User login
ACST-2: Carotid stenting, surgery on par in asymptomatic patients
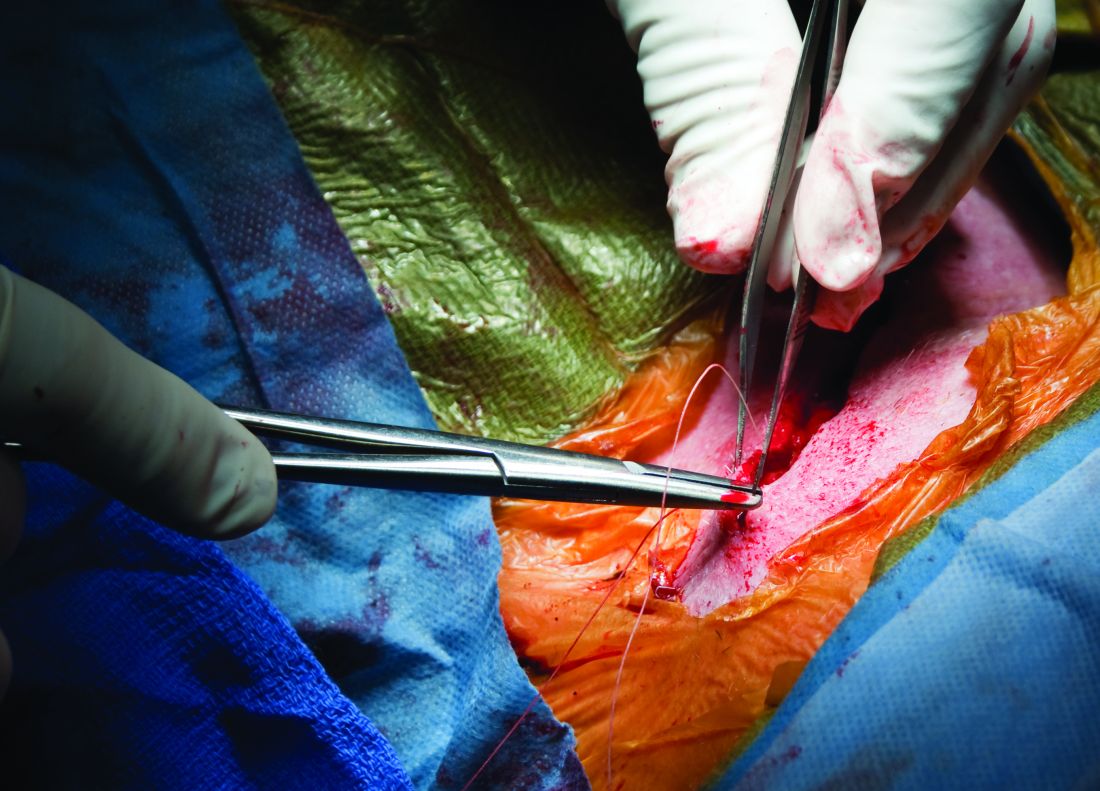
Carotid artery stenting (CAS) and carotid endarterectomy (CEA) provided comparable outcomes over time in asymptomatic patients receiving good medical therapy in the largest trial to date of what to do with severe carotid artery narrowing that is yet to cause a stroke.
Among more than 3,600 patients, stenting and surgery performed by experienced physicians involved a 1.0% risk for causing disabling stroke or death within 30 days.
The annual rate of fatal or disabling strokes was about 0.5% with either procedure over an average 5 years’ follow-up – essentially halving the annual stroke risk had neither procedure been performed, according to Alison Halliday, MD, principal investigator of the Asymptomatic Carotid Surgery Trial-2 (ACST-2).
The results were reported Aug. 29 in a Hot Line session at the virtual annual congress of the European Society of Cardiology and published simultaneously online in The Lancet.
Session chair Gilles Montalescot, MD, Sorbonne University, Paris, noted that ACST-2 doubled the number of randomly assigned patients with asymptomatic carotid stenosis studied in previous trials, “so, a huge contribution to the evidence base in this field and apparently good news for both revascularization techniques.”
Thirty-day and 5-year outcomes
The trial was conducted in 33 countries between January 2008 and December 2020, enrolling 3,625 patients (70% were male; mean age, 70 years) with carotid stenosis of at least 60% on ultrasonography, in whom stenting or surgery was suitable but both the doctor and patient were “substantially uncertain” which procedure to prefer.
Among the 1,811 patients assigned to stenting, 87% underwent the procedure at a median of 14 days; 6% crossed over to surgery, typically because of a highly calcified lesion or a more tortuous carotid than anticipated; and 6% had no intervention.
Among the 1,814 patients assigned to surgery, 92% had the procedure at a median of 14 days; 3% crossed over to stenting, typically because of patient or doctor preference or reluctance to undergo general anesthesia; and 4% had no intervention.
Patients without complications who had stenting stayed on average 1 day less than did those undergoing surgery.
During an earlier press briefing, Dr. Halliday highlighted the need for procedural competency and said doctors had to submit a record of their CEA or CAS experience and, consistent with current guidelines, had to demonstrate an independently verified stroke or death rate of 6% or less for symptomatic patients and 3% or lower for asymptomatic patients.
The results showed the 30-day risk for death, myocardial infarction (MI), or any stroke was 3.9% with carotid stenting and 3.2% with surgery (P = .26).
But with stenting, there was a slightly higher risk for procedural nondisabling strokes (48 vs. 29; P = .03), including 15 strokes vs. 5 strokes, respectively, that left patients with no residual symptoms. This is “consistent with large, recent nationally representative registry data,” observed Dr. Halliday, of the University of Oxford (England).
For those undergoing surgery, cranial nerve palsies were reported in 5.4% vs. no patients undergoing stenting.
At 5 years, the nonprocedural fatal or disabling stroke rate was 2.5% in each group (rate ratio [RR], 0.98; P = .91), with any nonprocedural stroke occurring in 5.3% of patients with stenting vs. 4.5% with surgery (RR, 1.16; P = .33).
The investigators performed a meta-analysis combining the ACST-2 results with those of eight prior trials (four in asymptomatic and four in symptomatic patients) that yielded a similar nonsignificant result for any nonprocedural stroke (RR, 1.11; P = .21).
Based on the results from ACST-2 plus the major trials, stenting and surgery involve “similar risks and similar benefits,” Dr. Halliday concluded.
Discussant Marco Roffi, MD, University Hospital of Geneva, said, “In centers with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic stenosis and suitable anatomy.”
While the trial provides “good news” for patients, he pointed out that a reduction in the sample size from 5,000 to 3,625 limited the statistical power and that enrollment over a long period of time may have introduced confounders, such as changes in equipment technique, and medical therapy.
Also, many centers enrolled few patients, raising the concern over low-volume centers and operators, Dr. Roffi said. “We know that 8% of the centers enrolled 39% of the patients,” and “information on the credentialing and experience of the interventionalists was limited.”
Further, a lack of systematic MI assessment may have favored the surgery group, and more recent developments in stenting with the potential of reducing periprocedural stroke were rarely used, such as proximal emboli protection in only 15% and double-layer stents in 11%.
Friedhelm Beyersdorf, MD, University Hospital of Freiburg, Germany, said that, as a vascular surgeon, he finds it understandable that there might be a higher incidence of nonfatal strokes when treating carotid stenosis with stents, given the vulnerability of these lesions.
“Nevertheless, the main conclusion from the entire study is that carotid artery treatment is extremely safe, it has to be done in order to avoid strokes, and, obviously, there seems to be an advantage for surgery in terms of nondisabling stroke,” he said.
Session chair Dr. Montalescot, however, said that what the study cannot address – and what was the subject of many online audience comments – is whether either intervention should be performed in these patients.
Unlike earlier trials comparing interventions to medical therapy, Dr. Halliday said ACST-2 enrolled patients for whom the decision had been made that revascularization was needed. In addition, 99%-100% were receiving antithrombotic therapy at baseline, 85%-90% were receiving antihypertensives, and about 85% were taking statins.
Longer-term follow-up should provide a better picture of the nonprocedural stroke risk, with patients asked annually about exactly what medications and doses they are taking, she said.
“We will have an enormous list of exactly what’s gone on and the intensity of that therapy, which is, of course, much more intense than when we carried out our first trial. But these were people in whom a procedure was thought to be necessary,” she noted.
When asked during the press conference which procedure she would choose, Dr. Halliday, a surgeon, observed that patient preference is important but that the nature of the lesion itself often determines the optimal choice.
“If you know the competence of the people doing it is equal, then the less invasive procedure – providing it has good long-term viability, and that’s why we’re following for 10 years – is the more important,” she added.
The study was funded by the UK Medical Research Council and Health Technology Assessment Programme. Dr. Halliday reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Carotid artery stenting (CAS) and carotid endarterectomy (CEA) provided comparable outcomes over time in asymptomatic patients receiving good medical therapy in the largest trial to date of what to do with severe carotid artery narrowing that is yet to cause a stroke.
Among more than 3,600 patients, stenting and surgery performed by experienced physicians involved a 1.0% risk for causing disabling stroke or death within 30 days.
The annual rate of fatal or disabling strokes was about 0.5% with either procedure over an average 5 years’ follow-up – essentially halving the annual stroke risk had neither procedure been performed, according to Alison Halliday, MD, principal investigator of the Asymptomatic Carotid Surgery Trial-2 (ACST-2).
The results were reported Aug. 29 in a Hot Line session at the virtual annual congress of the European Society of Cardiology and published simultaneously online in The Lancet.
Session chair Gilles Montalescot, MD, Sorbonne University, Paris, noted that ACST-2 doubled the number of randomly assigned patients with asymptomatic carotid stenosis studied in previous trials, “so, a huge contribution to the evidence base in this field and apparently good news for both revascularization techniques.”
Thirty-day and 5-year outcomes
The trial was conducted in 33 countries between January 2008 and December 2020, enrolling 3,625 patients (70% were male; mean age, 70 years) with carotid stenosis of at least 60% on ultrasonography, in whom stenting or surgery was suitable but both the doctor and patient were “substantially uncertain” which procedure to prefer.
Among the 1,811 patients assigned to stenting, 87% underwent the procedure at a median of 14 days; 6% crossed over to surgery, typically because of a highly calcified lesion or a more tortuous carotid than anticipated; and 6% had no intervention.
Among the 1,814 patients assigned to surgery, 92% had the procedure at a median of 14 days; 3% crossed over to stenting, typically because of patient or doctor preference or reluctance to undergo general anesthesia; and 4% had no intervention.
Patients without complications who had stenting stayed on average 1 day less than did those undergoing surgery.
During an earlier press briefing, Dr. Halliday highlighted the need for procedural competency and said doctors had to submit a record of their CEA or CAS experience and, consistent with current guidelines, had to demonstrate an independently verified stroke or death rate of 6% or less for symptomatic patients and 3% or lower for asymptomatic patients.
The results showed the 30-day risk for death, myocardial infarction (MI), or any stroke was 3.9% with carotid stenting and 3.2% with surgery (P = .26).
But with stenting, there was a slightly higher risk for procedural nondisabling strokes (48 vs. 29; P = .03), including 15 strokes vs. 5 strokes, respectively, that left patients with no residual symptoms. This is “consistent with large, recent nationally representative registry data,” observed Dr. Halliday, of the University of Oxford (England).
For those undergoing surgery, cranial nerve palsies were reported in 5.4% vs. no patients undergoing stenting.
At 5 years, the nonprocedural fatal or disabling stroke rate was 2.5% in each group (rate ratio [RR], 0.98; P = .91), with any nonprocedural stroke occurring in 5.3% of patients with stenting vs. 4.5% with surgery (RR, 1.16; P = .33).
The investigators performed a meta-analysis combining the ACST-2 results with those of eight prior trials (four in asymptomatic and four in symptomatic patients) that yielded a similar nonsignificant result for any nonprocedural stroke (RR, 1.11; P = .21).
Based on the results from ACST-2 plus the major trials, stenting and surgery involve “similar risks and similar benefits,” Dr. Halliday concluded.
Discussant Marco Roffi, MD, University Hospital of Geneva, said, “In centers with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic stenosis and suitable anatomy.”
While the trial provides “good news” for patients, he pointed out that a reduction in the sample size from 5,000 to 3,625 limited the statistical power and that enrollment over a long period of time may have introduced confounders, such as changes in equipment technique, and medical therapy.
Also, many centers enrolled few patients, raising the concern over low-volume centers and operators, Dr. Roffi said. “We know that 8% of the centers enrolled 39% of the patients,” and “information on the credentialing and experience of the interventionalists was limited.”
Further, a lack of systematic MI assessment may have favored the surgery group, and more recent developments in stenting with the potential of reducing periprocedural stroke were rarely used, such as proximal emboli protection in only 15% and double-layer stents in 11%.
Friedhelm Beyersdorf, MD, University Hospital of Freiburg, Germany, said that, as a vascular surgeon, he finds it understandable that there might be a higher incidence of nonfatal strokes when treating carotid stenosis with stents, given the vulnerability of these lesions.
“Nevertheless, the main conclusion from the entire study is that carotid artery treatment is extremely safe, it has to be done in order to avoid strokes, and, obviously, there seems to be an advantage for surgery in terms of nondisabling stroke,” he said.
Session chair Dr. Montalescot, however, said that what the study cannot address – and what was the subject of many online audience comments – is whether either intervention should be performed in these patients.
Unlike earlier trials comparing interventions to medical therapy, Dr. Halliday said ACST-2 enrolled patients for whom the decision had been made that revascularization was needed. In addition, 99%-100% were receiving antithrombotic therapy at baseline, 85%-90% were receiving antihypertensives, and about 85% were taking statins.
Longer-term follow-up should provide a better picture of the nonprocedural stroke risk, with patients asked annually about exactly what medications and doses they are taking, she said.
“We will have an enormous list of exactly what’s gone on and the intensity of that therapy, which is, of course, much more intense than when we carried out our first trial. But these were people in whom a procedure was thought to be necessary,” she noted.
When asked during the press conference which procedure she would choose, Dr. Halliday, a surgeon, observed that patient preference is important but that the nature of the lesion itself often determines the optimal choice.
“If you know the competence of the people doing it is equal, then the less invasive procedure – providing it has good long-term viability, and that’s why we’re following for 10 years – is the more important,” she added.
The study was funded by the UK Medical Research Council and Health Technology Assessment Programme. Dr. Halliday reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Carotid artery stenting (CAS) and carotid endarterectomy (CEA) provided comparable outcomes over time in asymptomatic patients receiving good medical therapy in the largest trial to date of what to do with severe carotid artery narrowing that is yet to cause a stroke.
Among more than 3,600 patients, stenting and surgery performed by experienced physicians involved a 1.0% risk for causing disabling stroke or death within 30 days.
The annual rate of fatal or disabling strokes was about 0.5% with either procedure over an average 5 years’ follow-up – essentially halving the annual stroke risk had neither procedure been performed, according to Alison Halliday, MD, principal investigator of the Asymptomatic Carotid Surgery Trial-2 (ACST-2).
The results were reported Aug. 29 in a Hot Line session at the virtual annual congress of the European Society of Cardiology and published simultaneously online in The Lancet.
Session chair Gilles Montalescot, MD, Sorbonne University, Paris, noted that ACST-2 doubled the number of randomly assigned patients with asymptomatic carotid stenosis studied in previous trials, “so, a huge contribution to the evidence base in this field and apparently good news for both revascularization techniques.”
Thirty-day and 5-year outcomes
The trial was conducted in 33 countries between January 2008 and December 2020, enrolling 3,625 patients (70% were male; mean age, 70 years) with carotid stenosis of at least 60% on ultrasonography, in whom stenting or surgery was suitable but both the doctor and patient were “substantially uncertain” which procedure to prefer.
Among the 1,811 patients assigned to stenting, 87% underwent the procedure at a median of 14 days; 6% crossed over to surgery, typically because of a highly calcified lesion or a more tortuous carotid than anticipated; and 6% had no intervention.
Among the 1,814 patients assigned to surgery, 92% had the procedure at a median of 14 days; 3% crossed over to stenting, typically because of patient or doctor preference or reluctance to undergo general anesthesia; and 4% had no intervention.
Patients without complications who had stenting stayed on average 1 day less than did those undergoing surgery.
During an earlier press briefing, Dr. Halliday highlighted the need for procedural competency and said doctors had to submit a record of their CEA or CAS experience and, consistent with current guidelines, had to demonstrate an independently verified stroke or death rate of 6% or less for symptomatic patients and 3% or lower for asymptomatic patients.
The results showed the 30-day risk for death, myocardial infarction (MI), or any stroke was 3.9% with carotid stenting and 3.2% with surgery (P = .26).
But with stenting, there was a slightly higher risk for procedural nondisabling strokes (48 vs. 29; P = .03), including 15 strokes vs. 5 strokes, respectively, that left patients with no residual symptoms. This is “consistent with large, recent nationally representative registry data,” observed Dr. Halliday, of the University of Oxford (England).
For those undergoing surgery, cranial nerve palsies were reported in 5.4% vs. no patients undergoing stenting.
At 5 years, the nonprocedural fatal or disabling stroke rate was 2.5% in each group (rate ratio [RR], 0.98; P = .91), with any nonprocedural stroke occurring in 5.3% of patients with stenting vs. 4.5% with surgery (RR, 1.16; P = .33).
The investigators performed a meta-analysis combining the ACST-2 results with those of eight prior trials (four in asymptomatic and four in symptomatic patients) that yielded a similar nonsignificant result for any nonprocedural stroke (RR, 1.11; P = .21).
Based on the results from ACST-2 plus the major trials, stenting and surgery involve “similar risks and similar benefits,” Dr. Halliday concluded.
Discussant Marco Roffi, MD, University Hospital of Geneva, said, “In centers with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic stenosis and suitable anatomy.”
While the trial provides “good news” for patients, he pointed out that a reduction in the sample size from 5,000 to 3,625 limited the statistical power and that enrollment over a long period of time may have introduced confounders, such as changes in equipment technique, and medical therapy.
Also, many centers enrolled few patients, raising the concern over low-volume centers and operators, Dr. Roffi said. “We know that 8% of the centers enrolled 39% of the patients,” and “information on the credentialing and experience of the interventionalists was limited.”
Further, a lack of systematic MI assessment may have favored the surgery group, and more recent developments in stenting with the potential of reducing periprocedural stroke were rarely used, such as proximal emboli protection in only 15% and double-layer stents in 11%.
Friedhelm Beyersdorf, MD, University Hospital of Freiburg, Germany, said that, as a vascular surgeon, he finds it understandable that there might be a higher incidence of nonfatal strokes when treating carotid stenosis with stents, given the vulnerability of these lesions.
“Nevertheless, the main conclusion from the entire study is that carotid artery treatment is extremely safe, it has to be done in order to avoid strokes, and, obviously, there seems to be an advantage for surgery in terms of nondisabling stroke,” he said.
Session chair Dr. Montalescot, however, said that what the study cannot address – and what was the subject of many online audience comments – is whether either intervention should be performed in these patients.
Unlike earlier trials comparing interventions to medical therapy, Dr. Halliday said ACST-2 enrolled patients for whom the decision had been made that revascularization was needed. In addition, 99%-100% were receiving antithrombotic therapy at baseline, 85%-90% were receiving antihypertensives, and about 85% were taking statins.
Longer-term follow-up should provide a better picture of the nonprocedural stroke risk, with patients asked annually about exactly what medications and doses they are taking, she said.
“We will have an enormous list of exactly what’s gone on and the intensity of that therapy, which is, of course, much more intense than when we carried out our first trial. But these were people in whom a procedure was thought to be necessary,” she noted.
When asked during the press conference which procedure she would choose, Dr. Halliday, a surgeon, observed that patient preference is important but that the nature of the lesion itself often determines the optimal choice.
“If you know the competence of the people doing it is equal, then the less invasive procedure – providing it has good long-term viability, and that’s why we’re following for 10 years – is the more important,” she added.
The study was funded by the UK Medical Research Council and Health Technology Assessment Programme. Dr. Halliday reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Angiography can wait for cardiac arrest without ST-elevation
A protocol of immediate angiography provided no mortality benefit over a strategy or delayed or more selective angiography among patients resuscitated from out-of-hospital cardiac arrest and without ST-segment elevation, new randomized results show.
“Among patients with resuscitated out-of-hospital cardiac arrest of possible cardiac origin, with shockable and nonshockable arrest rhythm and no ST-elevation, a strategy of immediate, unselected coronary angiography was not found to be beneficial over a delayed and selective approach with regard to the 30-day risk of all-cause death,” concluded principal investigator Steffen Desch, MD, University of Leipzig (Germany) Heart Center.
The results support previous results of the Coronary Angiography after Cardiac Arrest (COACT) trial, in patients with shockable rhythms, which also showed no differences in clinical outcomes between immediate and delayed coronary angiography at both 90 days and 1 year, he noted.
“What the clinicians wanted to know is, is it really necessary to get up at 3 a.m. in the morning to perform a coronary angiography on these patients, and that’s certainly out,” Dr. Desch said in an interview. “So, there’s really no room for this strategy anymore. You can take your time and wait a day or 2.”
These findings, from the TOMAHAWK trial, were presented Aug. 29 at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Larger group without ST-segment elevation
Prognosis after out-of-hospital cardiac arrest is extremely poor, with an overall survival rate of less than 10%, Dr. Desch noted. “Actually, only 20% make it to the hospital; the vast majority of these patients die out in the field, so there’s really a great need in improving treatment.”
Acute coronary syndrome accounts for up to 60% of out-of-hospital arrests in which a cardiac cause has been identified, the authors wrote in their report. ST-segment elevation on postresuscitation electrocardiography “has good positive predictive value” for acute coronary lesions triggering the arrest, but in the far larger subgroup of patients without ST-segment elevation, “the spectrum of underlying causes is considerably broader and includes both cardiac and noncardiac causes.”
In patients with myocardial infarction, early revascularization would prevent negative consequences of myocardial injury, but unselected early coronary angiography would put patients not having an MI at unnecessary risk for procedural complications or delay in the diagnosis of the actual cause of their arrest, they noted.
In this trial, the researchers randomly assigned 554 patients from 31 sites in Germany and Denmark who were successfully resuscitated after cardiac arrest of possible cardiac origin to immediate transfer for coronary angiography or to initial intensive care assessment with delayed or selective angiography after a minimum delay of at least 1 day.
In the end, the average delay in this arm was 2 days, Dr. Desch noted. If the clinical course indicated that a coronary cause was unlikely, angiography might not be performed at all in this group.
No patient had ST-segment elevation on postresuscitation electrocardiography. The primary endpoint was death from any cause at 30 days; secondary end points were death from any cause or severe neurologic deficit at 30 days.
Results showed that 95% of patients in the immediate angiography group actually underwent the procedure, compared with 62% of those in the delayed group, a finding that was “logical” given the study design, he said.
At 30 days, 54% of patients in the immediate angiography group and 46% in the delayed group had died, a nonsignificant difference (P = .06). Because the researchers had performed an interim analysis, Dr. Desch explained, the final P value for significance in this trial was not .05, but rather .034, to account for multiple comparisons.

The secondary end point of death from any cause or severe neurologic deficit at 30 days “was actually nominally significant in favor of the delayed group,” he said. “So, this is not corrected for multiple testing, it’s just a hypothesis that’s in the room, but it’s certainly worthy of discussion that the immediate strategy might actually cause harm.”

There was no difference between the groups in peak release of myocardial enzymes, or any other safety end points, including bleeding, stroke, or renal failure, Dr. Desch said.
Further analyses showed no large differences between subgroups, including age, diabetes, first monitored rhythm, confirmed MI as the trigger of the arrest, sex, and the time from cardiac arrest to the return of spontaneous circulation, he noted.
Opportunity to minimize harm
Discussant for the results during the presentation was Susanna Price, MBBS, PhD, Royal Brompton Hospital, London.
Dr. Price concluded: “What this means for me, is it gives me information that’s useful regarding the opportunity to minimize harm, which is a lot of what critical care is about, so we don’t necessarily now have to move these patients very acutely when they’ve just come in through the ED [emergency department]. It has implications for resource utilization, but also implications for mobilizing patients around the hospital during COVID-19.”
It’s also important to note that coronary angiography was still carried out in certain patients, “so we still have to have that dialogue with our interventional cardiologists for certain patients who may need to go to the cath lab, and what it should now allow us to do is give appropriate focus to how to manage these patients when they come in to the ED or to our ICUs [intensive care units],” she said.
Dr. Price added, though, that perhaps “the most important slide” in the presentation was that showing 90% of these patients had a witnessed cardiac arrest, “and yet a third of these patients, 168 of them, had no bystander CPR at all.”
She pointed to the “chain of survival” after cardiac arrest, of which Charles D. Deakin, MD, University Hospital Southampton (England), wrote that “not all links are equal.”
“Early recognition and calling for help, early CPR, early defibrillation where appropriate are very, very important, and we need to be addressing all of these, as well as what happens in the cath lab and after admission,” Dr. Price said.
This research was funded by the German Center for Cardiovascular Research. Dr. Desch and Dr. Price reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A protocol of immediate angiography provided no mortality benefit over a strategy or delayed or more selective angiography among patients resuscitated from out-of-hospital cardiac arrest and without ST-segment elevation, new randomized results show.
“Among patients with resuscitated out-of-hospital cardiac arrest of possible cardiac origin, with shockable and nonshockable arrest rhythm and no ST-elevation, a strategy of immediate, unselected coronary angiography was not found to be beneficial over a delayed and selective approach with regard to the 30-day risk of all-cause death,” concluded principal investigator Steffen Desch, MD, University of Leipzig (Germany) Heart Center.
The results support previous results of the Coronary Angiography after Cardiac Arrest (COACT) trial, in patients with shockable rhythms, which also showed no differences in clinical outcomes between immediate and delayed coronary angiography at both 90 days and 1 year, he noted.
“What the clinicians wanted to know is, is it really necessary to get up at 3 a.m. in the morning to perform a coronary angiography on these patients, and that’s certainly out,” Dr. Desch said in an interview. “So, there’s really no room for this strategy anymore. You can take your time and wait a day or 2.”
These findings, from the TOMAHAWK trial, were presented Aug. 29 at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Larger group without ST-segment elevation
Prognosis after out-of-hospital cardiac arrest is extremely poor, with an overall survival rate of less than 10%, Dr. Desch noted. “Actually, only 20% make it to the hospital; the vast majority of these patients die out in the field, so there’s really a great need in improving treatment.”
Acute coronary syndrome accounts for up to 60% of out-of-hospital arrests in which a cardiac cause has been identified, the authors wrote in their report. ST-segment elevation on postresuscitation electrocardiography “has good positive predictive value” for acute coronary lesions triggering the arrest, but in the far larger subgroup of patients without ST-segment elevation, “the spectrum of underlying causes is considerably broader and includes both cardiac and noncardiac causes.”
In patients with myocardial infarction, early revascularization would prevent negative consequences of myocardial injury, but unselected early coronary angiography would put patients not having an MI at unnecessary risk for procedural complications or delay in the diagnosis of the actual cause of their arrest, they noted.
In this trial, the researchers randomly assigned 554 patients from 31 sites in Germany and Denmark who were successfully resuscitated after cardiac arrest of possible cardiac origin to immediate transfer for coronary angiography or to initial intensive care assessment with delayed or selective angiography after a minimum delay of at least 1 day.
In the end, the average delay in this arm was 2 days, Dr. Desch noted. If the clinical course indicated that a coronary cause was unlikely, angiography might not be performed at all in this group.
No patient had ST-segment elevation on postresuscitation electrocardiography. The primary endpoint was death from any cause at 30 days; secondary end points were death from any cause or severe neurologic deficit at 30 days.
Results showed that 95% of patients in the immediate angiography group actually underwent the procedure, compared with 62% of those in the delayed group, a finding that was “logical” given the study design, he said.
At 30 days, 54% of patients in the immediate angiography group and 46% in the delayed group had died, a nonsignificant difference (P = .06). Because the researchers had performed an interim analysis, Dr. Desch explained, the final P value for significance in this trial was not .05, but rather .034, to account for multiple comparisons.

The secondary end point of death from any cause or severe neurologic deficit at 30 days “was actually nominally significant in favor of the delayed group,” he said. “So, this is not corrected for multiple testing, it’s just a hypothesis that’s in the room, but it’s certainly worthy of discussion that the immediate strategy might actually cause harm.”

There was no difference between the groups in peak release of myocardial enzymes, or any other safety end points, including bleeding, stroke, or renal failure, Dr. Desch said.
Further analyses showed no large differences between subgroups, including age, diabetes, first monitored rhythm, confirmed MI as the trigger of the arrest, sex, and the time from cardiac arrest to the return of spontaneous circulation, he noted.
Opportunity to minimize harm
Discussant for the results during the presentation was Susanna Price, MBBS, PhD, Royal Brompton Hospital, London.
Dr. Price concluded: “What this means for me, is it gives me information that’s useful regarding the opportunity to minimize harm, which is a lot of what critical care is about, so we don’t necessarily now have to move these patients very acutely when they’ve just come in through the ED [emergency department]. It has implications for resource utilization, but also implications for mobilizing patients around the hospital during COVID-19.”
It’s also important to note that coronary angiography was still carried out in certain patients, “so we still have to have that dialogue with our interventional cardiologists for certain patients who may need to go to the cath lab, and what it should now allow us to do is give appropriate focus to how to manage these patients when they come in to the ED or to our ICUs [intensive care units],” she said.
Dr. Price added, though, that perhaps “the most important slide” in the presentation was that showing 90% of these patients had a witnessed cardiac arrest, “and yet a third of these patients, 168 of them, had no bystander CPR at all.”
She pointed to the “chain of survival” after cardiac arrest, of which Charles D. Deakin, MD, University Hospital Southampton (England), wrote that “not all links are equal.”
“Early recognition and calling for help, early CPR, early defibrillation where appropriate are very, very important, and we need to be addressing all of these, as well as what happens in the cath lab and after admission,” Dr. Price said.
This research was funded by the German Center for Cardiovascular Research. Dr. Desch and Dr. Price reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A protocol of immediate angiography provided no mortality benefit over a strategy or delayed or more selective angiography among patients resuscitated from out-of-hospital cardiac arrest and without ST-segment elevation, new randomized results show.
“Among patients with resuscitated out-of-hospital cardiac arrest of possible cardiac origin, with shockable and nonshockable arrest rhythm and no ST-elevation, a strategy of immediate, unselected coronary angiography was not found to be beneficial over a delayed and selective approach with regard to the 30-day risk of all-cause death,” concluded principal investigator Steffen Desch, MD, University of Leipzig (Germany) Heart Center.
The results support previous results of the Coronary Angiography after Cardiac Arrest (COACT) trial, in patients with shockable rhythms, which also showed no differences in clinical outcomes between immediate and delayed coronary angiography at both 90 days and 1 year, he noted.
“What the clinicians wanted to know is, is it really necessary to get up at 3 a.m. in the morning to perform a coronary angiography on these patients, and that’s certainly out,” Dr. Desch said in an interview. “So, there’s really no room for this strategy anymore. You can take your time and wait a day or 2.”
These findings, from the TOMAHAWK trial, were presented Aug. 29 at the annual congress of the European Society of Cardiology and simultaneously published online in the New England Journal of Medicine.
Larger group without ST-segment elevation
Prognosis after out-of-hospital cardiac arrest is extremely poor, with an overall survival rate of less than 10%, Dr. Desch noted. “Actually, only 20% make it to the hospital; the vast majority of these patients die out in the field, so there’s really a great need in improving treatment.”
Acute coronary syndrome accounts for up to 60% of out-of-hospital arrests in which a cardiac cause has been identified, the authors wrote in their report. ST-segment elevation on postresuscitation electrocardiography “has good positive predictive value” for acute coronary lesions triggering the arrest, but in the far larger subgroup of patients without ST-segment elevation, “the spectrum of underlying causes is considerably broader and includes both cardiac and noncardiac causes.”
In patients with myocardial infarction, early revascularization would prevent negative consequences of myocardial injury, but unselected early coronary angiography would put patients not having an MI at unnecessary risk for procedural complications or delay in the diagnosis of the actual cause of their arrest, they noted.
In this trial, the researchers randomly assigned 554 patients from 31 sites in Germany and Denmark who were successfully resuscitated after cardiac arrest of possible cardiac origin to immediate transfer for coronary angiography or to initial intensive care assessment with delayed or selective angiography after a minimum delay of at least 1 day.
In the end, the average delay in this arm was 2 days, Dr. Desch noted. If the clinical course indicated that a coronary cause was unlikely, angiography might not be performed at all in this group.
No patient had ST-segment elevation on postresuscitation electrocardiography. The primary endpoint was death from any cause at 30 days; secondary end points were death from any cause or severe neurologic deficit at 30 days.
Results showed that 95% of patients in the immediate angiography group actually underwent the procedure, compared with 62% of those in the delayed group, a finding that was “logical” given the study design, he said.
At 30 days, 54% of patients in the immediate angiography group and 46% in the delayed group had died, a nonsignificant difference (P = .06). Because the researchers had performed an interim analysis, Dr. Desch explained, the final P value for significance in this trial was not .05, but rather .034, to account for multiple comparisons.

The secondary end point of death from any cause or severe neurologic deficit at 30 days “was actually nominally significant in favor of the delayed group,” he said. “So, this is not corrected for multiple testing, it’s just a hypothesis that’s in the room, but it’s certainly worthy of discussion that the immediate strategy might actually cause harm.”

There was no difference between the groups in peak release of myocardial enzymes, or any other safety end points, including bleeding, stroke, or renal failure, Dr. Desch said.
Further analyses showed no large differences between subgroups, including age, diabetes, first monitored rhythm, confirmed MI as the trigger of the arrest, sex, and the time from cardiac arrest to the return of spontaneous circulation, he noted.
Opportunity to minimize harm
Discussant for the results during the presentation was Susanna Price, MBBS, PhD, Royal Brompton Hospital, London.
Dr. Price concluded: “What this means for me, is it gives me information that’s useful regarding the opportunity to minimize harm, which is a lot of what critical care is about, so we don’t necessarily now have to move these patients very acutely when they’ve just come in through the ED [emergency department]. It has implications for resource utilization, but also implications for mobilizing patients around the hospital during COVID-19.”
It’s also important to note that coronary angiography was still carried out in certain patients, “so we still have to have that dialogue with our interventional cardiologists for certain patients who may need to go to the cath lab, and what it should now allow us to do is give appropriate focus to how to manage these patients when they come in to the ED or to our ICUs [intensive care units],” she said.
Dr. Price added, though, that perhaps “the most important slide” in the presentation was that showing 90% of these patients had a witnessed cardiac arrest, “and yet a third of these patients, 168 of them, had no bystander CPR at all.”
She pointed to the “chain of survival” after cardiac arrest, of which Charles D. Deakin, MD, University Hospital Southampton (England), wrote that “not all links are equal.”
“Early recognition and calling for help, early CPR, early defibrillation where appropriate are very, very important, and we need to be addressing all of these, as well as what happens in the cath lab and after admission,” Dr. Price said.
This research was funded by the German Center for Cardiovascular Research. Dr. Desch and Dr. Price reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Although inconclusive, CV safety study of cancer therapy attracts attention
The first global trial to compare the cardiovascular (CV) safety of two therapies for prostate cancer proved inconclusive because of inadequate enrollment and events, but the study is a harbinger of growth in the emerging specialty of cardio-oncology, according to experts.
“Many new cancer agents have extended patient survival, yet some of these agents have significant potential cardiovascular toxicity,” said Renato D. Lopes, MD, in presenting a study at the annual congress of the European Society of Cardiology.
In the context of improving survival in patients with or at risk for both cancer and cardiovascular disease, he suggested that the prostate cancer study he led could be “a model for interdisciplinary collaboration” needed to address the relative and sometimes competing risks of these disease states.
This point was seconded by several pioneers in cardio-oncology who participated in the discussion of the results of the trial, called PRONOUNCE.
“We know many drugs in oncology increase cardiovascular risk, so these are the types of trials we need,” according Thomas M. Suter, MD, who leads the cardio-oncology service at the University Hospital, Berne, Switzerland. He was the ESC-invited discussant for PRONOUNCE.
More than 100 centers in 12 countries involved
In PRONOUNCE, 545 patients with prostate cancer and established atherosclerotic cardiovascular disease were randomized to degarelix, a gonadotropin-releasing hormone antagonist, or leuprolide, a GnRH agonist. The patients were enrolled at 113 participating centers in 12 countries. All of the patients had an indication for an androgen-deprivation therapy (ADT).
In numerous previous studies, “ADT has been associated with higher CV morbidity and mortality, particularly in men with preexisting CV disease,” explained Dr. Lopes, but the relative cardiovascular safety of GnRH agonists relative to GnRH antagonists has been “controversial.”
The PRONOUNCE study was designed to resolve this issue, but the study was terminated early because of slow enrollment (not related to the COVID-19 pandemic). The planned enrollment was 900 patients.
In addition, the rate of major adverse cardiovascular events (MACE), defined as myocardial infarction, stroke, or death, was lower over the course of follow-up than anticipated in the study design.
No significant difference on primary endpoint
At the end of 12 months, MACE occurred in 11 (4.1%) of patients randomized to leuprolide and 15 (5.5%) of those randomized to degarelix. The greater hazard ratio for MACE in the degarelix group did not approach statistical significance (hazard ratio, 1.28; P = .53).
As a result, the question of the relative CV safety of these drugs “remains unresolved,” according to Dr. Lopes, professor of medicine at Duke University Medical Center, Durham, N.C.
This does not diminish the need to answer this question. In the addition to the fact that cancer is a malignancy primarily of advancing age when CV disease is prevalent – the mean age in this study was 73 years and 44% were over age 75 – it is often an indolent disease with long periods of survival, according to Dr. Lopes. About half of prostate cancer patients have concomitant CV disease, and about half will receive ADT at some point in their treatment.
In patients receiving ADT, leuprolide is far more commonly used than GnRH antagonists, which are offered in only about 4% of patients, according to data cited by Dr. Lopes. The underlying hypothesis of this study was that leuprolide is associated with greater CV risk, which might have been relevant to a risk-benefit calculation, if the hypothesis had been confirmed.
Cancer drugs can increase CV risk
Based on experimental data, “there is concern the leuprolide is involved in plaque destabilization,” said Dr. Lopes, but he noted that ADTs in general are associated with adverse metabolic changes, including increases in LDL cholesterol, insulin resistance, and body fat, all of which could be relevant to CV risk.
It is the improving rates of survival for prostate cancer as well for other types of cancer that have increased attention to the potential for cancer drugs to increase CV risk, another major cause of early mortality. For these competing risks, objective data are needed to evaluate a relative risk-to-benefit ratio for treatment choices.
This dilemma led the ESC to recently establish its Council on Cardio-Oncology, and many centers around the world are also creating interdisciplinary groups to guide treatment choices for patients with both diseases.
“You will certainly get a lot of referrals,” said Rudolf de Boer, MD, professor of translational cardiology, University Medical Center, Groningen, Netherlands. Basing his remark on his own experience starting a cardio-oncology clinic at his institution, he called this work challenging and agreed that the need for objective data is urgent.
“We need data to provide common ground on which to judge relative risks,” Dr. de Boer said. He also praised the PRONOUNCE investigators for their efforts even if the data failed to answer the question posed.
The PRONOUNCE results were published online in Circulation at the time of Dr. Lopes’s presentation.
The study received funding from Ferring Pharmaceuticals. Dr. Lopes reports financial relationships with Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, Pfizer, and Sanofi. Dr. Suter reports financial relationships with Boehringer Ingelheim, GlaxoSmithKline, and Roche. Dr. de Boer reports financial relationships with AstraZeneca, Abbott, Bristol-Myers Squibb, Novartis, Novo Nordisk, and Roche.
The first global trial to compare the cardiovascular (CV) safety of two therapies for prostate cancer proved inconclusive because of inadequate enrollment and events, but the study is a harbinger of growth in the emerging specialty of cardio-oncology, according to experts.
“Many new cancer agents have extended patient survival, yet some of these agents have significant potential cardiovascular toxicity,” said Renato D. Lopes, MD, in presenting a study at the annual congress of the European Society of Cardiology.
In the context of improving survival in patients with or at risk for both cancer and cardiovascular disease, he suggested that the prostate cancer study he led could be “a model for interdisciplinary collaboration” needed to address the relative and sometimes competing risks of these disease states.
This point was seconded by several pioneers in cardio-oncology who participated in the discussion of the results of the trial, called PRONOUNCE.
“We know many drugs in oncology increase cardiovascular risk, so these are the types of trials we need,” according Thomas M. Suter, MD, who leads the cardio-oncology service at the University Hospital, Berne, Switzerland. He was the ESC-invited discussant for PRONOUNCE.
More than 100 centers in 12 countries involved
In PRONOUNCE, 545 patients with prostate cancer and established atherosclerotic cardiovascular disease were randomized to degarelix, a gonadotropin-releasing hormone antagonist, or leuprolide, a GnRH agonist. The patients were enrolled at 113 participating centers in 12 countries. All of the patients had an indication for an androgen-deprivation therapy (ADT).
In numerous previous studies, “ADT has been associated with higher CV morbidity and mortality, particularly in men with preexisting CV disease,” explained Dr. Lopes, but the relative cardiovascular safety of GnRH agonists relative to GnRH antagonists has been “controversial.”
The PRONOUNCE study was designed to resolve this issue, but the study was terminated early because of slow enrollment (not related to the COVID-19 pandemic). The planned enrollment was 900 patients.
In addition, the rate of major adverse cardiovascular events (MACE), defined as myocardial infarction, stroke, or death, was lower over the course of follow-up than anticipated in the study design.
No significant difference on primary endpoint
At the end of 12 months, MACE occurred in 11 (4.1%) of patients randomized to leuprolide and 15 (5.5%) of those randomized to degarelix. The greater hazard ratio for MACE in the degarelix group did not approach statistical significance (hazard ratio, 1.28; P = .53).
As a result, the question of the relative CV safety of these drugs “remains unresolved,” according to Dr. Lopes, professor of medicine at Duke University Medical Center, Durham, N.C.
This does not diminish the need to answer this question. In the addition to the fact that cancer is a malignancy primarily of advancing age when CV disease is prevalent – the mean age in this study was 73 years and 44% were over age 75 – it is often an indolent disease with long periods of survival, according to Dr. Lopes. About half of prostate cancer patients have concomitant CV disease, and about half will receive ADT at some point in their treatment.
In patients receiving ADT, leuprolide is far more commonly used than GnRH antagonists, which are offered in only about 4% of patients, according to data cited by Dr. Lopes. The underlying hypothesis of this study was that leuprolide is associated with greater CV risk, which might have been relevant to a risk-benefit calculation, if the hypothesis had been confirmed.
Cancer drugs can increase CV risk
Based on experimental data, “there is concern the leuprolide is involved in plaque destabilization,” said Dr. Lopes, but he noted that ADTs in general are associated with adverse metabolic changes, including increases in LDL cholesterol, insulin resistance, and body fat, all of which could be relevant to CV risk.
It is the improving rates of survival for prostate cancer as well for other types of cancer that have increased attention to the potential for cancer drugs to increase CV risk, another major cause of early mortality. For these competing risks, objective data are needed to evaluate a relative risk-to-benefit ratio for treatment choices.
This dilemma led the ESC to recently establish its Council on Cardio-Oncology, and many centers around the world are also creating interdisciplinary groups to guide treatment choices for patients with both diseases.
“You will certainly get a lot of referrals,” said Rudolf de Boer, MD, professor of translational cardiology, University Medical Center, Groningen, Netherlands. Basing his remark on his own experience starting a cardio-oncology clinic at his institution, he called this work challenging and agreed that the need for objective data is urgent.
“We need data to provide common ground on which to judge relative risks,” Dr. de Boer said. He also praised the PRONOUNCE investigators for their efforts even if the data failed to answer the question posed.
The PRONOUNCE results were published online in Circulation at the time of Dr. Lopes’s presentation.
The study received funding from Ferring Pharmaceuticals. Dr. Lopes reports financial relationships with Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, Pfizer, and Sanofi. Dr. Suter reports financial relationships with Boehringer Ingelheim, GlaxoSmithKline, and Roche. Dr. de Boer reports financial relationships with AstraZeneca, Abbott, Bristol-Myers Squibb, Novartis, Novo Nordisk, and Roche.
The first global trial to compare the cardiovascular (CV) safety of two therapies for prostate cancer proved inconclusive because of inadequate enrollment and events, but the study is a harbinger of growth in the emerging specialty of cardio-oncology, according to experts.
“Many new cancer agents have extended patient survival, yet some of these agents have significant potential cardiovascular toxicity,” said Renato D. Lopes, MD, in presenting a study at the annual congress of the European Society of Cardiology.
In the context of improving survival in patients with or at risk for both cancer and cardiovascular disease, he suggested that the prostate cancer study he led could be “a model for interdisciplinary collaboration” needed to address the relative and sometimes competing risks of these disease states.
This point was seconded by several pioneers in cardio-oncology who participated in the discussion of the results of the trial, called PRONOUNCE.
“We know many drugs in oncology increase cardiovascular risk, so these are the types of trials we need,” according Thomas M. Suter, MD, who leads the cardio-oncology service at the University Hospital, Berne, Switzerland. He was the ESC-invited discussant for PRONOUNCE.
More than 100 centers in 12 countries involved
In PRONOUNCE, 545 patients with prostate cancer and established atherosclerotic cardiovascular disease were randomized to degarelix, a gonadotropin-releasing hormone antagonist, or leuprolide, a GnRH agonist. The patients were enrolled at 113 participating centers in 12 countries. All of the patients had an indication for an androgen-deprivation therapy (ADT).
In numerous previous studies, “ADT has been associated with higher CV morbidity and mortality, particularly in men with preexisting CV disease,” explained Dr. Lopes, but the relative cardiovascular safety of GnRH agonists relative to GnRH antagonists has been “controversial.”
The PRONOUNCE study was designed to resolve this issue, but the study was terminated early because of slow enrollment (not related to the COVID-19 pandemic). The planned enrollment was 900 patients.
In addition, the rate of major adverse cardiovascular events (MACE), defined as myocardial infarction, stroke, or death, was lower over the course of follow-up than anticipated in the study design.
No significant difference on primary endpoint
At the end of 12 months, MACE occurred in 11 (4.1%) of patients randomized to leuprolide and 15 (5.5%) of those randomized to degarelix. The greater hazard ratio for MACE in the degarelix group did not approach statistical significance (hazard ratio, 1.28; P = .53).
As a result, the question of the relative CV safety of these drugs “remains unresolved,” according to Dr. Lopes, professor of medicine at Duke University Medical Center, Durham, N.C.
This does not diminish the need to answer this question. In the addition to the fact that cancer is a malignancy primarily of advancing age when CV disease is prevalent – the mean age in this study was 73 years and 44% were over age 75 – it is often an indolent disease with long periods of survival, according to Dr. Lopes. About half of prostate cancer patients have concomitant CV disease, and about half will receive ADT at some point in their treatment.
In patients receiving ADT, leuprolide is far more commonly used than GnRH antagonists, which are offered in only about 4% of patients, according to data cited by Dr. Lopes. The underlying hypothesis of this study was that leuprolide is associated with greater CV risk, which might have been relevant to a risk-benefit calculation, if the hypothesis had been confirmed.
Cancer drugs can increase CV risk
Based on experimental data, “there is concern the leuprolide is involved in plaque destabilization,” said Dr. Lopes, but he noted that ADTs in general are associated with adverse metabolic changes, including increases in LDL cholesterol, insulin resistance, and body fat, all of which could be relevant to CV risk.
It is the improving rates of survival for prostate cancer as well for other types of cancer that have increased attention to the potential for cancer drugs to increase CV risk, another major cause of early mortality. For these competing risks, objective data are needed to evaluate a relative risk-to-benefit ratio for treatment choices.
This dilemma led the ESC to recently establish its Council on Cardio-Oncology, and many centers around the world are also creating interdisciplinary groups to guide treatment choices for patients with both diseases.
“You will certainly get a lot of referrals,” said Rudolf de Boer, MD, professor of translational cardiology, University Medical Center, Groningen, Netherlands. Basing his remark on his own experience starting a cardio-oncology clinic at his institution, he called this work challenging and agreed that the need for objective data is urgent.
“We need data to provide common ground on which to judge relative risks,” Dr. de Boer said. He also praised the PRONOUNCE investigators for their efforts even if the data failed to answer the question posed.
The PRONOUNCE results were published online in Circulation at the time of Dr. Lopes’s presentation.
The study received funding from Ferring Pharmaceuticals. Dr. Lopes reports financial relationships with Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, Pfizer, and Sanofi. Dr. Suter reports financial relationships with Boehringer Ingelheim, GlaxoSmithKline, and Roche. Dr. de Boer reports financial relationships with AstraZeneca, Abbott, Bristol-Myers Squibb, Novartis, Novo Nordisk, and Roche.
FROM ESC 2021
Walnuts lowered LDL cholesterol in healthy seniors: WAHA study
Benefit sustained over 2 years
Healthy elderly people who ate a walnut-supplemented diet for 2 years showed significant reductions in LDL cholesterol, according to a randomized study that used imaging to evaluate lipid changes.
“Regularly eating walnuts will lower your LDL cholesterol and improve the quality of LDL particles, rendering them less prone to enter the arterial wall and build up atherosclerosis, and this will occur without unwanted weight gain in spite of the high-fat – healthy vegetable fat, though – content of walnuts,” Emilio Ros, MD, PhD, senior author of the Walnuts and Healthy Aging (WAHA) study, said in an interview.
WAHA is a parallel-group, randomized, controlled trial that followed 636 patients over 2 years at centers in Loma Linda, Calif., and Barcelona. They were randomly assigned to either a walnut-free or walnut-supplemented diet, and every 2 months they were underwent nuclear magnetic resonance spectroscopy and recorded their compliance, toleration, medication changes, and body weight.
The researchers reported “significantly decreased” total cholesterol, LDL cholesterol and intermediate-density lipoprotein cholesterol, along with reductions in total LDL cholesterol particles and small LDL cholesterol particle number in patients on a walnut-supplemented diet, compared with controls. However, triglycerides and HDL cholesterol were unaffected.
Study results
The study reported mean reductions in the following lipid categories among what the researchers called the “walnut group”:
- Total cholesterol, –8.5 mg/dL (95% confidence interval, –11.2 to –5.4), a 4.4% mean reduction.
- LDL-C, –4.3 mg/dL (95% CI, –6.6 to –1.6), a 3.6% reduction.
- Intermediate-density lipoprotein cholesterol, –1.3 mg/dL (95% CI, –1.5 to –1.0] for a 16.8% reduction.
- Total LDL cholesterol particles, a reduction of 4.3%.
- Small LDL cholesterol particle number, a 6.1% decrease.
“WAHA is the largest and longest randomized nut trial to date, which overcomes power limitations of former trials, smaller and of shorter duration,” said Dr. Ros, of the lipid clinic, endocrinology, nutrition service at the Hospital Clinic Villarroel at the University of Barcelona. He noted that studies he has participated in have already shown that the walnut-supplemented diet had beneficial effects on blood pressure, systemic inflammation and endothelial function.
Other strengths of the study, he said, were that it recruited patients from two distinct locations and that it retained 90% of participants over 2 years (the study started out with 708 participants).
Christie Ballantyne, MD, concurred that the size and duration of the study are worth noting. “People always have questions about what they should eat,” said Dr. Ballantyne, chief of cardiology at Baylor College of Medicine and director of cardiovascular disease prevention at Methodist DeBakey Heart Center, both in Houston, said in an interview. “It’s very difficult to do nutritional studies. Most studies are small and short term, so it’s unusual to have study that’s large with 2 years of follow-up. This is a larger-than-usual study.”
Potential study limitations
Dr. Ros did acknowledge some limitations of the study. Participants weren’t blinded, the feeding setting wasn’t controlled, and participants were generally healthy and had average normal lipid profiles because they were taking statins, which may explain the modest lipid improvements in the study. “LDL cholesterol lowering by nuts is related to baseline levels, hence the reduction observed in our study was modest,” he said.
Additionally, because the study group was elderly, the results don’t apply to younger people. “Yet,” Dr. Ros added, “we know from many prior studies that nuts in general and walnuts in particular will lower blood cholesterol regardless of age.”
Dr. Ballantyne noted that the use of nuclear magnetic resonance spectroscopy to evaluate lipid levels involves a methodology that isn’t as systematic or as standardized as the typical lipid profile, and that different systems use proprietary software to interpret results. “That’s a little bit of an issue,” he said. “What exactly do the numbers mean?”
Overall, though, Dr. Ballantyne said the study is a significant addition to the literature. “The study is large, well done, and it confirms the benefits of something we’ve been telling patients is a good choice. It’s useful because there’s so much noise. It is important because there’s tremendous confusion and misinformation about what’s really healthy to eat.”
The study was supported by a grant from the California Walnut Commission (CWC), from which Dr. Ros and two coauthors received research funding through their institutions. Dr. Ros also reported receiving compensation from CWC and serves on a CWC advisory council. The other authors have no relationships to disclose. The WAHA study was supported by a grant from the CWC, from which Dr. Ros and some coinvestigators have received research funding through their institutions. Dr. Ballantyne has no relevant relationships to disclose.
Benefit sustained over 2 years
Benefit sustained over 2 years
Healthy elderly people who ate a walnut-supplemented diet for 2 years showed significant reductions in LDL cholesterol, according to a randomized study that used imaging to evaluate lipid changes.
“Regularly eating walnuts will lower your LDL cholesterol and improve the quality of LDL particles, rendering them less prone to enter the arterial wall and build up atherosclerosis, and this will occur without unwanted weight gain in spite of the high-fat – healthy vegetable fat, though – content of walnuts,” Emilio Ros, MD, PhD, senior author of the Walnuts and Healthy Aging (WAHA) study, said in an interview.
WAHA is a parallel-group, randomized, controlled trial that followed 636 patients over 2 years at centers in Loma Linda, Calif., and Barcelona. They were randomly assigned to either a walnut-free or walnut-supplemented diet, and every 2 months they were underwent nuclear magnetic resonance spectroscopy and recorded their compliance, toleration, medication changes, and body weight.
The researchers reported “significantly decreased” total cholesterol, LDL cholesterol and intermediate-density lipoprotein cholesterol, along with reductions in total LDL cholesterol particles and small LDL cholesterol particle number in patients on a walnut-supplemented diet, compared with controls. However, triglycerides and HDL cholesterol were unaffected.
Study results
The study reported mean reductions in the following lipid categories among what the researchers called the “walnut group”:
- Total cholesterol, –8.5 mg/dL (95% confidence interval, –11.2 to –5.4), a 4.4% mean reduction.
- LDL-C, –4.3 mg/dL (95% CI, –6.6 to –1.6), a 3.6% reduction.
- Intermediate-density lipoprotein cholesterol, –1.3 mg/dL (95% CI, –1.5 to –1.0] for a 16.8% reduction.
- Total LDL cholesterol particles, a reduction of 4.3%.
- Small LDL cholesterol particle number, a 6.1% decrease.
“WAHA is the largest and longest randomized nut trial to date, which overcomes power limitations of former trials, smaller and of shorter duration,” said Dr. Ros, of the lipid clinic, endocrinology, nutrition service at the Hospital Clinic Villarroel at the University of Barcelona. He noted that studies he has participated in have already shown that the walnut-supplemented diet had beneficial effects on blood pressure, systemic inflammation and endothelial function.
Other strengths of the study, he said, were that it recruited patients from two distinct locations and that it retained 90% of participants over 2 years (the study started out with 708 participants).
Christie Ballantyne, MD, concurred that the size and duration of the study are worth noting. “People always have questions about what they should eat,” said Dr. Ballantyne, chief of cardiology at Baylor College of Medicine and director of cardiovascular disease prevention at Methodist DeBakey Heart Center, both in Houston, said in an interview. “It’s very difficult to do nutritional studies. Most studies are small and short term, so it’s unusual to have study that’s large with 2 years of follow-up. This is a larger-than-usual study.”
Potential study limitations
Dr. Ros did acknowledge some limitations of the study. Participants weren’t blinded, the feeding setting wasn’t controlled, and participants were generally healthy and had average normal lipid profiles because they were taking statins, which may explain the modest lipid improvements in the study. “LDL cholesterol lowering by nuts is related to baseline levels, hence the reduction observed in our study was modest,” he said.
Additionally, because the study group was elderly, the results don’t apply to younger people. “Yet,” Dr. Ros added, “we know from many prior studies that nuts in general and walnuts in particular will lower blood cholesterol regardless of age.”
Dr. Ballantyne noted that the use of nuclear magnetic resonance spectroscopy to evaluate lipid levels involves a methodology that isn’t as systematic or as standardized as the typical lipid profile, and that different systems use proprietary software to interpret results. “That’s a little bit of an issue,” he said. “What exactly do the numbers mean?”
Overall, though, Dr. Ballantyne said the study is a significant addition to the literature. “The study is large, well done, and it confirms the benefits of something we’ve been telling patients is a good choice. It’s useful because there’s so much noise. It is important because there’s tremendous confusion and misinformation about what’s really healthy to eat.”
The study was supported by a grant from the California Walnut Commission (CWC), from which Dr. Ros and two coauthors received research funding through their institutions. Dr. Ros also reported receiving compensation from CWC and serves on a CWC advisory council. The other authors have no relationships to disclose. The WAHA study was supported by a grant from the CWC, from which Dr. Ros and some coinvestigators have received research funding through their institutions. Dr. Ballantyne has no relevant relationships to disclose.
Healthy elderly people who ate a walnut-supplemented diet for 2 years showed significant reductions in LDL cholesterol, according to a randomized study that used imaging to evaluate lipid changes.
“Regularly eating walnuts will lower your LDL cholesterol and improve the quality of LDL particles, rendering them less prone to enter the arterial wall and build up atherosclerosis, and this will occur without unwanted weight gain in spite of the high-fat – healthy vegetable fat, though – content of walnuts,” Emilio Ros, MD, PhD, senior author of the Walnuts and Healthy Aging (WAHA) study, said in an interview.
WAHA is a parallel-group, randomized, controlled trial that followed 636 patients over 2 years at centers in Loma Linda, Calif., and Barcelona. They were randomly assigned to either a walnut-free or walnut-supplemented diet, and every 2 months they were underwent nuclear magnetic resonance spectroscopy and recorded their compliance, toleration, medication changes, and body weight.
The researchers reported “significantly decreased” total cholesterol, LDL cholesterol and intermediate-density lipoprotein cholesterol, along with reductions in total LDL cholesterol particles and small LDL cholesterol particle number in patients on a walnut-supplemented diet, compared with controls. However, triglycerides and HDL cholesterol were unaffected.
Study results
The study reported mean reductions in the following lipid categories among what the researchers called the “walnut group”:
- Total cholesterol, –8.5 mg/dL (95% confidence interval, –11.2 to –5.4), a 4.4% mean reduction.
- LDL-C, –4.3 mg/dL (95% CI, –6.6 to –1.6), a 3.6% reduction.
- Intermediate-density lipoprotein cholesterol, –1.3 mg/dL (95% CI, –1.5 to –1.0] for a 16.8% reduction.
- Total LDL cholesterol particles, a reduction of 4.3%.
- Small LDL cholesterol particle number, a 6.1% decrease.
“WAHA is the largest and longest randomized nut trial to date, which overcomes power limitations of former trials, smaller and of shorter duration,” said Dr. Ros, of the lipid clinic, endocrinology, nutrition service at the Hospital Clinic Villarroel at the University of Barcelona. He noted that studies he has participated in have already shown that the walnut-supplemented diet had beneficial effects on blood pressure, systemic inflammation and endothelial function.
Other strengths of the study, he said, were that it recruited patients from two distinct locations and that it retained 90% of participants over 2 years (the study started out with 708 participants).
Christie Ballantyne, MD, concurred that the size and duration of the study are worth noting. “People always have questions about what they should eat,” said Dr. Ballantyne, chief of cardiology at Baylor College of Medicine and director of cardiovascular disease prevention at Methodist DeBakey Heart Center, both in Houston, said in an interview. “It’s very difficult to do nutritional studies. Most studies are small and short term, so it’s unusual to have study that’s large with 2 years of follow-up. This is a larger-than-usual study.”
Potential study limitations
Dr. Ros did acknowledge some limitations of the study. Participants weren’t blinded, the feeding setting wasn’t controlled, and participants were generally healthy and had average normal lipid profiles because they were taking statins, which may explain the modest lipid improvements in the study. “LDL cholesterol lowering by nuts is related to baseline levels, hence the reduction observed in our study was modest,” he said.
Additionally, because the study group was elderly, the results don’t apply to younger people. “Yet,” Dr. Ros added, “we know from many prior studies that nuts in general and walnuts in particular will lower blood cholesterol regardless of age.”
Dr. Ballantyne noted that the use of nuclear magnetic resonance spectroscopy to evaluate lipid levels involves a methodology that isn’t as systematic or as standardized as the typical lipid profile, and that different systems use proprietary software to interpret results. “That’s a little bit of an issue,” he said. “What exactly do the numbers mean?”
Overall, though, Dr. Ballantyne said the study is a significant addition to the literature. “The study is large, well done, and it confirms the benefits of something we’ve been telling patients is a good choice. It’s useful because there’s so much noise. It is important because there’s tremendous confusion and misinformation about what’s really healthy to eat.”
The study was supported by a grant from the California Walnut Commission (CWC), from which Dr. Ros and two coauthors received research funding through their institutions. Dr. Ros also reported receiving compensation from CWC and serves on a CWC advisory council. The other authors have no relationships to disclose. The WAHA study was supported by a grant from the CWC, from which Dr. Ros and some coinvestigators have received research funding through their institutions. Dr. Ballantyne has no relevant relationships to disclose.
FROM CIRCULATION
SSaSS: Salt substitute shows clear reduction in stroke, CV events, death
Switching from regular salt to a low-sodium salt substitute has major public health benefits, including a reduction in stroke, cardiovascular events, and death, a new landmark study shows.
The Salt Substitute and Stroke Study (SSaSS) was conducted in 21,000 people with a history of stroke or high blood pressure in rural China, with half of them using a lower-sodium salt substitute instead of regular salt.
Results showed that after 5 years, those using the salt substitute had a 14% reduction in stroke, a 13% reduction in major cardiovascular events, and a 12% reduction in death. These benefits were achieved without any apparent adverse effects.
The trial was presented by Bruce Neal, MB, George Institute for Global Health, Sydney, Australia, on Aug. 29 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“This is one of the largest dietary intervention trials ever conducted and has shown very clear evidence of protection against stroke, cardiovascular events, and premature death, with no adverse effects with a very simple and low-cost intervention,” Dr. Neal concluded. “This is a very easy thing to work into the diet. You just replace regular salt with a substitute that looks and tastes almost identical,” he added.
Addressing the issue of whether these results are generalizable to other populations, Dr. Neal said, “We believe the results are relevant to everyone who eats salt.
“The way the body manages sodium and potassium and their association with blood pressure is highly consistent across different populations,” he said. “Almost everyone, with the exception of a few people with serious kidney disease, should be avoiding salt or switching to a salt substitute and expect to see some benefit of this.”
Commentators at the ESC presentation lauded the study as “magnificent,” with “extraordinary” results and “very powerful implications.”
Designated discussant, hypertension expert Bryan Williams, MD, University College London, said the SSaSS was “probably the most important study with regards to public health that we will see.” He described the reductions in stroke, cardiovascular events, and death as “extraordinary for such a simple intervention.”
Dr. Williams added: “Those who have doubted the benefits of salt restriction must now admit they were wrong. The debate stops here. The data are in. Global health interventions to implement these findings must now begin.”
He also highlighted the large number of events in the trial. “This was a large, pragmatic, long-duration study in a high-risk population, and with 5,000 cardiovascular events it gives enormous power to show benefits.”
Chair of the ESC session, Barbara Casadei, MD, DPhil, John Radcliffe Hospital, Oxford (England), said the SSaSS “will change the way we think about salt and be remembered for years to come.”
Noting that the benefits were seen in all subgroups across the study, Bertram Pitt, MD, University of Michigan, Ann Arbor, was particularly excited about the stroke reduction seen in patients with diabetes, noting that several recent trials of new diabetes drugs have not managed to show a reduction in stroke.
“For patients with diabetes, this is a really important intervention,” he stated.
However, an editorial accompanying the NEJM publication gave a somewhat less enthusiastic response to the study than the ESC commentators.
Julie R. Ingelfinger, MD, deputy editor of the journal, points out that serial monitoring of potassium levels was not performed in the trial, so it is possible that hyperkalemic episodes were not detected, and persons with a history of medical conditions that may be associated with hyperkalemia were not studied.
She also noted that because the salt substitute was distributed to families, it would have been instructive to have data on the household members without risk factors, but no such data were obtained.
“Overall, the SSaSS provides some intriguing hints, but wider effectiveness is hard to predict, given limited generalizability,” she concluded.
Cluster-randomized trial
The SSaSS was an open-label, cluster-randomized trial involving 20,995 people from 600 villages in rural China who had a history of stroke or were 60 years of age or older and had uncontrolled hypertension. Patients with a history of severe kidney disease and those taking potassium supplements or potassium-sparing diuretics were excluded.
They were randomly assigned in a 1:1 ratio to the intervention group, in which the participants used a salt substitute (roughly 75% sodium chloride and 25% potassium chloride), or to the control group, in which the participants continued to use regular salt (100% sodium chloride).
Results showed that after a mean follow-up of 4.74 years, systolic blood pressure was reduced by 3.3 mm Hg in the salt substitute group.
The rate of stroke, the primary endpoint, was 29.14 events per 1,000 person-years in the salt substitute group vs. 33.65 events per 1,000 person-years with regular salt (rate ratio, 0.86; 95% confidence interval, 0.77-0.96; P = .006).
The rates of major cardiovascular events were 49.09 events per 1,000 person-years in the salt substitute group vs. 56.29 events per 1,000 person-years in those using regular salt (rate ratio, 0.87; 95% CI, 0.80-0.94; P < .001).
And the rate of death was 39.28 events per 1,000 person-years with the salt substitute vs. 44.61 events per 1,000 person-years with regular salt (rate ratio, 0.88; 95% CI, 0.82-0.95; P < .001).
The rate of serious adverse events attributed to hyperkalemia was not significantly higher with the salt substitute than with regular salt (3.35 events vs. 3.30 events per 1,000 person-years; rate ratio, 1.04; 95% CI, 0.80-1.37; P = .76).
Dr. Neal reported that 7%-8% of the control group started using salt substitute over the study period, so these results have likely underestimated the true effect of switching to a salt substitute product.
Noting that about 10 million cardiovascular events occur each year in China, he said the study results suggested that using salt substitute instead of regular salt could prevent about 10% of these events.
Food manufacturers must make changes
Dr. Neal acknowledged that a limitation of the study was the fact it was conducted in a single country, which would raise issues of generalizability. But he said he believes the results are generalizable to other populations.
Those who would get the most benefit from switching to a salt substitute are those who consume large amounts of discretionary salt – salt added at home at the time of cooking for preservation of food or seasoning. “This is salt that is easy to replace with salt substitute,” Dr. Neal noted.
“There are more than 5 billion people in the world that consume more than 50% of their salt intake as discretionary salt – mainly in the developing world. These people would expect to get significant health benefits from a switch to salt substitute.”
He pointed out that salt substitute is low cost and is easy to manufacture. “Salt substitutes cost around 50% more than regular salt, but this translates into just a dollar or two per person per year to make the switch.”
Dr. Neal said the results also apply to higher-income countries but must be implemented by governments and food manufactures, as most salt in these countries comes from processed foods.
“This study provides strong evidence to take to the food industry,” he concluded. “We would like to see food manufacturers switch to using salt substitute and for salt substitute products to be widely available on supermarket shelves. We also urge governments to take action to promote use of salt substitutes over regular salt. This could take the form of taxing regular salt or subsidies for use of salt substitutes.”
The SSaSS was supported by grants from the National Health and Medical Research Council of Australia. Dr. Neal reports no disclosures. Dr. Ingelfinger is employed by the New England Journal of Medicine as deputy editor.
A version of this article first appeared on Medscape.com.
Switching from regular salt to a low-sodium salt substitute has major public health benefits, including a reduction in stroke, cardiovascular events, and death, a new landmark study shows.
The Salt Substitute and Stroke Study (SSaSS) was conducted in 21,000 people with a history of stroke or high blood pressure in rural China, with half of them using a lower-sodium salt substitute instead of regular salt.
Results showed that after 5 years, those using the salt substitute had a 14% reduction in stroke, a 13% reduction in major cardiovascular events, and a 12% reduction in death. These benefits were achieved without any apparent adverse effects.
The trial was presented by Bruce Neal, MB, George Institute for Global Health, Sydney, Australia, on Aug. 29 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“This is one of the largest dietary intervention trials ever conducted and has shown very clear evidence of protection against stroke, cardiovascular events, and premature death, with no adverse effects with a very simple and low-cost intervention,” Dr. Neal concluded. “This is a very easy thing to work into the diet. You just replace regular salt with a substitute that looks and tastes almost identical,” he added.
Addressing the issue of whether these results are generalizable to other populations, Dr. Neal said, “We believe the results are relevant to everyone who eats salt.
“The way the body manages sodium and potassium and their association with blood pressure is highly consistent across different populations,” he said. “Almost everyone, with the exception of a few people with serious kidney disease, should be avoiding salt or switching to a salt substitute and expect to see some benefit of this.”
Commentators at the ESC presentation lauded the study as “magnificent,” with “extraordinary” results and “very powerful implications.”
Designated discussant, hypertension expert Bryan Williams, MD, University College London, said the SSaSS was “probably the most important study with regards to public health that we will see.” He described the reductions in stroke, cardiovascular events, and death as “extraordinary for such a simple intervention.”
Dr. Williams added: “Those who have doubted the benefits of salt restriction must now admit they were wrong. The debate stops here. The data are in. Global health interventions to implement these findings must now begin.”
He also highlighted the large number of events in the trial. “This was a large, pragmatic, long-duration study in a high-risk population, and with 5,000 cardiovascular events it gives enormous power to show benefits.”
Chair of the ESC session, Barbara Casadei, MD, DPhil, John Radcliffe Hospital, Oxford (England), said the SSaSS “will change the way we think about salt and be remembered for years to come.”
Noting that the benefits were seen in all subgroups across the study, Bertram Pitt, MD, University of Michigan, Ann Arbor, was particularly excited about the stroke reduction seen in patients with diabetes, noting that several recent trials of new diabetes drugs have not managed to show a reduction in stroke.
“For patients with diabetes, this is a really important intervention,” he stated.
However, an editorial accompanying the NEJM publication gave a somewhat less enthusiastic response to the study than the ESC commentators.
Julie R. Ingelfinger, MD, deputy editor of the journal, points out that serial monitoring of potassium levels was not performed in the trial, so it is possible that hyperkalemic episodes were not detected, and persons with a history of medical conditions that may be associated with hyperkalemia were not studied.
She also noted that because the salt substitute was distributed to families, it would have been instructive to have data on the household members without risk factors, but no such data were obtained.
“Overall, the SSaSS provides some intriguing hints, but wider effectiveness is hard to predict, given limited generalizability,” she concluded.
Cluster-randomized trial
The SSaSS was an open-label, cluster-randomized trial involving 20,995 people from 600 villages in rural China who had a history of stroke or were 60 years of age or older and had uncontrolled hypertension. Patients with a history of severe kidney disease and those taking potassium supplements or potassium-sparing diuretics were excluded.
They were randomly assigned in a 1:1 ratio to the intervention group, in which the participants used a salt substitute (roughly 75% sodium chloride and 25% potassium chloride), or to the control group, in which the participants continued to use regular salt (100% sodium chloride).
Results showed that after a mean follow-up of 4.74 years, systolic blood pressure was reduced by 3.3 mm Hg in the salt substitute group.
The rate of stroke, the primary endpoint, was 29.14 events per 1,000 person-years in the salt substitute group vs. 33.65 events per 1,000 person-years with regular salt (rate ratio, 0.86; 95% confidence interval, 0.77-0.96; P = .006).
The rates of major cardiovascular events were 49.09 events per 1,000 person-years in the salt substitute group vs. 56.29 events per 1,000 person-years in those using regular salt (rate ratio, 0.87; 95% CI, 0.80-0.94; P < .001).
And the rate of death was 39.28 events per 1,000 person-years with the salt substitute vs. 44.61 events per 1,000 person-years with regular salt (rate ratio, 0.88; 95% CI, 0.82-0.95; P < .001).
The rate of serious adverse events attributed to hyperkalemia was not significantly higher with the salt substitute than with regular salt (3.35 events vs. 3.30 events per 1,000 person-years; rate ratio, 1.04; 95% CI, 0.80-1.37; P = .76).
Dr. Neal reported that 7%-8% of the control group started using salt substitute over the study period, so these results have likely underestimated the true effect of switching to a salt substitute product.
Noting that about 10 million cardiovascular events occur each year in China, he said the study results suggested that using salt substitute instead of regular salt could prevent about 10% of these events.
Food manufacturers must make changes
Dr. Neal acknowledged that a limitation of the study was the fact it was conducted in a single country, which would raise issues of generalizability. But he said he believes the results are generalizable to other populations.
Those who would get the most benefit from switching to a salt substitute are those who consume large amounts of discretionary salt – salt added at home at the time of cooking for preservation of food or seasoning. “This is salt that is easy to replace with salt substitute,” Dr. Neal noted.
“There are more than 5 billion people in the world that consume more than 50% of their salt intake as discretionary salt – mainly in the developing world. These people would expect to get significant health benefits from a switch to salt substitute.”
He pointed out that salt substitute is low cost and is easy to manufacture. “Salt substitutes cost around 50% more than regular salt, but this translates into just a dollar or two per person per year to make the switch.”
Dr. Neal said the results also apply to higher-income countries but must be implemented by governments and food manufactures, as most salt in these countries comes from processed foods.
“This study provides strong evidence to take to the food industry,” he concluded. “We would like to see food manufacturers switch to using salt substitute and for salt substitute products to be widely available on supermarket shelves. We also urge governments to take action to promote use of salt substitutes over regular salt. This could take the form of taxing regular salt or subsidies for use of salt substitutes.”
The SSaSS was supported by grants from the National Health and Medical Research Council of Australia. Dr. Neal reports no disclosures. Dr. Ingelfinger is employed by the New England Journal of Medicine as deputy editor.
A version of this article first appeared on Medscape.com.
Switching from regular salt to a low-sodium salt substitute has major public health benefits, including a reduction in stroke, cardiovascular events, and death, a new landmark study shows.
The Salt Substitute and Stroke Study (SSaSS) was conducted in 21,000 people with a history of stroke or high blood pressure in rural China, with half of them using a lower-sodium salt substitute instead of regular salt.
Results showed that after 5 years, those using the salt substitute had a 14% reduction in stroke, a 13% reduction in major cardiovascular events, and a 12% reduction in death. These benefits were achieved without any apparent adverse effects.
The trial was presented by Bruce Neal, MB, George Institute for Global Health, Sydney, Australia, on Aug. 29 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“This is one of the largest dietary intervention trials ever conducted and has shown very clear evidence of protection against stroke, cardiovascular events, and premature death, with no adverse effects with a very simple and low-cost intervention,” Dr. Neal concluded. “This is a very easy thing to work into the diet. You just replace regular salt with a substitute that looks and tastes almost identical,” he added.
Addressing the issue of whether these results are generalizable to other populations, Dr. Neal said, “We believe the results are relevant to everyone who eats salt.
“The way the body manages sodium and potassium and their association with blood pressure is highly consistent across different populations,” he said. “Almost everyone, with the exception of a few people with serious kidney disease, should be avoiding salt or switching to a salt substitute and expect to see some benefit of this.”
Commentators at the ESC presentation lauded the study as “magnificent,” with “extraordinary” results and “very powerful implications.”
Designated discussant, hypertension expert Bryan Williams, MD, University College London, said the SSaSS was “probably the most important study with regards to public health that we will see.” He described the reductions in stroke, cardiovascular events, and death as “extraordinary for such a simple intervention.”
Dr. Williams added: “Those who have doubted the benefits of salt restriction must now admit they were wrong. The debate stops here. The data are in. Global health interventions to implement these findings must now begin.”
He also highlighted the large number of events in the trial. “This was a large, pragmatic, long-duration study in a high-risk population, and with 5,000 cardiovascular events it gives enormous power to show benefits.”
Chair of the ESC session, Barbara Casadei, MD, DPhil, John Radcliffe Hospital, Oxford (England), said the SSaSS “will change the way we think about salt and be remembered for years to come.”
Noting that the benefits were seen in all subgroups across the study, Bertram Pitt, MD, University of Michigan, Ann Arbor, was particularly excited about the stroke reduction seen in patients with diabetes, noting that several recent trials of new diabetes drugs have not managed to show a reduction in stroke.
“For patients with diabetes, this is a really important intervention,” he stated.
However, an editorial accompanying the NEJM publication gave a somewhat less enthusiastic response to the study than the ESC commentators.
Julie R. Ingelfinger, MD, deputy editor of the journal, points out that serial monitoring of potassium levels was not performed in the trial, so it is possible that hyperkalemic episodes were not detected, and persons with a history of medical conditions that may be associated with hyperkalemia were not studied.
She also noted that because the salt substitute was distributed to families, it would have been instructive to have data on the household members without risk factors, but no such data were obtained.
“Overall, the SSaSS provides some intriguing hints, but wider effectiveness is hard to predict, given limited generalizability,” she concluded.
Cluster-randomized trial
The SSaSS was an open-label, cluster-randomized trial involving 20,995 people from 600 villages in rural China who had a history of stroke or were 60 years of age or older and had uncontrolled hypertension. Patients with a history of severe kidney disease and those taking potassium supplements or potassium-sparing diuretics were excluded.
They were randomly assigned in a 1:1 ratio to the intervention group, in which the participants used a salt substitute (roughly 75% sodium chloride and 25% potassium chloride), or to the control group, in which the participants continued to use regular salt (100% sodium chloride).
Results showed that after a mean follow-up of 4.74 years, systolic blood pressure was reduced by 3.3 mm Hg in the salt substitute group.
The rate of stroke, the primary endpoint, was 29.14 events per 1,000 person-years in the salt substitute group vs. 33.65 events per 1,000 person-years with regular salt (rate ratio, 0.86; 95% confidence interval, 0.77-0.96; P = .006).
The rates of major cardiovascular events were 49.09 events per 1,000 person-years in the salt substitute group vs. 56.29 events per 1,000 person-years in those using regular salt (rate ratio, 0.87; 95% CI, 0.80-0.94; P < .001).
And the rate of death was 39.28 events per 1,000 person-years with the salt substitute vs. 44.61 events per 1,000 person-years with regular salt (rate ratio, 0.88; 95% CI, 0.82-0.95; P < .001).
The rate of serious adverse events attributed to hyperkalemia was not significantly higher with the salt substitute than with regular salt (3.35 events vs. 3.30 events per 1,000 person-years; rate ratio, 1.04; 95% CI, 0.80-1.37; P = .76).
Dr. Neal reported that 7%-8% of the control group started using salt substitute over the study period, so these results have likely underestimated the true effect of switching to a salt substitute product.
Noting that about 10 million cardiovascular events occur each year in China, he said the study results suggested that using salt substitute instead of regular salt could prevent about 10% of these events.
Food manufacturers must make changes
Dr. Neal acknowledged that a limitation of the study was the fact it was conducted in a single country, which would raise issues of generalizability. But he said he believes the results are generalizable to other populations.
Those who would get the most benefit from switching to a salt substitute are those who consume large amounts of discretionary salt – salt added at home at the time of cooking for preservation of food or seasoning. “This is salt that is easy to replace with salt substitute,” Dr. Neal noted.
“There are more than 5 billion people in the world that consume more than 50% of their salt intake as discretionary salt – mainly in the developing world. These people would expect to get significant health benefits from a switch to salt substitute.”
He pointed out that salt substitute is low cost and is easy to manufacture. “Salt substitutes cost around 50% more than regular salt, but this translates into just a dollar or two per person per year to make the switch.”
Dr. Neal said the results also apply to higher-income countries but must be implemented by governments and food manufactures, as most salt in these countries comes from processed foods.
“This study provides strong evidence to take to the food industry,” he concluded. “We would like to see food manufacturers switch to using salt substitute and for salt substitute products to be widely available on supermarket shelves. We also urge governments to take action to promote use of salt substitutes over regular salt. This could take the form of taxing regular salt or subsidies for use of salt substitutes.”
The SSaSS was supported by grants from the National Health and Medical Research Council of Australia. Dr. Neal reports no disclosures. Dr. Ingelfinger is employed by the New England Journal of Medicine as deputy editor.
A version of this article first appeared on Medscape.com.
MASTER DAPT: 1 month DAPT enough after high-bleeding-risk PCI
Another trial has added to the movement toward shortening the duration of dual antiplatelet therapy (DAPT) after percutaneous coronary intervention (PCI).
In the MASTER DAPT trial involving patients at high risk for bleeding who had undergone implantation of a biodegradable-polymer sirolimus-eluting stent, switching from DAPT to single antiplatelet therapy at a median of 34 days after PCI was noninferior to the continuation of DAPT treatment for a median duration of 193 days with regard to the incidence of major adverse cardiac or cerebral events, and was associated with a lower incidence of major or clinically relevant bleeding.
The results of the study were presented by Marco Valgimigli, MD, Cardiocentro Ticino Institute, Lugano, Switzerland, on Aug. 28 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“It has been suggested in previous studies that if patients are at high bleeding risk, then they do not seem to derive ischemic benefit from prolonging DAPT, they just get the increased bleeding risk,” Dr. Valgimigli said. “But this has never been prospectively tested until now.”
He pointed out that patients at high bleeding risk are a large group, representing up to 40% of patients undergoing PCI, and the MASTER DAPT trial included “all-comer” high-bleeding-risk patients with no selection based on ischemic risk.
The trial was very well received by commentators at the ESC Hot Line presentation.
Chair of the session, Roxana Mehran, MD, Icahn School of Medicine at Mount Sinai, New York, described the trial as “practice-changing.”
And Robert Byrne, MD, Mater Private Hospital, Dublin, added: “This is a standout trial. We have become more comfortable with abbreviated DAPT in high-bleeding-risk patients, but definite evidence for this has been lacking until now. This study tells us that just 1 month of DAPT appears to be safe in that there was no increase in ischemic complications and there was a clear reduction in bleeding.”
The MASTER DAPT study involved 4,579 patients at high bleeding risk who had undergone implantation of a biodegradable-polymer sirolimus-eluting coronary stent (Ultimaster, Terumo). Around half the patients had PCI for acute coronary syndrome (ACS) and half had it electively. One month after PCI they were randomly assigned to discontinue DAPT immediately (abbreviated therapy) or to continue it for at least 2 additional months (standard therapy).
The three co-primary outcomes were net adverse clinical events (a composite of death from any cause, myocardial infarction, stroke, or major bleeding), major adverse cardiac or cerebral events (a composite of death from any cause, myocardial infarction, or stroke), and major or clinically relevant nonmajor bleeding, all assessed cumulatively at 335 days. The first two outcomes were assessed for noninferiority in the per-protocol population, and the third outcome for superiority in the intention-to-treat population.
Dual antiplatelet therapy consisted of aspirin plus a P2Y12 inhibitor. The choices of the type of P2Y12 inhibitor for DAPT and the type of monotherapy after the discontinuation of DAPT were at the discretion of the investigator. Clopidogrel was the most popular choice, used as monotherapy in 54% of the patients in the abbreviated-therapy group and as part of DAPT in 79% of patients in the standard-therapy group.
Results showed that net adverse clinical events occurred in 7.5% of the abbreviated-therapy group and in 7.7% of the standard-therapy group (difference, –0.23 percentage points; 95% confidence interval, –1.80 to 1.33 percentage points; P < .001 for noninferiority).
Major adverse cardiac or cerebral events occurred in 6.1% of the abbreviated-therapy group and 5.9% of standard therapy group (difference, 0.11 percentage points; 95% CI, –1.29 to 1.51 percentage points; P = .001 for noninferiority).
Reduction in bleeding driven by BARC-2
Major bleeding or clinically relevant nonmajor bleeding occurred in 6.5% in the abbreviated-therapy group and in 9.4% in the standard-therapy group (difference, –2.82 percentage points; 95% CI, –4.40 to –1.24 percentage points; P < .001 for superiority).
“This is a highly statistically significant reduction in bleeding giving a number needed to treat of 35,” Dr. Valgimigli said.
The lower risk for bleeding in the abbreviated-therapy group was mainly due to the lower incidence of clinically relevant nonmajor bleeding events (BARC type 2) in this group than in the standard-therapy group (4.5% vs. 6.8%).
During the discussion, Dr. Byrne pointed out that the most serious type of bleeding (BARC type 3-5) was not reduced in the abbreviated DAPT group.
Dr. Valgimigli responded that the investigators were surprised about that because previous studies indicated that this most serious bleeding would be reduced, but he suggested that this may be explained by the standard group receiving 3-6 months of DAPT rather than a year or more in previous studies. “Having said that, BARC-2 bleeding is not a trivial event,” he added.
Can results be applied to other stents?
Dr. Byrne also questioned whether the results can be applied to patients receiving other types of stents – not just Ultimaster, which is not available everywhere. Dr. Valgimigli highlighted the low rate of stent thrombosis seen with the Ultimaster stent and said, “I would be scared to assume these results are reproducible with other stents.”
But Dr. Mehran challenged this view, saying, “I’m not so sure about that. I think we can probably extrapolate.”
In an interview, Dr. Mehran added: “I think this is one of the much-needed studies in our field. For the first time, we have a randomized trial on duration of DAPT in high-bleeding-risk patients. The study was inclusive, and enrolled truly high-bleeding-risk patients, including those on oral anticoagulants.
“These results show that, although high-bleeding-risk patients are at high risk of ischemic events, just 1 month of DAPT works well for them regardless, by reducing bleeding, net adverse clinical events, and without increasing ischemic events,” she concluded.
In an editorial accompanying the publication, E. Magnus Ohman, MB, from Duke University, Durham, N.C., pointed out the wide CIs in the results, which he said introduced some uncertainly to the findings.
But he concluded that: “The findings of Dr. Valgimigli and colleagues are important and move us toward a shorter and simpler antithrombotic strategy after PCI.”
In an interview, Dr. Ohman pointed out that the Ultimaster stent is not available in the United States. “We have to think about whether this stent would perform differently to other third- or fourth-generation stents. I wouldn’t have thought so, but it is hard to say for sure.
“All in all, we are looking at shorter periods of DAPT now after PCI. Several trials have now suggested that is the way to go. The forthcoming U.S. PCI guidelines should put all the studies together and come up with recommendations on different patient groups,” he concluded.
Several commentators said they would like to see the data on the patients receiving oral anticoagulants in the study before making firm conclusions on how to translate the results into clinical practice. “This is such an important group. It is difficult to interpret the results without this data,” Dr. Ohman noted. Patients receiving oral anticoagulants, who made up 36% of the study population, will be the subject of a separate report to be presented at the ESC meeting.
The MASTER DAPT trial was supported by Terumo. Dr. Valgimigli reports research grants from Terumo, Abbott, and SMT and consulting or speaker fees from Terumo, Abbott, Daiichi Sankyo, Chiesi, Vesalio, Vifor, Avimedica, Medtronic, Boston Scientific, and AstraZeneca. Dr. Ohman reports grants from Abiomed, grants from Chiesi USA, personal fees from Cara Therapeutics, Genentech, Imbria, Impulse Dynamics, Milestone Pharmaceuticals, XyloCor, Cytokinetics, Dispersol, Otsuka, Pfizer, Cytosorbents, Neurocrine, and Paradigm, outside the submitted work.
A version of this article first appeared on Medscape.com.
Another trial has added to the movement toward shortening the duration of dual antiplatelet therapy (DAPT) after percutaneous coronary intervention (PCI).
In the MASTER DAPT trial involving patients at high risk for bleeding who had undergone implantation of a biodegradable-polymer sirolimus-eluting stent, switching from DAPT to single antiplatelet therapy at a median of 34 days after PCI was noninferior to the continuation of DAPT treatment for a median duration of 193 days with regard to the incidence of major adverse cardiac or cerebral events, and was associated with a lower incidence of major or clinically relevant bleeding.
The results of the study were presented by Marco Valgimigli, MD, Cardiocentro Ticino Institute, Lugano, Switzerland, on Aug. 28 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“It has been suggested in previous studies that if patients are at high bleeding risk, then they do not seem to derive ischemic benefit from prolonging DAPT, they just get the increased bleeding risk,” Dr. Valgimigli said. “But this has never been prospectively tested until now.”
He pointed out that patients at high bleeding risk are a large group, representing up to 40% of patients undergoing PCI, and the MASTER DAPT trial included “all-comer” high-bleeding-risk patients with no selection based on ischemic risk.
The trial was very well received by commentators at the ESC Hot Line presentation.
Chair of the session, Roxana Mehran, MD, Icahn School of Medicine at Mount Sinai, New York, described the trial as “practice-changing.”
And Robert Byrne, MD, Mater Private Hospital, Dublin, added: “This is a standout trial. We have become more comfortable with abbreviated DAPT in high-bleeding-risk patients, but definite evidence for this has been lacking until now. This study tells us that just 1 month of DAPT appears to be safe in that there was no increase in ischemic complications and there was a clear reduction in bleeding.”
The MASTER DAPT study involved 4,579 patients at high bleeding risk who had undergone implantation of a biodegradable-polymer sirolimus-eluting coronary stent (Ultimaster, Terumo). Around half the patients had PCI for acute coronary syndrome (ACS) and half had it electively. One month after PCI they were randomly assigned to discontinue DAPT immediately (abbreviated therapy) or to continue it for at least 2 additional months (standard therapy).
The three co-primary outcomes were net adverse clinical events (a composite of death from any cause, myocardial infarction, stroke, or major bleeding), major adverse cardiac or cerebral events (a composite of death from any cause, myocardial infarction, or stroke), and major or clinically relevant nonmajor bleeding, all assessed cumulatively at 335 days. The first two outcomes were assessed for noninferiority in the per-protocol population, and the third outcome for superiority in the intention-to-treat population.
Dual antiplatelet therapy consisted of aspirin plus a P2Y12 inhibitor. The choices of the type of P2Y12 inhibitor for DAPT and the type of monotherapy after the discontinuation of DAPT were at the discretion of the investigator. Clopidogrel was the most popular choice, used as monotherapy in 54% of the patients in the abbreviated-therapy group and as part of DAPT in 79% of patients in the standard-therapy group.
Results showed that net adverse clinical events occurred in 7.5% of the abbreviated-therapy group and in 7.7% of the standard-therapy group (difference, –0.23 percentage points; 95% confidence interval, –1.80 to 1.33 percentage points; P < .001 for noninferiority).
Major adverse cardiac or cerebral events occurred in 6.1% of the abbreviated-therapy group and 5.9% of standard therapy group (difference, 0.11 percentage points; 95% CI, –1.29 to 1.51 percentage points; P = .001 for noninferiority).
Reduction in bleeding driven by BARC-2
Major bleeding or clinically relevant nonmajor bleeding occurred in 6.5% in the abbreviated-therapy group and in 9.4% in the standard-therapy group (difference, –2.82 percentage points; 95% CI, –4.40 to –1.24 percentage points; P < .001 for superiority).
“This is a highly statistically significant reduction in bleeding giving a number needed to treat of 35,” Dr. Valgimigli said.
The lower risk for bleeding in the abbreviated-therapy group was mainly due to the lower incidence of clinically relevant nonmajor bleeding events (BARC type 2) in this group than in the standard-therapy group (4.5% vs. 6.8%).
During the discussion, Dr. Byrne pointed out that the most serious type of bleeding (BARC type 3-5) was not reduced in the abbreviated DAPT group.
Dr. Valgimigli responded that the investigators were surprised about that because previous studies indicated that this most serious bleeding would be reduced, but he suggested that this may be explained by the standard group receiving 3-6 months of DAPT rather than a year or more in previous studies. “Having said that, BARC-2 bleeding is not a trivial event,” he added.
Can results be applied to other stents?
Dr. Byrne also questioned whether the results can be applied to patients receiving other types of stents – not just Ultimaster, which is not available everywhere. Dr. Valgimigli highlighted the low rate of stent thrombosis seen with the Ultimaster stent and said, “I would be scared to assume these results are reproducible with other stents.”
But Dr. Mehran challenged this view, saying, “I’m not so sure about that. I think we can probably extrapolate.”
In an interview, Dr. Mehran added: “I think this is one of the much-needed studies in our field. For the first time, we have a randomized trial on duration of DAPT in high-bleeding-risk patients. The study was inclusive, and enrolled truly high-bleeding-risk patients, including those on oral anticoagulants.
“These results show that, although high-bleeding-risk patients are at high risk of ischemic events, just 1 month of DAPT works well for them regardless, by reducing bleeding, net adverse clinical events, and without increasing ischemic events,” she concluded.
In an editorial accompanying the publication, E. Magnus Ohman, MB, from Duke University, Durham, N.C., pointed out the wide CIs in the results, which he said introduced some uncertainly to the findings.
But he concluded that: “The findings of Dr. Valgimigli and colleagues are important and move us toward a shorter and simpler antithrombotic strategy after PCI.”
In an interview, Dr. Ohman pointed out that the Ultimaster stent is not available in the United States. “We have to think about whether this stent would perform differently to other third- or fourth-generation stents. I wouldn’t have thought so, but it is hard to say for sure.
“All in all, we are looking at shorter periods of DAPT now after PCI. Several trials have now suggested that is the way to go. The forthcoming U.S. PCI guidelines should put all the studies together and come up with recommendations on different patient groups,” he concluded.
Several commentators said they would like to see the data on the patients receiving oral anticoagulants in the study before making firm conclusions on how to translate the results into clinical practice. “This is such an important group. It is difficult to interpret the results without this data,” Dr. Ohman noted. Patients receiving oral anticoagulants, who made up 36% of the study population, will be the subject of a separate report to be presented at the ESC meeting.
The MASTER DAPT trial was supported by Terumo. Dr. Valgimigli reports research grants from Terumo, Abbott, and SMT and consulting or speaker fees from Terumo, Abbott, Daiichi Sankyo, Chiesi, Vesalio, Vifor, Avimedica, Medtronic, Boston Scientific, and AstraZeneca. Dr. Ohman reports grants from Abiomed, grants from Chiesi USA, personal fees from Cara Therapeutics, Genentech, Imbria, Impulse Dynamics, Milestone Pharmaceuticals, XyloCor, Cytokinetics, Dispersol, Otsuka, Pfizer, Cytosorbents, Neurocrine, and Paradigm, outside the submitted work.
A version of this article first appeared on Medscape.com.
Another trial has added to the movement toward shortening the duration of dual antiplatelet therapy (DAPT) after percutaneous coronary intervention (PCI).
In the MASTER DAPT trial involving patients at high risk for bleeding who had undergone implantation of a biodegradable-polymer sirolimus-eluting stent, switching from DAPT to single antiplatelet therapy at a median of 34 days after PCI was noninferior to the continuation of DAPT treatment for a median duration of 193 days with regard to the incidence of major adverse cardiac or cerebral events, and was associated with a lower incidence of major or clinically relevant bleeding.
The results of the study were presented by Marco Valgimigli, MD, Cardiocentro Ticino Institute, Lugano, Switzerland, on Aug. 28 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“It has been suggested in previous studies that if patients are at high bleeding risk, then they do not seem to derive ischemic benefit from prolonging DAPT, they just get the increased bleeding risk,” Dr. Valgimigli said. “But this has never been prospectively tested until now.”
He pointed out that patients at high bleeding risk are a large group, representing up to 40% of patients undergoing PCI, and the MASTER DAPT trial included “all-comer” high-bleeding-risk patients with no selection based on ischemic risk.
The trial was very well received by commentators at the ESC Hot Line presentation.
Chair of the session, Roxana Mehran, MD, Icahn School of Medicine at Mount Sinai, New York, described the trial as “practice-changing.”
And Robert Byrne, MD, Mater Private Hospital, Dublin, added: “This is a standout trial. We have become more comfortable with abbreviated DAPT in high-bleeding-risk patients, but definite evidence for this has been lacking until now. This study tells us that just 1 month of DAPT appears to be safe in that there was no increase in ischemic complications and there was a clear reduction in bleeding.”
The MASTER DAPT study involved 4,579 patients at high bleeding risk who had undergone implantation of a biodegradable-polymer sirolimus-eluting coronary stent (Ultimaster, Terumo). Around half the patients had PCI for acute coronary syndrome (ACS) and half had it electively. One month after PCI they were randomly assigned to discontinue DAPT immediately (abbreviated therapy) or to continue it for at least 2 additional months (standard therapy).
The three co-primary outcomes were net adverse clinical events (a composite of death from any cause, myocardial infarction, stroke, or major bleeding), major adverse cardiac or cerebral events (a composite of death from any cause, myocardial infarction, or stroke), and major or clinically relevant nonmajor bleeding, all assessed cumulatively at 335 days. The first two outcomes were assessed for noninferiority in the per-protocol population, and the third outcome for superiority in the intention-to-treat population.
Dual antiplatelet therapy consisted of aspirin plus a P2Y12 inhibitor. The choices of the type of P2Y12 inhibitor for DAPT and the type of monotherapy after the discontinuation of DAPT were at the discretion of the investigator. Clopidogrel was the most popular choice, used as monotherapy in 54% of the patients in the abbreviated-therapy group and as part of DAPT in 79% of patients in the standard-therapy group.
Results showed that net adverse clinical events occurred in 7.5% of the abbreviated-therapy group and in 7.7% of the standard-therapy group (difference, –0.23 percentage points; 95% confidence interval, –1.80 to 1.33 percentage points; P < .001 for noninferiority).
Major adverse cardiac or cerebral events occurred in 6.1% of the abbreviated-therapy group and 5.9% of standard therapy group (difference, 0.11 percentage points; 95% CI, –1.29 to 1.51 percentage points; P = .001 for noninferiority).
Reduction in bleeding driven by BARC-2
Major bleeding or clinically relevant nonmajor bleeding occurred in 6.5% in the abbreviated-therapy group and in 9.4% in the standard-therapy group (difference, –2.82 percentage points; 95% CI, –4.40 to –1.24 percentage points; P < .001 for superiority).
“This is a highly statistically significant reduction in bleeding giving a number needed to treat of 35,” Dr. Valgimigli said.
The lower risk for bleeding in the abbreviated-therapy group was mainly due to the lower incidence of clinically relevant nonmajor bleeding events (BARC type 2) in this group than in the standard-therapy group (4.5% vs. 6.8%).
During the discussion, Dr. Byrne pointed out that the most serious type of bleeding (BARC type 3-5) was not reduced in the abbreviated DAPT group.
Dr. Valgimigli responded that the investigators were surprised about that because previous studies indicated that this most serious bleeding would be reduced, but he suggested that this may be explained by the standard group receiving 3-6 months of DAPT rather than a year or more in previous studies. “Having said that, BARC-2 bleeding is not a trivial event,” he added.
Can results be applied to other stents?
Dr. Byrne also questioned whether the results can be applied to patients receiving other types of stents – not just Ultimaster, which is not available everywhere. Dr. Valgimigli highlighted the low rate of stent thrombosis seen with the Ultimaster stent and said, “I would be scared to assume these results are reproducible with other stents.”
But Dr. Mehran challenged this view, saying, “I’m not so sure about that. I think we can probably extrapolate.”
In an interview, Dr. Mehran added: “I think this is one of the much-needed studies in our field. For the first time, we have a randomized trial on duration of DAPT in high-bleeding-risk patients. The study was inclusive, and enrolled truly high-bleeding-risk patients, including those on oral anticoagulants.
“These results show that, although high-bleeding-risk patients are at high risk of ischemic events, just 1 month of DAPT works well for them regardless, by reducing bleeding, net adverse clinical events, and without increasing ischemic events,” she concluded.
In an editorial accompanying the publication, E. Magnus Ohman, MB, from Duke University, Durham, N.C., pointed out the wide CIs in the results, which he said introduced some uncertainly to the findings.
But he concluded that: “The findings of Dr. Valgimigli and colleagues are important and move us toward a shorter and simpler antithrombotic strategy after PCI.”
In an interview, Dr. Ohman pointed out that the Ultimaster stent is not available in the United States. “We have to think about whether this stent would perform differently to other third- or fourth-generation stents. I wouldn’t have thought so, but it is hard to say for sure.
“All in all, we are looking at shorter periods of DAPT now after PCI. Several trials have now suggested that is the way to go. The forthcoming U.S. PCI guidelines should put all the studies together and come up with recommendations on different patient groups,” he concluded.
Several commentators said they would like to see the data on the patients receiving oral anticoagulants in the study before making firm conclusions on how to translate the results into clinical practice. “This is such an important group. It is difficult to interpret the results without this data,” Dr. Ohman noted. Patients receiving oral anticoagulants, who made up 36% of the study population, will be the subject of a separate report to be presented at the ESC meeting.
The MASTER DAPT trial was supported by Terumo. Dr. Valgimigli reports research grants from Terumo, Abbott, and SMT and consulting or speaker fees from Terumo, Abbott, Daiichi Sankyo, Chiesi, Vesalio, Vifor, Avimedica, Medtronic, Boston Scientific, and AstraZeneca. Dr. Ohman reports grants from Abiomed, grants from Chiesi USA, personal fees from Cara Therapeutics, Genentech, Imbria, Impulse Dynamics, Milestone Pharmaceuticals, XyloCor, Cytokinetics, Dispersol, Otsuka, Pfizer, Cytosorbents, Neurocrine, and Paradigm, outside the submitted work.
A version of this article first appeared on Medscape.com.
In all-comer approach, FFR adds no value to angiography: RIPCORD 2
Study confirms selective application
In patients with coronary artery disease scheduled for a percutaneous intervention (PCI), fractional flow reserve (FFR) assessment at the time of angiography significantly improves outcome, but it has no apparent value as a routine study in all CAD patients, according to the randomized RIPCORD 2 trial.
When compared to angiography alone in an all comer-strategy, the addition of FFR did not significantly change management or lower costs, but it was associated with a longer time for diagnostic assessment and more complications, Nicholas P. Curzen, BM, PhD, reported at the annual congress of the European Society of Cardiology.
As a tool for evaluating stenotic lesions in diseased vessels, FFR, also known as pressure wire assessment, allows interventionalists to target those vessels that induce ischemia without unnecessarily treating vessels with lesions that are hemodynamically nonsignificant. It is guideline recommended for patients with scheduled PCI on the basis of several randomized trials, including the landmark FAME trial.
“The results of these trials were spectacular. The clinical outcomes were significantly better in the FFR group despite less stents being placed and fewer vessels being stented. And there was significantly less resource utilization in the FFR group,” said Dr. Curzen, professor of interventional cardiology, University of Southampton, England.
Hypothesis: All-comers benefit from FFR
This prompted the new trial, called RIPCORD 2. The hypothesis was that systematic FFR early in the diagnosis of CAD would reduce resource utilization and improve quality of life relative to angiography alone. Both were addressed as primary endpoints. A reduction in clinical events at 12 months was a secondary endpoint.
The 1,136 participants, all scheduled for angiographic evaluation for stable angina or non-ST elevated myocardial infarction (NSTEMI), were randomized at 17 participating centers in the United Kingdom. All underwent angiography, but the experimental arm also underwent FFR for all arteries of a size suitable for revascularization.
Resource utilization evaluated through hospital costs at 12 months was somewhat higher in the FFR group, but the difference was not significant (P =.137). There was also no significant difference (P = 0.88) between the groups in quality of life, which was measured with EQ-5D-5L, an instrument for expressing five dimensions of health on a visual analog scale.
No impact from FFR on clinical events
Furthermore, there was no difference in the rate of clinical events, whether measured by a composite endpoint of major adverse cardiac events (MACE) (P = .64) or by the components of death, stroke, myocardial infarction, and unplanned revascularization, according to Dr. Curzen.
Finally, FFR did not appear to influence subsequent management. When the intervention and control groups were compared, the proportions triaged to optimal medical therapy, optimal medical therapy plus PCI, or optimal medical therapy plus bypass grafting did not differ significantly.
Given the lack of significant differences for FFR plus angiography relative to angiography alone for any clinically relevant outcome, the addition of FFR provides "no overall advantage" in this all comer study population, Dr. Curzen concluded.
However, FFR was associated with some relative disadvantages. These included significantly longer mean procedure times (69 vs. 42.4 minutes; P < .001), significantly greater mean use of contrast (206 vs. 146.3 mL; P < .001), and a significantly higher mean radiation dose (6608.7 vs. 5029.7 cGY/cm2; P < .001). There were 10 complications (1.8%) associated with FFR.
RIPCORD 1 results provided study rationale
In the previously published nonrandomized RIPCORD 1 study, interventionalists were asked to develop a management plan on the basis of angiography alone in 200 patients with stable chest pain. When these interventionalists were then provided with FFR results, the new information resulted in a change of management plan in 36% of cases.
According to Dr. Curzen, it was this study that raised all-comer FFR as a “logical and clinically plausible question.” RIPCORD 2 provided the answer.
While he is now conducting an evaluation of a subgroup of RIPCORD 2 patients with more severe disease, “it appears that the atheroma burden on angiography is adequate” to make an appropriate management determination in most or all cases.
The invited discussant for this study, Robert Byrne, MD, BCh, PhD, director of cardiology, Mater Private Hospital, Dublin, pointed out that more angiography-alone patients in RIPCORD 2 required additional evaluation to develop a management strategy (14.7% vs. 1.8%), but he agreed that FFR offered “no reasonable benefit” in the relatively low-risk patients who were enrolled.
Results do not alter FFR indications
However, he emphasized that the lack of an advantage in this trial should in no way diminish the evidence of benefit for selective FFR use as currently recommended in guidelines. This was echoed strongly in remarks by two other interventionalists who served on the same panel after the RIPCORD 2 results were presented.
“I want to make sure that our audience does not walk away thinking that FFR is useless. This is not what was shown,” said Roxana Mehran, MD, director of interventional cardiovascular research at Icahn School of Medicine at Mount Sinai, New York. She emphasized that this was a study that found no value in a low-risk, all-comer population and is not relevant to the populations where it now has an indication.
Marco Roffi, MD, director of the interventional cardiology unit, Geneva University Hospitals, made the same point.
“These results do not take away the value of FFR in a more selected population [than that enrolled in RIPCORD 2],” Dr. Roffi said. He did not rule out the potential for benefit from adding FFR to angiography even in early disease assessment if a benefit can be demonstrated in a higher-risk population.
Dr. Curzen reports financial relationships with Abbott, Beckman Coulter, HeartFlow, and Boston Scientific, which provided funding for RIPCORD 2. Dr. Byrne reported financial relationships with the trial sponsor as well as Abbott, Biosensors, and Biotronik. Dr. Mehran reports financial relationships with more than 15 medical product companies including the sponsor of this trial. Dr. Roffi reports no relevant financial disclosures.
Study confirms selective application
Study confirms selective application
In patients with coronary artery disease scheduled for a percutaneous intervention (PCI), fractional flow reserve (FFR) assessment at the time of angiography significantly improves outcome, but it has no apparent value as a routine study in all CAD patients, according to the randomized RIPCORD 2 trial.
When compared to angiography alone in an all comer-strategy, the addition of FFR did not significantly change management or lower costs, but it was associated with a longer time for diagnostic assessment and more complications, Nicholas P. Curzen, BM, PhD, reported at the annual congress of the European Society of Cardiology.
As a tool for evaluating stenotic lesions in diseased vessels, FFR, also known as pressure wire assessment, allows interventionalists to target those vessels that induce ischemia without unnecessarily treating vessels with lesions that are hemodynamically nonsignificant. It is guideline recommended for patients with scheduled PCI on the basis of several randomized trials, including the landmark FAME trial.
“The results of these trials were spectacular. The clinical outcomes were significantly better in the FFR group despite less stents being placed and fewer vessels being stented. And there was significantly less resource utilization in the FFR group,” said Dr. Curzen, professor of interventional cardiology, University of Southampton, England.
Hypothesis: All-comers benefit from FFR
This prompted the new trial, called RIPCORD 2. The hypothesis was that systematic FFR early in the diagnosis of CAD would reduce resource utilization and improve quality of life relative to angiography alone. Both were addressed as primary endpoints. A reduction in clinical events at 12 months was a secondary endpoint.
The 1,136 participants, all scheduled for angiographic evaluation for stable angina or non-ST elevated myocardial infarction (NSTEMI), were randomized at 17 participating centers in the United Kingdom. All underwent angiography, but the experimental arm also underwent FFR for all arteries of a size suitable for revascularization.
Resource utilization evaluated through hospital costs at 12 months was somewhat higher in the FFR group, but the difference was not significant (P =.137). There was also no significant difference (P = 0.88) between the groups in quality of life, which was measured with EQ-5D-5L, an instrument for expressing five dimensions of health on a visual analog scale.
No impact from FFR on clinical events
Furthermore, there was no difference in the rate of clinical events, whether measured by a composite endpoint of major adverse cardiac events (MACE) (P = .64) or by the components of death, stroke, myocardial infarction, and unplanned revascularization, according to Dr. Curzen.
Finally, FFR did not appear to influence subsequent management. When the intervention and control groups were compared, the proportions triaged to optimal medical therapy, optimal medical therapy plus PCI, or optimal medical therapy plus bypass grafting did not differ significantly.
Given the lack of significant differences for FFR plus angiography relative to angiography alone for any clinically relevant outcome, the addition of FFR provides "no overall advantage" in this all comer study population, Dr. Curzen concluded.
However, FFR was associated with some relative disadvantages. These included significantly longer mean procedure times (69 vs. 42.4 minutes; P < .001), significantly greater mean use of contrast (206 vs. 146.3 mL; P < .001), and a significantly higher mean radiation dose (6608.7 vs. 5029.7 cGY/cm2; P < .001). There were 10 complications (1.8%) associated with FFR.
RIPCORD 1 results provided study rationale
In the previously published nonrandomized RIPCORD 1 study, interventionalists were asked to develop a management plan on the basis of angiography alone in 200 patients with stable chest pain. When these interventionalists were then provided with FFR results, the new information resulted in a change of management plan in 36% of cases.
According to Dr. Curzen, it was this study that raised all-comer FFR as a “logical and clinically plausible question.” RIPCORD 2 provided the answer.
While he is now conducting an evaluation of a subgroup of RIPCORD 2 patients with more severe disease, “it appears that the atheroma burden on angiography is adequate” to make an appropriate management determination in most or all cases.
The invited discussant for this study, Robert Byrne, MD, BCh, PhD, director of cardiology, Mater Private Hospital, Dublin, pointed out that more angiography-alone patients in RIPCORD 2 required additional evaluation to develop a management strategy (14.7% vs. 1.8%), but he agreed that FFR offered “no reasonable benefit” in the relatively low-risk patients who were enrolled.
Results do not alter FFR indications
However, he emphasized that the lack of an advantage in this trial should in no way diminish the evidence of benefit for selective FFR use as currently recommended in guidelines. This was echoed strongly in remarks by two other interventionalists who served on the same panel after the RIPCORD 2 results were presented.
“I want to make sure that our audience does not walk away thinking that FFR is useless. This is not what was shown,” said Roxana Mehran, MD, director of interventional cardiovascular research at Icahn School of Medicine at Mount Sinai, New York. She emphasized that this was a study that found no value in a low-risk, all-comer population and is not relevant to the populations where it now has an indication.
Marco Roffi, MD, director of the interventional cardiology unit, Geneva University Hospitals, made the same point.
“These results do not take away the value of FFR in a more selected population [than that enrolled in RIPCORD 2],” Dr. Roffi said. He did not rule out the potential for benefit from adding FFR to angiography even in early disease assessment if a benefit can be demonstrated in a higher-risk population.
Dr. Curzen reports financial relationships with Abbott, Beckman Coulter, HeartFlow, and Boston Scientific, which provided funding for RIPCORD 2. Dr. Byrne reported financial relationships with the trial sponsor as well as Abbott, Biosensors, and Biotronik. Dr. Mehran reports financial relationships with more than 15 medical product companies including the sponsor of this trial. Dr. Roffi reports no relevant financial disclosures.
In patients with coronary artery disease scheduled for a percutaneous intervention (PCI), fractional flow reserve (FFR) assessment at the time of angiography significantly improves outcome, but it has no apparent value as a routine study in all CAD patients, according to the randomized RIPCORD 2 trial.
When compared to angiography alone in an all comer-strategy, the addition of FFR did not significantly change management or lower costs, but it was associated with a longer time for diagnostic assessment and more complications, Nicholas P. Curzen, BM, PhD, reported at the annual congress of the European Society of Cardiology.
As a tool for evaluating stenotic lesions in diseased vessels, FFR, also known as pressure wire assessment, allows interventionalists to target those vessels that induce ischemia without unnecessarily treating vessels with lesions that are hemodynamically nonsignificant. It is guideline recommended for patients with scheduled PCI on the basis of several randomized trials, including the landmark FAME trial.
“The results of these trials were spectacular. The clinical outcomes were significantly better in the FFR group despite less stents being placed and fewer vessels being stented. And there was significantly less resource utilization in the FFR group,” said Dr. Curzen, professor of interventional cardiology, University of Southampton, England.
Hypothesis: All-comers benefit from FFR
This prompted the new trial, called RIPCORD 2. The hypothesis was that systematic FFR early in the diagnosis of CAD would reduce resource utilization and improve quality of life relative to angiography alone. Both were addressed as primary endpoints. A reduction in clinical events at 12 months was a secondary endpoint.
The 1,136 participants, all scheduled for angiographic evaluation for stable angina or non-ST elevated myocardial infarction (NSTEMI), were randomized at 17 participating centers in the United Kingdom. All underwent angiography, but the experimental arm also underwent FFR for all arteries of a size suitable for revascularization.
Resource utilization evaluated through hospital costs at 12 months was somewhat higher in the FFR group, but the difference was not significant (P =.137). There was also no significant difference (P = 0.88) between the groups in quality of life, which was measured with EQ-5D-5L, an instrument for expressing five dimensions of health on a visual analog scale.
No impact from FFR on clinical events
Furthermore, there was no difference in the rate of clinical events, whether measured by a composite endpoint of major adverse cardiac events (MACE) (P = .64) or by the components of death, stroke, myocardial infarction, and unplanned revascularization, according to Dr. Curzen.
Finally, FFR did not appear to influence subsequent management. When the intervention and control groups were compared, the proportions triaged to optimal medical therapy, optimal medical therapy plus PCI, or optimal medical therapy plus bypass grafting did not differ significantly.
Given the lack of significant differences for FFR plus angiography relative to angiography alone for any clinically relevant outcome, the addition of FFR provides "no overall advantage" in this all comer study population, Dr. Curzen concluded.
However, FFR was associated with some relative disadvantages. These included significantly longer mean procedure times (69 vs. 42.4 minutes; P < .001), significantly greater mean use of contrast (206 vs. 146.3 mL; P < .001), and a significantly higher mean radiation dose (6608.7 vs. 5029.7 cGY/cm2; P < .001). There were 10 complications (1.8%) associated with FFR.
RIPCORD 1 results provided study rationale
In the previously published nonrandomized RIPCORD 1 study, interventionalists were asked to develop a management plan on the basis of angiography alone in 200 patients with stable chest pain. When these interventionalists were then provided with FFR results, the new information resulted in a change of management plan in 36% of cases.
According to Dr. Curzen, it was this study that raised all-comer FFR as a “logical and clinically plausible question.” RIPCORD 2 provided the answer.
While he is now conducting an evaluation of a subgroup of RIPCORD 2 patients with more severe disease, “it appears that the atheroma burden on angiography is adequate” to make an appropriate management determination in most or all cases.
The invited discussant for this study, Robert Byrne, MD, BCh, PhD, director of cardiology, Mater Private Hospital, Dublin, pointed out that more angiography-alone patients in RIPCORD 2 required additional evaluation to develop a management strategy (14.7% vs. 1.8%), but he agreed that FFR offered “no reasonable benefit” in the relatively low-risk patients who were enrolled.
Results do not alter FFR indications
However, he emphasized that the lack of an advantage in this trial should in no way diminish the evidence of benefit for selective FFR use as currently recommended in guidelines. This was echoed strongly in remarks by two other interventionalists who served on the same panel after the RIPCORD 2 results were presented.
“I want to make sure that our audience does not walk away thinking that FFR is useless. This is not what was shown,” said Roxana Mehran, MD, director of interventional cardiovascular research at Icahn School of Medicine at Mount Sinai, New York. She emphasized that this was a study that found no value in a low-risk, all-comer population and is not relevant to the populations where it now has an indication.
Marco Roffi, MD, director of the interventional cardiology unit, Geneva University Hospitals, made the same point.
“These results do not take away the value of FFR in a more selected population [than that enrolled in RIPCORD 2],” Dr. Roffi said. He did not rule out the potential for benefit from adding FFR to angiography even in early disease assessment if a benefit can be demonstrated in a higher-risk population.
Dr. Curzen reports financial relationships with Abbott, Beckman Coulter, HeartFlow, and Boston Scientific, which provided funding for RIPCORD 2. Dr. Byrne reported financial relationships with the trial sponsor as well as Abbott, Biosensors, and Biotronik. Dr. Mehran reports financial relationships with more than 15 medical product companies including the sponsor of this trial. Dr. Roffi reports no relevant financial disclosures.
FROM ESC CONGRESS 2021
Ablation at an early stage of fibrosis appears critical to improved AFib control
No benefit observed if fibrosis advanced
The addition of image-guided atrial fibrosis ablation did not significantly reduce the risk of recurrence relative to pulmonary vein isolation (PVI) alone in patients with treatment-resistant atrial fibrillation (AFib), according to results of an intention-to-treat analysis of the randomized DECAAF II trial.
However, there was a significant advantage for the addition of image-guided ablation in the subgroup of patients with stage I or II fibrosis, and this is a clinically meaningful finding, Nassir F. Marrouche, MD, reported at the annual congress of the European Society of Cardiology.
“Patients at early stages [of fibrosis] appear to do well if you do a good job covering the myopathy [with scar formation], and that is an important message,” said Dr. Marrouche, the principal investigator.
The underlying hypothesis of the DECAAF trial was that ablation guided with MRI imaging would prove superior to PVI alone in the treatment of resistant AF. There were 843 participants randomized at 44 centers. At baseline, all underwent a late gadolinium-enhancement MRI, a technique that allows detection of fibrotic tissue.
After randomization, those in the control group underwent standard of care PVI alone. Those in the intervention group underwent ablation of areas of the atrium revealed to be fibrotic on the MRI scan in addition to PVI.
Five percent risk reduction not significant
After a median follow-up of 12 months, recurrence of AFib, which was the primary endpoint, was observed in 43% in the intervention group and 46.1% in the control group. The relative 5% reduction for treatment was not statistically significant (hazard ratio, 0.95; 95% confidence interval, 0.778-1.17; P = .63).
As part of the study protocol, MRI was repeated 3 months after treatment in all patients. This permitted the investigators to evaluate the degree of scar formation in relation to the fibrosis covered in the intervention group. Independent reviewers rated this coverage on levels from 1 to 5, with 5 representing complete coverage.
In this analysis, it was found that ablation resulted in higher levels of lesion formation in those with early stages of disease, defined as stage I or II fibrosis, but lower levels in advanced stages.
“The more myopathy, the more disease, the less likelihood of lesion formation,” reported Dr. Marrouche, professor of medicine in the section of cardiology at Tulane University, New Orleans.
Attributed to the greater levels of fibrosis coverage, the risk of AF recurrence over the course of follow-up was significantly reduced in the intervention relative to the control group on as-treated analysis in patients who had stage I or II fibrosis at baseline. (HR 0.841, 95% CI, 0.732-0.968; P < .05).
Subgroup data called clinically meaningful
“This has huge implications going forward,” Dr. Marrouche maintained. In the context of a series of previous trials, including DECAAF I, which associated advanced fibrosis with higher risk of failing ablation, DECAAF II provides the groundwork for “where and how to ablate.”
Taken together, the DECAAF data suggest that there is no value in ablating advanced fibrosis. Due to the poor scar formation needed to reduce risk of AF recurrence, there are no benefits to outweigh the slightly greater risk of strokes and other adverse events observed among the intervention group in the DECAAF II trial, according to Dr. Marrouche.
“If the fibrosis is advanced, do PVI only,” he said.
However, if fibrosis remains at an early stage, defined by these data as stage II or lower, the data from DECAAF indicated that there is a benefit, according to Dr. Marrouche.
“DECAAF tells you to target early disease,” he said. Asked if he would now apply these data to treatment of patients with early fibrosis, he replied, “Yes, that’s what I am concluding.”
Several aspects of the design of DECAAF II, such as the use of a follow-up MRI to assess ablation at 3 months, were praised by Paul J. Wang, MD, director, Stanford Cardiac Arrhythmia Service, Stanford (Calif.) University, but he did not agree with Dr. Marrouche’s interpretation. This included the contention that scar formation was easier to achieve in patients with less atrial fibrosis.
DECAAF II is not a positive trial
Based on his reading of the correlation coefficients, expressed as an r value, which were 0.237 and 0.493 for the low- and high-fibrosis groups, respectively, “the difference in lesion formation in low- and high-fibrosis groups seems difficult to prove,” Dr. Wang pointed out.
In addition, “the authors suggest that the failure to achieve a good ablation lesion may account for the AFib recurrence,” said Dr. Wang, editor-in-chief of the American Heart Association’s Circulation: Arrhythmia and Electrophysiology. However, due to the many other potential variables influencing this risk, “this is difficult to show.”
Ultimately, despite a benefit observed among patients with a low level of fibrosis that was identified in an as-treated subgroup, “DECAAF II joins the numerous studies [evaluating the addition of an intervention relative to PVI alone] that have not achieved the primary endpoint,” Dr. Wang concluded.
An ESC-invited discussant, Christophe Leclercq, MD, chief of cardiology at Centre Hospitalier Universitaire, Rennes, France, made the same point. He said several previous studies have made the concept of achieving greater ablation to reduce AF recurrence “attractive,” but this “was not confirmed in DECAAF II.”
He also would not endorse MRI-guided ablation in resistant AFib among patients with early disease.
“There was a positive result observed in those with a low stage of fibrosis, but there were also more complications in those undergoing MRI-guided ablation,” he said.
Dr. Marrouche reports financial relationships with Abbott, which provided funding for this study. Dr. Wang had no disclosures. Dr. Leclercq reported financial relationships with Boston Scientific, Medtronic, Sorin Group, and St. Jude Medical.
No benefit observed if fibrosis advanced
No benefit observed if fibrosis advanced
The addition of image-guided atrial fibrosis ablation did not significantly reduce the risk of recurrence relative to pulmonary vein isolation (PVI) alone in patients with treatment-resistant atrial fibrillation (AFib), according to results of an intention-to-treat analysis of the randomized DECAAF II trial.
However, there was a significant advantage for the addition of image-guided ablation in the subgroup of patients with stage I or II fibrosis, and this is a clinically meaningful finding, Nassir F. Marrouche, MD, reported at the annual congress of the European Society of Cardiology.
“Patients at early stages [of fibrosis] appear to do well if you do a good job covering the myopathy [with scar formation], and that is an important message,” said Dr. Marrouche, the principal investigator.
The underlying hypothesis of the DECAAF trial was that ablation guided with MRI imaging would prove superior to PVI alone in the treatment of resistant AF. There were 843 participants randomized at 44 centers. At baseline, all underwent a late gadolinium-enhancement MRI, a technique that allows detection of fibrotic tissue.
After randomization, those in the control group underwent standard of care PVI alone. Those in the intervention group underwent ablation of areas of the atrium revealed to be fibrotic on the MRI scan in addition to PVI.
Five percent risk reduction not significant
After a median follow-up of 12 months, recurrence of AFib, which was the primary endpoint, was observed in 43% in the intervention group and 46.1% in the control group. The relative 5% reduction for treatment was not statistically significant (hazard ratio, 0.95; 95% confidence interval, 0.778-1.17; P = .63).
As part of the study protocol, MRI was repeated 3 months after treatment in all patients. This permitted the investigators to evaluate the degree of scar formation in relation to the fibrosis covered in the intervention group. Independent reviewers rated this coverage on levels from 1 to 5, with 5 representing complete coverage.
In this analysis, it was found that ablation resulted in higher levels of lesion formation in those with early stages of disease, defined as stage I or II fibrosis, but lower levels in advanced stages.
“The more myopathy, the more disease, the less likelihood of lesion formation,” reported Dr. Marrouche, professor of medicine in the section of cardiology at Tulane University, New Orleans.
Attributed to the greater levels of fibrosis coverage, the risk of AF recurrence over the course of follow-up was significantly reduced in the intervention relative to the control group on as-treated analysis in patients who had stage I or II fibrosis at baseline. (HR 0.841, 95% CI, 0.732-0.968; P < .05).
Subgroup data called clinically meaningful
“This has huge implications going forward,” Dr. Marrouche maintained. In the context of a series of previous trials, including DECAAF I, which associated advanced fibrosis with higher risk of failing ablation, DECAAF II provides the groundwork for “where and how to ablate.”
Taken together, the DECAAF data suggest that there is no value in ablating advanced fibrosis. Due to the poor scar formation needed to reduce risk of AF recurrence, there are no benefits to outweigh the slightly greater risk of strokes and other adverse events observed among the intervention group in the DECAAF II trial, according to Dr. Marrouche.
“If the fibrosis is advanced, do PVI only,” he said.
However, if fibrosis remains at an early stage, defined by these data as stage II or lower, the data from DECAAF indicated that there is a benefit, according to Dr. Marrouche.
“DECAAF tells you to target early disease,” he said. Asked if he would now apply these data to treatment of patients with early fibrosis, he replied, “Yes, that’s what I am concluding.”
Several aspects of the design of DECAAF II, such as the use of a follow-up MRI to assess ablation at 3 months, were praised by Paul J. Wang, MD, director, Stanford Cardiac Arrhythmia Service, Stanford (Calif.) University, but he did not agree with Dr. Marrouche’s interpretation. This included the contention that scar formation was easier to achieve in patients with less atrial fibrosis.
DECAAF II is not a positive trial
Based on his reading of the correlation coefficients, expressed as an r value, which were 0.237 and 0.493 for the low- and high-fibrosis groups, respectively, “the difference in lesion formation in low- and high-fibrosis groups seems difficult to prove,” Dr. Wang pointed out.
In addition, “the authors suggest that the failure to achieve a good ablation lesion may account for the AFib recurrence,” said Dr. Wang, editor-in-chief of the American Heart Association’s Circulation: Arrhythmia and Electrophysiology. However, due to the many other potential variables influencing this risk, “this is difficult to show.”
Ultimately, despite a benefit observed among patients with a low level of fibrosis that was identified in an as-treated subgroup, “DECAAF II joins the numerous studies [evaluating the addition of an intervention relative to PVI alone] that have not achieved the primary endpoint,” Dr. Wang concluded.
An ESC-invited discussant, Christophe Leclercq, MD, chief of cardiology at Centre Hospitalier Universitaire, Rennes, France, made the same point. He said several previous studies have made the concept of achieving greater ablation to reduce AF recurrence “attractive,” but this “was not confirmed in DECAAF II.”
He also would not endorse MRI-guided ablation in resistant AFib among patients with early disease.
“There was a positive result observed in those with a low stage of fibrosis, but there were also more complications in those undergoing MRI-guided ablation,” he said.
Dr. Marrouche reports financial relationships with Abbott, which provided funding for this study. Dr. Wang had no disclosures. Dr. Leclercq reported financial relationships with Boston Scientific, Medtronic, Sorin Group, and St. Jude Medical.
The addition of image-guided atrial fibrosis ablation did not significantly reduce the risk of recurrence relative to pulmonary vein isolation (PVI) alone in patients with treatment-resistant atrial fibrillation (AFib), according to results of an intention-to-treat analysis of the randomized DECAAF II trial.
However, there was a significant advantage for the addition of image-guided ablation in the subgroup of patients with stage I or II fibrosis, and this is a clinically meaningful finding, Nassir F. Marrouche, MD, reported at the annual congress of the European Society of Cardiology.
“Patients at early stages [of fibrosis] appear to do well if you do a good job covering the myopathy [with scar formation], and that is an important message,” said Dr. Marrouche, the principal investigator.
The underlying hypothesis of the DECAAF trial was that ablation guided with MRI imaging would prove superior to PVI alone in the treatment of resistant AF. There were 843 participants randomized at 44 centers. At baseline, all underwent a late gadolinium-enhancement MRI, a technique that allows detection of fibrotic tissue.
After randomization, those in the control group underwent standard of care PVI alone. Those in the intervention group underwent ablation of areas of the atrium revealed to be fibrotic on the MRI scan in addition to PVI.
Five percent risk reduction not significant
After a median follow-up of 12 months, recurrence of AFib, which was the primary endpoint, was observed in 43% in the intervention group and 46.1% in the control group. The relative 5% reduction for treatment was not statistically significant (hazard ratio, 0.95; 95% confidence interval, 0.778-1.17; P = .63).
As part of the study protocol, MRI was repeated 3 months after treatment in all patients. This permitted the investigators to evaluate the degree of scar formation in relation to the fibrosis covered in the intervention group. Independent reviewers rated this coverage on levels from 1 to 5, with 5 representing complete coverage.
In this analysis, it was found that ablation resulted in higher levels of lesion formation in those with early stages of disease, defined as stage I or II fibrosis, but lower levels in advanced stages.
“The more myopathy, the more disease, the less likelihood of lesion formation,” reported Dr. Marrouche, professor of medicine in the section of cardiology at Tulane University, New Orleans.
Attributed to the greater levels of fibrosis coverage, the risk of AF recurrence over the course of follow-up was significantly reduced in the intervention relative to the control group on as-treated analysis in patients who had stage I or II fibrosis at baseline. (HR 0.841, 95% CI, 0.732-0.968; P < .05).
Subgroup data called clinically meaningful
“This has huge implications going forward,” Dr. Marrouche maintained. In the context of a series of previous trials, including DECAAF I, which associated advanced fibrosis with higher risk of failing ablation, DECAAF II provides the groundwork for “where and how to ablate.”
Taken together, the DECAAF data suggest that there is no value in ablating advanced fibrosis. Due to the poor scar formation needed to reduce risk of AF recurrence, there are no benefits to outweigh the slightly greater risk of strokes and other adverse events observed among the intervention group in the DECAAF II trial, according to Dr. Marrouche.
“If the fibrosis is advanced, do PVI only,” he said.
However, if fibrosis remains at an early stage, defined by these data as stage II or lower, the data from DECAAF indicated that there is a benefit, according to Dr. Marrouche.
“DECAAF tells you to target early disease,” he said. Asked if he would now apply these data to treatment of patients with early fibrosis, he replied, “Yes, that’s what I am concluding.”
Several aspects of the design of DECAAF II, such as the use of a follow-up MRI to assess ablation at 3 months, were praised by Paul J. Wang, MD, director, Stanford Cardiac Arrhythmia Service, Stanford (Calif.) University, but he did not agree with Dr. Marrouche’s interpretation. This included the contention that scar formation was easier to achieve in patients with less atrial fibrosis.
DECAAF II is not a positive trial
Based on his reading of the correlation coefficients, expressed as an r value, which were 0.237 and 0.493 for the low- and high-fibrosis groups, respectively, “the difference in lesion formation in low- and high-fibrosis groups seems difficult to prove,” Dr. Wang pointed out.
In addition, “the authors suggest that the failure to achieve a good ablation lesion may account for the AFib recurrence,” said Dr. Wang, editor-in-chief of the American Heart Association’s Circulation: Arrhythmia and Electrophysiology. However, due to the many other potential variables influencing this risk, “this is difficult to show.”
Ultimately, despite a benefit observed among patients with a low level of fibrosis that was identified in an as-treated subgroup, “DECAAF II joins the numerous studies [evaluating the addition of an intervention relative to PVI alone] that have not achieved the primary endpoint,” Dr. Wang concluded.
An ESC-invited discussant, Christophe Leclercq, MD, chief of cardiology at Centre Hospitalier Universitaire, Rennes, France, made the same point. He said several previous studies have made the concept of achieving greater ablation to reduce AF recurrence “attractive,” but this “was not confirmed in DECAAF II.”
He also would not endorse MRI-guided ablation in resistant AFib among patients with early disease.
“There was a positive result observed in those with a low stage of fibrosis, but there were also more complications in those undergoing MRI-guided ablation,” he said.
Dr. Marrouche reports financial relationships with Abbott, which provided funding for this study. Dr. Wang had no disclosures. Dr. Leclercq reported financial relationships with Boston Scientific, Medtronic, Sorin Group, and St. Jude Medical.
FROM ESC CONGRESS 2021
Colchicine effective regardless of ACS history, timing: LoDoCo2
The benefits of low-dose colchicine (Colcrys) are consistent if started months or years after acute coronary syndrome (ACS) in patients with stable coronary artery disease, a new LoDoCo2 subanalysis suggests.
As previously reported, the parent trial showed that adding colchicine 0.5 mg daily to standard care reduced the risk of the primary endpoint – a composite of cardiovascular (CV) death, myocardial infarction (MI), ischemic stroke, or ischemia-driven coronary revascularization – by 31% compared with placebo.
In the new analysis, led by Tjerk S.J. Opstal, MD, the anti-inflammatory agent was equally effective in reducing the risk of the primary endpoint in patients with no prior ACS, a recent ACS (6-24 months), remote ACS (2-7 years), or very remote ACS (> 7 years), with no interaction found between groups (P = .59).
The incidence of the primary endpoint per 100 person-years and hazard ratios (HRs) for the four groups with colchicine and placebo are as follows:
- No prior ACS: 2.8 vs. 3.4; HR, 0.81 (95% confidence interval, 0.52-1.27).
- Recent ACS: 2.4 vs. 3.3; HR, 0.75 (95% CI, 0.51-1.10).
- Remote ACS: 1.8 vs. 3.2; HR, 0.55 (95% CI, 0.37-0.82)
- Very remote ACS: 3.0 vs. 4.3; HR, 0.70 (95% CI, 0.51-0.96).
The results were reported Aug. 23 in the Journal of the American College of Cardiology.
In contrast, however, a recent subgroup analysis from the COLCOT trial reported an even greater reduction in its primary composite CV endpoint when colchicine was started within 3 days of an MI.
“The result of COLCOT could imply that initiation of colchicine treatment would be best suited directly after myocardial infarction,” Dr. Opstal, from Radboud University Medical Center, Nijmegen, the Netherlands, said in an interview. “Our subanalysis shows that later initiation of colchicine therapy in patients visiting outpatient clinics years after their ACS events is equally effective. As such, colchicine therapy should not be limited to patients with recent ACS, and should be considered in all patients with coronary artery disease.”
Dr. Opstal pointed out that the two trials targeted different populations. COLCOT enrolled 4,765 patients within a month of MI, whereas LoDoCo2 enrolled 5,522 patients who were clinically stable for at least 6 months after an ACS or coronary revascularization.
Overall, 864 LoDoCo2 patients had no prior ACS and 86% had a history of ACS, of which 1,479 were recent, 1,582 were remote, and 1,597 were very remote.
Patients with a history of very remote ACS had a numerically higher event rate for the primary outcome, but the difference was not statistically significant and could be attributed to a play of chance, noted Dr. Opstal.
The team presumed patients with more recent prior ACS would remain at higher risk of ACS recurrence than would those with a more remote ACS that had proved to be clinically stable under standard medical therapy. But, he said, the data show they were at equal risk of the primary outcome.
“This implies that current optimal medical therapy does not result in an attenuation of residual risk over time regardless of whether patients are clinically stable, and that the ongoing process of atherosclerosis results in continuously elevated risk, which warrants new avenues of therapy, such as anti-inflammatory medication,” Dr. Opstal said.
In a binary analysis, there was no difference in composite cardiovascular events between patients with and without prior ACS (HR, 0.67 vs. HR, 0.81; P value for interaction, 0.43).
Dr. Opstal observed that a lack of statistical power precludes any definitive conclusions and that a large randomized controlled trial in patients with established coronary artery disease (CAD) but no prior ACS would elucidate whether early initiation of colchicine is “warranted at the moment CAD is established but before a first ACS event, as is common practice with acetylsalicylic acid and statins.”
In addition, the ongoing OASIS 9 trial will answer the question of whether patients with an estimated glomerular filtration rate of 30-60 mL/min can safely use low-dose colchicine. The gout medication is contraindicated in patients with severe renal or hepatic impairment and in patients on drugs that inhibit both CYP3A4 or the P-glycoprotein.
In an accompanying editorial, colchicine researchers Jean-Claude Tardif, MD, and Guillaume Marquis-Gravel, MD, of the Montreal Heart Institute, Quebec, Canada, suggest that study design features likely explain the discord between the LoDoCo2 and COLCOT subgroup analyses and the lack of difference in CV event rates between patients with and without prior ACS.
The editorialists say lingering questions remain, including the value of colchicine in patients with diabetes or peripheral artery disease without known CAD, but they also point out that three 2021 meta-analyses confirmed large reductions in the risk of CV events, MI, and coronary revascularization with low-dose colchicine.
“In light of the positive results from LoDoCo2, COLCOT, and meta-analyses; its good tolerability profile; and cost-effectiveness, inflammation reduction with low-dose colchicine should be considered to treat patients with coronary disease in the absence of severe renal dysfunction,” Dr. Tardif and Dr. Marquis-Gravel concluded.
The study was supported by the National Health Medical Research Council of Australia; a grant from the Sir Charles Gairdner Research Advisory Committee; the Withering Foundation; the Netherlands Heart Foundation; the Netherlands Organization for Health Research and Development; and a consortium of Teva, Disphar, and Tiofarma in the Netherlands. The funders had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Opstal reports no relevant financial relationships. Coauthor disclosures are listed in the original article.
Dr. Tardif has received grant support from Amarin, AstraZeneca, Ceapro, DalCor Pharmaceuticals, Esperion, Ionis, Novartis, Pfizer, RegenXBio, and Sanofi; has received honoraria from AstraZeneca, DalCor Pharmaceuticals, HLS Therapeutics, Pendopharm, and Sanofi; has minor equity interest in DalCor Pharmaceuticals; and is mentioned as an author on submitted patents on pharmacogenomics-guided CETP inhibition, use of colchicine after myocardial infarction, and use of colchicine in COVID-19 (he has waived his rights in the colchicine patents and does not stand to gain financially). Dr. Marquis-Gravel has received research grants from Bayer, has received speaker honoraria from Novartis, and has served on national advisory boards for Servier, JAMP, and Bayer.
A version of this article first appeared on Medscape.com.
The benefits of low-dose colchicine (Colcrys) are consistent if started months or years after acute coronary syndrome (ACS) in patients with stable coronary artery disease, a new LoDoCo2 subanalysis suggests.
As previously reported, the parent trial showed that adding colchicine 0.5 mg daily to standard care reduced the risk of the primary endpoint – a composite of cardiovascular (CV) death, myocardial infarction (MI), ischemic stroke, or ischemia-driven coronary revascularization – by 31% compared with placebo.
In the new analysis, led by Tjerk S.J. Opstal, MD, the anti-inflammatory agent was equally effective in reducing the risk of the primary endpoint in patients with no prior ACS, a recent ACS (6-24 months), remote ACS (2-7 years), or very remote ACS (> 7 years), with no interaction found between groups (P = .59).
The incidence of the primary endpoint per 100 person-years and hazard ratios (HRs) for the four groups with colchicine and placebo are as follows:
- No prior ACS: 2.8 vs. 3.4; HR, 0.81 (95% confidence interval, 0.52-1.27).
- Recent ACS: 2.4 vs. 3.3; HR, 0.75 (95% CI, 0.51-1.10).
- Remote ACS: 1.8 vs. 3.2; HR, 0.55 (95% CI, 0.37-0.82)
- Very remote ACS: 3.0 vs. 4.3; HR, 0.70 (95% CI, 0.51-0.96).
The results were reported Aug. 23 in the Journal of the American College of Cardiology.
In contrast, however, a recent subgroup analysis from the COLCOT trial reported an even greater reduction in its primary composite CV endpoint when colchicine was started within 3 days of an MI.
“The result of COLCOT could imply that initiation of colchicine treatment would be best suited directly after myocardial infarction,” Dr. Opstal, from Radboud University Medical Center, Nijmegen, the Netherlands, said in an interview. “Our subanalysis shows that later initiation of colchicine therapy in patients visiting outpatient clinics years after their ACS events is equally effective. As such, colchicine therapy should not be limited to patients with recent ACS, and should be considered in all patients with coronary artery disease.”
Dr. Opstal pointed out that the two trials targeted different populations. COLCOT enrolled 4,765 patients within a month of MI, whereas LoDoCo2 enrolled 5,522 patients who were clinically stable for at least 6 months after an ACS or coronary revascularization.
Overall, 864 LoDoCo2 patients had no prior ACS and 86% had a history of ACS, of which 1,479 were recent, 1,582 were remote, and 1,597 were very remote.
Patients with a history of very remote ACS had a numerically higher event rate for the primary outcome, but the difference was not statistically significant and could be attributed to a play of chance, noted Dr. Opstal.
The team presumed patients with more recent prior ACS would remain at higher risk of ACS recurrence than would those with a more remote ACS that had proved to be clinically stable under standard medical therapy. But, he said, the data show they were at equal risk of the primary outcome.
“This implies that current optimal medical therapy does not result in an attenuation of residual risk over time regardless of whether patients are clinically stable, and that the ongoing process of atherosclerosis results in continuously elevated risk, which warrants new avenues of therapy, such as anti-inflammatory medication,” Dr. Opstal said.
In a binary analysis, there was no difference in composite cardiovascular events between patients with and without prior ACS (HR, 0.67 vs. HR, 0.81; P value for interaction, 0.43).
Dr. Opstal observed that a lack of statistical power precludes any definitive conclusions and that a large randomized controlled trial in patients with established coronary artery disease (CAD) but no prior ACS would elucidate whether early initiation of colchicine is “warranted at the moment CAD is established but before a first ACS event, as is common practice with acetylsalicylic acid and statins.”
In addition, the ongoing OASIS 9 trial will answer the question of whether patients with an estimated glomerular filtration rate of 30-60 mL/min can safely use low-dose colchicine. The gout medication is contraindicated in patients with severe renal or hepatic impairment and in patients on drugs that inhibit both CYP3A4 or the P-glycoprotein.
In an accompanying editorial, colchicine researchers Jean-Claude Tardif, MD, and Guillaume Marquis-Gravel, MD, of the Montreal Heart Institute, Quebec, Canada, suggest that study design features likely explain the discord between the LoDoCo2 and COLCOT subgroup analyses and the lack of difference in CV event rates between patients with and without prior ACS.
The editorialists say lingering questions remain, including the value of colchicine in patients with diabetes or peripheral artery disease without known CAD, but they also point out that three 2021 meta-analyses confirmed large reductions in the risk of CV events, MI, and coronary revascularization with low-dose colchicine.
“In light of the positive results from LoDoCo2, COLCOT, and meta-analyses; its good tolerability profile; and cost-effectiveness, inflammation reduction with low-dose colchicine should be considered to treat patients with coronary disease in the absence of severe renal dysfunction,” Dr. Tardif and Dr. Marquis-Gravel concluded.
The study was supported by the National Health Medical Research Council of Australia; a grant from the Sir Charles Gairdner Research Advisory Committee; the Withering Foundation; the Netherlands Heart Foundation; the Netherlands Organization for Health Research and Development; and a consortium of Teva, Disphar, and Tiofarma in the Netherlands. The funders had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Opstal reports no relevant financial relationships. Coauthor disclosures are listed in the original article.
Dr. Tardif has received grant support from Amarin, AstraZeneca, Ceapro, DalCor Pharmaceuticals, Esperion, Ionis, Novartis, Pfizer, RegenXBio, and Sanofi; has received honoraria from AstraZeneca, DalCor Pharmaceuticals, HLS Therapeutics, Pendopharm, and Sanofi; has minor equity interest in DalCor Pharmaceuticals; and is mentioned as an author on submitted patents on pharmacogenomics-guided CETP inhibition, use of colchicine after myocardial infarction, and use of colchicine in COVID-19 (he has waived his rights in the colchicine patents and does not stand to gain financially). Dr. Marquis-Gravel has received research grants from Bayer, has received speaker honoraria from Novartis, and has served on national advisory boards for Servier, JAMP, and Bayer.
A version of this article first appeared on Medscape.com.
The benefits of low-dose colchicine (Colcrys) are consistent if started months or years after acute coronary syndrome (ACS) in patients with stable coronary artery disease, a new LoDoCo2 subanalysis suggests.
As previously reported, the parent trial showed that adding colchicine 0.5 mg daily to standard care reduced the risk of the primary endpoint – a composite of cardiovascular (CV) death, myocardial infarction (MI), ischemic stroke, or ischemia-driven coronary revascularization – by 31% compared with placebo.
In the new analysis, led by Tjerk S.J. Opstal, MD, the anti-inflammatory agent was equally effective in reducing the risk of the primary endpoint in patients with no prior ACS, a recent ACS (6-24 months), remote ACS (2-7 years), or very remote ACS (> 7 years), with no interaction found between groups (P = .59).
The incidence of the primary endpoint per 100 person-years and hazard ratios (HRs) for the four groups with colchicine and placebo are as follows:
- No prior ACS: 2.8 vs. 3.4; HR, 0.81 (95% confidence interval, 0.52-1.27).
- Recent ACS: 2.4 vs. 3.3; HR, 0.75 (95% CI, 0.51-1.10).
- Remote ACS: 1.8 vs. 3.2; HR, 0.55 (95% CI, 0.37-0.82)
- Very remote ACS: 3.0 vs. 4.3; HR, 0.70 (95% CI, 0.51-0.96).
The results were reported Aug. 23 in the Journal of the American College of Cardiology.
In contrast, however, a recent subgroup analysis from the COLCOT trial reported an even greater reduction in its primary composite CV endpoint when colchicine was started within 3 days of an MI.
“The result of COLCOT could imply that initiation of colchicine treatment would be best suited directly after myocardial infarction,” Dr. Opstal, from Radboud University Medical Center, Nijmegen, the Netherlands, said in an interview. “Our subanalysis shows that later initiation of colchicine therapy in patients visiting outpatient clinics years after their ACS events is equally effective. As such, colchicine therapy should not be limited to patients with recent ACS, and should be considered in all patients with coronary artery disease.”
Dr. Opstal pointed out that the two trials targeted different populations. COLCOT enrolled 4,765 patients within a month of MI, whereas LoDoCo2 enrolled 5,522 patients who were clinically stable for at least 6 months after an ACS or coronary revascularization.
Overall, 864 LoDoCo2 patients had no prior ACS and 86% had a history of ACS, of which 1,479 were recent, 1,582 were remote, and 1,597 were very remote.
Patients with a history of very remote ACS had a numerically higher event rate for the primary outcome, but the difference was not statistically significant and could be attributed to a play of chance, noted Dr. Opstal.
The team presumed patients with more recent prior ACS would remain at higher risk of ACS recurrence than would those with a more remote ACS that had proved to be clinically stable under standard medical therapy. But, he said, the data show they were at equal risk of the primary outcome.
“This implies that current optimal medical therapy does not result in an attenuation of residual risk over time regardless of whether patients are clinically stable, and that the ongoing process of atherosclerosis results in continuously elevated risk, which warrants new avenues of therapy, such as anti-inflammatory medication,” Dr. Opstal said.
In a binary analysis, there was no difference in composite cardiovascular events between patients with and without prior ACS (HR, 0.67 vs. HR, 0.81; P value for interaction, 0.43).
Dr. Opstal observed that a lack of statistical power precludes any definitive conclusions and that a large randomized controlled trial in patients with established coronary artery disease (CAD) but no prior ACS would elucidate whether early initiation of colchicine is “warranted at the moment CAD is established but before a first ACS event, as is common practice with acetylsalicylic acid and statins.”
In addition, the ongoing OASIS 9 trial will answer the question of whether patients with an estimated glomerular filtration rate of 30-60 mL/min can safely use low-dose colchicine. The gout medication is contraindicated in patients with severe renal or hepatic impairment and in patients on drugs that inhibit both CYP3A4 or the P-glycoprotein.
In an accompanying editorial, colchicine researchers Jean-Claude Tardif, MD, and Guillaume Marquis-Gravel, MD, of the Montreal Heart Institute, Quebec, Canada, suggest that study design features likely explain the discord between the LoDoCo2 and COLCOT subgroup analyses and the lack of difference in CV event rates between patients with and without prior ACS.
The editorialists say lingering questions remain, including the value of colchicine in patients with diabetes or peripheral artery disease without known CAD, but they also point out that three 2021 meta-analyses confirmed large reductions in the risk of CV events, MI, and coronary revascularization with low-dose colchicine.
“In light of the positive results from LoDoCo2, COLCOT, and meta-analyses; its good tolerability profile; and cost-effectiveness, inflammation reduction with low-dose colchicine should be considered to treat patients with coronary disease in the absence of severe renal dysfunction,” Dr. Tardif and Dr. Marquis-Gravel concluded.
The study was supported by the National Health Medical Research Council of Australia; a grant from the Sir Charles Gairdner Research Advisory Committee; the Withering Foundation; the Netherlands Heart Foundation; the Netherlands Organization for Health Research and Development; and a consortium of Teva, Disphar, and Tiofarma in the Netherlands. The funders had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Opstal reports no relevant financial relationships. Coauthor disclosures are listed in the original article.
Dr. Tardif has received grant support from Amarin, AstraZeneca, Ceapro, DalCor Pharmaceuticals, Esperion, Ionis, Novartis, Pfizer, RegenXBio, and Sanofi; has received honoraria from AstraZeneca, DalCor Pharmaceuticals, HLS Therapeutics, Pendopharm, and Sanofi; has minor equity interest in DalCor Pharmaceuticals; and is mentioned as an author on submitted patents on pharmacogenomics-guided CETP inhibition, use of colchicine after myocardial infarction, and use of colchicine in COVID-19 (he has waived his rights in the colchicine patents and does not stand to gain financially). Dr. Marquis-Gravel has received research grants from Bayer, has received speaker honoraria from Novartis, and has served on national advisory boards for Servier, JAMP, and Bayer.
A version of this article first appeared on Medscape.com.
Eyes on ESC ‘21: Hope for EMPEROR-Preserved, guidelines remade
There will be so much more to the annual congress of the European Society of Cardiology, which begins Aug. 27 with an all-virtual format, than detailed primary results of EMPEROR-Preserved, a trial that could mark a turning point for heart failure (HF) medical therapy.
Also among the featured Hot Line and Late-Breaking Science sessions are – along with many other studies – explorations of arrhythmia management (ablation or guided by loop recorder); secondary prevention, including by vaccination; oral anticoagulation, notably after transcatheter valve procedures; and colchicine or thrombosis prophylaxis in hospitalized patients with COVID-19.
There will even be a head-to-head comparison of two long-familiar left atrial appendage (LAA) occluders, and a population-based, randomized trial of sodium restriction through wide-scale use of a potassium-based salt substitute.
The congress will also introduce four guideline documents at sessions throughout the Congress, one on each day. They cover new and modified recommendations for heart failure; pacing, including cardiac resynchronization therapy (CRT); cardiovascular (CV) disease prevention; and, with cosponsorship from the European Association for Cardio-Thoracic Surgery, valvular heart disease.
The virtues of virtual
That next year’s Congress is slated for Aug. 27-30 in Barcelona should be welcome news for anyone whose “what if” curiosity about all-virtual conferences has already been satisfied. But with experience comes wisdom, as the medical societies have learned that online scientific meetings have some winning qualities that may be worth keeping, as least for a while.
“I think there is no doubt that the digital format will continue, for several reasons. One is that this pandemic is not over,” ESC Congress program committee chair Stephan Windecker, MD, Bern (Switzerland) University Hospital, , told this news organization. “As long as it is not over, the digital format is here to stay.”
But it also appears that people who haven’t been able to attend the congress in person are keen to log in and engage online, Dr. Windecker said. The 2020 all-virtual conference drew a much younger pool of registrants, on average, than did the live conferences before the pandemic.
“I think that’s an indication of people that may be in training, in early stages of their career, or they don’t have the support from departments or from their practice, or other financial means.” But they are able to participate via computer, tablet, or smartphone, he said.
“Another advantage is that the recorded content can be replayed at the convenience of whoever wants to consume it at a later point in time,” he added. “Those are just some examples why the digital format is likely to stay,” on its own or in a new age of hybrid meetings.
New and updated guidelines
Leading off the guideline series is the document on diagnosis and treatment of acute and chronic HF, which leveraged the past few busy years of HF clinical trials to arrive at a number of new recommendations and strengthened level-of-evidence ratings. It covers both drug and device therapy of HF with reduced ejection fraction (HFrEF) and acute decompensated HF, and tweaks and further enshrines the concept of HF with mildly reduced ejection fraction (HFmrEF).
Several updated recommendations for both long-used and novel medications, notably the sodium-glucose cotransporter 2 inhibitors, will be included because of the recently appreciated evidence-based impact in HFrEF, Dr. Windecker noted.
“I think it will be particularly interesting to look for the SGLT2 inhibitors as not a completely new class of drugs, but certainly one where there has been a lot of new evidence, to look at how those drugs will be integrated in the overall care pathway.”
A top-line preview of the new HF guideline limited to drug therapy, presented at July’s Heart Failure Association of the European Society of Cardiology (ESC-HFA), provided a simple answer to a common question in the new, bountiful age of HFrEF medications: Which meds, initiated in what order?
As it happens, the new recommendation for first-line HFrEF drug therapy is not a silver bullet, but a shotgun – prompt initiation of at least four meds, one from each of four drug classes: renin-angiotensin system inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and SGLT2 inhibitors. Each class, as described in the document, is to be started as soon as safely feasible, in a sequence deemed appropriate for each individual patient.
Spotlight on EMPEROR-Preserved
The world already knows that the trial, which tested the SGLT2 inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) on top of standard therapy, “met” its primary endpoint in almost 6,000 patients with HF with preserved ejection fraction (HFpEF), who included some with HFmrEF by more contemporary definitions.
That means patients in EMPEROR-Preserved assigned to take empagliflozin showed significantly fewer events that made up the study’s primary endpoint, a composite of CV death or HF hospitalization. It appears to be the first clearly significant overall medical therapy benefit for a clinical primary endpoint in a major randomized HFpEF drug trial.
And that, pending fuller presentation of trial results at the Congress on Aug. 27, could be a huge deal for the half of HF patients with left ventricular ejection fractions (LVEF) higher than the HFrEF range.
Those early top-line results weren’t a decisive bombshell for a field now filled with hope for a practice-changing empagliflozin outcome in EMPEROR-Preserved, which isn’t a certainty. They were more like the “boom” of a mortar launching a rocket of fireworks that may explode into a chrysanthemum or green comet or, sometimes, turn out to be no more than a dud. The promise of the early cursory results critically depends on further details.
“Provided there is a compelling benefit, this is what everyone has been waiting for in this condition for decades,” Mikhail N. Kosiborod, MD, director of cardiometabolic research at Saint Luke’s Mid-America Heart Institute, Kansas City, Mo., said.
“Already knowing that the trial met the primary endpoint is obviously very intriguing and encouraging,” he added. “But there are things we don’t know, such as: What is the magnitude of benefit? And whether that benefit, whatever the magnitude, is driven by reductions in both heart failure hospitalizations and cardiovascular death, or only one of the two.”
For example: “If we see an impressive benefit for reduction of hospitalizations, but not a significant reduction in death, that would still be a huge advance. That’s because, to date, we don’t have any drug for HFpEF that has convincingly demonstrated a compelling reduction in heart failure hospitalization or improvement in symptoms, function, or quality of life,” observed Dr. Kosiborod, who wasn’t part of EMPEROR-Preserved.
There have been “suggestions” from HFrEF trials that empagliflozin and dapagliflozin (Farxiga, AstraZeneca) “have very comparable effects on at least the endpoint of cardiovascular death or hospitalization for heart failure,” he said. “So, my expectation would be that whatever is observed in EMPEROR-Preserved is likely a class effect, as well.”
Following EMPEROR-Preserved on the agenda is EMPEROR-Pooled, a patient-level combined analysis of the EMPEROR series of trials that spans the range of HF, regardless of ejection fraction or diabetes status, primarily exploring the effects of empagliflozin on renal function.
Other offerings, Friday, Aug. 27
Scheduled immediately after EMPEROR-Preserved is a presentation on the SMART-MI trial, which should clarify whether management guided by continuous ambulatory monitoring is effective in patients considered at especially high arrhythmic risk. Entry called for recent myocardial infarction and an LVEF of 36%-50% with evidence of cardiac autonomic dysfunction.
The trial randomly assigned 400 such patients to be or not be implanted with a Reveal LINQ (Medtronic) loop recorder and followed them for up to 18 months, primarily for detection of potentially serious arrhythmic events. Endpoints that involved mortality, hospitalization or other clinical events were secondary.
In a time slot preceding both SMART-MI and EMPEROR-Preserved, the GUIDE-HF trial is following a projected 3,600 patients with HF implanted with a CardioMEMS HF System (Abbott) pulmonary artery (PA) pressure sensor to explore the its value for guiding management.
The trial’s three cohorts, followed for at least 12 months, include randomized sensor-monitored and control groups of patients with New York Heart Association class 2-4 symptoms, as well as a third observational set of patients in NYHA class 3. That’s the indication for which the CardioMEMS monitor gained approval in the United States in 2014 based on the 2011 CHAMPION trial, and which fared just as well in the 2017 CHAMPION Post-Approval Study.
The Friday Hot Lines also include Dal-GenE, which has entered about 6,000 patients with recent MI to test the once-abandoned cholesterol ester transfer protein (CETP) inhibitor dalcetrapib (DalCor) for any secondary-prevention benefits when used selectively. The trial’s hook: All its patients are confirmed to have the AA genotype of the rs1967309 variant in the ADCY9 gene, which has been associated with a pronounced clinical response to CETP inhibition.
Saturday, Aug. 28
The direct oral anticoagulants (DOACs) have largely replaced vitamin K antagonists in patients with nonvalvular atrial fibrillation (AFib). But whether DOACs are similarly preferable in the growing world population of people who have undergone transcatheter aortic valve replacement (TAVR or TAVI), an issue explored with variable results in the ATLANTIS and GALILEO trials, is far from settled.
The ENVISAGE-TAVI AF trial explored the question for the factor X inhibitor edoxaban (Savaysa, Lixiana, Daiichi-Sankyo) in 1,400 patients with AFib and a transfemoral TAVR in the previous 5 days, who were randomly assigned to the DOAC or standard management along with discretionary antiplatelet therapy. They’ve been followed for up to 3 years for a composite endpoint of clinical events – including death, MI, and stroke – and for major bleeding.
The day will also feature MASTER DAPT, a comparison of two dual-antiplatelet therapy (DAPT) regimens in an estimated 4,300 patients considered to be high-risk for bleeding who had received the sirolimus-eluting Ultimaster (Terumo) coronary stent, which has a bioresorbable polymer coating.
Investigators have randomly assigned patients to receive either very-short-duration DAPT, for about a month after stenting, followed by a P2Y12 inhibitor alone for up to a year after the procedure; or a more conventional regimen of a P2Y12 inhibitor for 6-12 months with aspirin maintained for a total of 12 months.
Later that day, investigators from the FIGARO-DKD trial will present their results based on 7,437 patients with type 2 diabetes and chronic kidney disease (CKD), a much fuller version than the top-line findings announced by sponsor Bayer 3 months ago.
Those top-line results suggested that patients assigned to receive the nonsteroidal nonselective mineralocorticoid receptor antagonist (MRA) finerenone (Kerendia) on top of standard care benefited with a drop in risk for the primary endpoint of CV death or nonfatal CV events.
Finerenone was recently approved in the United States for treating patients with both type 2 diabetes and CKD based on the published FIDELIO-DKD trial, which had seen less CKD progression and fewer CV events in such patients who took the novel MRA.
Although similar in design to FIGARO-DKD, FIDELIO-DKD had entered fewer patients with early-stage diabetic kidney disease (DKD). That led researchers to pool the two trials’ populations to create a cohort that spans the spectrum of DKD severity. An analysis of the pooled cohort, dubbed FIDELITY, is on the schedule after FIGARO-DKD.
After FIDELITY is the prospective APAF-CRT trial that is following a projected 1,830 patients with permanent, symptomatic AFib and a recent hospitalization for AFib or HF and who were not good candidates for standard ablation. They were assigned to receive either atrioventricular junctional ablation followed by CRT, with or without a defibrillation, on top of optimal meds – a so-called “ablate-and-pace” strategy – or an implantable cardioverter defibrillator with rate-control drug therapy.
The new analysis represents the trial’s second phase in which mortality was followed for 4 years as the primary endpoint, in contrast to the previously reported initial phase that followed the first 102 patients for 2 years for the composite primary endpoint of death, worsening HF, and HF hospitalization. The first phase had halted enrollment before reaching its planned target of 280 patients after an interim analysis showed a significant benefit for ablate and pace.
Next up: DECAAF 2, a randomized assessment of whether catheter ablation for AFib guided by delayed gadolinium enhancement on MRI, a proxy for scar tissue, can be more effective than standard AFib ablation by pulmonary vein isolation alone. An estimated 900 patients with persistent AFib who had never before undergone ablation for the arrhythmia were randomly assigned to one strategy or the other and followed for AFib recurrence over 18 months.
Sunday, Aug. 29
The TOMAHAWK trial aimed to clarify the optimal timing of invasive coronary angiography for resuscitated patients with non–ST-segment elevation out-of-hospital cardiac arrest, a broad population in a setting for which there is little randomized-trial guidance. Investigators randomly assigned 558 such patients to undergo immediate invasive angiography or to direct intensive care unit admission for initial standard care with discretionary delayed angiography. Patients were followed for all-cause mortality, with other clinical events and neurologic outcomes as secondary endpoints.
Next on the schedule, the RIPCORD-2 trial randomly assigned 1,100 patients with stable known or suspected coronary artery disease (CAD) to undergo conventional angiography alone or with added direct pressure-wire measurement of fractional flow reserve to guide management decisions. Primary outcomes include health care costs and patient-reported quality of life at 1 year.
Slated for later that day, the Asymptomatic Carotid Surgery Trial-2 (ACST-2) has entered an estimated 3600 patients with a substantial carotid artery narrowing not associated with symptoms but for which either carotid endarterectomy (CEA) or carotid artery stenting (CAS) was considered anatomically feasible. There also must have been “substantial uncertainty” regarding the optimal procedure choice.
The trial, conducted in 40 countries primarily in Europe and North America and launched in 2008, randomly assigned the patients to undergo either CEA or CAS, in both cases with appropriate medical therapy, and followed them for periprocedural events and up to 10 years for strokes and stroke-related events.
The LOOP study, which is to directly follow ACST-2, has explored whether screening for AFib using the Medtronic Reveal LINQ monitor in older patients with non-AFib stroke risk factors – with oral anticoagulation prescribed for those who test positive – can lower their risk for stroke or systemic embolism. It randomly assigned 6,000 such patients to care guided by the loop recorder or to standard care.
On a somewhat larger scale, the Salt Substitute and Stroke Study (SSaSS) randomly assigned a total of 20,996 people in about 600 villages across northern China and Tibet to sodium-restriction intervention and control groups by village. All participants had a history of stroke or were aged at least 60 years with uncontrolled hypertension.
As described by the trial’s online portal, participants in villages assigned to the intervention group were given a supply of a low-sodium, potassium-supplementing salt substitute to replace their own salt supplies, along with education on the health benefits of sodium restriction. Participants in control villages continued their normal diets and, at the trial’s beginning, received “advice to reduce their salt intake.” All were required to own a telephone.
Clinical events, including strokes and hospitalizations throughout a 5-year follow-up, were tracked by phone calls made to all participants every 6 months and were documented at follow-up home visits.
Sunday is also to feature a Late-Breaking Trials session with a focus on COVID-19, which leads off with COLCOVID, a test of colchicine in patients hospitalized for suspected SARS-CoV-2 infection and in acute respiratory distress.
The 1,279 participants in Argentina were randomly assigned to receive or not receive the potent anti-inflammatory agent on top of antivirals and other standard management and followed for death or new need for mechanical ventilation. A successful outcome would contrast with the RECOVERY trial, which terminated a colchicine group of patients hospitalized with COVID-19 because of a lack of efficacy earlier this year.
COLCOVID is to be followed by the MICHELLE trial of rivaroxaban (Xarelto, Bayer/Janssen) prophylaxis, compared with no preventive oral anticoagulant, in 320 patients who, when hospitalized with COVID-19, had been on parenteral anticoagulants because of an elevated risk for venous thromboembolism. The trial, conducted in Brazil, called for postdischarge rivaroxaban at a once-daily dosage of 10 mg for about 1 month.
The session also includes a presentation called “Insights into the Effects of the COVID-19 Pandemic: Comprehensive Analysis from the GUIDE-HF Trial,” the primary outcomes of which will be reported on the first day of the Congress.
Following is a presentation on the PREPARE-IT study of icosapent ethyl (Vascepa, Amarin), given at high dosages intended to be anti-inflammatory, compared with placebo, in an estimated 4,000 adults. The trial has two groups: A prevention group of adults living and circulating in the community; and a treatment group of patients aged at least 40 years with confirmed symptomatic SARS-CoV-2 infection for whom the need for hospitalization isn’t clear.
Monday, Aug. 30
The final day of the Congress features a trial called Influenza Vaccination after Myocardial Infarction (IAMI), which has tested the secondary preventive effect of influenza vaccination by randomly assigning 2,571 patients to receive a standard vaccine or a saline placebo injection on one occasion.
Entry to the international trial called for a diagnosis of MI with or without ST-segment elevation, or stable CAD and age at least 75 years with other risk factors. The patients were followed for death, MI, stent thrombosis, and a slew of secondary endpoints over 12 months.
Monday offerings continue later in a time block leading off with the STEP trial, which has randomly assigned an estimated 8,000 patients at 40 centers in China who are 60 to 80 years of age with a systolic blood pressure of 140 to <190 mm Hg to be on standard guideline-based therapy or an intensive drug-management strategy.
The systolic BP goals are 130 to <150 mm Hg for standard care and 110 to <130 mm Hg for the intensive regimen. The composite primary endpoint includes death and clinical events related to acute coronary syndromes, HF, revascularization, and stroke.
Following on heels of STEP, the Amulet IDE trial – the first major randomized comparison of two transcatheter LAA closure devices – entered 1,878 patients with nonvalvular AFib who were considered high-risk for bleeding and stroke or systemic embolism.
They were randomly assigned in the noninferiority trial to receive either the AMPLATZER Amulet (Abbott Medical Devices) or the WATCHMAN (Boston Scientific) closure devices and were followed for safety and efficacy for up to 5 years.
Both LAA closure devices, intended to make patients with AFib less reliant on oral anticoagulation, are now available on both sides of the Atlantic – as well as many other countries – after the Amulet’s United States market approval on Aug. 16, based largely on the Amulet IDE trial.
Rounding out the final Hot Line set is one of the latest efforts to show the efficacy and safety of a very short DAPT period after coronary stenting in patients with acute coronary syndromes, the STOPDAPT-2 ACS trial.
The study assigned 3,008 patients in Japan to receive aspirin and clopidogrel for either 1 month or 1 year after implantation with an everolimus-eluting cobalt-chromium stent and followed them for up to 5 years for a composite of MI, CV death, stent thrombosis, stroke, and bleeding.
The trial follows the published STOPDAPT-2 trial that showed superiority for the 1-month DAPT regimen in a predominantly stable-CAD population treated with the same kind of stent.
Program structure and format
A total of 15 online channels are to be available in the morning, European time, their schedules running in parallel. Presentations often are prerecorded, but also include live sessions at 8:00 a.m. Central time and 12 p.m. CET (2:00 a.m. and 6:00 a.m. Eastern time) to liven up the channel offerings, Dr. Windecker observed, and to make them more immediate and potentially interactive.
Many of the parallel channels are devoted throughout the Congress to particular silos of cardiology; for example, arrhythmias and device therapy is on channel 3; CAD and acute care is on 5; HF is on 6; and preventive cardiology is on 9.
Other channels swing across different topics from day to day, such as channel 1, which covers COVID-19 topics on the first and third day of the meeting, “advances in science” on day 2, and “digital health, public health, health economics” on day 4.
The focus each day, starting at 2:00 p.m. CET (8:00 a.m. ET) and continuing into the evening in Europe, shifts over to the Prime Time live program, which features the Hot Line and guideline presentations and many of the live abstract presentations.
Dr. Kosiborod, not a researcher with the EMPEROR trials, is chair of the Dapagliflozin in Preserved Ejection Fraction Heart Failure ( PRESERVED-HF ) trial, which is scheduled for presentation at the September 2021 Heart Failure Society of American meeting.
A version of this article first appeared on Medscape.com.
There will be so much more to the annual congress of the European Society of Cardiology, which begins Aug. 27 with an all-virtual format, than detailed primary results of EMPEROR-Preserved, a trial that could mark a turning point for heart failure (HF) medical therapy.
Also among the featured Hot Line and Late-Breaking Science sessions are – along with many other studies – explorations of arrhythmia management (ablation or guided by loop recorder); secondary prevention, including by vaccination; oral anticoagulation, notably after transcatheter valve procedures; and colchicine or thrombosis prophylaxis in hospitalized patients with COVID-19.
There will even be a head-to-head comparison of two long-familiar left atrial appendage (LAA) occluders, and a population-based, randomized trial of sodium restriction through wide-scale use of a potassium-based salt substitute.
The congress will also introduce four guideline documents at sessions throughout the Congress, one on each day. They cover new and modified recommendations for heart failure; pacing, including cardiac resynchronization therapy (CRT); cardiovascular (CV) disease prevention; and, with cosponsorship from the European Association for Cardio-Thoracic Surgery, valvular heart disease.
The virtues of virtual
That next year’s Congress is slated for Aug. 27-30 in Barcelona should be welcome news for anyone whose “what if” curiosity about all-virtual conferences has already been satisfied. But with experience comes wisdom, as the medical societies have learned that online scientific meetings have some winning qualities that may be worth keeping, as least for a while.
“I think there is no doubt that the digital format will continue, for several reasons. One is that this pandemic is not over,” ESC Congress program committee chair Stephan Windecker, MD, Bern (Switzerland) University Hospital, , told this news organization. “As long as it is not over, the digital format is here to stay.”
But it also appears that people who haven’t been able to attend the congress in person are keen to log in and engage online, Dr. Windecker said. The 2020 all-virtual conference drew a much younger pool of registrants, on average, than did the live conferences before the pandemic.
“I think that’s an indication of people that may be in training, in early stages of their career, or they don’t have the support from departments or from their practice, or other financial means.” But they are able to participate via computer, tablet, or smartphone, he said.
“Another advantage is that the recorded content can be replayed at the convenience of whoever wants to consume it at a later point in time,” he added. “Those are just some examples why the digital format is likely to stay,” on its own or in a new age of hybrid meetings.
New and updated guidelines
Leading off the guideline series is the document on diagnosis and treatment of acute and chronic HF, which leveraged the past few busy years of HF clinical trials to arrive at a number of new recommendations and strengthened level-of-evidence ratings. It covers both drug and device therapy of HF with reduced ejection fraction (HFrEF) and acute decompensated HF, and tweaks and further enshrines the concept of HF with mildly reduced ejection fraction (HFmrEF).
Several updated recommendations for both long-used and novel medications, notably the sodium-glucose cotransporter 2 inhibitors, will be included because of the recently appreciated evidence-based impact in HFrEF, Dr. Windecker noted.
“I think it will be particularly interesting to look for the SGLT2 inhibitors as not a completely new class of drugs, but certainly one where there has been a lot of new evidence, to look at how those drugs will be integrated in the overall care pathway.”
A top-line preview of the new HF guideline limited to drug therapy, presented at July’s Heart Failure Association of the European Society of Cardiology (ESC-HFA), provided a simple answer to a common question in the new, bountiful age of HFrEF medications: Which meds, initiated in what order?
As it happens, the new recommendation for first-line HFrEF drug therapy is not a silver bullet, but a shotgun – prompt initiation of at least four meds, one from each of four drug classes: renin-angiotensin system inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and SGLT2 inhibitors. Each class, as described in the document, is to be started as soon as safely feasible, in a sequence deemed appropriate for each individual patient.
Spotlight on EMPEROR-Preserved
The world already knows that the trial, which tested the SGLT2 inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) on top of standard therapy, “met” its primary endpoint in almost 6,000 patients with HF with preserved ejection fraction (HFpEF), who included some with HFmrEF by more contemporary definitions.
That means patients in EMPEROR-Preserved assigned to take empagliflozin showed significantly fewer events that made up the study’s primary endpoint, a composite of CV death or HF hospitalization. It appears to be the first clearly significant overall medical therapy benefit for a clinical primary endpoint in a major randomized HFpEF drug trial.
And that, pending fuller presentation of trial results at the Congress on Aug. 27, could be a huge deal for the half of HF patients with left ventricular ejection fractions (LVEF) higher than the HFrEF range.
Those early top-line results weren’t a decisive bombshell for a field now filled with hope for a practice-changing empagliflozin outcome in EMPEROR-Preserved, which isn’t a certainty. They were more like the “boom” of a mortar launching a rocket of fireworks that may explode into a chrysanthemum or green comet or, sometimes, turn out to be no more than a dud. The promise of the early cursory results critically depends on further details.
“Provided there is a compelling benefit, this is what everyone has been waiting for in this condition for decades,” Mikhail N. Kosiborod, MD, director of cardiometabolic research at Saint Luke’s Mid-America Heart Institute, Kansas City, Mo., said.
“Already knowing that the trial met the primary endpoint is obviously very intriguing and encouraging,” he added. “But there are things we don’t know, such as: What is the magnitude of benefit? And whether that benefit, whatever the magnitude, is driven by reductions in both heart failure hospitalizations and cardiovascular death, or only one of the two.”
For example: “If we see an impressive benefit for reduction of hospitalizations, but not a significant reduction in death, that would still be a huge advance. That’s because, to date, we don’t have any drug for HFpEF that has convincingly demonstrated a compelling reduction in heart failure hospitalization or improvement in symptoms, function, or quality of life,” observed Dr. Kosiborod, who wasn’t part of EMPEROR-Preserved.
There have been “suggestions” from HFrEF trials that empagliflozin and dapagliflozin (Farxiga, AstraZeneca) “have very comparable effects on at least the endpoint of cardiovascular death or hospitalization for heart failure,” he said. “So, my expectation would be that whatever is observed in EMPEROR-Preserved is likely a class effect, as well.”
Following EMPEROR-Preserved on the agenda is EMPEROR-Pooled, a patient-level combined analysis of the EMPEROR series of trials that spans the range of HF, regardless of ejection fraction or diabetes status, primarily exploring the effects of empagliflozin on renal function.
Other offerings, Friday, Aug. 27
Scheduled immediately after EMPEROR-Preserved is a presentation on the SMART-MI trial, which should clarify whether management guided by continuous ambulatory monitoring is effective in patients considered at especially high arrhythmic risk. Entry called for recent myocardial infarction and an LVEF of 36%-50% with evidence of cardiac autonomic dysfunction.
The trial randomly assigned 400 such patients to be or not be implanted with a Reveal LINQ (Medtronic) loop recorder and followed them for up to 18 months, primarily for detection of potentially serious arrhythmic events. Endpoints that involved mortality, hospitalization or other clinical events were secondary.
In a time slot preceding both SMART-MI and EMPEROR-Preserved, the GUIDE-HF trial is following a projected 3,600 patients with HF implanted with a CardioMEMS HF System (Abbott) pulmonary artery (PA) pressure sensor to explore the its value for guiding management.
The trial’s three cohorts, followed for at least 12 months, include randomized sensor-monitored and control groups of patients with New York Heart Association class 2-4 symptoms, as well as a third observational set of patients in NYHA class 3. That’s the indication for which the CardioMEMS monitor gained approval in the United States in 2014 based on the 2011 CHAMPION trial, and which fared just as well in the 2017 CHAMPION Post-Approval Study.
The Friday Hot Lines also include Dal-GenE, which has entered about 6,000 patients with recent MI to test the once-abandoned cholesterol ester transfer protein (CETP) inhibitor dalcetrapib (DalCor) for any secondary-prevention benefits when used selectively. The trial’s hook: All its patients are confirmed to have the AA genotype of the rs1967309 variant in the ADCY9 gene, which has been associated with a pronounced clinical response to CETP inhibition.
Saturday, Aug. 28
The direct oral anticoagulants (DOACs) have largely replaced vitamin K antagonists in patients with nonvalvular atrial fibrillation (AFib). But whether DOACs are similarly preferable in the growing world population of people who have undergone transcatheter aortic valve replacement (TAVR or TAVI), an issue explored with variable results in the ATLANTIS and GALILEO trials, is far from settled.
The ENVISAGE-TAVI AF trial explored the question for the factor X inhibitor edoxaban (Savaysa, Lixiana, Daiichi-Sankyo) in 1,400 patients with AFib and a transfemoral TAVR in the previous 5 days, who were randomly assigned to the DOAC or standard management along with discretionary antiplatelet therapy. They’ve been followed for up to 3 years for a composite endpoint of clinical events – including death, MI, and stroke – and for major bleeding.
The day will also feature MASTER DAPT, a comparison of two dual-antiplatelet therapy (DAPT) regimens in an estimated 4,300 patients considered to be high-risk for bleeding who had received the sirolimus-eluting Ultimaster (Terumo) coronary stent, which has a bioresorbable polymer coating.
Investigators have randomly assigned patients to receive either very-short-duration DAPT, for about a month after stenting, followed by a P2Y12 inhibitor alone for up to a year after the procedure; or a more conventional regimen of a P2Y12 inhibitor for 6-12 months with aspirin maintained for a total of 12 months.
Later that day, investigators from the FIGARO-DKD trial will present their results based on 7,437 patients with type 2 diabetes and chronic kidney disease (CKD), a much fuller version than the top-line findings announced by sponsor Bayer 3 months ago.
Those top-line results suggested that patients assigned to receive the nonsteroidal nonselective mineralocorticoid receptor antagonist (MRA) finerenone (Kerendia) on top of standard care benefited with a drop in risk for the primary endpoint of CV death or nonfatal CV events.
Finerenone was recently approved in the United States for treating patients with both type 2 diabetes and CKD based on the published FIDELIO-DKD trial, which had seen less CKD progression and fewer CV events in such patients who took the novel MRA.
Although similar in design to FIGARO-DKD, FIDELIO-DKD had entered fewer patients with early-stage diabetic kidney disease (DKD). That led researchers to pool the two trials’ populations to create a cohort that spans the spectrum of DKD severity. An analysis of the pooled cohort, dubbed FIDELITY, is on the schedule after FIGARO-DKD.
After FIDELITY is the prospective APAF-CRT trial that is following a projected 1,830 patients with permanent, symptomatic AFib and a recent hospitalization for AFib or HF and who were not good candidates for standard ablation. They were assigned to receive either atrioventricular junctional ablation followed by CRT, with or without a defibrillation, on top of optimal meds – a so-called “ablate-and-pace” strategy – or an implantable cardioverter defibrillator with rate-control drug therapy.
The new analysis represents the trial’s second phase in which mortality was followed for 4 years as the primary endpoint, in contrast to the previously reported initial phase that followed the first 102 patients for 2 years for the composite primary endpoint of death, worsening HF, and HF hospitalization. The first phase had halted enrollment before reaching its planned target of 280 patients after an interim analysis showed a significant benefit for ablate and pace.
Next up: DECAAF 2, a randomized assessment of whether catheter ablation for AFib guided by delayed gadolinium enhancement on MRI, a proxy for scar tissue, can be more effective than standard AFib ablation by pulmonary vein isolation alone. An estimated 900 patients with persistent AFib who had never before undergone ablation for the arrhythmia were randomly assigned to one strategy or the other and followed for AFib recurrence over 18 months.
Sunday, Aug. 29
The TOMAHAWK trial aimed to clarify the optimal timing of invasive coronary angiography for resuscitated patients with non–ST-segment elevation out-of-hospital cardiac arrest, a broad population in a setting for which there is little randomized-trial guidance. Investigators randomly assigned 558 such patients to undergo immediate invasive angiography or to direct intensive care unit admission for initial standard care with discretionary delayed angiography. Patients were followed for all-cause mortality, with other clinical events and neurologic outcomes as secondary endpoints.
Next on the schedule, the RIPCORD-2 trial randomly assigned 1,100 patients with stable known or suspected coronary artery disease (CAD) to undergo conventional angiography alone or with added direct pressure-wire measurement of fractional flow reserve to guide management decisions. Primary outcomes include health care costs and patient-reported quality of life at 1 year.
Slated for later that day, the Asymptomatic Carotid Surgery Trial-2 (ACST-2) has entered an estimated 3600 patients with a substantial carotid artery narrowing not associated with symptoms but for which either carotid endarterectomy (CEA) or carotid artery stenting (CAS) was considered anatomically feasible. There also must have been “substantial uncertainty” regarding the optimal procedure choice.
The trial, conducted in 40 countries primarily in Europe and North America and launched in 2008, randomly assigned the patients to undergo either CEA or CAS, in both cases with appropriate medical therapy, and followed them for periprocedural events and up to 10 years for strokes and stroke-related events.
The LOOP study, which is to directly follow ACST-2, has explored whether screening for AFib using the Medtronic Reveal LINQ monitor in older patients with non-AFib stroke risk factors – with oral anticoagulation prescribed for those who test positive – can lower their risk for stroke or systemic embolism. It randomly assigned 6,000 such patients to care guided by the loop recorder or to standard care.
On a somewhat larger scale, the Salt Substitute and Stroke Study (SSaSS) randomly assigned a total of 20,996 people in about 600 villages across northern China and Tibet to sodium-restriction intervention and control groups by village. All participants had a history of stroke or were aged at least 60 years with uncontrolled hypertension.
As described by the trial’s online portal, participants in villages assigned to the intervention group were given a supply of a low-sodium, potassium-supplementing salt substitute to replace their own salt supplies, along with education on the health benefits of sodium restriction. Participants in control villages continued their normal diets and, at the trial’s beginning, received “advice to reduce their salt intake.” All were required to own a telephone.
Clinical events, including strokes and hospitalizations throughout a 5-year follow-up, were tracked by phone calls made to all participants every 6 months and were documented at follow-up home visits.
Sunday is also to feature a Late-Breaking Trials session with a focus on COVID-19, which leads off with COLCOVID, a test of colchicine in patients hospitalized for suspected SARS-CoV-2 infection and in acute respiratory distress.
The 1,279 participants in Argentina were randomly assigned to receive or not receive the potent anti-inflammatory agent on top of antivirals and other standard management and followed for death or new need for mechanical ventilation. A successful outcome would contrast with the RECOVERY trial, which terminated a colchicine group of patients hospitalized with COVID-19 because of a lack of efficacy earlier this year.
COLCOVID is to be followed by the MICHELLE trial of rivaroxaban (Xarelto, Bayer/Janssen) prophylaxis, compared with no preventive oral anticoagulant, in 320 patients who, when hospitalized with COVID-19, had been on parenteral anticoagulants because of an elevated risk for venous thromboembolism. The trial, conducted in Brazil, called for postdischarge rivaroxaban at a once-daily dosage of 10 mg for about 1 month.
The session also includes a presentation called “Insights into the Effects of the COVID-19 Pandemic: Comprehensive Analysis from the GUIDE-HF Trial,” the primary outcomes of which will be reported on the first day of the Congress.
Following is a presentation on the PREPARE-IT study of icosapent ethyl (Vascepa, Amarin), given at high dosages intended to be anti-inflammatory, compared with placebo, in an estimated 4,000 adults. The trial has two groups: A prevention group of adults living and circulating in the community; and a treatment group of patients aged at least 40 years with confirmed symptomatic SARS-CoV-2 infection for whom the need for hospitalization isn’t clear.
Monday, Aug. 30
The final day of the Congress features a trial called Influenza Vaccination after Myocardial Infarction (IAMI), which has tested the secondary preventive effect of influenza vaccination by randomly assigning 2,571 patients to receive a standard vaccine or a saline placebo injection on one occasion.
Entry to the international trial called for a diagnosis of MI with or without ST-segment elevation, or stable CAD and age at least 75 years with other risk factors. The patients were followed for death, MI, stent thrombosis, and a slew of secondary endpoints over 12 months.
Monday offerings continue later in a time block leading off with the STEP trial, which has randomly assigned an estimated 8,000 patients at 40 centers in China who are 60 to 80 years of age with a systolic blood pressure of 140 to <190 mm Hg to be on standard guideline-based therapy or an intensive drug-management strategy.
The systolic BP goals are 130 to <150 mm Hg for standard care and 110 to <130 mm Hg for the intensive regimen. The composite primary endpoint includes death and clinical events related to acute coronary syndromes, HF, revascularization, and stroke.
Following on heels of STEP, the Amulet IDE trial – the first major randomized comparison of two transcatheter LAA closure devices – entered 1,878 patients with nonvalvular AFib who were considered high-risk for bleeding and stroke or systemic embolism.
They were randomly assigned in the noninferiority trial to receive either the AMPLATZER Amulet (Abbott Medical Devices) or the WATCHMAN (Boston Scientific) closure devices and were followed for safety and efficacy for up to 5 years.
Both LAA closure devices, intended to make patients with AFib less reliant on oral anticoagulation, are now available on both sides of the Atlantic – as well as many other countries – after the Amulet’s United States market approval on Aug. 16, based largely on the Amulet IDE trial.
Rounding out the final Hot Line set is one of the latest efforts to show the efficacy and safety of a very short DAPT period after coronary stenting in patients with acute coronary syndromes, the STOPDAPT-2 ACS trial.
The study assigned 3,008 patients in Japan to receive aspirin and clopidogrel for either 1 month or 1 year after implantation with an everolimus-eluting cobalt-chromium stent and followed them for up to 5 years for a composite of MI, CV death, stent thrombosis, stroke, and bleeding.
The trial follows the published STOPDAPT-2 trial that showed superiority for the 1-month DAPT regimen in a predominantly stable-CAD population treated with the same kind of stent.
Program structure and format
A total of 15 online channels are to be available in the morning, European time, their schedules running in parallel. Presentations often are prerecorded, but also include live sessions at 8:00 a.m. Central time and 12 p.m. CET (2:00 a.m. and 6:00 a.m. Eastern time) to liven up the channel offerings, Dr. Windecker observed, and to make them more immediate and potentially interactive.
Many of the parallel channels are devoted throughout the Congress to particular silos of cardiology; for example, arrhythmias and device therapy is on channel 3; CAD and acute care is on 5; HF is on 6; and preventive cardiology is on 9.
Other channels swing across different topics from day to day, such as channel 1, which covers COVID-19 topics on the first and third day of the meeting, “advances in science” on day 2, and “digital health, public health, health economics” on day 4.
The focus each day, starting at 2:00 p.m. CET (8:00 a.m. ET) and continuing into the evening in Europe, shifts over to the Prime Time live program, which features the Hot Line and guideline presentations and many of the live abstract presentations.
Dr. Kosiborod, not a researcher with the EMPEROR trials, is chair of the Dapagliflozin in Preserved Ejection Fraction Heart Failure ( PRESERVED-HF ) trial, which is scheduled for presentation at the September 2021 Heart Failure Society of American meeting.
A version of this article first appeared on Medscape.com.
There will be so much more to the annual congress of the European Society of Cardiology, which begins Aug. 27 with an all-virtual format, than detailed primary results of EMPEROR-Preserved, a trial that could mark a turning point for heart failure (HF) medical therapy.
Also among the featured Hot Line and Late-Breaking Science sessions are – along with many other studies – explorations of arrhythmia management (ablation or guided by loop recorder); secondary prevention, including by vaccination; oral anticoagulation, notably after transcatheter valve procedures; and colchicine or thrombosis prophylaxis in hospitalized patients with COVID-19.
There will even be a head-to-head comparison of two long-familiar left atrial appendage (LAA) occluders, and a population-based, randomized trial of sodium restriction through wide-scale use of a potassium-based salt substitute.
The congress will also introduce four guideline documents at sessions throughout the Congress, one on each day. They cover new and modified recommendations for heart failure; pacing, including cardiac resynchronization therapy (CRT); cardiovascular (CV) disease prevention; and, with cosponsorship from the European Association for Cardio-Thoracic Surgery, valvular heart disease.
The virtues of virtual
That next year’s Congress is slated for Aug. 27-30 in Barcelona should be welcome news for anyone whose “what if” curiosity about all-virtual conferences has already been satisfied. But with experience comes wisdom, as the medical societies have learned that online scientific meetings have some winning qualities that may be worth keeping, as least for a while.
“I think there is no doubt that the digital format will continue, for several reasons. One is that this pandemic is not over,” ESC Congress program committee chair Stephan Windecker, MD, Bern (Switzerland) University Hospital, , told this news organization. “As long as it is not over, the digital format is here to stay.”
But it also appears that people who haven’t been able to attend the congress in person are keen to log in and engage online, Dr. Windecker said. The 2020 all-virtual conference drew a much younger pool of registrants, on average, than did the live conferences before the pandemic.
“I think that’s an indication of people that may be in training, in early stages of their career, or they don’t have the support from departments or from their practice, or other financial means.” But they are able to participate via computer, tablet, or smartphone, he said.
“Another advantage is that the recorded content can be replayed at the convenience of whoever wants to consume it at a later point in time,” he added. “Those are just some examples why the digital format is likely to stay,” on its own or in a new age of hybrid meetings.
New and updated guidelines
Leading off the guideline series is the document on diagnosis and treatment of acute and chronic HF, which leveraged the past few busy years of HF clinical trials to arrive at a number of new recommendations and strengthened level-of-evidence ratings. It covers both drug and device therapy of HF with reduced ejection fraction (HFrEF) and acute decompensated HF, and tweaks and further enshrines the concept of HF with mildly reduced ejection fraction (HFmrEF).
Several updated recommendations for both long-used and novel medications, notably the sodium-glucose cotransporter 2 inhibitors, will be included because of the recently appreciated evidence-based impact in HFrEF, Dr. Windecker noted.
“I think it will be particularly interesting to look for the SGLT2 inhibitors as not a completely new class of drugs, but certainly one where there has been a lot of new evidence, to look at how those drugs will be integrated in the overall care pathway.”
A top-line preview of the new HF guideline limited to drug therapy, presented at July’s Heart Failure Association of the European Society of Cardiology (ESC-HFA), provided a simple answer to a common question in the new, bountiful age of HFrEF medications: Which meds, initiated in what order?
As it happens, the new recommendation for first-line HFrEF drug therapy is not a silver bullet, but a shotgun – prompt initiation of at least four meds, one from each of four drug classes: renin-angiotensin system inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and SGLT2 inhibitors. Each class, as described in the document, is to be started as soon as safely feasible, in a sequence deemed appropriate for each individual patient.
Spotlight on EMPEROR-Preserved
The world already knows that the trial, which tested the SGLT2 inhibitor empagliflozin (Jardiance, Boehringer Ingelheim/Eli Lilly) on top of standard therapy, “met” its primary endpoint in almost 6,000 patients with HF with preserved ejection fraction (HFpEF), who included some with HFmrEF by more contemporary definitions.
That means patients in EMPEROR-Preserved assigned to take empagliflozin showed significantly fewer events that made up the study’s primary endpoint, a composite of CV death or HF hospitalization. It appears to be the first clearly significant overall medical therapy benefit for a clinical primary endpoint in a major randomized HFpEF drug trial.
And that, pending fuller presentation of trial results at the Congress on Aug. 27, could be a huge deal for the half of HF patients with left ventricular ejection fractions (LVEF) higher than the HFrEF range.
Those early top-line results weren’t a decisive bombshell for a field now filled with hope for a practice-changing empagliflozin outcome in EMPEROR-Preserved, which isn’t a certainty. They were more like the “boom” of a mortar launching a rocket of fireworks that may explode into a chrysanthemum or green comet or, sometimes, turn out to be no more than a dud. The promise of the early cursory results critically depends on further details.
“Provided there is a compelling benefit, this is what everyone has been waiting for in this condition for decades,” Mikhail N. Kosiborod, MD, director of cardiometabolic research at Saint Luke’s Mid-America Heart Institute, Kansas City, Mo., said.
“Already knowing that the trial met the primary endpoint is obviously very intriguing and encouraging,” he added. “But there are things we don’t know, such as: What is the magnitude of benefit? And whether that benefit, whatever the magnitude, is driven by reductions in both heart failure hospitalizations and cardiovascular death, or only one of the two.”
For example: “If we see an impressive benefit for reduction of hospitalizations, but not a significant reduction in death, that would still be a huge advance. That’s because, to date, we don’t have any drug for HFpEF that has convincingly demonstrated a compelling reduction in heart failure hospitalization or improvement in symptoms, function, or quality of life,” observed Dr. Kosiborod, who wasn’t part of EMPEROR-Preserved.
There have been “suggestions” from HFrEF trials that empagliflozin and dapagliflozin (Farxiga, AstraZeneca) “have very comparable effects on at least the endpoint of cardiovascular death or hospitalization for heart failure,” he said. “So, my expectation would be that whatever is observed in EMPEROR-Preserved is likely a class effect, as well.”
Following EMPEROR-Preserved on the agenda is EMPEROR-Pooled, a patient-level combined analysis of the EMPEROR series of trials that spans the range of HF, regardless of ejection fraction or diabetes status, primarily exploring the effects of empagliflozin on renal function.
Other offerings, Friday, Aug. 27
Scheduled immediately after EMPEROR-Preserved is a presentation on the SMART-MI trial, which should clarify whether management guided by continuous ambulatory monitoring is effective in patients considered at especially high arrhythmic risk. Entry called for recent myocardial infarction and an LVEF of 36%-50% with evidence of cardiac autonomic dysfunction.
The trial randomly assigned 400 such patients to be or not be implanted with a Reveal LINQ (Medtronic) loop recorder and followed them for up to 18 months, primarily for detection of potentially serious arrhythmic events. Endpoints that involved mortality, hospitalization or other clinical events were secondary.
In a time slot preceding both SMART-MI and EMPEROR-Preserved, the GUIDE-HF trial is following a projected 3,600 patients with HF implanted with a CardioMEMS HF System (Abbott) pulmonary artery (PA) pressure sensor to explore the its value for guiding management.
The trial’s three cohorts, followed for at least 12 months, include randomized sensor-monitored and control groups of patients with New York Heart Association class 2-4 symptoms, as well as a third observational set of patients in NYHA class 3. That’s the indication for which the CardioMEMS monitor gained approval in the United States in 2014 based on the 2011 CHAMPION trial, and which fared just as well in the 2017 CHAMPION Post-Approval Study.
The Friday Hot Lines also include Dal-GenE, which has entered about 6,000 patients with recent MI to test the once-abandoned cholesterol ester transfer protein (CETP) inhibitor dalcetrapib (DalCor) for any secondary-prevention benefits when used selectively. The trial’s hook: All its patients are confirmed to have the AA genotype of the rs1967309 variant in the ADCY9 gene, which has been associated with a pronounced clinical response to CETP inhibition.
Saturday, Aug. 28
The direct oral anticoagulants (DOACs) have largely replaced vitamin K antagonists in patients with nonvalvular atrial fibrillation (AFib). But whether DOACs are similarly preferable in the growing world population of people who have undergone transcatheter aortic valve replacement (TAVR or TAVI), an issue explored with variable results in the ATLANTIS and GALILEO trials, is far from settled.
The ENVISAGE-TAVI AF trial explored the question for the factor X inhibitor edoxaban (Savaysa, Lixiana, Daiichi-Sankyo) in 1,400 patients with AFib and a transfemoral TAVR in the previous 5 days, who were randomly assigned to the DOAC or standard management along with discretionary antiplatelet therapy. They’ve been followed for up to 3 years for a composite endpoint of clinical events – including death, MI, and stroke – and for major bleeding.
The day will also feature MASTER DAPT, a comparison of two dual-antiplatelet therapy (DAPT) regimens in an estimated 4,300 patients considered to be high-risk for bleeding who had received the sirolimus-eluting Ultimaster (Terumo) coronary stent, which has a bioresorbable polymer coating.
Investigators have randomly assigned patients to receive either very-short-duration DAPT, for about a month after stenting, followed by a P2Y12 inhibitor alone for up to a year after the procedure; or a more conventional regimen of a P2Y12 inhibitor for 6-12 months with aspirin maintained for a total of 12 months.
Later that day, investigators from the FIGARO-DKD trial will present their results based on 7,437 patients with type 2 diabetes and chronic kidney disease (CKD), a much fuller version than the top-line findings announced by sponsor Bayer 3 months ago.
Those top-line results suggested that patients assigned to receive the nonsteroidal nonselective mineralocorticoid receptor antagonist (MRA) finerenone (Kerendia) on top of standard care benefited with a drop in risk for the primary endpoint of CV death or nonfatal CV events.
Finerenone was recently approved in the United States for treating patients with both type 2 diabetes and CKD based on the published FIDELIO-DKD trial, which had seen less CKD progression and fewer CV events in such patients who took the novel MRA.
Although similar in design to FIGARO-DKD, FIDELIO-DKD had entered fewer patients with early-stage diabetic kidney disease (DKD). That led researchers to pool the two trials’ populations to create a cohort that spans the spectrum of DKD severity. An analysis of the pooled cohort, dubbed FIDELITY, is on the schedule after FIGARO-DKD.
After FIDELITY is the prospective APAF-CRT trial that is following a projected 1,830 patients with permanent, symptomatic AFib and a recent hospitalization for AFib or HF and who were not good candidates for standard ablation. They were assigned to receive either atrioventricular junctional ablation followed by CRT, with or without a defibrillation, on top of optimal meds – a so-called “ablate-and-pace” strategy – or an implantable cardioverter defibrillator with rate-control drug therapy.
The new analysis represents the trial’s second phase in which mortality was followed for 4 years as the primary endpoint, in contrast to the previously reported initial phase that followed the first 102 patients for 2 years for the composite primary endpoint of death, worsening HF, and HF hospitalization. The first phase had halted enrollment before reaching its planned target of 280 patients after an interim analysis showed a significant benefit for ablate and pace.
Next up: DECAAF 2, a randomized assessment of whether catheter ablation for AFib guided by delayed gadolinium enhancement on MRI, a proxy for scar tissue, can be more effective than standard AFib ablation by pulmonary vein isolation alone. An estimated 900 patients with persistent AFib who had never before undergone ablation for the arrhythmia were randomly assigned to one strategy or the other and followed for AFib recurrence over 18 months.
Sunday, Aug. 29
The TOMAHAWK trial aimed to clarify the optimal timing of invasive coronary angiography for resuscitated patients with non–ST-segment elevation out-of-hospital cardiac arrest, a broad population in a setting for which there is little randomized-trial guidance. Investigators randomly assigned 558 such patients to undergo immediate invasive angiography or to direct intensive care unit admission for initial standard care with discretionary delayed angiography. Patients were followed for all-cause mortality, with other clinical events and neurologic outcomes as secondary endpoints.
Next on the schedule, the RIPCORD-2 trial randomly assigned 1,100 patients with stable known or suspected coronary artery disease (CAD) to undergo conventional angiography alone or with added direct pressure-wire measurement of fractional flow reserve to guide management decisions. Primary outcomes include health care costs and patient-reported quality of life at 1 year.
Slated for later that day, the Asymptomatic Carotid Surgery Trial-2 (ACST-2) has entered an estimated 3600 patients with a substantial carotid artery narrowing not associated with symptoms but for which either carotid endarterectomy (CEA) or carotid artery stenting (CAS) was considered anatomically feasible. There also must have been “substantial uncertainty” regarding the optimal procedure choice.
The trial, conducted in 40 countries primarily in Europe and North America and launched in 2008, randomly assigned the patients to undergo either CEA or CAS, in both cases with appropriate medical therapy, and followed them for periprocedural events and up to 10 years for strokes and stroke-related events.
The LOOP study, which is to directly follow ACST-2, has explored whether screening for AFib using the Medtronic Reveal LINQ monitor in older patients with non-AFib stroke risk factors – with oral anticoagulation prescribed for those who test positive – can lower their risk for stroke or systemic embolism. It randomly assigned 6,000 such patients to care guided by the loop recorder or to standard care.
On a somewhat larger scale, the Salt Substitute and Stroke Study (SSaSS) randomly assigned a total of 20,996 people in about 600 villages across northern China and Tibet to sodium-restriction intervention and control groups by village. All participants had a history of stroke or were aged at least 60 years with uncontrolled hypertension.
As described by the trial’s online portal, participants in villages assigned to the intervention group were given a supply of a low-sodium, potassium-supplementing salt substitute to replace their own salt supplies, along with education on the health benefits of sodium restriction. Participants in control villages continued their normal diets and, at the trial’s beginning, received “advice to reduce their salt intake.” All were required to own a telephone.
Clinical events, including strokes and hospitalizations throughout a 5-year follow-up, were tracked by phone calls made to all participants every 6 months and were documented at follow-up home visits.
Sunday is also to feature a Late-Breaking Trials session with a focus on COVID-19, which leads off with COLCOVID, a test of colchicine in patients hospitalized for suspected SARS-CoV-2 infection and in acute respiratory distress.
The 1,279 participants in Argentina were randomly assigned to receive or not receive the potent anti-inflammatory agent on top of antivirals and other standard management and followed for death or new need for mechanical ventilation. A successful outcome would contrast with the RECOVERY trial, which terminated a colchicine group of patients hospitalized with COVID-19 because of a lack of efficacy earlier this year.
COLCOVID is to be followed by the MICHELLE trial of rivaroxaban (Xarelto, Bayer/Janssen) prophylaxis, compared with no preventive oral anticoagulant, in 320 patients who, when hospitalized with COVID-19, had been on parenteral anticoagulants because of an elevated risk for venous thromboembolism. The trial, conducted in Brazil, called for postdischarge rivaroxaban at a once-daily dosage of 10 mg for about 1 month.
The session also includes a presentation called “Insights into the Effects of the COVID-19 Pandemic: Comprehensive Analysis from the GUIDE-HF Trial,” the primary outcomes of which will be reported on the first day of the Congress.
Following is a presentation on the PREPARE-IT study of icosapent ethyl (Vascepa, Amarin), given at high dosages intended to be anti-inflammatory, compared with placebo, in an estimated 4,000 adults. The trial has two groups: A prevention group of adults living and circulating in the community; and a treatment group of patients aged at least 40 years with confirmed symptomatic SARS-CoV-2 infection for whom the need for hospitalization isn’t clear.
Monday, Aug. 30
The final day of the Congress features a trial called Influenza Vaccination after Myocardial Infarction (IAMI), which has tested the secondary preventive effect of influenza vaccination by randomly assigning 2,571 patients to receive a standard vaccine or a saline placebo injection on one occasion.
Entry to the international trial called for a diagnosis of MI with or without ST-segment elevation, or stable CAD and age at least 75 years with other risk factors. The patients were followed for death, MI, stent thrombosis, and a slew of secondary endpoints over 12 months.
Monday offerings continue later in a time block leading off with the STEP trial, which has randomly assigned an estimated 8,000 patients at 40 centers in China who are 60 to 80 years of age with a systolic blood pressure of 140 to <190 mm Hg to be on standard guideline-based therapy or an intensive drug-management strategy.
The systolic BP goals are 130 to <150 mm Hg for standard care and 110 to <130 mm Hg for the intensive regimen. The composite primary endpoint includes death and clinical events related to acute coronary syndromes, HF, revascularization, and stroke.
Following on heels of STEP, the Amulet IDE trial – the first major randomized comparison of two transcatheter LAA closure devices – entered 1,878 patients with nonvalvular AFib who were considered high-risk for bleeding and stroke or systemic embolism.
They were randomly assigned in the noninferiority trial to receive either the AMPLATZER Amulet (Abbott Medical Devices) or the WATCHMAN (Boston Scientific) closure devices and were followed for safety and efficacy for up to 5 years.
Both LAA closure devices, intended to make patients with AFib less reliant on oral anticoagulation, are now available on both sides of the Atlantic – as well as many other countries – after the Amulet’s United States market approval on Aug. 16, based largely on the Amulet IDE trial.
Rounding out the final Hot Line set is one of the latest efforts to show the efficacy and safety of a very short DAPT period after coronary stenting in patients with acute coronary syndromes, the STOPDAPT-2 ACS trial.
The study assigned 3,008 patients in Japan to receive aspirin and clopidogrel for either 1 month or 1 year after implantation with an everolimus-eluting cobalt-chromium stent and followed them for up to 5 years for a composite of MI, CV death, stent thrombosis, stroke, and bleeding.
The trial follows the published STOPDAPT-2 trial that showed superiority for the 1-month DAPT regimen in a predominantly stable-CAD population treated with the same kind of stent.
Program structure and format
A total of 15 online channels are to be available in the morning, European time, their schedules running in parallel. Presentations often are prerecorded, but also include live sessions at 8:00 a.m. Central time and 12 p.m. CET (2:00 a.m. and 6:00 a.m. Eastern time) to liven up the channel offerings, Dr. Windecker observed, and to make them more immediate and potentially interactive.
Many of the parallel channels are devoted throughout the Congress to particular silos of cardiology; for example, arrhythmias and device therapy is on channel 3; CAD and acute care is on 5; HF is on 6; and preventive cardiology is on 9.
Other channels swing across different topics from day to day, such as channel 1, which covers COVID-19 topics on the first and third day of the meeting, “advances in science” on day 2, and “digital health, public health, health economics” on day 4.
The focus each day, starting at 2:00 p.m. CET (8:00 a.m. ET) and continuing into the evening in Europe, shifts over to the Prime Time live program, which features the Hot Line and guideline presentations and many of the live abstract presentations.
Dr. Kosiborod, not a researcher with the EMPEROR trials, is chair of the Dapagliflozin in Preserved Ejection Fraction Heart Failure ( PRESERVED-HF ) trial, which is scheduled for presentation at the September 2021 Heart Failure Society of American meeting.
A version of this article first appeared on Medscape.com.