User login
The hateful patient
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
FDA OKs stimulation device for anxiety in depression
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.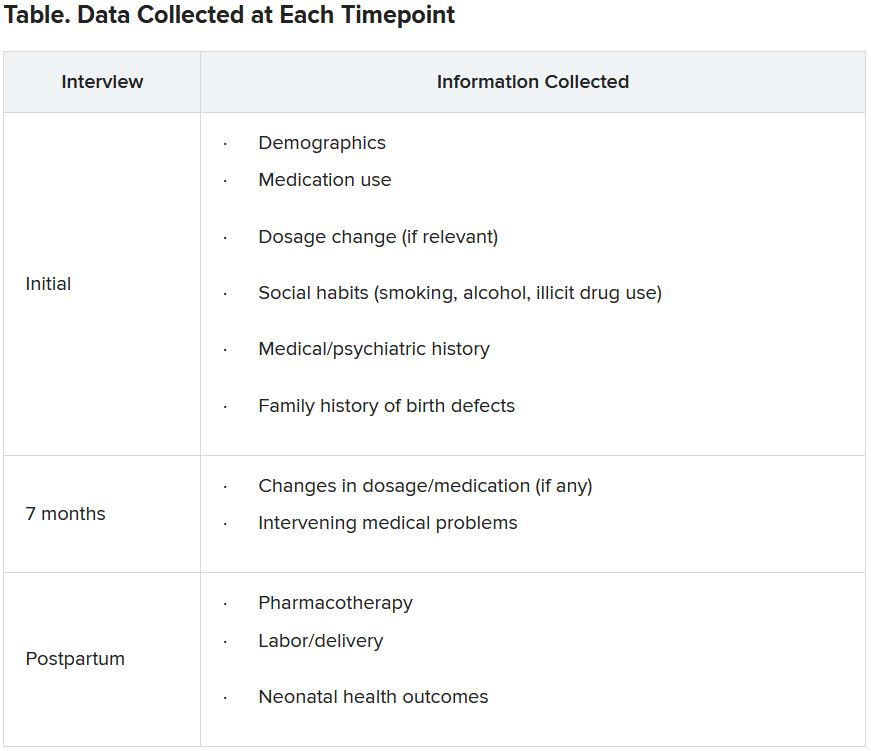
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.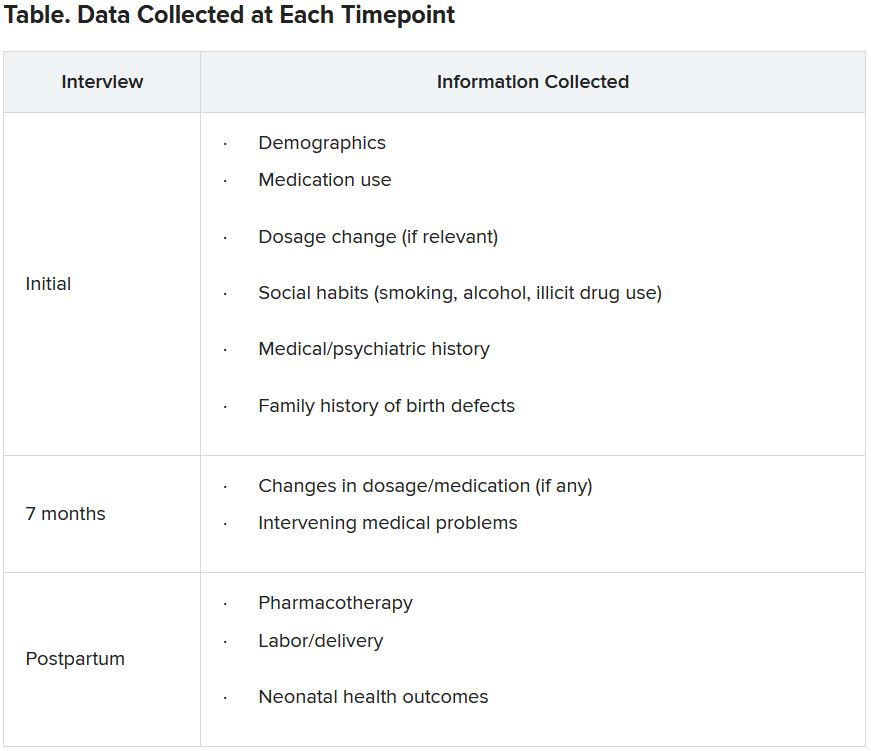
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.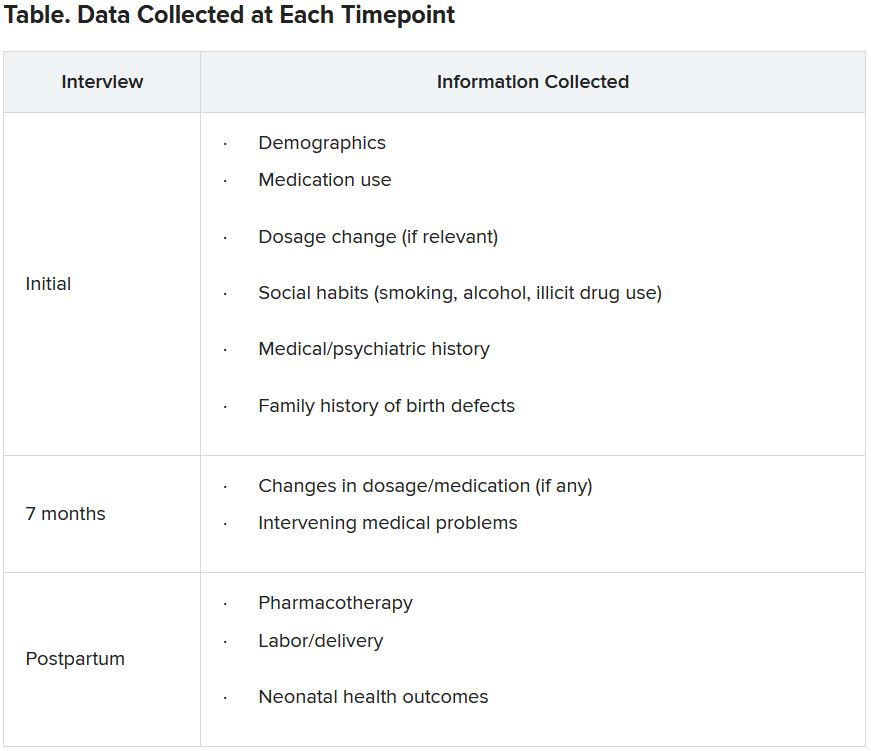
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Shedding the super-doctor myth requires an honest look at systemic racism
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Obesity leads to depression via social and metabolic factors
New research provides further evidence that a high body mass index (BMI) leads to depressed mood and poor well-being via social and physical factors.
Obesity and depression are “major global health challenges; our findings suggest that reducing obesity will lower depression and improve well-being,” co–lead author Jessica O’Loughlin, PhD student, University of Exeter Medical School, United Kingdom, told this news organization.
“Doctors should consider both the biological consequences of having a higher BMI as well as the social implications when treating patients with obesity in order to help reduce the odds of them developing depression,” Ms. O’Loughlin added.
The study was published online July 16 in Human Molecular Genetics.
Large body of evidence
A large body of evidence indicates that higher BMI leads to depression.
Ms. O’Loughlin and colleagues leveraged genetic data from more than 145,000 individuals in the UK Biobank and Mendelian randomization to determine whether the causal link between high BMI and depression is the result of psychosocial pathways, physical pathways, or both.
The analysis showed that a genetically determined 1 standard deviation higher BMI (4.6 kg/m2) was associated with higher likelihood of depression (odds ratio, 1.50; 95% confidence interval, 1.15-1.95) and lower well-being (beta, -0.15; 95% CI, -0.26 to -0.04).
Using genetics to distinguish metabolic and psychosocial effects, the results also indicate that, even in the absence of adverse metabolic effects, “higher adiposity remains causal to depression and lowers wellbeing,” the researchers report.
“ and when using genetic variants that make you fatter but metabolically healthier (favorable adiposity genetic variants),” said Ms. O’Loughlin.
“Although we can’t tell which factor plays a bigger role in the adiposity-depression relationship, our analysis suggests that both physical and social factors (e.g., social stigma) play a role in the relationship between higher BMI and higher odds of depression,” she added.
In contrast, there was little evidence that higher BMI in the presence or absence of adverse metabolic consequences causes generalized anxiety disorder.
“Finding ways to support people to lose weight could benefit their mental health as well as their physical health,” co–lead author Francesco Casanova, PhD, with the University of Exeter, said in a statement.
Unexpected finding
Reached for comment, Samoon Ahmad, MD, professor, department of psychiatry, New York University, said that “multiple studies have shown a correlation between stress, obesity, inflammation, overall well-being, and psychiatric disorders, particularly depressive and anxiety disorders.”
He said this new study is important for three reasons.
“The first is the cohort size. There were over 145,000 participants involved in the study, which is significant and serves to make its conclusions stronger,” Dr. Ahmad noted.
“The second point is that the authors found that the correlation between higher adiposity and depression and lower well-being scores occurred even in patients without adverse metabolic effects,” he said in an interview.
“Of note, obesity significantly increases the risk of developing type 2 diabetes, hypertension, and a host of other illnesses as well as inflammatory conditions, which can all have a negative impact on quality of life. Consequently, these can contribute to depression as well as anxiety,” Dr. Ahmad added.
“Interestingly, what this study suggests is that even people without these additional stressors are reporting higher rates of depression and lower scores of well-being, while higher adiposity is the common denominator,” he noted.
“Third, the paper found little to no correlation between higher adiposity and generalized anxiety disorder. This comes as a complete surprise because anxiety and depression are very common comorbidities,” Dr. Ahmad said.
“Moreover, numerous studies as well as clinical data suggest that obesity leads to chronic inflammation, which in turn is associated with less favorable metabolic profiles, and that anxiety and depressive disorders may in some way be psychiatric manifestations of inflammation. To see one but not the other was quite an unexpected finding,” Dr. Ahmad said.
The study was funded by the Academy of Medical Sciences. Ms. O’Loughlin, Dr. Casanova, and Dr. Ahmad have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New research provides further evidence that a high body mass index (BMI) leads to depressed mood and poor well-being via social and physical factors.
Obesity and depression are “major global health challenges; our findings suggest that reducing obesity will lower depression and improve well-being,” co–lead author Jessica O’Loughlin, PhD student, University of Exeter Medical School, United Kingdom, told this news organization.
“Doctors should consider both the biological consequences of having a higher BMI as well as the social implications when treating patients with obesity in order to help reduce the odds of them developing depression,” Ms. O’Loughlin added.
The study was published online July 16 in Human Molecular Genetics.
Large body of evidence
A large body of evidence indicates that higher BMI leads to depression.
Ms. O’Loughlin and colleagues leveraged genetic data from more than 145,000 individuals in the UK Biobank and Mendelian randomization to determine whether the causal link between high BMI and depression is the result of psychosocial pathways, physical pathways, or both.
The analysis showed that a genetically determined 1 standard deviation higher BMI (4.6 kg/m2) was associated with higher likelihood of depression (odds ratio, 1.50; 95% confidence interval, 1.15-1.95) and lower well-being (beta, -0.15; 95% CI, -0.26 to -0.04).
Using genetics to distinguish metabolic and psychosocial effects, the results also indicate that, even in the absence of adverse metabolic effects, “higher adiposity remains causal to depression and lowers wellbeing,” the researchers report.
“ and when using genetic variants that make you fatter but metabolically healthier (favorable adiposity genetic variants),” said Ms. O’Loughlin.
“Although we can’t tell which factor plays a bigger role in the adiposity-depression relationship, our analysis suggests that both physical and social factors (e.g., social stigma) play a role in the relationship between higher BMI and higher odds of depression,” she added.
In contrast, there was little evidence that higher BMI in the presence or absence of adverse metabolic consequences causes generalized anxiety disorder.
“Finding ways to support people to lose weight could benefit their mental health as well as their physical health,” co–lead author Francesco Casanova, PhD, with the University of Exeter, said in a statement.
Unexpected finding
Reached for comment, Samoon Ahmad, MD, professor, department of psychiatry, New York University, said that “multiple studies have shown a correlation between stress, obesity, inflammation, overall well-being, and psychiatric disorders, particularly depressive and anxiety disorders.”
He said this new study is important for three reasons.
“The first is the cohort size. There were over 145,000 participants involved in the study, which is significant and serves to make its conclusions stronger,” Dr. Ahmad noted.
“The second point is that the authors found that the correlation between higher adiposity and depression and lower well-being scores occurred even in patients without adverse metabolic effects,” he said in an interview.
“Of note, obesity significantly increases the risk of developing type 2 diabetes, hypertension, and a host of other illnesses as well as inflammatory conditions, which can all have a negative impact on quality of life. Consequently, these can contribute to depression as well as anxiety,” Dr. Ahmad added.
“Interestingly, what this study suggests is that even people without these additional stressors are reporting higher rates of depression and lower scores of well-being, while higher adiposity is the common denominator,” he noted.
“Third, the paper found little to no correlation between higher adiposity and generalized anxiety disorder. This comes as a complete surprise because anxiety and depression are very common comorbidities,” Dr. Ahmad said.
“Moreover, numerous studies as well as clinical data suggest that obesity leads to chronic inflammation, which in turn is associated with less favorable metabolic profiles, and that anxiety and depressive disorders may in some way be psychiatric manifestations of inflammation. To see one but not the other was quite an unexpected finding,” Dr. Ahmad said.
The study was funded by the Academy of Medical Sciences. Ms. O’Loughlin, Dr. Casanova, and Dr. Ahmad have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New research provides further evidence that a high body mass index (BMI) leads to depressed mood and poor well-being via social and physical factors.
Obesity and depression are “major global health challenges; our findings suggest that reducing obesity will lower depression and improve well-being,” co–lead author Jessica O’Loughlin, PhD student, University of Exeter Medical School, United Kingdom, told this news organization.
“Doctors should consider both the biological consequences of having a higher BMI as well as the social implications when treating patients with obesity in order to help reduce the odds of them developing depression,” Ms. O’Loughlin added.
The study was published online July 16 in Human Molecular Genetics.
Large body of evidence
A large body of evidence indicates that higher BMI leads to depression.
Ms. O’Loughlin and colleagues leveraged genetic data from more than 145,000 individuals in the UK Biobank and Mendelian randomization to determine whether the causal link between high BMI and depression is the result of psychosocial pathways, physical pathways, or both.
The analysis showed that a genetically determined 1 standard deviation higher BMI (4.6 kg/m2) was associated with higher likelihood of depression (odds ratio, 1.50; 95% confidence interval, 1.15-1.95) and lower well-being (beta, -0.15; 95% CI, -0.26 to -0.04).
Using genetics to distinguish metabolic and psychosocial effects, the results also indicate that, even in the absence of adverse metabolic effects, “higher adiposity remains causal to depression and lowers wellbeing,” the researchers report.
“ and when using genetic variants that make you fatter but metabolically healthier (favorable adiposity genetic variants),” said Ms. O’Loughlin.
“Although we can’t tell which factor plays a bigger role in the adiposity-depression relationship, our analysis suggests that both physical and social factors (e.g., social stigma) play a role in the relationship between higher BMI and higher odds of depression,” she added.
In contrast, there was little evidence that higher BMI in the presence or absence of adverse metabolic consequences causes generalized anxiety disorder.
“Finding ways to support people to lose weight could benefit their mental health as well as their physical health,” co–lead author Francesco Casanova, PhD, with the University of Exeter, said in a statement.
Unexpected finding
Reached for comment, Samoon Ahmad, MD, professor, department of psychiatry, New York University, said that “multiple studies have shown a correlation between stress, obesity, inflammation, overall well-being, and psychiatric disorders, particularly depressive and anxiety disorders.”
He said this new study is important for three reasons.
“The first is the cohort size. There were over 145,000 participants involved in the study, which is significant and serves to make its conclusions stronger,” Dr. Ahmad noted.
“The second point is that the authors found that the correlation between higher adiposity and depression and lower well-being scores occurred even in patients without adverse metabolic effects,” he said in an interview.
“Of note, obesity significantly increases the risk of developing type 2 diabetes, hypertension, and a host of other illnesses as well as inflammatory conditions, which can all have a negative impact on quality of life. Consequently, these can contribute to depression as well as anxiety,” Dr. Ahmad added.
“Interestingly, what this study suggests is that even people without these additional stressors are reporting higher rates of depression and lower scores of well-being, while higher adiposity is the common denominator,” he noted.
“Third, the paper found little to no correlation between higher adiposity and generalized anxiety disorder. This comes as a complete surprise because anxiety and depression are very common comorbidities,” Dr. Ahmad said.
“Moreover, numerous studies as well as clinical data suggest that obesity leads to chronic inflammation, which in turn is associated with less favorable metabolic profiles, and that anxiety and depressive disorders may in some way be psychiatric manifestations of inflammation. To see one but not the other was quite an unexpected finding,” Dr. Ahmad said.
The study was funded by the Academy of Medical Sciences. Ms. O’Loughlin, Dr. Casanova, and Dr. Ahmad have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Novel antidepressant shines in phase 2 trial, but FDA has issues with its NDA
Although a novel investigational drug that combines dextromethorphan and bupropion (AXS-05, Axsome Therapeutics) met its primary and key secondary endpoints in a phase 2 trial of patients with treatment-resistant depression (TRD), the U.S. Food and Drug Administration has voiced some concerns.
In the MERIT study, AXS-05 significantly delayed time to depression relapse compared with placebo (primary endpoint) – with no relapses observed for at least 6 months. It also significantly prevented depression relapse (secondary endpoint), the company said in a news release announcing the topline results.
The drug has been granted breakthrough therapy designations by the FDA for the treatment of major depressive disorder (MDD) and agitation associated with Alzheimer’s disease.
In addition,
However, Axsome stated that the FDA has identified “deficiencies that preclude labeling discussions at this time.”
The company is “attempting to learn the nature of these deficiencies with the goal of addressing them,” Herriot Tabuteau, MD, chief executive officer of Axsome, said in a statement.
However, Dr. Tabuteau acknowledged that this development “may lead to a delay in the potential approval of AXS-05.”
‘Well tolerated’
A total of 44 adults with TRD were enrolled into the MERIT study from the long-term, open-label phase 3 trial of AXS-05.
All patients were in stable remission after treatment with AXS-05 and were randomly assigned to continued treatment with AXS-05 (45 mg dextromethorphan/105 mg bupropion twice daily) or to switch to placebo.
Compared with placebo, AXS-05 significantly delayed time to depression relapse (P = .002) and prevented depression relapse (P = .004).
The novel drug was also well tolerated, with no treatment-emergent adverse events reported in more than one participant in the AXS-05 group, the company said.
One patient treated with AXS-05 did experience gout and bacteremia, but these incidents were deemed unrelated to the medication.
A version of this article first appeared on Medscape.com.
Although a novel investigational drug that combines dextromethorphan and bupropion (AXS-05, Axsome Therapeutics) met its primary and key secondary endpoints in a phase 2 trial of patients with treatment-resistant depression (TRD), the U.S. Food and Drug Administration has voiced some concerns.
In the MERIT study, AXS-05 significantly delayed time to depression relapse compared with placebo (primary endpoint) – with no relapses observed for at least 6 months. It also significantly prevented depression relapse (secondary endpoint), the company said in a news release announcing the topline results.
The drug has been granted breakthrough therapy designations by the FDA for the treatment of major depressive disorder (MDD) and agitation associated with Alzheimer’s disease.
In addition,
However, Axsome stated that the FDA has identified “deficiencies that preclude labeling discussions at this time.”
The company is “attempting to learn the nature of these deficiencies with the goal of addressing them,” Herriot Tabuteau, MD, chief executive officer of Axsome, said in a statement.
However, Dr. Tabuteau acknowledged that this development “may lead to a delay in the potential approval of AXS-05.”
‘Well tolerated’
A total of 44 adults with TRD were enrolled into the MERIT study from the long-term, open-label phase 3 trial of AXS-05.
All patients were in stable remission after treatment with AXS-05 and were randomly assigned to continued treatment with AXS-05 (45 mg dextromethorphan/105 mg bupropion twice daily) or to switch to placebo.
Compared with placebo, AXS-05 significantly delayed time to depression relapse (P = .002) and prevented depression relapse (P = .004).
The novel drug was also well tolerated, with no treatment-emergent adverse events reported in more than one participant in the AXS-05 group, the company said.
One patient treated with AXS-05 did experience gout and bacteremia, but these incidents were deemed unrelated to the medication.
A version of this article first appeared on Medscape.com.
Although a novel investigational drug that combines dextromethorphan and bupropion (AXS-05, Axsome Therapeutics) met its primary and key secondary endpoints in a phase 2 trial of patients with treatment-resistant depression (TRD), the U.S. Food and Drug Administration has voiced some concerns.
In the MERIT study, AXS-05 significantly delayed time to depression relapse compared with placebo (primary endpoint) – with no relapses observed for at least 6 months. It also significantly prevented depression relapse (secondary endpoint), the company said in a news release announcing the topline results.
The drug has been granted breakthrough therapy designations by the FDA for the treatment of major depressive disorder (MDD) and agitation associated with Alzheimer’s disease.
In addition,
However, Axsome stated that the FDA has identified “deficiencies that preclude labeling discussions at this time.”
The company is “attempting to learn the nature of these deficiencies with the goal of addressing them,” Herriot Tabuteau, MD, chief executive officer of Axsome, said in a statement.
However, Dr. Tabuteau acknowledged that this development “may lead to a delay in the potential approval of AXS-05.”
‘Well tolerated’
A total of 44 adults with TRD were enrolled into the MERIT study from the long-term, open-label phase 3 trial of AXS-05.
All patients were in stable remission after treatment with AXS-05 and were randomly assigned to continued treatment with AXS-05 (45 mg dextromethorphan/105 mg bupropion twice daily) or to switch to placebo.
Compared with placebo, AXS-05 significantly delayed time to depression relapse (P = .002) and prevented depression relapse (P = .004).
The novel drug was also well tolerated, with no treatment-emergent adverse events reported in more than one participant in the AXS-05 group, the company said.
One patient treated with AXS-05 did experience gout and bacteremia, but these incidents were deemed unrelated to the medication.
A version of this article first appeared on Medscape.com.
Clinical pearls for Muslim patients with suicide risk
The United States of America is home to a rapidly growing population of more than 3.5 million Muslims. The American Muslim population is a microcosm of global Islamic culture and religious practice, with heterogeneity across age, sex, ethnic origin, immigration status, socioeconomic background, and religiosity. Muslims in America face stressors, including challenges with migration, language barriers, and acculturation.
Some Muslim subgroups (for example, Black Muslims) face additional, intersectional struggles, such as racial discrimination and multigenerational trauma. These challenges may lead to the onset or exacerbation of psychopathology. Nevertheless, the mental health needs of this segment of the American population remain unmet.
Among mental health problems, suicide is inadequately researched among American Muslims. Global studies from both Muslim majority and non-Muslim majority countries consistently indicate that Muslims have among the lowest rates of suicide in comparison with other religious and nonreligious groups. Overall, this body of literature alludes to suicide resiliency in Muslim populations.
However, these studies may not depict the reality for American Muslims. A new research letter, published by two of us (R.A. and B.Z.) and other colleagues at Stanford (Calif.) University’s Muslim Mental Health and Islamic Psychology Lab, highlights the possibility of risk rather than resilience among American Muslims.
In a widely sampled population-based poll, we found that across religious groups in America, Muslims were up to twice as likely to endorse a lifetime history of suicide attempt than other religious or nonreligious groups.
Because of the paucity of suicide research, further inquiry is needed to explain American Muslim evident suicide risk. Nevertheless, our research shows that discrimination and marginalization, both religious and racial, are prominent suicide risk factors in the American Muslim narrative. From 2016 to 2020, almost two-thirds of American Muslims reported facing religious discrimination every year. In 2020, Muslim children in public K-12 systems were twice as likely to face bullying, a third of whom indicated that their bully was a school staff member. While the suicide literature has yet to explore Islamophobia in depth, marginalization and discrimination are demonstrably linked to suicide.
Here are a few clinical pearls that we think will help clinicians meet the needs of these patients:
1. Emphasize the basics. Muslims may be hesitant to engage with mental health practitioners and are often unfamiliar with confidentiality standards. Some may have experience with paternalistic health care cultures where patient privacy is violated. Consequently, some Muslim patients may have concerns that medical professionals can share personal medical history with family members or allied health professionals without obtaining consent. They may worry that private matters will be spread in their community, resulting in stigmatization or discrimination.
Providers should clearly communicate the terms of confidentiality and emphasize patient autonomy over information disclosed outside of the therapeutic partnership.
2. Develop a therapeutic alliance with cultural humility. Since Muslim patients have likely witnessed discrimination, either directly or indirectly, clinicians must adopt a nonjudgmental stance when discussing cultural, religious, or moral values different from their own. Muslim patients may find defending their faith and cultural norms stigmatizing, when faced with clinicians’ assumptions.
Providers should be transparent about their knowledge limitations, ask humbly for a partnership of shared learning, and allow the patient to lead where appropriate. Clinicians should develop a working understanding of Islamic values and cultural norms. See below for Muslim Mental Health resources.
3. Assess suicide risk and ask follow-up questions. Some clinicians may not deem suicide assessments valuable for Muslim patients, believing that strong religious values may preclude them from suicide risk. New findings that suicide risk is prominent among American Muslims highlights the necessity for assessment.
Practitioners should conduct thorough suicide risk assessments, including: past and present ideation, plan, intent, means, relevant risk, and resilience factors. Muslims may be culturally inclined to deny ideation, especially when accompanied by family members. Providers should be on alert for incongruent cues in patient affect and behavior.
4. Accommodate inpatient religious practice. Muslims navigate daily religious choices, from prayers at prescribed times to observing Islamic dietary guidelines. During psychiatric admissions, many of these norms are suspended temporarily. Treatments that do not include the flexibility to address these concerns may mirror patients’ experiences with Islamophobia. For example, being asked to remove the hijab, even with good cause (that is, self-harm precautions), may trigger familiar discriminatory threats to safety and belonging.
Religious accommodations should be addressed in rounds so that all interacting staff maintain collective accountability for religious needs. Accommodations may require adaptive solutions, such as one-piece pull-on–style hijabs as safer alternatives to rectangular wraps. To prevent pathologizing religious observance, providers should consider meeting with Muslim chaplains and patient advocates, including family members or religious care providers, where appropriate.
Addressing the mental health needs of Muslim patients not only requires cultural humility but knowledge about unique challenges facing this diverse community.
To help further advance understanding of these issues, consider taking the American Psychiatric Association’s Muslim Mental Health CME course, which will be taught by Dr. Awaad. In addition, we have included a list of resources below.
Further reading
Moffic S et al. Islamophobia and Psychiatry: Recognition, Prevention and Treatment. New York: Springer, 2019.
Keshavarzi H et al. Applying Islamic Principles to Clinical Mental Health Care: Introducing Traditional Islamically Integrated Psychotherapy. New York: Routledge, 2020.
Ahmed S and MM Amer. Counseling Muslims: Handbook of Mental Health Issues and Interventions. New York: Routledge/Taylor & Francis Group, 2012.
American Psychiatric Association. Stress & Trauma Toolkit for Treating Muslims in a Changing Political and Social Environment, 2019.
American Psychiatric Association. Mental Health Disparities: Muslim Americans, 2019.
Awaad R et al. JAMA Psychiatry. 2021 Jul 21. doi: 10.1001/jamapsychiatry.2021.1813.
Baca-Garcia E et al. J Affect Disord. 2011;134(1-3):327-32.
Institute for Muslim Mental Health: https://muslimmentalhealth.com/
Institute for Social Policy and Understanding. “Religious Discrimination in Multiple Forms Impacts Muslims of All Ages: American Muslim Poll, 2020.
Silverman JJ et al. Am J Psychiatry. 2015 Aug 1;172(8):798-802.
Resources
Stanford Muslim Mental Health and Islamic Psychology Lab: http://med.stanford.edu/psychiatry/research/MuslimMHLab.html
Maristan: https://maristan.org/
Naseeha mental health hotline: https://naseeha.org/
Dr. Awaad is a clinical associate professor in the department of psychiatry and behavioral sciences at Stanford University. She also serves as associate division chief of public mental health and population sciences, and diversity section chief in the psychiatry department. In addition, Dr. Awaad is executive director of Maristan, an organization focused on using authentic traditions to meet the mental health needs of the Islamic community, and is affiliated with the department of psychiatry and behavioral sciences at Stanford. Dr. Awaad is coeditor of “Islamophobia and Psychiatry: Recognition, Prevention and Treatment” (New York: Springer, 2019), and “Applying Islamic Principles to Clinical Mental Health Care: Introducing Traditional Islamically Integrated Psychotherapy” (New York: Routledge/Taylor & Francis Group, 2020).
Dr. Husain completed her medical degree from St. George’s University in True Blue, Grenada; she is currently a graduate student in the department of public health concentrating on mental health parity in the United States. She also works as a researcher at the Stanford Muslim Mental Health & Islamic Psychology Lab and as an organizer for Team Liyna, a national effort aimed at diversifying the stem cell registry responsible for more than 10,000 new registrants since 2019.
Mr. Zia, who has been affiliated with the department of psychiatry and behavioral sciences at Stanford, is a PhD candidate and Canada-Vanier scholar in the department of clinical psychology at the University of Manitoba, Winnipeg. Mr. Zia is also a psychological associate at the New Leaf Psychology Centre in Milton, Ont. He has no relevant financial relationships.
The United States of America is home to a rapidly growing population of more than 3.5 million Muslims. The American Muslim population is a microcosm of global Islamic culture and religious practice, with heterogeneity across age, sex, ethnic origin, immigration status, socioeconomic background, and religiosity. Muslims in America face stressors, including challenges with migration, language barriers, and acculturation.
Some Muslim subgroups (for example, Black Muslims) face additional, intersectional struggles, such as racial discrimination and multigenerational trauma. These challenges may lead to the onset or exacerbation of psychopathology. Nevertheless, the mental health needs of this segment of the American population remain unmet.
Among mental health problems, suicide is inadequately researched among American Muslims. Global studies from both Muslim majority and non-Muslim majority countries consistently indicate that Muslims have among the lowest rates of suicide in comparison with other religious and nonreligious groups. Overall, this body of literature alludes to suicide resiliency in Muslim populations.
However, these studies may not depict the reality for American Muslims. A new research letter, published by two of us (R.A. and B.Z.) and other colleagues at Stanford (Calif.) University’s Muslim Mental Health and Islamic Psychology Lab, highlights the possibility of risk rather than resilience among American Muslims.
In a widely sampled population-based poll, we found that across religious groups in America, Muslims were up to twice as likely to endorse a lifetime history of suicide attempt than other religious or nonreligious groups.
Because of the paucity of suicide research, further inquiry is needed to explain American Muslim evident suicide risk. Nevertheless, our research shows that discrimination and marginalization, both religious and racial, are prominent suicide risk factors in the American Muslim narrative. From 2016 to 2020, almost two-thirds of American Muslims reported facing religious discrimination every year. In 2020, Muslim children in public K-12 systems were twice as likely to face bullying, a third of whom indicated that their bully was a school staff member. While the suicide literature has yet to explore Islamophobia in depth, marginalization and discrimination are demonstrably linked to suicide.
Here are a few clinical pearls that we think will help clinicians meet the needs of these patients:
1. Emphasize the basics. Muslims may be hesitant to engage with mental health practitioners and are often unfamiliar with confidentiality standards. Some may have experience with paternalistic health care cultures where patient privacy is violated. Consequently, some Muslim patients may have concerns that medical professionals can share personal medical history with family members or allied health professionals without obtaining consent. They may worry that private matters will be spread in their community, resulting in stigmatization or discrimination.
Providers should clearly communicate the terms of confidentiality and emphasize patient autonomy over information disclosed outside of the therapeutic partnership.
2. Develop a therapeutic alliance with cultural humility. Since Muslim patients have likely witnessed discrimination, either directly or indirectly, clinicians must adopt a nonjudgmental stance when discussing cultural, religious, or moral values different from their own. Muslim patients may find defending their faith and cultural norms stigmatizing, when faced with clinicians’ assumptions.
Providers should be transparent about their knowledge limitations, ask humbly for a partnership of shared learning, and allow the patient to lead where appropriate. Clinicians should develop a working understanding of Islamic values and cultural norms. See below for Muslim Mental Health resources.
3. Assess suicide risk and ask follow-up questions. Some clinicians may not deem suicide assessments valuable for Muslim patients, believing that strong religious values may preclude them from suicide risk. New findings that suicide risk is prominent among American Muslims highlights the necessity for assessment.
Practitioners should conduct thorough suicide risk assessments, including: past and present ideation, plan, intent, means, relevant risk, and resilience factors. Muslims may be culturally inclined to deny ideation, especially when accompanied by family members. Providers should be on alert for incongruent cues in patient affect and behavior.
4. Accommodate inpatient religious practice. Muslims navigate daily religious choices, from prayers at prescribed times to observing Islamic dietary guidelines. During psychiatric admissions, many of these norms are suspended temporarily. Treatments that do not include the flexibility to address these concerns may mirror patients’ experiences with Islamophobia. For example, being asked to remove the hijab, even with good cause (that is, self-harm precautions), may trigger familiar discriminatory threats to safety and belonging.
Religious accommodations should be addressed in rounds so that all interacting staff maintain collective accountability for religious needs. Accommodations may require adaptive solutions, such as one-piece pull-on–style hijabs as safer alternatives to rectangular wraps. To prevent pathologizing religious observance, providers should consider meeting with Muslim chaplains and patient advocates, including family members or religious care providers, where appropriate.
Addressing the mental health needs of Muslim patients not only requires cultural humility but knowledge about unique challenges facing this diverse community.
To help further advance understanding of these issues, consider taking the American Psychiatric Association’s Muslim Mental Health CME course, which will be taught by Dr. Awaad. In addition, we have included a list of resources below.
Further reading
Moffic S et al. Islamophobia and Psychiatry: Recognition, Prevention and Treatment. New York: Springer, 2019.
Keshavarzi H et al. Applying Islamic Principles to Clinical Mental Health Care: Introducing Traditional Islamically Integrated Psychotherapy. New York: Routledge, 2020.
Ahmed S and MM Amer. Counseling Muslims: Handbook of Mental Health Issues and Interventions. New York: Routledge/Taylor & Francis Group, 2012.
American Psychiatric Association. Stress & Trauma Toolkit for Treating Muslims in a Changing Political and Social Environment, 2019.
American Psychiatric Association. Mental Health Disparities: Muslim Americans, 2019.
Awaad R et al. JAMA Psychiatry. 2021 Jul 21. doi: 10.1001/jamapsychiatry.2021.1813.
Baca-Garcia E et al. J Affect Disord. 2011;134(1-3):327-32.
Institute for Muslim Mental Health: https://muslimmentalhealth.com/
Institute for Social Policy and Understanding. “Religious Discrimination in Multiple Forms Impacts Muslims of All Ages: American Muslim Poll, 2020.
Silverman JJ et al. Am J Psychiatry. 2015 Aug 1;172(8):798-802.
Resources
Stanford Muslim Mental Health and Islamic Psychology Lab: http://med.stanford.edu/psychiatry/research/MuslimMHLab.html
Maristan: https://maristan.org/
Naseeha mental health hotline: https://naseeha.org/
Dr. Awaad is a clinical associate professor in the department of psychiatry and behavioral sciences at Stanford University. She also serves as associate division chief of public mental health and population sciences, and diversity section chief in the psychiatry department. In addition, Dr. Awaad is executive director of Maristan, an organization focused on using authentic traditions to meet the mental health needs of the Islamic community, and is affiliated with the department of psychiatry and behavioral sciences at Stanford. Dr. Awaad is coeditor of “Islamophobia and Psychiatry: Recognition, Prevention and Treatment” (New York: Springer, 2019), and “Applying Islamic Principles to Clinical Mental Health Care: Introducing Traditional Islamically Integrated Psychotherapy” (New York: Routledge/Taylor & Francis Group, 2020).
Dr. Husain completed her medical degree from St. George’s University in True Blue, Grenada; she is currently a graduate student in the department of public health concentrating on mental health parity in the United States. She also works as a researcher at the Stanford Muslim Mental Health & Islamic Psychology Lab and as an organizer for Team Liyna, a national effort aimed at diversifying the stem cell registry responsible for more than 10,000 new registrants since 2019.
Mr. Zia, who has been affiliated with the department of psychiatry and behavioral sciences at Stanford, is a PhD candidate and Canada-Vanier scholar in the department of clinical psychology at the University of Manitoba, Winnipeg. Mr. Zia is also a psychological associate at the New Leaf Psychology Centre in Milton, Ont. He has no relevant financial relationships.
The United States of America is home to a rapidly growing population of more than 3.5 million Muslims. The American Muslim population is a microcosm of global Islamic culture and religious practice, with heterogeneity across age, sex, ethnic origin, immigration status, socioeconomic background, and religiosity. Muslims in America face stressors, including challenges with migration, language barriers, and acculturation.
Some Muslim subgroups (for example, Black Muslims) face additional, intersectional struggles, such as racial discrimination and multigenerational trauma. These challenges may lead to the onset or exacerbation of psychopathology. Nevertheless, the mental health needs of this segment of the American population remain unmet.
Among mental health problems, suicide is inadequately researched among American Muslims. Global studies from both Muslim majority and non-Muslim majority countries consistently indicate that Muslims have among the lowest rates of suicide in comparison with other religious and nonreligious groups. Overall, this body of literature alludes to suicide resiliency in Muslim populations.
However, these studies may not depict the reality for American Muslims. A new research letter, published by two of us (R.A. and B.Z.) and other colleagues at Stanford (Calif.) University’s Muslim Mental Health and Islamic Psychology Lab, highlights the possibility of risk rather than resilience among American Muslims.
In a widely sampled population-based poll, we found that across religious groups in America, Muslims were up to twice as likely to endorse a lifetime history of suicide attempt than other religious or nonreligious groups.
Because of the paucity of suicide research, further inquiry is needed to explain American Muslim evident suicide risk. Nevertheless, our research shows that discrimination and marginalization, both religious and racial, are prominent suicide risk factors in the American Muslim narrative. From 2016 to 2020, almost two-thirds of American Muslims reported facing religious discrimination every year. In 2020, Muslim children in public K-12 systems were twice as likely to face bullying, a third of whom indicated that their bully was a school staff member. While the suicide literature has yet to explore Islamophobia in depth, marginalization and discrimination are demonstrably linked to suicide.
Here are a few clinical pearls that we think will help clinicians meet the needs of these patients:
1. Emphasize the basics. Muslims may be hesitant to engage with mental health practitioners and are often unfamiliar with confidentiality standards. Some may have experience with paternalistic health care cultures where patient privacy is violated. Consequently, some Muslim patients may have concerns that medical professionals can share personal medical history with family members or allied health professionals without obtaining consent. They may worry that private matters will be spread in their community, resulting in stigmatization or discrimination.
Providers should clearly communicate the terms of confidentiality and emphasize patient autonomy over information disclosed outside of the therapeutic partnership.
2. Develop a therapeutic alliance with cultural humility. Since Muslim patients have likely witnessed discrimination, either directly or indirectly, clinicians must adopt a nonjudgmental stance when discussing cultural, religious, or moral values different from their own. Muslim patients may find defending their faith and cultural norms stigmatizing, when faced with clinicians’ assumptions.
Providers should be transparent about their knowledge limitations, ask humbly for a partnership of shared learning, and allow the patient to lead where appropriate. Clinicians should develop a working understanding of Islamic values and cultural norms. See below for Muslim Mental Health resources.
3. Assess suicide risk and ask follow-up questions. Some clinicians may not deem suicide assessments valuable for Muslim patients, believing that strong religious values may preclude them from suicide risk. New findings that suicide risk is prominent among American Muslims highlights the necessity for assessment.
Practitioners should conduct thorough suicide risk assessments, including: past and present ideation, plan, intent, means, relevant risk, and resilience factors. Muslims may be culturally inclined to deny ideation, especially when accompanied by family members. Providers should be on alert for incongruent cues in patient affect and behavior.
4. Accommodate inpatient religious practice. Muslims navigate daily religious choices, from prayers at prescribed times to observing Islamic dietary guidelines. During psychiatric admissions, many of these norms are suspended temporarily. Treatments that do not include the flexibility to address these concerns may mirror patients’ experiences with Islamophobia. For example, being asked to remove the hijab, even with good cause (that is, self-harm precautions), may trigger familiar discriminatory threats to safety and belonging.
Religious accommodations should be addressed in rounds so that all interacting staff maintain collective accountability for religious needs. Accommodations may require adaptive solutions, such as one-piece pull-on–style hijabs as safer alternatives to rectangular wraps. To prevent pathologizing religious observance, providers should consider meeting with Muslim chaplains and patient advocates, including family members or religious care providers, where appropriate.
Addressing the mental health needs of Muslim patients not only requires cultural humility but knowledge about unique challenges facing this diverse community.
To help further advance understanding of these issues, consider taking the American Psychiatric Association’s Muslim Mental Health CME course, which will be taught by Dr. Awaad. In addition, we have included a list of resources below.
Further reading
Moffic S et al. Islamophobia and Psychiatry: Recognition, Prevention and Treatment. New York: Springer, 2019.
Keshavarzi H et al. Applying Islamic Principles to Clinical Mental Health Care: Introducing Traditional Islamically Integrated Psychotherapy. New York: Routledge, 2020.
Ahmed S and MM Amer. Counseling Muslims: Handbook of Mental Health Issues and Interventions. New York: Routledge/Taylor & Francis Group, 2012.
American Psychiatric Association. Stress & Trauma Toolkit for Treating Muslims in a Changing Political and Social Environment, 2019.
American Psychiatric Association. Mental Health Disparities: Muslim Americans, 2019.
Awaad R et al. JAMA Psychiatry. 2021 Jul 21. doi: 10.1001/jamapsychiatry.2021.1813.
Baca-Garcia E et al. J Affect Disord. 2011;134(1-3):327-32.
Institute for Muslim Mental Health: https://muslimmentalhealth.com/
Institute for Social Policy and Understanding. “Religious Discrimination in Multiple Forms Impacts Muslims of All Ages: American Muslim Poll, 2020.
Silverman JJ et al. Am J Psychiatry. 2015 Aug 1;172(8):798-802.
Resources
Stanford Muslim Mental Health and Islamic Psychology Lab: http://med.stanford.edu/psychiatry/research/MuslimMHLab.html
Maristan: https://maristan.org/
Naseeha mental health hotline: https://naseeha.org/
Dr. Awaad is a clinical associate professor in the department of psychiatry and behavioral sciences at Stanford University. She also serves as associate division chief of public mental health and population sciences, and diversity section chief in the psychiatry department. In addition, Dr. Awaad is executive director of Maristan, an organization focused on using authentic traditions to meet the mental health needs of the Islamic community, and is affiliated with the department of psychiatry and behavioral sciences at Stanford. Dr. Awaad is coeditor of “Islamophobia and Psychiatry: Recognition, Prevention and Treatment” (New York: Springer, 2019), and “Applying Islamic Principles to Clinical Mental Health Care: Introducing Traditional Islamically Integrated Psychotherapy” (New York: Routledge/Taylor & Francis Group, 2020).
Dr. Husain completed her medical degree from St. George’s University in True Blue, Grenada; she is currently a graduate student in the department of public health concentrating on mental health parity in the United States. She also works as a researcher at the Stanford Muslim Mental Health & Islamic Psychology Lab and as an organizer for Team Liyna, a national effort aimed at diversifying the stem cell registry responsible for more than 10,000 new registrants since 2019.
Mr. Zia, who has been affiliated with the department of psychiatry and behavioral sciences at Stanford, is a PhD candidate and Canada-Vanier scholar in the department of clinical psychology at the University of Manitoba, Winnipeg. Mr. Zia is also a psychological associate at the New Leaf Psychology Centre in Milton, Ont. He has no relevant financial relationships.
Global youth depression and anxiety doubled during pandemic
The COVID-19 pandemic doubled international rates of child and adolescent psychological disorders, according to results of a meta-analysis.
In the first year of the pandemic, an estimated one in four youth across various regions of the globe experienced clinically elevated depression symptoms, while one in five experienced clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double prepandemic estimates, according to Nicole Racine, PhD, RPsych, a clinical psychologist at the University of Calgary (Alta.) and colleagues.
Their meta-analysis of 29 studies, comprising 80,879 young people worldwide aged 18 years or less, found pooled prevalence estimates of clinically elevated youth depression and anxiety of 25.2% (95% confidence interval, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively.
“The prevalence of depression and anxiety symptoms during COVID-19 [has] doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls,” the researchers write online in JAMA Pediatrics.
Prepandemic estimates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% and 12.9%, respectively, the authors say.
The increases revealed in these international findings have implications for targeted mental health resource planning.
“One difficulty in the literature is that there are large discrepancies on the prevalence of child depression and anxiety during the COVID-19 pandemic, with published rates between 2% and 68%,” corresponding author Sheri Madigan, PhD, RPsych, of the University of Calgary department of psychology, said in an interview. “By conducting a synthesis of the 29 studies on over 80,000 children, we were able to determine that, on average across these studies, 25% of youth are experiencing depression and 20% are experiencing anxiety during the COVID-19 pandemic.”
The cohort
The mean age in the combined global cohort was 13 years (range 4.1-17.6 ), and the mean proportion of females was 52.7% (standard deviation) 12.3%). The findings were based on international data published from Jan. 1, 2020, to Feb. 16, 2021, in studies conducted in the Middle East (n = 1), Europe (n = 4), South America (n = 2), North America (n = 6), and East Asia (n = 16). Notably absent were data from most of Latin America and the Middle East, Africa, South East Asia, and the Pacific Islands.
As the year progressed, the prevalence of depressive symptoms rose (b = .26; 95% CI, .06-46) with the number of months elapsed. Prevalence rates also rose as both age (b = 0.08, 95% CI, 0.01-0.15), and the percentage of females in samples increased (b = .03; 95% CI, 0.01-0.05).
The authors surmise that this cumulative worsening might be because of prolonged social isolation, family financial difficulties, missed milestones, and school disruptions, which are compounded over time. A second possibility is that studies conducted in the earlier months of the pandemic were more likely to be conducted in East Asia, where the self-reported prevalence of mental health symptoms tends to be lower.
The findings highlight an urgent need for intervention and recovery efforts and also indicate the need to consider individual differences when determining targets for intervention, including age, sex, and exposure to COVID-19 stressors), they add.
Even more concerning, recent data from the Centers for Disease Control and Prevention suggest that the pandemic spurred an increase in suspected suicide attempts by teenage girls. In the United Kingdom, acute mental health presentations to emergency care tripled over 2019 at one pediatric facility during the pandemic.
The authors attribute the toll on the psychological well-being of the world’s young people to pandemic-mandated restrictions. Those entailed loss of peer interactions, social isolation, and reduced contact with support figures such as teachers, and, “In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs.” For many children, these services were rendered unavailable owing to school closures, Dr. Madigan and associates write.
In the context of clinical practice, doctors play a critical role. “With school closures, the physician’s office may be the only mental health checkpoint for youth,” Dr. Madigan said “So I recommend that family physicians screen for, and/or ask children and youth, about their mental health.”
On the home front, emerging research suggests that a predictable home environment can protect children’s mental well-being, with less depression and fewer behavioral problems observed in families adhering to regular routines during COVID-19. “Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity,” the authors write.
They also point to the need for research on the long-term effects of the pandemic on mental health, including studies in order to “augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.”
In an accompanying editorial, Tami D. Benton, MD, psychiatrist-in-chief at Children’s Hospital of Philadelphia, and colleagues, who were not involved in the meta-analysis, note certain limitations to the study. First, the included studies are based on self- or parent-reported symptoms. Second, the studies, more than half of which (55.2%) were done in China, may not be generalizable to all regions of the world, where 90% of children live in low- or middle-income countries.
Still, they write,“The increased mental health needs identified in the meta-analysis call for immediate action for every country. Our responses must consider the range of child mental health infrastructures available, which vary across countries, with some having well-developed and coordinated mental health services, while others have informal, limited, underfunded, or fragmented systems of care.”
Empirically supported and culturally appropriate intervention strategies for children and families according to countries and communities will be crucial, they stress.
“This meta-analysis provides the most complete evidence to date on the toll the COVID-19 pandemic has taken on child and adolescent mental health,” said Katie A. McLaughlin, PhD, a professor of psychology at Harvard University in Boston, who was not involved in the study. “The results confirm the substantial increases in symptoms of youth depression and anxiety that many clinicians and researchers have observed during the pandemic and highlight the critical need for greater investments in mental health services for children and adolescents.”
This study received no specific funding other than research support to the investigators from nonprivate entities. The authors disclosed no relevant conflicts of interest. Dr. Benton and associates and Dr. McLaughlin declared no competing interests.
The COVID-19 pandemic doubled international rates of child and adolescent psychological disorders, according to results of a meta-analysis.
In the first year of the pandemic, an estimated one in four youth across various regions of the globe experienced clinically elevated depression symptoms, while one in five experienced clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double prepandemic estimates, according to Nicole Racine, PhD, RPsych, a clinical psychologist at the University of Calgary (Alta.) and colleagues.
Their meta-analysis of 29 studies, comprising 80,879 young people worldwide aged 18 years or less, found pooled prevalence estimates of clinically elevated youth depression and anxiety of 25.2% (95% confidence interval, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively.
“The prevalence of depression and anxiety symptoms during COVID-19 [has] doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls,” the researchers write online in JAMA Pediatrics.
Prepandemic estimates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% and 12.9%, respectively, the authors say.
The increases revealed in these international findings have implications for targeted mental health resource planning.
“One difficulty in the literature is that there are large discrepancies on the prevalence of child depression and anxiety during the COVID-19 pandemic, with published rates between 2% and 68%,” corresponding author Sheri Madigan, PhD, RPsych, of the University of Calgary department of psychology, said in an interview. “By conducting a synthesis of the 29 studies on over 80,000 children, we were able to determine that, on average across these studies, 25% of youth are experiencing depression and 20% are experiencing anxiety during the COVID-19 pandemic.”
The cohort
The mean age in the combined global cohort was 13 years (range 4.1-17.6 ), and the mean proportion of females was 52.7% (standard deviation) 12.3%). The findings were based on international data published from Jan. 1, 2020, to Feb. 16, 2021, in studies conducted in the Middle East (n = 1), Europe (n = 4), South America (n = 2), North America (n = 6), and East Asia (n = 16). Notably absent were data from most of Latin America and the Middle East, Africa, South East Asia, and the Pacific Islands.
As the year progressed, the prevalence of depressive symptoms rose (b = .26; 95% CI, .06-46) with the number of months elapsed. Prevalence rates also rose as both age (b = 0.08, 95% CI, 0.01-0.15), and the percentage of females in samples increased (b = .03; 95% CI, 0.01-0.05).
The authors surmise that this cumulative worsening might be because of prolonged social isolation, family financial difficulties, missed milestones, and school disruptions, which are compounded over time. A second possibility is that studies conducted in the earlier months of the pandemic were more likely to be conducted in East Asia, where the self-reported prevalence of mental health symptoms tends to be lower.
The findings highlight an urgent need for intervention and recovery efforts and also indicate the need to consider individual differences when determining targets for intervention, including age, sex, and exposure to COVID-19 stressors), they add.
Even more concerning, recent data from the Centers for Disease Control and Prevention suggest that the pandemic spurred an increase in suspected suicide attempts by teenage girls. In the United Kingdom, acute mental health presentations to emergency care tripled over 2019 at one pediatric facility during the pandemic.
The authors attribute the toll on the psychological well-being of the world’s young people to pandemic-mandated restrictions. Those entailed loss of peer interactions, social isolation, and reduced contact with support figures such as teachers, and, “In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs.” For many children, these services were rendered unavailable owing to school closures, Dr. Madigan and associates write.
In the context of clinical practice, doctors play a critical role. “With school closures, the physician’s office may be the only mental health checkpoint for youth,” Dr. Madigan said “So I recommend that family physicians screen for, and/or ask children and youth, about their mental health.”
On the home front, emerging research suggests that a predictable home environment can protect children’s mental well-being, with less depression and fewer behavioral problems observed in families adhering to regular routines during COVID-19. “Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity,” the authors write.
They also point to the need for research on the long-term effects of the pandemic on mental health, including studies in order to “augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.”
In an accompanying editorial, Tami D. Benton, MD, psychiatrist-in-chief at Children’s Hospital of Philadelphia, and colleagues, who were not involved in the meta-analysis, note certain limitations to the study. First, the included studies are based on self- or parent-reported symptoms. Second, the studies, more than half of which (55.2%) were done in China, may not be generalizable to all regions of the world, where 90% of children live in low- or middle-income countries.
Still, they write,“The increased mental health needs identified in the meta-analysis call for immediate action for every country. Our responses must consider the range of child mental health infrastructures available, which vary across countries, with some having well-developed and coordinated mental health services, while others have informal, limited, underfunded, or fragmented systems of care.”
Empirically supported and culturally appropriate intervention strategies for children and families according to countries and communities will be crucial, they stress.
“This meta-analysis provides the most complete evidence to date on the toll the COVID-19 pandemic has taken on child and adolescent mental health,” said Katie A. McLaughlin, PhD, a professor of psychology at Harvard University in Boston, who was not involved in the study. “The results confirm the substantial increases in symptoms of youth depression and anxiety that many clinicians and researchers have observed during the pandemic and highlight the critical need for greater investments in mental health services for children and adolescents.”
This study received no specific funding other than research support to the investigators from nonprivate entities. The authors disclosed no relevant conflicts of interest. Dr. Benton and associates and Dr. McLaughlin declared no competing interests.
The COVID-19 pandemic doubled international rates of child and adolescent psychological disorders, according to results of a meta-analysis.
In the first year of the pandemic, an estimated one in four youth across various regions of the globe experienced clinically elevated depression symptoms, while one in five experienced clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double prepandemic estimates, according to Nicole Racine, PhD, RPsych, a clinical psychologist at the University of Calgary (Alta.) and colleagues.
Their meta-analysis of 29 studies, comprising 80,879 young people worldwide aged 18 years or less, found pooled prevalence estimates of clinically elevated youth depression and anxiety of 25.2% (95% confidence interval, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively.
“The prevalence of depression and anxiety symptoms during COVID-19 [has] doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls,” the researchers write online in JAMA Pediatrics.
Prepandemic estimates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% and 12.9%, respectively, the authors say.
The increases revealed in these international findings have implications for targeted mental health resource planning.
“One difficulty in the literature is that there are large discrepancies on the prevalence of child depression and anxiety during the COVID-19 pandemic, with published rates between 2% and 68%,” corresponding author Sheri Madigan, PhD, RPsych, of the University of Calgary department of psychology, said in an interview. “By conducting a synthesis of the 29 studies on over 80,000 children, we were able to determine that, on average across these studies, 25% of youth are experiencing depression and 20% are experiencing anxiety during the COVID-19 pandemic.”
The cohort
The mean age in the combined global cohort was 13 years (range 4.1-17.6 ), and the mean proportion of females was 52.7% (standard deviation) 12.3%). The findings were based on international data published from Jan. 1, 2020, to Feb. 16, 2021, in studies conducted in the Middle East (n = 1), Europe (n = 4), South America (n = 2), North America (n = 6), and East Asia (n = 16). Notably absent were data from most of Latin America and the Middle East, Africa, South East Asia, and the Pacific Islands.
As the year progressed, the prevalence of depressive symptoms rose (b = .26; 95% CI, .06-46) with the number of months elapsed. Prevalence rates also rose as both age (b = 0.08, 95% CI, 0.01-0.15), and the percentage of females in samples increased (b = .03; 95% CI, 0.01-0.05).
The authors surmise that this cumulative worsening might be because of prolonged social isolation, family financial difficulties, missed milestones, and school disruptions, which are compounded over time. A second possibility is that studies conducted in the earlier months of the pandemic were more likely to be conducted in East Asia, where the self-reported prevalence of mental health symptoms tends to be lower.
The findings highlight an urgent need for intervention and recovery efforts and also indicate the need to consider individual differences when determining targets for intervention, including age, sex, and exposure to COVID-19 stressors), they add.
Even more concerning, recent data from the Centers for Disease Control and Prevention suggest that the pandemic spurred an increase in suspected suicide attempts by teenage girls. In the United Kingdom, acute mental health presentations to emergency care tripled over 2019 at one pediatric facility during the pandemic.
The authors attribute the toll on the psychological well-being of the world’s young people to pandemic-mandated restrictions. Those entailed loss of peer interactions, social isolation, and reduced contact with support figures such as teachers, and, “In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs.” For many children, these services were rendered unavailable owing to school closures, Dr. Madigan and associates write.
In the context of clinical practice, doctors play a critical role. “With school closures, the physician’s office may be the only mental health checkpoint for youth,” Dr. Madigan said “So I recommend that family physicians screen for, and/or ask children and youth, about their mental health.”
On the home front, emerging research suggests that a predictable home environment can protect children’s mental well-being, with less depression and fewer behavioral problems observed in families adhering to regular routines during COVID-19. “Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity,” the authors write.
They also point to the need for research on the long-term effects of the pandemic on mental health, including studies in order to “augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.”
In an accompanying editorial, Tami D. Benton, MD, psychiatrist-in-chief at Children’s Hospital of Philadelphia, and colleagues, who were not involved in the meta-analysis, note certain limitations to the study. First, the included studies are based on self- or parent-reported symptoms. Second, the studies, more than half of which (55.2%) were done in China, may not be generalizable to all regions of the world, where 90% of children live in low- or middle-income countries.
Still, they write,“The increased mental health needs identified in the meta-analysis call for immediate action for every country. Our responses must consider the range of child mental health infrastructures available, which vary across countries, with some having well-developed and coordinated mental health services, while others have informal, limited, underfunded, or fragmented systems of care.”
Empirically supported and culturally appropriate intervention strategies for children and families according to countries and communities will be crucial, they stress.
“This meta-analysis provides the most complete evidence to date on the toll the COVID-19 pandemic has taken on child and adolescent mental health,” said Katie A. McLaughlin, PhD, a professor of psychology at Harvard University in Boston, who was not involved in the study. “The results confirm the substantial increases in symptoms of youth depression and anxiety that many clinicians and researchers have observed during the pandemic and highlight the critical need for greater investments in mental health services for children and adolescents.”
This study received no specific funding other than research support to the investigators from nonprivate entities. The authors disclosed no relevant conflicts of interest. Dr. Benton and associates and Dr. McLaughlin declared no competing interests.
Androgenetic alopecia fuels negative emotions and poor quality of life
and meta-analysis of 41 studies.
“Hair loss affects self-image, causes trichodynia, and plays a role in emotions and social activity, which may be associated with psychiatric problems and impaired health-related quality of life,” wrote Chun-Hsien Huang, MD, of Chang Gung Memorial Hospital, Linkou, Taiwan, and colleagues. However, systematic reviews of the associations between androgenetic alopecia (AGA) and health-related quality of life (HRQOL) are lacking, they said.
In a study published in JAMA Dermatology, the researchers reviewed data from a total of 7,995 AGA patients in 41 studies. The studies included 11 tools for HRQOL assessment and 29 tools for psychological assessment. Of these, the Dermatology Life Quality Index (DLQI) and the Hair-Specific Skindex-29 were used to assess quality of life, and the Center for Epidemiologic Studies Depression Scale (CES-D) was used for psychological assessment in the meta-analysis.
Overall, 27 studies identified 18 factors associated with HRQOL; those with an inverse effect were higher self-rated hair loss severity, lower VAS score, and higher educational level. Of note, neither physician-rated hair loss severity nor treatment response were factors in HRQOL, the researchers said.
The pooled DLQI score across studies was 8.16, and subgroup analysis showed no differences in HRQOL between men and women or between patients from European vs. Asian countries. However, five studies showed significant differences in HRQOL between men and women when different assessment tools were used, which emphasized the need for more studies to examine the association of AGA with HRQOL by sex, the researchers said.
The meta-analysis of the Hair-Specific Skindex-29 scores showed pooled averages of 21.95 for symptom dimension, 18.52 in function dimension, and 29.22 in emotion dimension. Of these, the emotion dimension scores indicated moderate emotional impairment.
The average pooled score on the CES-D in the meta-analysis was 14.98, indicating no association between AGA and depression, the researchers said. However, “depression accounts for only a part of the emotion dimension,” they said. “Therefore, emotion dimension could be impaired even if no depressive symptoms were noted.”
The pooled DLQI scores for AGA (8.16) were higher than scores for other skin conditions including alopecia areata (6.3), contact dermatitis (7.35), and acne vulgaris (7.45), but lower than the pooled scores for vitiligo (9.11), urticaria (9.8), psoriasis (10.53), and atopic dermatitis (11.2), the researchers noted. “However, additional head-to-head studies are needed for direct comparisons of HRQOL in patients with various dermatoses,” they said.
The study findings were limited by the cross-sectional design of many of the included studies, and the limited number of assessment tools included in the analysis, the researchers noted. Other limitations were the lack of specific domain scores and the inclusion of only three studies from China, they said.
However, the results are consistent with findings from previous studies, and suggest that patients with AGA may benefit from psychological and psychosocial support, the researchers said.
Quality of life issues deserve attention
“Studies of the quality-of-life impact of various conditions are becoming more common in the medical literature,” Jamie B. MacKelfresh, MD, associate professor of dermatology, Emory University, Atlanta, said in an interview.
“Androgenetic alopecia is the most common type of hair loss in men and women,” she noted. “Hair loss can be labeled as a cosmetic concern, so it is important that providers understand the significant quality-of-life impact androgenetic alopecia has on the many people with this diagnosis,” she emphasized.
Dr. MacKelfresh, who was asked to comment on the study, said she was surprised that the subgroup analysis of the DLQI showed no significant difference between men and women. “This surprised me because a number of past studies have highlighted the relatively greater quality-of-life impact of hair loss on women compared to men,” she noted.
However, she added, “I was not surprised to see that androgenetic alopecia has a significant quality-of-life impact on many patients, and that physician objective assessments of the hair loss do not always correlate with the amount of quality-of-life impact,” said Dr. MacKelfresh. “In the patients I see, I find hair loss very often has a significant quality-of-life impact on patients, regardless of gender, and the amount of quality-of-life impact definitely does not always correlate with the objective amount of hair loss,” she noted.
A takeaway message for clinicians is to be aware that androgenetic alopecia frequently has a significant impact on patients, “particularly in the emotional dimension,” and can affect both men and women, Dr. MacKelfresh said. “Objective assessments of hair loss severity by providers may not accurately predict the degree of quality-of-life impact a patient may experience; therefore providers should include quality-of-life questions as part of their standard evaluation of patients with androgenetic alopecia,” she said. In addition to treating the hair loss, providers can help these patients by guiding them to psychological support resources, she emphasized.
More research is needed to assess the impact of androgenetic alopecia on “men, women, and the non-binary gender population,” as well as the relationship between self-esteem and hair loss, she said. “Finally, it would be helpful to understand what interventions can best help improve androgenetic alopecia patients’ quality of life,” she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. MacKelfresh had no financial conflicts to disclose.
and meta-analysis of 41 studies.
“Hair loss affects self-image, causes trichodynia, and plays a role in emotions and social activity, which may be associated with psychiatric problems and impaired health-related quality of life,” wrote Chun-Hsien Huang, MD, of Chang Gung Memorial Hospital, Linkou, Taiwan, and colleagues. However, systematic reviews of the associations between androgenetic alopecia (AGA) and health-related quality of life (HRQOL) are lacking, they said.
In a study published in JAMA Dermatology, the researchers reviewed data from a total of 7,995 AGA patients in 41 studies. The studies included 11 tools for HRQOL assessment and 29 tools for psychological assessment. Of these, the Dermatology Life Quality Index (DLQI) and the Hair-Specific Skindex-29 were used to assess quality of life, and the Center for Epidemiologic Studies Depression Scale (CES-D) was used for psychological assessment in the meta-analysis.
Overall, 27 studies identified 18 factors associated with HRQOL; those with an inverse effect were higher self-rated hair loss severity, lower VAS score, and higher educational level. Of note, neither physician-rated hair loss severity nor treatment response were factors in HRQOL, the researchers said.
The pooled DLQI score across studies was 8.16, and subgroup analysis showed no differences in HRQOL between men and women or between patients from European vs. Asian countries. However, five studies showed significant differences in HRQOL between men and women when different assessment tools were used, which emphasized the need for more studies to examine the association of AGA with HRQOL by sex, the researchers said.
The meta-analysis of the Hair-Specific Skindex-29 scores showed pooled averages of 21.95 for symptom dimension, 18.52 in function dimension, and 29.22 in emotion dimension. Of these, the emotion dimension scores indicated moderate emotional impairment.
The average pooled score on the CES-D in the meta-analysis was 14.98, indicating no association between AGA and depression, the researchers said. However, “depression accounts for only a part of the emotion dimension,” they said. “Therefore, emotion dimension could be impaired even if no depressive symptoms were noted.”
The pooled DLQI scores for AGA (8.16) were higher than scores for other skin conditions including alopecia areata (6.3), contact dermatitis (7.35), and acne vulgaris (7.45), but lower than the pooled scores for vitiligo (9.11), urticaria (9.8), psoriasis (10.53), and atopic dermatitis (11.2), the researchers noted. “However, additional head-to-head studies are needed for direct comparisons of HRQOL in patients with various dermatoses,” they said.
The study findings were limited by the cross-sectional design of many of the included studies, and the limited number of assessment tools included in the analysis, the researchers noted. Other limitations were the lack of specific domain scores and the inclusion of only three studies from China, they said.
However, the results are consistent with findings from previous studies, and suggest that patients with AGA may benefit from psychological and psychosocial support, the researchers said.
Quality of life issues deserve attention
“Studies of the quality-of-life impact of various conditions are becoming more common in the medical literature,” Jamie B. MacKelfresh, MD, associate professor of dermatology, Emory University, Atlanta, said in an interview.
“Androgenetic alopecia is the most common type of hair loss in men and women,” she noted. “Hair loss can be labeled as a cosmetic concern, so it is important that providers understand the significant quality-of-life impact androgenetic alopecia has on the many people with this diagnosis,” she emphasized.
Dr. MacKelfresh, who was asked to comment on the study, said she was surprised that the subgroup analysis of the DLQI showed no significant difference between men and women. “This surprised me because a number of past studies have highlighted the relatively greater quality-of-life impact of hair loss on women compared to men,” she noted.
However, she added, “I was not surprised to see that androgenetic alopecia has a significant quality-of-life impact on many patients, and that physician objective assessments of the hair loss do not always correlate with the amount of quality-of-life impact,” said Dr. MacKelfresh. “In the patients I see, I find hair loss very often has a significant quality-of-life impact on patients, regardless of gender, and the amount of quality-of-life impact definitely does not always correlate with the objective amount of hair loss,” she noted.
A takeaway message for clinicians is to be aware that androgenetic alopecia frequently has a significant impact on patients, “particularly in the emotional dimension,” and can affect both men and women, Dr. MacKelfresh said. “Objective assessments of hair loss severity by providers may not accurately predict the degree of quality-of-life impact a patient may experience; therefore providers should include quality-of-life questions as part of their standard evaluation of patients with androgenetic alopecia,” she said. In addition to treating the hair loss, providers can help these patients by guiding them to psychological support resources, she emphasized.
More research is needed to assess the impact of androgenetic alopecia on “men, women, and the non-binary gender population,” as well as the relationship between self-esteem and hair loss, she said. “Finally, it would be helpful to understand what interventions can best help improve androgenetic alopecia patients’ quality of life,” she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. MacKelfresh had no financial conflicts to disclose.
and meta-analysis of 41 studies.
“Hair loss affects self-image, causes trichodynia, and plays a role in emotions and social activity, which may be associated with psychiatric problems and impaired health-related quality of life,” wrote Chun-Hsien Huang, MD, of Chang Gung Memorial Hospital, Linkou, Taiwan, and colleagues. However, systematic reviews of the associations between androgenetic alopecia (AGA) and health-related quality of life (HRQOL) are lacking, they said.
In a study published in JAMA Dermatology, the researchers reviewed data from a total of 7,995 AGA patients in 41 studies. The studies included 11 tools for HRQOL assessment and 29 tools for psychological assessment. Of these, the Dermatology Life Quality Index (DLQI) and the Hair-Specific Skindex-29 were used to assess quality of life, and the Center for Epidemiologic Studies Depression Scale (CES-D) was used for psychological assessment in the meta-analysis.
Overall, 27 studies identified 18 factors associated with HRQOL; those with an inverse effect were higher self-rated hair loss severity, lower VAS score, and higher educational level. Of note, neither physician-rated hair loss severity nor treatment response were factors in HRQOL, the researchers said.
The pooled DLQI score across studies was 8.16, and subgroup analysis showed no differences in HRQOL between men and women or between patients from European vs. Asian countries. However, five studies showed significant differences in HRQOL between men and women when different assessment tools were used, which emphasized the need for more studies to examine the association of AGA with HRQOL by sex, the researchers said.
The meta-analysis of the Hair-Specific Skindex-29 scores showed pooled averages of 21.95 for symptom dimension, 18.52 in function dimension, and 29.22 in emotion dimension. Of these, the emotion dimension scores indicated moderate emotional impairment.
The average pooled score on the CES-D in the meta-analysis was 14.98, indicating no association between AGA and depression, the researchers said. However, “depression accounts for only a part of the emotion dimension,” they said. “Therefore, emotion dimension could be impaired even if no depressive symptoms were noted.”
The pooled DLQI scores for AGA (8.16) were higher than scores for other skin conditions including alopecia areata (6.3), contact dermatitis (7.35), and acne vulgaris (7.45), but lower than the pooled scores for vitiligo (9.11), urticaria (9.8), psoriasis (10.53), and atopic dermatitis (11.2), the researchers noted. “However, additional head-to-head studies are needed for direct comparisons of HRQOL in patients with various dermatoses,” they said.
The study findings were limited by the cross-sectional design of many of the included studies, and the limited number of assessment tools included in the analysis, the researchers noted. Other limitations were the lack of specific domain scores and the inclusion of only three studies from China, they said.
However, the results are consistent with findings from previous studies, and suggest that patients with AGA may benefit from psychological and psychosocial support, the researchers said.
Quality of life issues deserve attention
“Studies of the quality-of-life impact of various conditions are becoming more common in the medical literature,” Jamie B. MacKelfresh, MD, associate professor of dermatology, Emory University, Atlanta, said in an interview.
“Androgenetic alopecia is the most common type of hair loss in men and women,” she noted. “Hair loss can be labeled as a cosmetic concern, so it is important that providers understand the significant quality-of-life impact androgenetic alopecia has on the many people with this diagnosis,” she emphasized.
Dr. MacKelfresh, who was asked to comment on the study, said she was surprised that the subgroup analysis of the DLQI showed no significant difference between men and women. “This surprised me because a number of past studies have highlighted the relatively greater quality-of-life impact of hair loss on women compared to men,” she noted.
However, she added, “I was not surprised to see that androgenetic alopecia has a significant quality-of-life impact on many patients, and that physician objective assessments of the hair loss do not always correlate with the amount of quality-of-life impact,” said Dr. MacKelfresh. “In the patients I see, I find hair loss very often has a significant quality-of-life impact on patients, regardless of gender, and the amount of quality-of-life impact definitely does not always correlate with the objective amount of hair loss,” she noted.
A takeaway message for clinicians is to be aware that androgenetic alopecia frequently has a significant impact on patients, “particularly in the emotional dimension,” and can affect both men and women, Dr. MacKelfresh said. “Objective assessments of hair loss severity by providers may not accurately predict the degree of quality-of-life impact a patient may experience; therefore providers should include quality-of-life questions as part of their standard evaluation of patients with androgenetic alopecia,” she said. In addition to treating the hair loss, providers can help these patients by guiding them to psychological support resources, she emphasized.
More research is needed to assess the impact of androgenetic alopecia on “men, women, and the non-binary gender population,” as well as the relationship between self-esteem and hair loss, she said. “Finally, it would be helpful to understand what interventions can best help improve androgenetic alopecia patients’ quality of life,” she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. MacKelfresh had no financial conflicts to disclose.
FROM JAMA DERMATOLOGY
Reckoning with America’s alarming rise in anti-Asian hate
On March 16, the world was witness to a horrific act of violence when a gunman killed six Asian American women and two others at spas in the Atlanta, Georgia area. The attack prompted a national outcry and protests against the rising levels of hate and violence directed at Asian Americans and Pacific Islanders (AAPI), a community that has experienced a profound and disturbing legacy of racism in American history.
Despite this fact, my own understanding and awareness of the hate and racism experienced by the AAPI community, then and now, would be described as limited at best. Was I aware on some level? Perhaps. But if I’m being honest, I have not fully appreciated the unique experiences of AAPI colleagues, friends, and students.
That changed when I attended a White Coats Against Asian Hate & Racism rally, held by the George Washington University School of Medicine and Health Sciences 2 months after the Atlanta killings. Hearing my colleagues speak of their personal experiences, I quickly realized my lack of education on the subject of how systemic racism has long affected Asian Americans in this country.
Measuring the alarming rise in anti-Asian hate
The data supporting a rise in anti-Asian hate crimes have been staring us in the face for decades but have drawn increasing attention since the beginning of the COVID-19 pandemic, when these already distressingly high numbers experienced a steep rise.
Before looking at these figures, though, we must begin by defining what is considered a hate crime versus a hate incident. The National Asian Pacific American Bar Association and Asian & Pacific Islander American Health Forum have produced a beneficial summary document on precisely what separates these terms:
- A hate crime is a crime committed on the basis of the victim’s perceived or actual race, color, religion, national origin, sexual orientation, gender identity, or disability. It differs from “regular” crime in that its victims include the immediate crime target and others like them. Hate crimes affect families, communities, and, at times, an entire nation.
- A hate incident describes acts of prejudice that are not crimes and do not involve violence, threats, or property damage. The most common examples are isolated forms of speech, such as racial slurs.
Stop AAPI Hate (SAH) was founded in March 2020 as a coalition to track and analyze incidents of hate against this community. SAH’s 2020-2021 national report details 3,795 hate incidents that occurred from March 19, 2020, to Feb. 28, 2021. In a notable parallel to the Georgia killings, SAH found that Asian American women reported hate incidents 2.3 times more often than men and that businesses were the primary site of discrimination.
This rise in hate incidents has occurred in parallel with an increase in Asian American hate crimes. Recently, the Center for the Study of Hate and Extremism (CSUSB) released its Report to the Nation: Anti-Asian Prejudice & Hate Crime. I re-read that data point multiple times, thinking it must be in error. If you’re asking exactly why I was having difficulty accepting this data, you have to appreciate these two critical points:
- Per the CSUSB, anti-Asian hate crimes were already surging by 146% in 2020.
- This surge occurred while overall hate crimes dropped by 7%.
So, if 2020 was a surge, the first quarter of 2021 is a hurricane. What’s perhaps most concerning is that these data only capture reported cases and therefore are a fraction of the total.
Undoubtedly, we are living through an unprecedented rise in anti-Asian hate incidents and hate crimes since the start of the pandemic. This rise in hate-related events paralleled the many pandemic-related stressors (disease, isolation, economics, mental health, etc.). Should anyone have been surprised when this most recent deadly spike of anti-Asian hate occurred in the first quarter of 2021?
Hate’s toll on mental health
As a psychiatrist, I’ve spent my entire career working with dedicated teams to treat patients with mental health disorders. Currently, hate is not classified by the Diagnostic and Statistical Manual of Mental Disorders as a mental illness. However, I can’t think of another emotion that is a better candidate for further research and scientific instigation, if for no other reason than to better understand when prejudice and bias transform into hatred and crime.
Surprisingly, there has been relatively little research on the topic of hate in the fields of psychology and psychiatry. I’d be willing to wager that if you asked a typical graduating class of medical students to give you an actual working definition of the emotion of hate, most would be at a loss for words.
Dr. Fischer and Dr. Halperin published a helpful article that gives a functional perspective on hate. The authors cover a great deal of research on hate and offer the following four starting points valuable in considering it:
- “Hate is different from anger because an anger target is appraised as someone whose behavior can be influenced and changed.”
- “A hate target, on the contrary, implies appraisals of the other’s malevolent nature and malicious intent.”
- “Hate is characterized by appraisals that imply a stable perception of a person or group and thus the incapability to change the extremely negative characteristics attributed to the target of hate.”
- “Everyday observations also suggest that hate is so powerful that it does, not just temporarily but permanently, destroy relations between individuals or groups.”
When I view hate with these insights in mind, it completely changes how I choose to utilize the word or concept. Hate is an emotion whose goal/action tendency is to eliminate groups (not just people or obstacles) and destroy any current or future relationships. We can take this a step further in noting that hate spreads, not only to the intended targets but potentially my “own” group. Similar to secondhand smoke, there is no risk-free exposure to hate or racism.
In the past decade, a robust body of evidence has emerged that clearly illustrates the negative health impacts of racism. Dr. Paradies and colleagues performed a systematic meta-analysis explicitly focused on racism as a determinant of health, finding that it was associated with poorer mental health, including depression, anxiety, and psychological distress. Over the past two decades, researchers have increasingly looked at the effects of racial discrimination on the AAPI community. In their 2009 review article, Dr. Gee and colleagues identified 62 empirical articles assessing the relation between discrimination and health among Asian Americans. Most of the studies found that discrimination was associated with poorer health. Of the 40 studies focused on mental health, 37 reported that discrimination was associated with poorer outcomes.
SAH recently released its very illuminating Mental Health Report. Among several key findings, two in particular caught my attention. First, Asian Americans who have experienced racism are more stressed by anti-Asian hate than the pandemic itself. Second, one in five Asian Americans who have experienced racism display racial trauma, the psychological and emotional harm caused by racism. Given the rise in hate crimes, there must be concern regarding the level of trauma being inflicted upon the Asian American community.
A complete review of the health effects of racism is beyond this article’s scope. Still, the previously mentioned studies further support the need to treat racism in general, and specifically anti-Asian hate, as the urgent public health concern that it truly is. The U.S. government recently outlined an action plan to respond to anti-Asian violence, xenophobia, and bias. These are helpful first steps, but much more is required on a societal and individual level, given the mental health disparities faced by the AAPI community.
Determining the best ways to address this urgent public health concern can be overwhelming, exhausting, and outright demoralizing. The bottom line is that if we do nothing, communities and groups will continue to suffer the effects of racial hatred. These consequences are severe and transgenerational.
But we must start somewhere. For me, that begins by gaining a better understanding of the emotion of hate and my role in either facilitating or stopping it, and by listening, listening, and listening some more to AAPI colleagues, friends, and family about their lived experience with anti-Asian hate.
A version of this article first appeared on Medscape.com.
On March 16, the world was witness to a horrific act of violence when a gunman killed six Asian American women and two others at spas in the Atlanta, Georgia area. The attack prompted a national outcry and protests against the rising levels of hate and violence directed at Asian Americans and Pacific Islanders (AAPI), a community that has experienced a profound and disturbing legacy of racism in American history.
Despite this fact, my own understanding and awareness of the hate and racism experienced by the AAPI community, then and now, would be described as limited at best. Was I aware on some level? Perhaps. But if I’m being honest, I have not fully appreciated the unique experiences of AAPI colleagues, friends, and students.
That changed when I attended a White Coats Against Asian Hate & Racism rally, held by the George Washington University School of Medicine and Health Sciences 2 months after the Atlanta killings. Hearing my colleagues speak of their personal experiences, I quickly realized my lack of education on the subject of how systemic racism has long affected Asian Americans in this country.
Measuring the alarming rise in anti-Asian hate
The data supporting a rise in anti-Asian hate crimes have been staring us in the face for decades but have drawn increasing attention since the beginning of the COVID-19 pandemic, when these already distressingly high numbers experienced a steep rise.
Before looking at these figures, though, we must begin by defining what is considered a hate crime versus a hate incident. The National Asian Pacific American Bar Association and Asian & Pacific Islander American Health Forum have produced a beneficial summary document on precisely what separates these terms:
- A hate crime is a crime committed on the basis of the victim’s perceived or actual race, color, religion, national origin, sexual orientation, gender identity, or disability. It differs from “regular” crime in that its victims include the immediate crime target and others like them. Hate crimes affect families, communities, and, at times, an entire nation.
- A hate incident describes acts of prejudice that are not crimes and do not involve violence, threats, or property damage. The most common examples are isolated forms of speech, such as racial slurs.
Stop AAPI Hate (SAH) was founded in March 2020 as a coalition to track and analyze incidents of hate against this community. SAH’s 2020-2021 national report details 3,795 hate incidents that occurred from March 19, 2020, to Feb. 28, 2021. In a notable parallel to the Georgia killings, SAH found that Asian American women reported hate incidents 2.3 times more often than men and that businesses were the primary site of discrimination.
This rise in hate incidents has occurred in parallel with an increase in Asian American hate crimes. Recently, the Center for the Study of Hate and Extremism (CSUSB) released its Report to the Nation: Anti-Asian Prejudice & Hate Crime. I re-read that data point multiple times, thinking it must be in error. If you’re asking exactly why I was having difficulty accepting this data, you have to appreciate these two critical points:
- Per the CSUSB, anti-Asian hate crimes were already surging by 146% in 2020.
- This surge occurred while overall hate crimes dropped by 7%.
So, if 2020 was a surge, the first quarter of 2021 is a hurricane. What’s perhaps most concerning is that these data only capture reported cases and therefore are a fraction of the total.
Undoubtedly, we are living through an unprecedented rise in anti-Asian hate incidents and hate crimes since the start of the pandemic. This rise in hate-related events paralleled the many pandemic-related stressors (disease, isolation, economics, mental health, etc.). Should anyone have been surprised when this most recent deadly spike of anti-Asian hate occurred in the first quarter of 2021?
Hate’s toll on mental health
As a psychiatrist, I’ve spent my entire career working with dedicated teams to treat patients with mental health disorders. Currently, hate is not classified by the Diagnostic and Statistical Manual of Mental Disorders as a mental illness. However, I can’t think of another emotion that is a better candidate for further research and scientific instigation, if for no other reason than to better understand when prejudice and bias transform into hatred and crime.
Surprisingly, there has been relatively little research on the topic of hate in the fields of psychology and psychiatry. I’d be willing to wager that if you asked a typical graduating class of medical students to give you an actual working definition of the emotion of hate, most would be at a loss for words.
Dr. Fischer and Dr. Halperin published a helpful article that gives a functional perspective on hate. The authors cover a great deal of research on hate and offer the following four starting points valuable in considering it:
- “Hate is different from anger because an anger target is appraised as someone whose behavior can be influenced and changed.”
- “A hate target, on the contrary, implies appraisals of the other’s malevolent nature and malicious intent.”
- “Hate is characterized by appraisals that imply a stable perception of a person or group and thus the incapability to change the extremely negative characteristics attributed to the target of hate.”
- “Everyday observations also suggest that hate is so powerful that it does, not just temporarily but permanently, destroy relations between individuals or groups.”
When I view hate with these insights in mind, it completely changes how I choose to utilize the word or concept. Hate is an emotion whose goal/action tendency is to eliminate groups (not just people or obstacles) and destroy any current or future relationships. We can take this a step further in noting that hate spreads, not only to the intended targets but potentially my “own” group. Similar to secondhand smoke, there is no risk-free exposure to hate or racism.
In the past decade, a robust body of evidence has emerged that clearly illustrates the negative health impacts of racism. Dr. Paradies and colleagues performed a systematic meta-analysis explicitly focused on racism as a determinant of health, finding that it was associated with poorer mental health, including depression, anxiety, and psychological distress. Over the past two decades, researchers have increasingly looked at the effects of racial discrimination on the AAPI community. In their 2009 review article, Dr. Gee and colleagues identified 62 empirical articles assessing the relation between discrimination and health among Asian Americans. Most of the studies found that discrimination was associated with poorer health. Of the 40 studies focused on mental health, 37 reported that discrimination was associated with poorer outcomes.
SAH recently released its very illuminating Mental Health Report. Among several key findings, two in particular caught my attention. First, Asian Americans who have experienced racism are more stressed by anti-Asian hate than the pandemic itself. Second, one in five Asian Americans who have experienced racism display racial trauma, the psychological and emotional harm caused by racism. Given the rise in hate crimes, there must be concern regarding the level of trauma being inflicted upon the Asian American community.
A complete review of the health effects of racism is beyond this article’s scope. Still, the previously mentioned studies further support the need to treat racism in general, and specifically anti-Asian hate, as the urgent public health concern that it truly is. The U.S. government recently outlined an action plan to respond to anti-Asian violence, xenophobia, and bias. These are helpful first steps, but much more is required on a societal and individual level, given the mental health disparities faced by the AAPI community.
Determining the best ways to address this urgent public health concern can be overwhelming, exhausting, and outright demoralizing. The bottom line is that if we do nothing, communities and groups will continue to suffer the effects of racial hatred. These consequences are severe and transgenerational.
But we must start somewhere. For me, that begins by gaining a better understanding of the emotion of hate and my role in either facilitating or stopping it, and by listening, listening, and listening some more to AAPI colleagues, friends, and family about their lived experience with anti-Asian hate.
A version of this article first appeared on Medscape.com.
On March 16, the world was witness to a horrific act of violence when a gunman killed six Asian American women and two others at spas in the Atlanta, Georgia area. The attack prompted a national outcry and protests against the rising levels of hate and violence directed at Asian Americans and Pacific Islanders (AAPI), a community that has experienced a profound and disturbing legacy of racism in American history.
Despite this fact, my own understanding and awareness of the hate and racism experienced by the AAPI community, then and now, would be described as limited at best. Was I aware on some level? Perhaps. But if I’m being honest, I have not fully appreciated the unique experiences of AAPI colleagues, friends, and students.
That changed when I attended a White Coats Against Asian Hate & Racism rally, held by the George Washington University School of Medicine and Health Sciences 2 months after the Atlanta killings. Hearing my colleagues speak of their personal experiences, I quickly realized my lack of education on the subject of how systemic racism has long affected Asian Americans in this country.
Measuring the alarming rise in anti-Asian hate
The data supporting a rise in anti-Asian hate crimes have been staring us in the face for decades but have drawn increasing attention since the beginning of the COVID-19 pandemic, when these already distressingly high numbers experienced a steep rise.
Before looking at these figures, though, we must begin by defining what is considered a hate crime versus a hate incident. The National Asian Pacific American Bar Association and Asian & Pacific Islander American Health Forum have produced a beneficial summary document on precisely what separates these terms:
- A hate crime is a crime committed on the basis of the victim’s perceived or actual race, color, religion, national origin, sexual orientation, gender identity, or disability. It differs from “regular” crime in that its victims include the immediate crime target and others like them. Hate crimes affect families, communities, and, at times, an entire nation.
- A hate incident describes acts of prejudice that are not crimes and do not involve violence, threats, or property damage. The most common examples are isolated forms of speech, such as racial slurs.
Stop AAPI Hate (SAH) was founded in March 2020 as a coalition to track and analyze incidents of hate against this community. SAH’s 2020-2021 national report details 3,795 hate incidents that occurred from March 19, 2020, to Feb. 28, 2021. In a notable parallel to the Georgia killings, SAH found that Asian American women reported hate incidents 2.3 times more often than men and that businesses were the primary site of discrimination.
This rise in hate incidents has occurred in parallel with an increase in Asian American hate crimes. Recently, the Center for the Study of Hate and Extremism (CSUSB) released its Report to the Nation: Anti-Asian Prejudice & Hate Crime. I re-read that data point multiple times, thinking it must be in error. If you’re asking exactly why I was having difficulty accepting this data, you have to appreciate these two critical points:
- Per the CSUSB, anti-Asian hate crimes were already surging by 146% in 2020.
- This surge occurred while overall hate crimes dropped by 7%.
So, if 2020 was a surge, the first quarter of 2021 is a hurricane. What’s perhaps most concerning is that these data only capture reported cases and therefore are a fraction of the total.
Undoubtedly, we are living through an unprecedented rise in anti-Asian hate incidents and hate crimes since the start of the pandemic. This rise in hate-related events paralleled the many pandemic-related stressors (disease, isolation, economics, mental health, etc.). Should anyone have been surprised when this most recent deadly spike of anti-Asian hate occurred in the first quarter of 2021?
Hate’s toll on mental health
As a psychiatrist, I’ve spent my entire career working with dedicated teams to treat patients with mental health disorders. Currently, hate is not classified by the Diagnostic and Statistical Manual of Mental Disorders as a mental illness. However, I can’t think of another emotion that is a better candidate for further research and scientific instigation, if for no other reason than to better understand when prejudice and bias transform into hatred and crime.
Surprisingly, there has been relatively little research on the topic of hate in the fields of psychology and psychiatry. I’d be willing to wager that if you asked a typical graduating class of medical students to give you an actual working definition of the emotion of hate, most would be at a loss for words.
Dr. Fischer and Dr. Halperin published a helpful article that gives a functional perspective on hate. The authors cover a great deal of research on hate and offer the following four starting points valuable in considering it:
- “Hate is different from anger because an anger target is appraised as someone whose behavior can be influenced and changed.”
- “A hate target, on the contrary, implies appraisals of the other’s malevolent nature and malicious intent.”
- “Hate is characterized by appraisals that imply a stable perception of a person or group and thus the incapability to change the extremely negative characteristics attributed to the target of hate.”
- “Everyday observations also suggest that hate is so powerful that it does, not just temporarily but permanently, destroy relations between individuals or groups.”
When I view hate with these insights in mind, it completely changes how I choose to utilize the word or concept. Hate is an emotion whose goal/action tendency is to eliminate groups (not just people or obstacles) and destroy any current or future relationships. We can take this a step further in noting that hate spreads, not only to the intended targets but potentially my “own” group. Similar to secondhand smoke, there is no risk-free exposure to hate or racism.
In the past decade, a robust body of evidence has emerged that clearly illustrates the negative health impacts of racism. Dr. Paradies and colleagues performed a systematic meta-analysis explicitly focused on racism as a determinant of health, finding that it was associated with poorer mental health, including depression, anxiety, and psychological distress. Over the past two decades, researchers have increasingly looked at the effects of racial discrimination on the AAPI community. In their 2009 review article, Dr. Gee and colleagues identified 62 empirical articles assessing the relation between discrimination and health among Asian Americans. Most of the studies found that discrimination was associated with poorer health. Of the 40 studies focused on mental health, 37 reported that discrimination was associated with poorer outcomes.
SAH recently released its very illuminating Mental Health Report. Among several key findings, two in particular caught my attention. First, Asian Americans who have experienced racism are more stressed by anti-Asian hate than the pandemic itself. Second, one in five Asian Americans who have experienced racism display racial trauma, the psychological and emotional harm caused by racism. Given the rise in hate crimes, there must be concern regarding the level of trauma being inflicted upon the Asian American community.
A complete review of the health effects of racism is beyond this article’s scope. Still, the previously mentioned studies further support the need to treat racism in general, and specifically anti-Asian hate, as the urgent public health concern that it truly is. The U.S. government recently outlined an action plan to respond to anti-Asian violence, xenophobia, and bias. These are helpful first steps, but much more is required on a societal and individual level, given the mental health disparities faced by the AAPI community.
Determining the best ways to address this urgent public health concern can be overwhelming, exhausting, and outright demoralizing. The bottom line is that if we do nothing, communities and groups will continue to suffer the effects of racial hatred. These consequences are severe and transgenerational.
But we must start somewhere. For me, that begins by gaining a better understanding of the emotion of hate and my role in either facilitating or stopping it, and by listening, listening, and listening some more to AAPI colleagues, friends, and family about their lived experience with anti-Asian hate.
A version of this article first appeared on Medscape.com.