User login
VIDEO: RBCs have extended shelf life, randomized trial shows
ORLANDO – Stored red blood cells kept for longer than a few weeks do not impair outcomes or harm the patients who receive them, Dr. Christine Cserti-Gazdewich reported at the annual meeting of the American Society of Hematology.
In a randomized clinical trial conducted in Kanpala, Uganda, where severe anemia with lactic acidosis is common, children who received RBCs that had been stored from 25-35 days had outcomes that were not inferior to those of children who received RBCs delivered within 10 days of collection. The findings have significant, positive implications for countries and geographic regions where there are chronic shortages of blood products, said Dr. Cserti-Gazdewich, of Toronto General Hospital.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Stored red blood cells kept for longer than a few weeks do not impair outcomes or harm the patients who receive them, Dr. Christine Cserti-Gazdewich reported at the annual meeting of the American Society of Hematology.
In a randomized clinical trial conducted in Kanpala, Uganda, where severe anemia with lactic acidosis is common, children who received RBCs that had been stored from 25-35 days had outcomes that were not inferior to those of children who received RBCs delivered within 10 days of collection. The findings have significant, positive implications for countries and geographic regions where there are chronic shortages of blood products, said Dr. Cserti-Gazdewich, of Toronto General Hospital.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Stored red blood cells kept for longer than a few weeks do not impair outcomes or harm the patients who receive them, Dr. Christine Cserti-Gazdewich reported at the annual meeting of the American Society of Hematology.
In a randomized clinical trial conducted in Kanpala, Uganda, where severe anemia with lactic acidosis is common, children who received RBCs that had been stored from 25-35 days had outcomes that were not inferior to those of children who received RBCs delivered within 10 days of collection. The findings have significant, positive implications for countries and geographic regions where there are chronic shortages of blood products, said Dr. Cserti-Gazdewich, of Toronto General Hospital.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASH 2015
ASH: Gene therapy eases effects of rare Wiskott-Aldrich syndrome
ORLANDO – Genetic modification of autologous stem cells provided sustained clinical benefit with good safety for children with the rare immunodeficiency disorder Wiskott-Aldrich syndrome, an international team of investigators report.
Six of eight children who received infusions of autologous stem cells that had been modified with a lentiviral vector to restore normal expression of the WAS gene had marked reductions in severe infections, fewer hospitalizations, improved hematologic parameters, and more robust immune responses than they had prior to transplant, reported Dr. Francesca Ferrua from the San Raffaele Telethon Institute for Gene Therapy in Milan, Italy.
“Importantly, with regards to safety we did not detect any serious adverse events related to gene therapy in follow up, and we did not observe any evidence of abnormal clonal proliferation after gene therapy,” she said at the American Society of Hematology annual meeting here.
The Wiskott-Aldrich syndrome is an x-linked syndrome caused by mutations in the WAS gene encoding for the WAS protein (WASP), which is involved in regulation of the cytoskeleton. The disorder, which primarily affects males, leads to immunodeficiency, microthrombocytopenia and leukocyte abnormalities. Patients develop severe eczema and other inflammatory disorders, and are at increased risk for autoimmune diseases and malignancies.
The syndrome is estimated to occur in 1-10 per 1 million males worldwide, according to The National Library of Medicine.
Allogeneic hematopoietic stem cell transplantion (HSCT) can be curative for patients with Wiskott-Aldrich syndrome, but the technique is associated with both acute transplant-related complications and long-term morbidities, particularly when there is not a perfect match between donor and recipient, Dr. Ferrua explained.Prior studies using a gamma-retroviral vector under the control of a strong viral promoter showed that gene therapy was feasible in these patients and could result in immunological improvement. The earlier attempts, however, were associated with a high risk of genotoxicity and insertional mutagenesis; seven of nine patients treated in one study developed leukemia.
In their current line of research, Dr. Ferrua and colleagues had previously reported on the use of autologous hematopoietic stem/progenitor cells modified ex vivo to correct the inherent defect in three patients with severe mutations in WAS who had no suitable stem-cell donors.
The researchers collected CD34-positive cells from each patient’s bone marrow and/or mobilized peripheral blood and transduced the cells in the laboratory with a lentivirus modified to promote normal expression of WAS. They then returned the cells to the patients after they underwent a reduced-intensity conditioning regimen using an anti-CD20 monoclonal antibody, busulfan, and fludarabine.
Long-term follow-up
At ASH 2015, Dr. Ferrua reported results on the first 8 patients treated as of October 2015. The patients were treated at a median age of 2.2 years; all are alive after a median of 3.3 years of follow up, with the longest follow up being 5.5 years
All had marked reductions in the annualized estimated rate of severe infections compared with the pre-transplant period.
Of the seven patients followed for more than 1 year, all were able to discontinue prophylaxis for infections, at a median of 13-15 months after gene therapy, and five were able to discontinue immunoglobulin supplementation.
Additionally, four of four patients had evidence of a normal immune response based on the development of specific antibodies after vaccination.
Four patients had resolution of their eczemas, and the other two with eczema had only mild cases.
At a median of 4 months after genetic therapy, none of the patients required platelet transfusions. Out to at least 1 year, there was no evidence of autoimmunity.
Among all patients, there were reductions in the frequency or severity of bleeding, no severe bleeding episodes, no hospitalizations for bleeding and a reduction in the number of hospitalizations for infections.
There were no serious adverse events related to the transplant.
The study was sponsored by IRCCS San Raffaele with support from the Fondazione Telethon and GlaxoSmithKline. Dr. Ferrua reported having no conflicts of interest.
ORLANDO – Genetic modification of autologous stem cells provided sustained clinical benefit with good safety for children with the rare immunodeficiency disorder Wiskott-Aldrich syndrome, an international team of investigators report.
Six of eight children who received infusions of autologous stem cells that had been modified with a lentiviral vector to restore normal expression of the WAS gene had marked reductions in severe infections, fewer hospitalizations, improved hematologic parameters, and more robust immune responses than they had prior to transplant, reported Dr. Francesca Ferrua from the San Raffaele Telethon Institute for Gene Therapy in Milan, Italy.
“Importantly, with regards to safety we did not detect any serious adverse events related to gene therapy in follow up, and we did not observe any evidence of abnormal clonal proliferation after gene therapy,” she said at the American Society of Hematology annual meeting here.
The Wiskott-Aldrich syndrome is an x-linked syndrome caused by mutations in the WAS gene encoding for the WAS protein (WASP), which is involved in regulation of the cytoskeleton. The disorder, which primarily affects males, leads to immunodeficiency, microthrombocytopenia and leukocyte abnormalities. Patients develop severe eczema and other inflammatory disorders, and are at increased risk for autoimmune diseases and malignancies.
The syndrome is estimated to occur in 1-10 per 1 million males worldwide, according to The National Library of Medicine.
Allogeneic hematopoietic stem cell transplantion (HSCT) can be curative for patients with Wiskott-Aldrich syndrome, but the technique is associated with both acute transplant-related complications and long-term morbidities, particularly when there is not a perfect match between donor and recipient, Dr. Ferrua explained.Prior studies using a gamma-retroviral vector under the control of a strong viral promoter showed that gene therapy was feasible in these patients and could result in immunological improvement. The earlier attempts, however, were associated with a high risk of genotoxicity and insertional mutagenesis; seven of nine patients treated in one study developed leukemia.
In their current line of research, Dr. Ferrua and colleagues had previously reported on the use of autologous hematopoietic stem/progenitor cells modified ex vivo to correct the inherent defect in three patients with severe mutations in WAS who had no suitable stem-cell donors.
The researchers collected CD34-positive cells from each patient’s bone marrow and/or mobilized peripheral blood and transduced the cells in the laboratory with a lentivirus modified to promote normal expression of WAS. They then returned the cells to the patients after they underwent a reduced-intensity conditioning regimen using an anti-CD20 monoclonal antibody, busulfan, and fludarabine.
Long-term follow-up
At ASH 2015, Dr. Ferrua reported results on the first 8 patients treated as of October 2015. The patients were treated at a median age of 2.2 years; all are alive after a median of 3.3 years of follow up, with the longest follow up being 5.5 years
All had marked reductions in the annualized estimated rate of severe infections compared with the pre-transplant period.
Of the seven patients followed for more than 1 year, all were able to discontinue prophylaxis for infections, at a median of 13-15 months after gene therapy, and five were able to discontinue immunoglobulin supplementation.
Additionally, four of four patients had evidence of a normal immune response based on the development of specific antibodies after vaccination.
Four patients had resolution of their eczemas, and the other two with eczema had only mild cases.
At a median of 4 months after genetic therapy, none of the patients required platelet transfusions. Out to at least 1 year, there was no evidence of autoimmunity.
Among all patients, there were reductions in the frequency or severity of bleeding, no severe bleeding episodes, no hospitalizations for bleeding and a reduction in the number of hospitalizations for infections.
There were no serious adverse events related to the transplant.
The study was sponsored by IRCCS San Raffaele with support from the Fondazione Telethon and GlaxoSmithKline. Dr. Ferrua reported having no conflicts of interest.
ORLANDO – Genetic modification of autologous stem cells provided sustained clinical benefit with good safety for children with the rare immunodeficiency disorder Wiskott-Aldrich syndrome, an international team of investigators report.
Six of eight children who received infusions of autologous stem cells that had been modified with a lentiviral vector to restore normal expression of the WAS gene had marked reductions in severe infections, fewer hospitalizations, improved hematologic parameters, and more robust immune responses than they had prior to transplant, reported Dr. Francesca Ferrua from the San Raffaele Telethon Institute for Gene Therapy in Milan, Italy.
“Importantly, with regards to safety we did not detect any serious adverse events related to gene therapy in follow up, and we did not observe any evidence of abnormal clonal proliferation after gene therapy,” she said at the American Society of Hematology annual meeting here.
The Wiskott-Aldrich syndrome is an x-linked syndrome caused by mutations in the WAS gene encoding for the WAS protein (WASP), which is involved in regulation of the cytoskeleton. The disorder, which primarily affects males, leads to immunodeficiency, microthrombocytopenia and leukocyte abnormalities. Patients develop severe eczema and other inflammatory disorders, and are at increased risk for autoimmune diseases and malignancies.
The syndrome is estimated to occur in 1-10 per 1 million males worldwide, according to The National Library of Medicine.
Allogeneic hematopoietic stem cell transplantion (HSCT) can be curative for patients with Wiskott-Aldrich syndrome, but the technique is associated with both acute transplant-related complications and long-term morbidities, particularly when there is not a perfect match between donor and recipient, Dr. Ferrua explained.Prior studies using a gamma-retroviral vector under the control of a strong viral promoter showed that gene therapy was feasible in these patients and could result in immunological improvement. The earlier attempts, however, were associated with a high risk of genotoxicity and insertional mutagenesis; seven of nine patients treated in one study developed leukemia.
In their current line of research, Dr. Ferrua and colleagues had previously reported on the use of autologous hematopoietic stem/progenitor cells modified ex vivo to correct the inherent defect in three patients with severe mutations in WAS who had no suitable stem-cell donors.
The researchers collected CD34-positive cells from each patient’s bone marrow and/or mobilized peripheral blood and transduced the cells in the laboratory with a lentivirus modified to promote normal expression of WAS. They then returned the cells to the patients after they underwent a reduced-intensity conditioning regimen using an anti-CD20 monoclonal antibody, busulfan, and fludarabine.
Long-term follow-up
At ASH 2015, Dr. Ferrua reported results on the first 8 patients treated as of October 2015. The patients were treated at a median age of 2.2 years; all are alive after a median of 3.3 years of follow up, with the longest follow up being 5.5 years
All had marked reductions in the annualized estimated rate of severe infections compared with the pre-transplant period.
Of the seven patients followed for more than 1 year, all were able to discontinue prophylaxis for infections, at a median of 13-15 months after gene therapy, and five were able to discontinue immunoglobulin supplementation.
Additionally, four of four patients had evidence of a normal immune response based on the development of specific antibodies after vaccination.
Four patients had resolution of their eczemas, and the other two with eczema had only mild cases.
At a median of 4 months after genetic therapy, none of the patients required platelet transfusions. Out to at least 1 year, there was no evidence of autoimmunity.
Among all patients, there were reductions in the frequency or severity of bleeding, no severe bleeding episodes, no hospitalizations for bleeding and a reduction in the number of hospitalizations for infections.
There were no serious adverse events related to the transplant.
The study was sponsored by IRCCS San Raffaele with support from the Fondazione Telethon and GlaxoSmithKline. Dr. Ferrua reported having no conflicts of interest.
AT ASH 2015
Key clinical point: Gene therapy might safely and effectively correct an inherited immunodeficiency syndrome.
Major finding: Six of eight children with Wiskott-Aldrich syndrome who received genetically modified autologous stem cells had marked clinical improvements.
Data source: International collaborative trial studying the safety and efficacy of WAS gene transfer into hematopoietic stem/progenitor cells.
Disclosures: The study was sponsored by IRCCS San Raffaele with support from the Fondazione Telethon and GlaxoSmithKline. Dr. Ferrua reported having no conflicts of interest.
Big declines seen in aspergillosis mortality
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
AT ICAAC 2015
Key clinical point: In-hospital mortality has more than halved for patients with aspergillosis-related hospitalization during a recent 10-year period.
Major finding: In-hospital mortality among patients with an aspergillosis-related hospitalization fell nationally from 18.8% in 2001 to 7.7% in 2011, with the biggest drop occurring in those at high risk.
Data source: A retrospective study of nationally representative data from the Healthcare Utilization and Cost Project–Nationwide Inpatient Sample for 2001-2011.
Disclosures: The presenter reported having no financial conflicts regarding this unfunded study.
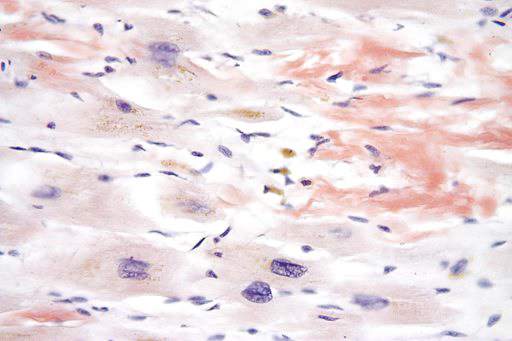
Excellent survival after ASCT for light-chain amyloidosis
Early mortality after autologous hematopoietic stem cell transplantation (ASCT) for light-chain amyloidosis has declined dramatically in recent years, and 5-year survival is now deemed “excellent” at 77%, according to a report published online Sept. 14 in Journal of Clinical Oncology.
Light-chain amyloidosis results in deposition of insoluble amyloid fibers in many tissues, particularly the heart and kidneys, and can lead to organ failure and death. While medical therapies target the plasma cell clone that is the source of the amyloid, treatments have minimal effect on amyloid that has already accumulated in tissues. Alternatively, ASCT can produce durable hematologic responses and has resulted in improved function of affected organs, based on several single-center studies.
However, the only large, prospective randomized clinical trial to compare ASCT and medical therapy was done in 2007. That study showed autotransplantation carried a high (24%) early mortality, which contributed heavily to inferior overall survival, said Dr. Anita D’Souza of the division of hematology and oncology, Medical College of Wisconsin, Milwaukee, and her associates.
Since that study, supportive care during the peritransplantation period has greatly improved. Large U.S. transplant centers now report that early mortality is less than 5%.
To assess time trends in autotransplantation mortality, Dr. D’Souza and her associates analyzed data from the Center for International Blood & Marrow Transplant Research, a registry that collects transplant data from 320 centers worldwide and captures information concerning most U.S. procedures. They focused on 1,536 North American patients with light-chain amyloidosis who underwent ASCT during three successive 5-year periods: 1995-2000, 2001-2006, and 2007-2012. The median follow-up was 56 months.
Over time, 30-day mortality declined from 11% to 5% to 3%, respectively; and 100-day mortality declined from 20% to 11% to 5%. One-year overall survival rose from 75% to 85% to 90%, and 5-year overall survival improved from 55% to 61% to 77%.
Even among patients with renal amyloidosis, 3-year overall survival improved over time from 78% during the earliest study period to 89% during the most recent time period. However, mortality did not improve significantly over time among patients with cardiac involvement, which continues to be the single most-important variable associated with poor outcomes, the researchers said (J Clin Oncol. 2015 Sep 14 [doi:10.1200/JCO.2015.62.4015]).
A transplant center’s experience with this procedure proved to be of crucial importance to early patient mortality. Centers that performed a low volume of ASCT for light-chain amyloidosis, defined as fewer than four transplants per year, had a 30-day mortality of 5% and a 100-day mortality of 7%, while centers that performed more than four procedures per year had significantly lower mortalities of 1% and 3%, respectively. There were no significant differences between low- and high-volume centers regarding patient, organ, or medication factors, which “led us to believe that high-volume centers do not necessarily select fitter patients for transplantation. Rather, they may be more experienced in supporting and treating these patients in the early posttransplantation period,” Dr. D’Souza and her associates said.
These “reassuring” findings, together with the recent development of novel plasma-cell–targeting agents such as bortezomib, suggest that it is time to consider performing a more current multicenter prospective study comparing autotransplantation against medical therapy, they added.
It is important to place these study findings in context, and note that approximately 20% of patients seen at most transplant centers are considered good candidates for autologous hematopoietic cell transplantation. The outcomes of the procedure remain unsatisfactory for most patients.
Delayed diagnosis appears to be a major obstacle to effective treatment. Many patients experience significant organ dysfunction before a diagnosis is established, even when the underlying plasma cell dyscrasia is being actively followed by a hematologist.
Dr. Noffar Bar, Dr. Terri L. Parker, and Dr. Madhav V. Dhodapkar are at Yale Cancer Center, New Haven Conn. They made these remarks in an editorial accompanying Dr. D’Souza’s report (J Clin Oncol. Sep 14 [doi:10.1200/HCO.2015.63.2224]). Their financial disclosures are available at www.jco.org.
It is important to place these study findings in context, and note that approximately 20% of patients seen at most transplant centers are considered good candidates for autologous hematopoietic cell transplantation. The outcomes of the procedure remain unsatisfactory for most patients.
Delayed diagnosis appears to be a major obstacle to effective treatment. Many patients experience significant organ dysfunction before a diagnosis is established, even when the underlying plasma cell dyscrasia is being actively followed by a hematologist.
Dr. Noffar Bar, Dr. Terri L. Parker, and Dr. Madhav V. Dhodapkar are at Yale Cancer Center, New Haven Conn. They made these remarks in an editorial accompanying Dr. D’Souza’s report (J Clin Oncol. Sep 14 [doi:10.1200/HCO.2015.63.2224]). Their financial disclosures are available at www.jco.org.
It is important to place these study findings in context, and note that approximately 20% of patients seen at most transplant centers are considered good candidates for autologous hematopoietic cell transplantation. The outcomes of the procedure remain unsatisfactory for most patients.
Delayed diagnosis appears to be a major obstacle to effective treatment. Many patients experience significant organ dysfunction before a diagnosis is established, even when the underlying plasma cell dyscrasia is being actively followed by a hematologist.
Dr. Noffar Bar, Dr. Terri L. Parker, and Dr. Madhav V. Dhodapkar are at Yale Cancer Center, New Haven Conn. They made these remarks in an editorial accompanying Dr. D’Souza’s report (J Clin Oncol. Sep 14 [doi:10.1200/HCO.2015.63.2224]). Their financial disclosures are available at www.jco.org.
Early mortality after autologous hematopoietic stem cell transplantation (ASCT) for light-chain amyloidosis has declined dramatically in recent years, and 5-year survival is now deemed “excellent” at 77%, according to a report published online Sept. 14 in Journal of Clinical Oncology.
Light-chain amyloidosis results in deposition of insoluble amyloid fibers in many tissues, particularly the heart and kidneys, and can lead to organ failure and death. While medical therapies target the plasma cell clone that is the source of the amyloid, treatments have minimal effect on amyloid that has already accumulated in tissues. Alternatively, ASCT can produce durable hematologic responses and has resulted in improved function of affected organs, based on several single-center studies.
However, the only large, prospective randomized clinical trial to compare ASCT and medical therapy was done in 2007. That study showed autotransplantation carried a high (24%) early mortality, which contributed heavily to inferior overall survival, said Dr. Anita D’Souza of the division of hematology and oncology, Medical College of Wisconsin, Milwaukee, and her associates.
Since that study, supportive care during the peritransplantation period has greatly improved. Large U.S. transplant centers now report that early mortality is less than 5%.
To assess time trends in autotransplantation mortality, Dr. D’Souza and her associates analyzed data from the Center for International Blood & Marrow Transplant Research, a registry that collects transplant data from 320 centers worldwide and captures information concerning most U.S. procedures. They focused on 1,536 North American patients with light-chain amyloidosis who underwent ASCT during three successive 5-year periods: 1995-2000, 2001-2006, and 2007-2012. The median follow-up was 56 months.
Over time, 30-day mortality declined from 11% to 5% to 3%, respectively; and 100-day mortality declined from 20% to 11% to 5%. One-year overall survival rose from 75% to 85% to 90%, and 5-year overall survival improved from 55% to 61% to 77%.
Even among patients with renal amyloidosis, 3-year overall survival improved over time from 78% during the earliest study period to 89% during the most recent time period. However, mortality did not improve significantly over time among patients with cardiac involvement, which continues to be the single most-important variable associated with poor outcomes, the researchers said (J Clin Oncol. 2015 Sep 14 [doi:10.1200/JCO.2015.62.4015]).
A transplant center’s experience with this procedure proved to be of crucial importance to early patient mortality. Centers that performed a low volume of ASCT for light-chain amyloidosis, defined as fewer than four transplants per year, had a 30-day mortality of 5% and a 100-day mortality of 7%, while centers that performed more than four procedures per year had significantly lower mortalities of 1% and 3%, respectively. There were no significant differences between low- and high-volume centers regarding patient, organ, or medication factors, which “led us to believe that high-volume centers do not necessarily select fitter patients for transplantation. Rather, they may be more experienced in supporting and treating these patients in the early posttransplantation period,” Dr. D’Souza and her associates said.
These “reassuring” findings, together with the recent development of novel plasma-cell–targeting agents such as bortezomib, suggest that it is time to consider performing a more current multicenter prospective study comparing autotransplantation against medical therapy, they added.
Early mortality after autologous hematopoietic stem cell transplantation (ASCT) for light-chain amyloidosis has declined dramatically in recent years, and 5-year survival is now deemed “excellent” at 77%, according to a report published online Sept. 14 in Journal of Clinical Oncology.
Light-chain amyloidosis results in deposition of insoluble amyloid fibers in many tissues, particularly the heart and kidneys, and can lead to organ failure and death. While medical therapies target the plasma cell clone that is the source of the amyloid, treatments have minimal effect on amyloid that has already accumulated in tissues. Alternatively, ASCT can produce durable hematologic responses and has resulted in improved function of affected organs, based on several single-center studies.
However, the only large, prospective randomized clinical trial to compare ASCT and medical therapy was done in 2007. That study showed autotransplantation carried a high (24%) early mortality, which contributed heavily to inferior overall survival, said Dr. Anita D’Souza of the division of hematology and oncology, Medical College of Wisconsin, Milwaukee, and her associates.
Since that study, supportive care during the peritransplantation period has greatly improved. Large U.S. transplant centers now report that early mortality is less than 5%.
To assess time trends in autotransplantation mortality, Dr. D’Souza and her associates analyzed data from the Center for International Blood & Marrow Transplant Research, a registry that collects transplant data from 320 centers worldwide and captures information concerning most U.S. procedures. They focused on 1,536 North American patients with light-chain amyloidosis who underwent ASCT during three successive 5-year periods: 1995-2000, 2001-2006, and 2007-2012. The median follow-up was 56 months.
Over time, 30-day mortality declined from 11% to 5% to 3%, respectively; and 100-day mortality declined from 20% to 11% to 5%. One-year overall survival rose from 75% to 85% to 90%, and 5-year overall survival improved from 55% to 61% to 77%.
Even among patients with renal amyloidosis, 3-year overall survival improved over time from 78% during the earliest study period to 89% during the most recent time period. However, mortality did not improve significantly over time among patients with cardiac involvement, which continues to be the single most-important variable associated with poor outcomes, the researchers said (J Clin Oncol. 2015 Sep 14 [doi:10.1200/JCO.2015.62.4015]).
A transplant center’s experience with this procedure proved to be of crucial importance to early patient mortality. Centers that performed a low volume of ASCT for light-chain amyloidosis, defined as fewer than four transplants per year, had a 30-day mortality of 5% and a 100-day mortality of 7%, while centers that performed more than four procedures per year had significantly lower mortalities of 1% and 3%, respectively. There were no significant differences between low- and high-volume centers regarding patient, organ, or medication factors, which “led us to believe that high-volume centers do not necessarily select fitter patients for transplantation. Rather, they may be more experienced in supporting and treating these patients in the early posttransplantation period,” Dr. D’Souza and her associates said.
These “reassuring” findings, together with the recent development of novel plasma-cell–targeting agents such as bortezomib, suggest that it is time to consider performing a more current multicenter prospective study comparing autotransplantation against medical therapy, they added.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Early mortality after autologous hematopoietic stem cell transplantation for light-chain amyloidosis has declined dramatically in recent years.
Major finding: 30-day mortality declined from 11% to 5% to 3% in three successive time periods, and 100-day mortality declined from 20% to 11% to 5%.
Data source: A retrospective international cohort study of mortality outcomes in 1,536 patients with light-chain amyloidosis treated during 1995-2012 and followed for a median of 56 months.
Disclosures: This study was supported by the National Cancer Institute; the National Heart, Lung, and Blood Institute; the Health Resources and Services Administration; the Department of the Navy, the Department of Defense, other government groups, several private organizations; and numerous industry sources. Dr. D’Souza reported having no relevant financial disclosures; her associates reported ties to numerous pharmaceutical and biomedical companies.
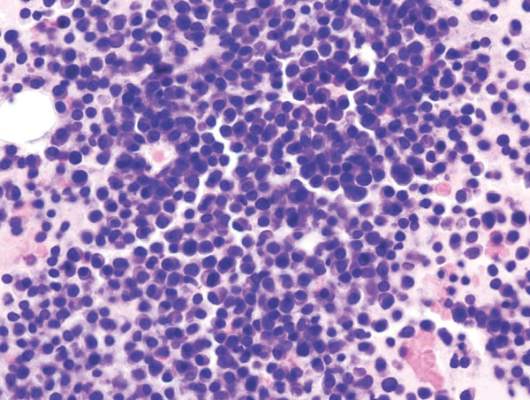
CTL019 induced a durable complete response in refractory MM
The first recipient of CTL019 for advanced refractory multiple myeloma achieved a durable complete response without developing cytokine release syndrome, according to a study published Sept. 9 in the New England Journal of Medicine.
“Twelve months after transplantation, the patient had no evidence of monoclonal immunoglobulin on serum and urine immunofixation and no clinical signs or symptoms of multiple myeloma,” said Dr. Alfred Garfall and his associates at the University of Pennsylvania in Philadelphia. “This response was achieved despite the absence of CD19 expression in 99.95% of the patient’s neoplastic plasma cells.”
CTL019 consists of autologous T cells modified to express an anti-CD19 chimeric antigen receptor (CAR) from a lentiviral vector. The cell therapy has yielded promising results in relapsed/refractory CLL and ALL,but was overlooked in MM because it was thought to infrequently express CD19, the researchers said.
“Several reports, however, have suggested that a minor component of the MM clone with drug-resistant, disease-propagating properties has a B-cell (i.e., CD19-positive) phenotype,” they noted. “In addition, our unpublished observations suggest that neoplastic plasma cells express low levels of CD19” (N Engl J Med. 2015 Sep 9;373:1040-7).
In response, they designed a pilot trial of adults whose MM relapsed or progressed within a year after initial autologous stem cell transplant. The first participant, a 43-year-old woman with IgA kappa MM, partially responded to lenalidomide, bortezomib, and dexamethasone but progressed when therapy was paused to collect stem cells for transplant. She then partially responded to cisplatin, doxorubicin, cyclophosphamide, and etoposide followed by high-dose melphalan and ASCT, but progressed again and continued to worsen despite a total of nine lines of therapy. A bone marrow sample revealed more than 95% plasma cells when the patient began the CTL019 trial, the researchers said.
For the study, the patient received a lower melphalan dose (140 mg/m2 of body surface area), followed by ASCT, CTL019 starting 2 weeks later, and maintenance lenalidomide. On day 100, her tumor burden had dropped by 5-log10, the researchers said. She also did not develop cytokine release syndrome, they added.
So far, 10 patients have been treated on study, of whom six remain progression free, according to the investigators. “The only additional CTL019-attributable toxic effects observed have been one instance of grade 1 cytokine release syndrome and one instance of grade 3 enterocolitis due to autologous graft-versus-host disease,” they reported.
Novartis supported the study and approved the manuscript. The work was also funded by the National Institutes of Health, the International Society for Advancement of Cytometry, the University of Pennsylvania Institute or Translational Medicine and Therapeutics, and a Conquer Cancer Foundation Young Investigator Award. The University of Pennsylvania has licensed technologies involved in this trial to Novartis. Several scientists involved in this trial hold patents for these technologies. As a result of the licensing relationship with Novartis, the University of Pennsylvania receives significant financial benefit, and these inventors have benefited financially or may benefit in the future.
The first recipient of CTL019 for advanced refractory multiple myeloma achieved a durable complete response without developing cytokine release syndrome, according to a study published Sept. 9 in the New England Journal of Medicine.
“Twelve months after transplantation, the patient had no evidence of monoclonal immunoglobulin on serum and urine immunofixation and no clinical signs or symptoms of multiple myeloma,” said Dr. Alfred Garfall and his associates at the University of Pennsylvania in Philadelphia. “This response was achieved despite the absence of CD19 expression in 99.95% of the patient’s neoplastic plasma cells.”
CTL019 consists of autologous T cells modified to express an anti-CD19 chimeric antigen receptor (CAR) from a lentiviral vector. The cell therapy has yielded promising results in relapsed/refractory CLL and ALL,but was overlooked in MM because it was thought to infrequently express CD19, the researchers said.
“Several reports, however, have suggested that a minor component of the MM clone with drug-resistant, disease-propagating properties has a B-cell (i.e., CD19-positive) phenotype,” they noted. “In addition, our unpublished observations suggest that neoplastic plasma cells express low levels of CD19” (N Engl J Med. 2015 Sep 9;373:1040-7).
In response, they designed a pilot trial of adults whose MM relapsed or progressed within a year after initial autologous stem cell transplant. The first participant, a 43-year-old woman with IgA kappa MM, partially responded to lenalidomide, bortezomib, and dexamethasone but progressed when therapy was paused to collect stem cells for transplant. She then partially responded to cisplatin, doxorubicin, cyclophosphamide, and etoposide followed by high-dose melphalan and ASCT, but progressed again and continued to worsen despite a total of nine lines of therapy. A bone marrow sample revealed more than 95% plasma cells when the patient began the CTL019 trial, the researchers said.
For the study, the patient received a lower melphalan dose (140 mg/m2 of body surface area), followed by ASCT, CTL019 starting 2 weeks later, and maintenance lenalidomide. On day 100, her tumor burden had dropped by 5-log10, the researchers said. She also did not develop cytokine release syndrome, they added.
So far, 10 patients have been treated on study, of whom six remain progression free, according to the investigators. “The only additional CTL019-attributable toxic effects observed have been one instance of grade 1 cytokine release syndrome and one instance of grade 3 enterocolitis due to autologous graft-versus-host disease,” they reported.
Novartis supported the study and approved the manuscript. The work was also funded by the National Institutes of Health, the International Society for Advancement of Cytometry, the University of Pennsylvania Institute or Translational Medicine and Therapeutics, and a Conquer Cancer Foundation Young Investigator Award. The University of Pennsylvania has licensed technologies involved in this trial to Novartis. Several scientists involved in this trial hold patents for these technologies. As a result of the licensing relationship with Novartis, the University of Pennsylvania receives significant financial benefit, and these inventors have benefited financially or may benefit in the future.
The first recipient of CTL019 for advanced refractory multiple myeloma achieved a durable complete response without developing cytokine release syndrome, according to a study published Sept. 9 in the New England Journal of Medicine.
“Twelve months after transplantation, the patient had no evidence of monoclonal immunoglobulin on serum and urine immunofixation and no clinical signs or symptoms of multiple myeloma,” said Dr. Alfred Garfall and his associates at the University of Pennsylvania in Philadelphia. “This response was achieved despite the absence of CD19 expression in 99.95% of the patient’s neoplastic plasma cells.”
CTL019 consists of autologous T cells modified to express an anti-CD19 chimeric antigen receptor (CAR) from a lentiviral vector. The cell therapy has yielded promising results in relapsed/refractory CLL and ALL,but was overlooked in MM because it was thought to infrequently express CD19, the researchers said.
“Several reports, however, have suggested that a minor component of the MM clone with drug-resistant, disease-propagating properties has a B-cell (i.e., CD19-positive) phenotype,” they noted. “In addition, our unpublished observations suggest that neoplastic plasma cells express low levels of CD19” (N Engl J Med. 2015 Sep 9;373:1040-7).
In response, they designed a pilot trial of adults whose MM relapsed or progressed within a year after initial autologous stem cell transplant. The first participant, a 43-year-old woman with IgA kappa MM, partially responded to lenalidomide, bortezomib, and dexamethasone but progressed when therapy was paused to collect stem cells for transplant. She then partially responded to cisplatin, doxorubicin, cyclophosphamide, and etoposide followed by high-dose melphalan and ASCT, but progressed again and continued to worsen despite a total of nine lines of therapy. A bone marrow sample revealed more than 95% plasma cells when the patient began the CTL019 trial, the researchers said.
For the study, the patient received a lower melphalan dose (140 mg/m2 of body surface area), followed by ASCT, CTL019 starting 2 weeks later, and maintenance lenalidomide. On day 100, her tumor burden had dropped by 5-log10, the researchers said. She also did not develop cytokine release syndrome, they added.
So far, 10 patients have been treated on study, of whom six remain progression free, according to the investigators. “The only additional CTL019-attributable toxic effects observed have been one instance of grade 1 cytokine release syndrome and one instance of grade 3 enterocolitis due to autologous graft-versus-host disease,” they reported.
Novartis supported the study and approved the manuscript. The work was also funded by the National Institutes of Health, the International Society for Advancement of Cytometry, the University of Pennsylvania Institute or Translational Medicine and Therapeutics, and a Conquer Cancer Foundation Young Investigator Award. The University of Pennsylvania has licensed technologies involved in this trial to Novartis. Several scientists involved in this trial hold patents for these technologies. As a result of the licensing relationship with Novartis, the University of Pennsylvania receives significant financial benefit, and these inventors have benefited financially or may benefit in the future.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: CTL019 cell therapy after stem cell transplant led to a durable complete response that persisted at 12 months in a patient with advanced, refractory multiple myeloma.
Major finding: The patient received a lower melphalan dose (140 mg/m2 of body surface area), followed by ASCT, CTL019 starting 2 weeks later, and maintenance lenalidomide. On day 100, her tumor burden had dropped by 5-log10.
Data source: Ongoing pilot trial of CTL019 for patients with MM who relapsed within 12 months of their first transplant.
Disclosures: Novartis funded the study and approved the manuscript. The work was also funded by the National Institutes of Health, the International Society for Advancement of Cytometry, the University of Pennsylvania Institute or Translational Medicine and Therapeutics, and a Conquer Cancer Foundation Young Investigator Award. The University of Pennsylvania has licensed technologies involved in this trial to Novartis. Several scientists involved in this trial hold patents for these technologies. As a result of the licensing relationship with Novartis, the University of Pennsylvania receives significant financial benefit, and these inventors have benefited financially or may benefit in the future.
Guideline updated on hematopoietic colony-stimulating factors
Hematopoietic colony-stimulating factors should now be considered for patients who are over age 64 years, have diffuse aggressive lymphoma, and are receiving curative chemotherapy (cyclophosphamide, doxorubicin, vincristine, prednisone, and rituximab), particularly those who have comorbidities.
This is one of several recommendations noted in the American Society of Clinical Oncology’s updated practice guidelines, published online in the Journal of Clinical Oncology, on the use of hematopoietic colony-stimulating factors (CSFs) to prevent or treat neutropenia and its complications in adults and children receiving chemotherapy.
This “moderately strong” recommendation is based on a single randomized clinical trial that found pegfilgrastim significantly reduced the risk of febrile neutropenia in this patient population, according to the guidelines (J. Clin. Oncol. 2015 July 13 [doi:10.1200/JCO.2015.62.3488]).
The updated guideline incorporates new evidence from 66 randomized controlled trials and meta-analyses published since its last update in 2006, said cochair Dr. Thomas J. Smith of the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore, and his associates on the update committee.
In addition to pegfilgrastim and filgrastim, the guideline now addresses the use of tbo-filgrastim, filgrastim-sndz, and other biosimilars as they become available. These new agents are effective at preventing chemotherapy-related febrile neutropenia, so the choice of agent depends on convenience, cost, and clinical factors, and in some cases may be dictated by the patient’s treatment schedule. Certain off-label uses of pegfilgrastim can now be considered, such as giving it on the same day as chemotherapy if that is the only feasible timing for some patients.
CSFs should only be used to enable dose-dense chemotherapy regimens “if supported by convincing efficacy data or within an appropriately designed clinical trial” – for example, to support treatment of urothelial cancer or high-risk breast cancer targeted with high-dose-intensity methotrexate, vinblastine, doxorubicin, and cisplatin.
In contrast, the use of CSFs to enable dose-dense chemotherapy for Hodgkin lymphoma is not recommended at this time because the current data supporting such use are limited and conflicting. Similarly, the current evidence strongly argues against giving CSFs to enable dose-dense chemotherapy for other lymphomas, lung cancer, ovarian cancer, osteosarcoma, or sarcoma.
The guideline update was supported by the American Society of Clinical Oncology. Dr. Smith reported stock or other ownership in United Healthcare; his associates reported ties to numerous industry sources.
The full guideline and supplementary material, including slide sets and clinical tools, are available at www.asco.org/guidelines/wbcgf.
Hematopoietic colony-stimulating factors should now be considered for patients who are over age 64 years, have diffuse aggressive lymphoma, and are receiving curative chemotherapy (cyclophosphamide, doxorubicin, vincristine, prednisone, and rituximab), particularly those who have comorbidities.
This is one of several recommendations noted in the American Society of Clinical Oncology’s updated practice guidelines, published online in the Journal of Clinical Oncology, on the use of hematopoietic colony-stimulating factors (CSFs) to prevent or treat neutropenia and its complications in adults and children receiving chemotherapy.
This “moderately strong” recommendation is based on a single randomized clinical trial that found pegfilgrastim significantly reduced the risk of febrile neutropenia in this patient population, according to the guidelines (J. Clin. Oncol. 2015 July 13 [doi:10.1200/JCO.2015.62.3488]).
The updated guideline incorporates new evidence from 66 randomized controlled trials and meta-analyses published since its last update in 2006, said cochair Dr. Thomas J. Smith of the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore, and his associates on the update committee.
In addition to pegfilgrastim and filgrastim, the guideline now addresses the use of tbo-filgrastim, filgrastim-sndz, and other biosimilars as they become available. These new agents are effective at preventing chemotherapy-related febrile neutropenia, so the choice of agent depends on convenience, cost, and clinical factors, and in some cases may be dictated by the patient’s treatment schedule. Certain off-label uses of pegfilgrastim can now be considered, such as giving it on the same day as chemotherapy if that is the only feasible timing for some patients.
CSFs should only be used to enable dose-dense chemotherapy regimens “if supported by convincing efficacy data or within an appropriately designed clinical trial” – for example, to support treatment of urothelial cancer or high-risk breast cancer targeted with high-dose-intensity methotrexate, vinblastine, doxorubicin, and cisplatin.
In contrast, the use of CSFs to enable dose-dense chemotherapy for Hodgkin lymphoma is not recommended at this time because the current data supporting such use are limited and conflicting. Similarly, the current evidence strongly argues against giving CSFs to enable dose-dense chemotherapy for other lymphomas, lung cancer, ovarian cancer, osteosarcoma, or sarcoma.
The guideline update was supported by the American Society of Clinical Oncology. Dr. Smith reported stock or other ownership in United Healthcare; his associates reported ties to numerous industry sources.
The full guideline and supplementary material, including slide sets and clinical tools, are available at www.asco.org/guidelines/wbcgf.
Hematopoietic colony-stimulating factors should now be considered for patients who are over age 64 years, have diffuse aggressive lymphoma, and are receiving curative chemotherapy (cyclophosphamide, doxorubicin, vincristine, prednisone, and rituximab), particularly those who have comorbidities.
This is one of several recommendations noted in the American Society of Clinical Oncology’s updated practice guidelines, published online in the Journal of Clinical Oncology, on the use of hematopoietic colony-stimulating factors (CSFs) to prevent or treat neutropenia and its complications in adults and children receiving chemotherapy.
This “moderately strong” recommendation is based on a single randomized clinical trial that found pegfilgrastim significantly reduced the risk of febrile neutropenia in this patient population, according to the guidelines (J. Clin. Oncol. 2015 July 13 [doi:10.1200/JCO.2015.62.3488]).
The updated guideline incorporates new evidence from 66 randomized controlled trials and meta-analyses published since its last update in 2006, said cochair Dr. Thomas J. Smith of the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore, and his associates on the update committee.
In addition to pegfilgrastim and filgrastim, the guideline now addresses the use of tbo-filgrastim, filgrastim-sndz, and other biosimilars as they become available. These new agents are effective at preventing chemotherapy-related febrile neutropenia, so the choice of agent depends on convenience, cost, and clinical factors, and in some cases may be dictated by the patient’s treatment schedule. Certain off-label uses of pegfilgrastim can now be considered, such as giving it on the same day as chemotherapy if that is the only feasible timing for some patients.
CSFs should only be used to enable dose-dense chemotherapy regimens “if supported by convincing efficacy data or within an appropriately designed clinical trial” – for example, to support treatment of urothelial cancer or high-risk breast cancer targeted with high-dose-intensity methotrexate, vinblastine, doxorubicin, and cisplatin.
In contrast, the use of CSFs to enable dose-dense chemotherapy for Hodgkin lymphoma is not recommended at this time because the current data supporting such use are limited and conflicting. Similarly, the current evidence strongly argues against giving CSFs to enable dose-dense chemotherapy for other lymphomas, lung cancer, ovarian cancer, osteosarcoma, or sarcoma.
The guideline update was supported by the American Society of Clinical Oncology. Dr. Smith reported stock or other ownership in United Healthcare; his associates reported ties to numerous industry sources.
The full guideline and supplementary material, including slide sets and clinical tools, are available at www.asco.org/guidelines/wbcgf.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
CD8 cell dose predicts outcomes in allogeneic stem cell transplantation with reduced-intensity conditioning
Peripheral blood stem cell (PBSC) grafts with high doses of CD8 cells were associated with significantly lower relapse risk and improved survival in patients who were treated for hematologic malignancies with reduced-intensity conditioning (RIC) hematopoietic allogeneic stem cell transplantation (allo-HSCT), according to a report online in the Journal of Clinical Oncology.
A multivariate analysis showed that CD8 cell dose was an independent predictor of relapse (adjusted hazard ratio [aHR], 0.43; P = .009), relapse-free survival (aHR, 0.50; P = .006), and overall survival (aHR, 0.57; P = .04). The data showed a linear association between CD8 cell dose and outcomes, and further analysis identified an optimum cutoff of CD8 cell dose (0.72 x 108 CD8 cells per kg) to segregate survival outcomes. Patients who received grafts with CD8 cell doses above the cutoff had significantly improved regression-free and overall survival (P = .005 and P = .007, respectively).
“These findings indicate that improved survival after RIC transplantations could be achieved by optimizing donor selection and PBSC collection to increase the likelihood of mobilizing grafts containing high CD8 cell doses,” wrote Dr. Ran Reshef of the department of medicine at the Hospital of the University of Pennsylvania, Philadelphia, and colleagues (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2014.60.1203]).
Younger donors were more likely to have CD8 cell doses above the cutoff (CD8hi), however, only 53% of donors younger than 30 years had CD8hi grafts. To find methods to predict graft composition during donor screening, the investigators studied 21 randomly selected allo-HSCT donors. They found no correlations between CD8 graft content and clinical variables such as weight, sex, viral serologies, or apheresis parameters. Donors with a higher proportion of CD8 cells donated grafts with higher CD8 cell dose, but the presence of higher CD4 counts negated this. Screening for the relative proportions of CD8 and CD4 cells identifies donors most likely to mobilize CD8hi grafts.
“This is also a practical consideration because the assay is rapid, is routinely performed in clinical laboratories, and can easily be done at the time of confirmatory HLA [human leukocyte antigen] typing,” the authors noted. Since the relationship between CD8 dose and survival is linear, the higher the dose the better, even if it is below the cutoff.
Previous studies showed conflicting results regarding the outcome of RIC transplantation with younger unrelated donors versus older sibling donors. Donor age inversely correlates with CD8 cell dose, and the results of this study showed that overall survival was significantly better with younger unrelated donors with a CD8hi graft, compared with older sibling donors (P = .03). No such benefit was observed with younger unrelated donors with CD8lo grafts (P = .28), indicating the benefit may rely on CD8 cell dose.
The study evaluated 200 patients with hematologic malignancy who underwent allo-HSCT with fludarabine plus busulfan conditioning from 2007 to 2014 at the Abramson Cancer Center, University of Pennsylvania in Philadelphia. The cumulative relapse incidence was 42% at 1 year and 47% at 5 years. The most common diseases in the cohort were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma.
High CD8 dose was associated with an increased, but nonsignificant risk of chronic graft-versus-host disease (GVHD); the risk for nonrelapse mortality was not associated with cell doses.
Peripheral blood stem cell (PBSC) grafts with high doses of CD8 cells were associated with significantly lower relapse risk and improved survival in patients who were treated for hematologic malignancies with reduced-intensity conditioning (RIC) hematopoietic allogeneic stem cell transplantation (allo-HSCT), according to a report online in the Journal of Clinical Oncology.
A multivariate analysis showed that CD8 cell dose was an independent predictor of relapse (adjusted hazard ratio [aHR], 0.43; P = .009), relapse-free survival (aHR, 0.50; P = .006), and overall survival (aHR, 0.57; P = .04). The data showed a linear association between CD8 cell dose and outcomes, and further analysis identified an optimum cutoff of CD8 cell dose (0.72 x 108 CD8 cells per kg) to segregate survival outcomes. Patients who received grafts with CD8 cell doses above the cutoff had significantly improved regression-free and overall survival (P = .005 and P = .007, respectively).
“These findings indicate that improved survival after RIC transplantations could be achieved by optimizing donor selection and PBSC collection to increase the likelihood of mobilizing grafts containing high CD8 cell doses,” wrote Dr. Ran Reshef of the department of medicine at the Hospital of the University of Pennsylvania, Philadelphia, and colleagues (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2014.60.1203]).
Younger donors were more likely to have CD8 cell doses above the cutoff (CD8hi), however, only 53% of donors younger than 30 years had CD8hi grafts. To find methods to predict graft composition during donor screening, the investigators studied 21 randomly selected allo-HSCT donors. They found no correlations between CD8 graft content and clinical variables such as weight, sex, viral serologies, or apheresis parameters. Donors with a higher proportion of CD8 cells donated grafts with higher CD8 cell dose, but the presence of higher CD4 counts negated this. Screening for the relative proportions of CD8 and CD4 cells identifies donors most likely to mobilize CD8hi grafts.
“This is also a practical consideration because the assay is rapid, is routinely performed in clinical laboratories, and can easily be done at the time of confirmatory HLA [human leukocyte antigen] typing,” the authors noted. Since the relationship between CD8 dose and survival is linear, the higher the dose the better, even if it is below the cutoff.
Previous studies showed conflicting results regarding the outcome of RIC transplantation with younger unrelated donors versus older sibling donors. Donor age inversely correlates with CD8 cell dose, and the results of this study showed that overall survival was significantly better with younger unrelated donors with a CD8hi graft, compared with older sibling donors (P = .03). No such benefit was observed with younger unrelated donors with CD8lo grafts (P = .28), indicating the benefit may rely on CD8 cell dose.
The study evaluated 200 patients with hematologic malignancy who underwent allo-HSCT with fludarabine plus busulfan conditioning from 2007 to 2014 at the Abramson Cancer Center, University of Pennsylvania in Philadelphia. The cumulative relapse incidence was 42% at 1 year and 47% at 5 years. The most common diseases in the cohort were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma.
High CD8 dose was associated with an increased, but nonsignificant risk of chronic graft-versus-host disease (GVHD); the risk for nonrelapse mortality was not associated with cell doses.
Peripheral blood stem cell (PBSC) grafts with high doses of CD8 cells were associated with significantly lower relapse risk and improved survival in patients who were treated for hematologic malignancies with reduced-intensity conditioning (RIC) hematopoietic allogeneic stem cell transplantation (allo-HSCT), according to a report online in the Journal of Clinical Oncology.
A multivariate analysis showed that CD8 cell dose was an independent predictor of relapse (adjusted hazard ratio [aHR], 0.43; P = .009), relapse-free survival (aHR, 0.50; P = .006), and overall survival (aHR, 0.57; P = .04). The data showed a linear association between CD8 cell dose and outcomes, and further analysis identified an optimum cutoff of CD8 cell dose (0.72 x 108 CD8 cells per kg) to segregate survival outcomes. Patients who received grafts with CD8 cell doses above the cutoff had significantly improved regression-free and overall survival (P = .005 and P = .007, respectively).
“These findings indicate that improved survival after RIC transplantations could be achieved by optimizing donor selection and PBSC collection to increase the likelihood of mobilizing grafts containing high CD8 cell doses,” wrote Dr. Ran Reshef of the department of medicine at the Hospital of the University of Pennsylvania, Philadelphia, and colleagues (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2014.60.1203]).
Younger donors were more likely to have CD8 cell doses above the cutoff (CD8hi), however, only 53% of donors younger than 30 years had CD8hi grafts. To find methods to predict graft composition during donor screening, the investigators studied 21 randomly selected allo-HSCT donors. They found no correlations between CD8 graft content and clinical variables such as weight, sex, viral serologies, or apheresis parameters. Donors with a higher proportion of CD8 cells donated grafts with higher CD8 cell dose, but the presence of higher CD4 counts negated this. Screening for the relative proportions of CD8 and CD4 cells identifies donors most likely to mobilize CD8hi grafts.
“This is also a practical consideration because the assay is rapid, is routinely performed in clinical laboratories, and can easily be done at the time of confirmatory HLA [human leukocyte antigen] typing,” the authors noted. Since the relationship between CD8 dose and survival is linear, the higher the dose the better, even if it is below the cutoff.
Previous studies showed conflicting results regarding the outcome of RIC transplantation with younger unrelated donors versus older sibling donors. Donor age inversely correlates with CD8 cell dose, and the results of this study showed that overall survival was significantly better with younger unrelated donors with a CD8hi graft, compared with older sibling donors (P = .03). No such benefit was observed with younger unrelated donors with CD8lo grafts (P = .28), indicating the benefit may rely on CD8 cell dose.
The study evaluated 200 patients with hematologic malignancy who underwent allo-HSCT with fludarabine plus busulfan conditioning from 2007 to 2014 at the Abramson Cancer Center, University of Pennsylvania in Philadelphia. The cumulative relapse incidence was 42% at 1 year and 47% at 5 years. The most common diseases in the cohort were acute myeloid leukemia, myelodysplastic syndrome, and non-Hodgkin lymphoma.
High CD8 dose was associated with an increased, but nonsignificant risk of chronic graft-versus-host disease (GVHD); the risk for nonrelapse mortality was not associated with cell doses.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: High CD8 cell dose in peripheral blood stem cell grafts was associated with reduced risk of relapse and increased survival in allogeneic stem cell transplantation with reduced-intensity conditioning.
Major finding: With a cumulative relapse incidence of 42% at 1 year, CD8 cell dose was an independent predictor of relapse (aHR, 0.43; P = .009), relapse-free survival (0.50; P = .006), and overall survival (0.57; P = .04).
Data source: The retrospective, single-institution study evaluated 200 patients who underwent peripheral blood alloHSCT with fludarabine plus busulfan conditioning from 2007 to 2014. Analysis of graft T-cell content used 21 randomly selected donors.
Disclosures: Dr. Reshef reported having consulting or advisory roles with Celgene, Spectrum Pharmaceuticals, Tobira Therapeutics, and Teva Pharmaceutical Industries. Many of his coauthors reported having financial relationships with industry.
Chemotherapy and stem-cell transplantation combination appears safe
In a population of patients with hematologic malignancies who refuse blood product transfusions, high-dose chemotherapy (HDC) followed by autologous stem-cell transplantation (ASCT) in the absence of hematopoietic support was shown to be relatively safe, according to a report published online April 13 in the Journal of Clinical Oncology.
From May of 1996 to March of 2014 at Pennsylvania Hospital, 125 Jehovah’s Witness patients with lymphoma (n = 55), multiple myeloma (n = 68), or amyloidosis (n = 2) were treated with HDC and ASCT without transfusion through the use of basic blood management techniques. These techniques included priming pretransplantation hemoglobin with erythropoiesis stimulating agents and intravenous iron, limiting iatrogenic blood loss by minimizing phlebotomy, and controlling or preventing bleeding with hemostatic agents, according to Dr. Patricia Ford and her colleagues at the hospital.
They described the low incidence of bleeding even in the absence of prophylactic platelet transfusions, which, they noted, challenges current American Society of Clinical Oncology guidelines that recommend transfusions at platelet counts less than 10 x 103/mcL. “The absence of major bleeding events observed at platelet counts greater than 5 x 103/mcL … suggests that a transfusion threshold trigger of 5 x 103/mcL may be appropriate in a select patient population,” they wrote (J. Clin. Oncol. 2015 April 13 [doi: 10.1200/JCO.2014.57.9912]).
Among the patients treated with HDC and ASCT, those with multiple myeloma (n = 68) received melphalan 200 mg/m2,and those with lymphoma (n = 55) received carmustine 300mg/m2 day 1, cyclophosphamide 1,500 mg/m2 days 2-5, and VP16 700 mg/m2 per day on days 2-4.
At 100 days post transplantation, 115 patients (92%) were still alive. Treatment-related mortality due to anemia, sepsis, pancytopenia, or cardiac events occurred in six patients (4.8%).
Out of 18 bleeding episodes, 2 were major (one grade 4 hemorrhagic temporal infarction with retinal hemorrhages and one grade 3 GI bleed) and 16 were minor. There were no bleeding-associated fatalities.
Cardiac complications occurred at an unexpectedly high rate of 32% (40 patients) and resulted in three treatment-related deaths. Subsequently, all candidates older than 50 years or at risk for cardiac disease were required to undergo cardiac consultation prior to transplantation. Given the cardiovascular risk associated with this population, in addition to ECHO testing, stress testing in patients with suspected coronary artery disease is recommended, the researchers wrote.
On the basis of the observed low mortality and morbidity, Dr. Ford and her associates suggested that HDC followed by ASCT be offered to certain patients who refuse or who have medical contraindications to transfusions, stating that simple blood management strategies were an effective alternative in select patients.
In a population of patients with hematologic malignancies who refuse blood product transfusions, high-dose chemotherapy (HDC) followed by autologous stem-cell transplantation (ASCT) in the absence of hematopoietic support was shown to be relatively safe, according to a report published online April 13 in the Journal of Clinical Oncology.
From May of 1996 to March of 2014 at Pennsylvania Hospital, 125 Jehovah’s Witness patients with lymphoma (n = 55), multiple myeloma (n = 68), or amyloidosis (n = 2) were treated with HDC and ASCT without transfusion through the use of basic blood management techniques. These techniques included priming pretransplantation hemoglobin with erythropoiesis stimulating agents and intravenous iron, limiting iatrogenic blood loss by minimizing phlebotomy, and controlling or preventing bleeding with hemostatic agents, according to Dr. Patricia Ford and her colleagues at the hospital.
They described the low incidence of bleeding even in the absence of prophylactic platelet transfusions, which, they noted, challenges current American Society of Clinical Oncology guidelines that recommend transfusions at platelet counts less than 10 x 103/mcL. “The absence of major bleeding events observed at platelet counts greater than 5 x 103/mcL … suggests that a transfusion threshold trigger of 5 x 103/mcL may be appropriate in a select patient population,” they wrote (J. Clin. Oncol. 2015 April 13 [doi: 10.1200/JCO.2014.57.9912]).
Among the patients treated with HDC and ASCT, those with multiple myeloma (n = 68) received melphalan 200 mg/m2,and those with lymphoma (n = 55) received carmustine 300mg/m2 day 1, cyclophosphamide 1,500 mg/m2 days 2-5, and VP16 700 mg/m2 per day on days 2-4.
At 100 days post transplantation, 115 patients (92%) were still alive. Treatment-related mortality due to anemia, sepsis, pancytopenia, or cardiac events occurred in six patients (4.8%).
Out of 18 bleeding episodes, 2 were major (one grade 4 hemorrhagic temporal infarction with retinal hemorrhages and one grade 3 GI bleed) and 16 were minor. There were no bleeding-associated fatalities.
Cardiac complications occurred at an unexpectedly high rate of 32% (40 patients) and resulted in three treatment-related deaths. Subsequently, all candidates older than 50 years or at risk for cardiac disease were required to undergo cardiac consultation prior to transplantation. Given the cardiovascular risk associated with this population, in addition to ECHO testing, stress testing in patients with suspected coronary artery disease is recommended, the researchers wrote.
On the basis of the observed low mortality and morbidity, Dr. Ford and her associates suggested that HDC followed by ASCT be offered to certain patients who refuse or who have medical contraindications to transfusions, stating that simple blood management strategies were an effective alternative in select patients.
In a population of patients with hematologic malignancies who refuse blood product transfusions, high-dose chemotherapy (HDC) followed by autologous stem-cell transplantation (ASCT) in the absence of hematopoietic support was shown to be relatively safe, according to a report published online April 13 in the Journal of Clinical Oncology.
From May of 1996 to March of 2014 at Pennsylvania Hospital, 125 Jehovah’s Witness patients with lymphoma (n = 55), multiple myeloma (n = 68), or amyloidosis (n = 2) were treated with HDC and ASCT without transfusion through the use of basic blood management techniques. These techniques included priming pretransplantation hemoglobin with erythropoiesis stimulating agents and intravenous iron, limiting iatrogenic blood loss by minimizing phlebotomy, and controlling or preventing bleeding with hemostatic agents, according to Dr. Patricia Ford and her colleagues at the hospital.
They described the low incidence of bleeding even in the absence of prophylactic platelet transfusions, which, they noted, challenges current American Society of Clinical Oncology guidelines that recommend transfusions at platelet counts less than 10 x 103/mcL. “The absence of major bleeding events observed at platelet counts greater than 5 x 103/mcL … suggests that a transfusion threshold trigger of 5 x 103/mcL may be appropriate in a select patient population,” they wrote (J. Clin. Oncol. 2015 April 13 [doi: 10.1200/JCO.2014.57.9912]).
Among the patients treated with HDC and ASCT, those with multiple myeloma (n = 68) received melphalan 200 mg/m2,and those with lymphoma (n = 55) received carmustine 300mg/m2 day 1, cyclophosphamide 1,500 mg/m2 days 2-5, and VP16 700 mg/m2 per day on days 2-4.
At 100 days post transplantation, 115 patients (92%) were still alive. Treatment-related mortality due to anemia, sepsis, pancytopenia, or cardiac events occurred in six patients (4.8%).
Out of 18 bleeding episodes, 2 were major (one grade 4 hemorrhagic temporal infarction with retinal hemorrhages and one grade 3 GI bleed) and 16 were minor. There were no bleeding-associated fatalities.
Cardiac complications occurred at an unexpectedly high rate of 32% (40 patients) and resulted in three treatment-related deaths. Subsequently, all candidates older than 50 years or at risk for cardiac disease were required to undergo cardiac consultation prior to transplantation. Given the cardiovascular risk associated with this population, in addition to ECHO testing, stress testing in patients with suspected coronary artery disease is recommended, the researchers wrote.
On the basis of the observed low mortality and morbidity, Dr. Ford and her associates suggested that HDC followed by ASCT be offered to certain patients who refuse or who have medical contraindications to transfusions, stating that simple blood management strategies were an effective alternative in select patients.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: In Jehovah’s Witness patients with relapsed lymphoma or multiple myeloma, high-dose chemotherapy (HDC) followed by autologous stem-cell transplantation (ASCT) was safely performed without hematopoietic support.
Major finding: At 100 days post transplantation, 115 patients (92%) were still alive. Treatment-related mortality due to anemia, sepsis, pancytopenia, or cardiac events occurred in six patients (4.8%). Cardiac complications occurred in 40 patients (32%). There were 18 bleeding episodes (2 major, 16 minor), and no bleeding-associated mortality.
Data source: A study of 125 Jehovah’s Witness patients with non-Hodgkin’s lymphoma (n = 36), Hodgkin’s lymphoma (n = 19), multiple myeloma (n = 68), and amyloidosis (n = 2) who were treated with HDC and ASCT without transfusion support.
Disclosures: Dr. Ford and coauthors reported having no disclosures.
Chronic lymphocytic leukemia prognosis relatively good after transplantation failure
Unlike for those with acute leukemia, patients with chronic lymphocytic leukemia who had disease progression after undergoing transplantation had a relatively good prognosis, with 2- and 5-year overall survival rates of 67% and 38%, investigators reported online April 6 in the Journal of Clinical Oncology.*
Patients with chronic lymphocytic leukemia (CLL) who experienced acute or chronic graft-versus-host disease (GVHD) had significantly longer overall survival (OS) than those who did not have GVHD (P = .04 and P = .05, respectively). “Nearly half our patients with active CLL after transplantation had chronic GVHD, and the association of chronic GVHD with achieving cure and its power to predict OS among patients for whom transplantation failed suggests that the GVL (graft-versus-leukemia) effect contributes to prolonged survival even in patients with a high burden of disease,” wrote Dr. Uri Rozovski and associates at the University of Texas MD Anderson Cancer Center, Houston (J. Clin. Oncol. 2015 Apr. 6 [doi:10.1200/JCO.2014.58.6750]).
A matched-pair analysis showed that patients who underwent allogeneic stem cell transplant (SCT) about the same time and did not relapse also had higher rates of acute and chronic GVHD (P = .004 and P = .011, respectively).
The retrospective review of the Bone Marrow Transplantation Program database identified 358 patients with CLL or RT who underwent SCT from 1998 to 2011. The study evaluated 72 patients who had disease progression at a median 74 months after SCT, most of whom received one to eight lines of treatment after relapse and had a median OS of almost 3 years from the time of progression. Multivariate analysis showed that low hemoglobin levels and the presence of Richter’s transformation (RT) were associated with shorter OS; chronic GVHD and response to the first post-SCT treatment predicted longer OS.
Patients with RT had a worse prognosis, with a median OS of 15 months (95% confidence interval, 2-28 months) and 2- and 5-year survival rates of 36% and 0%. Transplantation carried a significant risk for transformation: 16 (30%) patients with CLL developed RT after allogeneic SCT. Conversely, four patients with RT developed CLL after transplantation.
The authors note that even in patients who did not maintain a durable response, SCT was beneficial. The study cohort received a variety of salvage treatments, and patients who received ibrutinib responded well. “Because of the favorable outcomes with ibrutinib in relapsed/refractory CLL, we believe that ibrutinib might have a role in the treatment of disease progression following transplantation failure,” they wrote.
*Correction, 4/8/2015: A previous version of this article misstated the type of leukemia referenced in the study.
Unlike for those with acute leukemia, patients with chronic lymphocytic leukemia who had disease progression after undergoing transplantation had a relatively good prognosis, with 2- and 5-year overall survival rates of 67% and 38%, investigators reported online April 6 in the Journal of Clinical Oncology.*
Patients with chronic lymphocytic leukemia (CLL) who experienced acute or chronic graft-versus-host disease (GVHD) had significantly longer overall survival (OS) than those who did not have GVHD (P = .04 and P = .05, respectively). “Nearly half our patients with active CLL after transplantation had chronic GVHD, and the association of chronic GVHD with achieving cure and its power to predict OS among patients for whom transplantation failed suggests that the GVL (graft-versus-leukemia) effect contributes to prolonged survival even in patients with a high burden of disease,” wrote Dr. Uri Rozovski and associates at the University of Texas MD Anderson Cancer Center, Houston (J. Clin. Oncol. 2015 Apr. 6 [doi:10.1200/JCO.2014.58.6750]).
A matched-pair analysis showed that patients who underwent allogeneic stem cell transplant (SCT) about the same time and did not relapse also had higher rates of acute and chronic GVHD (P = .004 and P = .011, respectively).
The retrospective review of the Bone Marrow Transplantation Program database identified 358 patients with CLL or RT who underwent SCT from 1998 to 2011. The study evaluated 72 patients who had disease progression at a median 74 months after SCT, most of whom received one to eight lines of treatment after relapse and had a median OS of almost 3 years from the time of progression. Multivariate analysis showed that low hemoglobin levels and the presence of Richter’s transformation (RT) were associated with shorter OS; chronic GVHD and response to the first post-SCT treatment predicted longer OS.
Patients with RT had a worse prognosis, with a median OS of 15 months (95% confidence interval, 2-28 months) and 2- and 5-year survival rates of 36% and 0%. Transplantation carried a significant risk for transformation: 16 (30%) patients with CLL developed RT after allogeneic SCT. Conversely, four patients with RT developed CLL after transplantation.
The authors note that even in patients who did not maintain a durable response, SCT was beneficial. The study cohort received a variety of salvage treatments, and patients who received ibrutinib responded well. “Because of the favorable outcomes with ibrutinib in relapsed/refractory CLL, we believe that ibrutinib might have a role in the treatment of disease progression following transplantation failure,” they wrote.
*Correction, 4/8/2015: A previous version of this article misstated the type of leukemia referenced in the study.
Unlike for those with acute leukemia, patients with chronic lymphocytic leukemia who had disease progression after undergoing transplantation had a relatively good prognosis, with 2- and 5-year overall survival rates of 67% and 38%, investigators reported online April 6 in the Journal of Clinical Oncology.*
Patients with chronic lymphocytic leukemia (CLL) who experienced acute or chronic graft-versus-host disease (GVHD) had significantly longer overall survival (OS) than those who did not have GVHD (P = .04 and P = .05, respectively). “Nearly half our patients with active CLL after transplantation had chronic GVHD, and the association of chronic GVHD with achieving cure and its power to predict OS among patients for whom transplantation failed suggests that the GVL (graft-versus-leukemia) effect contributes to prolonged survival even in patients with a high burden of disease,” wrote Dr. Uri Rozovski and associates at the University of Texas MD Anderson Cancer Center, Houston (J. Clin. Oncol. 2015 Apr. 6 [doi:10.1200/JCO.2014.58.6750]).
A matched-pair analysis showed that patients who underwent allogeneic stem cell transplant (SCT) about the same time and did not relapse also had higher rates of acute and chronic GVHD (P = .004 and P = .011, respectively).
The retrospective review of the Bone Marrow Transplantation Program database identified 358 patients with CLL or RT who underwent SCT from 1998 to 2011. The study evaluated 72 patients who had disease progression at a median 74 months after SCT, most of whom received one to eight lines of treatment after relapse and had a median OS of almost 3 years from the time of progression. Multivariate analysis showed that low hemoglobin levels and the presence of Richter’s transformation (RT) were associated with shorter OS; chronic GVHD and response to the first post-SCT treatment predicted longer OS.
Patients with RT had a worse prognosis, with a median OS of 15 months (95% confidence interval, 2-28 months) and 2- and 5-year survival rates of 36% and 0%. Transplantation carried a significant risk for transformation: 16 (30%) patients with CLL developed RT after allogeneic SCT. Conversely, four patients with RT developed CLL after transplantation.
The authors note that even in patients who did not maintain a durable response, SCT was beneficial. The study cohort received a variety of salvage treatments, and patients who received ibrutinib responded well. “Because of the favorable outcomes with ibrutinib in relapsed/refractory CLL, we believe that ibrutinib might have a role in the treatment of disease progression following transplantation failure,” they wrote.
*Correction, 4/8/2015: A previous version of this article misstated the type of leukemia referenced in the study.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The prognosis for patients with chronic lymphocytic* leukemia who have undergone failed stem cell transplantation (SCT) is relatively good.
Major finding: From the time of progression after SCT, median OS was 36 months (95% CI, 24-48) for patients with CLL, and 38% survived 5 or more years.
Data source: The retrospective database review identified 72 patients with CLL or Richter’s transformation who underwent allogenic SCT from 1998 to 2011 and progressed after transplantation.
Disclosures: Dr. Rozovski reported having no disclosures. Two of the coauthors reported ties to several industry sources.
CAR-T cell therapy rolls on in pediatric ALL
SAN FRANCISCO – CAR-T cell therapy drove relapsed, refractory acute lymphoblastic leukemia into complete remission in 92% or all but three of 39 children in a phase I/IIa study.
Complete responses were seen within 28 days of receiving a chimeric antigen receptor (CAR)-T cell infusion and have persisted in 15 patients for a year or more, Dr. Stephan A. Grupp reported at the annual meeting of the American Society of Hematology.
Ten relapses have occurred during follow-up of up to 31 months (median 6 months). Half were due to disappearance of the T cells, resulting in CD19-positive relapse, and half were related to antigen escape, resulting in CD19-negative relapse.
Five of the relapsed patients died. No events have been seen in patients who remain in remission after 12 months.
Importantly, CAR-T cell therapy was not used as a bridge to transplant, with only three patients subsequently going on to stem cell transplantation, Dr. Grupp, a pediatric oncologist at the Children’s Hospital of Philadelphia (CHOP) and professor of pediatrics at the University of Pennsylvania, said during a press briefing.
When asked whether CAR-T therapy could be a replacement for transplantation in the future, Dr. Grupp responded, “That would be my fondest hope. We’re not quite there yet, but we’re a lot closer than we used to be.”
The novel immunotherapy first hit the front pages in 2011 after researchers at CHOP and the University of Pennsylvania reported breakthrough results in a handful of children treated with CTL019 cells. T cells are collected from the patient and then genetically reengineered with a CAR directed against tumor B cells expressing the CD19 surface antigen.
More than 130 patients have now been treated by the Pennsylvania team with the CTL019 approach, which received breakthrough therapy status from the Food and Drug Administration in July 2014.
The updated results presented by Dr. Grupp build on those reported earlier this year (N. Engl. J. Med. 2014;371:1507-17) and involve 39 children and young adults. This includes the first 30 pediatric patients with relapsed, refractory ALL treated in the pilot trial. Their median age was 10 years and most were refractory to multiple prior therapies.
At 6 months, the duration of response was 76% and event-free survival was 70%.
The ability of patients to retain their T cells for 6 months or longer was observed in about two-thirds of patients and “is a key point in maintaining remission in these patients,” Dr. Grupp said.
Response rates were independent of disease burden at the time of infusion: 82% response in patients with more than 50% leukemia blast cells, 88% in those with more than 5% blasts, and 100% in those with 0.01%-5% blasts or less than 0.01% blasts.
Patients with higher baseline disease burden (more than 50% blasts), however, were significantly more likely to experience severe cytokine release syndrome (CRS), compared with those with lower disease burden (P < .002).
CRS has been seen across CAR-T cell studies, but there are insufficient data to determine whether this toxicity differs between adult and pediatric patients.
“The key to the cytokine release syndrome, and I believe this carries across platforms and actually may also apply to blinatumomab, is the amplification of the macrophage system through interleukin-6,” Dr. Grupp explained. “This is a classical feedback loop that is actually druggable” using the IL-6 receptor blocker tocilizumab (Actemra).
This strategy produced “remarkable control” of the CRS toxicity, with many of the severe CRS cases experiencing resolution within hours and all cases resolving within 2-3 days, he said.
B-cell aplasia was observed in all responding patients to date and was managed with intravenous immunoglobulin replacement therapy.
The two key questions for the future of CTL019 therapy are toxicity and the logistics of collecting a cell sample and sending it to a centralized manufacturing facility, Dr. Grupp said. This process has already been done on a small scale at CHOP because their cells are made at the University of Pennsylvania. Novartis, which licensed the technology, has built a cell-manufacturing facility and an ongoing phase II study is evaluating whether the technology can be safely rolled out to eight or nine pediatric centers across the country. An adult study will follow, he said.
SAN FRANCISCO – CAR-T cell therapy drove relapsed, refractory acute lymphoblastic leukemia into complete remission in 92% or all but three of 39 children in a phase I/IIa study.
Complete responses were seen within 28 days of receiving a chimeric antigen receptor (CAR)-T cell infusion and have persisted in 15 patients for a year or more, Dr. Stephan A. Grupp reported at the annual meeting of the American Society of Hematology.
Ten relapses have occurred during follow-up of up to 31 months (median 6 months). Half were due to disappearance of the T cells, resulting in CD19-positive relapse, and half were related to antigen escape, resulting in CD19-negative relapse.
Five of the relapsed patients died. No events have been seen in patients who remain in remission after 12 months.
Importantly, CAR-T cell therapy was not used as a bridge to transplant, with only three patients subsequently going on to stem cell transplantation, Dr. Grupp, a pediatric oncologist at the Children’s Hospital of Philadelphia (CHOP) and professor of pediatrics at the University of Pennsylvania, said during a press briefing.
When asked whether CAR-T therapy could be a replacement for transplantation in the future, Dr. Grupp responded, “That would be my fondest hope. We’re not quite there yet, but we’re a lot closer than we used to be.”
The novel immunotherapy first hit the front pages in 2011 after researchers at CHOP and the University of Pennsylvania reported breakthrough results in a handful of children treated with CTL019 cells. T cells are collected from the patient and then genetically reengineered with a CAR directed against tumor B cells expressing the CD19 surface antigen.
More than 130 patients have now been treated by the Pennsylvania team with the CTL019 approach, which received breakthrough therapy status from the Food and Drug Administration in July 2014.
The updated results presented by Dr. Grupp build on those reported earlier this year (N. Engl. J. Med. 2014;371:1507-17) and involve 39 children and young adults. This includes the first 30 pediatric patients with relapsed, refractory ALL treated in the pilot trial. Their median age was 10 years and most were refractory to multiple prior therapies.
At 6 months, the duration of response was 76% and event-free survival was 70%.
The ability of patients to retain their T cells for 6 months or longer was observed in about two-thirds of patients and “is a key point in maintaining remission in these patients,” Dr. Grupp said.
Response rates were independent of disease burden at the time of infusion: 82% response in patients with more than 50% leukemia blast cells, 88% in those with more than 5% blasts, and 100% in those with 0.01%-5% blasts or less than 0.01% blasts.
Patients with higher baseline disease burden (more than 50% blasts), however, were significantly more likely to experience severe cytokine release syndrome (CRS), compared with those with lower disease burden (P < .002).
CRS has been seen across CAR-T cell studies, but there are insufficient data to determine whether this toxicity differs between adult and pediatric patients.
“The key to the cytokine release syndrome, and I believe this carries across platforms and actually may also apply to blinatumomab, is the amplification of the macrophage system through interleukin-6,” Dr. Grupp explained. “This is a classical feedback loop that is actually druggable” using the IL-6 receptor blocker tocilizumab (Actemra).
This strategy produced “remarkable control” of the CRS toxicity, with many of the severe CRS cases experiencing resolution within hours and all cases resolving within 2-3 days, he said.
B-cell aplasia was observed in all responding patients to date and was managed with intravenous immunoglobulin replacement therapy.
The two key questions for the future of CTL019 therapy are toxicity and the logistics of collecting a cell sample and sending it to a centralized manufacturing facility, Dr. Grupp said. This process has already been done on a small scale at CHOP because their cells are made at the University of Pennsylvania. Novartis, which licensed the technology, has built a cell-manufacturing facility and an ongoing phase II study is evaluating whether the technology can be safely rolled out to eight or nine pediatric centers across the country. An adult study will follow, he said.
SAN FRANCISCO – CAR-T cell therapy drove relapsed, refractory acute lymphoblastic leukemia into complete remission in 92% or all but three of 39 children in a phase I/IIa study.
Complete responses were seen within 28 days of receiving a chimeric antigen receptor (CAR)-T cell infusion and have persisted in 15 patients for a year or more, Dr. Stephan A. Grupp reported at the annual meeting of the American Society of Hematology.
Ten relapses have occurred during follow-up of up to 31 months (median 6 months). Half were due to disappearance of the T cells, resulting in CD19-positive relapse, and half were related to antigen escape, resulting in CD19-negative relapse.
Five of the relapsed patients died. No events have been seen in patients who remain in remission after 12 months.
Importantly, CAR-T cell therapy was not used as a bridge to transplant, with only three patients subsequently going on to stem cell transplantation, Dr. Grupp, a pediatric oncologist at the Children’s Hospital of Philadelphia (CHOP) and professor of pediatrics at the University of Pennsylvania, said during a press briefing.
When asked whether CAR-T therapy could be a replacement for transplantation in the future, Dr. Grupp responded, “That would be my fondest hope. We’re not quite there yet, but we’re a lot closer than we used to be.”
The novel immunotherapy first hit the front pages in 2011 after researchers at CHOP and the University of Pennsylvania reported breakthrough results in a handful of children treated with CTL019 cells. T cells are collected from the patient and then genetically reengineered with a CAR directed against tumor B cells expressing the CD19 surface antigen.
More than 130 patients have now been treated by the Pennsylvania team with the CTL019 approach, which received breakthrough therapy status from the Food and Drug Administration in July 2014.
The updated results presented by Dr. Grupp build on those reported earlier this year (N. Engl. J. Med. 2014;371:1507-17) and involve 39 children and young adults. This includes the first 30 pediatric patients with relapsed, refractory ALL treated in the pilot trial. Their median age was 10 years and most were refractory to multiple prior therapies.
At 6 months, the duration of response was 76% and event-free survival was 70%.
The ability of patients to retain their T cells for 6 months or longer was observed in about two-thirds of patients and “is a key point in maintaining remission in these patients,” Dr. Grupp said.
Response rates were independent of disease burden at the time of infusion: 82% response in patients with more than 50% leukemia blast cells, 88% in those with more than 5% blasts, and 100% in those with 0.01%-5% blasts or less than 0.01% blasts.
Patients with higher baseline disease burden (more than 50% blasts), however, were significantly more likely to experience severe cytokine release syndrome (CRS), compared with those with lower disease burden (P < .002).
CRS has been seen across CAR-T cell studies, but there are insufficient data to determine whether this toxicity differs between adult and pediatric patients.
“The key to the cytokine release syndrome, and I believe this carries across platforms and actually may also apply to blinatumomab, is the amplification of the macrophage system through interleukin-6,” Dr. Grupp explained. “This is a classical feedback loop that is actually druggable” using the IL-6 receptor blocker tocilizumab (Actemra).
This strategy produced “remarkable control” of the CRS toxicity, with many of the severe CRS cases experiencing resolution within hours and all cases resolving within 2-3 days, he said.
B-cell aplasia was observed in all responding patients to date and was managed with intravenous immunoglobulin replacement therapy.
The two key questions for the future of CTL019 therapy are toxicity and the logistics of collecting a cell sample and sending it to a centralized manufacturing facility, Dr. Grupp said. This process has already been done on a small scale at CHOP because their cells are made at the University of Pennsylvania. Novartis, which licensed the technology, has built a cell-manufacturing facility and an ongoing phase II study is evaluating whether the technology can be safely rolled out to eight or nine pediatric centers across the country. An adult study will follow, he said.
AT ASH 2014
Key clinical point: CAR-T cell therapy continues to provide durable responses in early studies of children with refractory ALL.
Major finding: Complete remission occurred in 36 of 39 patients (92%) treated with CAR-T cell therapy.
Data source: Phase I/IIa a study in 39 children and young adults with relapsed, refractory acute lymphoblastic leukemia.
Disclosures: The authors reported financial ties with Novartis, the study sponsor.