User login
Thymectomy improves clinical outcomes for myasthenia gravis
Thymectomy improved 3-year clinical outcomes and proved superior to medical therapy for mild to severe nonthymomatous myasthenia gravis, according to a report published online Aug. 11 in the New England Journal of Medicine.
Compared with standard prednisone therapy, thymectomy plus prednisone decreased the number and severity of symptoms, allowed the lowering of steroid doses, decreased the number and length of hospitalizations for disease exacerbations, reduced the need for immunosuppressive agents, and improved health-related quality of life in an international, randomized clinical trial, said Gil I. Wolfe, MD, of the department of neurology, State University of New York at Buffalo and his associates.
Until now, thymectomy was known to be beneficial in some cases of myasthenia gravis “but with widely varying rates of clinical improvement or remission.” And the success of immunotherapy has raised the question of whether an invasive surgery is necessary. Data from randomized, controlled studies have been sparse.
Moreover, thymectomy rarely causes adverse effects, but “the procedure can cost up to $80,000 and can be associated with operative complications that need to be weighed against benefits.” In comparison, medical therapy with glucocorticoids and other immunosuppressive agents is less invasive but is definitely associated with adverse events, including some that are life threatening, and negatively impacts quality of life, the investigators said.
To address the lack of randomized controlled trial data, they assessed 3-year outcomes in 126 patients treated at 67 medical centers in 18 countries during a 6-year period. The study participants were aged 18-65 years, had a disease duration of less than 5 years at enrollment (median duration, 1 year), and had class II (mild generalized disease) to class IV (severe generalized disease) myasthenia gravis. These patients were randomly assigned to undergo thymectomy and receive standard prednisone therapy (66 participants) or to receive standard prednisone alone (60 participants).
Thymectomy was performed using a median sternotomy “with the goal of an en bloc resection of all mediastinal tissue that could anatomically contain gross or microscopic thymus.”
At follow-up, time-weighted average scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group. Time-weighted average prednisone dose also was significantly lower, at an average alternate-day dose of 44 mg in the thymectomy group and 60 mg in the control group, Dr. Wolfe and his associates said (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMoa1602489).
On a measure of treatment-related complications, scores favored thymectomy with regard to the number of patients with symptoms, the total number of symptoms, and the distress level related to symptoms throughout the study period. Fewer patients in the thymectomy group required hospitalization for exacerbations of myasthenia gravis (9% vs. 37%), and the mean cumulative number of hospital days was lower with thymectomy (8.4 vs. 19.2).
In addition, scores on the Myasthenia Gravis Activities of Daily Living scale favored thymectomy (2.24 vs. 3.41). Fewer patients in the thymectomy group required azathioprine (17% vs. 0.48%). And the percentage of patients who reported having minimal manifestations of the disease at 3 years was significantly higher with thymectomy (67%) than with prednisone alone (47%).
This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
Landmark trial establishes effectiveness of thymectomy in myasthenia gravis
One of the many challenges of treating patients with myasthenia gravis (MG) is the fluctuating nature of symptoms and deficits. The neurologist or neuromuscular specialist must decide whether the disease is truly worsening, whether the patient is experiencing more pronounced symptoms from intercurrent illness or the effects of a medication known to affect the neuromuscular junction adversely, or whether the patient is concerned that there might be worsening disease when all objective measures indicate stability. These factors make treatment decisions more difficult in MG than for many other neuromuscular disorders.
Similarly, researchers considering a trial investigating treatment efficacy in MG face the complex issues of disease fluctuation in cohorts of individuals with the disease, varying levels of corticosteroid and immunosuppressant doses in different MG patients, and thorny ethical dilemmas in providing accepted therapies but not withholding effective treatments from those in need.
Dr. Wolfe and his colleagues demonstrate that they have navigated these treacherous waters. They have succeeded in completing a landmark controlled clinical trial which establishes the effectiveness of transsternal thymectomy with adjuvant corticosteroid therapy in nonthymomatous MG vs. oral prednisone without surgery. While this international 36-center trial managed to recruit 126 subjects over a 6-year period, using sound inclusion and exclusion criteria and a meticulous trial design, the number of patients is not sufficient to allow for as robust a subgroup analysis for age, gender, and a variety of clinical variables reflecting severity of disease as would have been hoped for by the MG community.
Nonetheless, this paper sets the use of thymectomy in nonthymomatous MG on firmer ground going forward. The investigators will doubtless be presenting further data from the trial, including clinical-pathologic correlates and other relevant novel observations. In addition, Wolfe et al. have opened the door for future trials of thymectomy in MG to address such issues as the benefits vs. risks of performing the operation via the traditional transsternal vs. alternative non–sternal splitting approaches.
Benn E. Smith, MD, is an associate professor of neurology at the Mayo Clinic in Scottsdale, Ariz. and is the director of the sensory laboratory there. Dr. Smith is on the Editorial Advisory Board of Clinical Neurology News.
End to an 80-year controversy
These findings from Wolfe et al. end an 80-year controversy over the effectiveness of thymectomy for patients with myasthenia gravis.
Perhaps the most important benefit for patients is that even when they require prednisone following the surgery, they can take lower doses, endure fewer glucocorticoid-related symptoms, and experience less distress from those symptoms than patients who don’t undergo thymectomy.
Unfortunately, the study results cannot offer further clarity regarding patient selection for thymectomy. The patient population in this trial was so small that subgroup analyses couldn’t allow conclusions regarding the relative effectiveness of thymectomy in men vs. women or younger vs. older patients.
Allan H. Ropper, MD, is in the department of neurology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. His financial disclosures are available at NEJM.org. Dr. Ropper made these remarks in an editorial accompanying Dr. Wolfe’s report (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMe1607953).
Landmark trial establishes effectiveness of thymectomy in myasthenia gravis
One of the many challenges of treating patients with myasthenia gravis (MG) is the fluctuating nature of symptoms and deficits. The neurologist or neuromuscular specialist must decide whether the disease is truly worsening, whether the patient is experiencing more pronounced symptoms from intercurrent illness or the effects of a medication known to affect the neuromuscular junction adversely, or whether the patient is concerned that there might be worsening disease when all objective measures indicate stability. These factors make treatment decisions more difficult in MG than for many other neuromuscular disorders.
Similarly, researchers considering a trial investigating treatment efficacy in MG face the complex issues of disease fluctuation in cohorts of individuals with the disease, varying levels of corticosteroid and immunosuppressant doses in different MG patients, and thorny ethical dilemmas in providing accepted therapies but not withholding effective treatments from those in need.
Dr. Wolfe and his colleagues demonstrate that they have navigated these treacherous waters. They have succeeded in completing a landmark controlled clinical trial which establishes the effectiveness of transsternal thymectomy with adjuvant corticosteroid therapy in nonthymomatous MG vs. oral prednisone without surgery. While this international 36-center trial managed to recruit 126 subjects over a 6-year period, using sound inclusion and exclusion criteria and a meticulous trial design, the number of patients is not sufficient to allow for as robust a subgroup analysis for age, gender, and a variety of clinical variables reflecting severity of disease as would have been hoped for by the MG community.
Nonetheless, this paper sets the use of thymectomy in nonthymomatous MG on firmer ground going forward. The investigators will doubtless be presenting further data from the trial, including clinical-pathologic correlates and other relevant novel observations. In addition, Wolfe et al. have opened the door for future trials of thymectomy in MG to address such issues as the benefits vs. risks of performing the operation via the traditional transsternal vs. alternative non–sternal splitting approaches.
Benn E. Smith, MD, is an associate professor of neurology at the Mayo Clinic in Scottsdale, Ariz. and is the director of the sensory laboratory there. Dr. Smith is on the Editorial Advisory Board of Clinical Neurology News.
End to an 80-year controversy
These findings from Wolfe et al. end an 80-year controversy over the effectiveness of thymectomy for patients with myasthenia gravis.
Perhaps the most important benefit for patients is that even when they require prednisone following the surgery, they can take lower doses, endure fewer glucocorticoid-related symptoms, and experience less distress from those symptoms than patients who don’t undergo thymectomy.
Unfortunately, the study results cannot offer further clarity regarding patient selection for thymectomy. The patient population in this trial was so small that subgroup analyses couldn’t allow conclusions regarding the relative effectiveness of thymectomy in men vs. women or younger vs. older patients.
Allan H. Ropper, MD, is in the department of neurology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. His financial disclosures are available at NEJM.org. Dr. Ropper made these remarks in an editorial accompanying Dr. Wolfe’s report (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMe1607953).
Landmark trial establishes effectiveness of thymectomy in myasthenia gravis
One of the many challenges of treating patients with myasthenia gravis (MG) is the fluctuating nature of symptoms and deficits. The neurologist or neuromuscular specialist must decide whether the disease is truly worsening, whether the patient is experiencing more pronounced symptoms from intercurrent illness or the effects of a medication known to affect the neuromuscular junction adversely, or whether the patient is concerned that there might be worsening disease when all objective measures indicate stability. These factors make treatment decisions more difficult in MG than for many other neuromuscular disorders.
Similarly, researchers considering a trial investigating treatment efficacy in MG face the complex issues of disease fluctuation in cohorts of individuals with the disease, varying levels of corticosteroid and immunosuppressant doses in different MG patients, and thorny ethical dilemmas in providing accepted therapies but not withholding effective treatments from those in need.
Dr. Wolfe and his colleagues demonstrate that they have navigated these treacherous waters. They have succeeded in completing a landmark controlled clinical trial which establishes the effectiveness of transsternal thymectomy with adjuvant corticosteroid therapy in nonthymomatous MG vs. oral prednisone without surgery. While this international 36-center trial managed to recruit 126 subjects over a 6-year period, using sound inclusion and exclusion criteria and a meticulous trial design, the number of patients is not sufficient to allow for as robust a subgroup analysis for age, gender, and a variety of clinical variables reflecting severity of disease as would have been hoped for by the MG community.
Nonetheless, this paper sets the use of thymectomy in nonthymomatous MG on firmer ground going forward. The investigators will doubtless be presenting further data from the trial, including clinical-pathologic correlates and other relevant novel observations. In addition, Wolfe et al. have opened the door for future trials of thymectomy in MG to address such issues as the benefits vs. risks of performing the operation via the traditional transsternal vs. alternative non–sternal splitting approaches.
Benn E. Smith, MD, is an associate professor of neurology at the Mayo Clinic in Scottsdale, Ariz. and is the director of the sensory laboratory there. Dr. Smith is on the Editorial Advisory Board of Clinical Neurology News.
End to an 80-year controversy
These findings from Wolfe et al. end an 80-year controversy over the effectiveness of thymectomy for patients with myasthenia gravis.
Perhaps the most important benefit for patients is that even when they require prednisone following the surgery, they can take lower doses, endure fewer glucocorticoid-related symptoms, and experience less distress from those symptoms than patients who don’t undergo thymectomy.
Unfortunately, the study results cannot offer further clarity regarding patient selection for thymectomy. The patient population in this trial was so small that subgroup analyses couldn’t allow conclusions regarding the relative effectiveness of thymectomy in men vs. women or younger vs. older patients.
Allan H. Ropper, MD, is in the department of neurology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. His financial disclosures are available at NEJM.org. Dr. Ropper made these remarks in an editorial accompanying Dr. Wolfe’s report (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMe1607953).
Thymectomy improved 3-year clinical outcomes and proved superior to medical therapy for mild to severe nonthymomatous myasthenia gravis, according to a report published online Aug. 11 in the New England Journal of Medicine.
Compared with standard prednisone therapy, thymectomy plus prednisone decreased the number and severity of symptoms, allowed the lowering of steroid doses, decreased the number and length of hospitalizations for disease exacerbations, reduced the need for immunosuppressive agents, and improved health-related quality of life in an international, randomized clinical trial, said Gil I. Wolfe, MD, of the department of neurology, State University of New York at Buffalo and his associates.
Until now, thymectomy was known to be beneficial in some cases of myasthenia gravis “but with widely varying rates of clinical improvement or remission.” And the success of immunotherapy has raised the question of whether an invasive surgery is necessary. Data from randomized, controlled studies have been sparse.
Moreover, thymectomy rarely causes adverse effects, but “the procedure can cost up to $80,000 and can be associated with operative complications that need to be weighed against benefits.” In comparison, medical therapy with glucocorticoids and other immunosuppressive agents is less invasive but is definitely associated with adverse events, including some that are life threatening, and negatively impacts quality of life, the investigators said.
To address the lack of randomized controlled trial data, they assessed 3-year outcomes in 126 patients treated at 67 medical centers in 18 countries during a 6-year period. The study participants were aged 18-65 years, had a disease duration of less than 5 years at enrollment (median duration, 1 year), and had class II (mild generalized disease) to class IV (severe generalized disease) myasthenia gravis. These patients were randomly assigned to undergo thymectomy and receive standard prednisone therapy (66 participants) or to receive standard prednisone alone (60 participants).
Thymectomy was performed using a median sternotomy “with the goal of an en bloc resection of all mediastinal tissue that could anatomically contain gross or microscopic thymus.”
At follow-up, time-weighted average scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group. Time-weighted average prednisone dose also was significantly lower, at an average alternate-day dose of 44 mg in the thymectomy group and 60 mg in the control group, Dr. Wolfe and his associates said (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMoa1602489).
On a measure of treatment-related complications, scores favored thymectomy with regard to the number of patients with symptoms, the total number of symptoms, and the distress level related to symptoms throughout the study period. Fewer patients in the thymectomy group required hospitalization for exacerbations of myasthenia gravis (9% vs. 37%), and the mean cumulative number of hospital days was lower with thymectomy (8.4 vs. 19.2).
In addition, scores on the Myasthenia Gravis Activities of Daily Living scale favored thymectomy (2.24 vs. 3.41). Fewer patients in the thymectomy group required azathioprine (17% vs. 0.48%). And the percentage of patients who reported having minimal manifestations of the disease at 3 years was significantly higher with thymectomy (67%) than with prednisone alone (47%).
This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
Thymectomy improved 3-year clinical outcomes and proved superior to medical therapy for mild to severe nonthymomatous myasthenia gravis, according to a report published online Aug. 11 in the New England Journal of Medicine.
Compared with standard prednisone therapy, thymectomy plus prednisone decreased the number and severity of symptoms, allowed the lowering of steroid doses, decreased the number and length of hospitalizations for disease exacerbations, reduced the need for immunosuppressive agents, and improved health-related quality of life in an international, randomized clinical trial, said Gil I. Wolfe, MD, of the department of neurology, State University of New York at Buffalo and his associates.
Until now, thymectomy was known to be beneficial in some cases of myasthenia gravis “but with widely varying rates of clinical improvement or remission.” And the success of immunotherapy has raised the question of whether an invasive surgery is necessary. Data from randomized, controlled studies have been sparse.
Moreover, thymectomy rarely causes adverse effects, but “the procedure can cost up to $80,000 and can be associated with operative complications that need to be weighed against benefits.” In comparison, medical therapy with glucocorticoids and other immunosuppressive agents is less invasive but is definitely associated with adverse events, including some that are life threatening, and negatively impacts quality of life, the investigators said.
To address the lack of randomized controlled trial data, they assessed 3-year outcomes in 126 patients treated at 67 medical centers in 18 countries during a 6-year period. The study participants were aged 18-65 years, had a disease duration of less than 5 years at enrollment (median duration, 1 year), and had class II (mild generalized disease) to class IV (severe generalized disease) myasthenia gravis. These patients were randomly assigned to undergo thymectomy and receive standard prednisone therapy (66 participants) or to receive standard prednisone alone (60 participants).
Thymectomy was performed using a median sternotomy “with the goal of an en bloc resection of all mediastinal tissue that could anatomically contain gross or microscopic thymus.”
At follow-up, time-weighted average scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group. Time-weighted average prednisone dose also was significantly lower, at an average alternate-day dose of 44 mg in the thymectomy group and 60 mg in the control group, Dr. Wolfe and his associates said (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMoa1602489).
On a measure of treatment-related complications, scores favored thymectomy with regard to the number of patients with symptoms, the total number of symptoms, and the distress level related to symptoms throughout the study period. Fewer patients in the thymectomy group required hospitalization for exacerbations of myasthenia gravis (9% vs. 37%), and the mean cumulative number of hospital days was lower with thymectomy (8.4 vs. 19.2).
In addition, scores on the Myasthenia Gravis Activities of Daily Living scale favored thymectomy (2.24 vs. 3.41). Fewer patients in the thymectomy group required azathioprine (17% vs. 0.48%). And the percentage of patients who reported having minimal manifestations of the disease at 3 years was significantly higher with thymectomy (67%) than with prednisone alone (47%).
This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Thymectomy improved 3-year clinical outcomes and was superior to medical therapy for mild to severe nonthymomatous myasthenia gravis.
Major finding: Scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group.
Data source: An international, randomized, medication-controlled trial involving 126 patients at 67 medical centers.
Disclosures: This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
Choosing the transaxillary or supraclavicular approach for neurogenic TOS
The transaxillary approach has its advantages
I began my vascular fellowship at UCLA on July 1, 1986 – the previous day I was a chief surgery resident running a VA general surgery service where my last emergency case that evening was an abdominal peroneal resection for perforated rectal cancer! I was delighted to begin my fellowship, and learned that on Tuesdays I would be operating with Herb Machleder, MD – the expert on thoracic outlet syndrome (TOS) who perfected the transaxillary approach. I remembered his service from when I was an intern holding the patient arm up by cradling it my arms while he and the fellow removed the rib and identified each structure—subclavius tendon, subclavian vein, anterior scalene muscle, subclavian artery brachial plexus and any other abnormal band or structure present. The rib was removed in entirety to ensure an excellent outcome and to prevent any possibility of recurrence from scarring to the brachial plexus to a portion of retained rib. Dr. Machleder then went on to design a rib retractor to better support the arm and afford superb visibility.
As I began my career, I included transaxillary first rib resection as part of my practice for all forms of TOS, except when we needed to replace the subclavian artery because of an aneurysm or thrombosis. In those instances, we would employ the supraclavicular approach with an infraclavicular incision when necessary. In my 5 years as chief of the division of vascular surgery at UCLA (1998-2003), we saw many patients with TOS thanks to the legacy and practice of Dr. Machleder. We performed approximately 300 such operations between three of us and saw probably three to four times as many patients in clinic who did not need surgery to treat their TOS or other conditions.
When I arrived at Johns Hopkins as department chair in 2003, a robust thoracic outlet program did not exist there, so we began one. By the time I left in 2014, we were seeing 5-7 new patients per week and were operating on 125 per year, of which half were neurogenic. Ying Wei Lum, MD, and Maggie Arnold, MD, are continuing that practice at Johns Hopkins today.
The most important point about the “approach” for neurogenic thoracic outlet syndrome is whether or not you should operate. At Johns Hopkins, we only operated on about a third of those who presented to us with neurogenic symptoms, as 60%-70% will get better with a thoracic outlet–focused physical therapy regimen. We developed a protocol for this, which we actually handed to the patients as the prescription as they came from all over for our opinion on their conditions. We are doing the same at UC Davis.
We have published a great deal about patients who do not do as well with the surgical approach to neurogenic TOS. These patients include those over the age of 40 and those who have had symptoms for more than 10 years, as they tend to be quite debilitated and never quite recover fully from the operation.1 A scalene block with lidocaine can predict success in patients with the operation, and I use it in older patients or those with multiple complaints.2 At UC Davis, our pain service can perform the block with ultrasound guidance, which is easier for the patient.
Other patients who do not do well with the surgical approach to neurogenic TOS include those with other comorbidities such as cervical spine disease and shoulder abnormalities or injuries, as well as those with a severe dependence on pain medication due to such medical issues as complex pain syndrome or myofasciitis caused by comorbid diseases.3
These patients cannot adequately perform the requisite postoperative physical therapy to completely improve, and some can take up to a year to get range of motion and strength back. We also found that patients who smoke get recurrent disease due to scarring.
At both UC Davis and Johns Hopkins, we created a YouTube video for patients to educate them on the procedure and expected results. The need for postoperative physical therapy should be emphasized in all patients. Some require more therapy than others, which means taking time off from work to focus on the therapy and not performing other activities until the pain and discomfort are gone and strength is back. In another study we performed, we found that if patients did improve the first year, they were more likely to stay symptom free over many years.
While we were doing a transaxillary rib resection case at UC Davis, my team, which includes my partner Misty Humphries, MD, created a list of the top 10 reasons that the transaxillary approach is preferred for neurogenic thoracic outlet syndrome:
1. The scar is less noticeable and painful for the patient than the scar in the supraclavicular fossa, allowing the patient to start physical therapy 2 weeks after surgery.
2. The Machleder retractor makes visualization easy and stable, and allows all members of the team to see the anatomy.
3. The brachial plexus does not have to be retracted and is out of harm’s way, so no temporary palsies are seen in the postoperative period.
4. The subclavius tendon can be seen in entirety and the anterior portion of the rib is easy to completely remove.
5. The subclavian vein can be seen in entirety and defines the anterior portion of the dissection.
6. Once the anterior scalenectomy muscle is cut, the subclavian artery naturally retracts cephalad and is no longer near the rib when it is to be removed.
7. The posterior portion of the rib can be completely removed by readjusting the retraction and a second cut can be done safely with either the rib cutter or the first rib rongeur. It is essential to remove the rib posteriorly behind the nerve root so the arm is adducted and the nerve does not come in contact with the remaining rib, as we feel that leads to increased recurrences.
8. Two operating surgeons can address the rib from their side of the table and completely resect the rib, depending on the patient’s soft bony anatomy, by angling the instruments from either side.
9. Even large muscular or obese patients can be safely approached from the axilla utilizing the Machleder retractor and a lighted retractor.
10. The transaxillary approach can be taught through the teaching video we have made and through the ability for both surgeons to see because of the retractor.
Some of my favorite memories as a vascular surgeon were operating on Tuesdays with Dr. Machleder – similar to Tuesdays with Morrie.4 Not only did we remove ribs safely and completely, but he also taught me philosophy of surgery and of life. I hope I am doing the same with my team as we remove ribs now on Thursday – “Thursdays with Freischlag” – at UC Davis.
Dr. Freischlag is vice chancellor for human health sciences and dean of the school of medicine at the University of California, Davis. She had no relevant disclosures.
References
1. J Vasc Surg. 2012;55(5):1370-5.
2. Curr Treat Options Cardiovasc Med. 2009;11(2):176-83.
3. J Vasc Surg. 2012;56(4):1061-7.
Use a supraclavicular approach: My way is best!
The best sense we have of the pathophysiology of neurogenic (NTOS) is that the scalene triangle is “too tight” with regard to what it contains – the brachial plexus and the subclavian artery. Whether this is due to the triangle being too small or the nerves being “too large” (inflammation) is unknown. Supporting the former theory are observations that the anterior scalene muscle is frequently inflamed and/or chronically injured.1 but others have suggested that the first rib is abnormally located or elevated.2 In addition, some have suggested that inflammatory tissue surrounding the plexus contributes to the process, at least for chronic cases.3
Given the fact that at least two of the three parts of the triangle, plus tissue surrounding the plexus itself, have all been implicated in the disease process, why not choose an approach that allows correction of all potential causes? The transaxillary approach has been used for decades for this condition, but can only decompress the base of the triangle (first rib) and, to varying degrees, only part of the anterior scalene. It does not allow thorough exploration of the nerves. The supraclavicular approach (and the supraclavicular half of paraclavicular excision) addresses these concerns. First, the anterior scalene muscle is essentially entirely removed. With proper technique it is completely visible from the scalene tubercle to its origin at the spine. This approach also allows removal of all muscular and associated tissue medially, completely clearing the parietal pleura at the apex of the lung, at least theoretically reducing the chances of scar tissue arising from residual tissue here.
Second, although no research has yet implicated the middle scalene (scalenus medius, which does not translate perfectly), many patients have impressively bulky musculature at this site. The middle scalene is also completely resected while approaching the first rib; perhaps removing this as well contributes to the excellent results we see today.
Third, the entire portion of the rib involved in NTOS (and the entire rib altogether if a paraclavicular approach is used) is very easily removed using this approach, as are any cervical ribs or Roos bands. Everything is seen, and everything can be evaluated and resected. Finally, many consider full neurolysis of the brachial plexus in this area an important part of the procedure. This is based on low-grade evidence only,3 but in the author’s experience, the incidence of improvement or cure seems to be higher, and recurrence rates lower, than with less-complete operations.
Parenthetically, related to this issue is that of visualization and education. The primary goal is ensuring the best outcome for the patient. Visualization is, by far, best if a supraclavicular approach is used. This is beneficial clinically by ensuring the most complete decompression of the nerves and avoidance of complications, but also is extremely helpful with regard to educating residents and fellows, learning the anatomy, identifying aberrant structures, and so on. Even with the best techniques (including a head- or retractor-mounted camera), no one can see what’s going on during a transaxillary approach except for the operator.
If the supraclavicular approach allows better access to and removal of all the potentially involved components causing NTOS, why doesn’t everyone use it? One answer is that the potential complication rate may be higher. Both the long thoracic and phrenic nerves are very much more at risk using this approach than using the transaxillary approach, and, on the left side, the risk of thoracic duct injury is higher. It must be conceded that published results, in general, do not show significant differences in outcomes between the two approaches.4 However, many would interpret this as a type II error, combined with the “fuzziness” of diagnosis and evaluation of outcomes this field has labored under. However, the opposite interpretation should be considered – there are no definitive data showing any higher complication rate between the two approaches. This debate likely is answerable in the same fashion as many other such debates in our field – someone who is good at the transaxillary approach will do a better job than someone who is not, and someone who is good at the supraclavicular approach will do a better job than someone who is not.
Is a prospective trial indicated? In theory, yes. However, the relative rarity of this condition, the fact that most surgeons follow almost exclusively one or the other technique, and the categorical nature of the outcome variable make such a trial relatively impractical. Pending this, the best suggestion is obviously to pick the best TOS surgeon you can find and have him or her fix the problem in the way they are most experienced!
Dr. Illig is professor of surgery and director, division of vascular surgery, and associate chair, faculty development and mentoring, University of South Florida, Morsani College of Medicine, Tampa, Fla. He had no relevant disclosures.
References
2. Thoracic Outlet Syndrome. London: Springer 2013; 319-21.
The transaxillary approach has its advantages
I began my vascular fellowship at UCLA on July 1, 1986 – the previous day I was a chief surgery resident running a VA general surgery service where my last emergency case that evening was an abdominal peroneal resection for perforated rectal cancer! I was delighted to begin my fellowship, and learned that on Tuesdays I would be operating with Herb Machleder, MD – the expert on thoracic outlet syndrome (TOS) who perfected the transaxillary approach. I remembered his service from when I was an intern holding the patient arm up by cradling it my arms while he and the fellow removed the rib and identified each structure—subclavius tendon, subclavian vein, anterior scalene muscle, subclavian artery brachial plexus and any other abnormal band or structure present. The rib was removed in entirety to ensure an excellent outcome and to prevent any possibility of recurrence from scarring to the brachial plexus to a portion of retained rib. Dr. Machleder then went on to design a rib retractor to better support the arm and afford superb visibility.
As I began my career, I included transaxillary first rib resection as part of my practice for all forms of TOS, except when we needed to replace the subclavian artery because of an aneurysm or thrombosis. In those instances, we would employ the supraclavicular approach with an infraclavicular incision when necessary. In my 5 years as chief of the division of vascular surgery at UCLA (1998-2003), we saw many patients with TOS thanks to the legacy and practice of Dr. Machleder. We performed approximately 300 such operations between three of us and saw probably three to four times as many patients in clinic who did not need surgery to treat their TOS or other conditions.
When I arrived at Johns Hopkins as department chair in 2003, a robust thoracic outlet program did not exist there, so we began one. By the time I left in 2014, we were seeing 5-7 new patients per week and were operating on 125 per year, of which half were neurogenic. Ying Wei Lum, MD, and Maggie Arnold, MD, are continuing that practice at Johns Hopkins today.
The most important point about the “approach” for neurogenic thoracic outlet syndrome is whether or not you should operate. At Johns Hopkins, we only operated on about a third of those who presented to us with neurogenic symptoms, as 60%-70% will get better with a thoracic outlet–focused physical therapy regimen. We developed a protocol for this, which we actually handed to the patients as the prescription as they came from all over for our opinion on their conditions. We are doing the same at UC Davis.
We have published a great deal about patients who do not do as well with the surgical approach to neurogenic TOS. These patients include those over the age of 40 and those who have had symptoms for more than 10 years, as they tend to be quite debilitated and never quite recover fully from the operation.1 A scalene block with lidocaine can predict success in patients with the operation, and I use it in older patients or those with multiple complaints.2 At UC Davis, our pain service can perform the block with ultrasound guidance, which is easier for the patient.
Other patients who do not do well with the surgical approach to neurogenic TOS include those with other comorbidities such as cervical spine disease and shoulder abnormalities or injuries, as well as those with a severe dependence on pain medication due to such medical issues as complex pain syndrome or myofasciitis caused by comorbid diseases.3
These patients cannot adequately perform the requisite postoperative physical therapy to completely improve, and some can take up to a year to get range of motion and strength back. We also found that patients who smoke get recurrent disease due to scarring.
At both UC Davis and Johns Hopkins, we created a YouTube video for patients to educate them on the procedure and expected results. The need for postoperative physical therapy should be emphasized in all patients. Some require more therapy than others, which means taking time off from work to focus on the therapy and not performing other activities until the pain and discomfort are gone and strength is back. In another study we performed, we found that if patients did improve the first year, they were more likely to stay symptom free over many years.
While we were doing a transaxillary rib resection case at UC Davis, my team, which includes my partner Misty Humphries, MD, created a list of the top 10 reasons that the transaxillary approach is preferred for neurogenic thoracic outlet syndrome:
1. The scar is less noticeable and painful for the patient than the scar in the supraclavicular fossa, allowing the patient to start physical therapy 2 weeks after surgery.
2. The Machleder retractor makes visualization easy and stable, and allows all members of the team to see the anatomy.
3. The brachial plexus does not have to be retracted and is out of harm’s way, so no temporary palsies are seen in the postoperative period.
4. The subclavius tendon can be seen in entirety and the anterior portion of the rib is easy to completely remove.
5. The subclavian vein can be seen in entirety and defines the anterior portion of the dissection.
6. Once the anterior scalenectomy muscle is cut, the subclavian artery naturally retracts cephalad and is no longer near the rib when it is to be removed.
7. The posterior portion of the rib can be completely removed by readjusting the retraction and a second cut can be done safely with either the rib cutter or the first rib rongeur. It is essential to remove the rib posteriorly behind the nerve root so the arm is adducted and the nerve does not come in contact with the remaining rib, as we feel that leads to increased recurrences.
8. Two operating surgeons can address the rib from their side of the table and completely resect the rib, depending on the patient’s soft bony anatomy, by angling the instruments from either side.
9. Even large muscular or obese patients can be safely approached from the axilla utilizing the Machleder retractor and a lighted retractor.
10. The transaxillary approach can be taught through the teaching video we have made and through the ability for both surgeons to see because of the retractor.
Some of my favorite memories as a vascular surgeon were operating on Tuesdays with Dr. Machleder – similar to Tuesdays with Morrie.4 Not only did we remove ribs safely and completely, but he also taught me philosophy of surgery and of life. I hope I am doing the same with my team as we remove ribs now on Thursday – “Thursdays with Freischlag” – at UC Davis.
Dr. Freischlag is vice chancellor for human health sciences and dean of the school of medicine at the University of California, Davis. She had no relevant disclosures.
References
1. J Vasc Surg. 2012;55(5):1370-5.
2. Curr Treat Options Cardiovasc Med. 2009;11(2):176-83.
3. J Vasc Surg. 2012;56(4):1061-7.
Use a supraclavicular approach: My way is best!
The best sense we have of the pathophysiology of neurogenic (NTOS) is that the scalene triangle is “too tight” with regard to what it contains – the brachial plexus and the subclavian artery. Whether this is due to the triangle being too small or the nerves being “too large” (inflammation) is unknown. Supporting the former theory are observations that the anterior scalene muscle is frequently inflamed and/or chronically injured.1 but others have suggested that the first rib is abnormally located or elevated.2 In addition, some have suggested that inflammatory tissue surrounding the plexus contributes to the process, at least for chronic cases.3
Given the fact that at least two of the three parts of the triangle, plus tissue surrounding the plexus itself, have all been implicated in the disease process, why not choose an approach that allows correction of all potential causes? The transaxillary approach has been used for decades for this condition, but can only decompress the base of the triangle (first rib) and, to varying degrees, only part of the anterior scalene. It does not allow thorough exploration of the nerves. The supraclavicular approach (and the supraclavicular half of paraclavicular excision) addresses these concerns. First, the anterior scalene muscle is essentially entirely removed. With proper technique it is completely visible from the scalene tubercle to its origin at the spine. This approach also allows removal of all muscular and associated tissue medially, completely clearing the parietal pleura at the apex of the lung, at least theoretically reducing the chances of scar tissue arising from residual tissue here.
Second, although no research has yet implicated the middle scalene (scalenus medius, which does not translate perfectly), many patients have impressively bulky musculature at this site. The middle scalene is also completely resected while approaching the first rib; perhaps removing this as well contributes to the excellent results we see today.
Third, the entire portion of the rib involved in NTOS (and the entire rib altogether if a paraclavicular approach is used) is very easily removed using this approach, as are any cervical ribs or Roos bands. Everything is seen, and everything can be evaluated and resected. Finally, many consider full neurolysis of the brachial plexus in this area an important part of the procedure. This is based on low-grade evidence only,3 but in the author’s experience, the incidence of improvement or cure seems to be higher, and recurrence rates lower, than with less-complete operations.
Parenthetically, related to this issue is that of visualization and education. The primary goal is ensuring the best outcome for the patient. Visualization is, by far, best if a supraclavicular approach is used. This is beneficial clinically by ensuring the most complete decompression of the nerves and avoidance of complications, but also is extremely helpful with regard to educating residents and fellows, learning the anatomy, identifying aberrant structures, and so on. Even with the best techniques (including a head- or retractor-mounted camera), no one can see what’s going on during a transaxillary approach except for the operator.
If the supraclavicular approach allows better access to and removal of all the potentially involved components causing NTOS, why doesn’t everyone use it? One answer is that the potential complication rate may be higher. Both the long thoracic and phrenic nerves are very much more at risk using this approach than using the transaxillary approach, and, on the left side, the risk of thoracic duct injury is higher. It must be conceded that published results, in general, do not show significant differences in outcomes between the two approaches.4 However, many would interpret this as a type II error, combined with the “fuzziness” of diagnosis and evaluation of outcomes this field has labored under. However, the opposite interpretation should be considered – there are no definitive data showing any higher complication rate between the two approaches. This debate likely is answerable in the same fashion as many other such debates in our field – someone who is good at the transaxillary approach will do a better job than someone who is not, and someone who is good at the supraclavicular approach will do a better job than someone who is not.
Is a prospective trial indicated? In theory, yes. However, the relative rarity of this condition, the fact that most surgeons follow almost exclusively one or the other technique, and the categorical nature of the outcome variable make such a trial relatively impractical. Pending this, the best suggestion is obviously to pick the best TOS surgeon you can find and have him or her fix the problem in the way they are most experienced!
Dr. Illig is professor of surgery and director, division of vascular surgery, and associate chair, faculty development and mentoring, University of South Florida, Morsani College of Medicine, Tampa, Fla. He had no relevant disclosures.
References
2. Thoracic Outlet Syndrome. London: Springer 2013; 319-21.
The transaxillary approach has its advantages
I began my vascular fellowship at UCLA on July 1, 1986 – the previous day I was a chief surgery resident running a VA general surgery service where my last emergency case that evening was an abdominal peroneal resection for perforated rectal cancer! I was delighted to begin my fellowship, and learned that on Tuesdays I would be operating with Herb Machleder, MD – the expert on thoracic outlet syndrome (TOS) who perfected the transaxillary approach. I remembered his service from when I was an intern holding the patient arm up by cradling it my arms while he and the fellow removed the rib and identified each structure—subclavius tendon, subclavian vein, anterior scalene muscle, subclavian artery brachial plexus and any other abnormal band or structure present. The rib was removed in entirety to ensure an excellent outcome and to prevent any possibility of recurrence from scarring to the brachial plexus to a portion of retained rib. Dr. Machleder then went on to design a rib retractor to better support the arm and afford superb visibility.
As I began my career, I included transaxillary first rib resection as part of my practice for all forms of TOS, except when we needed to replace the subclavian artery because of an aneurysm or thrombosis. In those instances, we would employ the supraclavicular approach with an infraclavicular incision when necessary. In my 5 years as chief of the division of vascular surgery at UCLA (1998-2003), we saw many patients with TOS thanks to the legacy and practice of Dr. Machleder. We performed approximately 300 such operations between three of us and saw probably three to four times as many patients in clinic who did not need surgery to treat their TOS or other conditions.
When I arrived at Johns Hopkins as department chair in 2003, a robust thoracic outlet program did not exist there, so we began one. By the time I left in 2014, we were seeing 5-7 new patients per week and were operating on 125 per year, of which half were neurogenic. Ying Wei Lum, MD, and Maggie Arnold, MD, are continuing that practice at Johns Hopkins today.
The most important point about the “approach” for neurogenic thoracic outlet syndrome is whether or not you should operate. At Johns Hopkins, we only operated on about a third of those who presented to us with neurogenic symptoms, as 60%-70% will get better with a thoracic outlet–focused physical therapy regimen. We developed a protocol for this, which we actually handed to the patients as the prescription as they came from all over for our opinion on their conditions. We are doing the same at UC Davis.
We have published a great deal about patients who do not do as well with the surgical approach to neurogenic TOS. These patients include those over the age of 40 and those who have had symptoms for more than 10 years, as they tend to be quite debilitated and never quite recover fully from the operation.1 A scalene block with lidocaine can predict success in patients with the operation, and I use it in older patients or those with multiple complaints.2 At UC Davis, our pain service can perform the block with ultrasound guidance, which is easier for the patient.
Other patients who do not do well with the surgical approach to neurogenic TOS include those with other comorbidities such as cervical spine disease and shoulder abnormalities or injuries, as well as those with a severe dependence on pain medication due to such medical issues as complex pain syndrome or myofasciitis caused by comorbid diseases.3
These patients cannot adequately perform the requisite postoperative physical therapy to completely improve, and some can take up to a year to get range of motion and strength back. We also found that patients who smoke get recurrent disease due to scarring.
At both UC Davis and Johns Hopkins, we created a YouTube video for patients to educate them on the procedure and expected results. The need for postoperative physical therapy should be emphasized in all patients. Some require more therapy than others, which means taking time off from work to focus on the therapy and not performing other activities until the pain and discomfort are gone and strength is back. In another study we performed, we found that if patients did improve the first year, they were more likely to stay symptom free over many years.
While we were doing a transaxillary rib resection case at UC Davis, my team, which includes my partner Misty Humphries, MD, created a list of the top 10 reasons that the transaxillary approach is preferred for neurogenic thoracic outlet syndrome:
1. The scar is less noticeable and painful for the patient than the scar in the supraclavicular fossa, allowing the patient to start physical therapy 2 weeks after surgery.
2. The Machleder retractor makes visualization easy and stable, and allows all members of the team to see the anatomy.
3. The brachial plexus does not have to be retracted and is out of harm’s way, so no temporary palsies are seen in the postoperative period.
4. The subclavius tendon can be seen in entirety and the anterior portion of the rib is easy to completely remove.
5. The subclavian vein can be seen in entirety and defines the anterior portion of the dissection.
6. Once the anterior scalenectomy muscle is cut, the subclavian artery naturally retracts cephalad and is no longer near the rib when it is to be removed.
7. The posterior portion of the rib can be completely removed by readjusting the retraction and a second cut can be done safely with either the rib cutter or the first rib rongeur. It is essential to remove the rib posteriorly behind the nerve root so the arm is adducted and the nerve does not come in contact with the remaining rib, as we feel that leads to increased recurrences.
8. Two operating surgeons can address the rib from their side of the table and completely resect the rib, depending on the patient’s soft bony anatomy, by angling the instruments from either side.
9. Even large muscular or obese patients can be safely approached from the axilla utilizing the Machleder retractor and a lighted retractor.
10. The transaxillary approach can be taught through the teaching video we have made and through the ability for both surgeons to see because of the retractor.
Some of my favorite memories as a vascular surgeon were operating on Tuesdays with Dr. Machleder – similar to Tuesdays with Morrie.4 Not only did we remove ribs safely and completely, but he also taught me philosophy of surgery and of life. I hope I am doing the same with my team as we remove ribs now on Thursday – “Thursdays with Freischlag” – at UC Davis.
Dr. Freischlag is vice chancellor for human health sciences and dean of the school of medicine at the University of California, Davis. She had no relevant disclosures.
References
1. J Vasc Surg. 2012;55(5):1370-5.
2. Curr Treat Options Cardiovasc Med. 2009;11(2):176-83.
3. J Vasc Surg. 2012;56(4):1061-7.
Use a supraclavicular approach: My way is best!
The best sense we have of the pathophysiology of neurogenic (NTOS) is that the scalene triangle is “too tight” with regard to what it contains – the brachial plexus and the subclavian artery. Whether this is due to the triangle being too small or the nerves being “too large” (inflammation) is unknown. Supporting the former theory are observations that the anterior scalene muscle is frequently inflamed and/or chronically injured.1 but others have suggested that the first rib is abnormally located or elevated.2 In addition, some have suggested that inflammatory tissue surrounding the plexus contributes to the process, at least for chronic cases.3
Given the fact that at least two of the three parts of the triangle, plus tissue surrounding the plexus itself, have all been implicated in the disease process, why not choose an approach that allows correction of all potential causes? The transaxillary approach has been used for decades for this condition, but can only decompress the base of the triangle (first rib) and, to varying degrees, only part of the anterior scalene. It does not allow thorough exploration of the nerves. The supraclavicular approach (and the supraclavicular half of paraclavicular excision) addresses these concerns. First, the anterior scalene muscle is essentially entirely removed. With proper technique it is completely visible from the scalene tubercle to its origin at the spine. This approach also allows removal of all muscular and associated tissue medially, completely clearing the parietal pleura at the apex of the lung, at least theoretically reducing the chances of scar tissue arising from residual tissue here.
Second, although no research has yet implicated the middle scalene (scalenus medius, which does not translate perfectly), many patients have impressively bulky musculature at this site. The middle scalene is also completely resected while approaching the first rib; perhaps removing this as well contributes to the excellent results we see today.
Third, the entire portion of the rib involved in NTOS (and the entire rib altogether if a paraclavicular approach is used) is very easily removed using this approach, as are any cervical ribs or Roos bands. Everything is seen, and everything can be evaluated and resected. Finally, many consider full neurolysis of the brachial plexus in this area an important part of the procedure. This is based on low-grade evidence only,3 but in the author’s experience, the incidence of improvement or cure seems to be higher, and recurrence rates lower, than with less-complete operations.
Parenthetically, related to this issue is that of visualization and education. The primary goal is ensuring the best outcome for the patient. Visualization is, by far, best if a supraclavicular approach is used. This is beneficial clinically by ensuring the most complete decompression of the nerves and avoidance of complications, but also is extremely helpful with regard to educating residents and fellows, learning the anatomy, identifying aberrant structures, and so on. Even with the best techniques (including a head- or retractor-mounted camera), no one can see what’s going on during a transaxillary approach except for the operator.
If the supraclavicular approach allows better access to and removal of all the potentially involved components causing NTOS, why doesn’t everyone use it? One answer is that the potential complication rate may be higher. Both the long thoracic and phrenic nerves are very much more at risk using this approach than using the transaxillary approach, and, on the left side, the risk of thoracic duct injury is higher. It must be conceded that published results, in general, do not show significant differences in outcomes between the two approaches.4 However, many would interpret this as a type II error, combined with the “fuzziness” of diagnosis and evaluation of outcomes this field has labored under. However, the opposite interpretation should be considered – there are no definitive data showing any higher complication rate between the two approaches. This debate likely is answerable in the same fashion as many other such debates in our field – someone who is good at the transaxillary approach will do a better job than someone who is not, and someone who is good at the supraclavicular approach will do a better job than someone who is not.
Is a prospective trial indicated? In theory, yes. However, the relative rarity of this condition, the fact that most surgeons follow almost exclusively one or the other technique, and the categorical nature of the outcome variable make such a trial relatively impractical. Pending this, the best suggestion is obviously to pick the best TOS surgeon you can find and have him or her fix the problem in the way they are most experienced!
Dr. Illig is professor of surgery and director, division of vascular surgery, and associate chair, faculty development and mentoring, University of South Florida, Morsani College of Medicine, Tampa, Fla. He had no relevant disclosures.
References
2. Thoracic Outlet Syndrome. London: Springer 2013; 319-21.
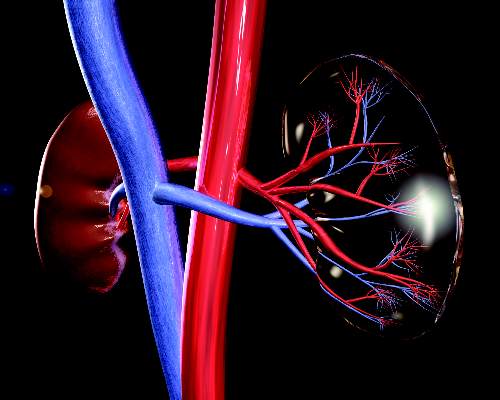
AAN recommends against routine closure of patent foramen ovale for secondary stroke prevention
An updated practice advisory from the American Academy of Neurology does not recommend the routine use of catheter-based closure of patent foramen ovale in patients with a history of cryptogenic ischemic stroke.
“Because of the limitations of the efficacy evidence and the potential for serious adverse effects, we judge the risk-benefit trade-offs of PFO [patent foramen ovale] closure by either the STARFlex or AMPLATZER PFO Occluder to be uncertain,” wrote Steven Messé, MD, associate professor of neurology at the University of Pennsylvania, Philadelphia, and his associates. “In rare circumstances, such as recurrent strokes despite adequate medical therapy with no other mechanism identified, clinicians may offer the AMPLATZER PFO Occluder if it is available,” they noted.
They also supported antiplatelet agents over anticoagulants unless patients have another indication for blood thinners, noting “the uncertainty surrounding the benefit of anticoagulation in the setting of PFO, and anticoagulation’s well-known harm profile.”
PFO affects about one in four individuals overall and up to half of cryptogenic stroke patients. The previous (2004) version of this practice advisory cited insufficient evidence to guide optimal therapy for secondary stroke prevention in these patients (Neurology. 2004;Apr 13;62[7]:1042-50). To update the guideline, Dr. Messé and his associates searched the literature for relevant randomized studies, excluding transient ischemic attacks when feasible because of their subjective nature, and focusing on intention-to-treat analyses to reduce bias (Neurology. 2016 Jul 27;doi: 10.1212/WNL.0000000000002961).
Among 809 initial articles, 5 were considered relevant – a randomized, open-label, multicenter study of the STARFlex device (CLOSURE I), two randomized, controlled trials of the AMPLATZER PFO Occluder (PC Trial and RESPECT), and two randomized studies of warfarin versus aspirin in cryptogenic stroke patients, the experts said.
Percutaneous PFO closure with the STARFlex device did not appear to prevent secondary stroke, compared with medical therapy alone, based on a small positive estimated difference in risk of about 0.1%, and a 95% confidence interval that crossed zero (–2.2% to 2.0%). In contrast, the AMPLATZER PFO Occluder decreased the risk of secondary stroke by about 1.7% (95% CI, –3.2% to –0.2%), but upped the risk of procedural complications by more than 3%, and also slightly increased the risk of new-onset atrial fibrillation (1.6%; 95% CI, 0.1% to 3.2%).
Efficacy data were insufficient to clearly support anticoagulants over antiplatelet therapy for recurrent stroke prevention, the experts concluded. Compared with antiplatelet therapy, anticoagulation was associated with a 2% increase in risk of recurrent stroke, but the 95% confidence interval for this estimate was wide and crossed zero. “In the absence of another indication for anticoagulation, clinicians may routinely offer antiplatelet medications instead of anticoagulation to patients with cryptogenic stroke and PFO,” they wrote. “In rare circumstances, such as stroke that recurs while a patient is undergoing antiplatelet therapy, clinicians may offer anticoagulation to patients with cryptogenic stroke and PFO.”
Their strongest recommendation was to counsel patients who are considering percutaneous PFO closure “that having a PFO is common; it occurs in about 1 in 4 people; it is impossible to determine with certainty whether their PFOs caused their strokes or TIAs; the effectiveness of the procedure for reducing stroke risk remains uncertain; and the procedure is associated with relatively uncommon, yet potentially serious, complications.”
The practice advisory was supported by the American Academy of Neurology. Dr. Messé disclosed ties to GlaxoSmithKline and WL Gore & Associates and has been an investigator for the REDUCE and CLOSURE-I trials. Five of his coauthors have been investigators for RESPECT, CLOSURE-I, and REDUCE, have been editors for Neurology, and have received compensation from Genentech, Pfizer, Gilead Sciences, and other pharmaceutical companies. One coauthor had no disclosures.
An updated practice advisory from the American Academy of Neurology does not recommend the routine use of catheter-based closure of patent foramen ovale in patients with a history of cryptogenic ischemic stroke.
“Because of the limitations of the efficacy evidence and the potential for serious adverse effects, we judge the risk-benefit trade-offs of PFO [patent foramen ovale] closure by either the STARFlex or AMPLATZER PFO Occluder to be uncertain,” wrote Steven Messé, MD, associate professor of neurology at the University of Pennsylvania, Philadelphia, and his associates. “In rare circumstances, such as recurrent strokes despite adequate medical therapy with no other mechanism identified, clinicians may offer the AMPLATZER PFO Occluder if it is available,” they noted.
They also supported antiplatelet agents over anticoagulants unless patients have another indication for blood thinners, noting “the uncertainty surrounding the benefit of anticoagulation in the setting of PFO, and anticoagulation’s well-known harm profile.”
PFO affects about one in four individuals overall and up to half of cryptogenic stroke patients. The previous (2004) version of this practice advisory cited insufficient evidence to guide optimal therapy for secondary stroke prevention in these patients (Neurology. 2004;Apr 13;62[7]:1042-50). To update the guideline, Dr. Messé and his associates searched the literature for relevant randomized studies, excluding transient ischemic attacks when feasible because of their subjective nature, and focusing on intention-to-treat analyses to reduce bias (Neurology. 2016 Jul 27;doi: 10.1212/WNL.0000000000002961).
Among 809 initial articles, 5 were considered relevant – a randomized, open-label, multicenter study of the STARFlex device (CLOSURE I), two randomized, controlled trials of the AMPLATZER PFO Occluder (PC Trial and RESPECT), and two randomized studies of warfarin versus aspirin in cryptogenic stroke patients, the experts said.
Percutaneous PFO closure with the STARFlex device did not appear to prevent secondary stroke, compared with medical therapy alone, based on a small positive estimated difference in risk of about 0.1%, and a 95% confidence interval that crossed zero (–2.2% to 2.0%). In contrast, the AMPLATZER PFO Occluder decreased the risk of secondary stroke by about 1.7% (95% CI, –3.2% to –0.2%), but upped the risk of procedural complications by more than 3%, and also slightly increased the risk of new-onset atrial fibrillation (1.6%; 95% CI, 0.1% to 3.2%).
Efficacy data were insufficient to clearly support anticoagulants over antiplatelet therapy for recurrent stroke prevention, the experts concluded. Compared with antiplatelet therapy, anticoagulation was associated with a 2% increase in risk of recurrent stroke, but the 95% confidence interval for this estimate was wide and crossed zero. “In the absence of another indication for anticoagulation, clinicians may routinely offer antiplatelet medications instead of anticoagulation to patients with cryptogenic stroke and PFO,” they wrote. “In rare circumstances, such as stroke that recurs while a patient is undergoing antiplatelet therapy, clinicians may offer anticoagulation to patients with cryptogenic stroke and PFO.”
Their strongest recommendation was to counsel patients who are considering percutaneous PFO closure “that having a PFO is common; it occurs in about 1 in 4 people; it is impossible to determine with certainty whether their PFOs caused their strokes or TIAs; the effectiveness of the procedure for reducing stroke risk remains uncertain; and the procedure is associated with relatively uncommon, yet potentially serious, complications.”
The practice advisory was supported by the American Academy of Neurology. Dr. Messé disclosed ties to GlaxoSmithKline and WL Gore & Associates and has been an investigator for the REDUCE and CLOSURE-I trials. Five of his coauthors have been investigators for RESPECT, CLOSURE-I, and REDUCE, have been editors for Neurology, and have received compensation from Genentech, Pfizer, Gilead Sciences, and other pharmaceutical companies. One coauthor had no disclosures.
An updated practice advisory from the American Academy of Neurology does not recommend the routine use of catheter-based closure of patent foramen ovale in patients with a history of cryptogenic ischemic stroke.
“Because of the limitations of the efficacy evidence and the potential for serious adverse effects, we judge the risk-benefit trade-offs of PFO [patent foramen ovale] closure by either the STARFlex or AMPLATZER PFO Occluder to be uncertain,” wrote Steven Messé, MD, associate professor of neurology at the University of Pennsylvania, Philadelphia, and his associates. “In rare circumstances, such as recurrent strokes despite adequate medical therapy with no other mechanism identified, clinicians may offer the AMPLATZER PFO Occluder if it is available,” they noted.
They also supported antiplatelet agents over anticoagulants unless patients have another indication for blood thinners, noting “the uncertainty surrounding the benefit of anticoagulation in the setting of PFO, and anticoagulation’s well-known harm profile.”
PFO affects about one in four individuals overall and up to half of cryptogenic stroke patients. The previous (2004) version of this practice advisory cited insufficient evidence to guide optimal therapy for secondary stroke prevention in these patients (Neurology. 2004;Apr 13;62[7]:1042-50). To update the guideline, Dr. Messé and his associates searched the literature for relevant randomized studies, excluding transient ischemic attacks when feasible because of their subjective nature, and focusing on intention-to-treat analyses to reduce bias (Neurology. 2016 Jul 27;doi: 10.1212/WNL.0000000000002961).
Among 809 initial articles, 5 were considered relevant – a randomized, open-label, multicenter study of the STARFlex device (CLOSURE I), two randomized, controlled trials of the AMPLATZER PFO Occluder (PC Trial and RESPECT), and two randomized studies of warfarin versus aspirin in cryptogenic stroke patients, the experts said.
Percutaneous PFO closure with the STARFlex device did not appear to prevent secondary stroke, compared with medical therapy alone, based on a small positive estimated difference in risk of about 0.1%, and a 95% confidence interval that crossed zero (–2.2% to 2.0%). In contrast, the AMPLATZER PFO Occluder decreased the risk of secondary stroke by about 1.7% (95% CI, –3.2% to –0.2%), but upped the risk of procedural complications by more than 3%, and also slightly increased the risk of new-onset atrial fibrillation (1.6%; 95% CI, 0.1% to 3.2%).
Efficacy data were insufficient to clearly support anticoagulants over antiplatelet therapy for recurrent stroke prevention, the experts concluded. Compared with antiplatelet therapy, anticoagulation was associated with a 2% increase in risk of recurrent stroke, but the 95% confidence interval for this estimate was wide and crossed zero. “In the absence of another indication for anticoagulation, clinicians may routinely offer antiplatelet medications instead of anticoagulation to patients with cryptogenic stroke and PFO,” they wrote. “In rare circumstances, such as stroke that recurs while a patient is undergoing antiplatelet therapy, clinicians may offer anticoagulation to patients with cryptogenic stroke and PFO.”
Their strongest recommendation was to counsel patients who are considering percutaneous PFO closure “that having a PFO is common; it occurs in about 1 in 4 people; it is impossible to determine with certainty whether their PFOs caused their strokes or TIAs; the effectiveness of the procedure for reducing stroke risk remains uncertain; and the procedure is associated with relatively uncommon, yet potentially serious, complications.”
The practice advisory was supported by the American Academy of Neurology. Dr. Messé disclosed ties to GlaxoSmithKline and WL Gore & Associates and has been an investigator for the REDUCE and CLOSURE-I trials. Five of his coauthors have been investigators for RESPECT, CLOSURE-I, and REDUCE, have been editors for Neurology, and have received compensation from Genentech, Pfizer, Gilead Sciences, and other pharmaceutical companies. One coauthor had no disclosures.
FROM NEUROLOGY
CMS proposes bundled payments for AMI, CABG
The Centers for Medicare & Medicaid Services is proposing new bundled payment models for acute myocardial infarction and coronary artery bypass grafting, and a separate payment to incentivize the use of cardiac rehabilitation.
As part of the proposal, CMS also is developing a pathway that would allow the bundle to be recognized as an advanced alternative payment model under the Medicare Access and CHIP Reauthorization Act and qualify the physicians and clinicians being paid through the model for the 5% incentive payment.
The proposed bundled payment model would place patient care accountability for 90 days after discharge on the hospital where acute myocardial infarction care or coronary artery bypass grafting occurred. Beginning July 1, 2017, hospitals in 98 randomly selected metropolitan statistical areas would be placed under this model and monitored for a 5-year period to test whether the model leads to improved outcomes and generates cost savings.
The proposed rule can be seen here and an advanced notice is expected to be published on the Federal Register website on July 26. CMS will be accepting comments on the proposal for 60 days following official publication in the Federal Register.
“In 2014, more than 200,000 Medicare beneficiaries were hospitalized for heart attack treatment or underwent bypass surgery, costing Medicare over $6 billion. But the cost of treating patients varied by 50% across hospitals, and the share of patients readmitted to the hospitals within 30 days varied by more than 50%. And patient experience also varies,” CMS Acting Principal Deputy Administrator and Chief Medical Officer Patrick Conway, MD, said during a July 25 press teleconference introducing the proposal. “In some cases, hospitals, doctors, and rehabilitation facilities work together to support a patient from heart attack or surgery all the way through recovery. But in other cases, coordination breaks down, especially when a patient leaves the hospital. By structuring a payment around a patient’s total experience of care, bundled payments support better care coordination and ultimately better outcomes for patients.”
The hospital would be paid a fixed target price for each care episode, with hospitals delivering higher-quality care receiving a higher target price. The hospital would either keep the savings achieved or, if the costs exceeded the target pricing, have to repay Medicare the difference.
Target prices will be based on historical cost data beginning with hospitalization and extending out 90 days following discharge and adjusted based on the complexity of treatment required. For the 18 months of the program (July 1, 2017, through Dec. 31, 2018) target prices would be based on a blend of two-thirds participant-specific data and one-third regional data. In the third performance year (2019), the mix would move to one-third participant data and two-thirds regional data. Beginning in 2020, only regional data would be used to set target prices.
For heart attacks, the following quality measures are being proposed: Hospital 30-day, all-cause, risk-standardized mortality following acute myocardial infarction hospitalization; excess days in acute care after hospitalization for acute myocardial infarction; Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores; and voluntary hybrid hospital 30-day, all-cause, risk-standardized mortality eMeasure data submission.
For bypass surgery, the quality measures will be the hospital 30-day all-cause, risk-standardized mortality rate following coronary artery bypass graft; and HCAHPS survey scores.
“CMS’s evaluation ... will examine quality during the episode period, after the episode period ends, and for longer durations such as 1-year mortality rates,” the agency said in a fact sheet describing the proposal. “CMS will examine outcomes and patient experience measures such as mortality, readmissions, complications, and other clinically relevant outcomes.”
Separately, the agency is proposing to test a cardiac rehabilitation incentive payment. The two-part cardiac rehabilitation incentive payment would be paid retrospectively based on the total cardiac rehabilitation use of beneficiaries attributable to participant hospitals.
“Currently, only 15% of heart attack patients receive cardiac rehabilitation, even though completing a rehabilitation program can lower the risk of the second heart attack or death,” Dr. Conway said. “Patients who receive cardiac rehabilitation are assigned a team of health care professionals such as cardiologists, dietitians, and physical therapists who help the patient to recover and regain cardiovascular fitness.”
The initial payment would be $25 per cardiac rehabilitation service for each of the first 11 services paid for by Medicare during the 90-day care period for a heart attack or bypass surgery. After 11 services, the payment would increase to $175 during the care period.
The number of sessions would be limited to two 1-hour sessions per day up to 36 sessions over up to 36 weeks, with the option for an additional 36 sessions over an extended period if approved by the local Medicare contractor. Intensive cardiac rehabilitation program sessions would be limited to 72 1-hour sessions, up to six sessions per day, over 18 weeks.
While officials from the American College of Cardiology said that the organization supports the concepts of value-based care, “it is important that bundled care models be carried out in such a way that clinicians are given the time and tools to truly impact patient care in the best ways possible. Changes in payment structures in health care can pose significant challenges to clinicians and must be driven by clinical practices that improve patient outcomes,” ACC President Richard A. Chazal, MD, said in a statement. “We are optimistic that CMS will listen to comments, incorporate feedback from clinicians, and provide ample time for implementation of these new payment models. Our ultimate goal is to improve patient care and to improve heart health.”
The Centers for Medicare & Medicaid Services is proposing new bundled payment models for acute myocardial infarction and coronary artery bypass grafting, and a separate payment to incentivize the use of cardiac rehabilitation.
As part of the proposal, CMS also is developing a pathway that would allow the bundle to be recognized as an advanced alternative payment model under the Medicare Access and CHIP Reauthorization Act and qualify the physicians and clinicians being paid through the model for the 5% incentive payment.
The proposed bundled payment model would place patient care accountability for 90 days after discharge on the hospital where acute myocardial infarction care or coronary artery bypass grafting occurred. Beginning July 1, 2017, hospitals in 98 randomly selected metropolitan statistical areas would be placed under this model and monitored for a 5-year period to test whether the model leads to improved outcomes and generates cost savings.
The proposed rule can be seen here and an advanced notice is expected to be published on the Federal Register website on July 26. CMS will be accepting comments on the proposal for 60 days following official publication in the Federal Register.
“In 2014, more than 200,000 Medicare beneficiaries were hospitalized for heart attack treatment or underwent bypass surgery, costing Medicare over $6 billion. But the cost of treating patients varied by 50% across hospitals, and the share of patients readmitted to the hospitals within 30 days varied by more than 50%. And patient experience also varies,” CMS Acting Principal Deputy Administrator and Chief Medical Officer Patrick Conway, MD, said during a July 25 press teleconference introducing the proposal. “In some cases, hospitals, doctors, and rehabilitation facilities work together to support a patient from heart attack or surgery all the way through recovery. But in other cases, coordination breaks down, especially when a patient leaves the hospital. By structuring a payment around a patient’s total experience of care, bundled payments support better care coordination and ultimately better outcomes for patients.”
The hospital would be paid a fixed target price for each care episode, with hospitals delivering higher-quality care receiving a higher target price. The hospital would either keep the savings achieved or, if the costs exceeded the target pricing, have to repay Medicare the difference.
Target prices will be based on historical cost data beginning with hospitalization and extending out 90 days following discharge and adjusted based on the complexity of treatment required. For the 18 months of the program (July 1, 2017, through Dec. 31, 2018) target prices would be based on a blend of two-thirds participant-specific data and one-third regional data. In the third performance year (2019), the mix would move to one-third participant data and two-thirds regional data. Beginning in 2020, only regional data would be used to set target prices.
For heart attacks, the following quality measures are being proposed: Hospital 30-day, all-cause, risk-standardized mortality following acute myocardial infarction hospitalization; excess days in acute care after hospitalization for acute myocardial infarction; Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores; and voluntary hybrid hospital 30-day, all-cause, risk-standardized mortality eMeasure data submission.
For bypass surgery, the quality measures will be the hospital 30-day all-cause, risk-standardized mortality rate following coronary artery bypass graft; and HCAHPS survey scores.
“CMS’s evaluation ... will examine quality during the episode period, after the episode period ends, and for longer durations such as 1-year mortality rates,” the agency said in a fact sheet describing the proposal. “CMS will examine outcomes and patient experience measures such as mortality, readmissions, complications, and other clinically relevant outcomes.”
Separately, the agency is proposing to test a cardiac rehabilitation incentive payment. The two-part cardiac rehabilitation incentive payment would be paid retrospectively based on the total cardiac rehabilitation use of beneficiaries attributable to participant hospitals.
“Currently, only 15% of heart attack patients receive cardiac rehabilitation, even though completing a rehabilitation program can lower the risk of the second heart attack or death,” Dr. Conway said. “Patients who receive cardiac rehabilitation are assigned a team of health care professionals such as cardiologists, dietitians, and physical therapists who help the patient to recover and regain cardiovascular fitness.”
The initial payment would be $25 per cardiac rehabilitation service for each of the first 11 services paid for by Medicare during the 90-day care period for a heart attack or bypass surgery. After 11 services, the payment would increase to $175 during the care period.
The number of sessions would be limited to two 1-hour sessions per day up to 36 sessions over up to 36 weeks, with the option for an additional 36 sessions over an extended period if approved by the local Medicare contractor. Intensive cardiac rehabilitation program sessions would be limited to 72 1-hour sessions, up to six sessions per day, over 18 weeks.
While officials from the American College of Cardiology said that the organization supports the concepts of value-based care, “it is important that bundled care models be carried out in such a way that clinicians are given the time and tools to truly impact patient care in the best ways possible. Changes in payment structures in health care can pose significant challenges to clinicians and must be driven by clinical practices that improve patient outcomes,” ACC President Richard A. Chazal, MD, said in a statement. “We are optimistic that CMS will listen to comments, incorporate feedback from clinicians, and provide ample time for implementation of these new payment models. Our ultimate goal is to improve patient care and to improve heart health.”
The Centers for Medicare & Medicaid Services is proposing new bundled payment models for acute myocardial infarction and coronary artery bypass grafting, and a separate payment to incentivize the use of cardiac rehabilitation.
As part of the proposal, CMS also is developing a pathway that would allow the bundle to be recognized as an advanced alternative payment model under the Medicare Access and CHIP Reauthorization Act and qualify the physicians and clinicians being paid through the model for the 5% incentive payment.
The proposed bundled payment model would place patient care accountability for 90 days after discharge on the hospital where acute myocardial infarction care or coronary artery bypass grafting occurred. Beginning July 1, 2017, hospitals in 98 randomly selected metropolitan statistical areas would be placed under this model and monitored for a 5-year period to test whether the model leads to improved outcomes and generates cost savings.
The proposed rule can be seen here and an advanced notice is expected to be published on the Federal Register website on July 26. CMS will be accepting comments on the proposal for 60 days following official publication in the Federal Register.
“In 2014, more than 200,000 Medicare beneficiaries were hospitalized for heart attack treatment or underwent bypass surgery, costing Medicare over $6 billion. But the cost of treating patients varied by 50% across hospitals, and the share of patients readmitted to the hospitals within 30 days varied by more than 50%. And patient experience also varies,” CMS Acting Principal Deputy Administrator and Chief Medical Officer Patrick Conway, MD, said during a July 25 press teleconference introducing the proposal. “In some cases, hospitals, doctors, and rehabilitation facilities work together to support a patient from heart attack or surgery all the way through recovery. But in other cases, coordination breaks down, especially when a patient leaves the hospital. By structuring a payment around a patient’s total experience of care, bundled payments support better care coordination and ultimately better outcomes for patients.”
The hospital would be paid a fixed target price for each care episode, with hospitals delivering higher-quality care receiving a higher target price. The hospital would either keep the savings achieved or, if the costs exceeded the target pricing, have to repay Medicare the difference.
Target prices will be based on historical cost data beginning with hospitalization and extending out 90 days following discharge and adjusted based on the complexity of treatment required. For the 18 months of the program (July 1, 2017, through Dec. 31, 2018) target prices would be based on a blend of two-thirds participant-specific data and one-third regional data. In the third performance year (2019), the mix would move to one-third participant data and two-thirds regional data. Beginning in 2020, only regional data would be used to set target prices.
For heart attacks, the following quality measures are being proposed: Hospital 30-day, all-cause, risk-standardized mortality following acute myocardial infarction hospitalization; excess days in acute care after hospitalization for acute myocardial infarction; Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores; and voluntary hybrid hospital 30-day, all-cause, risk-standardized mortality eMeasure data submission.
For bypass surgery, the quality measures will be the hospital 30-day all-cause, risk-standardized mortality rate following coronary artery bypass graft; and HCAHPS survey scores.
“CMS’s evaluation ... will examine quality during the episode period, after the episode period ends, and for longer durations such as 1-year mortality rates,” the agency said in a fact sheet describing the proposal. “CMS will examine outcomes and patient experience measures such as mortality, readmissions, complications, and other clinically relevant outcomes.”
Separately, the agency is proposing to test a cardiac rehabilitation incentive payment. The two-part cardiac rehabilitation incentive payment would be paid retrospectively based on the total cardiac rehabilitation use of beneficiaries attributable to participant hospitals.
“Currently, only 15% of heart attack patients receive cardiac rehabilitation, even though completing a rehabilitation program can lower the risk of the second heart attack or death,” Dr. Conway said. “Patients who receive cardiac rehabilitation are assigned a team of health care professionals such as cardiologists, dietitians, and physical therapists who help the patient to recover and regain cardiovascular fitness.”
The initial payment would be $25 per cardiac rehabilitation service for each of the first 11 services paid for by Medicare during the 90-day care period for a heart attack or bypass surgery. After 11 services, the payment would increase to $175 during the care period.
The number of sessions would be limited to two 1-hour sessions per day up to 36 sessions over up to 36 weeks, with the option for an additional 36 sessions over an extended period if approved by the local Medicare contractor. Intensive cardiac rehabilitation program sessions would be limited to 72 1-hour sessions, up to six sessions per day, over 18 weeks.
While officials from the American College of Cardiology said that the organization supports the concepts of value-based care, “it is important that bundled care models be carried out in such a way that clinicians are given the time and tools to truly impact patient care in the best ways possible. Changes in payment structures in health care can pose significant challenges to clinicians and must be driven by clinical practices that improve patient outcomes,” ACC President Richard A. Chazal, MD, said in a statement. “We are optimistic that CMS will listen to comments, incorporate feedback from clinicians, and provide ample time for implementation of these new payment models. Our ultimate goal is to improve patient care and to improve heart health.”
Anatomic repair of ccTGA did not yield superior survival
BALTIMORE – Anatomic repair did not outperform physiologic repair in patients with congenitally corrected transposition of the great arteries (ccTGA), according to a study presented by Maryam Al-Omair, M.D., of the University of Toronto at the annual meeting of the American Association for Thoracic Surgery.
Dr. Al-Omair and her colleagues hypothesized that patients undergoing anatomic repair for ccTGA would have superior systemic ventricular function and survival. However, their results showed that anatomic repair of ccTGA did not yield superior survival, compared with physiologic repair, and the long-term impact on systemic ventricular function was not certain.
Because of early evidence showing better outcomes of anatomic over physiologic repair for ccTGA, the surgical trend over time greatly favored the use of anatomic repair: At her team’s institution, anatomic repair went from 2.3% in the 1982-1989 period to 92.3% in the 2010-2015 period, Dr. Al-Omair said.
Their study assessed 200 patients (165 with biventricular ccTGA and 35 Fontan patients) who were managed from 1982 to 2015 at the Hospital for Sick Children, Toronto. The patient treatment groups were anatomic repair (38 patients), physiologic repair (89), single-ventricle (Fontan) repair (35), and palliated (no intracardiac repair) patients (38). The median follow-up was 3.4 years for anatomic repair, 13.5 years for physiologic repair, 7.5 years for single-ventricle repair, and 11.8 years with no repair (11.8 years), reflecting their change in practice.
The investigators followed the primary outcome of transplant-free survival and secondary outcomes of late systemic ventricular function and systemic atrioventricular valve function.
They found no significant difference in transplant-free survival at 20 years in the three repair groups assessed from 1892 to 2105: anatomic repair (58%), physiologic repair (71%), and single-ventricle (Fontan) repair (78%). Looking at the latter period of 2000-2015 for 10-year transplant-free survival, they found similar results: anatomic repair (77%), physiologic repair (85%), and single-ventricle (Fontan) repair (100%).
They also found that transplant-free survival in patients who required no intracadiac repair and had no associated lesions such as ventral septal defect or ventral septal defect with pulmonary stenosis was nearly 95% at 25 years.
A multivariate analysis showed no independent predictors of mortality among the three treatments, patient age at index operation, or period of treatment, as well as the need for a permanent pacemaker, or moderately to severely reduced ventricular function or moderate to severe valve regurgitation after the index operation, according to Dr. Al-Omair.
For the secondary outcome of late systemic ventricular function, a multivariate analysis showed that two of the variables were independent predictors: Index operation at or after 2000 was shown to be protective (hazard ratio, 0.152), while a negative association was seen with moderately to severely reduced ventricular function after the index operation (HR, 12.4).
For the secondary outcome of late systemic valve function, a multivariate analysis showed that three of the variables were independent predictors: Fontan operation (HR, 0.124) and index operation at or after 2000 (HR, 0.258) were shown to be protective, while a negative association was seen with moderately to severely reduced valve regurgitation after the index operation (HR, 9.00).
The researchers concluded that midterm Fontan survival was relatively favorable, pushing borderline repair may not be necessary, and “prophylactic banding” and the double-switch procedure should be looked on with caution for lower-risk patients.
“Our study also showed that survival was best in those having no associated lesions requiring operation, indicating that performing an anatomic repair for those not having associated lesions could be counterproductive,” Dr. Al-Omair concluded.
The webcast of the annual meeting presentation is available at www.aats.org.
Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
The choice of anatomic vs. physiologic repair of congenitally corrected transposition of the great arteries is a controversial area, with many well-known surgeons and centers advocating for anatomic repair (a much tougher and more challenging operation) as opposed to physiologic repair. The Toronto group is to be applauded for this honest conclusion, which goes a bit against the currently fashionable “more is better” approach.
Robert Jaquiss, M.D., of Duke University, Durham, N.C., is the congenital heart disease associate medical editor for Thoracic Surgery News.
The choice of anatomic vs. physiologic repair of congenitally corrected transposition of the great arteries is a controversial area, with many well-known surgeons and centers advocating for anatomic repair (a much tougher and more challenging operation) as opposed to physiologic repair. The Toronto group is to be applauded for this honest conclusion, which goes a bit against the currently fashionable “more is better” approach.
Robert Jaquiss, M.D., of Duke University, Durham, N.C., is the congenital heart disease associate medical editor for Thoracic Surgery News.
The choice of anatomic vs. physiologic repair of congenitally corrected transposition of the great arteries is a controversial area, with many well-known surgeons and centers advocating for anatomic repair (a much tougher and more challenging operation) as opposed to physiologic repair. The Toronto group is to be applauded for this honest conclusion, which goes a bit against the currently fashionable “more is better” approach.
Robert Jaquiss, M.D., of Duke University, Durham, N.C., is the congenital heart disease associate medical editor for Thoracic Surgery News.
BALTIMORE – Anatomic repair did not outperform physiologic repair in patients with congenitally corrected transposition of the great arteries (ccTGA), according to a study presented by Maryam Al-Omair, M.D., of the University of Toronto at the annual meeting of the American Association for Thoracic Surgery.
Dr. Al-Omair and her colleagues hypothesized that patients undergoing anatomic repair for ccTGA would have superior systemic ventricular function and survival. However, their results showed that anatomic repair of ccTGA did not yield superior survival, compared with physiologic repair, and the long-term impact on systemic ventricular function was not certain.
Because of early evidence showing better outcomes of anatomic over physiologic repair for ccTGA, the surgical trend over time greatly favored the use of anatomic repair: At her team’s institution, anatomic repair went from 2.3% in the 1982-1989 period to 92.3% in the 2010-2015 period, Dr. Al-Omair said.
Their study assessed 200 patients (165 with biventricular ccTGA and 35 Fontan patients) who were managed from 1982 to 2015 at the Hospital for Sick Children, Toronto. The patient treatment groups were anatomic repair (38 patients), physiologic repair (89), single-ventricle (Fontan) repair (35), and palliated (no intracardiac repair) patients (38). The median follow-up was 3.4 years for anatomic repair, 13.5 years for physiologic repair, 7.5 years for single-ventricle repair, and 11.8 years with no repair (11.8 years), reflecting their change in practice.
The investigators followed the primary outcome of transplant-free survival and secondary outcomes of late systemic ventricular function and systemic atrioventricular valve function.
They found no significant difference in transplant-free survival at 20 years in the three repair groups assessed from 1892 to 2105: anatomic repair (58%), physiologic repair (71%), and single-ventricle (Fontan) repair (78%). Looking at the latter period of 2000-2015 for 10-year transplant-free survival, they found similar results: anatomic repair (77%), physiologic repair (85%), and single-ventricle (Fontan) repair (100%).
They also found that transplant-free survival in patients who required no intracadiac repair and had no associated lesions such as ventral septal defect or ventral septal defect with pulmonary stenosis was nearly 95% at 25 years.
A multivariate analysis showed no independent predictors of mortality among the three treatments, patient age at index operation, or period of treatment, as well as the need for a permanent pacemaker, or moderately to severely reduced ventricular function or moderate to severe valve regurgitation after the index operation, according to Dr. Al-Omair.
For the secondary outcome of late systemic ventricular function, a multivariate analysis showed that two of the variables were independent predictors: Index operation at or after 2000 was shown to be protective (hazard ratio, 0.152), while a negative association was seen with moderately to severely reduced ventricular function after the index operation (HR, 12.4).
For the secondary outcome of late systemic valve function, a multivariate analysis showed that three of the variables were independent predictors: Fontan operation (HR, 0.124) and index operation at or after 2000 (HR, 0.258) were shown to be protective, while a negative association was seen with moderately to severely reduced valve regurgitation after the index operation (HR, 9.00).
The researchers concluded that midterm Fontan survival was relatively favorable, pushing borderline repair may not be necessary, and “prophylactic banding” and the double-switch procedure should be looked on with caution for lower-risk patients.
“Our study also showed that survival was best in those having no associated lesions requiring operation, indicating that performing an anatomic repair for those not having associated lesions could be counterproductive,” Dr. Al-Omair concluded.
The webcast of the annual meeting presentation is available at www.aats.org.
Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
BALTIMORE – Anatomic repair did not outperform physiologic repair in patients with congenitally corrected transposition of the great arteries (ccTGA), according to a study presented by Maryam Al-Omair, M.D., of the University of Toronto at the annual meeting of the American Association for Thoracic Surgery.
Dr. Al-Omair and her colleagues hypothesized that patients undergoing anatomic repair for ccTGA would have superior systemic ventricular function and survival. However, their results showed that anatomic repair of ccTGA did not yield superior survival, compared with physiologic repair, and the long-term impact on systemic ventricular function was not certain.
Because of early evidence showing better outcomes of anatomic over physiologic repair for ccTGA, the surgical trend over time greatly favored the use of anatomic repair: At her team’s institution, anatomic repair went from 2.3% in the 1982-1989 period to 92.3% in the 2010-2015 period, Dr. Al-Omair said.
Their study assessed 200 patients (165 with biventricular ccTGA and 35 Fontan patients) who were managed from 1982 to 2015 at the Hospital for Sick Children, Toronto. The patient treatment groups were anatomic repair (38 patients), physiologic repair (89), single-ventricle (Fontan) repair (35), and palliated (no intracardiac repair) patients (38). The median follow-up was 3.4 years for anatomic repair, 13.5 years for physiologic repair, 7.5 years for single-ventricle repair, and 11.8 years with no repair (11.8 years), reflecting their change in practice.
The investigators followed the primary outcome of transplant-free survival and secondary outcomes of late systemic ventricular function and systemic atrioventricular valve function.
They found no significant difference in transplant-free survival at 20 years in the three repair groups assessed from 1892 to 2105: anatomic repair (58%), physiologic repair (71%), and single-ventricle (Fontan) repair (78%). Looking at the latter period of 2000-2015 for 10-year transplant-free survival, they found similar results: anatomic repair (77%), physiologic repair (85%), and single-ventricle (Fontan) repair (100%).
They also found that transplant-free survival in patients who required no intracadiac repair and had no associated lesions such as ventral septal defect or ventral septal defect with pulmonary stenosis was nearly 95% at 25 years.
A multivariate analysis showed no independent predictors of mortality among the three treatments, patient age at index operation, or period of treatment, as well as the need for a permanent pacemaker, or moderately to severely reduced ventricular function or moderate to severe valve regurgitation after the index operation, according to Dr. Al-Omair.
For the secondary outcome of late systemic ventricular function, a multivariate analysis showed that two of the variables were independent predictors: Index operation at or after 2000 was shown to be protective (hazard ratio, 0.152), while a negative association was seen with moderately to severely reduced ventricular function after the index operation (HR, 12.4).
For the secondary outcome of late systemic valve function, a multivariate analysis showed that three of the variables were independent predictors: Fontan operation (HR, 0.124) and index operation at or after 2000 (HR, 0.258) were shown to be protective, while a negative association was seen with moderately to severely reduced valve regurgitation after the index operation (HR, 9.00).
The researchers concluded that midterm Fontan survival was relatively favorable, pushing borderline repair may not be necessary, and “prophylactic banding” and the double-switch procedure should be looked on with caution for lower-risk patients.
“Our study also showed that survival was best in those having no associated lesions requiring operation, indicating that performing an anatomic repair for those not having associated lesions could be counterproductive,” Dr. Al-Omair concluded.
The webcast of the annual meeting presentation is available at www.aats.org.
Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
AT THE AATS ANNUAL MEETING
Key clinical point: Performing an anatomic repair for ccTGA in patients without associated lesions could be counterproductive.
Major finding: There was no significant difference in transplant-free survival at 20 years among anatomic repair (58%), physiologic repair (71%), and single-ventricle repair (78%).
Data source: A single-institution study assessing 200 patients with ccGTA/Fontan who were managed from 1982 to 2015.
Disclosures: Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
MRI-VA improves view of anomalous coronary arteries
Failure to achieve a rounded and unobstructed ostia in children who have surgery to repair anomalous coronary arteries can put these children at continued risk for sudden death, but cardiac MRI with virtual angioscopy (VA) before and after the operation can give cardiologists a clear picture of a patient’s risk for sudden death and help direct ongoing management, according to a study in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:205-10).
“Cardiac MRI with virtual angioscopy is an important tool for evaluating anomalous coronary anatomy, myocardial function, and ischemia and should be considered for initial and postoperative assessment of children with anomalous coronary arteries,” lead author Julie A. Brothers, MD, and her coauthors said in reporting their findings.
Anomalous coronary artery is a rare congenital condition in which the left coronary artery (LCA) originates from the right sinus or the right coronary artery (RCA) originates from the left coronary sinus. Dr. Brothers, a pediatric cardiologist, and her colleagues from the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia, studied nine male patients who had operations for anomalous coronary arteries during Feb. 2009-May 2015 in what they said is the first study to document anomalous coronary artery anatomy both before and after surgery. The patients’ average age was 14.1 years; seven had right anomalous coronary arteries and two had left anomalous arteries. After the operations, MRI-VA revealed that two patients still had narrowing in the neo-orifices.
Previous reports recommend surgical repair for all patients with anomalous LCA and for symptomatic patients with anomalous RCA anatomy (Ann Thorac Surg. 2011;92:691-7; Ann Thorac Surg. 2014;98:941-5). MRI-VA allows the surgical team to survey the ostial stenosis before the operation “as if standing within the vessel itself,” Dr. Brothers and her coauthors wrote. Afterward, MRI-VA lets the surgeon and team see if the operation succeeded in repairing the orifices.
In the study population, VA before surgery confirmed elliptical, slit-like orifices in all patients. The operations involved unroofing procedures; two patients also had detachment and resuspension procedures during surgery. After surgery, VA showed that seven patients had round, patent, unobstructed repaired orifices; but two had orifices that were still narrow and somewhat stenotic, Dr. Brothers and her coauthors said. The study group had postoperative MRI-VA an average of 8.6 months after surgery.
“The significance of these findings is unknown; however, if the proposed mechanism of ischemia is due to a slit-like orifice, a continued stenotic orifice may place subjects at risk for sudden death,” the researchers said. The two study patients with the narrowed, stenotic orifices have remained symptom free, with no evidence of ischemia on exercise stress test or cardiac MRI. “These subjects will need to be followed up in the future to monitor for progression or resolution,” the study authors wrote.
Sudden cardiac death (SCD) is more common in anomalous aortic origin of the LCA than the RCA, Dr. Brothers and her colleagues said. Thus, an elliptical, slit-like neo-orifice is a concern because it can become blocked during exercise, possibly leading to lethal ventricular arrhythmia, they said. Ischemia in patients with anomalous coronary artery seems to result from a cumulative effect of exercise.
Patients who undergo the modified unroofing procedure typically have electrocardiography and echocardiography afterward and then get cleared to return to competitive sports in about 3 months if their stress test indicates it. Dr. Brothers and her colleagues said this activity recommendation may need alteration for those patients who have had a heart attack or sudden cardiac arrest, because they may remain at increased risk of SCD after surgery. “At the very least, additional imaging, such as with MRI-VA, should be used in this population,” the study authors said.
While Dr. Brothers and her colleagues acknowledged the small sample size is a limitation of the study, they also pointed out that anomalous coronary artery is a rare disease. They also noted that high-quality VA images can be difficult to obtain in noncompliant patients or those have arrhythmia or irregular breathing. “The images obtained in this study were acquired at an institution very familiar with pediatric cardiac coronary MRI and would be appropriate for assessing the coronary ostia with VA,” they said.
Dr. Brothers and her coauthors had no financial disclosures.
The MRI technique that Dr. Brothers and her colleagues reported on can provide important details of the anomalous coronary anatomy and about myocardial function, Philip S. Naimo, MD, Edward Buratto, MBBS, and Igor Konstantinov, MD, PhD, FRACS, of the Royal Children’s Hospital, University of Melbourne, wrote in their invited commentary. But, the ability to evaluate the neo-ostium after surgery had “particular value,” the commentators said (J. Thorac. Cardiovasc. Surg. 2016 Jul;152:211-12).
MRI with virtual angioscopy can fill help fill in the gaps where the significance of a narrowed neo-ostium is unknown, the commentators said. “The combination of anatomic information on the ostium size, shape, and location, as well as functional information on wall motion and myocardial perfusion, which can be provided by MRI-VA, would be particularly valuable in these patients,” they said.
They also pointed out that MRI-VA could be used in patients who have ongoing but otherwise undetected narrowing of the ostia after the unroofing procedure. At the same time, the technique will also require sufficient caseloads to maintain expertise. “It is safe to say that MRI-VA is here to stay,” Dr. Naimo, Dr. Buratto, and Dr. Konstantinov wrote. “The actual application of this virtual modality will need further refinement to be used routinely.”
The commentary authors had no financial relationships to disclose.
The MRI technique that Dr. Brothers and her colleagues reported on can provide important details of the anomalous coronary anatomy and about myocardial function, Philip S. Naimo, MD, Edward Buratto, MBBS, and Igor Konstantinov, MD, PhD, FRACS, of the Royal Children’s Hospital, University of Melbourne, wrote in their invited commentary. But, the ability to evaluate the neo-ostium after surgery had “particular value,” the commentators said (J. Thorac. Cardiovasc. Surg. 2016 Jul;152:211-12).
MRI with virtual angioscopy can fill help fill in the gaps where the significance of a narrowed neo-ostium is unknown, the commentators said. “The combination of anatomic information on the ostium size, shape, and location, as well as functional information on wall motion and myocardial perfusion, which can be provided by MRI-VA, would be particularly valuable in these patients,” they said.
They also pointed out that MRI-VA could be used in patients who have ongoing but otherwise undetected narrowing of the ostia after the unroofing procedure. At the same time, the technique will also require sufficient caseloads to maintain expertise. “It is safe to say that MRI-VA is here to stay,” Dr. Naimo, Dr. Buratto, and Dr. Konstantinov wrote. “The actual application of this virtual modality will need further refinement to be used routinely.”
The commentary authors had no financial relationships to disclose.
The MRI technique that Dr. Brothers and her colleagues reported on can provide important details of the anomalous coronary anatomy and about myocardial function, Philip S. Naimo, MD, Edward Buratto, MBBS, and Igor Konstantinov, MD, PhD, FRACS, of the Royal Children’s Hospital, University of Melbourne, wrote in their invited commentary. But, the ability to evaluate the neo-ostium after surgery had “particular value,” the commentators said (J. Thorac. Cardiovasc. Surg. 2016 Jul;152:211-12).
MRI with virtual angioscopy can fill help fill in the gaps where the significance of a narrowed neo-ostium is unknown, the commentators said. “The combination of anatomic information on the ostium size, shape, and location, as well as functional information on wall motion and myocardial perfusion, which can be provided by MRI-VA, would be particularly valuable in these patients,” they said.
They also pointed out that MRI-VA could be used in patients who have ongoing but otherwise undetected narrowing of the ostia after the unroofing procedure. At the same time, the technique will also require sufficient caseloads to maintain expertise. “It is safe to say that MRI-VA is here to stay,” Dr. Naimo, Dr. Buratto, and Dr. Konstantinov wrote. “The actual application of this virtual modality will need further refinement to be used routinely.”
The commentary authors had no financial relationships to disclose.
Failure to achieve a rounded and unobstructed ostia in children who have surgery to repair anomalous coronary arteries can put these children at continued risk for sudden death, but cardiac MRI with virtual angioscopy (VA) before and after the operation can give cardiologists a clear picture of a patient’s risk for sudden death and help direct ongoing management, according to a study in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:205-10).
“Cardiac MRI with virtual angioscopy is an important tool for evaluating anomalous coronary anatomy, myocardial function, and ischemia and should be considered for initial and postoperative assessment of children with anomalous coronary arteries,” lead author Julie A. Brothers, MD, and her coauthors said in reporting their findings.
Anomalous coronary artery is a rare congenital condition in which the left coronary artery (LCA) originates from the right sinus or the right coronary artery (RCA) originates from the left coronary sinus. Dr. Brothers, a pediatric cardiologist, and her colleagues from the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia, studied nine male patients who had operations for anomalous coronary arteries during Feb. 2009-May 2015 in what they said is the first study to document anomalous coronary artery anatomy both before and after surgery. The patients’ average age was 14.1 years; seven had right anomalous coronary arteries and two had left anomalous arteries. After the operations, MRI-VA revealed that two patients still had narrowing in the neo-orifices.
Previous reports recommend surgical repair for all patients with anomalous LCA and for symptomatic patients with anomalous RCA anatomy (Ann Thorac Surg. 2011;92:691-7; Ann Thorac Surg. 2014;98:941-5). MRI-VA allows the surgical team to survey the ostial stenosis before the operation “as if standing within the vessel itself,” Dr. Brothers and her coauthors wrote. Afterward, MRI-VA lets the surgeon and team see if the operation succeeded in repairing the orifices.
In the study population, VA before surgery confirmed elliptical, slit-like orifices in all patients. The operations involved unroofing procedures; two patients also had detachment and resuspension procedures during surgery. After surgery, VA showed that seven patients had round, patent, unobstructed repaired orifices; but two had orifices that were still narrow and somewhat stenotic, Dr. Brothers and her coauthors said. The study group had postoperative MRI-VA an average of 8.6 months after surgery.
“The significance of these findings is unknown; however, if the proposed mechanism of ischemia is due to a slit-like orifice, a continued stenotic orifice may place subjects at risk for sudden death,” the researchers said. The two study patients with the narrowed, stenotic orifices have remained symptom free, with no evidence of ischemia on exercise stress test or cardiac MRI. “These subjects will need to be followed up in the future to monitor for progression or resolution,” the study authors wrote.
Sudden cardiac death (SCD) is more common in anomalous aortic origin of the LCA than the RCA, Dr. Brothers and her colleagues said. Thus, an elliptical, slit-like neo-orifice is a concern because it can become blocked during exercise, possibly leading to lethal ventricular arrhythmia, they said. Ischemia in patients with anomalous coronary artery seems to result from a cumulative effect of exercise.
Patients who undergo the modified unroofing procedure typically have electrocardiography and echocardiography afterward and then get cleared to return to competitive sports in about 3 months if their stress test indicates it. Dr. Brothers and her colleagues said this activity recommendation may need alteration for those patients who have had a heart attack or sudden cardiac arrest, because they may remain at increased risk of SCD after surgery. “At the very least, additional imaging, such as with MRI-VA, should be used in this population,” the study authors said.
While Dr. Brothers and her colleagues acknowledged the small sample size is a limitation of the study, they also pointed out that anomalous coronary artery is a rare disease. They also noted that high-quality VA images can be difficult to obtain in noncompliant patients or those have arrhythmia or irregular breathing. “The images obtained in this study were acquired at an institution very familiar with pediatric cardiac coronary MRI and would be appropriate for assessing the coronary ostia with VA,” they said.
Dr. Brothers and her coauthors had no financial disclosures.
Failure to achieve a rounded and unobstructed ostia in children who have surgery to repair anomalous coronary arteries can put these children at continued risk for sudden death, but cardiac MRI with virtual angioscopy (VA) before and after the operation can give cardiologists a clear picture of a patient’s risk for sudden death and help direct ongoing management, according to a study in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:205-10).
“Cardiac MRI with virtual angioscopy is an important tool for evaluating anomalous coronary anatomy, myocardial function, and ischemia and should be considered for initial and postoperative assessment of children with anomalous coronary arteries,” lead author Julie A. Brothers, MD, and her coauthors said in reporting their findings.
Anomalous coronary artery is a rare congenital condition in which the left coronary artery (LCA) originates from the right sinus or the right coronary artery (RCA) originates from the left coronary sinus. Dr. Brothers, a pediatric cardiologist, and her colleagues from the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia, studied nine male patients who had operations for anomalous coronary arteries during Feb. 2009-May 2015 in what they said is the first study to document anomalous coronary artery anatomy both before and after surgery. The patients’ average age was 14.1 years; seven had right anomalous coronary arteries and two had left anomalous arteries. After the operations, MRI-VA revealed that two patients still had narrowing in the neo-orifices.
Previous reports recommend surgical repair for all patients with anomalous LCA and for symptomatic patients with anomalous RCA anatomy (Ann Thorac Surg. 2011;92:691-7; Ann Thorac Surg. 2014;98:941-5). MRI-VA allows the surgical team to survey the ostial stenosis before the operation “as if standing within the vessel itself,” Dr. Brothers and her coauthors wrote. Afterward, MRI-VA lets the surgeon and team see if the operation succeeded in repairing the orifices.
In the study population, VA before surgery confirmed elliptical, slit-like orifices in all patients. The operations involved unroofing procedures; two patients also had detachment and resuspension procedures during surgery. After surgery, VA showed that seven patients had round, patent, unobstructed repaired orifices; but two had orifices that were still narrow and somewhat stenotic, Dr. Brothers and her coauthors said. The study group had postoperative MRI-VA an average of 8.6 months after surgery.
“The significance of these findings is unknown; however, if the proposed mechanism of ischemia is due to a slit-like orifice, a continued stenotic orifice may place subjects at risk for sudden death,” the researchers said. The two study patients with the narrowed, stenotic orifices have remained symptom free, with no evidence of ischemia on exercise stress test or cardiac MRI. “These subjects will need to be followed up in the future to monitor for progression or resolution,” the study authors wrote.
Sudden cardiac death (SCD) is more common in anomalous aortic origin of the LCA than the RCA, Dr. Brothers and her colleagues said. Thus, an elliptical, slit-like neo-orifice is a concern because it can become blocked during exercise, possibly leading to lethal ventricular arrhythmia, they said. Ischemia in patients with anomalous coronary artery seems to result from a cumulative effect of exercise.
Patients who undergo the modified unroofing procedure typically have electrocardiography and echocardiography afterward and then get cleared to return to competitive sports in about 3 months if their stress test indicates it. Dr. Brothers and her colleagues said this activity recommendation may need alteration for those patients who have had a heart attack or sudden cardiac arrest, because they may remain at increased risk of SCD after surgery. “At the very least, additional imaging, such as with MRI-VA, should be used in this population,” the study authors said.
While Dr. Brothers and her colleagues acknowledged the small sample size is a limitation of the study, they also pointed out that anomalous coronary artery is a rare disease. They also noted that high-quality VA images can be difficult to obtain in noncompliant patients or those have arrhythmia or irregular breathing. “The images obtained in this study were acquired at an institution very familiar with pediatric cardiac coronary MRI and would be appropriate for assessing the coronary ostia with VA,” they said.
Dr. Brothers and her coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Cardiac MRI with virtual angioscopy (VA) can perform pre- and postoperative assessment in pediatric patients with anomalous coronary arteries.
Major finding: MRI-VA showed that neo-ostium in seven patients were round and unobstructed after surgery, but remained elliptical and somewhat stenotic in two patients.
Data source: Nine male patients aged 5-19 years who had modified unroofing procedure for anomalous coronary artery anatomy at a single institution between February 2009 and May 2015.
Disclosures: Dr. Brothers and coauthors had no financial relationships to disclose.
Syndecan-1 may predict kidney injury after ped heart surgery
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The biomarker syndecan-1 may aid in determining acute kidney injury risk for children having cardiac surgery.
Major finding: Children with elevated levels of syndecan-1 had a two- to ninefold greater risk of acute kidney injury.
Data source: Single-institution, prospective cohort study of 289 pediatric patients who had cardiac surgery from September 2013 to December 2014.
Disclosures: Dr. Cavalcante and coauthors had no financial relationships to disclose.
Making the case for CABG using bilateral thoracic arteries
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: No specific technique for bilateral internal thoracic artery (BITA) graft in coronary artery bypass grafting (CABG) has an advantage over other techniques.
Major finding: Among four different BITA configurations, no in-hospital deaths occurred and the late cardiac death rate was around 5% for three of the four groups and 0% for the fourth group.
Data source: Single-center, retrospective study of 762 patients who had CABG with use of BITA from 1997 to 2014.
Disclosures: Dr. Magruder and colleagues reported having no financial disclosures.
Four-branched arch replacement gets acceptable results
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
AT THE AATS AORTIC SYMPOSIUM 2016
Key clinical point: Four-branched total aortic arch replacement can achieve acceptable early and late results.
Major finding: Overall in-hospital mortality was 5.2% and 5-year survival was 80.7%.
Data source: Consecutive series of 1,005 patients who had total arch replacement between 2001 and 2016 at two centers in Japan.
Disclosures: Dr. Minatoya reported having no financial disclosures.
Pediatric autologous aortic repair built to last
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Surgeons must think of outcomes for operations to correct aortic arch disease in children in the context of decades, not years.
Major finding: Five principles should guide autologous aortic arch repair in newborns, infants, and children.
Data source: Case studies from Texas Children’s Hospital.
Disclosures: Dr. Fraser reported having no relevant financial disclosures.