User login
The Surfside tragedy: A call for healing the healers
The mental health toll from the Surfside, Fla., Champlain Tower collapse will be felt by our patients for years to come. As mental health professionals in Miami-Dade County, it has been difficult to deal with the catastrophe layered on the escalating COVID-19 crisis.
With each passing day after the June 24 incident, we all learned who the 98 victims were. In session after session, the enormous impact of this unfathomable tragedy unfolded. Some mental health care professionals were directly affected with the loss of family members; some lost patients, and a large number of our patients lost someone or knew someone who lost someone. It was reminiscent of our work during the COVID-19 crisis when we found that we were dealing with the same stressors as those of our patients. As it was said then, we were all in the same storm – just in very different boats.
It was heartening to see how many colleagues rushed to the site of the building where family waiting areas were established. So many professionals wanted to assist that some had to be turned away.
The days right after the collapse were agonizing for all as we waited and hoped for survivors to be found. Search teams from across the United States and from Mexico and Israel – specifically, Israeli Defense Forces personnel with experience conducting operations in the wake of earthquakes in both Haiti and Nepal, took on the dangerous work. When no one was recovered after the first day, hope faded, and after 10 days, the search and rescue efforts turned to search and recovery. We were indeed a county and community in mourning.
According to Lina Haji, PsyD, GIA Miami, in addition to the direct impact of loss, clinicians who engaged in crisis response and bereavement counseling with those affected by the Surfside tragedy were subjected to vicarious trauma. Mental health care providers in the Miami area not only experienced the direct effect of this tragedy but have been hearing details and harrowing stories about the unimaginable experiences their patients endured over those critical weeks. Vicarious trauma can result in our own symptoms, compassion fatigue, or burnout as clinicians. This resulted in a call for mental health providers to come to the aid of their fellow colleagues.
So, on the 1-month anniversary of the initial collapse, at the urging of Patricia Stauber, RN, LCSW, a clinician with more than 30 years’ experience in providing grief counseling in hospital and private practice settings; Antonello Bonci, MD, the founder of GIA Miami; Charlotte Tomic, director of public relations for the Institute for the Study of Global Antisemitism; and I cohosted what we hope will be several Mental Health Appreciation retreats. Our goal was to create a space to focus on healing the healers. We had hoped to hold an in-person event, but at the last moment we opted for a Zoom-based event because COVID-19 cases were rising rapidly again.
Working on the front lines
Cassie Feldman, PsyD, a licensed clinical psychologist with extensive experience working with grief, loss, end of life, and responding to trauma-related consults, reflected on her experience responding to the collapse in the earliest days – first independently at the request of community religious leaders and then as part of CADENA Foundation, a nonprofit organization dedicated to rescue, humanitarian aid, and disaster response and prevention worldwide.
Dr. Feldman worked alongside other mental health professionals, local Miami-Dade police and fire officials, and the domestic and international rescue teams (CADENA’s Go Team from Mexico and the Israeli Defense Force’s Search and Rescue Delegation), providing Psychological First Aid, crisis intervention, and disaster response to the victims’ families and survivors.
This initially was a 24-hour coverage effort, requiring Dr. Feldman and her colleagues to clear their schedules, and at times to work 18-hour shifts in the early days of the crisis to address the need for consistency and continuity. Their commitment was to show up for the victims’ families and survivors, fully embracing the chaos and the demands of the situation. She noted that the disaster brought out the best of her and her colleagues.
They divided and conquered the work, alongside clinicians from Jewish Community Services and Project Chai intervening acutely where possible, and coordinating long-term care plans for those survivors and members of the victims’ support networks in need of consistent care.
Dr. Feldman reflected on the notion that we have all been processing losses prior to this – loss of normalcy because of the pandemic, loss of people we loved as a result, other personal losses – and that this community tragedy is yet another loss to disentangle. It didn’t feel good or natural for her to passively absorb the news knowing she had both the skill set and capacity to take on an active supportive role. The first days at the community center were disorganized; it was hard to know who was who and what was what. She described parents crying out for their children and children longing for their parents. Individuals were so overcome with emotion that they grew faint. Friends and families flooded in but were unaware of how to be fully supportive. The level of trauma was so high that the only interventions that were absorbed were those that were nonverbal or that fully addressed practical needs. People were frightened and in a state of shock.
Day by day, more order ensued and the efforts became more coordinated, but it became apparent to her that the “family reunification center” was devoid of reunification. She and her colleagues’ primary role became aiding the police department in making death notifications to the families and being supportive of the victims’ families and their loved ones during and in between the formal briefings, where so many concerned family members and friends gathered and waited.
“As the days went on, things became more structured and predictable,” Dr. Feldman noted. “We continued to connect with the victims’ families and survivors, [listened to] their stories, shared meals with them, spent downtime with them, began to intimately know their loved ones, and all the barriers they were now facing. We became invested in them, their unique intricacies, and to care deeply for them like our own families and loved ones. Small talk and conversation morphed into silent embraces where spoken words weren’t necessary.”
Dr. Feldman said some of her earliest memories were visiting ICU patients alongside her father, a critical care and ICU physician. Her father taught her that nonverbal communication and connection can be offered to patients in the most poignant moments of suffering.
Her “nascent experiences in the ICU,” she said, taught her that “the most useful of interventions was just being with people in their pain and bearing witness at times when there were just no words.”
Dr. Feldman said that when many of her colleagues learned about the switch from rescue to recovery, the pull was to jump in their cars and drive to the hotel where the families were based to offer support.
The unity she witnessed – from the disparate clinicians who were virtual strangers before the incident but a team afterward, from the families and the community, and from the first responders and rescue teams – was inspiring, Dr. Feldman said.
“We were all forced to think beyond ourselves, push ourselves past our limits, and unify in a way that remedied this period in history of deep fragmentation,” she said.
Understanding the role of psychoneuroimmunology
In another presentation during the Zoom event, Ms. Stauber offered her insights about the importance of support among mental health clinicians.
She cited research on women with HIV showing that those who are part of a support group had a stronger immune response than those who were not.
Ms. Stauber said the impact of COVID-19 and its ramifications – including fear, grief over losing loved ones, isolation from friends and family, and interference/cessation of normal routines – has put an enormous strain on clinicians and clients. One of her clients had to take her mother to the emergency room – never to see her again. She continues to ask: “If I’d been there, could I have saved her?”
Another client whose husband died of COVID-19–related illness agonizes over not being able to be at her husband’s side, not being able to hold his hand, not being able to say goodbye.
She said other cultures are more accepting of suffering as a condition of life and the acknowledgment that our time on earth is limited.
The “quick fix for everything” society carries over to people’s grief, said Ms. Stauber. As a result, many find it difficult to appreciate how much time it takes to heal.
Normal uncomplicated grief can take approximately 2-3 years, she said. By then, the shock has been wearing off, the emotional roller coaster of loss is calming down, coping skills are strengthened, and life can once again be more fulfilling or meaningful. Complicated grief or grief with trauma takes much longer, said Ms. Stauber, who is a consultant with a national crisis and debriefing company providing trauma and bereavement support to Fortune 500 companies.
Trauma adds another complexity to loss. To begin to appreciate the rough road ahead, Ms. Stauber said, it is important to understand the basic challenges facing grieving people.
“This is where our profession may be needed; we are providing support for those suffering the immense pain of loss in a world that often has difficulty being present or patient with loss,” she said. “We are indeed providing an emotional life raft.”
Ultimately, self-care is critical, Ms. Stauber said. “Consider self-care a job requirement” to be successful. She also offered the following tips for self-care:
1. Share your own loss experience with a caring and nonjudgmental person.
2. Consider ongoing supervision and consultation with colleagues who understand the nature of your work.
3. Be willing to ask for help.
4. Be aware of risks and countertransference in our work.
5. Attend workshops.
6. Remember that you do not have to and cannot do it all by yourself – we absolutely need more grief and trauma trained therapists.
7. Involve yourself in activities outside of work that feed your soul and nourish your spirit.
8. Schedule play.
9. Develop a healthy self-care regimen to remain present doing this work.
10. Consider the benefits of exercise.
11. Enjoy the beauty and wonder of nature.
12. Consider yoga, meditation, spa retreats – such as Kripalu, Miraval, and Canyon Ranch.
13. Spend time with loving family and friends.
14. Adopt a pet.
15. Eat healthy foods; get plenty of rest.
16. Walk in the rain.
17. Listen to music.
18. Enjoy a relaxing bubble bath.
19. Sing, dance, and enjoy the blessings of this life.
20. Love yourself; you truly can be your own best friend.
To advocate on behalf of mental health for patients, we must do the same for mental health professionals. The retreat was well received, and we learned a lot from our speakers. After the program, we offered a 45-minute yoga class and then 30-minute sound bowl meditation. We plan to repeat the event in September to help our community deal with the ongoing stress of such overwhelming loss.
While our community will never be the same, we hope that, by coming together, we can all find a way to support one another and strive to help ourselves and others manage as we navigate yet another unprecedented crisis.
Dr. Ritvo, who has more than 30 years’ experience in psychiatry, practices telemedicine. She is author of “BeKindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). Dr. Ritvo has no disclosures.
The mental health toll from the Surfside, Fla., Champlain Tower collapse will be felt by our patients for years to come. As mental health professionals in Miami-Dade County, it has been difficult to deal with the catastrophe layered on the escalating COVID-19 crisis.
With each passing day after the June 24 incident, we all learned who the 98 victims were. In session after session, the enormous impact of this unfathomable tragedy unfolded. Some mental health care professionals were directly affected with the loss of family members; some lost patients, and a large number of our patients lost someone or knew someone who lost someone. It was reminiscent of our work during the COVID-19 crisis when we found that we were dealing with the same stressors as those of our patients. As it was said then, we were all in the same storm – just in very different boats.
It was heartening to see how many colleagues rushed to the site of the building where family waiting areas were established. So many professionals wanted to assist that some had to be turned away.
The days right after the collapse were agonizing for all as we waited and hoped for survivors to be found. Search teams from across the United States and from Mexico and Israel – specifically, Israeli Defense Forces personnel with experience conducting operations in the wake of earthquakes in both Haiti and Nepal, took on the dangerous work. When no one was recovered after the first day, hope faded, and after 10 days, the search and rescue efforts turned to search and recovery. We were indeed a county and community in mourning.
According to Lina Haji, PsyD, GIA Miami, in addition to the direct impact of loss, clinicians who engaged in crisis response and bereavement counseling with those affected by the Surfside tragedy were subjected to vicarious trauma. Mental health care providers in the Miami area not only experienced the direct effect of this tragedy but have been hearing details and harrowing stories about the unimaginable experiences their patients endured over those critical weeks. Vicarious trauma can result in our own symptoms, compassion fatigue, or burnout as clinicians. This resulted in a call for mental health providers to come to the aid of their fellow colleagues.
So, on the 1-month anniversary of the initial collapse, at the urging of Patricia Stauber, RN, LCSW, a clinician with more than 30 years’ experience in providing grief counseling in hospital and private practice settings; Antonello Bonci, MD, the founder of GIA Miami; Charlotte Tomic, director of public relations for the Institute for the Study of Global Antisemitism; and I cohosted what we hope will be several Mental Health Appreciation retreats. Our goal was to create a space to focus on healing the healers. We had hoped to hold an in-person event, but at the last moment we opted for a Zoom-based event because COVID-19 cases were rising rapidly again.
Working on the front lines
Cassie Feldman, PsyD, a licensed clinical psychologist with extensive experience working with grief, loss, end of life, and responding to trauma-related consults, reflected on her experience responding to the collapse in the earliest days – first independently at the request of community religious leaders and then as part of CADENA Foundation, a nonprofit organization dedicated to rescue, humanitarian aid, and disaster response and prevention worldwide.
Dr. Feldman worked alongside other mental health professionals, local Miami-Dade police and fire officials, and the domestic and international rescue teams (CADENA’s Go Team from Mexico and the Israeli Defense Force’s Search and Rescue Delegation), providing Psychological First Aid, crisis intervention, and disaster response to the victims’ families and survivors.
This initially was a 24-hour coverage effort, requiring Dr. Feldman and her colleagues to clear their schedules, and at times to work 18-hour shifts in the early days of the crisis to address the need for consistency and continuity. Their commitment was to show up for the victims’ families and survivors, fully embracing the chaos and the demands of the situation. She noted that the disaster brought out the best of her and her colleagues.
They divided and conquered the work, alongside clinicians from Jewish Community Services and Project Chai intervening acutely where possible, and coordinating long-term care plans for those survivors and members of the victims’ support networks in need of consistent care.
Dr. Feldman reflected on the notion that we have all been processing losses prior to this – loss of normalcy because of the pandemic, loss of people we loved as a result, other personal losses – and that this community tragedy is yet another loss to disentangle. It didn’t feel good or natural for her to passively absorb the news knowing she had both the skill set and capacity to take on an active supportive role. The first days at the community center were disorganized; it was hard to know who was who and what was what. She described parents crying out for their children and children longing for their parents. Individuals were so overcome with emotion that they grew faint. Friends and families flooded in but were unaware of how to be fully supportive. The level of trauma was so high that the only interventions that were absorbed were those that were nonverbal or that fully addressed practical needs. People were frightened and in a state of shock.
Day by day, more order ensued and the efforts became more coordinated, but it became apparent to her that the “family reunification center” was devoid of reunification. She and her colleagues’ primary role became aiding the police department in making death notifications to the families and being supportive of the victims’ families and their loved ones during and in between the formal briefings, where so many concerned family members and friends gathered and waited.
“As the days went on, things became more structured and predictable,” Dr. Feldman noted. “We continued to connect with the victims’ families and survivors, [listened to] their stories, shared meals with them, spent downtime with them, began to intimately know their loved ones, and all the barriers they were now facing. We became invested in them, their unique intricacies, and to care deeply for them like our own families and loved ones. Small talk and conversation morphed into silent embraces where spoken words weren’t necessary.”
Dr. Feldman said some of her earliest memories were visiting ICU patients alongside her father, a critical care and ICU physician. Her father taught her that nonverbal communication and connection can be offered to patients in the most poignant moments of suffering.
Her “nascent experiences in the ICU,” she said, taught her that “the most useful of interventions was just being with people in their pain and bearing witness at times when there were just no words.”
Dr. Feldman said that when many of her colleagues learned about the switch from rescue to recovery, the pull was to jump in their cars and drive to the hotel where the families were based to offer support.
The unity she witnessed – from the disparate clinicians who were virtual strangers before the incident but a team afterward, from the families and the community, and from the first responders and rescue teams – was inspiring, Dr. Feldman said.
“We were all forced to think beyond ourselves, push ourselves past our limits, and unify in a way that remedied this period in history of deep fragmentation,” she said.
Understanding the role of psychoneuroimmunology
In another presentation during the Zoom event, Ms. Stauber offered her insights about the importance of support among mental health clinicians.
She cited research on women with HIV showing that those who are part of a support group had a stronger immune response than those who were not.
Ms. Stauber said the impact of COVID-19 and its ramifications – including fear, grief over losing loved ones, isolation from friends and family, and interference/cessation of normal routines – has put an enormous strain on clinicians and clients. One of her clients had to take her mother to the emergency room – never to see her again. She continues to ask: “If I’d been there, could I have saved her?”
Another client whose husband died of COVID-19–related illness agonizes over not being able to be at her husband’s side, not being able to hold his hand, not being able to say goodbye.
She said other cultures are more accepting of suffering as a condition of life and the acknowledgment that our time on earth is limited.
The “quick fix for everything” society carries over to people’s grief, said Ms. Stauber. As a result, many find it difficult to appreciate how much time it takes to heal.
Normal uncomplicated grief can take approximately 2-3 years, she said. By then, the shock has been wearing off, the emotional roller coaster of loss is calming down, coping skills are strengthened, and life can once again be more fulfilling or meaningful. Complicated grief or grief with trauma takes much longer, said Ms. Stauber, who is a consultant with a national crisis and debriefing company providing trauma and bereavement support to Fortune 500 companies.
Trauma adds another complexity to loss. To begin to appreciate the rough road ahead, Ms. Stauber said, it is important to understand the basic challenges facing grieving people.
“This is where our profession may be needed; we are providing support for those suffering the immense pain of loss in a world that often has difficulty being present or patient with loss,” she said. “We are indeed providing an emotional life raft.”
Ultimately, self-care is critical, Ms. Stauber said. “Consider self-care a job requirement” to be successful. She also offered the following tips for self-care:
1. Share your own loss experience with a caring and nonjudgmental person.
2. Consider ongoing supervision and consultation with colleagues who understand the nature of your work.
3. Be willing to ask for help.
4. Be aware of risks and countertransference in our work.
5. Attend workshops.
6. Remember that you do not have to and cannot do it all by yourself – we absolutely need more grief and trauma trained therapists.
7. Involve yourself in activities outside of work that feed your soul and nourish your spirit.
8. Schedule play.
9. Develop a healthy self-care regimen to remain present doing this work.
10. Consider the benefits of exercise.
11. Enjoy the beauty and wonder of nature.
12. Consider yoga, meditation, spa retreats – such as Kripalu, Miraval, and Canyon Ranch.
13. Spend time with loving family and friends.
14. Adopt a pet.
15. Eat healthy foods; get plenty of rest.
16. Walk in the rain.
17. Listen to music.
18. Enjoy a relaxing bubble bath.
19. Sing, dance, and enjoy the blessings of this life.
20. Love yourself; you truly can be your own best friend.
To advocate on behalf of mental health for patients, we must do the same for mental health professionals. The retreat was well received, and we learned a lot from our speakers. After the program, we offered a 45-minute yoga class and then 30-minute sound bowl meditation. We plan to repeat the event in September to help our community deal with the ongoing stress of such overwhelming loss.
While our community will never be the same, we hope that, by coming together, we can all find a way to support one another and strive to help ourselves and others manage as we navigate yet another unprecedented crisis.
Dr. Ritvo, who has more than 30 years’ experience in psychiatry, practices telemedicine. She is author of “BeKindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). Dr. Ritvo has no disclosures.
The mental health toll from the Surfside, Fla., Champlain Tower collapse will be felt by our patients for years to come. As mental health professionals in Miami-Dade County, it has been difficult to deal with the catastrophe layered on the escalating COVID-19 crisis.
With each passing day after the June 24 incident, we all learned who the 98 victims were. In session after session, the enormous impact of this unfathomable tragedy unfolded. Some mental health care professionals were directly affected with the loss of family members; some lost patients, and a large number of our patients lost someone or knew someone who lost someone. It was reminiscent of our work during the COVID-19 crisis when we found that we were dealing with the same stressors as those of our patients. As it was said then, we were all in the same storm – just in very different boats.
It was heartening to see how many colleagues rushed to the site of the building where family waiting areas were established. So many professionals wanted to assist that some had to be turned away.
The days right after the collapse were agonizing for all as we waited and hoped for survivors to be found. Search teams from across the United States and from Mexico and Israel – specifically, Israeli Defense Forces personnel with experience conducting operations in the wake of earthquakes in both Haiti and Nepal, took on the dangerous work. When no one was recovered after the first day, hope faded, and after 10 days, the search and rescue efforts turned to search and recovery. We were indeed a county and community in mourning.
According to Lina Haji, PsyD, GIA Miami, in addition to the direct impact of loss, clinicians who engaged in crisis response and bereavement counseling with those affected by the Surfside tragedy were subjected to vicarious trauma. Mental health care providers in the Miami area not only experienced the direct effect of this tragedy but have been hearing details and harrowing stories about the unimaginable experiences their patients endured over those critical weeks. Vicarious trauma can result in our own symptoms, compassion fatigue, or burnout as clinicians. This resulted in a call for mental health providers to come to the aid of their fellow colleagues.
So, on the 1-month anniversary of the initial collapse, at the urging of Patricia Stauber, RN, LCSW, a clinician with more than 30 years’ experience in providing grief counseling in hospital and private practice settings; Antonello Bonci, MD, the founder of GIA Miami; Charlotte Tomic, director of public relations for the Institute for the Study of Global Antisemitism; and I cohosted what we hope will be several Mental Health Appreciation retreats. Our goal was to create a space to focus on healing the healers. We had hoped to hold an in-person event, but at the last moment we opted for a Zoom-based event because COVID-19 cases were rising rapidly again.
Working on the front lines
Cassie Feldman, PsyD, a licensed clinical psychologist with extensive experience working with grief, loss, end of life, and responding to trauma-related consults, reflected on her experience responding to the collapse in the earliest days – first independently at the request of community religious leaders and then as part of CADENA Foundation, a nonprofit organization dedicated to rescue, humanitarian aid, and disaster response and prevention worldwide.
Dr. Feldman worked alongside other mental health professionals, local Miami-Dade police and fire officials, and the domestic and international rescue teams (CADENA’s Go Team from Mexico and the Israeli Defense Force’s Search and Rescue Delegation), providing Psychological First Aid, crisis intervention, and disaster response to the victims’ families and survivors.
This initially was a 24-hour coverage effort, requiring Dr. Feldman and her colleagues to clear their schedules, and at times to work 18-hour shifts in the early days of the crisis to address the need for consistency and continuity. Their commitment was to show up for the victims’ families and survivors, fully embracing the chaos and the demands of the situation. She noted that the disaster brought out the best of her and her colleagues.
They divided and conquered the work, alongside clinicians from Jewish Community Services and Project Chai intervening acutely where possible, and coordinating long-term care plans for those survivors and members of the victims’ support networks in need of consistent care.
Dr. Feldman reflected on the notion that we have all been processing losses prior to this – loss of normalcy because of the pandemic, loss of people we loved as a result, other personal losses – and that this community tragedy is yet another loss to disentangle. It didn’t feel good or natural for her to passively absorb the news knowing she had both the skill set and capacity to take on an active supportive role. The first days at the community center were disorganized; it was hard to know who was who and what was what. She described parents crying out for their children and children longing for their parents. Individuals were so overcome with emotion that they grew faint. Friends and families flooded in but were unaware of how to be fully supportive. The level of trauma was so high that the only interventions that were absorbed were those that were nonverbal or that fully addressed practical needs. People were frightened and in a state of shock.
Day by day, more order ensued and the efforts became more coordinated, but it became apparent to her that the “family reunification center” was devoid of reunification. She and her colleagues’ primary role became aiding the police department in making death notifications to the families and being supportive of the victims’ families and their loved ones during and in between the formal briefings, where so many concerned family members and friends gathered and waited.
“As the days went on, things became more structured and predictable,” Dr. Feldman noted. “We continued to connect with the victims’ families and survivors, [listened to] their stories, shared meals with them, spent downtime with them, began to intimately know their loved ones, and all the barriers they were now facing. We became invested in them, their unique intricacies, and to care deeply for them like our own families and loved ones. Small talk and conversation morphed into silent embraces where spoken words weren’t necessary.”
Dr. Feldman said some of her earliest memories were visiting ICU patients alongside her father, a critical care and ICU physician. Her father taught her that nonverbal communication and connection can be offered to patients in the most poignant moments of suffering.
Her “nascent experiences in the ICU,” she said, taught her that “the most useful of interventions was just being with people in their pain and bearing witness at times when there were just no words.”
Dr. Feldman said that when many of her colleagues learned about the switch from rescue to recovery, the pull was to jump in their cars and drive to the hotel where the families were based to offer support.
The unity she witnessed – from the disparate clinicians who were virtual strangers before the incident but a team afterward, from the families and the community, and from the first responders and rescue teams – was inspiring, Dr. Feldman said.
“We were all forced to think beyond ourselves, push ourselves past our limits, and unify in a way that remedied this period in history of deep fragmentation,” she said.
Understanding the role of psychoneuroimmunology
In another presentation during the Zoom event, Ms. Stauber offered her insights about the importance of support among mental health clinicians.
She cited research on women with HIV showing that those who are part of a support group had a stronger immune response than those who were not.
Ms. Stauber said the impact of COVID-19 and its ramifications – including fear, grief over losing loved ones, isolation from friends and family, and interference/cessation of normal routines – has put an enormous strain on clinicians and clients. One of her clients had to take her mother to the emergency room – never to see her again. She continues to ask: “If I’d been there, could I have saved her?”
Another client whose husband died of COVID-19–related illness agonizes over not being able to be at her husband’s side, not being able to hold his hand, not being able to say goodbye.
She said other cultures are more accepting of suffering as a condition of life and the acknowledgment that our time on earth is limited.
The “quick fix for everything” society carries over to people’s grief, said Ms. Stauber. As a result, many find it difficult to appreciate how much time it takes to heal.
Normal uncomplicated grief can take approximately 2-3 years, she said. By then, the shock has been wearing off, the emotional roller coaster of loss is calming down, coping skills are strengthened, and life can once again be more fulfilling or meaningful. Complicated grief or grief with trauma takes much longer, said Ms. Stauber, who is a consultant with a national crisis and debriefing company providing trauma and bereavement support to Fortune 500 companies.
Trauma adds another complexity to loss. To begin to appreciate the rough road ahead, Ms. Stauber said, it is important to understand the basic challenges facing grieving people.
“This is where our profession may be needed; we are providing support for those suffering the immense pain of loss in a world that often has difficulty being present or patient with loss,” she said. “We are indeed providing an emotional life raft.”
Ultimately, self-care is critical, Ms. Stauber said. “Consider self-care a job requirement” to be successful. She also offered the following tips for self-care:
1. Share your own loss experience with a caring and nonjudgmental person.
2. Consider ongoing supervision and consultation with colleagues who understand the nature of your work.
3. Be willing to ask for help.
4. Be aware of risks and countertransference in our work.
5. Attend workshops.
6. Remember that you do not have to and cannot do it all by yourself – we absolutely need more grief and trauma trained therapists.
7. Involve yourself in activities outside of work that feed your soul and nourish your spirit.
8. Schedule play.
9. Develop a healthy self-care regimen to remain present doing this work.
10. Consider the benefits of exercise.
11. Enjoy the beauty and wonder of nature.
12. Consider yoga, meditation, spa retreats – such as Kripalu, Miraval, and Canyon Ranch.
13. Spend time with loving family and friends.
14. Adopt a pet.
15. Eat healthy foods; get plenty of rest.
16. Walk in the rain.
17. Listen to music.
18. Enjoy a relaxing bubble bath.
19. Sing, dance, and enjoy the blessings of this life.
20. Love yourself; you truly can be your own best friend.
To advocate on behalf of mental health for patients, we must do the same for mental health professionals. The retreat was well received, and we learned a lot from our speakers. After the program, we offered a 45-minute yoga class and then 30-minute sound bowl meditation. We plan to repeat the event in September to help our community deal with the ongoing stress of such overwhelming loss.
While our community will never be the same, we hope that, by coming together, we can all find a way to support one another and strive to help ourselves and others manage as we navigate yet another unprecedented crisis.
Dr. Ritvo, who has more than 30 years’ experience in psychiatry, practices telemedicine. She is author of “BeKindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). Dr. Ritvo has no disclosures.
Late-onset, treatment-resistant anxiety and depression
CASE Anxious and can’t sleep
Mr. A, age 41, presents to his primary care physician (PCP) with anxiety and insomnia. He describes having generalized anxiety with initial and middle insomnia, and says he is sleeping an average of 2 hours per night. He denies any other psychiatric symptoms. Mr. A has no significant psychiatric or medical history.
Mr. A is initiated on zolpidem tartrate, 12.5 mg every night at bedtime, and paroxetine, 20 mg every night at bedtime, for anxiety and insomnia, but these medications result in little to no improvement.
During a 4-month period, he is treated with trials of alprazolam, 0.5 mg every 8 hours as needed; diazepam 5 mg twice a day as needed; diphenhydramine, 50 mg at bedtime; and eszopiclone, 3 mg at bedtime. Despite these treatments, he experiences increased anxiety and insomnia, and develops depressive symptoms, including depressed mood, poor concentration, general malaise, extreme fatigue, a 15-pound unintentional weight loss, erectile dysfunction, and decreased libido. Mr. A denies having suicidal or homicidal ideations. Additionally, he typically goes to the gym approximately 3 times per week, and has noticed that the amount of weight he is able to lift has decreased, which is distressing. Previously, he had been able to lift 300 pounds, but now he can only lift 200 pounds.
[polldaddy:10891920]
The authors’ observations
Insomnia, anxiety, and depression are common chief complaints in medical settings. However, some psychiatric presentations may have an underlying medical etiology.
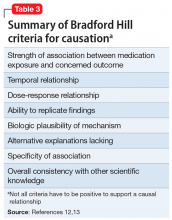
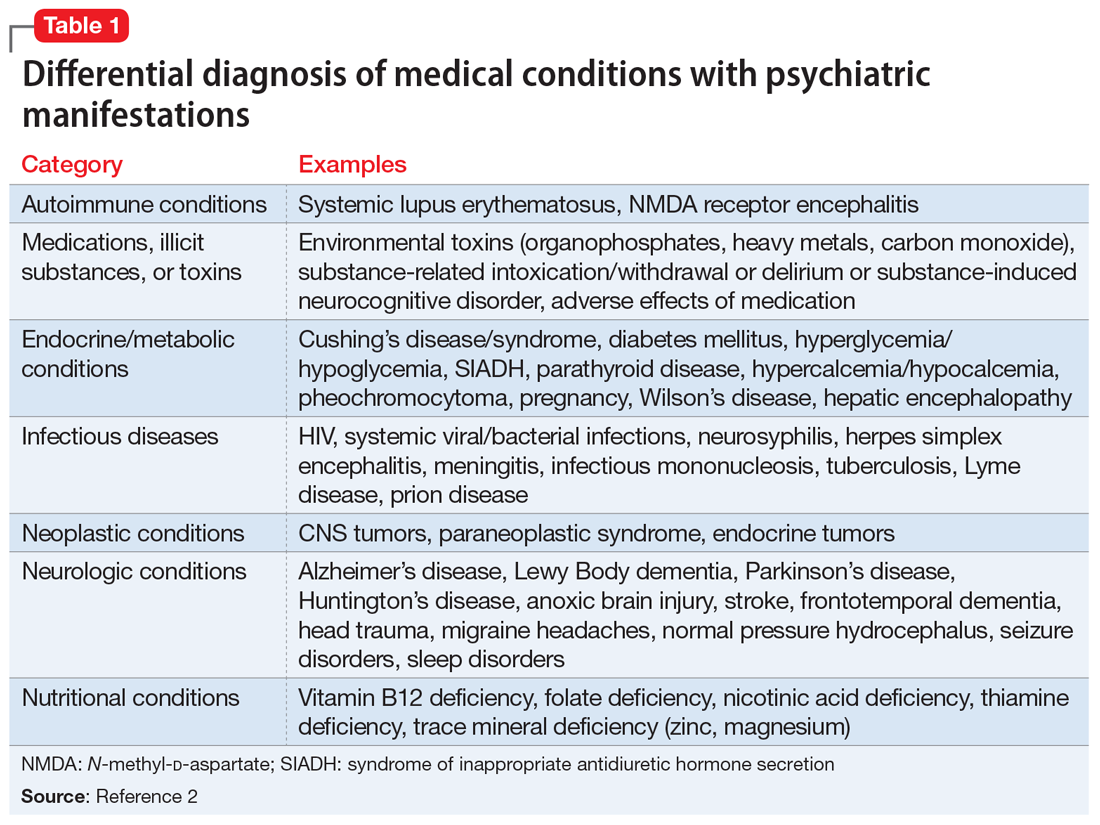
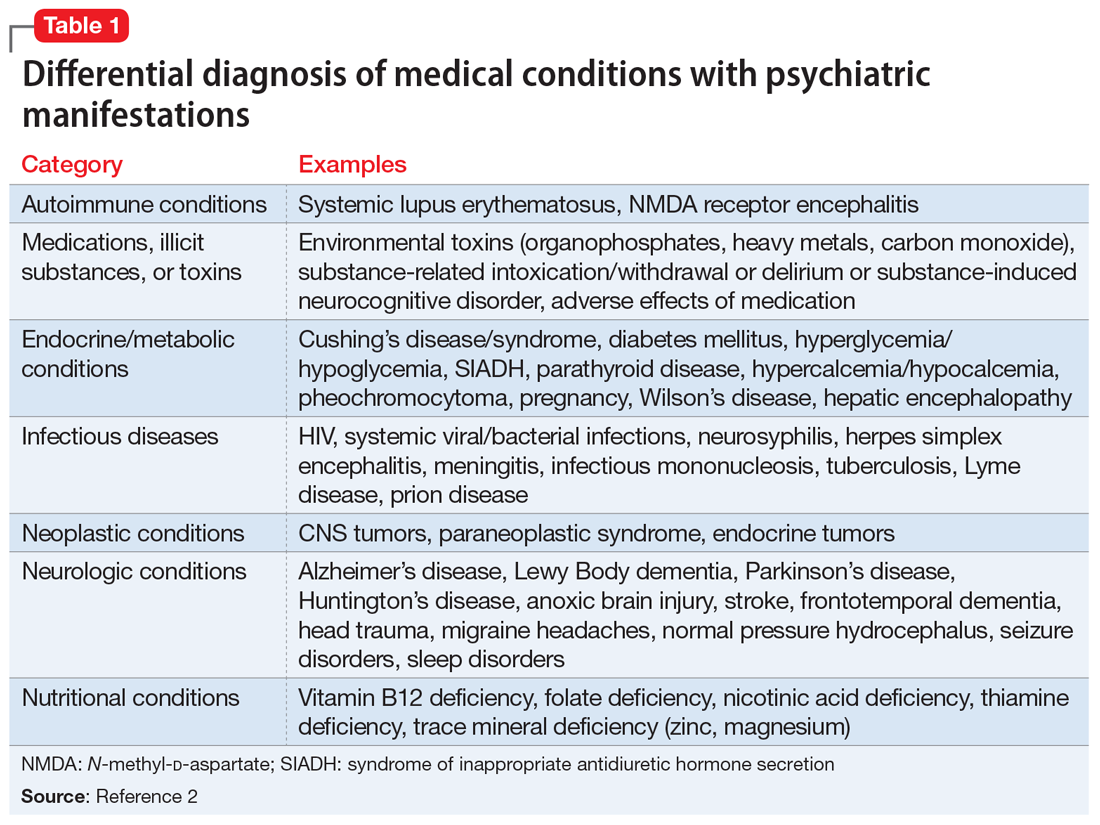
DSM-5 requires that medical conditions be ruled out in order for a patient to meet criteria for a psychiatric diagnosis.1 Medical differential diagnoses for patients with psychiatric symptoms can include autoimmune, drug/toxin, metabolic, infectious, neoplastic, neurologic, and nutritional etiologies (Table 12). To rule out the possibility of an underlying medical etiology, general screening guidelines include complete blood count, complete metabolic panel, urinalysis, and urine drug screen with alcohol. Human immunodeficiency virus testing and thyroid hormone testing are also commonly ordered.3 Further laboratory testing and imaging is typically not warranted in the absence of historical or physical findings because they are not advocated as cost-effective, so health care professionals must use their clinical judgment to determine appropriate further evaluation. The onset of anxiety most commonly occurs in late adolescence early and adulthood, but Mr. A experienced his first symptoms of anxiety at age 41.2 Mr. A’s age, lack of psychiatric or family history of mental illness, acute onset of symptoms, and failure of symptoms to abate with standard psychiatric treatments warrant a more extensive workup.
EVALUATION Imaging reveals an important finding
Because Mr. A’s symptoms do not improve with standard psychiatric treatments, his PCP orders standard laboratory bloodwork to investigate a possible medical etiology; however, his results are all within normal range.
After the PCP’s niece is coincidentally diagnosed with a pituitary macroadenoma, the PCP orders brain imaging for Mr. A. Results of an MRI show that Mr. A has a 1.6-cm macroadenoma of the pituitary. He is referred to an endocrinologist, who orders additional laboratory tests that show an elevated 24-hour free urine cortisol level of 73 μg/24 h (normal range: 3.5 to 45 μg/24 h), suggesting that Mr. A’s anxiety may be due to Cushing’s disease or that his anxiety caused falsely elevated urinary cortisol levels. Four weeks later, bloodwork is repeated and shows an abnormal dexamethasone suppression test, and 2 more elevated 24-hour free urine cortisol levels of 76 μg/24 h and 150 μg/24 h. A repeat MRI shows a 1.8-cm, mostly cystic sellar mass, indicating the need for surgical intervention. Although the tumor is large and shows optic nerve compression, Mr. A does not complain of headaches or changes in vision.
Continue to: Two months later...
Two months later, Mr. A undergoes a transsphenoidal tumor resection of the pituitary adenoma, and biopsy results confirm an adrenocorticotropic hormone (ACTH)-secreting pituitary macroadenoma, which is consistent with Cushing’s disease. Following surgery, steroid treatment with dexamethasone is discontinued due to a persistently elevated
[polldaddy:10891923]
The authors’ observations
Chronic excess glucocorticoid production is the underlying pathophysiology of Cushing’s disease, which is most commonly caused by an ACTH-producing adenoma.4,5 When these hormones become dysregulated, the result can be over- or underproduction of cortisol, which can lead to physical and psychiatric manifestations.6
Cushing’s disease most commonly manifests with the physical symptoms of centripetal fat deposition, abdominal striae, facial plethora, muscle atrophy, bone density loss, immunosuppression, and cardiovascular complications.5
Hypercortisolism can precipitate anxiety (12% to 79%), mood disorders (50% to 70%), and (less commonly) psychotic disorders; however, in a clinical setting, if a patient presented with one of these as a chief complaint, they would likely first be treated psychiatrically rather than worked up medically for a rare medical condition.5,7-13
Mr. A’s initial bloodwork was unremarkable, but cortisol levels were not obtained at that time because testing for cortisol levels to rule out an underlying medical condition is not routine in patients with depression and anxiety. In Mr. A’s case, a neuroendocrine workup was only ordered once his PCP’s niece coincidentally was diagnosed with a pituitary adenoma.
Continue to: For Mr. A...
For Mr. A, Cushing’s disease presented as a psychiatric disorder with anxiety and insomnia that were resistant to numerous psychiatric medications during an 8-month period. If Mr. A’s PCP had not ordered a brain MRI, he may have continued to receive ineffective psychiatric treatment for some time. Many of Mr. A’s physical symptoms were consistent with Cushing’s disease and mental illness, including erectile dysfunction, fatigue, and muscle weakness; however, his 15-pound weight loss pointed more toward psychiatric illness and further disguised his underlying medical diagnosis, because sudden weight gain is commonly seen in Cushing’s disease (Table 24,5,7,9).
TREATMENT Persistent psychiatric symptoms, then finally relief
Four weeks after surgery, Mr. A’s psychiatric symptoms gradually intensify, which prompts him to see a psychiatrist. A mental status examination (MSE) shows that he is well-nourished, with normal activity, appropriate behavior, and coherent thought process, but depressed mood and flat affect. He denies suicidal or homicidal ideation. He reports that despite being advised to have realistic expectations, he had high hopes that the surgery would lead to remission of all his symptoms, and expresses disappointment that he does not feel “back to normal.”
Six days later, Mr. A’s wife takes him to the hospital. His MSE shows that he has a tense appearance, fidgety activity, depressed and anxious mood, restricted affect, circumstantial thought process, and paranoid delusions that his wife was plotting against him. He says he still is experiencing insomnia. He also discloses having suicidal ideations with a plan and intent to overdose on medication, as well as homicidal ideations about killing his wife and children. Mr. A provides reasons for why he would want to hurt his family, and does not appear to be bothered by these thoughts.
Mr. A is admitted to the inpatient psychiatric unit and is prescribed quetiapine, 100 mg every night at bedtime. During the next 2 days, quetiapine is titrated to 300 mg every night at bedtime. On hospital Day 3, Mr. A says he is feeling worse than the previous days. He is still having vague suicidal thoughts and feels agitated, guilty, and depressed. To treat these persistent symptoms, quetiapine is further increased to 400 mg every night at bedtime, and he is initiated on bupropion XL, 150 mg, to treat persistent symptoms.
After 1 week of hospitalization, the treatment team meets with Mr. A and his wife, who has been supportive throughout her husband’s hospitalization. During the meeting, they both agree that Mr. A has experienced some improvement because he is no longer having suicidal or homicidal thoughts, but he is still feeling depressed and frustrated by his continued insomnia. Following the meeting, Mr. A’s quetiapine is further increased to 450 mg every night at bedtime to address continued insomnia, and bupropion XL is increased to 300 mg/d to address continued depressive symptoms. During the next few days, his affective symptoms improve; however, his initial insomnia continues, and quetiapine is further increased to 500 mg every night at bedtime.
Continue to: On hospital Day 20...
On hospital Day 20, Mr. A is discharged back to his outpatient psychiatrist and receives quetiapine, 500 mg every night at bedtime, and bupropion XL, 300 mg/d. Although Mr. A’s depression and anxiety continue to be well controlled, his insomnia persists. Sleep hygiene is addressed, and alprazolam, 0.5 mg every night at bedtime, is added to his regimen, which proves to be effective.
OUTCOME A slow remission
After a year of treatment, Mr. A is slowly tapered off of all medications. Two years later, he is in complete remission of all psychiatric symptoms and no longer requires any psychotropic medications.
The authors’ observations
Treatment for hypercortisolism in patients with psychiatric symptoms triggered by glucocorticoid imbalance has typically resulted in a decrease in the severity of their psychiatric symptoms.9,11 A prospective longitudinal study examining 33 patients found that correction of hypercortisolism in patients with Cushing’s syndrome often led to resolution of their psychiatric symptoms, with 87.9% of patients back to baseline within 1 year.14 However, to our knowledge, few reports have described the management of patients whose symptoms are resistant to treatment of hypercortisolism.
In our case, after transsphenoidal resection of an adenoma, Mr. A became suicidal and paranoid, and his anxiety and insomnia also persisted. A possible explanation for the worsening of Mr. A’s symptoms after surgery could be the slow recovery of the hypothalamic-pituitary-adrenal (HPA) axis and therefore a temporary deficiency in glucocorticoid, which caused an increase in catecholamines, leading to an increase in stress.14 This concept of a “slow recovery” is supported by the fact that Mr. A was successfully weaned off all medication after 1 year of treatment, and achieved complete remission of psychiatric symptoms for >2 years. Furthermore, the severity of Mr. A’s symptoms appeared to correlate with his 24-hour urine cortisol and
Future research should evaluate the utility of screening all patients with treatment-resistant anxiety and/or insomnia for hypercortisolism. Even without other clues to endocrinopathies, serum cortisol levels can be used as a screening tool for diagnosing underlying medical causes in patients with anxiety and depression.2 A greater understanding of the relationship between medical and psychiatric manifestations will allow clinicians to better care for patients. Further research is needed to elucidate the quantitative relationship between cortisol levels and anxiety to evaluate severity, guide treatment planning, and follow treatment response for patients with anxiety. It may be useful to determine the threshold between elevated cortisol levels due to anxiety vs elevated cortisol due to an underlying medical pathology such as Cushing’s disease. Additionally, little research has been conducted to compare how psychiatric symptoms respond to pituitary macroadenoma resection alone, pharmaceutical intervention alone, or a combination of these approaches. It would be beneficial to evaluate these treatment strategies to elucidate the most effective method to reduce psychiatric symptoms in patients with hypercortisolism, and perhaps to reduce the incidence of post-resection worsening of psychiatric symptoms.
Continue to: This case was challenging...
This case was challenging because Mr. A did not initially respond to psychiatric intervention, his psychiatric symptoms worsened after transsphenoidal resection of the pituitary adenoma, and his symptoms were alleviated only after psychiatric medications were re-initiated following surgery. This case highlights the importance of considering an underlying medically diagnosable and treatable cause of psychiatric illness, and illustrates the complex ongoing management that may be necessary to help a patient with this condition achieve their baseline. Further, Mr. A’s case shows that the absence of response to standard psychiatric therapies should warrant earlier laboratory and/or imaging evaluation prior to or in conjunction with psychiatric referral. Additionally, testing for cortisol levels is not typically done for a patient with treatment-resistant anxiety, and this case highlights the importance of considering hypercortisolism in such circumstances.
Bottom Line
Consider testing cortisol levels in patients with treatment-resistant anxiety and insomnia, because cortisol plays a role in Cushing’s disease and anxiety. The severity of psychiatric manifestations of Cushing’s disease may correlate with cortisol levels. Treatment should focus on symptomatic management and underlying etiology.
Related Resources
- Roberts LW, Hales RE, Yudofsky SC, ed. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019.
- Rotham J. Cushing’s syndrome: a tale of frequent misdiagnosis. National Center for Health Research. 2020. www.center4research.org/cushings-syndrome-frequent-misdiagnosis/
- Middleman D. Psychiatric issues of Cushing’s patients: coping with Cushing’s. Cushing’s Support and Research Foundation. www.csrf.net/coping-with-cushings/psychiatric-issues-of-cushings-patients/
Drug Brand Names
Alprazolam • Xanax
Bupropion • Wellbutrin
Dexamethasone • Decadron
Diazepam • Valium
Eszopiclone • Lunesta
Paroxetine • Paxil
Quetiapine • Seroquel
Zolpidem tartrate • Ambien CR
1. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
2. Sadock BJ, Sadock VA, Ruiz P, et al. Neural sciences. In: Sadock BJ, Sadock VA, Ruiz P, et al. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Wolters Kluwer; 2015.
3. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry. 1992;14(4):248-257.
4. Fehm HL, Voigt KH. Pathophysiology of Cushing’s disease. Pathobiol Annu. 1979;9:225-255.
5. Fujii Y, Mizoguchi Y, Masuoka J, et al. Cushing’s syndrome and psychosis: a case report and literature review. Prim Care Companion CNS Disord. 2018;20(5):18.
6. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing’s syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2011;4(2):739-769.
7. Santos A, Resimini E, Pascual JC, et al. Psychiatric symptoms in patients with Cushing’s syndrome: prevalence diagnosis, and management. Drugs. 2017;77(8):829-842.
8. Arnaldi G, Angeli A, Atkinson B, et al. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593-5602.
9. Sonino N, Fava GA. Psychosomatic aspects of Cushing’s disease. Psychother Psychosom. 1998;67(3):140-146.
10. Loosen PT, Chambliss B, DeBold CR, et al. Psychiatric phenomenology in Cushing’s disease. Pharmacopsychiatry. 1992;25(4):192-198.
11. Kelly WF, Kelly MJ, Faragher B. A prospective study of psychiatric and psychological aspects of Cushing’s syndrome. Clin Endocrinol. 1996;45(6):715-720.
12. Katho RG, Delahunt JW, Hannah L. Transition from bipolar affective disorder to intermittent Cushing’s syndrome: case report. J Clin Psychiatry. 1985;46(5):194-196.
13. Hirsh D, Orr G, Kantarovich V, et al. Cushing’s syndrome presenting as a schizophrenia-like psychotic state. Isr J Psychiatry Relat Sci. 2000;37(1):46-50.
14. Dorn LD, Burgess ES, Friedman TC, et al. The longitudinal course of psychopathology in Cushing’s syndrome after correction of hypercortisolism. J Clin Endocrinol Metab. 1997;82(3):912-919.
15. Starkman MN, Schteingart DE, Schork MA. Cushing’s syndrome after treatment: changes in cortisol and ACTH levels, and amelioration of the depressive syndrome. Psychiatry Res. 1986;19(3):177-178.
CASE Anxious and can’t sleep
Mr. A, age 41, presents to his primary care physician (PCP) with anxiety and insomnia. He describes having generalized anxiety with initial and middle insomnia, and says he is sleeping an average of 2 hours per night. He denies any other psychiatric symptoms. Mr. A has no significant psychiatric or medical history.
Mr. A is initiated on zolpidem tartrate, 12.5 mg every night at bedtime, and paroxetine, 20 mg every night at bedtime, for anxiety and insomnia, but these medications result in little to no improvement.
During a 4-month period, he is treated with trials of alprazolam, 0.5 mg every 8 hours as needed; diazepam 5 mg twice a day as needed; diphenhydramine, 50 mg at bedtime; and eszopiclone, 3 mg at bedtime. Despite these treatments, he experiences increased anxiety and insomnia, and develops depressive symptoms, including depressed mood, poor concentration, general malaise, extreme fatigue, a 15-pound unintentional weight loss, erectile dysfunction, and decreased libido. Mr. A denies having suicidal or homicidal ideations. Additionally, he typically goes to the gym approximately 3 times per week, and has noticed that the amount of weight he is able to lift has decreased, which is distressing. Previously, he had been able to lift 300 pounds, but now he can only lift 200 pounds.
[polldaddy:10891920]
The authors’ observations
Insomnia, anxiety, and depression are common chief complaints in medical settings. However, some psychiatric presentations may have an underlying medical etiology.
DSM-5 requires that medical conditions be ruled out in order for a patient to meet criteria for a psychiatric diagnosis.1 Medical differential diagnoses for patients with psychiatric symptoms can include autoimmune, drug/toxin, metabolic, infectious, neoplastic, neurologic, and nutritional etiologies (Table 12). To rule out the possibility of an underlying medical etiology, general screening guidelines include complete blood count, complete metabolic panel, urinalysis, and urine drug screen with alcohol. Human immunodeficiency virus testing and thyroid hormone testing are also commonly ordered.3 Further laboratory testing and imaging is typically not warranted in the absence of historical or physical findings because they are not advocated as cost-effective, so health care professionals must use their clinical judgment to determine appropriate further evaluation. The onset of anxiety most commonly occurs in late adolescence early and adulthood, but Mr. A experienced his first symptoms of anxiety at age 41.2 Mr. A’s age, lack of psychiatric or family history of mental illness, acute onset of symptoms, and failure of symptoms to abate with standard psychiatric treatments warrant a more extensive workup.
EVALUATION Imaging reveals an important finding
Because Mr. A’s symptoms do not improve with standard psychiatric treatments, his PCP orders standard laboratory bloodwork to investigate a possible medical etiology; however, his results are all within normal range.
After the PCP’s niece is coincidentally diagnosed with a pituitary macroadenoma, the PCP orders brain imaging for Mr. A. Results of an MRI show that Mr. A has a 1.6-cm macroadenoma of the pituitary. He is referred to an endocrinologist, who orders additional laboratory tests that show an elevated 24-hour free urine cortisol level of 73 μg/24 h (normal range: 3.5 to 45 μg/24 h), suggesting that Mr. A’s anxiety may be due to Cushing’s disease or that his anxiety caused falsely elevated urinary cortisol levels. Four weeks later, bloodwork is repeated and shows an abnormal dexamethasone suppression test, and 2 more elevated 24-hour free urine cortisol levels of 76 μg/24 h and 150 μg/24 h. A repeat MRI shows a 1.8-cm, mostly cystic sellar mass, indicating the need for surgical intervention. Although the tumor is large and shows optic nerve compression, Mr. A does not complain of headaches or changes in vision.
Continue to: Two months later...
Two months later, Mr. A undergoes a transsphenoidal tumor resection of the pituitary adenoma, and biopsy results confirm an adrenocorticotropic hormone (ACTH)-secreting pituitary macroadenoma, which is consistent with Cushing’s disease. Following surgery, steroid treatment with dexamethasone is discontinued due to a persistently elevated
[polldaddy:10891923]
The authors’ observations
Chronic excess glucocorticoid production is the underlying pathophysiology of Cushing’s disease, which is most commonly caused by an ACTH-producing adenoma.4,5 When these hormones become dysregulated, the result can be over- or underproduction of cortisol, which can lead to physical and psychiatric manifestations.6
Cushing’s disease most commonly manifests with the physical symptoms of centripetal fat deposition, abdominal striae, facial plethora, muscle atrophy, bone density loss, immunosuppression, and cardiovascular complications.5
Hypercortisolism can precipitate anxiety (12% to 79%), mood disorders (50% to 70%), and (less commonly) psychotic disorders; however, in a clinical setting, if a patient presented with one of these as a chief complaint, they would likely first be treated psychiatrically rather than worked up medically for a rare medical condition.5,7-13
Mr. A’s initial bloodwork was unremarkable, but cortisol levels were not obtained at that time because testing for cortisol levels to rule out an underlying medical condition is not routine in patients with depression and anxiety. In Mr. A’s case, a neuroendocrine workup was only ordered once his PCP’s niece coincidentally was diagnosed with a pituitary adenoma.
Continue to: For Mr. A...
For Mr. A, Cushing’s disease presented as a psychiatric disorder with anxiety and insomnia that were resistant to numerous psychiatric medications during an 8-month period. If Mr. A’s PCP had not ordered a brain MRI, he may have continued to receive ineffective psychiatric treatment for some time. Many of Mr. A’s physical symptoms were consistent with Cushing’s disease and mental illness, including erectile dysfunction, fatigue, and muscle weakness; however, his 15-pound weight loss pointed more toward psychiatric illness and further disguised his underlying medical diagnosis, because sudden weight gain is commonly seen in Cushing’s disease (Table 24,5,7,9).
TREATMENT Persistent psychiatric symptoms, then finally relief
Four weeks after surgery, Mr. A’s psychiatric symptoms gradually intensify, which prompts him to see a psychiatrist. A mental status examination (MSE) shows that he is well-nourished, with normal activity, appropriate behavior, and coherent thought process, but depressed mood and flat affect. He denies suicidal or homicidal ideation. He reports that despite being advised to have realistic expectations, he had high hopes that the surgery would lead to remission of all his symptoms, and expresses disappointment that he does not feel “back to normal.”
Six days later, Mr. A’s wife takes him to the hospital. His MSE shows that he has a tense appearance, fidgety activity, depressed and anxious mood, restricted affect, circumstantial thought process, and paranoid delusions that his wife was plotting against him. He says he still is experiencing insomnia. He also discloses having suicidal ideations with a plan and intent to overdose on medication, as well as homicidal ideations about killing his wife and children. Mr. A provides reasons for why he would want to hurt his family, and does not appear to be bothered by these thoughts.
Mr. A is admitted to the inpatient psychiatric unit and is prescribed quetiapine, 100 mg every night at bedtime. During the next 2 days, quetiapine is titrated to 300 mg every night at bedtime. On hospital Day 3, Mr. A says he is feeling worse than the previous days. He is still having vague suicidal thoughts and feels agitated, guilty, and depressed. To treat these persistent symptoms, quetiapine is further increased to 400 mg every night at bedtime, and he is initiated on bupropion XL, 150 mg, to treat persistent symptoms.
After 1 week of hospitalization, the treatment team meets with Mr. A and his wife, who has been supportive throughout her husband’s hospitalization. During the meeting, they both agree that Mr. A has experienced some improvement because he is no longer having suicidal or homicidal thoughts, but he is still feeling depressed and frustrated by his continued insomnia. Following the meeting, Mr. A’s quetiapine is further increased to 450 mg every night at bedtime to address continued insomnia, and bupropion XL is increased to 300 mg/d to address continued depressive symptoms. During the next few days, his affective symptoms improve; however, his initial insomnia continues, and quetiapine is further increased to 500 mg every night at bedtime.
Continue to: On hospital Day 20...
On hospital Day 20, Mr. A is discharged back to his outpatient psychiatrist and receives quetiapine, 500 mg every night at bedtime, and bupropion XL, 300 mg/d. Although Mr. A’s depression and anxiety continue to be well controlled, his insomnia persists. Sleep hygiene is addressed, and alprazolam, 0.5 mg every night at bedtime, is added to his regimen, which proves to be effective.
OUTCOME A slow remission
After a year of treatment, Mr. A is slowly tapered off of all medications. Two years later, he is in complete remission of all psychiatric symptoms and no longer requires any psychotropic medications.
The authors’ observations
Treatment for hypercortisolism in patients with psychiatric symptoms triggered by glucocorticoid imbalance has typically resulted in a decrease in the severity of their psychiatric symptoms.9,11 A prospective longitudinal study examining 33 patients found that correction of hypercortisolism in patients with Cushing’s syndrome often led to resolution of their psychiatric symptoms, with 87.9% of patients back to baseline within 1 year.14 However, to our knowledge, few reports have described the management of patients whose symptoms are resistant to treatment of hypercortisolism.
In our case, after transsphenoidal resection of an adenoma, Mr. A became suicidal and paranoid, and his anxiety and insomnia also persisted. A possible explanation for the worsening of Mr. A’s symptoms after surgery could be the slow recovery of the hypothalamic-pituitary-adrenal (HPA) axis and therefore a temporary deficiency in glucocorticoid, which caused an increase in catecholamines, leading to an increase in stress.14 This concept of a “slow recovery” is supported by the fact that Mr. A was successfully weaned off all medication after 1 year of treatment, and achieved complete remission of psychiatric symptoms for >2 years. Furthermore, the severity of Mr. A’s symptoms appeared to correlate with his 24-hour urine cortisol and
Future research should evaluate the utility of screening all patients with treatment-resistant anxiety and/or insomnia for hypercortisolism. Even without other clues to endocrinopathies, serum cortisol levels can be used as a screening tool for diagnosing underlying medical causes in patients with anxiety and depression.2 A greater understanding of the relationship between medical and psychiatric manifestations will allow clinicians to better care for patients. Further research is needed to elucidate the quantitative relationship between cortisol levels and anxiety to evaluate severity, guide treatment planning, and follow treatment response for patients with anxiety. It may be useful to determine the threshold between elevated cortisol levels due to anxiety vs elevated cortisol due to an underlying medical pathology such as Cushing’s disease. Additionally, little research has been conducted to compare how psychiatric symptoms respond to pituitary macroadenoma resection alone, pharmaceutical intervention alone, or a combination of these approaches. It would be beneficial to evaluate these treatment strategies to elucidate the most effective method to reduce psychiatric symptoms in patients with hypercortisolism, and perhaps to reduce the incidence of post-resection worsening of psychiatric symptoms.
Continue to: This case was challenging...
This case was challenging because Mr. A did not initially respond to psychiatric intervention, his psychiatric symptoms worsened after transsphenoidal resection of the pituitary adenoma, and his symptoms were alleviated only after psychiatric medications were re-initiated following surgery. This case highlights the importance of considering an underlying medically diagnosable and treatable cause of psychiatric illness, and illustrates the complex ongoing management that may be necessary to help a patient with this condition achieve their baseline. Further, Mr. A’s case shows that the absence of response to standard psychiatric therapies should warrant earlier laboratory and/or imaging evaluation prior to or in conjunction with psychiatric referral. Additionally, testing for cortisol levels is not typically done for a patient with treatment-resistant anxiety, and this case highlights the importance of considering hypercortisolism in such circumstances.
Bottom Line
Consider testing cortisol levels in patients with treatment-resistant anxiety and insomnia, because cortisol plays a role in Cushing’s disease and anxiety. The severity of psychiatric manifestations of Cushing’s disease may correlate with cortisol levels. Treatment should focus on symptomatic management and underlying etiology.
Related Resources
- Roberts LW, Hales RE, Yudofsky SC, ed. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019.
- Rotham J. Cushing’s syndrome: a tale of frequent misdiagnosis. National Center for Health Research. 2020. www.center4research.org/cushings-syndrome-frequent-misdiagnosis/
- Middleman D. Psychiatric issues of Cushing’s patients: coping with Cushing’s. Cushing’s Support and Research Foundation. www.csrf.net/coping-with-cushings/psychiatric-issues-of-cushings-patients/
Drug Brand Names
Alprazolam • Xanax
Bupropion • Wellbutrin
Dexamethasone • Decadron
Diazepam • Valium
Eszopiclone • Lunesta
Paroxetine • Paxil
Quetiapine • Seroquel
Zolpidem tartrate • Ambien CR
CASE Anxious and can’t sleep
Mr. A, age 41, presents to his primary care physician (PCP) with anxiety and insomnia. He describes having generalized anxiety with initial and middle insomnia, and says he is sleeping an average of 2 hours per night. He denies any other psychiatric symptoms. Mr. A has no significant psychiatric or medical history.
Mr. A is initiated on zolpidem tartrate, 12.5 mg every night at bedtime, and paroxetine, 20 mg every night at bedtime, for anxiety and insomnia, but these medications result in little to no improvement.
During a 4-month period, he is treated with trials of alprazolam, 0.5 mg every 8 hours as needed; diazepam 5 mg twice a day as needed; diphenhydramine, 50 mg at bedtime; and eszopiclone, 3 mg at bedtime. Despite these treatments, he experiences increased anxiety and insomnia, and develops depressive symptoms, including depressed mood, poor concentration, general malaise, extreme fatigue, a 15-pound unintentional weight loss, erectile dysfunction, and decreased libido. Mr. A denies having suicidal or homicidal ideations. Additionally, he typically goes to the gym approximately 3 times per week, and has noticed that the amount of weight he is able to lift has decreased, which is distressing. Previously, he had been able to lift 300 pounds, but now he can only lift 200 pounds.
[polldaddy:10891920]
The authors’ observations
Insomnia, anxiety, and depression are common chief complaints in medical settings. However, some psychiatric presentations may have an underlying medical etiology.
DSM-5 requires that medical conditions be ruled out in order for a patient to meet criteria for a psychiatric diagnosis.1 Medical differential diagnoses for patients with psychiatric symptoms can include autoimmune, drug/toxin, metabolic, infectious, neoplastic, neurologic, and nutritional etiologies (Table 12). To rule out the possibility of an underlying medical etiology, general screening guidelines include complete blood count, complete metabolic panel, urinalysis, and urine drug screen with alcohol. Human immunodeficiency virus testing and thyroid hormone testing are also commonly ordered.3 Further laboratory testing and imaging is typically not warranted in the absence of historical or physical findings because they are not advocated as cost-effective, so health care professionals must use their clinical judgment to determine appropriate further evaluation. The onset of anxiety most commonly occurs in late adolescence early and adulthood, but Mr. A experienced his first symptoms of anxiety at age 41.2 Mr. A’s age, lack of psychiatric or family history of mental illness, acute onset of symptoms, and failure of symptoms to abate with standard psychiatric treatments warrant a more extensive workup.
EVALUATION Imaging reveals an important finding
Because Mr. A’s symptoms do not improve with standard psychiatric treatments, his PCP orders standard laboratory bloodwork to investigate a possible medical etiology; however, his results are all within normal range.
After the PCP’s niece is coincidentally diagnosed with a pituitary macroadenoma, the PCP orders brain imaging for Mr. A. Results of an MRI show that Mr. A has a 1.6-cm macroadenoma of the pituitary. He is referred to an endocrinologist, who orders additional laboratory tests that show an elevated 24-hour free urine cortisol level of 73 μg/24 h (normal range: 3.5 to 45 μg/24 h), suggesting that Mr. A’s anxiety may be due to Cushing’s disease or that his anxiety caused falsely elevated urinary cortisol levels. Four weeks later, bloodwork is repeated and shows an abnormal dexamethasone suppression test, and 2 more elevated 24-hour free urine cortisol levels of 76 μg/24 h and 150 μg/24 h. A repeat MRI shows a 1.8-cm, mostly cystic sellar mass, indicating the need for surgical intervention. Although the tumor is large and shows optic nerve compression, Mr. A does not complain of headaches or changes in vision.
Continue to: Two months later...
Two months later, Mr. A undergoes a transsphenoidal tumor resection of the pituitary adenoma, and biopsy results confirm an adrenocorticotropic hormone (ACTH)-secreting pituitary macroadenoma, which is consistent with Cushing’s disease. Following surgery, steroid treatment with dexamethasone is discontinued due to a persistently elevated
[polldaddy:10891923]
The authors’ observations
Chronic excess glucocorticoid production is the underlying pathophysiology of Cushing’s disease, which is most commonly caused by an ACTH-producing adenoma.4,5 When these hormones become dysregulated, the result can be over- or underproduction of cortisol, which can lead to physical and psychiatric manifestations.6
Cushing’s disease most commonly manifests with the physical symptoms of centripetal fat deposition, abdominal striae, facial plethora, muscle atrophy, bone density loss, immunosuppression, and cardiovascular complications.5
Hypercortisolism can precipitate anxiety (12% to 79%), mood disorders (50% to 70%), and (less commonly) psychotic disorders; however, in a clinical setting, if a patient presented with one of these as a chief complaint, they would likely first be treated psychiatrically rather than worked up medically for a rare medical condition.5,7-13
Mr. A’s initial bloodwork was unremarkable, but cortisol levels were not obtained at that time because testing for cortisol levels to rule out an underlying medical condition is not routine in patients with depression and anxiety. In Mr. A’s case, a neuroendocrine workup was only ordered once his PCP’s niece coincidentally was diagnosed with a pituitary adenoma.
Continue to: For Mr. A...
For Mr. A, Cushing’s disease presented as a psychiatric disorder with anxiety and insomnia that were resistant to numerous psychiatric medications during an 8-month period. If Mr. A’s PCP had not ordered a brain MRI, he may have continued to receive ineffective psychiatric treatment for some time. Many of Mr. A’s physical symptoms were consistent with Cushing’s disease and mental illness, including erectile dysfunction, fatigue, and muscle weakness; however, his 15-pound weight loss pointed more toward psychiatric illness and further disguised his underlying medical diagnosis, because sudden weight gain is commonly seen in Cushing’s disease (Table 24,5,7,9).
TREATMENT Persistent psychiatric symptoms, then finally relief
Four weeks after surgery, Mr. A’s psychiatric symptoms gradually intensify, which prompts him to see a psychiatrist. A mental status examination (MSE) shows that he is well-nourished, with normal activity, appropriate behavior, and coherent thought process, but depressed mood and flat affect. He denies suicidal or homicidal ideation. He reports that despite being advised to have realistic expectations, he had high hopes that the surgery would lead to remission of all his symptoms, and expresses disappointment that he does not feel “back to normal.”
Six days later, Mr. A’s wife takes him to the hospital. His MSE shows that he has a tense appearance, fidgety activity, depressed and anxious mood, restricted affect, circumstantial thought process, and paranoid delusions that his wife was plotting against him. He says he still is experiencing insomnia. He also discloses having suicidal ideations with a plan and intent to overdose on medication, as well as homicidal ideations about killing his wife and children. Mr. A provides reasons for why he would want to hurt his family, and does not appear to be bothered by these thoughts.
Mr. A is admitted to the inpatient psychiatric unit and is prescribed quetiapine, 100 mg every night at bedtime. During the next 2 days, quetiapine is titrated to 300 mg every night at bedtime. On hospital Day 3, Mr. A says he is feeling worse than the previous days. He is still having vague suicidal thoughts and feels agitated, guilty, and depressed. To treat these persistent symptoms, quetiapine is further increased to 400 mg every night at bedtime, and he is initiated on bupropion XL, 150 mg, to treat persistent symptoms.
After 1 week of hospitalization, the treatment team meets with Mr. A and his wife, who has been supportive throughout her husband’s hospitalization. During the meeting, they both agree that Mr. A has experienced some improvement because he is no longer having suicidal or homicidal thoughts, but he is still feeling depressed and frustrated by his continued insomnia. Following the meeting, Mr. A’s quetiapine is further increased to 450 mg every night at bedtime to address continued insomnia, and bupropion XL is increased to 300 mg/d to address continued depressive symptoms. During the next few days, his affective symptoms improve; however, his initial insomnia continues, and quetiapine is further increased to 500 mg every night at bedtime.
Continue to: On hospital Day 20...
On hospital Day 20, Mr. A is discharged back to his outpatient psychiatrist and receives quetiapine, 500 mg every night at bedtime, and bupropion XL, 300 mg/d. Although Mr. A’s depression and anxiety continue to be well controlled, his insomnia persists. Sleep hygiene is addressed, and alprazolam, 0.5 mg every night at bedtime, is added to his regimen, which proves to be effective.
OUTCOME A slow remission
After a year of treatment, Mr. A is slowly tapered off of all medications. Two years later, he is in complete remission of all psychiatric symptoms and no longer requires any psychotropic medications.
The authors’ observations
Treatment for hypercortisolism in patients with psychiatric symptoms triggered by glucocorticoid imbalance has typically resulted in a decrease in the severity of their psychiatric symptoms.9,11 A prospective longitudinal study examining 33 patients found that correction of hypercortisolism in patients with Cushing’s syndrome often led to resolution of their psychiatric symptoms, with 87.9% of patients back to baseline within 1 year.14 However, to our knowledge, few reports have described the management of patients whose symptoms are resistant to treatment of hypercortisolism.
In our case, after transsphenoidal resection of an adenoma, Mr. A became suicidal and paranoid, and his anxiety and insomnia also persisted. A possible explanation for the worsening of Mr. A’s symptoms after surgery could be the slow recovery of the hypothalamic-pituitary-adrenal (HPA) axis and therefore a temporary deficiency in glucocorticoid, which caused an increase in catecholamines, leading to an increase in stress.14 This concept of a “slow recovery” is supported by the fact that Mr. A was successfully weaned off all medication after 1 year of treatment, and achieved complete remission of psychiatric symptoms for >2 years. Furthermore, the severity of Mr. A’s symptoms appeared to correlate with his 24-hour urine cortisol and
Future research should evaluate the utility of screening all patients with treatment-resistant anxiety and/or insomnia for hypercortisolism. Even without other clues to endocrinopathies, serum cortisol levels can be used as a screening tool for diagnosing underlying medical causes in patients with anxiety and depression.2 A greater understanding of the relationship between medical and psychiatric manifestations will allow clinicians to better care for patients. Further research is needed to elucidate the quantitative relationship between cortisol levels and anxiety to evaluate severity, guide treatment planning, and follow treatment response for patients with anxiety. It may be useful to determine the threshold between elevated cortisol levels due to anxiety vs elevated cortisol due to an underlying medical pathology such as Cushing’s disease. Additionally, little research has been conducted to compare how psychiatric symptoms respond to pituitary macroadenoma resection alone, pharmaceutical intervention alone, or a combination of these approaches. It would be beneficial to evaluate these treatment strategies to elucidate the most effective method to reduce psychiatric symptoms in patients with hypercortisolism, and perhaps to reduce the incidence of post-resection worsening of psychiatric symptoms.
Continue to: This case was challenging...
This case was challenging because Mr. A did not initially respond to psychiatric intervention, his psychiatric symptoms worsened after transsphenoidal resection of the pituitary adenoma, and his symptoms were alleviated only after psychiatric medications were re-initiated following surgery. This case highlights the importance of considering an underlying medically diagnosable and treatable cause of psychiatric illness, and illustrates the complex ongoing management that may be necessary to help a patient with this condition achieve their baseline. Further, Mr. A’s case shows that the absence of response to standard psychiatric therapies should warrant earlier laboratory and/or imaging evaluation prior to or in conjunction with psychiatric referral. Additionally, testing for cortisol levels is not typically done for a patient with treatment-resistant anxiety, and this case highlights the importance of considering hypercortisolism in such circumstances.
Bottom Line
Consider testing cortisol levels in patients with treatment-resistant anxiety and insomnia, because cortisol plays a role in Cushing’s disease and anxiety. The severity of psychiatric manifestations of Cushing’s disease may correlate with cortisol levels. Treatment should focus on symptomatic management and underlying etiology.
Related Resources
- Roberts LW, Hales RE, Yudofsky SC, ed. The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019.
- Rotham J. Cushing’s syndrome: a tale of frequent misdiagnosis. National Center for Health Research. 2020. www.center4research.org/cushings-syndrome-frequent-misdiagnosis/
- Middleman D. Psychiatric issues of Cushing’s patients: coping with Cushing’s. Cushing’s Support and Research Foundation. www.csrf.net/coping-with-cushings/psychiatric-issues-of-cushings-patients/
Drug Brand Names
Alprazolam • Xanax
Bupropion • Wellbutrin
Dexamethasone • Decadron
Diazepam • Valium
Eszopiclone • Lunesta
Paroxetine • Paxil
Quetiapine • Seroquel
Zolpidem tartrate • Ambien CR
1. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
2. Sadock BJ, Sadock VA, Ruiz P, et al. Neural sciences. In: Sadock BJ, Sadock VA, Ruiz P, et al. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Wolters Kluwer; 2015.
3. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry. 1992;14(4):248-257.
4. Fehm HL, Voigt KH. Pathophysiology of Cushing’s disease. Pathobiol Annu. 1979;9:225-255.
5. Fujii Y, Mizoguchi Y, Masuoka J, et al. Cushing’s syndrome and psychosis: a case report and literature review. Prim Care Companion CNS Disord. 2018;20(5):18.
6. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing’s syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2011;4(2):739-769.
7. Santos A, Resimini E, Pascual JC, et al. Psychiatric symptoms in patients with Cushing’s syndrome: prevalence diagnosis, and management. Drugs. 2017;77(8):829-842.
8. Arnaldi G, Angeli A, Atkinson B, et al. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593-5602.
9. Sonino N, Fava GA. Psychosomatic aspects of Cushing’s disease. Psychother Psychosom. 1998;67(3):140-146.
10. Loosen PT, Chambliss B, DeBold CR, et al. Psychiatric phenomenology in Cushing’s disease. Pharmacopsychiatry. 1992;25(4):192-198.
11. Kelly WF, Kelly MJ, Faragher B. A prospective study of psychiatric and psychological aspects of Cushing’s syndrome. Clin Endocrinol. 1996;45(6):715-720.
12. Katho RG, Delahunt JW, Hannah L. Transition from bipolar affective disorder to intermittent Cushing’s syndrome: case report. J Clin Psychiatry. 1985;46(5):194-196.
13. Hirsh D, Orr G, Kantarovich V, et al. Cushing’s syndrome presenting as a schizophrenia-like psychotic state. Isr J Psychiatry Relat Sci. 2000;37(1):46-50.
14. Dorn LD, Burgess ES, Friedman TC, et al. The longitudinal course of psychopathology in Cushing’s syndrome after correction of hypercortisolism. J Clin Endocrinol Metab. 1997;82(3):912-919.
15. Starkman MN, Schteingart DE, Schork MA. Cushing’s syndrome after treatment: changes in cortisol and ACTH levels, and amelioration of the depressive syndrome. Psychiatry Res. 1986;19(3):177-178.
1. Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013.
2. Sadock BJ, Sadock VA, Ruiz P, et al. Neural sciences. In: Sadock BJ, Sadock VA, Ruiz P, et al. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Wolters Kluwer; 2015.
3. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry. 1992;14(4):248-257.
4. Fehm HL, Voigt KH. Pathophysiology of Cushing’s disease. Pathobiol Annu. 1979;9:225-255.
5. Fujii Y, Mizoguchi Y, Masuoka J, et al. Cushing’s syndrome and psychosis: a case report and literature review. Prim Care Companion CNS Disord. 2018;20(5):18.
6. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing’s syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2011;4(2):739-769.
7. Santos A, Resimini E, Pascual JC, et al. Psychiatric symptoms in patients with Cushing’s syndrome: prevalence diagnosis, and management. Drugs. 2017;77(8):829-842.
8. Arnaldi G, Angeli A, Atkinson B, et al. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593-5602.
9. Sonino N, Fava GA. Psychosomatic aspects of Cushing’s disease. Psychother Psychosom. 1998;67(3):140-146.
10. Loosen PT, Chambliss B, DeBold CR, et al. Psychiatric phenomenology in Cushing’s disease. Pharmacopsychiatry. 1992;25(4):192-198.
11. Kelly WF, Kelly MJ, Faragher B. A prospective study of psychiatric and psychological aspects of Cushing’s syndrome. Clin Endocrinol. 1996;45(6):715-720.
12. Katho RG, Delahunt JW, Hannah L. Transition from bipolar affective disorder to intermittent Cushing’s syndrome: case report. J Clin Psychiatry. 1985;46(5):194-196.
13. Hirsh D, Orr G, Kantarovich V, et al. Cushing’s syndrome presenting as a schizophrenia-like psychotic state. Isr J Psychiatry Relat Sci. 2000;37(1):46-50.
14. Dorn LD, Burgess ES, Friedman TC, et al. The longitudinal course of psychopathology in Cushing’s syndrome after correction of hypercortisolism. J Clin Endocrinol Metab. 1997;82(3):912-919.
15. Starkman MN, Schteingart DE, Schork MA. Cushing’s syndrome after treatment: changes in cortisol and ACTH levels, and amelioration of the depressive syndrome. Psychiatry Res. 1986;19(3):177-178.
Avoiding malpractice while treating depression in pregnant women
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
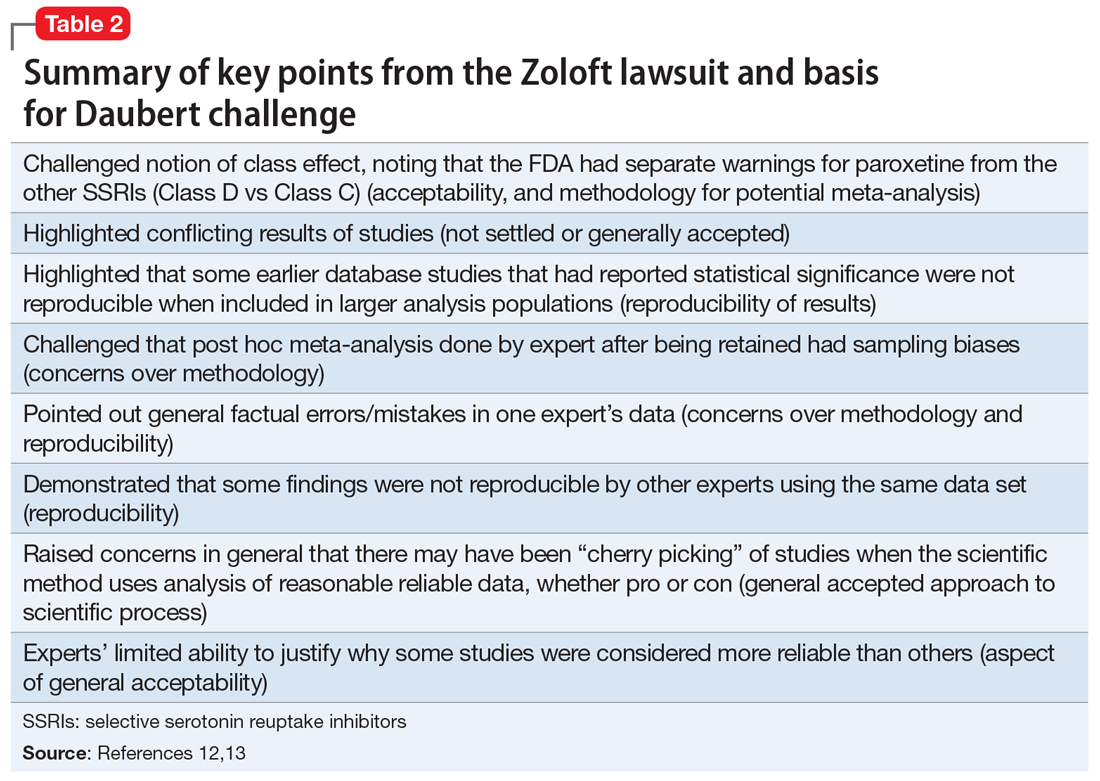
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
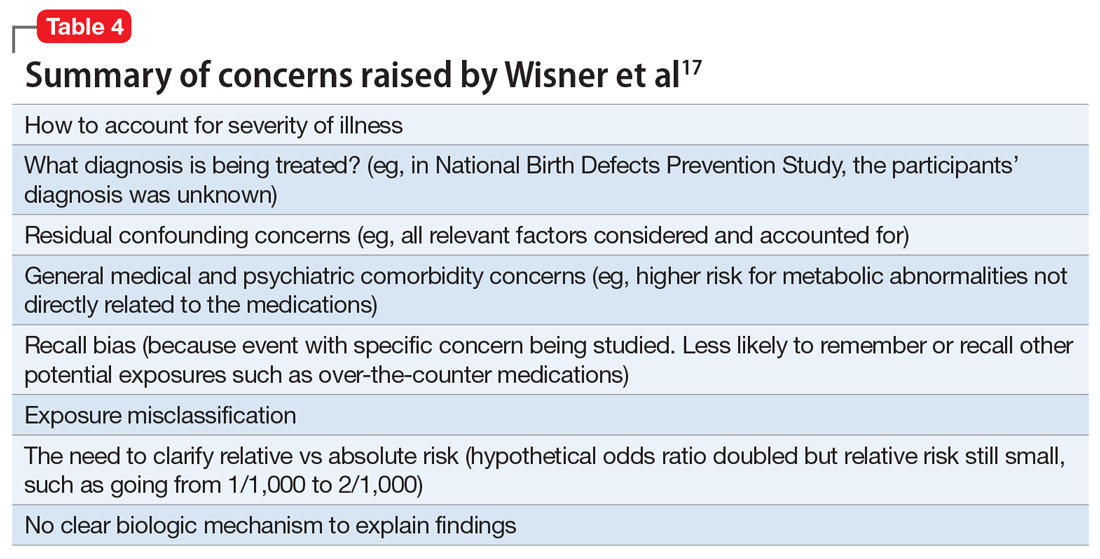
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
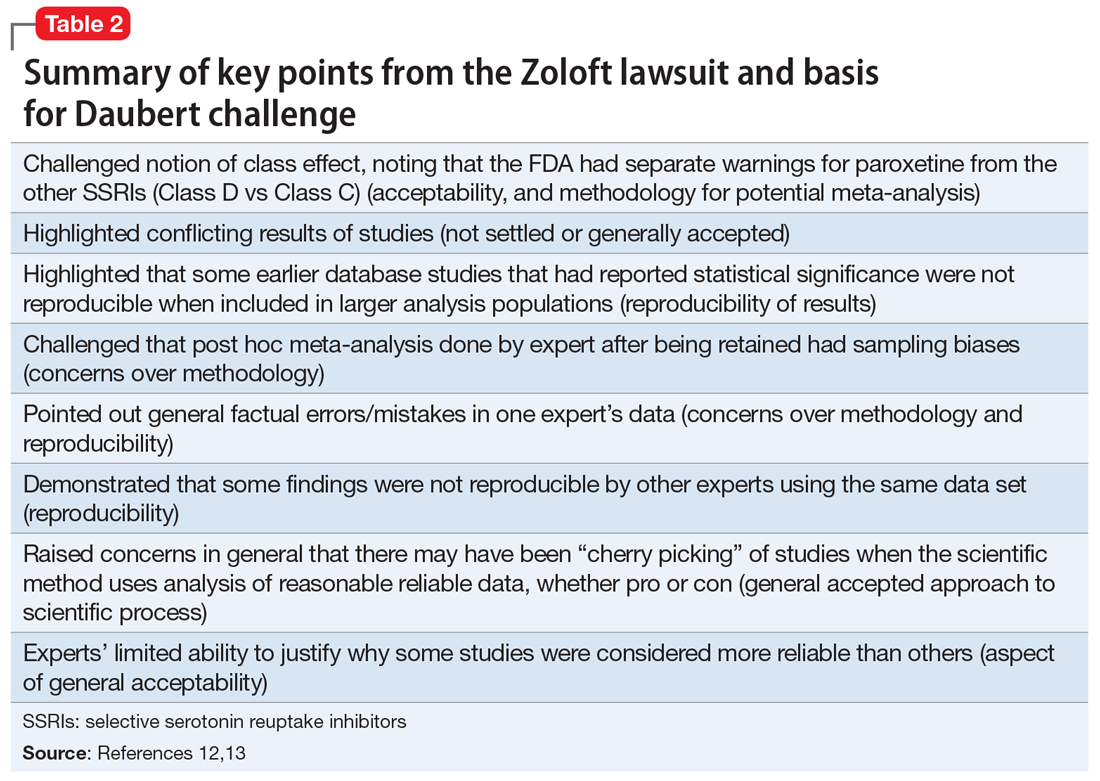
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
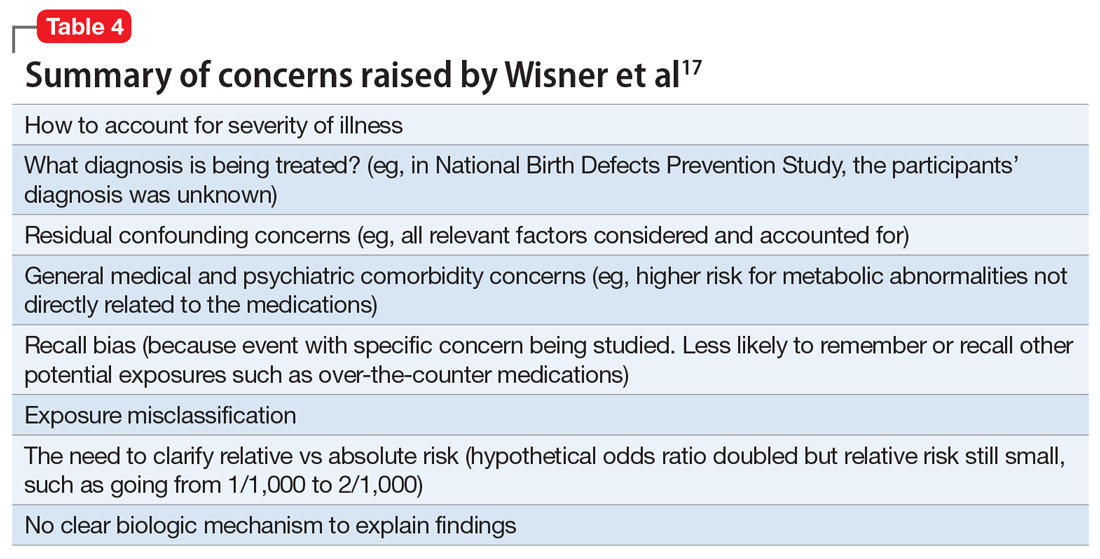
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
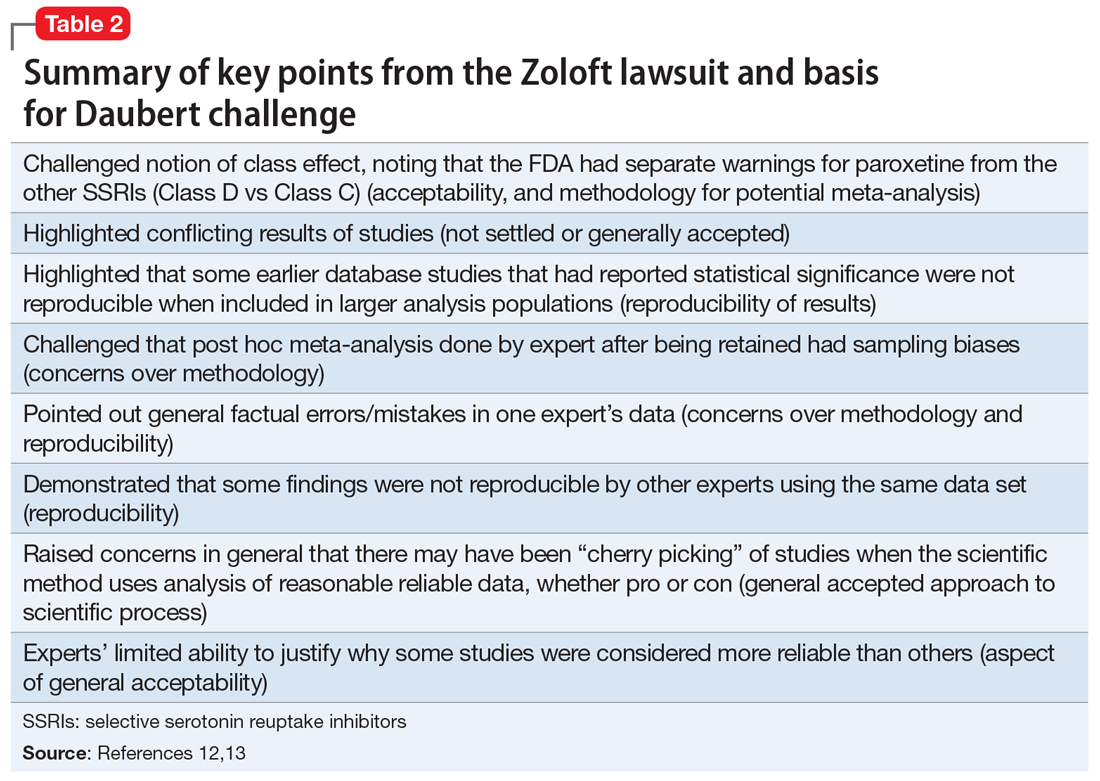
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
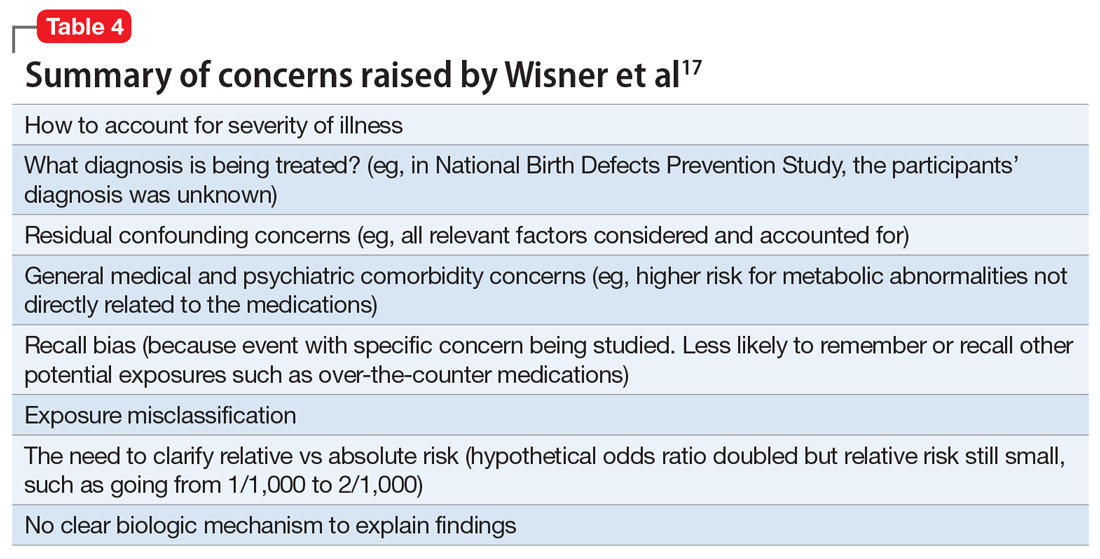
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Mental illness admissions: 18-44 is the age of prevalence
More mental and/or substance use disorders are ranked among the top-five diagnoses for hospitalized men and women aged 18-44 years than for any other age group, according to a recent report from the Agency for Healthcare Research and Quality.
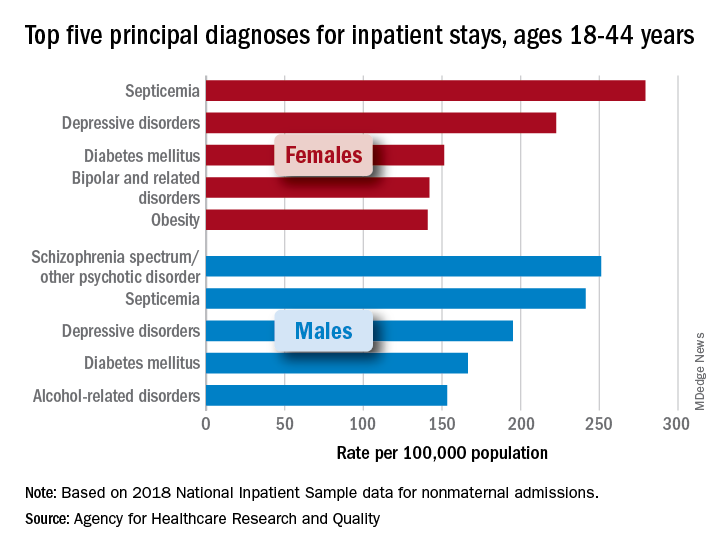
aged 18-44, while depressive disorders were the third-most common (195.0 stays per 100,000) and alcohol-related disorders were fifth at 153.2 per 100,000, Kimberly W. McDermott, PhD, and Marc Roemer, MS, said in an AHRQ statistical brief.
Prevalence was somewhat lower in women aged 18-44 years, with two mental illnesses appearing among the top five nonmaternal diagnoses: Depressive disorders were second at 222.5 stays per 100,000 and bipolar and related disorders were fourth at 142.0 per 100,000. The leading primary diagnosis in women in 2018 was septicemia, which was the most common cause overall in the age group at a rate of 279.3 per 100,000, the investigators reported.
There were no mental and/or substance use disorders in the top five primary diagnoses for any of the other adult age groups – 45-64, 65-74, and ≥75 – included in the report. Septicemia was the leading diagnosis for men in all three groups and for women in two of three (45-64 and ≥75), with osteoarthritis first among women aged 65-74 years, they said.
There was one mental illness among the top-five diagnoses for children under age 18 years, as depressive disorders were the most common reason for stays in girls (176.6 per 100,000 population) and the fifth most common for boys (74.0 per 100,000), said Dr. McDermott of IBM Watson Health and Mr. Roemer of AHRQ.
Septicemia was the leading nonmaternal, nonneonatal diagnosis for all inpatient stays and all ages in 2018 with a rate of 679.5 per 100,000, followed by heart failure (347.9), osteoarthritis (345.5), pneumonia not related to tuberculosis (226.8), and diabetes mellitus (207.8), based on data from the National Inpatient Sample.
Depressive disorders were most common mental health diagnosis in those admitted to hospitals and the 12th most common diagnosis overall; schizophrenia, in 16th place overall, was the only other mental illness among the top 20, the investigators said.
“This information can help establish national health priorities, initiatives, and action plans,” Dr. McDermott and Mr. Roemer wrote, and “at the hospital level, administrators can use diagnosis-related information to inform planning and resource allocation, such as optimizing subspecialty services or units for the care of high-priority conditions.”
More mental and/or substance use disorders are ranked among the top-five diagnoses for hospitalized men and women aged 18-44 years than for any other age group, according to a recent report from the Agency for Healthcare Research and Quality.
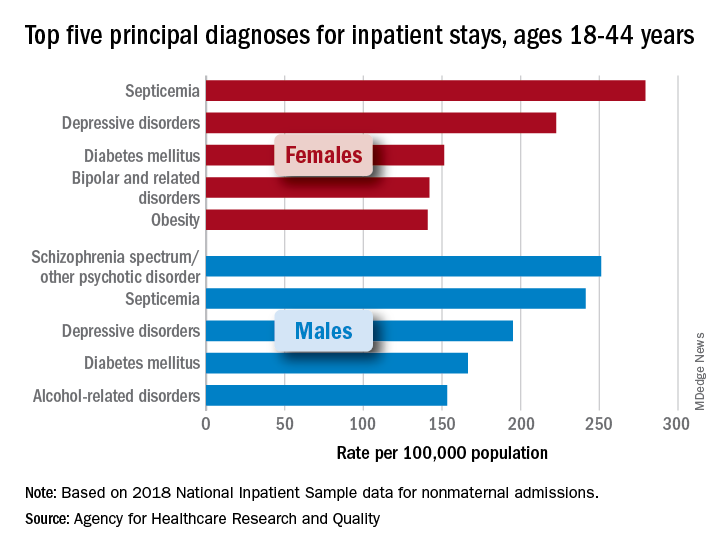
aged 18-44, while depressive disorders were the third-most common (195.0 stays per 100,000) and alcohol-related disorders were fifth at 153.2 per 100,000, Kimberly W. McDermott, PhD, and Marc Roemer, MS, said in an AHRQ statistical brief.
Prevalence was somewhat lower in women aged 18-44 years, with two mental illnesses appearing among the top five nonmaternal diagnoses: Depressive disorders were second at 222.5 stays per 100,000 and bipolar and related disorders were fourth at 142.0 per 100,000. The leading primary diagnosis in women in 2018 was septicemia, which was the most common cause overall in the age group at a rate of 279.3 per 100,000, the investigators reported.
There were no mental and/or substance use disorders in the top five primary diagnoses for any of the other adult age groups – 45-64, 65-74, and ≥75 – included in the report. Septicemia was the leading diagnosis for men in all three groups and for women in two of three (45-64 and ≥75), with osteoarthritis first among women aged 65-74 years, they said.
There was one mental illness among the top-five diagnoses for children under age 18 years, as depressive disorders were the most common reason for stays in girls (176.6 per 100,000 population) and the fifth most common for boys (74.0 per 100,000), said Dr. McDermott of IBM Watson Health and Mr. Roemer of AHRQ.
Septicemia was the leading nonmaternal, nonneonatal diagnosis for all inpatient stays and all ages in 2018 with a rate of 679.5 per 100,000, followed by heart failure (347.9), osteoarthritis (345.5), pneumonia not related to tuberculosis (226.8), and diabetes mellitus (207.8), based on data from the National Inpatient Sample.
Depressive disorders were most common mental health diagnosis in those admitted to hospitals and the 12th most common diagnosis overall; schizophrenia, in 16th place overall, was the only other mental illness among the top 20, the investigators said.
“This information can help establish national health priorities, initiatives, and action plans,” Dr. McDermott and Mr. Roemer wrote, and “at the hospital level, administrators can use diagnosis-related information to inform planning and resource allocation, such as optimizing subspecialty services or units for the care of high-priority conditions.”
More mental and/or substance use disorders are ranked among the top-five diagnoses for hospitalized men and women aged 18-44 years than for any other age group, according to a recent report from the Agency for Healthcare Research and Quality.
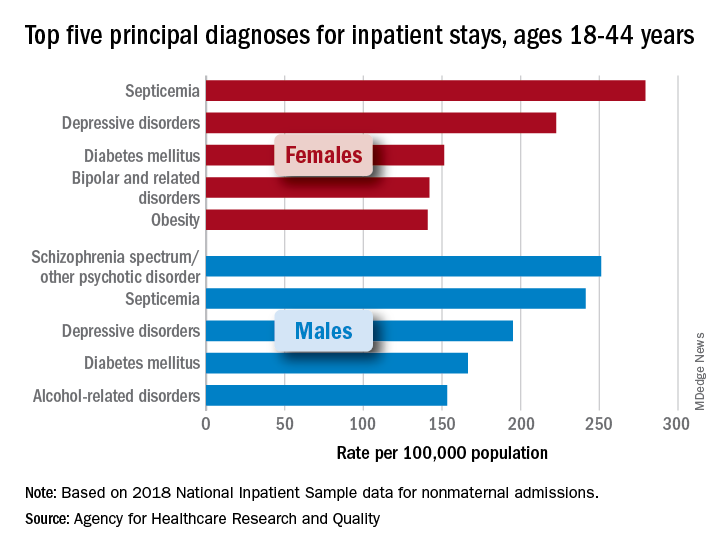
aged 18-44, while depressive disorders were the third-most common (195.0 stays per 100,000) and alcohol-related disorders were fifth at 153.2 per 100,000, Kimberly W. McDermott, PhD, and Marc Roemer, MS, said in an AHRQ statistical brief.
Prevalence was somewhat lower in women aged 18-44 years, with two mental illnesses appearing among the top five nonmaternal diagnoses: Depressive disorders were second at 222.5 stays per 100,000 and bipolar and related disorders were fourth at 142.0 per 100,000. The leading primary diagnosis in women in 2018 was septicemia, which was the most common cause overall in the age group at a rate of 279.3 per 100,000, the investigators reported.
There were no mental and/or substance use disorders in the top five primary diagnoses for any of the other adult age groups – 45-64, 65-74, and ≥75 – included in the report. Septicemia was the leading diagnosis for men in all three groups and for women in two of three (45-64 and ≥75), with osteoarthritis first among women aged 65-74 years, they said.
There was one mental illness among the top-five diagnoses for children under age 18 years, as depressive disorders were the most common reason for stays in girls (176.6 per 100,000 population) and the fifth most common for boys (74.0 per 100,000), said Dr. McDermott of IBM Watson Health and Mr. Roemer of AHRQ.
Septicemia was the leading nonmaternal, nonneonatal diagnosis for all inpatient stays and all ages in 2018 with a rate of 679.5 per 100,000, followed by heart failure (347.9), osteoarthritis (345.5), pneumonia not related to tuberculosis (226.8), and diabetes mellitus (207.8), based on data from the National Inpatient Sample.
Depressive disorders were most common mental health diagnosis in those admitted to hospitals and the 12th most common diagnosis overall; schizophrenia, in 16th place overall, was the only other mental illness among the top 20, the investigators said.
“This information can help establish national health priorities, initiatives, and action plans,” Dr. McDermott and Mr. Roemer wrote, and “at the hospital level, administrators can use diagnosis-related information to inform planning and resource allocation, such as optimizing subspecialty services or units for the care of high-priority conditions.”
Bronchitis the leader at putting children in the hospital

About 7% (99,000) of the 1.47 million nonmaternal, nonneonatal hospital stays in children aged 0-17 years involved a primary diagnosis of acute bronchitis in 2018, representing the leading cause of admissions in boys (154.7 stays per 100,000 population) and the second-leading diagnosis in girls (113.1 stays per 100,000), Kimberly W. McDermott, PhD, and Marc Roemer, MS, said in a statistical brief.
Depressive disorders were the most common primary diagnosis in girls, with a rate of 176.7 stays per 100,000, and the second-leading diagnosis overall, although the rate was less than half that (74.0 per 100,000) in boys. Two other respiratory conditions, asthma and pneumonia, were among the top five for both girls and boys, as was epilepsy, they reported.
The combined rate for all diagnoses was slightly higher for boys, 2,051 per 100,000, compared with 1,922 for girls, they said based on data from the National Inpatient Sample.
“Identifying the most frequent primary conditions for which patients are admitted to the hospital is important to the implementation and improvement of health care delivery, quality initiatives, and health policy,” said Dr. McDermott of IBM Watson Health and Mr. Roemer of the AHRQ.

About 7% (99,000) of the 1.47 million nonmaternal, nonneonatal hospital stays in children aged 0-17 years involved a primary diagnosis of acute bronchitis in 2018, representing the leading cause of admissions in boys (154.7 stays per 100,000 population) and the second-leading diagnosis in girls (113.1 stays per 100,000), Kimberly W. McDermott, PhD, and Marc Roemer, MS, said in a statistical brief.
Depressive disorders were the most common primary diagnosis in girls, with a rate of 176.7 stays per 100,000, and the second-leading diagnosis overall, although the rate was less than half that (74.0 per 100,000) in boys. Two other respiratory conditions, asthma and pneumonia, were among the top five for both girls and boys, as was epilepsy, they reported.
The combined rate for all diagnoses was slightly higher for boys, 2,051 per 100,000, compared with 1,922 for girls, they said based on data from the National Inpatient Sample.
“Identifying the most frequent primary conditions for which patients are admitted to the hospital is important to the implementation and improvement of health care delivery, quality initiatives, and health policy,” said Dr. McDermott of IBM Watson Health and Mr. Roemer of the AHRQ.

About 7% (99,000) of the 1.47 million nonmaternal, nonneonatal hospital stays in children aged 0-17 years involved a primary diagnosis of acute bronchitis in 2018, representing the leading cause of admissions in boys (154.7 stays per 100,000 population) and the second-leading diagnosis in girls (113.1 stays per 100,000), Kimberly W. McDermott, PhD, and Marc Roemer, MS, said in a statistical brief.
Depressive disorders were the most common primary diagnosis in girls, with a rate of 176.7 stays per 100,000, and the second-leading diagnosis overall, although the rate was less than half that (74.0 per 100,000) in boys. Two other respiratory conditions, asthma and pneumonia, were among the top five for both girls and boys, as was epilepsy, they reported.
The combined rate for all diagnoses was slightly higher for boys, 2,051 per 100,000, compared with 1,922 for girls, they said based on data from the National Inpatient Sample.
“Identifying the most frequent primary conditions for which patients are admitted to the hospital is important to the implementation and improvement of health care delivery, quality initiatives, and health policy,” said Dr. McDermott of IBM Watson Health and Mr. Roemer of the AHRQ.
COVID-19, hearings on Jan. 6 attack reignite interest in PTSD
After Sept. 11, 2001, and the subsequent long war in Iraq and Afghanistan, both mental health providers and the general public focused on posttraumatic stress disorder (PTSD). However, after almost 20 years of war and the COVID-19 epidemic, attention waned away from military service members and PTSD.
COVID-19–related PTSD and the hearings on the Jan. 6 attack on the Capitol have reignited interest in PTSD diagnosis and treatment. Testimony from police officers at the House select committee hearing about their experiences during the assault and PTSD was harrowing. One of the police officers had also served in Iraq, perhaps leading to “layered PTSD” – symptoms from war abroad and at home.
Thus, I thought a brief review of updates about diagnosis and treatment would be useful. Note: These are my opinions based on my extensive experience and do not represent the official opinion of my employer (MedStar Health).
PTSD was first classified as a disorder in 1980, based mainly on the experiences of military service members in Vietnam, as well as sexual assault victims and disaster survivors. Readers may look elsewhere for a fuller history of the disorder.
However, in brief, we have evolved from strict reliance on a variety of symptoms in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to a more global determination of the experience of trauma and related symptoms of distress. We still rely for diagnosis on trauma-related anxiety and depression symptoms, such as nightmare, flashbacks, numbness, and disassociation.
Treatment has evolved. Patients may benefit from treatment even if they do not meet all the PTSD criteria. As many of my colleagues who treat patients have said, “if it smells like PTSD, treat it like PTSD.”
What is the most effective treatment? The literature declares that evidence-based treatments include two selective serotonin reuptake inhibitors (Zoloft and Paxil) and several psychotherapies. The psychotherapies include cognitive-behavioral therapies, exposure therapy, and EMDR (eye movement desensitization reprocessing).
The problem is that many patients cannot tolerate these therapies. SSRIs do have side effects, the most distressing being sexual dysfunction. Many service members do not enter the psychotherapies, or they drop out of trials, because they cannot tolerate the reimagining of their trauma.
I now counsel patients about the “three buckets” of treatment. The first bucket is medication, which as a psychiatrist is what I focus on. The second bucket is psychotherapy as discussed above. The third bucket is “everything else.”
“Everything else” includes a variety of methods the patients can use to reduce symptoms of anxiety, depression, and PTSD symptoms: exercising; deep breathing through the nose; doing yoga; doing meditation; playing or working with animals; gardening; and engaging in other activities that “self sooth.” I also recommend always doing “small acts of kindness” for others. I myself contribute to food banks and bring cookies or watermelons to the staff at my hospital.
Why is this approach useful? A menu of options gives control back to the patient. It provides activities that can reduce anxiety. Thinking about caring for others helps patients get out of their own “swamp of distress.”
We do live in very difficult times. We’re coping with COVID-19 Delta variant, attacks on the Capitol, and gun violence. I have not yet mentioned climate change, which is extremely frightening to many of us. So all providers need to be aware of all the strategies at our disposal to treat anxiety, depression, and PTSD.
Dr. Ritchie is chair of psychiatry at Medstar Washington (D.C.) Hospital Center. She has no conflicts of interest.
After Sept. 11, 2001, and the subsequent long war in Iraq and Afghanistan, both mental health providers and the general public focused on posttraumatic stress disorder (PTSD). However, after almost 20 years of war and the COVID-19 epidemic, attention waned away from military service members and PTSD.
COVID-19–related PTSD and the hearings on the Jan. 6 attack on the Capitol have reignited interest in PTSD diagnosis and treatment. Testimony from police officers at the House select committee hearing about their experiences during the assault and PTSD was harrowing. One of the police officers had also served in Iraq, perhaps leading to “layered PTSD” – symptoms from war abroad and at home.
Thus, I thought a brief review of updates about diagnosis and treatment would be useful. Note: These are my opinions based on my extensive experience and do not represent the official opinion of my employer (MedStar Health).
PTSD was first classified as a disorder in 1980, based mainly on the experiences of military service members in Vietnam, as well as sexual assault victims and disaster survivors. Readers may look elsewhere for a fuller history of the disorder.
However, in brief, we have evolved from strict reliance on a variety of symptoms in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to a more global determination of the experience of trauma and related symptoms of distress. We still rely for diagnosis on trauma-related anxiety and depression symptoms, such as nightmare, flashbacks, numbness, and disassociation.
Treatment has evolved. Patients may benefit from treatment even if they do not meet all the PTSD criteria. As many of my colleagues who treat patients have said, “if it smells like PTSD, treat it like PTSD.”
What is the most effective treatment? The literature declares that evidence-based treatments include two selective serotonin reuptake inhibitors (Zoloft and Paxil) and several psychotherapies. The psychotherapies include cognitive-behavioral therapies, exposure therapy, and EMDR (eye movement desensitization reprocessing).
The problem is that many patients cannot tolerate these therapies. SSRIs do have side effects, the most distressing being sexual dysfunction. Many service members do not enter the psychotherapies, or they drop out of trials, because they cannot tolerate the reimagining of their trauma.
I now counsel patients about the “three buckets” of treatment. The first bucket is medication, which as a psychiatrist is what I focus on. The second bucket is psychotherapy as discussed above. The third bucket is “everything else.”
“Everything else” includes a variety of methods the patients can use to reduce symptoms of anxiety, depression, and PTSD symptoms: exercising; deep breathing through the nose; doing yoga; doing meditation; playing or working with animals; gardening; and engaging in other activities that “self sooth.” I also recommend always doing “small acts of kindness” for others. I myself contribute to food banks and bring cookies or watermelons to the staff at my hospital.
Why is this approach useful? A menu of options gives control back to the patient. It provides activities that can reduce anxiety. Thinking about caring for others helps patients get out of their own “swamp of distress.”
We do live in very difficult times. We’re coping with COVID-19 Delta variant, attacks on the Capitol, and gun violence. I have not yet mentioned climate change, which is extremely frightening to many of us. So all providers need to be aware of all the strategies at our disposal to treat anxiety, depression, and PTSD.
Dr. Ritchie is chair of psychiatry at Medstar Washington (D.C.) Hospital Center. She has no conflicts of interest.
After Sept. 11, 2001, and the subsequent long war in Iraq and Afghanistan, both mental health providers and the general public focused on posttraumatic stress disorder (PTSD). However, after almost 20 years of war and the COVID-19 epidemic, attention waned away from military service members and PTSD.
COVID-19–related PTSD and the hearings on the Jan. 6 attack on the Capitol have reignited interest in PTSD diagnosis and treatment. Testimony from police officers at the House select committee hearing about their experiences during the assault and PTSD was harrowing. One of the police officers had also served in Iraq, perhaps leading to “layered PTSD” – symptoms from war abroad and at home.
Thus, I thought a brief review of updates about diagnosis and treatment would be useful. Note: These are my opinions based on my extensive experience and do not represent the official opinion of my employer (MedStar Health).
PTSD was first classified as a disorder in 1980, based mainly on the experiences of military service members in Vietnam, as well as sexual assault victims and disaster survivors. Readers may look elsewhere for a fuller history of the disorder.
However, in brief, we have evolved from strict reliance on a variety of symptoms in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to a more global determination of the experience of trauma and related symptoms of distress. We still rely for diagnosis on trauma-related anxiety and depression symptoms, such as nightmare, flashbacks, numbness, and disassociation.
Treatment has evolved. Patients may benefit from treatment even if they do not meet all the PTSD criteria. As many of my colleagues who treat patients have said, “if it smells like PTSD, treat it like PTSD.”
What is the most effective treatment? The literature declares that evidence-based treatments include two selective serotonin reuptake inhibitors (Zoloft and Paxil) and several psychotherapies. The psychotherapies include cognitive-behavioral therapies, exposure therapy, and EMDR (eye movement desensitization reprocessing).
The problem is that many patients cannot tolerate these therapies. SSRIs do have side effects, the most distressing being sexual dysfunction. Many service members do not enter the psychotherapies, or they drop out of trials, because they cannot tolerate the reimagining of their trauma.
I now counsel patients about the “three buckets” of treatment. The first bucket is medication, which as a psychiatrist is what I focus on. The second bucket is psychotherapy as discussed above. The third bucket is “everything else.”
“Everything else” includes a variety of methods the patients can use to reduce symptoms of anxiety, depression, and PTSD symptoms: exercising; deep breathing through the nose; doing yoga; doing meditation; playing or working with animals; gardening; and engaging in other activities that “self sooth.” I also recommend always doing “small acts of kindness” for others. I myself contribute to food banks and bring cookies or watermelons to the staff at my hospital.
Why is this approach useful? A menu of options gives control back to the patient. It provides activities that can reduce anxiety. Thinking about caring for others helps patients get out of their own “swamp of distress.”
We do live in very difficult times. We’re coping with COVID-19 Delta variant, attacks on the Capitol, and gun violence. I have not yet mentioned climate change, which is extremely frightening to many of us. So all providers need to be aware of all the strategies at our disposal to treat anxiety, depression, and PTSD.
Dr. Ritchie is chair of psychiatry at Medstar Washington (D.C.) Hospital Center. She has no conflicts of interest.
Let’s talk about race
“I feel like my aggression is being racialized.” “Of course I wouldn’t call the cops if I felt like hurting myself. I’m Black.”
Those statements represent the heightened trauma our Black and Brown patients with mental health issues have been experiencing. In the wake of increasingly publicized police brutality against Black and Brown communities, the role race plays in mental health decompensation is evident. At this moment in time, we must continue to improve our understanding of the role race plays in psychiatric disorders. We must also ask ourselves: At times, does psychiatry worsen the traumas of the communities we serve?
Some psychiatrists are afraid to speak about race. They may believe it to be too “political.” But avoiding these necessary conversations perpetuates the trauma of those we treat. It suggests that physicians are ignorant of an issue at the forefront of patients’ mental health. Psychiatry, today, is primarily focused on the biological aspects of disease. We must not forget that psychiatry is biopsychosocial. It is imperative that psychiatrists have conversations about race – and its significance to our patients and their care.
Only 10.4% of psychiatrists in the United States comprise those considered underrepresented in medicine (URM). Yet, those very groups make up 32.6% of the U.S. population and are overrepresented in psychiatric hospitals.1 Many studies have shown that concordant racial backgrounds between patient and physician lead to a more positive patient experience2 and arguably, the subsequent potential for better health outcomes. Our efforts in addressing this disparity often fall short. URM applicants may be hesitant to join an institution where diversity is lacking or where they may be the only minority.3 While there is no simple solution, I propose that psychiatrists promote the importance of mental health to Black and Brown students of all ages by collaborating with schools and community leaders.
It is important to acknowledge that the lack of diversity within psychiatry is reflective of that among all physicians. This in part stems from the barriers to medical education that Black and Brown communities face. Those who start off with more resources or have parents who are physicians are at an advantage when trying to get into medical school. In fact, one in five medical students have a parent who is a physician4 and about three-fourths of students come from families whose income falls among the top two quintiles.5 Impoverished communities, which have a disproportionate share of Black and Brown people, cannot afford to take MCAT preparatory classes or to accept unpaid “resume building” opportunities. Many medical schools continue to place more weight on test scores and research/medical experiences, despite a shift to a more holistic review process. Institutions that have tried a different approach and accepted students from more diverse backgrounds may often overlook the challenges that URM students face while in medical school and fail to provide appropriate support resources.
The result is a failure to retain such students. A study conducted at Stony Brook (N.Y.) University showed that those underrepresented in medicine were six times more likely to get dismissed from medical school, and three times more likely to both withdraw or graduate beyond 4 years, compared with their White counterparts.6 This is a serious issue that needs to change on a structural and systemic level.
Any discussion of race and psychiatry must acknowledge psychiatry’s history of racism against Black and Brown communities to engage in racially informed discussions with our patients. Only then can we play a better role advocating against racism within the field in the future. Dating back to the 18th century, psychiatry has promoted ideologies that promote racism. Benjamin Rush, considered the “father of American Psychiatry,” believed that Black skin was a disease derived from leprosy called “negritude.” In the late 19th century, this twisted ideology continued with the invention of the term “drapetomania,” which was used to describe enslaved people who ran away as having a mental disorder.7 Black prisoners were subjected to experimental treatment with substances such as LSD and bulbocapnine to subdue them.8 This idea that minorities were dangerous and needed to be subdued translated into a higher number of schizophrenia diagnoses, particularly among Black men, as it was used as a tool to vilify them in the 1970s. Although schizophrenia is equally prevalent among Whites and non-Whites, Black people are four times more likely to be diagnosed, compared with their White counterparts, while Hispanics are three times more likely. Studies have shown that Black and Brown men are also more likely to receive higher doses of antipsychotics.9
Given this history, it is not surprising that Black and Brown representation within the field is lacking and that patients may be hesitant to share their feelings about race with us. While we can’t change history, we can take a stance condemning the harmful behavior of the past. The American Psychiatric Association issued an apology earlier this year to Black, Indigenous, and People of Color for its support in structural racism.10 This is a step in the right direction, but we need more than statements or performative actions. We need to amplify the voices of Black and Brown psychiatrists and patients, as well as highlight their current and past contributions to the field. While my educational experiences focused on the work of prominent White scholars, medical curricula should showcase the work of people like Solomon Carter Fuller, MD, a Black psychiatrist who was essential to understanding Alzheimer’s, or Joseph White, PhD, sometimes referred to as the “godfather of Black psychology.”11
At times, I have found myself witness to situations where colleagues make statements that not only do not condemn racism, but in fact encourage it. I have unfortunately heard some use the all-too-familiar rhetoric of reverse racism, such as: “They just assume I am racist because I am a White male” or “They’re being racist against me” or statements like “Don’t you think it is far-fetched to believe she was just sitting on a college campus doing nothing when the police were called?” Rhetoric such as this is problematic to the field of psychiatry and medicine as a whole – and only serves to further invalidate the feelings of our Black and Brown patients. We must increase exposure and education regarding racism to address this, especially the meaning of microaggressions, a concept many fail to understand.
Attention to the subject of racism has increased within medical schools and residency training programs in the wake of George Floyd’s death. However, most programs often make these lectures optional or only have one to two limited sessions. Furthermore, many do not make it mandatory for faculty to attend; they are arguably the most in need of this training given that they set the precedent of how to practice psychiatry. Some institutions have incorporated comprehensive antiracist curriculums into medical training. One model that has been successful is the Social Justice and Health Equity program within Yale University’s psychiatry residency. The curriculum has four tracks:
- Structural competency, which focuses on the mental health impact of extraclinical structures, for example a patient’s neighborhood and associated barriers of access.
- Human experience, which explores the interaction of patients and providers and how biases play a role.
- Advocacy, which teaches residents the written and oral skills to lobby for patient interests on a community and legislative level.
- History of psychiatry, which focuses on understanding psychiatry’s prior role in racism.
In each track, there are group discussions, cases led by faculty, and meetings with community leaders. Through this curriculum, residents learn about power, privilege, and how to interact with and advocate for patients in a way that promotes equity, rather than racial disparity.12,13 This is a model that other psychiatric residency programs can promote, emulate, and benefit from.
Educating ourselves will hopefully lead to a deeper introspection of how we interact with patients and if we are promoting antiracism through our attitude and actions. Reflecting on my own personal practice, I have noted that the interplay of race, mental health, and provider decision-making becomes particularly complex when dealing with situations in which a patient exhibits increased aggression or agitation. As a second-year psychiatric resident immersed in the inpatient world, I have become familiar with patients at higher risk and greater need. The first attempt toward de-escalation involves verbal cues without any other more intrusive measures. If that fails, intramuscular (IM) medications are typically considered. If a patient has a history of aggressive behavior, the threshold to use IM medications can decrease dramatically. This is mainly to protect ourselves and our nursing staff and to prioritize safety. While I understand this rationale, I wonder about the patient’s experience. What constitutes “aggressive” behavior? For patients who have had violence used against them because of their race or who have suffered from police brutality, having police present or threatening IM medications will increasingly trigger them and escalate the situation. The aftermath can deepen the distrust of psychiatry by Black and Brown people.
How do we then handle such situations in a way that both protects our staff from physical harm and protects our patients from racial trauma? While I don’t have a great answer, I think we can benefit from standardizing what we consider aggressive behavior and have specific criteria that patients need to exhibit before administering an IM medication. In addition, discussions with the team, including residents, nurses, and attending physicians, about how to address an emergent situation before it actually happens are essential. Specifically discussing the patient’s history and race and how it may affect the situation is not something to be shied away from. Lastly, in the event that an IM medication is administered and police are present, debriefing with the patient afterward is necessary. The patient may not be willing or able to listen to you or trust you, but taking accountability and acknowledging what happened, justified or not, is a part of the process of rebuilding rapport.
Both in the purview of the individual psychiatrist and the field of psychiatry as a whole, we need to examine our behavior and not be afraid to make changes for the betterment of our patients. We must learn to talk about race with our patients and in the process, advocate for more representation of Black and Brown psychiatrists, understanding the barriers faced by these communities when pursuing the medical field. We must educate ourselves on psychiatry’s history, and equip ourselves with knowledge and tools to promote antiracism and shape psychiatry’s future. We can then apply these very tools to challenging situations we may encounter daily with the ultimate goal of improving the mental health of our patients. This is the only way we will progress and ensure that psychiatry is an equitable, antiracist field. As Ibram X. Kendi, PhD, has written, “The heartbeat of antiracism is self-reflection, recognition, admission, and fundamentally self-critique.”
Dr. Malik is a second-year psychiatry resident at the University of California, San Diego. She has a background in policy and grassroots organizing through her time working at the National Coalition for the Homeless and the Women’s Law Project. Dr. Malik has no disclosures.
References
1. Wyse R et al. Acad Psychiatry. 2020 Oct;44(5):523-30.
2. Cooper LA et al. Ann Intern Med. 2003;139:907-15.
3. Pierre JM et al. Acad Psychiatry. 2017;41:226-32.
4. Hartocollis A. “Getting into med school without hard sciences.” New York Times. 2010 Jul 29.
5. AAMC. An updated look at the economic diversity of U.S. medical students. Analysis in Brief. 2018 Oct;18(5).
6. Rainey ML. How do we retain minority health professions students. In: Smedley BD et al. The right thing to do, the smart thing to do: Enhancing diversity in the health professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D. Institute of Medicine. National Academies Press. 2001.
7. Geller J. “Structural racism in American psychiatry and APA: Part 1.” Psychiatric News. 2020 Jun 23.
8. Mohr CL and Gordon JE. Tulane: The emergence of a modern university, 1945-1980. Louisiana State University Press, Baton Rouge. 2001.
9. Metzl JM. The protest psychosis: How schizophrenia became a Black disease. Beacon Press. 2010.
10. APA’s apology to Black, indigenous and people of color for its support of structural racism in psychiatry. American Psychiatric Association. 2021 Jan 18.
11. Black pioneers in mental health. Mental Health America. 2021.
12. Belli B. For Yale’s emerging psychiatrists, confronting racism is in the curriculum. Yale News. 2020 Jul 30.
13. Jordan A and Jackson D. Social justice and health equity curriculum. Yale School of Medicine. 2019 Sep 24.
“I feel like my aggression is being racialized.” “Of course I wouldn’t call the cops if I felt like hurting myself. I’m Black.”
Those statements represent the heightened trauma our Black and Brown patients with mental health issues have been experiencing. In the wake of increasingly publicized police brutality against Black and Brown communities, the role race plays in mental health decompensation is evident. At this moment in time, we must continue to improve our understanding of the role race plays in psychiatric disorders. We must also ask ourselves: At times, does psychiatry worsen the traumas of the communities we serve?
Some psychiatrists are afraid to speak about race. They may believe it to be too “political.” But avoiding these necessary conversations perpetuates the trauma of those we treat. It suggests that physicians are ignorant of an issue at the forefront of patients’ mental health. Psychiatry, today, is primarily focused on the biological aspects of disease. We must not forget that psychiatry is biopsychosocial. It is imperative that psychiatrists have conversations about race – and its significance to our patients and their care.
Only 10.4% of psychiatrists in the United States comprise those considered underrepresented in medicine (URM). Yet, those very groups make up 32.6% of the U.S. population and are overrepresented in psychiatric hospitals.1 Many studies have shown that concordant racial backgrounds between patient and physician lead to a more positive patient experience2 and arguably, the subsequent potential for better health outcomes. Our efforts in addressing this disparity often fall short. URM applicants may be hesitant to join an institution where diversity is lacking or where they may be the only minority.3 While there is no simple solution, I propose that psychiatrists promote the importance of mental health to Black and Brown students of all ages by collaborating with schools and community leaders.
It is important to acknowledge that the lack of diversity within psychiatry is reflective of that among all physicians. This in part stems from the barriers to medical education that Black and Brown communities face. Those who start off with more resources or have parents who are physicians are at an advantage when trying to get into medical school. In fact, one in five medical students have a parent who is a physician4 and about three-fourths of students come from families whose income falls among the top two quintiles.5 Impoverished communities, which have a disproportionate share of Black and Brown people, cannot afford to take MCAT preparatory classes or to accept unpaid “resume building” opportunities. Many medical schools continue to place more weight on test scores and research/medical experiences, despite a shift to a more holistic review process. Institutions that have tried a different approach and accepted students from more diverse backgrounds may often overlook the challenges that URM students face while in medical school and fail to provide appropriate support resources.
The result is a failure to retain such students. A study conducted at Stony Brook (N.Y.) University showed that those underrepresented in medicine were six times more likely to get dismissed from medical school, and three times more likely to both withdraw or graduate beyond 4 years, compared with their White counterparts.6 This is a serious issue that needs to change on a structural and systemic level.
Any discussion of race and psychiatry must acknowledge psychiatry’s history of racism against Black and Brown communities to engage in racially informed discussions with our patients. Only then can we play a better role advocating against racism within the field in the future. Dating back to the 18th century, psychiatry has promoted ideologies that promote racism. Benjamin Rush, considered the “father of American Psychiatry,” believed that Black skin was a disease derived from leprosy called “negritude.” In the late 19th century, this twisted ideology continued with the invention of the term “drapetomania,” which was used to describe enslaved people who ran away as having a mental disorder.7 Black prisoners were subjected to experimental treatment with substances such as LSD and bulbocapnine to subdue them.8 This idea that minorities were dangerous and needed to be subdued translated into a higher number of schizophrenia diagnoses, particularly among Black men, as it was used as a tool to vilify them in the 1970s. Although schizophrenia is equally prevalent among Whites and non-Whites, Black people are four times more likely to be diagnosed, compared with their White counterparts, while Hispanics are three times more likely. Studies have shown that Black and Brown men are also more likely to receive higher doses of antipsychotics.9
Given this history, it is not surprising that Black and Brown representation within the field is lacking and that patients may be hesitant to share their feelings about race with us. While we can’t change history, we can take a stance condemning the harmful behavior of the past. The American Psychiatric Association issued an apology earlier this year to Black, Indigenous, and People of Color for its support in structural racism.10 This is a step in the right direction, but we need more than statements or performative actions. We need to amplify the voices of Black and Brown psychiatrists and patients, as well as highlight their current and past contributions to the field. While my educational experiences focused on the work of prominent White scholars, medical curricula should showcase the work of people like Solomon Carter Fuller, MD, a Black psychiatrist who was essential to understanding Alzheimer’s, or Joseph White, PhD, sometimes referred to as the “godfather of Black psychology.”11
At times, I have found myself witness to situations where colleagues make statements that not only do not condemn racism, but in fact encourage it. I have unfortunately heard some use the all-too-familiar rhetoric of reverse racism, such as: “They just assume I am racist because I am a White male” or “They’re being racist against me” or statements like “Don’t you think it is far-fetched to believe she was just sitting on a college campus doing nothing when the police were called?” Rhetoric such as this is problematic to the field of psychiatry and medicine as a whole – and only serves to further invalidate the feelings of our Black and Brown patients. We must increase exposure and education regarding racism to address this, especially the meaning of microaggressions, a concept many fail to understand.
Attention to the subject of racism has increased within medical schools and residency training programs in the wake of George Floyd’s death. However, most programs often make these lectures optional or only have one to two limited sessions. Furthermore, many do not make it mandatory for faculty to attend; they are arguably the most in need of this training given that they set the precedent of how to practice psychiatry. Some institutions have incorporated comprehensive antiracist curriculums into medical training. One model that has been successful is the Social Justice and Health Equity program within Yale University’s psychiatry residency. The curriculum has four tracks:
- Structural competency, which focuses on the mental health impact of extraclinical structures, for example a patient’s neighborhood and associated barriers of access.
- Human experience, which explores the interaction of patients and providers and how biases play a role.
- Advocacy, which teaches residents the written and oral skills to lobby for patient interests on a community and legislative level.
- History of psychiatry, which focuses on understanding psychiatry’s prior role in racism.
In each track, there are group discussions, cases led by faculty, and meetings with community leaders. Through this curriculum, residents learn about power, privilege, and how to interact with and advocate for patients in a way that promotes equity, rather than racial disparity.12,13 This is a model that other psychiatric residency programs can promote, emulate, and benefit from.
Educating ourselves will hopefully lead to a deeper introspection of how we interact with patients and if we are promoting antiracism through our attitude and actions. Reflecting on my own personal practice, I have noted that the interplay of race, mental health, and provider decision-making becomes particularly complex when dealing with situations in which a patient exhibits increased aggression or agitation. As a second-year psychiatric resident immersed in the inpatient world, I have become familiar with patients at higher risk and greater need. The first attempt toward de-escalation involves verbal cues without any other more intrusive measures. If that fails, intramuscular (IM) medications are typically considered. If a patient has a history of aggressive behavior, the threshold to use IM medications can decrease dramatically. This is mainly to protect ourselves and our nursing staff and to prioritize safety. While I understand this rationale, I wonder about the patient’s experience. What constitutes “aggressive” behavior? For patients who have had violence used against them because of their race or who have suffered from police brutality, having police present or threatening IM medications will increasingly trigger them and escalate the situation. The aftermath can deepen the distrust of psychiatry by Black and Brown people.
How do we then handle such situations in a way that both protects our staff from physical harm and protects our patients from racial trauma? While I don’t have a great answer, I think we can benefit from standardizing what we consider aggressive behavior and have specific criteria that patients need to exhibit before administering an IM medication. In addition, discussions with the team, including residents, nurses, and attending physicians, about how to address an emergent situation before it actually happens are essential. Specifically discussing the patient’s history and race and how it may affect the situation is not something to be shied away from. Lastly, in the event that an IM medication is administered and police are present, debriefing with the patient afterward is necessary. The patient may not be willing or able to listen to you or trust you, but taking accountability and acknowledging what happened, justified or not, is a part of the process of rebuilding rapport.
Both in the purview of the individual psychiatrist and the field of psychiatry as a whole, we need to examine our behavior and not be afraid to make changes for the betterment of our patients. We must learn to talk about race with our patients and in the process, advocate for more representation of Black and Brown psychiatrists, understanding the barriers faced by these communities when pursuing the medical field. We must educate ourselves on psychiatry’s history, and equip ourselves with knowledge and tools to promote antiracism and shape psychiatry’s future. We can then apply these very tools to challenging situations we may encounter daily with the ultimate goal of improving the mental health of our patients. This is the only way we will progress and ensure that psychiatry is an equitable, antiracist field. As Ibram X. Kendi, PhD, has written, “The heartbeat of antiracism is self-reflection, recognition, admission, and fundamentally self-critique.”
Dr. Malik is a second-year psychiatry resident at the University of California, San Diego. She has a background in policy and grassroots organizing through her time working at the National Coalition for the Homeless and the Women’s Law Project. Dr. Malik has no disclosures.
References
1. Wyse R et al. Acad Psychiatry. 2020 Oct;44(5):523-30.
2. Cooper LA et al. Ann Intern Med. 2003;139:907-15.
3. Pierre JM et al. Acad Psychiatry. 2017;41:226-32.
4. Hartocollis A. “Getting into med school without hard sciences.” New York Times. 2010 Jul 29.
5. AAMC. An updated look at the economic diversity of U.S. medical students. Analysis in Brief. 2018 Oct;18(5).
6. Rainey ML. How do we retain minority health professions students. In: Smedley BD et al. The right thing to do, the smart thing to do: Enhancing diversity in the health professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D. Institute of Medicine. National Academies Press. 2001.
7. Geller J. “Structural racism in American psychiatry and APA: Part 1.” Psychiatric News. 2020 Jun 23.
8. Mohr CL and Gordon JE. Tulane: The emergence of a modern university, 1945-1980. Louisiana State University Press, Baton Rouge. 2001.
9. Metzl JM. The protest psychosis: How schizophrenia became a Black disease. Beacon Press. 2010.
10. APA’s apology to Black, indigenous and people of color for its support of structural racism in psychiatry. American Psychiatric Association. 2021 Jan 18.
11. Black pioneers in mental health. Mental Health America. 2021.
12. Belli B. For Yale’s emerging psychiatrists, confronting racism is in the curriculum. Yale News. 2020 Jul 30.
13. Jordan A and Jackson D. Social justice and health equity curriculum. Yale School of Medicine. 2019 Sep 24.
“I feel like my aggression is being racialized.” “Of course I wouldn’t call the cops if I felt like hurting myself. I’m Black.”
Those statements represent the heightened trauma our Black and Brown patients with mental health issues have been experiencing. In the wake of increasingly publicized police brutality against Black and Brown communities, the role race plays in mental health decompensation is evident. At this moment in time, we must continue to improve our understanding of the role race plays in psychiatric disorders. We must also ask ourselves: At times, does psychiatry worsen the traumas of the communities we serve?
Some psychiatrists are afraid to speak about race. They may believe it to be too “political.” But avoiding these necessary conversations perpetuates the trauma of those we treat. It suggests that physicians are ignorant of an issue at the forefront of patients’ mental health. Psychiatry, today, is primarily focused on the biological aspects of disease. We must not forget that psychiatry is biopsychosocial. It is imperative that psychiatrists have conversations about race – and its significance to our patients and their care.
Only 10.4% of psychiatrists in the United States comprise those considered underrepresented in medicine (URM). Yet, those very groups make up 32.6% of the U.S. population and are overrepresented in psychiatric hospitals.1 Many studies have shown that concordant racial backgrounds between patient and physician lead to a more positive patient experience2 and arguably, the subsequent potential for better health outcomes. Our efforts in addressing this disparity often fall short. URM applicants may be hesitant to join an institution where diversity is lacking or where they may be the only minority.3 While there is no simple solution, I propose that psychiatrists promote the importance of mental health to Black and Brown students of all ages by collaborating with schools and community leaders.
It is important to acknowledge that the lack of diversity within psychiatry is reflective of that among all physicians. This in part stems from the barriers to medical education that Black and Brown communities face. Those who start off with more resources or have parents who are physicians are at an advantage when trying to get into medical school. In fact, one in five medical students have a parent who is a physician4 and about three-fourths of students come from families whose income falls among the top two quintiles.5 Impoverished communities, which have a disproportionate share of Black and Brown people, cannot afford to take MCAT preparatory classes or to accept unpaid “resume building” opportunities. Many medical schools continue to place more weight on test scores and research/medical experiences, despite a shift to a more holistic review process. Institutions that have tried a different approach and accepted students from more diverse backgrounds may often overlook the challenges that URM students face while in medical school and fail to provide appropriate support resources.
The result is a failure to retain such students. A study conducted at Stony Brook (N.Y.) University showed that those underrepresented in medicine were six times more likely to get dismissed from medical school, and three times more likely to both withdraw or graduate beyond 4 years, compared with their White counterparts.6 This is a serious issue that needs to change on a structural and systemic level.
Any discussion of race and psychiatry must acknowledge psychiatry’s history of racism against Black and Brown communities to engage in racially informed discussions with our patients. Only then can we play a better role advocating against racism within the field in the future. Dating back to the 18th century, psychiatry has promoted ideologies that promote racism. Benjamin Rush, considered the “father of American Psychiatry,” believed that Black skin was a disease derived from leprosy called “negritude.” In the late 19th century, this twisted ideology continued with the invention of the term “drapetomania,” which was used to describe enslaved people who ran away as having a mental disorder.7 Black prisoners were subjected to experimental treatment with substances such as LSD and bulbocapnine to subdue them.8 This idea that minorities were dangerous and needed to be subdued translated into a higher number of schizophrenia diagnoses, particularly among Black men, as it was used as a tool to vilify them in the 1970s. Although schizophrenia is equally prevalent among Whites and non-Whites, Black people are four times more likely to be diagnosed, compared with their White counterparts, while Hispanics are three times more likely. Studies have shown that Black and Brown men are also more likely to receive higher doses of antipsychotics.9
Given this history, it is not surprising that Black and Brown representation within the field is lacking and that patients may be hesitant to share their feelings about race with us. While we can’t change history, we can take a stance condemning the harmful behavior of the past. The American Psychiatric Association issued an apology earlier this year to Black, Indigenous, and People of Color for its support in structural racism.10 This is a step in the right direction, but we need more than statements or performative actions. We need to amplify the voices of Black and Brown psychiatrists and patients, as well as highlight their current and past contributions to the field. While my educational experiences focused on the work of prominent White scholars, medical curricula should showcase the work of people like Solomon Carter Fuller, MD, a Black psychiatrist who was essential to understanding Alzheimer’s, or Joseph White, PhD, sometimes referred to as the “godfather of Black psychology.”11
At times, I have found myself witness to situations where colleagues make statements that not only do not condemn racism, but in fact encourage it. I have unfortunately heard some use the all-too-familiar rhetoric of reverse racism, such as: “They just assume I am racist because I am a White male” or “They’re being racist against me” or statements like “Don’t you think it is far-fetched to believe she was just sitting on a college campus doing nothing when the police were called?” Rhetoric such as this is problematic to the field of psychiatry and medicine as a whole – and only serves to further invalidate the feelings of our Black and Brown patients. We must increase exposure and education regarding racism to address this, especially the meaning of microaggressions, a concept many fail to understand.
Attention to the subject of racism has increased within medical schools and residency training programs in the wake of George Floyd’s death. However, most programs often make these lectures optional or only have one to two limited sessions. Furthermore, many do not make it mandatory for faculty to attend; they are arguably the most in need of this training given that they set the precedent of how to practice psychiatry. Some institutions have incorporated comprehensive antiracist curriculums into medical training. One model that has been successful is the Social Justice and Health Equity program within Yale University’s psychiatry residency. The curriculum has four tracks:
- Structural competency, which focuses on the mental health impact of extraclinical structures, for example a patient’s neighborhood and associated barriers of access.
- Human experience, which explores the interaction of patients and providers and how biases play a role.
- Advocacy, which teaches residents the written and oral skills to lobby for patient interests on a community and legislative level.
- History of psychiatry, which focuses on understanding psychiatry’s prior role in racism.
In each track, there are group discussions, cases led by faculty, and meetings with community leaders. Through this curriculum, residents learn about power, privilege, and how to interact with and advocate for patients in a way that promotes equity, rather than racial disparity.12,13 This is a model that other psychiatric residency programs can promote, emulate, and benefit from.
Educating ourselves will hopefully lead to a deeper introspection of how we interact with patients and if we are promoting antiracism through our attitude and actions. Reflecting on my own personal practice, I have noted that the interplay of race, mental health, and provider decision-making becomes particularly complex when dealing with situations in which a patient exhibits increased aggression or agitation. As a second-year psychiatric resident immersed in the inpatient world, I have become familiar with patients at higher risk and greater need. The first attempt toward de-escalation involves verbal cues without any other more intrusive measures. If that fails, intramuscular (IM) medications are typically considered. If a patient has a history of aggressive behavior, the threshold to use IM medications can decrease dramatically. This is mainly to protect ourselves and our nursing staff and to prioritize safety. While I understand this rationale, I wonder about the patient’s experience. What constitutes “aggressive” behavior? For patients who have had violence used against them because of their race or who have suffered from police brutality, having police present or threatening IM medications will increasingly trigger them and escalate the situation. The aftermath can deepen the distrust of psychiatry by Black and Brown people.
How do we then handle such situations in a way that both protects our staff from physical harm and protects our patients from racial trauma? While I don’t have a great answer, I think we can benefit from standardizing what we consider aggressive behavior and have specific criteria that patients need to exhibit before administering an IM medication. In addition, discussions with the team, including residents, nurses, and attending physicians, about how to address an emergent situation before it actually happens are essential. Specifically discussing the patient’s history and race and how it may affect the situation is not something to be shied away from. Lastly, in the event that an IM medication is administered and police are present, debriefing with the patient afterward is necessary. The patient may not be willing or able to listen to you or trust you, but taking accountability and acknowledging what happened, justified or not, is a part of the process of rebuilding rapport.
Both in the purview of the individual psychiatrist and the field of psychiatry as a whole, we need to examine our behavior and not be afraid to make changes for the betterment of our patients. We must learn to talk about race with our patients and in the process, advocate for more representation of Black and Brown psychiatrists, understanding the barriers faced by these communities when pursuing the medical field. We must educate ourselves on psychiatry’s history, and equip ourselves with knowledge and tools to promote antiracism and shape psychiatry’s future. We can then apply these very tools to challenging situations we may encounter daily with the ultimate goal of improving the mental health of our patients. This is the only way we will progress and ensure that psychiatry is an equitable, antiracist field. As Ibram X. Kendi, PhD, has written, “The heartbeat of antiracism is self-reflection, recognition, admission, and fundamentally self-critique.”
Dr. Malik is a second-year psychiatry resident at the University of California, San Diego. She has a background in policy and grassroots organizing through her time working at the National Coalition for the Homeless and the Women’s Law Project. Dr. Malik has no disclosures.
References
1. Wyse R et al. Acad Psychiatry. 2020 Oct;44(5):523-30.
2. Cooper LA et al. Ann Intern Med. 2003;139:907-15.
3. Pierre JM et al. Acad Psychiatry. 2017;41:226-32.
4. Hartocollis A. “Getting into med school without hard sciences.” New York Times. 2010 Jul 29.
5. AAMC. An updated look at the economic diversity of U.S. medical students. Analysis in Brief. 2018 Oct;18(5).
6. Rainey ML. How do we retain minority health professions students. In: Smedley BD et al. The right thing to do, the smart thing to do: Enhancing diversity in the health professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D. Institute of Medicine. National Academies Press. 2001.
7. Geller J. “Structural racism in American psychiatry and APA: Part 1.” Psychiatric News. 2020 Jun 23.
8. Mohr CL and Gordon JE. Tulane: The emergence of a modern university, 1945-1980. Louisiana State University Press, Baton Rouge. 2001.
9. Metzl JM. The protest psychosis: How schizophrenia became a Black disease. Beacon Press. 2010.
10. APA’s apology to Black, indigenous and people of color for its support of structural racism in psychiatry. American Psychiatric Association. 2021 Jan 18.
11. Black pioneers in mental health. Mental Health America. 2021.
12. Belli B. For Yale’s emerging psychiatrists, confronting racism is in the curriculum. Yale News. 2020 Jul 30.
13. Jordan A and Jackson D. Social justice and health equity curriculum. Yale School of Medicine. 2019 Sep 24.
MDs rebut claims of toxic culture after resident suicides
The tragic loss of three medical residents in our beloved South Bronx hospital shook us to the core. They were our colleagues and friends – promising young physicians whose lives and contributions to our hospital family will never be forgotten. We miss them and we grieve them.
We have been keenly aware of the growing trend of physician suicides across the country. That’s one of the reasons why, years ago, we established the nationally recognized Helping Healers Heal program across our health system and more recently expanded other mental health counseling and support to our frontline clinicians.
Our focus is wellness and prevention, as well as helping address the sadness, anxiety, and depression that so many of us experience after a traumatic event. During the surge of the COVID pandemic, these programs proved to be essential, as we expanded these services to all staff, not just those on the frontlines of patient care.
We share Dr. Pamela Wible’s concerns about the physician suicide crisis in this country. However, she misrepresented our residency program and made numerous statements that are false and simply hurtful.
Out of respect for our colleagues and their families, we cannot share everything that we know about this tragic and irreparable loss. But we must set the record straight about a number of incorrect references made by Dr. Wible:
1. We lost two residents to suicide. Though no less horrific, the third death was investigated and declared an accident by the police department.
2. Resident work hours and workload are closely monitored to follow guidance set by the New York State Department of Health and by ACGME. In fact, at the peak of the COVID pandemic, when we were caring for nearly 130 intubated patients at a time, we adopted a strict residency program schedule with built-in breaks and reduced shifts and hours. Even at that tasking time, no one worked more than 80 hours. Although the maximum number of patients assigned to an intern allowed by ACGME is 10, we rarely have more than five or six patients assigned to each of our interns.
3. We swiftly investigate any allegation and do not hesitate to take the appropriate action against anyone who does not honor our values of professionalism and respect.
4. Our ACGME survey results are close to the mean of all internal medicine residency programs in the country. The fact that the results range from 75% to 95% clearly indicates that residents respond independently, and there is no coaching.
5. No resident has ever been threatened to have their visa canceled or withdrawn. Never. And the implication that we were intolerant because of their nationality is reprehensible. At NYC Health + Hospitals, we celebrate diversity. We are deeply committed to serving everyone, regardless of where they come from, what language they speak, what religion they practice. If you spend one day, or one hour, in our facility, you will see and feel our pride and commitment to this mission. We take pride in the fact that our staff and residents reflect the diversity of the community we serve.
6. As for the allegations of “toxic culture at Lincoln” – many of our graduates chose to stay on as attendings, serve the local community, and train new residents. Out of the 67 attendings in our department, 24 are former graduates. They are being joined by another five graduates from this year’s graduating class. There is no better testament to how our graduates feel about our residency program, Department of Medicine, and Lincoln Hospital.
Dr. Wible poses a legitimate question: How to prevent another suicide. No one has the exact answer. But it is a question we will keep asking ourselves as we continue to do all we can to meet our residents’ needs, extend the social and mental health support they need to thrive, and provide the learning and training they need to offer the best care to our patients.
A version of this article first appeared on Medscape.com.
The tragic loss of three medical residents in our beloved South Bronx hospital shook us to the core. They were our colleagues and friends – promising young physicians whose lives and contributions to our hospital family will never be forgotten. We miss them and we grieve them.
We have been keenly aware of the growing trend of physician suicides across the country. That’s one of the reasons why, years ago, we established the nationally recognized Helping Healers Heal program across our health system and more recently expanded other mental health counseling and support to our frontline clinicians.
Our focus is wellness and prevention, as well as helping address the sadness, anxiety, and depression that so many of us experience after a traumatic event. During the surge of the COVID pandemic, these programs proved to be essential, as we expanded these services to all staff, not just those on the frontlines of patient care.
We share Dr. Pamela Wible’s concerns about the physician suicide crisis in this country. However, she misrepresented our residency program and made numerous statements that are false and simply hurtful.
Out of respect for our colleagues and their families, we cannot share everything that we know about this tragic and irreparable loss. But we must set the record straight about a number of incorrect references made by Dr. Wible:
1. We lost two residents to suicide. Though no less horrific, the third death was investigated and declared an accident by the police department.
2. Resident work hours and workload are closely monitored to follow guidance set by the New York State Department of Health and by ACGME. In fact, at the peak of the COVID pandemic, when we were caring for nearly 130 intubated patients at a time, we adopted a strict residency program schedule with built-in breaks and reduced shifts and hours. Even at that tasking time, no one worked more than 80 hours. Although the maximum number of patients assigned to an intern allowed by ACGME is 10, we rarely have more than five or six patients assigned to each of our interns.
3. We swiftly investigate any allegation and do not hesitate to take the appropriate action against anyone who does not honor our values of professionalism and respect.
4. Our ACGME survey results are close to the mean of all internal medicine residency programs in the country. The fact that the results range from 75% to 95% clearly indicates that residents respond independently, and there is no coaching.
5. No resident has ever been threatened to have their visa canceled or withdrawn. Never. And the implication that we were intolerant because of their nationality is reprehensible. At NYC Health + Hospitals, we celebrate diversity. We are deeply committed to serving everyone, regardless of where they come from, what language they speak, what religion they practice. If you spend one day, or one hour, in our facility, you will see and feel our pride and commitment to this mission. We take pride in the fact that our staff and residents reflect the diversity of the community we serve.
6. As for the allegations of “toxic culture at Lincoln” – many of our graduates chose to stay on as attendings, serve the local community, and train new residents. Out of the 67 attendings in our department, 24 are former graduates. They are being joined by another five graduates from this year’s graduating class. There is no better testament to how our graduates feel about our residency program, Department of Medicine, and Lincoln Hospital.
Dr. Wible poses a legitimate question: How to prevent another suicide. No one has the exact answer. But it is a question we will keep asking ourselves as we continue to do all we can to meet our residents’ needs, extend the social and mental health support they need to thrive, and provide the learning and training they need to offer the best care to our patients.
A version of this article first appeared on Medscape.com.
The tragic loss of three medical residents in our beloved South Bronx hospital shook us to the core. They were our colleagues and friends – promising young physicians whose lives and contributions to our hospital family will never be forgotten. We miss them and we grieve them.
We have been keenly aware of the growing trend of physician suicides across the country. That’s one of the reasons why, years ago, we established the nationally recognized Helping Healers Heal program across our health system and more recently expanded other mental health counseling and support to our frontline clinicians.
Our focus is wellness and prevention, as well as helping address the sadness, anxiety, and depression that so many of us experience after a traumatic event. During the surge of the COVID pandemic, these programs proved to be essential, as we expanded these services to all staff, not just those on the frontlines of patient care.
We share Dr. Pamela Wible’s concerns about the physician suicide crisis in this country. However, she misrepresented our residency program and made numerous statements that are false and simply hurtful.
Out of respect for our colleagues and their families, we cannot share everything that we know about this tragic and irreparable loss. But we must set the record straight about a number of incorrect references made by Dr. Wible:
1. We lost two residents to suicide. Though no less horrific, the third death was investigated and declared an accident by the police department.
2. Resident work hours and workload are closely monitored to follow guidance set by the New York State Department of Health and by ACGME. In fact, at the peak of the COVID pandemic, when we were caring for nearly 130 intubated patients at a time, we adopted a strict residency program schedule with built-in breaks and reduced shifts and hours. Even at that tasking time, no one worked more than 80 hours. Although the maximum number of patients assigned to an intern allowed by ACGME is 10, we rarely have more than five or six patients assigned to each of our interns.
3. We swiftly investigate any allegation and do not hesitate to take the appropriate action against anyone who does not honor our values of professionalism and respect.
4. Our ACGME survey results are close to the mean of all internal medicine residency programs in the country. The fact that the results range from 75% to 95% clearly indicates that residents respond independently, and there is no coaching.
5. No resident has ever been threatened to have their visa canceled or withdrawn. Never. And the implication that we were intolerant because of their nationality is reprehensible. At NYC Health + Hospitals, we celebrate diversity. We are deeply committed to serving everyone, regardless of where they come from, what language they speak, what religion they practice. If you spend one day, or one hour, in our facility, you will see and feel our pride and commitment to this mission. We take pride in the fact that our staff and residents reflect the diversity of the community we serve.
6. As for the allegations of “toxic culture at Lincoln” – many of our graduates chose to stay on as attendings, serve the local community, and train new residents. Out of the 67 attendings in our department, 24 are former graduates. They are being joined by another five graduates from this year’s graduating class. There is no better testament to how our graduates feel about our residency program, Department of Medicine, and Lincoln Hospital.
Dr. Wible poses a legitimate question: How to prevent another suicide. No one has the exact answer. But it is a question we will keep asking ourselves as we continue to do all we can to meet our residents’ needs, extend the social and mental health support they need to thrive, and provide the learning and training they need to offer the best care to our patients.
A version of this article first appeared on Medscape.com.
Ketamine and psychosis risk: New data
Ketamine used to treat severe depression in patients with a history of psychosis does not exacerbate psychosis risk, new research suggests.
A meta-analysis of nine studies, encompassing 41 patients with TRD and a history of psychosis, suggests ketamine is safe and effective and did not exacerbate psychotic symptoms in this patient population.
“We believe our findings could encourage clinicians and researchers to examine a broadened indication for ketamine treatment in individual patients with high levels of treatment resistance, carefully monitoring both clinical response and side effects, specifically looking at possible increases in psychotic symptoms,” study investigator Jolien K. E. Veraart, MD, University of Groningen, University Medical Center Groningen, the Netherlands, told this news organization.
The study was published online July 13 in the Journal of Clinical Psychiatry.
Rapid, robust effects
Ketamine has shown “rapid and robust antidepressant effects” in clinical studies. However, this research has not included patients with past or current psychosis, based on the assumption that psychosis will increase with ketamine administration, since side effects of ketamine can include transient “schizophrenia-like” psychotomimetic phenomena, including perceptual disorders and hallucinations in healthy individuals, the investigators note.
Dr. Veraart said psychotic symptoms are “common in people with severe depression,” and these patients have poorer outcomes with pharmacotherapy, psychotherapy, and electroconvulsive therapy.
Additionally, up to 60% of patients with schizophrenia experience negative symptomatology, including loss of motivation, affective blunting, and anhedonia, which “has a clear phenomenological overlap with depression,” the authors write. They also note anti-anhedonic effects of subanesthetic ketamine doses have been reported, without adversely impacting long-term psychotic symptoms in patients with schizophrenia.
“Positive results from carefully monitored trials with ketamine treatment in these patients have motivated us to summarize the currently available knowledge to inform our colleagues,” she said.
To investigate, the researchers conducted a literature search and selected 9 articles (N = 41 patients) that reported on ketamine treatment in patients with a history of psychosis or current psychotic symptoms.
All studies were either case reports or pilot studies, the authors report. Types of patients included those with bipolar or unipolar depression, or depression in schizoaffective disorder , or patients with schizophrenia and concurrent depression. Depressive symptomatology was the treatment target in eight studies, and one study targeted negative symptoms in patients with schizophrenia.
Dosing, frequency, and types of administration (ketamine IV, esketamine IV, or esketamine subcutaneous) varied from study to study.
In seven studies, ketamine was found to improve depressive symptoms, and in two studies, improvement in psychotic symptoms was also shown. Two studies revealed improvement in symptoms of suicidality. Results of the study that measured negative symptoms showed “significant improvement” in five of six patients, with a -37.3% decrease in mean Brief Negative Symptoms Scale (BNSS) from the baseline to the end of four infusions.
“Ketamine showed good antidepressant effects, and, in some cases, the comorbid symptoms even improved or disappeared after ketamine treatment,” Dr. Veraart summarized. However, the effect size of ketamine might be lower in those with a history of psychosis, she added.
She also noted that
She pointed to one study limitation, which is that only small, uncontrolled trials were included and that there is a risk for publication bias.
Larger trials needed
Commenting on the study, Dan Iosifescu, MD, MSc, associate professor of psychiatry, New York University School of Medicine, said that if the finding “were based on a larger study it would be very important, as a theoretical risk of psychosis is preventing such patients from access to an otherwise beneficial treatment.”
However, “since the review is based on a small sample, a low risk of psychosis exacerbation after IV ketamine is still possible,” said Dr. Iosifescu, who is also the director of clinical research at the Kline Institute for Psychiatric Research in Orangeburg, New York, and was not involved with the study.
Dr. Veraart agreed, adding that the “efficacy, safety, and tolerability of ketamine in depressed patients with a vulnerability to psychosis should be investigated in well-designed randomized controlled trials before application on a large scale is promoted.”
The study had no specific funding. Dr. Veraart has received speaker honoraria from Janssen outside of the submitted work. The other authors’ disclosures are listed in the original article. Dr. Iosifescu has been a consultant to the Centers of Psychiatric Excellence, advising clinics on the best methods of providing treatment with IV ketamine.
A version of this article first appeared on Medscape.com.
Ketamine used to treat severe depression in patients with a history of psychosis does not exacerbate psychosis risk, new research suggests.
A meta-analysis of nine studies, encompassing 41 patients with TRD and a history of psychosis, suggests ketamine is safe and effective and did not exacerbate psychotic symptoms in this patient population.
“We believe our findings could encourage clinicians and researchers to examine a broadened indication for ketamine treatment in individual patients with high levels of treatment resistance, carefully monitoring both clinical response and side effects, specifically looking at possible increases in psychotic symptoms,” study investigator Jolien K. E. Veraart, MD, University of Groningen, University Medical Center Groningen, the Netherlands, told this news organization.
The study was published online July 13 in the Journal of Clinical Psychiatry.
Rapid, robust effects
Ketamine has shown “rapid and robust antidepressant effects” in clinical studies. However, this research has not included patients with past or current psychosis, based on the assumption that psychosis will increase with ketamine administration, since side effects of ketamine can include transient “schizophrenia-like” psychotomimetic phenomena, including perceptual disorders and hallucinations in healthy individuals, the investigators note.
Dr. Veraart said psychotic symptoms are “common in people with severe depression,” and these patients have poorer outcomes with pharmacotherapy, psychotherapy, and electroconvulsive therapy.
Additionally, up to 60% of patients with schizophrenia experience negative symptomatology, including loss of motivation, affective blunting, and anhedonia, which “has a clear phenomenological overlap with depression,” the authors write. They also note anti-anhedonic effects of subanesthetic ketamine doses have been reported, without adversely impacting long-term psychotic symptoms in patients with schizophrenia.
“Positive results from carefully monitored trials with ketamine treatment in these patients have motivated us to summarize the currently available knowledge to inform our colleagues,” she said.
To investigate, the researchers conducted a literature search and selected 9 articles (N = 41 patients) that reported on ketamine treatment in patients with a history of psychosis or current psychotic symptoms.
All studies were either case reports or pilot studies, the authors report. Types of patients included those with bipolar or unipolar depression, or depression in schizoaffective disorder , or patients with schizophrenia and concurrent depression. Depressive symptomatology was the treatment target in eight studies, and one study targeted negative symptoms in patients with schizophrenia.
Dosing, frequency, and types of administration (ketamine IV, esketamine IV, or esketamine subcutaneous) varied from study to study.
In seven studies, ketamine was found to improve depressive symptoms, and in two studies, improvement in psychotic symptoms was also shown. Two studies revealed improvement in symptoms of suicidality. Results of the study that measured negative symptoms showed “significant improvement” in five of six patients, with a -37.3% decrease in mean Brief Negative Symptoms Scale (BNSS) from the baseline to the end of four infusions.
“Ketamine showed good antidepressant effects, and, in some cases, the comorbid symptoms even improved or disappeared after ketamine treatment,” Dr. Veraart summarized. However, the effect size of ketamine might be lower in those with a history of psychosis, she added.
She also noted that
She pointed to one study limitation, which is that only small, uncontrolled trials were included and that there is a risk for publication bias.
Larger trials needed
Commenting on the study, Dan Iosifescu, MD, MSc, associate professor of psychiatry, New York University School of Medicine, said that if the finding “were based on a larger study it would be very important, as a theoretical risk of psychosis is preventing such patients from access to an otherwise beneficial treatment.”
However, “since the review is based on a small sample, a low risk of psychosis exacerbation after IV ketamine is still possible,” said Dr. Iosifescu, who is also the director of clinical research at the Kline Institute for Psychiatric Research in Orangeburg, New York, and was not involved with the study.
Dr. Veraart agreed, adding that the “efficacy, safety, and tolerability of ketamine in depressed patients with a vulnerability to psychosis should be investigated in well-designed randomized controlled trials before application on a large scale is promoted.”
The study had no specific funding. Dr. Veraart has received speaker honoraria from Janssen outside of the submitted work. The other authors’ disclosures are listed in the original article. Dr. Iosifescu has been a consultant to the Centers of Psychiatric Excellence, advising clinics on the best methods of providing treatment with IV ketamine.
A version of this article first appeared on Medscape.com.
Ketamine used to treat severe depression in patients with a history of psychosis does not exacerbate psychosis risk, new research suggests.
A meta-analysis of nine studies, encompassing 41 patients with TRD and a history of psychosis, suggests ketamine is safe and effective and did not exacerbate psychotic symptoms in this patient population.
“We believe our findings could encourage clinicians and researchers to examine a broadened indication for ketamine treatment in individual patients with high levels of treatment resistance, carefully monitoring both clinical response and side effects, specifically looking at possible increases in psychotic symptoms,” study investigator Jolien K. E. Veraart, MD, University of Groningen, University Medical Center Groningen, the Netherlands, told this news organization.
The study was published online July 13 in the Journal of Clinical Psychiatry.
Rapid, robust effects
Ketamine has shown “rapid and robust antidepressant effects” in clinical studies. However, this research has not included patients with past or current psychosis, based on the assumption that psychosis will increase with ketamine administration, since side effects of ketamine can include transient “schizophrenia-like” psychotomimetic phenomena, including perceptual disorders and hallucinations in healthy individuals, the investigators note.
Dr. Veraart said psychotic symptoms are “common in people with severe depression,” and these patients have poorer outcomes with pharmacotherapy, psychotherapy, and electroconvulsive therapy.
Additionally, up to 60% of patients with schizophrenia experience negative symptomatology, including loss of motivation, affective blunting, and anhedonia, which “has a clear phenomenological overlap with depression,” the authors write. They also note anti-anhedonic effects of subanesthetic ketamine doses have been reported, without adversely impacting long-term psychotic symptoms in patients with schizophrenia.
“Positive results from carefully monitored trials with ketamine treatment in these patients have motivated us to summarize the currently available knowledge to inform our colleagues,” she said.
To investigate, the researchers conducted a literature search and selected 9 articles (N = 41 patients) that reported on ketamine treatment in patients with a history of psychosis or current psychotic symptoms.
All studies were either case reports or pilot studies, the authors report. Types of patients included those with bipolar or unipolar depression, or depression in schizoaffective disorder , or patients with schizophrenia and concurrent depression. Depressive symptomatology was the treatment target in eight studies, and one study targeted negative symptoms in patients with schizophrenia.
Dosing, frequency, and types of administration (ketamine IV, esketamine IV, or esketamine subcutaneous) varied from study to study.
In seven studies, ketamine was found to improve depressive symptoms, and in two studies, improvement in psychotic symptoms was also shown. Two studies revealed improvement in symptoms of suicidality. Results of the study that measured negative symptoms showed “significant improvement” in five of six patients, with a -37.3% decrease in mean Brief Negative Symptoms Scale (BNSS) from the baseline to the end of four infusions.
“Ketamine showed good antidepressant effects, and, in some cases, the comorbid symptoms even improved or disappeared after ketamine treatment,” Dr. Veraart summarized. However, the effect size of ketamine might be lower in those with a history of psychosis, she added.
She also noted that
She pointed to one study limitation, which is that only small, uncontrolled trials were included and that there is a risk for publication bias.
Larger trials needed
Commenting on the study, Dan Iosifescu, MD, MSc, associate professor of psychiatry, New York University School of Medicine, said that if the finding “were based on a larger study it would be very important, as a theoretical risk of psychosis is preventing such patients from access to an otherwise beneficial treatment.”
However, “since the review is based on a small sample, a low risk of psychosis exacerbation after IV ketamine is still possible,” said Dr. Iosifescu, who is also the director of clinical research at the Kline Institute for Psychiatric Research in Orangeburg, New York, and was not involved with the study.
Dr. Veraart agreed, adding that the “efficacy, safety, and tolerability of ketamine in depressed patients with a vulnerability to psychosis should be investigated in well-designed randomized controlled trials before application on a large scale is promoted.”
The study had no specific funding. Dr. Veraart has received speaker honoraria from Janssen outside of the submitted work. The other authors’ disclosures are listed in the original article. Dr. Iosifescu has been a consultant to the Centers of Psychiatric Excellence, advising clinics on the best methods of providing treatment with IV ketamine.
A version of this article first appeared on Medscape.com.
Church-based services may help close gaps in mental health care
Black individuals who received mental health services through a church-based program reported high levels of satisfaction, data from a small, qualitative study show.
“This model of providing mental health services adjacent to or supported by a trusted institution, with providers who may have a more nuanced and intimate knowledge of the experiences of and perceptions held by community members, may facilitate important therapy-mediating factors, such as trust,” wrote Angela Coombs, MD, of Columbia University, New York, and colleagues.
Black Americans continue to face barriers to mental health services, and fewer than one-third of Black Americans with a mental health condition receive formal mental health care, Dr. Coombs and colleagues reported. Barriers to treatment include stigma and distrust of medical institutions, and strategies are needed to address these barriers to improve access. Consequently, “one approach includes the development of mental health programming and supports with trusted institutions, such as churches,” they said. Data are limited, however, on the perspectives of individuals who have used church-based services.
In the study, published in Psychiatric Services, Dr. Coombs and colleagues recruited 15 adults aged 27-69 years who were receiving or had received mental health services at the HOPE (Healing On Purpose and Evolving) Center, a freestanding mental health clinic affiliated with the First Corinthian Baptist Church in Harlem, New York. At the time of the study in 2019, those attending the center (referred to as “innovators” rather than patients or clients to reduce stigma) received 10 free sessions of evidence-based psychotherapy.
Treatment included cognitive-behavioral therapy (CBT), religiously integrated CBT, and interpersonal psychotherapy (IPT) to individuals, couples, and families. Group psychotherapy also was an option. Clinicians at the HOPE Center included licensed social workers with doctoral and master’s-level degrees, as well as supervised social work student interns.
Study participants took part in a 30-minute interview, in person or by phone, with a female psychiatrist who was not employed by the HOPE Center or involved in treating the patients. There were 15 participants: 13 women and 2 men, with mean ages of 48 and 51 years, respectively; 14 identified as Black, non-Hispanic. Most (13 individuals) identified as heterosexual, 11 had never married, and 14 had some college or technical school education.
Notably, 11 participants reported attending church once a week, and 13 said they considered religion or spirituality highly important. Participants “reported that services that could integrate their spiritual beliefs with their current mental health challenges enhanced the therapeutic experience,” the researchers said.
Positive messaging about mental health care from the church and senior pastor also encouraged the participants to take advantage of the HOPE Center services.
As one participant said, “I’ve always believed that I can handle my own issues ... but listening to the pastor always talking about the [HOPE] Center and not to be ashamed if you have weaknesses, that’s when I said, ‘You know what, let me just start seeking mental health services because I really need [them].’ ”
, including recognizing cycles of unproductive behavior, processing traumatic experiences and learning self-love, and embracing meditation at home.
“A common theme among participants was that the HOPE Center provided them with tools to destress, process trauma, and manage anxiety,” the researchers wrote. In particular, several participants cited group sessions on teaching and practicing mindfulness as their favorite services. They described the HOPE Center as a positive, peaceful, and welcoming environment where they felt safe.
Cost issues were important as well. Participants noted that the HOPE Center’s ability to provide services that were free made it easier for them to attend. “Although participants said that it was helpful that the HOPE Center provided referrals to external providers and agencies for additional services, some said they wished that the HOPE Center would provide long-term therapy,” the researchers noted.
Overall, “most participants said that establishing more mental health resources within faith-based spaces could accelerate normalization of seeking and receiving mental health care within religious Black communities,” they said.
The study findings were limited by the absence of clinical data – and data on participants’ frequency and location of church attendance, the researchers noted. In addition, the positive results could be tied to selection bias, Dr. Coombs and colleagues said. Another possible limitation is the overrepresentation of cisgender women among the participants. Still, “the perspectives shared by participants suggest that this model of care may address several important barriers to care faced by some Black American populations,” the researchers wrote.
Bridging gap between spirituality and mental health
In an interview, Atasha Jordan, MD, said Black Americans with mental illnesses have long lacked equal access to mental health services. “However, in light of the COVID-19 pandemic, published studies have shown that rates of mental illness increased concurrently with a rise in spirituality and faith. That said, we currently live in a time where mental health and spirituality are more likely to intersect,” noted Dr. Jordan, of the University of Pennsylvania, Philadelphia.
She said it is not surprising that the study participants felt more comfortable receiving mental health services at a clinic that was church affiliated.
“We have known for years that people of faith are more likely to seek comfort for psychological distress from clergy, rather than mental health professionals. Providing a more familiar entry point to mental health services through a church-affiliated mental health clinic helps to bridge the existing gap between spirituality and mental health,” Dr. Jordan said. “For many Black Americans, spirituality is a central component of culturally-informed mental health care.
“Mental health providers may find improved service utilization and outcomes for their patients by collaborating with faith-based organizations or investing time to learn spiritually-based psychotherapies.”
Recently published data, notably a study published May 1, 2021, in Psychiatric Services, continue to support the existing knowledge “that many patients with psychiatric illnesses want increased attention paid to spirituality during their mental health care,” Dr. Jordan noted. “Moreover, they showed that nonreligious clinicians may be more apt than religious clinicians to provide objective, spiritually-oriented mental health care. In this vein, further research aimed at understanding the most effective methods to address spiritual health in times of mental distress can help all mental health providers better meet their patients’ psychiatric and psychological needs.”
Overcoming stigma, mistrust
During the pandemic, clinicians have seen an increase in mental health distress in the form of anxiety, depression, and trauma symptoms, Lorenzo Norris, MD, of George Washington University, Washington, said in an interview.
“Historically, African Americans have faced numerous barriers to mental health care, including stigma and mistrust of medical institutions,” Dr. Norris said. “At this time, perhaps more than in recent decades, novel ways of eliminating and navigating these barriers must be explored in an evidence-based fashion that will inform future interventions.”
Dr. Norris also found that the study findings make sense.
“Historically, the Black church has been a central institution in the community,” he said. “In my personal experience, the church served in a variety of roles, including but not limited to advocacy, employment, social services, peer support, and notably a trusted source of advice pertaining to health. In addition, Black churches may be in an ideal position to serve as culturally sensitive facilitators to build trust,” he said.
The study’s message for clinicians, according to Dr. Norris, is to “carefully consider partnering with faith-based organizations and community leaders if you want to supplement your efforts at decreasing mental health care disparities in the African American community.”
He pointed out, however, that in addition to the small number of participants, the study did not examine clinical outcomes. “So we must be careful how much we take from the initial conclusions,” Dr. Norris said.
Additional research is needed on a much larger scale to add support to the study findings, he said. “This study focused on one church and its particular program,” Dr. Norris noted. “There is likely a great deal of heterogeneity with Black churches and definitely among church members they serve,” he said. “Although it may be tempting to go with an ‘of course it will work’ approach, it is best to have additional qualitative and quantitative research of a much larger scale, with clinical controls that examine the ability of Black churches to address barriers African Americans face in receiving and utilizing mental health services,” he concluded.
Dr. Jordan disclosed receiving a 2021-2022 American Psychiatric Association/Substance Abuse and Mental Health Services Administration Minority Fellowship Program grant to study mental health literacy in the Black church. Dr. Norris disclosed serving as CEO of the Cleveland Clergy Alliance, a nonprofit organization providing outreach assistance as a mechanism to help seniors and the disabled population through community programming. The study authors reported no disclosures.
Black individuals who received mental health services through a church-based program reported high levels of satisfaction, data from a small, qualitative study show.
“This model of providing mental health services adjacent to or supported by a trusted institution, with providers who may have a more nuanced and intimate knowledge of the experiences of and perceptions held by community members, may facilitate important therapy-mediating factors, such as trust,” wrote Angela Coombs, MD, of Columbia University, New York, and colleagues.
Black Americans continue to face barriers to mental health services, and fewer than one-third of Black Americans with a mental health condition receive formal mental health care, Dr. Coombs and colleagues reported. Barriers to treatment include stigma and distrust of medical institutions, and strategies are needed to address these barriers to improve access. Consequently, “one approach includes the development of mental health programming and supports with trusted institutions, such as churches,” they said. Data are limited, however, on the perspectives of individuals who have used church-based services.
In the study, published in Psychiatric Services, Dr. Coombs and colleagues recruited 15 adults aged 27-69 years who were receiving or had received mental health services at the HOPE (Healing On Purpose and Evolving) Center, a freestanding mental health clinic affiliated with the First Corinthian Baptist Church in Harlem, New York. At the time of the study in 2019, those attending the center (referred to as “innovators” rather than patients or clients to reduce stigma) received 10 free sessions of evidence-based psychotherapy.
Treatment included cognitive-behavioral therapy (CBT), religiously integrated CBT, and interpersonal psychotherapy (IPT) to individuals, couples, and families. Group psychotherapy also was an option. Clinicians at the HOPE Center included licensed social workers with doctoral and master’s-level degrees, as well as supervised social work student interns.
Study participants took part in a 30-minute interview, in person or by phone, with a female psychiatrist who was not employed by the HOPE Center or involved in treating the patients. There were 15 participants: 13 women and 2 men, with mean ages of 48 and 51 years, respectively; 14 identified as Black, non-Hispanic. Most (13 individuals) identified as heterosexual, 11 had never married, and 14 had some college or technical school education.
Notably, 11 participants reported attending church once a week, and 13 said they considered religion or spirituality highly important. Participants “reported that services that could integrate their spiritual beliefs with their current mental health challenges enhanced the therapeutic experience,” the researchers said.
Positive messaging about mental health care from the church and senior pastor also encouraged the participants to take advantage of the HOPE Center services.
As one participant said, “I’ve always believed that I can handle my own issues ... but listening to the pastor always talking about the [HOPE] Center and not to be ashamed if you have weaknesses, that’s when I said, ‘You know what, let me just start seeking mental health services because I really need [them].’ ”
, including recognizing cycles of unproductive behavior, processing traumatic experiences and learning self-love, and embracing meditation at home.
“A common theme among participants was that the HOPE Center provided them with tools to destress, process trauma, and manage anxiety,” the researchers wrote. In particular, several participants cited group sessions on teaching and practicing mindfulness as their favorite services. They described the HOPE Center as a positive, peaceful, and welcoming environment where they felt safe.
Cost issues were important as well. Participants noted that the HOPE Center’s ability to provide services that were free made it easier for them to attend. “Although participants said that it was helpful that the HOPE Center provided referrals to external providers and agencies for additional services, some said they wished that the HOPE Center would provide long-term therapy,” the researchers noted.
Overall, “most participants said that establishing more mental health resources within faith-based spaces could accelerate normalization of seeking and receiving mental health care within religious Black communities,” they said.
The study findings were limited by the absence of clinical data – and data on participants’ frequency and location of church attendance, the researchers noted. In addition, the positive results could be tied to selection bias, Dr. Coombs and colleagues said. Another possible limitation is the overrepresentation of cisgender women among the participants. Still, “the perspectives shared by participants suggest that this model of care may address several important barriers to care faced by some Black American populations,” the researchers wrote.
Bridging gap between spirituality and mental health
In an interview, Atasha Jordan, MD, said Black Americans with mental illnesses have long lacked equal access to mental health services. “However, in light of the COVID-19 pandemic, published studies have shown that rates of mental illness increased concurrently with a rise in spirituality and faith. That said, we currently live in a time where mental health and spirituality are more likely to intersect,” noted Dr. Jordan, of the University of Pennsylvania, Philadelphia.
She said it is not surprising that the study participants felt more comfortable receiving mental health services at a clinic that was church affiliated.
“We have known for years that people of faith are more likely to seek comfort for psychological distress from clergy, rather than mental health professionals. Providing a more familiar entry point to mental health services through a church-affiliated mental health clinic helps to bridge the existing gap between spirituality and mental health,” Dr. Jordan said. “For many Black Americans, spirituality is a central component of culturally-informed mental health care.
“Mental health providers may find improved service utilization and outcomes for their patients by collaborating with faith-based organizations or investing time to learn spiritually-based psychotherapies.”
Recently published data, notably a study published May 1, 2021, in Psychiatric Services, continue to support the existing knowledge “that many patients with psychiatric illnesses want increased attention paid to spirituality during their mental health care,” Dr. Jordan noted. “Moreover, they showed that nonreligious clinicians may be more apt than religious clinicians to provide objective, spiritually-oriented mental health care. In this vein, further research aimed at understanding the most effective methods to address spiritual health in times of mental distress can help all mental health providers better meet their patients’ psychiatric and psychological needs.”
Overcoming stigma, mistrust
During the pandemic, clinicians have seen an increase in mental health distress in the form of anxiety, depression, and trauma symptoms, Lorenzo Norris, MD, of George Washington University, Washington, said in an interview.
“Historically, African Americans have faced numerous barriers to mental health care, including stigma and mistrust of medical institutions,” Dr. Norris said. “At this time, perhaps more than in recent decades, novel ways of eliminating and navigating these barriers must be explored in an evidence-based fashion that will inform future interventions.”
Dr. Norris also found that the study findings make sense.
“Historically, the Black church has been a central institution in the community,” he said. “In my personal experience, the church served in a variety of roles, including but not limited to advocacy, employment, social services, peer support, and notably a trusted source of advice pertaining to health. In addition, Black churches may be in an ideal position to serve as culturally sensitive facilitators to build trust,” he said.
The study’s message for clinicians, according to Dr. Norris, is to “carefully consider partnering with faith-based organizations and community leaders if you want to supplement your efforts at decreasing mental health care disparities in the African American community.”
He pointed out, however, that in addition to the small number of participants, the study did not examine clinical outcomes. “So we must be careful how much we take from the initial conclusions,” Dr. Norris said.
Additional research is needed on a much larger scale to add support to the study findings, he said. “This study focused on one church and its particular program,” Dr. Norris noted. “There is likely a great deal of heterogeneity with Black churches and definitely among church members they serve,” he said. “Although it may be tempting to go with an ‘of course it will work’ approach, it is best to have additional qualitative and quantitative research of a much larger scale, with clinical controls that examine the ability of Black churches to address barriers African Americans face in receiving and utilizing mental health services,” he concluded.
Dr. Jordan disclosed receiving a 2021-2022 American Psychiatric Association/Substance Abuse and Mental Health Services Administration Minority Fellowship Program grant to study mental health literacy in the Black church. Dr. Norris disclosed serving as CEO of the Cleveland Clergy Alliance, a nonprofit organization providing outreach assistance as a mechanism to help seniors and the disabled population through community programming. The study authors reported no disclosures.
Black individuals who received mental health services through a church-based program reported high levels of satisfaction, data from a small, qualitative study show.
“This model of providing mental health services adjacent to or supported by a trusted institution, with providers who may have a more nuanced and intimate knowledge of the experiences of and perceptions held by community members, may facilitate important therapy-mediating factors, such as trust,” wrote Angela Coombs, MD, of Columbia University, New York, and colleagues.
Black Americans continue to face barriers to mental health services, and fewer than one-third of Black Americans with a mental health condition receive formal mental health care, Dr. Coombs and colleagues reported. Barriers to treatment include stigma and distrust of medical institutions, and strategies are needed to address these barriers to improve access. Consequently, “one approach includes the development of mental health programming and supports with trusted institutions, such as churches,” they said. Data are limited, however, on the perspectives of individuals who have used church-based services.
In the study, published in Psychiatric Services, Dr. Coombs and colleagues recruited 15 adults aged 27-69 years who were receiving or had received mental health services at the HOPE (Healing On Purpose and Evolving) Center, a freestanding mental health clinic affiliated with the First Corinthian Baptist Church in Harlem, New York. At the time of the study in 2019, those attending the center (referred to as “innovators” rather than patients or clients to reduce stigma) received 10 free sessions of evidence-based psychotherapy.
Treatment included cognitive-behavioral therapy (CBT), religiously integrated CBT, and interpersonal psychotherapy (IPT) to individuals, couples, and families. Group psychotherapy also was an option. Clinicians at the HOPE Center included licensed social workers with doctoral and master’s-level degrees, as well as supervised social work student interns.
Study participants took part in a 30-minute interview, in person or by phone, with a female psychiatrist who was not employed by the HOPE Center or involved in treating the patients. There were 15 participants: 13 women and 2 men, with mean ages of 48 and 51 years, respectively; 14 identified as Black, non-Hispanic. Most (13 individuals) identified as heterosexual, 11 had never married, and 14 had some college or technical school education.
Notably, 11 participants reported attending church once a week, and 13 said they considered religion or spirituality highly important. Participants “reported that services that could integrate their spiritual beliefs with their current mental health challenges enhanced the therapeutic experience,” the researchers said.
Positive messaging about mental health care from the church and senior pastor also encouraged the participants to take advantage of the HOPE Center services.
As one participant said, “I’ve always believed that I can handle my own issues ... but listening to the pastor always talking about the [HOPE] Center and not to be ashamed if you have weaknesses, that’s when I said, ‘You know what, let me just start seeking mental health services because I really need [them].’ ”
, including recognizing cycles of unproductive behavior, processing traumatic experiences and learning self-love, and embracing meditation at home.
“A common theme among participants was that the HOPE Center provided them with tools to destress, process trauma, and manage anxiety,” the researchers wrote. In particular, several participants cited group sessions on teaching and practicing mindfulness as their favorite services. They described the HOPE Center as a positive, peaceful, and welcoming environment where they felt safe.
Cost issues were important as well. Participants noted that the HOPE Center’s ability to provide services that were free made it easier for them to attend. “Although participants said that it was helpful that the HOPE Center provided referrals to external providers and agencies for additional services, some said they wished that the HOPE Center would provide long-term therapy,” the researchers noted.
Overall, “most participants said that establishing more mental health resources within faith-based spaces could accelerate normalization of seeking and receiving mental health care within religious Black communities,” they said.
The study findings were limited by the absence of clinical data – and data on participants’ frequency and location of church attendance, the researchers noted. In addition, the positive results could be tied to selection bias, Dr. Coombs and colleagues said. Another possible limitation is the overrepresentation of cisgender women among the participants. Still, “the perspectives shared by participants suggest that this model of care may address several important barriers to care faced by some Black American populations,” the researchers wrote.
Bridging gap between spirituality and mental health
In an interview, Atasha Jordan, MD, said Black Americans with mental illnesses have long lacked equal access to mental health services. “However, in light of the COVID-19 pandemic, published studies have shown that rates of mental illness increased concurrently with a rise in spirituality and faith. That said, we currently live in a time where mental health and spirituality are more likely to intersect,” noted Dr. Jordan, of the University of Pennsylvania, Philadelphia.
She said it is not surprising that the study participants felt more comfortable receiving mental health services at a clinic that was church affiliated.
“We have known for years that people of faith are more likely to seek comfort for psychological distress from clergy, rather than mental health professionals. Providing a more familiar entry point to mental health services through a church-affiliated mental health clinic helps to bridge the existing gap between spirituality and mental health,” Dr. Jordan said. “For many Black Americans, spirituality is a central component of culturally-informed mental health care.
“Mental health providers may find improved service utilization and outcomes for their patients by collaborating with faith-based organizations or investing time to learn spiritually-based psychotherapies.”
Recently published data, notably a study published May 1, 2021, in Psychiatric Services, continue to support the existing knowledge “that many patients with psychiatric illnesses want increased attention paid to spirituality during their mental health care,” Dr. Jordan noted. “Moreover, they showed that nonreligious clinicians may be more apt than religious clinicians to provide objective, spiritually-oriented mental health care. In this vein, further research aimed at understanding the most effective methods to address spiritual health in times of mental distress can help all mental health providers better meet their patients’ psychiatric and psychological needs.”
Overcoming stigma, mistrust
During the pandemic, clinicians have seen an increase in mental health distress in the form of anxiety, depression, and trauma symptoms, Lorenzo Norris, MD, of George Washington University, Washington, said in an interview.
“Historically, African Americans have faced numerous barriers to mental health care, including stigma and mistrust of medical institutions,” Dr. Norris said. “At this time, perhaps more than in recent decades, novel ways of eliminating and navigating these barriers must be explored in an evidence-based fashion that will inform future interventions.”
Dr. Norris also found that the study findings make sense.
“Historically, the Black church has been a central institution in the community,” he said. “In my personal experience, the church served in a variety of roles, including but not limited to advocacy, employment, social services, peer support, and notably a trusted source of advice pertaining to health. In addition, Black churches may be in an ideal position to serve as culturally sensitive facilitators to build trust,” he said.
The study’s message for clinicians, according to Dr. Norris, is to “carefully consider partnering with faith-based organizations and community leaders if you want to supplement your efforts at decreasing mental health care disparities in the African American community.”
He pointed out, however, that in addition to the small number of participants, the study did not examine clinical outcomes. “So we must be careful how much we take from the initial conclusions,” Dr. Norris said.
Additional research is needed on a much larger scale to add support to the study findings, he said. “This study focused on one church and its particular program,” Dr. Norris noted. “There is likely a great deal of heterogeneity with Black churches and definitely among church members they serve,” he said. “Although it may be tempting to go with an ‘of course it will work’ approach, it is best to have additional qualitative and quantitative research of a much larger scale, with clinical controls that examine the ability of Black churches to address barriers African Americans face in receiving and utilizing mental health services,” he concluded.
Dr. Jordan disclosed receiving a 2021-2022 American Psychiatric Association/Substance Abuse and Mental Health Services Administration Minority Fellowship Program grant to study mental health literacy in the Black church. Dr. Norris disclosed serving as CEO of the Cleveland Clergy Alliance, a nonprofit organization providing outreach assistance as a mechanism to help seniors and the disabled population through community programming. The study authors reported no disclosures.
FROM PSYCHIATRIC SERVICES