User login
Youths have strong opinions on language about body weight
With youth obesity on the rise – an estimated 1 in 5 youths are impacted by obesity, according to the Centers for Disease Control and Prevention – conversations about healthy weight are becoming more commonplace, not only in the pediatrician’s office, but at home, too. But the language we use around this sensitive topic is important, as youths are acutely aware that words have a direct impact on their mental health.
Sixteen-year-old Avery DiCocco of Northbrook, Ill., knows how vulnerable teenagers feel.
“I think it definitely matters the way that parents and doctors address weight,” she said. “You never know who may be insecure, and using negative words could go a lot further than they think with impacting self-esteem.”
A new study published in Pediatrics brings light to the words that parents (and providers) use when speaking to youths (ages 10-17) about their weight.
Researchers from the University of Connecticut Rudd Center for Food Policy & Health, Hartford, led an online survey of youths and their parents. Those who took part were asked about 27 terms related to body weight. Parents were asked to comment on their use of these words, while youths commented on the emotional response. The researchers said 1,936 parents and 2,032 adolescents were surveyed between September and December 2021.
Although results skewed toward the use of more positive words, such as “healthy weight,” over terms like “obese,” “fat” or “large,” there was variation across ethnicity, sexual orientation, and weight status. For example, it was noted in the study, funded by WW International, that preference for the word “curvy” was higher among Hispanic/Latino youths, sexual minority youths, and those with a body mass index in the 95th percentile, compared with their White, heterosexual, and lower-weight peers.
Words matter
In 2017, the American Academy of Pediatrics came out with a policy statement on weight stigma and the need for doctors to use more neutral language and less stigmatizing terms in practice when discussing weight among youths.
But one of the reasons this new study is important, said Gregory Germain, MD, associate chief of pediatrics at Yale New Haven (Conn.) Children’s Hospital, is that this study focuses on parents who interact with their kids much more often than a pediatrician who sees them a few times a year.
“Parental motivation, discussion, interaction on a consistent basis – that dialogue is so critical in kids with obesity,” said Germain, who stresses that all adults, coaches, and educators should consider this study as well.
“When we think about those detrimental impacts on mental health when more stigmatizing language is used, just us being more mindful in how we are talking to youth can make such a profound impact,” said Rebecca Kamody, PhD, a clinical psychologist at Yale University, with a research and clinical focus on eating and weight disorders.
“In essence, this is a low-hanging fruit intervention,” she said.
Dr. Kamody recommends we take a lesson from “cultural humility” in psychology to understand how to approach this with kids, calling for “the humbleness as parents or providers in asking someone what they want used to make it the safest place for a discussion with our youth.”
One piece of the puzzle
Dr. Germain and Dr. Kamody agreed that language in discussing this topic is important but that we need to recognize that this topic in general is extremely tricky.
For one, “there are these very real metabolic complications of having high weight at a young age,” said Kamody, who stresses the need for balance to make real change.
Dr. Germain agreed. “Finding a fine line between discussing obesity and not kicking your kid into disordered eating is important.”
The researchers also recognize the limits of an online study, where self-reporting parents may not want to admit using negative weight terminology, but certainly believe it’s a start in identifying some of the undesirable patterns that may be occurring when it comes to weight.
“The overarching message is a positive one, that with our preteens and teenage kids, we need to watch our language, to create a nonjudgmental and safe environment to discuss weight and any issue involved with taking care of themselves,” said Dr. Germain.
A version of this article first appeared on Medscape.com.
With youth obesity on the rise – an estimated 1 in 5 youths are impacted by obesity, according to the Centers for Disease Control and Prevention – conversations about healthy weight are becoming more commonplace, not only in the pediatrician’s office, but at home, too. But the language we use around this sensitive topic is important, as youths are acutely aware that words have a direct impact on their mental health.
Sixteen-year-old Avery DiCocco of Northbrook, Ill., knows how vulnerable teenagers feel.
“I think it definitely matters the way that parents and doctors address weight,” she said. “You never know who may be insecure, and using negative words could go a lot further than they think with impacting self-esteem.”
A new study published in Pediatrics brings light to the words that parents (and providers) use when speaking to youths (ages 10-17) about their weight.
Researchers from the University of Connecticut Rudd Center for Food Policy & Health, Hartford, led an online survey of youths and their parents. Those who took part were asked about 27 terms related to body weight. Parents were asked to comment on their use of these words, while youths commented on the emotional response. The researchers said 1,936 parents and 2,032 adolescents were surveyed between September and December 2021.
Although results skewed toward the use of more positive words, such as “healthy weight,” over terms like “obese,” “fat” or “large,” there was variation across ethnicity, sexual orientation, and weight status. For example, it was noted in the study, funded by WW International, that preference for the word “curvy” was higher among Hispanic/Latino youths, sexual minority youths, and those with a body mass index in the 95th percentile, compared with their White, heterosexual, and lower-weight peers.
Words matter
In 2017, the American Academy of Pediatrics came out with a policy statement on weight stigma and the need for doctors to use more neutral language and less stigmatizing terms in practice when discussing weight among youths.
But one of the reasons this new study is important, said Gregory Germain, MD, associate chief of pediatrics at Yale New Haven (Conn.) Children’s Hospital, is that this study focuses on parents who interact with their kids much more often than a pediatrician who sees them a few times a year.
“Parental motivation, discussion, interaction on a consistent basis – that dialogue is so critical in kids with obesity,” said Germain, who stresses that all adults, coaches, and educators should consider this study as well.
“When we think about those detrimental impacts on mental health when more stigmatizing language is used, just us being more mindful in how we are talking to youth can make such a profound impact,” said Rebecca Kamody, PhD, a clinical psychologist at Yale University, with a research and clinical focus on eating and weight disorders.
“In essence, this is a low-hanging fruit intervention,” she said.
Dr. Kamody recommends we take a lesson from “cultural humility” in psychology to understand how to approach this with kids, calling for “the humbleness as parents or providers in asking someone what they want used to make it the safest place for a discussion with our youth.”
One piece of the puzzle
Dr. Germain and Dr. Kamody agreed that language in discussing this topic is important but that we need to recognize that this topic in general is extremely tricky.
For one, “there are these very real metabolic complications of having high weight at a young age,” said Kamody, who stresses the need for balance to make real change.
Dr. Germain agreed. “Finding a fine line between discussing obesity and not kicking your kid into disordered eating is important.”
The researchers also recognize the limits of an online study, where self-reporting parents may not want to admit using negative weight terminology, but certainly believe it’s a start in identifying some of the undesirable patterns that may be occurring when it comes to weight.
“The overarching message is a positive one, that with our preteens and teenage kids, we need to watch our language, to create a nonjudgmental and safe environment to discuss weight and any issue involved with taking care of themselves,” said Dr. Germain.
A version of this article first appeared on Medscape.com.
With youth obesity on the rise – an estimated 1 in 5 youths are impacted by obesity, according to the Centers for Disease Control and Prevention – conversations about healthy weight are becoming more commonplace, not only in the pediatrician’s office, but at home, too. But the language we use around this sensitive topic is important, as youths are acutely aware that words have a direct impact on their mental health.
Sixteen-year-old Avery DiCocco of Northbrook, Ill., knows how vulnerable teenagers feel.
“I think it definitely matters the way that parents and doctors address weight,” she said. “You never know who may be insecure, and using negative words could go a lot further than they think with impacting self-esteem.”
A new study published in Pediatrics brings light to the words that parents (and providers) use when speaking to youths (ages 10-17) about their weight.
Researchers from the University of Connecticut Rudd Center for Food Policy & Health, Hartford, led an online survey of youths and their parents. Those who took part were asked about 27 terms related to body weight. Parents were asked to comment on their use of these words, while youths commented on the emotional response. The researchers said 1,936 parents and 2,032 adolescents were surveyed between September and December 2021.
Although results skewed toward the use of more positive words, such as “healthy weight,” over terms like “obese,” “fat” or “large,” there was variation across ethnicity, sexual orientation, and weight status. For example, it was noted in the study, funded by WW International, that preference for the word “curvy” was higher among Hispanic/Latino youths, sexual minority youths, and those with a body mass index in the 95th percentile, compared with their White, heterosexual, and lower-weight peers.
Words matter
In 2017, the American Academy of Pediatrics came out with a policy statement on weight stigma and the need for doctors to use more neutral language and less stigmatizing terms in practice when discussing weight among youths.
But one of the reasons this new study is important, said Gregory Germain, MD, associate chief of pediatrics at Yale New Haven (Conn.) Children’s Hospital, is that this study focuses on parents who interact with their kids much more often than a pediatrician who sees them a few times a year.
“Parental motivation, discussion, interaction on a consistent basis – that dialogue is so critical in kids with obesity,” said Germain, who stresses that all adults, coaches, and educators should consider this study as well.
“When we think about those detrimental impacts on mental health when more stigmatizing language is used, just us being more mindful in how we are talking to youth can make such a profound impact,” said Rebecca Kamody, PhD, a clinical psychologist at Yale University, with a research and clinical focus on eating and weight disorders.
“In essence, this is a low-hanging fruit intervention,” she said.
Dr. Kamody recommends we take a lesson from “cultural humility” in psychology to understand how to approach this with kids, calling for “the humbleness as parents or providers in asking someone what they want used to make it the safest place for a discussion with our youth.”
One piece of the puzzle
Dr. Germain and Dr. Kamody agreed that language in discussing this topic is important but that we need to recognize that this topic in general is extremely tricky.
For one, “there are these very real metabolic complications of having high weight at a young age,” said Kamody, who stresses the need for balance to make real change.
Dr. Germain agreed. “Finding a fine line between discussing obesity and not kicking your kid into disordered eating is important.”
The researchers also recognize the limits of an online study, where self-reporting parents may not want to admit using negative weight terminology, but certainly believe it’s a start in identifying some of the undesirable patterns that may be occurring when it comes to weight.
“The overarching message is a positive one, that with our preteens and teenage kids, we need to watch our language, to create a nonjudgmental and safe environment to discuss weight and any issue involved with taking care of themselves,” said Dr. Germain.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Intermittent fasting diet trend linked to disordered eating
Researchers from the University of Toronto analyzed data from more than 2700 adolescents and young adults from the Canadian Study of Adolescent Health Behaviors, and found that for women, IF was significantly associated with overeating, binge eating, vomiting, laxative use, and compulsive exercise.
IF in women was also associated with higher scores on the Eating Disorder Examination Questionnaire (EDE-Q), which was used to determine ED psychopathology.
Study investigator Kyle Ganson, PhD, assistant professor in the Factor-Inwentash Faculty of Social Work at the University of Toronto, said in an interview that evidence on the effectiveness of IF for weight loss and disease prevention is mixed, and that it’s important to understand the potential harms of IF – even if there are benefits for some.
“If anything, this study shines light on the fact that engagement in IF may be connected with problematic ED behaviors, requiring health care professionals to be very aware of this contemporary and popular dietary trend, despite proponents on social media touting the effectiveness and benefits,” he said.
The study was published online in Eating Behaviors.
Touted for health benefits
The practice of IF has been gaining popularity partly because of reputable medical experts touting its health benefits. Johns Hopkins Medicine, for instance, cited evidence that IF boosts working memory, improves blood pressure, enhances physical performance, and prevents obesity. Yet there has been little research on its harms.
As part of the Canadian Study of Adolescent Health Behaviors, Dr. Ganson and associates analyzed data on 2,700 adolescents and young adults aged 16-30 recruited from social media ads in November and December 2021. The sample included women, men, and transgender or gender-nonconforming individuals.
Study participants answered questions about weight perception, current weight change behavior, engagement in IF, and participation in eating disorder behaviors. They were also administered the EDE-Q, which measures eating disorder psychopathology.
In total, 47% of women (n = 1,470), 38% of men (n = 1,060), and 52% transgender or gender-nonconforming individuals (n = 225) reported engaging in IF during the past year.
Dr. Ganson and associates found that, for women, IF in the past 12 months and past 30 days were significantly associated with all eating disorder behaviors, including overeating, loss of control, binge eating, vomiting, laxative use, compulsive exercise, and fasting – as well as higher overall EDE-Q global scores.
For men, IF in the past 12 months was significantly associated with compulsive exercise, and higher overall EDE-Q global scores.
The team found that for TGNC participants, IF was positively associated with higher EDE-Q global scores.
The investigators acknowledged some limitations with the study – the method of recruiting, which involved ads placed on social media, could cause selection bias. In addition to this, data collection methods relied heavily on participants’ self-reporting, which could also be susceptible to bias.
“Certainly, there needs to be more investigation on this dietary practice,” said Dr. Ganson. “If anything, this study shines light on the fact that engagement in IF may be connected with problematic ED behaviors requiring healthcare professionals to be very aware of this contemporary and popular dietary trend – despite proponents on social media touting the effectiveness and benefits.”
Screening warranted
Dr. Ganson noted that additional research is needed to support the findings from his study, and to further illuminate the potential harms of IF.
Health care professionals “need to be aware of common, contemporary dietary trends that young people engage in and are commonly discussed on social media, such as IF,” he noted. In addition, he’d like to see health care professionals assess their patients for IF who are dieting and to follow-up with assessments for ED-related attitudes and behaviors.
“Additionally, there are likely bidirectional relationships between IF and ED attitudes and behaviors, so professionals should be aware the ways in which ED behaviors are masked as IF engagement,” Dr. Ganson said.
More research needed
Commenting on the findings, Angela Guarda, MD, professor of eating disorders at Johns Hopkins University and director of the eating disorders program at Johns Hopkins Hospital, both in Baltimore, said more research is needed on outcomes for IF.
“We lack a definitive answer. The reality is that IF may help some and harm others and is most likely not healthy for all,” she said, noting that the study results “support what many in the eating disorders field believe, namely that IF for someone who is at risk for an eating disorder is likely to be ill advised.”
She added that “continued research is needed to establish its safety, and for whom it may be a therapeutic versus an iatrogenic recommendation.”
The study was funded by the Connaught New Researcher Award. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers from the University of Toronto analyzed data from more than 2700 adolescents and young adults from the Canadian Study of Adolescent Health Behaviors, and found that for women, IF was significantly associated with overeating, binge eating, vomiting, laxative use, and compulsive exercise.
IF in women was also associated with higher scores on the Eating Disorder Examination Questionnaire (EDE-Q), which was used to determine ED psychopathology.
Study investigator Kyle Ganson, PhD, assistant professor in the Factor-Inwentash Faculty of Social Work at the University of Toronto, said in an interview that evidence on the effectiveness of IF for weight loss and disease prevention is mixed, and that it’s important to understand the potential harms of IF – even if there are benefits for some.
“If anything, this study shines light on the fact that engagement in IF may be connected with problematic ED behaviors, requiring health care professionals to be very aware of this contemporary and popular dietary trend, despite proponents on social media touting the effectiveness and benefits,” he said.
The study was published online in Eating Behaviors.
Touted for health benefits
The practice of IF has been gaining popularity partly because of reputable medical experts touting its health benefits. Johns Hopkins Medicine, for instance, cited evidence that IF boosts working memory, improves blood pressure, enhances physical performance, and prevents obesity. Yet there has been little research on its harms.
As part of the Canadian Study of Adolescent Health Behaviors, Dr. Ganson and associates analyzed data on 2,700 adolescents and young adults aged 16-30 recruited from social media ads in November and December 2021. The sample included women, men, and transgender or gender-nonconforming individuals.
Study participants answered questions about weight perception, current weight change behavior, engagement in IF, and participation in eating disorder behaviors. They were also administered the EDE-Q, which measures eating disorder psychopathology.
In total, 47% of women (n = 1,470), 38% of men (n = 1,060), and 52% transgender or gender-nonconforming individuals (n = 225) reported engaging in IF during the past year.
Dr. Ganson and associates found that, for women, IF in the past 12 months and past 30 days were significantly associated with all eating disorder behaviors, including overeating, loss of control, binge eating, vomiting, laxative use, compulsive exercise, and fasting – as well as higher overall EDE-Q global scores.
For men, IF in the past 12 months was significantly associated with compulsive exercise, and higher overall EDE-Q global scores.
The team found that for TGNC participants, IF was positively associated with higher EDE-Q global scores.
The investigators acknowledged some limitations with the study – the method of recruiting, which involved ads placed on social media, could cause selection bias. In addition to this, data collection methods relied heavily on participants’ self-reporting, which could also be susceptible to bias.
“Certainly, there needs to be more investigation on this dietary practice,” said Dr. Ganson. “If anything, this study shines light on the fact that engagement in IF may be connected with problematic ED behaviors requiring healthcare professionals to be very aware of this contemporary and popular dietary trend – despite proponents on social media touting the effectiveness and benefits.”
Screening warranted
Dr. Ganson noted that additional research is needed to support the findings from his study, and to further illuminate the potential harms of IF.
Health care professionals “need to be aware of common, contemporary dietary trends that young people engage in and are commonly discussed on social media, such as IF,” he noted. In addition, he’d like to see health care professionals assess their patients for IF who are dieting and to follow-up with assessments for ED-related attitudes and behaviors.
“Additionally, there are likely bidirectional relationships between IF and ED attitudes and behaviors, so professionals should be aware the ways in which ED behaviors are masked as IF engagement,” Dr. Ganson said.
More research needed
Commenting on the findings, Angela Guarda, MD, professor of eating disorders at Johns Hopkins University and director of the eating disorders program at Johns Hopkins Hospital, both in Baltimore, said more research is needed on outcomes for IF.
“We lack a definitive answer. The reality is that IF may help some and harm others and is most likely not healthy for all,” she said, noting that the study results “support what many in the eating disorders field believe, namely that IF for someone who is at risk for an eating disorder is likely to be ill advised.”
She added that “continued research is needed to establish its safety, and for whom it may be a therapeutic versus an iatrogenic recommendation.”
The study was funded by the Connaught New Researcher Award. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers from the University of Toronto analyzed data from more than 2700 adolescents and young adults from the Canadian Study of Adolescent Health Behaviors, and found that for women, IF was significantly associated with overeating, binge eating, vomiting, laxative use, and compulsive exercise.
IF in women was also associated with higher scores on the Eating Disorder Examination Questionnaire (EDE-Q), which was used to determine ED psychopathology.
Study investigator Kyle Ganson, PhD, assistant professor in the Factor-Inwentash Faculty of Social Work at the University of Toronto, said in an interview that evidence on the effectiveness of IF for weight loss and disease prevention is mixed, and that it’s important to understand the potential harms of IF – even if there are benefits for some.
“If anything, this study shines light on the fact that engagement in IF may be connected with problematic ED behaviors, requiring health care professionals to be very aware of this contemporary and popular dietary trend, despite proponents on social media touting the effectiveness and benefits,” he said.
The study was published online in Eating Behaviors.
Touted for health benefits
The practice of IF has been gaining popularity partly because of reputable medical experts touting its health benefits. Johns Hopkins Medicine, for instance, cited evidence that IF boosts working memory, improves blood pressure, enhances physical performance, and prevents obesity. Yet there has been little research on its harms.
As part of the Canadian Study of Adolescent Health Behaviors, Dr. Ganson and associates analyzed data on 2,700 adolescents and young adults aged 16-30 recruited from social media ads in November and December 2021. The sample included women, men, and transgender or gender-nonconforming individuals.
Study participants answered questions about weight perception, current weight change behavior, engagement in IF, and participation in eating disorder behaviors. They were also administered the EDE-Q, which measures eating disorder psychopathology.
In total, 47% of women (n = 1,470), 38% of men (n = 1,060), and 52% transgender or gender-nonconforming individuals (n = 225) reported engaging in IF during the past year.
Dr. Ganson and associates found that, for women, IF in the past 12 months and past 30 days were significantly associated with all eating disorder behaviors, including overeating, loss of control, binge eating, vomiting, laxative use, compulsive exercise, and fasting – as well as higher overall EDE-Q global scores.
For men, IF in the past 12 months was significantly associated with compulsive exercise, and higher overall EDE-Q global scores.
The team found that for TGNC participants, IF was positively associated with higher EDE-Q global scores.
The investigators acknowledged some limitations with the study – the method of recruiting, which involved ads placed on social media, could cause selection bias. In addition to this, data collection methods relied heavily on participants’ self-reporting, which could also be susceptible to bias.
“Certainly, there needs to be more investigation on this dietary practice,” said Dr. Ganson. “If anything, this study shines light on the fact that engagement in IF may be connected with problematic ED behaviors requiring healthcare professionals to be very aware of this contemporary and popular dietary trend – despite proponents on social media touting the effectiveness and benefits.”
Screening warranted
Dr. Ganson noted that additional research is needed to support the findings from his study, and to further illuminate the potential harms of IF.
Health care professionals “need to be aware of common, contemporary dietary trends that young people engage in and are commonly discussed on social media, such as IF,” he noted. In addition, he’d like to see health care professionals assess their patients for IF who are dieting and to follow-up with assessments for ED-related attitudes and behaviors.
“Additionally, there are likely bidirectional relationships between IF and ED attitudes and behaviors, so professionals should be aware the ways in which ED behaviors are masked as IF engagement,” Dr. Ganson said.
More research needed
Commenting on the findings, Angela Guarda, MD, professor of eating disorders at Johns Hopkins University and director of the eating disorders program at Johns Hopkins Hospital, both in Baltimore, said more research is needed on outcomes for IF.
“We lack a definitive answer. The reality is that IF may help some and harm others and is most likely not healthy for all,” she said, noting that the study results “support what many in the eating disorders field believe, namely that IF for someone who is at risk for an eating disorder is likely to be ill advised.”
She added that “continued research is needed to establish its safety, and for whom it may be a therapeutic versus an iatrogenic recommendation.”
The study was funded by the Connaught New Researcher Award. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EATING DISORDERS
Electrolyte disturbances a harbinger of eating disorders?
Electrolyte abnormalities may serve as a precursor to a future eating disorder diagnosis, a finding that may help pinpoint candidates for screening.
Researchers found that adolescents and adults with electrolyte abnormalities on routine outpatient lab work were twice as likely as those without these disturbances to be subsequently diagnosed with an eating disorder.
“These electrolyte abnormalities were in fact seen well ahead (> 1 year on average) of the time when patients were diagnosed with eating disorders,” study investigator Gregory Hundemer, MD, department of nephrology, University of Ottawa, told this news organization.
“Incidentally discovered outpatient electrolyte abnormalities may help to identify individuals who may benefit from more targeted screening into an underlying eating disorder. This, in turn, may allow for earlier diagnosis and therapeutic intervention,” Dr. Hundemer said.
The study was published online in JAMA Network Open.
Tailored screening?
Electrolyte abnormalities are often found when an individual is diagnosed with an eating disorder, but it’s largely unknown whether electrolyte abnormalities prior to the acute presentation of an eating disorder are associated with the future diagnosis of an eating disorder.
To investigate, the researchers used administrative health data to match 6,970 individuals (mean age, 28 years; 13% male) with an eating disorder diagnosis to 27,878 controls without an eating disorder diagnosis.
They found that individuals with an eating disorder were more likely to have a preceding electrolyte abnormality, compared with peers without an eating disorder (18.4% vs. 7.5%).
An outpatient electrolyte abnormality present 3 years to 30 days prior to diagnosis was associated with about a twofold higher odds for subsequent eating disorder diagnosis (adjusted odds ratio, 2.12; 95% confidence interval, 1.86-2.41).
The median time from the earliest electrolyte abnormality to eating disorder diagnosis was 386 days (range, 157-716 days).
Hypokalemia was the most common electrolyte abnormality (present in 12% of cases vs. 5% of controls), while hyponatremia, hypernatremia, hypophosphatemia, and metabolic alkalosis were the most specific for a subsequent eating disorder diagnosis.
Severe hypokalemia (serum potassium levels of 3.0 mmol/L or lower) and severe hyponatremia (serum sodium, 128 mmol/L or lower) were associated with over sevenfold and fivefold higher odds for the diagnosis of an eating disorder, respectively.
The U.S. Preventive Services Task Force issued its first-ever statement on screening for eating disorders earlier this year.
The task force concluded that there is insufficient evidence to weigh the balance of benefits and harms of screening for eating disorders in adolescents and adults with no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder.
Dr. Hundemer and colleagues believe an incidental electrolyte abnormality may identify candidates at high risk for an underlying eating disorder who many benefit from screening.
Several screening tools of varying complexity have been developed that are validated and accurate in identifying individuals with a potential eating disorder.
They include the SCOFF questionnaire, the Eating Disorder Screen for Primary Care, the Eating Attitudes Test, and the Primary Care Evaluation of Mental Disorders Patient Health Questionnaire.
Underdiagnosed, undertreated
Offering perspective on the findings, Kamryn T. Eddy, PhD, codirector, Eating Disorders Clinical and Research Program, Massachusetts General Hospital, Boston, said the notion “that a physical sign may help to promote eating disorder assessment is important particularly given that early detection can improve outcomes.”
“But this finding appears in the current context of eating disorders going largely underdetected, underdiagnosed, and undertreated across medical and psychiatric settings,” said Dr. Eddy, associate professor, department of psychiatry, Harvard Medical School, Boston.
“Indeed, eating disorders are prevalent and cut across age, sex, gender, weight, race, ethnicity, and socioeconomic strata, and still, many providers do not routinely assess for eating disorders,” Dr. Eddy said.
“I might suggest that perhaps in addition to letting electrolyte abnormalities be a cue to screen for eating disorders, an even more powerful shift toward routine screening and assessment of eating disorders by medical providers be made,” Dr. Eddy said in an interview.
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Health and Long-Term Care. Dr. Hundemer and Dr. Eddy have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Electrolyte abnormalities may serve as a precursor to a future eating disorder diagnosis, a finding that may help pinpoint candidates for screening.
Researchers found that adolescents and adults with electrolyte abnormalities on routine outpatient lab work were twice as likely as those without these disturbances to be subsequently diagnosed with an eating disorder.
“These electrolyte abnormalities were in fact seen well ahead (> 1 year on average) of the time when patients were diagnosed with eating disorders,” study investigator Gregory Hundemer, MD, department of nephrology, University of Ottawa, told this news organization.
“Incidentally discovered outpatient electrolyte abnormalities may help to identify individuals who may benefit from more targeted screening into an underlying eating disorder. This, in turn, may allow for earlier diagnosis and therapeutic intervention,” Dr. Hundemer said.
The study was published online in JAMA Network Open.
Tailored screening?
Electrolyte abnormalities are often found when an individual is diagnosed with an eating disorder, but it’s largely unknown whether electrolyte abnormalities prior to the acute presentation of an eating disorder are associated with the future diagnosis of an eating disorder.
To investigate, the researchers used administrative health data to match 6,970 individuals (mean age, 28 years; 13% male) with an eating disorder diagnosis to 27,878 controls without an eating disorder diagnosis.
They found that individuals with an eating disorder were more likely to have a preceding electrolyte abnormality, compared with peers without an eating disorder (18.4% vs. 7.5%).
An outpatient electrolyte abnormality present 3 years to 30 days prior to diagnosis was associated with about a twofold higher odds for subsequent eating disorder diagnosis (adjusted odds ratio, 2.12; 95% confidence interval, 1.86-2.41).
The median time from the earliest electrolyte abnormality to eating disorder diagnosis was 386 days (range, 157-716 days).
Hypokalemia was the most common electrolyte abnormality (present in 12% of cases vs. 5% of controls), while hyponatremia, hypernatremia, hypophosphatemia, and metabolic alkalosis were the most specific for a subsequent eating disorder diagnosis.
Severe hypokalemia (serum potassium levels of 3.0 mmol/L or lower) and severe hyponatremia (serum sodium, 128 mmol/L or lower) were associated with over sevenfold and fivefold higher odds for the diagnosis of an eating disorder, respectively.
The U.S. Preventive Services Task Force issued its first-ever statement on screening for eating disorders earlier this year.
The task force concluded that there is insufficient evidence to weigh the balance of benefits and harms of screening for eating disorders in adolescents and adults with no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder.
Dr. Hundemer and colleagues believe an incidental electrolyte abnormality may identify candidates at high risk for an underlying eating disorder who many benefit from screening.
Several screening tools of varying complexity have been developed that are validated and accurate in identifying individuals with a potential eating disorder.
They include the SCOFF questionnaire, the Eating Disorder Screen for Primary Care, the Eating Attitudes Test, and the Primary Care Evaluation of Mental Disorders Patient Health Questionnaire.
Underdiagnosed, undertreated
Offering perspective on the findings, Kamryn T. Eddy, PhD, codirector, Eating Disorders Clinical and Research Program, Massachusetts General Hospital, Boston, said the notion “that a physical sign may help to promote eating disorder assessment is important particularly given that early detection can improve outcomes.”
“But this finding appears in the current context of eating disorders going largely underdetected, underdiagnosed, and undertreated across medical and psychiatric settings,” said Dr. Eddy, associate professor, department of psychiatry, Harvard Medical School, Boston.
“Indeed, eating disorders are prevalent and cut across age, sex, gender, weight, race, ethnicity, and socioeconomic strata, and still, many providers do not routinely assess for eating disorders,” Dr. Eddy said.
“I might suggest that perhaps in addition to letting electrolyte abnormalities be a cue to screen for eating disorders, an even more powerful shift toward routine screening and assessment of eating disorders by medical providers be made,” Dr. Eddy said in an interview.
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Health and Long-Term Care. Dr. Hundemer and Dr. Eddy have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Electrolyte abnormalities may serve as a precursor to a future eating disorder diagnosis, a finding that may help pinpoint candidates for screening.
Researchers found that adolescents and adults with electrolyte abnormalities on routine outpatient lab work were twice as likely as those without these disturbances to be subsequently diagnosed with an eating disorder.
“These electrolyte abnormalities were in fact seen well ahead (> 1 year on average) of the time when patients were diagnosed with eating disorders,” study investigator Gregory Hundemer, MD, department of nephrology, University of Ottawa, told this news organization.
“Incidentally discovered outpatient electrolyte abnormalities may help to identify individuals who may benefit from more targeted screening into an underlying eating disorder. This, in turn, may allow for earlier diagnosis and therapeutic intervention,” Dr. Hundemer said.
The study was published online in JAMA Network Open.
Tailored screening?
Electrolyte abnormalities are often found when an individual is diagnosed with an eating disorder, but it’s largely unknown whether electrolyte abnormalities prior to the acute presentation of an eating disorder are associated with the future diagnosis of an eating disorder.
To investigate, the researchers used administrative health data to match 6,970 individuals (mean age, 28 years; 13% male) with an eating disorder diagnosis to 27,878 controls without an eating disorder diagnosis.
They found that individuals with an eating disorder were more likely to have a preceding electrolyte abnormality, compared with peers without an eating disorder (18.4% vs. 7.5%).
An outpatient electrolyte abnormality present 3 years to 30 days prior to diagnosis was associated with about a twofold higher odds for subsequent eating disorder diagnosis (adjusted odds ratio, 2.12; 95% confidence interval, 1.86-2.41).
The median time from the earliest electrolyte abnormality to eating disorder diagnosis was 386 days (range, 157-716 days).
Hypokalemia was the most common electrolyte abnormality (present in 12% of cases vs. 5% of controls), while hyponatremia, hypernatremia, hypophosphatemia, and metabolic alkalosis were the most specific for a subsequent eating disorder diagnosis.
Severe hypokalemia (serum potassium levels of 3.0 mmol/L or lower) and severe hyponatremia (serum sodium, 128 mmol/L or lower) were associated with over sevenfold and fivefold higher odds for the diagnosis of an eating disorder, respectively.
The U.S. Preventive Services Task Force issued its first-ever statement on screening for eating disorders earlier this year.
The task force concluded that there is insufficient evidence to weigh the balance of benefits and harms of screening for eating disorders in adolescents and adults with no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder.
Dr. Hundemer and colleagues believe an incidental electrolyte abnormality may identify candidates at high risk for an underlying eating disorder who many benefit from screening.
Several screening tools of varying complexity have been developed that are validated and accurate in identifying individuals with a potential eating disorder.
They include the SCOFF questionnaire, the Eating Disorder Screen for Primary Care, the Eating Attitudes Test, and the Primary Care Evaluation of Mental Disorders Patient Health Questionnaire.
Underdiagnosed, undertreated
Offering perspective on the findings, Kamryn T. Eddy, PhD, codirector, Eating Disorders Clinical and Research Program, Massachusetts General Hospital, Boston, said the notion “that a physical sign may help to promote eating disorder assessment is important particularly given that early detection can improve outcomes.”
“But this finding appears in the current context of eating disorders going largely underdetected, underdiagnosed, and undertreated across medical and psychiatric settings,” said Dr. Eddy, associate professor, department of psychiatry, Harvard Medical School, Boston.
“Indeed, eating disorders are prevalent and cut across age, sex, gender, weight, race, ethnicity, and socioeconomic strata, and still, many providers do not routinely assess for eating disorders,” Dr. Eddy said.
“I might suggest that perhaps in addition to letting electrolyte abnormalities be a cue to screen for eating disorders, an even more powerful shift toward routine screening and assessment of eating disorders by medical providers be made,” Dr. Eddy said in an interview.
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Health and Long-Term Care. Dr. Hundemer and Dr. Eddy have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
COVID pandemic associated with anorexia in Canadian youth
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Two states aim to curb diet pill sales to minors
California and New York are on the cusp of going further than the Food and Drug Administration in restricting the sale of nonprescription diet pills to minors as pediatricians and public health advocates try to protect kids from extreme weight-loss gimmicks online.
A bill before Gov. Gavin Newsom would bar anyone under 18 in California from buying over-the-counter weight-loss supplements – whether online or in shops – without a prescription. A similar bill passed by New York lawmakers is on Gov. Kathy Hochul’s desk. Neither Democrat has indicated how he or she will act.
If both bills are signed into law, proponents hope the momentum will build to restrict diet pill sales to children in more states. Massachusetts, New Jersey, and Missouri have introduced similar bills and backers plan to continue their push next year.
Nearly 30 million people in the United States will have an eating disorder in their lifetime; 95% of them are aged between 12 and 25, according to Johns Hopkins All Children’s Hospital. The hospital added that eating disorders pose the highest risk of mortality of any mental health disorder. And it has become easier than ever for minors to get pills that are sold online or on drugstore shelves. All dietary supplements, which include those for weight loss, accounted for nearly 35% of the $63 billion over-the-counter health products industry in 2021, according to Vision Research Reports, a market research firm.
Dietary supplements, which encompass a broad range of vitamins, herbs, and minerals, are classified by the FDA as food and don’t undergo scientific and safety testing as prescription drugs and over-the-counter medicines do.
Public health advocates want to keep weight-loss products – with ads that may promise to “Drop 5 pounds a week!” and pill names like Slim Sense – away from young people, particularly girls, since some research has linked some products to eating disorders. A study in the American Journal of Public Health, which followed more than 10,000 women aged 14-36 over 15 years, found that “those who used diet pills had more than 5 times higher adjusted odds of receiving an eating disorder diagnosis from a health care provider within 1-3 years than those who did not.”
Many pills have been found tainted with banned and dangerous ingredients that may cause cancer, heart attacks, strokes, and other ailments. For example, the FDA advised the public to avoid Slim Sense by Dr. Reade because it contains lorcaserin, which has been found to cause psychiatric disturbances and impairments in attention or memory. The FDA ordered it discontinued and the company couldn’t be reached for comment.
“Unscrupulous manufacturers are willing to take risks with consumers’ health – and they are lacing their products with illegal pharmaceuticals, banned pharmaceuticals, steroids, excessive stimulants, even experimental stimulants,” said S. Bryn Austin, ScD, founding director of the Strategic Training Initiative for the Prevention of Eating Disorders, or STRIPED, which supports the restrictions. “Consumers have no idea that this is what’s in these types of products.”
STRIPED is a public health initiative based at the Harvard School of Public Health, Boston, and Boston Children’s Hospital.
An industry trade group, the Natural Products Association, disputes that diet pills cause eating disorders, citing the lack of consumer complaints to the FDA of adverse events from their members’ products. “According to FDA data, there is no association between the two,” said Kyle Turk, the association’s director of government affairs.
The association contends that its members adhere to safe manufacturing processes, random product testing, and appropriate marketing guidelines. Representatives also worry that if minors can’t buy supplements over the counter, they may buy them from “crooks” on the black market and undermine the integrity of the industry. Under the bills, minors purchasing weight-loss products must show identification along with a prescription.
Not all business groups oppose the ban. The American Herbal Products Association, a trade group representing dietary supplement manufacturers and retailers, dropped its opposition to California’s bill once it was amended to remove ingredient categories that are found in non-diet supplements and vitamins, according to Robert Marriott, director of regulatory affairs.
Children’s advocates have found worrisome trends among young people who envision their ideal body type based on what they see on social media. According to a study commissioned by Fairplay, a nonprofit that seeks to stop harmful marketing practices targeting children, kids as young as 9 were found to be following three or more eating disorder accounts on Instagram, while the median age was 19. The authors called it a “pro–eating disorder bubble.”
Meta, which owns Instagram and Facebook, said the report lacks nuance, such as recognizing the human need to share life’s difficult moments. The company argues that blanket censorship isn’t the answer. “Experts and safety organizations have told us it’s important to strike a balance and allow people to share their personal stories while removing any content that encourages or promotes eating disorders,” Liza Crenshaw, a Meta spokesperson, said in an email.
Jason Nagata, MD, a pediatrician who cares for children and young adults with life-threatening eating disorders, believes that easy access to diet pills contributes to his patients’ conditions at UCSF Benioff Children’s Hospital in San Francisco. That was the case for one of his patients, an emaciated 11-year-old girl.
“She had basically entered a starvation state because she was not getting enough nutrition,” said Dr. Nagata, who provided supporting testimony for the California bill. “She was taking these pills and using other kinds of extreme behaviors to lose weight.”
Dr. Nagata said the number of patients he sees with eating disorders has tripled since the pandemic began. They are desperate to get diet pills, some with modest results. “We’ve had patients who have been so dependent on these products that they will be hospitalized and they’re still ordering these products on Amazon,” he said.
Public health advocates turned to state legislatures in response to the federal government’s limited authority to regulate diet pills. Under a 1994 federal law known as the Dietary Supplement Health and Education Act, the FDA “cannot step in until after there is a clear issue of harm to consumers,” said Dr. Austin.
No match for the supplement industry’s heavy lobbying on Capitol Hill, public health advocates shifted to a state-by-state approach.
There is, however, a push for the FDA to improve oversight of what goes into diet pills. Sen. Dick Durbin (D-Ill.) in April introduced a bill that would require dietary supplement manufacturers to register their products – along with the ingredients – with the regulator.
Proponents say the change is needed because manufacturers have been known to include dangerous ingredients. C. Michael White, PharmD, of the University of Connecticut, Storrs, found 35% of tainted health products came from weight-loss supplements in a review of a health fraud database.
A few ingredients have been banned, including sibutramine, a stimulant. “It was a very commonly used weight-loss supplement that ended up being removed from the U.S. market because of its elevated risk of causing things like heart attacks, strokes, and arrhythmias,” Dr. White said.
Another ingredient was phenolphthalein, which was used in laxatives until it was identified as a suspected carcinogen and banned in 1999. “To think,” he said, “that that product would still be on the U.S. market is just unconscionable.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
California and New York are on the cusp of going further than the Food and Drug Administration in restricting the sale of nonprescription diet pills to minors as pediatricians and public health advocates try to protect kids from extreme weight-loss gimmicks online.
A bill before Gov. Gavin Newsom would bar anyone under 18 in California from buying over-the-counter weight-loss supplements – whether online or in shops – without a prescription. A similar bill passed by New York lawmakers is on Gov. Kathy Hochul’s desk. Neither Democrat has indicated how he or she will act.
If both bills are signed into law, proponents hope the momentum will build to restrict diet pill sales to children in more states. Massachusetts, New Jersey, and Missouri have introduced similar bills and backers plan to continue their push next year.
Nearly 30 million people in the United States will have an eating disorder in their lifetime; 95% of them are aged between 12 and 25, according to Johns Hopkins All Children’s Hospital. The hospital added that eating disorders pose the highest risk of mortality of any mental health disorder. And it has become easier than ever for minors to get pills that are sold online or on drugstore shelves. All dietary supplements, which include those for weight loss, accounted for nearly 35% of the $63 billion over-the-counter health products industry in 2021, according to Vision Research Reports, a market research firm.
Dietary supplements, which encompass a broad range of vitamins, herbs, and minerals, are classified by the FDA as food and don’t undergo scientific and safety testing as prescription drugs and over-the-counter medicines do.
Public health advocates want to keep weight-loss products – with ads that may promise to “Drop 5 pounds a week!” and pill names like Slim Sense – away from young people, particularly girls, since some research has linked some products to eating disorders. A study in the American Journal of Public Health, which followed more than 10,000 women aged 14-36 over 15 years, found that “those who used diet pills had more than 5 times higher adjusted odds of receiving an eating disorder diagnosis from a health care provider within 1-3 years than those who did not.”
Many pills have been found tainted with banned and dangerous ingredients that may cause cancer, heart attacks, strokes, and other ailments. For example, the FDA advised the public to avoid Slim Sense by Dr. Reade because it contains lorcaserin, which has been found to cause psychiatric disturbances and impairments in attention or memory. The FDA ordered it discontinued and the company couldn’t be reached for comment.
“Unscrupulous manufacturers are willing to take risks with consumers’ health – and they are lacing their products with illegal pharmaceuticals, banned pharmaceuticals, steroids, excessive stimulants, even experimental stimulants,” said S. Bryn Austin, ScD, founding director of the Strategic Training Initiative for the Prevention of Eating Disorders, or STRIPED, which supports the restrictions. “Consumers have no idea that this is what’s in these types of products.”
STRIPED is a public health initiative based at the Harvard School of Public Health, Boston, and Boston Children’s Hospital.
An industry trade group, the Natural Products Association, disputes that diet pills cause eating disorders, citing the lack of consumer complaints to the FDA of adverse events from their members’ products. “According to FDA data, there is no association between the two,” said Kyle Turk, the association’s director of government affairs.
The association contends that its members adhere to safe manufacturing processes, random product testing, and appropriate marketing guidelines. Representatives also worry that if minors can’t buy supplements over the counter, they may buy them from “crooks” on the black market and undermine the integrity of the industry. Under the bills, minors purchasing weight-loss products must show identification along with a prescription.
Not all business groups oppose the ban. The American Herbal Products Association, a trade group representing dietary supplement manufacturers and retailers, dropped its opposition to California’s bill once it was amended to remove ingredient categories that are found in non-diet supplements and vitamins, according to Robert Marriott, director of regulatory affairs.
Children’s advocates have found worrisome trends among young people who envision their ideal body type based on what they see on social media. According to a study commissioned by Fairplay, a nonprofit that seeks to stop harmful marketing practices targeting children, kids as young as 9 were found to be following three or more eating disorder accounts on Instagram, while the median age was 19. The authors called it a “pro–eating disorder bubble.”
Meta, which owns Instagram and Facebook, said the report lacks nuance, such as recognizing the human need to share life’s difficult moments. The company argues that blanket censorship isn’t the answer. “Experts and safety organizations have told us it’s important to strike a balance and allow people to share their personal stories while removing any content that encourages or promotes eating disorders,” Liza Crenshaw, a Meta spokesperson, said in an email.
Jason Nagata, MD, a pediatrician who cares for children and young adults with life-threatening eating disorders, believes that easy access to diet pills contributes to his patients’ conditions at UCSF Benioff Children’s Hospital in San Francisco. That was the case for one of his patients, an emaciated 11-year-old girl.
“She had basically entered a starvation state because she was not getting enough nutrition,” said Dr. Nagata, who provided supporting testimony for the California bill. “She was taking these pills and using other kinds of extreme behaviors to lose weight.”
Dr. Nagata said the number of patients he sees with eating disorders has tripled since the pandemic began. They are desperate to get diet pills, some with modest results. “We’ve had patients who have been so dependent on these products that they will be hospitalized and they’re still ordering these products on Amazon,” he said.
Public health advocates turned to state legislatures in response to the federal government’s limited authority to regulate diet pills. Under a 1994 federal law known as the Dietary Supplement Health and Education Act, the FDA “cannot step in until after there is a clear issue of harm to consumers,” said Dr. Austin.
No match for the supplement industry’s heavy lobbying on Capitol Hill, public health advocates shifted to a state-by-state approach.
There is, however, a push for the FDA to improve oversight of what goes into diet pills. Sen. Dick Durbin (D-Ill.) in April introduced a bill that would require dietary supplement manufacturers to register their products – along with the ingredients – with the regulator.
Proponents say the change is needed because manufacturers have been known to include dangerous ingredients. C. Michael White, PharmD, of the University of Connecticut, Storrs, found 35% of tainted health products came from weight-loss supplements in a review of a health fraud database.
A few ingredients have been banned, including sibutramine, a stimulant. “It was a very commonly used weight-loss supplement that ended up being removed from the U.S. market because of its elevated risk of causing things like heart attacks, strokes, and arrhythmias,” Dr. White said.
Another ingredient was phenolphthalein, which was used in laxatives until it was identified as a suspected carcinogen and banned in 1999. “To think,” he said, “that that product would still be on the U.S. market is just unconscionable.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
California and New York are on the cusp of going further than the Food and Drug Administration in restricting the sale of nonprescription diet pills to minors as pediatricians and public health advocates try to protect kids from extreme weight-loss gimmicks online.
A bill before Gov. Gavin Newsom would bar anyone under 18 in California from buying over-the-counter weight-loss supplements – whether online or in shops – without a prescription. A similar bill passed by New York lawmakers is on Gov. Kathy Hochul’s desk. Neither Democrat has indicated how he or she will act.
If both bills are signed into law, proponents hope the momentum will build to restrict diet pill sales to children in more states. Massachusetts, New Jersey, and Missouri have introduced similar bills and backers plan to continue their push next year.
Nearly 30 million people in the United States will have an eating disorder in their lifetime; 95% of them are aged between 12 and 25, according to Johns Hopkins All Children’s Hospital. The hospital added that eating disorders pose the highest risk of mortality of any mental health disorder. And it has become easier than ever for minors to get pills that are sold online or on drugstore shelves. All dietary supplements, which include those for weight loss, accounted for nearly 35% of the $63 billion over-the-counter health products industry in 2021, according to Vision Research Reports, a market research firm.
Dietary supplements, which encompass a broad range of vitamins, herbs, and minerals, are classified by the FDA as food and don’t undergo scientific and safety testing as prescription drugs and over-the-counter medicines do.
Public health advocates want to keep weight-loss products – with ads that may promise to “Drop 5 pounds a week!” and pill names like Slim Sense – away from young people, particularly girls, since some research has linked some products to eating disorders. A study in the American Journal of Public Health, which followed more than 10,000 women aged 14-36 over 15 years, found that “those who used diet pills had more than 5 times higher adjusted odds of receiving an eating disorder diagnosis from a health care provider within 1-3 years than those who did not.”
Many pills have been found tainted with banned and dangerous ingredients that may cause cancer, heart attacks, strokes, and other ailments. For example, the FDA advised the public to avoid Slim Sense by Dr. Reade because it contains lorcaserin, which has been found to cause psychiatric disturbances and impairments in attention or memory. The FDA ordered it discontinued and the company couldn’t be reached for comment.
“Unscrupulous manufacturers are willing to take risks with consumers’ health – and they are lacing their products with illegal pharmaceuticals, banned pharmaceuticals, steroids, excessive stimulants, even experimental stimulants,” said S. Bryn Austin, ScD, founding director of the Strategic Training Initiative for the Prevention of Eating Disorders, or STRIPED, which supports the restrictions. “Consumers have no idea that this is what’s in these types of products.”
STRIPED is a public health initiative based at the Harvard School of Public Health, Boston, and Boston Children’s Hospital.
An industry trade group, the Natural Products Association, disputes that diet pills cause eating disorders, citing the lack of consumer complaints to the FDA of adverse events from their members’ products. “According to FDA data, there is no association between the two,” said Kyle Turk, the association’s director of government affairs.
The association contends that its members adhere to safe manufacturing processes, random product testing, and appropriate marketing guidelines. Representatives also worry that if minors can’t buy supplements over the counter, they may buy them from “crooks” on the black market and undermine the integrity of the industry. Under the bills, minors purchasing weight-loss products must show identification along with a prescription.
Not all business groups oppose the ban. The American Herbal Products Association, a trade group representing dietary supplement manufacturers and retailers, dropped its opposition to California’s bill once it was amended to remove ingredient categories that are found in non-diet supplements and vitamins, according to Robert Marriott, director of regulatory affairs.
Children’s advocates have found worrisome trends among young people who envision their ideal body type based on what they see on social media. According to a study commissioned by Fairplay, a nonprofit that seeks to stop harmful marketing practices targeting children, kids as young as 9 were found to be following three or more eating disorder accounts on Instagram, while the median age was 19. The authors called it a “pro–eating disorder bubble.”
Meta, which owns Instagram and Facebook, said the report lacks nuance, such as recognizing the human need to share life’s difficult moments. The company argues that blanket censorship isn’t the answer. “Experts and safety organizations have told us it’s important to strike a balance and allow people to share their personal stories while removing any content that encourages or promotes eating disorders,” Liza Crenshaw, a Meta spokesperson, said in an email.
Jason Nagata, MD, a pediatrician who cares for children and young adults with life-threatening eating disorders, believes that easy access to diet pills contributes to his patients’ conditions at UCSF Benioff Children’s Hospital in San Francisco. That was the case for one of his patients, an emaciated 11-year-old girl.
“She had basically entered a starvation state because she was not getting enough nutrition,” said Dr. Nagata, who provided supporting testimony for the California bill. “She was taking these pills and using other kinds of extreme behaviors to lose weight.”
Dr. Nagata said the number of patients he sees with eating disorders has tripled since the pandemic began. They are desperate to get diet pills, some with modest results. “We’ve had patients who have been so dependent on these products that they will be hospitalized and they’re still ordering these products on Amazon,” he said.
Public health advocates turned to state legislatures in response to the federal government’s limited authority to regulate diet pills. Under a 1994 federal law known as the Dietary Supplement Health and Education Act, the FDA “cannot step in until after there is a clear issue of harm to consumers,” said Dr. Austin.
No match for the supplement industry’s heavy lobbying on Capitol Hill, public health advocates shifted to a state-by-state approach.
There is, however, a push for the FDA to improve oversight of what goes into diet pills. Sen. Dick Durbin (D-Ill.) in April introduced a bill that would require dietary supplement manufacturers to register their products – along with the ingredients – with the regulator.
Proponents say the change is needed because manufacturers have been known to include dangerous ingredients. C. Michael White, PharmD, of the University of Connecticut, Storrs, found 35% of tainted health products came from weight-loss supplements in a review of a health fraud database.
A few ingredients have been banned, including sibutramine, a stimulant. “It was a very commonly used weight-loss supplement that ended up being removed from the U.S. market because of its elevated risk of causing things like heart attacks, strokes, and arrhythmias,” Dr. White said.
Another ingredient was phenolphthalein, which was used in laxatives until it was identified as a suspected carcinogen and banned in 1999. “To think,” he said, “that that product would still be on the U.S. market is just unconscionable.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
People really can get ‘hangry’ when hungry
The notion that people get ‘hangry’ – irritable and short-tempered when they’re hungry – is such an established part of modern folklore that the word has even been added to the Oxford English Dictionary. Although experimental studies in the past have shown that low blood glucose levels increase impulsivity, anger, and aggression, there has been little solid evidence that this translates to real-life settings.
Now new research has confirmed that the phenomenon does really exist in everyday life. The study, published in the journal PLOS ONE, is the first to investigate how hunger affects people’s emotions on a day-to-day level. Lead author Viren Swami, professor of social psychology at Anglia Ruskin University, Cambridge, England, said: “Many of us are aware that being hungry can influence our emotions, but surprisingly little scientific research has focused on being ‘hangry’.”
He and coauthors from Karl Landsteiner University of Health Sciences in Krems an der Donau, Austria, recruited 64 participants from Central Europe who completed a 21-day experience sampling phase, in which they were prompted to report their feelings on a smartphone app five times a day. At each prompt, they reported their levels of hunger, anger, irritability, pleasure, and arousal on a visual analog scale.
Participants were on average 29.9 years old (range = 18-60), predominantly (81.3%) women, and had a mean body mass index of 23.8 kg/m2 (range 15.8-36.5 kg/m2).
Anger was rated on a 5-point scale but the team explained that the effects of hunger are unlikely to be unique to anger per se, so they also asked about experiences of irritability and, in order to obtain a more holistic view of emotionality, also about pleasure and arousal, as indexed using Russell’s affect grid.
They also asked about eating behaviors over the previous 3 weeks, including frequency of main meals, snacking behavior, healthy eating, feeling hungry, and sense of satiety, and about dietary behaviors including restrictive eating, emotionally induced eating, and externally determined eating behavior.
Analysis of the resulting total of 9,142 responses showed that higher levels of self-reported hunger were associated with greater feelings of anger and irritability, and with lower levels of pleasure. These findings remained significant after accounting for participants’ sex, age, body mass index, dietary behaviors, and trait anger. However, associations with arousal were not significant.
The authors commented that the use of the app allowed data collection to take place in subjects’ everyday environments, such as their workplace and at home. “These results provide evidence that everyday levels of hunger are associated with negative emotionality and supports the notion of being ‘hangry.’ ”
‘Substantial’ effects
“The effects were substantial,” the team said, “even after taking into account demographic factors” such as age and sex, body mass index, dietary behavior, and individual personality traits. Hunger was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants.
The research also showed that the negative emotions – irritability, anger, and unpleasantness – were caused by both day-to-day fluctuations in hunger and residual levels of hunger measured by averages over the 3-week period.
The authors said their findings “suggest that the experience of being hangry is real, insofar as hunger was associated with greater anger and irritability, and lower pleasure, in our sample over a period of 3 weeks.
“These results may have important implications for understanding everyday experiences of emotions, and may also assist practitioners to more effectively ensure productive individual behaviors and interpersonal relationships (for example, by ensuring that no one goes hungry).”
Although the majority of participants (55%) said they paid attention to hunger pangs, only 23% said that they knew when they were full and then stopped eating, whereas 63% said they could tell when they were full but sometimes continued to eat. Few (4.7%) people said they could not tell when they were full and therefore oriented their eating based on the size of the meal, but 9% described frequent overeating because of not feeling satiated, and 13% stated they ate when they were stressed, upset, angry, or bored.
Professor Swami said: “Ours is the first study to examine being ‘hangry’ outside of a lab. By following people in their day-to-day lives, we found that hunger was related to levels of anger, irritability, and pleasure.
“Although our study doesn’t present ways to mitigate negative hunger-induced emotions, research suggests that being able to label an emotion can help people to regulate it, such as by recognizing that we feel angry simply because we are hungry. Therefore, greater awareness of being ‘hangry’ could reduce the likelihood that hunger results in negative emotions and behaviors in individuals.”
A version of this article first appeared on Medscape UK.
The notion that people get ‘hangry’ – irritable and short-tempered when they’re hungry – is such an established part of modern folklore that the word has even been added to the Oxford English Dictionary. Although experimental studies in the past have shown that low blood glucose levels increase impulsivity, anger, and aggression, there has been little solid evidence that this translates to real-life settings.
Now new research has confirmed that the phenomenon does really exist in everyday life. The study, published in the journal PLOS ONE, is the first to investigate how hunger affects people’s emotions on a day-to-day level. Lead author Viren Swami, professor of social psychology at Anglia Ruskin University, Cambridge, England, said: “Many of us are aware that being hungry can influence our emotions, but surprisingly little scientific research has focused on being ‘hangry’.”
He and coauthors from Karl Landsteiner University of Health Sciences in Krems an der Donau, Austria, recruited 64 participants from Central Europe who completed a 21-day experience sampling phase, in which they were prompted to report their feelings on a smartphone app five times a day. At each prompt, they reported their levels of hunger, anger, irritability, pleasure, and arousal on a visual analog scale.
Participants were on average 29.9 years old (range = 18-60), predominantly (81.3%) women, and had a mean body mass index of 23.8 kg/m2 (range 15.8-36.5 kg/m2).
Anger was rated on a 5-point scale but the team explained that the effects of hunger are unlikely to be unique to anger per se, so they also asked about experiences of irritability and, in order to obtain a more holistic view of emotionality, also about pleasure and arousal, as indexed using Russell’s affect grid.
They also asked about eating behaviors over the previous 3 weeks, including frequency of main meals, snacking behavior, healthy eating, feeling hungry, and sense of satiety, and about dietary behaviors including restrictive eating, emotionally induced eating, and externally determined eating behavior.
Analysis of the resulting total of 9,142 responses showed that higher levels of self-reported hunger were associated with greater feelings of anger and irritability, and with lower levels of pleasure. These findings remained significant after accounting for participants’ sex, age, body mass index, dietary behaviors, and trait anger. However, associations with arousal were not significant.
The authors commented that the use of the app allowed data collection to take place in subjects’ everyday environments, such as their workplace and at home. “These results provide evidence that everyday levels of hunger are associated with negative emotionality and supports the notion of being ‘hangry.’ ”
‘Substantial’ effects
“The effects were substantial,” the team said, “even after taking into account demographic factors” such as age and sex, body mass index, dietary behavior, and individual personality traits. Hunger was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants.
The research also showed that the negative emotions – irritability, anger, and unpleasantness – were caused by both day-to-day fluctuations in hunger and residual levels of hunger measured by averages over the 3-week period.
The authors said their findings “suggest that the experience of being hangry is real, insofar as hunger was associated with greater anger and irritability, and lower pleasure, in our sample over a period of 3 weeks.
“These results may have important implications for understanding everyday experiences of emotions, and may also assist practitioners to more effectively ensure productive individual behaviors and interpersonal relationships (for example, by ensuring that no one goes hungry).”
Although the majority of participants (55%) said they paid attention to hunger pangs, only 23% said that they knew when they were full and then stopped eating, whereas 63% said they could tell when they were full but sometimes continued to eat. Few (4.7%) people said they could not tell when they were full and therefore oriented their eating based on the size of the meal, but 9% described frequent overeating because of not feeling satiated, and 13% stated they ate when they were stressed, upset, angry, or bored.
Professor Swami said: “Ours is the first study to examine being ‘hangry’ outside of a lab. By following people in their day-to-day lives, we found that hunger was related to levels of anger, irritability, and pleasure.
“Although our study doesn’t present ways to mitigate negative hunger-induced emotions, research suggests that being able to label an emotion can help people to regulate it, such as by recognizing that we feel angry simply because we are hungry. Therefore, greater awareness of being ‘hangry’ could reduce the likelihood that hunger results in negative emotions and behaviors in individuals.”
A version of this article first appeared on Medscape UK.
The notion that people get ‘hangry’ – irritable and short-tempered when they’re hungry – is such an established part of modern folklore that the word has even been added to the Oxford English Dictionary. Although experimental studies in the past have shown that low blood glucose levels increase impulsivity, anger, and aggression, there has been little solid evidence that this translates to real-life settings.
Now new research has confirmed that the phenomenon does really exist in everyday life. The study, published in the journal PLOS ONE, is the first to investigate how hunger affects people’s emotions on a day-to-day level. Lead author Viren Swami, professor of social psychology at Anglia Ruskin University, Cambridge, England, said: “Many of us are aware that being hungry can influence our emotions, but surprisingly little scientific research has focused on being ‘hangry’.”
He and coauthors from Karl Landsteiner University of Health Sciences in Krems an der Donau, Austria, recruited 64 participants from Central Europe who completed a 21-day experience sampling phase, in which they were prompted to report their feelings on a smartphone app five times a day. At each prompt, they reported their levels of hunger, anger, irritability, pleasure, and arousal on a visual analog scale.
Participants were on average 29.9 years old (range = 18-60), predominantly (81.3%) women, and had a mean body mass index of 23.8 kg/m2 (range 15.8-36.5 kg/m2).
Anger was rated on a 5-point scale but the team explained that the effects of hunger are unlikely to be unique to anger per se, so they also asked about experiences of irritability and, in order to obtain a more holistic view of emotionality, also about pleasure and arousal, as indexed using Russell’s affect grid.
They also asked about eating behaviors over the previous 3 weeks, including frequency of main meals, snacking behavior, healthy eating, feeling hungry, and sense of satiety, and about dietary behaviors including restrictive eating, emotionally induced eating, and externally determined eating behavior.
Analysis of the resulting total of 9,142 responses showed that higher levels of self-reported hunger were associated with greater feelings of anger and irritability, and with lower levels of pleasure. These findings remained significant after accounting for participants’ sex, age, body mass index, dietary behaviors, and trait anger. However, associations with arousal were not significant.
The authors commented that the use of the app allowed data collection to take place in subjects’ everyday environments, such as their workplace and at home. “These results provide evidence that everyday levels of hunger are associated with negative emotionality and supports the notion of being ‘hangry.’ ”
‘Substantial’ effects
“The effects were substantial,” the team said, “even after taking into account demographic factors” such as age and sex, body mass index, dietary behavior, and individual personality traits. Hunger was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants.
The research also showed that the negative emotions – irritability, anger, and unpleasantness – were caused by both day-to-day fluctuations in hunger and residual levels of hunger measured by averages over the 3-week period.
The authors said their findings “suggest that the experience of being hangry is real, insofar as hunger was associated with greater anger and irritability, and lower pleasure, in our sample over a period of 3 weeks.
“These results may have important implications for understanding everyday experiences of emotions, and may also assist practitioners to more effectively ensure productive individual behaviors and interpersonal relationships (for example, by ensuring that no one goes hungry).”
Although the majority of participants (55%) said they paid attention to hunger pangs, only 23% said that they knew when they were full and then stopped eating, whereas 63% said they could tell when they were full but sometimes continued to eat. Few (4.7%) people said they could not tell when they were full and therefore oriented their eating based on the size of the meal, but 9% described frequent overeating because of not feeling satiated, and 13% stated they ate when they were stressed, upset, angry, or bored.
Professor Swami said: “Ours is the first study to examine being ‘hangry’ outside of a lab. By following people in their day-to-day lives, we found that hunger was related to levels of anger, irritability, and pleasure.
“Although our study doesn’t present ways to mitigate negative hunger-induced emotions, research suggests that being able to label an emotion can help people to regulate it, such as by recognizing that we feel angry simply because we are hungry. Therefore, greater awareness of being ‘hangry’ could reduce the likelihood that hunger results in negative emotions and behaviors in individuals.”
A version of this article first appeared on Medscape UK.
FROM PLOS ONE
Anorexia linked to notable shrinkage of key brain structures
, a new brain imaging study shows.
The reductions of cortical thickness, subcortical volumes, and cortical surface area were “very pronounced in acutely underweight anorexia,” Stefan Ehrlich, MD, PhD, head of the Eating Disorder Treatment and Research Center, Technical University, Dresden, Germany, told this news organization.
Yet even a “partial weight gain brings some normalization of these shrinkages. From this it can be deduced that a fast/early normalization of weight is also very important for brain health,” said Dr. Ehrlich.
The study was published online in Biological Psychiatry.
‘A wake-up call’
Researchers with the international ENIGMA Eating Disorders Working Group analyzed T1-weighted structural magnetic resonance imaging scans for nearly 2,000 people with AN (including those in recovery) and healthy controls across 22 sites worldwide.
In the AN sample, reductions in cortical thickness, subcortical volumes, and, to a lesser extent, cortical surface area, were “sizable (Cohen’s d up to 0.95), widespread, and co-localized with hub regions,” they report.
These reductions were two and four times larger than the abnormalities in brain size and shape seen in patients with other mental illnesses, the researchers note.
Noting the harmful impact of anorexia-related undernutrition on the brain, these deficits were associated with lower body mass index in the AN sample and were less severe in partially weight-restored patients – implying that, with appropriate early treatment and support, the brain might be able to repair itself, the investigators note.
“This really is a wake-up call, showing the need for early interventions for people with eating disorders,” Paul Thompson, PhD, author and lead scientist for the ENIGMA Consortium, said in a news release.
“The international scale of this work is extraordinary. Scientists from 22 centers worldwide pooled their brain scans to create the most detailed picture to date of how anorexia affects the brain,” Dr. Thompson added.
“The brain changes in anorexia were more severe than in other any psychiatric condition we have studied. Effects of treatments and interventions can now be evaluated, using these new brain maps as a reference,” he noted.
Immediate clinical implications
Reached for comment, Allison Eliscu, MD, chief of the division of adolescent medicine, department of pediatrics, at Stony Brook (N.Y.) University, said the findings have immediate implications for clinical care.
“When we talk to our patients and the parents, a lot of them focus on things that they can see, such as the way they look. It adds a lot to the conversation to be able to say: You’re obviously not seeing these changes in the brain, but they’re happening and could be potentially long term if you don’t start weight restoring, or if you weight restore and then continue to drop again,” Dr. Eliscu said in an interview.
The findings, she said, really do highlight what anorexia can do to the brain.
“Adolescents need to know, anorexia can absolutely decrease the size of your brain in different areas; you’re not just losing weight in your belly and your thighs, you’re losing weight in the brain as well and that’s really concerning,” said Dr. Eliscu.
The study had no commercial funding. The authors and Dr. Eliscu report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
, a new brain imaging study shows.
The reductions of cortical thickness, subcortical volumes, and cortical surface area were “very pronounced in acutely underweight anorexia,” Stefan Ehrlich, MD, PhD, head of the Eating Disorder Treatment and Research Center, Technical University, Dresden, Germany, told this news organization.
Yet even a “partial weight gain brings some normalization of these shrinkages. From this it can be deduced that a fast/early normalization of weight is also very important for brain health,” said Dr. Ehrlich.
The study was published online in Biological Psychiatry.
‘A wake-up call’
Researchers with the international ENIGMA Eating Disorders Working Group analyzed T1-weighted structural magnetic resonance imaging scans for nearly 2,000 people with AN (including those in recovery) and healthy controls across 22 sites worldwide.
In the AN sample, reductions in cortical thickness, subcortical volumes, and, to a lesser extent, cortical surface area, were “sizable (Cohen’s d up to 0.95), widespread, and co-localized with hub regions,” they report.
These reductions were two and four times larger than the abnormalities in brain size and shape seen in patients with other mental illnesses, the researchers note.
Noting the harmful impact of anorexia-related undernutrition on the brain, these deficits were associated with lower body mass index in the AN sample and were less severe in partially weight-restored patients – implying that, with appropriate early treatment and support, the brain might be able to repair itself, the investigators note.
“This really is a wake-up call, showing the need for early interventions for people with eating disorders,” Paul Thompson, PhD, author and lead scientist for the ENIGMA Consortium, said in a news release.
“The international scale of this work is extraordinary. Scientists from 22 centers worldwide pooled their brain scans to create the most detailed picture to date of how anorexia affects the brain,” Dr. Thompson added.
“The brain changes in anorexia were more severe than in other any psychiatric condition we have studied. Effects of treatments and interventions can now be evaluated, using these new brain maps as a reference,” he noted.
Immediate clinical implications
Reached for comment, Allison Eliscu, MD, chief of the division of adolescent medicine, department of pediatrics, at Stony Brook (N.Y.) University, said the findings have immediate implications for clinical care.
“When we talk to our patients and the parents, a lot of them focus on things that they can see, such as the way they look. It adds a lot to the conversation to be able to say: You’re obviously not seeing these changes in the brain, but they’re happening and could be potentially long term if you don’t start weight restoring, or if you weight restore and then continue to drop again,” Dr. Eliscu said in an interview.
The findings, she said, really do highlight what anorexia can do to the brain.
“Adolescents need to know, anorexia can absolutely decrease the size of your brain in different areas; you’re not just losing weight in your belly and your thighs, you’re losing weight in the brain as well and that’s really concerning,” said Dr. Eliscu.
The study had no commercial funding. The authors and Dr. Eliscu report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
, a new brain imaging study shows.
The reductions of cortical thickness, subcortical volumes, and cortical surface area were “very pronounced in acutely underweight anorexia,” Stefan Ehrlich, MD, PhD, head of the Eating Disorder Treatment and Research Center, Technical University, Dresden, Germany, told this news organization.
Yet even a “partial weight gain brings some normalization of these shrinkages. From this it can be deduced that a fast/early normalization of weight is also very important for brain health,” said Dr. Ehrlich.
The study was published online in Biological Psychiatry.
‘A wake-up call’
Researchers with the international ENIGMA Eating Disorders Working Group analyzed T1-weighted structural magnetic resonance imaging scans for nearly 2,000 people with AN (including those in recovery) and healthy controls across 22 sites worldwide.
In the AN sample, reductions in cortical thickness, subcortical volumes, and, to a lesser extent, cortical surface area, were “sizable (Cohen’s d up to 0.95), widespread, and co-localized with hub regions,” they report.
These reductions were two and four times larger than the abnormalities in brain size and shape seen in patients with other mental illnesses, the researchers note.
Noting the harmful impact of anorexia-related undernutrition on the brain, these deficits were associated with lower body mass index in the AN sample and were less severe in partially weight-restored patients – implying that, with appropriate early treatment and support, the brain might be able to repair itself, the investigators note.
“This really is a wake-up call, showing the need for early interventions for people with eating disorders,” Paul Thompson, PhD, author and lead scientist for the ENIGMA Consortium, said in a news release.
“The international scale of this work is extraordinary. Scientists from 22 centers worldwide pooled their brain scans to create the most detailed picture to date of how anorexia affects the brain,” Dr. Thompson added.
“The brain changes in anorexia were more severe than in other any psychiatric condition we have studied. Effects of treatments and interventions can now be evaluated, using these new brain maps as a reference,” he noted.
Immediate clinical implications
Reached for comment, Allison Eliscu, MD, chief of the division of adolescent medicine, department of pediatrics, at Stony Brook (N.Y.) University, said the findings have immediate implications for clinical care.
“When we talk to our patients and the parents, a lot of them focus on things that they can see, such as the way they look. It adds a lot to the conversation to be able to say: You’re obviously not seeing these changes in the brain, but they’re happening and could be potentially long term if you don’t start weight restoring, or if you weight restore and then continue to drop again,” Dr. Eliscu said in an interview.
The findings, she said, really do highlight what anorexia can do to the brain.
“Adolescents need to know, anorexia can absolutely decrease the size of your brain in different areas; you’re not just losing weight in your belly and your thighs, you’re losing weight in the brain as well and that’s really concerning,” said Dr. Eliscu.
The study had no commercial funding. The authors and Dr. Eliscu report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM BIOLOGICAL PSYCHIATRY
Youth with bipolar disorder at high risk of eating disorders
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.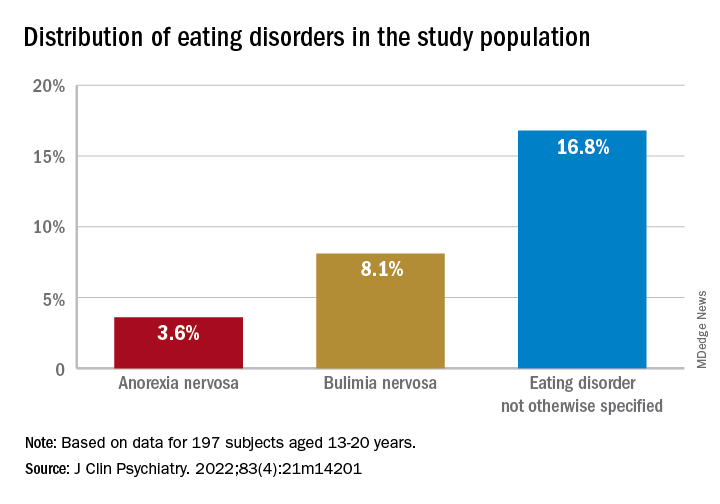
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.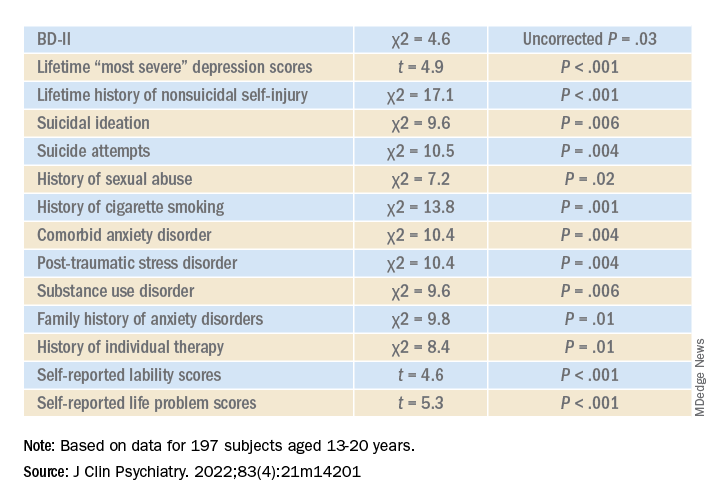
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”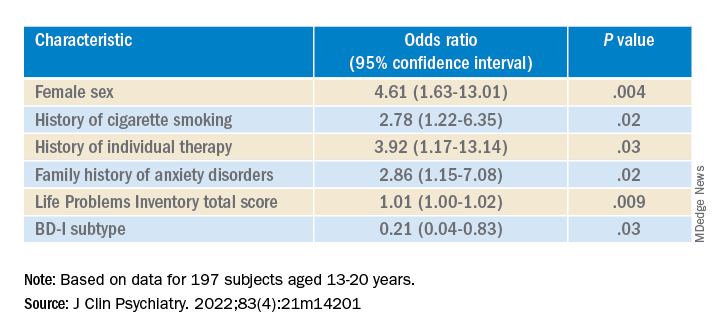
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.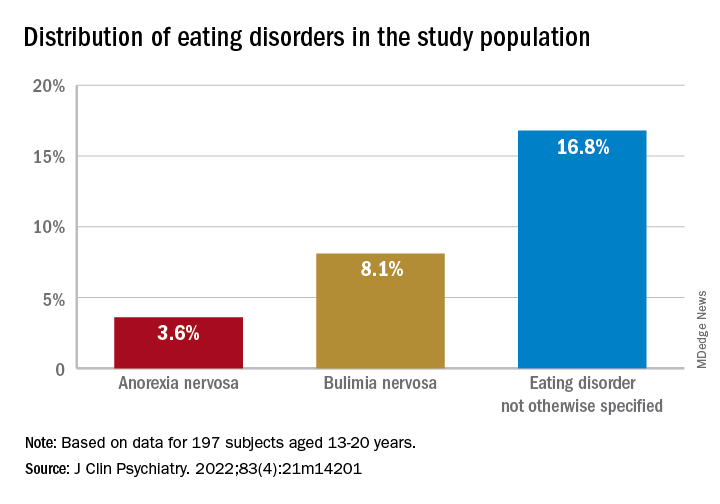
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.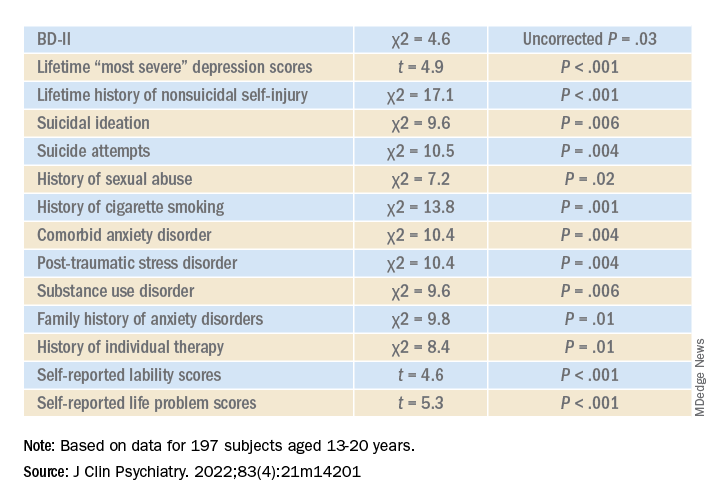
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”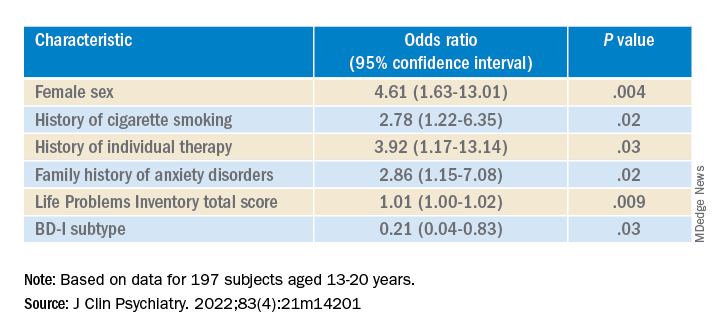
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.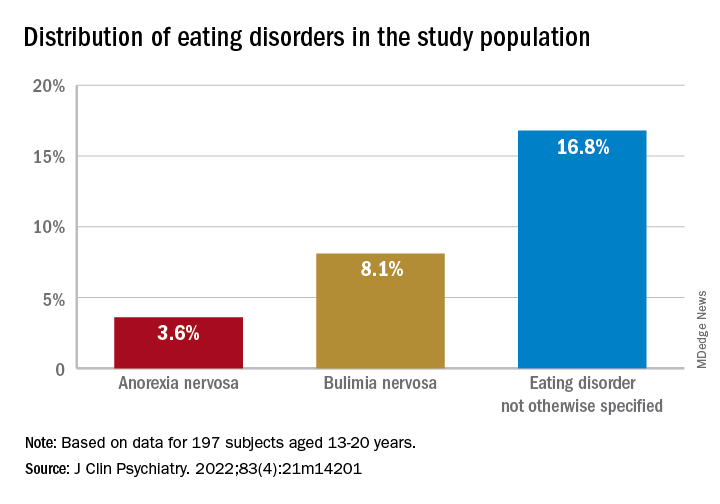
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.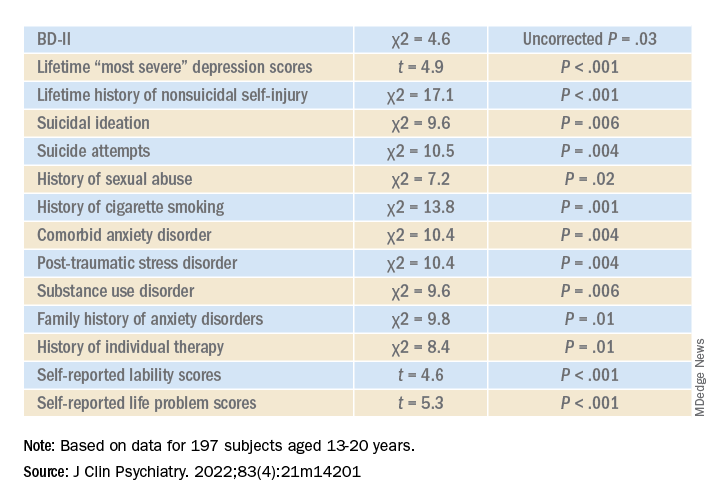
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”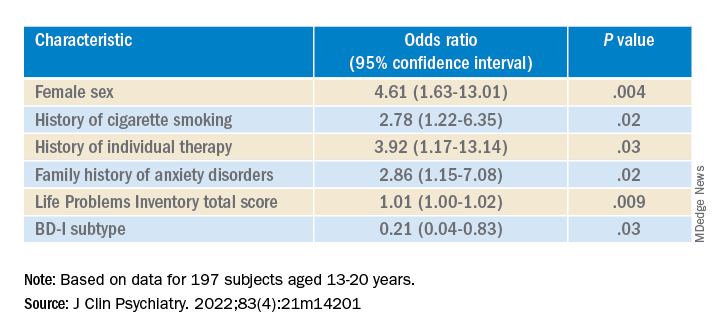
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
New tool may identify pregnant women with eating disorders
A newly developed screening tool may help clinicians identify pregnant women with eating disorders.
The 12-question instrument is intended to be a quick way to help clinicians identify women who may need to be referred to a mental health expert for further evaluation, according to the researchers, who reported on the instrument in a study published in Archives of Women’s Mental Health.
“It would be most appropriate for clinical encounters so that women can get screened and referred,” said Elizabeth Claydon, MD, assistant professor in the department of social and behavioral sciences at West Virginia University’s School of Public Health, Morgantown, who led the study. “If you miss it, they may carry on their eating disorder throughout their pregnancy.”
Pregnant women who have an eating disorder are at increased risk for gestational diabetes, premature birth, labor complications, difficulties nursing, and postpartum depression, according to the National Eating Disorders Association. Their babies are at increased risk for premature birth, low birth weight, and poor development. However, clinicians have not had an accurate way of screening pregnant women who may have an eating disorder.
The American College of Obstetricians and Gynecologists offered its first clinical guidelines for managing anorexia in pregnancy in April 2022. The group’s recommendations include regular monitoring of cardiac and liver function, blood pressure, and heart rate, as well as tests to monitor iron, sodium, potassium, bone density, and blood sugar levels. Anorexia, bulimia, binge eating, and subthreshold disorders – also known as other specified feeding or eating disorders – are among the most common eating disorders among pregnant women.
There are no recent data on the incidence or prevalence of eating disorders among pregnant women, according to Lauren Smolar, vice president of mission and education at the National Eating Disorders Association.
“It’s hard to capture the number of pregnant women affected, since it so often goes undetected,” Ms. Smolar said.
Existing screening tools for eating disorders ask patients whether they’re currently pregnant; a questionnaire specifically tailored to pregnant women may help to better gather data on the prevalence within this group, Ms. Smolar said.
For the new study, Dr. Claydon and her colleagues tested the questionnaire among more than 400 mostly White women aged 25-34 years. They found that it could reliably identify women who may have an eating disorder. The questionnaire was validated for women to take during any trimester, according to the findings.
A score of 39 or above would serve as an indicator for follow-up. Women who score at least 39 were up to 16 times more likely to receive a diagnosis of an eating disorder, compared with women who scored less, the researchers found.
Eating disorders often escape the eye
Researchers developed the tool to screen all women, rather than just patients who present with recognizable symptoms, according to Dr. Claydon.
“Some people may relapse during pregnancy, some may develop [a disorder] while pregnant,” she said. “This makes sure there are no assumptions, because sometimes you can’t tell someone has an eating disorder just by looking at them.”
The researchers also worked to eliminate stigmatizing language to reduce the possibility of women withholding information about their symptoms.
The tool was developed following a qualitative study by Dr. Claydon and her colleagues that was published in 2018. In that study, the researchers analyzed self-perceptions and self-reported experiences of women going through pregnancy with an eating disorder.
“I heard a lot about how difficult it was to disclose eating disorders during pregnancy,” Dr. Claydon said. “It’s wonderful to do something applied to these findings. It’s very meaningful and personal work to me.”
Dr. Claydon said she and her colleagues now plan to test the tool by introducing it into clinics in West Virginia.
The Ophelia Fund/Rhode Island Foundation supported the creation of the tool and dissemination of the tool to clinicians. Research reported in the study was supported by the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
A newly developed screening tool may help clinicians identify pregnant women with eating disorders.
The 12-question instrument is intended to be a quick way to help clinicians identify women who may need to be referred to a mental health expert for further evaluation, according to the researchers, who reported on the instrument in a study published in Archives of Women’s Mental Health.
“It would be most appropriate for clinical encounters so that women can get screened and referred,” said Elizabeth Claydon, MD, assistant professor in the department of social and behavioral sciences at West Virginia University’s School of Public Health, Morgantown, who led the study. “If you miss it, they may carry on their eating disorder throughout their pregnancy.”
Pregnant women who have an eating disorder are at increased risk for gestational diabetes, premature birth, labor complications, difficulties nursing, and postpartum depression, according to the National Eating Disorders Association. Their babies are at increased risk for premature birth, low birth weight, and poor development. However, clinicians have not had an accurate way of screening pregnant women who may have an eating disorder.
The American College of Obstetricians and Gynecologists offered its first clinical guidelines for managing anorexia in pregnancy in April 2022. The group’s recommendations include regular monitoring of cardiac and liver function, blood pressure, and heart rate, as well as tests to monitor iron, sodium, potassium, bone density, and blood sugar levels. Anorexia, bulimia, binge eating, and subthreshold disorders – also known as other specified feeding or eating disorders – are among the most common eating disorders among pregnant women.
There are no recent data on the incidence or prevalence of eating disorders among pregnant women, according to Lauren Smolar, vice president of mission and education at the National Eating Disorders Association.
“It’s hard to capture the number of pregnant women affected, since it so often goes undetected,” Ms. Smolar said.
Existing screening tools for eating disorders ask patients whether they’re currently pregnant; a questionnaire specifically tailored to pregnant women may help to better gather data on the prevalence within this group, Ms. Smolar said.
For the new study, Dr. Claydon and her colleagues tested the questionnaire among more than 400 mostly White women aged 25-34 years. They found that it could reliably identify women who may have an eating disorder. The questionnaire was validated for women to take during any trimester, according to the findings.
A score of 39 or above would serve as an indicator for follow-up. Women who score at least 39 were up to 16 times more likely to receive a diagnosis of an eating disorder, compared with women who scored less, the researchers found.
Eating disorders often escape the eye
Researchers developed the tool to screen all women, rather than just patients who present with recognizable symptoms, according to Dr. Claydon.
“Some people may relapse during pregnancy, some may develop [a disorder] while pregnant,” she said. “This makes sure there are no assumptions, because sometimes you can’t tell someone has an eating disorder just by looking at them.”
The researchers also worked to eliminate stigmatizing language to reduce the possibility of women withholding information about their symptoms.
The tool was developed following a qualitative study by Dr. Claydon and her colleagues that was published in 2018. In that study, the researchers analyzed self-perceptions and self-reported experiences of women going through pregnancy with an eating disorder.
“I heard a lot about how difficult it was to disclose eating disorders during pregnancy,” Dr. Claydon said. “It’s wonderful to do something applied to these findings. It’s very meaningful and personal work to me.”
Dr. Claydon said she and her colleagues now plan to test the tool by introducing it into clinics in West Virginia.
The Ophelia Fund/Rhode Island Foundation supported the creation of the tool and dissemination of the tool to clinicians. Research reported in the study was supported by the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
A newly developed screening tool may help clinicians identify pregnant women with eating disorders.
The 12-question instrument is intended to be a quick way to help clinicians identify women who may need to be referred to a mental health expert for further evaluation, according to the researchers, who reported on the instrument in a study published in Archives of Women’s Mental Health.
“It would be most appropriate for clinical encounters so that women can get screened and referred,” said Elizabeth Claydon, MD, assistant professor in the department of social and behavioral sciences at West Virginia University’s School of Public Health, Morgantown, who led the study. “If you miss it, they may carry on their eating disorder throughout their pregnancy.”
Pregnant women who have an eating disorder are at increased risk for gestational diabetes, premature birth, labor complications, difficulties nursing, and postpartum depression, according to the National Eating Disorders Association. Their babies are at increased risk for premature birth, low birth weight, and poor development. However, clinicians have not had an accurate way of screening pregnant women who may have an eating disorder.
The American College of Obstetricians and Gynecologists offered its first clinical guidelines for managing anorexia in pregnancy in April 2022. The group’s recommendations include regular monitoring of cardiac and liver function, blood pressure, and heart rate, as well as tests to monitor iron, sodium, potassium, bone density, and blood sugar levels. Anorexia, bulimia, binge eating, and subthreshold disorders – also known as other specified feeding or eating disorders – are among the most common eating disorders among pregnant women.
There are no recent data on the incidence or prevalence of eating disorders among pregnant women, according to Lauren Smolar, vice president of mission and education at the National Eating Disorders Association.
“It’s hard to capture the number of pregnant women affected, since it so often goes undetected,” Ms. Smolar said.
Existing screening tools for eating disorders ask patients whether they’re currently pregnant; a questionnaire specifically tailored to pregnant women may help to better gather data on the prevalence within this group, Ms. Smolar said.
For the new study, Dr. Claydon and her colleagues tested the questionnaire among more than 400 mostly White women aged 25-34 years. They found that it could reliably identify women who may have an eating disorder. The questionnaire was validated for women to take during any trimester, according to the findings.
A score of 39 or above would serve as an indicator for follow-up. Women who score at least 39 were up to 16 times more likely to receive a diagnosis of an eating disorder, compared with women who scored less, the researchers found.
Eating disorders often escape the eye
Researchers developed the tool to screen all women, rather than just patients who present with recognizable symptoms, according to Dr. Claydon.
“Some people may relapse during pregnancy, some may develop [a disorder] while pregnant,” she said. “This makes sure there are no assumptions, because sometimes you can’t tell someone has an eating disorder just by looking at them.”
The researchers also worked to eliminate stigmatizing language to reduce the possibility of women withholding information about their symptoms.
The tool was developed following a qualitative study by Dr. Claydon and her colleagues that was published in 2018. In that study, the researchers analyzed self-perceptions and self-reported experiences of women going through pregnancy with an eating disorder.
“I heard a lot about how difficult it was to disclose eating disorders during pregnancy,” Dr. Claydon said. “It’s wonderful to do something applied to these findings. It’s very meaningful and personal work to me.”
Dr. Claydon said she and her colleagues now plan to test the tool by introducing it into clinics in West Virginia.
The Ophelia Fund/Rhode Island Foundation supported the creation of the tool and dissemination of the tool to clinicians. Research reported in the study was supported by the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Multiple mental health woes? Blame it on genetics
Investigators conducted a genetic analysis of 11 major psychiatric disorders, including schizophrenia and bipolar disorder.
“Our findings confirm that high comorbidity across some disorders in part reflects overlapping pathways of genetic risk,” lead author Andrew Grotzinger, PhD, department of psychology and neuroscience, University of Colorado at Boulder, said in a press release.
The results could lead to the development of treatments that address multiple psychiatric disorders at once and help reshape the way diagnoses are established, the researchers note.
The findings were published online in Nature Genetics.
Common genetic patterns
Using the massive UK Biobank and the Psychiatric Genomics Consortium, the researchers applied novel statistical genetic methods to identify common patterns across 11 major psychiatric disorders: schizophrenia, bipolar disorder, major depressive disorder, anxiety disorder, anorexia nervosa, obsessive-compulsive disorder (OCD), Tourette syndrome, post traumatic stress disorder, problematic alcohol use, attention deficit hyperactive disorder, and autism.
The average total sample size per disorder was 156,771 participants, with a range of 9,725 to 802,939 participants.
In all, the investigators identified 152 genetic variants shared across multiple disorders, including those already known to influence certain types of brain cells.
For example, they found that 70% of the genetic signal associated with schizophrenia was also associated with bipolar disorder.
Results also showed that anorexia nervosa and OCD have a strong, shared genetic architecture and that individuals with a genetic predisposition to low body mass index also tend to have a genetic predisposition to these two disorders.
Not surprisingly, the researchers note, there was a large genetic overlap between anxiety disorder and major depressive disorder.
They also observed that psychiatric disorders that tend to cluster together also tend to share genes that influence how and when individuals are physically active during the day.
For example, patients with internalizing disorders such as anxiety and depression tend to have a genetic architecture associated with low movement throughout the day. On the other hand, those with OCD and anorexia tend to have genes associated with higher movement throughout the day.
“When you think about it, it makes sense,” said Dr. Grotzinger. Depressed individuals often experience fatigue or low energy while those with compulsive disorders may have a tough time sitting still, he noted.
One treatment for multiple disorders?
“Collectively, these results offer key insights into the shared and disorder-specific mechanisms of genetic risk for psychiatric disease,” the investigators write.
Their research is also a first step toward developing therapies that can address multiple disorders with one treatment, they add.
“People are more likely today to be prescribed multiple medications intended to treat multiple diagnoses, and in some instances those medicines can have side effects,” Dr. Grotzinger said.
“By identifying what is shared across these issues, we can hopefully come up with ways to target them in a different way that doesn’t require four separate pills or four separate psychotherapy interventions,” he added.
Dr. Grotzinger noted that, for now, the knowledge that genetics are underlying their disorders may provide comfort to some patients.
“It’s important for people to know that they didn’t just get a terrible roll of the dice in life – that they are not facing multiple different issues but rather one set of risk factors bleeding into them all,” he said.
This research had no commercial funding. Dr. Grotzinger reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Investigators conducted a genetic analysis of 11 major psychiatric disorders, including schizophrenia and bipolar disorder.
“Our findings confirm that high comorbidity across some disorders in part reflects overlapping pathways of genetic risk,” lead author Andrew Grotzinger, PhD, department of psychology and neuroscience, University of Colorado at Boulder, said in a press release.
The results could lead to the development of treatments that address multiple psychiatric disorders at once and help reshape the way diagnoses are established, the researchers note.
The findings were published online in Nature Genetics.
Common genetic patterns
Using the massive UK Biobank and the Psychiatric Genomics Consortium, the researchers applied novel statistical genetic methods to identify common patterns across 11 major psychiatric disorders: schizophrenia, bipolar disorder, major depressive disorder, anxiety disorder, anorexia nervosa, obsessive-compulsive disorder (OCD), Tourette syndrome, post traumatic stress disorder, problematic alcohol use, attention deficit hyperactive disorder, and autism.
The average total sample size per disorder was 156,771 participants, with a range of 9,725 to 802,939 participants.
In all, the investigators identified 152 genetic variants shared across multiple disorders, including those already known to influence certain types of brain cells.
For example, they found that 70% of the genetic signal associated with schizophrenia was also associated with bipolar disorder.
Results also showed that anorexia nervosa and OCD have a strong, shared genetic architecture and that individuals with a genetic predisposition to low body mass index also tend to have a genetic predisposition to these two disorders.
Not surprisingly, the researchers note, there was a large genetic overlap between anxiety disorder and major depressive disorder.
They also observed that psychiatric disorders that tend to cluster together also tend to share genes that influence how and when individuals are physically active during the day.
For example, patients with internalizing disorders such as anxiety and depression tend to have a genetic architecture associated with low movement throughout the day. On the other hand, those with OCD and anorexia tend to have genes associated with higher movement throughout the day.
“When you think about it, it makes sense,” said Dr. Grotzinger. Depressed individuals often experience fatigue or low energy while those with compulsive disorders may have a tough time sitting still, he noted.
One treatment for multiple disorders?
“Collectively, these results offer key insights into the shared and disorder-specific mechanisms of genetic risk for psychiatric disease,” the investigators write.
Their research is also a first step toward developing therapies that can address multiple disorders with one treatment, they add.
“People are more likely today to be prescribed multiple medications intended to treat multiple diagnoses, and in some instances those medicines can have side effects,” Dr. Grotzinger said.
“By identifying what is shared across these issues, we can hopefully come up with ways to target them in a different way that doesn’t require four separate pills or four separate psychotherapy interventions,” he added.
Dr. Grotzinger noted that, for now, the knowledge that genetics are underlying their disorders may provide comfort to some patients.
“It’s important for people to know that they didn’t just get a terrible roll of the dice in life – that they are not facing multiple different issues but rather one set of risk factors bleeding into them all,” he said.
This research had no commercial funding. Dr. Grotzinger reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Investigators conducted a genetic analysis of 11 major psychiatric disorders, including schizophrenia and bipolar disorder.
“Our findings confirm that high comorbidity across some disorders in part reflects overlapping pathways of genetic risk,” lead author Andrew Grotzinger, PhD, department of psychology and neuroscience, University of Colorado at Boulder, said in a press release.
The results could lead to the development of treatments that address multiple psychiatric disorders at once and help reshape the way diagnoses are established, the researchers note.
The findings were published online in Nature Genetics.
Common genetic patterns
Using the massive UK Biobank and the Psychiatric Genomics Consortium, the researchers applied novel statistical genetic methods to identify common patterns across 11 major psychiatric disorders: schizophrenia, bipolar disorder, major depressive disorder, anxiety disorder, anorexia nervosa, obsessive-compulsive disorder (OCD), Tourette syndrome, post traumatic stress disorder, problematic alcohol use, attention deficit hyperactive disorder, and autism.
The average total sample size per disorder was 156,771 participants, with a range of 9,725 to 802,939 participants.
In all, the investigators identified 152 genetic variants shared across multiple disorders, including those already known to influence certain types of brain cells.
For example, they found that 70% of the genetic signal associated with schizophrenia was also associated with bipolar disorder.
Results also showed that anorexia nervosa and OCD have a strong, shared genetic architecture and that individuals with a genetic predisposition to low body mass index also tend to have a genetic predisposition to these two disorders.
Not surprisingly, the researchers note, there was a large genetic overlap between anxiety disorder and major depressive disorder.
They also observed that psychiatric disorders that tend to cluster together also tend to share genes that influence how and when individuals are physically active during the day.
For example, patients with internalizing disorders such as anxiety and depression tend to have a genetic architecture associated with low movement throughout the day. On the other hand, those with OCD and anorexia tend to have genes associated with higher movement throughout the day.
“When you think about it, it makes sense,” said Dr. Grotzinger. Depressed individuals often experience fatigue or low energy while those with compulsive disorders may have a tough time sitting still, he noted.
One treatment for multiple disorders?
“Collectively, these results offer key insights into the shared and disorder-specific mechanisms of genetic risk for psychiatric disease,” the investigators write.
Their research is also a first step toward developing therapies that can address multiple disorders with one treatment, they add.
“People are more likely today to be prescribed multiple medications intended to treat multiple diagnoses, and in some instances those medicines can have side effects,” Dr. Grotzinger said.
“By identifying what is shared across these issues, we can hopefully come up with ways to target them in a different way that doesn’t require four separate pills or four separate psychotherapy interventions,” he added.
Dr. Grotzinger noted that, for now, the knowledge that genetics are underlying their disorders may provide comfort to some patients.
“It’s important for people to know that they didn’t just get a terrible roll of the dice in life – that they are not facing multiple different issues but rather one set of risk factors bleeding into them all,” he said.
This research had no commercial funding. Dr. Grotzinger reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE GENETICS



