User login
Women at higher risk of serious adverse events from cancer therapy
and this is seen with chemotherapy, targeted agents, and especially with immunotherapy.
The finding comes from a review of more than 23,000 participants across 202 trials of various cancers (excluding sex-related cancers) that has been conducted over the past 40 years.
The investigators found a 34% increased risk of severe AEs among women, compared with men, climbing to a 49% higher risk with immunotherapy.
Women had a substantially greater risk of severe symptomatic AEs, including with immune checkpoint inhibitors and targeted tyrosine kinase inhibitors, and were more likely to experience severe hematologic AEs with chemotherapy and immunotherapy.
The particularly large sex differences with immunotherapy suggest “that studying AEs from these agents is a priority,” the investigators comment.
The article was published online on Feb. 4 in the Journal of Clinical Oncology.
“It has been understood that women have more toxicity from chemotherapy than men, but almost no research has aimed to understand whether that pattern held for novel treatments like immunotherapy or targeted therapies. We found similar large differences, especially for immune treatments,” said lead investigator Joseph Unger, PhD, a biostatistician and health services researcher at the Fred Hutchinson Cancer Research Center, Seattle, in an institutional press release.
A “better understanding of the nature of the underlying mechanisms could potentially lead to interventions or delivery modifications to reduce toxicity in women,” the investigators comment in their article.
Among a sea of possible explanations for the finding, there could be differences in how men and women metabolize cancer therapies or differences in how they perceive symptoms. Women may also receive relatively higher doses because of their body size or have higher adherence to treatment.
Whatever the case, as cancer treatment becomes increasingly individualized, “sex may be an important consideration,” Dr. Unger said.
Study details
The study involved 8,838 women and 14,458 men across the trials, which were phase 2 or 3 investigations conducted by the SWOG Cancer Research Network from 1980 to 2019. Trials including sex-related cancers were excluded. In the trials included in the review, the most common cancers were gastrointestinal and lung, followed by leukemia.
Seventy-five percent of the subjects received chemotherapy, and the rest received either targeted therapy or immunotherapy.
Two-thirds of the subjects had at least one grade 3 or higher AE; women had a 25% higher risk than men of having AEs of grade 5 or higher.
After adjusting for age, race, disease prognosis, and other factors, women were at increased risk of severe symptomatic AEs, such as nausea and pain, across all treatment lines and especially with immunotherapy, for which reports of symptomatic AEs were 66% higher.
Women also had a higher risk of symptomatic gastrointestinal AEs with all three treatments and a higher risk of sleep-related AEs with chemotherapy and immunotherapy, which “could be a function of hormonal effects interacting with cancer treatment,” the investigators said.
As for readily measurable AEs, women were at higher risk than men for objective hematologic AEs with chemotherapy, immunotherapy, and targeted therapy. There were no statistically significant sex differences in the risk of nonhematologic objective AEs.
The team notes that increased toxicity among women has been associated with improved survival, which may give AEs more time to develop. Higher rates of AEs might also signal increased delivery or efficacy of cancer treatments.
However, a previous study found that men may have a better response to immunotherapy than women. Immune checkpoint inhibitors were twice as effective as standard cancer therapies in the treatment of men with advanced solid tumors compared to their female counterparts, concluded a team that carried out a meta-analysis of 20 randomized controlled trials involving more than 11,351 patients.
The study was funded by the National Cancer Institute and others. Dr. Unger has disclosed no relevant financial relationships. Several coauthors have reported ties to a handful of companies, including Johnson & Johnson and Seattle Genetics. One is an employee of AIM Specialty Health.
A version of this article first appeared on Medscape.com.
and this is seen with chemotherapy, targeted agents, and especially with immunotherapy.
The finding comes from a review of more than 23,000 participants across 202 trials of various cancers (excluding sex-related cancers) that has been conducted over the past 40 years.
The investigators found a 34% increased risk of severe AEs among women, compared with men, climbing to a 49% higher risk with immunotherapy.
Women had a substantially greater risk of severe symptomatic AEs, including with immune checkpoint inhibitors and targeted tyrosine kinase inhibitors, and were more likely to experience severe hematologic AEs with chemotherapy and immunotherapy.
The particularly large sex differences with immunotherapy suggest “that studying AEs from these agents is a priority,” the investigators comment.
The article was published online on Feb. 4 in the Journal of Clinical Oncology.
“It has been understood that women have more toxicity from chemotherapy than men, but almost no research has aimed to understand whether that pattern held for novel treatments like immunotherapy or targeted therapies. We found similar large differences, especially for immune treatments,” said lead investigator Joseph Unger, PhD, a biostatistician and health services researcher at the Fred Hutchinson Cancer Research Center, Seattle, in an institutional press release.
A “better understanding of the nature of the underlying mechanisms could potentially lead to interventions or delivery modifications to reduce toxicity in women,” the investigators comment in their article.
Among a sea of possible explanations for the finding, there could be differences in how men and women metabolize cancer therapies or differences in how they perceive symptoms. Women may also receive relatively higher doses because of their body size or have higher adherence to treatment.
Whatever the case, as cancer treatment becomes increasingly individualized, “sex may be an important consideration,” Dr. Unger said.
Study details
The study involved 8,838 women and 14,458 men across the trials, which were phase 2 or 3 investigations conducted by the SWOG Cancer Research Network from 1980 to 2019. Trials including sex-related cancers were excluded. In the trials included in the review, the most common cancers were gastrointestinal and lung, followed by leukemia.
Seventy-five percent of the subjects received chemotherapy, and the rest received either targeted therapy or immunotherapy.
Two-thirds of the subjects had at least one grade 3 or higher AE; women had a 25% higher risk than men of having AEs of grade 5 or higher.
After adjusting for age, race, disease prognosis, and other factors, women were at increased risk of severe symptomatic AEs, such as nausea and pain, across all treatment lines and especially with immunotherapy, for which reports of symptomatic AEs were 66% higher.
Women also had a higher risk of symptomatic gastrointestinal AEs with all three treatments and a higher risk of sleep-related AEs with chemotherapy and immunotherapy, which “could be a function of hormonal effects interacting with cancer treatment,” the investigators said.
As for readily measurable AEs, women were at higher risk than men for objective hematologic AEs with chemotherapy, immunotherapy, and targeted therapy. There were no statistically significant sex differences in the risk of nonhematologic objective AEs.
The team notes that increased toxicity among women has been associated with improved survival, which may give AEs more time to develop. Higher rates of AEs might also signal increased delivery or efficacy of cancer treatments.
However, a previous study found that men may have a better response to immunotherapy than women. Immune checkpoint inhibitors were twice as effective as standard cancer therapies in the treatment of men with advanced solid tumors compared to their female counterparts, concluded a team that carried out a meta-analysis of 20 randomized controlled trials involving more than 11,351 patients.
The study was funded by the National Cancer Institute and others. Dr. Unger has disclosed no relevant financial relationships. Several coauthors have reported ties to a handful of companies, including Johnson & Johnson and Seattle Genetics. One is an employee of AIM Specialty Health.
A version of this article first appeared on Medscape.com.
and this is seen with chemotherapy, targeted agents, and especially with immunotherapy.
The finding comes from a review of more than 23,000 participants across 202 trials of various cancers (excluding sex-related cancers) that has been conducted over the past 40 years.
The investigators found a 34% increased risk of severe AEs among women, compared with men, climbing to a 49% higher risk with immunotherapy.
Women had a substantially greater risk of severe symptomatic AEs, including with immune checkpoint inhibitors and targeted tyrosine kinase inhibitors, and were more likely to experience severe hematologic AEs with chemotherapy and immunotherapy.
The particularly large sex differences with immunotherapy suggest “that studying AEs from these agents is a priority,” the investigators comment.
The article was published online on Feb. 4 in the Journal of Clinical Oncology.
“It has been understood that women have more toxicity from chemotherapy than men, but almost no research has aimed to understand whether that pattern held for novel treatments like immunotherapy or targeted therapies. We found similar large differences, especially for immune treatments,” said lead investigator Joseph Unger, PhD, a biostatistician and health services researcher at the Fred Hutchinson Cancer Research Center, Seattle, in an institutional press release.
A “better understanding of the nature of the underlying mechanisms could potentially lead to interventions or delivery modifications to reduce toxicity in women,” the investigators comment in their article.
Among a sea of possible explanations for the finding, there could be differences in how men and women metabolize cancer therapies or differences in how they perceive symptoms. Women may also receive relatively higher doses because of their body size or have higher adherence to treatment.
Whatever the case, as cancer treatment becomes increasingly individualized, “sex may be an important consideration,” Dr. Unger said.
Study details
The study involved 8,838 women and 14,458 men across the trials, which were phase 2 or 3 investigations conducted by the SWOG Cancer Research Network from 1980 to 2019. Trials including sex-related cancers were excluded. In the trials included in the review, the most common cancers were gastrointestinal and lung, followed by leukemia.
Seventy-five percent of the subjects received chemotherapy, and the rest received either targeted therapy or immunotherapy.
Two-thirds of the subjects had at least one grade 3 or higher AE; women had a 25% higher risk than men of having AEs of grade 5 or higher.
After adjusting for age, race, disease prognosis, and other factors, women were at increased risk of severe symptomatic AEs, such as nausea and pain, across all treatment lines and especially with immunotherapy, for which reports of symptomatic AEs were 66% higher.
Women also had a higher risk of symptomatic gastrointestinal AEs with all three treatments and a higher risk of sleep-related AEs with chemotherapy and immunotherapy, which “could be a function of hormonal effects interacting with cancer treatment,” the investigators said.
As for readily measurable AEs, women were at higher risk than men for objective hematologic AEs with chemotherapy, immunotherapy, and targeted therapy. There were no statistically significant sex differences in the risk of nonhematologic objective AEs.
The team notes that increased toxicity among women has been associated with improved survival, which may give AEs more time to develop. Higher rates of AEs might also signal increased delivery or efficacy of cancer treatments.
However, a previous study found that men may have a better response to immunotherapy than women. Immune checkpoint inhibitors were twice as effective as standard cancer therapies in the treatment of men with advanced solid tumors compared to their female counterparts, concluded a team that carried out a meta-analysis of 20 randomized controlled trials involving more than 11,351 patients.
The study was funded by the National Cancer Institute and others. Dr. Unger has disclosed no relevant financial relationships. Several coauthors have reported ties to a handful of companies, including Johnson & Johnson and Seattle Genetics. One is an employee of AIM Specialty Health.
A version of this article first appeared on Medscape.com.
President Biden’s ‘Cancer Moonshot’ to be relaunched
The “Cancer Moonshot” is about to be relaunched.
In a White House briefing, President Joe Biden announced that he is “reigniting” the initiative he spearheaded when he was vice president during the Obama administration.
During the livestreamed event, the president discussed his plans to bring a “fierce sense of urgency” to the fight against cancer and better support patients with cancer and their families.
He emphasized that cancer is one of the truly bipartisan issues. There is strong support from both “sides of the aisle,” he said, and he sees it as an issue that can bring the country together.
“We can do this. I promise you, we can do this. For all those we lost, for all those we miss. We can end cancer as we know it,” he said. “This is a presidential White House priority.”
The aim is to reduce the death rate from cancer by at least 50% over the next 25 years.
There is also a proposal to create the Advanced Research Projects Agency for Health, which would focus on driving cutting-edge innovation in health research.
Part of the plan is to assemble a “cancer cabinet” that includes 18 federal departments, agencies, and offices, including leaders from the departments of Health & Human Services, Veterans Affairs, Defense, Energy, and Agriculture.
At present, there are few details about the new program or how it will be funded.
Presumably more will be revealed at the Cancer Moonshot Summit being planned, as well as on a planned new website where people can track its progress.
President priority
Cancer Moonshot began back in 2016, when during his last State of the Union Address, former President Barack Obama announced the ambitious initiative. A few days later, Obama asked Congress for $1 billion to send cancer to the moon, and he put Biden, then vice president, in charge of “mission control” in the remaining months of the administration.
The new initiative will be headed by Danielle Carnival, PhD, who serves in the White House Office of Science and Technology Policy and has been appointed as White House Cancer Moonshot coordinator.
At the briefing, Mr. Biden and Vice President Kamala Harris spoke about losing family members to cancer. The president spoke about his eldest son, Beau, who died from brain cancer when he was 46 years old, while Ms. Harris spoke about her mother, Shyamala Gopalan, a breast cancer researcher who died of colon cancer in 2009.
Accolades but a bit of caution
The president’s speech was applauded by many cancer groups, both professional organizations and patient advocacy groups.
Karen E. Knudsen, PhD, chief executive officer of the American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, commended Mr. Biden for reigniting Cancer Moonshot.
“In 2022 alone, there will be an estimated 1.9 million people diagnosed with cancer and more than 600,000 people in the U.S. will die. Marshaling the resources of the federal government will be critical in our ability to reduce death and suffering from this disease,” she said.
The American Society for Radiation Oncology issued a press release, saying: “On behalf of radiation oncologists who treat people with cancer every day, we support the Biden-Harris administration’s move to drastically reduce the number of cancer deaths in the United States and improve the lives of people diagnosed with this disease.
“We believe the administration’s commitment to expand cancer prevention efforts and to increase equitable access to screenings and treatments will help mitigate some of the negative impact of the COVID-19 pandemic,” the society added.
At the American Association for Cancer Research, Chief Executive Officer Margaret Foti, MD, PhD, said she was thrilled to hear the announcement after the devastating interruptions in cancer research and patient care over the past 2 years.
“The reignited Cancer Moonshot will provide an important framework to help improve cancer prevention strategies, increase cancer screenings and early detection, reduce cancer disparities, and propel new lifesaving cures for patients with cancer,” she said.
However, increased funding from Congress will be needed for these goals to be achieved, she emphasized.
A version of this article first appeared on Medscape.com.
The “Cancer Moonshot” is about to be relaunched.
In a White House briefing, President Joe Biden announced that he is “reigniting” the initiative he spearheaded when he was vice president during the Obama administration.
During the livestreamed event, the president discussed his plans to bring a “fierce sense of urgency” to the fight against cancer and better support patients with cancer and their families.
He emphasized that cancer is one of the truly bipartisan issues. There is strong support from both “sides of the aisle,” he said, and he sees it as an issue that can bring the country together.
“We can do this. I promise you, we can do this. For all those we lost, for all those we miss. We can end cancer as we know it,” he said. “This is a presidential White House priority.”
The aim is to reduce the death rate from cancer by at least 50% over the next 25 years.
There is also a proposal to create the Advanced Research Projects Agency for Health, which would focus on driving cutting-edge innovation in health research.
Part of the plan is to assemble a “cancer cabinet” that includes 18 federal departments, agencies, and offices, including leaders from the departments of Health & Human Services, Veterans Affairs, Defense, Energy, and Agriculture.
At present, there are few details about the new program or how it will be funded.
Presumably more will be revealed at the Cancer Moonshot Summit being planned, as well as on a planned new website where people can track its progress.
President priority
Cancer Moonshot began back in 2016, when during his last State of the Union Address, former President Barack Obama announced the ambitious initiative. A few days later, Obama asked Congress for $1 billion to send cancer to the moon, and he put Biden, then vice president, in charge of “mission control” in the remaining months of the administration.
The new initiative will be headed by Danielle Carnival, PhD, who serves in the White House Office of Science and Technology Policy and has been appointed as White House Cancer Moonshot coordinator.
At the briefing, Mr. Biden and Vice President Kamala Harris spoke about losing family members to cancer. The president spoke about his eldest son, Beau, who died from brain cancer when he was 46 years old, while Ms. Harris spoke about her mother, Shyamala Gopalan, a breast cancer researcher who died of colon cancer in 2009.
Accolades but a bit of caution
The president’s speech was applauded by many cancer groups, both professional organizations and patient advocacy groups.
Karen E. Knudsen, PhD, chief executive officer of the American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, commended Mr. Biden for reigniting Cancer Moonshot.
“In 2022 alone, there will be an estimated 1.9 million people diagnosed with cancer and more than 600,000 people in the U.S. will die. Marshaling the resources of the federal government will be critical in our ability to reduce death and suffering from this disease,” she said.
The American Society for Radiation Oncology issued a press release, saying: “On behalf of radiation oncologists who treat people with cancer every day, we support the Biden-Harris administration’s move to drastically reduce the number of cancer deaths in the United States and improve the lives of people diagnosed with this disease.
“We believe the administration’s commitment to expand cancer prevention efforts and to increase equitable access to screenings and treatments will help mitigate some of the negative impact of the COVID-19 pandemic,” the society added.
At the American Association for Cancer Research, Chief Executive Officer Margaret Foti, MD, PhD, said she was thrilled to hear the announcement after the devastating interruptions in cancer research and patient care over the past 2 years.
“The reignited Cancer Moonshot will provide an important framework to help improve cancer prevention strategies, increase cancer screenings and early detection, reduce cancer disparities, and propel new lifesaving cures for patients with cancer,” she said.
However, increased funding from Congress will be needed for these goals to be achieved, she emphasized.
A version of this article first appeared on Medscape.com.
The “Cancer Moonshot” is about to be relaunched.
In a White House briefing, President Joe Biden announced that he is “reigniting” the initiative he spearheaded when he was vice president during the Obama administration.
During the livestreamed event, the president discussed his plans to bring a “fierce sense of urgency” to the fight against cancer and better support patients with cancer and their families.
He emphasized that cancer is one of the truly bipartisan issues. There is strong support from both “sides of the aisle,” he said, and he sees it as an issue that can bring the country together.
“We can do this. I promise you, we can do this. For all those we lost, for all those we miss. We can end cancer as we know it,” he said. “This is a presidential White House priority.”
The aim is to reduce the death rate from cancer by at least 50% over the next 25 years.
There is also a proposal to create the Advanced Research Projects Agency for Health, which would focus on driving cutting-edge innovation in health research.
Part of the plan is to assemble a “cancer cabinet” that includes 18 federal departments, agencies, and offices, including leaders from the departments of Health & Human Services, Veterans Affairs, Defense, Energy, and Agriculture.
At present, there are few details about the new program or how it will be funded.
Presumably more will be revealed at the Cancer Moonshot Summit being planned, as well as on a planned new website where people can track its progress.
President priority
Cancer Moonshot began back in 2016, when during his last State of the Union Address, former President Barack Obama announced the ambitious initiative. A few days later, Obama asked Congress for $1 billion to send cancer to the moon, and he put Biden, then vice president, in charge of “mission control” in the remaining months of the administration.
The new initiative will be headed by Danielle Carnival, PhD, who serves in the White House Office of Science and Technology Policy and has been appointed as White House Cancer Moonshot coordinator.
At the briefing, Mr. Biden and Vice President Kamala Harris spoke about losing family members to cancer. The president spoke about his eldest son, Beau, who died from brain cancer when he was 46 years old, while Ms. Harris spoke about her mother, Shyamala Gopalan, a breast cancer researcher who died of colon cancer in 2009.
Accolades but a bit of caution
The president’s speech was applauded by many cancer groups, both professional organizations and patient advocacy groups.
Karen E. Knudsen, PhD, chief executive officer of the American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, commended Mr. Biden for reigniting Cancer Moonshot.
“In 2022 alone, there will be an estimated 1.9 million people diagnosed with cancer and more than 600,000 people in the U.S. will die. Marshaling the resources of the federal government will be critical in our ability to reduce death and suffering from this disease,” she said.
The American Society for Radiation Oncology issued a press release, saying: “On behalf of radiation oncologists who treat people with cancer every day, we support the Biden-Harris administration’s move to drastically reduce the number of cancer deaths in the United States and improve the lives of people diagnosed with this disease.
“We believe the administration’s commitment to expand cancer prevention efforts and to increase equitable access to screenings and treatments will help mitigate some of the negative impact of the COVID-19 pandemic,” the society added.
At the American Association for Cancer Research, Chief Executive Officer Margaret Foti, MD, PhD, said she was thrilled to hear the announcement after the devastating interruptions in cancer research and patient care over the past 2 years.
“The reignited Cancer Moonshot will provide an important framework to help improve cancer prevention strategies, increase cancer screenings and early detection, reduce cancer disparities, and propel new lifesaving cures for patients with cancer,” she said.
However, increased funding from Congress will be needed for these goals to be achieved, she emphasized.
A version of this article first appeared on Medscape.com.
Earlier diagnosis could prevent more than 20% of cancer deaths
Those figures translate to 2,064 to 2,677 fewer cancer deaths annually in the state of New South Wales between 2005 and 2014, the most recent period studied.
“While it is well established that diagnosing cancers at an earlier stage is ‘better,’ our study is unique in that it quantifies what that ‘better’ might look like in terms of how many deaths would be avoided within 10 years of diagnosis,” the authors write in an article published online Jan. 17 in the International Journal of Cancer. “By doing so, it is hoped that these results will provide continued motivation to develop more effective strategies to diagnose cancers at an earlier stage.”
Of course, achieving such a “stage-shift in practice is difficult,” study author Xue Qin Yu, PhD, of The Daffodil Centre in Sydney and colleagues, acknowledge. First, Dr. Yu and colleagues note, “diagnosis at an earlier stage can be challenging due to the nonspecific nature of many common symptoms which may not be recognized by either patients or doctors.” Plus, they add, a challenge for diagnosing cancers at an earlier stage “is the overall low uptake of screening.”
For their study, the researchers used data from a cohort of more than 716,000 people aged 15 to 89 years diagnosed with a solid cancer in New South Wales between 1985 and 2014 and followed through 2015.
To estimate how many deaths could be avoided if tumors were caught earlier, the authors looked at two scenarios. In scenario 1, they assumed all known cases of distant cancer were instead diagnosed at the regional stage, and in scenario 2, they assumed half of the cases were diagnosed as regional and half as localized disease.
Under the conservative scenario 1, about 18% of the observed cancer deaths in males and 26% in females could be avoided. In total, this corresponded to 21% of observed deaths.
Colorectal cancer topped the list of avoidable deaths in both men (27%) and women (33%), followed by prostate cancer in men (19%), breast cancer in women (18%), and melanoma in women (16%) and men (13%).
Under scenario 2, 24% of cancer deaths in males and 32% in females – or 28% overall – were avoidable.
The researchers caution that their study is limited by a high proportion of cases of unknown stage. Still, they say their findings are consistent with results from the United States indicating 15% to 25% of cancer-related deaths were potentially avoidable if tumors were detected before metastasizing.
“Given our study cohort was sourced from a population-based cancer registry with complete enumeration of cancers diagnosed during the study period, it is likely that our study findings, particularly in terms of the population rate of avoidable deaths, would be generalizable to other populations with similar characteristics,” Dr. Yu and colleagues write. “However, results may be different in countries that have a different mix of cancer types or distribution of stage at diagnosis.”
A version of this article first appeared on Medscape.com.
Those figures translate to 2,064 to 2,677 fewer cancer deaths annually in the state of New South Wales between 2005 and 2014, the most recent period studied.
“While it is well established that diagnosing cancers at an earlier stage is ‘better,’ our study is unique in that it quantifies what that ‘better’ might look like in terms of how many deaths would be avoided within 10 years of diagnosis,” the authors write in an article published online Jan. 17 in the International Journal of Cancer. “By doing so, it is hoped that these results will provide continued motivation to develop more effective strategies to diagnose cancers at an earlier stage.”
Of course, achieving such a “stage-shift in practice is difficult,” study author Xue Qin Yu, PhD, of The Daffodil Centre in Sydney and colleagues, acknowledge. First, Dr. Yu and colleagues note, “diagnosis at an earlier stage can be challenging due to the nonspecific nature of many common symptoms which may not be recognized by either patients or doctors.” Plus, they add, a challenge for diagnosing cancers at an earlier stage “is the overall low uptake of screening.”
For their study, the researchers used data from a cohort of more than 716,000 people aged 15 to 89 years diagnosed with a solid cancer in New South Wales between 1985 and 2014 and followed through 2015.
To estimate how many deaths could be avoided if tumors were caught earlier, the authors looked at two scenarios. In scenario 1, they assumed all known cases of distant cancer were instead diagnosed at the regional stage, and in scenario 2, they assumed half of the cases were diagnosed as regional and half as localized disease.
Under the conservative scenario 1, about 18% of the observed cancer deaths in males and 26% in females could be avoided. In total, this corresponded to 21% of observed deaths.
Colorectal cancer topped the list of avoidable deaths in both men (27%) and women (33%), followed by prostate cancer in men (19%), breast cancer in women (18%), and melanoma in women (16%) and men (13%).
Under scenario 2, 24% of cancer deaths in males and 32% in females – or 28% overall – were avoidable.
The researchers caution that their study is limited by a high proportion of cases of unknown stage. Still, they say their findings are consistent with results from the United States indicating 15% to 25% of cancer-related deaths were potentially avoidable if tumors were detected before metastasizing.
“Given our study cohort was sourced from a population-based cancer registry with complete enumeration of cancers diagnosed during the study period, it is likely that our study findings, particularly in terms of the population rate of avoidable deaths, would be generalizable to other populations with similar characteristics,” Dr. Yu and colleagues write. “However, results may be different in countries that have a different mix of cancer types or distribution of stage at diagnosis.”
A version of this article first appeared on Medscape.com.
Those figures translate to 2,064 to 2,677 fewer cancer deaths annually in the state of New South Wales between 2005 and 2014, the most recent period studied.
“While it is well established that diagnosing cancers at an earlier stage is ‘better,’ our study is unique in that it quantifies what that ‘better’ might look like in terms of how many deaths would be avoided within 10 years of diagnosis,” the authors write in an article published online Jan. 17 in the International Journal of Cancer. “By doing so, it is hoped that these results will provide continued motivation to develop more effective strategies to diagnose cancers at an earlier stage.”
Of course, achieving such a “stage-shift in practice is difficult,” study author Xue Qin Yu, PhD, of The Daffodil Centre in Sydney and colleagues, acknowledge. First, Dr. Yu and colleagues note, “diagnosis at an earlier stage can be challenging due to the nonspecific nature of many common symptoms which may not be recognized by either patients or doctors.” Plus, they add, a challenge for diagnosing cancers at an earlier stage “is the overall low uptake of screening.”
For their study, the researchers used data from a cohort of more than 716,000 people aged 15 to 89 years diagnosed with a solid cancer in New South Wales between 1985 and 2014 and followed through 2015.
To estimate how many deaths could be avoided if tumors were caught earlier, the authors looked at two scenarios. In scenario 1, they assumed all known cases of distant cancer were instead diagnosed at the regional stage, and in scenario 2, they assumed half of the cases were diagnosed as regional and half as localized disease.
Under the conservative scenario 1, about 18% of the observed cancer deaths in males and 26% in females could be avoided. In total, this corresponded to 21% of observed deaths.
Colorectal cancer topped the list of avoidable deaths in both men (27%) and women (33%), followed by prostate cancer in men (19%), breast cancer in women (18%), and melanoma in women (16%) and men (13%).
Under scenario 2, 24% of cancer deaths in males and 32% in females – or 28% overall – were avoidable.
The researchers caution that their study is limited by a high proportion of cases of unknown stage. Still, they say their findings are consistent with results from the United States indicating 15% to 25% of cancer-related deaths were potentially avoidable if tumors were detected before metastasizing.
“Given our study cohort was sourced from a population-based cancer registry with complete enumeration of cancers diagnosed during the study period, it is likely that our study findings, particularly in terms of the population rate of avoidable deaths, would be generalizable to other populations with similar characteristics,” Dr. Yu and colleagues write. “However, results may be different in countries that have a different mix of cancer types or distribution of stage at diagnosis.”
A version of this article first appeared on Medscape.com.
Breast cancer now leading cause of cancer death in Black women
Breast cancer has replaced lung cancer as the leading cause of cancer-related death among Black women, but lung cancer remains the leading cause of cancer death in Black men, according to a new report from the American Cancer Society (ACS).
Lung cancer remains the second most commonly diagnosed cancer in both Black women and Black men.
These are among the key findings of the report, Cancer Statistics for African American/Black People 2022 – a triannual compilation of U.S. data on cancer incidence, mortality, survival, screening, and risk factors for Black people – and it marks a major shift as of 2019.
“African American/Black people have a disproportionately high cancer burden compared to other population groups. According to the report, the risk of cancer death for Black individuals remains 19% higher for men and 12% higher for women compared to White individuals,” the ACS says in a statement.
“The gap for breast cancer is more alarming,” it adds. “Black women are 41% more likely to die from breast cancer than White women despite a lower risk of being diagnosed with the disease.”
The new report, published online on Feb. 10 in CA: A Cancer Journal for Clinicians, also notes the following:
An estimated 224,080 new cancer cases and 73,680 cancer deaths will occur among Black people in 2022.
Over the past 5 data years, Black women had an 8% lower overall cancer incidence than White women but 12% higher mortality; Black men have 6% higher cancer incidence than White men but 19% higher cancer mortality.
Prostate cancer mortality among Black men decreased by 1.3% per year from 2015 to 2019 despite a 5% increase in the diagnosis of distant-stage prostate cancer annually since 2012, but the decline was slower than the 5% per year decline from 2010 to 2014.
The overall cancer mortality gap between Black and White people is narrowing. This is due to a steeper drop in prostate, lung, and other smoking-related cancers among Black people.
Colorectal cancer incidence and mortality rates are 21% and 44% higher, respectively, in Black men in comparison with White men and 18% and 31% higher, respectively, in Black women in comparison with White women.
The reasons for the disparities are complex but “largely stem from less access to high-quality care and optimal treatment as a repercussion of long-standing institutional racism,” the report concludes.
“We must address structural racism as a public health issue to close the gaps and advance health equity,” Tawana Thomas-Johnson, senior vice president and chief diversity officer at the ACS, said in the press release.
A version of this article first appeared on Medscape.com.
Breast cancer has replaced lung cancer as the leading cause of cancer-related death among Black women, but lung cancer remains the leading cause of cancer death in Black men, according to a new report from the American Cancer Society (ACS).
Lung cancer remains the second most commonly diagnosed cancer in both Black women and Black men.
These are among the key findings of the report, Cancer Statistics for African American/Black People 2022 – a triannual compilation of U.S. data on cancer incidence, mortality, survival, screening, and risk factors for Black people – and it marks a major shift as of 2019.
“African American/Black people have a disproportionately high cancer burden compared to other population groups. According to the report, the risk of cancer death for Black individuals remains 19% higher for men and 12% higher for women compared to White individuals,” the ACS says in a statement.
“The gap for breast cancer is more alarming,” it adds. “Black women are 41% more likely to die from breast cancer than White women despite a lower risk of being diagnosed with the disease.”
The new report, published online on Feb. 10 in CA: A Cancer Journal for Clinicians, also notes the following:
An estimated 224,080 new cancer cases and 73,680 cancer deaths will occur among Black people in 2022.
Over the past 5 data years, Black women had an 8% lower overall cancer incidence than White women but 12% higher mortality; Black men have 6% higher cancer incidence than White men but 19% higher cancer mortality.
Prostate cancer mortality among Black men decreased by 1.3% per year from 2015 to 2019 despite a 5% increase in the diagnosis of distant-stage prostate cancer annually since 2012, but the decline was slower than the 5% per year decline from 2010 to 2014.
The overall cancer mortality gap between Black and White people is narrowing. This is due to a steeper drop in prostate, lung, and other smoking-related cancers among Black people.
Colorectal cancer incidence and mortality rates are 21% and 44% higher, respectively, in Black men in comparison with White men and 18% and 31% higher, respectively, in Black women in comparison with White women.
The reasons for the disparities are complex but “largely stem from less access to high-quality care and optimal treatment as a repercussion of long-standing institutional racism,” the report concludes.
“We must address structural racism as a public health issue to close the gaps and advance health equity,” Tawana Thomas-Johnson, senior vice president and chief diversity officer at the ACS, said in the press release.
A version of this article first appeared on Medscape.com.
Breast cancer has replaced lung cancer as the leading cause of cancer-related death among Black women, but lung cancer remains the leading cause of cancer death in Black men, according to a new report from the American Cancer Society (ACS).
Lung cancer remains the second most commonly diagnosed cancer in both Black women and Black men.
These are among the key findings of the report, Cancer Statistics for African American/Black People 2022 – a triannual compilation of U.S. data on cancer incidence, mortality, survival, screening, and risk factors for Black people – and it marks a major shift as of 2019.
“African American/Black people have a disproportionately high cancer burden compared to other population groups. According to the report, the risk of cancer death for Black individuals remains 19% higher for men and 12% higher for women compared to White individuals,” the ACS says in a statement.
“The gap for breast cancer is more alarming,” it adds. “Black women are 41% more likely to die from breast cancer than White women despite a lower risk of being diagnosed with the disease.”
The new report, published online on Feb. 10 in CA: A Cancer Journal for Clinicians, also notes the following:
An estimated 224,080 new cancer cases and 73,680 cancer deaths will occur among Black people in 2022.
Over the past 5 data years, Black women had an 8% lower overall cancer incidence than White women but 12% higher mortality; Black men have 6% higher cancer incidence than White men but 19% higher cancer mortality.
Prostate cancer mortality among Black men decreased by 1.3% per year from 2015 to 2019 despite a 5% increase in the diagnosis of distant-stage prostate cancer annually since 2012, but the decline was slower than the 5% per year decline from 2010 to 2014.
The overall cancer mortality gap between Black and White people is narrowing. This is due to a steeper drop in prostate, lung, and other smoking-related cancers among Black people.
Colorectal cancer incidence and mortality rates are 21% and 44% higher, respectively, in Black men in comparison with White men and 18% and 31% higher, respectively, in Black women in comparison with White women.
The reasons for the disparities are complex but “largely stem from less access to high-quality care and optimal treatment as a repercussion of long-standing institutional racism,” the report concludes.
“We must address structural racism as a public health issue to close the gaps and advance health equity,” Tawana Thomas-Johnson, senior vice president and chief diversity officer at the ACS, said in the press release.
A version of this article first appeared on Medscape.com.
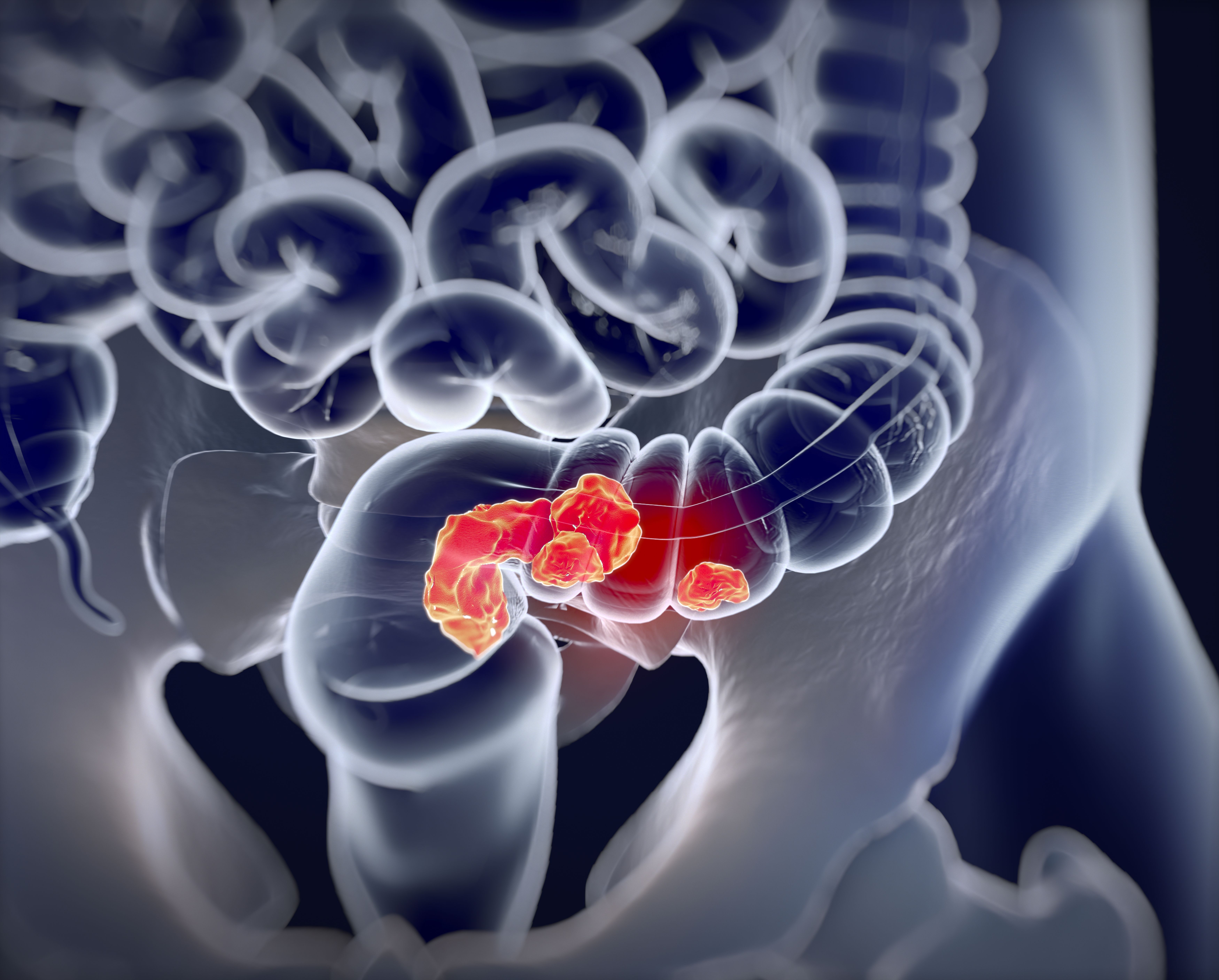
Gum disease linked to colorectal cancer: COLDENT study
findings from the population-based case-control COLDENT study suggest.
The rate of new CRC diagnoses among individuals in the study who had a history of PD was nearly 50% higher than in those with no such history, after adjustment for a host of medical and demographic factors, the investigators noted.
This isn’t the first time PD has been linked with extra-oral health outcomes, including gastrointestinal cancers. It has been shown to be associated with several major systemic diseases, such as cardiovascular, respiratory, chronic kidney, and metabolic diseases. Evidence also suggests a link between PD and Alzheimer’s disease.
However, prior studies that looked at the connection between PD and CRC have relied on secondary analyses of data from other studies and are limited by other methodologic shortcomings, noted the researchers, led by Amal Idrissi Janati, DDS, University of Montreal.
To better assess the etiologic role of PD in the development of CRC, Dr. Janati and colleagues analyzed 348 histologically confirmed cases of colon or rectal cancer diagnosed from January 2013 to December 2019 and compared them to 310 matched controls.
The rate of new CRC diagnoses among individuals with a history of PD was 1.4 times higher than among those with no PD history after adjustment for age and gender. It increased to 1.45 times higher when the researchers also adjusted for body mass index, education, income, diabetes, family history of CRC, regular use of aspirin and non-aspirin nonsteroidal anti-inflammatory drugs, and lifetime cumulative smoking, consumption of red and processed meats, alcohol consumption, and total physical activity score.
The findings were published online Jan. 26 in Cancer Causes and Control.
“Our results support the hypothesis of an association between PD and sporadic CRC risk,” the researchers said, adding that further epidemiologic studies are recommended.
They speculated that the “putative mechanism of PD and cancer association involves the spread of periodontal pathogens to extra-oral sites, dissemination of bacteria endotoxins, and release of inflammation products directly into the bloodstream.”
The chronic inflammation associated with PD “promotes carcinogenesis by induction of gene mutations, inhibition of apoptosis, stimulation of angiogenesis, cell proliferation, and epigenetic alterations,” they added.
The COLDENT study was supported by the Cancer Research Society. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
findings from the population-based case-control COLDENT study suggest.
The rate of new CRC diagnoses among individuals in the study who had a history of PD was nearly 50% higher than in those with no such history, after adjustment for a host of medical and demographic factors, the investigators noted.
This isn’t the first time PD has been linked with extra-oral health outcomes, including gastrointestinal cancers. It has been shown to be associated with several major systemic diseases, such as cardiovascular, respiratory, chronic kidney, and metabolic diseases. Evidence also suggests a link between PD and Alzheimer’s disease.
However, prior studies that looked at the connection between PD and CRC have relied on secondary analyses of data from other studies and are limited by other methodologic shortcomings, noted the researchers, led by Amal Idrissi Janati, DDS, University of Montreal.
To better assess the etiologic role of PD in the development of CRC, Dr. Janati and colleagues analyzed 348 histologically confirmed cases of colon or rectal cancer diagnosed from January 2013 to December 2019 and compared them to 310 matched controls.
The rate of new CRC diagnoses among individuals with a history of PD was 1.4 times higher than among those with no PD history after adjustment for age and gender. It increased to 1.45 times higher when the researchers also adjusted for body mass index, education, income, diabetes, family history of CRC, regular use of aspirin and non-aspirin nonsteroidal anti-inflammatory drugs, and lifetime cumulative smoking, consumption of red and processed meats, alcohol consumption, and total physical activity score.
The findings were published online Jan. 26 in Cancer Causes and Control.
“Our results support the hypothesis of an association between PD and sporadic CRC risk,” the researchers said, adding that further epidemiologic studies are recommended.
They speculated that the “putative mechanism of PD and cancer association involves the spread of periodontal pathogens to extra-oral sites, dissemination of bacteria endotoxins, and release of inflammation products directly into the bloodstream.”
The chronic inflammation associated with PD “promotes carcinogenesis by induction of gene mutations, inhibition of apoptosis, stimulation of angiogenesis, cell proliferation, and epigenetic alterations,” they added.
The COLDENT study was supported by the Cancer Research Society. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
findings from the population-based case-control COLDENT study suggest.
The rate of new CRC diagnoses among individuals in the study who had a history of PD was nearly 50% higher than in those with no such history, after adjustment for a host of medical and demographic factors, the investigators noted.
This isn’t the first time PD has been linked with extra-oral health outcomes, including gastrointestinal cancers. It has been shown to be associated with several major systemic diseases, such as cardiovascular, respiratory, chronic kidney, and metabolic diseases. Evidence also suggests a link between PD and Alzheimer’s disease.
However, prior studies that looked at the connection between PD and CRC have relied on secondary analyses of data from other studies and are limited by other methodologic shortcomings, noted the researchers, led by Amal Idrissi Janati, DDS, University of Montreal.
To better assess the etiologic role of PD in the development of CRC, Dr. Janati and colleagues analyzed 348 histologically confirmed cases of colon or rectal cancer diagnosed from January 2013 to December 2019 and compared them to 310 matched controls.
The rate of new CRC diagnoses among individuals with a history of PD was 1.4 times higher than among those with no PD history after adjustment for age and gender. It increased to 1.45 times higher when the researchers also adjusted for body mass index, education, income, diabetes, family history of CRC, regular use of aspirin and non-aspirin nonsteroidal anti-inflammatory drugs, and lifetime cumulative smoking, consumption of red and processed meats, alcohol consumption, and total physical activity score.
The findings were published online Jan. 26 in Cancer Causes and Control.
“Our results support the hypothesis of an association between PD and sporadic CRC risk,” the researchers said, adding that further epidemiologic studies are recommended.
They speculated that the “putative mechanism of PD and cancer association involves the spread of periodontal pathogens to extra-oral sites, dissemination of bacteria endotoxins, and release of inflammation products directly into the bloodstream.”
The chronic inflammation associated with PD “promotes carcinogenesis by induction of gene mutations, inhibition of apoptosis, stimulation of angiogenesis, cell proliferation, and epigenetic alterations,” they added.
The COLDENT study was supported by the Cancer Research Society. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANCER CAUSES AND CONTROL
Biomarkers in saliva may detect hepatocellular carcinoma
MicroRNAs (miRNAs) that signal hepatocellular carcinoma (HCC), the most common type of liver cancer, have been detected in saliva for the first time, according to results from a pilot study.
The findings were published online in PeerJ.
The small, noncoding RNAs regulate many cellular functions and affect cancer development and progression.
The discovery has the potential to offer a noninvasive alternative or complement to available detection tools – ultrasound and the blood biomarker alpha fetoprotein (AFP) – which lack sensitivity, said Daniel Rotroff, PhD, MSPH, senior author of the study and a researcher in the Department of Quantitative Health Sciences at the Cleveland Clinic.
“Right now, the current clinical tools are not adequate,” he told this news organization. “They miss approximately 40% to 50% of the patients who have HCC.”
Scientists are interested in finding better ways to detect liver cancer, the rates of which are growing rapidly. HCC represents 80% of all liver cancers.
“HCC and liver cancer are the fastest growing cancers in the United States,” Dr. Rotroff said. “They are the fifth and seventh leading cause of cancer death in men and women, respectively.”
Driving the growth are increases in hepatitis C, obesity, fatty liver disease, and alcoholism.
Nancy Reau, MD, the Richard B. Capps Chair of Hepatology and section chief, Hepatology, at Rush Medical College, Chicago, who was not part of the study, told this news organization that despite the study’s being relatively small in scale, the preliminary information it provides is nonetheless “really attractive.”
If larger studies confirm the results, the discovery could open up the possibility of patients mailing in saliva samples from their homes to screen for liver cancer.
The pandemic, she noted, highlighted the shortcomings of ultrasound in screening for liver cancer, as it required patients to come into a facility.
“You’d love to have a biomarker that was more accessible and accurate,” she said. “It would have lots of applicability where cancer surveillance is less available.”
Dr. Rotroff added that “we do know saliva samples can be stable at room temperature. It opens up possibilities to expand the net of being able to screen a wider number of patients.”
Differentiating HCC from cirrhosis
Investigators at the Cleveland Clinic performed small RNA sequencing in 20 patients with HCC and compared the findings to sequencing of 19 patients with cirrhosis.
Liver cirrhosis is the primary risk factor for developing HCC, so distinguishing patients with HCC from this cohort of high-risk patients serves as a proof of principle.
The sequencing showed that 4,565 precursor and mature miRNAs were detected in saliva and that 365 were significantly different between those with HCC compared to cirrhosis (false discovery rate, P < .05).
“Interestingly, 283 of these miRNAs were significantly downregulated in patients with HCC,” the authors write.
Machine learning found a combination of 10 miRNAs and covariates that accurately classified patients with HCC (area under the curve = 0.87).
The researchers note that miRNAs have been found in saliva and have shown potential as noninvasive biomarkers for a number of other cancers, including breast, oral, and lung cancers.
Additionally, Dr. Rotroff said, microRNAs have been shown to be altered in the tumor tissue of HCC, compared with the surrounding tissue.
Catching cancer early
Dr. Reau noted that a strength of the study is that it validated the biomarker in a diverse group of patients already diagnosed with liver cancer, including people with early-stage cancer, those who underwent transplantation, and those with recurrent cancer.
“Everyone searching for biomarkers is looking to make sure that the surveillance tool identifies the patient when it can pay off with early treatment,” Dr. Reau said.
“You don’t want to identify cancer when it’s bad, and you don’t have any options.
This is a little bit where AFP sometimes fails. Even if ultrasound isn’t that accurate, it still generally identifies people when they fit within curative guidelines.”
Dr. Rotroff also stressed the importance of detecting the cancers early, noting that the prognosis for patients with HCC before it has metastasized is greater than 4 years, but the prognosis drops to less than 1 year if it has metastasized.
Dr. Rotroff has an equity stake in Clarified Precision Medicine. He holds intellectual property related to the detection of HCC. Dr. Reau reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MicroRNAs (miRNAs) that signal hepatocellular carcinoma (HCC), the most common type of liver cancer, have been detected in saliva for the first time, according to results from a pilot study.
The findings were published online in PeerJ.
The small, noncoding RNAs regulate many cellular functions and affect cancer development and progression.
The discovery has the potential to offer a noninvasive alternative or complement to available detection tools – ultrasound and the blood biomarker alpha fetoprotein (AFP) – which lack sensitivity, said Daniel Rotroff, PhD, MSPH, senior author of the study and a researcher in the Department of Quantitative Health Sciences at the Cleveland Clinic.
“Right now, the current clinical tools are not adequate,” he told this news organization. “They miss approximately 40% to 50% of the patients who have HCC.”
Scientists are interested in finding better ways to detect liver cancer, the rates of which are growing rapidly. HCC represents 80% of all liver cancers.
“HCC and liver cancer are the fastest growing cancers in the United States,” Dr. Rotroff said. “They are the fifth and seventh leading cause of cancer death in men and women, respectively.”
Driving the growth are increases in hepatitis C, obesity, fatty liver disease, and alcoholism.
Nancy Reau, MD, the Richard B. Capps Chair of Hepatology and section chief, Hepatology, at Rush Medical College, Chicago, who was not part of the study, told this news organization that despite the study’s being relatively small in scale, the preliminary information it provides is nonetheless “really attractive.”
If larger studies confirm the results, the discovery could open up the possibility of patients mailing in saliva samples from their homes to screen for liver cancer.
The pandemic, she noted, highlighted the shortcomings of ultrasound in screening for liver cancer, as it required patients to come into a facility.
“You’d love to have a biomarker that was more accessible and accurate,” she said. “It would have lots of applicability where cancer surveillance is less available.”
Dr. Rotroff added that “we do know saliva samples can be stable at room temperature. It opens up possibilities to expand the net of being able to screen a wider number of patients.”
Differentiating HCC from cirrhosis
Investigators at the Cleveland Clinic performed small RNA sequencing in 20 patients with HCC and compared the findings to sequencing of 19 patients with cirrhosis.
Liver cirrhosis is the primary risk factor for developing HCC, so distinguishing patients with HCC from this cohort of high-risk patients serves as a proof of principle.
The sequencing showed that 4,565 precursor and mature miRNAs were detected in saliva and that 365 were significantly different between those with HCC compared to cirrhosis (false discovery rate, P < .05).
“Interestingly, 283 of these miRNAs were significantly downregulated in patients with HCC,” the authors write.
Machine learning found a combination of 10 miRNAs and covariates that accurately classified patients with HCC (area under the curve = 0.87).
The researchers note that miRNAs have been found in saliva and have shown potential as noninvasive biomarkers for a number of other cancers, including breast, oral, and lung cancers.
Additionally, Dr. Rotroff said, microRNAs have been shown to be altered in the tumor tissue of HCC, compared with the surrounding tissue.
Catching cancer early
Dr. Reau noted that a strength of the study is that it validated the biomarker in a diverse group of patients already diagnosed with liver cancer, including people with early-stage cancer, those who underwent transplantation, and those with recurrent cancer.
“Everyone searching for biomarkers is looking to make sure that the surveillance tool identifies the patient when it can pay off with early treatment,” Dr. Reau said.
“You don’t want to identify cancer when it’s bad, and you don’t have any options.
This is a little bit where AFP sometimes fails. Even if ultrasound isn’t that accurate, it still generally identifies people when they fit within curative guidelines.”
Dr. Rotroff also stressed the importance of detecting the cancers early, noting that the prognosis for patients with HCC before it has metastasized is greater than 4 years, but the prognosis drops to less than 1 year if it has metastasized.
Dr. Rotroff has an equity stake in Clarified Precision Medicine. He holds intellectual property related to the detection of HCC. Dr. Reau reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MicroRNAs (miRNAs) that signal hepatocellular carcinoma (HCC), the most common type of liver cancer, have been detected in saliva for the first time, according to results from a pilot study.
The findings were published online in PeerJ.
The small, noncoding RNAs regulate many cellular functions and affect cancer development and progression.
The discovery has the potential to offer a noninvasive alternative or complement to available detection tools – ultrasound and the blood biomarker alpha fetoprotein (AFP) – which lack sensitivity, said Daniel Rotroff, PhD, MSPH, senior author of the study and a researcher in the Department of Quantitative Health Sciences at the Cleveland Clinic.
“Right now, the current clinical tools are not adequate,” he told this news organization. “They miss approximately 40% to 50% of the patients who have HCC.”
Scientists are interested in finding better ways to detect liver cancer, the rates of which are growing rapidly. HCC represents 80% of all liver cancers.
“HCC and liver cancer are the fastest growing cancers in the United States,” Dr. Rotroff said. “They are the fifth and seventh leading cause of cancer death in men and women, respectively.”
Driving the growth are increases in hepatitis C, obesity, fatty liver disease, and alcoholism.
Nancy Reau, MD, the Richard B. Capps Chair of Hepatology and section chief, Hepatology, at Rush Medical College, Chicago, who was not part of the study, told this news organization that despite the study’s being relatively small in scale, the preliminary information it provides is nonetheless “really attractive.”
If larger studies confirm the results, the discovery could open up the possibility of patients mailing in saliva samples from their homes to screen for liver cancer.
The pandemic, she noted, highlighted the shortcomings of ultrasound in screening for liver cancer, as it required patients to come into a facility.
“You’d love to have a biomarker that was more accessible and accurate,” she said. “It would have lots of applicability where cancer surveillance is less available.”
Dr. Rotroff added that “we do know saliva samples can be stable at room temperature. It opens up possibilities to expand the net of being able to screen a wider number of patients.”
Differentiating HCC from cirrhosis
Investigators at the Cleveland Clinic performed small RNA sequencing in 20 patients with HCC and compared the findings to sequencing of 19 patients with cirrhosis.
Liver cirrhosis is the primary risk factor for developing HCC, so distinguishing patients with HCC from this cohort of high-risk patients serves as a proof of principle.
The sequencing showed that 4,565 precursor and mature miRNAs were detected in saliva and that 365 were significantly different between those with HCC compared to cirrhosis (false discovery rate, P < .05).
“Interestingly, 283 of these miRNAs were significantly downregulated in patients with HCC,” the authors write.
Machine learning found a combination of 10 miRNAs and covariates that accurately classified patients with HCC (area under the curve = 0.87).
The researchers note that miRNAs have been found in saliva and have shown potential as noninvasive biomarkers for a number of other cancers, including breast, oral, and lung cancers.
Additionally, Dr. Rotroff said, microRNAs have been shown to be altered in the tumor tissue of HCC, compared with the surrounding tissue.
Catching cancer early
Dr. Reau noted that a strength of the study is that it validated the biomarker in a diverse group of patients already diagnosed with liver cancer, including people with early-stage cancer, those who underwent transplantation, and those with recurrent cancer.
“Everyone searching for biomarkers is looking to make sure that the surveillance tool identifies the patient when it can pay off with early treatment,” Dr. Reau said.
“You don’t want to identify cancer when it’s bad, and you don’t have any options.
This is a little bit where AFP sometimes fails. Even if ultrasound isn’t that accurate, it still generally identifies people when they fit within curative guidelines.”
Dr. Rotroff also stressed the importance of detecting the cancers early, noting that the prognosis for patients with HCC before it has metastasized is greater than 4 years, but the prognosis drops to less than 1 year if it has metastasized.
Dr. Rotroff has an equity stake in Clarified Precision Medicine. He holds intellectual property related to the detection of HCC. Dr. Reau reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Stopping venetoclax treatment early reduces CLL survival outcomes
“There’s not a lot of awareness about the fact that you’re probably better off not permanently discontinuing treatment,” Anthony R. Mato, first author of the research published in Haematologica, said in an interview.
“Instead, attempting dose reductions with later resumption to complete the planned schedule for treatment probably could improve outcomes,” said Dr. Mato, who is director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Venetoclax, a potent B-cell lymphoma-2 (BCL2) inhibitor, provides a novel, chemotherapy-free treatment option for first-line and r/r CLL. While its safety profile is manageable, treatment interruptions are very common, and premature discontinuations are reported in about a third of patients, often because of adverse events.
Lacking data on the effects of those interruptions on survival outcomes, Dr. Mato and colleagues conducted a post hoc analysis of the phase 3 MURANO trial. In this open-label study, treatment with six cycles of venetoclax in combination with rituximab followed by venetoclax once daily for a total of 2 years showed superior progression-free survival, compared with six cycles of bendamustine plus rituximab in patients with r/r CLL (P < .0001).
The current analysis involved 194 intention-to-treat patients from the trial’s venetoclax arm, among whom 140 (72%) completed 2 years of therapy, and 54 (28%) prematurely discontinued treatment. The most common reasons for discontinuation were adverse events (53.7%) and disease progression (22.2%).
Among those with early discontinuation for any reason except disease progression, the rate of progression-free survival was significantly inferior, compared with those who completed the treatment (hazard ratio, 5.98; P < .0001), as was the rate or discontinuation caused specifically by adverse events, which most commonly involved neutropenia or thrombocytopenia (HR, 5.82; P < .0001).
Those who discontinued had a mean duration of venetoclax therapy of 11.3 months, compared with 24.4 months for all patients. For each additional month of venetoclax therapy, there was a significantly lower risk of a progression-free survival event (P = .0263) and of an overall survival event (P < .0001).
The treatment interruption rate was much higher, at 69% (134), involving neutropenia in 43% (84) of instances and requiring dose reductions in 23% (45) of cases.
However, in contrast to permanent discontinuations, the temporary interruptions and dose reductions had no significant effect on progression-free or overall survival, regardless of the duration.
“Improved progression-free and overall survival were associated with greater cumulative venetoclax treatment exposure,” the authors wrote.
“The results of these analyses highlight the importance of appropriately managing treatment modifications to ensure optimal outcomes for patients receiving targeted treatment for CLL,” they said.
Key measures including “better supportive care, use of growth factors, and more aggressive strategies for dose reduction could potentially help to improve or decrease the number of patients discontinuing due to an adverse event,” Dr. Mato added.“We can’t say definitively because this is not a randomized study – it’s a retrospective analysis from a randomized study – but those measures likely could have a positive impact on patient outcomes.”
The study received support from Genentech and AbbVie. Dr. Mato reported consulting or other relationships with AbbVie, AstraZeneca, Celgene, DTRM, Genentech, Janssen, Loxo, PCYC, Sunesis, and TG Therapeutics.
“There’s not a lot of awareness about the fact that you’re probably better off not permanently discontinuing treatment,” Anthony R. Mato, first author of the research published in Haematologica, said in an interview.
“Instead, attempting dose reductions with later resumption to complete the planned schedule for treatment probably could improve outcomes,” said Dr. Mato, who is director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Venetoclax, a potent B-cell lymphoma-2 (BCL2) inhibitor, provides a novel, chemotherapy-free treatment option for first-line and r/r CLL. While its safety profile is manageable, treatment interruptions are very common, and premature discontinuations are reported in about a third of patients, often because of adverse events.
Lacking data on the effects of those interruptions on survival outcomes, Dr. Mato and colleagues conducted a post hoc analysis of the phase 3 MURANO trial. In this open-label study, treatment with six cycles of venetoclax in combination with rituximab followed by venetoclax once daily for a total of 2 years showed superior progression-free survival, compared with six cycles of bendamustine plus rituximab in patients with r/r CLL (P < .0001).
The current analysis involved 194 intention-to-treat patients from the trial’s venetoclax arm, among whom 140 (72%) completed 2 years of therapy, and 54 (28%) prematurely discontinued treatment. The most common reasons for discontinuation were adverse events (53.7%) and disease progression (22.2%).
Among those with early discontinuation for any reason except disease progression, the rate of progression-free survival was significantly inferior, compared with those who completed the treatment (hazard ratio, 5.98; P < .0001), as was the rate or discontinuation caused specifically by adverse events, which most commonly involved neutropenia or thrombocytopenia (HR, 5.82; P < .0001).
Those who discontinued had a mean duration of venetoclax therapy of 11.3 months, compared with 24.4 months for all patients. For each additional month of venetoclax therapy, there was a significantly lower risk of a progression-free survival event (P = .0263) and of an overall survival event (P < .0001).
The treatment interruption rate was much higher, at 69% (134), involving neutropenia in 43% (84) of instances and requiring dose reductions in 23% (45) of cases.
However, in contrast to permanent discontinuations, the temporary interruptions and dose reductions had no significant effect on progression-free or overall survival, regardless of the duration.
“Improved progression-free and overall survival were associated with greater cumulative venetoclax treatment exposure,” the authors wrote.
“The results of these analyses highlight the importance of appropriately managing treatment modifications to ensure optimal outcomes for patients receiving targeted treatment for CLL,” they said.
Key measures including “better supportive care, use of growth factors, and more aggressive strategies for dose reduction could potentially help to improve or decrease the number of patients discontinuing due to an adverse event,” Dr. Mato added.“We can’t say definitively because this is not a randomized study – it’s a retrospective analysis from a randomized study – but those measures likely could have a positive impact on patient outcomes.”
The study received support from Genentech and AbbVie. Dr. Mato reported consulting or other relationships with AbbVie, AstraZeneca, Celgene, DTRM, Genentech, Janssen, Loxo, PCYC, Sunesis, and TG Therapeutics.
“There’s not a lot of awareness about the fact that you’re probably better off not permanently discontinuing treatment,” Anthony R. Mato, first author of the research published in Haematologica, said in an interview.
“Instead, attempting dose reductions with later resumption to complete the planned schedule for treatment probably could improve outcomes,” said Dr. Mato, who is director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Venetoclax, a potent B-cell lymphoma-2 (BCL2) inhibitor, provides a novel, chemotherapy-free treatment option for first-line and r/r CLL. While its safety profile is manageable, treatment interruptions are very common, and premature discontinuations are reported in about a third of patients, often because of adverse events.
Lacking data on the effects of those interruptions on survival outcomes, Dr. Mato and colleagues conducted a post hoc analysis of the phase 3 MURANO trial. In this open-label study, treatment with six cycles of venetoclax in combination with rituximab followed by venetoclax once daily for a total of 2 years showed superior progression-free survival, compared with six cycles of bendamustine plus rituximab in patients with r/r CLL (P < .0001).
The current analysis involved 194 intention-to-treat patients from the trial’s venetoclax arm, among whom 140 (72%) completed 2 years of therapy, and 54 (28%) prematurely discontinued treatment. The most common reasons for discontinuation were adverse events (53.7%) and disease progression (22.2%).
Among those with early discontinuation for any reason except disease progression, the rate of progression-free survival was significantly inferior, compared with those who completed the treatment (hazard ratio, 5.98; P < .0001), as was the rate or discontinuation caused specifically by adverse events, which most commonly involved neutropenia or thrombocytopenia (HR, 5.82; P < .0001).
Those who discontinued had a mean duration of venetoclax therapy of 11.3 months, compared with 24.4 months for all patients. For each additional month of venetoclax therapy, there was a significantly lower risk of a progression-free survival event (P = .0263) and of an overall survival event (P < .0001).
The treatment interruption rate was much higher, at 69% (134), involving neutropenia in 43% (84) of instances and requiring dose reductions in 23% (45) of cases.
However, in contrast to permanent discontinuations, the temporary interruptions and dose reductions had no significant effect on progression-free or overall survival, regardless of the duration.
“Improved progression-free and overall survival were associated with greater cumulative venetoclax treatment exposure,” the authors wrote.
“The results of these analyses highlight the importance of appropriately managing treatment modifications to ensure optimal outcomes for patients receiving targeted treatment for CLL,” they said.
Key measures including “better supportive care, use of growth factors, and more aggressive strategies for dose reduction could potentially help to improve or decrease the number of patients discontinuing due to an adverse event,” Dr. Mato added.“We can’t say definitively because this is not a randomized study – it’s a retrospective analysis from a randomized study – but those measures likely could have a positive impact on patient outcomes.”
The study received support from Genentech and AbbVie. Dr. Mato reported consulting or other relationships with AbbVie, AstraZeneca, Celgene, DTRM, Genentech, Janssen, Loxo, PCYC, Sunesis, and TG Therapeutics.
Primer message boosts colorectal cancer screening rates
Researchers have found a simple, low-cost way to get more adults to complete a fecal immunochemical test (FIT) to screen for colorectal cancer (CRC).
In a randomized controlled trial, patients who received an electronic “primer” message through their patient portal before the test kit arrived in their mailbox were more apt to complete and return the test than peers who didn’t get the electronic message.
“We were thrilled by the magnitude of the impact,” Gregory Goshgarian, MSc, MPH, and Daniel Croymans, MD, with the department of medicine, David Geffen School of Medicine, University of California, Los Angeles, said in a joint email to this news organization.
At UCLA Health, “including a primer patient portal message is now standard practice for our FIT mailer program,” they added.
Their study was published online Feb. 4 in JAMA Network Open.
Heads-up message boosts compliance
CRC screening rates in the United States remain well below the national benchmark of 80%, and COVID-19 hasn’t helped. As a result, multiple medical and professional societies have emphasized the use of a mailed FIT outreach program.
As part of the outreach program, researchers at UCLA Health developed an electronic primer message within the electronic patient portal to alert patients due for CRC screening that they would be receiving a FIT kit in the mail.
They tested the impact of the primer messages in a randomized controlled trial involving 2,339 adults (mean age, 59 years, 57.5% women). Out of these, 1,157 received the standard mailed FIT kit (control group) and 1,182 received the standard mailed FIT kit plus a primer message sent through their personal patient portal.
Adding the primer message significantly increased the FIT completion rate at 6 months by 5.5%, with rates of 37.6% in the intervention group versus 32.1% in the control group.
After adjusting for patient demographics, the primer (versus no primer) led to significantly increased odds of completing CRC screening (adjusted odds ratio: 1.29; 95% confidence interval, 1.08-1.53; P = .004).
The primer message also shortened the time to FIT screening by 3 days (35 days with the primer vs. 38 days without).
Dr. Goshgarian and Dr. Croymans believe the priming messages worked well in their patient population because at the beginning of the intervention they identified a potential lack of awareness of the incoming FIT kit mailer as a barrier to uptake.
“We believe patients were receiving the kits with minimal advanced warning and discarding it as a mistake or hesitant to complete it because they did not understand the value to them,” they told this news organization.
“Therefore, a priming message helped to bridge that gap and allowed patients to be aware of the incoming FIT kits, know why it was important to do the FIT kit, and ultimately led to increasing our FIT kit return rates and thus CRC screening,” they said.
The researchers caution that their findings may be more relevant to patient populations who are more engaged in their health or who are more technologically savvy. In the UCLA Health system, roughly 84% of patients have an activated patient portal.
‘Good enhancement’ for health care systems
Reached for comment, Aasma Shaukat, MD, MPH, professor of medicine, NYU Langone Health, and first author of the American College of Gastroenterology (ACG) 2021 CRC screening guidelines, said the results are “interesting but not entirely surprising.”
“There’s literature supporting that a letter or notification prior to the FIT being mailed improves its uptake. Here, the authors applied it to their health care system in a quality improvement study and demonstrated it works,” Dr. Shaukat said.
“This is a good enhancement for health care systems where most of their patients are using or accessing their health chart portal,” added Dr. Shaukat.
“Caveats are that the generalizability is not known. It requires EHR [electronic health record] support tools and patients with access to a computer and enrolled and able to access their electronic chart, likely those with high literacy and English speaking.”
Funding for the study was provided by the UCLA Health Department of Medicine. Dr. Goshgarian, Dr. Croymans, and Dr. Shaukat have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have found a simple, low-cost way to get more adults to complete a fecal immunochemical test (FIT) to screen for colorectal cancer (CRC).
In a randomized controlled trial, patients who received an electronic “primer” message through their patient portal before the test kit arrived in their mailbox were more apt to complete and return the test than peers who didn’t get the electronic message.
“We were thrilled by the magnitude of the impact,” Gregory Goshgarian, MSc, MPH, and Daniel Croymans, MD, with the department of medicine, David Geffen School of Medicine, University of California, Los Angeles, said in a joint email to this news organization.
At UCLA Health, “including a primer patient portal message is now standard practice for our FIT mailer program,” they added.
Their study was published online Feb. 4 in JAMA Network Open.
Heads-up message boosts compliance
CRC screening rates in the United States remain well below the national benchmark of 80%, and COVID-19 hasn’t helped. As a result, multiple medical and professional societies have emphasized the use of a mailed FIT outreach program.
As part of the outreach program, researchers at UCLA Health developed an electronic primer message within the electronic patient portal to alert patients due for CRC screening that they would be receiving a FIT kit in the mail.
They tested the impact of the primer messages in a randomized controlled trial involving 2,339 adults (mean age, 59 years, 57.5% women). Out of these, 1,157 received the standard mailed FIT kit (control group) and 1,182 received the standard mailed FIT kit plus a primer message sent through their personal patient portal.
Adding the primer message significantly increased the FIT completion rate at 6 months by 5.5%, with rates of 37.6% in the intervention group versus 32.1% in the control group.
After adjusting for patient demographics, the primer (versus no primer) led to significantly increased odds of completing CRC screening (adjusted odds ratio: 1.29; 95% confidence interval, 1.08-1.53; P = .004).
The primer message also shortened the time to FIT screening by 3 days (35 days with the primer vs. 38 days without).
Dr. Goshgarian and Dr. Croymans believe the priming messages worked well in their patient population because at the beginning of the intervention they identified a potential lack of awareness of the incoming FIT kit mailer as a barrier to uptake.
“We believe patients were receiving the kits with minimal advanced warning and discarding it as a mistake or hesitant to complete it because they did not understand the value to them,” they told this news organization.
“Therefore, a priming message helped to bridge that gap and allowed patients to be aware of the incoming FIT kits, know why it was important to do the FIT kit, and ultimately led to increasing our FIT kit return rates and thus CRC screening,” they said.
The researchers caution that their findings may be more relevant to patient populations who are more engaged in their health or who are more technologically savvy. In the UCLA Health system, roughly 84% of patients have an activated patient portal.
‘Good enhancement’ for health care systems
Reached for comment, Aasma Shaukat, MD, MPH, professor of medicine, NYU Langone Health, and first author of the American College of Gastroenterology (ACG) 2021 CRC screening guidelines, said the results are “interesting but not entirely surprising.”
“There’s literature supporting that a letter or notification prior to the FIT being mailed improves its uptake. Here, the authors applied it to their health care system in a quality improvement study and demonstrated it works,” Dr. Shaukat said.
“This is a good enhancement for health care systems where most of their patients are using or accessing their health chart portal,” added Dr. Shaukat.
“Caveats are that the generalizability is not known. It requires EHR [electronic health record] support tools and patients with access to a computer and enrolled and able to access their electronic chart, likely those with high literacy and English speaking.”
Funding for the study was provided by the UCLA Health Department of Medicine. Dr. Goshgarian, Dr. Croymans, and Dr. Shaukat have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have found a simple, low-cost way to get more adults to complete a fecal immunochemical test (FIT) to screen for colorectal cancer (CRC).
In a randomized controlled trial, patients who received an electronic “primer” message through their patient portal before the test kit arrived in their mailbox were more apt to complete and return the test than peers who didn’t get the electronic message.
“We were thrilled by the magnitude of the impact,” Gregory Goshgarian, MSc, MPH, and Daniel Croymans, MD, with the department of medicine, David Geffen School of Medicine, University of California, Los Angeles, said in a joint email to this news organization.
At UCLA Health, “including a primer patient portal message is now standard practice for our FIT mailer program,” they added.
Their study was published online Feb. 4 in JAMA Network Open.
Heads-up message boosts compliance
CRC screening rates in the United States remain well below the national benchmark of 80%, and COVID-19 hasn’t helped. As a result, multiple medical and professional societies have emphasized the use of a mailed FIT outreach program.
As part of the outreach program, researchers at UCLA Health developed an electronic primer message within the electronic patient portal to alert patients due for CRC screening that they would be receiving a FIT kit in the mail.
They tested the impact of the primer messages in a randomized controlled trial involving 2,339 adults (mean age, 59 years, 57.5% women). Out of these, 1,157 received the standard mailed FIT kit (control group) and 1,182 received the standard mailed FIT kit plus a primer message sent through their personal patient portal.
Adding the primer message significantly increased the FIT completion rate at 6 months by 5.5%, with rates of 37.6% in the intervention group versus 32.1% in the control group.
After adjusting for patient demographics, the primer (versus no primer) led to significantly increased odds of completing CRC screening (adjusted odds ratio: 1.29; 95% confidence interval, 1.08-1.53; P = .004).
The primer message also shortened the time to FIT screening by 3 days (35 days with the primer vs. 38 days without).
Dr. Goshgarian and Dr. Croymans believe the priming messages worked well in their patient population because at the beginning of the intervention they identified a potential lack of awareness of the incoming FIT kit mailer as a barrier to uptake.
“We believe patients were receiving the kits with minimal advanced warning and discarding it as a mistake or hesitant to complete it because they did not understand the value to them,” they told this news organization.
“Therefore, a priming message helped to bridge that gap and allowed patients to be aware of the incoming FIT kits, know why it was important to do the FIT kit, and ultimately led to increasing our FIT kit return rates and thus CRC screening,” they said.
The researchers caution that their findings may be more relevant to patient populations who are more engaged in their health or who are more technologically savvy. In the UCLA Health system, roughly 84% of patients have an activated patient portal.
‘Good enhancement’ for health care systems
Reached for comment, Aasma Shaukat, MD, MPH, professor of medicine, NYU Langone Health, and first author of the American College of Gastroenterology (ACG) 2021 CRC screening guidelines, said the results are “interesting but not entirely surprising.”
“There’s literature supporting that a letter or notification prior to the FIT being mailed improves its uptake. Here, the authors applied it to their health care system in a quality improvement study and demonstrated it works,” Dr. Shaukat said.
“This is a good enhancement for health care systems where most of their patients are using or accessing their health chart portal,” added Dr. Shaukat.
“Caveats are that the generalizability is not known. It requires EHR [electronic health record] support tools and patients with access to a computer and enrolled and able to access their electronic chart, likely those with high literacy and English speaking.”
Funding for the study was provided by the UCLA Health Department of Medicine. Dr. Goshgarian, Dr. Croymans, and Dr. Shaukat have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Alleviating chemo-related nausea is a huge unmet need
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
This is Mark Kris from chilly New York and Memorial Sloan Kettering. Today I want to talk about a recent article in the Journal of Clinical Oncology that reported a study of a new neurokinin-1 antagonist called fosnetupitant. This was a well-conducted trial that demonstrates the noninferiority of IV fosnetupitant when compared with IV fosaprepitant. By their study criteria, fosnetupitant was not inferior.
But my reason for discussing this is that the paper and the trial miss the point for the field right now. Although the authors talk about the prevention of nausea and vomiting in the introduction, in the paper itself and in the abstract results section, there’s not a single mention about the medication’s ability to control nausea, which is the critical issue for our patients today. You have to go into the supplementary data to find it mentioned, and what you find is that the prevention of nausea is 50% for both the control and this new drug. We control nausea in only half of the patients who receive cisplatin in 2022. That is a huge issue.
When you ask patients what are the effects of cancer treatment that they fear most, that concerns them most, it’s nausea and emesis; indeed, nausea has replaced emesis as the biggest concern. And although this trial used emesis as the main endpoint, and it was useful in defining the drug, it was not useful in coming up with a new treatment that addresses a huge need. Further, the authors talk about an advantage to fosnetupitant based on infusion reactions, but it is a difference of 0.3% vs. 3%. They talk about that sort of thing in the abstract and in the discussion section but don’t include nausea as part of the key endpoint of this trial. Again, you had to dig deeply to find out that, frankly, fosnetupitant was no better than the drugs we already have.
The other concerning point is that we do have another drug that works well. If you go to the American Society of Clinical Oncology or National Comprehensive Cancer Network guidelines for patients receiving high dosages of cisplatin, you find a four-drug regimen, including olanzapine, and that was not used here. Why is olanzapine so critical? It’s an available drug, it’s an inexpensive drug, it’s a safe drug, and it improves nausea by 15%.
So they did this huge trial to show noninferiority, and they neglected to give a drug that could deal with the most serious side effect of cancer therapy – nausea – and improve things by 15%.
A challenge to people in this field: We have to do better. Nausea is a big problem. While noninferiority trials can be helpful for drug development, they’re not really helpful for the field. With a problem of this magnitude, we need better drugs to control nausea. In the meantime, I urge you all to follow the guidelines for high doses of cisplatin. Please use the four-drug regimen that is recommended in the guidelines and widely used in the United States. Going forward, make sure that when we expend huge amounts of energy to develop new agents and report them in our medical journals, that we look for ways to advance care where there are significant gaps in our ability to deliver what we want. Delivering better control of nausea is something we all need to be committed to. It’s a huge unmet need, and I hope future trials will address that need. Our patients will be better for it and we’ll be better in that we’re delivering what patients deserve, what they need, and what they ask for.
Mark G. Kris, MD, is chief of the thoracic oncology service and the William and Joy Ruane Chair in Thoracic Oncology at Memorial Sloan Kettering Cancer Center in New York City. He reported serving as a director, officer, partner, employee, adviser, consultant, or trustee for AstraZeneca, Roche/Genentech, and Ariad Pharmaceuticals, and has received research grants from Pfizer, PUMA, and Roche/Genentech.
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
This is Mark Kris from chilly New York and Memorial Sloan Kettering. Today I want to talk about a recent article in the Journal of Clinical Oncology that reported a study of a new neurokinin-1 antagonist called fosnetupitant. This was a well-conducted trial that demonstrates the noninferiority of IV fosnetupitant when compared with IV fosaprepitant. By their study criteria, fosnetupitant was not inferior.
But my reason for discussing this is that the paper and the trial miss the point for the field right now. Although the authors talk about the prevention of nausea and vomiting in the introduction, in the paper itself and in the abstract results section, there’s not a single mention about the medication’s ability to control nausea, which is the critical issue for our patients today. You have to go into the supplementary data to find it mentioned, and what you find is that the prevention of nausea is 50% for both the control and this new drug. We control nausea in only half of the patients who receive cisplatin in 2022. That is a huge issue.
When you ask patients what are the effects of cancer treatment that they fear most, that concerns them most, it’s nausea and emesis; indeed, nausea has replaced emesis as the biggest concern. And although this trial used emesis as the main endpoint, and it was useful in defining the drug, it was not useful in coming up with a new treatment that addresses a huge need. Further, the authors talk about an advantage to fosnetupitant based on infusion reactions, but it is a difference of 0.3% vs. 3%. They talk about that sort of thing in the abstract and in the discussion section but don’t include nausea as part of the key endpoint of this trial. Again, you had to dig deeply to find out that, frankly, fosnetupitant was no better than the drugs we already have.
The other concerning point is that we do have another drug that works well. If you go to the American Society of Clinical Oncology or National Comprehensive Cancer Network guidelines for patients receiving high dosages of cisplatin, you find a four-drug regimen, including olanzapine, and that was not used here. Why is olanzapine so critical? It’s an available drug, it’s an inexpensive drug, it’s a safe drug, and it improves nausea by 15%.
So they did this huge trial to show noninferiority, and they neglected to give a drug that could deal with the most serious side effect of cancer therapy – nausea – and improve things by 15%.
A challenge to people in this field: We have to do better. Nausea is a big problem. While noninferiority trials can be helpful for drug development, they’re not really helpful for the field. With a problem of this magnitude, we need better drugs to control nausea. In the meantime, I urge you all to follow the guidelines for high doses of cisplatin. Please use the four-drug regimen that is recommended in the guidelines and widely used in the United States. Going forward, make sure that when we expend huge amounts of energy to develop new agents and report them in our medical journals, that we look for ways to advance care where there are significant gaps in our ability to deliver what we want. Delivering better control of nausea is something we all need to be committed to. It’s a huge unmet need, and I hope future trials will address that need. Our patients will be better for it and we’ll be better in that we’re delivering what patients deserve, what they need, and what they ask for.
Mark G. Kris, MD, is chief of the thoracic oncology service and the William and Joy Ruane Chair in Thoracic Oncology at Memorial Sloan Kettering Cancer Center in New York City. He reported serving as a director, officer, partner, employee, adviser, consultant, or trustee for AstraZeneca, Roche/Genentech, and Ariad Pharmaceuticals, and has received research grants from Pfizer, PUMA, and Roche/Genentech.
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
This is Mark Kris from chilly New York and Memorial Sloan Kettering. Today I want to talk about a recent article in the Journal of Clinical Oncology that reported a study of a new neurokinin-1 antagonist called fosnetupitant. This was a well-conducted trial that demonstrates the noninferiority of IV fosnetupitant when compared with IV fosaprepitant. By their study criteria, fosnetupitant was not inferior.
But my reason for discussing this is that the paper and the trial miss the point for the field right now. Although the authors talk about the prevention of nausea and vomiting in the introduction, in the paper itself and in the abstract results section, there’s not a single mention about the medication’s ability to control nausea, which is the critical issue for our patients today. You have to go into the supplementary data to find it mentioned, and what you find is that the prevention of nausea is 50% for both the control and this new drug. We control nausea in only half of the patients who receive cisplatin in 2022. That is a huge issue.
When you ask patients what are the effects of cancer treatment that they fear most, that concerns them most, it’s nausea and emesis; indeed, nausea has replaced emesis as the biggest concern. And although this trial used emesis as the main endpoint, and it was useful in defining the drug, it was not useful in coming up with a new treatment that addresses a huge need. Further, the authors talk about an advantage to fosnetupitant based on infusion reactions, but it is a difference of 0.3% vs. 3%. They talk about that sort of thing in the abstract and in the discussion section but don’t include nausea as part of the key endpoint of this trial. Again, you had to dig deeply to find out that, frankly, fosnetupitant was no better than the drugs we already have.
The other concerning point is that we do have another drug that works well. If you go to the American Society of Clinical Oncology or National Comprehensive Cancer Network guidelines for patients receiving high dosages of cisplatin, you find a four-drug regimen, including olanzapine, and that was not used here. Why is olanzapine so critical? It’s an available drug, it’s an inexpensive drug, it’s a safe drug, and it improves nausea by 15%.
So they did this huge trial to show noninferiority, and they neglected to give a drug that could deal with the most serious side effect of cancer therapy – nausea – and improve things by 15%.
A challenge to people in this field: We have to do better. Nausea is a big problem. While noninferiority trials can be helpful for drug development, they’re not really helpful for the field. With a problem of this magnitude, we need better drugs to control nausea. In the meantime, I urge you all to follow the guidelines for high doses of cisplatin. Please use the four-drug regimen that is recommended in the guidelines and widely used in the United States. Going forward, make sure that when we expend huge amounts of energy to develop new agents and report them in our medical journals, that we look for ways to advance care where there are significant gaps in our ability to deliver what we want. Delivering better control of nausea is something we all need to be committed to. It’s a huge unmet need, and I hope future trials will address that need. Our patients will be better for it and we’ll be better in that we’re delivering what patients deserve, what they need, and what they ask for.
Mark G. Kris, MD, is chief of the thoracic oncology service and the William and Joy Ruane Chair in Thoracic Oncology at Memorial Sloan Kettering Cancer Center in New York City. He reported serving as a director, officer, partner, employee, adviser, consultant, or trustee for AstraZeneca, Roche/Genentech, and Ariad Pharmaceuticals, and has received research grants from Pfizer, PUMA, and Roche/Genentech.
“I didn’t want to meet you.” Dispelling myths about palliative care
The names of health care professionals and patients cited within the dialogue text have been changed to protect their privacy.
but over the years I have come to realize that she was right – most people, including many within health care, don’t have a good appreciation of what palliative care is or how it can help patients and health care teams.
A recent national survey about cancer-related health information found that of more than 1,000 surveyed Americans, less than 30% professed any knowledge of palliative care. Of those who had some knowledge of palliative care, around 30% believed palliative care was synonymous with hospice.1 Another 15% believed that a patient would have to give up cancer-directed treatments to receive palliative care.1
It’s not giving up
This persistent belief that palliative care is equivalent to hospice, or is tantamount to “giving up,” is one of the most commonly held myths I encounter in everyday practice.
I knock on the exam door and walk in.
A small, trim woman in her late 50s is sitting in a chair, arms folded across her chest, face drawn in.
“Hi,” I start. “I’m Sarah, the palliative care nurse practitioner who works in this clinic. I work closely with Dr. Smith.”
Dr. Smith is the patient’s oncologist.
“I really didn’t want to meet you,” she says in a quiet voice, her eyes large with concern.
I don’t take it personally. Few patients really want to be in the position of needing to meet the palliative care team.
“I looked up palliative care on Google and saw the word hospice.”
“Yeah,” I say. “I hear that a lot. Well, I can reassure you that this isn’t hospice.
In this clinic, our focus is on your cancer symptoms, your treatment side effects, and your quality of life.”
She looks visibly relieved. “Quality of life,” she echoes. “I need more of that.”
“OK,” I say. “So, tell me what you’re struggling with the most right now.”
That’s how many palliative care visits start. I actually prefer if patients haven’t heard of palliative care because it allows me to frame it for them, rather than having to start by addressing a myth or a prior negative experience. Even when patients haven’t had a negative experience with palliative care per se, typically, if they’ve interacted with palliative care in the past, it’s usually because someone they loved died in a hospital setting and it is the memory of that terrible loss that becomes synonymous with their recollection of palliative care.
Many patients I meet have never seen another outpatient palliative care practitioner – and this makes sense – we are still too few and far between. Most established palliative care teams are hospital based and many patients seen in the community do not have easy access to palliative care teams where they receive oncologic care.2 As an embedded practitioner, I see patients in the same exam rooms and infusion centers where they receive their cancer therapies, so I’m effectively woven into the fabric of their oncology experience. Just being there in the cancer center allows me to be in the right place at the right time for the right patients and their care teams.
More than pain management
Another myth I tend to dispel a lot is that palliative care is just a euphemism for “pain management.” I have seen this less lately, but still occasionally in the chart I’ll see documented in a note, “patient is seeing palliative/pain management,” when a patient is seeing me or one of my colleagues. Unfortunately, when providers have limited or outdated views of what palliative care is or the value it brings to patient-centered cancer care, referrals to palliative care tend to be delayed.3
“I really think Ms. Lopez could benefit from seeing palliative care,” an oncology nurse practitioner says to an oncologist.
I’m standing nearby, about to see another patient in one of the exam rooms in our clinic.
“But I don’t think she’s ready. And besides, she doesn’t have any pain,” he says.
He turns to me quizzically. “What do you think?”
“Tell me about the patient,” I ask, taking a few steps in their direction.
“Well, she’s a 64-year-old woman with metastatic cancer.
She has a really poor appetite and is losing some weight.
Seems a bit down, kind of pessimistic about things.
Her scan showed some new growth, so guess I’m not surprised by that.”
“I might be able to help her with the appetite and the mood changes.
I can at least talk with her and see where she’s at,” I offer.
“Alright,” he says. “We’ll put the palliative referral in.”
He hesitates. “But are you sure you want to see her?
She doesn’t have any pain.” He sounds skeptical.
“Yeah, I mean, it sounds like she has symptoms that are bothering her, so I’d be happy to see her. She sounds completely appropriate for palliative care.”
I hear this assumption a lot – that palliative care is somehow equivalent to pain management and that unless a patient’s pain is severe, it’s not worth referring the patient to palliative care. Don’t get me wrong – we do a lot of pain management, but at its heart, palliative care is an interdisciplinary specialty focused on improving or maintaining quality of life for people with serious illness. Because the goal is so broad, care can take many shapes.4
In addition to pain, palliative care clinicians commonly treat nausea, shortness of breath, constipation or diarrhea, poor appetite, fatigue, anxiety, depression, and insomnia.
Palliative care is more than medical or nursing care
A related misconception about palliative care held by many lay people and health care workers alike is that palliative care is primarily medical or nursing care focused mostly on alleviating physical symptoms such as pain or nausea. This couldn’t be further from the truth.
We’ve been talking for a while.
Ms. Lopez tells me about her struggles to maintain her weight while undergoing chemotherapy. She has low-grade nausea that is impacting her ability and desire to eat more and didn’t think that her weight loss was severe enough to warrant taking medication.
We talk about how she may be able to use antinausea medication sparingly to alleviate nausea while also limiting side effects from the medications—which was a big concern for her.
I ask her what else is bothering her.
She tells me that she has always been a strong Catholic and even when life has gotten tough, her faith was never shaken – until now.
She is struggling to understand why she ended up with metastatic cancer at such a relatively young age—why would God do this to her?
She had plans for retirement that have since evaporated in the face of a foreshortened life.
Why did this happen to her of all people? She was completely healthy until her diagnosis.
Her face is wet with tears.
We talk a little about how a diagnosis like this can change so much of a person’s life and identity. I try to validate her experience. She’s clearly suffering from a sense that her life is not what she expected, and she is struggling to integrate how her future looks at this point.
I ask her what conversations with her priest have been like.
At this point you may be wondering where this conversation is going. Why are we talking about Ms. Lopez’s religion? Palliative care is best delivered through high functioning interdisciplinary teams that can include other supportive people in a patient’s life. We work in concert to try to bring comfort to a patient and their family.4 That support network can include nurses, physicians, social workers, and chaplains. In this case, Ms. Lopez had not yet reached out to her priest. She hasn’t had the time or energy to contact her priest given her symptoms.
“Can I contact your priest for you?
Maybe he can visit or call and chat with you?”
She nods and wipes tears away.
“That would be really nice,” she says. “I’d love it if he could pray with me.”
A few hours after the visit, I call Ms. Lopez’s priest.
I ask him to reach out to her and about her request for prayer.
He says he’s been thinking about her and that her presence has been missed at weekly Mass. He thanks me for the call and says he’ll call her tomorrow.
I say my own small prayer for Ms. Lopez and head home, the day’s work completed.
Sarah D'Ambruoso was born and raised in Maine. She completed her undergraduate and graduate nursing education at New York University and UCLA, respectively, and currently works as a palliative care nurse practitioner in an oncology clinic in Los Angeles.
References
1. Cheng BT et al. Patterns of palliative care beliefs among adults in the U.S.: Analysis of a National Cancer Database. J Pain Symptom Manage. 2019 Aug 10. doi: 10.1016/j.jpainsymman.2019.07.030.
2. Finlay E et al. Filling the gap: Creating an outpatient palliative care program in your institution. Am Soc Clin Oncol Educ Book. 2018 May 23. doi: 10.1200/EDBK_200775.
3. Von Roenn JH et al. Barriers and approaches to the successful integration of palliative care and oncology practice. J Natl Compr Canc Netw. 2013 Mar. doi: 10.6004/jnccn.2013.0209.
4. Ferrell BR et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2016 Oct 31. doi: 10.1200/JCO.2016.70.1474.
The names of health care professionals and patients cited within the dialogue text have been changed to protect their privacy.
but over the years I have come to realize that she was right – most people, including many within health care, don’t have a good appreciation of what palliative care is or how it can help patients and health care teams.
A recent national survey about cancer-related health information found that of more than 1,000 surveyed Americans, less than 30% professed any knowledge of palliative care. Of those who had some knowledge of palliative care, around 30% believed palliative care was synonymous with hospice.1 Another 15% believed that a patient would have to give up cancer-directed treatments to receive palliative care.1
It’s not giving up
This persistent belief that palliative care is equivalent to hospice, or is tantamount to “giving up,” is one of the most commonly held myths I encounter in everyday practice.
I knock on the exam door and walk in.
A small, trim woman in her late 50s is sitting in a chair, arms folded across her chest, face drawn in.
“Hi,” I start. “I’m Sarah, the palliative care nurse practitioner who works in this clinic. I work closely with Dr. Smith.”
Dr. Smith is the patient’s oncologist.
“I really didn’t want to meet you,” she says in a quiet voice, her eyes large with concern.
I don’t take it personally. Few patients really want to be in the position of needing to meet the palliative care team.
“I looked up palliative care on Google and saw the word hospice.”
“Yeah,” I say. “I hear that a lot. Well, I can reassure you that this isn’t hospice.
In this clinic, our focus is on your cancer symptoms, your treatment side effects, and your quality of life.”
She looks visibly relieved. “Quality of life,” she echoes. “I need more of that.”
“OK,” I say. “So, tell me what you’re struggling with the most right now.”
That’s how many palliative care visits start. I actually prefer if patients haven’t heard of palliative care because it allows me to frame it for them, rather than having to start by addressing a myth or a prior negative experience. Even when patients haven’t had a negative experience with palliative care per se, typically, if they’ve interacted with palliative care in the past, it’s usually because someone they loved died in a hospital setting and it is the memory of that terrible loss that becomes synonymous with their recollection of palliative care.
Many patients I meet have never seen another outpatient palliative care practitioner – and this makes sense – we are still too few and far between. Most established palliative care teams are hospital based and many patients seen in the community do not have easy access to palliative care teams where they receive oncologic care.2 As an embedded practitioner, I see patients in the same exam rooms and infusion centers where they receive their cancer therapies, so I’m effectively woven into the fabric of their oncology experience. Just being there in the cancer center allows me to be in the right place at the right time for the right patients and their care teams.
More than pain management
Another myth I tend to dispel a lot is that palliative care is just a euphemism for “pain management.” I have seen this less lately, but still occasionally in the chart I’ll see documented in a note, “patient is seeing palliative/pain management,” when a patient is seeing me or one of my colleagues. Unfortunately, when providers have limited or outdated views of what palliative care is or the value it brings to patient-centered cancer care, referrals to palliative care tend to be delayed.3
“I really think Ms. Lopez could benefit from seeing palliative care,” an oncology nurse practitioner says to an oncologist.
I’m standing nearby, about to see another patient in one of the exam rooms in our clinic.
“But I don’t think she’s ready. And besides, she doesn’t have any pain,” he says.
He turns to me quizzically. “What do you think?”
“Tell me about the patient,” I ask, taking a few steps in their direction.
“Well, she’s a 64-year-old woman with metastatic cancer.
She has a really poor appetite and is losing some weight.
Seems a bit down, kind of pessimistic about things.
Her scan showed some new growth, so guess I’m not surprised by that.”
“I might be able to help her with the appetite and the mood changes.
I can at least talk with her and see where she’s at,” I offer.
“Alright,” he says. “We’ll put the palliative referral in.”
He hesitates. “But are you sure you want to see her?
She doesn’t have any pain.” He sounds skeptical.
“Yeah, I mean, it sounds like she has symptoms that are bothering her, so I’d be happy to see her. She sounds completely appropriate for palliative care.”
I hear this assumption a lot – that palliative care is somehow equivalent to pain management and that unless a patient’s pain is severe, it’s not worth referring the patient to palliative care. Don’t get me wrong – we do a lot of pain management, but at its heart, palliative care is an interdisciplinary specialty focused on improving or maintaining quality of life for people with serious illness. Because the goal is so broad, care can take many shapes.4
In addition to pain, palliative care clinicians commonly treat nausea, shortness of breath, constipation or diarrhea, poor appetite, fatigue, anxiety, depression, and insomnia.
Palliative care is more than medical or nursing care
A related misconception about palliative care held by many lay people and health care workers alike is that palliative care is primarily medical or nursing care focused mostly on alleviating physical symptoms such as pain or nausea. This couldn’t be further from the truth.
We’ve been talking for a while.
Ms. Lopez tells me about her struggles to maintain her weight while undergoing chemotherapy. She has low-grade nausea that is impacting her ability and desire to eat more and didn’t think that her weight loss was severe enough to warrant taking medication.
We talk about how she may be able to use antinausea medication sparingly to alleviate nausea while also limiting side effects from the medications—which was a big concern for her.
I ask her what else is bothering her.
She tells me that she has always been a strong Catholic and even when life has gotten tough, her faith was never shaken – until now.
She is struggling to understand why she ended up with metastatic cancer at such a relatively young age—why would God do this to her?
She had plans for retirement that have since evaporated in the face of a foreshortened life.
Why did this happen to her of all people? She was completely healthy until her diagnosis.
Her face is wet with tears.
We talk a little about how a diagnosis like this can change so much of a person’s life and identity. I try to validate her experience. She’s clearly suffering from a sense that her life is not what she expected, and she is struggling to integrate how her future looks at this point.
I ask her what conversations with her priest have been like.
At this point you may be wondering where this conversation is going. Why are we talking about Ms. Lopez’s religion? Palliative care is best delivered through high functioning interdisciplinary teams that can include other supportive people in a patient’s life. We work in concert to try to bring comfort to a patient and their family.4 That support network can include nurses, physicians, social workers, and chaplains. In this case, Ms. Lopez had not yet reached out to her priest. She hasn’t had the time or energy to contact her priest given her symptoms.
“Can I contact your priest for you?
Maybe he can visit or call and chat with you?”
She nods and wipes tears away.
“That would be really nice,” she says. “I’d love it if he could pray with me.”
A few hours after the visit, I call Ms. Lopez’s priest.
I ask him to reach out to her and about her request for prayer.
He says he’s been thinking about her and that her presence has been missed at weekly Mass. He thanks me for the call and says he’ll call her tomorrow.
I say my own small prayer for Ms. Lopez and head home, the day’s work completed.
Sarah D'Ambruoso was born and raised in Maine. She completed her undergraduate and graduate nursing education at New York University and UCLA, respectively, and currently works as a palliative care nurse practitioner in an oncology clinic in Los Angeles.
References
1. Cheng BT et al. Patterns of palliative care beliefs among adults in the U.S.: Analysis of a National Cancer Database. J Pain Symptom Manage. 2019 Aug 10. doi: 10.1016/j.jpainsymman.2019.07.030.
2. Finlay E et al. Filling the gap: Creating an outpatient palliative care program in your institution. Am Soc Clin Oncol Educ Book. 2018 May 23. doi: 10.1200/EDBK_200775.
3. Von Roenn JH et al. Barriers and approaches to the successful integration of palliative care and oncology practice. J Natl Compr Canc Netw. 2013 Mar. doi: 10.6004/jnccn.2013.0209.
4. Ferrell BR et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2016 Oct 31. doi: 10.1200/JCO.2016.70.1474.
The names of health care professionals and patients cited within the dialogue text have been changed to protect their privacy.
but over the years I have come to realize that she was right – most people, including many within health care, don’t have a good appreciation of what palliative care is or how it can help patients and health care teams.
A recent national survey about cancer-related health information found that of more than 1,000 surveyed Americans, less than 30% professed any knowledge of palliative care. Of those who had some knowledge of palliative care, around 30% believed palliative care was synonymous with hospice.1 Another 15% believed that a patient would have to give up cancer-directed treatments to receive palliative care.1
It’s not giving up
This persistent belief that palliative care is equivalent to hospice, or is tantamount to “giving up,” is one of the most commonly held myths I encounter in everyday practice.
I knock on the exam door and walk in.
A small, trim woman in her late 50s is sitting in a chair, arms folded across her chest, face drawn in.
“Hi,” I start. “I’m Sarah, the palliative care nurse practitioner who works in this clinic. I work closely with Dr. Smith.”
Dr. Smith is the patient’s oncologist.
“I really didn’t want to meet you,” she says in a quiet voice, her eyes large with concern.
I don’t take it personally. Few patients really want to be in the position of needing to meet the palliative care team.
“I looked up palliative care on Google and saw the word hospice.”
“Yeah,” I say. “I hear that a lot. Well, I can reassure you that this isn’t hospice.
In this clinic, our focus is on your cancer symptoms, your treatment side effects, and your quality of life.”
She looks visibly relieved. “Quality of life,” she echoes. “I need more of that.”
“OK,” I say. “So, tell me what you’re struggling with the most right now.”
That’s how many palliative care visits start. I actually prefer if patients haven’t heard of palliative care because it allows me to frame it for them, rather than having to start by addressing a myth or a prior negative experience. Even when patients haven’t had a negative experience with palliative care per se, typically, if they’ve interacted with palliative care in the past, it’s usually because someone they loved died in a hospital setting and it is the memory of that terrible loss that becomes synonymous with their recollection of palliative care.
Many patients I meet have never seen another outpatient palliative care practitioner – and this makes sense – we are still too few and far between. Most established palliative care teams are hospital based and many patients seen in the community do not have easy access to palliative care teams where they receive oncologic care.2 As an embedded practitioner, I see patients in the same exam rooms and infusion centers where they receive their cancer therapies, so I’m effectively woven into the fabric of their oncology experience. Just being there in the cancer center allows me to be in the right place at the right time for the right patients and their care teams.
More than pain management
Another myth I tend to dispel a lot is that palliative care is just a euphemism for “pain management.” I have seen this less lately, but still occasionally in the chart I’ll see documented in a note, “patient is seeing palliative/pain management,” when a patient is seeing me or one of my colleagues. Unfortunately, when providers have limited or outdated views of what palliative care is or the value it brings to patient-centered cancer care, referrals to palliative care tend to be delayed.3
“I really think Ms. Lopez could benefit from seeing palliative care,” an oncology nurse practitioner says to an oncologist.
I’m standing nearby, about to see another patient in one of the exam rooms in our clinic.
“But I don’t think she’s ready. And besides, she doesn’t have any pain,” he says.
He turns to me quizzically. “What do you think?”
“Tell me about the patient,” I ask, taking a few steps in their direction.
“Well, she’s a 64-year-old woman with metastatic cancer.
She has a really poor appetite and is losing some weight.
Seems a bit down, kind of pessimistic about things.
Her scan showed some new growth, so guess I’m not surprised by that.”
“I might be able to help her with the appetite and the mood changes.
I can at least talk with her and see where she’s at,” I offer.
“Alright,” he says. “We’ll put the palliative referral in.”
He hesitates. “But are you sure you want to see her?
She doesn’t have any pain.” He sounds skeptical.
“Yeah, I mean, it sounds like she has symptoms that are bothering her, so I’d be happy to see her. She sounds completely appropriate for palliative care.”
I hear this assumption a lot – that palliative care is somehow equivalent to pain management and that unless a patient’s pain is severe, it’s not worth referring the patient to palliative care. Don’t get me wrong – we do a lot of pain management, but at its heart, palliative care is an interdisciplinary specialty focused on improving or maintaining quality of life for people with serious illness. Because the goal is so broad, care can take many shapes.4
In addition to pain, palliative care clinicians commonly treat nausea, shortness of breath, constipation or diarrhea, poor appetite, fatigue, anxiety, depression, and insomnia.
Palliative care is more than medical or nursing care
A related misconception about palliative care held by many lay people and health care workers alike is that palliative care is primarily medical or nursing care focused mostly on alleviating physical symptoms such as pain or nausea. This couldn’t be further from the truth.
We’ve been talking for a while.
Ms. Lopez tells me about her struggles to maintain her weight while undergoing chemotherapy. She has low-grade nausea that is impacting her ability and desire to eat more and didn’t think that her weight loss was severe enough to warrant taking medication.
We talk about how she may be able to use antinausea medication sparingly to alleviate nausea while also limiting side effects from the medications—which was a big concern for her.
I ask her what else is bothering her.
She tells me that she has always been a strong Catholic and even when life has gotten tough, her faith was never shaken – until now.
She is struggling to understand why she ended up with metastatic cancer at such a relatively young age—why would God do this to her?
She had plans for retirement that have since evaporated in the face of a foreshortened life.
Why did this happen to her of all people? She was completely healthy until her diagnosis.
Her face is wet with tears.
We talk a little about how a diagnosis like this can change so much of a person’s life and identity. I try to validate her experience. She’s clearly suffering from a sense that her life is not what she expected, and she is struggling to integrate how her future looks at this point.
I ask her what conversations with her priest have been like.
At this point you may be wondering where this conversation is going. Why are we talking about Ms. Lopez’s religion? Palliative care is best delivered through high functioning interdisciplinary teams that can include other supportive people in a patient’s life. We work in concert to try to bring comfort to a patient and their family.4 That support network can include nurses, physicians, social workers, and chaplains. In this case, Ms. Lopez had not yet reached out to her priest. She hasn’t had the time or energy to contact her priest given her symptoms.
“Can I contact your priest for you?
Maybe he can visit or call and chat with you?”
She nods and wipes tears away.
“That would be really nice,” she says. “I’d love it if he could pray with me.”
A few hours after the visit, I call Ms. Lopez’s priest.
I ask him to reach out to her and about her request for prayer.
He says he’s been thinking about her and that her presence has been missed at weekly Mass. He thanks me for the call and says he’ll call her tomorrow.
I say my own small prayer for Ms. Lopez and head home, the day’s work completed.
Sarah D'Ambruoso was born and raised in Maine. She completed her undergraduate and graduate nursing education at New York University and UCLA, respectively, and currently works as a palliative care nurse practitioner in an oncology clinic in Los Angeles.
References
1. Cheng BT et al. Patterns of palliative care beliefs among adults in the U.S.: Analysis of a National Cancer Database. J Pain Symptom Manage. 2019 Aug 10. doi: 10.1016/j.jpainsymman.2019.07.030.
2. Finlay E et al. Filling the gap: Creating an outpatient palliative care program in your institution. Am Soc Clin Oncol Educ Book. 2018 May 23. doi: 10.1200/EDBK_200775.
3. Von Roenn JH et al. Barriers and approaches to the successful integration of palliative care and oncology practice. J Natl Compr Canc Netw. 2013 Mar. doi: 10.6004/jnccn.2013.0209.
4. Ferrell BR et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2016 Oct 31. doi: 10.1200/JCO.2016.70.1474.