User login
Hypothyroidism carries higher surgical risk not captured by calculator
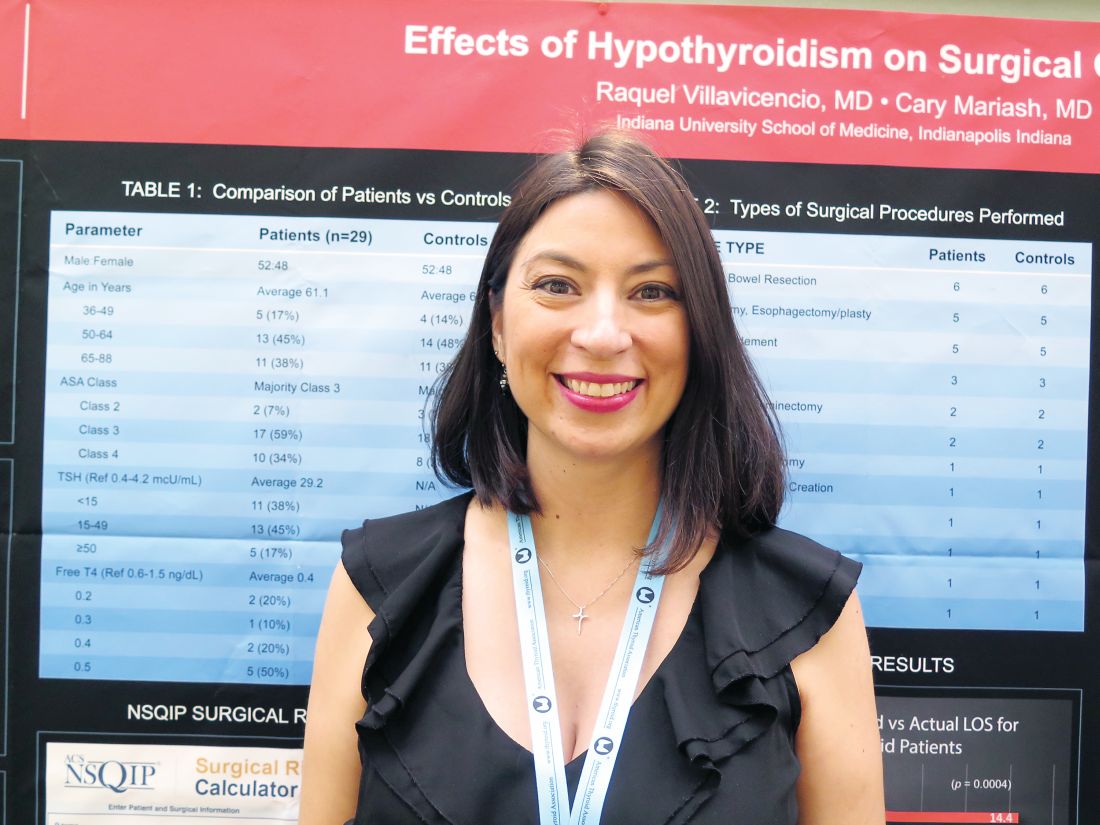
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
VICTORIA, B.C. – Even with contemporary anesthesia and surgical techniques, patients who are overtly hypothyroid at the time of major surgery have a rockier course, suggests a retrospective cohort study of 58 patients in a poster presentation at the annual meeting of the American Thyroid Association.
Actual length of stay for hypothyroid patients was twice that predicted by a commonly used risk calculator, whereas actual and predicted stays aligned well for euthyroid patients. The hypothyroid group had more cases of postoperative atrial fibrillation, ileus, reintubation, and death, although numbers were too small for statistical comparison.
“This will have an impact on how we look at patients, especially from a hospital standpoint and management. That’s quite a bit longer stay and quite a bit more cost. And the longer you stay, the more complications you have, too, so it could be riskier for the patient as well,” said first author Raquel Villavicencio, MD, a fellow at Indiana University at the time of the study, and now a clinical endocrinologist at Community Hospital in Indianapolis.
“Although we don’t consider hypothyroidism an absolute contraindication to surgery, especially if it’s necessary surgery, certainly anybody who is having elective surgery should have it postponed, in our opinion, until they are rendered euthyroid,” she said. “More studies are needed to look at this a little bit closer.”
Explaining the study’s rationale, Dr. Villavicencio noted, “This was a question that came up maybe three or four times a year, where we would get a hypothyroid patient and had to decide whether or not to clear them for surgery.”
Previous studies conducted at large institutions, the Mayo Clinic and Massachusetts General Hospital, had conflicting findings and were done about 30 years ago, she said. Anesthesia and surgical care have improved substantially since then, leading the investigators to hypothesize that hypothyroidism would not carry higher surgical risk today.
Dr. Villavicencio and her coinvestigator, Cary Mariash, MD, used their institutional database to identify 29 adult patients with a thyroid-stimulating hormone (TSH) level of greater than 10 mcU/mL alone or with a TSH level exceeding the upper limit of normal along with a free thyroxine (T4) level of less than 0.6 ng/dL who underwent surgery during 2010-2015. They matched each patient on age, sex, and surgical procedure with a control euthyroid patient.
The mean TSH level in the hypothyroid group was 29.2 mcU/mL. The majority of patients in each group – 59% of the hypothyroid group and 62% of the euthyroid group – had an American Surgical Association class of 3, denoting that this was a fairly sick population. The groups were generally similar on rates of comorbidity, except that the euthyroid patients had a slightly higher prevalence of obstructive sleep apnea.
In both groups, the majority of procedures were laparotomy and/or bowel resection; pharyngolaryngectomy and esophagectomy/esophagoplasty; and wound or bone debridement.
Main results showed that in the hypothyroid group, hospital length of stay predicted with the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator was 6.9 days, but actual length of stay was 14.4 days (P = .0004). In contrast, in the euthyroid group, predicted length of stay was a similar at 7.1 days, and actual length of stay was statistically indistinguishable at 9.2 days (P = .1).
“Hypothyroidism is not taken into account with this calculator,” Dr. Villavicencio noted, adding that she was unaware of any surgical calculators that do.
One patient in the hypothyroid group died, compared with none in the euthyroid group. In terms of postoperative cardiac complications, two patients in the hypothyroid group experienced atrial fibrillation, and there was one case of pulseless electrical–activity arrest in each group.
The groups did not differ on incidence of hypothermia, bradycardia, hyponatremia, time to extubation, and hypotension. However, mean arterial pressure tended to be lower in the hypothyroid group (51 mm Hg) than in the euthyroid group (56 mm Hg), and the former more often needed vasopressors. Furthermore, postoperative ileus and reintubation were more common in the hypothyroid group.
“I think that there are kind of a lot of little things that add up to explain [the longer stay],” said Dr. Villavicencio, who disclosed that she had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: Actual length of stay was significantly longer than calculator-predicted length of stay among hypothyroid patients (14.4 vs. 6.9 days, P = .0004) but not among euthyroid patients (9.2 vs. 7.1 days; P = .1).
Data source: A retrospective cohort study of 29 hypothyroid patients and 29 matched euthyroid patients undergoing major surgery.
Disclosures: Dr. Villavicencio disclosed that she had no relevant conflicts of interest.
PCI advances produce CABG-like 1-year outcomes
BARCELONA – Improvements in percutaneous coronary intervention over the past decade have made a difference. Coronary stenting to treat triple-vessel disease produced roughly the same 1-year results as coronary artery bypass surgery, based on results from 454 patients in an uncontrolled, prospective trial.
With state-of-the-art percutaneous coronary intervention (PCI), the 1-year incidence of major cardiac and cerebrovascular events was 11% in the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) II trial, a PCI outcome substantially better than the 18% rate with PCI seen in the original SYNTAX trial, run during 2005-2007. That incidence was similar to the 11% 1-year major adverse event rate seen in patients who underwent coronary artery bypass grafting (CABG) in the first SYNTAX trial (N Engl J Med. 2009 Mar 5;360[10]:961-72), said Javier Escaned, MD, who reported the results at the annual congress of the European Society of Cardiology.
- Initial assessment of patients using both clinical and anatomic criteria with the SYNTAX score II (Lancet. 2013 Feb 23;381[9867]:639-50), an improvement over the original SYNTAX score that only used anatomic data.
- Assessment of each coronary stenosis for its physiologic impact using a pressure wire to measure the instantaneous wave-free ratio and fractional flow reserve of each suspicious lesion.
- Performing PCI with a second-generation everolimus-eluting stent with a bioabsorbable polymer stent (Synergy) instead of the paclitaxel-eluting first-generation stent (Taxus) used in the first SYNTAX trial.
- Optimization of stent placement with intravascular ultrasound.
- Application of contemporary methods for treating total chronic occlusions that produce higher success rates than a decade ago.
- Prescription of current guideline-directed medical therapy to each patient following PCI.
“To get the best results you need to do all of this; none of these steps takes full credit by itself,” said Dr. Escaned, an interventional cardiologist at the Hospital Clinic San Carlos in Madrid. “The message from SYNTAX II is that if you put all of these steps together, this is the result,” he said in an interview.
An underlying assumption of the single-arm design of SYNTAX II and its “exploratory” comparison to a 334-patient subset of the 897 patients who underwent CABG in the original SYNTAX trial who retrospectively met the SYNTAX score II enrollment criteria used in the current trial was that “CABG has not changed much” since the first SYNTAX trial, Dr. Escaned said. Although he acknowledged that some progress also occurred with CABG in the subsequent 10 years, “it has not been as big a change” as going to second-generation drug-eluting stents, using a pressure wire assessment to target physiologically important stenoses, and improved techniques for treating chronic total occlusions that have nearly doubled success rates in patients with these lesions.
The SYNTAX II trial enrolled 454 patients with de novo triple-vessel coronary disease without left main stem involvement at 22 centers in four European countries during 2014 and 2015. The improvement in the primary 1-year endpoint in the current patients compared with PCI patients from the first SYNTAX trial was driven primarily by reductions in MI and in repeat revascularizations. The SYNTAX II patients also had a 0.7% rate of definite stent thrombosis events, compared with a 2.4% rate in the original SYNTAX PCI patients, a statistically significant difference. Concurrently with Dr. Escaned’s report at the meeting an article with the results appeared online (Eur Heart J. 2017 Aug 26;doi: 10.1093/eurheartj/ehx512).
Dr. Escaned cautioned that longer-term follow-up is needed to more fully compare the PCI results with CABG.
SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
[email protected]
On Twitter @mitchelzoler
BARCELONA – Improvements in percutaneous coronary intervention over the past decade have made a difference. Coronary stenting to treat triple-vessel disease produced roughly the same 1-year results as coronary artery bypass surgery, based on results from 454 patients in an uncontrolled, prospective trial.
With state-of-the-art percutaneous coronary intervention (PCI), the 1-year incidence of major cardiac and cerebrovascular events was 11% in the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) II trial, a PCI outcome substantially better than the 18% rate with PCI seen in the original SYNTAX trial, run during 2005-2007. That incidence was similar to the 11% 1-year major adverse event rate seen in patients who underwent coronary artery bypass grafting (CABG) in the first SYNTAX trial (N Engl J Med. 2009 Mar 5;360[10]:961-72), said Javier Escaned, MD, who reported the results at the annual congress of the European Society of Cardiology.
- Initial assessment of patients using both clinical and anatomic criteria with the SYNTAX score II (Lancet. 2013 Feb 23;381[9867]:639-50), an improvement over the original SYNTAX score that only used anatomic data.
- Assessment of each coronary stenosis for its physiologic impact using a pressure wire to measure the instantaneous wave-free ratio and fractional flow reserve of each suspicious lesion.
- Performing PCI with a second-generation everolimus-eluting stent with a bioabsorbable polymer stent (Synergy) instead of the paclitaxel-eluting first-generation stent (Taxus) used in the first SYNTAX trial.
- Optimization of stent placement with intravascular ultrasound.
- Application of contemporary methods for treating total chronic occlusions that produce higher success rates than a decade ago.
- Prescription of current guideline-directed medical therapy to each patient following PCI.
“To get the best results you need to do all of this; none of these steps takes full credit by itself,” said Dr. Escaned, an interventional cardiologist at the Hospital Clinic San Carlos in Madrid. “The message from SYNTAX II is that if you put all of these steps together, this is the result,” he said in an interview.
An underlying assumption of the single-arm design of SYNTAX II and its “exploratory” comparison to a 334-patient subset of the 897 patients who underwent CABG in the original SYNTAX trial who retrospectively met the SYNTAX score II enrollment criteria used in the current trial was that “CABG has not changed much” since the first SYNTAX trial, Dr. Escaned said. Although he acknowledged that some progress also occurred with CABG in the subsequent 10 years, “it has not been as big a change” as going to second-generation drug-eluting stents, using a pressure wire assessment to target physiologically important stenoses, and improved techniques for treating chronic total occlusions that have nearly doubled success rates in patients with these lesions.
The SYNTAX II trial enrolled 454 patients with de novo triple-vessel coronary disease without left main stem involvement at 22 centers in four European countries during 2014 and 2015. The improvement in the primary 1-year endpoint in the current patients compared with PCI patients from the first SYNTAX trial was driven primarily by reductions in MI and in repeat revascularizations. The SYNTAX II patients also had a 0.7% rate of definite stent thrombosis events, compared with a 2.4% rate in the original SYNTAX PCI patients, a statistically significant difference. Concurrently with Dr. Escaned’s report at the meeting an article with the results appeared online (Eur Heart J. 2017 Aug 26;doi: 10.1093/eurheartj/ehx512).
Dr. Escaned cautioned that longer-term follow-up is needed to more fully compare the PCI results with CABG.
SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
[email protected]
On Twitter @mitchelzoler
BARCELONA – Improvements in percutaneous coronary intervention over the past decade have made a difference. Coronary stenting to treat triple-vessel disease produced roughly the same 1-year results as coronary artery bypass surgery, based on results from 454 patients in an uncontrolled, prospective trial.
With state-of-the-art percutaneous coronary intervention (PCI), the 1-year incidence of major cardiac and cerebrovascular events was 11% in the Synergy Between PCI with Taxus and Cardiac Surgery (SYNTAX) II trial, a PCI outcome substantially better than the 18% rate with PCI seen in the original SYNTAX trial, run during 2005-2007. That incidence was similar to the 11% 1-year major adverse event rate seen in patients who underwent coronary artery bypass grafting (CABG) in the first SYNTAX trial (N Engl J Med. 2009 Mar 5;360[10]:961-72), said Javier Escaned, MD, who reported the results at the annual congress of the European Society of Cardiology.
- Initial assessment of patients using both clinical and anatomic criteria with the SYNTAX score II (Lancet. 2013 Feb 23;381[9867]:639-50), an improvement over the original SYNTAX score that only used anatomic data.
- Assessment of each coronary stenosis for its physiologic impact using a pressure wire to measure the instantaneous wave-free ratio and fractional flow reserve of each suspicious lesion.
- Performing PCI with a second-generation everolimus-eluting stent with a bioabsorbable polymer stent (Synergy) instead of the paclitaxel-eluting first-generation stent (Taxus) used in the first SYNTAX trial.
- Optimization of stent placement with intravascular ultrasound.
- Application of contemporary methods for treating total chronic occlusions that produce higher success rates than a decade ago.
- Prescription of current guideline-directed medical therapy to each patient following PCI.
“To get the best results you need to do all of this; none of these steps takes full credit by itself,” said Dr. Escaned, an interventional cardiologist at the Hospital Clinic San Carlos in Madrid. “The message from SYNTAX II is that if you put all of these steps together, this is the result,” he said in an interview.
An underlying assumption of the single-arm design of SYNTAX II and its “exploratory” comparison to a 334-patient subset of the 897 patients who underwent CABG in the original SYNTAX trial who retrospectively met the SYNTAX score II enrollment criteria used in the current trial was that “CABG has not changed much” since the first SYNTAX trial, Dr. Escaned said. Although he acknowledged that some progress also occurred with CABG in the subsequent 10 years, “it has not been as big a change” as going to second-generation drug-eluting stents, using a pressure wire assessment to target physiologically important stenoses, and improved techniques for treating chronic total occlusions that have nearly doubled success rates in patients with these lesions.
The SYNTAX II trial enrolled 454 patients with de novo triple-vessel coronary disease without left main stem involvement at 22 centers in four European countries during 2014 and 2015. The improvement in the primary 1-year endpoint in the current patients compared with PCI patients from the first SYNTAX trial was driven primarily by reductions in MI and in repeat revascularizations. The SYNTAX II patients also had a 0.7% rate of definite stent thrombosis events, compared with a 2.4% rate in the original SYNTAX PCI patients, a statistically significant difference. Concurrently with Dr. Escaned’s report at the meeting an article with the results appeared online (Eur Heart J. 2017 Aug 26;doi: 10.1093/eurheartj/ehx512).
Dr. Escaned cautioned that longer-term follow-up is needed to more fully compare the PCI results with CABG.
SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
[email protected]
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: At 1 year, the combined major adverse event rate was 11%, similar to the CABG rate in the original SYNTAX trial.
Data source: SYNTAX II, a prospective, multicenter, single-arm study with 454 patients.
Disclosures: SYNTAX II received unrestricted grant support from Philips/Volcano and Boston Scientific, the companies that market the pressure wires and stents used in the study. Dr. Escaned reported ties to Abbott, AstraZeneca, Biosensors, Boston Scientific, Medtronic, OrbusNeich, Philips/Volcano, and Boston Scientific.
Robotic-assisted pulmonary lobectomy effective for large tumors
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
Robotic-assisted pulmonary lobectomy is a safe and effective way to remove large tumors in patients with non–small cell lung cancer (NSCLC), according to the abstract of a study scheduled to be presented at the CHEST annual meeting.
The study covers a retrospective analysis of 345 NSCLC patients with tumors who underwent robotic-assisted pulmonary lobectomy performed by one surgeon from September 2010 through August 2016. The participants were grouped into the following three cohorts: patients with tumors less than 5 cm in diameter, patients with tumors from 5 to 7 cm, and patients with tumors larger than 7 cm. The researchers excluded patients with pulmonary metastases or benign lesions from the study.
Patients with smaller tumors were more likely to have simple lobectomy or lobectomy plus wedge, while patients with larger tumors were more likely to require lobectomy with chest wall resection. Increased tumor size was also associated with increased intraoperative estimated blood loss, skin-to-skin operative time, hospital length of stay, and overall conversion to open lobectomy.
There was no association found between tumor size and increased overall intraoperative or postoperative complications, or in-hospital mortality.
Nirav Patel, MD, FCCP, of the Tampa Bay Sleep Center is scheduled to present his abstract on Sunday Oct. 29th, between 2:15 and 2:30 p.m. in Convention Center – 606. Dr. Patel’s research is part of the Cardiothoracic Surgery session, running from 1:30 p.m. to 3:00 p.m. at the CHEST annual meeting.
FROM CHEST 2017
New appropriate use criteria reframe severe aortic stenosis
New appropriate use criteria (AUC) for severe aortic stenosis (AS) run the full gamut of clinical scenarios and treatment options.
“Cardiology is seeing a radical change in the management of aortic stenosis. This new document incorporates all therapies currently available in the world,” said Vinod H. Thourani, MD, who served on the AUC’s writing group on behalf of the American College of Cardiology. “The AUC highlights state-of-the-art therapy for aortic stenosis and, even more importantly, helps clarify the right indications for surgical and transcatheter valve replacement.”
Surgical risk is assessed based on the Society of Thoracic Surgeons Predicted Risk of Mortality score plus additional anatomic and functional considerations that should be assessed by a multidisciplinary heart team. The AUC repeatedly emphasizes this team’s importance. “Multiple comorbidities can change the pathway of treating AS, and this determination is best made by a heart team that at least includes a noninvasive cardiologist, an interventional cardiologist, and a cardiac surgeon,” Dr. Thourani said. “That’s how patients get the best care.”
Historically, aortic stenosis typically was managed medically or with balloon aortic valvuloplasty (BAV) or open aortic valve replacement, Dr. Thourani said. However, BAV is less common now, and indications for surgical or transcatheter aortic valve replacement (SAVR or TAVR) are expanding. Balloon aortic valvuloplasty sometimes does provide palliative treatment or serve as a bridge to a decision, the AUC states. For example, for a high-risk patient with severe aortic stenosis and severe secondary mitral regurgitation, BAV can help the heart team decide whether TAVR alone will improve mitral regurgitation or whether a double valve procedure is preferable.
Regardless of risk score, the AUC considers a wait-and-see approach as potentially appropriate for patients with asymptomatic high-grade AS whose left ventricular ejection fraction is at least 50%, peak aortic valve velocity is 4.0-4.9 m/sec, and exercise stress test is normal and with no predictors of symptom onset or rapid progression. Asymptomatic patients who are likely to become symptomatic but who have a low risk of sudden death are candidates for intervention (rated “appropriate”) or medical management (“may be appropriate”). In contrast, a positive stress test in an otherwise asymptomatic patient merits consideration of SAVR or TAVR regardless of surgical risk. The recommendations for asymptomatic patients reflect a lack of head-to-head trials in this population, Dr. Thourani said. “We don’t have good randomized data to show one therapy is better than another.”
Symptomatic, high-gradient, severe AS with associated coronary artery disease merits consideration of SAVR with coronary artery bypass graft or, in some cases, TAVR with percutaneous coronary intervention, according to the AUC. Less evidence supports SAVR with PCI. “Optimal management of coronary artery disease in patients with AS is a complex decision process requiring clinical, anatomical, and technical considerations that is best achieved with close collaboration between heart team members,” the authors stress.
The document covers other valvular and structural heart conditions that commonly accompany severe AS, such as symptomatic AS with bicuspid aortic valve and ascending aortic dilation. “Although there remains an increasing prevalence of transcatheter valve usage in bicuspid aortic valve, the standard of care remains surgical therapy, especially in patients who have a dilated aorta,” Dr. Thourani said.
For the first time, the AUC also addresses failing aortic valve prostheses, presenting six relevant clinical scenarios. The AUC consistently recommends SAVR, although the use of TAVR has “dramatically increased” in these patients, Dr. Thourani said. “Long-term data are still pending, but TAVR appears to be a less morbid procedure, when done appropriately.”
The societies involved in creating the AUC statement were the American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons.
Dr. Thourani disclosed ties to Edwards Lifesciences, St. Jude Medical, Abbott, Boston Scientific, and Medtronic.
New appropriate use criteria (AUC) for severe aortic stenosis (AS) run the full gamut of clinical scenarios and treatment options.
“Cardiology is seeing a radical change in the management of aortic stenosis. This new document incorporates all therapies currently available in the world,” said Vinod H. Thourani, MD, who served on the AUC’s writing group on behalf of the American College of Cardiology. “The AUC highlights state-of-the-art therapy for aortic stenosis and, even more importantly, helps clarify the right indications for surgical and transcatheter valve replacement.”
Surgical risk is assessed based on the Society of Thoracic Surgeons Predicted Risk of Mortality score plus additional anatomic and functional considerations that should be assessed by a multidisciplinary heart team. The AUC repeatedly emphasizes this team’s importance. “Multiple comorbidities can change the pathway of treating AS, and this determination is best made by a heart team that at least includes a noninvasive cardiologist, an interventional cardiologist, and a cardiac surgeon,” Dr. Thourani said. “That’s how patients get the best care.”
Historically, aortic stenosis typically was managed medically or with balloon aortic valvuloplasty (BAV) or open aortic valve replacement, Dr. Thourani said. However, BAV is less common now, and indications for surgical or transcatheter aortic valve replacement (SAVR or TAVR) are expanding. Balloon aortic valvuloplasty sometimes does provide palliative treatment or serve as a bridge to a decision, the AUC states. For example, for a high-risk patient with severe aortic stenosis and severe secondary mitral regurgitation, BAV can help the heart team decide whether TAVR alone will improve mitral regurgitation or whether a double valve procedure is preferable.
Regardless of risk score, the AUC considers a wait-and-see approach as potentially appropriate for patients with asymptomatic high-grade AS whose left ventricular ejection fraction is at least 50%, peak aortic valve velocity is 4.0-4.9 m/sec, and exercise stress test is normal and with no predictors of symptom onset or rapid progression. Asymptomatic patients who are likely to become symptomatic but who have a low risk of sudden death are candidates for intervention (rated “appropriate”) or medical management (“may be appropriate”). In contrast, a positive stress test in an otherwise asymptomatic patient merits consideration of SAVR or TAVR regardless of surgical risk. The recommendations for asymptomatic patients reflect a lack of head-to-head trials in this population, Dr. Thourani said. “We don’t have good randomized data to show one therapy is better than another.”
Symptomatic, high-gradient, severe AS with associated coronary artery disease merits consideration of SAVR with coronary artery bypass graft or, in some cases, TAVR with percutaneous coronary intervention, according to the AUC. Less evidence supports SAVR with PCI. “Optimal management of coronary artery disease in patients with AS is a complex decision process requiring clinical, anatomical, and technical considerations that is best achieved with close collaboration between heart team members,” the authors stress.
The document covers other valvular and structural heart conditions that commonly accompany severe AS, such as symptomatic AS with bicuspid aortic valve and ascending aortic dilation. “Although there remains an increasing prevalence of transcatheter valve usage in bicuspid aortic valve, the standard of care remains surgical therapy, especially in patients who have a dilated aorta,” Dr. Thourani said.
For the first time, the AUC also addresses failing aortic valve prostheses, presenting six relevant clinical scenarios. The AUC consistently recommends SAVR, although the use of TAVR has “dramatically increased” in these patients, Dr. Thourani said. “Long-term data are still pending, but TAVR appears to be a less morbid procedure, when done appropriately.”
The societies involved in creating the AUC statement were the American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons.
Dr. Thourani disclosed ties to Edwards Lifesciences, St. Jude Medical, Abbott, Boston Scientific, and Medtronic.
New appropriate use criteria (AUC) for severe aortic stenosis (AS) run the full gamut of clinical scenarios and treatment options.
“Cardiology is seeing a radical change in the management of aortic stenosis. This new document incorporates all therapies currently available in the world,” said Vinod H. Thourani, MD, who served on the AUC’s writing group on behalf of the American College of Cardiology. “The AUC highlights state-of-the-art therapy for aortic stenosis and, even more importantly, helps clarify the right indications for surgical and transcatheter valve replacement.”
Surgical risk is assessed based on the Society of Thoracic Surgeons Predicted Risk of Mortality score plus additional anatomic and functional considerations that should be assessed by a multidisciplinary heart team. The AUC repeatedly emphasizes this team’s importance. “Multiple comorbidities can change the pathway of treating AS, and this determination is best made by a heart team that at least includes a noninvasive cardiologist, an interventional cardiologist, and a cardiac surgeon,” Dr. Thourani said. “That’s how patients get the best care.”
Historically, aortic stenosis typically was managed medically or with balloon aortic valvuloplasty (BAV) or open aortic valve replacement, Dr. Thourani said. However, BAV is less common now, and indications for surgical or transcatheter aortic valve replacement (SAVR or TAVR) are expanding. Balloon aortic valvuloplasty sometimes does provide palliative treatment or serve as a bridge to a decision, the AUC states. For example, for a high-risk patient with severe aortic stenosis and severe secondary mitral regurgitation, BAV can help the heart team decide whether TAVR alone will improve mitral regurgitation or whether a double valve procedure is preferable.
Regardless of risk score, the AUC considers a wait-and-see approach as potentially appropriate for patients with asymptomatic high-grade AS whose left ventricular ejection fraction is at least 50%, peak aortic valve velocity is 4.0-4.9 m/sec, and exercise stress test is normal and with no predictors of symptom onset or rapid progression. Asymptomatic patients who are likely to become symptomatic but who have a low risk of sudden death are candidates for intervention (rated “appropriate”) or medical management (“may be appropriate”). In contrast, a positive stress test in an otherwise asymptomatic patient merits consideration of SAVR or TAVR regardless of surgical risk. The recommendations for asymptomatic patients reflect a lack of head-to-head trials in this population, Dr. Thourani said. “We don’t have good randomized data to show one therapy is better than another.”
Symptomatic, high-gradient, severe AS with associated coronary artery disease merits consideration of SAVR with coronary artery bypass graft or, in some cases, TAVR with percutaneous coronary intervention, according to the AUC. Less evidence supports SAVR with PCI. “Optimal management of coronary artery disease in patients with AS is a complex decision process requiring clinical, anatomical, and technical considerations that is best achieved with close collaboration between heart team members,” the authors stress.
The document covers other valvular and structural heart conditions that commonly accompany severe AS, such as symptomatic AS with bicuspid aortic valve and ascending aortic dilation. “Although there remains an increasing prevalence of transcatheter valve usage in bicuspid aortic valve, the standard of care remains surgical therapy, especially in patients who have a dilated aorta,” Dr. Thourani said.
For the first time, the AUC also addresses failing aortic valve prostheses, presenting six relevant clinical scenarios. The AUC consistently recommends SAVR, although the use of TAVR has “dramatically increased” in these patients, Dr. Thourani said. “Long-term data are still pending, but TAVR appears to be a less morbid procedure, when done appropriately.”
The societies involved in creating the AUC statement were the American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons.
Dr. Thourani disclosed ties to Edwards Lifesciences, St. Jude Medical, Abbott, Boston Scientific, and Medtronic.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
CardioMEMS shows real-world success as use expands
DALLAS – Management of outpatients with advanced heart failure using an implanted pulmonary artery pressure monitor continues to show real-world efficacy and safety at least as impressive as in the pivotal trial for the device.
Data from the first waves of patients to receive the CardioMEMS implanted pulmonary artery pressure (PAP) monitor since it got Food and Drug Administration marketing approval in May 2014 also showed steady uptake of this fluid volume management strategy for patients with advanced heart failure, despite Medicare reimbursement issues in some U.S. regions, J. Thomas Heywood, MD, said at the at the annual scientific meeting of the Heart Failure Society of America. He estimated that more than 6,000 U.S. heart failure patients have now had a CardioMEMS PAP monitor implanted.

“The clinicians using CardioMEMS now have a lot more experience” than they had during the trial, he said in an interview. “They have more experience using the device, they know what treatments to use to lower PAP more effectively, and they are now convinced that patients will benefit from reducing diastolic PAP.”
Dr. Heywood estimated that tens of thousands more U.S. heart failure patients with New York Heart Association class III disease and a recent history of at least one heart failure hospitalization are eligible to receive an implanted PAP monitor, dwarfing the more than 6,000 patients who received a device so far.
The postapproval study
The newest efficacy data come from the first 300 patients enrolled in the CardioMEMS HF System Post Approval Study, a registry of patients receiving an implanted PAP monitor funded by the device’s manufacturer and scheduled to include a total of 1,200 patients. Dr. Heywood said full enrollment was on track for completion by the end of October 2017.
The first 300 patients enrolled in the postapproval study were older than the CHAMPION cohort; they averaged about 69 years of age, compared with about 62 years in CHAMPION, were more often women (38% vs. 28% in CHAMPION), and were more likely to have heart failure with preserved ejection fraction (41% vs. about 22%).

A similar pattern existed for the 6-month cumulative tally of PAP area under the curve, which showed an average rise of 42 mm Hg/day in the CHAMPION control patients, an average drop of 160 mm Hg/day in the CHAMPION patients managed using their CardioMEMS data, and a drop of 281 mm Hg/day in the 300 postapproval study patients.
“We’re now using the implanted sensor in a broader population of patients, and one wonders whether the effect will be diluted. What we see is at least as good as in the CHAMPION trial. This is just an early snapshot, but it is exciting that we see no erosion of the benefit. It’s a great indication that the correct patients are receiving it,” Dr. Raval said while presenting a poster at the meeting.
Further scrutiny of the same 300 patients showed another feature of the impact of PAP monitoring on patient outcomes: The first 90 days with the PAP monitor in place led to a greater number of tweaks in patient treatment and a steady fall in PAP. During days 91-180, PAP tended to level off, the number of medication adjustments dropped, and heart failure hospitalizations fell even more than in the first 90 days, Joanna M. Joly, MD, reported in a separate poster at the meeting.

The data showed “effective reduction” of PAP during the second half of the study despite fewer medication adjustments. How was that possible? Patients who transmit data on their PAPs undergo “modeling of their behavior” based on the feedback they receive from the device, Dr. Joly suggested. Regular measurement of their PAP and seeing how the number relates to their clinical status helps patients “understand the impact of their nonadherence to diet and their medications.” Another factor could be the growing familiarity clinicians develop over time with PAP fluctuations that individual patients display repeatedly that are usually self-correcting. Also, patients may undergo “hemodynamic remodeling” that results in improved self-correction of minor shifts in fluid volume and vascular tone, she said.
This pattern of a reduced need for interventions after the first 90 days with a PAP implant suggests that many patients managed this way may be able to transition to care largely delivered by local providers, or even play a greater role in their own self-care once their PAP and clinical state stabilizes, Dr. Joly said.
The findings imply that by the end of the first 90 days, “patients accept the device and manage themselves better. It becomes basically a behavioral device” that helps patients better optimize their diet and behavior, Dr. Raval observed.
Safety holds steady
Continued real-world use of PAP monitoring has also resulted in new safety insights. During the first 3 years when the CardioMEMS device was on the U.S. market, May 2014–May 2017, the FDA’s adverse event reporting system for devices, the Manufacturer and User Facility Device Experience (MAUDE) received reports on 177 unique adverse events in 155 patients implanted with a PAP monitor, Muthiah Vaduganathan, MD, reported at the meeting. During the same 3-year period, he estimated that at least 5,500 U.S. patients had received a CardioMEMS device, based on data Dr. Vaduganathan obtained from the manufacturer, Abbott. This works out to an adverse event rate of about 2.8%, virtually identical to the rate reported from CHAMPION, noted Dr. Vaduganathan, a cardiologist also at Brigham and Women’s.
Analysis of both the 22 deaths as well as the episodes of pulmonary artery injury or hemoptysis showed that the preponderance occurred relatively early after introduction for U.S. use, suggesting that “a learning curve may exist for the most serious complications,” he said. “Improved safety and device durability may result from careful patient selection, increased operator training, and refined technologies.”
Dr. Vaduganathan cautioned that the MAUDE database is limited by its bias toward serious adverse events, selective reporting, and lack of adjudication for the reported events. Concurrently with his report at the meeting, a written version appeared online (JAMA Cardiol. 2017 Sep 18. doi:10.1001/jamacardio.2017.3791).
“The adverse event rate was reassuringly low, well below the accepted threshold for device safety. It bodes favorably for the device,” he said in an interview.
“But with a passive surveillance system like MAUDE, adverse events are likely underreported; we see in MAUDE the most severe adverse events. There is certainly a larger spectrum of more minor events that we are not seeing, but I think these numbers accurately reflect serious events.” A full registry of every U.S. patient who receives the device, similar to what’s in place for U.S. patients who undergo transcatheter aortic valve replacement, would provide a more complete picture of the risks, Dr. Vaduganathan suggested.
He also voiced some surprise about the frequency of pulmonary artery injury, which was not as apparent in the 550 total patients enrolled in CHAMPION. Clinicians who place the PAP monitor are required to first take a training program, but the manufacturer has no mandated minimum number of placements an operator must assist on before launching a new CardioMEMS practice, Dr. Vaduganathan said. Many of the pulmonary artery injuries reported to MAUDE resulted from wire perforations that resulted from loss of wire control, he noted.
Clarifying the optimal CardioMEMS recipients
PAP monitoring for patients with advanced heart failure “is a major advance for certain patients who have historically been very challenging to manage,” especially patients with heart failure with preserved ejection fraction, which has few other treatment options. But “it’s often difficult to know when to pull the trigger” and proceed with placing a PAP monitor in an eligible patient, he said. “Greater experience will help us better understand that,” Dr. Vaduganathan predicted.
Dr. Heywood said that, in addition to the standard criteria of NYHA class III symptoms and a recent history of a heart failure hospitalization, the other clinical feature he looks for in a patient who is a possible CardioMEMS recipient is a persistently elevated systolic PAP as measured using echocardiography.
“These are patients with evidence of an ongoing hemodynamic problem despite treatment, and I need more data to do a better job of getting their PAP down.” Although the PAP that patients self-measure once they have the device in place is their diastolic PAP, measuring systolic PAP by echo is usually a good surrogate for finding patients who also have a persistently elevated diastolic PAP, he explained.
Another important selection criterion is to look for the patients who are dying from heart failure rather than with heart failure, Dr. Heywood added.
“If heart failure is the major thing wrong, then we can improve their quality of life” by guiding fluid management with regular PAP measurement, especially patients with preserved left ventricular ejection fraction who have few other treatment options right now, he said.
The CardioMEMS HF System Post Approval Study is sponsored by Abbott, which markets CardioMEMS. Dr Heywood has been a consultant to and/or has received research funding from Abbott as well as Impedimed, Medtronic, Novartis, and Otsuka. Dr. Raval has been a consultant to Abbott. Dr. Joly and Dr. Vaduganathan had no disclosures.
[email protected]
On Twitter @mitchelzoler
DALLAS – Management of outpatients with advanced heart failure using an implanted pulmonary artery pressure monitor continues to show real-world efficacy and safety at least as impressive as in the pivotal trial for the device.
Data from the first waves of patients to receive the CardioMEMS implanted pulmonary artery pressure (PAP) monitor since it got Food and Drug Administration marketing approval in May 2014 also showed steady uptake of this fluid volume management strategy for patients with advanced heart failure, despite Medicare reimbursement issues in some U.S. regions, J. Thomas Heywood, MD, said at the at the annual scientific meeting of the Heart Failure Society of America. He estimated that more than 6,000 U.S. heart failure patients have now had a CardioMEMS PAP monitor implanted.

“The clinicians using CardioMEMS now have a lot more experience” than they had during the trial, he said in an interview. “They have more experience using the device, they know what treatments to use to lower PAP more effectively, and they are now convinced that patients will benefit from reducing diastolic PAP.”
Dr. Heywood estimated that tens of thousands more U.S. heart failure patients with New York Heart Association class III disease and a recent history of at least one heart failure hospitalization are eligible to receive an implanted PAP monitor, dwarfing the more than 6,000 patients who received a device so far.
The postapproval study
The newest efficacy data come from the first 300 patients enrolled in the CardioMEMS HF System Post Approval Study, a registry of patients receiving an implanted PAP monitor funded by the device’s manufacturer and scheduled to include a total of 1,200 patients. Dr. Heywood said full enrollment was on track for completion by the end of October 2017.
The first 300 patients enrolled in the postapproval study were older than the CHAMPION cohort; they averaged about 69 years of age, compared with about 62 years in CHAMPION, were more often women (38% vs. 28% in CHAMPION), and were more likely to have heart failure with preserved ejection fraction (41% vs. about 22%).

A similar pattern existed for the 6-month cumulative tally of PAP area under the curve, which showed an average rise of 42 mm Hg/day in the CHAMPION control patients, an average drop of 160 mm Hg/day in the CHAMPION patients managed using their CardioMEMS data, and a drop of 281 mm Hg/day in the 300 postapproval study patients.
“We’re now using the implanted sensor in a broader population of patients, and one wonders whether the effect will be diluted. What we see is at least as good as in the CHAMPION trial. This is just an early snapshot, but it is exciting that we see no erosion of the benefit. It’s a great indication that the correct patients are receiving it,” Dr. Raval said while presenting a poster at the meeting.
Further scrutiny of the same 300 patients showed another feature of the impact of PAP monitoring on patient outcomes: The first 90 days with the PAP monitor in place led to a greater number of tweaks in patient treatment and a steady fall in PAP. During days 91-180, PAP tended to level off, the number of medication adjustments dropped, and heart failure hospitalizations fell even more than in the first 90 days, Joanna M. Joly, MD, reported in a separate poster at the meeting.

The data showed “effective reduction” of PAP during the second half of the study despite fewer medication adjustments. How was that possible? Patients who transmit data on their PAPs undergo “modeling of their behavior” based on the feedback they receive from the device, Dr. Joly suggested. Regular measurement of their PAP and seeing how the number relates to their clinical status helps patients “understand the impact of their nonadherence to diet and their medications.” Another factor could be the growing familiarity clinicians develop over time with PAP fluctuations that individual patients display repeatedly that are usually self-correcting. Also, patients may undergo “hemodynamic remodeling” that results in improved self-correction of minor shifts in fluid volume and vascular tone, she said.
This pattern of a reduced need for interventions after the first 90 days with a PAP implant suggests that many patients managed this way may be able to transition to care largely delivered by local providers, or even play a greater role in their own self-care once their PAP and clinical state stabilizes, Dr. Joly said.
The findings imply that by the end of the first 90 days, “patients accept the device and manage themselves better. It becomes basically a behavioral device” that helps patients better optimize their diet and behavior, Dr. Raval observed.
Safety holds steady
Continued real-world use of PAP monitoring has also resulted in new safety insights. During the first 3 years when the CardioMEMS device was on the U.S. market, May 2014–May 2017, the FDA’s adverse event reporting system for devices, the Manufacturer and User Facility Device Experience (MAUDE) received reports on 177 unique adverse events in 155 patients implanted with a PAP monitor, Muthiah Vaduganathan, MD, reported at the meeting. During the same 3-year period, he estimated that at least 5,500 U.S. patients had received a CardioMEMS device, based on data Dr. Vaduganathan obtained from the manufacturer, Abbott. This works out to an adverse event rate of about 2.8%, virtually identical to the rate reported from CHAMPION, noted Dr. Vaduganathan, a cardiologist also at Brigham and Women’s.
Analysis of both the 22 deaths as well as the episodes of pulmonary artery injury or hemoptysis showed that the preponderance occurred relatively early after introduction for U.S. use, suggesting that “a learning curve may exist for the most serious complications,” he said. “Improved safety and device durability may result from careful patient selection, increased operator training, and refined technologies.”
Dr. Vaduganathan cautioned that the MAUDE database is limited by its bias toward serious adverse events, selective reporting, and lack of adjudication for the reported events. Concurrently with his report at the meeting, a written version appeared online (JAMA Cardiol. 2017 Sep 18. doi:10.1001/jamacardio.2017.3791).
“The adverse event rate was reassuringly low, well below the accepted threshold for device safety. It bodes favorably for the device,” he said in an interview.
“But with a passive surveillance system like MAUDE, adverse events are likely underreported; we see in MAUDE the most severe adverse events. There is certainly a larger spectrum of more minor events that we are not seeing, but I think these numbers accurately reflect serious events.” A full registry of every U.S. patient who receives the device, similar to what’s in place for U.S. patients who undergo transcatheter aortic valve replacement, would provide a more complete picture of the risks, Dr. Vaduganathan suggested.
He also voiced some surprise about the frequency of pulmonary artery injury, which was not as apparent in the 550 total patients enrolled in CHAMPION. Clinicians who place the PAP monitor are required to first take a training program, but the manufacturer has no mandated minimum number of placements an operator must assist on before launching a new CardioMEMS practice, Dr. Vaduganathan said. Many of the pulmonary artery injuries reported to MAUDE resulted from wire perforations that resulted from loss of wire control, he noted.
Clarifying the optimal CardioMEMS recipients
PAP monitoring for patients with advanced heart failure “is a major advance for certain patients who have historically been very challenging to manage,” especially patients with heart failure with preserved ejection fraction, which has few other treatment options. But “it’s often difficult to know when to pull the trigger” and proceed with placing a PAP monitor in an eligible patient, he said. “Greater experience will help us better understand that,” Dr. Vaduganathan predicted.
Dr. Heywood said that, in addition to the standard criteria of NYHA class III symptoms and a recent history of a heart failure hospitalization, the other clinical feature he looks for in a patient who is a possible CardioMEMS recipient is a persistently elevated systolic PAP as measured using echocardiography.
“These are patients with evidence of an ongoing hemodynamic problem despite treatment, and I need more data to do a better job of getting their PAP down.” Although the PAP that patients self-measure once they have the device in place is their diastolic PAP, measuring systolic PAP by echo is usually a good surrogate for finding patients who also have a persistently elevated diastolic PAP, he explained.
Another important selection criterion is to look for the patients who are dying from heart failure rather than with heart failure, Dr. Heywood added.
“If heart failure is the major thing wrong, then we can improve their quality of life” by guiding fluid management with regular PAP measurement, especially patients with preserved left ventricular ejection fraction who have few other treatment options right now, he said.
The CardioMEMS HF System Post Approval Study is sponsored by Abbott, which markets CardioMEMS. Dr Heywood has been a consultant to and/or has received research funding from Abbott as well as Impedimed, Medtronic, Novartis, and Otsuka. Dr. Raval has been a consultant to Abbott. Dr. Joly and Dr. Vaduganathan had no disclosures.
[email protected]
On Twitter @mitchelzoler
DALLAS – Management of outpatients with advanced heart failure using an implanted pulmonary artery pressure monitor continues to show real-world efficacy and safety at least as impressive as in the pivotal trial for the device.
Data from the first waves of patients to receive the CardioMEMS implanted pulmonary artery pressure (PAP) monitor since it got Food and Drug Administration marketing approval in May 2014 also showed steady uptake of this fluid volume management strategy for patients with advanced heart failure, despite Medicare reimbursement issues in some U.S. regions, J. Thomas Heywood, MD, said at the at the annual scientific meeting of the Heart Failure Society of America. He estimated that more than 6,000 U.S. heart failure patients have now had a CardioMEMS PAP monitor implanted.

“The clinicians using CardioMEMS now have a lot more experience” than they had during the trial, he said in an interview. “They have more experience using the device, they know what treatments to use to lower PAP more effectively, and they are now convinced that patients will benefit from reducing diastolic PAP.”
Dr. Heywood estimated that tens of thousands more U.S. heart failure patients with New York Heart Association class III disease and a recent history of at least one heart failure hospitalization are eligible to receive an implanted PAP monitor, dwarfing the more than 6,000 patients who received a device so far.
The postapproval study
The newest efficacy data come from the first 300 patients enrolled in the CardioMEMS HF System Post Approval Study, a registry of patients receiving an implanted PAP monitor funded by the device’s manufacturer and scheduled to include a total of 1,200 patients. Dr. Heywood said full enrollment was on track for completion by the end of October 2017.
The first 300 patients enrolled in the postapproval study were older than the CHAMPION cohort; they averaged about 69 years of age, compared with about 62 years in CHAMPION, were more often women (38% vs. 28% in CHAMPION), and were more likely to have heart failure with preserved ejection fraction (41% vs. about 22%).

A similar pattern existed for the 6-month cumulative tally of PAP area under the curve, which showed an average rise of 42 mm Hg/day in the CHAMPION control patients, an average drop of 160 mm Hg/day in the CHAMPION patients managed using their CardioMEMS data, and a drop of 281 mm Hg/day in the 300 postapproval study patients.
“We’re now using the implanted sensor in a broader population of patients, and one wonders whether the effect will be diluted. What we see is at least as good as in the CHAMPION trial. This is just an early snapshot, but it is exciting that we see no erosion of the benefit. It’s a great indication that the correct patients are receiving it,” Dr. Raval said while presenting a poster at the meeting.
Further scrutiny of the same 300 patients showed another feature of the impact of PAP monitoring on patient outcomes: The first 90 days with the PAP monitor in place led to a greater number of tweaks in patient treatment and a steady fall in PAP. During days 91-180, PAP tended to level off, the number of medication adjustments dropped, and heart failure hospitalizations fell even more than in the first 90 days, Joanna M. Joly, MD, reported in a separate poster at the meeting.

The data showed “effective reduction” of PAP during the second half of the study despite fewer medication adjustments. How was that possible? Patients who transmit data on their PAPs undergo “modeling of their behavior” based on the feedback they receive from the device, Dr. Joly suggested. Regular measurement of their PAP and seeing how the number relates to their clinical status helps patients “understand the impact of their nonadherence to diet and their medications.” Another factor could be the growing familiarity clinicians develop over time with PAP fluctuations that individual patients display repeatedly that are usually self-correcting. Also, patients may undergo “hemodynamic remodeling” that results in improved self-correction of minor shifts in fluid volume and vascular tone, she said.
This pattern of a reduced need for interventions after the first 90 days with a PAP implant suggests that many patients managed this way may be able to transition to care largely delivered by local providers, or even play a greater role in their own self-care once their PAP and clinical state stabilizes, Dr. Joly said.
The findings imply that by the end of the first 90 days, “patients accept the device and manage themselves better. It becomes basically a behavioral device” that helps patients better optimize their diet and behavior, Dr. Raval observed.
Safety holds steady
Continued real-world use of PAP monitoring has also resulted in new safety insights. During the first 3 years when the CardioMEMS device was on the U.S. market, May 2014–May 2017, the FDA’s adverse event reporting system for devices, the Manufacturer and User Facility Device Experience (MAUDE) received reports on 177 unique adverse events in 155 patients implanted with a PAP monitor, Muthiah Vaduganathan, MD, reported at the meeting. During the same 3-year period, he estimated that at least 5,500 U.S. patients had received a CardioMEMS device, based on data Dr. Vaduganathan obtained from the manufacturer, Abbott. This works out to an adverse event rate of about 2.8%, virtually identical to the rate reported from CHAMPION, noted Dr. Vaduganathan, a cardiologist also at Brigham and Women’s.
Analysis of both the 22 deaths as well as the episodes of pulmonary artery injury or hemoptysis showed that the preponderance occurred relatively early after introduction for U.S. use, suggesting that “a learning curve may exist for the most serious complications,” he said. “Improved safety and device durability may result from careful patient selection, increased operator training, and refined technologies.”
Dr. Vaduganathan cautioned that the MAUDE database is limited by its bias toward serious adverse events, selective reporting, and lack of adjudication for the reported events. Concurrently with his report at the meeting, a written version appeared online (JAMA Cardiol. 2017 Sep 18. doi:10.1001/jamacardio.2017.3791).
“The adverse event rate was reassuringly low, well below the accepted threshold for device safety. It bodes favorably for the device,” he said in an interview.
“But with a passive surveillance system like MAUDE, adverse events are likely underreported; we see in MAUDE the most severe adverse events. There is certainly a larger spectrum of more minor events that we are not seeing, but I think these numbers accurately reflect serious events.” A full registry of every U.S. patient who receives the device, similar to what’s in place for U.S. patients who undergo transcatheter aortic valve replacement, would provide a more complete picture of the risks, Dr. Vaduganathan suggested.
He also voiced some surprise about the frequency of pulmonary artery injury, which was not as apparent in the 550 total patients enrolled in CHAMPION. Clinicians who place the PAP monitor are required to first take a training program, but the manufacturer has no mandated minimum number of placements an operator must assist on before launching a new CardioMEMS practice, Dr. Vaduganathan said. Many of the pulmonary artery injuries reported to MAUDE resulted from wire perforations that resulted from loss of wire control, he noted.
Clarifying the optimal CardioMEMS recipients
PAP monitoring for patients with advanced heart failure “is a major advance for certain patients who have historically been very challenging to manage,” especially patients with heart failure with preserved ejection fraction, which has few other treatment options. But “it’s often difficult to know when to pull the trigger” and proceed with placing a PAP monitor in an eligible patient, he said. “Greater experience will help us better understand that,” Dr. Vaduganathan predicted.
Dr. Heywood said that, in addition to the standard criteria of NYHA class III symptoms and a recent history of a heart failure hospitalization, the other clinical feature he looks for in a patient who is a possible CardioMEMS recipient is a persistently elevated systolic PAP as measured using echocardiography.
“These are patients with evidence of an ongoing hemodynamic problem despite treatment, and I need more data to do a better job of getting their PAP down.” Although the PAP that patients self-measure once they have the device in place is their diastolic PAP, measuring systolic PAP by echo is usually a good surrogate for finding patients who also have a persistently elevated diastolic PAP, he explained.
Another important selection criterion is to look for the patients who are dying from heart failure rather than with heart failure, Dr. Heywood added.
“If heart failure is the major thing wrong, then we can improve their quality of life” by guiding fluid management with regular PAP measurement, especially patients with preserved left ventricular ejection fraction who have few other treatment options right now, he said.
The CardioMEMS HF System Post Approval Study is sponsored by Abbott, which markets CardioMEMS. Dr Heywood has been a consultant to and/or has received research funding from Abbott as well as Impedimed, Medtronic, Novartis, and Otsuka. Dr. Raval has been a consultant to Abbott. Dr. Joly and Dr. Vaduganathan had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Ideal intubation position still unknown
In critically ill adults undergoing endotracheal intubation, the ramped position does not significantly improve oxygenation compared with the sniffing position, according to results of a multicenter, randomized trial of 260 patients treated in an intensive care unit.
Moreover, “[ramped] position appeared to worsen glottic view and increase the number of attempts required for successful intubation,” wrote Matthew W. Semler, MD, of Vanderbilt University Medical Center, Nashville, Tenn., and his coauthors (Chest. 2017 Oct. doi: 10.1016/j.chest.2017.03.061).
The ramped and sniffing positions are the two most common patient positions used during emergent intubation, according to investigators. The sniffing position is characterized by supine torso, neck flexed forward, and head extended, while ramped position involves elevating the torso and head.
Some believe the ramped position may offer superior anatomic alignment of the upper airway; however, only a few observational studies suggest it is associated with fewer complications than the sniffing position, the authors wrote.
Accordingly, they conducted a multicenter randomized trial with a primary endpoint of lowest arterial oxygen saturation, hypothesizing that the endpoint would be higher for the ramped position: “Our primary outcome of lowest arterial oxygen saturation is an established endpoint in ICU intubation trials, and is linked to periprocedural cardiac arrest and death,” they wrote.
The investigators instead found that median lowest arterial oxygen saturation was not statistically different between groups, at 93% for the ramped position, and 92% for the sniffing position (P = 0.27), published data show.
Further results showed that the ramped position appeared to be associated with poor glottic view and more difficult intubation. The incidence of grade III (only epiglottis) or grade IV (no visible glottis structures) views were 25.4% for ramped vs. 11.5% for sniffing (P = .01), while the rate of first-attempt intubation was 76.2% for ramped vs 85.4% for sniffing (P = .02).
While the findings are compelling, the authors were forthcoming about the potential limitations of the study and differences compared with earlier investigations. Notably, they said, all prior controlled trials of patient positioning during endotracheal intubation were conducted in the operating room, rather than in the ICU.
Also, the operators’ skill levels may further explain differences in this study’s outcomes from those of similar studies, the researchers noted. Earlier studies included patients intubated by one or two senior anesthesiologists from one center, while this trial involved 30 operators across multiple centers, with the average operator having performed 60 previous intubations. “Thus, our findings may generalize to settings in which airway management is performed by trainees, but whether results would be similar among expert operators remains unknown,” the investigators noted.
The authors reported no potential conflicts of interest. One coauthor reported serving on an advisory board for Avisa Pharma.
Editorialists praised the multicenter, randomized design of this study, and its total recruitment of 260 patients. They also noted several limitations of the study that “could shed some light” on the group’s conclusions (Chest. 2017 Oct. doi: 10.1016/j.chest.2017.06.002).
“The results diverge from [operating room] literature of the past 15 years that suggest that the ramped position is the preferred intubation position for obese patients or those with an anticipated difficult airway.” This may have been caused by shortcomings of this study’s design and differences between it and other research exploring the topic of patient positioning during endotracheal intubation, they wrote.
The study lacked a prespecified algorithm for preoxygenation and the operators had relatively low amounts of experience with intubations. Finally, the beds used in this study could contribute to the divergences between this intensive care unit experience and the operating room literature. The operating room table is narrower, firmer, and more stable, while by contrast, the ICU bed is wider and softer, they noted. This “may make initial positioning, maintenance of positioning, and accessing the patient’s head more difficult.”
Nevertheless, “[this] important study provides ideas for further study of optimal positioning in the ICU and adds valuable data to the sparse literature on the subject in the ICU setting,” they concluded.
James Aaron Scott, DO, Jens Matthias Walz, MD, FCCP, and Stephen O. Heard, MD, FCCP, are in the department of anesthesiology and perioperative medicine, UMass Memorial Medical Center, Worcester, Mass. The authors reported no conflicts of interest. These comments are based on their editorial.
Editorialists praised the multicenter, randomized design of this study, and its total recruitment of 260 patients. They also noted several limitations of the study that “could shed some light” on the group’s conclusions (Chest. 2017 Oct. doi: 10.1016/j.chest.2017.06.002).
“The results diverge from [operating room] literature of the past 15 years that suggest that the ramped position is the preferred intubation position for obese patients or those with an anticipated difficult airway.” This may have been caused by shortcomings of this study’s design and differences between it and other research exploring the topic of patient positioning during endotracheal intubation, they wrote.
The study lacked a prespecified algorithm for preoxygenation and the operators had relatively low amounts of experience with intubations. Finally, the beds used in this study could contribute to the divergences between this intensive care unit experience and the operating room literature. The operating room table is narrower, firmer, and more stable, while by contrast, the ICU bed is wider and softer, they noted. This “may make initial positioning, maintenance of positioning, and accessing the patient’s head more difficult.”
Nevertheless, “[this] important study provides ideas for further study of optimal positioning in the ICU and adds valuable data to the sparse literature on the subject in the ICU setting,” they concluded.
James Aaron Scott, DO, Jens Matthias Walz, MD, FCCP, and Stephen O. Heard, MD, FCCP, are in the department of anesthesiology and perioperative medicine, UMass Memorial Medical Center, Worcester, Mass. The authors reported no conflicts of interest. These comments are based on their editorial.
Editorialists praised the multicenter, randomized design of this study, and its total recruitment of 260 patients. They also noted several limitations of the study that “could shed some light” on the group’s conclusions (Chest. 2017 Oct. doi: 10.1016/j.chest.2017.06.002).
“The results diverge from [operating room] literature of the past 15 years that suggest that the ramped position is the preferred intubation position for obese patients or those with an anticipated difficult airway.” This may have been caused by shortcomings of this study’s design and differences between it and other research exploring the topic of patient positioning during endotracheal intubation, they wrote.
The study lacked a prespecified algorithm for preoxygenation and the operators had relatively low amounts of experience with intubations. Finally, the beds used in this study could contribute to the divergences between this intensive care unit experience and the operating room literature. The operating room table is narrower, firmer, and more stable, while by contrast, the ICU bed is wider and softer, they noted. This “may make initial positioning, maintenance of positioning, and accessing the patient’s head more difficult.”
Nevertheless, “[this] important study provides ideas for further study of optimal positioning in the ICU and adds valuable data to the sparse literature on the subject in the ICU setting,” they concluded.
James Aaron Scott, DO, Jens Matthias Walz, MD, FCCP, and Stephen O. Heard, MD, FCCP, are in the department of anesthesiology and perioperative medicine, UMass Memorial Medical Center, Worcester, Mass. The authors reported no conflicts of interest. These comments are based on their editorial.
In critically ill adults undergoing endotracheal intubation, the ramped position does not significantly improve oxygenation compared with the sniffing position, according to results of a multicenter, randomized trial of 260 patients treated in an intensive care unit.
Moreover, “[ramped] position appeared to worsen glottic view and increase the number of attempts required for successful intubation,” wrote Matthew W. Semler, MD, of Vanderbilt University Medical Center, Nashville, Tenn., and his coauthors (Chest. 2017 Oct. doi: 10.1016/j.chest.2017.03.061).
The ramped and sniffing positions are the two most common patient positions used during emergent intubation, according to investigators. The sniffing position is characterized by supine torso, neck flexed forward, and head extended, while ramped position involves elevating the torso and head.
Some believe the ramped position may offer superior anatomic alignment of the upper airway; however, only a few observational studies suggest it is associated with fewer complications than the sniffing position, the authors wrote.
Accordingly, they conducted a multicenter randomized trial with a primary endpoint of lowest arterial oxygen saturation, hypothesizing that the endpoint would be higher for the ramped position: “Our primary outcome of lowest arterial oxygen saturation is an established endpoint in ICU intubation trials, and is linked to periprocedural cardiac arrest and death,” they wrote.
The investigators instead found that median lowest arterial oxygen saturation was not statistically different between groups, at 93% for the ramped position, and 92% for the sniffing position (P = 0.27), published data show.
Further results showed that the ramped position appeared to be associated with poor glottic view and more difficult intubation. The incidence of grade III (only epiglottis) or grade IV (no visible glottis structures) views were 25.4% for ramped vs. 11.5% for sniffing (P = .01), while the rate of first-attempt intubation was 76.2% for ramped vs 85.4% for sniffing (P = .02).
While the findings are compelling, the authors were forthcoming about the potential limitations of the study and differences compared with earlier investigations. Notably, they said, all prior controlled trials of patient positioning during endotracheal intubation were conducted in the operating room, rather than in the ICU.
Also, the operators’ skill levels may further explain differences in this study’s outcomes from those of similar studies, the researchers noted. Earlier studies included patients intubated by one or two senior anesthesiologists from one center, while this trial involved 30 operators across multiple centers, with the average operator having performed 60 previous intubations. “Thus, our findings may generalize to settings in which airway management is performed by trainees, but whether results would be similar among expert operators remains unknown,” the investigators noted.
The authors reported no potential conflicts of interest. One coauthor reported serving on an advisory board for Avisa Pharma.
In critically ill adults undergoing endotracheal intubation, the ramped position does not significantly improve oxygenation compared with the sniffing position, according to results of a multicenter, randomized trial of 260 patients treated in an intensive care unit.
Moreover, “[ramped] position appeared to worsen glottic view and increase the number of attempts required for successful intubation,” wrote Matthew W. Semler, MD, of Vanderbilt University Medical Center, Nashville, Tenn., and his coauthors (Chest. 2017 Oct. doi: 10.1016/j.chest.2017.03.061).
The ramped and sniffing positions are the two most common patient positions used during emergent intubation, according to investigators. The sniffing position is characterized by supine torso, neck flexed forward, and head extended, while ramped position involves elevating the torso and head.
Some believe the ramped position may offer superior anatomic alignment of the upper airway; however, only a few observational studies suggest it is associated with fewer complications than the sniffing position, the authors wrote.
Accordingly, they conducted a multicenter randomized trial with a primary endpoint of lowest arterial oxygen saturation, hypothesizing that the endpoint would be higher for the ramped position: “Our primary outcome of lowest arterial oxygen saturation is an established endpoint in ICU intubation trials, and is linked to periprocedural cardiac arrest and death,” they wrote.
The investigators instead found that median lowest arterial oxygen saturation was not statistically different between groups, at 93% for the ramped position, and 92% for the sniffing position (P = 0.27), published data show.
Further results showed that the ramped position appeared to be associated with poor glottic view and more difficult intubation. The incidence of grade III (only epiglottis) or grade IV (no visible glottis structures) views were 25.4% for ramped vs. 11.5% for sniffing (P = .01), while the rate of first-attempt intubation was 76.2% for ramped vs 85.4% for sniffing (P = .02).
While the findings are compelling, the authors were forthcoming about the potential limitations of the study and differences compared with earlier investigations. Notably, they said, all prior controlled trials of patient positioning during endotracheal intubation were conducted in the operating room, rather than in the ICU.
Also, the operators’ skill levels may further explain differences in this study’s outcomes from those of similar studies, the researchers noted. Earlier studies included patients intubated by one or two senior anesthesiologists from one center, while this trial involved 30 operators across multiple centers, with the average operator having performed 60 previous intubations. “Thus, our findings may generalize to settings in which airway management is performed by trainees, but whether results would be similar among expert operators remains unknown,” the investigators noted.
The authors reported no potential conflicts of interest. One coauthor reported serving on an advisory board for Avisa Pharma.
FROM CHEST
Key clinical point: During endotracheal intubation of critically ill adults, use of the ramped position did not significantly improve oxygenation compared with the sniffing position, and it increased the number of attempts needed to achieve successful intubation.
Major finding: The median lowest arterial oxygen saturation was 93% for the ramped position and 92% for the sniffing position (P = .27).
Data source: Multicenter, randomized trial of 260 critically ill adults undergoing endotracheal intubation.
Disclosures: The authors reported no potential conflicts of interest. One coauthor reported serving on an advisory board for Avisa Pharma.
Surgical left atrial appendage closure slashes stroke risk
BARCELONA – Routine surgical closure of the left atrial appendage during open heart surgery provides long-term protection against cerebral ischemic events, according to the findings of the first-ever randomized controlled trial to address the issue.
“I think we can say, based on our study, that it would be advisable to routinely add surgical closure of the left atrial appendage to planned open heart surgery,” Jesper Park-Hansen, MD, said at the annual congress of the European Society of Cardiology.
In light of the demonstrated success of percutaneous closure of the LAA using the Watchman and other devices for stroke prevention in patients with atrial fibrillation, Dr. Park-Hansen and his coinvestigators at the University of Copenhagen organized LAACS (the Left Atrial Appendage Closure Study). The goal was to generate solid, randomized trial evidence as to whether preemptive routine surgical closure of the LAA at the time of cardiac surgery is of benefit. Some cardiac surgeons already do this routinely; many others don’t because of the lack of Level 1 supporting evidence.
LAACS included 141 patients randomized to surgical LAA closure or not at the point of first-time open heart surgery. The study population included patients with and without a history of atrial fibrillation. LAA closure was accomplished via a purse string closure with a silk string around the neck of the appendage backed up by an additional single running suture. Transesophageal echocardiography performed in 10 patients a mean of 520 days post closure showed no signs of leakage or incomplete closure.
The primary composite outcome was comprised of clinical stroke or transient ischemic attack diagnosed by a neurologist, or a silent cerebral infarct detected on MRI performed 2-4 weeks post discharge and again at least 6 months later. At a mean follow-up of 3.7 years and a maximum of 6 years, this outcome had occurred in 6.3% of the LAAC group, significantly lower than the 18.3% rate in controls. All but one patient with a cerebral ischemic event in the control group had atrial fibrillation. The risk of an event was unrelated to whether or not a patient had a history of atrial fibrillation prior to surgery or to CHA2DS2-VASc score.
Dr. Park-Hansen emphasized that he and his coinvestigators don’t consider LAACS to be the final word on routine prophylactic appendage closure.
“This is the first randomized study. We are eager to move on to another randomized study on a larger scale. That is the next step for us,” he said.
“The challenge now – and what we will be discussing with our surgeons – is to agree on a feasible safe and effective means of left atrial appendage closure. My personal opinion is the Lariat suture delivery device or some other easily reproducible method of closure could be a good way to go,” Dr. Park-Hansen added.
The research group’s cardiac surgeons already have ruled out excision and stapling because of concerns about bleeding risk and the additional cost imposed by stapling.
Discussant Volkmar Falk, MD, commented that LAACS was too small, probably severely underpowered, should have included a preoperative MRI so investigators could reliably capture perioperative silent cerebral infarcts, and the double suture purse string is “probably not the best method” to occlude the LAA.
“LAACS addresses an important question, but alas, it does not provide the answer,” declared Dr. Falk, professor and director of the department of cardiothoracic and vascular surgery at Charité Medical University in Berlin.
Dr. Park-Hansen and Dr. Falk reported having no financial conflicts of interest.
BARCELONA – Routine surgical closure of the left atrial appendage during open heart surgery provides long-term protection against cerebral ischemic events, according to the findings of the first-ever randomized controlled trial to address the issue.
“I think we can say, based on our study, that it would be advisable to routinely add surgical closure of the left atrial appendage to planned open heart surgery,” Jesper Park-Hansen, MD, said at the annual congress of the European Society of Cardiology.
In light of the demonstrated success of percutaneous closure of the LAA using the Watchman and other devices for stroke prevention in patients with atrial fibrillation, Dr. Park-Hansen and his coinvestigators at the University of Copenhagen organized LAACS (the Left Atrial Appendage Closure Study). The goal was to generate solid, randomized trial evidence as to whether preemptive routine surgical closure of the LAA at the time of cardiac surgery is of benefit. Some cardiac surgeons already do this routinely; many others don’t because of the lack of Level 1 supporting evidence.
LAACS included 141 patients randomized to surgical LAA closure or not at the point of first-time open heart surgery. The study population included patients with and without a history of atrial fibrillation. LAA closure was accomplished via a purse string closure with a silk string around the neck of the appendage backed up by an additional single running suture. Transesophageal echocardiography performed in 10 patients a mean of 520 days post closure showed no signs of leakage or incomplete closure.
The primary composite outcome was comprised of clinical stroke or transient ischemic attack diagnosed by a neurologist, or a silent cerebral infarct detected on MRI performed 2-4 weeks post discharge and again at least 6 months later. At a mean follow-up of 3.7 years and a maximum of 6 years, this outcome had occurred in 6.3% of the LAAC group, significantly lower than the 18.3% rate in controls. All but one patient with a cerebral ischemic event in the control group had atrial fibrillation. The risk of an event was unrelated to whether or not a patient had a history of atrial fibrillation prior to surgery or to CHA2DS2-VASc score.
Dr. Park-Hansen emphasized that he and his coinvestigators don’t consider LAACS to be the final word on routine prophylactic appendage closure.
“This is the first randomized study. We are eager to move on to another randomized study on a larger scale. That is the next step for us,” he said.
“The challenge now – and what we will be discussing with our surgeons – is to agree on a feasible safe and effective means of left atrial appendage closure. My personal opinion is the Lariat suture delivery device or some other easily reproducible method of closure could be a good way to go,” Dr. Park-Hansen added.
The research group’s cardiac surgeons already have ruled out excision and stapling because of concerns about bleeding risk and the additional cost imposed by stapling.
Discussant Volkmar Falk, MD, commented that LAACS was too small, probably severely underpowered, should have included a preoperative MRI so investigators could reliably capture perioperative silent cerebral infarcts, and the double suture purse string is “probably not the best method” to occlude the LAA.
“LAACS addresses an important question, but alas, it does not provide the answer,” declared Dr. Falk, professor and director of the department of cardiothoracic and vascular surgery at Charité Medical University in Berlin.
Dr. Park-Hansen and Dr. Falk reported having no financial conflicts of interest.
BARCELONA – Routine surgical closure of the left atrial appendage during open heart surgery provides long-term protection against cerebral ischemic events, according to the findings of the first-ever randomized controlled trial to address the issue.
“I think we can say, based on our study, that it would be advisable to routinely add surgical closure of the left atrial appendage to planned open heart surgery,” Jesper Park-Hansen, MD, said at the annual congress of the European Society of Cardiology.
In light of the demonstrated success of percutaneous closure of the LAA using the Watchman and other devices for stroke prevention in patients with atrial fibrillation, Dr. Park-Hansen and his coinvestigators at the University of Copenhagen organized LAACS (the Left Atrial Appendage Closure Study). The goal was to generate solid, randomized trial evidence as to whether preemptive routine surgical closure of the LAA at the time of cardiac surgery is of benefit. Some cardiac surgeons already do this routinely; many others don’t because of the lack of Level 1 supporting evidence.
LAACS included 141 patients randomized to surgical LAA closure or not at the point of first-time open heart surgery. The study population included patients with and without a history of atrial fibrillation. LAA closure was accomplished via a purse string closure with a silk string around the neck of the appendage backed up by an additional single running suture. Transesophageal echocardiography performed in 10 patients a mean of 520 days post closure showed no signs of leakage or incomplete closure.
The primary composite outcome was comprised of clinical stroke or transient ischemic attack diagnosed by a neurologist, or a silent cerebral infarct detected on MRI performed 2-4 weeks post discharge and again at least 6 months later. At a mean follow-up of 3.7 years and a maximum of 6 years, this outcome had occurred in 6.3% of the LAAC group, significantly lower than the 18.3% rate in controls. All but one patient with a cerebral ischemic event in the control group had atrial fibrillation. The risk of an event was unrelated to whether or not a patient had a history of atrial fibrillation prior to surgery or to CHA2DS2-VASc score.
Dr. Park-Hansen emphasized that he and his coinvestigators don’t consider LAACS to be the final word on routine prophylactic appendage closure.
“This is the first randomized study. We are eager to move on to another randomized study on a larger scale. That is the next step for us,” he said.
“The challenge now – and what we will be discussing with our surgeons – is to agree on a feasible safe and effective means of left atrial appendage closure. My personal opinion is the Lariat suture delivery device or some other easily reproducible method of closure could be a good way to go,” Dr. Park-Hansen added.
The research group’s cardiac surgeons already have ruled out excision and stapling because of concerns about bleeding risk and the additional cost imposed by stapling.
Discussant Volkmar Falk, MD, commented that LAACS was too small, probably severely underpowered, should have included a preoperative MRI so investigators could reliably capture perioperative silent cerebral infarcts, and the double suture purse string is “probably not the best method” to occlude the LAA.
“LAACS addresses an important question, but alas, it does not provide the answer,” declared Dr. Falk, professor and director of the department of cardiothoracic and vascular surgery at Charité Medical University in Berlin.
Dr. Park-Hansen and Dr. Falk reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: The composite rate of clinical stroke, TIA, or silent cerebral infarct in the years following open heart surgery was threefold higher in patients randomized to no prophylactic surgical closure of the left atrial appendage, compared with patients who got appendage closure during their surgery.
Data source: A randomized trial in which 141 patients undergoing first-time open heart surgery were assigned to prophylactic surgical closure of the left atrial appendage or not.
Disclosures: The study was conducted free of commercial support. The presenter reported having no financial conflicts of interest.
Hepatitis C falls as barrier to heart transplantation
DALLAS – The heart transplant team at Vanderbilt University has successfully placed hearts from deceased, hepatitis C virus–positive patients into recipients, and then eradicated the subsequent infection that appeared in most recipients using a standard regimen.
So far, five of nine heart transplant recipients who developed a posttransplant hepatitis C virus (HCV) infection had the infection eradicated using one of the highly effective HCV drug regimens, and an additional three patients from the series are nearing their 12th week without detectable virus following treatment that marks a sustained response, Kelly H. Schlendorf, MD, said at the annual scientific meeting of the Heart Failure Society of America. The ninth patient died after developing a pulmonary embolism during the 7th week on antiviral therapy.

The recipients have been patients in a marginal clinical state and facing a long projected wait on the heart-recipient queue of the United Network for Organ Sharing (UNOS), Dr. Schlendorf said in an interview.
These have been “patients with a morbidity and mortality risk from waiting that can be mitigated by expanding the donor pool.” She gave an example of a patient with a left ventricular assist device that required replacement by either a second device or transplant, “so getting the transplant quickly was a good thing,” said Dr. Schlendorf, a cardiologist at Vanderbilt in Nashville.
Based on her analysis of UNOS data, “upwards of 100” and perhaps as many as 300 additional donor hearts could be available annually for U.S. transplants if the organs weren’t excluded because of HCV infection.
The Vanderbilt team has so far approached 15 patients in their program wait-listed for hearts about the possibility of accepting an HCV-positive organ, and all 15 have given their consent, she said. “We spend a lot of time talking with patients and their caregivers about the risks and benefits and possible complications.”
The 13 recipients, starting in September 2016, included 12 patients who were HCV naive and 1 patient with a history of HCV exposure. All 13 received the program’s standard three-drug regimen for immunosuppression.
During close surveillance, 9 of the 13 developed an infection. Patients with genotype 1 HCV received 12 weeks of treatment with ledipasvir plus sofosbuvir. Those infected with genotype 3 received 12-24 weeks of treatment with sofosbuvir plus velpatasvir. Treatment with these direct-acting antivirals meant that patients had to adjust the time when they took their proton-pump inhibitors, and they needed to stop treatment with diltiazem and statins while on the antivirals.
“In the era of direct-acting antivirals, HCV-positive donors may provide a safe and effective way to expand the donor pool and reduce wait-list times,” Dr. Schlendorf said. She noted that in recent years an increased number of potential organ donors have been HCV positive. She also cautioned that so far follow-up has been relatively brief, with no patient yet followed as long as 1 year after transplant.
The direct-acting HCV antivirals are expensive, and some payers established clinical criteria that patients must meet to qualify for coverage of these regimens. “We have not encountered difficulties getting insurers to pay,” Dr. Schlendorf said. Despite the antivirals’ cost there are significant cost savings from fewer days in the ICU waiting for heart transplantation and a reduced need for mechanical support as a bridge to transplant, she noted.
[email protected]
On Twitter @mitchelzoler
DALLAS – The heart transplant team at Vanderbilt University has successfully placed hearts from deceased, hepatitis C virus–positive patients into recipients, and then eradicated the subsequent infection that appeared in most recipients using a standard regimen.
So far, five of nine heart transplant recipients who developed a posttransplant hepatitis C virus (HCV) infection had the infection eradicated using one of the highly effective HCV drug regimens, and an additional three patients from the series are nearing their 12th week without detectable virus following treatment that marks a sustained response, Kelly H. Schlendorf, MD, said at the annual scientific meeting of the Heart Failure Society of America. The ninth patient died after developing a pulmonary embolism during the 7th week on antiviral therapy.

The recipients have been patients in a marginal clinical state and facing a long projected wait on the heart-recipient queue of the United Network for Organ Sharing (UNOS), Dr. Schlendorf said in an interview.
These have been “patients with a morbidity and mortality risk from waiting that can be mitigated by expanding the donor pool.” She gave an example of a patient with a left ventricular assist device that required replacement by either a second device or transplant, “so getting the transplant quickly was a good thing,” said Dr. Schlendorf, a cardiologist at Vanderbilt in Nashville.
Based on her analysis of UNOS data, “upwards of 100” and perhaps as many as 300 additional donor hearts could be available annually for U.S. transplants if the organs weren’t excluded because of HCV infection.
The Vanderbilt team has so far approached 15 patients in their program wait-listed for hearts about the possibility of accepting an HCV-positive organ, and all 15 have given their consent, she said. “We spend a lot of time talking with patients and their caregivers about the risks and benefits and possible complications.”
The 13 recipients, starting in September 2016, included 12 patients who were HCV naive and 1 patient with a history of HCV exposure. All 13 received the program’s standard three-drug regimen for immunosuppression.
During close surveillance, 9 of the 13 developed an infection. Patients with genotype 1 HCV received 12 weeks of treatment with ledipasvir plus sofosbuvir. Those infected with genotype 3 received 12-24 weeks of treatment with sofosbuvir plus velpatasvir. Treatment with these direct-acting antivirals meant that patients had to adjust the time when they took their proton-pump inhibitors, and they needed to stop treatment with diltiazem and statins while on the antivirals.
“In the era of direct-acting antivirals, HCV-positive donors may provide a safe and effective way to expand the donor pool and reduce wait-list times,” Dr. Schlendorf said. She noted that in recent years an increased number of potential organ donors have been HCV positive. She also cautioned that so far follow-up has been relatively brief, with no patient yet followed as long as 1 year after transplant.
The direct-acting HCV antivirals are expensive, and some payers established clinical criteria that patients must meet to qualify for coverage of these regimens. “We have not encountered difficulties getting insurers to pay,” Dr. Schlendorf said. Despite the antivirals’ cost there are significant cost savings from fewer days in the ICU waiting for heart transplantation and a reduced need for mechanical support as a bridge to transplant, she noted.
[email protected]
On Twitter @mitchelzoler
DALLAS – The heart transplant team at Vanderbilt University has successfully placed hearts from deceased, hepatitis C virus–positive patients into recipients, and then eradicated the subsequent infection that appeared in most recipients using a standard regimen.
So far, five of nine heart transplant recipients who developed a posttransplant hepatitis C virus (HCV) infection had the infection eradicated using one of the highly effective HCV drug regimens, and an additional three patients from the series are nearing their 12th week without detectable virus following treatment that marks a sustained response, Kelly H. Schlendorf, MD, said at the annual scientific meeting of the Heart Failure Society of America. The ninth patient died after developing a pulmonary embolism during the 7th week on antiviral therapy.

The recipients have been patients in a marginal clinical state and facing a long projected wait on the heart-recipient queue of the United Network for Organ Sharing (UNOS), Dr. Schlendorf said in an interview.
These have been “patients with a morbidity and mortality risk from waiting that can be mitigated by expanding the donor pool.” She gave an example of a patient with a left ventricular assist device that required replacement by either a second device or transplant, “so getting the transplant quickly was a good thing,” said Dr. Schlendorf, a cardiologist at Vanderbilt in Nashville.
Based on her analysis of UNOS data, “upwards of 100” and perhaps as many as 300 additional donor hearts could be available annually for U.S. transplants if the organs weren’t excluded because of HCV infection.
The Vanderbilt team has so far approached 15 patients in their program wait-listed for hearts about the possibility of accepting an HCV-positive organ, and all 15 have given their consent, she said. “We spend a lot of time talking with patients and their caregivers about the risks and benefits and possible complications.”
The 13 recipients, starting in September 2016, included 12 patients who were HCV naive and 1 patient with a history of HCV exposure. All 13 received the program’s standard three-drug regimen for immunosuppression.
During close surveillance, 9 of the 13 developed an infection. Patients with genotype 1 HCV received 12 weeks of treatment with ledipasvir plus sofosbuvir. Those infected with genotype 3 received 12-24 weeks of treatment with sofosbuvir plus velpatasvir. Treatment with these direct-acting antivirals meant that patients had to adjust the time when they took their proton-pump inhibitors, and they needed to stop treatment with diltiazem and statins while on the antivirals.
“In the era of direct-acting antivirals, HCV-positive donors may provide a safe and effective way to expand the donor pool and reduce wait-list times,” Dr. Schlendorf said. She noted that in recent years an increased number of potential organ donors have been HCV positive. She also cautioned that so far follow-up has been relatively brief, with no patient yet followed as long as 1 year after transplant.
The direct-acting HCV antivirals are expensive, and some payers established clinical criteria that patients must meet to qualify for coverage of these regimens. “We have not encountered difficulties getting insurers to pay,” Dr. Schlendorf said. Despite the antivirals’ cost there are significant cost savings from fewer days in the ICU waiting for heart transplantation and a reduced need for mechanical support as a bridge to transplant, she noted.
[email protected]
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Eight of nine patients who developed HCV infection had it eradicated by a direct-acting antiviral regimen.
Data source: A series of 13 patients treated at one U.S. center.
Disclosures: Dr. Schlendorf had no disclosures.
Intraoperative ketamine makes no dent in postop delirium or pain
Postoperative delirium remains a problem without an effective solution, wrote Michael S. Avidan, MBBCh, FCASA, of Washington University, Saint Louis, and his colleagues (Lancet 2017;390[10091]:267-75).
Recent guidelines published by the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council include ketamine as a recommended component of multimodal pain therapy for several commonly performed surgeries. “Before recommending widespread administration of an intraoperative bolus of subanaesthetic ketamine, demonstrating that ketamine decreases either delirium or pain, or both, without incurring adverse effects in a large, pragmatic trial was warranted,” the researchers said.
In the PODCAST (Prevention of Delirium and Complications Associated With Surgical Treatments) trial, the researchers randomized 672 patients over the age of 60 undergoing major open surgery under general anesthesia (such as open cardiac or noncardiac surgery, urological surgery, gynecologic surgery, or intra-abdominal surgery) to 0.5 mg/kg ketamine (227), 1.0 mg/kg ketamine (223), or placebo (222). The ketamine or placebo was given after anesthesia and before surgical incision.
Overall, no difference in the incidence of delirium occurred between patients in the combined ketamine groups (19.5%) and the placebo group (19.8%), and there was no significant difference in delirium across all three treatment groups.
No differences in pain based on visual analog scale scores were observed across the three groups, and overall adverse event rates were similar as well: approximately 40.8% in the 1.0-mg ketamine group, 39.6% in the 0.5-mg ketamine group, and 36.9% in the placebo group.
The study findings were limited by several factors, including a study population potentially too small to show an effect of ketamine on delirium, and a lack of data on other variables that might contribute to delirium and pain, the researchers noted. However, the results suggest that “despite present evidence and guidelines, the administration of a subanaesthetic ketamine dose during surgery is not useful for preventing postoperative delirium (primary outcome) or reducing postoperative pain and minimising opioid consumption (related secondary outcomes),” and appears to increase postoperative hallucinations and nightmares to an extent that might be prohibitive, they said.
The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
Postoperative delirium remains a problem without an effective solution, wrote Michael S. Avidan, MBBCh, FCASA, of Washington University, Saint Louis, and his colleagues (Lancet 2017;390[10091]:267-75).
Recent guidelines published by the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council include ketamine as a recommended component of multimodal pain therapy for several commonly performed surgeries. “Before recommending widespread administration of an intraoperative bolus of subanaesthetic ketamine, demonstrating that ketamine decreases either delirium or pain, or both, without incurring adverse effects in a large, pragmatic trial was warranted,” the researchers said.
In the PODCAST (Prevention of Delirium and Complications Associated With Surgical Treatments) trial, the researchers randomized 672 patients over the age of 60 undergoing major open surgery under general anesthesia (such as open cardiac or noncardiac surgery, urological surgery, gynecologic surgery, or intra-abdominal surgery) to 0.5 mg/kg ketamine (227), 1.0 mg/kg ketamine (223), or placebo (222). The ketamine or placebo was given after anesthesia and before surgical incision.
Overall, no difference in the incidence of delirium occurred between patients in the combined ketamine groups (19.5%) and the placebo group (19.8%), and there was no significant difference in delirium across all three treatment groups.
No differences in pain based on visual analog scale scores were observed across the three groups, and overall adverse event rates were similar as well: approximately 40.8% in the 1.0-mg ketamine group, 39.6% in the 0.5-mg ketamine group, and 36.9% in the placebo group.
The study findings were limited by several factors, including a study population potentially too small to show an effect of ketamine on delirium, and a lack of data on other variables that might contribute to delirium and pain, the researchers noted. However, the results suggest that “despite present evidence and guidelines, the administration of a subanaesthetic ketamine dose during surgery is not useful for preventing postoperative delirium (primary outcome) or reducing postoperative pain and minimising opioid consumption (related secondary outcomes),” and appears to increase postoperative hallucinations and nightmares to an extent that might be prohibitive, they said.
The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
Postoperative delirium remains a problem without an effective solution, wrote Michael S. Avidan, MBBCh, FCASA, of Washington University, Saint Louis, and his colleagues (Lancet 2017;390[10091]:267-75).
Recent guidelines published by the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council include ketamine as a recommended component of multimodal pain therapy for several commonly performed surgeries. “Before recommending widespread administration of an intraoperative bolus of subanaesthetic ketamine, demonstrating that ketamine decreases either delirium or pain, or both, without incurring adverse effects in a large, pragmatic trial was warranted,” the researchers said.
In the PODCAST (Prevention of Delirium and Complications Associated With Surgical Treatments) trial, the researchers randomized 672 patients over the age of 60 undergoing major open surgery under general anesthesia (such as open cardiac or noncardiac surgery, urological surgery, gynecologic surgery, or intra-abdominal surgery) to 0.5 mg/kg ketamine (227), 1.0 mg/kg ketamine (223), or placebo (222). The ketamine or placebo was given after anesthesia and before surgical incision.
Overall, no difference in the incidence of delirium occurred between patients in the combined ketamine groups (19.5%) and the placebo group (19.8%), and there was no significant difference in delirium across all three treatment groups.
No differences in pain based on visual analog scale scores were observed across the three groups, and overall adverse event rates were similar as well: approximately 40.8% in the 1.0-mg ketamine group, 39.6% in the 0.5-mg ketamine group, and 36.9% in the placebo group.
The study findings were limited by several factors, including a study population potentially too small to show an effect of ketamine on delirium, and a lack of data on other variables that might contribute to delirium and pain, the researchers noted. However, the results suggest that “despite present evidence and guidelines, the administration of a subanaesthetic ketamine dose during surgery is not useful for preventing postoperative delirium (primary outcome) or reducing postoperative pain and minimising opioid consumption (related secondary outcomes),” and appears to increase postoperative hallucinations and nightmares to an extent that might be prohibitive, they said.
The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
FROM THE LANCET
Key clinical point: Ketamine failed to reduce postoperative delirium in older adults.
Major finding: No difference was observed in the incidence of postoperative delirium between patients given ketamine before surgical incision and patients on placebo.
Data source: The Prevention of Delirium and Complications Associated With Surgical Treatments study, a randomized, multicenter trial of 672 adults older than 60 years.
Disclosures: The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
Sinus of Valsalva preserved in aortic valve replacement
The sinus of Valsalva segment can be preserved during aortic valve replacement irrespective of the type of valve pathology, according to a recent study by Rita Karianna Milewski, MD, and her colleagues at the Hospital of the University of Pennsylvania, Philadelphia.
Severe aortic root dilation coupled to aortic valve disease requires root replacement in patients with a tricuspid or bicuspid aortic valve. Commonly, an aortic valve replacement and supracoronary ascending aorta replacement (AVRSCAAR) procedure has been used for patients who have a mild to moderately dilated sinus segment. One advantage of the procedure is that it retains the sinus of Valsalva (SOV) and preserves the intact coronary ostia.
However, the long-term behavior and risk of aortic events for the retained SOV in both BAV and TAV patients remains unclear, according to Dr. Milewski and her colleagues.
Previous researchers have suggested that patients with BAV and TAV have different rates of complications of the remaining aorta and dilation of the proximal aorta and retained sinus segment. In addition, it has been suggested that the cause of aortic dilation is different in patients with aortic stenosis (AS) and aortic insufficiency (AI) and is based on TAV and BAV morphology, histology, and hemodynamic flow patterns.
However, in the August issue of the Journal of Thoracic and Cardiovascular Surgery, Dr. Milewski and her colleagues reported on their study showing that, in patients with nonaneurysmal SOV undergoing AVRSCAAR, the sinus of Valsalva segment can be preserved regardless of the type of valvular pathology (aortic stenosis vs. aortic insufficiency) or valvular morphology (BAV vs. TAV).
The researchers retrospectively reviewed a prospectively maintained institutional database to stratify all patients by BAV or TAV valvular pathology with concomitant ascending aortic aneurysm who underwent an elective AVRSCAAR from 2002 to 2015 (J Thorac Cardiovasc Surg. 2017;154:421-32).
The distribution of the 428 patients meeting inclusion criteria by subgroups was: BAV group (254 patients: BAV-AS = 178; BAV-AI = 76); TAV group (174 patients: TAV-AS = 61; TAV-AI =113). Preoperative sinus of Valsalva dimensions were divided into 3 subgroups (less than 40 mm, 40-45 mm, and greater than 45 mm).
The mean patient age for patients with BAV and TAV was 59 years and 72 years (P less than .001), respectively (with 78% with BAV being men and 57% with TAV being men). There was a significantly higher subpopulation of AS in the BAV cohort vs. TAV-AS (70% vs. 35%; P less than .001).
With regard to SOV sizing, there was no significant difference in mean preoperative aortic root diameters between BAV and TAV cohorts for the AS or AI subpopulations.
In-hospital/30-day mortality was significantly higher in patients with TAV (5.2%) than in patients with BAV (1.6%, P = .033). In addition, the incidence of transient ischemic attack/stroke was significantly higher in the TAV group (3.4%) vs. the BAV group (0.8%, P = .04).
Valvular morphology and pathology at baseline, preoperative SOV diameter, postoperative time course, and interaction effect of preoperative SOV diameters and postoperative time course were used as covariates to assess outcomes. Within-subject and within–stratified subgroup comparison failed to show main effects across the follow-up times on postoperative SOV size patterns (P = .935), implying that the SOV trends were stable and sustained (discharge to greater than or equal to 10 years) irrespective of valvular morphology and pathology (BAV-AI, BAV-AS, TAV-AI, and TAV-AS).
Preoperative SOV dimensions significantly affected the retained postoperative sinus dimensions (P less than .001), according to Dr. Milewski and her colleagues.
The data indicated that an initial and pronounced postoperative decrease in SOV dimensions occurs with AVRSCAAR independently of aortic valve morphology, aortic valve pathology, and age, they added.
The 10-year freedom from aortic reoperation rates were 97% and 95% in the BAV and TAV subgroups, respectively. The BAV group had significantly improved reoperation-free survival, compared with the TAV group (P less than .001), while the type of valvular pathology within each group did not show a significant survival difference.
“Irrespective of the aortic valve morphology or valve pathology, in patients with mild to moderate aortic root dilatation (less than 45 mm), preservation of the SOV segment in the context of an AVRSCAAR procedure is justified. Continued further follow-up will be important to understand the long-term outcomes of sinus preservation, especially in the younger population with BAVs,” the researchers concluded.
The authors reported having no financial conflicts to disclose.
With regard to the question, ‘‘Is it necessary to replace the sinuses of Valsalva in the setting of bicuspid aortic valve aortopathy?’’, the researchers “leverage their enormous institutional experience to find an answer. The results suggest that this answer is ‘no.’ At least not in all cases,” Thoralf M. Sundt, MD, wrote in his invited commentary on the paper (J Thorac Cardiovasc Surg. 2017;154:419-20).
“The findings of this study argue for us to take a step back and ask how much really needs be done,” he added. And although “it is hard to ask a surgeon to do less rather than more; however, the balance of judgment has to be between the operative risk of the more aggressive approach and the natural history of the disease. In other words, what does it ‘cost’ to be aggressive, and what do we gain?” he asked.
Bicuspid aortic valve aortopathy, it would appear, is not cancer after all. Regardless of theoretic arguments that are based on embryology and the migration of neural crest cells, it does not appear to require resection to ‘clean margins,’ even if we believe that the operative risk ‘in our hands’ is low,” concluded Dr. Sundt.
Thoralf M. Sundt, MD, is at Harvard Medical School, Boston. He reported having no disclosures.
With regard to the question, ‘‘Is it necessary to replace the sinuses of Valsalva in the setting of bicuspid aortic valve aortopathy?’’, the researchers “leverage their enormous institutional experience to find an answer. The results suggest that this answer is ‘no.’ At least not in all cases,” Thoralf M. Sundt, MD, wrote in his invited commentary on the paper (J Thorac Cardiovasc Surg. 2017;154:419-20).
“The findings of this study argue for us to take a step back and ask how much really needs be done,” he added. And although “it is hard to ask a surgeon to do less rather than more; however, the balance of judgment has to be between the operative risk of the more aggressive approach and the natural history of the disease. In other words, what does it ‘cost’ to be aggressive, and what do we gain?” he asked.
Bicuspid aortic valve aortopathy, it would appear, is not cancer after all. Regardless of theoretic arguments that are based on embryology and the migration of neural crest cells, it does not appear to require resection to ‘clean margins,’ even if we believe that the operative risk ‘in our hands’ is low,” concluded Dr. Sundt.
Thoralf M. Sundt, MD, is at Harvard Medical School, Boston. He reported having no disclosures.
With regard to the question, ‘‘Is it necessary to replace the sinuses of Valsalva in the setting of bicuspid aortic valve aortopathy?’’, the researchers “leverage their enormous institutional experience to find an answer. The results suggest that this answer is ‘no.’ At least not in all cases,” Thoralf M. Sundt, MD, wrote in his invited commentary on the paper (J Thorac Cardiovasc Surg. 2017;154:419-20).
“The findings of this study argue for us to take a step back and ask how much really needs be done,” he added. And although “it is hard to ask a surgeon to do less rather than more; however, the balance of judgment has to be between the operative risk of the more aggressive approach and the natural history of the disease. In other words, what does it ‘cost’ to be aggressive, and what do we gain?” he asked.
Bicuspid aortic valve aortopathy, it would appear, is not cancer after all. Regardless of theoretic arguments that are based on embryology and the migration of neural crest cells, it does not appear to require resection to ‘clean margins,’ even if we believe that the operative risk ‘in our hands’ is low,” concluded Dr. Sundt.
Thoralf M. Sundt, MD, is at Harvard Medical School, Boston. He reported having no disclosures.
The sinus of Valsalva segment can be preserved during aortic valve replacement irrespective of the type of valve pathology, according to a recent study by Rita Karianna Milewski, MD, and her colleagues at the Hospital of the University of Pennsylvania, Philadelphia.
Severe aortic root dilation coupled to aortic valve disease requires root replacement in patients with a tricuspid or bicuspid aortic valve. Commonly, an aortic valve replacement and supracoronary ascending aorta replacement (AVRSCAAR) procedure has been used for patients who have a mild to moderately dilated sinus segment. One advantage of the procedure is that it retains the sinus of Valsalva (SOV) and preserves the intact coronary ostia.
However, the long-term behavior and risk of aortic events for the retained SOV in both BAV and TAV patients remains unclear, according to Dr. Milewski and her colleagues.
Previous researchers have suggested that patients with BAV and TAV have different rates of complications of the remaining aorta and dilation of the proximal aorta and retained sinus segment. In addition, it has been suggested that the cause of aortic dilation is different in patients with aortic stenosis (AS) and aortic insufficiency (AI) and is based on TAV and BAV morphology, histology, and hemodynamic flow patterns.
However, in the August issue of the Journal of Thoracic and Cardiovascular Surgery, Dr. Milewski and her colleagues reported on their study showing that, in patients with nonaneurysmal SOV undergoing AVRSCAAR, the sinus of Valsalva segment can be preserved regardless of the type of valvular pathology (aortic stenosis vs. aortic insufficiency) or valvular morphology (BAV vs. TAV).
The researchers retrospectively reviewed a prospectively maintained institutional database to stratify all patients by BAV or TAV valvular pathology with concomitant ascending aortic aneurysm who underwent an elective AVRSCAAR from 2002 to 2015 (J Thorac Cardiovasc Surg. 2017;154:421-32).
The distribution of the 428 patients meeting inclusion criteria by subgroups was: BAV group (254 patients: BAV-AS = 178; BAV-AI = 76); TAV group (174 patients: TAV-AS = 61; TAV-AI =113). Preoperative sinus of Valsalva dimensions were divided into 3 subgroups (less than 40 mm, 40-45 mm, and greater than 45 mm).
The mean patient age for patients with BAV and TAV was 59 years and 72 years (P less than .001), respectively (with 78% with BAV being men and 57% with TAV being men). There was a significantly higher subpopulation of AS in the BAV cohort vs. TAV-AS (70% vs. 35%; P less than .001).
With regard to SOV sizing, there was no significant difference in mean preoperative aortic root diameters between BAV and TAV cohorts for the AS or AI subpopulations.
In-hospital/30-day mortality was significantly higher in patients with TAV (5.2%) than in patients with BAV (1.6%, P = .033). In addition, the incidence of transient ischemic attack/stroke was significantly higher in the TAV group (3.4%) vs. the BAV group (0.8%, P = .04).
Valvular morphology and pathology at baseline, preoperative SOV diameter, postoperative time course, and interaction effect of preoperative SOV diameters and postoperative time course were used as covariates to assess outcomes. Within-subject and within–stratified subgroup comparison failed to show main effects across the follow-up times on postoperative SOV size patterns (P = .935), implying that the SOV trends were stable and sustained (discharge to greater than or equal to 10 years) irrespective of valvular morphology and pathology (BAV-AI, BAV-AS, TAV-AI, and TAV-AS).
Preoperative SOV dimensions significantly affected the retained postoperative sinus dimensions (P less than .001), according to Dr. Milewski and her colleagues.
The data indicated that an initial and pronounced postoperative decrease in SOV dimensions occurs with AVRSCAAR independently of aortic valve morphology, aortic valve pathology, and age, they added.
The 10-year freedom from aortic reoperation rates were 97% and 95% in the BAV and TAV subgroups, respectively. The BAV group had significantly improved reoperation-free survival, compared with the TAV group (P less than .001), while the type of valvular pathology within each group did not show a significant survival difference.
“Irrespective of the aortic valve morphology or valve pathology, in patients with mild to moderate aortic root dilatation (less than 45 mm), preservation of the SOV segment in the context of an AVRSCAAR procedure is justified. Continued further follow-up will be important to understand the long-term outcomes of sinus preservation, especially in the younger population with BAVs,” the researchers concluded.
The authors reported having no financial conflicts to disclose.
The sinus of Valsalva segment can be preserved during aortic valve replacement irrespective of the type of valve pathology, according to a recent study by Rita Karianna Milewski, MD, and her colleagues at the Hospital of the University of Pennsylvania, Philadelphia.
Severe aortic root dilation coupled to aortic valve disease requires root replacement in patients with a tricuspid or bicuspid aortic valve. Commonly, an aortic valve replacement and supracoronary ascending aorta replacement (AVRSCAAR) procedure has been used for patients who have a mild to moderately dilated sinus segment. One advantage of the procedure is that it retains the sinus of Valsalva (SOV) and preserves the intact coronary ostia.
However, the long-term behavior and risk of aortic events for the retained SOV in both BAV and TAV patients remains unclear, according to Dr. Milewski and her colleagues.
Previous researchers have suggested that patients with BAV and TAV have different rates of complications of the remaining aorta and dilation of the proximal aorta and retained sinus segment. In addition, it has been suggested that the cause of aortic dilation is different in patients with aortic stenosis (AS) and aortic insufficiency (AI) and is based on TAV and BAV morphology, histology, and hemodynamic flow patterns.
However, in the August issue of the Journal of Thoracic and Cardiovascular Surgery, Dr. Milewski and her colleagues reported on their study showing that, in patients with nonaneurysmal SOV undergoing AVRSCAAR, the sinus of Valsalva segment can be preserved regardless of the type of valvular pathology (aortic stenosis vs. aortic insufficiency) or valvular morphology (BAV vs. TAV).
The researchers retrospectively reviewed a prospectively maintained institutional database to stratify all patients by BAV or TAV valvular pathology with concomitant ascending aortic aneurysm who underwent an elective AVRSCAAR from 2002 to 2015 (J Thorac Cardiovasc Surg. 2017;154:421-32).
The distribution of the 428 patients meeting inclusion criteria by subgroups was: BAV group (254 patients: BAV-AS = 178; BAV-AI = 76); TAV group (174 patients: TAV-AS = 61; TAV-AI =113). Preoperative sinus of Valsalva dimensions were divided into 3 subgroups (less than 40 mm, 40-45 mm, and greater than 45 mm).
The mean patient age for patients with BAV and TAV was 59 years and 72 years (P less than .001), respectively (with 78% with BAV being men and 57% with TAV being men). There was a significantly higher subpopulation of AS in the BAV cohort vs. TAV-AS (70% vs. 35%; P less than .001).
With regard to SOV sizing, there was no significant difference in mean preoperative aortic root diameters between BAV and TAV cohorts for the AS or AI subpopulations.
In-hospital/30-day mortality was significantly higher in patients with TAV (5.2%) than in patients with BAV (1.6%, P = .033). In addition, the incidence of transient ischemic attack/stroke was significantly higher in the TAV group (3.4%) vs. the BAV group (0.8%, P = .04).
Valvular morphology and pathology at baseline, preoperative SOV diameter, postoperative time course, and interaction effect of preoperative SOV diameters and postoperative time course were used as covariates to assess outcomes. Within-subject and within–stratified subgroup comparison failed to show main effects across the follow-up times on postoperative SOV size patterns (P = .935), implying that the SOV trends were stable and sustained (discharge to greater than or equal to 10 years) irrespective of valvular morphology and pathology (BAV-AI, BAV-AS, TAV-AI, and TAV-AS).
Preoperative SOV dimensions significantly affected the retained postoperative sinus dimensions (P less than .001), according to Dr. Milewski and her colleagues.
The data indicated that an initial and pronounced postoperative decrease in SOV dimensions occurs with AVRSCAAR independently of aortic valve morphology, aortic valve pathology, and age, they added.
The 10-year freedom from aortic reoperation rates were 97% and 95% in the BAV and TAV subgroups, respectively. The BAV group had significantly improved reoperation-free survival, compared with the TAV group (P less than .001), while the type of valvular pathology within each group did not show a significant survival difference.
“Irrespective of the aortic valve morphology or valve pathology, in patients with mild to moderate aortic root dilatation (less than 45 mm), preservation of the SOV segment in the context of an AVRSCAAR procedure is justified. Continued further follow-up will be important to understand the long-term outcomes of sinus preservation, especially in the younger population with BAVs,” the researchers concluded.
The authors reported having no financial conflicts to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:
Major finding: The 10-year freedom from aortic reoperation rates were 97% and 95% in the BAV and TAV subgroups, respectively.
Data source: A retrospective review of 428 patients in a prospectively maintained database who met study inclusion criteria and were operated on between 2002 and 2015.
Disclosures: The authors reported having no financial conflicts to disclose.