User login
VIDEO: Consider cognitive function in elderly before surgery
COPENHAGEN – Almost half of patients with mild cognitive impairment progressed to dementia within 1 year of undergoing either arthroplasty or coronary angiography, according to a small Australian study.
Baseline cognitive impairment appeared to be the main driver of progression, increasing the risk more than sevenfold – significantly more than age or heart attack, Lisbeth Evered, Ph.D., said at the annual Alzheimer’s Association International Conference.
"After 12 months, 42% met the criteria for dementia," said Dr. Evered, a researcher at the University of Melbourne. "The expected annual progression from mild cognitive impairment [MCI] to dementia would be about 10%-12% per year."
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Her study included 67 patients with a mean age of 70 years. All had MCI at baseline, with a mean score of 23 on the Mini-Mental State Exam (MMSE). They underwent either arthroplasty (26 patients) or coronary angiography (41 patients).
A year after surgery, about 34% of the arthroplasty patients and 46% of the angiography patients had progressed to dementia. Baseline cognitive impairment was the only factor significantly associated with the change.
Postsurgical cognitive decline, both transient and long lasting, is a well-documented phenomenon, with studies going back to the late 1800s. Although the causative link isn’t entirely clear, anesthetics have long been implicated, said Dr. Evered. In animal models, some anesthesia drugs do seem to precipitate an Alzheimer’s-like amyloidosis and tau hyperphosphorylation.
More recent animal data suggest that inflammation might be a powerful influence.
"When a patient has surgery with a general anesthetic, they experience peripheral inflammation," Dr. Evered explained. "In a healthy normal brain, there’s plenty of cognitive reserve, and although there might be some cognitive decline afterward, the person won’t really notice and will certainly recover."
In a vulnerable brain, however, the inflammation may be amplified and may cause significant collateral damage that accelerates cognitive decline. "The problem is, we don’t know why they are vulnerable or what we might do about it," she noted.
The best approach now is to routinely assess cognition before surgery and monitor it afterward, Dr. Evered explained. "Then, the perioperative period is not something occurring in isolation," she noted. "We will be better able to identify those at risk and implement strategies to improve their outcomes."
In a video interview, Dr. Evered and Dr. Brendan Silbert of St. Vincent’s Hospital, Melbourne, discuss the study and its implications.
Dr. Evered had no financial disclosures
On Twitter @alz_gal
COPENHAGEN – Almost half of patients with mild cognitive impairment progressed to dementia within 1 year of undergoing either arthroplasty or coronary angiography, according to a small Australian study.
Baseline cognitive impairment appeared to be the main driver of progression, increasing the risk more than sevenfold – significantly more than age or heart attack, Lisbeth Evered, Ph.D., said at the annual Alzheimer’s Association International Conference.
"After 12 months, 42% met the criteria for dementia," said Dr. Evered, a researcher at the University of Melbourne. "The expected annual progression from mild cognitive impairment [MCI] to dementia would be about 10%-12% per year."
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Her study included 67 patients with a mean age of 70 years. All had MCI at baseline, with a mean score of 23 on the Mini-Mental State Exam (MMSE). They underwent either arthroplasty (26 patients) or coronary angiography (41 patients).
A year after surgery, about 34% of the arthroplasty patients and 46% of the angiography patients had progressed to dementia. Baseline cognitive impairment was the only factor significantly associated with the change.
Postsurgical cognitive decline, both transient and long lasting, is a well-documented phenomenon, with studies going back to the late 1800s. Although the causative link isn’t entirely clear, anesthetics have long been implicated, said Dr. Evered. In animal models, some anesthesia drugs do seem to precipitate an Alzheimer’s-like amyloidosis and tau hyperphosphorylation.
More recent animal data suggest that inflammation might be a powerful influence.
"When a patient has surgery with a general anesthetic, they experience peripheral inflammation," Dr. Evered explained. "In a healthy normal brain, there’s plenty of cognitive reserve, and although there might be some cognitive decline afterward, the person won’t really notice and will certainly recover."
In a vulnerable brain, however, the inflammation may be amplified and may cause significant collateral damage that accelerates cognitive decline. "The problem is, we don’t know why they are vulnerable or what we might do about it," she noted.
The best approach now is to routinely assess cognition before surgery and monitor it afterward, Dr. Evered explained. "Then, the perioperative period is not something occurring in isolation," she noted. "We will be better able to identify those at risk and implement strategies to improve their outcomes."
In a video interview, Dr. Evered and Dr. Brendan Silbert of St. Vincent’s Hospital, Melbourne, discuss the study and its implications.
Dr. Evered had no financial disclosures
On Twitter @alz_gal
COPENHAGEN – Almost half of patients with mild cognitive impairment progressed to dementia within 1 year of undergoing either arthroplasty or coronary angiography, according to a small Australian study.
Baseline cognitive impairment appeared to be the main driver of progression, increasing the risk more than sevenfold – significantly more than age or heart attack, Lisbeth Evered, Ph.D., said at the annual Alzheimer’s Association International Conference.
"After 12 months, 42% met the criteria for dementia," said Dr. Evered, a researcher at the University of Melbourne. "The expected annual progression from mild cognitive impairment [MCI] to dementia would be about 10%-12% per year."
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Her study included 67 patients with a mean age of 70 years. All had MCI at baseline, with a mean score of 23 on the Mini-Mental State Exam (MMSE). They underwent either arthroplasty (26 patients) or coronary angiography (41 patients).
A year after surgery, about 34% of the arthroplasty patients and 46% of the angiography patients had progressed to dementia. Baseline cognitive impairment was the only factor significantly associated with the change.
Postsurgical cognitive decline, both transient and long lasting, is a well-documented phenomenon, with studies going back to the late 1800s. Although the causative link isn’t entirely clear, anesthetics have long been implicated, said Dr. Evered. In animal models, some anesthesia drugs do seem to precipitate an Alzheimer’s-like amyloidosis and tau hyperphosphorylation.
More recent animal data suggest that inflammation might be a powerful influence.
"When a patient has surgery with a general anesthetic, they experience peripheral inflammation," Dr. Evered explained. "In a healthy normal brain, there’s plenty of cognitive reserve, and although there might be some cognitive decline afterward, the person won’t really notice and will certainly recover."
In a vulnerable brain, however, the inflammation may be amplified and may cause significant collateral damage that accelerates cognitive decline. "The problem is, we don’t know why they are vulnerable or what we might do about it," she noted.
The best approach now is to routinely assess cognition before surgery and monitor it afterward, Dr. Evered explained. "Then, the perioperative period is not something occurring in isolation," she noted. "We will be better able to identify those at risk and implement strategies to improve their outcomes."
In a video interview, Dr. Evered and Dr. Brendan Silbert of St. Vincent’s Hospital, Melbourne, discuss the study and its implications.
Dr. Evered had no financial disclosures
On Twitter @alz_gal
AT AAIC 2014
Achieving aortic arch replacement without deep hypothermic circulatory arrest
NEW YORK – A novel technique for aortic arch repair, which avoids both circulatory arrest and profound hypothermia, was associated with low mortality and low cerebral morbidity in a group of 62 patients who underwent aortic arch replacement using this procedure.
Advantages of the "branch-first" procedure include visceral organ and cardiac protection and less need for blood/product transfusions, according to Dr. George Matalanis, who presented the findings at the meeting sponsored by the American Association for Thoracic Surgery.
The branch-first technique avoids many of the pitfalls associated with the widely used combination of antegrade perfusion and deep hypothermic circulatory arrest (DHTA). Such pitfalls include a higher incidence of cerebral injury than with proximal aortic surgery, as well as renal failure, ischemic hepatitis, and paraplegia, said Dr. Matalanis, a cardiothoracic surgeon at Austin Hospital, Kew, Australia. He noted that perfusion cannulas used for antegrade perfusion increase the risk of particulate and air emboli and branch injury or dissection, and their insertion extends cumulative cerebral circulatory arrest time.
DHTA also has a number of clinically significant disadvantages, such as prolongation of cardiopulmonary bypass times during cooling and rewarming, increased potential for cerebral ischemic reperfusion injury, and imposition of time constraints.
A feature of the branch-first technique is that it allows a complete and unhurried repair, allowing the surgeon to systematically interrogate each branch anastomosis, resulting in a low incidence of blood product use. By maintaining cardiac and distal body perfusion, even the most complex reconstructions can be carefully accomplished without concern about incomplete organ protection, allowing complete correction of pathology, according to Dr. Matalanis. The technique avoids the need for deep hypothermia, circulatory arrest, extended periods of cardiopulmonary bypass, and cerebral, cardiac and other organ circulatory exclusion.
Dr. Matalanis presented the results of a study involving 62 patients who underwent arch replacement using the branch-first procedure. The mean age was 65 years, and 60% were men. Almost 40% were urgent/emergent, and 32% had acute type A aortic dissection. One quarter had previous cardiac surgery. This work is an extension of an earlier study, which reported outcomes in 42 patients (Ann. Cardiothorac. Surg. 2013;2:194-201).
There were two deaths (3%), both in patients with acute type A aortic dissection with malperfusion. Neurological events occurred in 5%, with one permanent deficit. Six percent required renal support and 2% intra-aortic balloon support. One-quarter did not need red blood cell transfusion, and 15% did not require red blood cells or platelets/factors. Patients awakened as if they had undergone coronary artery bypass grafting (80% within 48 hours and 25% within 11 hours).
"This technique relies on two basic principles," explained Dr. Matalanis "The first is the extensive collateral network that exists between the three major arch branches, in addition to and far more expansive than the circle of Willis, allowing the brief interruption of one branch to be compensated by collateral flow from the other two. The second is the use of a modified trifurcation graft with a perfusion side arm to reconstruct the arch branches, allowing antegrade perfusion to resume as soon as each branch is reconstructed."
The procedure consists of establishing bypass using femoral inflow and moderate hypothermia (28° C), followed by serial disconnection and reconstruction of each arch branch, proceeding from the innominate to left subclavian, using a trifurcation arch graft with a perfusion side arm port. The proximal descending aorta is clamped, the distal arch anastomosis is constructed, and the aortic root reconstruction is completed. Finally, a connection is made between the common stem of the trifurcation graft and the ascending aorta graft.
There are no periods of global circulatory arrest, no interruption to cerebral perfusion during the anastomosis of the two grafts, and cardiac perfusion is maintained during the whole phase of arch branch reconstruction. Distal organ perfusion is also maintained throughout the procedure, says Dr. Matalanis.
Disadvantages of the branch-first technique include loss of the deep hypothermia "security blanket," the possibility of clamp injuries or air/thrombo-embolism, and difficulties with femoral cannulation. Issues may also arise with kinking or stenosis of the trifurcation graft and adhesions.
Dr. Matalanis reported having no relevant financial disclosures.
NEW YORK – A novel technique for aortic arch repair, which avoids both circulatory arrest and profound hypothermia, was associated with low mortality and low cerebral morbidity in a group of 62 patients who underwent aortic arch replacement using this procedure.
Advantages of the "branch-first" procedure include visceral organ and cardiac protection and less need for blood/product transfusions, according to Dr. George Matalanis, who presented the findings at the meeting sponsored by the American Association for Thoracic Surgery.
The branch-first technique avoids many of the pitfalls associated with the widely used combination of antegrade perfusion and deep hypothermic circulatory arrest (DHTA). Such pitfalls include a higher incidence of cerebral injury than with proximal aortic surgery, as well as renal failure, ischemic hepatitis, and paraplegia, said Dr. Matalanis, a cardiothoracic surgeon at Austin Hospital, Kew, Australia. He noted that perfusion cannulas used for antegrade perfusion increase the risk of particulate and air emboli and branch injury or dissection, and their insertion extends cumulative cerebral circulatory arrest time.
DHTA also has a number of clinically significant disadvantages, such as prolongation of cardiopulmonary bypass times during cooling and rewarming, increased potential for cerebral ischemic reperfusion injury, and imposition of time constraints.
A feature of the branch-first technique is that it allows a complete and unhurried repair, allowing the surgeon to systematically interrogate each branch anastomosis, resulting in a low incidence of blood product use. By maintaining cardiac and distal body perfusion, even the most complex reconstructions can be carefully accomplished without concern about incomplete organ protection, allowing complete correction of pathology, according to Dr. Matalanis. The technique avoids the need for deep hypothermia, circulatory arrest, extended periods of cardiopulmonary bypass, and cerebral, cardiac and other organ circulatory exclusion.
Dr. Matalanis presented the results of a study involving 62 patients who underwent arch replacement using the branch-first procedure. The mean age was 65 years, and 60% were men. Almost 40% were urgent/emergent, and 32% had acute type A aortic dissection. One quarter had previous cardiac surgery. This work is an extension of an earlier study, which reported outcomes in 42 patients (Ann. Cardiothorac. Surg. 2013;2:194-201).
There were two deaths (3%), both in patients with acute type A aortic dissection with malperfusion. Neurological events occurred in 5%, with one permanent deficit. Six percent required renal support and 2% intra-aortic balloon support. One-quarter did not need red blood cell transfusion, and 15% did not require red blood cells or platelets/factors. Patients awakened as if they had undergone coronary artery bypass grafting (80% within 48 hours and 25% within 11 hours).
"This technique relies on two basic principles," explained Dr. Matalanis "The first is the extensive collateral network that exists between the three major arch branches, in addition to and far more expansive than the circle of Willis, allowing the brief interruption of one branch to be compensated by collateral flow from the other two. The second is the use of a modified trifurcation graft with a perfusion side arm to reconstruct the arch branches, allowing antegrade perfusion to resume as soon as each branch is reconstructed."
The procedure consists of establishing bypass using femoral inflow and moderate hypothermia (28° C), followed by serial disconnection and reconstruction of each arch branch, proceeding from the innominate to left subclavian, using a trifurcation arch graft with a perfusion side arm port. The proximal descending aorta is clamped, the distal arch anastomosis is constructed, and the aortic root reconstruction is completed. Finally, a connection is made between the common stem of the trifurcation graft and the ascending aorta graft.
There are no periods of global circulatory arrest, no interruption to cerebral perfusion during the anastomosis of the two grafts, and cardiac perfusion is maintained during the whole phase of arch branch reconstruction. Distal organ perfusion is also maintained throughout the procedure, says Dr. Matalanis.
Disadvantages of the branch-first technique include loss of the deep hypothermia "security blanket," the possibility of clamp injuries or air/thrombo-embolism, and difficulties with femoral cannulation. Issues may also arise with kinking or stenosis of the trifurcation graft and adhesions.
Dr. Matalanis reported having no relevant financial disclosures.
NEW YORK – A novel technique for aortic arch repair, which avoids both circulatory arrest and profound hypothermia, was associated with low mortality and low cerebral morbidity in a group of 62 patients who underwent aortic arch replacement using this procedure.
Advantages of the "branch-first" procedure include visceral organ and cardiac protection and less need for blood/product transfusions, according to Dr. George Matalanis, who presented the findings at the meeting sponsored by the American Association for Thoracic Surgery.
The branch-first technique avoids many of the pitfalls associated with the widely used combination of antegrade perfusion and deep hypothermic circulatory arrest (DHTA). Such pitfalls include a higher incidence of cerebral injury than with proximal aortic surgery, as well as renal failure, ischemic hepatitis, and paraplegia, said Dr. Matalanis, a cardiothoracic surgeon at Austin Hospital, Kew, Australia. He noted that perfusion cannulas used for antegrade perfusion increase the risk of particulate and air emboli and branch injury or dissection, and their insertion extends cumulative cerebral circulatory arrest time.
DHTA also has a number of clinically significant disadvantages, such as prolongation of cardiopulmonary bypass times during cooling and rewarming, increased potential for cerebral ischemic reperfusion injury, and imposition of time constraints.
A feature of the branch-first technique is that it allows a complete and unhurried repair, allowing the surgeon to systematically interrogate each branch anastomosis, resulting in a low incidence of blood product use. By maintaining cardiac and distal body perfusion, even the most complex reconstructions can be carefully accomplished without concern about incomplete organ protection, allowing complete correction of pathology, according to Dr. Matalanis. The technique avoids the need for deep hypothermia, circulatory arrest, extended periods of cardiopulmonary bypass, and cerebral, cardiac and other organ circulatory exclusion.
Dr. Matalanis presented the results of a study involving 62 patients who underwent arch replacement using the branch-first procedure. The mean age was 65 years, and 60% were men. Almost 40% were urgent/emergent, and 32% had acute type A aortic dissection. One quarter had previous cardiac surgery. This work is an extension of an earlier study, which reported outcomes in 42 patients (Ann. Cardiothorac. Surg. 2013;2:194-201).
There were two deaths (3%), both in patients with acute type A aortic dissection with malperfusion. Neurological events occurred in 5%, with one permanent deficit. Six percent required renal support and 2% intra-aortic balloon support. One-quarter did not need red blood cell transfusion, and 15% did not require red blood cells or platelets/factors. Patients awakened as if they had undergone coronary artery bypass grafting (80% within 48 hours and 25% within 11 hours).
"This technique relies on two basic principles," explained Dr. Matalanis "The first is the extensive collateral network that exists between the three major arch branches, in addition to and far more expansive than the circle of Willis, allowing the brief interruption of one branch to be compensated by collateral flow from the other two. The second is the use of a modified trifurcation graft with a perfusion side arm to reconstruct the arch branches, allowing antegrade perfusion to resume as soon as each branch is reconstructed."
The procedure consists of establishing bypass using femoral inflow and moderate hypothermia (28° C), followed by serial disconnection and reconstruction of each arch branch, proceeding from the innominate to left subclavian, using a trifurcation arch graft with a perfusion side arm port. The proximal descending aorta is clamped, the distal arch anastomosis is constructed, and the aortic root reconstruction is completed. Finally, a connection is made between the common stem of the trifurcation graft and the ascending aorta graft.
There are no periods of global circulatory arrest, no interruption to cerebral perfusion during the anastomosis of the two grafts, and cardiac perfusion is maintained during the whole phase of arch branch reconstruction. Distal organ perfusion is also maintained throughout the procedure, says Dr. Matalanis.
Disadvantages of the branch-first technique include loss of the deep hypothermia "security blanket," the possibility of clamp injuries or air/thrombo-embolism, and difficulties with femoral cannulation. Issues may also arise with kinking or stenosis of the trifurcation graft and adhesions.
Dr. Matalanis reported having no relevant financial disclosures.
AT AATS AORTIC SYMPOSIUM 2014
Key clinical point: By maintaining cardiac and distal body perfusion, complex reconstructions can be accomplished without concern about organ protection, allowing complete correction of aortic pathology.
Major finding: A method that avoids deep hypothermic circulatory arrest was associated with low mortality (3.2%) and low cerebral morbidity (5%).
Data source: Cohort study of 62 patients.
Disclosures: Dr. Matalanis reported having no relevant financial disclosures.
Stentless aortic bioprosthesis: Good 1-year outcomes, ‘remarkable’ functional improvement
TORONTO – In a multicenter European study, 30-day mortality and 1-year mortality after implantation of the stentless Freedom Solo aortic bioprosthetic valve were 1.4% and 4.4%, respectively. Patients in the study experienced "remarkable" functional status improvement at 1 year, reported principal investigator Dr. Markus Thalmann at the annual meeting of the American Association for Thoracic Surgery.
"Our trial showed excellent results in terms of morbidity and mortality and low rates of valve-related adverse events in a 12-month follow-up period," said Dr. Thalmann during his late-breaking clinical trials presentation. "It also demonstrated good hemodynamics leading to a remarkable functional status improvement."
The Sorin Freedom Solo aortic bioprosthesis is made of two layers of bovine pericardium, with no synthetic material added. The valve is implanted with a single running suture line technique in a strict supra-annular position and has no contact with the native annulus. The bioprosthesis is not approved in the United States.
Dr. Thalmann, of Krankenhaus Hietzing, Vienna, noted the importance of performing a careful decalcification of the annulus during implantation. "You should do it as properly as you’d do it when implanting a stented valve, even if you don’t put your stitches through the annulus," he said.
In response to a question, he said that the trial was requested by the Food and Drug Administration to provide more information on the single-line suture technique used to implant the valve.
The researchers conducted a prospective, nonrandomized, multicenter trial at 18 clinical centers in eight European countries. All patients with an indication for prosthetic aortic valve replacement were included, except those with a preexisting valve prosthesis in the mitral, pulmonary, or tricuspid positions. Patients needing double or triple valve replacement were also excluded, as were those with active endocarditis and congenital bicuspid valves.
A total of 616 patients received the valve. Patients had a mean age of 74.5 years, 45.9% were female, and the mean logistic EuroSCORE was 10.1%. Concomitant cardiac procedures, including coronary artery bypass grafting, were performed in 43.2% of patients.
Early (30-day) mortality was 1.4%, rising to 4.4% at 1 year. Valve-related mortality at 30 days and 1 year was 0.3% and 1.1%, respectively.
Overall morbidity was low. At 30 days, 4.5% of patients required reintervention for bleeding, 0.3% for perivalvular leakage. No structural valve dysfunction or valve thrombosis was noted at 30 days, with one case of each seen at 1 year (0.2% and 0.2%).
Preoperatively, 49.3% of patients were in New York Heart Association class III or IV heart failure. At 1 year, 97.0% were in NYHA class I or II heart failure.
"We found good hemodynamics after 1 year," said Dr. Thalmann. The overall mean gradient was 7.2 mm Hg, and the effective orifice area was 1.5 cm2.
Patients will be followed for up to 5 years.
The Freedom Solo valve is currently being tested in an investigational device exemption (IDE) study in the United States. The Sorin Solo Smart valve, the evolution of the Freedom Solo valve, received a European CE mark approval in November 2013.
Dr. Thalmann is a consultant for the Sorin Group, which funded the study.
TORONTO – In a multicenter European study, 30-day mortality and 1-year mortality after implantation of the stentless Freedom Solo aortic bioprosthetic valve were 1.4% and 4.4%, respectively. Patients in the study experienced "remarkable" functional status improvement at 1 year, reported principal investigator Dr. Markus Thalmann at the annual meeting of the American Association for Thoracic Surgery.
"Our trial showed excellent results in terms of morbidity and mortality and low rates of valve-related adverse events in a 12-month follow-up period," said Dr. Thalmann during his late-breaking clinical trials presentation. "It also demonstrated good hemodynamics leading to a remarkable functional status improvement."
The Sorin Freedom Solo aortic bioprosthesis is made of two layers of bovine pericardium, with no synthetic material added. The valve is implanted with a single running suture line technique in a strict supra-annular position and has no contact with the native annulus. The bioprosthesis is not approved in the United States.
Dr. Thalmann, of Krankenhaus Hietzing, Vienna, noted the importance of performing a careful decalcification of the annulus during implantation. "You should do it as properly as you’d do it when implanting a stented valve, even if you don’t put your stitches through the annulus," he said.
In response to a question, he said that the trial was requested by the Food and Drug Administration to provide more information on the single-line suture technique used to implant the valve.
The researchers conducted a prospective, nonrandomized, multicenter trial at 18 clinical centers in eight European countries. All patients with an indication for prosthetic aortic valve replacement were included, except those with a preexisting valve prosthesis in the mitral, pulmonary, or tricuspid positions. Patients needing double or triple valve replacement were also excluded, as were those with active endocarditis and congenital bicuspid valves.
A total of 616 patients received the valve. Patients had a mean age of 74.5 years, 45.9% were female, and the mean logistic EuroSCORE was 10.1%. Concomitant cardiac procedures, including coronary artery bypass grafting, were performed in 43.2% of patients.
Early (30-day) mortality was 1.4%, rising to 4.4% at 1 year. Valve-related mortality at 30 days and 1 year was 0.3% and 1.1%, respectively.
Overall morbidity was low. At 30 days, 4.5% of patients required reintervention for bleeding, 0.3% for perivalvular leakage. No structural valve dysfunction or valve thrombosis was noted at 30 days, with one case of each seen at 1 year (0.2% and 0.2%).
Preoperatively, 49.3% of patients were in New York Heart Association class III or IV heart failure. At 1 year, 97.0% were in NYHA class I or II heart failure.
"We found good hemodynamics after 1 year," said Dr. Thalmann. The overall mean gradient was 7.2 mm Hg, and the effective orifice area was 1.5 cm2.
Patients will be followed for up to 5 years.
The Freedom Solo valve is currently being tested in an investigational device exemption (IDE) study in the United States. The Sorin Solo Smart valve, the evolution of the Freedom Solo valve, received a European CE mark approval in November 2013.
Dr. Thalmann is a consultant for the Sorin Group, which funded the study.
TORONTO – In a multicenter European study, 30-day mortality and 1-year mortality after implantation of the stentless Freedom Solo aortic bioprosthetic valve were 1.4% and 4.4%, respectively. Patients in the study experienced "remarkable" functional status improvement at 1 year, reported principal investigator Dr. Markus Thalmann at the annual meeting of the American Association for Thoracic Surgery.
"Our trial showed excellent results in terms of morbidity and mortality and low rates of valve-related adverse events in a 12-month follow-up period," said Dr. Thalmann during his late-breaking clinical trials presentation. "It also demonstrated good hemodynamics leading to a remarkable functional status improvement."
The Sorin Freedom Solo aortic bioprosthesis is made of two layers of bovine pericardium, with no synthetic material added. The valve is implanted with a single running suture line technique in a strict supra-annular position and has no contact with the native annulus. The bioprosthesis is not approved in the United States.
Dr. Thalmann, of Krankenhaus Hietzing, Vienna, noted the importance of performing a careful decalcification of the annulus during implantation. "You should do it as properly as you’d do it when implanting a stented valve, even if you don’t put your stitches through the annulus," he said.
In response to a question, he said that the trial was requested by the Food and Drug Administration to provide more information on the single-line suture technique used to implant the valve.
The researchers conducted a prospective, nonrandomized, multicenter trial at 18 clinical centers in eight European countries. All patients with an indication for prosthetic aortic valve replacement were included, except those with a preexisting valve prosthesis in the mitral, pulmonary, or tricuspid positions. Patients needing double or triple valve replacement were also excluded, as were those with active endocarditis and congenital bicuspid valves.
A total of 616 patients received the valve. Patients had a mean age of 74.5 years, 45.9% were female, and the mean logistic EuroSCORE was 10.1%. Concomitant cardiac procedures, including coronary artery bypass grafting, were performed in 43.2% of patients.
Early (30-day) mortality was 1.4%, rising to 4.4% at 1 year. Valve-related mortality at 30 days and 1 year was 0.3% and 1.1%, respectively.
Overall morbidity was low. At 30 days, 4.5% of patients required reintervention for bleeding, 0.3% for perivalvular leakage. No structural valve dysfunction or valve thrombosis was noted at 30 days, with one case of each seen at 1 year (0.2% and 0.2%).
Preoperatively, 49.3% of patients were in New York Heart Association class III or IV heart failure. At 1 year, 97.0% were in NYHA class I or II heart failure.
"We found good hemodynamics after 1 year," said Dr. Thalmann. The overall mean gradient was 7.2 mm Hg, and the effective orifice area was 1.5 cm2.
Patients will be followed for up to 5 years.
The Freedom Solo valve is currently being tested in an investigational device exemption (IDE) study in the United States. The Sorin Solo Smart valve, the evolution of the Freedom Solo valve, received a European CE mark approval in November 2013.
Dr. Thalmann is a consultant for the Sorin Group, which funded the study.
AT THE AATS ANNUAL MEETING
Key clinical point: The valve is implanted with a single suture line in a supra-annular position, with no contact with the native annulus.
Major finding: Thirty-day mortality and 1-year mortality after implantation of the stentless Freedom Solo bioprosthesis were 1.4% and 4.4%, respectively.
Data source: Nonrandomized, prospective study of 616 patients at 18 centers in eight European countries.
Disclosures: Dr. Thalmann is a consultant for the Sorin Group, which funded the study.
Transcatheter mitral valve redos work, except in highest-risk patients
TORONTO – Transcatheter mitral valve-in-valve/valve-in-ring implantation is an effective option in most patients with degenerative mitral valves after surgical intervention, according to Dr. Danny Dvir.
In the highest-risk patients (STS scores greater than 20%), however, mortality after this percutaneous technique approached 50% at 1 year, Dr. Dvir reported at the American Association for Thoracic Surgery annual meeting.
"Most of these procedures were clinically effective, with 1-year results that are comparable to native aortic valve transcatheter implantation," said Dr. Dvir of St. Paul’s Hospital, Vancouver, B.C.
"However, we saw safety and efficacy concerns that included relatively high in-hospital mortality, device malposition, sporadic cases with elevated LVOT [left ventricular outflow tract] gradient, and elevated postprocedural gradients in procedures performed inside small surgical valves."
Dr. Joseph E. Bavaria, professor of surgery and director of the thoracic aortic surgery program at the University of Pennsylvania Health System, Philadelphia, the scheduled discussant of the abstract, asked, referring to the STS score greater than 20% group: "Is this really a cohort C or futile situation, where [the intervention] is probably not better than medical management?"
Transcatheter VIV/VIR
The majority of prosthetic heart valves are tissue valves that tend to degenerate and eventually fail over time. Surgical replacement of these valves is associated with significant risks.
Transcatheter valve-in-valve/valve-in-ring (VIV/VIR) implantation within a failed bioprosthesis performed in the mitral position has been reported in only small case series, with the safety and efficacy of the technique being largely unknown. The Global Valve-in-Valve Registry, with 765 patients from 73 centers worldwide, was designed to track the efficacy and safety of this nonsurgical redo in either the aortic or mitral valve position. The registry included 190 patients from 23 centers who underwent percutaneous mitral valve procedures (VIV in 157 patients and VIR in 33).
The mechanism of failure was regurgitation in 37%, stenosis in 25%, and a combination of the two in 38%. Patients were a median of 9 years past their last cardiac surgery and were deemed at high risk, with a mean STS score of 14.4. The mean age was 73.6 years, and 65.2% were female. The median length of hospital stay was 8 days.
A SAPIEN or SAPIEN XT device was used in the majority of cases (93.7%), mostly deployed via transapical access (84.7%).
During the procedure, initial device malpositioning occurred in 5.3% of cases, with a second device implanted in 4.3%. Postimplantation valvuloplasty was utilized in 8%.
"We saw a high rate of malpositioning," Dr. Dvir said. "In some of the cases, this led to a decision to leave the malpositioned device in the left atrium and implant a second device."
The incidence of all-cause death at 30 days was 8.9%, with cardiovascular death seen in 6.8% and major stroke in 2.2%. Importantly, 85.8% of patients were in NYHA function class I or II at 30 days, Dr. Dvir said.
"We were very happy to see this," he commented. "If you survive the valve-in-valve or valve-in-ring procedure, you will most likely have a good functional class.
Overall, the Kaplan-Meier mortality rate was 22.3% at 1 year. When stratified according to STS score, however, mortality in the group of patients with an STS score greater than 20% was 45.6%, falling to 23.2% for an STS score of 10%-20% and 12.9% for an STS score less than 10%. Predictors of 1-year mortality included STS score and renal failure.
"In these patients with STS greater than 20%, there is really a big problem. We need to understand which patients should not undergo a procedure, and maybe should be treated with an alternative approach," Dr. Dvir said. He noted that 28% of cases in the registry were in this highest-risk category.
"An 8.9% mortality at 1 year is not so bad in a group with a mean STS score of 14.1," noted Dr. Bavaria. "[But] this is not really a benign procedure as the length of stay was over 8 days."
Surgical valve sizing gone wrong?
After the VIV/VIR procedure, the mean mitral valve area was 2.1 ± 0.7 cm2, with a mean residual gradient of 6.2 mm Hg. Significant mitral regurgitation was noted in 4.2% of patients, and a left ventricular outflow tract mean gradient greater than 20 mm Hg was noted in only 2.1% of cases.
"We saw a trend for elevated gradients especially when we were treating small valves with a valve-in-valve approach," Dr. Dvir said.
Indeed, in the patients with smaller surgical valve label size, one-third had postprocedural mean gradients greater than 10 mm Hg. The rates of mean gradient greater than 10 mm Hg dropped to 7.4% and 5.3% with progressively larger surgical valve label sizes.
"I am very worried about the cardiac surgery and interventional cardiology decision-making process, as over 60% of valve-in-ring cases were 26-mm and 28-mm rings and over 56% of valve-in-valve cases were less than or equal to 27-mm prosthetic valves," said Dr. Bavaria. "There will obviously be significant mitral gradients in these cases, as this study showed. Is this simply a lack of knowledge in the operators, should these small valve-in-valve cases be done, or is this a limit of this technology?"
"I think this issue of residual gradients will haunt valve in valve for many years to come," said Dr. Dvir. "However, we know from the aortic arena, that even if you have a high residual gradient, the results at 1 year are not different than the other groups. So, it doesn’t affect 1-year outcomes, although I predict that it will affect the durability of the device and the long-term outcome."
TORONTO – Transcatheter mitral valve-in-valve/valve-in-ring implantation is an effective option in most patients with degenerative mitral valves after surgical intervention, according to Dr. Danny Dvir.
In the highest-risk patients (STS scores greater than 20%), however, mortality after this percutaneous technique approached 50% at 1 year, Dr. Dvir reported at the American Association for Thoracic Surgery annual meeting.
"Most of these procedures were clinically effective, with 1-year results that are comparable to native aortic valve transcatheter implantation," said Dr. Dvir of St. Paul’s Hospital, Vancouver, B.C.
"However, we saw safety and efficacy concerns that included relatively high in-hospital mortality, device malposition, sporadic cases with elevated LVOT [left ventricular outflow tract] gradient, and elevated postprocedural gradients in procedures performed inside small surgical valves."
Dr. Joseph E. Bavaria, professor of surgery and director of the thoracic aortic surgery program at the University of Pennsylvania Health System, Philadelphia, the scheduled discussant of the abstract, asked, referring to the STS score greater than 20% group: "Is this really a cohort C or futile situation, where [the intervention] is probably not better than medical management?"
Transcatheter VIV/VIR
The majority of prosthetic heart valves are tissue valves that tend to degenerate and eventually fail over time. Surgical replacement of these valves is associated with significant risks.
Transcatheter valve-in-valve/valve-in-ring (VIV/VIR) implantation within a failed bioprosthesis performed in the mitral position has been reported in only small case series, with the safety and efficacy of the technique being largely unknown. The Global Valve-in-Valve Registry, with 765 patients from 73 centers worldwide, was designed to track the efficacy and safety of this nonsurgical redo in either the aortic or mitral valve position. The registry included 190 patients from 23 centers who underwent percutaneous mitral valve procedures (VIV in 157 patients and VIR in 33).
The mechanism of failure was regurgitation in 37%, stenosis in 25%, and a combination of the two in 38%. Patients were a median of 9 years past their last cardiac surgery and were deemed at high risk, with a mean STS score of 14.4. The mean age was 73.6 years, and 65.2% were female. The median length of hospital stay was 8 days.
A SAPIEN or SAPIEN XT device was used in the majority of cases (93.7%), mostly deployed via transapical access (84.7%).
During the procedure, initial device malpositioning occurred in 5.3% of cases, with a second device implanted in 4.3%. Postimplantation valvuloplasty was utilized in 8%.
"We saw a high rate of malpositioning," Dr. Dvir said. "In some of the cases, this led to a decision to leave the malpositioned device in the left atrium and implant a second device."
The incidence of all-cause death at 30 days was 8.9%, with cardiovascular death seen in 6.8% and major stroke in 2.2%. Importantly, 85.8% of patients were in NYHA function class I or II at 30 days, Dr. Dvir said.
"We were very happy to see this," he commented. "If you survive the valve-in-valve or valve-in-ring procedure, you will most likely have a good functional class.
Overall, the Kaplan-Meier mortality rate was 22.3% at 1 year. When stratified according to STS score, however, mortality in the group of patients with an STS score greater than 20% was 45.6%, falling to 23.2% for an STS score of 10%-20% and 12.9% for an STS score less than 10%. Predictors of 1-year mortality included STS score and renal failure.
"In these patients with STS greater than 20%, there is really a big problem. We need to understand which patients should not undergo a procedure, and maybe should be treated with an alternative approach," Dr. Dvir said. He noted that 28% of cases in the registry were in this highest-risk category.
"An 8.9% mortality at 1 year is not so bad in a group with a mean STS score of 14.1," noted Dr. Bavaria. "[But] this is not really a benign procedure as the length of stay was over 8 days."
Surgical valve sizing gone wrong?
After the VIV/VIR procedure, the mean mitral valve area was 2.1 ± 0.7 cm2, with a mean residual gradient of 6.2 mm Hg. Significant mitral regurgitation was noted in 4.2% of patients, and a left ventricular outflow tract mean gradient greater than 20 mm Hg was noted in only 2.1% of cases.
"We saw a trend for elevated gradients especially when we were treating small valves with a valve-in-valve approach," Dr. Dvir said.
Indeed, in the patients with smaller surgical valve label size, one-third had postprocedural mean gradients greater than 10 mm Hg. The rates of mean gradient greater than 10 mm Hg dropped to 7.4% and 5.3% with progressively larger surgical valve label sizes.
"I am very worried about the cardiac surgery and interventional cardiology decision-making process, as over 60% of valve-in-ring cases were 26-mm and 28-mm rings and over 56% of valve-in-valve cases were less than or equal to 27-mm prosthetic valves," said Dr. Bavaria. "There will obviously be significant mitral gradients in these cases, as this study showed. Is this simply a lack of knowledge in the operators, should these small valve-in-valve cases be done, or is this a limit of this technology?"
"I think this issue of residual gradients will haunt valve in valve for many years to come," said Dr. Dvir. "However, we know from the aortic arena, that even if you have a high residual gradient, the results at 1 year are not different than the other groups. So, it doesn’t affect 1-year outcomes, although I predict that it will affect the durability of the device and the long-term outcome."
TORONTO – Transcatheter mitral valve-in-valve/valve-in-ring implantation is an effective option in most patients with degenerative mitral valves after surgical intervention, according to Dr. Danny Dvir.
In the highest-risk patients (STS scores greater than 20%), however, mortality after this percutaneous technique approached 50% at 1 year, Dr. Dvir reported at the American Association for Thoracic Surgery annual meeting.
"Most of these procedures were clinically effective, with 1-year results that are comparable to native aortic valve transcatheter implantation," said Dr. Dvir of St. Paul’s Hospital, Vancouver, B.C.
"However, we saw safety and efficacy concerns that included relatively high in-hospital mortality, device malposition, sporadic cases with elevated LVOT [left ventricular outflow tract] gradient, and elevated postprocedural gradients in procedures performed inside small surgical valves."
Dr. Joseph E. Bavaria, professor of surgery and director of the thoracic aortic surgery program at the University of Pennsylvania Health System, Philadelphia, the scheduled discussant of the abstract, asked, referring to the STS score greater than 20% group: "Is this really a cohort C or futile situation, where [the intervention] is probably not better than medical management?"
Transcatheter VIV/VIR
The majority of prosthetic heart valves are tissue valves that tend to degenerate and eventually fail over time. Surgical replacement of these valves is associated with significant risks.
Transcatheter valve-in-valve/valve-in-ring (VIV/VIR) implantation within a failed bioprosthesis performed in the mitral position has been reported in only small case series, with the safety and efficacy of the technique being largely unknown. The Global Valve-in-Valve Registry, with 765 patients from 73 centers worldwide, was designed to track the efficacy and safety of this nonsurgical redo in either the aortic or mitral valve position. The registry included 190 patients from 23 centers who underwent percutaneous mitral valve procedures (VIV in 157 patients and VIR in 33).
The mechanism of failure was regurgitation in 37%, stenosis in 25%, and a combination of the two in 38%. Patients were a median of 9 years past their last cardiac surgery and were deemed at high risk, with a mean STS score of 14.4. The mean age was 73.6 years, and 65.2% were female. The median length of hospital stay was 8 days.
A SAPIEN or SAPIEN XT device was used in the majority of cases (93.7%), mostly deployed via transapical access (84.7%).
During the procedure, initial device malpositioning occurred in 5.3% of cases, with a second device implanted in 4.3%. Postimplantation valvuloplasty was utilized in 8%.
"We saw a high rate of malpositioning," Dr. Dvir said. "In some of the cases, this led to a decision to leave the malpositioned device in the left atrium and implant a second device."
The incidence of all-cause death at 30 days was 8.9%, with cardiovascular death seen in 6.8% and major stroke in 2.2%. Importantly, 85.8% of patients were in NYHA function class I or II at 30 days, Dr. Dvir said.
"We were very happy to see this," he commented. "If you survive the valve-in-valve or valve-in-ring procedure, you will most likely have a good functional class.
Overall, the Kaplan-Meier mortality rate was 22.3% at 1 year. When stratified according to STS score, however, mortality in the group of patients with an STS score greater than 20% was 45.6%, falling to 23.2% for an STS score of 10%-20% and 12.9% for an STS score less than 10%. Predictors of 1-year mortality included STS score and renal failure.
"In these patients with STS greater than 20%, there is really a big problem. We need to understand which patients should not undergo a procedure, and maybe should be treated with an alternative approach," Dr. Dvir said. He noted that 28% of cases in the registry were in this highest-risk category.
"An 8.9% mortality at 1 year is not so bad in a group with a mean STS score of 14.1," noted Dr. Bavaria. "[But] this is not really a benign procedure as the length of stay was over 8 days."
Surgical valve sizing gone wrong?
After the VIV/VIR procedure, the mean mitral valve area was 2.1 ± 0.7 cm2, with a mean residual gradient of 6.2 mm Hg. Significant mitral regurgitation was noted in 4.2% of patients, and a left ventricular outflow tract mean gradient greater than 20 mm Hg was noted in only 2.1% of cases.
"We saw a trend for elevated gradients especially when we were treating small valves with a valve-in-valve approach," Dr. Dvir said.
Indeed, in the patients with smaller surgical valve label size, one-third had postprocedural mean gradients greater than 10 mm Hg. The rates of mean gradient greater than 10 mm Hg dropped to 7.4% and 5.3% with progressively larger surgical valve label sizes.
"I am very worried about the cardiac surgery and interventional cardiology decision-making process, as over 60% of valve-in-ring cases were 26-mm and 28-mm rings and over 56% of valve-in-valve cases were less than or equal to 27-mm prosthetic valves," said Dr. Bavaria. "There will obviously be significant mitral gradients in these cases, as this study showed. Is this simply a lack of knowledge in the operators, should these small valve-in-valve cases be done, or is this a limit of this technology?"
"I think this issue of residual gradients will haunt valve in valve for many years to come," said Dr. Dvir. "However, we know from the aortic arena, that even if you have a high residual gradient, the results at 1 year are not different than the other groups. So, it doesn’t affect 1-year outcomes, although I predict that it will affect the durability of the device and the long-term outcome."
AT THE AATS ANNUAL MEETING
Key clinical point: High-risk patients should avoid transcatheter mitral valve-in-valve implantation.
Major finding: Outcomes after mitral valve-in-valve/valve-in-ring implantations were acceptable, with 1-year mortality similar to that with transcather aortic valve implantation, except in patients with an STS score greater than 20%, where 1-year mortality was 45.6%.
Data source: The Global Valve-in-Valve Registry, 765 patients from 73 centers worldwide, of which 190 from 23 centers had mitral valve redo procedures.
Disclosures: Dr. Dvir reported having no financial disclosures.
TEVAR slows progression of type B uncomplicated aortic dissection
NEW YORK – Five-year results from the INSTEAD trial showed that patients with stable type B aortic dissections who were randomized to receive thoracic endovascular aneurysm repair plus optimal medical treatment showed significantly less aorta-specific mortality and delayed disease progression than did those who received OMT alone, according to Rachel Clough Ph.D., MRCS, who presented the findings at Aortic Symposium 2014, a meeting sponsored by the American Association for Thoracic Surgery.
The results indicate that delayed adverse events, such as sudden fatalities, expansion of the false lumen, rupture, and other late complications that occur in patients treated medically in the years subsequent to dissection are prevented or attenuated in those who receive stent grafts.
"Uncomplicated patients with type B aortic dissection have traditionally been treated with antihypertensive medication but what we see is, even in patients with very good blood pressure control, there is a continued attrition rate looking out toward 5 years. In some series, more than 50% of patients are dead [at that time point]," said Dr. Clough of Guy’s and St. Thomas NHS Foundation Trust and King’s College London (England).
INSTEAD (Investigation of Stent Grafts in Aortic Dissection) is the first randomized trial comparing thoracic endovascular aneurysm repair (TEVAR) with a stent graft. When 2-year results were published in 2009 (Circulation 2009;120:2519-28), there was criticism that the study was underpowered as no differences were seen in all-cause deaths, aorta-related deaths due to aortic rupture, or dissection progression plus rupture. There was even a trend toward better cumulative survival in the OMT group.
Sixty-eight patients were randomized to receive OMT and 72 patients received TEVAR + OMT. Eighty-three percent had one stent placed, 11% had two stents, and 6% had three stents. The proximal thoracic aorta was covered in all cases, and the range of coverage was 15-35 cm. No significant differences between groups were found in the comorbidity profile, presence of risk factors, or dissection morphology. There were two periprocedural deaths (one retrograde type A dissection and one rupture of the iliac vessels) and a "reasonably low" incidence of neurologic events, according to Dr. Clough.
By following the patients for 5 years, differences in outcomes between patients who had undergone TEVAR plus OMT and those who only received OMT began to emerge. Analysis of this long-term data shows that patients with stable type B aortic dissections who were randomized to receive TEVAR plus OMT showed less aorta-specific mortality (7 vs 19%, P = .04) and delayed disease progression (27% vs 46%, P = .04) than did those who received OMT alone. Landmark analysis suggested a benefit of TEVAR for all endpoints between 2 and 5 years, including all-cause mortality (0 vs 17%, P = .0003).
Both improved survival and less progression of disease over 5 years after elective TEVAR were associated with stent graft–induced false lumen thrombosis in 91% of cases (P less than .0001). Placement of the stent graft resulted in a significant reduction in false lumen diameter (P less than .0001) and significant increase in true lumen diameter (P less than .001). In contrast, a significant increase in aortic diameter was noted in those who received only OMT (P less than .0001).
"In conclusion, endovascular therapy in addition to medical therapy is associated with improved 5-year aortic specific survival and delayed disease progression. In uncomplicated type B dissection with suitable anatomy, preemptive TEVAR should be considered to improve late outcomes," said Dr. Clough.
Dr. Clough had nothing to disclose. INSTEAD was sponsored by the Medtronic Bakken Research Center. Medtronic manufactures the Medtronic Talent Stent-Graft-System used as the endograft.
NEW YORK – Five-year results from the INSTEAD trial showed that patients with stable type B aortic dissections who were randomized to receive thoracic endovascular aneurysm repair plus optimal medical treatment showed significantly less aorta-specific mortality and delayed disease progression than did those who received OMT alone, according to Rachel Clough Ph.D., MRCS, who presented the findings at Aortic Symposium 2014, a meeting sponsored by the American Association for Thoracic Surgery.
The results indicate that delayed adverse events, such as sudden fatalities, expansion of the false lumen, rupture, and other late complications that occur in patients treated medically in the years subsequent to dissection are prevented or attenuated in those who receive stent grafts.
"Uncomplicated patients with type B aortic dissection have traditionally been treated with antihypertensive medication but what we see is, even in patients with very good blood pressure control, there is a continued attrition rate looking out toward 5 years. In some series, more than 50% of patients are dead [at that time point]," said Dr. Clough of Guy’s and St. Thomas NHS Foundation Trust and King’s College London (England).
INSTEAD (Investigation of Stent Grafts in Aortic Dissection) is the first randomized trial comparing thoracic endovascular aneurysm repair (TEVAR) with a stent graft. When 2-year results were published in 2009 (Circulation 2009;120:2519-28), there was criticism that the study was underpowered as no differences were seen in all-cause deaths, aorta-related deaths due to aortic rupture, or dissection progression plus rupture. There was even a trend toward better cumulative survival in the OMT group.
Sixty-eight patients were randomized to receive OMT and 72 patients received TEVAR + OMT. Eighty-three percent had one stent placed, 11% had two stents, and 6% had three stents. The proximal thoracic aorta was covered in all cases, and the range of coverage was 15-35 cm. No significant differences between groups were found in the comorbidity profile, presence of risk factors, or dissection morphology. There were two periprocedural deaths (one retrograde type A dissection and one rupture of the iliac vessels) and a "reasonably low" incidence of neurologic events, according to Dr. Clough.
By following the patients for 5 years, differences in outcomes between patients who had undergone TEVAR plus OMT and those who only received OMT began to emerge. Analysis of this long-term data shows that patients with stable type B aortic dissections who were randomized to receive TEVAR plus OMT showed less aorta-specific mortality (7 vs 19%, P = .04) and delayed disease progression (27% vs 46%, P = .04) than did those who received OMT alone. Landmark analysis suggested a benefit of TEVAR for all endpoints between 2 and 5 years, including all-cause mortality (0 vs 17%, P = .0003).
Both improved survival and less progression of disease over 5 years after elective TEVAR were associated with stent graft–induced false lumen thrombosis in 91% of cases (P less than .0001). Placement of the stent graft resulted in a significant reduction in false lumen diameter (P less than .0001) and significant increase in true lumen diameter (P less than .001). In contrast, a significant increase in aortic diameter was noted in those who received only OMT (P less than .0001).
"In conclusion, endovascular therapy in addition to medical therapy is associated with improved 5-year aortic specific survival and delayed disease progression. In uncomplicated type B dissection with suitable anatomy, preemptive TEVAR should be considered to improve late outcomes," said Dr. Clough.
Dr. Clough had nothing to disclose. INSTEAD was sponsored by the Medtronic Bakken Research Center. Medtronic manufactures the Medtronic Talent Stent-Graft-System used as the endograft.
NEW YORK – Five-year results from the INSTEAD trial showed that patients with stable type B aortic dissections who were randomized to receive thoracic endovascular aneurysm repair plus optimal medical treatment showed significantly less aorta-specific mortality and delayed disease progression than did those who received OMT alone, according to Rachel Clough Ph.D., MRCS, who presented the findings at Aortic Symposium 2014, a meeting sponsored by the American Association for Thoracic Surgery.
The results indicate that delayed adverse events, such as sudden fatalities, expansion of the false lumen, rupture, and other late complications that occur in patients treated medically in the years subsequent to dissection are prevented or attenuated in those who receive stent grafts.
"Uncomplicated patients with type B aortic dissection have traditionally been treated with antihypertensive medication but what we see is, even in patients with very good blood pressure control, there is a continued attrition rate looking out toward 5 years. In some series, more than 50% of patients are dead [at that time point]," said Dr. Clough of Guy’s and St. Thomas NHS Foundation Trust and King’s College London (England).
INSTEAD (Investigation of Stent Grafts in Aortic Dissection) is the first randomized trial comparing thoracic endovascular aneurysm repair (TEVAR) with a stent graft. When 2-year results were published in 2009 (Circulation 2009;120:2519-28), there was criticism that the study was underpowered as no differences were seen in all-cause deaths, aorta-related deaths due to aortic rupture, or dissection progression plus rupture. There was even a trend toward better cumulative survival in the OMT group.
Sixty-eight patients were randomized to receive OMT and 72 patients received TEVAR + OMT. Eighty-three percent had one stent placed, 11% had two stents, and 6% had three stents. The proximal thoracic aorta was covered in all cases, and the range of coverage was 15-35 cm. No significant differences between groups were found in the comorbidity profile, presence of risk factors, or dissection morphology. There were two periprocedural deaths (one retrograde type A dissection and one rupture of the iliac vessels) and a "reasonably low" incidence of neurologic events, according to Dr. Clough.
By following the patients for 5 years, differences in outcomes between patients who had undergone TEVAR plus OMT and those who only received OMT began to emerge. Analysis of this long-term data shows that patients with stable type B aortic dissections who were randomized to receive TEVAR plus OMT showed less aorta-specific mortality (7 vs 19%, P = .04) and delayed disease progression (27% vs 46%, P = .04) than did those who received OMT alone. Landmark analysis suggested a benefit of TEVAR for all endpoints between 2 and 5 years, including all-cause mortality (0 vs 17%, P = .0003).
Both improved survival and less progression of disease over 5 years after elective TEVAR were associated with stent graft–induced false lumen thrombosis in 91% of cases (P less than .0001). Placement of the stent graft resulted in a significant reduction in false lumen diameter (P less than .0001) and significant increase in true lumen diameter (P less than .001). In contrast, a significant increase in aortic diameter was noted in those who received only OMT (P less than .0001).
"In conclusion, endovascular therapy in addition to medical therapy is associated with improved 5-year aortic specific survival and delayed disease progression. In uncomplicated type B dissection with suitable anatomy, preemptive TEVAR should be considered to improve late outcomes," said Dr. Clough.
Dr. Clough had nothing to disclose. INSTEAD was sponsored by the Medtronic Bakken Research Center. Medtronic manufactures the Medtronic Talent Stent-Graft-System used as the endograft.
Major finding: Patients with stable type B aortic dissections who were randomized to receive TEVAR plus optimal medical treatment (OMT) showed significantly less aorta-specific mortality and delayed disease progression than did those who received OMT alone.
Data source: The study assessed the 5-year results of the INSTEAD trial of 68 patients randomized to receive OMT and 72 patients received TEVAR plus OMT
Disclosures: Dr. Clough had nothing to disclose. INSTEAD was sponsored by the Medtronic Bakken Research Center. Medtronic manufactures the Medtronic Talent Stent-Graft-System used as the endograft.
Thrombolysis may offer benefit in stable pulmonary embolism
Thrombolytic therapy decreased all-cause mortality in patients with hemodynamically stable pulmonary embolism associated with right ventricular dysfunction – those at "intermediate risk," according to a meta-analysis published online June 17 in JAMA.
The investigators described their study of 16 randomized, controlled clinical trials involving 2,115 patients as "the first analysis of thrombolysis in PE that has sufficient statistical power to detect associations with a meaningful mortality reduction." If their findings are confirmed in future randomized clinical trials, "there may be a shift in the treatment of selected patients with intermediate-risk PE using thrombolytics."
However, "the optimism regarding this clinical advantage must be tempered by [our] finding of significantly increased risk of major bleeding and intracranial hemorrhage associated with thrombolytic therapy, particularly for patients older than 65 years," said Dr. Saurav Chatterjee of the division of cardiology, St. Luke’s-Roosevelt Hospital Center of the Mount Sinai Health System, New York, and his associates (JAMA 2014;311:2414-21).
The study population included 1,499 patients who had hemodynamically stable PE associated with right ventricular dysfunction, the largest subset of patients seen in clinical practice and the group for whom the risks and benefits of thrombolysis are the most unclear.
After a mean follow-up of 82 days, overall mortality was 2.17% in patients who received thrombolysis, compared with 3.89% in those who received anticoagulation. In addition, the risk of recurrent PE was significantly lower with thrombolytic therapy (1.17%) than with anticoagulation (3.04%).
However, the rate of major bleeding was 9.24% for thrombolytic therapy, compared with 3.42% for anticoagulation. And the rate of intracranial hemorrhage was 1.46% for thrombolysis, compared with 0.19% for anticoagulation, the investigators said.
The bleeding risk was especially high in patients aged 65 years and older. Attenuation of this risk in younger patients suggests that they may be considered stronger candidates for thrombolytic therapy, Dr. Chatterjee and his associates said.
Dr. Chatterjee reported no financial conflicts; his associates reported ties to AstraZeneca, Boston Scientific, Cardiostem, Cordis, EKOS Corporation, Embolitech, GenWay, Johnson & Johnson, Soteria, and Vascular Magnetics.

|
|
Dr. Chatterjee and his associates calculated the net clinical benefit of thrombolysis, and their result "suggests evidence of modest efficacy in intermediate-risk PE," said Dr. Joshua A. Beckman.
But their findings do not yet add up to a change in the standard of care. Each clinician must decide on an individualized basis which of these patients should receive thrombolytic therapy, based on clinical presentation, comorbid conditions, and both the physician’s and the patient’s tolerance of risk.
Dr. Beckman is in the cardiovascular division at Brigham and Women’s Hospital, Boston. He reported being a board member for Vascular Interventional Advances; receiving grant funding from Bristol-Myers Squibb; and consulting for AstraZeneca, Boston Scientific, Ferring, Merck, and Novartis. These remarks were taken from his editorial accompanying Dr. Chatterjee’s report (JAMA 2014;311:2385-6).

|
|
Dr. Chatterjee and his associates calculated the net clinical benefit of thrombolysis, and their result "suggests evidence of modest efficacy in intermediate-risk PE," said Dr. Joshua A. Beckman.
But their findings do not yet add up to a change in the standard of care. Each clinician must decide on an individualized basis which of these patients should receive thrombolytic therapy, based on clinical presentation, comorbid conditions, and both the physician’s and the patient’s tolerance of risk.
Dr. Beckman is in the cardiovascular division at Brigham and Women’s Hospital, Boston. He reported being a board member for Vascular Interventional Advances; receiving grant funding from Bristol-Myers Squibb; and consulting for AstraZeneca, Boston Scientific, Ferring, Merck, and Novartis. These remarks were taken from his editorial accompanying Dr. Chatterjee’s report (JAMA 2014;311:2385-6).

|
|
Dr. Chatterjee and his associates calculated the net clinical benefit of thrombolysis, and their result "suggests evidence of modest efficacy in intermediate-risk PE," said Dr. Joshua A. Beckman.
But their findings do not yet add up to a change in the standard of care. Each clinician must decide on an individualized basis which of these patients should receive thrombolytic therapy, based on clinical presentation, comorbid conditions, and both the physician’s and the patient’s tolerance of risk.
Dr. Beckman is in the cardiovascular division at Brigham and Women’s Hospital, Boston. He reported being a board member for Vascular Interventional Advances; receiving grant funding from Bristol-Myers Squibb; and consulting for AstraZeneca, Boston Scientific, Ferring, Merck, and Novartis. These remarks were taken from his editorial accompanying Dr. Chatterjee’s report (JAMA 2014;311:2385-6).
Thrombolytic therapy decreased all-cause mortality in patients with hemodynamically stable pulmonary embolism associated with right ventricular dysfunction – those at "intermediate risk," according to a meta-analysis published online June 17 in JAMA.
The investigators described their study of 16 randomized, controlled clinical trials involving 2,115 patients as "the first analysis of thrombolysis in PE that has sufficient statistical power to detect associations with a meaningful mortality reduction." If their findings are confirmed in future randomized clinical trials, "there may be a shift in the treatment of selected patients with intermediate-risk PE using thrombolytics."
However, "the optimism regarding this clinical advantage must be tempered by [our] finding of significantly increased risk of major bleeding and intracranial hemorrhage associated with thrombolytic therapy, particularly for patients older than 65 years," said Dr. Saurav Chatterjee of the division of cardiology, St. Luke’s-Roosevelt Hospital Center of the Mount Sinai Health System, New York, and his associates (JAMA 2014;311:2414-21).
The study population included 1,499 patients who had hemodynamically stable PE associated with right ventricular dysfunction, the largest subset of patients seen in clinical practice and the group for whom the risks and benefits of thrombolysis are the most unclear.
After a mean follow-up of 82 days, overall mortality was 2.17% in patients who received thrombolysis, compared with 3.89% in those who received anticoagulation. In addition, the risk of recurrent PE was significantly lower with thrombolytic therapy (1.17%) than with anticoagulation (3.04%).
However, the rate of major bleeding was 9.24% for thrombolytic therapy, compared with 3.42% for anticoagulation. And the rate of intracranial hemorrhage was 1.46% for thrombolysis, compared with 0.19% for anticoagulation, the investigators said.
The bleeding risk was especially high in patients aged 65 years and older. Attenuation of this risk in younger patients suggests that they may be considered stronger candidates for thrombolytic therapy, Dr. Chatterjee and his associates said.
Dr. Chatterjee reported no financial conflicts; his associates reported ties to AstraZeneca, Boston Scientific, Cardiostem, Cordis, EKOS Corporation, Embolitech, GenWay, Johnson & Johnson, Soteria, and Vascular Magnetics.
Thrombolytic therapy decreased all-cause mortality in patients with hemodynamically stable pulmonary embolism associated with right ventricular dysfunction – those at "intermediate risk," according to a meta-analysis published online June 17 in JAMA.
The investigators described their study of 16 randomized, controlled clinical trials involving 2,115 patients as "the first analysis of thrombolysis in PE that has sufficient statistical power to detect associations with a meaningful mortality reduction." If their findings are confirmed in future randomized clinical trials, "there may be a shift in the treatment of selected patients with intermediate-risk PE using thrombolytics."
However, "the optimism regarding this clinical advantage must be tempered by [our] finding of significantly increased risk of major bleeding and intracranial hemorrhage associated with thrombolytic therapy, particularly for patients older than 65 years," said Dr. Saurav Chatterjee of the division of cardiology, St. Luke’s-Roosevelt Hospital Center of the Mount Sinai Health System, New York, and his associates (JAMA 2014;311:2414-21).
The study population included 1,499 patients who had hemodynamically stable PE associated with right ventricular dysfunction, the largest subset of patients seen in clinical practice and the group for whom the risks and benefits of thrombolysis are the most unclear.
After a mean follow-up of 82 days, overall mortality was 2.17% in patients who received thrombolysis, compared with 3.89% in those who received anticoagulation. In addition, the risk of recurrent PE was significantly lower with thrombolytic therapy (1.17%) than with anticoagulation (3.04%).
However, the rate of major bleeding was 9.24% for thrombolytic therapy, compared with 3.42% for anticoagulation. And the rate of intracranial hemorrhage was 1.46% for thrombolysis, compared with 0.19% for anticoagulation, the investigators said.
The bleeding risk was especially high in patients aged 65 years and older. Attenuation of this risk in younger patients suggests that they may be considered stronger candidates for thrombolytic therapy, Dr. Chatterjee and his associates said.
Dr. Chatterjee reported no financial conflicts; his associates reported ties to AstraZeneca, Boston Scientific, Cardiostem, Cordis, EKOS Corporation, Embolitech, GenWay, Johnson & Johnson, Soteria, and Vascular Magnetics.
FROM JAMA
Key clinical point: Thrombolysis may be a therapeutic alternative to anticoagulation in some patients with stable, intermediate-risk pulmonary embolism.
Major finding: Mortality was 2.17% in PE patients who received thrombolysis, compared with 3.89% in those who received anticoagulation; the risk of recurrent PE also was significantly lower with thrombolytic therapy (1.17%) than with anticoagulation (3.04%).
Data source: A meta-analysis of 16 randomized, controlled trials involving 2,115 patients with PE, including 1,499 with intermediate-risk PE, who were followed for a mean of 82 days.
Disclosures: Dr. Chatterjee reported no financial conflicts; his associates reported ties to AstraZeneca, Boston Scientific, Cardiostem, Cordis, EKOS Corporation, Embolitech, GenWay, Johnson & Johnson, Soteria, and Vascular Magnetics.
VIDEO: Statins flop in COPD, but hope remains
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN DIEGO – Two randomized, controlled trials presented at the American Thoracic Society international conference reported that statins did not improve pulmonary function or reduce exacerbations in patients with chronic obstructive pulmonary disease. But not everyone has given up on statins.
When a drug that showed promise in large observational studies doesn’t pan out in randomized, controlled trials, physicians start looking for subgroups of patients that still might benefit, Dr. Nicholas Gross told us. Hear his perspective on the STATCOPE trial (in which simvastatin did not prevent exacerbations in moderate to severe COPD) and the RODEO trial (in which rosuvastatin improved endothelial function only in a subset of patients with evidence of systemic inflammation.)
Dr. Gross is an emeritus professor of medicine and molecular biochemistry at Stritch-Loyola University, Chicago. He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT ATS 2014
Patient outcomes not affected by attendings running ‘simultaneous’ ORs
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
TORONTO – In academic medical centers, attending cardiothoracic surgeons often perform simultaneous procedures in different operating rooms as a means of increasing training opportunities for surgical fellows and to decrease hospital costs.
However, the practice of running simultaneous operating rooms did not appear to affect perioperative timing or negatively affect patient outcomes, according to the results of a single-institution review presented by Dr. Kenan W. Yount at the annual meeting of the American Association for Thoracic Surgery.
He and his colleagues at the University of Virginia, Charlottesville, wanted to examine their own data in guiding hospital policy as several major centers have recently proposed implementing a 1:1 ratio of attending surgeon to operating room.
In his presentation, Dr. Yount discussed the results of their review, which categorized 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations. "Our institution adheres to a strict policy of attending surgeon oversight of and involvement in the critical and key portions of all operations," said Dr. Yount.
They compared operative duration, starting and closing times, postoperative complications, and 30-day mortality in each category. They also compared rates of postoperative complications, hospital length of stay, and operative mortality in each category.
Interestingly, timing effects varied between the two overall types of surgery. Running two rooms had no effect on room start times, but thoracic rooms finished 16 minutes later than scheduled. Across six surgeons and 15 types of surgery, however, there were no differences in operative times.
"Furthermore, running two rooms was not associated with any differences in operative duration, morbidity, or mortality in our multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category," Dr. Yount said.
"In academic cardiothoracic surgical centers that rely on surgical support from fellowship training, the practice of running simultaneous operating rooms can be efficient and does not appear to negatively impact patient outcomes," said Dr. Yount. "In addition, the practice did not significantly increase operative duration or dramatically impact operating room starting or closing times," he concluded.
In discussing the implications of these results, he said, "Obviously, there are caveats: Attendings must be intimately involved in operations and scrubbed for every key and critical portion of the operation; also, operations being scheduled in separate rooms must be done so with reasonable foresight." As long as institutions are following these practices, he concluded, "it would appear that lens of current policy efforts is too narrow by focusing on perception. The debate should be refocused by challenging training programs to strengthen attending involvement and ensure the requisite competence of their trainees."
Dr. Yount reported no relevant disclosures.
AT THE AATS ANNUAL MEETING
Major finding: Running two rooms was not associated with any differences in operative duration, morbidity, or mortality in multivariate regression analyses, and there were no statistically significant differences in observed outcomes in any category.
Data source: The study reviewed 1,377 cardiac and 1,682 general thoracic operations performed from July 2011 to July 2013 by attending, case type, and whether the attending was simultaneously supervising two operations.
Disclosures: Dr. Yount had no disclosures.
System overhaul eliminated CABG surgical site infections
ORLANDO – A system-wide quality improvement process that utilized define, measure, analyze, improve, and control and rapid adoption methodology eliminated surgical site infections among patients undergoing isolated coronary artery bypass with donor site surgery at a regional medical center.
Between March 2012 and March 2013 the overall decline in the rate of surgical site infections among 250 patients surpassed the center’s goal of a 40% decrease in the infection rate to a rate of 1.61; instead, the center achieved a rate of 0.7 during that time period. Since May, 2012, no surgical site infections have occurred among coronary artery bypass graft patients, Candis Kles, a critical care nurse at Athens (Ga.) Regional Medical Center, reported at the annual meeting of the Society of Thoracic Surgeons.
"We are now into our 23rd month without a deep/organ space infection with over 454 patients," Ms. Kles said in a May interview.
The quality improvement process was initiated after the infection rates at the center were found to be high (ranging up to 6.1), compared with National Healthcare Safety Network data. Using the define, measure, analyze, improve, and control methodology, a multidisciplinary team was convened, including cardiothoracic surgeons, nurses, and support personnel, and a 6-month process was undertaken to identify areas for improvement, said Ms. Kles who chaired the team.
"We also at this time partnered with the VHA National Hospital Engagement Network for some extra training and to help us along the process," she noted.
The team flow-charted processes – from scheduled surgery to discharge – and posted the flow charts in the operating room and cardiac intensive care unit to identify inconsistencies and potential problem areas. Frontline staff members were engaged and encouraged to participate in the improvement process by posting notes, suggestions, and questions on the flow charts.
A literature review was conducted to ensure that current practices mirrored best practices.
Despite an extensive evaluation of possible patient-, procedure-, and hospital-related factors that might be associated with the infection rate, no single cause of the high rate was identified, although a number of areas for improvement were recognized. Among the changes that were implemented were use of chlorhexidine oral rinse, which was administered until discharge; use of disposable EKG leads (after high bacterial counts were found on the leads in use prior to program initiation); use of silver-impregnated midsternal dressings; a change in surgical and suture techniques; development of patient educational materials, and standardization of all processes, Ms. Kles said, noting that the changes were implemented rapidly.
The success of the program is largely attributable to input from all levels and disciplines within the organization – including physicians who championed the process, and to staff engagement and buy in, she said.
The improvement in the infection rate resulted in cost avoidance of $212,355 (compared with a total excess cost of surgical site infections of $250,965 in 2011), and in a reduction from 156 to 24 excess hospital days.
Ms. Kles reported that as of February 2014 she is a member of the speakers bureau for Mölnlycke Health Care, a maker of surgical and wound care products.
ORLANDO – A system-wide quality improvement process that utilized define, measure, analyze, improve, and control and rapid adoption methodology eliminated surgical site infections among patients undergoing isolated coronary artery bypass with donor site surgery at a regional medical center.
Between March 2012 and March 2013 the overall decline in the rate of surgical site infections among 250 patients surpassed the center’s goal of a 40% decrease in the infection rate to a rate of 1.61; instead, the center achieved a rate of 0.7 during that time period. Since May, 2012, no surgical site infections have occurred among coronary artery bypass graft patients, Candis Kles, a critical care nurse at Athens (Ga.) Regional Medical Center, reported at the annual meeting of the Society of Thoracic Surgeons.
"We are now into our 23rd month without a deep/organ space infection with over 454 patients," Ms. Kles said in a May interview.
The quality improvement process was initiated after the infection rates at the center were found to be high (ranging up to 6.1), compared with National Healthcare Safety Network data. Using the define, measure, analyze, improve, and control methodology, a multidisciplinary team was convened, including cardiothoracic surgeons, nurses, and support personnel, and a 6-month process was undertaken to identify areas for improvement, said Ms. Kles who chaired the team.
"We also at this time partnered with the VHA National Hospital Engagement Network for some extra training and to help us along the process," she noted.
The team flow-charted processes – from scheduled surgery to discharge – and posted the flow charts in the operating room and cardiac intensive care unit to identify inconsistencies and potential problem areas. Frontline staff members were engaged and encouraged to participate in the improvement process by posting notes, suggestions, and questions on the flow charts.
A literature review was conducted to ensure that current practices mirrored best practices.
Despite an extensive evaluation of possible patient-, procedure-, and hospital-related factors that might be associated with the infection rate, no single cause of the high rate was identified, although a number of areas for improvement were recognized. Among the changes that were implemented were use of chlorhexidine oral rinse, which was administered until discharge; use of disposable EKG leads (after high bacterial counts were found on the leads in use prior to program initiation); use of silver-impregnated midsternal dressings; a change in surgical and suture techniques; development of patient educational materials, and standardization of all processes, Ms. Kles said, noting that the changes were implemented rapidly.
The success of the program is largely attributable to input from all levels and disciplines within the organization – including physicians who championed the process, and to staff engagement and buy in, she said.
The improvement in the infection rate resulted in cost avoidance of $212,355 (compared with a total excess cost of surgical site infections of $250,965 in 2011), and in a reduction from 156 to 24 excess hospital days.
Ms. Kles reported that as of February 2014 she is a member of the speakers bureau for Mölnlycke Health Care, a maker of surgical and wound care products.
ORLANDO – A system-wide quality improvement process that utilized define, measure, analyze, improve, and control and rapid adoption methodology eliminated surgical site infections among patients undergoing isolated coronary artery bypass with donor site surgery at a regional medical center.
Between March 2012 and March 2013 the overall decline in the rate of surgical site infections among 250 patients surpassed the center’s goal of a 40% decrease in the infection rate to a rate of 1.61; instead, the center achieved a rate of 0.7 during that time period. Since May, 2012, no surgical site infections have occurred among coronary artery bypass graft patients, Candis Kles, a critical care nurse at Athens (Ga.) Regional Medical Center, reported at the annual meeting of the Society of Thoracic Surgeons.
"We are now into our 23rd month without a deep/organ space infection with over 454 patients," Ms. Kles said in a May interview.
The quality improvement process was initiated after the infection rates at the center were found to be high (ranging up to 6.1), compared with National Healthcare Safety Network data. Using the define, measure, analyze, improve, and control methodology, a multidisciplinary team was convened, including cardiothoracic surgeons, nurses, and support personnel, and a 6-month process was undertaken to identify areas for improvement, said Ms. Kles who chaired the team.
"We also at this time partnered with the VHA National Hospital Engagement Network for some extra training and to help us along the process," she noted.
The team flow-charted processes – from scheduled surgery to discharge – and posted the flow charts in the operating room and cardiac intensive care unit to identify inconsistencies and potential problem areas. Frontline staff members were engaged and encouraged to participate in the improvement process by posting notes, suggestions, and questions on the flow charts.
A literature review was conducted to ensure that current practices mirrored best practices.
Despite an extensive evaluation of possible patient-, procedure-, and hospital-related factors that might be associated with the infection rate, no single cause of the high rate was identified, although a number of areas for improvement were recognized. Among the changes that were implemented were use of chlorhexidine oral rinse, which was administered until discharge; use of disposable EKG leads (after high bacterial counts were found on the leads in use prior to program initiation); use of silver-impregnated midsternal dressings; a change in surgical and suture techniques; development of patient educational materials, and standardization of all processes, Ms. Kles said, noting that the changes were implemented rapidly.
The success of the program is largely attributable to input from all levels and disciplines within the organization – including physicians who championed the process, and to staff engagement and buy in, she said.
The improvement in the infection rate resulted in cost avoidance of $212,355 (compared with a total excess cost of surgical site infections of $250,965 in 2011), and in a reduction from 156 to 24 excess hospital days.
Ms. Kles reported that as of February 2014 she is a member of the speakers bureau for Mölnlycke Health Care, a maker of surgical and wound care products.
AT THE STS ANNUAL MEETING
Key clinical point: Cross-discipline buy in obliterated CABG surgical site infections.
Major finding: Since May, 2012, no surgical site infections have occurred among CABG patients.
Data source: An overview of a quality improvement process at a regional medical center.
Disclosures: Ms. Kles reported that as of February, 2014 she is a member of the speakers bureau for Mölnlycke Health Care.
CDC: Policy changes could prevent 100,000 deaths a year
About one-third of heart disease deaths and one-fifth of cancer deaths could be prevented if overall U.S. death rates were the same as those in the states with the lowest rates, the Centers for Disease Control and Prevention reported May 1.
By using an average of the three states with the lowest death rates as a benchmark for each of the five causes, the analysis showed that 91,757 deaths from heart disease could be prevented each year. For cancer, 84,443 deaths could be prevented annually, according to the CDC report (MMWR 2014;63:369-74).
The total number of potentially preventable deaths is around 100,000, because the figures for each cause cannot be added together because someone who doesn’t die of heart disease may die of cancer or stroke, CDC Director Tom Frieden noted in a press briefing. For the rest of the top five causes of death, the numbers of avoidable deaths were 36,836 for unintentional injuries, 28,831 for chronic lower respiratory disease, and 16,973 for cerebrovascular disease.
The report highlights "the enormous variability among states" when it comes to public health policy, he said, with deaths for all five causes highest in the Southeast.
"In this country, your health and safety are determined more by your ZIP code than your genetic code," Dr. Frieden said. "We need to move the needle on policy change and programmatic change."
The analysis used mortality data from 2008 to 2010 for those younger than age 80 years from the National Vital Statistics System.
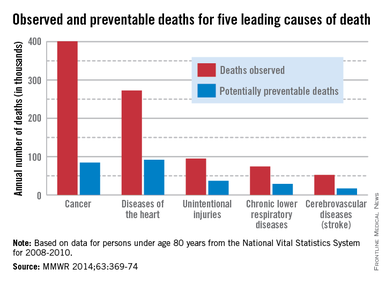
About one-third of heart disease deaths and one-fifth of cancer deaths could be prevented if overall U.S. death rates were the same as those in the states with the lowest rates, the Centers for Disease Control and Prevention reported May 1.
By using an average of the three states with the lowest death rates as a benchmark for each of the five causes, the analysis showed that 91,757 deaths from heart disease could be prevented each year. For cancer, 84,443 deaths could be prevented annually, according to the CDC report (MMWR 2014;63:369-74).
The total number of potentially preventable deaths is around 100,000, because the figures for each cause cannot be added together because someone who doesn’t die of heart disease may die of cancer or stroke, CDC Director Tom Frieden noted in a press briefing. For the rest of the top five causes of death, the numbers of avoidable deaths were 36,836 for unintentional injuries, 28,831 for chronic lower respiratory disease, and 16,973 for cerebrovascular disease.
The report highlights "the enormous variability among states" when it comes to public health policy, he said, with deaths for all five causes highest in the Southeast.
"In this country, your health and safety are determined more by your ZIP code than your genetic code," Dr. Frieden said. "We need to move the needle on policy change and programmatic change."
The analysis used mortality data from 2008 to 2010 for those younger than age 80 years from the National Vital Statistics System.
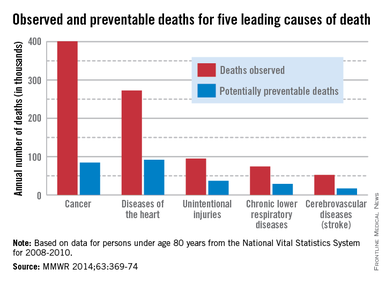
About one-third of heart disease deaths and one-fifth of cancer deaths could be prevented if overall U.S. death rates were the same as those in the states with the lowest rates, the Centers for Disease Control and Prevention reported May 1.
By using an average of the three states with the lowest death rates as a benchmark for each of the five causes, the analysis showed that 91,757 deaths from heart disease could be prevented each year. For cancer, 84,443 deaths could be prevented annually, according to the CDC report (MMWR 2014;63:369-74).
The total number of potentially preventable deaths is around 100,000, because the figures for each cause cannot be added together because someone who doesn’t die of heart disease may die of cancer or stroke, CDC Director Tom Frieden noted in a press briefing. For the rest of the top five causes of death, the numbers of avoidable deaths were 36,836 for unintentional injuries, 28,831 for chronic lower respiratory disease, and 16,973 for cerebrovascular disease.
The report highlights "the enormous variability among states" when it comes to public health policy, he said, with deaths for all five causes highest in the Southeast.
"In this country, your health and safety are determined more by your ZIP code than your genetic code," Dr. Frieden said. "We need to move the needle on policy change and programmatic change."
The analysis used mortality data from 2008 to 2010 for those younger than age 80 years from the National Vital Statistics System.
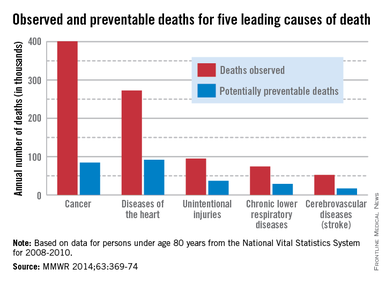
FROM MMWR