User login
Acoustic pulse boosts laser tattoo removal
In tattoo removal, the impact of laser treatments in single office visits is limited because of the laser’s effects on the skin. Now, a new study suggests that a
“As a result,” the authors of the study wrote, “a lower total number of office visits will likely be required for complete tattoo removal leading to improved convenience and efficiency as well as increased satisfaction for both patients and clinicians.” The study, led by cosmetic surgeon Michael S. Kaminer, MD, of SkinCare Physicians in Chestnut Hill, Mass., appeared in Lasers in Surgery and Medicine.
In the study, he and his coauthors pointed out that tattoos are most frequently removed with short-pulse high-fluence lasers, such as a 1064-nm Nd:YAG Q‐switched (QS) laser. However, “the QS laser has a limited ability to affect the tattoo ink pigment particles in each treatment session due to shielding of the pigment particles caused by both the agglomeration of the pigment particles and laser‐induced epidermal and dermal vacuoles known as ‘whitening.’ ” Therefore, “use of the QS laser often requires 10 or more single‐pass office sessions to achieve acceptable fading results.”
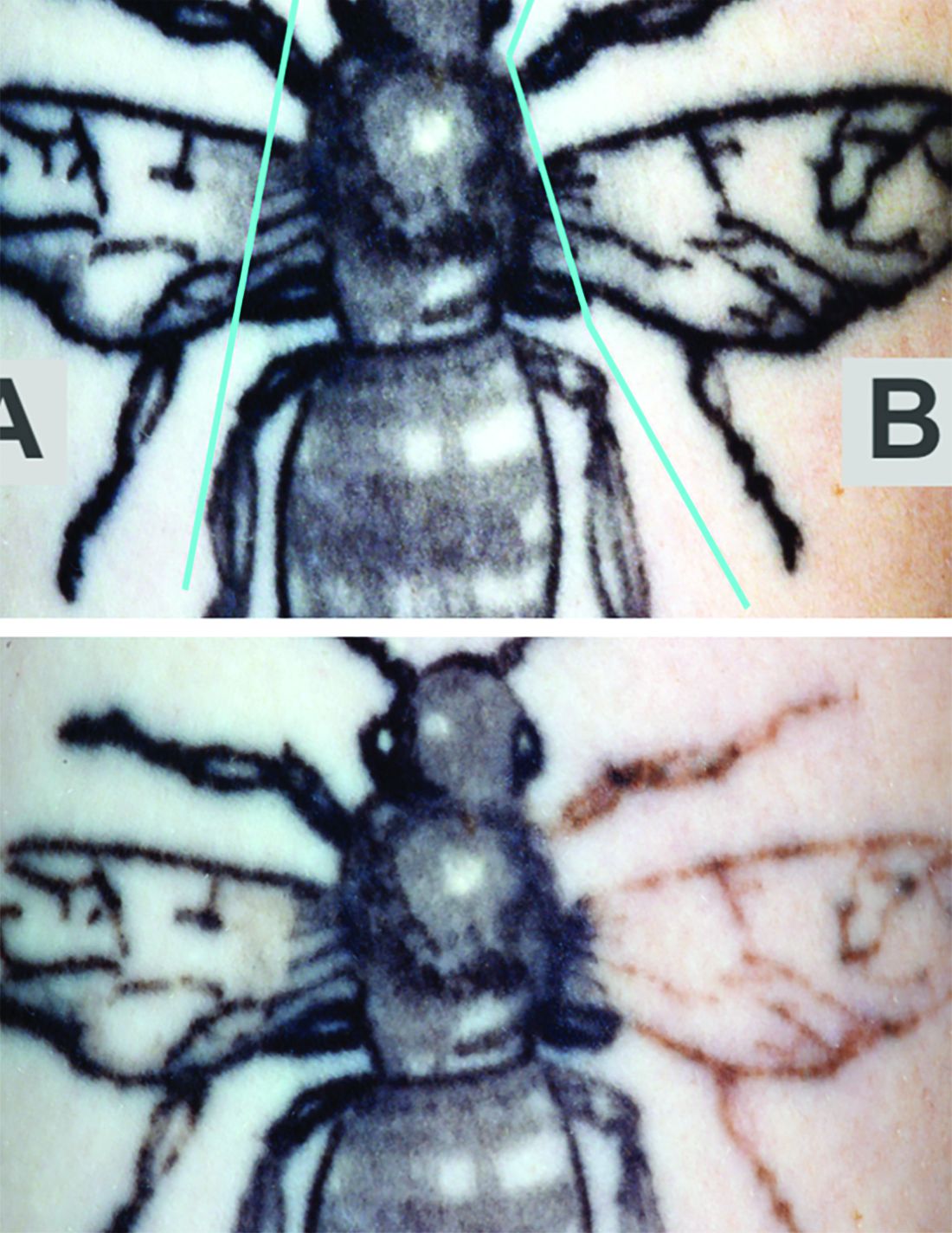
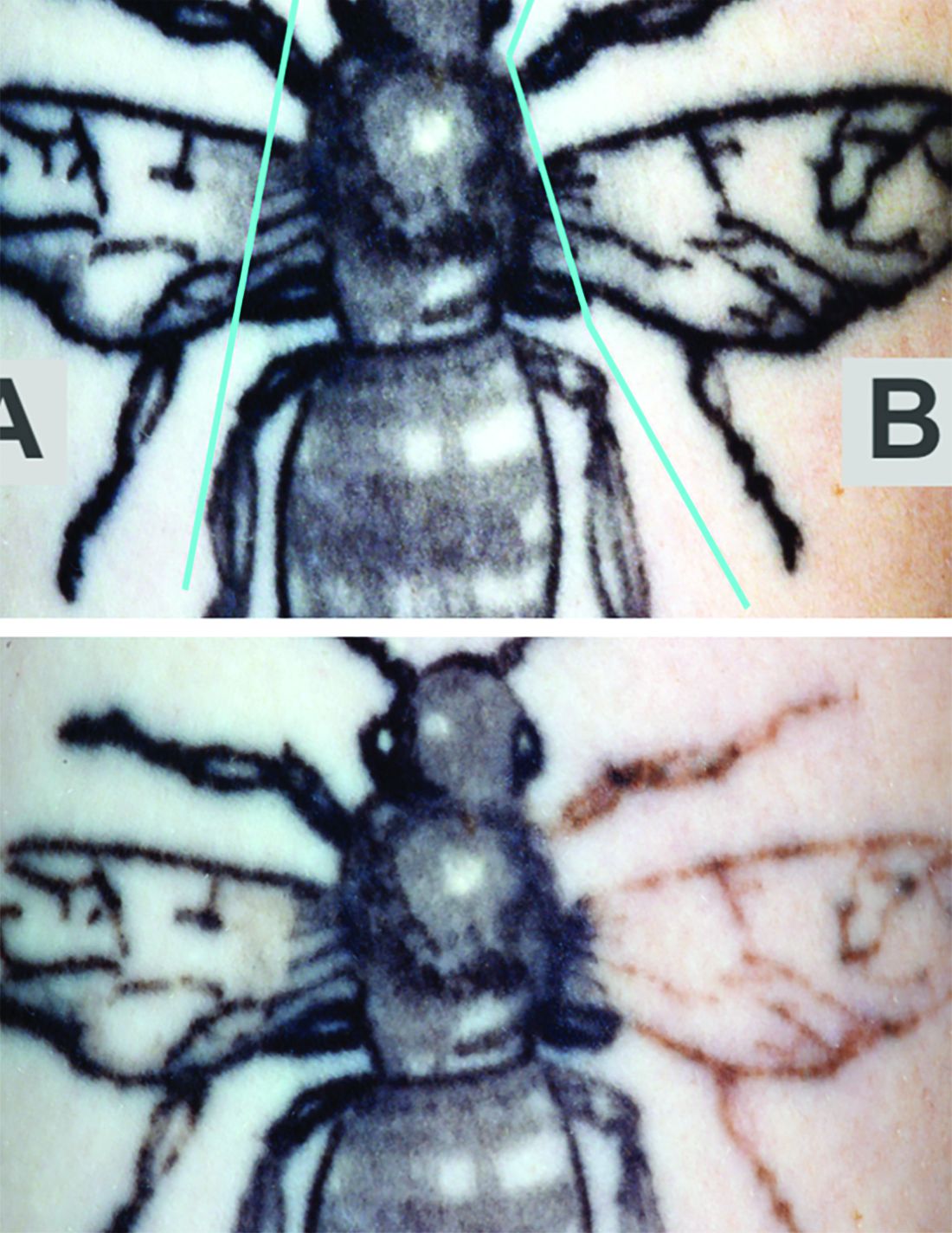
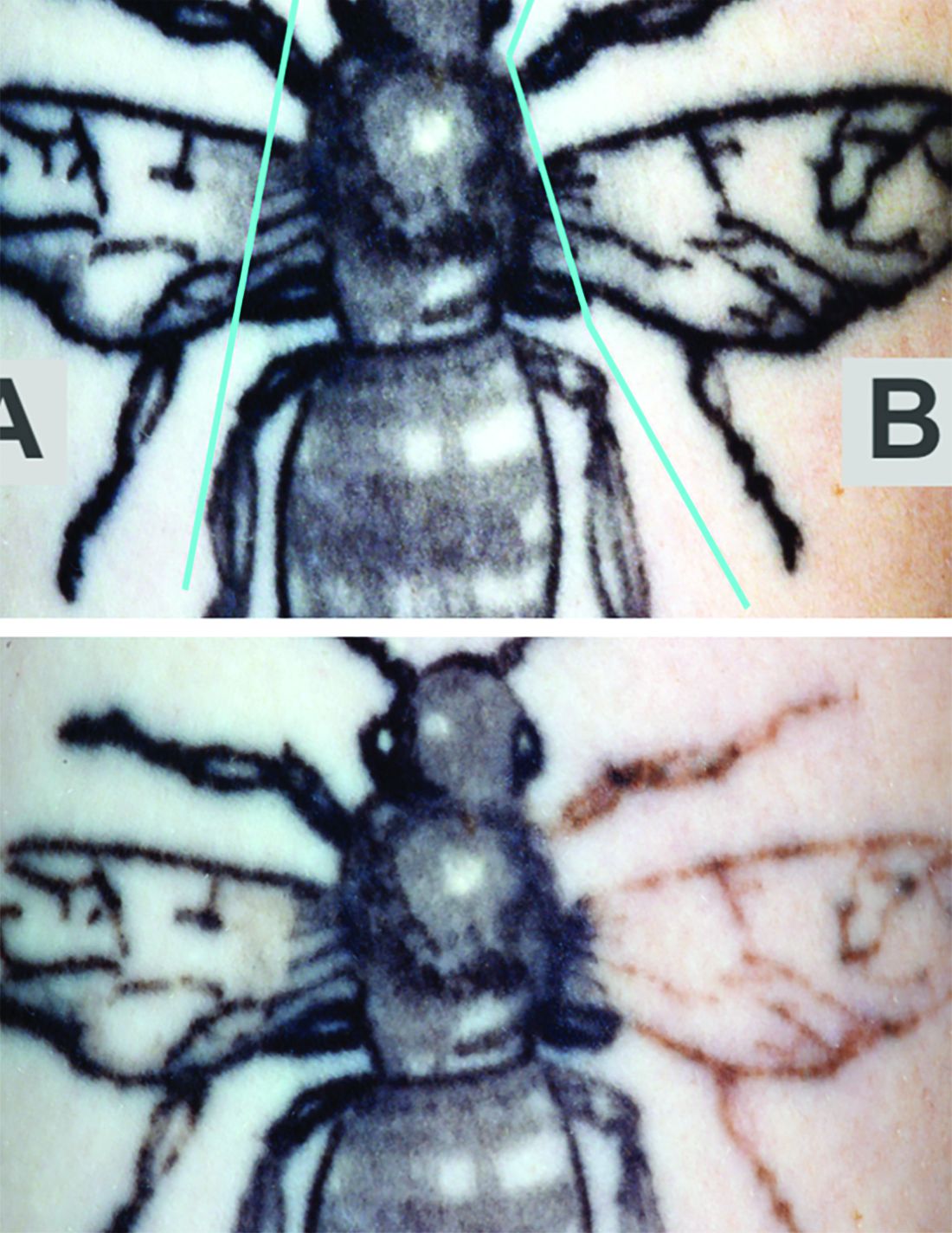
The study evaluated whether the use of a rapid acoustic pulse (RAP) device could reduce the whitening effect by clearing vacuoles and make it possible to increase the number of potential laser passes. In the single-center, prospective trial, they treated 32 black-ink tattoos in 21 patients, dividing the tattoos into zones and treating them differently: One zone received at least three consecutive laser passes alternating with a minute of treatment with the RAP device, one received single-pass laser treatment, and one received no treatment.
Reviewers assessed the tattoos for fading at 12 weeks. Average percent fading was higher in the laser/RAP group, compared with the laser-only group (44% and 25%, respectively, P less than .01). The percentages of tattoos with more than 50% fading (38% vs. 9%, P less than .01) and more than 75% fading (22% vs. 3%, P less than .05) were also higher in the laser/RAP group, compared with the laser-only group.
“Further clinical studies will be performed to investigate the broader applicability of the RAP device as an accessory device to reduce the number of laser tattoo removal sessions for other tattoo ink colors in a broader range of skin types,” the researchers commented, noting that the study included patients with Fitzpatrick skin types I-III.
The study was funded by Soliton, which provided the equipment. One of the six authors is an employee of the company The other authors reported no relevant disclosures.
SOURCE: Kaminer MS et al. Lasers Surg Med. 2019 Sep 19. doi: 10.1002/lsm.23163.
In tattoo removal, the impact of laser treatments in single office visits is limited because of the laser’s effects on the skin. Now, a new study suggests that a
“As a result,” the authors of the study wrote, “a lower total number of office visits will likely be required for complete tattoo removal leading to improved convenience and efficiency as well as increased satisfaction for both patients and clinicians.” The study, led by cosmetic surgeon Michael S. Kaminer, MD, of SkinCare Physicians in Chestnut Hill, Mass., appeared in Lasers in Surgery and Medicine.
In the study, he and his coauthors pointed out that tattoos are most frequently removed with short-pulse high-fluence lasers, such as a 1064-nm Nd:YAG Q‐switched (QS) laser. However, “the QS laser has a limited ability to affect the tattoo ink pigment particles in each treatment session due to shielding of the pigment particles caused by both the agglomeration of the pigment particles and laser‐induced epidermal and dermal vacuoles known as ‘whitening.’ ” Therefore, “use of the QS laser often requires 10 or more single‐pass office sessions to achieve acceptable fading results.”
The study evaluated whether the use of a rapid acoustic pulse (RAP) device could reduce the whitening effect by clearing vacuoles and make it possible to increase the number of potential laser passes. In the single-center, prospective trial, they treated 32 black-ink tattoos in 21 patients, dividing the tattoos into zones and treating them differently: One zone received at least three consecutive laser passes alternating with a minute of treatment with the RAP device, one received single-pass laser treatment, and one received no treatment.
Reviewers assessed the tattoos for fading at 12 weeks. Average percent fading was higher in the laser/RAP group, compared with the laser-only group (44% and 25%, respectively, P less than .01). The percentages of tattoos with more than 50% fading (38% vs. 9%, P less than .01) and more than 75% fading (22% vs. 3%, P less than .05) were also higher in the laser/RAP group, compared with the laser-only group.
“Further clinical studies will be performed to investigate the broader applicability of the RAP device as an accessory device to reduce the number of laser tattoo removal sessions for other tattoo ink colors in a broader range of skin types,” the researchers commented, noting that the study included patients with Fitzpatrick skin types I-III.
The study was funded by Soliton, which provided the equipment. One of the six authors is an employee of the company The other authors reported no relevant disclosures.
SOURCE: Kaminer MS et al. Lasers Surg Med. 2019 Sep 19. doi: 10.1002/lsm.23163.
In tattoo removal, the impact of laser treatments in single office visits is limited because of the laser’s effects on the skin. Now, a new study suggests that a
“As a result,” the authors of the study wrote, “a lower total number of office visits will likely be required for complete tattoo removal leading to improved convenience and efficiency as well as increased satisfaction for both patients and clinicians.” The study, led by cosmetic surgeon Michael S. Kaminer, MD, of SkinCare Physicians in Chestnut Hill, Mass., appeared in Lasers in Surgery and Medicine.
In the study, he and his coauthors pointed out that tattoos are most frequently removed with short-pulse high-fluence lasers, such as a 1064-nm Nd:YAG Q‐switched (QS) laser. However, “the QS laser has a limited ability to affect the tattoo ink pigment particles in each treatment session due to shielding of the pigment particles caused by both the agglomeration of the pigment particles and laser‐induced epidermal and dermal vacuoles known as ‘whitening.’ ” Therefore, “use of the QS laser often requires 10 or more single‐pass office sessions to achieve acceptable fading results.”
The study evaluated whether the use of a rapid acoustic pulse (RAP) device could reduce the whitening effect by clearing vacuoles and make it possible to increase the number of potential laser passes. In the single-center, prospective trial, they treated 32 black-ink tattoos in 21 patients, dividing the tattoos into zones and treating them differently: One zone received at least three consecutive laser passes alternating with a minute of treatment with the RAP device, one received single-pass laser treatment, and one received no treatment.
Reviewers assessed the tattoos for fading at 12 weeks. Average percent fading was higher in the laser/RAP group, compared with the laser-only group (44% and 25%, respectively, P less than .01). The percentages of tattoos with more than 50% fading (38% vs. 9%, P less than .01) and more than 75% fading (22% vs. 3%, P less than .05) were also higher in the laser/RAP group, compared with the laser-only group.
“Further clinical studies will be performed to investigate the broader applicability of the RAP device as an accessory device to reduce the number of laser tattoo removal sessions for other tattoo ink colors in a broader range of skin types,” the researchers commented, noting that the study included patients with Fitzpatrick skin types I-III.
The study was funded by Soliton, which provided the equipment. One of the six authors is an employee of the company The other authors reported no relevant disclosures.
SOURCE: Kaminer MS et al. Lasers Surg Med. 2019 Sep 19. doi: 10.1002/lsm.23163.
FROM LASERS IN SURGERY AND MEDICINE
Thread lifts making a comeback, but long-term effects remain unclear
SAN DIEGO – The use of threads to improve skin laxity is making a comeback, thanks largely to advances in absorbable sutures.
“Thread lifts were popularized in the 1990s, but I think they were misrepresented as an alternative to a surgical face-lift, which remains the gold standard,” Arisa E. Ortiz, MD, said at the annual Masters of Aesthetics Symposium. “A thread lift is certainly not like a traditional face-lift; it’s much more subtle.”
In the 1990s, clinicians used nonabsorbable sutures for thread lifts, including polypropylene-barbed threads, which caused adverse events ranging from extrusion and migration to thread expulsion, dimpling, granuloma formation, and prolonged pain. As a result, the Food and Drug Administration withdrew its approval of contour thread aesthetic procedures in 2009. Since then, the development of absorbable threads made from polydioxanone (PDO) and poly-
“There are some nice benefits to thread lifts,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “You get immediate results, which is always nice for patients, but with tissue tightening using energy-based devices, results are unpredictable and it can take 6 months to see the results. With resorbable sutures, we’re seeing fewer complications, and the amount of lifting is more predictable because you’re physically lifting the tissue. In some cases, threads are able to lift tissue more than energy-based devices. There is minimal recovery, it requires local anesthesia, and it’s less expensive than a surgical face-lift, which can run $10,000-$15,000 or more.”
For skin lifting, clinicians implant threads subcutaneously. When tugged in the opposite direction, the barbs anchor in adipose tissue, increasing tensile strength while suspended in the dermis and overlying tissue. This produces a fibrous adhesion capsule that helps to solidify anchorage of the suture long term. Fibrosis has been shown to increase local collagen production. PDO and PLLA are known collagen stimulants and are postulated to stimulate a long-term benefit in rejuvenation, Dr. Ortiz said, but overall evidence regarding their use in thread lifts is weak.
“Existing studies have a very short follow-up period and there is really no standardized protocol, so we don’t know really know a lot about them yet,” she said. Lana Tong, MD, and Evan A. Rieder, MD, of New York University recently published a systematic review of the literature on the topic (Dermatol Surg. 2019 45[7]:931-40).
PDO is biodegradable by hydrolysis over 4-8 months and is used as absorbable suture material for prolonged tension–bearing areas. “It causes neocollagenesis with a foreign-body reaction,” Dr. Ortiz said. Meanwhile, PLLA is a collagen stimulator used for prolonged volume restoration. “It’s used an aesthetic filler, but a known complication with PLLA injections is the formation of subcutaneous nodules and late onset granulomas,” she said.
Early in 2019, Korean researchers published results of a study that set out to evaluate the collagen-producing effects of powdered PDO injection, compared with PLLA injection, in a murine model (J Cosmet Dermatol. 2019 Feb 27. doi: 10.1111/jocd.12894). “It showed both PDO and PLLA induced granulomatous reactions and collagen formation, but this decreased at 12 weeks,” said Dr. Ortiz, who was not involved with the work. “PDO had slightly more collagen formation than PLLA.”
Indications for thread lifts, she continued, are for jawline lift, cheek enhancement, brow lift, wrinkle reduction, body contouring, acne scarring, and texturing. “Choose patients with good skin quality: not too thick/heavy, and not too thin. Patients with moderate skin sagging are going to better candidates than those with severe skin sagging.”
One type of absorbable suspension suture, the Silhouette InstaLift, is made of polyglycolide/
In terms of adverse events following thread lift procedures, patients usually feel tender for about a week or 2. “They can have some bruising, mostly from the anesthesia,” she said.
To prevent temporary dimpling, Dr. Ortiz undermines with an 18-gauge needle and inserts perpendicular to the skin surface. “Extrusions can still occur,” she said. To prevent this, she pulls on the end and makes sure it’s buried subcutaneously.
Dr. Ortiz reported having financial relationships with numerous pharmaceutical and device companies, though none related to the content of her presentation. She is also cochair of the Masters of Aesthetics symposium.
SAN DIEGO – The use of threads to improve skin laxity is making a comeback, thanks largely to advances in absorbable sutures.
“Thread lifts were popularized in the 1990s, but I think they were misrepresented as an alternative to a surgical face-lift, which remains the gold standard,” Arisa E. Ortiz, MD, said at the annual Masters of Aesthetics Symposium. “A thread lift is certainly not like a traditional face-lift; it’s much more subtle.”
In the 1990s, clinicians used nonabsorbable sutures for thread lifts, including polypropylene-barbed threads, which caused adverse events ranging from extrusion and migration to thread expulsion, dimpling, granuloma formation, and prolonged pain. As a result, the Food and Drug Administration withdrew its approval of contour thread aesthetic procedures in 2009. Since then, the development of absorbable threads made from polydioxanone (PDO) and poly-
“There are some nice benefits to thread lifts,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “You get immediate results, which is always nice for patients, but with tissue tightening using energy-based devices, results are unpredictable and it can take 6 months to see the results. With resorbable sutures, we’re seeing fewer complications, and the amount of lifting is more predictable because you’re physically lifting the tissue. In some cases, threads are able to lift tissue more than energy-based devices. There is minimal recovery, it requires local anesthesia, and it’s less expensive than a surgical face-lift, which can run $10,000-$15,000 or more.”
For skin lifting, clinicians implant threads subcutaneously. When tugged in the opposite direction, the barbs anchor in adipose tissue, increasing tensile strength while suspended in the dermis and overlying tissue. This produces a fibrous adhesion capsule that helps to solidify anchorage of the suture long term. Fibrosis has been shown to increase local collagen production. PDO and PLLA are known collagen stimulants and are postulated to stimulate a long-term benefit in rejuvenation, Dr. Ortiz said, but overall evidence regarding their use in thread lifts is weak.
“Existing studies have a very short follow-up period and there is really no standardized protocol, so we don’t know really know a lot about them yet,” she said. Lana Tong, MD, and Evan A. Rieder, MD, of New York University recently published a systematic review of the literature on the topic (Dermatol Surg. 2019 45[7]:931-40).
PDO is biodegradable by hydrolysis over 4-8 months and is used as absorbable suture material for prolonged tension–bearing areas. “It causes neocollagenesis with a foreign-body reaction,” Dr. Ortiz said. Meanwhile, PLLA is a collagen stimulator used for prolonged volume restoration. “It’s used an aesthetic filler, but a known complication with PLLA injections is the formation of subcutaneous nodules and late onset granulomas,” she said.
Early in 2019, Korean researchers published results of a study that set out to evaluate the collagen-producing effects of powdered PDO injection, compared with PLLA injection, in a murine model (J Cosmet Dermatol. 2019 Feb 27. doi: 10.1111/jocd.12894). “It showed both PDO and PLLA induced granulomatous reactions and collagen formation, but this decreased at 12 weeks,” said Dr. Ortiz, who was not involved with the work. “PDO had slightly more collagen formation than PLLA.”
Indications for thread lifts, she continued, are for jawline lift, cheek enhancement, brow lift, wrinkle reduction, body contouring, acne scarring, and texturing. “Choose patients with good skin quality: not too thick/heavy, and not too thin. Patients with moderate skin sagging are going to better candidates than those with severe skin sagging.”
One type of absorbable suspension suture, the Silhouette InstaLift, is made of polyglycolide/
In terms of adverse events following thread lift procedures, patients usually feel tender for about a week or 2. “They can have some bruising, mostly from the anesthesia,” she said.
To prevent temporary dimpling, Dr. Ortiz undermines with an 18-gauge needle and inserts perpendicular to the skin surface. “Extrusions can still occur,” she said. To prevent this, she pulls on the end and makes sure it’s buried subcutaneously.
Dr. Ortiz reported having financial relationships with numerous pharmaceutical and device companies, though none related to the content of her presentation. She is also cochair of the Masters of Aesthetics symposium.
SAN DIEGO – The use of threads to improve skin laxity is making a comeback, thanks largely to advances in absorbable sutures.
“Thread lifts were popularized in the 1990s, but I think they were misrepresented as an alternative to a surgical face-lift, which remains the gold standard,” Arisa E. Ortiz, MD, said at the annual Masters of Aesthetics Symposium. “A thread lift is certainly not like a traditional face-lift; it’s much more subtle.”
In the 1990s, clinicians used nonabsorbable sutures for thread lifts, including polypropylene-barbed threads, which caused adverse events ranging from extrusion and migration to thread expulsion, dimpling, granuloma formation, and prolonged pain. As a result, the Food and Drug Administration withdrew its approval of contour thread aesthetic procedures in 2009. Since then, the development of absorbable threads made from polydioxanone (PDO) and poly-
“There are some nice benefits to thread lifts,” said Dr. Ortiz, who is director of laser and cosmetic dermatology at the University of California, San Diego. “You get immediate results, which is always nice for patients, but with tissue tightening using energy-based devices, results are unpredictable and it can take 6 months to see the results. With resorbable sutures, we’re seeing fewer complications, and the amount of lifting is more predictable because you’re physically lifting the tissue. In some cases, threads are able to lift tissue more than energy-based devices. There is minimal recovery, it requires local anesthesia, and it’s less expensive than a surgical face-lift, which can run $10,000-$15,000 or more.”
For skin lifting, clinicians implant threads subcutaneously. When tugged in the opposite direction, the barbs anchor in adipose tissue, increasing tensile strength while suspended in the dermis and overlying tissue. This produces a fibrous adhesion capsule that helps to solidify anchorage of the suture long term. Fibrosis has been shown to increase local collagen production. PDO and PLLA are known collagen stimulants and are postulated to stimulate a long-term benefit in rejuvenation, Dr. Ortiz said, but overall evidence regarding their use in thread lifts is weak.
“Existing studies have a very short follow-up period and there is really no standardized protocol, so we don’t know really know a lot about them yet,” she said. Lana Tong, MD, and Evan A. Rieder, MD, of New York University recently published a systematic review of the literature on the topic (Dermatol Surg. 2019 45[7]:931-40).
PDO is biodegradable by hydrolysis over 4-8 months and is used as absorbable suture material for prolonged tension–bearing areas. “It causes neocollagenesis with a foreign-body reaction,” Dr. Ortiz said. Meanwhile, PLLA is a collagen stimulator used for prolonged volume restoration. “It’s used an aesthetic filler, but a known complication with PLLA injections is the formation of subcutaneous nodules and late onset granulomas,” she said.
Early in 2019, Korean researchers published results of a study that set out to evaluate the collagen-producing effects of powdered PDO injection, compared with PLLA injection, in a murine model (J Cosmet Dermatol. 2019 Feb 27. doi: 10.1111/jocd.12894). “It showed both PDO and PLLA induced granulomatous reactions and collagen formation, but this decreased at 12 weeks,” said Dr. Ortiz, who was not involved with the work. “PDO had slightly more collagen formation than PLLA.”
Indications for thread lifts, she continued, are for jawline lift, cheek enhancement, brow lift, wrinkle reduction, body contouring, acne scarring, and texturing. “Choose patients with good skin quality: not too thick/heavy, and not too thin. Patients with moderate skin sagging are going to better candidates than those with severe skin sagging.”
One type of absorbable suspension suture, the Silhouette InstaLift, is made of polyglycolide/
In terms of adverse events following thread lift procedures, patients usually feel tender for about a week or 2. “They can have some bruising, mostly from the anesthesia,” she said.
To prevent temporary dimpling, Dr. Ortiz undermines with an 18-gauge needle and inserts perpendicular to the skin surface. “Extrusions can still occur,” she said. To prevent this, she pulls on the end and makes sure it’s buried subcutaneously.
Dr. Ortiz reported having financial relationships with numerous pharmaceutical and device companies, though none related to the content of her presentation. She is also cochair of the Masters of Aesthetics symposium.
EXPERT ANALYSIS FROM MOA 2019
Another study supports safety of 2-cm margins for thick melanomas
based on data from a randomized, multicenter trial of 936 patients.
“Over time, and in light of the findings of several randomized studies, less extensive surgery for primary melanoma with tumor thickness greater than 2 mm has become more established,” and most recent guidelines recommend a 2-cm margin for these tumors, wrote Deborah Utjés, MD, of the Karolinska Institute in Stockholm and colleagues.
To reinforce the safety and effectiveness of the 2-cm margin, the researchers conducted an open-label, randomized trial of clinically staged melanoma patients aged 75 years and younger with localized cutaneous melanomas thicker than 2 mm, from January 1992 to May 2004. Patients were treated in Denmark, Estonia, Norway, and Sweden. The findings were published in the Lancet.
Patients were randomized to treatment with a 2-cm (471) or 4-cm excision margin (465). The melanomas were located on the trunk, upper extremities, or lower extremities.
The primary outcome of overall survival was similar between the groups. Over a median 20-year follow-up period, the death rate was approximately 50% in each group (49% in the 2-cm group and 51% in the 4-cm group). Disease-specific survival rates were similar as well. Of the 621 reported deaths, 397 were attributed to melanoma: 192 (48%) in the 2-cm group and 205 (52%) in the 4-cm group.
The study findings were limited by several factors, including a lower-than-expected number of patients, lack of nodal staging during the study period, and a focus only on the surgical margin without recording data on pathological excision margins.
However, the extended follow-up supports the safe use of the 2-cm margin for the treatment of melanomas thicker than 2 mm, the investigators wrote. In addition, results from an ongoing trial comparing 1-cm and 2-cm margins for melanomas at least 1 mm thick may yield more evidence to support still narrower surgical margins for some cutaneous melanomas.
The study notes that guidelines from organizations that include the American National Comprehensive Cancer Network and the American Academy of Dermatology recommend the 2-cm margin for tumors that are thicker than 2 mm.
The study was supported by the Swedish Cancer Society, Stockholm Cancer Society, Swedish Society for Medical Research, and the Stockholm County Council, and by funds from Radiumhemmet Research and Wallström. The authors reported no disclosures.
SOURCE: Utjés D et al. Lancet. 2019 Jul 4. doi: 10.1016/S0140-6736(19)31132-8.
based on data from a randomized, multicenter trial of 936 patients.
“Over time, and in light of the findings of several randomized studies, less extensive surgery for primary melanoma with tumor thickness greater than 2 mm has become more established,” and most recent guidelines recommend a 2-cm margin for these tumors, wrote Deborah Utjés, MD, of the Karolinska Institute in Stockholm and colleagues.
To reinforce the safety and effectiveness of the 2-cm margin, the researchers conducted an open-label, randomized trial of clinically staged melanoma patients aged 75 years and younger with localized cutaneous melanomas thicker than 2 mm, from January 1992 to May 2004. Patients were treated in Denmark, Estonia, Norway, and Sweden. The findings were published in the Lancet.
Patients were randomized to treatment with a 2-cm (471) or 4-cm excision margin (465). The melanomas were located on the trunk, upper extremities, or lower extremities.
The primary outcome of overall survival was similar between the groups. Over a median 20-year follow-up period, the death rate was approximately 50% in each group (49% in the 2-cm group and 51% in the 4-cm group). Disease-specific survival rates were similar as well. Of the 621 reported deaths, 397 were attributed to melanoma: 192 (48%) in the 2-cm group and 205 (52%) in the 4-cm group.
The study findings were limited by several factors, including a lower-than-expected number of patients, lack of nodal staging during the study period, and a focus only on the surgical margin without recording data on pathological excision margins.
However, the extended follow-up supports the safe use of the 2-cm margin for the treatment of melanomas thicker than 2 mm, the investigators wrote. In addition, results from an ongoing trial comparing 1-cm and 2-cm margins for melanomas at least 1 mm thick may yield more evidence to support still narrower surgical margins for some cutaneous melanomas.
The study notes that guidelines from organizations that include the American National Comprehensive Cancer Network and the American Academy of Dermatology recommend the 2-cm margin for tumors that are thicker than 2 mm.
The study was supported by the Swedish Cancer Society, Stockholm Cancer Society, Swedish Society for Medical Research, and the Stockholm County Council, and by funds from Radiumhemmet Research and Wallström. The authors reported no disclosures.
SOURCE: Utjés D et al. Lancet. 2019 Jul 4. doi: 10.1016/S0140-6736(19)31132-8.
based on data from a randomized, multicenter trial of 936 patients.
“Over time, and in light of the findings of several randomized studies, less extensive surgery for primary melanoma with tumor thickness greater than 2 mm has become more established,” and most recent guidelines recommend a 2-cm margin for these tumors, wrote Deborah Utjés, MD, of the Karolinska Institute in Stockholm and colleagues.
To reinforce the safety and effectiveness of the 2-cm margin, the researchers conducted an open-label, randomized trial of clinically staged melanoma patients aged 75 years and younger with localized cutaneous melanomas thicker than 2 mm, from January 1992 to May 2004. Patients were treated in Denmark, Estonia, Norway, and Sweden. The findings were published in the Lancet.
Patients were randomized to treatment with a 2-cm (471) or 4-cm excision margin (465). The melanomas were located on the trunk, upper extremities, or lower extremities.
The primary outcome of overall survival was similar between the groups. Over a median 20-year follow-up period, the death rate was approximately 50% in each group (49% in the 2-cm group and 51% in the 4-cm group). Disease-specific survival rates were similar as well. Of the 621 reported deaths, 397 were attributed to melanoma: 192 (48%) in the 2-cm group and 205 (52%) in the 4-cm group.
The study findings were limited by several factors, including a lower-than-expected number of patients, lack of nodal staging during the study period, and a focus only on the surgical margin without recording data on pathological excision margins.
However, the extended follow-up supports the safe use of the 2-cm margin for the treatment of melanomas thicker than 2 mm, the investigators wrote. In addition, results from an ongoing trial comparing 1-cm and 2-cm margins for melanomas at least 1 mm thick may yield more evidence to support still narrower surgical margins for some cutaneous melanomas.
The study notes that guidelines from organizations that include the American National Comprehensive Cancer Network and the American Academy of Dermatology recommend the 2-cm margin for tumors that are thicker than 2 mm.
The study was supported by the Swedish Cancer Society, Stockholm Cancer Society, Swedish Society for Medical Research, and the Stockholm County Council, and by funds from Radiumhemmet Research and Wallström. The authors reported no disclosures.
SOURCE: Utjés D et al. Lancet. 2019 Jul 4. doi: 10.1016/S0140-6736(19)31132-8.
FROM THE LANCET
Smoking linked to increased complication risk after Mohs surgery
, based on data from a retrospective case-control study of 1,008 adult patients.
The increased risk of complications for smokers following many types of surgery is well documented; however, “the effect of smoking in the specific setting of cutaneous tissue transfer is not well characterized in the literature describing outcomes after Mohs reconstruction,” wrote Chang Ye Wang, MD, of St. Louis University, Missouri, and colleagues.
To determine the impact of smoking on acute and long-term complications, the researchers reviewed data from 1,008 adults (396 women and 612 men) who underwent Mohs surgery between July 1, 2012, and June 30, 2016, at a single center. The study population included 128 current smokers, 385 former smokers, and 495 never smokers. The age of the patients ranged from 21 years to 90 years, with a median of 70 years. The results were published in JAMA Facial Plastic Surgery.
The overall rate of acute complications was 4.1%, and the most common complication was infection, in 19 cases; others were 10 cases of flap or graft necrosis, 10 cases of wound dehiscence, and 6 of cases of hematoma or uncontrolled bleeding; some patients experienced more than one of these complications. The risk of acute complications increased for current smokers (odds ratio 9.58) and former smokers (OR, 3.64) in a multivariate analysis. Increased risk of acute complications also was associated with a larger defect (OR, 2.25) and use of free cartilage graft (OR, 8.19).
The researchers defined acute complications as “any postsurgical infection, dehiscence, hematoma, uncontrolled bleeding, and tissue necrosis that required medical counseling or intervention,” and long-term complications as “any postsurgical functional defect or unsatisfactory cosmesis that prompted the patient to request an additional procedural intervention or the surgeon to offer it.”
The overall rate of long-term complications was 7.4%. A procedure in the center of the face was associated with a 25% increased risk of long-term complications (OR, 25.4). Other factors associated with an increased risk of long-term complications were the use of interpolation flap or flap-graft combination (OR, 3.49), larger flaps (OR, 1.42), and presence of basal cell carcinomas or other basaloid tumors (OR, 3.43). Smoking was not associated with an increased risk of long-term complications, and an older age was associated with a decreased risk of long-term complications (OR, 0.66).
The findings were limited by the retrospective study design and unblinded data collection, as well as a lack of photographs of all patients at matching time points, the researchers said. However, the results are consistent with previous studies and “may allow the surgeon to better quantify the magnitude of risk and provide helpful information for patient counseling,” they added.
The researchers had no financial conflicts to disclose.
SOURCE: Wang CY et al. JAMA Facial Plast. Surg. 2019 June 13. doi: 10.1001/jamafacial.2019.0243.
, based on data from a retrospective case-control study of 1,008 adult patients.
The increased risk of complications for smokers following many types of surgery is well documented; however, “the effect of smoking in the specific setting of cutaneous tissue transfer is not well characterized in the literature describing outcomes after Mohs reconstruction,” wrote Chang Ye Wang, MD, of St. Louis University, Missouri, and colleagues.
To determine the impact of smoking on acute and long-term complications, the researchers reviewed data from 1,008 adults (396 women and 612 men) who underwent Mohs surgery between July 1, 2012, and June 30, 2016, at a single center. The study population included 128 current smokers, 385 former smokers, and 495 never smokers. The age of the patients ranged from 21 years to 90 years, with a median of 70 years. The results were published in JAMA Facial Plastic Surgery.
The overall rate of acute complications was 4.1%, and the most common complication was infection, in 19 cases; others were 10 cases of flap or graft necrosis, 10 cases of wound dehiscence, and 6 of cases of hematoma or uncontrolled bleeding; some patients experienced more than one of these complications. The risk of acute complications increased for current smokers (odds ratio 9.58) and former smokers (OR, 3.64) in a multivariate analysis. Increased risk of acute complications also was associated with a larger defect (OR, 2.25) and use of free cartilage graft (OR, 8.19).
The researchers defined acute complications as “any postsurgical infection, dehiscence, hematoma, uncontrolled bleeding, and tissue necrosis that required medical counseling or intervention,” and long-term complications as “any postsurgical functional defect or unsatisfactory cosmesis that prompted the patient to request an additional procedural intervention or the surgeon to offer it.”
The overall rate of long-term complications was 7.4%. A procedure in the center of the face was associated with a 25% increased risk of long-term complications (OR, 25.4). Other factors associated with an increased risk of long-term complications were the use of interpolation flap or flap-graft combination (OR, 3.49), larger flaps (OR, 1.42), and presence of basal cell carcinomas or other basaloid tumors (OR, 3.43). Smoking was not associated with an increased risk of long-term complications, and an older age was associated with a decreased risk of long-term complications (OR, 0.66).
The findings were limited by the retrospective study design and unblinded data collection, as well as a lack of photographs of all patients at matching time points, the researchers said. However, the results are consistent with previous studies and “may allow the surgeon to better quantify the magnitude of risk and provide helpful information for patient counseling,” they added.
The researchers had no financial conflicts to disclose.
SOURCE: Wang CY et al. JAMA Facial Plast. Surg. 2019 June 13. doi: 10.1001/jamafacial.2019.0243.
, based on data from a retrospective case-control study of 1,008 adult patients.
The increased risk of complications for smokers following many types of surgery is well documented; however, “the effect of smoking in the specific setting of cutaneous tissue transfer is not well characterized in the literature describing outcomes after Mohs reconstruction,” wrote Chang Ye Wang, MD, of St. Louis University, Missouri, and colleagues.
To determine the impact of smoking on acute and long-term complications, the researchers reviewed data from 1,008 adults (396 women and 612 men) who underwent Mohs surgery between July 1, 2012, and June 30, 2016, at a single center. The study population included 128 current smokers, 385 former smokers, and 495 never smokers. The age of the patients ranged from 21 years to 90 years, with a median of 70 years. The results were published in JAMA Facial Plastic Surgery.
The overall rate of acute complications was 4.1%, and the most common complication was infection, in 19 cases; others were 10 cases of flap or graft necrosis, 10 cases of wound dehiscence, and 6 of cases of hematoma or uncontrolled bleeding; some patients experienced more than one of these complications. The risk of acute complications increased for current smokers (odds ratio 9.58) and former smokers (OR, 3.64) in a multivariate analysis. Increased risk of acute complications also was associated with a larger defect (OR, 2.25) and use of free cartilage graft (OR, 8.19).
The researchers defined acute complications as “any postsurgical infection, dehiscence, hematoma, uncontrolled bleeding, and tissue necrosis that required medical counseling or intervention,” and long-term complications as “any postsurgical functional defect or unsatisfactory cosmesis that prompted the patient to request an additional procedural intervention or the surgeon to offer it.”
The overall rate of long-term complications was 7.4%. A procedure in the center of the face was associated with a 25% increased risk of long-term complications (OR, 25.4). Other factors associated with an increased risk of long-term complications were the use of interpolation flap or flap-graft combination (OR, 3.49), larger flaps (OR, 1.42), and presence of basal cell carcinomas or other basaloid tumors (OR, 3.43). Smoking was not associated with an increased risk of long-term complications, and an older age was associated with a decreased risk of long-term complications (OR, 0.66).
The findings were limited by the retrospective study design and unblinded data collection, as well as a lack of photographs of all patients at matching time points, the researchers said. However, the results are consistent with previous studies and “may allow the surgeon to better quantify the magnitude of risk and provide helpful information for patient counseling,” they added.
The researchers had no financial conflicts to disclose.
SOURCE: Wang CY et al. JAMA Facial Plast. Surg. 2019 June 13. doi: 10.1001/jamafacial.2019.0243.
FROM JAMA FACIAL PLASTIC SURGERY
Social media use linked to acceptance of cosmetic surgery
Use of social media platforms such as Tinder, Snapchat, and Instagram, particularly in conjunction with photo-editing applications, may increase an individual’s acceptance of cosmetic surgery, a new study suggests.
In JAMA Facial Plastic Surgery, researchers report the outcomes of a web-based survey study involving 252 participants, 73.0% of whom were female. The survey asked participants about their use of social media, photo-editing tools such as Photoshop, VSCO, and Snapchat filters, and answered questionnaires to assess their self-esteem, self-worth, and attitudes toward cosmetic surgery.
All participants used at least one social media platform, with a mean of seven, and used a mean of two photo-editing applications; the analysis found that those who used more social media platforms were more likely to consider cosmetic surgery.
People who used Tinder and Snapchat – with or without photo filters – showed greater acceptance of cosmetic surgery, while those who used the photography mobile app VSCO and Instagram photo filters showed greater consideration but not acceptance of cosmetic surgery, compared with nonusers.
Participants whose self-worth was more closely tied to their appearance showed greater acceptance of cosmetic surgery. When it came to self-esteem, participants who used YouTube, WhatsApp, VSCO, and Photoshop had lower self-esteem scores, compared with nonusers.
Overall, nearly two-thirds of survey participants said they used photo-editing applications to change the lighting of images, but only 5.16% said they used these applications to make changes to face or body shape. This distinction was also seen in their acceptance of cosmetic surgery scores: Those who said they made changes to face and body shape showed higher acceptance scores than nonusers, but this was not seen in those who only used it for lighting adjustments.
“The rising trend of pursuing cosmetic surgery based on social media inspiration highlights the need to better understand patients’ motivations to seek cosmetic surgery,” wrote Jonlin Chen, a medical student at Johns Hopkins University, Baltimore, and coauthors.
Commenting on the association between YouTube use, lower self-esteem, and higher acceptance of cosmetic surgery, the authors suggested that the platform may generate appearance comparisons between users by allowing them to access beauty-related videos and connect with other users interested in cosmetics.
Michael J. Reilly, MD, department of otolaryngology–head and neck surgery and Keon M. Parsa, MD, from the department of psychiatry at MedStar Georgetown University Hospital in Washington, commented in an accompanying editorial that the findings of this study illustrate an increased trend seen by facial plastic surgeons (JAMA Facial Plast Surg. 2019 June 27. doi: 10.1001/jamafacial.2019.0419). The study “shows the importance of understanding the underlying motives and characteristics of individuals seeking cosmetic surgery.” They noted that facial plastic surgeons can play a role in helping patients to improve their self-esteem, but it is also important to be aware of the clinical signs of depression, anxiety, and social isolation and refer for appropriate nonsurgical support when there are mental health concerns that go beyond the knife and needle.
The authors of the study did note that their choice of a web-based survey meant the demographic was likely to be skewed toward a younger, more social media–savvy demographic, and may not necessarily represent the broader population of individuals seeking cosmetic surgery.
No funding or conflicts of interest were declared.
SOURCE: Chen J et al. JAMA Facial Plast Surg. 2019 Jun 27. doi: 10.1001/jamafacial.2019.0328.
Use of social media platforms such as Tinder, Snapchat, and Instagram, particularly in conjunction with photo-editing applications, may increase an individual’s acceptance of cosmetic surgery, a new study suggests.
In JAMA Facial Plastic Surgery, researchers report the outcomes of a web-based survey study involving 252 participants, 73.0% of whom were female. The survey asked participants about their use of social media, photo-editing tools such as Photoshop, VSCO, and Snapchat filters, and answered questionnaires to assess their self-esteem, self-worth, and attitudes toward cosmetic surgery.
All participants used at least one social media platform, with a mean of seven, and used a mean of two photo-editing applications; the analysis found that those who used more social media platforms were more likely to consider cosmetic surgery.
People who used Tinder and Snapchat – with or without photo filters – showed greater acceptance of cosmetic surgery, while those who used the photography mobile app VSCO and Instagram photo filters showed greater consideration but not acceptance of cosmetic surgery, compared with nonusers.
Participants whose self-worth was more closely tied to their appearance showed greater acceptance of cosmetic surgery. When it came to self-esteem, participants who used YouTube, WhatsApp, VSCO, and Photoshop had lower self-esteem scores, compared with nonusers.
Overall, nearly two-thirds of survey participants said they used photo-editing applications to change the lighting of images, but only 5.16% said they used these applications to make changes to face or body shape. This distinction was also seen in their acceptance of cosmetic surgery scores: Those who said they made changes to face and body shape showed higher acceptance scores than nonusers, but this was not seen in those who only used it for lighting adjustments.
“The rising trend of pursuing cosmetic surgery based on social media inspiration highlights the need to better understand patients’ motivations to seek cosmetic surgery,” wrote Jonlin Chen, a medical student at Johns Hopkins University, Baltimore, and coauthors.
Commenting on the association between YouTube use, lower self-esteem, and higher acceptance of cosmetic surgery, the authors suggested that the platform may generate appearance comparisons between users by allowing them to access beauty-related videos and connect with other users interested in cosmetics.
Michael J. Reilly, MD, department of otolaryngology–head and neck surgery and Keon M. Parsa, MD, from the department of psychiatry at MedStar Georgetown University Hospital in Washington, commented in an accompanying editorial that the findings of this study illustrate an increased trend seen by facial plastic surgeons (JAMA Facial Plast Surg. 2019 June 27. doi: 10.1001/jamafacial.2019.0419). The study “shows the importance of understanding the underlying motives and characteristics of individuals seeking cosmetic surgery.” They noted that facial plastic surgeons can play a role in helping patients to improve their self-esteem, but it is also important to be aware of the clinical signs of depression, anxiety, and social isolation and refer for appropriate nonsurgical support when there are mental health concerns that go beyond the knife and needle.
The authors of the study did note that their choice of a web-based survey meant the demographic was likely to be skewed toward a younger, more social media–savvy demographic, and may not necessarily represent the broader population of individuals seeking cosmetic surgery.
No funding or conflicts of interest were declared.
SOURCE: Chen J et al. JAMA Facial Plast Surg. 2019 Jun 27. doi: 10.1001/jamafacial.2019.0328.
Use of social media platforms such as Tinder, Snapchat, and Instagram, particularly in conjunction with photo-editing applications, may increase an individual’s acceptance of cosmetic surgery, a new study suggests.
In JAMA Facial Plastic Surgery, researchers report the outcomes of a web-based survey study involving 252 participants, 73.0% of whom were female. The survey asked participants about their use of social media, photo-editing tools such as Photoshop, VSCO, and Snapchat filters, and answered questionnaires to assess their self-esteem, self-worth, and attitudes toward cosmetic surgery.
All participants used at least one social media platform, with a mean of seven, and used a mean of two photo-editing applications; the analysis found that those who used more social media platforms were more likely to consider cosmetic surgery.
People who used Tinder and Snapchat – with or without photo filters – showed greater acceptance of cosmetic surgery, while those who used the photography mobile app VSCO and Instagram photo filters showed greater consideration but not acceptance of cosmetic surgery, compared with nonusers.
Participants whose self-worth was more closely tied to their appearance showed greater acceptance of cosmetic surgery. When it came to self-esteem, participants who used YouTube, WhatsApp, VSCO, and Photoshop had lower self-esteem scores, compared with nonusers.
Overall, nearly two-thirds of survey participants said they used photo-editing applications to change the lighting of images, but only 5.16% said they used these applications to make changes to face or body shape. This distinction was also seen in their acceptance of cosmetic surgery scores: Those who said they made changes to face and body shape showed higher acceptance scores than nonusers, but this was not seen in those who only used it for lighting adjustments.
“The rising trend of pursuing cosmetic surgery based on social media inspiration highlights the need to better understand patients’ motivations to seek cosmetic surgery,” wrote Jonlin Chen, a medical student at Johns Hopkins University, Baltimore, and coauthors.
Commenting on the association between YouTube use, lower self-esteem, and higher acceptance of cosmetic surgery, the authors suggested that the platform may generate appearance comparisons between users by allowing them to access beauty-related videos and connect with other users interested in cosmetics.
Michael J. Reilly, MD, department of otolaryngology–head and neck surgery and Keon M. Parsa, MD, from the department of psychiatry at MedStar Georgetown University Hospital in Washington, commented in an accompanying editorial that the findings of this study illustrate an increased trend seen by facial plastic surgeons (JAMA Facial Plast Surg. 2019 June 27. doi: 10.1001/jamafacial.2019.0419). The study “shows the importance of understanding the underlying motives and characteristics of individuals seeking cosmetic surgery.” They noted that facial plastic surgeons can play a role in helping patients to improve their self-esteem, but it is also important to be aware of the clinical signs of depression, anxiety, and social isolation and refer for appropriate nonsurgical support when there are mental health concerns that go beyond the knife and needle.
The authors of the study did note that their choice of a web-based survey meant the demographic was likely to be skewed toward a younger, more social media–savvy demographic, and may not necessarily represent the broader population of individuals seeking cosmetic surgery.
No funding or conflicts of interest were declared.
SOURCE: Chen J et al. JAMA Facial Plast Surg. 2019 Jun 27. doi: 10.1001/jamafacial.2019.0328.
FROM JAMA FACIAL PLASTIC SURGERY
Systematic review indicates cutaneous laser therapy may be safe during pregnancy
according to the results of a systematic review of 22 studies.
Among 380 women in all trimesters of pregnancy who were treated with various laser wavelengths, the only clinically significant event was a case of premature rupture of membranes (PROM) “without further morbidity,” wrote Eric C. Wilkerson, MD, of Skin Laser & Surgery Specialists of NY and NJ in New York, and associates. In that case, the cause was not clear, there was no further morbidity, “and it was uncertain whether this was related to the laser procedure.”
However, only 22 studies were identified between 1960 and 2017, all of which were case reports or series, published from 1994 to 2015. “[Thus far,] the best evidence exists for the safety of the carbon dioxide laser, particularly in the treatment of condyloma,” they wrote in Dermatologic Surgery.
Elective laser treatments are usually not recommended during pregnancy, but no evidence supports this, Dr. Wilkerson and coauthors wrote. Therefore, they searched for studies indexed in PubMed, Google Scholar, the Cochrane Library, or the EBSCO CINAHL Plus Database from 1960 to 2017. They also searched LexisNexis for relevant legal cases, but found none.
The women in the 22 case reports and series were aged 14-41 years and received laser therapy for cervical adenocarcinoma, urolithiasis, condyloma acuminata, cervical carcinoma in situ, cutaneous scarring, Buschke-Löwenstein tumor, verrucous carcinoma, and acne vulgaris. Modalities included 504-nm pulsed-dye laser, 532-nm potassium titanyl phosphate, 1,064-nm neodymium:YAG, 2,100-nm holmium:YAG, and 10,600-nm CO2.
Apart from the case of PROM, there were no instances of fetal morbidity or mortality, premature labor or preterm birth, or detectable fetal stress, the authors wrote. The case of PROM occurred at 35 weeks, 4 days after the mother had received CO2 laser therapy for condyloma acuminata. She delivered normally approximately 1 week later. There also were several cases of premature contractions without true labor, all of which responded to tocolytic therapy. (In the same study, there also were two cases of PROM in women 7 and 10 weeks after the same procedure, but were thought to be unrelated.)
The thickness of the pregnant abdomen, uterus, and amniotic fluid makes it “very unlikely” that clinically significant amounts of laser energy would reach the fetus during cutaneous laser therapy, the authors noted. Certain topical anesthetics, such as lidocaine and prilocaine, also appear safe during pregnancy “and may potentially decrease concern for fetal stress secondary to maternal stress or pain during the procedure,” they added. “Appropriate safety measures including eye protection and laser plume management should continue to be used during laser treatment.”
The authors reported no funding sources or conflicts of interest.
SOURCE: Wilkerson EJ et al. Dermatol Surg. 2019 Jun;45(6):818-28.
according to the results of a systematic review of 22 studies.
Among 380 women in all trimesters of pregnancy who were treated with various laser wavelengths, the only clinically significant event was a case of premature rupture of membranes (PROM) “without further morbidity,” wrote Eric C. Wilkerson, MD, of Skin Laser & Surgery Specialists of NY and NJ in New York, and associates. In that case, the cause was not clear, there was no further morbidity, “and it was uncertain whether this was related to the laser procedure.”
However, only 22 studies were identified between 1960 and 2017, all of which were case reports or series, published from 1994 to 2015. “[Thus far,] the best evidence exists for the safety of the carbon dioxide laser, particularly in the treatment of condyloma,” they wrote in Dermatologic Surgery.
Elective laser treatments are usually not recommended during pregnancy, but no evidence supports this, Dr. Wilkerson and coauthors wrote. Therefore, they searched for studies indexed in PubMed, Google Scholar, the Cochrane Library, or the EBSCO CINAHL Plus Database from 1960 to 2017. They also searched LexisNexis for relevant legal cases, but found none.
The women in the 22 case reports and series were aged 14-41 years and received laser therapy for cervical adenocarcinoma, urolithiasis, condyloma acuminata, cervical carcinoma in situ, cutaneous scarring, Buschke-Löwenstein tumor, verrucous carcinoma, and acne vulgaris. Modalities included 504-nm pulsed-dye laser, 532-nm potassium titanyl phosphate, 1,064-nm neodymium:YAG, 2,100-nm holmium:YAG, and 10,600-nm CO2.
Apart from the case of PROM, there were no instances of fetal morbidity or mortality, premature labor or preterm birth, or detectable fetal stress, the authors wrote. The case of PROM occurred at 35 weeks, 4 days after the mother had received CO2 laser therapy for condyloma acuminata. She delivered normally approximately 1 week later. There also were several cases of premature contractions without true labor, all of which responded to tocolytic therapy. (In the same study, there also were two cases of PROM in women 7 and 10 weeks after the same procedure, but were thought to be unrelated.)
The thickness of the pregnant abdomen, uterus, and amniotic fluid makes it “very unlikely” that clinically significant amounts of laser energy would reach the fetus during cutaneous laser therapy, the authors noted. Certain topical anesthetics, such as lidocaine and prilocaine, also appear safe during pregnancy “and may potentially decrease concern for fetal stress secondary to maternal stress or pain during the procedure,” they added. “Appropriate safety measures including eye protection and laser plume management should continue to be used during laser treatment.”
The authors reported no funding sources or conflicts of interest.
SOURCE: Wilkerson EJ et al. Dermatol Surg. 2019 Jun;45(6):818-28.
according to the results of a systematic review of 22 studies.
Among 380 women in all trimesters of pregnancy who were treated with various laser wavelengths, the only clinically significant event was a case of premature rupture of membranes (PROM) “without further morbidity,” wrote Eric C. Wilkerson, MD, of Skin Laser & Surgery Specialists of NY and NJ in New York, and associates. In that case, the cause was not clear, there was no further morbidity, “and it was uncertain whether this was related to the laser procedure.”
However, only 22 studies were identified between 1960 and 2017, all of which were case reports or series, published from 1994 to 2015. “[Thus far,] the best evidence exists for the safety of the carbon dioxide laser, particularly in the treatment of condyloma,” they wrote in Dermatologic Surgery.
Elective laser treatments are usually not recommended during pregnancy, but no evidence supports this, Dr. Wilkerson and coauthors wrote. Therefore, they searched for studies indexed in PubMed, Google Scholar, the Cochrane Library, or the EBSCO CINAHL Plus Database from 1960 to 2017. They also searched LexisNexis for relevant legal cases, but found none.
The women in the 22 case reports and series were aged 14-41 years and received laser therapy for cervical adenocarcinoma, urolithiasis, condyloma acuminata, cervical carcinoma in situ, cutaneous scarring, Buschke-Löwenstein tumor, verrucous carcinoma, and acne vulgaris. Modalities included 504-nm pulsed-dye laser, 532-nm potassium titanyl phosphate, 1,064-nm neodymium:YAG, 2,100-nm holmium:YAG, and 10,600-nm CO2.
Apart from the case of PROM, there were no instances of fetal morbidity or mortality, premature labor or preterm birth, or detectable fetal stress, the authors wrote. The case of PROM occurred at 35 weeks, 4 days after the mother had received CO2 laser therapy for condyloma acuminata. She delivered normally approximately 1 week later. There also were several cases of premature contractions without true labor, all of which responded to tocolytic therapy. (In the same study, there also were two cases of PROM in women 7 and 10 weeks after the same procedure, but were thought to be unrelated.)
The thickness of the pregnant abdomen, uterus, and amniotic fluid makes it “very unlikely” that clinically significant amounts of laser energy would reach the fetus during cutaneous laser therapy, the authors noted. Certain topical anesthetics, such as lidocaine and prilocaine, also appear safe during pregnancy “and may potentially decrease concern for fetal stress secondary to maternal stress or pain during the procedure,” they added. “Appropriate safety measures including eye protection and laser plume management should continue to be used during laser treatment.”
The authors reported no funding sources or conflicts of interest.
SOURCE: Wilkerson EJ et al. Dermatol Surg. 2019 Jun;45(6):818-28.
FROM DERMATOLOGIC SURGERY
Five rules for evaluating melanonychia
WAIKOLOA, HAWAII – Many dermatologists find melanonychia to be intimidating. The clinical features are ambiguous, and the prospect of doing a painful nail apparatus biopsy can be daunting for the inexperienced. As a result, the biopsy gets delayed and melanoma of the nail is often initially a missed diagnosis, not uncommonly for years, with devastating consequences.
Here are five at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Rule #1: Always look beyond the nail
When a light-skinned person presents with more than one nail with pigmentation, the likelihood that one of them is melanoma is much less than if there is only one nail with melanonychia, according to Dr. Jellinek, a dermatologist in private practice in East Greenwich, R.I.
Also, be sure to look at the skin and mucosa. Consider the medications the patients may be taking: For example, cyclophosphamide (Cytoxan) is notorious for causing nail changes as a side effect. A past medical history of lichen planus, carpal tunnel syndrome, Addison disease, or other conditions may explain the melanonychia.
Laugier-Hunziker syndrome is a condition worth getting to know. It’s an acquired disorder characterized longitudinal melanonychia and other pigmentary changes, which may include diffuse hyperpigmentation of the orolabial mucosa, ocular pigment, and/or pigmented palmoplantar lesions. It’s said to be rare, but Dr. Jellinek disagrees.
“Learn this one if you don’t know it. I see a case about every 2 weeks. It’s not heritable and not associated with any other medical condition,” he said.
Rule #2: Your dermatoscope is great for nails
What Dr. Jellinek considers to be among the all-time best papers on the value of dermoscopy for nail pigmentation was authored by French investigators. They analyzed 148 consecutive cases of longitudinal melanonychia and concluded that the dermoscopic combination of a brown background coupled with irregular longitudinal lines in terms of color, spacing, diameter, and/or lack of parallelism strongly suggests melanoma. A micro-Hutchinson’s sign, while a rare finding, occurred only in melanoma, where it represented periungual spread of a radial growth phase malignancy (Arch Dermatol. 2002 Oct;138[10]:1327-33).
“I think nail dermoscopy is most helpful for subungual hemorrhage. I average one referral per week for hemorrhage under the nail. On dermoscopy it’s as if someone took paint and threw it at the nail. Purple to brown blood spots, with no background color. This should be a doorway diagnosis of hemorrhage,” Dr. Jellinek said.
Rule #3: Know when you don’t know
“This is really the key for me,” the dermatologist commented. “There are automatic cases for biopsy, and more commonly routine cases for reassurance. But the gray zone, when you know you don’t know, is the key decision making moment.”
When something just doesn’t feel right, there’s absolutely nothing wrong with getting a second opinion, he stressed.
“It’s worthwhile getting to know people whose opinions you trust. There’s a saying I like to teach our fellows: ‘Never worry alone.’ So if you’re worried about someone, listen to that inner voice. There’s no shame in getting a second opinion. It’s great! Patients are never upset, either. They feel really well taken care of,” he said.
Rule #4: Don’t wimp out when a biopsy is warranted
Many dermatologists hem and haw about doing a biopsy for a concerning lesion on the nail, when they wouldn’t hesitate to biopsy a similarly suspicious lesion on the face.
But it’s essential to biopsy the right area, he added. For longitudinal melanonychia, that’s the matrix. The nail plate is the wrong place; a biopsy obtained there will result in an inappropriate benign diagnosis.
“The starter set is to do a punch biopsy. This is your gateway drug to the world of nail surgery. Lots of dermatologists are intimidated by nail surgery, but if you can do any minor surgery, you can do a punch of the matrix. All it takes is a little practice. And if all you can do is punch biopsies, you’re good for your career. If you can do that, you’re golden. There are people who’ve just done punch biopsies for their whole career and they don’t miss melanomas,” he said.
Step one is to undermine the proximal nail fold using a pediatric elevator, which costs only about $30. “If you’re going to do a lot of nail surgery, they’re really helpful,” he said.
There’s no need at all to evulse the nail. Just make oblique incisions in the proximal nail fold in order to reflect it and look at the matrix. A 3-mm punch is standard, directed right over the origin of the pigment. Resist the temptation to force or squeeze the specimen in order to extract it. Instead, use really fine-tipped scissors to nibble at the base of the specimen, then gently pull it out, making an effort to keep the nail plate attached to the digit and avoid getting it stuck up in the punch.
Rule #5: Have dermatopathologists extensively experienced with nail pathology on your Rolodex
The histopathologic findings present in early subungual melanoma in situ are often too subtle for general dermatopathologists to appreciate, in Dr. Jellinek’s experience. He cited other investigators’ study of 18 cases of subungual melanoma in situ, all marked by longitudinal melanonychia. Only half showed the classic giveaway on the original nail matrix biopsy, consisting of a significantly increased number of atypical melanocytes with marked nuclear atypia. Blatant pagetoid spread was infrequent. However, all 18 cases displayed a novel, more subtle, and previously undescribed finding: haphazard and uneven distribution of atypical solitary melanocytes with variably sized and shaped hyperchromatic nuclei (J Cutan Pathol. 2016 Jan;43[1]:41-52).
Dr. Jellinek reported having no financial conflicts regarding his presentation. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Many dermatologists find melanonychia to be intimidating. The clinical features are ambiguous, and the prospect of doing a painful nail apparatus biopsy can be daunting for the inexperienced. As a result, the biopsy gets delayed and melanoma of the nail is often initially a missed diagnosis, not uncommonly for years, with devastating consequences.
Here are five at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Rule #1: Always look beyond the nail
When a light-skinned person presents with more than one nail with pigmentation, the likelihood that one of them is melanoma is much less than if there is only one nail with melanonychia, according to Dr. Jellinek, a dermatologist in private practice in East Greenwich, R.I.
Also, be sure to look at the skin and mucosa. Consider the medications the patients may be taking: For example, cyclophosphamide (Cytoxan) is notorious for causing nail changes as a side effect. A past medical history of lichen planus, carpal tunnel syndrome, Addison disease, or other conditions may explain the melanonychia.
Laugier-Hunziker syndrome is a condition worth getting to know. It’s an acquired disorder characterized longitudinal melanonychia and other pigmentary changes, which may include diffuse hyperpigmentation of the orolabial mucosa, ocular pigment, and/or pigmented palmoplantar lesions. It’s said to be rare, but Dr. Jellinek disagrees.
“Learn this one if you don’t know it. I see a case about every 2 weeks. It’s not heritable and not associated with any other medical condition,” he said.
Rule #2: Your dermatoscope is great for nails
What Dr. Jellinek considers to be among the all-time best papers on the value of dermoscopy for nail pigmentation was authored by French investigators. They analyzed 148 consecutive cases of longitudinal melanonychia and concluded that the dermoscopic combination of a brown background coupled with irregular longitudinal lines in terms of color, spacing, diameter, and/or lack of parallelism strongly suggests melanoma. A micro-Hutchinson’s sign, while a rare finding, occurred only in melanoma, where it represented periungual spread of a radial growth phase malignancy (Arch Dermatol. 2002 Oct;138[10]:1327-33).
“I think nail dermoscopy is most helpful for subungual hemorrhage. I average one referral per week for hemorrhage under the nail. On dermoscopy it’s as if someone took paint and threw it at the nail. Purple to brown blood spots, with no background color. This should be a doorway diagnosis of hemorrhage,” Dr. Jellinek said.
Rule #3: Know when you don’t know
“This is really the key for me,” the dermatologist commented. “There are automatic cases for biopsy, and more commonly routine cases for reassurance. But the gray zone, when you know you don’t know, is the key decision making moment.”
When something just doesn’t feel right, there’s absolutely nothing wrong with getting a second opinion, he stressed.
“It’s worthwhile getting to know people whose opinions you trust. There’s a saying I like to teach our fellows: ‘Never worry alone.’ So if you’re worried about someone, listen to that inner voice. There’s no shame in getting a second opinion. It’s great! Patients are never upset, either. They feel really well taken care of,” he said.
Rule #4: Don’t wimp out when a biopsy is warranted
Many dermatologists hem and haw about doing a biopsy for a concerning lesion on the nail, when they wouldn’t hesitate to biopsy a similarly suspicious lesion on the face.
But it’s essential to biopsy the right area, he added. For longitudinal melanonychia, that’s the matrix. The nail plate is the wrong place; a biopsy obtained there will result in an inappropriate benign diagnosis.
“The starter set is to do a punch biopsy. This is your gateway drug to the world of nail surgery. Lots of dermatologists are intimidated by nail surgery, but if you can do any minor surgery, you can do a punch of the matrix. All it takes is a little practice. And if all you can do is punch biopsies, you’re good for your career. If you can do that, you’re golden. There are people who’ve just done punch biopsies for their whole career and they don’t miss melanomas,” he said.
Step one is to undermine the proximal nail fold using a pediatric elevator, which costs only about $30. “If you’re going to do a lot of nail surgery, they’re really helpful,” he said.
There’s no need at all to evulse the nail. Just make oblique incisions in the proximal nail fold in order to reflect it and look at the matrix. A 3-mm punch is standard, directed right over the origin of the pigment. Resist the temptation to force or squeeze the specimen in order to extract it. Instead, use really fine-tipped scissors to nibble at the base of the specimen, then gently pull it out, making an effort to keep the nail plate attached to the digit and avoid getting it stuck up in the punch.
Rule #5: Have dermatopathologists extensively experienced with nail pathology on your Rolodex
The histopathologic findings present in early subungual melanoma in situ are often too subtle for general dermatopathologists to appreciate, in Dr. Jellinek’s experience. He cited other investigators’ study of 18 cases of subungual melanoma in situ, all marked by longitudinal melanonychia. Only half showed the classic giveaway on the original nail matrix biopsy, consisting of a significantly increased number of atypical melanocytes with marked nuclear atypia. Blatant pagetoid spread was infrequent. However, all 18 cases displayed a novel, more subtle, and previously undescribed finding: haphazard and uneven distribution of atypical solitary melanocytes with variably sized and shaped hyperchromatic nuclei (J Cutan Pathol. 2016 Jan;43[1]:41-52).
Dr. Jellinek reported having no financial conflicts regarding his presentation. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Many dermatologists find melanonychia to be intimidating. The clinical features are ambiguous, and the prospect of doing a painful nail apparatus biopsy can be daunting for the inexperienced. As a result, the biopsy gets delayed and melanoma of the nail is often initially a missed diagnosis, not uncommonly for years, with devastating consequences.
Here are five at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Rule #1: Always look beyond the nail
When a light-skinned person presents with more than one nail with pigmentation, the likelihood that one of them is melanoma is much less than if there is only one nail with melanonychia, according to Dr. Jellinek, a dermatologist in private practice in East Greenwich, R.I.
Also, be sure to look at the skin and mucosa. Consider the medications the patients may be taking: For example, cyclophosphamide (Cytoxan) is notorious for causing nail changes as a side effect. A past medical history of lichen planus, carpal tunnel syndrome, Addison disease, or other conditions may explain the melanonychia.
Laugier-Hunziker syndrome is a condition worth getting to know. It’s an acquired disorder characterized longitudinal melanonychia and other pigmentary changes, which may include diffuse hyperpigmentation of the orolabial mucosa, ocular pigment, and/or pigmented palmoplantar lesions. It’s said to be rare, but Dr. Jellinek disagrees.
“Learn this one if you don’t know it. I see a case about every 2 weeks. It’s not heritable and not associated with any other medical condition,” he said.
Rule #2: Your dermatoscope is great for nails
What Dr. Jellinek considers to be among the all-time best papers on the value of dermoscopy for nail pigmentation was authored by French investigators. They analyzed 148 consecutive cases of longitudinal melanonychia and concluded that the dermoscopic combination of a brown background coupled with irregular longitudinal lines in terms of color, spacing, diameter, and/or lack of parallelism strongly suggests melanoma. A micro-Hutchinson’s sign, while a rare finding, occurred only in melanoma, where it represented periungual spread of a radial growth phase malignancy (Arch Dermatol. 2002 Oct;138[10]:1327-33).
“I think nail dermoscopy is most helpful for subungual hemorrhage. I average one referral per week for hemorrhage under the nail. On dermoscopy it’s as if someone took paint and threw it at the nail. Purple to brown blood spots, with no background color. This should be a doorway diagnosis of hemorrhage,” Dr. Jellinek said.
Rule #3: Know when you don’t know
“This is really the key for me,” the dermatologist commented. “There are automatic cases for biopsy, and more commonly routine cases for reassurance. But the gray zone, when you know you don’t know, is the key decision making moment.”
When something just doesn’t feel right, there’s absolutely nothing wrong with getting a second opinion, he stressed.
“It’s worthwhile getting to know people whose opinions you trust. There’s a saying I like to teach our fellows: ‘Never worry alone.’ So if you’re worried about someone, listen to that inner voice. There’s no shame in getting a second opinion. It’s great! Patients are never upset, either. They feel really well taken care of,” he said.
Rule #4: Don’t wimp out when a biopsy is warranted
Many dermatologists hem and haw about doing a biopsy for a concerning lesion on the nail, when they wouldn’t hesitate to biopsy a similarly suspicious lesion on the face.
But it’s essential to biopsy the right area, he added. For longitudinal melanonychia, that’s the matrix. The nail plate is the wrong place; a biopsy obtained there will result in an inappropriate benign diagnosis.
“The starter set is to do a punch biopsy. This is your gateway drug to the world of nail surgery. Lots of dermatologists are intimidated by nail surgery, but if you can do any minor surgery, you can do a punch of the matrix. All it takes is a little practice. And if all you can do is punch biopsies, you’re good for your career. If you can do that, you’re golden. There are people who’ve just done punch biopsies for their whole career and they don’t miss melanomas,” he said.
Step one is to undermine the proximal nail fold using a pediatric elevator, which costs only about $30. “If you’re going to do a lot of nail surgery, they’re really helpful,” he said.
There’s no need at all to evulse the nail. Just make oblique incisions in the proximal nail fold in order to reflect it and look at the matrix. A 3-mm punch is standard, directed right over the origin of the pigment. Resist the temptation to force or squeeze the specimen in order to extract it. Instead, use really fine-tipped scissors to nibble at the base of the specimen, then gently pull it out, making an effort to keep the nail plate attached to the digit and avoid getting it stuck up in the punch.
Rule #5: Have dermatopathologists extensively experienced with nail pathology on your Rolodex
The histopathologic findings present in early subungual melanoma in situ are often too subtle for general dermatopathologists to appreciate, in Dr. Jellinek’s experience. He cited other investigators’ study of 18 cases of subungual melanoma in situ, all marked by longitudinal melanonychia. Only half showed the classic giveaway on the original nail matrix biopsy, consisting of a significantly increased number of atypical melanocytes with marked nuclear atypia. Blatant pagetoid spread was infrequent. However, all 18 cases displayed a novel, more subtle, and previously undescribed finding: haphazard and uneven distribution of atypical solitary melanocytes with variably sized and shaped hyperchromatic nuclei (J Cutan Pathol. 2016 Jan;43[1]:41-52).
Dr. Jellinek reported having no financial conflicts regarding his presentation. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Ultrasound offers advantages for long-term lymph node surveillance in high-grade SCC patients
BALTIMORE – Ultrasound can be a very effective way to track early nodal metastasis in patients with high-stage cutaneous squamous cell carcinomas, and at a fraction of the cost of other imaging modalities.
The technique shows not only abnormal variations in the shape of nodes, but changes in the core and outer density, and vascular patterns, Emily Ruiz, MD, said at the annual meeting of the American College of Mohs Surgery. And over a 2-year surveillance period, this costs thousands less than radiation-based imaging.
Dr. Ruiz, director of the High-Risk Skin Cancer Clinic at Dana-Farber/Brigham and Women’s Cancer Center, Boston, said the standard imaging technique at that center used to be serial CT scans performed at diagnosis and every 6 months thereafter, for 2 years. But recently, the protocol changed: Ultrasound is now the preferred technique.
“The big problem with CT in this earlier disease, is that it can only identify the nodes that are enlarged, and doesn’t tell us anything about the etiology. Ultrasound, on the other hand, looks at a number of different features of the node.”
Tracking high-risk squamous cell carcinoma patients is a must, she said. “About 4% of people diagnosed with high-risk SCC will develop nodal metastases, and 1.5% of those will die from disease-specific death,” most often from locoregional disease. “So it’s critical to identify nodal diseases early as possible. Earlier identification leads to better outcomes.” Ultrasound simply provides more information about nodal metastasis, Dr. Ruiz added.
“The first thing we look at is the general architecture of the node. Resting and reactive nodes have a hypoechoic hilus and a hyperechoic cortex. As they become infiltrated with tumor, the hilus becomes more hyperechoic, and areas of metastasis stand out as much more hyperechoic than the surrounding node.”
Another tip-off is overall shape. If the ratio of the long axis to short axis diameter is less than 2, the lymph node is more likely to be malignant, she said.
“One more important factor that can’t be seen on CT is the node’s vascular pattern. Both resting and reactive nodes tend to have a centralized vascular pattern in the hilus. With tumor infiltration you start to see an asymmetrical vascularization as the nodes are replaced by tumor. The perfusion becomes much more peripheral.”
Cost is another consideration, Dr. Ruiz said. Five CT scans conducted over the recommended 2 years of follow-up will run about $5,000. Five scans with magnetic resonance imaging come in at about $6,500. PET CT is, of course, the most expensive, racking up a national average cost of $28,500 for five scans.
Ultrasound is amazingly inexpensive, Dr. Ruiz said. The national average cost of one scan is around $180, bringing the 2-year cost of five surveillance scans to $900.
Finally, clinicians and patients should consider the potential impact of repeated radiation exposure. “This can really add up over the follow-up period. Because there’s a 10-year latency period for these cancers, this might not be an issue for our older patients, but it really is something to consider in younger ones. “
However, she acknowledged that it’s not a completely rosy picture.
“Ultrasound is very user dependent, but we do think that by putting this in the hands of dermatologists with special training, we can solve this issue. In Europe, ultrasound’s very high sensitivity and specificity, combined with clinical exams, really improves disease detection.”
Unfortunately, at this point, anyone who wants to learn the technique has to go to Europe. “I trained in Germany, where I took a standard 3-day course, did 250 supervised scans, and completed an exam. I realize that’s unrealistic for most people,” she said. But a training protocol is being developed at Brigham and Women’s, under the auspices of the institution’s imaging experts, who felt that 3 days and 250 supervised scans was excessive. The Brigham and Women’s program comprises 8 hours of didactic training and at least 30 supervised scans with at least three abnormalities correctly identified, and will be put into place soon, Dr. Ruiz said.
The biggest obstacle to large-scale adoption of this protocol is data – there are not a lot, at least now.
“We are working on that, too. In conjunction with the Skin Cancer Foundation, we’re launching a prospective study. We want to recruit 80 patients with T2B/T3 cutaneous SCCs. They get both and ultrasound and a CT scan at diagnosis and every 6 months for 2 years,” she said.
BALTIMORE – Ultrasound can be a very effective way to track early nodal metastasis in patients with high-stage cutaneous squamous cell carcinomas, and at a fraction of the cost of other imaging modalities.
The technique shows not only abnormal variations in the shape of nodes, but changes in the core and outer density, and vascular patterns, Emily Ruiz, MD, said at the annual meeting of the American College of Mohs Surgery. And over a 2-year surveillance period, this costs thousands less than radiation-based imaging.
Dr. Ruiz, director of the High-Risk Skin Cancer Clinic at Dana-Farber/Brigham and Women’s Cancer Center, Boston, said the standard imaging technique at that center used to be serial CT scans performed at diagnosis and every 6 months thereafter, for 2 years. But recently, the protocol changed: Ultrasound is now the preferred technique.
“The big problem with CT in this earlier disease, is that it can only identify the nodes that are enlarged, and doesn’t tell us anything about the etiology. Ultrasound, on the other hand, looks at a number of different features of the node.”
Tracking high-risk squamous cell carcinoma patients is a must, she said. “About 4% of people diagnosed with high-risk SCC will develop nodal metastases, and 1.5% of those will die from disease-specific death,” most often from locoregional disease. “So it’s critical to identify nodal diseases early as possible. Earlier identification leads to better outcomes.” Ultrasound simply provides more information about nodal metastasis, Dr. Ruiz added.
“The first thing we look at is the general architecture of the node. Resting and reactive nodes have a hypoechoic hilus and a hyperechoic cortex. As they become infiltrated with tumor, the hilus becomes more hyperechoic, and areas of metastasis stand out as much more hyperechoic than the surrounding node.”
Another tip-off is overall shape. If the ratio of the long axis to short axis diameter is less than 2, the lymph node is more likely to be malignant, she said.
“One more important factor that can’t be seen on CT is the node’s vascular pattern. Both resting and reactive nodes tend to have a centralized vascular pattern in the hilus. With tumor infiltration you start to see an asymmetrical vascularization as the nodes are replaced by tumor. The perfusion becomes much more peripheral.”
Cost is another consideration, Dr. Ruiz said. Five CT scans conducted over the recommended 2 years of follow-up will run about $5,000. Five scans with magnetic resonance imaging come in at about $6,500. PET CT is, of course, the most expensive, racking up a national average cost of $28,500 for five scans.
Ultrasound is amazingly inexpensive, Dr. Ruiz said. The national average cost of one scan is around $180, bringing the 2-year cost of five surveillance scans to $900.
Finally, clinicians and patients should consider the potential impact of repeated radiation exposure. “This can really add up over the follow-up period. Because there’s a 10-year latency period for these cancers, this might not be an issue for our older patients, but it really is something to consider in younger ones. “
However, she acknowledged that it’s not a completely rosy picture.
“Ultrasound is very user dependent, but we do think that by putting this in the hands of dermatologists with special training, we can solve this issue. In Europe, ultrasound’s very high sensitivity and specificity, combined with clinical exams, really improves disease detection.”
Unfortunately, at this point, anyone who wants to learn the technique has to go to Europe. “I trained in Germany, where I took a standard 3-day course, did 250 supervised scans, and completed an exam. I realize that’s unrealistic for most people,” she said. But a training protocol is being developed at Brigham and Women’s, under the auspices of the institution’s imaging experts, who felt that 3 days and 250 supervised scans was excessive. The Brigham and Women’s program comprises 8 hours of didactic training and at least 30 supervised scans with at least three abnormalities correctly identified, and will be put into place soon, Dr. Ruiz said.
The biggest obstacle to large-scale adoption of this protocol is data – there are not a lot, at least now.
“We are working on that, too. In conjunction with the Skin Cancer Foundation, we’re launching a prospective study. We want to recruit 80 patients with T2B/T3 cutaneous SCCs. They get both and ultrasound and a CT scan at diagnosis and every 6 months for 2 years,” she said.
BALTIMORE – Ultrasound can be a very effective way to track early nodal metastasis in patients with high-stage cutaneous squamous cell carcinomas, and at a fraction of the cost of other imaging modalities.
The technique shows not only abnormal variations in the shape of nodes, but changes in the core and outer density, and vascular patterns, Emily Ruiz, MD, said at the annual meeting of the American College of Mohs Surgery. And over a 2-year surveillance period, this costs thousands less than radiation-based imaging.
Dr. Ruiz, director of the High-Risk Skin Cancer Clinic at Dana-Farber/Brigham and Women’s Cancer Center, Boston, said the standard imaging technique at that center used to be serial CT scans performed at diagnosis and every 6 months thereafter, for 2 years. But recently, the protocol changed: Ultrasound is now the preferred technique.
“The big problem with CT in this earlier disease, is that it can only identify the nodes that are enlarged, and doesn’t tell us anything about the etiology. Ultrasound, on the other hand, looks at a number of different features of the node.”
Tracking high-risk squamous cell carcinoma patients is a must, she said. “About 4% of people diagnosed with high-risk SCC will develop nodal metastases, and 1.5% of those will die from disease-specific death,” most often from locoregional disease. “So it’s critical to identify nodal diseases early as possible. Earlier identification leads to better outcomes.” Ultrasound simply provides more information about nodal metastasis, Dr. Ruiz added.
“The first thing we look at is the general architecture of the node. Resting and reactive nodes have a hypoechoic hilus and a hyperechoic cortex. As they become infiltrated with tumor, the hilus becomes more hyperechoic, and areas of metastasis stand out as much more hyperechoic than the surrounding node.”
Another tip-off is overall shape. If the ratio of the long axis to short axis diameter is less than 2, the lymph node is more likely to be malignant, she said.
“One more important factor that can’t be seen on CT is the node’s vascular pattern. Both resting and reactive nodes tend to have a centralized vascular pattern in the hilus. With tumor infiltration you start to see an asymmetrical vascularization as the nodes are replaced by tumor. The perfusion becomes much more peripheral.”
Cost is another consideration, Dr. Ruiz said. Five CT scans conducted over the recommended 2 years of follow-up will run about $5,000. Five scans with magnetic resonance imaging come in at about $6,500. PET CT is, of course, the most expensive, racking up a national average cost of $28,500 for five scans.
Ultrasound is amazingly inexpensive, Dr. Ruiz said. The national average cost of one scan is around $180, bringing the 2-year cost of five surveillance scans to $900.
Finally, clinicians and patients should consider the potential impact of repeated radiation exposure. “This can really add up over the follow-up period. Because there’s a 10-year latency period for these cancers, this might not be an issue for our older patients, but it really is something to consider in younger ones. “
However, she acknowledged that it’s not a completely rosy picture.
“Ultrasound is very user dependent, but we do think that by putting this in the hands of dermatologists with special training, we can solve this issue. In Europe, ultrasound’s very high sensitivity and specificity, combined with clinical exams, really improves disease detection.”
Unfortunately, at this point, anyone who wants to learn the technique has to go to Europe. “I trained in Germany, where I took a standard 3-day course, did 250 supervised scans, and completed an exam. I realize that’s unrealistic for most people,” she said. But a training protocol is being developed at Brigham and Women’s, under the auspices of the institution’s imaging experts, who felt that 3 days and 250 supervised scans was excessive. The Brigham and Women’s program comprises 8 hours of didactic training and at least 30 supervised scans with at least three abnormalities correctly identified, and will be put into place soon, Dr. Ruiz said.
The biggest obstacle to large-scale adoption of this protocol is data – there are not a lot, at least now.
“We are working on that, too. In conjunction with the Skin Cancer Foundation, we’re launching a prospective study. We want to recruit 80 patients with T2B/T3 cutaneous SCCs. They get both and ultrasound and a CT scan at diagnosis and every 6 months for 2 years,” she said.
EXPERT ANALYSIS FROM the ACMS Annual Meeting
Study finds increase in dermatologic prescriptions for postsurgical antibiotics
WASHINGTON – , according to an analysis presented at the annual meeting of the American Academy of Dermatology.
John Barbieri, MD, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, who presented the results, and colleagues examined data about antibiotic use in dermatology between 2008 and 2016. Overall, antibiotic use decreased during this period, primarily for chronic conditions such as acne and rosacea. On the other hand, antibiotic use associated with surgical visits increased by approximately 70%.
Using data from 2008 to 2016 in the Optum Clinformatics DataMart deidentified commercial claims database, the researchers performed a repeated cross-sectional analysis of oral antibiotic prescriptions associated with encounters for surgical procedures performed by dermatologists. They found that oral antibiotic prescriptions increased from 2.9% to 4.4% of visits for benign excisions, from 4.2% to 6.3% of visits for malignant excisions, and from 9.9% to 13.8% of visits for Mohs procedures during this time period. Oral antibiotic prescribing was more common for procedures that entailed a flap or graft and among patients with diabetes, female patients, and younger patients.
The investigators observed greater than twofold variation in antibiotic-prescribing rates across geographic census divisions. “If higher-prescribing divisions were to develop antibiotic prescribing rates similar to [those of] lower-prescribing divisions, antibiotic use could be decreased by over 50%,” Dr. Barbieri said. Before prescribing antibiotic prophylaxis, dermatologists should consider which patients benefit most from it, he added.
The investigators also examined the duration of antibiotic courses. The median course duration of postoperative antibiotics was 7 days. Randomized, controlled trials that collectively included more than 600 patients have failed to demonstrate a benefit of long postoperative courses of antibiotics, compared with perioperative antibiotics alone, said Dr. Barbieri. “While it may be hard to have true perioperative antibiotics available in a dermatology surgical clinic, there likely are opportunities to reduce these postoperative courses to a day or 3 days from this mean of 7 days that we observed in the study.” Reducing these courses would decrease the risk of antibiotic-associated complications such as nausea, diarrhea, and skin rashes, he added.
SOURCE: AAD 2019, Abstract 11356.
WASHINGTON – , according to an analysis presented at the annual meeting of the American Academy of Dermatology.
John Barbieri, MD, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, who presented the results, and colleagues examined data about antibiotic use in dermatology between 2008 and 2016. Overall, antibiotic use decreased during this period, primarily for chronic conditions such as acne and rosacea. On the other hand, antibiotic use associated with surgical visits increased by approximately 70%.
Using data from 2008 to 2016 in the Optum Clinformatics DataMart deidentified commercial claims database, the researchers performed a repeated cross-sectional analysis of oral antibiotic prescriptions associated with encounters for surgical procedures performed by dermatologists. They found that oral antibiotic prescriptions increased from 2.9% to 4.4% of visits for benign excisions, from 4.2% to 6.3% of visits for malignant excisions, and from 9.9% to 13.8% of visits for Mohs procedures during this time period. Oral antibiotic prescribing was more common for procedures that entailed a flap or graft and among patients with diabetes, female patients, and younger patients.
The investigators observed greater than twofold variation in antibiotic-prescribing rates across geographic census divisions. “If higher-prescribing divisions were to develop antibiotic prescribing rates similar to [those of] lower-prescribing divisions, antibiotic use could be decreased by over 50%,” Dr. Barbieri said. Before prescribing antibiotic prophylaxis, dermatologists should consider which patients benefit most from it, he added.
The investigators also examined the duration of antibiotic courses. The median course duration of postoperative antibiotics was 7 days. Randomized, controlled trials that collectively included more than 600 patients have failed to demonstrate a benefit of long postoperative courses of antibiotics, compared with perioperative antibiotics alone, said Dr. Barbieri. “While it may be hard to have true perioperative antibiotics available in a dermatology surgical clinic, there likely are opportunities to reduce these postoperative courses to a day or 3 days from this mean of 7 days that we observed in the study.” Reducing these courses would decrease the risk of antibiotic-associated complications such as nausea, diarrhea, and skin rashes, he added.
SOURCE: AAD 2019, Abstract 11356.
WASHINGTON – , according to an analysis presented at the annual meeting of the American Academy of Dermatology.
John Barbieri, MD, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, who presented the results, and colleagues examined data about antibiotic use in dermatology between 2008 and 2016. Overall, antibiotic use decreased during this period, primarily for chronic conditions such as acne and rosacea. On the other hand, antibiotic use associated with surgical visits increased by approximately 70%.
Using data from 2008 to 2016 in the Optum Clinformatics DataMart deidentified commercial claims database, the researchers performed a repeated cross-sectional analysis of oral antibiotic prescriptions associated with encounters for surgical procedures performed by dermatologists. They found that oral antibiotic prescriptions increased from 2.9% to 4.4% of visits for benign excisions, from 4.2% to 6.3% of visits for malignant excisions, and from 9.9% to 13.8% of visits for Mohs procedures during this time period. Oral antibiotic prescribing was more common for procedures that entailed a flap or graft and among patients with diabetes, female patients, and younger patients.
The investigators observed greater than twofold variation in antibiotic-prescribing rates across geographic census divisions. “If higher-prescribing divisions were to develop antibiotic prescribing rates similar to [those of] lower-prescribing divisions, antibiotic use could be decreased by over 50%,” Dr. Barbieri said. Before prescribing antibiotic prophylaxis, dermatologists should consider which patients benefit most from it, he added.
The investigators also examined the duration of antibiotic courses. The median course duration of postoperative antibiotics was 7 days. Randomized, controlled trials that collectively included more than 600 patients have failed to demonstrate a benefit of long postoperative courses of antibiotics, compared with perioperative antibiotics alone, said Dr. Barbieri. “While it may be hard to have true perioperative antibiotics available in a dermatology surgical clinic, there likely are opportunities to reduce these postoperative courses to a day or 3 days from this mean of 7 days that we observed in the study.” Reducing these courses would decrease the risk of antibiotic-associated complications such as nausea, diarrhea, and skin rashes, he added.
SOURCE: AAD 2019, Abstract 11356.
REPORTING FROM AAD 2019
International registry of laser surgery outcomes in the works
DENVER – Researchers in the early stages of from existing studies in the medical literature. They’ve also observed insufficient reporting of outcome definitions and under-representation of life impact domains.
“Today, laser therapy is not only an important treatment modality for cosmetic indications, but also for medical skin disorders and diseases,” lead study author Frederike Fransen said at the annual conference of the American Society for Laser Medicine and Surgery. “These disorders include inflammatory lesions, vascular and pigmented lesions, tumors, and scars. Although there are a lot of options for laser therapy, the evidence for most of these skin conditions is quite low, consisting mostly of case reports and case series. However, if we want more evidence-based practice, we need more practice-based evidence.”
A new effort to gain insight into safety and effectiveness of laser treatments known as the international Laser Treatment Dermatology Registry (LEAD) is a platform to address this challenge. “We envision a registry that connects expertise and experience of a large international team of laser specialists, clinicians, and researchers,” said Ms. Fransen, a PhD candidate in the department of dermatology at Amsterdam University Medical Center. “Our goal is to gain insight into safety and effectiveness of laser treatments.” The collaboration includes researchers from the Netherlands, Denmark, France, Germany, Italy, and Switzerland, and the team will be complemented by experts from the United States, Asia, and North Africa.
For the first phase of the endeavor, Ms. Fransen and Albert Wolkerstorfer, MD, PhD, of the University of Amsterdam worked with colleagues from the Cochrane Skin-Core Outcome Set Initiative (CS-COUSIN) to develop a consensus of outcomes to be included in the registry. This involved a literature review of 350 articles to explore the outcomes used in laser research. From these, the researchers identified 100 articles for outcome mapping: 25 randomized, controlled trials, 44 trials that were not randomized or controlled, and 31 case reports. Their review yielded 98 outcomes and 53 outcome instruments.
Ultimately, outcomes were assigned to eight domains, Ms. Fransen said: appearance, long-term effects, physician-reported physical signs, patient-reported physical signs, satisfaction, health-related quality of life, psychological functioning, and adverse events. Of these domains, the most commonly used in existing medical literature were appearance such as clinical improvement and clearance (81%), followed by adverse effects such as erythema and scarring (55%), physician-reported signs such as morphology (30%), and long-term effects such as recurrence (27%). Ms. Fransen and Dr. Wolkerstorfer observed under-representation of patient-centered outcomes, including satisfaction of appearance or treatment (29%), patient-reported physical signs such as overall state and severity of disease (12%), health-related quality of life (4%), and psychological functioning such as anxiety and depression (1%).
The analysis also revealed that different outcomes measures were used in the various studies, and inconstant definitions within scaling systems. For example, for clearance of lesions/no clearance of lesions, some studies defined excellent clearance as 75% or greater, and others defined marked clearance as 70% or greater. In addition, some studies that used percentage quintile grading as an outcome defined grade 5 as a greater than 95% improvement, while others defined grade 5 as “clear,” or a greater than 90% improvement.
The next step in developing the LEAD registry involves performing an international e-Delphi survey, a method to obtain agreement on outcomes for the registry among health care professionals and patients with different opinions and backgrounds. “The process ends when sufficient agreement is obtained,” Ms. Fransen said. “Looking at future steps, the development of this collaborative initiative with a minimum set of outcomes is essential. When establishing this registry we can achieve sufficient sample size and confirmatory cases toward stronger evidence of laser treatments for orphan diseases.”
The project was supported by the European Academy of Dermatology and Venereology and by an educational grant from ASLMS.
[email protected]
DENVER – Researchers in the early stages of from existing studies in the medical literature. They’ve also observed insufficient reporting of outcome definitions and under-representation of life impact domains.
“Today, laser therapy is not only an important treatment modality for cosmetic indications, but also for medical skin disorders and diseases,” lead study author Frederike Fransen said at the annual conference of the American Society for Laser Medicine and Surgery. “These disorders include inflammatory lesions, vascular and pigmented lesions, tumors, and scars. Although there are a lot of options for laser therapy, the evidence for most of these skin conditions is quite low, consisting mostly of case reports and case series. However, if we want more evidence-based practice, we need more practice-based evidence.”
A new effort to gain insight into safety and effectiveness of laser treatments known as the international Laser Treatment Dermatology Registry (LEAD) is a platform to address this challenge. “We envision a registry that connects expertise and experience of a large international team of laser specialists, clinicians, and researchers,” said Ms. Fransen, a PhD candidate in the department of dermatology at Amsterdam University Medical Center. “Our goal is to gain insight into safety and effectiveness of laser treatments.” The collaboration includes researchers from the Netherlands, Denmark, France, Germany, Italy, and Switzerland, and the team will be complemented by experts from the United States, Asia, and North Africa.
For the first phase of the endeavor, Ms. Fransen and Albert Wolkerstorfer, MD, PhD, of the University of Amsterdam worked with colleagues from the Cochrane Skin-Core Outcome Set Initiative (CS-COUSIN) to develop a consensus of outcomes to be included in the registry. This involved a literature review of 350 articles to explore the outcomes used in laser research. From these, the researchers identified 100 articles for outcome mapping: 25 randomized, controlled trials, 44 trials that were not randomized or controlled, and 31 case reports. Their review yielded 98 outcomes and 53 outcome instruments.
Ultimately, outcomes were assigned to eight domains, Ms. Fransen said: appearance, long-term effects, physician-reported physical signs, patient-reported physical signs, satisfaction, health-related quality of life, psychological functioning, and adverse events. Of these domains, the most commonly used in existing medical literature were appearance such as clinical improvement and clearance (81%), followed by adverse effects such as erythema and scarring (55%), physician-reported signs such as morphology (30%), and long-term effects such as recurrence (27%). Ms. Fransen and Dr. Wolkerstorfer observed under-representation of patient-centered outcomes, including satisfaction of appearance or treatment (29%), patient-reported physical signs such as overall state and severity of disease (12%), health-related quality of life (4%), and psychological functioning such as anxiety and depression (1%).
The analysis also revealed that different outcomes measures were used in the various studies, and inconstant definitions within scaling systems. For example, for clearance of lesions/no clearance of lesions, some studies defined excellent clearance as 75% or greater, and others defined marked clearance as 70% or greater. In addition, some studies that used percentage quintile grading as an outcome defined grade 5 as a greater than 95% improvement, while others defined grade 5 as “clear,” or a greater than 90% improvement.
The next step in developing the LEAD registry involves performing an international e-Delphi survey, a method to obtain agreement on outcomes for the registry among health care professionals and patients with different opinions and backgrounds. “The process ends when sufficient agreement is obtained,” Ms. Fransen said. “Looking at future steps, the development of this collaborative initiative with a minimum set of outcomes is essential. When establishing this registry we can achieve sufficient sample size and confirmatory cases toward stronger evidence of laser treatments for orphan diseases.”
The project was supported by the European Academy of Dermatology and Venereology and by an educational grant from ASLMS.
[email protected]
DENVER – Researchers in the early stages of from existing studies in the medical literature. They’ve also observed insufficient reporting of outcome definitions and under-representation of life impact domains.
“Today, laser therapy is not only an important treatment modality for cosmetic indications, but also for medical skin disorders and diseases,” lead study author Frederike Fransen said at the annual conference of the American Society for Laser Medicine and Surgery. “These disorders include inflammatory lesions, vascular and pigmented lesions, tumors, and scars. Although there are a lot of options for laser therapy, the evidence for most of these skin conditions is quite low, consisting mostly of case reports and case series. However, if we want more evidence-based practice, we need more practice-based evidence.”
A new effort to gain insight into safety and effectiveness of laser treatments known as the international Laser Treatment Dermatology Registry (LEAD) is a platform to address this challenge. “We envision a registry that connects expertise and experience of a large international team of laser specialists, clinicians, and researchers,” said Ms. Fransen, a PhD candidate in the department of dermatology at Amsterdam University Medical Center. “Our goal is to gain insight into safety and effectiveness of laser treatments.” The collaboration includes researchers from the Netherlands, Denmark, France, Germany, Italy, and Switzerland, and the team will be complemented by experts from the United States, Asia, and North Africa.
For the first phase of the endeavor, Ms. Fransen and Albert Wolkerstorfer, MD, PhD, of the University of Amsterdam worked with colleagues from the Cochrane Skin-Core Outcome Set Initiative (CS-COUSIN) to develop a consensus of outcomes to be included in the registry. This involved a literature review of 350 articles to explore the outcomes used in laser research. From these, the researchers identified 100 articles for outcome mapping: 25 randomized, controlled trials, 44 trials that were not randomized or controlled, and 31 case reports. Their review yielded 98 outcomes and 53 outcome instruments.
Ultimately, outcomes were assigned to eight domains, Ms. Fransen said: appearance, long-term effects, physician-reported physical signs, patient-reported physical signs, satisfaction, health-related quality of life, psychological functioning, and adverse events. Of these domains, the most commonly used in existing medical literature were appearance such as clinical improvement and clearance (81%), followed by adverse effects such as erythema and scarring (55%), physician-reported signs such as morphology (30%), and long-term effects such as recurrence (27%). Ms. Fransen and Dr. Wolkerstorfer observed under-representation of patient-centered outcomes, including satisfaction of appearance or treatment (29%), patient-reported physical signs such as overall state and severity of disease (12%), health-related quality of life (4%), and psychological functioning such as anxiety and depression (1%).
The analysis also revealed that different outcomes measures were used in the various studies, and inconstant definitions within scaling systems. For example, for clearance of lesions/no clearance of lesions, some studies defined excellent clearance as 75% or greater, and others defined marked clearance as 70% or greater. In addition, some studies that used percentage quintile grading as an outcome defined grade 5 as a greater than 95% improvement, while others defined grade 5 as “clear,” or a greater than 90% improvement.
The next step in developing the LEAD registry involves performing an international e-Delphi survey, a method to obtain agreement on outcomes for the registry among health care professionals and patients with different opinions and backgrounds. “The process ends when sufficient agreement is obtained,” Ms. Fransen said. “Looking at future steps, the development of this collaborative initiative with a minimum set of outcomes is essential. When establishing this registry we can achieve sufficient sample size and confirmatory cases toward stronger evidence of laser treatments for orphan diseases.”
The project was supported by the European Academy of Dermatology and Venereology and by an educational grant from ASLMS.
[email protected]
REPORTING FROM ASLMS 2019