User login
Management, Evaluation of Chronic Itch in Older Adults
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
WASHINGTON — , Shawn G. Kwatra, MD, said at the ElderDerm conference on dermatology in older patients hosted by the GW School of Medicine & Health Sciences.
“We found a few years ago that eosinophils seem to differentiate this group, and now we’re finding that IgE and CBC [complete blood count] differential can help you get a little better sense of who has an immune-driven itch vs something more neuropathic,” said Dr. Kwatra, professor and chair of dermatology at the University of Maryland, Baltimore, who founded and directed the Johns Hopkins Itch Center before coming to the University of Maryland in 2023. Not all patients with immune-driven itch will have these biomarkers, “but it’s a helpful tool,” he said.
CPUO is the term that is increasingly being used, he said, to describe intense, chronic pruritus without primary skin lesions or rashes and without any known systemic cause. It becomes more common as people get older and is sometimes debilitating. The initial evaluation should be kept “simple and straightforward,” he advised, with heightened concern for underlying malignancy in those who present with an itch of less than 12 months’ duration.
Biologics, JAK Inhibitors: Case Reports, Ongoing Research
Research conducted by Dr. Kwatra and Jaya Manjunath, a fourth-year medical student at The George Washington University, Washington, documented higher levels of Th2-associated cytokines and inflammatory markers in patients with CPUO who had elevated IgE or eosinophil levels, or both than in patients with itch who had low IgE and eosinophil levels. The patients with higher levels also had a greater response to off-label treatment with immunomodulatory therapy.
“Multiple Th2-related inflammatory markers, like IL [interleukin]-5 and eotaxin-3, were reduced after dupilumab” in patients who responded to the therapy, said Ms. Manjunath, who co-presented the meeting session on chronic itch with Dr. Kwatra. Other changes in the plasma cytokine profile included a reduction in the serum level of thymus and activation-regulated chemokine, which is a biomarker for atopic dermatitis. The research is under review for publication.
Meanwhile, a phase 3 trial (LIBERTY-CPUO-CHIC) of dupilumab for CPUO is currently underway, Dr. Kwatra noted. Investigators are randomizing patients with severe pruritus (Worst Itch Numeric Rating Scale [WI-NRS] ≥ 7) to dupilumab or placebo for 12 or 24 weeks.
In one of several cases shared by Dr. Kwatra and Ms. Manjunath, a 71-year-old Black woman with a 6-month history of generalized itch (WI-NRS = 10) and a history of type 2 diabetes, hypertension, and chronic kidney disease was found to have elevated eosinophil levels and a negative malignancy workup. Previous therapies included antihistamines and topical steroids. She was started on a 600-mg loading dose of subcutaneous dupilumab followed by 300 mg every 14 days. At the 2-month follow-up, her WI-NRS score was 0.
Because “dupilumab is off label right now for this form of itch, oftentimes our first line is methotrexate,” Dr. Kwatra said. Patients “can have a good response with this therapeutic.”
He also described the case of a 72-year-old Black woman with total body itch for 2 years (WI-NRS = 10) and a history of seasonal allergies, thyroid disease, and hypertension. Previous therapies included prednisone, antihistamines, topical steroids, and gabapentin. The patient was found to have high IgE (447 kU/L) and eosinophil levels (4.9%), was started on methotrexate, and had an itch score of 0 at the 8-month follow-up.
JAK inhibitors may also have a role in the management of CPUO. A phase 2 nonrandomized controlled trial of abrocitinib for adults with prurigo nodularis (PN) or CPUO, recently published in JAMA Dermatology, showed itch scores decreased by 53.7% in the CPUO group (and 78.3% in the PN group) after 12 weeks of treatment with oral abrocitinib 200 mg daily. Patients had significant improvements in quality of life and no serious adverse events, said Dr. Kwatra, the lead author of the paper.
One of these patients was a 73-year-old White man who had experienced total body itch for 1.5 years (predominantly affecting his upper extremities; WI-NRS = 10) and a history of ascending aortic aneurysm, hypertension, and hyperlipidemia. Previous failed therapies included dupilumab (> 6 months), topical steroids, tacrolimus, and antihistamines. Labs showed elevated IgE (456 kU/L) and eosinophil levels (11.7%). After 12 weeks of treatment with abrocitinib, the WI-NRS decreased to 2.
PD-1 Inhibitors As a Trigger
Chronic pruritus caused by the anticancer PD-1 inhibitors is becoming more common as the utilization of these immune checkpoint inhibitors increases, Dr. Kwatra noted. “You don’t see much in the skin, but [these patients have] very high IgE and eosinophils,” he said. “We’ve been seeing more reports recently of utilizing agents that target type 2 inflammation off label for PD-1 inhibitor–related skin manifestations.”
One such patient with PD-1 inhibitor–induced pruritus was a 65-year-old White man with metastatic melanoma who reported a 6-month history of itching that began 3 weeks after the start of treatment with the PD-1 inhibitor pembrolizumab. His WI-NRS score was 10 despite treatment with topical steroids and antihistamines. He had a history of psoriasis. Labs showed elevated IgE (1350 kU/L) and eosinophil levels (4.5%). At a 4-month follow-up after treatment with off-label dupilumab (a 600-mg subcutaneous loading dose followed by 300 mg every 14 days), his WI-NRS score was 0.
In a paper recently published in JAAD International, Dr. Kwatra, Ms. Manjunath, and coinvestigators reported on a series of 15 patients who developed chronic pruritus following an immune stimulus exposure, including immunotherapy and vaccination (2024 Apr 7:16:97-102. doi: 10.1016/j.jdin.2024.03.022). Most immunotherapy-treated patients experienced pruritus during treatment or after 21-60 days of receiving treatment, and the patients with vaccine-stimulated pruritus (after Tdap and messenger RNA COVID-19 vaccination) developed pruritus within a week of vaccination.
In addition to the elevated levels of IgE and eosinophils, plasma cytokine analysis showed elevated levels of IL-5, thymic stromal lymphopoietin, and other Th2-related cytokines and inflammatory markers in patients with immune-stimulated pruritus compared with healthy controls, Ms. Manjunath said at the meeting.
When a Malignancy Workup Becomes Important
The initial part of any diagnostic workup for CPUO should include CBC with differential, liver function tests, renal function tests, and thyroid function testing, said Kwatra, referring to a diagnostic algorithm he developed, which was published as part of a CME review in the Journal of the American Academy of Dermatology in 2022.
Then, as indicated by risk factors in the history and physical, one could order other tests such as HIV serology, hepatitis B/C serologies, bullous pemphigoid testing, chest x-rays, evaluation for gammopathies, stool examination for ova and parasites, or heavy metal testing. “Do you do everything at once? We like to keep it straightforward,” Dr. Kwatra said. “Depending on the patient’s risk factors, you could order more or less.”
A malignancy workup should be strongly considered in patients whose itch duration is less than 12 months — and especially if the duration is less than 3 months — with an emphasis on cancers more frequently associated with itch: Hematologic and hepatobiliary cancers. This is “when concern should be heightened ... when there should be a lower threshold for workup,” he said.
The 12-month recommendation stems from a Danish cohort study published in 2014 that demonstrated a twofold increased incidence of cancer among patients with pruritus in the first 3 months after the diagnosis of pruritus. The 1-year absolute cancer risk was 1.63%.
Other risk factors for underlying malignancy or malignancy development in patients with CPUO include age older than 60 years, male sex, liver disease, and current or prior smoking, according to another study, noted Dr. Kwatra.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Pfizer, Regeneron, Sanofi, and other companies and an investigator for Galderma, Incyte, Pfizer, and Sanofi. Manjunath served as the codirector of the ElderDerm conference.
A version of this article first appeared on Medscape.com.
FROM ELDERDERM 2024
Study Links Melasma With Comorbidities, Races, Ethnicities
TOPLINE:
A study found significant associations between melasma and several comorbidities, including hypertension and hormonal contraception use, which were the most common.
METHODOLOGY:
- Melasma predominantly affects young women of color and often worsens in hyperestrogen states; understanding the association with comorbidities can improve surveillance and treatment strategies.
- Researchers evaluated 41,283 patients with melasma (mean age, 48.8 years; 93% women) from the TriNetX database and an equal number of matched control individuals.
- The main outcome was comorbidities including allergic rhinitis, atopic dermatitis, anticonvulsants, diabetes, hormonal contraceptives, hypothyroidism, hypertension, lupus, rosacea, skin cancer, and malignancy.
TAKEAWAY:
- Among those with melasma, 25% had hypertension and 24% used hormonal contraception, the two most commonly associated risk factors identified.
- Rosacea (odds ratio [OR], 5.1), atopic dermatitis (OR, 3.3), lupus (OR, 2.5), history of skin cancer (OR, 2.5), and history of internal malignancy (OR, 2.1) were associated with the highest risk of developing melasma (P < .01 for all).
- Asian (OR, 2.0; P < .01) and “other/unknown” races (OR, 1.7; P < .01) and Hispanic ethnicity (OR, 1.3; P < .01) were also significantly associated with melasma, while the odds were slightly lower among White, Black/African American, and “not Hispanic” groups (ORs, 0.8; P < .01 for all groups).
IN PRACTICE:
the authors wrote.
SOURCE:
The study, led by Ajay N. Sharma, MD, MBA, of the Department of Dermatology at the University of California, Irvine, was published online in Journal of Drugs in Dermatology.
LIMITATIONS:
The study limitations included the retrospective design, potential misclassification of diagnoses, and the inability to establish causality.
DISCLOSURES:
The study did not disclose any funding sources. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
A study found significant associations between melasma and several comorbidities, including hypertension and hormonal contraception use, which were the most common.
METHODOLOGY:
- Melasma predominantly affects young women of color and often worsens in hyperestrogen states; understanding the association with comorbidities can improve surveillance and treatment strategies.
- Researchers evaluated 41,283 patients with melasma (mean age, 48.8 years; 93% women) from the TriNetX database and an equal number of matched control individuals.
- The main outcome was comorbidities including allergic rhinitis, atopic dermatitis, anticonvulsants, diabetes, hormonal contraceptives, hypothyroidism, hypertension, lupus, rosacea, skin cancer, and malignancy.
TAKEAWAY:
- Among those with melasma, 25% had hypertension and 24% used hormonal contraception, the two most commonly associated risk factors identified.
- Rosacea (odds ratio [OR], 5.1), atopic dermatitis (OR, 3.3), lupus (OR, 2.5), history of skin cancer (OR, 2.5), and history of internal malignancy (OR, 2.1) were associated with the highest risk of developing melasma (P < .01 for all).
- Asian (OR, 2.0; P < .01) and “other/unknown” races (OR, 1.7; P < .01) and Hispanic ethnicity (OR, 1.3; P < .01) were also significantly associated with melasma, while the odds were slightly lower among White, Black/African American, and “not Hispanic” groups (ORs, 0.8; P < .01 for all groups).
IN PRACTICE:
the authors wrote.
SOURCE:
The study, led by Ajay N. Sharma, MD, MBA, of the Department of Dermatology at the University of California, Irvine, was published online in Journal of Drugs in Dermatology.
LIMITATIONS:
The study limitations included the retrospective design, potential misclassification of diagnoses, and the inability to establish causality.
DISCLOSURES:
The study did not disclose any funding sources. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
A study found significant associations between melasma and several comorbidities, including hypertension and hormonal contraception use, which were the most common.
METHODOLOGY:
- Melasma predominantly affects young women of color and often worsens in hyperestrogen states; understanding the association with comorbidities can improve surveillance and treatment strategies.
- Researchers evaluated 41,283 patients with melasma (mean age, 48.8 years; 93% women) from the TriNetX database and an equal number of matched control individuals.
- The main outcome was comorbidities including allergic rhinitis, atopic dermatitis, anticonvulsants, diabetes, hormonal contraceptives, hypothyroidism, hypertension, lupus, rosacea, skin cancer, and malignancy.
TAKEAWAY:
- Among those with melasma, 25% had hypertension and 24% used hormonal contraception, the two most commonly associated risk factors identified.
- Rosacea (odds ratio [OR], 5.1), atopic dermatitis (OR, 3.3), lupus (OR, 2.5), history of skin cancer (OR, 2.5), and history of internal malignancy (OR, 2.1) were associated with the highest risk of developing melasma (P < .01 for all).
- Asian (OR, 2.0; P < .01) and “other/unknown” races (OR, 1.7; P < .01) and Hispanic ethnicity (OR, 1.3; P < .01) were also significantly associated with melasma, while the odds were slightly lower among White, Black/African American, and “not Hispanic” groups (ORs, 0.8; P < .01 for all groups).
IN PRACTICE:
the authors wrote.
SOURCE:
The study, led by Ajay N. Sharma, MD, MBA, of the Department of Dermatology at the University of California, Irvine, was published online in Journal of Drugs in Dermatology.
LIMITATIONS:
The study limitations included the retrospective design, potential misclassification of diagnoses, and the inability to establish causality.
DISCLOSURES:
The study did not disclose any funding sources. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
Case Series: Upadacitinib Effective for Granulomatous Cheilitis
TOPLINE:
in a small retrospective case series.
METHODOLOGY:
- Granulomatous cheilitis is a rare, nonnecrotizing granulomatous inflammatory disorder characterized by intermittent or persistent swelling of the lips.
- In a retrospective case series of five patients (median age, 30 years; four women) with granulomatous cheilitis resistant to systemic treatments at a Belgian hospital between June 2023 and March 2024, all five were treated with a high dose of upadacitinib (30 mg daily).
- The primary endpoint was objective clinical improvement in lip swelling and infiltration over a median follow-up of 7.2 months.
- Three patients had concomitant dormant Crohn’s disease (CD); a secondary outcome was disease activity in these patients.
TAKEAWAY:
- Upadacitinib treatment resulted in a complete response in four patients (80%) within a median of 3.8 months and a partial response in one patient.
- CD remained dormant in the three patients with CD.
- The safety profile of upadacitinib was favorable, and no serious adverse events were reported. Two patients experienced headaches, acne, mild changes in lipids, and/or transaminitis.
IN PRACTICE:
“Upadacitinib was effective in treating patients with recalcitrant and long-lasting granulomatous cheilitis, even in cases of concomitant CD, which could substantially improve the quality of life of affected patients,” the authors wrote. More studies are needed to confirm these results in larger groups of patients over longer periods of time, “and with other JAK inhibitors.”
SOURCE:
The study was led by Axel De Greef, MD, Department of Dermatology, Cliniques universitaires Saint-Luc, Université catholique de Louvain (UCLouvain), Brussels, Belgium. It was published online in JAMA Dermatology.
LIMITATIONS:
The small sample size and short follow-up may limit the generalizability of the findings to a larger population of patients with granulomatous cheilitis.
DISCLOSURES:
The study did not report any funding sources. Some authors reported receiving nonfinancial support and personal fees from various pharmaceutical companies outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
in a small retrospective case series.
METHODOLOGY:
- Granulomatous cheilitis is a rare, nonnecrotizing granulomatous inflammatory disorder characterized by intermittent or persistent swelling of the lips.
- In a retrospective case series of five patients (median age, 30 years; four women) with granulomatous cheilitis resistant to systemic treatments at a Belgian hospital between June 2023 and March 2024, all five were treated with a high dose of upadacitinib (30 mg daily).
- The primary endpoint was objective clinical improvement in lip swelling and infiltration over a median follow-up of 7.2 months.
- Three patients had concomitant dormant Crohn’s disease (CD); a secondary outcome was disease activity in these patients.
TAKEAWAY:
- Upadacitinib treatment resulted in a complete response in four patients (80%) within a median of 3.8 months and a partial response in one patient.
- CD remained dormant in the three patients with CD.
- The safety profile of upadacitinib was favorable, and no serious adverse events were reported. Two patients experienced headaches, acne, mild changes in lipids, and/or transaminitis.
IN PRACTICE:
“Upadacitinib was effective in treating patients with recalcitrant and long-lasting granulomatous cheilitis, even in cases of concomitant CD, which could substantially improve the quality of life of affected patients,” the authors wrote. More studies are needed to confirm these results in larger groups of patients over longer periods of time, “and with other JAK inhibitors.”
SOURCE:
The study was led by Axel De Greef, MD, Department of Dermatology, Cliniques universitaires Saint-Luc, Université catholique de Louvain (UCLouvain), Brussels, Belgium. It was published online in JAMA Dermatology.
LIMITATIONS:
The small sample size and short follow-up may limit the generalizability of the findings to a larger population of patients with granulomatous cheilitis.
DISCLOSURES:
The study did not report any funding sources. Some authors reported receiving nonfinancial support and personal fees from various pharmaceutical companies outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
in a small retrospective case series.
METHODOLOGY:
- Granulomatous cheilitis is a rare, nonnecrotizing granulomatous inflammatory disorder characterized by intermittent or persistent swelling of the lips.
- In a retrospective case series of five patients (median age, 30 years; four women) with granulomatous cheilitis resistant to systemic treatments at a Belgian hospital between June 2023 and March 2024, all five were treated with a high dose of upadacitinib (30 mg daily).
- The primary endpoint was objective clinical improvement in lip swelling and infiltration over a median follow-up of 7.2 months.
- Three patients had concomitant dormant Crohn’s disease (CD); a secondary outcome was disease activity in these patients.
TAKEAWAY:
- Upadacitinib treatment resulted in a complete response in four patients (80%) within a median of 3.8 months and a partial response in one patient.
- CD remained dormant in the three patients with CD.
- The safety profile of upadacitinib was favorable, and no serious adverse events were reported. Two patients experienced headaches, acne, mild changes in lipids, and/or transaminitis.
IN PRACTICE:
“Upadacitinib was effective in treating patients with recalcitrant and long-lasting granulomatous cheilitis, even in cases of concomitant CD, which could substantially improve the quality of life of affected patients,” the authors wrote. More studies are needed to confirm these results in larger groups of patients over longer periods of time, “and with other JAK inhibitors.”
SOURCE:
The study was led by Axel De Greef, MD, Department of Dermatology, Cliniques universitaires Saint-Luc, Université catholique de Louvain (UCLouvain), Brussels, Belgium. It was published online in JAMA Dermatology.
LIMITATIONS:
The small sample size and short follow-up may limit the generalizability of the findings to a larger population of patients with granulomatous cheilitis.
DISCLOSURES:
The study did not report any funding sources. Some authors reported receiving nonfinancial support and personal fees from various pharmaceutical companies outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Psychiatric, Autoimmune Comorbidities Increased in Patients with Alopecia Areata
TOPLINE:
and were at greater risk of developing those comorbidities after diagnosis.
METHODOLOGY:
- Researchers evaluated 63,384 patients with AA and 3,309,107 individuals without AA (aged 12-64 years) from the Merative MarketScan Research Databases.
- The matched cohorts included 16,512 patients with AA and 66,048 control individuals.
- Outcomes were the prevalence of psychiatric and autoimmune diseases at baseline and the incidence of new-onset psychiatric and autoimmune diseases during the year after diagnosis.
TAKEAWAY:
- Overall, patients with AA showed a greater prevalence of any psychiatric disease (30.9% vs 26.8%; P < .001) and any immune-mediated or autoimmune disease (16.1% vs 8.9%; P < .0001) than those with controls.
- In matched cohorts, patients with AA also showed a higher incidence of any new-onset psychiatric diseases (10.2% vs 6.8%; P < .001) or immune-mediated or autoimmune disease (6.2% vs 1.5%; P <.001) within the first 12 months of AA diagnosis than those with controls.
- Among patients with AA, the risk of developing a psychiatric comorbidity was higher (adjusted hazard ratio [aHR], 1.3; 95% CI, 1.3-1.4). The highest risks were seen for adjustment disorder (aHR, 1.5), panic disorder (aHR, 1.4), and sexual dysfunction (aHR, 1.4).
- Compared with controls, patients with AA were also at an increased risk of developing immune-mediated or autoimmune comorbidities (aHR, 2.7; 95% CI, 2.5-2.8), with the highest for systemic lupus (aHR, 5.7), atopic dermatitis (aHR, 4.3), and vitiligo (aHR, 3.8).
IN PRACTICE:
“Routine monitoring of patients with AA, especially those at risk of developing comorbidities, may permit earlier and more effective intervention,” the authors wrote.
SOURCE:
The study was led by Arash Mostaghimi, MD, MPA, MPH, Brigham and Women’s Hospital and Harvard University, Boston. It was published online on July 31, 2024, in JAMA Dermatology.
LIMITATIONS:
Causality could not be inferred because of the retrospective nature of the study. Comorbidities were solely diagnosed on the basis of diagnostic codes, and researchers did not have access to characteristics such as lab values that could have indicated any underlying comorbidity before the AA diagnosis. This study also did not account for the varying levels of severity of the disease, which may have led to an underestimation of disease burden and the risk for comorbidities.
DISCLOSURES:
AbbVie provided funding for this study. Mostaghimi disclosed receiving personal fees from Abbvie and several other companies outside of this work. The other four authors were current or former employees of Abbvie and have or may have stock and/or stock options in AbbVie.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
and were at greater risk of developing those comorbidities after diagnosis.
METHODOLOGY:
- Researchers evaluated 63,384 patients with AA and 3,309,107 individuals without AA (aged 12-64 years) from the Merative MarketScan Research Databases.
- The matched cohorts included 16,512 patients with AA and 66,048 control individuals.
- Outcomes were the prevalence of psychiatric and autoimmune diseases at baseline and the incidence of new-onset psychiatric and autoimmune diseases during the year after diagnosis.
TAKEAWAY:
- Overall, patients with AA showed a greater prevalence of any psychiatric disease (30.9% vs 26.8%; P < .001) and any immune-mediated or autoimmune disease (16.1% vs 8.9%; P < .0001) than those with controls.
- In matched cohorts, patients with AA also showed a higher incidence of any new-onset psychiatric diseases (10.2% vs 6.8%; P < .001) or immune-mediated or autoimmune disease (6.2% vs 1.5%; P <.001) within the first 12 months of AA diagnosis than those with controls.
- Among patients with AA, the risk of developing a psychiatric comorbidity was higher (adjusted hazard ratio [aHR], 1.3; 95% CI, 1.3-1.4). The highest risks were seen for adjustment disorder (aHR, 1.5), panic disorder (aHR, 1.4), and sexual dysfunction (aHR, 1.4).
- Compared with controls, patients with AA were also at an increased risk of developing immune-mediated or autoimmune comorbidities (aHR, 2.7; 95% CI, 2.5-2.8), with the highest for systemic lupus (aHR, 5.7), atopic dermatitis (aHR, 4.3), and vitiligo (aHR, 3.8).
IN PRACTICE:
“Routine monitoring of patients with AA, especially those at risk of developing comorbidities, may permit earlier and more effective intervention,” the authors wrote.
SOURCE:
The study was led by Arash Mostaghimi, MD, MPA, MPH, Brigham and Women’s Hospital and Harvard University, Boston. It was published online on July 31, 2024, in JAMA Dermatology.
LIMITATIONS:
Causality could not be inferred because of the retrospective nature of the study. Comorbidities were solely diagnosed on the basis of diagnostic codes, and researchers did not have access to characteristics such as lab values that could have indicated any underlying comorbidity before the AA diagnosis. This study also did not account for the varying levels of severity of the disease, which may have led to an underestimation of disease burden and the risk for comorbidities.
DISCLOSURES:
AbbVie provided funding for this study. Mostaghimi disclosed receiving personal fees from Abbvie and several other companies outside of this work. The other four authors were current or former employees of Abbvie and have or may have stock and/or stock options in AbbVie.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
and were at greater risk of developing those comorbidities after diagnosis.
METHODOLOGY:
- Researchers evaluated 63,384 patients with AA and 3,309,107 individuals without AA (aged 12-64 years) from the Merative MarketScan Research Databases.
- The matched cohorts included 16,512 patients with AA and 66,048 control individuals.
- Outcomes were the prevalence of psychiatric and autoimmune diseases at baseline and the incidence of new-onset psychiatric and autoimmune diseases during the year after diagnosis.
TAKEAWAY:
- Overall, patients with AA showed a greater prevalence of any psychiatric disease (30.9% vs 26.8%; P < .001) and any immune-mediated or autoimmune disease (16.1% vs 8.9%; P < .0001) than those with controls.
- In matched cohorts, patients with AA also showed a higher incidence of any new-onset psychiatric diseases (10.2% vs 6.8%; P < .001) or immune-mediated or autoimmune disease (6.2% vs 1.5%; P <.001) within the first 12 months of AA diagnosis than those with controls.
- Among patients with AA, the risk of developing a psychiatric comorbidity was higher (adjusted hazard ratio [aHR], 1.3; 95% CI, 1.3-1.4). The highest risks were seen for adjustment disorder (aHR, 1.5), panic disorder (aHR, 1.4), and sexual dysfunction (aHR, 1.4).
- Compared with controls, patients with AA were also at an increased risk of developing immune-mediated or autoimmune comorbidities (aHR, 2.7; 95% CI, 2.5-2.8), with the highest for systemic lupus (aHR, 5.7), atopic dermatitis (aHR, 4.3), and vitiligo (aHR, 3.8).
IN PRACTICE:
“Routine monitoring of patients with AA, especially those at risk of developing comorbidities, may permit earlier and more effective intervention,” the authors wrote.
SOURCE:
The study was led by Arash Mostaghimi, MD, MPA, MPH, Brigham and Women’s Hospital and Harvard University, Boston. It was published online on July 31, 2024, in JAMA Dermatology.
LIMITATIONS:
Causality could not be inferred because of the retrospective nature of the study. Comorbidities were solely diagnosed on the basis of diagnostic codes, and researchers did not have access to characteristics such as lab values that could have indicated any underlying comorbidity before the AA diagnosis. This study also did not account for the varying levels of severity of the disease, which may have led to an underestimation of disease burden and the risk for comorbidities.
DISCLOSURES:
AbbVie provided funding for this study. Mostaghimi disclosed receiving personal fees from Abbvie and several other companies outside of this work. The other four authors were current or former employees of Abbvie and have or may have stock and/or stock options in AbbVie.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Expanded Surface Area Safe, Well-Tolerated for AK treatment
TOPLINE:
METHODOLOGY:
- This phase 3 multicenter, single-arm trial evaluated the safety and tolerability of tirbanibulin ointment 1% in 105 adults with 4-12 clinically typical, visible, and discrete AKs on the face or balding scalp from June to December 2022 in the United States. (In June 2024, the Food and Drug Administration approved a supplemental new drug application for tirbanibulin 1%, a microtubule inhibitor, allowing the expansion of the surface area treated for AKs of the face or scalp from 25 cm2 to 100 cm2.)
- Participants applied tirbanibulin ointment 1% once daily for 5 days over a treatment field of about 100 cm2 on the face or balding scalp. A total of 102 patients completed the study.
- Safety and tolerability were evaluated with reports of treatment-emergent adverse events (TEAEs) and a composite score of six local tolerability signs on days 5, 8, 15, and 29, and on completion of the evaluation period on day 57.
TAKEAWAY:
- The most common local effects of treatment were erythema (96.1% of patients) and flaking or scaling (84.4%), with severe cases reported in 5.8% and 8.7% of the patients, respectively.
- The mean maximum local tolerability composite score was 4.1 out of 18, which peaked around day 8 and returned to baseline by day 29.
- TEAEs considered related to the treatment were reported in 18.1% of patients; the most frequent were application site pruritus (10.5%) and application site pain (8.6%). No adverse events led to the discontinuation of treatment.
- The mean percent reduction in the lesion count from baseline was 77.8% at day 57, with a mean lesion count of 1.8 at the end of the study.
IN PRACTICE:
In this study, “local tolerability and safety profiles were well characterized in patients with 4-12 clinically typical, visible, and discrete AK lesions in a field of 100 cm2 and were consistent with those previously reported in patients with AK treated in pivotal trials with tirbanibulin over a smaller field (25 cm2),” the authors wrote.
SOURCE:
The study, led by Neal Bhatia, MD, of Therapeutics Clinical Research, San Diego, was published online in JAAD International.
LIMITATIONS:
The study was limited by the lack of a placebo group and the absence of long-term follow-up.
DISCLOSURES:
This study was funded by Almirall. Five authors reported being employees of Almirall. Other authors declared having ties with various other sources, including Almirall.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- This phase 3 multicenter, single-arm trial evaluated the safety and tolerability of tirbanibulin ointment 1% in 105 adults with 4-12 clinically typical, visible, and discrete AKs on the face or balding scalp from June to December 2022 in the United States. (In June 2024, the Food and Drug Administration approved a supplemental new drug application for tirbanibulin 1%, a microtubule inhibitor, allowing the expansion of the surface area treated for AKs of the face or scalp from 25 cm2 to 100 cm2.)
- Participants applied tirbanibulin ointment 1% once daily for 5 days over a treatment field of about 100 cm2 on the face or balding scalp. A total of 102 patients completed the study.
- Safety and tolerability were evaluated with reports of treatment-emergent adverse events (TEAEs) and a composite score of six local tolerability signs on days 5, 8, 15, and 29, and on completion of the evaluation period on day 57.
TAKEAWAY:
- The most common local effects of treatment were erythema (96.1% of patients) and flaking or scaling (84.4%), with severe cases reported in 5.8% and 8.7% of the patients, respectively.
- The mean maximum local tolerability composite score was 4.1 out of 18, which peaked around day 8 and returned to baseline by day 29.
- TEAEs considered related to the treatment were reported in 18.1% of patients; the most frequent were application site pruritus (10.5%) and application site pain (8.6%). No adverse events led to the discontinuation of treatment.
- The mean percent reduction in the lesion count from baseline was 77.8% at day 57, with a mean lesion count of 1.8 at the end of the study.
IN PRACTICE:
In this study, “local tolerability and safety profiles were well characterized in patients with 4-12 clinically typical, visible, and discrete AK lesions in a field of 100 cm2 and were consistent with those previously reported in patients with AK treated in pivotal trials with tirbanibulin over a smaller field (25 cm2),” the authors wrote.
SOURCE:
The study, led by Neal Bhatia, MD, of Therapeutics Clinical Research, San Diego, was published online in JAAD International.
LIMITATIONS:
The study was limited by the lack of a placebo group and the absence of long-term follow-up.
DISCLOSURES:
This study was funded by Almirall. Five authors reported being employees of Almirall. Other authors declared having ties with various other sources, including Almirall.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- This phase 3 multicenter, single-arm trial evaluated the safety and tolerability of tirbanibulin ointment 1% in 105 adults with 4-12 clinically typical, visible, and discrete AKs on the face or balding scalp from June to December 2022 in the United States. (In June 2024, the Food and Drug Administration approved a supplemental new drug application for tirbanibulin 1%, a microtubule inhibitor, allowing the expansion of the surface area treated for AKs of the face or scalp from 25 cm2 to 100 cm2.)
- Participants applied tirbanibulin ointment 1% once daily for 5 days over a treatment field of about 100 cm2 on the face or balding scalp. A total of 102 patients completed the study.
- Safety and tolerability were evaluated with reports of treatment-emergent adverse events (TEAEs) and a composite score of six local tolerability signs on days 5, 8, 15, and 29, and on completion of the evaluation period on day 57.
TAKEAWAY:
- The most common local effects of treatment were erythema (96.1% of patients) and flaking or scaling (84.4%), with severe cases reported in 5.8% and 8.7% of the patients, respectively.
- The mean maximum local tolerability composite score was 4.1 out of 18, which peaked around day 8 and returned to baseline by day 29.
- TEAEs considered related to the treatment were reported in 18.1% of patients; the most frequent were application site pruritus (10.5%) and application site pain (8.6%). No adverse events led to the discontinuation of treatment.
- The mean percent reduction in the lesion count from baseline was 77.8% at day 57, with a mean lesion count of 1.8 at the end of the study.
IN PRACTICE:
In this study, “local tolerability and safety profiles were well characterized in patients with 4-12 clinically typical, visible, and discrete AK lesions in a field of 100 cm2 and were consistent with those previously reported in patients with AK treated in pivotal trials with tirbanibulin over a smaller field (25 cm2),” the authors wrote.
SOURCE:
The study, led by Neal Bhatia, MD, of Therapeutics Clinical Research, San Diego, was published online in JAAD International.
LIMITATIONS:
The study was limited by the lack of a placebo group and the absence of long-term follow-up.
DISCLOSURES:
This study was funded by Almirall. Five authors reported being employees of Almirall. Other authors declared having ties with various other sources, including Almirall.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Skin Dxs in Children in Refugee Camps Include Fungal Infections, Leishmaniasis
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
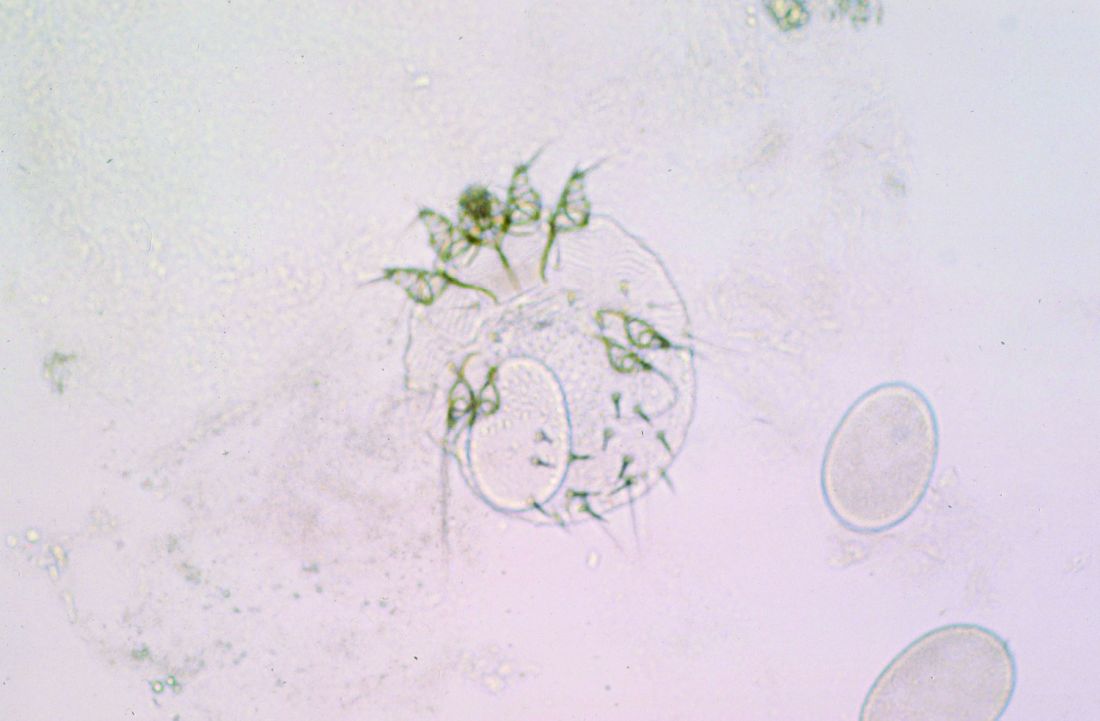
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Consider Risks, Toxicity of Some Topical Ingredients in Infants, Young Children
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Advantages of a Pediatric Rheumatology/Dermatology Clinic Evaluated
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Underserved Families Share Ways to Improve Access to Pediatric Dermatologists
, a theme emerged that surprised lead study author Lucinda L. Kohn, MD, MHS.
“Most families said that racial concordance didn’t matter that much, but they did place high value on being heard,” Dr. Kohn, of the Department of Dermatology at the University of Colorado, Aurora, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “Being heard means that their experience was respected; that their questions and worries were anticipated, addressed, and answered; and that their feelings were acknowledged.”
As a way to understand these families’ knowledge, attitudes, and beliefs about access to pediatric dermatology care and how the hospital system and medical team could better support them, Dr. Kohn and colleagues conducted in-depth, semi-structured interviews with 32 English-speaking parents and/or guardians of children who received care at the Children’s Hospital Colorado Anschutz Medical Campus pediatric dermatology clinic. The researchers conducted and recorded the 30- to 60-minute interviews via Zoom or phone call from October 17, 2023, to January 23, 2024. Domains of interest included participant background and experiences, communication preferences, and experience accessing pediatric dermatology care. Next, Dr. Kohn and colleagues used a reflexive, team-based inductive approach to carry out a thematic analysis from the interviews.
The mean age of the 32 study participants was 38.9 years; 14 (43.75%) identified as Hispanic, 11 (34.38%) as Black, and 12 (37.50%) as American Indian/Alaska Native (response categories were not mutually exclusive). Several themes emerged from analysis of the interviews. Barriers to receiving pediatric dermatology care included distrust of the healthcare system, generational and community lack of awareness about dermatology, distance to the hospital, and household income.
“One family mentioned that they needed to save up for 3 months to be able to afford the drive, hotel, and food needed for their child to attend their pediatric dermatology visit,” Dr. Kohn said. “As we know, most pediatric dermatology visits are 10-15 minutes long, so that they needed to cut groceries for 3 months to be able to see a pediatric dermatologist for 10-15 minutes is just heart wrenching. Families also didn’t understand the large teams that we have in medicine: The medical students, residents, nurses, medical assistants, attendings, and physician extenders.”
One key facilitator to receiving pediatric dermatology care was the family’s perception that the provider shares their minoritized experience because of similarities in skin tone. “When it’s your own race, whether it’s Black, Hispanic, or you know, we feel like when it’s someone like me, they will look out for me more,” one study participant said. Other facilitators expressed by the study participants included increased representation from the family’s community at all levels of healthcare (“the more you see providers and people in a space that look like you, I think the more welcoming it will feel,” one said) and normalizing dermatology care (“letting it be known that going to the dermatologist is just like going to a regular doctor,” another said).
Dr. Kohn acknowledged certain limitations of the study, including its single-center qualitative design. “Qualitative studies are not generalizable, but they do dive into the lived experiences of a few,” she said. “There aren’t a lot of qualitative studies in derm, so even though this was a very simple study, we hope the findings will help us to support our most diverse and underserved families access the pediatric dermatology care that they need.”
The researchers reported having no relevant financial disclosures. The study was recognized as an award-winning poster at the meeting.
A version of this article appeared on Medscape.com.
, a theme emerged that surprised lead study author Lucinda L. Kohn, MD, MHS.
“Most families said that racial concordance didn’t matter that much, but they did place high value on being heard,” Dr. Kohn, of the Department of Dermatology at the University of Colorado, Aurora, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “Being heard means that their experience was respected; that their questions and worries were anticipated, addressed, and answered; and that their feelings were acknowledged.”
As a way to understand these families’ knowledge, attitudes, and beliefs about access to pediatric dermatology care and how the hospital system and medical team could better support them, Dr. Kohn and colleagues conducted in-depth, semi-structured interviews with 32 English-speaking parents and/or guardians of children who received care at the Children’s Hospital Colorado Anschutz Medical Campus pediatric dermatology clinic. The researchers conducted and recorded the 30- to 60-minute interviews via Zoom or phone call from October 17, 2023, to January 23, 2024. Domains of interest included participant background and experiences, communication preferences, and experience accessing pediatric dermatology care. Next, Dr. Kohn and colleagues used a reflexive, team-based inductive approach to carry out a thematic analysis from the interviews.
The mean age of the 32 study participants was 38.9 years; 14 (43.75%) identified as Hispanic, 11 (34.38%) as Black, and 12 (37.50%) as American Indian/Alaska Native (response categories were not mutually exclusive). Several themes emerged from analysis of the interviews. Barriers to receiving pediatric dermatology care included distrust of the healthcare system, generational and community lack of awareness about dermatology, distance to the hospital, and household income.
“One family mentioned that they needed to save up for 3 months to be able to afford the drive, hotel, and food needed for their child to attend their pediatric dermatology visit,” Dr. Kohn said. “As we know, most pediatric dermatology visits are 10-15 minutes long, so that they needed to cut groceries for 3 months to be able to see a pediatric dermatologist for 10-15 minutes is just heart wrenching. Families also didn’t understand the large teams that we have in medicine: The medical students, residents, nurses, medical assistants, attendings, and physician extenders.”
One key facilitator to receiving pediatric dermatology care was the family’s perception that the provider shares their minoritized experience because of similarities in skin tone. “When it’s your own race, whether it’s Black, Hispanic, or you know, we feel like when it’s someone like me, they will look out for me more,” one study participant said. Other facilitators expressed by the study participants included increased representation from the family’s community at all levels of healthcare (“the more you see providers and people in a space that look like you, I think the more welcoming it will feel,” one said) and normalizing dermatology care (“letting it be known that going to the dermatologist is just like going to a regular doctor,” another said).
Dr. Kohn acknowledged certain limitations of the study, including its single-center qualitative design. “Qualitative studies are not generalizable, but they do dive into the lived experiences of a few,” she said. “There aren’t a lot of qualitative studies in derm, so even though this was a very simple study, we hope the findings will help us to support our most diverse and underserved families access the pediatric dermatology care that they need.”
The researchers reported having no relevant financial disclosures. The study was recognized as an award-winning poster at the meeting.
A version of this article appeared on Medscape.com.
, a theme emerged that surprised lead study author Lucinda L. Kohn, MD, MHS.
“Most families said that racial concordance didn’t matter that much, but they did place high value on being heard,” Dr. Kohn, of the Department of Dermatology at the University of Colorado, Aurora, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “Being heard means that their experience was respected; that their questions and worries were anticipated, addressed, and answered; and that their feelings were acknowledged.”
As a way to understand these families’ knowledge, attitudes, and beliefs about access to pediatric dermatology care and how the hospital system and medical team could better support them, Dr. Kohn and colleagues conducted in-depth, semi-structured interviews with 32 English-speaking parents and/or guardians of children who received care at the Children’s Hospital Colorado Anschutz Medical Campus pediatric dermatology clinic. The researchers conducted and recorded the 30- to 60-minute interviews via Zoom or phone call from October 17, 2023, to January 23, 2024. Domains of interest included participant background and experiences, communication preferences, and experience accessing pediatric dermatology care. Next, Dr. Kohn and colleagues used a reflexive, team-based inductive approach to carry out a thematic analysis from the interviews.
The mean age of the 32 study participants was 38.9 years; 14 (43.75%) identified as Hispanic, 11 (34.38%) as Black, and 12 (37.50%) as American Indian/Alaska Native (response categories were not mutually exclusive). Several themes emerged from analysis of the interviews. Barriers to receiving pediatric dermatology care included distrust of the healthcare system, generational and community lack of awareness about dermatology, distance to the hospital, and household income.
“One family mentioned that they needed to save up for 3 months to be able to afford the drive, hotel, and food needed for their child to attend their pediatric dermatology visit,” Dr. Kohn said. “As we know, most pediatric dermatology visits are 10-15 minutes long, so that they needed to cut groceries for 3 months to be able to see a pediatric dermatologist for 10-15 minutes is just heart wrenching. Families also didn’t understand the large teams that we have in medicine: The medical students, residents, nurses, medical assistants, attendings, and physician extenders.”
One key facilitator to receiving pediatric dermatology care was the family’s perception that the provider shares their minoritized experience because of similarities in skin tone. “When it’s your own race, whether it’s Black, Hispanic, or you know, we feel like when it’s someone like me, they will look out for me more,” one study participant said. Other facilitators expressed by the study participants included increased representation from the family’s community at all levels of healthcare (“the more you see providers and people in a space that look like you, I think the more welcoming it will feel,” one said) and normalizing dermatology care (“letting it be known that going to the dermatologist is just like going to a regular doctor,” another said).
Dr. Kohn acknowledged certain limitations of the study, including its single-center qualitative design. “Qualitative studies are not generalizable, but they do dive into the lived experiences of a few,” she said. “There aren’t a lot of qualitative studies in derm, so even though this was a very simple study, we hope the findings will help us to support our most diverse and underserved families access the pediatric dermatology care that they need.”
The researchers reported having no relevant financial disclosures. The study was recognized as an award-winning poster at the meeting.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Study Finds Gout Drug Effective for Aphthous Ulcers in Children
“Complex aphthous stomatitis in children is typically treated with topical supportive care, which is often not effective,” one of the study investigators, Ananya Shah, a third-year medical student at the University of Rochester School of Medicine & Dentistry, Rochester, New York, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “There is limited research on CAS and its treatment in children. Colchicine is often used for treatment of CAS in adults, but its use in children has not been studied.”
Ms. Shah, in collaboration with Hilary Kunkel, MD, Nessa Aghazadeh, MD, and Megha Tollefson, MD, of the Department of Dermatology, Mayo Clinic, Rochester, Minnesota, retrospectively reviewed the charts of 20 children diagnosed with CAS who were treated with colchicine, an anti-inflammatory drug often used to treat gout, at the clinic between 2000 and 2023. Treatment responses were defined as no response, partial response, and complete response. Half of the patients were girls, and their median age at presentation was 5 years.
Ulcers were most commonly located in the buccal mucosa (80%), followed by the gingiva (50%), the mucosal lip (50%), and the palate (40%). Nearly all patients (95%) reported that the CAS caused difficulties with eating or drinking. Other effects on their quality of life included weight loss (35%), bleeding (30%), and difficulty brushing teeth (25%). “I was surprised by how much CAS impacts pediatric patients’ quality of life,” Ms. Shah said. “Almost all of the patients experienced trouble with basic activities of daily living, including eating and drinking. In addition, CAS negatively impacted mental health and led to missed school for patients.”
The researchers had follow-up data on responses to colchicine for 14 of the 20 patients. Of these, 12 (86%) had symptom improvement, 5 (36%) had a complete response, 8 (57%) had a partial response, and 1 (7%) did not respond. Nine patients (64%) experienced side effects. Of these, six had diarrhea, two had nausea, and one had constipation.
“Colchicine should be considered as a treatment in pediatric patients who have refractory complex aphthous stomatitis as it is generally well tolerated with minimal side effects,” Ms. Shah said. She acknowledged certain limitations of the study, including its single-center, retrospective design.
The researchers reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
“Complex aphthous stomatitis in children is typically treated with topical supportive care, which is often not effective,” one of the study investigators, Ananya Shah, a third-year medical student at the University of Rochester School of Medicine & Dentistry, Rochester, New York, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “There is limited research on CAS and its treatment in children. Colchicine is often used for treatment of CAS in adults, but its use in children has not been studied.”
Ms. Shah, in collaboration with Hilary Kunkel, MD, Nessa Aghazadeh, MD, and Megha Tollefson, MD, of the Department of Dermatology, Mayo Clinic, Rochester, Minnesota, retrospectively reviewed the charts of 20 children diagnosed with CAS who were treated with colchicine, an anti-inflammatory drug often used to treat gout, at the clinic between 2000 and 2023. Treatment responses were defined as no response, partial response, and complete response. Half of the patients were girls, and their median age at presentation was 5 years.
Ulcers were most commonly located in the buccal mucosa (80%), followed by the gingiva (50%), the mucosal lip (50%), and the palate (40%). Nearly all patients (95%) reported that the CAS caused difficulties with eating or drinking. Other effects on their quality of life included weight loss (35%), bleeding (30%), and difficulty brushing teeth (25%). “I was surprised by how much CAS impacts pediatric patients’ quality of life,” Ms. Shah said. “Almost all of the patients experienced trouble with basic activities of daily living, including eating and drinking. In addition, CAS negatively impacted mental health and led to missed school for patients.”
The researchers had follow-up data on responses to colchicine for 14 of the 20 patients. Of these, 12 (86%) had symptom improvement, 5 (36%) had a complete response, 8 (57%) had a partial response, and 1 (7%) did not respond. Nine patients (64%) experienced side effects. Of these, six had diarrhea, two had nausea, and one had constipation.
“Colchicine should be considered as a treatment in pediatric patients who have refractory complex aphthous stomatitis as it is generally well tolerated with minimal side effects,” Ms. Shah said. She acknowledged certain limitations of the study, including its single-center, retrospective design.
The researchers reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
“Complex aphthous stomatitis in children is typically treated with topical supportive care, which is often not effective,” one of the study investigators, Ananya Shah, a third-year medical student at the University of Rochester School of Medicine & Dentistry, Rochester, New York, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “There is limited research on CAS and its treatment in children. Colchicine is often used for treatment of CAS in adults, but its use in children has not been studied.”
Ms. Shah, in collaboration with Hilary Kunkel, MD, Nessa Aghazadeh, MD, and Megha Tollefson, MD, of the Department of Dermatology, Mayo Clinic, Rochester, Minnesota, retrospectively reviewed the charts of 20 children diagnosed with CAS who were treated with colchicine, an anti-inflammatory drug often used to treat gout, at the clinic between 2000 and 2023. Treatment responses were defined as no response, partial response, and complete response. Half of the patients were girls, and their median age at presentation was 5 years.
Ulcers were most commonly located in the buccal mucosa (80%), followed by the gingiva (50%), the mucosal lip (50%), and the palate (40%). Nearly all patients (95%) reported that the CAS caused difficulties with eating or drinking. Other effects on their quality of life included weight loss (35%), bleeding (30%), and difficulty brushing teeth (25%). “I was surprised by how much CAS impacts pediatric patients’ quality of life,” Ms. Shah said. “Almost all of the patients experienced trouble with basic activities of daily living, including eating and drinking. In addition, CAS negatively impacted mental health and led to missed school for patients.”
The researchers had follow-up data on responses to colchicine for 14 of the 20 patients. Of these, 12 (86%) had symptom improvement, 5 (36%) had a complete response, 8 (57%) had a partial response, and 1 (7%) did not respond. Nine patients (64%) experienced side effects. Of these, six had diarrhea, two had nausea, and one had constipation.
“Colchicine should be considered as a treatment in pediatric patients who have refractory complex aphthous stomatitis as it is generally well tolerated with minimal side effects,” Ms. Shah said. She acknowledged certain limitations of the study, including its single-center, retrospective design.
The researchers reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024