User login
Pretreatment Lab Testing for Chronic Skin Diseases Diverges From Guidelines
in a national commercial insurance claims database.
Because of concerns for the potential reactivation of tuberculosis or hepatitis B or C, or for an increased risk for infections, myelosuppression, and hepatoxicity in the wake of immunomodulator use, some medical societies recommend screening patients for hepatitis B, hepatitis C, and tuberculosis before starting these medications, wrote Maria C. Schneeweiss, MD, of Brigham and Women’s Hospital, Boston, Massachusetts, and colleagues.
“Conducting this study was crucial because of the increasing use of systemic immunomodulatory agents for chronic inflammatory skin diseases and the recognized need for pretreatment testing to prevent complications,” coauthor Denys Shay, a PhD candidate in population health sciences at Harvard University, Cambridge, Massachusetts, said in an interview.
“Despite recommendations from professional societies, there was a lack of clarity on how consistently these guidelines were being followed in the United States. This study aimed to fill that gap in knowledge, providing a comprehensive view of current practices and highlighting areas for improvement,” he said.
In the study, published online in JAMA Dermatology, he and his coauthors identified 122,308 adults in the United States with psoriasis, hidradenitis suppurativa, or atopic dermatitis who started an immunomodulatory agent, including methotrexate (28,684 patients), tumor necrosis factor (TNF)–alpha inhibitors (40,965), ustekinumab (12,841), interleukin (IL)-23 inhibitors (6116), IL-17A inhibitors (9799), dupilumab (7787), and apremilast (16,116). The data were from a commercial insurance claims database from December 31, 2002, to December 31, 2020.
The primary outcome was the proportion of patients who underwent recommended screening lab tests including tuberculosis, hepatitis, liver function, complete blood cell counts (CBCs), and lipid panels within 6 months before treatment initiation and during the first 2 years of treatment. The median age of the study population was 49 years, and 52.1% were male.
A CBC was the most common pretreatment test across treatments, performed in 41%-69% of patients before starting treatment. Tuberculosis screening occurred in 11%-59% of patients within 6 months of initiating treatment, and 3%-26% had updated tests after 1 year. Similarly, 13%-41% of patients underwent hepatitis screening prior to treatment.
The highest levels of pretreatment testing occurred for TNF-alpha inhibitors, ustekinumab, IL-17A inhibitors, and IL-23 inhibitors, with similar patterns, while the lowest levels of testing occurred with apremilast and dupilumab.
Testing prevalence before starting apremilast and after a year of treatment was 15%-45% and 9%-36%, respectively. Testing before initiation and a year into treatment with dupilumab was 11%-41% and 3%-25%, respectively.
The findings were limited by several factors including the descriptive design, which does not allow for evaluation of the testing practices, the researchers said.
However, the results show the extent of patients with chronic inflammatory skin diseases (CISDs) who do not undergo pretreatment testing, and research is needed to create testing practices on the basis of recommendations for each agent and incorporating each patient’s history and clinical profile, they concluded.
“The finding that less than 60% of patients received recommended pretreatment testing was initially somewhat surprising,” Shay said in the interview. “However, the context provided by higher rates of baseline testing within the 6-12 months before treatment initiation and the potential for additional testing not captured by the dataset — such as hospital stays — suggests that the gap may not be as large as this estimate,” he said.
“The key message for clinicians is that there are considerable variations in laboratory testing practices with regard to the initiation of systemic immunomodulatory agents in patients with CISDs,” Shay said. “This represents a divergence from existing testing guidelines.”
“Further research is needed to understand the reasons for the variations in pretreatment testing practices and whether this heterogeneity affects patient outcomes,” he added.
Resist Routine Testing
The study findings represent a call to action in the form of ongoing assessment of the safety, clinical utility, and cost-effectiveness of pretreatment testing, wrote Clinton W. Enos, MD, Ana Ormaza Vera, MD, and Abby S. Van Voorhees, MD, of the Department of Dermatology, Eastern Virginia Medical School, Norfolk, Virginia, in an accompanying editorial.
The data in the current study suggesting less frequent laboratory testing compared with current guidelines could stem from a high comfort level with many of the therapies that have been available and in use for many years, they noted. Clinicians’ lack of knowledge of the laboratory screening and monitoring guidelines also may play a role, they said.
However, the authors cautioned against routine checking of laboratory results “without purpose” and without attention to their clinical utility and cost. “A thorough medical history is essential and can serve as a sensitive indicator of which patients are more at risk for diseases such as TB or hepatitis, thereby allowing for more meaningful laboratory screening use,” they said.
Evidence supporting prescreening labs for the spectrum of systemic agents used in dermatology varies considerably, “some trapped in time and carried forward for decades until finally questioned, others rooted in treatment mechanism and clinical data,” Adam Friedman, MD, professor and chief of dermatology at George Washington University, Washington, DC, said in an interview.
The study elucidated the current state of clinical practice, said Friedman, who was not involved with the study. This includes screening even if the label says it is not necessary and letting screening slide when guidelines say otherwise — even if the guidelines are outdated and insurance requires certain metrics prior to approval, he said.
Looking ahead, “we need better consensus and even better communication/education on said guidance,” Dr. Friedman said. “Clear, concise, evidenced-based, and expert-validated guidance to ensure we are meaningfully using medical resources” is what is needed, he added. “It will certainly take a village, and close collaboration between the industry and practitioners is key to success.”
The study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Shay had no financial conflicts to disclose. Lead author Dr. Schneeweiss disclosed grants from UCB Pharma and AbbVie to Brigham and Women’s Hospital outside the submitted work. Other authors disclosed receiving personal fees from Aetion and grants from UCB Pharma and Takeda outside the submitted work; grants from Amarin, Kowa, Novartis, and Pfizer outside the submitted work; and personal fees from Hims & Hers, AbbVie, Sun Pharmaceuticals, Pfizer, Digital Diagnostics, Lilly, Equillium, ASLAN, Boehringer Ingelheim, ACOM, Olaplex, and Legacy Healthcare during the study. No other disclosures were reported.
Editorial author Dr. Enos disclosed serving as an investigator for Amgen and Castle Biosciences and receiving grants from Arcutis Biotherapeutics outside the submitted work. Dr. Van Voorhees disclosed an honorarium outside the submitted work.
Dr. Friedman had no relevant financial conflicts to disclose.
A version of this article appeared on Medscape.com.
in a national commercial insurance claims database.
Because of concerns for the potential reactivation of tuberculosis or hepatitis B or C, or for an increased risk for infections, myelosuppression, and hepatoxicity in the wake of immunomodulator use, some medical societies recommend screening patients for hepatitis B, hepatitis C, and tuberculosis before starting these medications, wrote Maria C. Schneeweiss, MD, of Brigham and Women’s Hospital, Boston, Massachusetts, and colleagues.
“Conducting this study was crucial because of the increasing use of systemic immunomodulatory agents for chronic inflammatory skin diseases and the recognized need for pretreatment testing to prevent complications,” coauthor Denys Shay, a PhD candidate in population health sciences at Harvard University, Cambridge, Massachusetts, said in an interview.
“Despite recommendations from professional societies, there was a lack of clarity on how consistently these guidelines were being followed in the United States. This study aimed to fill that gap in knowledge, providing a comprehensive view of current practices and highlighting areas for improvement,” he said.
In the study, published online in JAMA Dermatology, he and his coauthors identified 122,308 adults in the United States with psoriasis, hidradenitis suppurativa, or atopic dermatitis who started an immunomodulatory agent, including methotrexate (28,684 patients), tumor necrosis factor (TNF)–alpha inhibitors (40,965), ustekinumab (12,841), interleukin (IL)-23 inhibitors (6116), IL-17A inhibitors (9799), dupilumab (7787), and apremilast (16,116). The data were from a commercial insurance claims database from December 31, 2002, to December 31, 2020.
The primary outcome was the proportion of patients who underwent recommended screening lab tests including tuberculosis, hepatitis, liver function, complete blood cell counts (CBCs), and lipid panels within 6 months before treatment initiation and during the first 2 years of treatment. The median age of the study population was 49 years, and 52.1% were male.
A CBC was the most common pretreatment test across treatments, performed in 41%-69% of patients before starting treatment. Tuberculosis screening occurred in 11%-59% of patients within 6 months of initiating treatment, and 3%-26% had updated tests after 1 year. Similarly, 13%-41% of patients underwent hepatitis screening prior to treatment.
The highest levels of pretreatment testing occurred for TNF-alpha inhibitors, ustekinumab, IL-17A inhibitors, and IL-23 inhibitors, with similar patterns, while the lowest levels of testing occurred with apremilast and dupilumab.
Testing prevalence before starting apremilast and after a year of treatment was 15%-45% and 9%-36%, respectively. Testing before initiation and a year into treatment with dupilumab was 11%-41% and 3%-25%, respectively.
The findings were limited by several factors including the descriptive design, which does not allow for evaluation of the testing practices, the researchers said.
However, the results show the extent of patients with chronic inflammatory skin diseases (CISDs) who do not undergo pretreatment testing, and research is needed to create testing practices on the basis of recommendations for each agent and incorporating each patient’s history and clinical profile, they concluded.
“The finding that less than 60% of patients received recommended pretreatment testing was initially somewhat surprising,” Shay said in the interview. “However, the context provided by higher rates of baseline testing within the 6-12 months before treatment initiation and the potential for additional testing not captured by the dataset — such as hospital stays — suggests that the gap may not be as large as this estimate,” he said.
“The key message for clinicians is that there are considerable variations in laboratory testing practices with regard to the initiation of systemic immunomodulatory agents in patients with CISDs,” Shay said. “This represents a divergence from existing testing guidelines.”
“Further research is needed to understand the reasons for the variations in pretreatment testing practices and whether this heterogeneity affects patient outcomes,” he added.
Resist Routine Testing
The study findings represent a call to action in the form of ongoing assessment of the safety, clinical utility, and cost-effectiveness of pretreatment testing, wrote Clinton W. Enos, MD, Ana Ormaza Vera, MD, and Abby S. Van Voorhees, MD, of the Department of Dermatology, Eastern Virginia Medical School, Norfolk, Virginia, in an accompanying editorial.
The data in the current study suggesting less frequent laboratory testing compared with current guidelines could stem from a high comfort level with many of the therapies that have been available and in use for many years, they noted. Clinicians’ lack of knowledge of the laboratory screening and monitoring guidelines also may play a role, they said.
However, the authors cautioned against routine checking of laboratory results “without purpose” and without attention to their clinical utility and cost. “A thorough medical history is essential and can serve as a sensitive indicator of which patients are more at risk for diseases such as TB or hepatitis, thereby allowing for more meaningful laboratory screening use,” they said.
Evidence supporting prescreening labs for the spectrum of systemic agents used in dermatology varies considerably, “some trapped in time and carried forward for decades until finally questioned, others rooted in treatment mechanism and clinical data,” Adam Friedman, MD, professor and chief of dermatology at George Washington University, Washington, DC, said in an interview.
The study elucidated the current state of clinical practice, said Friedman, who was not involved with the study. This includes screening even if the label says it is not necessary and letting screening slide when guidelines say otherwise — even if the guidelines are outdated and insurance requires certain metrics prior to approval, he said.
Looking ahead, “we need better consensus and even better communication/education on said guidance,” Dr. Friedman said. “Clear, concise, evidenced-based, and expert-validated guidance to ensure we are meaningfully using medical resources” is what is needed, he added. “It will certainly take a village, and close collaboration between the industry and practitioners is key to success.”
The study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Shay had no financial conflicts to disclose. Lead author Dr. Schneeweiss disclosed grants from UCB Pharma and AbbVie to Brigham and Women’s Hospital outside the submitted work. Other authors disclosed receiving personal fees from Aetion and grants from UCB Pharma and Takeda outside the submitted work; grants from Amarin, Kowa, Novartis, and Pfizer outside the submitted work; and personal fees from Hims & Hers, AbbVie, Sun Pharmaceuticals, Pfizer, Digital Diagnostics, Lilly, Equillium, ASLAN, Boehringer Ingelheim, ACOM, Olaplex, and Legacy Healthcare during the study. No other disclosures were reported.
Editorial author Dr. Enos disclosed serving as an investigator for Amgen and Castle Biosciences and receiving grants from Arcutis Biotherapeutics outside the submitted work. Dr. Van Voorhees disclosed an honorarium outside the submitted work.
Dr. Friedman had no relevant financial conflicts to disclose.
A version of this article appeared on Medscape.com.
in a national commercial insurance claims database.
Because of concerns for the potential reactivation of tuberculosis or hepatitis B or C, or for an increased risk for infections, myelosuppression, and hepatoxicity in the wake of immunomodulator use, some medical societies recommend screening patients for hepatitis B, hepatitis C, and tuberculosis before starting these medications, wrote Maria C. Schneeweiss, MD, of Brigham and Women’s Hospital, Boston, Massachusetts, and colleagues.
“Conducting this study was crucial because of the increasing use of systemic immunomodulatory agents for chronic inflammatory skin diseases and the recognized need for pretreatment testing to prevent complications,” coauthor Denys Shay, a PhD candidate in population health sciences at Harvard University, Cambridge, Massachusetts, said in an interview.
“Despite recommendations from professional societies, there was a lack of clarity on how consistently these guidelines were being followed in the United States. This study aimed to fill that gap in knowledge, providing a comprehensive view of current practices and highlighting areas for improvement,” he said.
In the study, published online in JAMA Dermatology, he and his coauthors identified 122,308 adults in the United States with psoriasis, hidradenitis suppurativa, or atopic dermatitis who started an immunomodulatory agent, including methotrexate (28,684 patients), tumor necrosis factor (TNF)–alpha inhibitors (40,965), ustekinumab (12,841), interleukin (IL)-23 inhibitors (6116), IL-17A inhibitors (9799), dupilumab (7787), and apremilast (16,116). The data were from a commercial insurance claims database from December 31, 2002, to December 31, 2020.
The primary outcome was the proportion of patients who underwent recommended screening lab tests including tuberculosis, hepatitis, liver function, complete blood cell counts (CBCs), and lipid panels within 6 months before treatment initiation and during the first 2 years of treatment. The median age of the study population was 49 years, and 52.1% were male.
A CBC was the most common pretreatment test across treatments, performed in 41%-69% of patients before starting treatment. Tuberculosis screening occurred in 11%-59% of patients within 6 months of initiating treatment, and 3%-26% had updated tests after 1 year. Similarly, 13%-41% of patients underwent hepatitis screening prior to treatment.
The highest levels of pretreatment testing occurred for TNF-alpha inhibitors, ustekinumab, IL-17A inhibitors, and IL-23 inhibitors, with similar patterns, while the lowest levels of testing occurred with apremilast and dupilumab.
Testing prevalence before starting apremilast and after a year of treatment was 15%-45% and 9%-36%, respectively. Testing before initiation and a year into treatment with dupilumab was 11%-41% and 3%-25%, respectively.
The findings were limited by several factors including the descriptive design, which does not allow for evaluation of the testing practices, the researchers said.
However, the results show the extent of patients with chronic inflammatory skin diseases (CISDs) who do not undergo pretreatment testing, and research is needed to create testing practices on the basis of recommendations for each agent and incorporating each patient’s history and clinical profile, they concluded.
“The finding that less than 60% of patients received recommended pretreatment testing was initially somewhat surprising,” Shay said in the interview. “However, the context provided by higher rates of baseline testing within the 6-12 months before treatment initiation and the potential for additional testing not captured by the dataset — such as hospital stays — suggests that the gap may not be as large as this estimate,” he said.
“The key message for clinicians is that there are considerable variations in laboratory testing practices with regard to the initiation of systemic immunomodulatory agents in patients with CISDs,” Shay said. “This represents a divergence from existing testing guidelines.”
“Further research is needed to understand the reasons for the variations in pretreatment testing practices and whether this heterogeneity affects patient outcomes,” he added.
Resist Routine Testing
The study findings represent a call to action in the form of ongoing assessment of the safety, clinical utility, and cost-effectiveness of pretreatment testing, wrote Clinton W. Enos, MD, Ana Ormaza Vera, MD, and Abby S. Van Voorhees, MD, of the Department of Dermatology, Eastern Virginia Medical School, Norfolk, Virginia, in an accompanying editorial.
The data in the current study suggesting less frequent laboratory testing compared with current guidelines could stem from a high comfort level with many of the therapies that have been available and in use for many years, they noted. Clinicians’ lack of knowledge of the laboratory screening and monitoring guidelines also may play a role, they said.
However, the authors cautioned against routine checking of laboratory results “without purpose” and without attention to their clinical utility and cost. “A thorough medical history is essential and can serve as a sensitive indicator of which patients are more at risk for diseases such as TB or hepatitis, thereby allowing for more meaningful laboratory screening use,” they said.
Evidence supporting prescreening labs for the spectrum of systemic agents used in dermatology varies considerably, “some trapped in time and carried forward for decades until finally questioned, others rooted in treatment mechanism and clinical data,” Adam Friedman, MD, professor and chief of dermatology at George Washington University, Washington, DC, said in an interview.
The study elucidated the current state of clinical practice, said Friedman, who was not involved with the study. This includes screening even if the label says it is not necessary and letting screening slide when guidelines say otherwise — even if the guidelines are outdated and insurance requires certain metrics prior to approval, he said.
Looking ahead, “we need better consensus and even better communication/education on said guidance,” Dr. Friedman said. “Clear, concise, evidenced-based, and expert-validated guidance to ensure we are meaningfully using medical resources” is what is needed, he added. “It will certainly take a village, and close collaboration between the industry and practitioners is key to success.”
The study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Shay had no financial conflicts to disclose. Lead author Dr. Schneeweiss disclosed grants from UCB Pharma and AbbVie to Brigham and Women’s Hospital outside the submitted work. Other authors disclosed receiving personal fees from Aetion and grants from UCB Pharma and Takeda outside the submitted work; grants from Amarin, Kowa, Novartis, and Pfizer outside the submitted work; and personal fees from Hims & Hers, AbbVie, Sun Pharmaceuticals, Pfizer, Digital Diagnostics, Lilly, Equillium, ASLAN, Boehringer Ingelheim, ACOM, Olaplex, and Legacy Healthcare during the study. No other disclosures were reported.
Editorial author Dr. Enos disclosed serving as an investigator for Amgen and Castle Biosciences and receiving grants from Arcutis Biotherapeutics outside the submitted work. Dr. Van Voorhees disclosed an honorarium outside the submitted work.
Dr. Friedman had no relevant financial conflicts to disclose.
A version of this article appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Tapinarof Cream Under FDA Review for Atopic Dermatitis Indication
On February 14, Dermavant Sciences announced that the company had submitted a supplemental New Drug Application (sNDA) to the Food and Drug Administration for tapinarof cream, 1%, for treating atopic dermatitis (AD) in adults and children 2 years of age and older.
Tapinarof cream, 1%, is an aryl hydrocarbon receptor agonist marketed under the brand name VTAMA that was approved in 2022 for treating plaque psoriasis in adults.
According to a Dermavant press release, the sNDA is based on positive data from the phase 3 ADORING 1 and ADORING 2 pivotal trials and interim results from the phase 3 ADORING 3 open-label, long-term extension 48-week trial. In ADORING 1 and ADORING 2, tapinarof cream demonstrated statistically significant improvements in the primary endpoint of Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) treatment success, defined as a vIGA-AD score of 0 (clear) or 1 (almost clear) with at least a 2-grade improvement from baseline; demonstrated treatment success over vehicle at week 8; and met all key secondary endpoints with statistical significance, according to the company.
The most common adverse reactions in patients treated with VTAMA cream include folliculitis, nasopharyngitis, contact dermatitis, headache, and pruritus.
On February 14, Dermavant Sciences announced that the company had submitted a supplemental New Drug Application (sNDA) to the Food and Drug Administration for tapinarof cream, 1%, for treating atopic dermatitis (AD) in adults and children 2 years of age and older.
Tapinarof cream, 1%, is an aryl hydrocarbon receptor agonist marketed under the brand name VTAMA that was approved in 2022 for treating plaque psoriasis in adults.
According to a Dermavant press release, the sNDA is based on positive data from the phase 3 ADORING 1 and ADORING 2 pivotal trials and interim results from the phase 3 ADORING 3 open-label, long-term extension 48-week trial. In ADORING 1 and ADORING 2, tapinarof cream demonstrated statistically significant improvements in the primary endpoint of Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) treatment success, defined as a vIGA-AD score of 0 (clear) or 1 (almost clear) with at least a 2-grade improvement from baseline; demonstrated treatment success over vehicle at week 8; and met all key secondary endpoints with statistical significance, according to the company.
The most common adverse reactions in patients treated with VTAMA cream include folliculitis, nasopharyngitis, contact dermatitis, headache, and pruritus.
On February 14, Dermavant Sciences announced that the company had submitted a supplemental New Drug Application (sNDA) to the Food and Drug Administration for tapinarof cream, 1%, for treating atopic dermatitis (AD) in adults and children 2 years of age and older.
Tapinarof cream, 1%, is an aryl hydrocarbon receptor agonist marketed under the brand name VTAMA that was approved in 2022 for treating plaque psoriasis in adults.
According to a Dermavant press release, the sNDA is based on positive data from the phase 3 ADORING 1 and ADORING 2 pivotal trials and interim results from the phase 3 ADORING 3 open-label, long-term extension 48-week trial. In ADORING 1 and ADORING 2, tapinarof cream demonstrated statistically significant improvements in the primary endpoint of Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) treatment success, defined as a vIGA-AD score of 0 (clear) or 1 (almost clear) with at least a 2-grade improvement from baseline; demonstrated treatment success over vehicle at week 8; and met all key secondary endpoints with statistical significance, according to the company.
The most common adverse reactions in patients treated with VTAMA cream include folliculitis, nasopharyngitis, contact dermatitis, headache, and pruritus.
Management of Tinea Capitis in Children Varies, Survey Finds
TOPLINE:
METHODOLOGY:
- The fungal scalp infection tinea capitis affects an estimated 3%-13% of children.
- While international guidelines exist for the treatment of tinea capitis in infants and children, no such document has been developed in the United States.
- Researchers distributed a survey by email to dermatologists through the and the Society for Pediatric Dermatology in the United States, asking about how they treated and managed pediatric patients with tinea capitis; 56 dermatologists participated.
TAKEAWAY:
- Most respondents (88.2%) said they felt comfortable prescribing oral medications prior to confirmation for those aged 2-18 years ( was the most common choice in 60.4% of cases), compared with 81.6% for those aged 2 months to 2 years ( was the most common treatment choice in 41.5% of cases), and 48.7% for those aged 0-2 months ( was the most common choice in 28.6% of cases).
- When asked what topical medication they would start prior to confirmation, most respondents said shampoo (62.3% for those aged 0-2 months and 75.5% each for those aged 2 months to 2 years and those aged 2-18 years), yet between 11.3% and 13% said they would use none.
- The most common form of confirmatory testing was , followed by potassium hydroxide preparation, trichoscopy, and Wood’s lamp.
- More than half of survey respondents would alter their choice of oral medication based on culture results, but most would not change their topical medication preference.
IN PRACTICE:
“The management of tinea capitis in the United States is currently variable, particularly with the introduction of newer antifungals,” the authors wrote. “Future steps involve establishing evidence-based clinical practice guidelines that consider drug efficacy, safety profiles, and costs.”
SOURCE:
Bernard Cohen, MD, of the Departments of Pediatrics and Dermatology at Johns Hopkins University, Baltimore, Maryland, led the research, which was published in Pediatric Dermatology.
LIMITATIONS:
Lower response rates associated with online surveys and predefined age groups restrict the granularity of responses.
DISCLOSURES:
The authors reported having no financial disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The fungal scalp infection tinea capitis affects an estimated 3%-13% of children.
- While international guidelines exist for the treatment of tinea capitis in infants and children, no such document has been developed in the United States.
- Researchers distributed a survey by email to dermatologists through the and the Society for Pediatric Dermatology in the United States, asking about how they treated and managed pediatric patients with tinea capitis; 56 dermatologists participated.
TAKEAWAY:
- Most respondents (88.2%) said they felt comfortable prescribing oral medications prior to confirmation for those aged 2-18 years ( was the most common choice in 60.4% of cases), compared with 81.6% for those aged 2 months to 2 years ( was the most common treatment choice in 41.5% of cases), and 48.7% for those aged 0-2 months ( was the most common choice in 28.6% of cases).
- When asked what topical medication they would start prior to confirmation, most respondents said shampoo (62.3% for those aged 0-2 months and 75.5% each for those aged 2 months to 2 years and those aged 2-18 years), yet between 11.3% and 13% said they would use none.
- The most common form of confirmatory testing was , followed by potassium hydroxide preparation, trichoscopy, and Wood’s lamp.
- More than half of survey respondents would alter their choice of oral medication based on culture results, but most would not change their topical medication preference.
IN PRACTICE:
“The management of tinea capitis in the United States is currently variable, particularly with the introduction of newer antifungals,” the authors wrote. “Future steps involve establishing evidence-based clinical practice guidelines that consider drug efficacy, safety profiles, and costs.”
SOURCE:
Bernard Cohen, MD, of the Departments of Pediatrics and Dermatology at Johns Hopkins University, Baltimore, Maryland, led the research, which was published in Pediatric Dermatology.
LIMITATIONS:
Lower response rates associated with online surveys and predefined age groups restrict the granularity of responses.
DISCLOSURES:
The authors reported having no financial disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The fungal scalp infection tinea capitis affects an estimated 3%-13% of children.
- While international guidelines exist for the treatment of tinea capitis in infants and children, no such document has been developed in the United States.
- Researchers distributed a survey by email to dermatologists through the and the Society for Pediatric Dermatology in the United States, asking about how they treated and managed pediatric patients with tinea capitis; 56 dermatologists participated.
TAKEAWAY:
- Most respondents (88.2%) said they felt comfortable prescribing oral medications prior to confirmation for those aged 2-18 years ( was the most common choice in 60.4% of cases), compared with 81.6% for those aged 2 months to 2 years ( was the most common treatment choice in 41.5% of cases), and 48.7% for those aged 0-2 months ( was the most common choice in 28.6% of cases).
- When asked what topical medication they would start prior to confirmation, most respondents said shampoo (62.3% for those aged 0-2 months and 75.5% each for those aged 2 months to 2 years and those aged 2-18 years), yet between 11.3% and 13% said they would use none.
- The most common form of confirmatory testing was , followed by potassium hydroxide preparation, trichoscopy, and Wood’s lamp.
- More than half of survey respondents would alter their choice of oral medication based on culture results, but most would not change their topical medication preference.
IN PRACTICE:
“The management of tinea capitis in the United States is currently variable, particularly with the introduction of newer antifungals,” the authors wrote. “Future steps involve establishing evidence-based clinical practice guidelines that consider drug efficacy, safety profiles, and costs.”
SOURCE:
Bernard Cohen, MD, of the Departments of Pediatrics and Dermatology at Johns Hopkins University, Baltimore, Maryland, led the research, which was published in Pediatric Dermatology.
LIMITATIONS:
Lower response rates associated with online surveys and predefined age groups restrict the granularity of responses.
DISCLOSURES:
The authors reported having no financial disclosures.
A version of this article appeared on Medscape.com.
Expert Hopes to Expand Ohio Model of Melanoma Case Reporting
SAN DIEGO – Soon after Brett M. Coldiron, MD, launched his Cincinnati-based dermatology and Mohs surgery practice more than 20 years ago, he reported his first three cases of thin melanomas to the Ohio Department of Health, as mandated by state law.
“I got sent reams of paperwork to fill out that I did not understand,” Dr. Coldiron, a past president of the American College of Mohs Surgery and the American Academy of Dermatology, recalled at the annual Cutaneous Malignancy Update. “Then, I got chewed out for not reporting sooner and threatened with thousands of dollars in fines if I did not promptly report the forms in the future. It was an obnoxious experience.”
About 15 years later, while testifying at the Ohio Legislature on medical reasons to restrict the use of tanning beds, a lobbyist for the tanning bed industry told him that the melanoma rates had been stable in Ohio for the previous 5 years. “It turns out they were cherry picking certain segments of data to fit their narrative,” Dr. Coldiron said. “I was stunned and it kind of deflated me. I thought about this for a long time, and thought, ‘how do we solve this issue of reporting melanoma cases without adding work to existing staff if you’re a small practice and without spending significant amounts of money? Let’s make this easier.’ ”
In addition to reducing the use of tanning beds, proper reporting of melanoma cases is important for reasons that include efforts to increase sunscreen use and to be counted in ongoing research efforts to obtain a realistic snapshot of melanoma prevalence and incidence, he said.
Quality of melanoma case reporting relies on the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR), and the National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) Program, which collects data on the incidence, treatment, staging, and survival for 28% of the US population. All 50 states and US territories require melanoma to be reported to the NPCR, but while most hospital systems have reporting protocols and dedicated data registrars, private practices may not.
Also, many dermatopathology practices operate independently and do not have dedicated registrars and may not report cases. “Melanoma is unique in that it is often completely managed in outpatient settings and these melanomas may never be reported,” said Dr. Coldiron, current president of the Ohio Dermatological Foundation. “That’s the practice gap.” One study published in 2018 found that only 49% of dermatologists knew that melanoma was a reportable disease and only 34% routinely reported newly diagnosed cases to their state’s cancer registry. He characterized melanoma reporting as an unfunded mandate.
“Hospitals are doing the most of them, because they have a registrar,” he said. “Small practices have to assign someone to do this, and it can be difficult to train that person. It’s time consuming. The first time we did it, it took an hour,” but, he said, taking a 2-hour tutorial from the Ohio Department of Health helped.
He noted that there is a lack of awareness and clinicians think it’s the dermatopathologist’s job to report cases, “while the dermatopathologist thinks it’s the clinician’s job,” and many of the entry fields are not applicable to thinner melanomas.
There is also a “patchwork” of ways that state departments of health accept the information, not all electronically, he continued. For example, those in Arizona, Montana, West Virginia, Delaware, Vermont, and Maine accept paper copies only, “meaning you have to download a PDF, fill it out, and fax it back to them,” Dr. Coldiron said at the meeting, which was hosted by Scripps Cancer Center.
“We have them sign a HIPAA form and take the two-hour online tutorial,” he said. They download data that Ohio dermatologists have faxed to a dedicated secure HIPAA-compliant cloud-based fax line that Dr. Coldiron has set up, and the cases are then sent to the Ohio Department of Health.
Dr. Coldiron and colleagues have also partnered with the University of Cincinnati Clermont, which offers a National Cancer Registries Association–accredited certificate program — one of several nationwide. Students in this program are trained to become cancer registrars. “The university staff are gung-ho about it because they are looking for easy cases to train the students on. Also, the Ohio Department of Health staff are keen to help train the students and even help them find jobs or hire them after they complete the degree. Staff from the department of health and college faculty are fully engaged and supervising. It’s a win-win for all.”
According to Dr. Coldiron, in 2023, 8 Ohio dermatology practices were sending their reports to the fax line he set up and 7 more have signed up in recent months, making 15 practices to date. “It’s self-perpetuating at this point,” he said. “The Ohio Department of Health and the University of Cincinnati are invested in this program long-term.” The fax service costs Dr. Coldiron $42 per month — a small price to pay, he said, for being a clearinghouse for private Ohio dermatology practices looking for a practical way to report their melanoma cases. The model has increased melanoma reporting in Ohio by 2.8% in the last 2 years, “which doesn’t seem like that many, but if there are 6500 cases of melanoma, and you can increase reporting by a couple hundred cases, that’s a lot,” he said.
His goal is to expand this model to more states. “Dermatologists, surgical oncologists, and cancer center administrators should embrace this opportunity to make their practices a clearinghouse for their state,” he said. “This is an opportunity to improve state health, quality improvement projects, help providers, and gain recognition as a center of excellence. The increase in incidence of melanoma will lend great clout to public and legislative requests for prevention, treatment, and research dollars.”
In an interview, Hugh Greenway, MD, the head of Mohs and dermatologic surgery at Scripps Clinic in San Diego, also noted that cutaneous melanoma is significantly underreported in spite of individual state requirements. “As Dr. Coldiron reminds us, the main reason is that in many cases the pathology diagnosis and report come from the dermatologist’s/dermatopathologist’s office,” Dr. Greenway said. “With no hospital or large multispecialty laboratory involved, the reporting may be incomplete or not done. This is not the case with almost all other cancers where a hospital laboratory is involved.”
If widespread adoption of Dr. Coldiron’s model can occur, he added, “then we will have much better melanoma reporting data on which to both help our patients and specialty. He is to be applauded for producing a workable solution to the problem of underreporting.”
Dr. Coldiron reported having no relevant disclosures. Dr. Greenway reported that he conducts research for Castle Biosciences. He is also course director of the annual Cutaneous Malignancy Update.
SAN DIEGO – Soon after Brett M. Coldiron, MD, launched his Cincinnati-based dermatology and Mohs surgery practice more than 20 years ago, he reported his first three cases of thin melanomas to the Ohio Department of Health, as mandated by state law.
“I got sent reams of paperwork to fill out that I did not understand,” Dr. Coldiron, a past president of the American College of Mohs Surgery and the American Academy of Dermatology, recalled at the annual Cutaneous Malignancy Update. “Then, I got chewed out for not reporting sooner and threatened with thousands of dollars in fines if I did not promptly report the forms in the future. It was an obnoxious experience.”
About 15 years later, while testifying at the Ohio Legislature on medical reasons to restrict the use of tanning beds, a lobbyist for the tanning bed industry told him that the melanoma rates had been stable in Ohio for the previous 5 years. “It turns out they were cherry picking certain segments of data to fit their narrative,” Dr. Coldiron said. “I was stunned and it kind of deflated me. I thought about this for a long time, and thought, ‘how do we solve this issue of reporting melanoma cases without adding work to existing staff if you’re a small practice and without spending significant amounts of money? Let’s make this easier.’ ”
In addition to reducing the use of tanning beds, proper reporting of melanoma cases is important for reasons that include efforts to increase sunscreen use and to be counted in ongoing research efforts to obtain a realistic snapshot of melanoma prevalence and incidence, he said.
Quality of melanoma case reporting relies on the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR), and the National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) Program, which collects data on the incidence, treatment, staging, and survival for 28% of the US population. All 50 states and US territories require melanoma to be reported to the NPCR, but while most hospital systems have reporting protocols and dedicated data registrars, private practices may not.
Also, many dermatopathology practices operate independently and do not have dedicated registrars and may not report cases. “Melanoma is unique in that it is often completely managed in outpatient settings and these melanomas may never be reported,” said Dr. Coldiron, current president of the Ohio Dermatological Foundation. “That’s the practice gap.” One study published in 2018 found that only 49% of dermatologists knew that melanoma was a reportable disease and only 34% routinely reported newly diagnosed cases to their state’s cancer registry. He characterized melanoma reporting as an unfunded mandate.
“Hospitals are doing the most of them, because they have a registrar,” he said. “Small practices have to assign someone to do this, and it can be difficult to train that person. It’s time consuming. The first time we did it, it took an hour,” but, he said, taking a 2-hour tutorial from the Ohio Department of Health helped.
He noted that there is a lack of awareness and clinicians think it’s the dermatopathologist’s job to report cases, “while the dermatopathologist thinks it’s the clinician’s job,” and many of the entry fields are not applicable to thinner melanomas.
There is also a “patchwork” of ways that state departments of health accept the information, not all electronically, he continued. For example, those in Arizona, Montana, West Virginia, Delaware, Vermont, and Maine accept paper copies only, “meaning you have to download a PDF, fill it out, and fax it back to them,” Dr. Coldiron said at the meeting, which was hosted by Scripps Cancer Center.
“We have them sign a HIPAA form and take the two-hour online tutorial,” he said. They download data that Ohio dermatologists have faxed to a dedicated secure HIPAA-compliant cloud-based fax line that Dr. Coldiron has set up, and the cases are then sent to the Ohio Department of Health.
Dr. Coldiron and colleagues have also partnered with the University of Cincinnati Clermont, which offers a National Cancer Registries Association–accredited certificate program — one of several nationwide. Students in this program are trained to become cancer registrars. “The university staff are gung-ho about it because they are looking for easy cases to train the students on. Also, the Ohio Department of Health staff are keen to help train the students and even help them find jobs or hire them after they complete the degree. Staff from the department of health and college faculty are fully engaged and supervising. It’s a win-win for all.”
According to Dr. Coldiron, in 2023, 8 Ohio dermatology practices were sending their reports to the fax line he set up and 7 more have signed up in recent months, making 15 practices to date. “It’s self-perpetuating at this point,” he said. “The Ohio Department of Health and the University of Cincinnati are invested in this program long-term.” The fax service costs Dr. Coldiron $42 per month — a small price to pay, he said, for being a clearinghouse for private Ohio dermatology practices looking for a practical way to report their melanoma cases. The model has increased melanoma reporting in Ohio by 2.8% in the last 2 years, “which doesn’t seem like that many, but if there are 6500 cases of melanoma, and you can increase reporting by a couple hundred cases, that’s a lot,” he said.
His goal is to expand this model to more states. “Dermatologists, surgical oncologists, and cancer center administrators should embrace this opportunity to make their practices a clearinghouse for their state,” he said. “This is an opportunity to improve state health, quality improvement projects, help providers, and gain recognition as a center of excellence. The increase in incidence of melanoma will lend great clout to public and legislative requests for prevention, treatment, and research dollars.”
In an interview, Hugh Greenway, MD, the head of Mohs and dermatologic surgery at Scripps Clinic in San Diego, also noted that cutaneous melanoma is significantly underreported in spite of individual state requirements. “As Dr. Coldiron reminds us, the main reason is that in many cases the pathology diagnosis and report come from the dermatologist’s/dermatopathologist’s office,” Dr. Greenway said. “With no hospital or large multispecialty laboratory involved, the reporting may be incomplete or not done. This is not the case with almost all other cancers where a hospital laboratory is involved.”
If widespread adoption of Dr. Coldiron’s model can occur, he added, “then we will have much better melanoma reporting data on which to both help our patients and specialty. He is to be applauded for producing a workable solution to the problem of underreporting.”
Dr. Coldiron reported having no relevant disclosures. Dr. Greenway reported that he conducts research for Castle Biosciences. He is also course director of the annual Cutaneous Malignancy Update.
SAN DIEGO – Soon after Brett M. Coldiron, MD, launched his Cincinnati-based dermatology and Mohs surgery practice more than 20 years ago, he reported his first three cases of thin melanomas to the Ohio Department of Health, as mandated by state law.
“I got sent reams of paperwork to fill out that I did not understand,” Dr. Coldiron, a past president of the American College of Mohs Surgery and the American Academy of Dermatology, recalled at the annual Cutaneous Malignancy Update. “Then, I got chewed out for not reporting sooner and threatened with thousands of dollars in fines if I did not promptly report the forms in the future. It was an obnoxious experience.”
About 15 years later, while testifying at the Ohio Legislature on medical reasons to restrict the use of tanning beds, a lobbyist for the tanning bed industry told him that the melanoma rates had been stable in Ohio for the previous 5 years. “It turns out they were cherry picking certain segments of data to fit their narrative,” Dr. Coldiron said. “I was stunned and it kind of deflated me. I thought about this for a long time, and thought, ‘how do we solve this issue of reporting melanoma cases without adding work to existing staff if you’re a small practice and without spending significant amounts of money? Let’s make this easier.’ ”
In addition to reducing the use of tanning beds, proper reporting of melanoma cases is important for reasons that include efforts to increase sunscreen use and to be counted in ongoing research efforts to obtain a realistic snapshot of melanoma prevalence and incidence, he said.
Quality of melanoma case reporting relies on the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR), and the National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) Program, which collects data on the incidence, treatment, staging, and survival for 28% of the US population. All 50 states and US territories require melanoma to be reported to the NPCR, but while most hospital systems have reporting protocols and dedicated data registrars, private practices may not.
Also, many dermatopathology practices operate independently and do not have dedicated registrars and may not report cases. “Melanoma is unique in that it is often completely managed in outpatient settings and these melanomas may never be reported,” said Dr. Coldiron, current president of the Ohio Dermatological Foundation. “That’s the practice gap.” One study published in 2018 found that only 49% of dermatologists knew that melanoma was a reportable disease and only 34% routinely reported newly diagnosed cases to their state’s cancer registry. He characterized melanoma reporting as an unfunded mandate.
“Hospitals are doing the most of them, because they have a registrar,” he said. “Small practices have to assign someone to do this, and it can be difficult to train that person. It’s time consuming. The first time we did it, it took an hour,” but, he said, taking a 2-hour tutorial from the Ohio Department of Health helped.
He noted that there is a lack of awareness and clinicians think it’s the dermatopathologist’s job to report cases, “while the dermatopathologist thinks it’s the clinician’s job,” and many of the entry fields are not applicable to thinner melanomas.
There is also a “patchwork” of ways that state departments of health accept the information, not all electronically, he continued. For example, those in Arizona, Montana, West Virginia, Delaware, Vermont, and Maine accept paper copies only, “meaning you have to download a PDF, fill it out, and fax it back to them,” Dr. Coldiron said at the meeting, which was hosted by Scripps Cancer Center.
“We have them sign a HIPAA form and take the two-hour online tutorial,” he said. They download data that Ohio dermatologists have faxed to a dedicated secure HIPAA-compliant cloud-based fax line that Dr. Coldiron has set up, and the cases are then sent to the Ohio Department of Health.
Dr. Coldiron and colleagues have also partnered with the University of Cincinnati Clermont, which offers a National Cancer Registries Association–accredited certificate program — one of several nationwide. Students in this program are trained to become cancer registrars. “The university staff are gung-ho about it because they are looking for easy cases to train the students on. Also, the Ohio Department of Health staff are keen to help train the students and even help them find jobs or hire them after they complete the degree. Staff from the department of health and college faculty are fully engaged and supervising. It’s a win-win for all.”
According to Dr. Coldiron, in 2023, 8 Ohio dermatology practices were sending their reports to the fax line he set up and 7 more have signed up in recent months, making 15 practices to date. “It’s self-perpetuating at this point,” he said. “The Ohio Department of Health and the University of Cincinnati are invested in this program long-term.” The fax service costs Dr. Coldiron $42 per month — a small price to pay, he said, for being a clearinghouse for private Ohio dermatology practices looking for a practical way to report their melanoma cases. The model has increased melanoma reporting in Ohio by 2.8% in the last 2 years, “which doesn’t seem like that many, but if there are 6500 cases of melanoma, and you can increase reporting by a couple hundred cases, that’s a lot,” he said.
His goal is to expand this model to more states. “Dermatologists, surgical oncologists, and cancer center administrators should embrace this opportunity to make their practices a clearinghouse for their state,” he said. “This is an opportunity to improve state health, quality improvement projects, help providers, and gain recognition as a center of excellence. The increase in incidence of melanoma will lend great clout to public and legislative requests for prevention, treatment, and research dollars.”
In an interview, Hugh Greenway, MD, the head of Mohs and dermatologic surgery at Scripps Clinic in San Diego, also noted that cutaneous melanoma is significantly underreported in spite of individual state requirements. “As Dr. Coldiron reminds us, the main reason is that in many cases the pathology diagnosis and report come from the dermatologist’s/dermatopathologist’s office,” Dr. Greenway said. “With no hospital or large multispecialty laboratory involved, the reporting may be incomplete or not done. This is not the case with almost all other cancers where a hospital laboratory is involved.”
If widespread adoption of Dr. Coldiron’s model can occur, he added, “then we will have much better melanoma reporting data on which to both help our patients and specialty. He is to be applauded for producing a workable solution to the problem of underreporting.”
Dr. Coldiron reported having no relevant disclosures. Dr. Greenway reported that he conducts research for Castle Biosciences. He is also course director of the annual Cutaneous Malignancy Update.
FROM MELANOMA 2024
OTC Topical Scar Products May Contain Allergens, Study Finds
TOPLINE:
METHODOLOGY:
- OTC topical scar treatments have the potential to cause an allergic reaction, but the prevalence of North American Contact Dermatitis Group (NACDG) core allergens in these products is unclear.
- Researchers used the word scar in a query of Amazon.com and four other retail websites to identify topical scar products for consumers and noted the list of ingredients.
- The investigators also surveyed the American Contact Dermatitis Society’s Contact Allergen Management Program (CAMP), a resource that helps patients with allergies find personal care products that are safe to use, for pertinent products.
TAKEAWAY:
- The search query identified 156 products. Of these, 119 (76.2%) were gels, creams, or oils and 37 (23.7%) were sheets, strips, or tape.
- Of the 125 products that had a list of ingredients, 69 (55.2%) contained at least one NACDG allergen and 45 (36%) contained more than one.
- The top six most common allergens listed in the ingredients were fragrance (16.8%), phenoxyethanol (16.8%), parabens (14.4%), panthenol (12.8%), sodium benzoate (9.60%), and ethylhexylglycerin (8%).
- Analysis of CAMP revealed that the program only had five unique scar products in its list, suggesting that CAMP might not be a reliable source of scar product information for patients with known allergies to pertinent NACDG allergens.
IN PRACTICE:
“Patients can consider trying a ‘use test’ on the inner forearm before applying to the surgical site,” the authors wrote. “It may reveal they are sensitive or sensitized by a product.
SOURCE:
First author Meera Kattapuram, MD, of the Department of Internal Medicine at Mount Sinai Hospital, New York, led the study, published in the February issue of Dermatologic Surgery.
LIMITATIONS:
Limitations include the selection of five retailers and the top 100 products from each website and the potential for ingredient list inaccuracies.
DISCLOSURES:
The authors reported having no financial conflicts of interest. The research was supported by a grant from the National Institutes of Health/National Cancer Institute.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- OTC topical scar treatments have the potential to cause an allergic reaction, but the prevalence of North American Contact Dermatitis Group (NACDG) core allergens in these products is unclear.
- Researchers used the word scar in a query of Amazon.com and four other retail websites to identify topical scar products for consumers and noted the list of ingredients.
- The investigators also surveyed the American Contact Dermatitis Society’s Contact Allergen Management Program (CAMP), a resource that helps patients with allergies find personal care products that are safe to use, for pertinent products.
TAKEAWAY:
- The search query identified 156 products. Of these, 119 (76.2%) were gels, creams, or oils and 37 (23.7%) were sheets, strips, or tape.
- Of the 125 products that had a list of ingredients, 69 (55.2%) contained at least one NACDG allergen and 45 (36%) contained more than one.
- The top six most common allergens listed in the ingredients were fragrance (16.8%), phenoxyethanol (16.8%), parabens (14.4%), panthenol (12.8%), sodium benzoate (9.60%), and ethylhexylglycerin (8%).
- Analysis of CAMP revealed that the program only had five unique scar products in its list, suggesting that CAMP might not be a reliable source of scar product information for patients with known allergies to pertinent NACDG allergens.
IN PRACTICE:
“Patients can consider trying a ‘use test’ on the inner forearm before applying to the surgical site,” the authors wrote. “It may reveal they are sensitive or sensitized by a product.
SOURCE:
First author Meera Kattapuram, MD, of the Department of Internal Medicine at Mount Sinai Hospital, New York, led the study, published in the February issue of Dermatologic Surgery.
LIMITATIONS:
Limitations include the selection of five retailers and the top 100 products from each website and the potential for ingredient list inaccuracies.
DISCLOSURES:
The authors reported having no financial conflicts of interest. The research was supported by a grant from the National Institutes of Health/National Cancer Institute.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- OTC topical scar treatments have the potential to cause an allergic reaction, but the prevalence of North American Contact Dermatitis Group (NACDG) core allergens in these products is unclear.
- Researchers used the word scar in a query of Amazon.com and four other retail websites to identify topical scar products for consumers and noted the list of ingredients.
- The investigators also surveyed the American Contact Dermatitis Society’s Contact Allergen Management Program (CAMP), a resource that helps patients with allergies find personal care products that are safe to use, for pertinent products.
TAKEAWAY:
- The search query identified 156 products. Of these, 119 (76.2%) were gels, creams, or oils and 37 (23.7%) were sheets, strips, or tape.
- Of the 125 products that had a list of ingredients, 69 (55.2%) contained at least one NACDG allergen and 45 (36%) contained more than one.
- The top six most common allergens listed in the ingredients were fragrance (16.8%), phenoxyethanol (16.8%), parabens (14.4%), panthenol (12.8%), sodium benzoate (9.60%), and ethylhexylglycerin (8%).
- Analysis of CAMP revealed that the program only had five unique scar products in its list, suggesting that CAMP might not be a reliable source of scar product information for patients with known allergies to pertinent NACDG allergens.
IN PRACTICE:
“Patients can consider trying a ‘use test’ on the inner forearm before applying to the surgical site,” the authors wrote. “It may reveal they are sensitive or sensitized by a product.
SOURCE:
First author Meera Kattapuram, MD, of the Department of Internal Medicine at Mount Sinai Hospital, New York, led the study, published in the February issue of Dermatologic Surgery.
LIMITATIONS:
Limitations include the selection of five retailers and the top 100 products from each website and the potential for ingredient list inaccuracies.
DISCLOSURES:
The authors reported having no financial conflicts of interest. The research was supported by a grant from the National Institutes of Health/National Cancer Institute.
A version of this article appeared on Medscape.com.
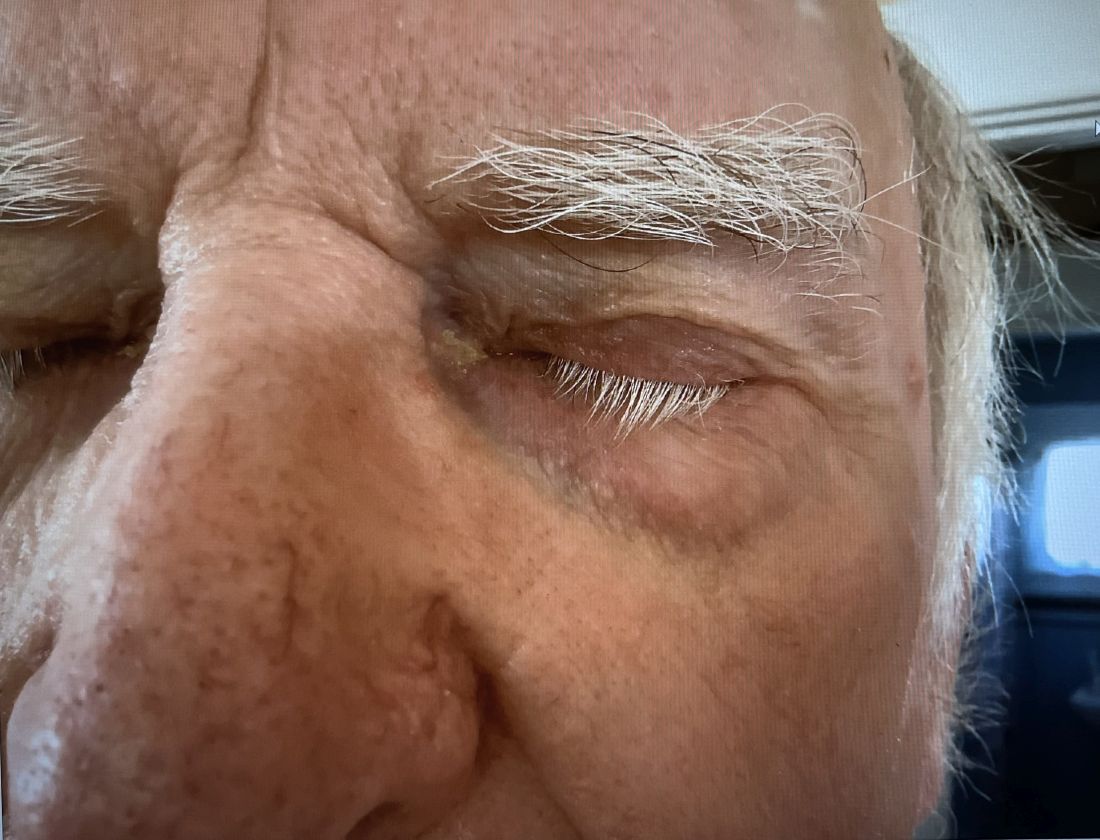
A 74-year-old White male presented with a 1-year history of depigmented patches on the hands, arms, and face, as well as white eyelashes and eyebrows
This patient showed no evidence of recurrence in the scar where the melanoma was excised, and had no enlarged lymph nodes on palpation. His complete blood count and liver function tests were normal. A positron emission tomography (PET) scan was ordered by Dr. Nasser that revealed hypermetabolic right paratracheal, right hilar, and subcarinal lymph nodes, highly suspicious for malignant lymph nodes. The patient was referred to oncology for metastatic melanoma treatment and has been doing well on ipilimumab and nivolumab.
Vitiligo is an autoimmune condition characterized by the progressive destruction of melanocytes resulting in hypopigmentation or depigmentation of the skin. Vitiligo has been associated with cutaneous melanoma. Melanoma-associated leukoderma occurs in a portion of patients with melanoma and is correlated with a favorable prognosis. Additionally, leukoderma has been described as a side effect of melanoma treatment itself. However, cases such as this one have also been reported of vitiligo-like depigmentation presenting prior to the diagnosis of metastatic melanoma.
Melanoma, like vitiligo, is considered highly immunogenic, and cytotoxic T lymphocytes (CTLs) can recognize antigens in melanoma. Furthermore, studies have shown a vitiligo-like halo around melanoma tumors, likely caused by T-cell recruitment, and this may lead to tumor destruction, but rarely total clearance. It seems that the CTL infiltrate in both diseases is similar, but regulatory T cells are decreased in vitiligo, whereas they are present in melanomas and may contribute to the immunosuppressive tumor microenvironment found at the margin of these lesions.
Leukoderma is also associated with melanoma immunotherapy which may be described as drug-induced leukoderma. Additionally, the frequency of recognition of melanoma cells by CTLs leading to hypopigmentation appears to be higher in those with metastatic disease. High immune infiltrate with CTLs and interferon-gamma (IFN-gamma) expression by type 1 T helper cells is associated with favorable prognosis. Immunotherapy with checkpoint inhibitors has shown promise in treatment augmentation for melanoma, but not all patients fully respond to therapy. Nonetheless, development of leukoderma with these treatments has been significantly associated with good therapeutic response. Depigmentation of hair and retinal epithelium has also been reported. However, drug-induced leukoderma and vitiligo seem to have clinical and biological differences, including family history of disease and serum chemokine levels. Vaccines are in production to aid in the treatment of melanoma, but researchers must first identify the appropriate antigen(s) to include.
Conversely, vitiligo-like depigmentation has been reported as a harbinger of metastatic melanoma. Patients with previous excision of primary melanoma have presented months or years later with depigmentation and, upon further evaluation, have been diagnosed with metastatic melanoma. The prevalence of depigmentation in melanoma patients is about 3%-6%, and is estimated to be 7-10 times more common in those with melanoma than in the general population. In most cases, hypopigmentation follows the diagnosis of melanoma, with an average of 4.8 years after the initial diagnosis and 1-2 years after lymph node or distant metastases. It is unclear whether hypopigmentation occurs before or after the growth of metastatic lesions, but this clinical finding in a patient with previous melanoma may serve as an important clue to conduct further investigation for metastasis.
This case and the photos were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Natalie Y. Nasser, MD, Kaiser Permanente Riverside Medical Center; Riverside, California. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
Cerci FB et al. Cutis. 2017 Jun;99(6):E1-E2. PMID: 28686764.
Cho EA et al. Ann Dermatol. 2009 May;21(2):178-181.
Failla CM et al. Int J Mol Sci. 2019 Nov 15;20(22):5731.
This patient showed no evidence of recurrence in the scar where the melanoma was excised, and had no enlarged lymph nodes on palpation. His complete blood count and liver function tests were normal. A positron emission tomography (PET) scan was ordered by Dr. Nasser that revealed hypermetabolic right paratracheal, right hilar, and subcarinal lymph nodes, highly suspicious for malignant lymph nodes. The patient was referred to oncology for metastatic melanoma treatment and has been doing well on ipilimumab and nivolumab.
Vitiligo is an autoimmune condition characterized by the progressive destruction of melanocytes resulting in hypopigmentation or depigmentation of the skin. Vitiligo has been associated with cutaneous melanoma. Melanoma-associated leukoderma occurs in a portion of patients with melanoma and is correlated with a favorable prognosis. Additionally, leukoderma has been described as a side effect of melanoma treatment itself. However, cases such as this one have also been reported of vitiligo-like depigmentation presenting prior to the diagnosis of metastatic melanoma.
Melanoma, like vitiligo, is considered highly immunogenic, and cytotoxic T lymphocytes (CTLs) can recognize antigens in melanoma. Furthermore, studies have shown a vitiligo-like halo around melanoma tumors, likely caused by T-cell recruitment, and this may lead to tumor destruction, but rarely total clearance. It seems that the CTL infiltrate in both diseases is similar, but regulatory T cells are decreased in vitiligo, whereas they are present in melanomas and may contribute to the immunosuppressive tumor microenvironment found at the margin of these lesions.
Leukoderma is also associated with melanoma immunotherapy which may be described as drug-induced leukoderma. Additionally, the frequency of recognition of melanoma cells by CTLs leading to hypopigmentation appears to be higher in those with metastatic disease. High immune infiltrate with CTLs and interferon-gamma (IFN-gamma) expression by type 1 T helper cells is associated with favorable prognosis. Immunotherapy with checkpoint inhibitors has shown promise in treatment augmentation for melanoma, but not all patients fully respond to therapy. Nonetheless, development of leukoderma with these treatments has been significantly associated with good therapeutic response. Depigmentation of hair and retinal epithelium has also been reported. However, drug-induced leukoderma and vitiligo seem to have clinical and biological differences, including family history of disease and serum chemokine levels. Vaccines are in production to aid in the treatment of melanoma, but researchers must first identify the appropriate antigen(s) to include.
Conversely, vitiligo-like depigmentation has been reported as a harbinger of metastatic melanoma. Patients with previous excision of primary melanoma have presented months or years later with depigmentation and, upon further evaluation, have been diagnosed with metastatic melanoma. The prevalence of depigmentation in melanoma patients is about 3%-6%, and is estimated to be 7-10 times more common in those with melanoma than in the general population. In most cases, hypopigmentation follows the diagnosis of melanoma, with an average of 4.8 years after the initial diagnosis and 1-2 years after lymph node or distant metastases. It is unclear whether hypopigmentation occurs before or after the growth of metastatic lesions, but this clinical finding in a patient with previous melanoma may serve as an important clue to conduct further investigation for metastasis.
This case and the photos were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Natalie Y. Nasser, MD, Kaiser Permanente Riverside Medical Center; Riverside, California. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
Cerci FB et al. Cutis. 2017 Jun;99(6):E1-E2. PMID: 28686764.
Cho EA et al. Ann Dermatol. 2009 May;21(2):178-181.
Failla CM et al. Int J Mol Sci. 2019 Nov 15;20(22):5731.
This patient showed no evidence of recurrence in the scar where the melanoma was excised, and had no enlarged lymph nodes on palpation. His complete blood count and liver function tests were normal. A positron emission tomography (PET) scan was ordered by Dr. Nasser that revealed hypermetabolic right paratracheal, right hilar, and subcarinal lymph nodes, highly suspicious for malignant lymph nodes. The patient was referred to oncology for metastatic melanoma treatment and has been doing well on ipilimumab and nivolumab.
Vitiligo is an autoimmune condition characterized by the progressive destruction of melanocytes resulting in hypopigmentation or depigmentation of the skin. Vitiligo has been associated with cutaneous melanoma. Melanoma-associated leukoderma occurs in a portion of patients with melanoma and is correlated with a favorable prognosis. Additionally, leukoderma has been described as a side effect of melanoma treatment itself. However, cases such as this one have also been reported of vitiligo-like depigmentation presenting prior to the diagnosis of metastatic melanoma.
Melanoma, like vitiligo, is considered highly immunogenic, and cytotoxic T lymphocytes (CTLs) can recognize antigens in melanoma. Furthermore, studies have shown a vitiligo-like halo around melanoma tumors, likely caused by T-cell recruitment, and this may lead to tumor destruction, but rarely total clearance. It seems that the CTL infiltrate in both diseases is similar, but regulatory T cells are decreased in vitiligo, whereas they are present in melanomas and may contribute to the immunosuppressive tumor microenvironment found at the margin of these lesions.
Leukoderma is also associated with melanoma immunotherapy which may be described as drug-induced leukoderma. Additionally, the frequency of recognition of melanoma cells by CTLs leading to hypopigmentation appears to be higher in those with metastatic disease. High immune infiltrate with CTLs and interferon-gamma (IFN-gamma) expression by type 1 T helper cells is associated with favorable prognosis. Immunotherapy with checkpoint inhibitors has shown promise in treatment augmentation for melanoma, but not all patients fully respond to therapy. Nonetheless, development of leukoderma with these treatments has been significantly associated with good therapeutic response. Depigmentation of hair and retinal epithelium has also been reported. However, drug-induced leukoderma and vitiligo seem to have clinical and biological differences, including family history of disease and serum chemokine levels. Vaccines are in production to aid in the treatment of melanoma, but researchers must first identify the appropriate antigen(s) to include.
Conversely, vitiligo-like depigmentation has been reported as a harbinger of metastatic melanoma. Patients with previous excision of primary melanoma have presented months or years later with depigmentation and, upon further evaluation, have been diagnosed with metastatic melanoma. The prevalence of depigmentation in melanoma patients is about 3%-6%, and is estimated to be 7-10 times more common in those with melanoma than in the general population. In most cases, hypopigmentation follows the diagnosis of melanoma, with an average of 4.8 years after the initial diagnosis and 1-2 years after lymph node or distant metastases. It is unclear whether hypopigmentation occurs before or after the growth of metastatic lesions, but this clinical finding in a patient with previous melanoma may serve as an important clue to conduct further investigation for metastasis.
This case and the photos were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Natalie Y. Nasser, MD, Kaiser Permanente Riverside Medical Center; Riverside, California. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
Cerci FB et al. Cutis. 2017 Jun;99(6):E1-E2. PMID: 28686764.
Cho EA et al. Ann Dermatol. 2009 May;21(2):178-181.
Failla CM et al. Int J Mol Sci. 2019 Nov 15;20(22):5731.
Oral IL-23 Inhibitor Calms Moderate to Severe Psoriasis
A novel oral drug for plaque psoriasis that targets the same inflammatory pathway as currently available parenteral therapies showed promise for treating moderate to severe disease in a phase 2 dose-finding trial.
Among 255 at week 16 of at least 75% (PASI 75) compared with 9% of patients assigned to placebo, reported Robert Bissonnette, MD, from Innovaderm Research in Montreal, Quebec, Canada, and colleagues.
“The level of reduction of psoriasis that was observed with higher doses of JNJ-77242113 at week 16 was similar in magnitude to the responses seen with several of the injectable biologics that are currently approved for psoriasis,” investigators in the FRONTIER 1 trial wrote in The New England Journal of Medicine.
The investigators noted that among patients assigned to the 100-mg dose of the active drug, 60% had a PASI 90 response, which compares favorably with that seen in phase 3 trials of two other orally available therapies for psoriasis, deucravacitinib (Sotyktu) and apremilast (Otezla). They cautioned, however, against drawing any further inferences from these data, because these agents have not been tested head-to-head against JNJ-77242113 in comparison trials.
Targets IL-23 and IL-17
The investigational agent is an oral IL-23 receptor antagonist peptide that selectively blocks IL-23 proximal signaling as well as the production of downstream inflammatory cytokines such as IL-17, according to the authors.
“Modulation of the interleukin-23 pathway with the use of monoclonal antibodies has shown efficacy in the treatment of psoriasis and is considered to be associated with a more favorable safety profile than older oral therapies (eg, cyclosporine, acitretin, methotrexate, and dimethyl fumarate),” the investigators wrote.
Currently available biologic agents targeting IL-23 include guselkumab (Tremfya), risankizumab (Skyrizi) and tildrakizumab (Ilumya). These agents require intravenous or subcutaneous administration, whereas JNJ-77242113 is taken orally, giving it a theoretical advantage in terms of patient preference.
The novel drug must be taken twice daily on an empty stomach at least 2 hours before food or drink, and those who take it must wait an additional 30 minutes to eat or drink after taking the drug. (This news organization has learned that in planned phase 3 studies, patients will be instructed to take a double daily dose on awakening and then wait 30 minutes for eating or drinking.)
‘Profoundly Effective’
The results of this study have convinced at least one former skeptic of the efficacy of the novel agent.
“They asked me to do the trial, and I turned it down, because I didn’t believe it would work,” said Mark G. Lebwohl, MD, dean for Clinical Therapeutics at the Icahn School of Medicine at Mount Sinai and professor and chairman emeritus of the Department of Dermatology at Mount Sinai Medicine in New York, NY.
In an interview with this news organization, Dr. Lebwohl said that he was initially dubious that a peptide, a short chain of amino acids directed against a receptor, could be effective because it would likely be digested in the intestinal tract.
“Indeed, more than 99% of it is digested, but the data show that the tiny amount that gets through is profoundly effective,” he said.
“I would never have believed that this was going to work – and it did,” Dr. Lebwohl added.
He has signed on as an investigator in the currently recruiting phase 3 ICONIC-LEAD trial, in which JNJ-77242113 will be tested against placebo in adolescents and adults with moderate to severe plaque psoriasis.
In an editorial accompanying the study in the NEJM, Joel M. Gelfand, MD, MSCE, vice chair of clinical research and medical director of the Dermatology Clinical Studies Unit at the University of Pennsylvania in Philadelphia, noted that if confirmed in larger studies, the PASI 90 rate at the highest dose “would be similar to the most effective injectable biologics,” with no evidence of increased adverse events at higher doses.
“However, two occurrences of infection (COVID-19 and an infected cyst) and a suicide attempt were reported as serious adverse events; larger trials will be needed to determine whether such events are attributable to chance, psoriasis itself, or inhibition of interleukin-23 signaling,” cautioned Dr. Gelfand, director of the psoriasis and phototherapy treatment center at the University of Pennsylvania.
In an interview, Dr. Lebwohl said that currently available IL-23 signaling inhibitors have an excellent safety profile and that the investigational oral agent also appears to be very safe. “It’s seeing a target whose effects are known, and the effects are all good and not bad,” he said.
FRONTIER-1 Details
The investigators enrolled eligible adults aged 18 years or older who had moderate to severe plaque psoriasis as defined by an Investigator’s Global Assessment score ≥ 3, a total body-surface area of psoriasis involvement of at least 10%, and a PASI score ≥ 12 who had received their diagnosis of plaque psoriasis at least 6 months before starting the trial. The participants had to be candidates for phototherapy or systemic psoriasis therapy.
Patients were randomly assigned to the active agent at doses of 25 mg once or twice daily, 50 mg once daily, or 100 mg once or twice daily for 16 weeks.
There was a clear dose response, with 37% of patients assigned to 25-mg once-daily dose meeting the primary endpoint of a PASI 75 response at week 16 compared with 51% of those assigned to the 25-mg twice-daily dose, 58% assigned to 50-mg once-daily dose, 65% assigned to 100-mg once-daily dose, and 79% assigned to 100-mg twice-daily dose (P for dose response < .001).
As noted previously, 9% of patients in the placebo group had a PASI 75 response at week 16.
After a mean duration of 15.9 weeks, adverse events after the first dose of JNJ-77242113 (all dose groups were pooled for the safety analysis) were reported in 47% of patients on the 25-mg once-daily dose, 49% on 25-mg twice-daily dose, 60% on 50-mg once-daily dose, 44% on 100-mg once-daily dose, and 62% on 100-mg twice-daily dose. Adverse events after the first dose occurred in 51% of patients assigned to placebo.
The incidence of adverse events did not increase significantly with successively higher dose levels.
As noted by Dr. Gelfand in his editorial, there were three serious adverse events, all occurring in patients on the active drug: a case of COVID-19 in one patient and a suicide attempt in one patient, both in the 100-mg once-daily dose group, and an infected cyst in the 50-mg once-daily group. All three events were determined by the principal investigator and the sponsor to be unrelated to JNJ-77242113.
There were no reports of deaths, major adverse cardiovascular events, or incident cancers during the trial.
The study was supported by Janssen Research and Development. Dr. Bissonnette disclosed institutional research funding and advisory board participation and honoraria with Janssen. Dr. Gelfand disclosed consulting for Janssen Biotech. Dr. Lebwohl disclosed institutional research funding from Janssen but no personal fees.
A version of this article first appeared on Medscape.com.
A novel oral drug for plaque psoriasis that targets the same inflammatory pathway as currently available parenteral therapies showed promise for treating moderate to severe disease in a phase 2 dose-finding trial.
Among 255 at week 16 of at least 75% (PASI 75) compared with 9% of patients assigned to placebo, reported Robert Bissonnette, MD, from Innovaderm Research in Montreal, Quebec, Canada, and colleagues.
“The level of reduction of psoriasis that was observed with higher doses of JNJ-77242113 at week 16 was similar in magnitude to the responses seen with several of the injectable biologics that are currently approved for psoriasis,” investigators in the FRONTIER 1 trial wrote in The New England Journal of Medicine.
The investigators noted that among patients assigned to the 100-mg dose of the active drug, 60% had a PASI 90 response, which compares favorably with that seen in phase 3 trials of two other orally available therapies for psoriasis, deucravacitinib (Sotyktu) and apremilast (Otezla). They cautioned, however, against drawing any further inferences from these data, because these agents have not been tested head-to-head against JNJ-77242113 in comparison trials.
Targets IL-23 and IL-17
The investigational agent is an oral IL-23 receptor antagonist peptide that selectively blocks IL-23 proximal signaling as well as the production of downstream inflammatory cytokines such as IL-17, according to the authors.
“Modulation of the interleukin-23 pathway with the use of monoclonal antibodies has shown efficacy in the treatment of psoriasis and is considered to be associated with a more favorable safety profile than older oral therapies (eg, cyclosporine, acitretin, methotrexate, and dimethyl fumarate),” the investigators wrote.
Currently available biologic agents targeting IL-23 include guselkumab (Tremfya), risankizumab (Skyrizi) and tildrakizumab (Ilumya). These agents require intravenous or subcutaneous administration, whereas JNJ-77242113 is taken orally, giving it a theoretical advantage in terms of patient preference.
The novel drug must be taken twice daily on an empty stomach at least 2 hours before food or drink, and those who take it must wait an additional 30 minutes to eat or drink after taking the drug. (This news organization has learned that in planned phase 3 studies, patients will be instructed to take a double daily dose on awakening and then wait 30 minutes for eating or drinking.)
‘Profoundly Effective’
The results of this study have convinced at least one former skeptic of the efficacy of the novel agent.
“They asked me to do the trial, and I turned it down, because I didn’t believe it would work,” said Mark G. Lebwohl, MD, dean for Clinical Therapeutics at the Icahn School of Medicine at Mount Sinai and professor and chairman emeritus of the Department of Dermatology at Mount Sinai Medicine in New York, NY.
In an interview with this news organization, Dr. Lebwohl said that he was initially dubious that a peptide, a short chain of amino acids directed against a receptor, could be effective because it would likely be digested in the intestinal tract.
“Indeed, more than 99% of it is digested, but the data show that the tiny amount that gets through is profoundly effective,” he said.
“I would never have believed that this was going to work – and it did,” Dr. Lebwohl added.
He has signed on as an investigator in the currently recruiting phase 3 ICONIC-LEAD trial, in which JNJ-77242113 will be tested against placebo in adolescents and adults with moderate to severe plaque psoriasis.
In an editorial accompanying the study in the NEJM, Joel M. Gelfand, MD, MSCE, vice chair of clinical research and medical director of the Dermatology Clinical Studies Unit at the University of Pennsylvania in Philadelphia, noted that if confirmed in larger studies, the PASI 90 rate at the highest dose “would be similar to the most effective injectable biologics,” with no evidence of increased adverse events at higher doses.
“However, two occurrences of infection (COVID-19 and an infected cyst) and a suicide attempt were reported as serious adverse events; larger trials will be needed to determine whether such events are attributable to chance, psoriasis itself, or inhibition of interleukin-23 signaling,” cautioned Dr. Gelfand, director of the psoriasis and phototherapy treatment center at the University of Pennsylvania.
In an interview, Dr. Lebwohl said that currently available IL-23 signaling inhibitors have an excellent safety profile and that the investigational oral agent also appears to be very safe. “It’s seeing a target whose effects are known, and the effects are all good and not bad,” he said.
FRONTIER-1 Details
The investigators enrolled eligible adults aged 18 years or older who had moderate to severe plaque psoriasis as defined by an Investigator’s Global Assessment score ≥ 3, a total body-surface area of psoriasis involvement of at least 10%, and a PASI score ≥ 12 who had received their diagnosis of plaque psoriasis at least 6 months before starting the trial. The participants had to be candidates for phototherapy or systemic psoriasis therapy.
Patients were randomly assigned to the active agent at doses of 25 mg once or twice daily, 50 mg once daily, or 100 mg once or twice daily for 16 weeks.
There was a clear dose response, with 37% of patients assigned to 25-mg once-daily dose meeting the primary endpoint of a PASI 75 response at week 16 compared with 51% of those assigned to the 25-mg twice-daily dose, 58% assigned to 50-mg once-daily dose, 65% assigned to 100-mg once-daily dose, and 79% assigned to 100-mg twice-daily dose (P for dose response < .001).
As noted previously, 9% of patients in the placebo group had a PASI 75 response at week 16.
After a mean duration of 15.9 weeks, adverse events after the first dose of JNJ-77242113 (all dose groups were pooled for the safety analysis) were reported in 47% of patients on the 25-mg once-daily dose, 49% on 25-mg twice-daily dose, 60% on 50-mg once-daily dose, 44% on 100-mg once-daily dose, and 62% on 100-mg twice-daily dose. Adverse events after the first dose occurred in 51% of patients assigned to placebo.
The incidence of adverse events did not increase significantly with successively higher dose levels.
As noted by Dr. Gelfand in his editorial, there were three serious adverse events, all occurring in patients on the active drug: a case of COVID-19 in one patient and a suicide attempt in one patient, both in the 100-mg once-daily dose group, and an infected cyst in the 50-mg once-daily group. All three events were determined by the principal investigator and the sponsor to be unrelated to JNJ-77242113.
There were no reports of deaths, major adverse cardiovascular events, or incident cancers during the trial.
The study was supported by Janssen Research and Development. Dr. Bissonnette disclosed institutional research funding and advisory board participation and honoraria with Janssen. Dr. Gelfand disclosed consulting for Janssen Biotech. Dr. Lebwohl disclosed institutional research funding from Janssen but no personal fees.
A version of this article first appeared on Medscape.com.
A novel oral drug for plaque psoriasis that targets the same inflammatory pathway as currently available parenteral therapies showed promise for treating moderate to severe disease in a phase 2 dose-finding trial.
Among 255 at week 16 of at least 75% (PASI 75) compared with 9% of patients assigned to placebo, reported Robert Bissonnette, MD, from Innovaderm Research in Montreal, Quebec, Canada, and colleagues.
“The level of reduction of psoriasis that was observed with higher doses of JNJ-77242113 at week 16 was similar in magnitude to the responses seen with several of the injectable biologics that are currently approved for psoriasis,” investigators in the FRONTIER 1 trial wrote in The New England Journal of Medicine.
The investigators noted that among patients assigned to the 100-mg dose of the active drug, 60% had a PASI 90 response, which compares favorably with that seen in phase 3 trials of two other orally available therapies for psoriasis, deucravacitinib (Sotyktu) and apremilast (Otezla). They cautioned, however, against drawing any further inferences from these data, because these agents have not been tested head-to-head against JNJ-77242113 in comparison trials.
Targets IL-23 and IL-17
The investigational agent is an oral IL-23 receptor antagonist peptide that selectively blocks IL-23 proximal signaling as well as the production of downstream inflammatory cytokines such as IL-17, according to the authors.
“Modulation of the interleukin-23 pathway with the use of monoclonal antibodies has shown efficacy in the treatment of psoriasis and is considered to be associated with a more favorable safety profile than older oral therapies (eg, cyclosporine, acitretin, methotrexate, and dimethyl fumarate),” the investigators wrote.
Currently available biologic agents targeting IL-23 include guselkumab (Tremfya), risankizumab (Skyrizi) and tildrakizumab (Ilumya). These agents require intravenous or subcutaneous administration, whereas JNJ-77242113 is taken orally, giving it a theoretical advantage in terms of patient preference.
The novel drug must be taken twice daily on an empty stomach at least 2 hours before food or drink, and those who take it must wait an additional 30 minutes to eat or drink after taking the drug. (This news organization has learned that in planned phase 3 studies, patients will be instructed to take a double daily dose on awakening and then wait 30 minutes for eating or drinking.)
‘Profoundly Effective’
The results of this study have convinced at least one former skeptic of the efficacy of the novel agent.
“They asked me to do the trial, and I turned it down, because I didn’t believe it would work,” said Mark G. Lebwohl, MD, dean for Clinical Therapeutics at the Icahn School of Medicine at Mount Sinai and professor and chairman emeritus of the Department of Dermatology at Mount Sinai Medicine in New York, NY.
In an interview with this news organization, Dr. Lebwohl said that he was initially dubious that a peptide, a short chain of amino acids directed against a receptor, could be effective because it would likely be digested in the intestinal tract.
“Indeed, more than 99% of it is digested, but the data show that the tiny amount that gets through is profoundly effective,” he said.
“I would never have believed that this was going to work – and it did,” Dr. Lebwohl added.
He has signed on as an investigator in the currently recruiting phase 3 ICONIC-LEAD trial, in which JNJ-77242113 will be tested against placebo in adolescents and adults with moderate to severe plaque psoriasis.
In an editorial accompanying the study in the NEJM, Joel M. Gelfand, MD, MSCE, vice chair of clinical research and medical director of the Dermatology Clinical Studies Unit at the University of Pennsylvania in Philadelphia, noted that if confirmed in larger studies, the PASI 90 rate at the highest dose “would be similar to the most effective injectable biologics,” with no evidence of increased adverse events at higher doses.
“However, two occurrences of infection (COVID-19 and an infected cyst) and a suicide attempt were reported as serious adverse events; larger trials will be needed to determine whether such events are attributable to chance, psoriasis itself, or inhibition of interleukin-23 signaling,” cautioned Dr. Gelfand, director of the psoriasis and phototherapy treatment center at the University of Pennsylvania.
In an interview, Dr. Lebwohl said that currently available IL-23 signaling inhibitors have an excellent safety profile and that the investigational oral agent also appears to be very safe. “It’s seeing a target whose effects are known, and the effects are all good and not bad,” he said.
FRONTIER-1 Details
The investigators enrolled eligible adults aged 18 years or older who had moderate to severe plaque psoriasis as defined by an Investigator’s Global Assessment score ≥ 3, a total body-surface area of psoriasis involvement of at least 10%, and a PASI score ≥ 12 who had received their diagnosis of plaque psoriasis at least 6 months before starting the trial. The participants had to be candidates for phototherapy or systemic psoriasis therapy.
Patients were randomly assigned to the active agent at doses of 25 mg once or twice daily, 50 mg once daily, or 100 mg once or twice daily for 16 weeks.
There was a clear dose response, with 37% of patients assigned to 25-mg once-daily dose meeting the primary endpoint of a PASI 75 response at week 16 compared with 51% of those assigned to the 25-mg twice-daily dose, 58% assigned to 50-mg once-daily dose, 65% assigned to 100-mg once-daily dose, and 79% assigned to 100-mg twice-daily dose (P for dose response < .001).
As noted previously, 9% of patients in the placebo group had a PASI 75 response at week 16.
After a mean duration of 15.9 weeks, adverse events after the first dose of JNJ-77242113 (all dose groups were pooled for the safety analysis) were reported in 47% of patients on the 25-mg once-daily dose, 49% on 25-mg twice-daily dose, 60% on 50-mg once-daily dose, 44% on 100-mg once-daily dose, and 62% on 100-mg twice-daily dose. Adverse events after the first dose occurred in 51% of patients assigned to placebo.
The incidence of adverse events did not increase significantly with successively higher dose levels.
As noted by Dr. Gelfand in his editorial, there were three serious adverse events, all occurring in patients on the active drug: a case of COVID-19 in one patient and a suicide attempt in one patient, both in the 100-mg once-daily dose group, and an infected cyst in the 50-mg once-daily group. All three events were determined by the principal investigator and the sponsor to be unrelated to JNJ-77242113.
There were no reports of deaths, major adverse cardiovascular events, or incident cancers during the trial.
The study was supported by Janssen Research and Development. Dr. Bissonnette disclosed institutional research funding and advisory board participation and honoraria with Janssen. Dr. Gelfand disclosed consulting for Janssen Biotech. Dr. Lebwohl disclosed institutional research funding from Janssen but no personal fees.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Study: Lifetime Cost of Vyjuvek Gene Therapy for DEB Could Be $15-$22 Million
according to the authors of a new study.
The US Food and Drug Administration (FDA) approved Vyjuvek (Krystal Biotech) in May 2023 for the treatment of wounds in patients ages 6 months and older with dystrophic epidermolysis bullosa (DEB), which includes two types, the most severe form (autosomal recessive, or RDEB) and the autosomal dominant form of DEB (DDEB), which tends to be milder.
Treatment with Vyjuvek “represents an important advance in the treatment of RDEB,” wrote Adam J.N. Raymakers, PhD, and colleagues at the Program on Regulation, Therapeutics, and Law; the Department of Dermatology; and the Division of Pulmonary and Critical Care Medicine at Brigham & Women’s Hospital in Boston, Massachusetts, in their paper, published in JAMA Dermatology. But the price “will be high, potentially limiting patients’ access to it,” they added. Evidence to support it in DDEB “is less conclusive,” they wrote, noting that the pivotal phase 3 study that led to approval included one patient with DDEB.
“The wider indication granted by the FDA may lead to friction between payers on the one hand and patients and physicians on the other,” they wrote, noting a potential minimum price of $300,000 per patient a year, which was based on Krystal’s regulatory filings.
There is no cure for DEB. Vyjuvek, applied as a gel on an ongoing basis, uses a nonreplicating herpes simplex virus type 1 vector to deliver the COL7A1 gene directly to skin cells, restoring the COL7 protein fibrils that stabilize skin structure.
The authors estimated that in the United States, 894 individuals – largely children – with both forms of the disease would be eligible for Vyjuvek treatment in the first year. Based on the $300,000 price, spending on gene therapy could range from $179 million to $357 million for those 894 patients, they reported in the study.
Over the first 3 years, spending could range as high as $1 billion, the authors estimated. Even if patients with only the most severe disease (RDEB) — an estimated 442 patients — received treatment, spending could be $132 million and up to $400 million or more over the first 3 years, they wrote.
Some media outlets have reported that Vyjuvek could cost as much as $600,000, said Dr. Raymakers, a research fellow. That price “would double all of our estimates,” he told this news organization.
The study assumed that patients with RDEB would only live to age 50, which led to a lifetime cost estimate of $15 million. But that is likely a conservative estimate, he and his coauthors wrote, noting that many patients with RDEB die from squamous cell carcinoma, but that Vyjuvek could, by attenuating skin damage, also potentially prevent skin cancer.
Dr. Raymakers said he and his colleagues began their study when Vyjuvek was approved, and thus they did not have any real-world data on the price or payer responses. Their estimates also did not include differing dosing regimens, which also could change their spending figures.
Krystal Biotech recently reported that in its third quarter of 2023 – representing just 1 month of Vyjuvek availability – it received requests to begin treatment for 284 patients from 136 unique clinicians. Twenty percent of the start requests were for patients with the milder form (DDEB), and a third of all the requests were for patients 10 years of age or younger. The company also said that it had “received positive coverage determinations from all major commercial national health plans” and that it was on track to receive approval from most state Medicaid plans.
In 1 month, Krystal reported net Vyjuvek revenues of $8.6 million.
The authors suggested that one way to evaluate Vyjuvek’s value — especially for those with DDEB — would be through a cost-effectiveness study. While important, a cost-effectiveness study would not get at the impact on a payer, said Dr. Raymakers. “Something can be cost-effective but unaffordable to the system,” he said.
“When there’s one of these very expensive therapies, that’s one thing,” he said. “But when there’s more and more coming to market, you wonder how much can be tolerated,” said Dr. Raymakers.
CMS Launching Gene Therapy Program
The Biden administration recently announced that it was launching a program aimed at increasing access, curbing costs, and ensuring value of gene therapies, starting with sickle cell disease. The program will begin in early 2025. Among other aspects, the federal government will negotiate the price of the product with the manufacturer.
“The goal of the Cell and Gene Therapy Access Model is to increase access to innovative cell and gene therapies for people with Medicaid by making it easier for states to pay for these therapies,” said Liz Fowler, CMS Deputy Administrator and Director of the CMS Innovation Center, in a statement announcing the program.
Whether the new program takes a look at Vyjuvek – and when – is not clear.
But the authors of the study noted that the lifetime costs of treating a patient with Vyjuvek “exceed the costs of all other one-time gene therapies for other diseases.” And they wrote, even at the most conservative estimates, Vyjuvek “will be the most expensive gene therapy currently marketed in the US.”
The study was funded by a grant from Arnold Ventures, grants from the Kaiser Permanente Institute for Health Policy, the Commonwealth Fund, and the National Heart, Lung, and Blood Institute. Dr. Raymakers and co-authors reported no financial relationships relevant to the work.
according to the authors of a new study.
The US Food and Drug Administration (FDA) approved Vyjuvek (Krystal Biotech) in May 2023 for the treatment of wounds in patients ages 6 months and older with dystrophic epidermolysis bullosa (DEB), which includes two types, the most severe form (autosomal recessive, or RDEB) and the autosomal dominant form of DEB (DDEB), which tends to be milder.
Treatment with Vyjuvek “represents an important advance in the treatment of RDEB,” wrote Adam J.N. Raymakers, PhD, and colleagues at the Program on Regulation, Therapeutics, and Law; the Department of Dermatology; and the Division of Pulmonary and Critical Care Medicine at Brigham & Women’s Hospital in Boston, Massachusetts, in their paper, published in JAMA Dermatology. But the price “will be high, potentially limiting patients’ access to it,” they added. Evidence to support it in DDEB “is less conclusive,” they wrote, noting that the pivotal phase 3 study that led to approval included one patient with DDEB.
“The wider indication granted by the FDA may lead to friction between payers on the one hand and patients and physicians on the other,” they wrote, noting a potential minimum price of $300,000 per patient a year, which was based on Krystal’s regulatory filings.
There is no cure for DEB. Vyjuvek, applied as a gel on an ongoing basis, uses a nonreplicating herpes simplex virus type 1 vector to deliver the COL7A1 gene directly to skin cells, restoring the COL7 protein fibrils that stabilize skin structure.
The authors estimated that in the United States, 894 individuals – largely children – with both forms of the disease would be eligible for Vyjuvek treatment in the first year. Based on the $300,000 price, spending on gene therapy could range from $179 million to $357 million for those 894 patients, they reported in the study.
Over the first 3 years, spending could range as high as $1 billion, the authors estimated. Even if patients with only the most severe disease (RDEB) — an estimated 442 patients — received treatment, spending could be $132 million and up to $400 million or more over the first 3 years, they wrote.
Some media outlets have reported that Vyjuvek could cost as much as $600,000, said Dr. Raymakers, a research fellow. That price “would double all of our estimates,” he told this news organization.
The study assumed that patients with RDEB would only live to age 50, which led to a lifetime cost estimate of $15 million. But that is likely a conservative estimate, he and his coauthors wrote, noting that many patients with RDEB die from squamous cell carcinoma, but that Vyjuvek could, by attenuating skin damage, also potentially prevent skin cancer.
Dr. Raymakers said he and his colleagues began their study when Vyjuvek was approved, and thus they did not have any real-world data on the price or payer responses. Their estimates also did not include differing dosing regimens, which also could change their spending figures.
Krystal Biotech recently reported that in its third quarter of 2023 – representing just 1 month of Vyjuvek availability – it received requests to begin treatment for 284 patients from 136 unique clinicians. Twenty percent of the start requests were for patients with the milder form (DDEB), and a third of all the requests were for patients 10 years of age or younger. The company also said that it had “received positive coverage determinations from all major commercial national health plans” and that it was on track to receive approval from most state Medicaid plans.
In 1 month, Krystal reported net Vyjuvek revenues of $8.6 million.
The authors suggested that one way to evaluate Vyjuvek’s value — especially for those with DDEB — would be through a cost-effectiveness study. While important, a cost-effectiveness study would not get at the impact on a payer, said Dr. Raymakers. “Something can be cost-effective but unaffordable to the system,” he said.
“When there’s one of these very expensive therapies, that’s one thing,” he said. “But when there’s more and more coming to market, you wonder how much can be tolerated,” said Dr. Raymakers.
CMS Launching Gene Therapy Program
The Biden administration recently announced that it was launching a program aimed at increasing access, curbing costs, and ensuring value of gene therapies, starting with sickle cell disease. The program will begin in early 2025. Among other aspects, the federal government will negotiate the price of the product with the manufacturer.
“The goal of the Cell and Gene Therapy Access Model is to increase access to innovative cell and gene therapies for people with Medicaid by making it easier for states to pay for these therapies,” said Liz Fowler, CMS Deputy Administrator and Director of the CMS Innovation Center, in a statement announcing the program.
Whether the new program takes a look at Vyjuvek – and when – is not clear.
But the authors of the study noted that the lifetime costs of treating a patient with Vyjuvek “exceed the costs of all other one-time gene therapies for other diseases.” And they wrote, even at the most conservative estimates, Vyjuvek “will be the most expensive gene therapy currently marketed in the US.”
The study was funded by a grant from Arnold Ventures, grants from the Kaiser Permanente Institute for Health Policy, the Commonwealth Fund, and the National Heart, Lung, and Blood Institute. Dr. Raymakers and co-authors reported no financial relationships relevant to the work.
according to the authors of a new study.
The US Food and Drug Administration (FDA) approved Vyjuvek (Krystal Biotech) in May 2023 for the treatment of wounds in patients ages 6 months and older with dystrophic epidermolysis bullosa (DEB), which includes two types, the most severe form (autosomal recessive, or RDEB) and the autosomal dominant form of DEB (DDEB), which tends to be milder.
Treatment with Vyjuvek “represents an important advance in the treatment of RDEB,” wrote Adam J.N. Raymakers, PhD, and colleagues at the Program on Regulation, Therapeutics, and Law; the Department of Dermatology; and the Division of Pulmonary and Critical Care Medicine at Brigham & Women’s Hospital in Boston, Massachusetts, in their paper, published in JAMA Dermatology. But the price “will be high, potentially limiting patients’ access to it,” they added. Evidence to support it in DDEB “is less conclusive,” they wrote, noting that the pivotal phase 3 study that led to approval included one patient with DDEB.
“The wider indication granted by the FDA may lead to friction between payers on the one hand and patients and physicians on the other,” they wrote, noting a potential minimum price of $300,000 per patient a year, which was based on Krystal’s regulatory filings.
There is no cure for DEB. Vyjuvek, applied as a gel on an ongoing basis, uses a nonreplicating herpes simplex virus type 1 vector to deliver the COL7A1 gene directly to skin cells, restoring the COL7 protein fibrils that stabilize skin structure.
The authors estimated that in the United States, 894 individuals – largely children – with both forms of the disease would be eligible for Vyjuvek treatment in the first year. Based on the $300,000 price, spending on gene therapy could range from $179 million to $357 million for those 894 patients, they reported in the study.
Over the first 3 years, spending could range as high as $1 billion, the authors estimated. Even if patients with only the most severe disease (RDEB) — an estimated 442 patients — received treatment, spending could be $132 million and up to $400 million or more over the first 3 years, they wrote.
Some media outlets have reported that Vyjuvek could cost as much as $600,000, said Dr. Raymakers, a research fellow. That price “would double all of our estimates,” he told this news organization.
The study assumed that patients with RDEB would only live to age 50, which led to a lifetime cost estimate of $15 million. But that is likely a conservative estimate, he and his coauthors wrote, noting that many patients with RDEB die from squamous cell carcinoma, but that Vyjuvek could, by attenuating skin damage, also potentially prevent skin cancer.
Dr. Raymakers said he and his colleagues began their study when Vyjuvek was approved, and thus they did not have any real-world data on the price or payer responses. Their estimates also did not include differing dosing regimens, which also could change their spending figures.
Krystal Biotech recently reported that in its third quarter of 2023 – representing just 1 month of Vyjuvek availability – it received requests to begin treatment for 284 patients from 136 unique clinicians. Twenty percent of the start requests were for patients with the milder form (DDEB), and a third of all the requests were for patients 10 years of age or younger. The company also said that it had “received positive coverage determinations from all major commercial national health plans” and that it was on track to receive approval from most state Medicaid plans.
In 1 month, Krystal reported net Vyjuvek revenues of $8.6 million.
The authors suggested that one way to evaluate Vyjuvek’s value — especially for those with DDEB — would be through a cost-effectiveness study. While important, a cost-effectiveness study would not get at the impact on a payer, said Dr. Raymakers. “Something can be cost-effective but unaffordable to the system,” he said.
“When there’s one of these very expensive therapies, that’s one thing,” he said. “But when there’s more and more coming to market, you wonder how much can be tolerated,” said Dr. Raymakers.
CMS Launching Gene Therapy Program
The Biden administration recently announced that it was launching a program aimed at increasing access, curbing costs, and ensuring value of gene therapies, starting with sickle cell disease. The program will begin in early 2025. Among other aspects, the federal government will negotiate the price of the product with the manufacturer.
“The goal of the Cell and Gene Therapy Access Model is to increase access to innovative cell and gene therapies for people with Medicaid by making it easier for states to pay for these therapies,” said Liz Fowler, CMS Deputy Administrator and Director of the CMS Innovation Center, in a statement announcing the program.
Whether the new program takes a look at Vyjuvek – and when – is not clear.
But the authors of the study noted that the lifetime costs of treating a patient with Vyjuvek “exceed the costs of all other one-time gene therapies for other diseases.” And they wrote, even at the most conservative estimates, Vyjuvek “will be the most expensive gene therapy currently marketed in the US.”
The study was funded by a grant from Arnold Ventures, grants from the Kaiser Permanente Institute for Health Policy, the Commonwealth Fund, and the National Heart, Lung, and Blood Institute. Dr. Raymakers and co-authors reported no financial relationships relevant to the work.
FROM JAMA DERMATOLOGY
Dupilumab Improves AD Affecting the Hands, Feet
TOPLINE:
compared with placebo.
METHODOLOGY:
- The multinational phase 3 LIBERTY-AD-HAFT trial of adults and adolescents with moderate to severe chronic atopic dermatitis (AD) of the hands, feet, or both included 67 participants at 48 sites randomized to dupilumab monotherapy and 66 to placebo.
- The primary endpoint was the proportion of patients scoring 0 or 1 on Hand and Foot Investigator’s Global Assessment (HF-IGA) at week 16.
- Secondary endpoints were severity and extent of signs, symptom intensity (itch and pain), sleep, and quality of life.
TAKEAWAY:
- At week 16, 27 patients receiving dupilumab vs 11 receiving placebo achieved an HF-IGA score of 0 or 1 (40.3% vs 16.7%; P = .003).
- At week 16, 35 participants receiving dupilumab vs nine receiving placebo improved at least four points in the weekly average of daily HF-Peak Pruritus Numeric Rating Scale (52.2% vs 13.6%; P < .0001).
- At week 16, Quality of Life Hand Eczema Questionnaire results improved in the dupilumab group compared with controls (P < .0001), and weekly average of daily Sleep Numeric Rating Scale results improved in the dupilumab group compared with controls (P < .05).
- The safety profile was similar to the known profile in adults and adolescents with moderate to severe AD.
IN PRACTICE:
The results of the study “support dupilumab” as an “efficacious systemic therapy for moderate to severe H/F AD,” the authors wrote.
SOURCE:
The study, led by Eric L. Simpson, MD, MCR, professor of dermatology at the Oregon Health & Science University in Portland, was published on January 29, 2024, in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The short duration of the study and the large proportion of patients with positive patch tests (31 of 133) suggested that some participants may have had concurrent AD and allergic contact dermatitis, so the effect of dupilumab on those patients needs further evaluation.
DISCLOSURES:
The study was sponsored by Sanofi and Regeneron. All but one author had financial relationships with Sanofi, Regeneron, or both. Several authors were employees of, and may hold stocks or stock options in, Sanofi or Regeneron.
TOPLINE:
compared with placebo.
METHODOLOGY:
- The multinational phase 3 LIBERTY-AD-HAFT trial of adults and adolescents with moderate to severe chronic atopic dermatitis (AD) of the hands, feet, or both included 67 participants at 48 sites randomized to dupilumab monotherapy and 66 to placebo.
- The primary endpoint was the proportion of patients scoring 0 or 1 on Hand and Foot Investigator’s Global Assessment (HF-IGA) at week 16.
- Secondary endpoints were severity and extent of signs, symptom intensity (itch and pain), sleep, and quality of life.
TAKEAWAY:
- At week 16, 27 patients receiving dupilumab vs 11 receiving placebo achieved an HF-IGA score of 0 or 1 (40.3% vs 16.7%; P = .003).
- At week 16, 35 participants receiving dupilumab vs nine receiving placebo improved at least four points in the weekly average of daily HF-Peak Pruritus Numeric Rating Scale (52.2% vs 13.6%; P < .0001).
- At week 16, Quality of Life Hand Eczema Questionnaire results improved in the dupilumab group compared with controls (P < .0001), and weekly average of daily Sleep Numeric Rating Scale results improved in the dupilumab group compared with controls (P < .05).
- The safety profile was similar to the known profile in adults and adolescents with moderate to severe AD.
IN PRACTICE:
The results of the study “support dupilumab” as an “efficacious systemic therapy for moderate to severe H/F AD,” the authors wrote.
SOURCE:
The study, led by Eric L. Simpson, MD, MCR, professor of dermatology at the Oregon Health & Science University in Portland, was published on January 29, 2024, in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The short duration of the study and the large proportion of patients with positive patch tests (31 of 133) suggested that some participants may have had concurrent AD and allergic contact dermatitis, so the effect of dupilumab on those patients needs further evaluation.
DISCLOSURES:
The study was sponsored by Sanofi and Regeneron. All but one author had financial relationships with Sanofi, Regeneron, or both. Several authors were employees of, and may hold stocks or stock options in, Sanofi or Regeneron.
TOPLINE:
compared with placebo.
METHODOLOGY:
- The multinational phase 3 LIBERTY-AD-HAFT trial of adults and adolescents with moderate to severe chronic atopic dermatitis (AD) of the hands, feet, or both included 67 participants at 48 sites randomized to dupilumab monotherapy and 66 to placebo.
- The primary endpoint was the proportion of patients scoring 0 or 1 on Hand and Foot Investigator’s Global Assessment (HF-IGA) at week 16.
- Secondary endpoints were severity and extent of signs, symptom intensity (itch and pain), sleep, and quality of life.
TAKEAWAY:
- At week 16, 27 patients receiving dupilumab vs 11 receiving placebo achieved an HF-IGA score of 0 or 1 (40.3% vs 16.7%; P = .003).
- At week 16, 35 participants receiving dupilumab vs nine receiving placebo improved at least four points in the weekly average of daily HF-Peak Pruritus Numeric Rating Scale (52.2% vs 13.6%; P < .0001).
- At week 16, Quality of Life Hand Eczema Questionnaire results improved in the dupilumab group compared with controls (P < .0001), and weekly average of daily Sleep Numeric Rating Scale results improved in the dupilumab group compared with controls (P < .05).
- The safety profile was similar to the known profile in adults and adolescents with moderate to severe AD.
IN PRACTICE:
The results of the study “support dupilumab” as an “efficacious systemic therapy for moderate to severe H/F AD,” the authors wrote.
SOURCE:
The study, led by Eric L. Simpson, MD, MCR, professor of dermatology at the Oregon Health & Science University in Portland, was published on January 29, 2024, in the Journal of the American Academy of Dermatology.
LIMITATIONS:
The short duration of the study and the large proportion of patients with positive patch tests (31 of 133) suggested that some participants may have had concurrent AD and allergic contact dermatitis, so the effect of dupilumab on those patients needs further evaluation.
DISCLOSURES:
The study was sponsored by Sanofi and Regeneron. All but one author had financial relationships with Sanofi, Regeneron, or both. Several authors were employees of, and may hold stocks or stock options in, Sanofi or Regeneron.
Survey: Dermatology Residents Shortchanged on Sensitive Skin Education
Although sensitive skin affects an estimated 40%-70% of the population, knowledge of the pathophysiology of sensitive skin is incomplete, and consensus is lacking as to the best diagnosis and treatment strategies, and the inclusion of sensitive skin education in dermatology curricula has not been examined, according to Erika T. McCormick, BS, and Adam Friedman, MD, of George Washington University, Washington, DC.
For the study, published in the Journal of Drugs in Dermatology, they developed a 26-question survey for dermatology residents that asked about sensitive skin in dermatology residency training. Participants came from the Orlando Dermatology, Aesthetic, and Surgical Conference email list.
Survey respondents included 214 residents at various levels of training at programs across the United States; 67.1% were female, 92.1% were aged 25-34 years, and 85.5% were in academic or university programs.
Overall, 99% of respondents believed that sensitive skin issues should be part of their residency training to some extent, and 84% reported experiences with patients for whom the chief presenting complaint was sensitive skin.
However, fewer than half (48%) of the residents reported specific resident education in sensitive skin, while 51% reported nonspecific education about sensitive skin education in the context of other skin diseases, and 1% reported no education about sensitive skin.
Less than one-quarter of the respondents who received any sensitive skin education reported feeling comfortable in their ability to diagnose, evaluate, and manage sensitive skin, while those with sensitive skin–specific education were significantly more likely to describe themselves as “very knowledgeable.”
As for treatment approaches, residents with specific sensitive skin education were more likely than were those without sensitive skin–specific training to ask patients about allergies and past reactions to skin products, and to counsel them about environmental triggers.
Notably, 96% of the respondents were not familiar with the Sensitive Skin (SS) Scale–10, a validated measure of sensitive skin severity.
The most common challenges in care of patients with sensitive skin were assessing improvement over time, reported by 25% of respondents, recommending products (23%), and prescribing/medical management (22%). The topics residents expressed most interest in learning about were product recommendations (78%), patient counseling (77%), reviewing research on sensitive skin (70%), diagnosing sensitive skin (67%), using the SS-10 (48%), and clinical research updates (40%).
The findings were limited by several factors including the reliance on self-reports, the researchers noted. However, the results highlight the lack of consensus in treatment of sensitive skin and the need to address this knowledge gap at the residency level, they said.
Improving Tools for Practice
“Many practice patterns and approaches are forged in the fires of training,” corresponding author Dr. Friedman, professor and chair of dermatology and residency program director at George Washington University, said in an interview. “Identifying gaps, especially for heavily prevalent issues, questions, and concerns such as sensitive skin that residents will encounter in practice is important to ensure an educated workforce,” he said.
Education on sensitive skin is lacking because, until recently, research and clinical guidance have been lacking, Dr. Friedman said. The root of the problem is that sensitive skin is mainly considered a symptom, rather than an independent condition, he explained. “Depending on the study, the prevalence of sensitive skin has been reported as high as 70%, with roughly 40% of these patients having no primary skin condition,” he said. This means sensitive skin can be both a symptom and a condition, which causes confusion for clinicians and patients, he added.
“Therefore, in order to overcome this gap, the condition itself at a minimum needs a standard definition and a way to diagnosis, which we fortunately have in the validated research tool known as the SS-10,” said Dr. Friedman.
Almost all residents surveyed in the current study had never heard of the SS-10, but more than half found it to be useful after learning of it through the study survey, he noted.
Looking ahead, greater elucidation of the pathophysiology of sensitive skin is needed to effectively pursue studies of products and treatments for these patients, but the SS-10 can be used to define and monitor the condition to evaluate improvement, he added.
The study was funded by an independent fellowship grant from Galderma. Ms. McCormick is supported by an unrestricted fellowship grant funded by Galderma. Dr. Friedman has served as a consultant for Galderma.
Although sensitive skin affects an estimated 40%-70% of the population, knowledge of the pathophysiology of sensitive skin is incomplete, and consensus is lacking as to the best diagnosis and treatment strategies, and the inclusion of sensitive skin education in dermatology curricula has not been examined, according to Erika T. McCormick, BS, and Adam Friedman, MD, of George Washington University, Washington, DC.
For the study, published in the Journal of Drugs in Dermatology, they developed a 26-question survey for dermatology residents that asked about sensitive skin in dermatology residency training. Participants came from the Orlando Dermatology, Aesthetic, and Surgical Conference email list.
Survey respondents included 214 residents at various levels of training at programs across the United States; 67.1% were female, 92.1% were aged 25-34 years, and 85.5% were in academic or university programs.
Overall, 99% of respondents believed that sensitive skin issues should be part of their residency training to some extent, and 84% reported experiences with patients for whom the chief presenting complaint was sensitive skin.
However, fewer than half (48%) of the residents reported specific resident education in sensitive skin, while 51% reported nonspecific education about sensitive skin education in the context of other skin diseases, and 1% reported no education about sensitive skin.
Less than one-quarter of the respondents who received any sensitive skin education reported feeling comfortable in their ability to diagnose, evaluate, and manage sensitive skin, while those with sensitive skin–specific education were significantly more likely to describe themselves as “very knowledgeable.”
As for treatment approaches, residents with specific sensitive skin education were more likely than were those without sensitive skin–specific training to ask patients about allergies and past reactions to skin products, and to counsel them about environmental triggers.
Notably, 96% of the respondents were not familiar with the Sensitive Skin (SS) Scale–10, a validated measure of sensitive skin severity.
The most common challenges in care of patients with sensitive skin were assessing improvement over time, reported by 25% of respondents, recommending products (23%), and prescribing/medical management (22%). The topics residents expressed most interest in learning about were product recommendations (78%), patient counseling (77%), reviewing research on sensitive skin (70%), diagnosing sensitive skin (67%), using the SS-10 (48%), and clinical research updates (40%).
The findings were limited by several factors including the reliance on self-reports, the researchers noted. However, the results highlight the lack of consensus in treatment of sensitive skin and the need to address this knowledge gap at the residency level, they said.
Improving Tools for Practice
“Many practice patterns and approaches are forged in the fires of training,” corresponding author Dr. Friedman, professor and chair of dermatology and residency program director at George Washington University, said in an interview. “Identifying gaps, especially for heavily prevalent issues, questions, and concerns such as sensitive skin that residents will encounter in practice is important to ensure an educated workforce,” he said.
Education on sensitive skin is lacking because, until recently, research and clinical guidance have been lacking, Dr. Friedman said. The root of the problem is that sensitive skin is mainly considered a symptom, rather than an independent condition, he explained. “Depending on the study, the prevalence of sensitive skin has been reported as high as 70%, with roughly 40% of these patients having no primary skin condition,” he said. This means sensitive skin can be both a symptom and a condition, which causes confusion for clinicians and patients, he added.
“Therefore, in order to overcome this gap, the condition itself at a minimum needs a standard definition and a way to diagnosis, which we fortunately have in the validated research tool known as the SS-10,” said Dr. Friedman.
Almost all residents surveyed in the current study had never heard of the SS-10, but more than half found it to be useful after learning of it through the study survey, he noted.
Looking ahead, greater elucidation of the pathophysiology of sensitive skin is needed to effectively pursue studies of products and treatments for these patients, but the SS-10 can be used to define and monitor the condition to evaluate improvement, he added.
The study was funded by an independent fellowship grant from Galderma. Ms. McCormick is supported by an unrestricted fellowship grant funded by Galderma. Dr. Friedman has served as a consultant for Galderma.
Although sensitive skin affects an estimated 40%-70% of the population, knowledge of the pathophysiology of sensitive skin is incomplete, and consensus is lacking as to the best diagnosis and treatment strategies, and the inclusion of sensitive skin education in dermatology curricula has not been examined, according to Erika T. McCormick, BS, and Adam Friedman, MD, of George Washington University, Washington, DC.
For the study, published in the Journal of Drugs in Dermatology, they developed a 26-question survey for dermatology residents that asked about sensitive skin in dermatology residency training. Participants came from the Orlando Dermatology, Aesthetic, and Surgical Conference email list.
Survey respondents included 214 residents at various levels of training at programs across the United States; 67.1% were female, 92.1% were aged 25-34 years, and 85.5% were in academic or university programs.
Overall, 99% of respondents believed that sensitive skin issues should be part of their residency training to some extent, and 84% reported experiences with patients for whom the chief presenting complaint was sensitive skin.
However, fewer than half (48%) of the residents reported specific resident education in sensitive skin, while 51% reported nonspecific education about sensitive skin education in the context of other skin diseases, and 1% reported no education about sensitive skin.
Less than one-quarter of the respondents who received any sensitive skin education reported feeling comfortable in their ability to diagnose, evaluate, and manage sensitive skin, while those with sensitive skin–specific education were significantly more likely to describe themselves as “very knowledgeable.”
As for treatment approaches, residents with specific sensitive skin education were more likely than were those without sensitive skin–specific training to ask patients about allergies and past reactions to skin products, and to counsel them about environmental triggers.
Notably, 96% of the respondents were not familiar with the Sensitive Skin (SS) Scale–10, a validated measure of sensitive skin severity.
The most common challenges in care of patients with sensitive skin were assessing improvement over time, reported by 25% of respondents, recommending products (23%), and prescribing/medical management (22%). The topics residents expressed most interest in learning about were product recommendations (78%), patient counseling (77%), reviewing research on sensitive skin (70%), diagnosing sensitive skin (67%), using the SS-10 (48%), and clinical research updates (40%).
The findings were limited by several factors including the reliance on self-reports, the researchers noted. However, the results highlight the lack of consensus in treatment of sensitive skin and the need to address this knowledge gap at the residency level, they said.
Improving Tools for Practice
“Many practice patterns and approaches are forged in the fires of training,” corresponding author Dr. Friedman, professor and chair of dermatology and residency program director at George Washington University, said in an interview. “Identifying gaps, especially for heavily prevalent issues, questions, and concerns such as sensitive skin that residents will encounter in practice is important to ensure an educated workforce,” he said.
Education on sensitive skin is lacking because, until recently, research and clinical guidance have been lacking, Dr. Friedman said. The root of the problem is that sensitive skin is mainly considered a symptom, rather than an independent condition, he explained. “Depending on the study, the prevalence of sensitive skin has been reported as high as 70%, with roughly 40% of these patients having no primary skin condition,” he said. This means sensitive skin can be both a symptom and a condition, which causes confusion for clinicians and patients, he added.
“Therefore, in order to overcome this gap, the condition itself at a minimum needs a standard definition and a way to diagnosis, which we fortunately have in the validated research tool known as the SS-10,” said Dr. Friedman.
Almost all residents surveyed in the current study had never heard of the SS-10, but more than half found it to be useful after learning of it through the study survey, he noted.
Looking ahead, greater elucidation of the pathophysiology of sensitive skin is needed to effectively pursue studies of products and treatments for these patients, but the SS-10 can be used to define and monitor the condition to evaluate improvement, he added.
The study was funded by an independent fellowship grant from Galderma. Ms. McCormick is supported by an unrestricted fellowship grant funded by Galderma. Dr. Friedman has served as a consultant for Galderma.
FROM THE JOURNAL OF DRUGS IN DERMATOLOGY