User login
Lung cryobiopsies could reduce need for surgical biopsy
LONDON – The vast majority of surgical lung biopsies currently used to diagnose interstitial lung diseases (ILDs) could be avoided, suggests research presented at the annual congress of the European Respiratory Society.
During an oral presentation, Benjamin Bondue, MD, of Hopital Erasme, Brussels, presented the preliminary results of a Belgian prospective study evaluating the role of transbronchial lung cryobiopsies in 24 patients with undefined ILD treated at three participating centers.
Cryobiopsies were found to have a diagnostic yield of 79%, meaning that patients might be able to avoid undergoing a more invasive surgical removal of tissue in many cases. Compared with surgical biopsy, cryobiopsies offered the potential advantage of lower morbidity and shorter hospitalization time, Dr. Bondue said. He reported that patients needed to stay in hospital just 1.2 days after the procedure in the study.
“Our data also show that there is some benefit of surgical lung biopsy after cryobiopsy if we identify an NSIP [nonspecific interstitial pneumonia] pattern or idiopathic conditions, or if we cannot obtain a clear pathological diagnosis,” he reported. Acknowledging the study was small and conducted in a single center, he said the use of cryobiopsies following surgical biopsy might be worth further study.
Transbronchial lung cryobiopsy is a relatively new technique that uses a cryoprobe inserted down through a bronchoscope about 1-2 cm from the thoracic wall. Once in place, the probe is cooled for between 3 and 6 seconds, lung tissue freezes to the probe, and the probe and bronchoscope are removed together. This method allows for larger samples of tissue to be taken than does traditional transbronchial biopsy, which involves using large forceps to obtain tissue samples (Respirology. 2014;19:645-54).
In the Belgian study, Dr. Bondue noted that a Fogarty balloon was used to control any bleeding and that four transbronchial lung cryobiopsies were obtained from two different segments of the same lobe of a patient’s lungs. All biopsies were then analyzed by an expert pathologist in ILDs, and reviewed by two other expert pathologists when needed. The mean sample size obtained was 16 mm2.
The patients included in the study had undergone chest X-ray and had inconclusive findings in the majority (84%) of cases. They then had the option to undergo cryobiopsy or surgical lung biopsy, with the latter performed following discussion among a multidisciplinary team’s members.
Following cryobiopsy, 16 of the 24 patients – who were a mean age of 62 years, and over half of whom were past (56%) or current (12%) smokers – were diagnosed with a specific pattern of ILD not due to NSIP. Of the 16 cases, 6 were due to hypersensitive pneumonitis, 4 were due to interstitial pulmonary fibrosis, and 2 were due to sarcoidosis. The other four cases included patients with one of the following conditions: adenocarcinoma, desquamative interstitial pneumonia, eosinophilic pneumonia, and amyloidosis.
Six of the 24 cases were defined as NSIP, with 2 reclassified as definite and 1 as probable hypersensitive pneumonitis, after discussion within the multidisciplinary team.
Five patients – three who had been diagnosed with NSIP and two who had been given no pathological diagnosis after cryobiopsy – underwent surgical lung biopsy. Of these, following the surgical biopsies, only one patient was considered to have NSIP and the other four were eventually diagnosed with interstitial pulmonary fibrosis.
In terms of safety, five patients experienced pneumothorax, two patients required chest drainage, two needed simple aspiration and one underwent observation. In the majority of cases, patients experienced mild bleeding, with only one patient having experienced severe bleeding. During this study, none of the participants experienced significant chest pain, acute exacerbations, or infections, and none of them died.
Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
LONDON – The vast majority of surgical lung biopsies currently used to diagnose interstitial lung diseases (ILDs) could be avoided, suggests research presented at the annual congress of the European Respiratory Society.
During an oral presentation, Benjamin Bondue, MD, of Hopital Erasme, Brussels, presented the preliminary results of a Belgian prospective study evaluating the role of transbronchial lung cryobiopsies in 24 patients with undefined ILD treated at three participating centers.
Cryobiopsies were found to have a diagnostic yield of 79%, meaning that patients might be able to avoid undergoing a more invasive surgical removal of tissue in many cases. Compared with surgical biopsy, cryobiopsies offered the potential advantage of lower morbidity and shorter hospitalization time, Dr. Bondue said. He reported that patients needed to stay in hospital just 1.2 days after the procedure in the study.
“Our data also show that there is some benefit of surgical lung biopsy after cryobiopsy if we identify an NSIP [nonspecific interstitial pneumonia] pattern or idiopathic conditions, or if we cannot obtain a clear pathological diagnosis,” he reported. Acknowledging the study was small and conducted in a single center, he said the use of cryobiopsies following surgical biopsy might be worth further study.
Transbronchial lung cryobiopsy is a relatively new technique that uses a cryoprobe inserted down through a bronchoscope about 1-2 cm from the thoracic wall. Once in place, the probe is cooled for between 3 and 6 seconds, lung tissue freezes to the probe, and the probe and bronchoscope are removed together. This method allows for larger samples of tissue to be taken than does traditional transbronchial biopsy, which involves using large forceps to obtain tissue samples (Respirology. 2014;19:645-54).
In the Belgian study, Dr. Bondue noted that a Fogarty balloon was used to control any bleeding and that four transbronchial lung cryobiopsies were obtained from two different segments of the same lobe of a patient’s lungs. All biopsies were then analyzed by an expert pathologist in ILDs, and reviewed by two other expert pathologists when needed. The mean sample size obtained was 16 mm2.
The patients included in the study had undergone chest X-ray and had inconclusive findings in the majority (84%) of cases. They then had the option to undergo cryobiopsy or surgical lung biopsy, with the latter performed following discussion among a multidisciplinary team’s members.
Following cryobiopsy, 16 of the 24 patients – who were a mean age of 62 years, and over half of whom were past (56%) or current (12%) smokers – were diagnosed with a specific pattern of ILD not due to NSIP. Of the 16 cases, 6 were due to hypersensitive pneumonitis, 4 were due to interstitial pulmonary fibrosis, and 2 were due to sarcoidosis. The other four cases included patients with one of the following conditions: adenocarcinoma, desquamative interstitial pneumonia, eosinophilic pneumonia, and amyloidosis.
Six of the 24 cases were defined as NSIP, with 2 reclassified as definite and 1 as probable hypersensitive pneumonitis, after discussion within the multidisciplinary team.
Five patients – three who had been diagnosed with NSIP and two who had been given no pathological diagnosis after cryobiopsy – underwent surgical lung biopsy. Of these, following the surgical biopsies, only one patient was considered to have NSIP and the other four were eventually diagnosed with interstitial pulmonary fibrosis.
In terms of safety, five patients experienced pneumothorax, two patients required chest drainage, two needed simple aspiration and one underwent observation. In the majority of cases, patients experienced mild bleeding, with only one patient having experienced severe bleeding. During this study, none of the participants experienced significant chest pain, acute exacerbations, or infections, and none of them died.
Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
LONDON – The vast majority of surgical lung biopsies currently used to diagnose interstitial lung diseases (ILDs) could be avoided, suggests research presented at the annual congress of the European Respiratory Society.
During an oral presentation, Benjamin Bondue, MD, of Hopital Erasme, Brussels, presented the preliminary results of a Belgian prospective study evaluating the role of transbronchial lung cryobiopsies in 24 patients with undefined ILD treated at three participating centers.
Cryobiopsies were found to have a diagnostic yield of 79%, meaning that patients might be able to avoid undergoing a more invasive surgical removal of tissue in many cases. Compared with surgical biopsy, cryobiopsies offered the potential advantage of lower morbidity and shorter hospitalization time, Dr. Bondue said. He reported that patients needed to stay in hospital just 1.2 days after the procedure in the study.
“Our data also show that there is some benefit of surgical lung biopsy after cryobiopsy if we identify an NSIP [nonspecific interstitial pneumonia] pattern or idiopathic conditions, or if we cannot obtain a clear pathological diagnosis,” he reported. Acknowledging the study was small and conducted in a single center, he said the use of cryobiopsies following surgical biopsy might be worth further study.
Transbronchial lung cryobiopsy is a relatively new technique that uses a cryoprobe inserted down through a bronchoscope about 1-2 cm from the thoracic wall. Once in place, the probe is cooled for between 3 and 6 seconds, lung tissue freezes to the probe, and the probe and bronchoscope are removed together. This method allows for larger samples of tissue to be taken than does traditional transbronchial biopsy, which involves using large forceps to obtain tissue samples (Respirology. 2014;19:645-54).
In the Belgian study, Dr. Bondue noted that a Fogarty balloon was used to control any bleeding and that four transbronchial lung cryobiopsies were obtained from two different segments of the same lobe of a patient’s lungs. All biopsies were then analyzed by an expert pathologist in ILDs, and reviewed by two other expert pathologists when needed. The mean sample size obtained was 16 mm2.
The patients included in the study had undergone chest X-ray and had inconclusive findings in the majority (84%) of cases. They then had the option to undergo cryobiopsy or surgical lung biopsy, with the latter performed following discussion among a multidisciplinary team’s members.
Following cryobiopsy, 16 of the 24 patients – who were a mean age of 62 years, and over half of whom were past (56%) or current (12%) smokers – were diagnosed with a specific pattern of ILD not due to NSIP. Of the 16 cases, 6 were due to hypersensitive pneumonitis, 4 were due to interstitial pulmonary fibrosis, and 2 were due to sarcoidosis. The other four cases included patients with one of the following conditions: adenocarcinoma, desquamative interstitial pneumonia, eosinophilic pneumonia, and amyloidosis.
Six of the 24 cases were defined as NSIP, with 2 reclassified as definite and 1 as probable hypersensitive pneumonitis, after discussion within the multidisciplinary team.
Five patients – three who had been diagnosed with NSIP and two who had been given no pathological diagnosis after cryobiopsy – underwent surgical lung biopsy. Of these, following the surgical biopsies, only one patient was considered to have NSIP and the other four were eventually diagnosed with interstitial pulmonary fibrosis.
In terms of safety, five patients experienced pneumothorax, two patients required chest drainage, two needed simple aspiration and one underwent observation. In the majority of cases, patients experienced mild bleeding, with only one patient having experienced severe bleeding. During this study, none of the participants experienced significant chest pain, acute exacerbations, or infections, and none of them died.
Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
AT THE ERS CONGRESS 2016 LONDON
Key clinical point: Transbronchial lung cryobiopsies are useful for the diagnosis of interstitial lung diseases and could help avoid surgical lung biopsies.
Major finding: Transbronchial lung cryobiopsy had a diagnostic yield of 79%.
Data source: Single-center study of 24 patients with interstitial lung diseases who underwent transbronchial lung cryobiopsies, surgical lung biopsies, or both.
Disclosures: Dr. Bondue has received research grants and fees for consulting from Boehringer Ingelheim and Roche.
Cerebral protection in TAVI reduces ischemic brain lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
These findings are compelling and encouraging, even though we don’t yet know whether the reduction in the number and volume of ischemic brain lesions translates into clinical benefit.
The results also confirm what previous research has suggested: that emboli to the brain are extremely common and do cause small infarctions detectable on MRI. In this trial, virtually every patient demonstrated such acute lesions, though the vast majority were quite small.
Steven R. Messe, MD, is in the department of neurology at the Hospital of the University of Pennsylvania, Philadelphia. Michael J. Mack, MD, is in the department of cardiac surgery at The Heart Hospital Baylor Plano in Plano, Tex. Dr. Messe reported ties to GlaxoSmithKline; Dr. Mack reported having no relevant financial disclosures. Dr. Messe and Dr. Mack made these remarks in an editorial accompanying Dr. Haussig’s report (JAMA 2016;316[6]:587-8).
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Key clinical point: In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions.
Major finding: At 2 days, the number of new brain lesions was markedly lower in the filter group than in the control group (8 vs. 16), as was the lesion volume (466 mm vs. 800 mm).
Data source: A prospective single-center randomized clinical trial involving 100 patients undergoing TAVI for severe aortic stenosis.
Disclosures: This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Survival shorter in extended-criteria lung recipients
The availability of lungs for transplant has been severely limited by usable donors, but organs from so-called extended criteria donors – those aged 65 years or older, had a 20 pack-years or more smoking history or history of diabetes mellitus, or were black – were found to be associated with shorter survival than lungs from standard donor lungs, and recipients with more severe lung disease had the lowest survival rates from extended-criteria organs, an analysis of the national donor database found.
“Matching donor quality to recipient severity is critical to achieve optimal outcomes in lung transplantation,” Matthew J. Mulligan, MD, and his colleagues from the University of Maryland, Baltimore, said in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:891-8). Dr. Mulligan previously presented the study results in April 2015 at the annual meeting of the American Association for Thoracic Surgery in Seattle.
The researchers analyzed 10,995 patients who received donor lungs between May 2005 and December 2012, 3,792 of whom received extended-criteria donor (ECD) organs. The study population was taken from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database. Dr. Mulligan and his coauthors said this is the largest study examining ECD in lung transplants to date.
The goal of the study was to identify donor factors associated with reduced 1-year survival after transplantation, Dr. Mulligan and his colleagues said. “In the current literature, there is a paucity of data to guide the decision of matching donor quality to recipient severity,” the study authors said.
Recipients of extended-criteria lungs had a 41% increased risk of death, compared with recipients standard donor lungs, but individuals with more severe lung disease were at even greater risk with extended-criterial lungs, Dr. Mulligan and his colleagues said. Those who had a lung allocation score (LAS) less than 70 had a 1-year survival of 87% with standard donor lungs vs. 82% with extended-criteria lungs, while those who had a LAS of 70 or greater had survival rates of 80% and 72%, respectively.
Other donor factors that were inconsequential in recipient survival, Dr. Mulligan and his coauthors reported, included an abnormal chest x-ray, purulent secretions on bronchoscopy, blood type, mechanism of death (stroke, blunt trauma, gunshot, asphyxiation, and so on), or diagnosis of coronary artery disease and hypertension.
The researchers also did a Cox regression analysis, and found that recipients of extended-criteria lungs with a LAS greater than 70 had an 81% greater risk of death, compared with 37% for those with a LAS of 70 or greater who received standard-donor lungs, and 42% with a LAS of 70 or less and an extended-criteria donor lung.
These findings support the idea of not using ECD lungs in high-risk individuals with LAS greater than 70. “More important, ECD lungs were associated with the worst survival when transplanted into high-risk recipients,” Dr. Mulligan and his colleagues said.
The authors did acknowledge the inherent limitations of a retrospective analysis, but the large patient population is a redeeming factor of the study, Dr. Mulligan and his colleagues said. “Notwithstanding these limitations, the current study provides a rigorous analysis of a large number of lung transplants in the modern era, and the results reported will be useful to the lung transplant community,” the study authors said.
Dr. Mulligan and his coauthors had no relationships to disclose.
This study provides “greater clarity to the definition and significance of using lungs from an extended-criteria donor,” Benjamin Wei, MD, of the University of Alabama at Birmingham said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:899-900). “Now, we have more data about what constitutes an ECD for lung transplantation.”
The study also brought clarity on components of donor factors that do not affect survival – namely radiologic, bronchoscope, or laboratory criteria – Dr. Wei said. At the same time, the study raises questions about how transplant surgeons should use the findings. “Do we shy away from using donors with these high risk factors in low-risk recipients, high-risk recipients, neither, or both?” Dr. Wei asks. The study did not compare ECD lungs vs. no transplant, and becoming more selective in donors could cause more patients to die on the waiting list, he said.
A host of other questions also remain unanswered, Dr. Wei said, such as how a single standard-donor lung transplant compares with bilateral ECD transplants, or a single ECD lung vs. bilateral ECD lungs, and if use of ECD lungs by the criteria Dr. Mulligan and his coauthors outlined influences allograft patient survival.
“Of note, this study also did not include recipients receiving donor after cardiac death lungs or extracorporeal membrane oxygenation, both increasingly common situations,” he said. Nonetheless, the findings provide more information that transplant surgeons can base their decision-making on.
Dr. Wei had no financial relationships to disclose.
This study provides “greater clarity to the definition and significance of using lungs from an extended-criteria donor,” Benjamin Wei, MD, of the University of Alabama at Birmingham said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:899-900). “Now, we have more data about what constitutes an ECD for lung transplantation.”
The study also brought clarity on components of donor factors that do not affect survival – namely radiologic, bronchoscope, or laboratory criteria – Dr. Wei said. At the same time, the study raises questions about how transplant surgeons should use the findings. “Do we shy away from using donors with these high risk factors in low-risk recipients, high-risk recipients, neither, or both?” Dr. Wei asks. The study did not compare ECD lungs vs. no transplant, and becoming more selective in donors could cause more patients to die on the waiting list, he said.
A host of other questions also remain unanswered, Dr. Wei said, such as how a single standard-donor lung transplant compares with bilateral ECD transplants, or a single ECD lung vs. bilateral ECD lungs, and if use of ECD lungs by the criteria Dr. Mulligan and his coauthors outlined influences allograft patient survival.
“Of note, this study also did not include recipients receiving donor after cardiac death lungs or extracorporeal membrane oxygenation, both increasingly common situations,” he said. Nonetheless, the findings provide more information that transplant surgeons can base their decision-making on.
Dr. Wei had no financial relationships to disclose.
This study provides “greater clarity to the definition and significance of using lungs from an extended-criteria donor,” Benjamin Wei, MD, of the University of Alabama at Birmingham said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:899-900). “Now, we have more data about what constitutes an ECD for lung transplantation.”
The study also brought clarity on components of donor factors that do not affect survival – namely radiologic, bronchoscope, or laboratory criteria – Dr. Wei said. At the same time, the study raises questions about how transplant surgeons should use the findings. “Do we shy away from using donors with these high risk factors in low-risk recipients, high-risk recipients, neither, or both?” Dr. Wei asks. The study did not compare ECD lungs vs. no transplant, and becoming more selective in donors could cause more patients to die on the waiting list, he said.
A host of other questions also remain unanswered, Dr. Wei said, such as how a single standard-donor lung transplant compares with bilateral ECD transplants, or a single ECD lung vs. bilateral ECD lungs, and if use of ECD lungs by the criteria Dr. Mulligan and his coauthors outlined influences allograft patient survival.
“Of note, this study also did not include recipients receiving donor after cardiac death lungs or extracorporeal membrane oxygenation, both increasingly common situations,” he said. Nonetheless, the findings provide more information that transplant surgeons can base their decision-making on.
Dr. Wei had no financial relationships to disclose.
The availability of lungs for transplant has been severely limited by usable donors, but organs from so-called extended criteria donors – those aged 65 years or older, had a 20 pack-years or more smoking history or history of diabetes mellitus, or were black – were found to be associated with shorter survival than lungs from standard donor lungs, and recipients with more severe lung disease had the lowest survival rates from extended-criteria organs, an analysis of the national donor database found.
“Matching donor quality to recipient severity is critical to achieve optimal outcomes in lung transplantation,” Matthew J. Mulligan, MD, and his colleagues from the University of Maryland, Baltimore, said in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:891-8). Dr. Mulligan previously presented the study results in April 2015 at the annual meeting of the American Association for Thoracic Surgery in Seattle.
The researchers analyzed 10,995 patients who received donor lungs between May 2005 and December 2012, 3,792 of whom received extended-criteria donor (ECD) organs. The study population was taken from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database. Dr. Mulligan and his coauthors said this is the largest study examining ECD in lung transplants to date.
The goal of the study was to identify donor factors associated with reduced 1-year survival after transplantation, Dr. Mulligan and his colleagues said. “In the current literature, there is a paucity of data to guide the decision of matching donor quality to recipient severity,” the study authors said.
Recipients of extended-criteria lungs had a 41% increased risk of death, compared with recipients standard donor lungs, but individuals with more severe lung disease were at even greater risk with extended-criterial lungs, Dr. Mulligan and his colleagues said. Those who had a lung allocation score (LAS) less than 70 had a 1-year survival of 87% with standard donor lungs vs. 82% with extended-criteria lungs, while those who had a LAS of 70 or greater had survival rates of 80% and 72%, respectively.
Other donor factors that were inconsequential in recipient survival, Dr. Mulligan and his coauthors reported, included an abnormal chest x-ray, purulent secretions on bronchoscopy, blood type, mechanism of death (stroke, blunt trauma, gunshot, asphyxiation, and so on), or diagnosis of coronary artery disease and hypertension.
The researchers also did a Cox regression analysis, and found that recipients of extended-criteria lungs with a LAS greater than 70 had an 81% greater risk of death, compared with 37% for those with a LAS of 70 or greater who received standard-donor lungs, and 42% with a LAS of 70 or less and an extended-criteria donor lung.
These findings support the idea of not using ECD lungs in high-risk individuals with LAS greater than 70. “More important, ECD lungs were associated with the worst survival when transplanted into high-risk recipients,” Dr. Mulligan and his colleagues said.
The authors did acknowledge the inherent limitations of a retrospective analysis, but the large patient population is a redeeming factor of the study, Dr. Mulligan and his colleagues said. “Notwithstanding these limitations, the current study provides a rigorous analysis of a large number of lung transplants in the modern era, and the results reported will be useful to the lung transplant community,” the study authors said.
Dr. Mulligan and his coauthors had no relationships to disclose.
The availability of lungs for transplant has been severely limited by usable donors, but organs from so-called extended criteria donors – those aged 65 years or older, had a 20 pack-years or more smoking history or history of diabetes mellitus, or were black – were found to be associated with shorter survival than lungs from standard donor lungs, and recipients with more severe lung disease had the lowest survival rates from extended-criteria organs, an analysis of the national donor database found.
“Matching donor quality to recipient severity is critical to achieve optimal outcomes in lung transplantation,” Matthew J. Mulligan, MD, and his colleagues from the University of Maryland, Baltimore, said in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:891-8). Dr. Mulligan previously presented the study results in April 2015 at the annual meeting of the American Association for Thoracic Surgery in Seattle.
The researchers analyzed 10,995 patients who received donor lungs between May 2005 and December 2012, 3,792 of whom received extended-criteria donor (ECD) organs. The study population was taken from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database. Dr. Mulligan and his coauthors said this is the largest study examining ECD in lung transplants to date.
The goal of the study was to identify donor factors associated with reduced 1-year survival after transplantation, Dr. Mulligan and his colleagues said. “In the current literature, there is a paucity of data to guide the decision of matching donor quality to recipient severity,” the study authors said.
Recipients of extended-criteria lungs had a 41% increased risk of death, compared with recipients standard donor lungs, but individuals with more severe lung disease were at even greater risk with extended-criterial lungs, Dr. Mulligan and his colleagues said. Those who had a lung allocation score (LAS) less than 70 had a 1-year survival of 87% with standard donor lungs vs. 82% with extended-criteria lungs, while those who had a LAS of 70 or greater had survival rates of 80% and 72%, respectively.
Other donor factors that were inconsequential in recipient survival, Dr. Mulligan and his coauthors reported, included an abnormal chest x-ray, purulent secretions on bronchoscopy, blood type, mechanism of death (stroke, blunt trauma, gunshot, asphyxiation, and so on), or diagnosis of coronary artery disease and hypertension.
The researchers also did a Cox regression analysis, and found that recipients of extended-criteria lungs with a LAS greater than 70 had an 81% greater risk of death, compared with 37% for those with a LAS of 70 or greater who received standard-donor lungs, and 42% with a LAS of 70 or less and an extended-criteria donor lung.
These findings support the idea of not using ECD lungs in high-risk individuals with LAS greater than 70. “More important, ECD lungs were associated with the worst survival when transplanted into high-risk recipients,” Dr. Mulligan and his colleagues said.
The authors did acknowledge the inherent limitations of a retrospective analysis, but the large patient population is a redeeming factor of the study, Dr. Mulligan and his colleagues said. “Notwithstanding these limitations, the current study provides a rigorous analysis of a large number of lung transplants in the modern era, and the results reported will be useful to the lung transplant community,” the study authors said.
Dr. Mulligan and his coauthors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Lung transplant recipients who received extended-criteria donor (ECD) lungs have lower rates of 1-year survival than recipients of standard donor lungs.
Major finding: Recipients of ECD lungs had a 41% higher risk of death than recipients of standard lungs, and those who had more severe lung disease had lower rates of 1-year survival after receiving ECD lungs, compared with standard donor lungs.
Data source: Retrospective analysis of 10,995 lung recipients, from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database, 3,792 of whom who received extended-criteria donor organs over 7.5 years.
Disclosures: Dr. Mulligan and his coauthors had no financial relationships to disclose.
Transcatheter mitral valve therapy at ‘event horizon’
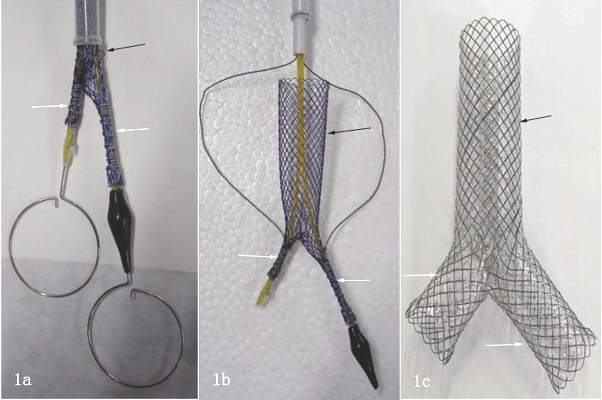
As investigational transcatheter mitral valve therapies continue to explode onto the scene, cardiac surgeons must act now to seize and assert their place in the multidisciplinary team with interventional, imaging, and heart failure colleagues to deliver these treatments to people with complex mitral valve regurgitation, an expert opinion report in the August issue of the Journal of Thoracic and Cardiovascular Surgery states (J Thorac Cardiovasc Surg. 2016;152:330-6).
“There is a growing population of patients with primary and secondary mitral regurgitation underserved by surgical therapy because of comorbid risk,” Vinay Badhwar, MD, of West Virginia University and his colleagues said. “This has led to a tremendous activity of device development.”
With more than 25 different transcatheter mitral valve devices in development (MitraClip, Abbott Vascular, is the only FDA-approved transcatheter for primary mitral regurgitation [MR]), cardiac surgeons will soon have the tools to offer transcatheter mitral valve repair (TMVr) and transcatheter mitral valve replacement (TMVR) to more complex patients who have MR along with other health problems. Today about half of those patients do not get surgery because they are too frail, Dr. Badhwar and his colleagues said.
The authors used the astrophysical phrase “event horizon” to define the current state of transcatheter mitral valve therapies – “a point of no return.” They expect surgery to remain the treatment of choice for MR for the next 10 years. “However, as our patient cohorts become increasingly more complex and transcatheter mitral therapies more facile, the day when this will become a daily clinical reality will soon be upon us,” Dr. Badhwar and his colleagues said.
The multidisciplinary team approach will be integral in achieving the full potential of transcatheter mitral valve replacement or repair, Dr. Badhwar and his coauthors said. While surgery is the most effective treatment for primary MR, cardiac surgeons are challenged to introduce transcatheter treatments in patients who have other health problems. “The best way to adjudicate innovative surgical and interventional mitral therapies is through a robust collaboration within a well-functioning heart team that includes not only a cardiac surgeon and interventional cardiologist but also an imaging specialist,” the authors said.
The time to reach out to those other specialties is now, before those investigational devices start emerging from the development pipeline, Dr. Badhwar and his colleagues said. “This will soon enable the team-based mitral specialist to be facile in safely transitioning patients from open mitral surgery to TMVr or TMVR as most appropriate for durable long-term outcomes.”
Dr. Badhwar disclosed he is an uncompensated member of the Abbott Vascular advisory board. Coauthor Vinod Thourani, MD, disclosed relationships with Edwards Lifesciences, Medtronic Cardiovascular, Abbott Vascular, St. Jude Medical, Mitralign, and AtriCure. Coauthor Michael Mack, MD, serves on the Edwards Lifesciences steering committee Partner Trial and is an uncompensated co-principal investigator of the Abbott Vascular Clinical Outcomes Assessment of the MitraClip Percutaneous Therapy Trial.
Channeling Bob Dylan’s “The Times They Are A-Changin’” in his invited commentary, W. Randolph Chitwood Jr., MD, of East Carolina University in Greenville, N.C., called Dr. Badhwar’s expert opinion “the clarion call for cardiac surgeons to become engaged in this rapidly evolving parade.”

|
Dr. W. Randolph Chitwood Jr. |
The evidence supporting the safety and efficacy of transcatheter aortic valve replacement (TAVR) is already strong, Dr. Chitwood noted. “It seems reasonable to suspect that the evolving pathway for the development of transcatheter mitral valve replacement (TMVR) could recapitulate the success of TAVR, with each generation having improved results,” he said (J Thorac Cardiovasc Surg. 2016;152:336-7).
Cardiac surgeons need to develop alternate access platforms and acquire the skills to use the new generation of transcatheter mitral devices, Dr. Chitwood said. The expert opinion “should encourage cardiac surgeons to become members of a heart team,” he said. “Guidewire skills are at the pinnacle of necessity to remain a player in this new world.”
Dr. Chitwood’s advice to colleagues: “Then you better start swimming or you’ll sink like a stone, For the times they are a-changin’.”
Dr. Chitwood disclosed he is a consultant to Direct Flow Medical and co-principal investigator for the Edwards Lifesciences Transform Trial.
Channeling Bob Dylan’s “The Times They Are A-Changin’” in his invited commentary, W. Randolph Chitwood Jr., MD, of East Carolina University in Greenville, N.C., called Dr. Badhwar’s expert opinion “the clarion call for cardiac surgeons to become engaged in this rapidly evolving parade.”

|
Dr. W. Randolph Chitwood Jr. |
The evidence supporting the safety and efficacy of transcatheter aortic valve replacement (TAVR) is already strong, Dr. Chitwood noted. “It seems reasonable to suspect that the evolving pathway for the development of transcatheter mitral valve replacement (TMVR) could recapitulate the success of TAVR, with each generation having improved results,” he said (J Thorac Cardiovasc Surg. 2016;152:336-7).
Cardiac surgeons need to develop alternate access platforms and acquire the skills to use the new generation of transcatheter mitral devices, Dr. Chitwood said. The expert opinion “should encourage cardiac surgeons to become members of a heart team,” he said. “Guidewire skills are at the pinnacle of necessity to remain a player in this new world.”
Dr. Chitwood’s advice to colleagues: “Then you better start swimming or you’ll sink like a stone, For the times they are a-changin’.”
Dr. Chitwood disclosed he is a consultant to Direct Flow Medical and co-principal investigator for the Edwards Lifesciences Transform Trial.
Channeling Bob Dylan’s “The Times They Are A-Changin’” in his invited commentary, W. Randolph Chitwood Jr., MD, of East Carolina University in Greenville, N.C., called Dr. Badhwar’s expert opinion “the clarion call for cardiac surgeons to become engaged in this rapidly evolving parade.”

|
Dr. W. Randolph Chitwood Jr. |
The evidence supporting the safety and efficacy of transcatheter aortic valve replacement (TAVR) is already strong, Dr. Chitwood noted. “It seems reasonable to suspect that the evolving pathway for the development of transcatheter mitral valve replacement (TMVR) could recapitulate the success of TAVR, with each generation having improved results,” he said (J Thorac Cardiovasc Surg. 2016;152:336-7).
Cardiac surgeons need to develop alternate access platforms and acquire the skills to use the new generation of transcatheter mitral devices, Dr. Chitwood said. The expert opinion “should encourage cardiac surgeons to become members of a heart team,” he said. “Guidewire skills are at the pinnacle of necessity to remain a player in this new world.”
Dr. Chitwood’s advice to colleagues: “Then you better start swimming or you’ll sink like a stone, For the times they are a-changin’.”
Dr. Chitwood disclosed he is a consultant to Direct Flow Medical and co-principal investigator for the Edwards Lifesciences Transform Trial.
As investigational transcatheter mitral valve therapies continue to explode onto the scene, cardiac surgeons must act now to seize and assert their place in the multidisciplinary team with interventional, imaging, and heart failure colleagues to deliver these treatments to people with complex mitral valve regurgitation, an expert opinion report in the August issue of the Journal of Thoracic and Cardiovascular Surgery states (J Thorac Cardiovasc Surg. 2016;152:330-6).
“There is a growing population of patients with primary and secondary mitral regurgitation underserved by surgical therapy because of comorbid risk,” Vinay Badhwar, MD, of West Virginia University and his colleagues said. “This has led to a tremendous activity of device development.”
With more than 25 different transcatheter mitral valve devices in development (MitraClip, Abbott Vascular, is the only FDA-approved transcatheter for primary mitral regurgitation [MR]), cardiac surgeons will soon have the tools to offer transcatheter mitral valve repair (TMVr) and transcatheter mitral valve replacement (TMVR) to more complex patients who have MR along with other health problems. Today about half of those patients do not get surgery because they are too frail, Dr. Badhwar and his colleagues said.
The authors used the astrophysical phrase “event horizon” to define the current state of transcatheter mitral valve therapies – “a point of no return.” They expect surgery to remain the treatment of choice for MR for the next 10 years. “However, as our patient cohorts become increasingly more complex and transcatheter mitral therapies more facile, the day when this will become a daily clinical reality will soon be upon us,” Dr. Badhwar and his colleagues said.
The multidisciplinary team approach will be integral in achieving the full potential of transcatheter mitral valve replacement or repair, Dr. Badhwar and his coauthors said. While surgery is the most effective treatment for primary MR, cardiac surgeons are challenged to introduce transcatheter treatments in patients who have other health problems. “The best way to adjudicate innovative surgical and interventional mitral therapies is through a robust collaboration within a well-functioning heart team that includes not only a cardiac surgeon and interventional cardiologist but also an imaging specialist,” the authors said.
The time to reach out to those other specialties is now, before those investigational devices start emerging from the development pipeline, Dr. Badhwar and his colleagues said. “This will soon enable the team-based mitral specialist to be facile in safely transitioning patients from open mitral surgery to TMVr or TMVR as most appropriate for durable long-term outcomes.”
Dr. Badhwar disclosed he is an uncompensated member of the Abbott Vascular advisory board. Coauthor Vinod Thourani, MD, disclosed relationships with Edwards Lifesciences, Medtronic Cardiovascular, Abbott Vascular, St. Jude Medical, Mitralign, and AtriCure. Coauthor Michael Mack, MD, serves on the Edwards Lifesciences steering committee Partner Trial and is an uncompensated co-principal investigator of the Abbott Vascular Clinical Outcomes Assessment of the MitraClip Percutaneous Therapy Trial.
As investigational transcatheter mitral valve therapies continue to explode onto the scene, cardiac surgeons must act now to seize and assert their place in the multidisciplinary team with interventional, imaging, and heart failure colleagues to deliver these treatments to people with complex mitral valve regurgitation, an expert opinion report in the August issue of the Journal of Thoracic and Cardiovascular Surgery states (J Thorac Cardiovasc Surg. 2016;152:330-6).
“There is a growing population of patients with primary and secondary mitral regurgitation underserved by surgical therapy because of comorbid risk,” Vinay Badhwar, MD, of West Virginia University and his colleagues said. “This has led to a tremendous activity of device development.”
With more than 25 different transcatheter mitral valve devices in development (MitraClip, Abbott Vascular, is the only FDA-approved transcatheter for primary mitral regurgitation [MR]), cardiac surgeons will soon have the tools to offer transcatheter mitral valve repair (TMVr) and transcatheter mitral valve replacement (TMVR) to more complex patients who have MR along with other health problems. Today about half of those patients do not get surgery because they are too frail, Dr. Badhwar and his colleagues said.
The authors used the astrophysical phrase “event horizon” to define the current state of transcatheter mitral valve therapies – “a point of no return.” They expect surgery to remain the treatment of choice for MR for the next 10 years. “However, as our patient cohorts become increasingly more complex and transcatheter mitral therapies more facile, the day when this will become a daily clinical reality will soon be upon us,” Dr. Badhwar and his colleagues said.
The multidisciplinary team approach will be integral in achieving the full potential of transcatheter mitral valve replacement or repair, Dr. Badhwar and his coauthors said. While surgery is the most effective treatment for primary MR, cardiac surgeons are challenged to introduce transcatheter treatments in patients who have other health problems. “The best way to adjudicate innovative surgical and interventional mitral therapies is through a robust collaboration within a well-functioning heart team that includes not only a cardiac surgeon and interventional cardiologist but also an imaging specialist,” the authors said.
The time to reach out to those other specialties is now, before those investigational devices start emerging from the development pipeline, Dr. Badhwar and his colleagues said. “This will soon enable the team-based mitral specialist to be facile in safely transitioning patients from open mitral surgery to TMVr or TMVR as most appropriate for durable long-term outcomes.”
Dr. Badhwar disclosed he is an uncompensated member of the Abbott Vascular advisory board. Coauthor Vinod Thourani, MD, disclosed relationships with Edwards Lifesciences, Medtronic Cardiovascular, Abbott Vascular, St. Jude Medical, Mitralign, and AtriCure. Coauthor Michael Mack, MD, serves on the Edwards Lifesciences steering committee Partner Trial and is an uncompensated co-principal investigator of the Abbott Vascular Clinical Outcomes Assessment of the MitraClip Percutaneous Therapy Trial.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Transcatheter mitral valve repair and replacement technology has reached a critical point that requires cardiac surgeons to assume their place in a multidisciplinary team.
Major finding: One transcatheter device is commercially available in the United States and more than 25 companies have devices in development.
Data source: Review of 22 published reports on transcatheter mitral valve technology.
Disclosures: Dr. Badhwar disclosed he is an uncompensated member of the Abbott Vascular advisory board. Coauthor Vinod Thourani, MD, disclosed relationships with Edwards Lifesciences, Medtronic Cardiovascular, Abbott Vascular, St. Jude Medical, Mitralign and AtriCure. Coauthor Michael Mack, MD, serves on the Edwards Lifesciences steering committee Partner Trial, and is an uncompensated co-principal investigator of the Abbott Vascular Clinical Outcomes Assessment of the MitraClip Percutaneous Therapy Trial.
Think outside the ‘cardiac box’ to predict cardiac injury
WAIKOLOA, HI. – For gunshot wounds, the current “cardiac box” was the poorest predictor of cardiac injury, results from a single-center retrospective study demonstrated.
“We determined that, from a statistical standpoint, the cardiac box should be redefined to include the area of the thorax that extends from the clavicle to xiphoid and from the anterior midline to the posterior midline of the left thorax,” Bryan C. Morse, MD, said in an interview in advance of the annual meeting of the American Association for the Surgery of Trauma. “The classic cardiac box is inadequate to discriminate whether a gunshot wound will create a cardiac injury.”
Dr. Morse of Emory University and Grady Memorial Hospital, Atlanta, and his associates recently published their experience with penetrating cardiac injuries over the past 36 years and documented an increase in the number of cardiac injuries from gunshots over the past 10 years (J. Trauma Acute Care Surg. 2016 Jul 6. doi: 10.1097/TA.0000000000001165). They also noted that several of these injuries were caused by penetrating thoracic wounds outside the cardiac box.
The cardiac box is currently defined as the area of the chest overlying the heart, bounded by the midclavicular lines (laterally) and from the clavicles to the tip of the xiphoid. “Surgical teaching dictates that penetrating injuries (i.e. stab wounds and gunshot wounds) in the box have the highest likelihood of cardiac injury and thereby mandate further evaluation,” Dr. Morse said. “These studies, however, are based on small patient sample sizes in which the majority were stab wound victims and underwent minimal statistical scrutiny.”
In what he said is the largest study of its kind, Dr. Morse and his associates conducted a retrospective review of trauma registry data from Grady’s trauma center and autopsy reports to identify patients with penetrating thoracic gunshot wounds and cardiac injury from 2011 to 2013 and to evaluate the relationship between penetrating injuries and the likelihood of a cardiac injury. Using a circumferential grid system around the thorax, the researchers employed logistic regression analysis to compare differences in rates of cardiac injury from entrance/exit wounds in the cardiac box, versus outside the box. They repeated the process to identify potential regions that yield improved predictions for cardiac injury over the current definition of the cardiac box.
Over the 3-year study period, 263 patients sustained 735 penetrating thoracic wounds, of which 80% were gunshot wounds (GSWs). Most of the patients were males (89%) with a median of two injuries each. After stab wounds were excluded, 277 GSWs to the thorax were included for study and 95 (34%) injured the heart. Of the 233 GSWs entering the cardiac box, 30% caused cardiac injury while, of the 44 GSWs outside the cardiac box, 32% penetrated the heart, suggesting that the current cardiac box is a poor predictor of cardiac injury relative to the thoracic non–cardiac box regions (OR 1.1; P = .71).
The researchers observed that the regions from the anterior to the posterior midline of the left thorax provided the highest positive predictive value, with a sensitivity of 90% and a specificity of 31%, making this region the most statistically significant discriminator of cardiac injury (OR, 4.4; P less than .01). This finding was primarily based on the fact that gunshots to the left lateral chest (an area not currently included in the box) had a high rate of cardiac injury (41%; OR, 1.4).
“The current cardiac box is unable to discriminate between gunshot wounds that will cause a cardiac injury and those that will not,” Dr. Morse said. “Any gunshot wound to the chest can cause a cardiac injury. While clinically relevant box borders would include the left chest, the bottom line for surgeons is to think outside the current cardiac box.”
The improved cardiac box that he and his associates proposed includes the area from the clavicles to the xiphoid and from the anterior to the posterior midline over the left thorax. “While this may be intuitive, it is not what we as surgeons have been teaching,” he said. “Finally, gunshots to areas such as the right posterior and posterolateral chest were associated with rates of cardiac injury greater than 30% despite their distance from the heart. This led us to conclude that a gunshot anywhere to the chest should be considered to potentially cause a cardiac injury.”
Dr. Morse acknowledged certain limitations of the study, including the fact that the study excluded graze wounds and gunshots above the clavicles and below the xiphoid. “However, a small percentage of these did cause cardiac injuries, which emphasizes the point that gunshot wounds from any entrance can cause cardiac injury.”
Invited discussant Nicholas Namias, MD, professor and chief of the division of acute care surgery at Jackson Memorial Hospital, Miami, said that the study by Dr. Morse and his associates “confirms what Dr. [Grace] Rozycki showed 20 years ago: Forget the [cardiac] box; it’s dead. Just throw an ultrasound probe on.”
Dr. Morse reported having no relevant financial disclosures.
WAIKOLOA, HI. – For gunshot wounds, the current “cardiac box” was the poorest predictor of cardiac injury, results from a single-center retrospective study demonstrated.
“We determined that, from a statistical standpoint, the cardiac box should be redefined to include the area of the thorax that extends from the clavicle to xiphoid and from the anterior midline to the posterior midline of the left thorax,” Bryan C. Morse, MD, said in an interview in advance of the annual meeting of the American Association for the Surgery of Trauma. “The classic cardiac box is inadequate to discriminate whether a gunshot wound will create a cardiac injury.”
Dr. Morse of Emory University and Grady Memorial Hospital, Atlanta, and his associates recently published their experience with penetrating cardiac injuries over the past 36 years and documented an increase in the number of cardiac injuries from gunshots over the past 10 years (J. Trauma Acute Care Surg. 2016 Jul 6. doi: 10.1097/TA.0000000000001165). They also noted that several of these injuries were caused by penetrating thoracic wounds outside the cardiac box.
The cardiac box is currently defined as the area of the chest overlying the heart, bounded by the midclavicular lines (laterally) and from the clavicles to the tip of the xiphoid. “Surgical teaching dictates that penetrating injuries (i.e. stab wounds and gunshot wounds) in the box have the highest likelihood of cardiac injury and thereby mandate further evaluation,” Dr. Morse said. “These studies, however, are based on small patient sample sizes in which the majority were stab wound victims and underwent minimal statistical scrutiny.”
In what he said is the largest study of its kind, Dr. Morse and his associates conducted a retrospective review of trauma registry data from Grady’s trauma center and autopsy reports to identify patients with penetrating thoracic gunshot wounds and cardiac injury from 2011 to 2013 and to evaluate the relationship between penetrating injuries and the likelihood of a cardiac injury. Using a circumferential grid system around the thorax, the researchers employed logistic regression analysis to compare differences in rates of cardiac injury from entrance/exit wounds in the cardiac box, versus outside the box. They repeated the process to identify potential regions that yield improved predictions for cardiac injury over the current definition of the cardiac box.
Over the 3-year study period, 263 patients sustained 735 penetrating thoracic wounds, of which 80% were gunshot wounds (GSWs). Most of the patients were males (89%) with a median of two injuries each. After stab wounds were excluded, 277 GSWs to the thorax were included for study and 95 (34%) injured the heart. Of the 233 GSWs entering the cardiac box, 30% caused cardiac injury while, of the 44 GSWs outside the cardiac box, 32% penetrated the heart, suggesting that the current cardiac box is a poor predictor of cardiac injury relative to the thoracic non–cardiac box regions (OR 1.1; P = .71).
The researchers observed that the regions from the anterior to the posterior midline of the left thorax provided the highest positive predictive value, with a sensitivity of 90% and a specificity of 31%, making this region the most statistically significant discriminator of cardiac injury (OR, 4.4; P less than .01). This finding was primarily based on the fact that gunshots to the left lateral chest (an area not currently included in the box) had a high rate of cardiac injury (41%; OR, 1.4).
“The current cardiac box is unable to discriminate between gunshot wounds that will cause a cardiac injury and those that will not,” Dr. Morse said. “Any gunshot wound to the chest can cause a cardiac injury. While clinically relevant box borders would include the left chest, the bottom line for surgeons is to think outside the current cardiac box.”
The improved cardiac box that he and his associates proposed includes the area from the clavicles to the xiphoid and from the anterior to the posterior midline over the left thorax. “While this may be intuitive, it is not what we as surgeons have been teaching,” he said. “Finally, gunshots to areas such as the right posterior and posterolateral chest were associated with rates of cardiac injury greater than 30% despite their distance from the heart. This led us to conclude that a gunshot anywhere to the chest should be considered to potentially cause a cardiac injury.”
Dr. Morse acknowledged certain limitations of the study, including the fact that the study excluded graze wounds and gunshots above the clavicles and below the xiphoid. “However, a small percentage of these did cause cardiac injuries, which emphasizes the point that gunshot wounds from any entrance can cause cardiac injury.”
Invited discussant Nicholas Namias, MD, professor and chief of the division of acute care surgery at Jackson Memorial Hospital, Miami, said that the study by Dr. Morse and his associates “confirms what Dr. [Grace] Rozycki showed 20 years ago: Forget the [cardiac] box; it’s dead. Just throw an ultrasound probe on.”
Dr. Morse reported having no relevant financial disclosures.
WAIKOLOA, HI. – For gunshot wounds, the current “cardiac box” was the poorest predictor of cardiac injury, results from a single-center retrospective study demonstrated.
“We determined that, from a statistical standpoint, the cardiac box should be redefined to include the area of the thorax that extends from the clavicle to xiphoid and from the anterior midline to the posterior midline of the left thorax,” Bryan C. Morse, MD, said in an interview in advance of the annual meeting of the American Association for the Surgery of Trauma. “The classic cardiac box is inadequate to discriminate whether a gunshot wound will create a cardiac injury.”
Dr. Morse of Emory University and Grady Memorial Hospital, Atlanta, and his associates recently published their experience with penetrating cardiac injuries over the past 36 years and documented an increase in the number of cardiac injuries from gunshots over the past 10 years (J. Trauma Acute Care Surg. 2016 Jul 6. doi: 10.1097/TA.0000000000001165). They also noted that several of these injuries were caused by penetrating thoracic wounds outside the cardiac box.
The cardiac box is currently defined as the area of the chest overlying the heart, bounded by the midclavicular lines (laterally) and from the clavicles to the tip of the xiphoid. “Surgical teaching dictates that penetrating injuries (i.e. stab wounds and gunshot wounds) in the box have the highest likelihood of cardiac injury and thereby mandate further evaluation,” Dr. Morse said. “These studies, however, are based on small patient sample sizes in which the majority were stab wound victims and underwent minimal statistical scrutiny.”
In what he said is the largest study of its kind, Dr. Morse and his associates conducted a retrospective review of trauma registry data from Grady’s trauma center and autopsy reports to identify patients with penetrating thoracic gunshot wounds and cardiac injury from 2011 to 2013 and to evaluate the relationship between penetrating injuries and the likelihood of a cardiac injury. Using a circumferential grid system around the thorax, the researchers employed logistic regression analysis to compare differences in rates of cardiac injury from entrance/exit wounds in the cardiac box, versus outside the box. They repeated the process to identify potential regions that yield improved predictions for cardiac injury over the current definition of the cardiac box.
Over the 3-year study period, 263 patients sustained 735 penetrating thoracic wounds, of which 80% were gunshot wounds (GSWs). Most of the patients were males (89%) with a median of two injuries each. After stab wounds were excluded, 277 GSWs to the thorax were included for study and 95 (34%) injured the heart. Of the 233 GSWs entering the cardiac box, 30% caused cardiac injury while, of the 44 GSWs outside the cardiac box, 32% penetrated the heart, suggesting that the current cardiac box is a poor predictor of cardiac injury relative to the thoracic non–cardiac box regions (OR 1.1; P = .71).
The researchers observed that the regions from the anterior to the posterior midline of the left thorax provided the highest positive predictive value, with a sensitivity of 90% and a specificity of 31%, making this region the most statistically significant discriminator of cardiac injury (OR, 4.4; P less than .01). This finding was primarily based on the fact that gunshots to the left lateral chest (an area not currently included in the box) had a high rate of cardiac injury (41%; OR, 1.4).
“The current cardiac box is unable to discriminate between gunshot wounds that will cause a cardiac injury and those that will not,” Dr. Morse said. “Any gunshot wound to the chest can cause a cardiac injury. While clinically relevant box borders would include the left chest, the bottom line for surgeons is to think outside the current cardiac box.”
The improved cardiac box that he and his associates proposed includes the area from the clavicles to the xiphoid and from the anterior to the posterior midline over the left thorax. “While this may be intuitive, it is not what we as surgeons have been teaching,” he said. “Finally, gunshots to areas such as the right posterior and posterolateral chest were associated with rates of cardiac injury greater than 30% despite their distance from the heart. This led us to conclude that a gunshot anywhere to the chest should be considered to potentially cause a cardiac injury.”
Dr. Morse acknowledged certain limitations of the study, including the fact that the study excluded graze wounds and gunshots above the clavicles and below the xiphoid. “However, a small percentage of these did cause cardiac injuries, which emphasizes the point that gunshot wounds from any entrance can cause cardiac injury.”
Invited discussant Nicholas Namias, MD, professor and chief of the division of acute care surgery at Jackson Memorial Hospital, Miami, said that the study by Dr. Morse and his associates “confirms what Dr. [Grace] Rozycki showed 20 years ago: Forget the [cardiac] box; it’s dead. Just throw an ultrasound probe on.”
Dr. Morse reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: The current cardiac box is inadequate to discriminate whether a gunshot wound will create a cardiac injury.
Major finding: Of the 233 gunshot wounds entering the cardiac box, 30% caused cardiac injury while, of the 44 GSWs outside the cardiac box, 32% penetrated the heart, suggesting that the current cardiac box is a poor predictor of cardiac injury relative to the thoracic non–cardiac box regions (OR 1.1; P = .71).
Data source: A retrospective review of 236 patients with penetrating thoracic gunshot wounds and cardiac injury from 2011 to 2013.
Disclosures: Dr. Morse reported having no relevant financial disclosures.
Four factors raise risk of post-TAVR endocarditis
Four factors – younger patient age, male sex, diabetes, and moderate to severe residual aortic regurgitation – are associated with a significantly increased risk of infective endocarditis after transcatheter aortic valve replacement, according to a report published online Sept. 13 in JAMA.
Until now, data pertaining to endocarditis following TAVR “have been limited to case reports and relatively small series with limited follow-up,” said Ander Regueiro, MD, of Laval University, Quebec City, and his associates.
They performed a retrospective analysis of data in a large international registry of TAVR cases to better characterize post-TAVR endocarditis.
Dr. Regueiro and his colleagues focused on 20,006 TAVR procedures done at 47 medical centers in Europe, North America, and South America during a 10-year period. The median time to symptom onset was 5.3 months after the procedure.
Infective endocarditis was definitively diagnosed in 250 of these cases. This incidence is similar to that reported for endocarditis following surgical aortic valve replacement, indicating that TAVR is no less predisposing to endocarditis despite being a less invasive approach.
The mean age of patients who developed post-TAVR endocarditis was 78.9 years, compared with 81.8 years for those who did not (HR, 0.97). The reason for this association is unclear, but it is possible that younger patients chosen for TAVR because of their prohibitive surgical risk carry a higher burden of comorbidity than do older patients. Similarly, 62% of endocarditis cases arose in men (HR, 1.69), and sex differences in comorbid conditions may explain the higher risk among men.
More patients who developed endocarditis had diabetes (41.7%), compared with those who did not develop endocarditis (30%), for an HR of 1.52. And patients who had moderate to severe residual aortic regurgitation after TAVR also were at much higher risk for endocarditis than were those who did not (HR, 2.05), the investigators noted (JAMA. 2016 Sep 13;316[10]:1083-92).
In contrast, factors that were not associated with endocarditis risk included chronic pulmonary disease, type of valve (self-expandable or balloon-expandable), and setting of the procedure (catheterization lab vs. operating room).
The bacteria that most commonly caused infective endocarditis were Enterococci species (24.6% of cases), Staphylococcus aureus (23.8%), and coagulase-negative staphylococci (16.8%). This should be taken into consideration when selecting antibiotics for prophylaxis before TAVR and when choosing empirical antibiotics for treatment while waiting for blood culture results, wrote Dr. Regueiro and his associates.
“This information may help clinicians identify patients at higher risk [for endocarditis] and aid in implementing appropriate preventive measures,” they noted.
This study was supported by a grant from the Alfonso Martin Escudero Foundation. Dr. Regueiro reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Four factors – younger patient age, male sex, diabetes, and moderate to severe residual aortic regurgitation – are associated with a significantly increased risk of infective endocarditis after transcatheter aortic valve replacement, according to a report published online Sept. 13 in JAMA.
Until now, data pertaining to endocarditis following TAVR “have been limited to case reports and relatively small series with limited follow-up,” said Ander Regueiro, MD, of Laval University, Quebec City, and his associates.
They performed a retrospective analysis of data in a large international registry of TAVR cases to better characterize post-TAVR endocarditis.
Dr. Regueiro and his colleagues focused on 20,006 TAVR procedures done at 47 medical centers in Europe, North America, and South America during a 10-year period. The median time to symptom onset was 5.3 months after the procedure.
Infective endocarditis was definitively diagnosed in 250 of these cases. This incidence is similar to that reported for endocarditis following surgical aortic valve replacement, indicating that TAVR is no less predisposing to endocarditis despite being a less invasive approach.
The mean age of patients who developed post-TAVR endocarditis was 78.9 years, compared with 81.8 years for those who did not (HR, 0.97). The reason for this association is unclear, but it is possible that younger patients chosen for TAVR because of their prohibitive surgical risk carry a higher burden of comorbidity than do older patients. Similarly, 62% of endocarditis cases arose in men (HR, 1.69), and sex differences in comorbid conditions may explain the higher risk among men.
More patients who developed endocarditis had diabetes (41.7%), compared with those who did not develop endocarditis (30%), for an HR of 1.52. And patients who had moderate to severe residual aortic regurgitation after TAVR also were at much higher risk for endocarditis than were those who did not (HR, 2.05), the investigators noted (JAMA. 2016 Sep 13;316[10]:1083-92).
In contrast, factors that were not associated with endocarditis risk included chronic pulmonary disease, type of valve (self-expandable or balloon-expandable), and setting of the procedure (catheterization lab vs. operating room).
The bacteria that most commonly caused infective endocarditis were Enterococci species (24.6% of cases), Staphylococcus aureus (23.8%), and coagulase-negative staphylococci (16.8%). This should be taken into consideration when selecting antibiotics for prophylaxis before TAVR and when choosing empirical antibiotics for treatment while waiting for blood culture results, wrote Dr. Regueiro and his associates.
“This information may help clinicians identify patients at higher risk [for endocarditis] and aid in implementing appropriate preventive measures,” they noted.
This study was supported by a grant from the Alfonso Martin Escudero Foundation. Dr. Regueiro reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Four factors – younger patient age, male sex, diabetes, and moderate to severe residual aortic regurgitation – are associated with a significantly increased risk of infective endocarditis after transcatheter aortic valve replacement, according to a report published online Sept. 13 in JAMA.
Until now, data pertaining to endocarditis following TAVR “have been limited to case reports and relatively small series with limited follow-up,” said Ander Regueiro, MD, of Laval University, Quebec City, and his associates.
They performed a retrospective analysis of data in a large international registry of TAVR cases to better characterize post-TAVR endocarditis.
Dr. Regueiro and his colleagues focused on 20,006 TAVR procedures done at 47 medical centers in Europe, North America, and South America during a 10-year period. The median time to symptom onset was 5.3 months after the procedure.
Infective endocarditis was definitively diagnosed in 250 of these cases. This incidence is similar to that reported for endocarditis following surgical aortic valve replacement, indicating that TAVR is no less predisposing to endocarditis despite being a less invasive approach.
The mean age of patients who developed post-TAVR endocarditis was 78.9 years, compared with 81.8 years for those who did not (HR, 0.97). The reason for this association is unclear, but it is possible that younger patients chosen for TAVR because of their prohibitive surgical risk carry a higher burden of comorbidity than do older patients. Similarly, 62% of endocarditis cases arose in men (HR, 1.69), and sex differences in comorbid conditions may explain the higher risk among men.
More patients who developed endocarditis had diabetes (41.7%), compared with those who did not develop endocarditis (30%), for an HR of 1.52. And patients who had moderate to severe residual aortic regurgitation after TAVR also were at much higher risk for endocarditis than were those who did not (HR, 2.05), the investigators noted (JAMA. 2016 Sep 13;316[10]:1083-92).
In contrast, factors that were not associated with endocarditis risk included chronic pulmonary disease, type of valve (self-expandable or balloon-expandable), and setting of the procedure (catheterization lab vs. operating room).
The bacteria that most commonly caused infective endocarditis were Enterococci species (24.6% of cases), Staphylococcus aureus (23.8%), and coagulase-negative staphylococci (16.8%). This should be taken into consideration when selecting antibiotics for prophylaxis before TAVR and when choosing empirical antibiotics for treatment while waiting for blood culture results, wrote Dr. Regueiro and his associates.
“This information may help clinicians identify patients at higher risk [for endocarditis] and aid in implementing appropriate preventive measures,” they noted.
This study was supported by a grant from the Alfonso Martin Escudero Foundation. Dr. Regueiro reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
FROM JAMA
Key clinical point: Four factors raise the risk that patients undergoing transcatheter aortic valve replacement will develop infective endocarditis.
Major finding: The mean age of patients who developed post-TAVR endocarditis was 78.9 years, compared with 81.8 years for those who didn’t (HR, 0.97).
Data source: A retrospective analysis of data in an international registry involving 20,006 patients who underwent TAVR at 47 medical centers during a 10-year period.
Disclosures: This study was supported by a grant from the Alfonso Martin Escudero Foundation. Dr. Regueiro reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Multiarterial grafting survival exceeds conventional CABG, PCI
A large, 16-year single-center study of patients with multivessel disease has determined that multivessel coronary artery bypass grafting achieved longer survival than not only percutaneous coronary interventions, but also conventional coronary artery bypass grafting, researchers from the Mayo Clinic reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:369-79).
Lead author Chaim Locker, MD, and his colleagues said the use of what they called MultiArt, for multivessel arterial grafting, also known as MAG, “must increase.”
The evolution of bare-metal and then drug-eluting stents may have favored percutaneous coronary interventions (PCI) over coronary artery bypass grafting (CABG), but, Dr. Locker and his coauthors said, “Evidence is accumulating that late outcome of surgical revascularization is improved when at least two arterial grafts are used.”
The study analyzed results of 12,615 patients who had either isolated primary CABG (6,667) or PCI (5,948) from 1993 to 2009. Among the CABG patients, 5,712 had the more conventional approach involving arterial grafts into the left internal thoracic artery/saphenous vein (ITA/SV) and 955 had MAG. Patients in the PCI group had three different procedures: balloon angioplasty (1,020), drug-eluting stent (1,686), or bare-metal stent (3,242). The study excluded patients who had revascularization procedures after a heart attack.
While the overall 15-year survival for patients with CABG was lower than it was for those who had PCI (36% vs. 46%), the survival for those who had MAG was significantly higher: 65% vs. 31% for those who had left ITA/SV revascularization. 8-year survival for the MAG subgroup was also significantly higher than all other subgroups: 87% vs. 69% for left ITA/SV, 75% for bare-metal stent, 73% for balloon angioplasty, and 70% for drug-eluting stent.
Propensity matching found similar survivability for balloon angioplasty and left ITA/SV when compared with MAG: 66% for MAG vs. 57% for the former; and 64% for MAG vs. 56% for the latter. The researchers also estimated the hazard ratio during the first 5 years of follow-up and found that those who had bare-metal stents had “significantly worse” survival, compared with MAG, but that survival evened out after that. Survival in the bare-metal stent group was similar to that of the left ITA/SV group, but “significantly worse” during the first 5 years for those who had balloon angioplasty.
Dr. Locker and his colleagues acknowledged that multiple randomized studies have compared CABG and PCI over the years, but they said that in most of those studies “the enrolled patients were highly selected and likely did not represent the broader population of patients with MVD [multivessel disease] undergoing revascularization.” With the exception of the SYNTAX trial (Synergy Between PCI With Taxus and Cardiac Surgery) (N Engl J Med. 2009;360:961-72; Lancet. 2013;381:629-38), those studies did not report on the frequency of MAG within the study population. The Mayo study, on the other hand, included all treated patients, excluding those who had a previous heart attack.
However, MAG is used infrequently, Dr. Locker and his colleagues said. The average annual rate of MAG in their Mayo practice was 15.2%, higher than the 5% annual rate the Society of Thoracic Surgeons National Cardiac Surgery Database (J Thorac Cardiovasc Surg. 2012;143:273-81) reported, and higher than the 12% rate in Europe (Eur J Cardiothorac Surg. 2006;29: 486-91). The SYNTAX trial reported an annual MAG rate of 27.6% for all CABG cases.
“It seems clear that use of MultiArt should be more frequent in patients with MVD undergoing CABG,” Dr. Locker and his coauthors said. “MultiArt can be used in most patients with MVD, including diabetic patients and elderly patients, and this strategy will improve outcomes of surgical revascularization.”
Dr. Locker and his coauthors had no financial relationships to disclose.
One might wonder about the validity of another retrospective, single-center study comparing revascularization techniques, but the study by Dr. Locker and his colleagues is “compelling” for two reasons, Paul Kurlansky, MD, of Columbia University, New York, pointed out in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:380-1).

|
Dr. Paul Kurlansky |
Dr. Kurlansky noted the finding of equivalent survival at up to 8 years among propensity-matched patients who had left coronary artery bypass grafting with the use of a single internal thoracic artery with supplemental vein grafts (left ITA/SV) and those who received drug-eluting stents was “a bit more provocative” than some of the expected study results; and the reversal of the survival benefit of left ITA/SV, compared with both balloon angioplasty and bare-metal stents after 7 to 10 years was “more perturbing for the surgical community.”
This study underscores that increased use of multiple arterial grafting is essential to give patients the best revascularization option, even in the age of growing percutaneous interventions, Dr. Kurlansky said.
“Limitations notwithstanding, the message for the surgical community is clear – if we wish to have the opportunity to treat patients with advanced, multivessel coronary artery disease, we will need to more fully embrace a strategy of MAG,” he said.
Dr. Kurlansky had no financial relationships to disclose.
One might wonder about the validity of another retrospective, single-center study comparing revascularization techniques, but the study by Dr. Locker and his colleagues is “compelling” for two reasons, Paul Kurlansky, MD, of Columbia University, New York, pointed out in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:380-1).

|
Dr. Paul Kurlansky |
Dr. Kurlansky noted the finding of equivalent survival at up to 8 years among propensity-matched patients who had left coronary artery bypass grafting with the use of a single internal thoracic artery with supplemental vein grafts (left ITA/SV) and those who received drug-eluting stents was “a bit more provocative” than some of the expected study results; and the reversal of the survival benefit of left ITA/SV, compared with both balloon angioplasty and bare-metal stents after 7 to 10 years was “more perturbing for the surgical community.”
This study underscores that increased use of multiple arterial grafting is essential to give patients the best revascularization option, even in the age of growing percutaneous interventions, Dr. Kurlansky said.
“Limitations notwithstanding, the message for the surgical community is clear – if we wish to have the opportunity to treat patients with advanced, multivessel coronary artery disease, we will need to more fully embrace a strategy of MAG,” he said.
Dr. Kurlansky had no financial relationships to disclose.
One might wonder about the validity of another retrospective, single-center study comparing revascularization techniques, but the study by Dr. Locker and his colleagues is “compelling” for two reasons, Paul Kurlansky, MD, of Columbia University, New York, pointed out in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:380-1).

|
Dr. Paul Kurlansky |
Dr. Kurlansky noted the finding of equivalent survival at up to 8 years among propensity-matched patients who had left coronary artery bypass grafting with the use of a single internal thoracic artery with supplemental vein grafts (left ITA/SV) and those who received drug-eluting stents was “a bit more provocative” than some of the expected study results; and the reversal of the survival benefit of left ITA/SV, compared with both balloon angioplasty and bare-metal stents after 7 to 10 years was “more perturbing for the surgical community.”
This study underscores that increased use of multiple arterial grafting is essential to give patients the best revascularization option, even in the age of growing percutaneous interventions, Dr. Kurlansky said.
“Limitations notwithstanding, the message for the surgical community is clear – if we wish to have the opportunity to treat patients with advanced, multivessel coronary artery disease, we will need to more fully embrace a strategy of MAG,” he said.
Dr. Kurlansky had no financial relationships to disclose.
A large, 16-year single-center study of patients with multivessel disease has determined that multivessel coronary artery bypass grafting achieved longer survival than not only percutaneous coronary interventions, but also conventional coronary artery bypass grafting, researchers from the Mayo Clinic reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:369-79).
Lead author Chaim Locker, MD, and his colleagues said the use of what they called MultiArt, for multivessel arterial grafting, also known as MAG, “must increase.”
The evolution of bare-metal and then drug-eluting stents may have favored percutaneous coronary interventions (PCI) over coronary artery bypass grafting (CABG), but, Dr. Locker and his coauthors said, “Evidence is accumulating that late outcome of surgical revascularization is improved when at least two arterial grafts are used.”
The study analyzed results of 12,615 patients who had either isolated primary CABG (6,667) or PCI (5,948) from 1993 to 2009. Among the CABG patients, 5,712 had the more conventional approach involving arterial grafts into the left internal thoracic artery/saphenous vein (ITA/SV) and 955 had MAG. Patients in the PCI group had three different procedures: balloon angioplasty (1,020), drug-eluting stent (1,686), or bare-metal stent (3,242). The study excluded patients who had revascularization procedures after a heart attack.
While the overall 15-year survival for patients with CABG was lower than it was for those who had PCI (36% vs. 46%), the survival for those who had MAG was significantly higher: 65% vs. 31% for those who had left ITA/SV revascularization. 8-year survival for the MAG subgroup was also significantly higher than all other subgroups: 87% vs. 69% for left ITA/SV, 75% for bare-metal stent, 73% for balloon angioplasty, and 70% for drug-eluting stent.
Propensity matching found similar survivability for balloon angioplasty and left ITA/SV when compared with MAG: 66% for MAG vs. 57% for the former; and 64% for MAG vs. 56% for the latter. The researchers also estimated the hazard ratio during the first 5 years of follow-up and found that those who had bare-metal stents had “significantly worse” survival, compared with MAG, but that survival evened out after that. Survival in the bare-metal stent group was similar to that of the left ITA/SV group, but “significantly worse” during the first 5 years for those who had balloon angioplasty.
Dr. Locker and his colleagues acknowledged that multiple randomized studies have compared CABG and PCI over the years, but they said that in most of those studies “the enrolled patients were highly selected and likely did not represent the broader population of patients with MVD [multivessel disease] undergoing revascularization.” With the exception of the SYNTAX trial (Synergy Between PCI With Taxus and Cardiac Surgery) (N Engl J Med. 2009;360:961-72; Lancet. 2013;381:629-38), those studies did not report on the frequency of MAG within the study population. The Mayo study, on the other hand, included all treated patients, excluding those who had a previous heart attack.
However, MAG is used infrequently, Dr. Locker and his colleagues said. The average annual rate of MAG in their Mayo practice was 15.2%, higher than the 5% annual rate the Society of Thoracic Surgeons National Cardiac Surgery Database (J Thorac Cardiovasc Surg. 2012;143:273-81) reported, and higher than the 12% rate in Europe (Eur J Cardiothorac Surg. 2006;29: 486-91). The SYNTAX trial reported an annual MAG rate of 27.6% for all CABG cases.
“It seems clear that use of MultiArt should be more frequent in patients with MVD undergoing CABG,” Dr. Locker and his coauthors said. “MultiArt can be used in most patients with MVD, including diabetic patients and elderly patients, and this strategy will improve outcomes of surgical revascularization.”
Dr. Locker and his coauthors had no financial relationships to disclose.
A large, 16-year single-center study of patients with multivessel disease has determined that multivessel coronary artery bypass grafting achieved longer survival than not only percutaneous coronary interventions, but also conventional coronary artery bypass grafting, researchers from the Mayo Clinic reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:369-79).
Lead author Chaim Locker, MD, and his colleagues said the use of what they called MultiArt, for multivessel arterial grafting, also known as MAG, “must increase.”
The evolution of bare-metal and then drug-eluting stents may have favored percutaneous coronary interventions (PCI) over coronary artery bypass grafting (CABG), but, Dr. Locker and his coauthors said, “Evidence is accumulating that late outcome of surgical revascularization is improved when at least two arterial grafts are used.”
The study analyzed results of 12,615 patients who had either isolated primary CABG (6,667) or PCI (5,948) from 1993 to 2009. Among the CABG patients, 5,712 had the more conventional approach involving arterial grafts into the left internal thoracic artery/saphenous vein (ITA/SV) and 955 had MAG. Patients in the PCI group had three different procedures: balloon angioplasty (1,020), drug-eluting stent (1,686), or bare-metal stent (3,242). The study excluded patients who had revascularization procedures after a heart attack.
While the overall 15-year survival for patients with CABG was lower than it was for those who had PCI (36% vs. 46%), the survival for those who had MAG was significantly higher: 65% vs. 31% for those who had left ITA/SV revascularization. 8-year survival for the MAG subgroup was also significantly higher than all other subgroups: 87% vs. 69% for left ITA/SV, 75% for bare-metal stent, 73% for balloon angioplasty, and 70% for drug-eluting stent.
Propensity matching found similar survivability for balloon angioplasty and left ITA/SV when compared with MAG: 66% for MAG vs. 57% for the former; and 64% for MAG vs. 56% for the latter. The researchers also estimated the hazard ratio during the first 5 years of follow-up and found that those who had bare-metal stents had “significantly worse” survival, compared with MAG, but that survival evened out after that. Survival in the bare-metal stent group was similar to that of the left ITA/SV group, but “significantly worse” during the first 5 years for those who had balloon angioplasty.
Dr. Locker and his colleagues acknowledged that multiple randomized studies have compared CABG and PCI over the years, but they said that in most of those studies “the enrolled patients were highly selected and likely did not represent the broader population of patients with MVD [multivessel disease] undergoing revascularization.” With the exception of the SYNTAX trial (Synergy Between PCI With Taxus and Cardiac Surgery) (N Engl J Med. 2009;360:961-72; Lancet. 2013;381:629-38), those studies did not report on the frequency of MAG within the study population. The Mayo study, on the other hand, included all treated patients, excluding those who had a previous heart attack.
However, MAG is used infrequently, Dr. Locker and his colleagues said. The average annual rate of MAG in their Mayo practice was 15.2%, higher than the 5% annual rate the Society of Thoracic Surgeons National Cardiac Surgery Database (J Thorac Cardiovasc Surg. 2012;143:273-81) reported, and higher than the 12% rate in Europe (Eur J Cardiothorac Surg. 2006;29: 486-91). The SYNTAX trial reported an annual MAG rate of 27.6% for all CABG cases.
“It seems clear that use of MultiArt should be more frequent in patients with MVD undergoing CABG,” Dr. Locker and his coauthors said. “MultiArt can be used in most patients with MVD, including diabetic patients and elderly patients, and this strategy will improve outcomes of surgical revascularization.”
Dr. Locker and his coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Cardiac surgeons should use multiple arterial coronary artery bypass grafting (MAG) more frequently because it achieves superior survival, compared with conventional bypass surgery or percutaneous coronary interventions.
Major finding: The overall 8-year survival of those who had MAG was 87% vs. 69% for conventional coronary bypass surgery and 70%-75% for percutaneous procedures.
Data source: Retrospective, single-institution study of 12,615 patients with multivessel disease who had revascularization procedures at the Mayo Clinic from 1993 to 2009.
Disclosures: Dr. Locker and his coauthors had no financial relationships to disclose.
Can anesthesia in infants affect IQ scores?
About 10,000 newborns receive general anesthesia for congenital heart defects every year, and the more exposure they have to inhaled anesthetic agents, the greater effect it may have on their neurologic development, investigators at Children’s Hospital of Philadelphia reported in a study of newborns with hypoplastic left heart syndrome.
While previous studies have linked worse neurodevelopment to patient factors like prematurity and genetics, this is the first study to show a consistent relationship between neurodevelopment outcomes and modifiable factors during cardiac surgery in infants, Laura K. Diaz, MD, and her colleagues reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:482-9).
They studied 96 patients with hypoplastic left heart syndrome (HLHS) or similar syndromes who received volatile anesthetic agents (VAA) at their institution from 1998 to 2003. The patients underwent a battery of neurodevelopmental tests between the ages of 4 and 5 years that included full-scale IQ (FSIQ), verbal IQ (VIQ), performance IQ (PIQ), and processing speed.
“This study provides evidence that in children undergoing staged reconstructive surgery for HLHS, increasing cumulative exposure to VAAs beginning in infancy is associated with worse performance for FSIQ and VIQ, suggesting that VAA exposure may be a modifiable risk factor for adverse neurodevelopment outcomes,” Dr. Diaz and her colleagues wrote.
While survival has improved significantly in recent years for infants with hypoplastic left heart syndrome, physicians have harbored concerns that these children encounter neurodevelopmental issues later on. Dr. Diaz and her colleagues acknowledged that previous studies have shown factors, such as the use of cardiopulmonary bypass (CPB) and hospital length of stay, that could affect neurodevelopment in these children, but the findings have been inconsistent. Instead, those studies have shown such patient-specific factors as birth weight, ethnicity, and hereditary disorders were strong determinants of neurodevelopment in infants who have cardiac surgery, Dr. Diaz and her coauthors pointed out.
Their own previous study of patients with single-ventricle congenital heart disease concurred with the findings of those other studies, but it did not evaluate exposure to anesthesia (J. Thorac. Cardiovasc. Surg. 2014;147:1276-82). That was the focus of their current study.
Among the study group, 94 patients had an initial operation with CPB in their first 30 days of life. All 96 infants in the study group had additional operations, whether cardiac or noncardiac. The study tracked all anesthetic exposures up until the neurodevelopment evaluation in February 2008. All but 2 patients had initial VAA exposure at less than 1 year of age, and 45 at less than 1 month of age. Deep hypothermic circulatory arrest was used uniformly for aortic arch reconstruction.
The study used four different generalized linear models to evaluate anesthesia exposure and neurodevelopment.
For both FSIQ and PIQ, total minimum alveolar concentration hours were deemed to be statistically significant factors for lower scores. For PIQ, birth weight and length of postoperative hospital stay were statistically significant. For processing speed, gestational age and length of hospital stay were statistically significant.
Dr. Diaz and her colleagues said their findings are preliminary and do not justify a change in practice. “Prospective randomized, controlled multicenter clinical trials are indicated to continue to clarify the effects of early and repetitive exposure to VAA in this and other pediatric populations,” the study authors concluded.
Dr. Diaz and the study authors had no financial relationships to disclose.
The study by Dr. Diaz and her colleagues makes all the more clear the need for a prospective randomized trial on the effect inhaled anesthetic agents in infants can have on their neurologic development, Richard A. Jonas, MD, of Children’s National Heart Institute, Children’s National Medical Center, Washington, said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2016;152:490).

|
Dr. Richard A. Jonas |
However, besides the study limitations that Dr. Diaz and her colleagues pointed out in their study, another “problem” Dr. Jonas noted with the study subjects was that they had staged reconstruction for hypoplastic left heart syndrome. “Not only is this group of patients at risk for prenatal effects of their abnormal in utero circulation, but in addition, they all underwent additional cardiac or noncardiac procedures after their initial cardiac surgery,” he said. These factors, along with some degree of cyanosis in their formative years, may help explain why this study is an outlier in that it did not implicate nonoperative factors that other studies implicated, Dr. Jonas said.
Nonetheless, the study is “an important contribution that adds further evidence to the observation that volatile agents can affect neurodevelopmental outcome,” Dr. Jonas said. Hence the need for a prospective randomized trial.
Dr. Jonas had no financial relationships to disclose.
The study by Dr. Diaz and her colleagues makes all the more clear the need for a prospective randomized trial on the effect inhaled anesthetic agents in infants can have on their neurologic development, Richard A. Jonas, MD, of Children’s National Heart Institute, Children’s National Medical Center, Washington, said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2016;152:490).

|
Dr. Richard A. Jonas |
However, besides the study limitations that Dr. Diaz and her colleagues pointed out in their study, another “problem” Dr. Jonas noted with the study subjects was that they had staged reconstruction for hypoplastic left heart syndrome. “Not only is this group of patients at risk for prenatal effects of their abnormal in utero circulation, but in addition, they all underwent additional cardiac or noncardiac procedures after their initial cardiac surgery,” he said. These factors, along with some degree of cyanosis in their formative years, may help explain why this study is an outlier in that it did not implicate nonoperative factors that other studies implicated, Dr. Jonas said.
Nonetheless, the study is “an important contribution that adds further evidence to the observation that volatile agents can affect neurodevelopmental outcome,” Dr. Jonas said. Hence the need for a prospective randomized trial.
Dr. Jonas had no financial relationships to disclose.
The study by Dr. Diaz and her colleagues makes all the more clear the need for a prospective randomized trial on the effect inhaled anesthetic agents in infants can have on their neurologic development, Richard A. Jonas, MD, of Children’s National Heart Institute, Children’s National Medical Center, Washington, said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2016;152:490).

|
Dr. Richard A. Jonas |
However, besides the study limitations that Dr. Diaz and her colleagues pointed out in their study, another “problem” Dr. Jonas noted with the study subjects was that they had staged reconstruction for hypoplastic left heart syndrome. “Not only is this group of patients at risk for prenatal effects of their abnormal in utero circulation, but in addition, they all underwent additional cardiac or noncardiac procedures after their initial cardiac surgery,” he said. These factors, along with some degree of cyanosis in their formative years, may help explain why this study is an outlier in that it did not implicate nonoperative factors that other studies implicated, Dr. Jonas said.
Nonetheless, the study is “an important contribution that adds further evidence to the observation that volatile agents can affect neurodevelopmental outcome,” Dr. Jonas said. Hence the need for a prospective randomized trial.
Dr. Jonas had no financial relationships to disclose.
About 10,000 newborns receive general anesthesia for congenital heart defects every year, and the more exposure they have to inhaled anesthetic agents, the greater effect it may have on their neurologic development, investigators at Children’s Hospital of Philadelphia reported in a study of newborns with hypoplastic left heart syndrome.
While previous studies have linked worse neurodevelopment to patient factors like prematurity and genetics, this is the first study to show a consistent relationship between neurodevelopment outcomes and modifiable factors during cardiac surgery in infants, Laura K. Diaz, MD, and her colleagues reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:482-9).
They studied 96 patients with hypoplastic left heart syndrome (HLHS) or similar syndromes who received volatile anesthetic agents (VAA) at their institution from 1998 to 2003. The patients underwent a battery of neurodevelopmental tests between the ages of 4 and 5 years that included full-scale IQ (FSIQ), verbal IQ (VIQ), performance IQ (PIQ), and processing speed.
“This study provides evidence that in children undergoing staged reconstructive surgery for HLHS, increasing cumulative exposure to VAAs beginning in infancy is associated with worse performance for FSIQ and VIQ, suggesting that VAA exposure may be a modifiable risk factor for adverse neurodevelopment outcomes,” Dr. Diaz and her colleagues wrote.
While survival has improved significantly in recent years for infants with hypoplastic left heart syndrome, physicians have harbored concerns that these children encounter neurodevelopmental issues later on. Dr. Diaz and her colleagues acknowledged that previous studies have shown factors, such as the use of cardiopulmonary bypass (CPB) and hospital length of stay, that could affect neurodevelopment in these children, but the findings have been inconsistent. Instead, those studies have shown such patient-specific factors as birth weight, ethnicity, and hereditary disorders were strong determinants of neurodevelopment in infants who have cardiac surgery, Dr. Diaz and her coauthors pointed out.
Their own previous study of patients with single-ventricle congenital heart disease concurred with the findings of those other studies, but it did not evaluate exposure to anesthesia (J. Thorac. Cardiovasc. Surg. 2014;147:1276-82). That was the focus of their current study.
Among the study group, 94 patients had an initial operation with CPB in their first 30 days of life. All 96 infants in the study group had additional operations, whether cardiac or noncardiac. The study tracked all anesthetic exposures up until the neurodevelopment evaluation in February 2008. All but 2 patients had initial VAA exposure at less than 1 year of age, and 45 at less than 1 month of age. Deep hypothermic circulatory arrest was used uniformly for aortic arch reconstruction.
The study used four different generalized linear models to evaluate anesthesia exposure and neurodevelopment.
For both FSIQ and PIQ, total minimum alveolar concentration hours were deemed to be statistically significant factors for lower scores. For PIQ, birth weight and length of postoperative hospital stay were statistically significant. For processing speed, gestational age and length of hospital stay were statistically significant.
Dr. Diaz and her colleagues said their findings are preliminary and do not justify a change in practice. “Prospective randomized, controlled multicenter clinical trials are indicated to continue to clarify the effects of early and repetitive exposure to VAA in this and other pediatric populations,” the study authors concluded.
Dr. Diaz and the study authors had no financial relationships to disclose.
About 10,000 newborns receive general anesthesia for congenital heart defects every year, and the more exposure they have to inhaled anesthetic agents, the greater effect it may have on their neurologic development, investigators at Children’s Hospital of Philadelphia reported in a study of newborns with hypoplastic left heart syndrome.
While previous studies have linked worse neurodevelopment to patient factors like prematurity and genetics, this is the first study to show a consistent relationship between neurodevelopment outcomes and modifiable factors during cardiac surgery in infants, Laura K. Diaz, MD, and her colleagues reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:482-9).
They studied 96 patients with hypoplastic left heart syndrome (HLHS) or similar syndromes who received volatile anesthetic agents (VAA) at their institution from 1998 to 2003. The patients underwent a battery of neurodevelopmental tests between the ages of 4 and 5 years that included full-scale IQ (FSIQ), verbal IQ (VIQ), performance IQ (PIQ), and processing speed.
“This study provides evidence that in children undergoing staged reconstructive surgery for HLHS, increasing cumulative exposure to VAAs beginning in infancy is associated with worse performance for FSIQ and VIQ, suggesting that VAA exposure may be a modifiable risk factor for adverse neurodevelopment outcomes,” Dr. Diaz and her colleagues wrote.
While survival has improved significantly in recent years for infants with hypoplastic left heart syndrome, physicians have harbored concerns that these children encounter neurodevelopmental issues later on. Dr. Diaz and her colleagues acknowledged that previous studies have shown factors, such as the use of cardiopulmonary bypass (CPB) and hospital length of stay, that could affect neurodevelopment in these children, but the findings have been inconsistent. Instead, those studies have shown such patient-specific factors as birth weight, ethnicity, and hereditary disorders were strong determinants of neurodevelopment in infants who have cardiac surgery, Dr. Diaz and her coauthors pointed out.
Their own previous study of patients with single-ventricle congenital heart disease concurred with the findings of those other studies, but it did not evaluate exposure to anesthesia (J. Thorac. Cardiovasc. Surg. 2014;147:1276-82). That was the focus of their current study.
Among the study group, 94 patients had an initial operation with CPB in their first 30 days of life. All 96 infants in the study group had additional operations, whether cardiac or noncardiac. The study tracked all anesthetic exposures up until the neurodevelopment evaluation in February 2008. All but 2 patients had initial VAA exposure at less than 1 year of age, and 45 at less than 1 month of age. Deep hypothermic circulatory arrest was used uniformly for aortic arch reconstruction.
The study used four different generalized linear models to evaluate anesthesia exposure and neurodevelopment.
For both FSIQ and PIQ, total minimum alveolar concentration hours were deemed to be statistically significant factors for lower scores. For PIQ, birth weight and length of postoperative hospital stay were statistically significant. For processing speed, gestational age and length of hospital stay were statistically significant.
Dr. Diaz and her colleagues said their findings are preliminary and do not justify a change in practice. “Prospective randomized, controlled multicenter clinical trials are indicated to continue to clarify the effects of early and repetitive exposure to VAA in this and other pediatric populations,” the study authors concluded.
Dr. Diaz and the study authors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Volatile inhaled anesthesia may affect neurodevelopment in infants with hypoplastic left heart syndrome.
Major finding: Different generalized linear models determined an association between minimum alveolar concentration hours and hospital length of stay with lower IQ scores and processing speed.
Data source: Meta-analysis reviewed a subgroup of 96 patients with hypoplastic left heart syndrome who had neurodevelopmental testing at a single center between 1998 and 2003.
Disclosures: The authors have no financial relationships to disclose.
A dual Y-shaped stent can improve QOL with airway fistulas
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: A combined type Y-shaped self-expandable coated metallic stent is a new approach for treatment of airway fistulas.
Major finding: Ten patients received the stents; all of them reported improved quality of life. Six died within 8 months because of unrelated factors.
Data source: Single-institution retrospective review of 10 patients with gastrotracheal or gastrobronchial fistulas who received the stent to reopen the airway.
Disclosures: Dr. Li and coauthors had no financial relationships to disclose. The study received support from the National High-Tech R&D Program of China.
Model estimates risk of pneumonia after CABG
A model incorporating 17 easily obtainable preoperative variables may help clinicians estimate patients’ risk of developing pneumonia after undergoing coronary artery bypass graft surgery, according to a report published in Annals of Thoracic Surgery.
“This model may be used to inform clinician-patient decision making and to identify opportunities for mitigating a patient’s risk,” said Raymond J. Strobel, a medical student at the University of Michigan, Ann Arbor, and his associates.
Postoperative pneumonia is the most common hospital-acquired infection following CABG, and it raises mortality risk fourfold and increases length of stay threefold. But reliable estimation of patient risk of post-CABG pneumonia has been difficult because of its low relative incidence – roughly 3% – and because most studies of the disorder are nearly a decade out of date.
To devise a predictive model using current data, Mr. Strobel and his associates assessed numerous potential risk factors and outcomes for 16,084 consecutive patients undergoing CABG at all 33 cardiac centers across Michigan during a 3-year period. They identified 531 cases of post-CABG pneumonia (3.3%) in this cohort.
The investigators performed a univariate analysis to test the associations between pneumonia and numerous factors related to patient demographics, medical history, comorbid diseases, laboratory values, cardiac anatomy, cardiac function, pulmonary function, the CABG procedure, and the institution where the procedure was performed. Variables that were found to be significantly associated with pneumonia (though usually with small absolute magnitudes) were then assessed in a multivariate analysis, which was further refined to create the final model.
The final model includes 17 factors that clearly raise the risk of post-CABG pneumonia. These include an elevated leukocyte count; a decreased hematocrit; older patient age; comorbidities such as peripheral vascular disease, diabetes, and liver disease; markers of pulmonary impairment such as cigarette smoking, the need for home oxygen therapy, and chronic lung disease; markers of cardiac dysfunction such as a recent history of arrhythmia and decreased ejection fraction; and emergency or urgent rather than elective operative status.
“This model performs well and demonstrates robustness across important clinical subgroups and centers,” the investigators said (Ann Thorac Surg. 2016 Jun 1; doi: 10.1016/j.athoracsur.2016.03.074).
In particular, this study identified preoperative leukocytosis to be a significant predictor of post-CABG pneumonia across several subgroups of patients. “We speculate that patients presenting with an elevated white blood cell count before surgery may be mounting an immune response against a pathogen and that the insult of CABG significantly increases their odds of postoperative pneumonia. ... It may be prudent to delay surgery until the source of leukocytosis is satisfactorily investigated, if not identified and treated, or the leukocytosis has otherwise resolved,” Mr. Strobel and his associates noted.
A model incorporating 17 easily obtainable preoperative variables may help clinicians estimate patients’ risk of developing pneumonia after undergoing coronary artery bypass graft surgery, according to a report published in Annals of Thoracic Surgery.
“This model may be used to inform clinician-patient decision making and to identify opportunities for mitigating a patient’s risk,” said Raymond J. Strobel, a medical student at the University of Michigan, Ann Arbor, and his associates.
Postoperative pneumonia is the most common hospital-acquired infection following CABG, and it raises mortality risk fourfold and increases length of stay threefold. But reliable estimation of patient risk of post-CABG pneumonia has been difficult because of its low relative incidence – roughly 3% – and because most studies of the disorder are nearly a decade out of date.
To devise a predictive model using current data, Mr. Strobel and his associates assessed numerous potential risk factors and outcomes for 16,084 consecutive patients undergoing CABG at all 33 cardiac centers across Michigan during a 3-year period. They identified 531 cases of post-CABG pneumonia (3.3%) in this cohort.
The investigators performed a univariate analysis to test the associations between pneumonia and numerous factors related to patient demographics, medical history, comorbid diseases, laboratory values, cardiac anatomy, cardiac function, pulmonary function, the CABG procedure, and the institution where the procedure was performed. Variables that were found to be significantly associated with pneumonia (though usually with small absolute magnitudes) were then assessed in a multivariate analysis, which was further refined to create the final model.
The final model includes 17 factors that clearly raise the risk of post-CABG pneumonia. These include an elevated leukocyte count; a decreased hematocrit; older patient age; comorbidities such as peripheral vascular disease, diabetes, and liver disease; markers of pulmonary impairment such as cigarette smoking, the need for home oxygen therapy, and chronic lung disease; markers of cardiac dysfunction such as a recent history of arrhythmia and decreased ejection fraction; and emergency or urgent rather than elective operative status.
“This model performs well and demonstrates robustness across important clinical subgroups and centers,” the investigators said (Ann Thorac Surg. 2016 Jun 1; doi: 10.1016/j.athoracsur.2016.03.074).
In particular, this study identified preoperative leukocytosis to be a significant predictor of post-CABG pneumonia across several subgroups of patients. “We speculate that patients presenting with an elevated white blood cell count before surgery may be mounting an immune response against a pathogen and that the insult of CABG significantly increases their odds of postoperative pneumonia. ... It may be prudent to delay surgery until the source of leukocytosis is satisfactorily investigated, if not identified and treated, or the leukocytosis has otherwise resolved,” Mr. Strobel and his associates noted.
A model incorporating 17 easily obtainable preoperative variables may help clinicians estimate patients’ risk of developing pneumonia after undergoing coronary artery bypass graft surgery, according to a report published in Annals of Thoracic Surgery.
“This model may be used to inform clinician-patient decision making and to identify opportunities for mitigating a patient’s risk,” said Raymond J. Strobel, a medical student at the University of Michigan, Ann Arbor, and his associates.
Postoperative pneumonia is the most common hospital-acquired infection following CABG, and it raises mortality risk fourfold and increases length of stay threefold. But reliable estimation of patient risk of post-CABG pneumonia has been difficult because of its low relative incidence – roughly 3% – and because most studies of the disorder are nearly a decade out of date.
To devise a predictive model using current data, Mr. Strobel and his associates assessed numerous potential risk factors and outcomes for 16,084 consecutive patients undergoing CABG at all 33 cardiac centers across Michigan during a 3-year period. They identified 531 cases of post-CABG pneumonia (3.3%) in this cohort.
The investigators performed a univariate analysis to test the associations between pneumonia and numerous factors related to patient demographics, medical history, comorbid diseases, laboratory values, cardiac anatomy, cardiac function, pulmonary function, the CABG procedure, and the institution where the procedure was performed. Variables that were found to be significantly associated with pneumonia (though usually with small absolute magnitudes) were then assessed in a multivariate analysis, which was further refined to create the final model.
The final model includes 17 factors that clearly raise the risk of post-CABG pneumonia. These include an elevated leukocyte count; a decreased hematocrit; older patient age; comorbidities such as peripheral vascular disease, diabetes, and liver disease; markers of pulmonary impairment such as cigarette smoking, the need for home oxygen therapy, and chronic lung disease; markers of cardiac dysfunction such as a recent history of arrhythmia and decreased ejection fraction; and emergency or urgent rather than elective operative status.
“This model performs well and demonstrates robustness across important clinical subgroups and centers,” the investigators said (Ann Thorac Surg. 2016 Jun 1; doi: 10.1016/j.athoracsur.2016.03.074).
In particular, this study identified preoperative leukocytosis to be a significant predictor of post-CABG pneumonia across several subgroups of patients. “We speculate that patients presenting with an elevated white blood cell count before surgery may be mounting an immune response against a pathogen and that the insult of CABG significantly increases their odds of postoperative pneumonia. ... It may be prudent to delay surgery until the source of leukocytosis is satisfactorily investigated, if not identified and treated, or the leukocytosis has otherwise resolved,” Mr. Strobel and his associates noted.
FROM ANNALS OF THORACIC SURGERY
Key clinical point: A model incorporating 17 easily obtainable preoperative variables helps estimate patients’ risk of developing pneumonia after coronary artery bypass surgery.
Major finding: Seventeen factors clearly raise the risk of post-CABG pneumonia, including an elevated leukocyte count, a decreased hematocrit, cigarette smoking, and the need for home oxygen therapy.
Data source: A prospective observational cohort study assessing numerous risk factors in 16,084 CABG patients.
Disclosures: This study was funded in part by the U.S. Agency for Healthcare Research and Quality, Blue Cross and Blue Shield of Michigan, and Blue Care Network. The authors’ financial disclosures were not provided.