”
After the DoD moved to Cerner for a new EHR system, the VA decided to follow suit. The goal was to create a “seamless, longitudinal record”—and that was the beginning of the largest health IT modernization project in history, Glueck said. And, although he didn’t mention it, the beginning of one of the VA’s biggest headaches. The problem, Glueck wrote, was that the new project involved “standardizing procedures and workflows that may have been different across 130 VistA implementations at largely autonomous VA medical centers.”
In June 2022—a significant month in the whole rollout process—Cerner was acquired by Oracle. By Glueck’s lights, that meant the VA “now has essentially 2 vendors for the price of one—one with extensive clinical expertise and one with extensive engineering expertise.”
Oracle, he said, “is hard at work to stabilize and improve performance; make fixes to functionality and design issues; improve training and build a better user experience.” He noted that significant improvements to the system’s capacity and performance have included reducing the most severe outage incidents by 67%.
In a recent statement, House VA Committee Chairman Mike Bost (R-IL) and Technology Modernization Subcommittee Chairman Matt Rosendale (R-MT) said, “We support Secretary McDonough’s decision in the strongest possible terms. The best way to get out of a hole is to stop digging, and we’re encouraged that VA and Oracle Cerner have finally realized that.”
VA and Oracle Cerner are currently working toward an amended contract that will "increase Oracle Cerner’s accountability to deliver a high-functioning, high-reliability, world-class EHR system,” the VA says. As part of the re-set, the VA also will work with Congress on resource requirements. The VA estimates FY 2023 costs will be reduced by $400 million.
What are the main reasons patients sue dermatologists?
PHOENIX – , and the defendants were more likely to be male.
Those are among key findings from a study that aimed to determine the reasons patients pursue litigation against dermatologists.
“The number of lawsuits against physicians continues to climb annually,” Young Lim, MD, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the results were presented during an abstract session. “Depending on the study, anywhere between 75 to 99 percent of physicians will face a lawsuit by age 65. A clear understanding of prior litigations will help mitigate similar errors in future practice and promote safer, higher quality care.”
Dr. Lim, a dermatology resident at Massachusetts General Hospital and Harvard Medical School, Boston, along with Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at MGH, and H. Ray Jalian, MD, a cosmetic dermatologist who practices in Los Angeles, used two large national database repositories, WestlawNext and LexisNexis, to retrospectively analyze legal documents following a query using “dermatology” and “dermatologist” as search terms to capture all variety of litigations. They excluded cases in which litigation did not involve patient care as well as those in which the dermatologist was the plaintiff and those in which the dermatologist was involved as a third party.
The final analysis consisted of 54 claims, comprising 43 state and 11 federal cases. Of the 54 cases, 35 involved a male defendant, 12 involved a female defendant, and 7 cases either did not specify the gender of the defendant or involved multiple defendants. Of the 35 cases involving a male defendant, 23 (66%) were brought by female plaintiffs.
Most cases (49, or 91%) involved a defendant dermatologist in private practice while the remaining 5 involved a defendant dermatologist in an academic setting.
The most common reason for litigation was accidental injury (27 cases, or 50%), followed by incorrect or delayed diagnoses (22 cases, or 41%). Five cases resulted from the dermatologist failing to communicate important information, such as postop care instructions or obtaining informed consent.
Of all 54 cases 30 (56%) were dismissed prior to trial, while 24 (44%) resulted in a judgment for the plaintiff. According to Dr. Lim, payout information was available for only five cases, and ranged from $15,000 (injury from laser) to $1,950,000 (delayed diagnosis of malignant melanoma).
“While lawsuits from patients against dermatologists largely involve injury from elective procedures, clinicians should practice caution regarding missed or delayed diagnoses when practicing medical dermatology,” the authors concluded in their abstract. “Ensuring that critical information is shared with patients and obtaining proper written consent will also safeguard against easily-avoidable litigations.”
Christopher B. Zachary, MBBS, professor and chair emeritus of the department of dermatology at the University of California, Irvine, who was asked to comment on the study, said that the findings are a reminder that lack of attention to the most simply performed aspects of care can be the reasons patients will seek medical malpractice redress.
“Consent requires careful and thoughtful explanation of a planned procedure, which should then be recorded in the chart to avoid future confusion,” Dr. Zachary told this news organization. “A patient’s signature on a consent form obtained by a staff member is clearly inadequate if not accompanied by a clear and understandable preoperative discussion. Words, images, video are all elements that aid patients’ comprehension of a planned procedure. And postoperative instructions given to the patients while on the laser table are commonly forgotten by the patient and must be accompanied by written advice summary. Patients will frequently misremember instructions and can be overwhelmed by medical jargon.”
Neither the researchers nor Dr. Zachary reported having relevant financial disclosures.
PHOENIX – , and the defendants were more likely to be male.
Those are among key findings from a study that aimed to determine the reasons patients pursue litigation against dermatologists.
“The number of lawsuits against physicians continues to climb annually,” Young Lim, MD, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the results were presented during an abstract session. “Depending on the study, anywhere between 75 to 99 percent of physicians will face a lawsuit by age 65. A clear understanding of prior litigations will help mitigate similar errors in future practice and promote safer, higher quality care.”
Dr. Lim, a dermatology resident at Massachusetts General Hospital and Harvard Medical School, Boston, along with Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at MGH, and H. Ray Jalian, MD, a cosmetic dermatologist who practices in Los Angeles, used two large national database repositories, WestlawNext and LexisNexis, to retrospectively analyze legal documents following a query using “dermatology” and “dermatologist” as search terms to capture all variety of litigations. They excluded cases in which litigation did not involve patient care as well as those in which the dermatologist was the plaintiff and those in which the dermatologist was involved as a third party.
The final analysis consisted of 54 claims, comprising 43 state and 11 federal cases. Of the 54 cases, 35 involved a male defendant, 12 involved a female defendant, and 7 cases either did not specify the gender of the defendant or involved multiple defendants. Of the 35 cases involving a male defendant, 23 (66%) were brought by female plaintiffs.
Most cases (49, or 91%) involved a defendant dermatologist in private practice while the remaining 5 involved a defendant dermatologist in an academic setting.
The most common reason for litigation was accidental injury (27 cases, or 50%), followed by incorrect or delayed diagnoses (22 cases, or 41%). Five cases resulted from the dermatologist failing to communicate important information, such as postop care instructions or obtaining informed consent.
Of all 54 cases 30 (56%) were dismissed prior to trial, while 24 (44%) resulted in a judgment for the plaintiff. According to Dr. Lim, payout information was available for only five cases, and ranged from $15,000 (injury from laser) to $1,950,000 (delayed diagnosis of malignant melanoma).
“While lawsuits from patients against dermatologists largely involve injury from elective procedures, clinicians should practice caution regarding missed or delayed diagnoses when practicing medical dermatology,” the authors concluded in their abstract. “Ensuring that critical information is shared with patients and obtaining proper written consent will also safeguard against easily-avoidable litigations.”
Christopher B. Zachary, MBBS, professor and chair emeritus of the department of dermatology at the University of California, Irvine, who was asked to comment on the study, said that the findings are a reminder that lack of attention to the most simply performed aspects of care can be the reasons patients will seek medical malpractice redress.
“Consent requires careful and thoughtful explanation of a planned procedure, which should then be recorded in the chart to avoid future confusion,” Dr. Zachary told this news organization. “A patient’s signature on a consent form obtained by a staff member is clearly inadequate if not accompanied by a clear and understandable preoperative discussion. Words, images, video are all elements that aid patients’ comprehension of a planned procedure. And postoperative instructions given to the patients while on the laser table are commonly forgotten by the patient and must be accompanied by written advice summary. Patients will frequently misremember instructions and can be overwhelmed by medical jargon.”
Neither the researchers nor Dr. Zachary reported having relevant financial disclosures.
PHOENIX – , and the defendants were more likely to be male.
Those are among key findings from a study that aimed to determine the reasons patients pursue litigation against dermatologists.
“The number of lawsuits against physicians continues to climb annually,” Young Lim, MD, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the results were presented during an abstract session. “Depending on the study, anywhere between 75 to 99 percent of physicians will face a lawsuit by age 65. A clear understanding of prior litigations will help mitigate similar errors in future practice and promote safer, higher quality care.”
Dr. Lim, a dermatology resident at Massachusetts General Hospital and Harvard Medical School, Boston, along with Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at MGH, and H. Ray Jalian, MD, a cosmetic dermatologist who practices in Los Angeles, used two large national database repositories, WestlawNext and LexisNexis, to retrospectively analyze legal documents following a query using “dermatology” and “dermatologist” as search terms to capture all variety of litigations. They excluded cases in which litigation did not involve patient care as well as those in which the dermatologist was the plaintiff and those in which the dermatologist was involved as a third party.
The final analysis consisted of 54 claims, comprising 43 state and 11 federal cases. Of the 54 cases, 35 involved a male defendant, 12 involved a female defendant, and 7 cases either did not specify the gender of the defendant or involved multiple defendants. Of the 35 cases involving a male defendant, 23 (66%) were brought by female plaintiffs.
Most cases (49, or 91%) involved a defendant dermatologist in private practice while the remaining 5 involved a defendant dermatologist in an academic setting.
The most common reason for litigation was accidental injury (27 cases, or 50%), followed by incorrect or delayed diagnoses (22 cases, or 41%). Five cases resulted from the dermatologist failing to communicate important information, such as postop care instructions or obtaining informed consent.
Of all 54 cases 30 (56%) were dismissed prior to trial, while 24 (44%) resulted in a judgment for the plaintiff. According to Dr. Lim, payout information was available for only five cases, and ranged from $15,000 (injury from laser) to $1,950,000 (delayed diagnosis of malignant melanoma).
“While lawsuits from patients against dermatologists largely involve injury from elective procedures, clinicians should practice caution regarding missed or delayed diagnoses when practicing medical dermatology,” the authors concluded in their abstract. “Ensuring that critical information is shared with patients and obtaining proper written consent will also safeguard against easily-avoidable litigations.”
Christopher B. Zachary, MBBS, professor and chair emeritus of the department of dermatology at the University of California, Irvine, who was asked to comment on the study, said that the findings are a reminder that lack of attention to the most simply performed aspects of care can be the reasons patients will seek medical malpractice redress.
“Consent requires careful and thoughtful explanation of a planned procedure, which should then be recorded in the chart to avoid future confusion,” Dr. Zachary told this news organization. “A patient’s signature on a consent form obtained by a staff member is clearly inadequate if not accompanied by a clear and understandable preoperative discussion. Words, images, video are all elements that aid patients’ comprehension of a planned procedure. And postoperative instructions given to the patients while on the laser table are commonly forgotten by the patient and must be accompanied by written advice summary. Patients will frequently misremember instructions and can be overwhelmed by medical jargon.”
Neither the researchers nor Dr. Zachary reported having relevant financial disclosures.
AT ASLMS 2023
Proposed Medicare bill would raise docs’ pay with inflation
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Surgeons, intensivists earn more than do colleagues from private insurance
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
NPF provides guidance for virtual psoriasis visits
.
The success of telemedicine in managing chronic inflammatory skin conditions including psoriasis during the COVID-19 pandemic “highlighted that teledermatology can be used beyond the context of a global health crisis to provide continuity of care and improve access to health care more broadly,” the task force wrote in a paper published online in JAAD International.
Co–senior author George Han, MD, PhD, said in an interview that the impetus for the guidelines came from NPF patient advocates, who realized that the organization needed something to take to payers and governmental agencies to advocate for better access to dermatologic care. He is associate professor of dermatology and director of teledermatology at the Hofstra/Northwell department of dermatology, Hyde Park, New York.
“We realized that, in many places around the country, people don’t have access to dermatology.” In upstate New York, said Dr. Han, his anecdotal research has revealed wait times of 6 months or more.
As a guiding principle, the authors pronounce teledermatology “a reasonable alternative for providing long-term management of patients with psoriasis.” Research shows that nearly all dermatologists used teledermatology during the pandemic, the authors noted, and that well-run programs improve Psoriasis Area and Severity Index (PASI) scores and other measures on par with in-person care. Telemedicine may be especially useful for initial visits, they added, particularly when distance, patient incapacity, and circumstances prevent face-to-face evaluation.
Additional position statements emphasize that teledermatology should support rather than supplant in-person visits, and that this balance may be particularly important in cases involving psoriatic arthritis (PsA). “Even though we can’t do a physical exam and palpate some of those joints in person,” said Dr. Han, “tools have been developed that, through a series of questions the patient can answer, can guide you towards whether there is a high index of suspicion for psoriatic arthritis.” Such patients require in-person evaluation with urgency, he said, because delays in PsA diagnosis and treatment can lead to irreversible joint damage and significant functional impairment.
Another motivation for producing the guidelines, said Dr. Han, was that, even when underserved patients get a dermatology appointment, some providers may not have all the latest tools or medicines available for treating psoriasis. In such cases, telemedicine may allow dermatologists specializing in psoriasis care to extend their reach in comanaging patients with primary care physicians and community dermatologists.
Before the appointment, guidelines suggest determining what form of teledermatology will best suit each patient. Authors recommended gauging patients’ savviness with computers and cameras, and counseling patients regarding available virtual evaluation tools – such as live video visits, store-and-forward photo strategies, and assessment-tool training videos.
A subsequent guideline underscores the importance of continuously improving technology to support expeditious image capture and workflows that emulate in-person practice. Dr. Han explained, “we wanted to make sure that on the back end there’s adequate support such that – if through teledermatology, we determine that the patient should get, say, a systemic treatment – the patient is able to get the appropriate lab tests, get the medicine, and know how to inject it.”
Regarding reimbursement, Dr. Han said that policies varied prepandemic, but many commercial insurers covered telemedicine at a rate 20% lower than the in-person rate. During the pandemic, he said, insurers shifted to provide the higher rate for telemedicine, consistent with policies adopted by the Centers for Medicare & Medicaid Services.
“There are differences in coverage and reimbursement from plan to plan,” Dr. Han added. “And even within the same plan, there are carve-outs so that some plans don’t allow certain services. The big picture is that for the most part these services are covered at a level comparable to an in-person visit at present.”
With the Department of Health & Human Services’ public health emergency declaration expiring in May, he said, physicians have worried that some of the allowances made by CMS – such as lifting requirements that Medicare patients in rural areas be seen at care sites – will expire. “It seems that some of those limitations have been addressed, and those allowances are going to be extended until Congress is able to pass something that gives us durable access to telemedicine care. We think that based on the current environment telemedicine is here to stay.”
The study was funded by the NPF. Dr. Han has been an investigator, adviser, speaker, or researcher for AbbVie, Amgen, Apogee Therapeutics, Arcutis, Athenex, Bausch Health, Beiersdorf, Boehringer Ingelheim, Bond Avillion, Bristol Myers Squibb, Celgene, CeraVe, Dermavant, DermTech, Eli Lilly, EPI Health, Janssen Pharmaceuticals, LEO Pharma, L’Oreal, MC2 Therapeutics, Novartis, Ortho Dermatologics, PellePharm, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, SUN Pharmaceuticals, and UCB.
.
The success of telemedicine in managing chronic inflammatory skin conditions including psoriasis during the COVID-19 pandemic “highlighted that teledermatology can be used beyond the context of a global health crisis to provide continuity of care and improve access to health care more broadly,” the task force wrote in a paper published online in JAAD International.
Co–senior author George Han, MD, PhD, said in an interview that the impetus for the guidelines came from NPF patient advocates, who realized that the organization needed something to take to payers and governmental agencies to advocate for better access to dermatologic care. He is associate professor of dermatology and director of teledermatology at the Hofstra/Northwell department of dermatology, Hyde Park, New York.
“We realized that, in many places around the country, people don’t have access to dermatology.” In upstate New York, said Dr. Han, his anecdotal research has revealed wait times of 6 months or more.
As a guiding principle, the authors pronounce teledermatology “a reasonable alternative for providing long-term management of patients with psoriasis.” Research shows that nearly all dermatologists used teledermatology during the pandemic, the authors noted, and that well-run programs improve Psoriasis Area and Severity Index (PASI) scores and other measures on par with in-person care. Telemedicine may be especially useful for initial visits, they added, particularly when distance, patient incapacity, and circumstances prevent face-to-face evaluation.
Additional position statements emphasize that teledermatology should support rather than supplant in-person visits, and that this balance may be particularly important in cases involving psoriatic arthritis (PsA). “Even though we can’t do a physical exam and palpate some of those joints in person,” said Dr. Han, “tools have been developed that, through a series of questions the patient can answer, can guide you towards whether there is a high index of suspicion for psoriatic arthritis.” Such patients require in-person evaluation with urgency, he said, because delays in PsA diagnosis and treatment can lead to irreversible joint damage and significant functional impairment.
Another motivation for producing the guidelines, said Dr. Han, was that, even when underserved patients get a dermatology appointment, some providers may not have all the latest tools or medicines available for treating psoriasis. In such cases, telemedicine may allow dermatologists specializing in psoriasis care to extend their reach in comanaging patients with primary care physicians and community dermatologists.
Before the appointment, guidelines suggest determining what form of teledermatology will best suit each patient. Authors recommended gauging patients’ savviness with computers and cameras, and counseling patients regarding available virtual evaluation tools – such as live video visits, store-and-forward photo strategies, and assessment-tool training videos.
A subsequent guideline underscores the importance of continuously improving technology to support expeditious image capture and workflows that emulate in-person practice. Dr. Han explained, “we wanted to make sure that on the back end there’s adequate support such that – if through teledermatology, we determine that the patient should get, say, a systemic treatment – the patient is able to get the appropriate lab tests, get the medicine, and know how to inject it.”
Regarding reimbursement, Dr. Han said that policies varied prepandemic, but many commercial insurers covered telemedicine at a rate 20% lower than the in-person rate. During the pandemic, he said, insurers shifted to provide the higher rate for telemedicine, consistent with policies adopted by the Centers for Medicare & Medicaid Services.
“There are differences in coverage and reimbursement from plan to plan,” Dr. Han added. “And even within the same plan, there are carve-outs so that some plans don’t allow certain services. The big picture is that for the most part these services are covered at a level comparable to an in-person visit at present.”
With the Department of Health & Human Services’ public health emergency declaration expiring in May, he said, physicians have worried that some of the allowances made by CMS – such as lifting requirements that Medicare patients in rural areas be seen at care sites – will expire. “It seems that some of those limitations have been addressed, and those allowances are going to be extended until Congress is able to pass something that gives us durable access to telemedicine care. We think that based on the current environment telemedicine is here to stay.”
The study was funded by the NPF. Dr. Han has been an investigator, adviser, speaker, or researcher for AbbVie, Amgen, Apogee Therapeutics, Arcutis, Athenex, Bausch Health, Beiersdorf, Boehringer Ingelheim, Bond Avillion, Bristol Myers Squibb, Celgene, CeraVe, Dermavant, DermTech, Eli Lilly, EPI Health, Janssen Pharmaceuticals, LEO Pharma, L’Oreal, MC2 Therapeutics, Novartis, Ortho Dermatologics, PellePharm, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, SUN Pharmaceuticals, and UCB.
.
The success of telemedicine in managing chronic inflammatory skin conditions including psoriasis during the COVID-19 pandemic “highlighted that teledermatology can be used beyond the context of a global health crisis to provide continuity of care and improve access to health care more broadly,” the task force wrote in a paper published online in JAAD International.
Co–senior author George Han, MD, PhD, said in an interview that the impetus for the guidelines came from NPF patient advocates, who realized that the organization needed something to take to payers and governmental agencies to advocate for better access to dermatologic care. He is associate professor of dermatology and director of teledermatology at the Hofstra/Northwell department of dermatology, Hyde Park, New York.
“We realized that, in many places around the country, people don’t have access to dermatology.” In upstate New York, said Dr. Han, his anecdotal research has revealed wait times of 6 months or more.
As a guiding principle, the authors pronounce teledermatology “a reasonable alternative for providing long-term management of patients with psoriasis.” Research shows that nearly all dermatologists used teledermatology during the pandemic, the authors noted, and that well-run programs improve Psoriasis Area and Severity Index (PASI) scores and other measures on par with in-person care. Telemedicine may be especially useful for initial visits, they added, particularly when distance, patient incapacity, and circumstances prevent face-to-face evaluation.
Additional position statements emphasize that teledermatology should support rather than supplant in-person visits, and that this balance may be particularly important in cases involving psoriatic arthritis (PsA). “Even though we can’t do a physical exam and palpate some of those joints in person,” said Dr. Han, “tools have been developed that, through a series of questions the patient can answer, can guide you towards whether there is a high index of suspicion for psoriatic arthritis.” Such patients require in-person evaluation with urgency, he said, because delays in PsA diagnosis and treatment can lead to irreversible joint damage and significant functional impairment.
Another motivation for producing the guidelines, said Dr. Han, was that, even when underserved patients get a dermatology appointment, some providers may not have all the latest tools or medicines available for treating psoriasis. In such cases, telemedicine may allow dermatologists specializing in psoriasis care to extend their reach in comanaging patients with primary care physicians and community dermatologists.
Before the appointment, guidelines suggest determining what form of teledermatology will best suit each patient. Authors recommended gauging patients’ savviness with computers and cameras, and counseling patients regarding available virtual evaluation tools – such as live video visits, store-and-forward photo strategies, and assessment-tool training videos.
A subsequent guideline underscores the importance of continuously improving technology to support expeditious image capture and workflows that emulate in-person practice. Dr. Han explained, “we wanted to make sure that on the back end there’s adequate support such that – if through teledermatology, we determine that the patient should get, say, a systemic treatment – the patient is able to get the appropriate lab tests, get the medicine, and know how to inject it.”
Regarding reimbursement, Dr. Han said that policies varied prepandemic, but many commercial insurers covered telemedicine at a rate 20% lower than the in-person rate. During the pandemic, he said, insurers shifted to provide the higher rate for telemedicine, consistent with policies adopted by the Centers for Medicare & Medicaid Services.
“There are differences in coverage and reimbursement from plan to plan,” Dr. Han added. “And even within the same plan, there are carve-outs so that some plans don’t allow certain services. The big picture is that for the most part these services are covered at a level comparable to an in-person visit at present.”
With the Department of Health & Human Services’ public health emergency declaration expiring in May, he said, physicians have worried that some of the allowances made by CMS – such as lifting requirements that Medicare patients in rural areas be seen at care sites – will expire. “It seems that some of those limitations have been addressed, and those allowances are going to be extended until Congress is able to pass something that gives us durable access to telemedicine care. We think that based on the current environment telemedicine is here to stay.”
The study was funded by the NPF. Dr. Han has been an investigator, adviser, speaker, or researcher for AbbVie, Amgen, Apogee Therapeutics, Arcutis, Athenex, Bausch Health, Beiersdorf, Boehringer Ingelheim, Bond Avillion, Bristol Myers Squibb, Celgene, CeraVe, Dermavant, DermTech, Eli Lilly, EPI Health, Janssen Pharmaceuticals, LEO Pharma, L’Oreal, MC2 Therapeutics, Novartis, Ortho Dermatologics, PellePharm, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, SUN Pharmaceuticals, and UCB.
FROM JAAD INTERNATIONAL
Students, docs ponder U.S. News med school rankings after Harvard quits
When weighing medical schools, Hannah Gewaid admits that she kept the annual rankings from U.S. News & World Report in mind. “If I could get into a school of higher prestige, then I could have better odds for a good residency placement,” the pre-med student at the University of California, San Diego, told this news organization.
Although Ms. Gewaid considered other factors, she ultimately chose the highest-ranked medical school to which she was accepted: Rocky Vista University, Ivins, Utah. But it was the school’s environment that appealed to her most, she said. “Medical school can be pretty cut-throat, and I felt like the community at Rocky Vista was supportive. They also have one of the highest pass rates for boards in the nation, so it felt like the right combination for me.”
Likewise, Ramie Fathy, MD, a PGY1 internal medicine resident at Pennsylvania Hospital, Philadelphia, considered the report’s rankings when applying to medical schools. He chose the Perelman School of Medicine at the University of Pennsylvania, which ranked fifth in the nation at the time, and graduated a year ago.
In January, Harvard Medical School pulled out of the popular U.S. News rankings that many students use to guide their application decisions. Soon afterwards,
Although Dr. Fathy doesn’t regret selecting Perelman before it joined the list of exiting schools, he wonders if he was shortsighted using the rankings as criteria. “It’s hard to know what makes a school unique from others, and the rankings serve as a metric to guide you,” he said. “But in the end, it’s not a reliable or reflective way to judge a school.”
Dr. Fathy said he is proud that Perelman opted out of the rankings: “I think it will help ensure that they prioritize what is best for the students and the quality of their training, rather than aspects that are relevant to rankings but don’t translate to a better overall student experience.”
Dr. Fathy’s viewpoint seems to be shared by the medical schools that announced they will no longer participate in the U.S. News rankings. The Association of American Medical Colleges recently reported that more than a dozen of the top 20 medical schools in the 2023 report have publicly exited the rankings.
USNWR’s chairman and CEO Eric Gertler said in a prepared statement that students turn to the rankings for help in making a key career decision in the face of competitive admissions and high tuition costs.
“We know that comparing diverse academic institutions across a common data set is challenging, and that is why we have consistently stated that the rankings should be one component in a prospective student’s decision-making process.”
The schools’ reasons for exiting vary. In Harvard’s case, Dean George Q. Daley, MD, PhD, said in a statement that the rankings don’t align with the school’s high standards of the school’s medical education programs.
Critics of the rankings say they rely too much on the grades and test scores of accepted students, AAMC reported. Stanford Dean, Lloyd Minor, MD, said the rankings fail to “capture the full extent of what makes an exceptional learning environment.” A school’s mission, curriculum, and other metrics should also be used to judge educational value, he said.
Medical schools that publicly announced their decisions to withdraw from the rankings also pointed to the extensive time and resources needed to gather data to submit to USNWR, rise in the standings, and remain at the top.
Bryan Carmody, MD, a Norfolk, Va.-based pediatric nephrologist and pediatrics professor known for his medical school commentaries, said in an interview that he doesn’t see the value of the rankings. “If you look at the data and factors the report collects, it has almost no impact on the day-to-day experience and quality of the medical school. It doesn’t assess meaningful educational outputs.”
Using MCAT scores and the GPAs of incoming students is irrelevant to the value the school can provide a student, Dr. Carmody said.
“The stated idea of the rankings is to measure quality, but in reality, it’s to maintain a certain hierarchy,” he said. “The content of the MCAT is only peripherally relevant. Real patients don’t come in as a multiple-choice question.”
The withdrawal of Harvard – which held the top ranking – put the report’s shortcomings in the spotlight, Dr. Carmody said. But Harvard wasn’t the first to pull out. In 2016, the Uniformed Services University in Maryland exited the rankings. Some schools chose never to participate, including most Historically Black Colleges and Universities, as well as osteopathic medical schools.
Given the ripple effect of high-ranking schools like Harvard pulling out of the rankings, prospective students are left to find other criteria to measure their future med schools.
Weighing other factors
If he could apply again, Dr. Fathy said he has the experience to know he wouldn’t have put as much weight in the U.S. News rankings. “At the time I was applying, it was hard to understand exactly what the rankings stood for,” he said. “I thought maybe a higher ranking meant better research opportunities and better connections. It’s hard to let go of the prestige relative to it all.”
His final two options had been Penn or Stanford. “Penn was the better choice for me, not because of its rankings, but because I had unique mentors and research opportunities there, and also because I had a scholarship,” he said. “I also had no family on the West Coast, which would have made a difference had I chosen Stanford.”
Dr. Fathy is happy the rankings have lost some of their prestige.
“I’m hoping that as schools pull out, it will demonstrate to applicants that the rankings aren’t where they should focus,” he said. “I also hope that down the line, it will prevent the name of a school from being such a big factor in residency applications.”
Dr. Fathy added that applying to residency programs has been an inequitable process, as institutions seem to judge applicants based on where they went to medical school. “When you look at the match lists, I believe programs put preference on students coming out of higher-ranking institutions,” he said.
Ahmed Mukhtar Ahmed, MPP, MSc, who will graduate soon from Harvard Medical School, said he hopes that the withdrawals from the ranking system will benefit future students. His initial choice of Harvard wasn’t the result of the rankings, he said. His family came from Somalia in 1996. “My mom sacrificed so much for me to get where I am, and when I was choosing a school, Harvard was the only name she recognized. It meant so much for her that I was accepted here.”
Beyond the emotional tie-in, however, Mr. Ahmed found Harvard to be the right fit for other reasons. “There’s so much opportunity here for someone with a focus on public health, and it has served me well.”
Still, Mr. Ahmed was not ignorant of the rankings. “I don’t know too many students who didn’t have their fingers on the pulse of the rankings,” he said. “There’s awareness that it’s not a good metric, but when applying to residencies, they keep in mind where you went to med school. So, we all have it in the back of our minds, for better or worse.”
Like Dr. Fathy, Mr. Ahmed can see the cracks in the ranking system. “I think the exodus from the rankings is good for applicants and also for the landscape of institutions, in general,” he said. “There’s nothing that says the number-one school is the best school for you.”
Mr. Ahmed points to other criteria, including financing opportunities, when judging a prospective school. “Talk to students and ask about how responsive administration is should a concern pop up,” he said. “Are they invested in student well-being? Also look at the diversity of institutions and experiences you will have. That’s something I didn’t appreciate until I was a student. I learned new things from the different hospitals I rotated through.”
What the future holds
Dr. Carmody recommends that students determine what information about a school matters to them. “What is their residency placement like, for instance? Keep in mind that most schools don’t convey this entirely truthfully, but it’s a measurement.”
Mr. Ahmed points to the Medical School Admission Requirements database compiled by the AAMC. “Look in the database to filter out where you should apply without the numbers attached to it,” he said. “Look at the faculty-to-student ratio, how much debt you might have to take on, and what housing is like, for instance. We should move toward a weighing system like that, rather than rankings.”
If the withdrawals of medical schools eventually lead to the demise of the rankings, Dr. Carmody noted the downsides. “There’s some concern that this will hurt pre-med students because it was the one place to find a certain amount of credible, objective data. There’s a ring of truth to that and a worry that schools won’t provide data in any sort of standardized way for an apples-to-apples comparison.”
It would also take time – probably as much as a decade – for the legacy of the U.S. News rankings to completely disappear, according to Dr. Carmody. Dr. Fathy agrees. “The rankings are ingrained on so many levels,” he said. “The better the ranking, the better the funding, so it’s self-reinforcing.”
In the future, other factors should guide students’ decision-making, including distance from family and friends, available research opportunities, and whether students are happy at the school, Dr. Fathy said. “There are so many experiential points to consider that go beyond the flawed ranking system.”
A version of this article first appeared on Medscape.com.
When weighing medical schools, Hannah Gewaid admits that she kept the annual rankings from U.S. News & World Report in mind. “If I could get into a school of higher prestige, then I could have better odds for a good residency placement,” the pre-med student at the University of California, San Diego, told this news organization.
Although Ms. Gewaid considered other factors, she ultimately chose the highest-ranked medical school to which she was accepted: Rocky Vista University, Ivins, Utah. But it was the school’s environment that appealed to her most, she said. “Medical school can be pretty cut-throat, and I felt like the community at Rocky Vista was supportive. They also have one of the highest pass rates for boards in the nation, so it felt like the right combination for me.”
Likewise, Ramie Fathy, MD, a PGY1 internal medicine resident at Pennsylvania Hospital, Philadelphia, considered the report’s rankings when applying to medical schools. He chose the Perelman School of Medicine at the University of Pennsylvania, which ranked fifth in the nation at the time, and graduated a year ago.
In January, Harvard Medical School pulled out of the popular U.S. News rankings that many students use to guide their application decisions. Soon afterwards,
Although Dr. Fathy doesn’t regret selecting Perelman before it joined the list of exiting schools, he wonders if he was shortsighted using the rankings as criteria. “It’s hard to know what makes a school unique from others, and the rankings serve as a metric to guide you,” he said. “But in the end, it’s not a reliable or reflective way to judge a school.”
Dr. Fathy said he is proud that Perelman opted out of the rankings: “I think it will help ensure that they prioritize what is best for the students and the quality of their training, rather than aspects that are relevant to rankings but don’t translate to a better overall student experience.”
Dr. Fathy’s viewpoint seems to be shared by the medical schools that announced they will no longer participate in the U.S. News rankings. The Association of American Medical Colleges recently reported that more than a dozen of the top 20 medical schools in the 2023 report have publicly exited the rankings.
USNWR’s chairman and CEO Eric Gertler said in a prepared statement that students turn to the rankings for help in making a key career decision in the face of competitive admissions and high tuition costs.
“We know that comparing diverse academic institutions across a common data set is challenging, and that is why we have consistently stated that the rankings should be one component in a prospective student’s decision-making process.”
The schools’ reasons for exiting vary. In Harvard’s case, Dean George Q. Daley, MD, PhD, said in a statement that the rankings don’t align with the school’s high standards of the school’s medical education programs.
Critics of the rankings say they rely too much on the grades and test scores of accepted students, AAMC reported. Stanford Dean, Lloyd Minor, MD, said the rankings fail to “capture the full extent of what makes an exceptional learning environment.” A school’s mission, curriculum, and other metrics should also be used to judge educational value, he said.
Medical schools that publicly announced their decisions to withdraw from the rankings also pointed to the extensive time and resources needed to gather data to submit to USNWR, rise in the standings, and remain at the top.
Bryan Carmody, MD, a Norfolk, Va.-based pediatric nephrologist and pediatrics professor known for his medical school commentaries, said in an interview that he doesn’t see the value of the rankings. “If you look at the data and factors the report collects, it has almost no impact on the day-to-day experience and quality of the medical school. It doesn’t assess meaningful educational outputs.”
Using MCAT scores and the GPAs of incoming students is irrelevant to the value the school can provide a student, Dr. Carmody said.
“The stated idea of the rankings is to measure quality, but in reality, it’s to maintain a certain hierarchy,” he said. “The content of the MCAT is only peripherally relevant. Real patients don’t come in as a multiple-choice question.”
The withdrawal of Harvard – which held the top ranking – put the report’s shortcomings in the spotlight, Dr. Carmody said. But Harvard wasn’t the first to pull out. In 2016, the Uniformed Services University in Maryland exited the rankings. Some schools chose never to participate, including most Historically Black Colleges and Universities, as well as osteopathic medical schools.
Given the ripple effect of high-ranking schools like Harvard pulling out of the rankings, prospective students are left to find other criteria to measure their future med schools.
Weighing other factors
If he could apply again, Dr. Fathy said he has the experience to know he wouldn’t have put as much weight in the U.S. News rankings. “At the time I was applying, it was hard to understand exactly what the rankings stood for,” he said. “I thought maybe a higher ranking meant better research opportunities and better connections. It’s hard to let go of the prestige relative to it all.”
His final two options had been Penn or Stanford. “Penn was the better choice for me, not because of its rankings, but because I had unique mentors and research opportunities there, and also because I had a scholarship,” he said. “I also had no family on the West Coast, which would have made a difference had I chosen Stanford.”
Dr. Fathy is happy the rankings have lost some of their prestige.
“I’m hoping that as schools pull out, it will demonstrate to applicants that the rankings aren’t where they should focus,” he said. “I also hope that down the line, it will prevent the name of a school from being such a big factor in residency applications.”
Dr. Fathy added that applying to residency programs has been an inequitable process, as institutions seem to judge applicants based on where they went to medical school. “When you look at the match lists, I believe programs put preference on students coming out of higher-ranking institutions,” he said.
Ahmed Mukhtar Ahmed, MPP, MSc, who will graduate soon from Harvard Medical School, said he hopes that the withdrawals from the ranking system will benefit future students. His initial choice of Harvard wasn’t the result of the rankings, he said. His family came from Somalia in 1996. “My mom sacrificed so much for me to get where I am, and when I was choosing a school, Harvard was the only name she recognized. It meant so much for her that I was accepted here.”
Beyond the emotional tie-in, however, Mr. Ahmed found Harvard to be the right fit for other reasons. “There’s so much opportunity here for someone with a focus on public health, and it has served me well.”
Still, Mr. Ahmed was not ignorant of the rankings. “I don’t know too many students who didn’t have their fingers on the pulse of the rankings,” he said. “There’s awareness that it’s not a good metric, but when applying to residencies, they keep in mind where you went to med school. So, we all have it in the back of our minds, for better or worse.”
Like Dr. Fathy, Mr. Ahmed can see the cracks in the ranking system. “I think the exodus from the rankings is good for applicants and also for the landscape of institutions, in general,” he said. “There’s nothing that says the number-one school is the best school for you.”
Mr. Ahmed points to other criteria, including financing opportunities, when judging a prospective school. “Talk to students and ask about how responsive administration is should a concern pop up,” he said. “Are they invested in student well-being? Also look at the diversity of institutions and experiences you will have. That’s something I didn’t appreciate until I was a student. I learned new things from the different hospitals I rotated through.”
What the future holds
Dr. Carmody recommends that students determine what information about a school matters to them. “What is their residency placement like, for instance? Keep in mind that most schools don’t convey this entirely truthfully, but it’s a measurement.”
Mr. Ahmed points to the Medical School Admission Requirements database compiled by the AAMC. “Look in the database to filter out where you should apply without the numbers attached to it,” he said. “Look at the faculty-to-student ratio, how much debt you might have to take on, and what housing is like, for instance. We should move toward a weighing system like that, rather than rankings.”
If the withdrawals of medical schools eventually lead to the demise of the rankings, Dr. Carmody noted the downsides. “There’s some concern that this will hurt pre-med students because it was the one place to find a certain amount of credible, objective data. There’s a ring of truth to that and a worry that schools won’t provide data in any sort of standardized way for an apples-to-apples comparison.”
It would also take time – probably as much as a decade – for the legacy of the U.S. News rankings to completely disappear, according to Dr. Carmody. Dr. Fathy agrees. “The rankings are ingrained on so many levels,” he said. “The better the ranking, the better the funding, so it’s self-reinforcing.”
In the future, other factors should guide students’ decision-making, including distance from family and friends, available research opportunities, and whether students are happy at the school, Dr. Fathy said. “There are so many experiential points to consider that go beyond the flawed ranking system.”
A version of this article first appeared on Medscape.com.
When weighing medical schools, Hannah Gewaid admits that she kept the annual rankings from U.S. News & World Report in mind. “If I could get into a school of higher prestige, then I could have better odds for a good residency placement,” the pre-med student at the University of California, San Diego, told this news organization.
Although Ms. Gewaid considered other factors, she ultimately chose the highest-ranked medical school to which she was accepted: Rocky Vista University, Ivins, Utah. But it was the school’s environment that appealed to her most, she said. “Medical school can be pretty cut-throat, and I felt like the community at Rocky Vista was supportive. They also have one of the highest pass rates for boards in the nation, so it felt like the right combination for me.”
Likewise, Ramie Fathy, MD, a PGY1 internal medicine resident at Pennsylvania Hospital, Philadelphia, considered the report’s rankings when applying to medical schools. He chose the Perelman School of Medicine at the University of Pennsylvania, which ranked fifth in the nation at the time, and graduated a year ago.
In January, Harvard Medical School pulled out of the popular U.S. News rankings that many students use to guide their application decisions. Soon afterwards,
Although Dr. Fathy doesn’t regret selecting Perelman before it joined the list of exiting schools, he wonders if he was shortsighted using the rankings as criteria. “It’s hard to know what makes a school unique from others, and the rankings serve as a metric to guide you,” he said. “But in the end, it’s not a reliable or reflective way to judge a school.”
Dr. Fathy said he is proud that Perelman opted out of the rankings: “I think it will help ensure that they prioritize what is best for the students and the quality of their training, rather than aspects that are relevant to rankings but don’t translate to a better overall student experience.”
Dr. Fathy’s viewpoint seems to be shared by the medical schools that announced they will no longer participate in the U.S. News rankings. The Association of American Medical Colleges recently reported that more than a dozen of the top 20 medical schools in the 2023 report have publicly exited the rankings.
USNWR’s chairman and CEO Eric Gertler said in a prepared statement that students turn to the rankings for help in making a key career decision in the face of competitive admissions and high tuition costs.
“We know that comparing diverse academic institutions across a common data set is challenging, and that is why we have consistently stated that the rankings should be one component in a prospective student’s decision-making process.”
The schools’ reasons for exiting vary. In Harvard’s case, Dean George Q. Daley, MD, PhD, said in a statement that the rankings don’t align with the school’s high standards of the school’s medical education programs.
Critics of the rankings say they rely too much on the grades and test scores of accepted students, AAMC reported. Stanford Dean, Lloyd Minor, MD, said the rankings fail to “capture the full extent of what makes an exceptional learning environment.” A school’s mission, curriculum, and other metrics should also be used to judge educational value, he said.
Medical schools that publicly announced their decisions to withdraw from the rankings also pointed to the extensive time and resources needed to gather data to submit to USNWR, rise in the standings, and remain at the top.
Bryan Carmody, MD, a Norfolk, Va.-based pediatric nephrologist and pediatrics professor known for his medical school commentaries, said in an interview that he doesn’t see the value of the rankings. “If you look at the data and factors the report collects, it has almost no impact on the day-to-day experience and quality of the medical school. It doesn’t assess meaningful educational outputs.”
Using MCAT scores and the GPAs of incoming students is irrelevant to the value the school can provide a student, Dr. Carmody said.
“The stated idea of the rankings is to measure quality, but in reality, it’s to maintain a certain hierarchy,” he said. “The content of the MCAT is only peripherally relevant. Real patients don’t come in as a multiple-choice question.”
The withdrawal of Harvard – which held the top ranking – put the report’s shortcomings in the spotlight, Dr. Carmody said. But Harvard wasn’t the first to pull out. In 2016, the Uniformed Services University in Maryland exited the rankings. Some schools chose never to participate, including most Historically Black Colleges and Universities, as well as osteopathic medical schools.
Given the ripple effect of high-ranking schools like Harvard pulling out of the rankings, prospective students are left to find other criteria to measure their future med schools.
Weighing other factors
If he could apply again, Dr. Fathy said he has the experience to know he wouldn’t have put as much weight in the U.S. News rankings. “At the time I was applying, it was hard to understand exactly what the rankings stood for,” he said. “I thought maybe a higher ranking meant better research opportunities and better connections. It’s hard to let go of the prestige relative to it all.”
His final two options had been Penn or Stanford. “Penn was the better choice for me, not because of its rankings, but because I had unique mentors and research opportunities there, and also because I had a scholarship,” he said. “I also had no family on the West Coast, which would have made a difference had I chosen Stanford.”
Dr. Fathy is happy the rankings have lost some of their prestige.
“I’m hoping that as schools pull out, it will demonstrate to applicants that the rankings aren’t where they should focus,” he said. “I also hope that down the line, it will prevent the name of a school from being such a big factor in residency applications.”
Dr. Fathy added that applying to residency programs has been an inequitable process, as institutions seem to judge applicants based on where they went to medical school. “When you look at the match lists, I believe programs put preference on students coming out of higher-ranking institutions,” he said.
Ahmed Mukhtar Ahmed, MPP, MSc, who will graduate soon from Harvard Medical School, said he hopes that the withdrawals from the ranking system will benefit future students. His initial choice of Harvard wasn’t the result of the rankings, he said. His family came from Somalia in 1996. “My mom sacrificed so much for me to get where I am, and when I was choosing a school, Harvard was the only name she recognized. It meant so much for her that I was accepted here.”
Beyond the emotional tie-in, however, Mr. Ahmed found Harvard to be the right fit for other reasons. “There’s so much opportunity here for someone with a focus on public health, and it has served me well.”
Still, Mr. Ahmed was not ignorant of the rankings. “I don’t know too many students who didn’t have their fingers on the pulse of the rankings,” he said. “There’s awareness that it’s not a good metric, but when applying to residencies, they keep in mind where you went to med school. So, we all have it in the back of our minds, for better or worse.”
Like Dr. Fathy, Mr. Ahmed can see the cracks in the ranking system. “I think the exodus from the rankings is good for applicants and also for the landscape of institutions, in general,” he said. “There’s nothing that says the number-one school is the best school for you.”
Mr. Ahmed points to other criteria, including financing opportunities, when judging a prospective school. “Talk to students and ask about how responsive administration is should a concern pop up,” he said. “Are they invested in student well-being? Also look at the diversity of institutions and experiences you will have. That’s something I didn’t appreciate until I was a student. I learned new things from the different hospitals I rotated through.”
What the future holds
Dr. Carmody recommends that students determine what information about a school matters to them. “What is their residency placement like, for instance? Keep in mind that most schools don’t convey this entirely truthfully, but it’s a measurement.”
Mr. Ahmed points to the Medical School Admission Requirements database compiled by the AAMC. “Look in the database to filter out where you should apply without the numbers attached to it,” he said. “Look at the faculty-to-student ratio, how much debt you might have to take on, and what housing is like, for instance. We should move toward a weighing system like that, rather than rankings.”
If the withdrawals of medical schools eventually lead to the demise of the rankings, Dr. Carmody noted the downsides. “There’s some concern that this will hurt pre-med students because it was the one place to find a certain amount of credible, objective data. There’s a ring of truth to that and a worry that schools won’t provide data in any sort of standardized way for an apples-to-apples comparison.”
It would also take time – probably as much as a decade – for the legacy of the U.S. News rankings to completely disappear, according to Dr. Carmody. Dr. Fathy agrees. “The rankings are ingrained on so many levels,” he said. “The better the ranking, the better the funding, so it’s self-reinforcing.”
In the future, other factors should guide students’ decision-making, including distance from family and friends, available research opportunities, and whether students are happy at the school, Dr. Fathy said. “There are so many experiential points to consider that go beyond the flawed ranking system.”
A version of this article first appeared on Medscape.com.
CMS inpatient payment rule for 2024: Key takeaways
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
AI predicts endometrial cancer recurrence
Endometrial cancer is the most frequently occurring uterine cancer. Early-stage patients have about a 95% 5-year survival, but distant recurrence is associated with very poor survival, according to Sarah Fremond, MSc, an author of the research (Abstract 5695), which she presented at the annual meeting of the American Association for Cancer Research.
“Most patients with endometrial cancer have a good prognosis and would not require any adjuvant treatment, but there is a proportion that will develop distant recurrence. For those you want to recommend adjuvant chemotherapy, because currently in the adjuvant setting, that’s the only treatment that is known to lower the risk of distant recurrence. But that also causes morbidity. Therefore, our clinical question was how to accurately identify patients at low and high risk of distant recurrence to reduce under- and overtreatment,” said Ms. Fremond, a PhD candidate at Leiden (the Netherlands) University Medical Center.
Pathologists can attempt such predictions, but Ms. Fremond noted that there are challenges. “There is a lot of variability between pathologists, and we don’t even use the entire visual information present in the H&E [hematoxylin and eosin] tumor slide. When it comes to molecular testing, it is hampered by cost, turnaround time, and sometimes interpretation. It’s quite complex to combine those data to specifically target risk of distant recurrence for patients with endometrial cancer.”
In her presentation, Ms. Fremond described how she and her colleagues used digitized histopathological slides in their research. She and her coauthors developed the AI model as part of a collaboration that included the AIRMEC Consortium, Leiden University Medical Center, the TransPORTEC Consortium, and the University of Zürich.
The researchers used long-term follow-up data from 1,408 patients drawn from three clinical cohorts and participants in the PORTEC-1, PORTEC-2, and PORTEC-3 studies, which tested radiotherapy and adjuvant therapy outcomes in endometrial cancer. Patients who had received prior adjuvant chemotherapy were excluded. In the model development phase, the system analyzed a single representative histopathological slide image from each patient and compared it with the known time to distant recurrence to identify patterns.
Once the system had been trained, the researchers applied it to a novel group of 353 patients. It ranked 89 patients as having a low risk of recurrence, 175 at intermediate risk, and 89 at high risk of recurrence. The system performed well: 3.37% of low-risk patients experienced a distant recurrence, as did 15.43% of the intermediate-risk group and 36% of the high-risk group.
The researchers also employed an external validation group with 152 patients and three slides per patient, with a 2.8-year follow-up. The model performed with a C index of 0.805 (±0.0136) when a random slide was selected for each patient, and the median predicted risk score per patient was associated with differences in distant recurrence-free survival between the three risk groups with a C index of 0.816 (P < .0001).
Questions about research and their answers
Session moderator Kristin Swanson, PhD, asked if the AI could be used with the pathology slide’s visible features to learn more about the underlying biology and pathophysiology of tumors.
“Overlying the HECTOR on to the tissue seems like a logical opportunity to go and then explore the biology and what’s attributed as a high-risk region,” said Dr. Swanson, who is director of the Mathematical NeuroOncology Lab and codirector of the Precision NeuroTherapeutics Innovation Program at Mayo Clinic Arizona, Phoenix.
Ms. Fremond agreed that the AI has the potential to be used that way.”
During the Q&A, an audience member asked how likely the model is to perform in populations that differ significantly from the populations used in her study.
Ms. Fremond responded that the populations used to develop and test the models were in or close to the Netherlands, and little information was available regarding patient ethnicity. “There is a possibility that perhaps we would have a different performance on a population that includes more minorities. That needs to be checked,” said Ms. Fremond.
The study is limited by its retrospective nature.
Ms. Fremond and Dr. Swanson have no relevant financial disclosures.
Endometrial cancer is the most frequently occurring uterine cancer. Early-stage patients have about a 95% 5-year survival, but distant recurrence is associated with very poor survival, according to Sarah Fremond, MSc, an author of the research (Abstract 5695), which she presented at the annual meeting of the American Association for Cancer Research.
“Most patients with endometrial cancer have a good prognosis and would not require any adjuvant treatment, but there is a proportion that will develop distant recurrence. For those you want to recommend adjuvant chemotherapy, because currently in the adjuvant setting, that’s the only treatment that is known to lower the risk of distant recurrence. But that also causes morbidity. Therefore, our clinical question was how to accurately identify patients at low and high risk of distant recurrence to reduce under- and overtreatment,” said Ms. Fremond, a PhD candidate at Leiden (the Netherlands) University Medical Center.
Pathologists can attempt such predictions, but Ms. Fremond noted that there are challenges. “There is a lot of variability between pathologists, and we don’t even use the entire visual information present in the H&E [hematoxylin and eosin] tumor slide. When it comes to molecular testing, it is hampered by cost, turnaround time, and sometimes interpretation. It’s quite complex to combine those data to specifically target risk of distant recurrence for patients with endometrial cancer.”
In her presentation, Ms. Fremond described how she and her colleagues used digitized histopathological slides in their research. She and her coauthors developed the AI model as part of a collaboration that included the AIRMEC Consortium, Leiden University Medical Center, the TransPORTEC Consortium, and the University of Zürich.
The researchers used long-term follow-up data from 1,408 patients drawn from three clinical cohorts and participants in the PORTEC-1, PORTEC-2, and PORTEC-3 studies, which tested radiotherapy and adjuvant therapy outcomes in endometrial cancer. Patients who had received prior adjuvant chemotherapy were excluded. In the model development phase, the system analyzed a single representative histopathological slide image from each patient and compared it with the known time to distant recurrence to identify patterns.
Once the system had been trained, the researchers applied it to a novel group of 353 patients. It ranked 89 patients as having a low risk of recurrence, 175 at intermediate risk, and 89 at high risk of recurrence. The system performed well: 3.37% of low-risk patients experienced a distant recurrence, as did 15.43% of the intermediate-risk group and 36% of the high-risk group.
The researchers also employed an external validation group with 152 patients and three slides per patient, with a 2.8-year follow-up. The model performed with a C index of 0.805 (±0.0136) when a random slide was selected for each patient, and the median predicted risk score per patient was associated with differences in distant recurrence-free survival between the three risk groups with a C index of 0.816 (P < .0001).
Questions about research and their answers
Session moderator Kristin Swanson, PhD, asked if the AI could be used with the pathology slide’s visible features to learn more about the underlying biology and pathophysiology of tumors.
“Overlying the HECTOR on to the tissue seems like a logical opportunity to go and then explore the biology and what’s attributed as a high-risk region,” said Dr. Swanson, who is director of the Mathematical NeuroOncology Lab and codirector of the Precision NeuroTherapeutics Innovation Program at Mayo Clinic Arizona, Phoenix.
Ms. Fremond agreed that the AI has the potential to be used that way.”
During the Q&A, an audience member asked how likely the model is to perform in populations that differ significantly from the populations used in her study.
Ms. Fremond responded that the populations used to develop and test the models were in or close to the Netherlands, and little information was available regarding patient ethnicity. “There is a possibility that perhaps we would have a different performance on a population that includes more minorities. That needs to be checked,” said Ms. Fremond.
The study is limited by its retrospective nature.
Ms. Fremond and Dr. Swanson have no relevant financial disclosures.
Endometrial cancer is the most frequently occurring uterine cancer. Early-stage patients have about a 95% 5-year survival, but distant recurrence is associated with very poor survival, according to Sarah Fremond, MSc, an author of the research (Abstract 5695), which she presented at the annual meeting of the American Association for Cancer Research.
“Most patients with endometrial cancer have a good prognosis and would not require any adjuvant treatment, but there is a proportion that will develop distant recurrence. For those you want to recommend adjuvant chemotherapy, because currently in the adjuvant setting, that’s the only treatment that is known to lower the risk of distant recurrence. But that also causes morbidity. Therefore, our clinical question was how to accurately identify patients at low and high risk of distant recurrence to reduce under- and overtreatment,” said Ms. Fremond, a PhD candidate at Leiden (the Netherlands) University Medical Center.
Pathologists can attempt such predictions, but Ms. Fremond noted that there are challenges. “There is a lot of variability between pathologists, and we don’t even use the entire visual information present in the H&E [hematoxylin and eosin] tumor slide. When it comes to molecular testing, it is hampered by cost, turnaround time, and sometimes interpretation. It’s quite complex to combine those data to specifically target risk of distant recurrence for patients with endometrial cancer.”
In her presentation, Ms. Fremond described how she and her colleagues used digitized histopathological slides in their research. She and her coauthors developed the AI model as part of a collaboration that included the AIRMEC Consortium, Leiden University Medical Center, the TransPORTEC Consortium, and the University of Zürich.
The researchers used long-term follow-up data from 1,408 patients drawn from three clinical cohorts and participants in the PORTEC-1, PORTEC-2, and PORTEC-3 studies, which tested radiotherapy and adjuvant therapy outcomes in endometrial cancer. Patients who had received prior adjuvant chemotherapy were excluded. In the model development phase, the system analyzed a single representative histopathological slide image from each patient and compared it with the known time to distant recurrence to identify patterns.
Once the system had been trained, the researchers applied it to a novel group of 353 patients. It ranked 89 patients as having a low risk of recurrence, 175 at intermediate risk, and 89 at high risk of recurrence. The system performed well: 3.37% of low-risk patients experienced a distant recurrence, as did 15.43% of the intermediate-risk group and 36% of the high-risk group.
The researchers also employed an external validation group with 152 patients and three slides per patient, with a 2.8-year follow-up. The model performed with a C index of 0.805 (±0.0136) when a random slide was selected for each patient, and the median predicted risk score per patient was associated with differences in distant recurrence-free survival between the three risk groups with a C index of 0.816 (P < .0001).
Questions about research and their answers
Session moderator Kristin Swanson, PhD, asked if the AI could be used with the pathology slide’s visible features to learn more about the underlying biology and pathophysiology of tumors.
“Overlying the HECTOR on to the tissue seems like a logical opportunity to go and then explore the biology and what’s attributed as a high-risk region,” said Dr. Swanson, who is director of the Mathematical NeuroOncology Lab and codirector of the Precision NeuroTherapeutics Innovation Program at Mayo Clinic Arizona, Phoenix.
Ms. Fremond agreed that the AI has the potential to be used that way.”
During the Q&A, an audience member asked how likely the model is to perform in populations that differ significantly from the populations used in her study.
Ms. Fremond responded that the populations used to develop and test the models were in or close to the Netherlands, and little information was available regarding patient ethnicity. “There is a possibility that perhaps we would have a different performance on a population that includes more minorities. That needs to be checked,” said Ms. Fremond.
The study is limited by its retrospective nature.
Ms. Fremond and Dr. Swanson have no relevant financial disclosures.
FROM AACR 2023
Infographic: Is your compensation rising as fast as your peers?
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.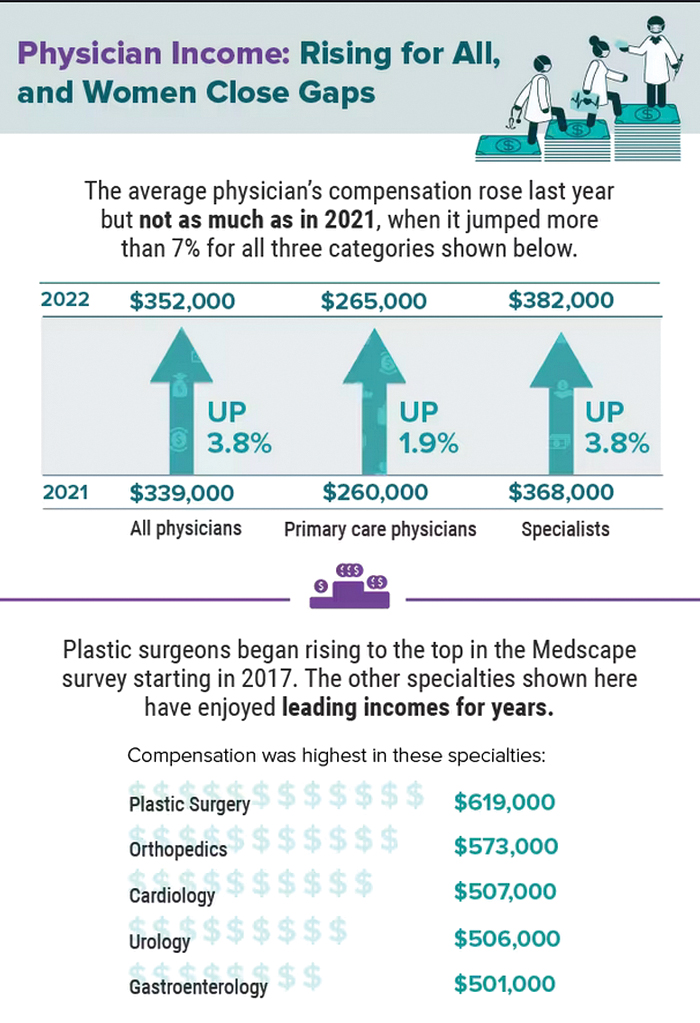
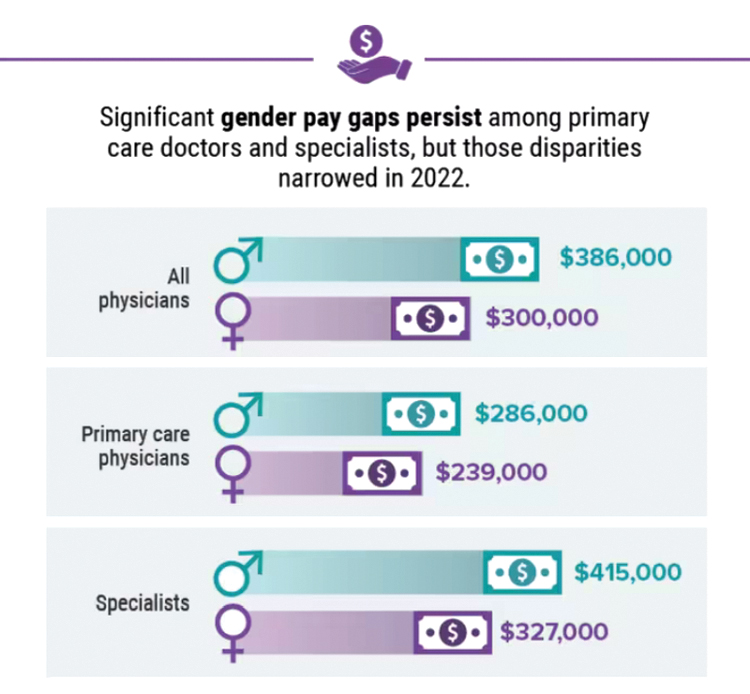
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.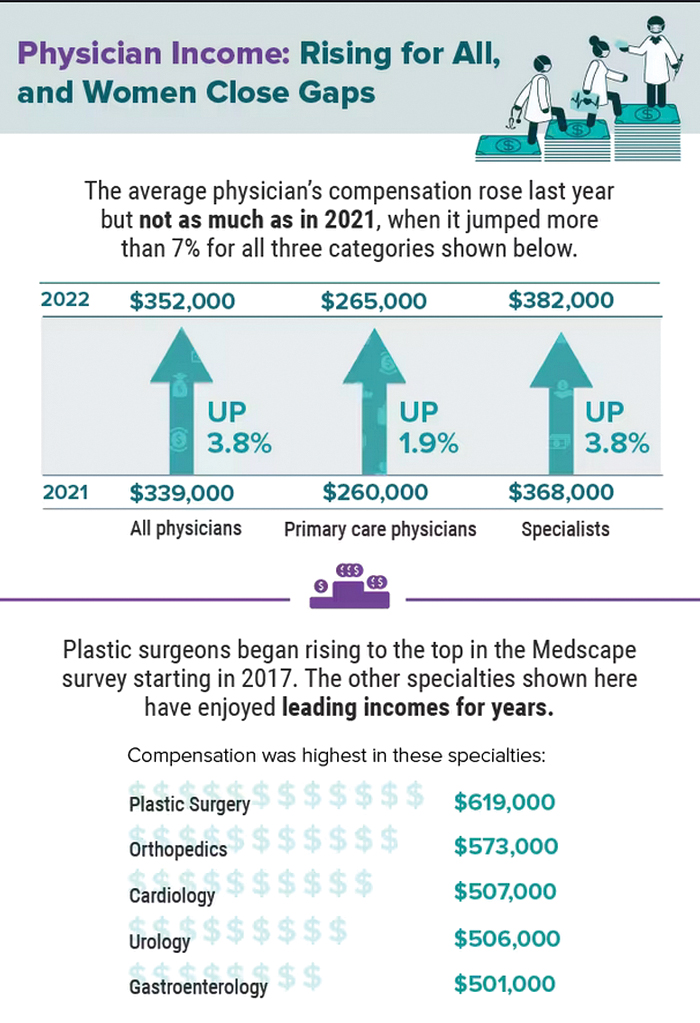
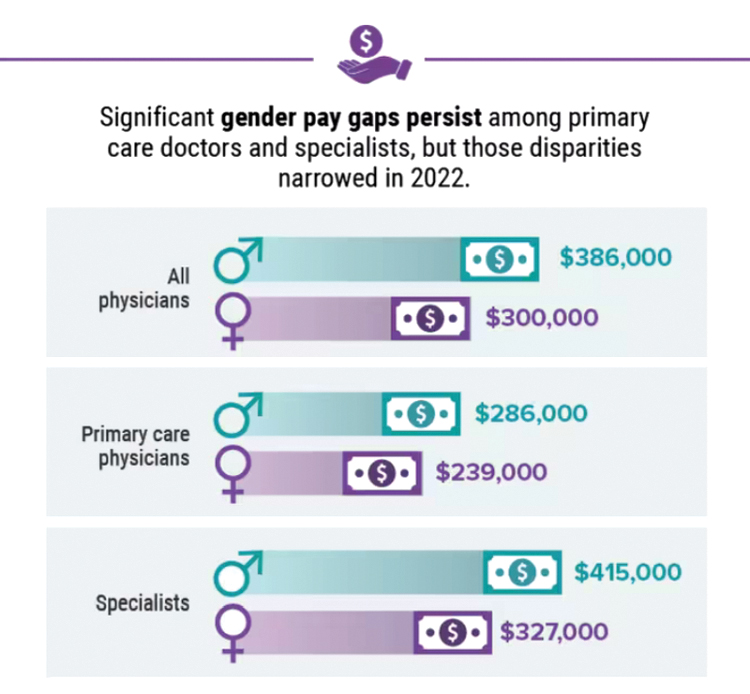
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.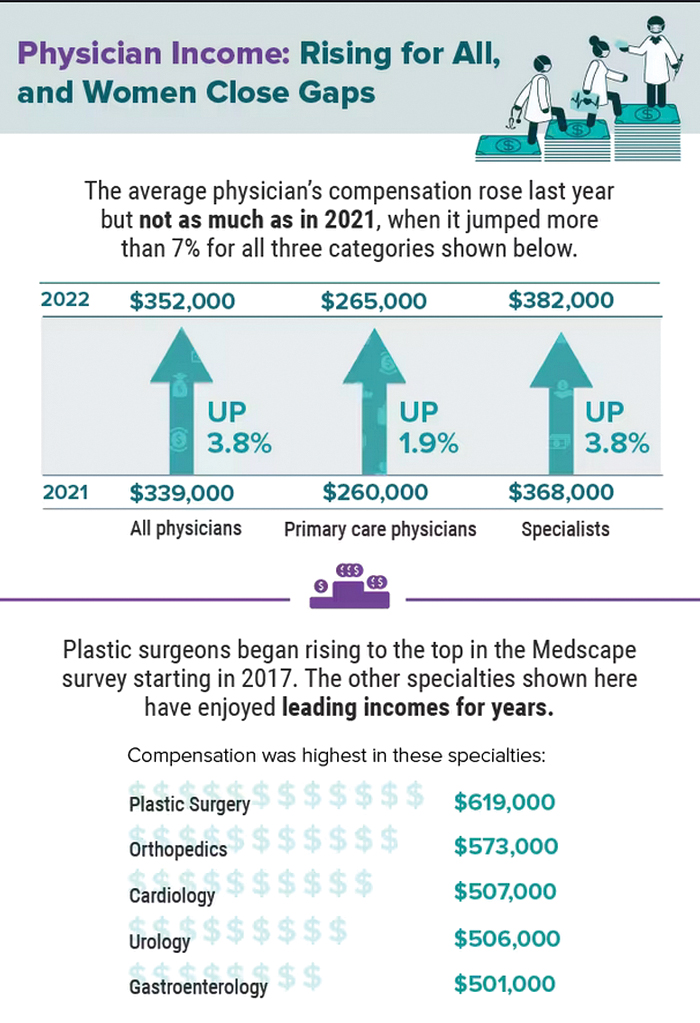
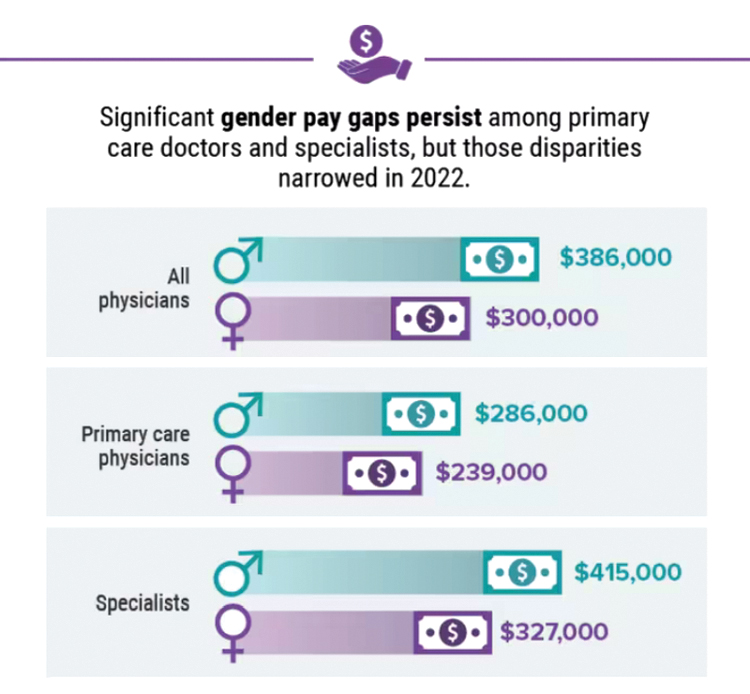
A version of this article first appeared on Medscape.com.
Five chronic mistakes that can sabotage your medical practice
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.