User login
Pandemic prompts spike in eating disorder hospitalization for adolescents
Hospital admission for children with eating disorders approximately tripled during the COVID-19 pandemic, based on data from 85 patients.
Eating disorders are common among adolescents and often require hospital admission for nutritional restoration, according to May Shum of Yale University, New Haven, Conn., and colleagues
During the COVID-19 pandemic, the volume of hospital admissions for adolescents with eating disorders has increased, the researchers wrote in a poster presented at the annual meeting of the Pediatric Academic Societies. This increase may be driven both by interruptions in medical care and increased psychological distress, but data on changes in patient characteristics and hospitalization course are lacking, they said.
The researchers reviewed charts from patients with eating disorders admitted to a single center between Jan. 1, 2017, and June 30, 2021. The majority of the patients were female (90.6%), and White (78.8%), had restrictive eating behaviors (97.2%), and had private insurance (80.0%).
Overall, the number of monthly admissions increased from 1.4 before the onset of the pandemic to 3.6 during the pandemic (P < .001).
Length of stay increased significantly from before to during pandemic cases (12.8 days vs. 17.3 days, P = .04) and age younger than 13 years was significantly associated with a longer length of stay (P < .001).
The number of patients for whom psychotropic medications were initiated or changed increased significantly (12.5% vs. 28.3%, P = .04); as did the proportion of patients discharged to partial hospitalization, residential, or inpatient psychiatric treatment rather than discharged home with outpatient therapy (56.2% vs. 75.0%, P = .04).
No significant differences were noted in demographics, comorbidities, admission parameters, EKG abnormalities, electrolyte repletion, or tube feeding.
The study findings were limited by the use of data from a single center. However, the results suggest an increase in severity of hospital admissions that have implications for use of hospital resources, the researchers said.
“In addition to an increase in hospital admissions for eating disorder management during the pandemic, longer inpatient stays of younger children with higher acuity at discharge is an added strain on hospital resources and warrants attention,” they concluded.
Considerations for younger patients
The current study is especially important at this time, Margaret Thew, DNP, FNP-BC, medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, said in an interview. “There have been reports of the rising numbers in eating disorders, but until research has been conducted, we cannot quantify the volumes,” said Ms. Thew, who was not involved in the study. “There have been many reports of the rise in mental health issues during the pandemic, so it seems accurate that the rate of eating disorders would rise,” she said. “Additionally, from a clinical perspective there seemed to be many younger-age patients with eating disorders presenting to the inpatient units who seemed sicker,” she noted.
Ms. Thew said she was not surprised by the study findings. “Working with adolescents with eating disorders we saw the increased numbers of both hospitalizations and outpatient referrals during the pandemic,” said Ms. Thew. “Length of stay was higher across the nation regarding admissions for concerns of eating disorders. These patients are sicker and fewer went home after medical stabilization,” she emphasized.
“Clinicians should be more aware of the rise in patients presenting with eating disorders at younger ages to their clinics and provide early interventions to prevent severe illness and medical instability,” said Ms. Thew. Clinicians also should be more proactive in managing younger children and adolescents who express mood disorders, disordered eating, or weight loss, given the significant rise in eating disorders and mental health concerns, she said.
Additional research is needed to continue following the rate of eating disorders into 2022, said Ms. Thew. More research is needed on early interventions and recognition of eating disorders for preteens and teens to prevent severe illness, as is research on how the younger patient with an eating disorder may present differently to the primary care doctor or emergency department, she said.
“We may need to study treatment of the younger population, as they may not do as well with admissions into behavioral health facilities,” Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Hospital admission for children with eating disorders approximately tripled during the COVID-19 pandemic, based on data from 85 patients.
Eating disorders are common among adolescents and often require hospital admission for nutritional restoration, according to May Shum of Yale University, New Haven, Conn., and colleagues
During the COVID-19 pandemic, the volume of hospital admissions for adolescents with eating disorders has increased, the researchers wrote in a poster presented at the annual meeting of the Pediatric Academic Societies. This increase may be driven both by interruptions in medical care and increased psychological distress, but data on changes in patient characteristics and hospitalization course are lacking, they said.
The researchers reviewed charts from patients with eating disorders admitted to a single center between Jan. 1, 2017, and June 30, 2021. The majority of the patients were female (90.6%), and White (78.8%), had restrictive eating behaviors (97.2%), and had private insurance (80.0%).
Overall, the number of monthly admissions increased from 1.4 before the onset of the pandemic to 3.6 during the pandemic (P < .001).
Length of stay increased significantly from before to during pandemic cases (12.8 days vs. 17.3 days, P = .04) and age younger than 13 years was significantly associated with a longer length of stay (P < .001).
The number of patients for whom psychotropic medications were initiated or changed increased significantly (12.5% vs. 28.3%, P = .04); as did the proportion of patients discharged to partial hospitalization, residential, or inpatient psychiatric treatment rather than discharged home with outpatient therapy (56.2% vs. 75.0%, P = .04).
No significant differences were noted in demographics, comorbidities, admission parameters, EKG abnormalities, electrolyte repletion, or tube feeding.
The study findings were limited by the use of data from a single center. However, the results suggest an increase in severity of hospital admissions that have implications for use of hospital resources, the researchers said.
“In addition to an increase in hospital admissions for eating disorder management during the pandemic, longer inpatient stays of younger children with higher acuity at discharge is an added strain on hospital resources and warrants attention,” they concluded.
Considerations for younger patients
The current study is especially important at this time, Margaret Thew, DNP, FNP-BC, medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, said in an interview. “There have been reports of the rising numbers in eating disorders, but until research has been conducted, we cannot quantify the volumes,” said Ms. Thew, who was not involved in the study. “There have been many reports of the rise in mental health issues during the pandemic, so it seems accurate that the rate of eating disorders would rise,” she said. “Additionally, from a clinical perspective there seemed to be many younger-age patients with eating disorders presenting to the inpatient units who seemed sicker,” she noted.
Ms. Thew said she was not surprised by the study findings. “Working with adolescents with eating disorders we saw the increased numbers of both hospitalizations and outpatient referrals during the pandemic,” said Ms. Thew. “Length of stay was higher across the nation regarding admissions for concerns of eating disorders. These patients are sicker and fewer went home after medical stabilization,” she emphasized.
“Clinicians should be more aware of the rise in patients presenting with eating disorders at younger ages to their clinics and provide early interventions to prevent severe illness and medical instability,” said Ms. Thew. Clinicians also should be more proactive in managing younger children and adolescents who express mood disorders, disordered eating, or weight loss, given the significant rise in eating disorders and mental health concerns, she said.
Additional research is needed to continue following the rate of eating disorders into 2022, said Ms. Thew. More research is needed on early interventions and recognition of eating disorders for preteens and teens to prevent severe illness, as is research on how the younger patient with an eating disorder may present differently to the primary care doctor or emergency department, she said.
“We may need to study treatment of the younger population, as they may not do as well with admissions into behavioral health facilities,” Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Hospital admission for children with eating disorders approximately tripled during the COVID-19 pandemic, based on data from 85 patients.
Eating disorders are common among adolescents and often require hospital admission for nutritional restoration, according to May Shum of Yale University, New Haven, Conn., and colleagues
During the COVID-19 pandemic, the volume of hospital admissions for adolescents with eating disorders has increased, the researchers wrote in a poster presented at the annual meeting of the Pediatric Academic Societies. This increase may be driven both by interruptions in medical care and increased psychological distress, but data on changes in patient characteristics and hospitalization course are lacking, they said.
The researchers reviewed charts from patients with eating disorders admitted to a single center between Jan. 1, 2017, and June 30, 2021. The majority of the patients were female (90.6%), and White (78.8%), had restrictive eating behaviors (97.2%), and had private insurance (80.0%).
Overall, the number of monthly admissions increased from 1.4 before the onset of the pandemic to 3.6 during the pandemic (P < .001).
Length of stay increased significantly from before to during pandemic cases (12.8 days vs. 17.3 days, P = .04) and age younger than 13 years was significantly associated with a longer length of stay (P < .001).
The number of patients for whom psychotropic medications were initiated or changed increased significantly (12.5% vs. 28.3%, P = .04); as did the proportion of patients discharged to partial hospitalization, residential, or inpatient psychiatric treatment rather than discharged home with outpatient therapy (56.2% vs. 75.0%, P = .04).
No significant differences were noted in demographics, comorbidities, admission parameters, EKG abnormalities, electrolyte repletion, or tube feeding.
The study findings were limited by the use of data from a single center. However, the results suggest an increase in severity of hospital admissions that have implications for use of hospital resources, the researchers said.
“In addition to an increase in hospital admissions for eating disorder management during the pandemic, longer inpatient stays of younger children with higher acuity at discharge is an added strain on hospital resources and warrants attention,” they concluded.
Considerations for younger patients
The current study is especially important at this time, Margaret Thew, DNP, FNP-BC, medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, said in an interview. “There have been reports of the rising numbers in eating disorders, but until research has been conducted, we cannot quantify the volumes,” said Ms. Thew, who was not involved in the study. “There have been many reports of the rise in mental health issues during the pandemic, so it seems accurate that the rate of eating disorders would rise,” she said. “Additionally, from a clinical perspective there seemed to be many younger-age patients with eating disorders presenting to the inpatient units who seemed sicker,” she noted.
Ms. Thew said she was not surprised by the study findings. “Working with adolescents with eating disorders we saw the increased numbers of both hospitalizations and outpatient referrals during the pandemic,” said Ms. Thew. “Length of stay was higher across the nation regarding admissions for concerns of eating disorders. These patients are sicker and fewer went home after medical stabilization,” she emphasized.
“Clinicians should be more aware of the rise in patients presenting with eating disorders at younger ages to their clinics and provide early interventions to prevent severe illness and medical instability,” said Ms. Thew. Clinicians also should be more proactive in managing younger children and adolescents who express mood disorders, disordered eating, or weight loss, given the significant rise in eating disorders and mental health concerns, she said.
Additional research is needed to continue following the rate of eating disorders into 2022, said Ms. Thew. More research is needed on early interventions and recognition of eating disorders for preteens and teens to prevent severe illness, as is research on how the younger patient with an eating disorder may present differently to the primary care doctor or emergency department, she said.
“We may need to study treatment of the younger population, as they may not do as well with admissions into behavioral health facilities,” Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM PAS 2022
Mental illness tied to COVID-19 breakthrough infection
“Psychiatric disorders remained significantly associated with incident breakthrough infections above and beyond sociodemographic and medical factors, suggesting that mental health is important to consider in conjunction with other risk factors,” wrote the investigators, led by Aoife O’Donovan, PhD, University of California, San Francisco.
Individuals with psychiatric disorders “should be prioritized for booster vaccinations and other critical preventive efforts, including increased SARS-CoV-2 screening, public health campaigns, or COVID-19 discussions during clinical care,” they added.
The study was published online in JAMA Network Open.
Elderly most vulnerable
The researchers reviewed the records of 263,697 veterans who were fully vaccinated against COVID-19.
Just over a half (51.4%) had one or more psychiatric diagnoses within the last 5 years and 14.8% developed breakthrough COVID-19 infections, confirmed by a positive SARS-CoV-2 test.
Psychiatric diagnoses among the veterans included depression, posttraumatic stress, anxiety, adjustment disorder, substance use disorder, bipolar disorder, psychosis, ADHD, dissociation, and eating disorders.
In the overall sample, a history of any psychiatric disorder was associated with a 7% higher incidence of breakthrough COVID-19 infection in models adjusted for potential confounders (adjusted relative risk, 1.07; 95% confidence interval, 1.05-1.09) and a 3% higher incidence in models additionally adjusted for underlying medical comorbidities and smoking (aRR, 1.03; 95% CI, 1.01-1.05).
Most psychiatric disorders were associated with a higher incidence of breakthrough infection, with the highest relative risk observed for substance use disorders (aRR, 1.16; 95% CI, 1.12 -1.21) and adjustment disorder (aRR, 1.13; 95% CI, 1.10-1.16) in fully adjusted models.
Older vaccinated veterans with psychiatric illnesses appear to be most vulnerable to COVID-19 reinfection.
In veterans aged 65 and older, all psychiatric disorders were associated with an increased incidence of breakthrough infection, with increases in the incidence rate ranging from 3% to 24% in fully adjusted models.
In the younger veterans, in contrast, only anxiety, adjustment, and substance use disorders were associated with an increased incidence of breakthrough infection in fully adjusted models.
Psychotic disorders were associated with a 10% lower incidence of breakthrough infection among younger veterans, perhaps because of greater social isolation, the researchers said.
Risky behavior or impaired immunity?
“Although some of the larger observed effect sizes are compelling at an individual level, even the relatively modest effect sizes may have a large effect at the population level when considering the high prevalence of psychiatric disorders and the global reach and scale of the pandemic,” Dr. O’Donovan and colleagues wrote.
They noted that psychiatric disorders, including depression, schizophrenia, and bipolar disorders, have been associated with impaired cellular immunity and blunted response to vaccines. Therefore, it’s possible that those with psychiatric disorders have poorer responses to COVID-19 vaccination.
It’s also possible that immunity following vaccination wanes more quickly or more strongly in people with psychiatric disorders and they could have less protection against new variants, they added.
Patients with psychiatric disorders could be more apt to engage in risky behaviors for contracting COVID-19, which could also increase the risk for breakthrough infection, they said.
The study was supported by a UCSF Department of Psychiatry Rapid Award and UCSF Faculty Resource Fund Award. Dr. O’Donovan reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
“Psychiatric disorders remained significantly associated with incident breakthrough infections above and beyond sociodemographic and medical factors, suggesting that mental health is important to consider in conjunction with other risk factors,” wrote the investigators, led by Aoife O’Donovan, PhD, University of California, San Francisco.
Individuals with psychiatric disorders “should be prioritized for booster vaccinations and other critical preventive efforts, including increased SARS-CoV-2 screening, public health campaigns, or COVID-19 discussions during clinical care,” they added.
The study was published online in JAMA Network Open.
Elderly most vulnerable
The researchers reviewed the records of 263,697 veterans who were fully vaccinated against COVID-19.
Just over a half (51.4%) had one or more psychiatric diagnoses within the last 5 years and 14.8% developed breakthrough COVID-19 infections, confirmed by a positive SARS-CoV-2 test.
Psychiatric diagnoses among the veterans included depression, posttraumatic stress, anxiety, adjustment disorder, substance use disorder, bipolar disorder, psychosis, ADHD, dissociation, and eating disorders.
In the overall sample, a history of any psychiatric disorder was associated with a 7% higher incidence of breakthrough COVID-19 infection in models adjusted for potential confounders (adjusted relative risk, 1.07; 95% confidence interval, 1.05-1.09) and a 3% higher incidence in models additionally adjusted for underlying medical comorbidities and smoking (aRR, 1.03; 95% CI, 1.01-1.05).
Most psychiatric disorders were associated with a higher incidence of breakthrough infection, with the highest relative risk observed for substance use disorders (aRR, 1.16; 95% CI, 1.12 -1.21) and adjustment disorder (aRR, 1.13; 95% CI, 1.10-1.16) in fully adjusted models.
Older vaccinated veterans with psychiatric illnesses appear to be most vulnerable to COVID-19 reinfection.
In veterans aged 65 and older, all psychiatric disorders were associated with an increased incidence of breakthrough infection, with increases in the incidence rate ranging from 3% to 24% in fully adjusted models.
In the younger veterans, in contrast, only anxiety, adjustment, and substance use disorders were associated with an increased incidence of breakthrough infection in fully adjusted models.
Psychotic disorders were associated with a 10% lower incidence of breakthrough infection among younger veterans, perhaps because of greater social isolation, the researchers said.
Risky behavior or impaired immunity?
“Although some of the larger observed effect sizes are compelling at an individual level, even the relatively modest effect sizes may have a large effect at the population level when considering the high prevalence of psychiatric disorders and the global reach and scale of the pandemic,” Dr. O’Donovan and colleagues wrote.
They noted that psychiatric disorders, including depression, schizophrenia, and bipolar disorders, have been associated with impaired cellular immunity and blunted response to vaccines. Therefore, it’s possible that those with psychiatric disorders have poorer responses to COVID-19 vaccination.
It’s also possible that immunity following vaccination wanes more quickly or more strongly in people with psychiatric disorders and they could have less protection against new variants, they added.
Patients with psychiatric disorders could be more apt to engage in risky behaviors for contracting COVID-19, which could also increase the risk for breakthrough infection, they said.
The study was supported by a UCSF Department of Psychiatry Rapid Award and UCSF Faculty Resource Fund Award. Dr. O’Donovan reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
“Psychiatric disorders remained significantly associated with incident breakthrough infections above and beyond sociodemographic and medical factors, suggesting that mental health is important to consider in conjunction with other risk factors,” wrote the investigators, led by Aoife O’Donovan, PhD, University of California, San Francisco.
Individuals with psychiatric disorders “should be prioritized for booster vaccinations and other critical preventive efforts, including increased SARS-CoV-2 screening, public health campaigns, or COVID-19 discussions during clinical care,” they added.
The study was published online in JAMA Network Open.
Elderly most vulnerable
The researchers reviewed the records of 263,697 veterans who were fully vaccinated against COVID-19.
Just over a half (51.4%) had one or more psychiatric diagnoses within the last 5 years and 14.8% developed breakthrough COVID-19 infections, confirmed by a positive SARS-CoV-2 test.
Psychiatric diagnoses among the veterans included depression, posttraumatic stress, anxiety, adjustment disorder, substance use disorder, bipolar disorder, psychosis, ADHD, dissociation, and eating disorders.
In the overall sample, a history of any psychiatric disorder was associated with a 7% higher incidence of breakthrough COVID-19 infection in models adjusted for potential confounders (adjusted relative risk, 1.07; 95% confidence interval, 1.05-1.09) and a 3% higher incidence in models additionally adjusted for underlying medical comorbidities and smoking (aRR, 1.03; 95% CI, 1.01-1.05).
Most psychiatric disorders were associated with a higher incidence of breakthrough infection, with the highest relative risk observed for substance use disorders (aRR, 1.16; 95% CI, 1.12 -1.21) and adjustment disorder (aRR, 1.13; 95% CI, 1.10-1.16) in fully adjusted models.
Older vaccinated veterans with psychiatric illnesses appear to be most vulnerable to COVID-19 reinfection.
In veterans aged 65 and older, all psychiatric disorders were associated with an increased incidence of breakthrough infection, with increases in the incidence rate ranging from 3% to 24% in fully adjusted models.
In the younger veterans, in contrast, only anxiety, adjustment, and substance use disorders were associated with an increased incidence of breakthrough infection in fully adjusted models.
Psychotic disorders were associated with a 10% lower incidence of breakthrough infection among younger veterans, perhaps because of greater social isolation, the researchers said.
Risky behavior or impaired immunity?
“Although some of the larger observed effect sizes are compelling at an individual level, even the relatively modest effect sizes may have a large effect at the population level when considering the high prevalence of psychiatric disorders and the global reach and scale of the pandemic,” Dr. O’Donovan and colleagues wrote.
They noted that psychiatric disorders, including depression, schizophrenia, and bipolar disorders, have been associated with impaired cellular immunity and blunted response to vaccines. Therefore, it’s possible that those with psychiatric disorders have poorer responses to COVID-19 vaccination.
It’s also possible that immunity following vaccination wanes more quickly or more strongly in people with psychiatric disorders and they could have less protection against new variants, they added.
Patients with psychiatric disorders could be more apt to engage in risky behaviors for contracting COVID-19, which could also increase the risk for breakthrough infection, they said.
The study was supported by a UCSF Department of Psychiatry Rapid Award and UCSF Faculty Resource Fund Award. Dr. O’Donovan reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
First comprehensive guidelines for managing anorexia in pregnancy
The first comprehensive guidelines to manage pregnant women with anorexia nervosa (AN) have been released.
Pregnant women with AN are at greater risk of poor outcomes, including stillbirth, underweight infant, or pre-term birth, yet there are no clear guidelines on the management of the condition.
“Anorexia in pregnancy has been an overlooked area of clinical care, as many believed only women in remission become pregnant, and it is clear that is not the case,” lead author Megan Galbally, MBBS, PhD, professor and director, Centre of Women’s and Children’s Mental Health at Monash University School of Clinical Sciences, Melbourne, told this news organization.
“There are great opportunities to support women in their mental health and give them and their babies a healthier start to parenthood and life,” said Dr. Galbally.
“For instance, reducing the likelihood of prematurity or low birth weight at birth that can be associated with anorexia in pregnancy has extraordinary benefits for that child for lifelong health and well-being,” she added.
The guidelines were published online in Lancet Psychiatry.
Spike in cases
Dr. Galbally noted that during her 20 years of working in perinatal mental health within tertiary maternity services, she only ever saw an occasional pregnant woman with current AN.
In contrast, over the last 3 to 4 years, there has been a “steep increase in women presenting in pregnancy with very low body mass index (BMI) and current anorexia nervosa requiring treatment in pregnancy,” Dr. Galbally said.
Despite the complexity of managing AN in pregnancy, few studies are available to guide care. In a systematic literature review, the researchers identified only eight studies that addressed the management of AN in pregnancy. These studies were case studies or case reports examining narrow aspects of management.
Digging deeper, the researchers conducted a state-of-the-art research review in relevant disciplines and areas of expertise for managing anorexia nervosa in pregnancy. They synthesized their findings into “recommendations and principles” for multidisciplinary care of pregnant women with AN.
The researchers note that AN in pregnancy is associated with increased risks of pregnancy complications and poorer outcomes for infants, and measures such as BMI are less accurate in pregnancy for assessing severity or change in anorexia nervosa.
Anorexia affects pregnancy and neonatal outcomes through low calorie intake, nutritional and vitamin deficiencies, stress, fasting, low body mass, and poor placentation and uteroplacental function.
The authors note that managing AN in pregnancy requires multidisciplinary care that considers the substantial physiological changes for women and requirements for monitoring fetal growth and development.
At a minimum, they recommend monitoring the following:
- Sodium, potassium, magnesium, phosphate, and chloride concentration
- Iron status, vitamin D and bone mineral density, blood sugar concentration (fasting or random), and A1c
- Liver function (including bilirubin, aspartate transaminase, alanine aminotransferase, and gamma-glutamyl transferase) and bone marrow function (including full blood examination, white cell count, neutrophil count, platelets, and hemoglobin)
- Inflammatory markers (C-reactive protein and erythrocyte sedimentation rate)
- Cardiac function (electrocardiogram and echocardiogram)
- Blood pressure and heart rate (lying and standing) and body temperature
“There are considerable risks for women and their unborn child in managing moderate to severe AN in pregnancy,” said Dr. Galbally.
“While we have provided some recommendations, it still requires considerable adaptation to individual presentations and circumstances, and this is best done with a maternity service that manages other high-risk pregnancies such as through maternal-fetal medicine teams,” she said.
“While this area of clinical care can be new to high-risk pregnancy teams, it is clearly important that high-risk pregnancy services and mental health work together to improve care for women with anorexia in pregnancy,” Dr. Galbally added.
A nightmare, a dream come true
Reached for comment, Kamryn T. Eddy, PhD, co-director, Eating Disorders Clinical and Research Program, Massachusetts General Hospital, said, “for many with anorexia nervosa, pregnancy realizes their greatest nightmare and dream come true, both at once.”
“The physical demands of pregnancy can be taxing, and for those with anorexia nervosa, closer clinical management makes sense and may help to support patients who are at risk for return to or worsening of symptoms with the increased nutritional needs and weight gain that occur in pregnancy,” Dr. Eddy, associate professor, department of psychiatry, Harvard Medical School, Boston, told this news organization.
“At the same time, the desire to have a child can be a strong motivator for patients to make the changes needed to recover, and for some, the transition to mother can also help in recovery by broadening the range of things that influence their self-worth,” Dr. Eddy added.
This research had no specific funding. Dr. Galbally and Dr. Eddy report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The first comprehensive guidelines to manage pregnant women with anorexia nervosa (AN) have been released.
Pregnant women with AN are at greater risk of poor outcomes, including stillbirth, underweight infant, or pre-term birth, yet there are no clear guidelines on the management of the condition.
“Anorexia in pregnancy has been an overlooked area of clinical care, as many believed only women in remission become pregnant, and it is clear that is not the case,” lead author Megan Galbally, MBBS, PhD, professor and director, Centre of Women’s and Children’s Mental Health at Monash University School of Clinical Sciences, Melbourne, told this news organization.
“There are great opportunities to support women in their mental health and give them and their babies a healthier start to parenthood and life,” said Dr. Galbally.
“For instance, reducing the likelihood of prematurity or low birth weight at birth that can be associated with anorexia in pregnancy has extraordinary benefits for that child for lifelong health and well-being,” she added.
The guidelines were published online in Lancet Psychiatry.
Spike in cases
Dr. Galbally noted that during her 20 years of working in perinatal mental health within tertiary maternity services, she only ever saw an occasional pregnant woman with current AN.
In contrast, over the last 3 to 4 years, there has been a “steep increase in women presenting in pregnancy with very low body mass index (BMI) and current anorexia nervosa requiring treatment in pregnancy,” Dr. Galbally said.
Despite the complexity of managing AN in pregnancy, few studies are available to guide care. In a systematic literature review, the researchers identified only eight studies that addressed the management of AN in pregnancy. These studies were case studies or case reports examining narrow aspects of management.
Digging deeper, the researchers conducted a state-of-the-art research review in relevant disciplines and areas of expertise for managing anorexia nervosa in pregnancy. They synthesized their findings into “recommendations and principles” for multidisciplinary care of pregnant women with AN.
The researchers note that AN in pregnancy is associated with increased risks of pregnancy complications and poorer outcomes for infants, and measures such as BMI are less accurate in pregnancy for assessing severity or change in anorexia nervosa.
Anorexia affects pregnancy and neonatal outcomes through low calorie intake, nutritional and vitamin deficiencies, stress, fasting, low body mass, and poor placentation and uteroplacental function.
The authors note that managing AN in pregnancy requires multidisciplinary care that considers the substantial physiological changes for women and requirements for monitoring fetal growth and development.
At a minimum, they recommend monitoring the following:
- Sodium, potassium, magnesium, phosphate, and chloride concentration
- Iron status, vitamin D and bone mineral density, blood sugar concentration (fasting or random), and A1c
- Liver function (including bilirubin, aspartate transaminase, alanine aminotransferase, and gamma-glutamyl transferase) and bone marrow function (including full blood examination, white cell count, neutrophil count, platelets, and hemoglobin)
- Inflammatory markers (C-reactive protein and erythrocyte sedimentation rate)
- Cardiac function (electrocardiogram and echocardiogram)
- Blood pressure and heart rate (lying and standing) and body temperature
“There are considerable risks for women and their unborn child in managing moderate to severe AN in pregnancy,” said Dr. Galbally.
“While we have provided some recommendations, it still requires considerable adaptation to individual presentations and circumstances, and this is best done with a maternity service that manages other high-risk pregnancies such as through maternal-fetal medicine teams,” she said.
“While this area of clinical care can be new to high-risk pregnancy teams, it is clearly important that high-risk pregnancy services and mental health work together to improve care for women with anorexia in pregnancy,” Dr. Galbally added.
A nightmare, a dream come true
Reached for comment, Kamryn T. Eddy, PhD, co-director, Eating Disorders Clinical and Research Program, Massachusetts General Hospital, said, “for many with anorexia nervosa, pregnancy realizes their greatest nightmare and dream come true, both at once.”
“The physical demands of pregnancy can be taxing, and for those with anorexia nervosa, closer clinical management makes sense and may help to support patients who are at risk for return to or worsening of symptoms with the increased nutritional needs and weight gain that occur in pregnancy,” Dr. Eddy, associate professor, department of psychiatry, Harvard Medical School, Boston, told this news organization.
“At the same time, the desire to have a child can be a strong motivator for patients to make the changes needed to recover, and for some, the transition to mother can also help in recovery by broadening the range of things that influence their self-worth,” Dr. Eddy added.
This research had no specific funding. Dr. Galbally and Dr. Eddy report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The first comprehensive guidelines to manage pregnant women with anorexia nervosa (AN) have been released.
Pregnant women with AN are at greater risk of poor outcomes, including stillbirth, underweight infant, or pre-term birth, yet there are no clear guidelines on the management of the condition.
“Anorexia in pregnancy has been an overlooked area of clinical care, as many believed only women in remission become pregnant, and it is clear that is not the case,” lead author Megan Galbally, MBBS, PhD, professor and director, Centre of Women’s and Children’s Mental Health at Monash University School of Clinical Sciences, Melbourne, told this news organization.
“There are great opportunities to support women in their mental health and give them and their babies a healthier start to parenthood and life,” said Dr. Galbally.
“For instance, reducing the likelihood of prematurity or low birth weight at birth that can be associated with anorexia in pregnancy has extraordinary benefits for that child for lifelong health and well-being,” she added.
The guidelines were published online in Lancet Psychiatry.
Spike in cases
Dr. Galbally noted that during her 20 years of working in perinatal mental health within tertiary maternity services, she only ever saw an occasional pregnant woman with current AN.
In contrast, over the last 3 to 4 years, there has been a “steep increase in women presenting in pregnancy with very low body mass index (BMI) and current anorexia nervosa requiring treatment in pregnancy,” Dr. Galbally said.
Despite the complexity of managing AN in pregnancy, few studies are available to guide care. In a systematic literature review, the researchers identified only eight studies that addressed the management of AN in pregnancy. These studies were case studies or case reports examining narrow aspects of management.
Digging deeper, the researchers conducted a state-of-the-art research review in relevant disciplines and areas of expertise for managing anorexia nervosa in pregnancy. They synthesized their findings into “recommendations and principles” for multidisciplinary care of pregnant women with AN.
The researchers note that AN in pregnancy is associated with increased risks of pregnancy complications and poorer outcomes for infants, and measures such as BMI are less accurate in pregnancy for assessing severity or change in anorexia nervosa.
Anorexia affects pregnancy and neonatal outcomes through low calorie intake, nutritional and vitamin deficiencies, stress, fasting, low body mass, and poor placentation and uteroplacental function.
The authors note that managing AN in pregnancy requires multidisciplinary care that considers the substantial physiological changes for women and requirements for monitoring fetal growth and development.
At a minimum, they recommend monitoring the following:
- Sodium, potassium, magnesium, phosphate, and chloride concentration
- Iron status, vitamin D and bone mineral density, blood sugar concentration (fasting or random), and A1c
- Liver function (including bilirubin, aspartate transaminase, alanine aminotransferase, and gamma-glutamyl transferase) and bone marrow function (including full blood examination, white cell count, neutrophil count, platelets, and hemoglobin)
- Inflammatory markers (C-reactive protein and erythrocyte sedimentation rate)
- Cardiac function (electrocardiogram and echocardiogram)
- Blood pressure and heart rate (lying and standing) and body temperature
“There are considerable risks for women and their unborn child in managing moderate to severe AN in pregnancy,” said Dr. Galbally.
“While we have provided some recommendations, it still requires considerable adaptation to individual presentations and circumstances, and this is best done with a maternity service that manages other high-risk pregnancies such as through maternal-fetal medicine teams,” she said.
“While this area of clinical care can be new to high-risk pregnancy teams, it is clearly important that high-risk pregnancy services and mental health work together to improve care for women with anorexia in pregnancy,” Dr. Galbally added.
A nightmare, a dream come true
Reached for comment, Kamryn T. Eddy, PhD, co-director, Eating Disorders Clinical and Research Program, Massachusetts General Hospital, said, “for many with anorexia nervosa, pregnancy realizes their greatest nightmare and dream come true, both at once.”
“The physical demands of pregnancy can be taxing, and for those with anorexia nervosa, closer clinical management makes sense and may help to support patients who are at risk for return to or worsening of symptoms with the increased nutritional needs and weight gain that occur in pregnancy,” Dr. Eddy, associate professor, department of psychiatry, Harvard Medical School, Boston, told this news organization.
“At the same time, the desire to have a child can be a strong motivator for patients to make the changes needed to recover, and for some, the transition to mother can also help in recovery by broadening the range of things that influence their self-worth,” Dr. Eddy added.
This research had no specific funding. Dr. Galbally and Dr. Eddy report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Food for thought: Dangerous weight loss in an older adult
CASE Fixated on health and nutrition
At the insistence of her daughter, Ms. L, age 75, presents to the emergency department (ED) for self-neglect and severe weight loss, with a body mass index (BMI) of 13.5 kg/m2 (normal: 18.5 to 24.9 kg/m2). When asked why she is in the ED, Ms. L says she doesn’t know. She attributes her significant weight loss (approximately 20 pounds in the last few months) to gastroesophageal reflux disease (GERD). She constantly worries about her esophagus. She had been diagnosed with esophageal dysphagia 7 years ago after undergoing radiofrequency ablation for esophageal cancer. Ms. L fixates on the negative effects certain foods and ingredients might have on her stomach and esophagus.
Following transfer from the ED, Ms. L is involuntarily admitted to our inpatient unit. Although she acknowledges weight loss, she minimizes the severity of her illness and indicates she would like to gain weight, but only by eating healthy foods she is comfortable with, including kale, quinoa, and vegetables. Ms. L says that she has always been interested in “healthful foods” and that she “loves sugar,” but “it’s bad for you,” mentioning that “sugar fuels cancer.” She has daily thoughts about sugar causing cancer. Ms. L also mentions that she stopped eating flour, sugar, fried food, and oils because those foods affect her “stomach acid” and cause “pimples on my face and weight loss.” While in the inpatient unit, Ms. L requests a special diet and demands to know the origin and ingredients of the foods she is offered. She emphasizes that her esophageal cancer diagnosis and dysphagia exacerbate worries that certain foods cause cancer, and wants to continue her diet restrictions. Nonetheless, she says she wants to get healthy, and denies an intense fear of gaining weight or feeling fat.
HISTORY Multiple psychiatric diagnoses
Ms. L lives alone and enjoys spending time with her grandchildren, visiting museums, and listening to classical music. However, her family, social workers, and records from a previous psychiatric hospitalization reveal that Ms. L has a history of psychiatric illness and fears regarding certain types of foods for much of her adult life. Ms. L’s family also described a range of compulsive behaviors, including shoplifting, hoarding art, multiple plastic surgeries, and phases where Ms. L ate only frozen yogurt without sugar.
Ms. L’s daughter reported that Ms. L had seen a psychologist in the late 1990s for depression and had been diagnosed with obsessive-compulsive disorder (OCD) and attention deficit/hyperactivity disorder in the early 2000s. In 2006, during a depressive episode after her divorce, Ms. L had a suicide attempt with pills and alcohol, and was hospitalized. Records from that stay described a history of mood dysregulation with fears regarding food and nutrition. Ms. L was treated with aripiprazole 5 mg/d. A trial of trazodone 25 mg/d did not have any effect. When discharged, she was receiving lamotrigine 100 mg/d. However, her daughter believes she stopped taking all psychiatric medications shortly after discharge.
Her daughter says that in the past 2 years, Ms. L has seen multiple doctors for treatment of somatic gastrointestinal (GI) complaints. A 2018 note from a social worker indicated that Ms. L endorsed taking >80 supplements per day and constantly researched nutrition online. In the months leading to her current hospitalization, Ms. L suffered from severe self-neglect and fear regarding foods she felt were not healthy for her. She had stopped leaving her apartment.
Continue to: EVALUATION Poor insight, normal lab results...
EVALUATION Poor insight, normal lab results
During her evaluation, Ms. L appears cachectic and frail. She has a heavily constricted affect and is guarded, dismissive, and vague. Although her thought processes are linear and goal-directed, her insight into her condition is extremely poor and she appears surprised when clinicians inform her that her self-neglect would lead to death. Instead, Ms. L insists she is eating healthily and demonstrates severe anxiety in relation to her GI symptoms.
Ms. L is oriented to person, place, and time. She scores 27/30 on the Montreal Cognitive Assessment, indicating normal cognition. She denies any depressive symptoms or suicidal intent. She does not appear to be internally preoccupied and denies having auditory or visual hallucinations or manic symptoms.
A neurologic examination reveals that her cranial nerves are normal, and cerebellar function, strength, and sensory testing are intact. Her gait is steady and she walks without a walker. Despite her severely low BMI and recent history of self-neglect, Ms. L’s laboratory results are remarkably normal and show no liver, metabolic, or electrolyte abnormalities, no signs of infection, and normal vitamin B12 levels. She has slightly elevated creatinine and blood urea nitrogen levels, but a normal glomerular filtration rate.
Her medical history is significant for squamous cell esophageal cancer, treated with radiofrequency ablation. Although Ms. L is constantly worried about the recurrence of cancer, pathology reports demonstrate no esophageal dysplasia. However, she does show evidence of an approximately 1 cm × 1 cm mild, noncircumferential esophageal stenosis, likely resulting from radiofrequency ablation.
[polldaddy:11079394]
The authors’ observations
Several health- and physical symptom-related psychiatric disorders have overlapping features, which can complicate the differential diagnosis (Table 11). Ms. L presented to the ED with a severely low BMI of 13.5 kg/m2, obsessions regarding specific types of food, and preoccupations regarding her esophagus. Despite her extensive psychiatric history (including intense fears regarding food), we ruled out a primary psychotic disorder because she did not describe auditory or visual hallucinations and never appeared internally preoccupied. While her BMI and persistent minimization of the extent of her disease meet criteria for anorexia nervosa, she denied body dysmorphia and did not have any fear of gaining weight.
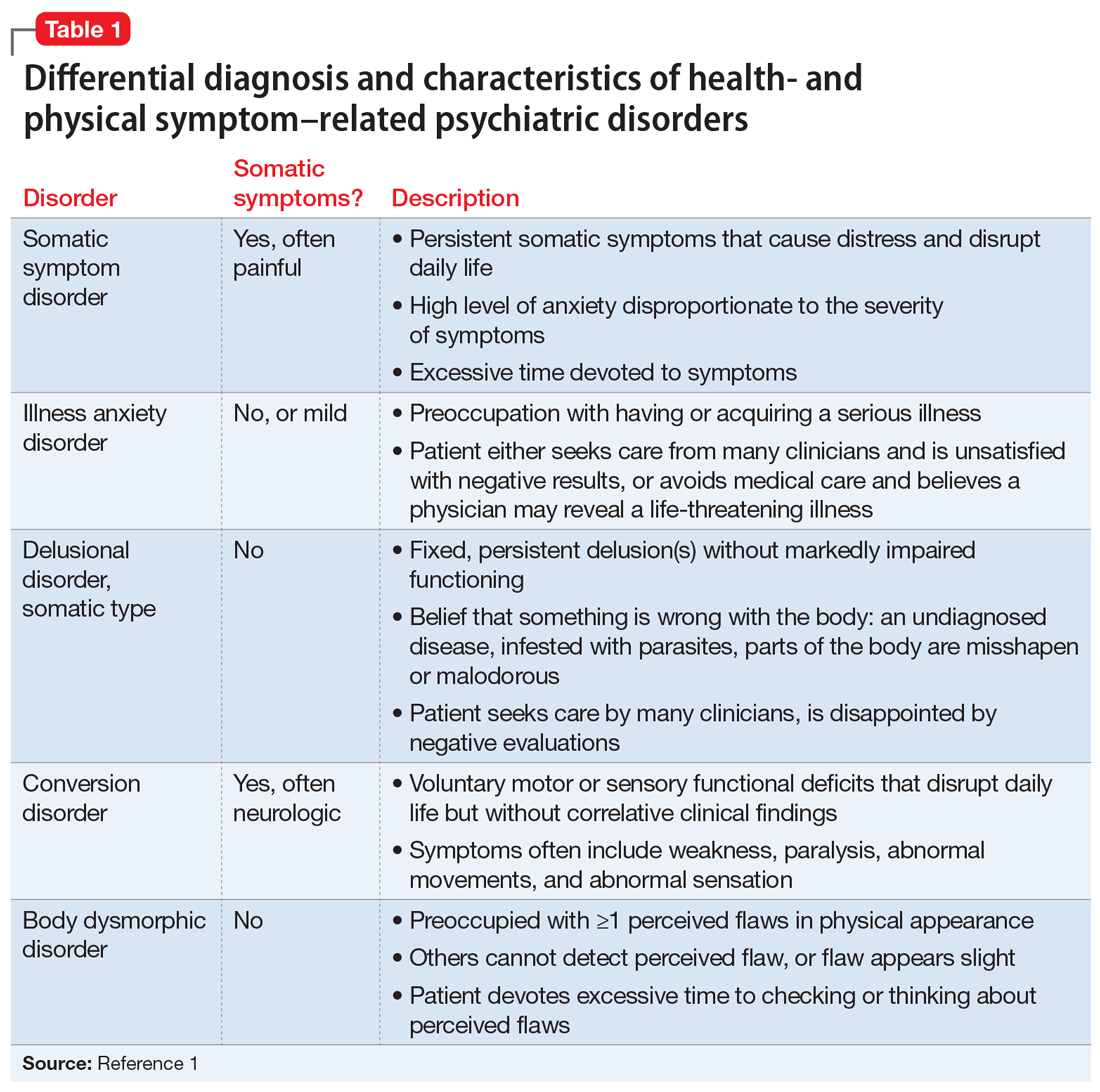
A central element of Ms. L’s presentation was her anxiety regarding how certain types of foods impact her health as well as her anxieties regarding her esophagus. While Ms. L was in remission from esophageal cancer and had a diagnosis of esophageal dysphagia, these preoccupations and obsessions regarding how certain types of foods affect her esophagus drove her to self-neglect and thus represent pathologic thought processes out of proportion to her symptoms. Illness anxiety disorder was considered because Ms. L met many of its criteria: preoccupation with having a serious illness, disproportionate preoccupation with somatic symptoms if they are present, extreme anxiety over health, and performance of health-related behaviors.1 However, illness anxiety disorder is a diagnosis of exclusion, and 1 criterion is that these symptoms cannot be explained by another mental disorder. We felt other diagnoses better fit Ms. L’s condition and ruled out illness anxiety disorder.
Ms. L’s long history of food and non-food–related obsessions and compulsions that interrupted her ability to perform daily activities were strongly suggestive for OCD. Additionally, her intense preoccupation, high level of anxiety, amount of time and energy spent seeking care for her esophagus and GERD symptoms, and the resulting significant disruption of daily life, met criteria for somatic symptom disorder (SSD). However, we did not believe that a diagnosis of OCD and SSD alone explained the entirety of Ms. L’s clinical picture. Despite ruling out anorexia nervosa, Ms. L nonetheless demonstrated disordered eating.
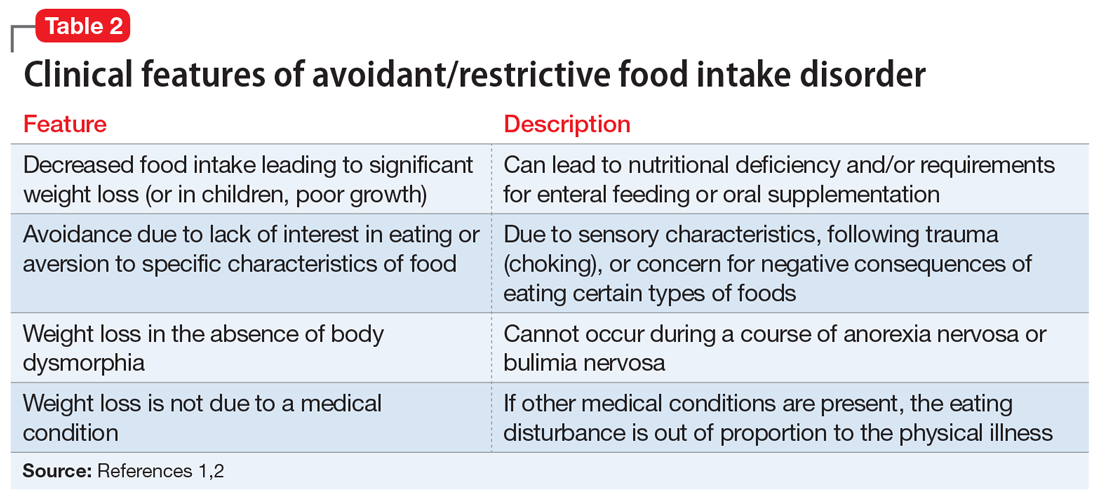
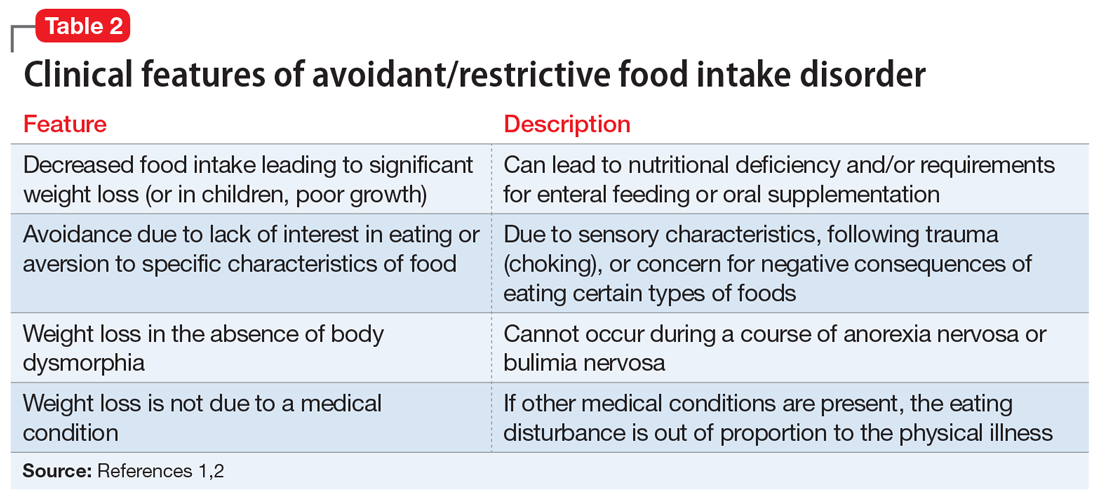
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder in which patients restrict their diet and do not meet nutritional needs for any number of reasons, do not experience body dysmorphia, and do not fear weight gain.1 A common feature of ARFID is a fear of negative consequences from eating specific types of food.2 Table 21,2 summarizes additional clinical features of ARFID. Although ARFID is typically diagnosed in children and adolescents, particularly in individuals with autism with heightened sensory sensitivities, ARFID is also common among adult patients with GI disorders.3 In a retrospective chart review of 410 adults ages 18 to 90 (73% women) referred to a neurogastroenterology care center, 6.3% met the full criteria for ARFID and 17.3% had clinically significant avoidant or restrictive eating behaviors. Among patients with ARFID symptoms, 93% stated that a fear of GI symptoms was the driver of their avoidant or restrictive eating behaviors.2 Patients with GI diseases often develop dietary control and avoidance coping mechanisms to alleviate their symptoms.4 These strategies can exacerbate health anxieties and have a detrimental effect on mental health.5 Patients with GI disorders have a high degree of comorbidity with affective disorders, including anxiety disorders.6 These trends may arise from hypervigilance and the need to gain control over physical symptoms.7 Feeling a need for control, actions driven by anxiety and fear, and the need for compensatory behaviors are cardinal features of OCD and eating disorders.8 Multiple studies have demonstrated comorbidities between irritable bowel syndrome and eating disorders,9 SSD,10 and OCD.11 Taken together with observations that ARFID is also found in patients with GI disorders,2 these findings demonstrate that patients with a history of GI disease are at high risk of developing extreme health anxieties and behavioral coping strategies that can lead to disordered eating.
The rise in “healthy” eating materials online—particularly on social media—has created an atmosphere in which misinformation regarding diet and health is common and widespread. For patients with OCD and a predisposition to health anxiety, such as Ms. L, searching online for nutrition information and healthy living habits can exacerbate food-related anxieties and can lead to a pathological drive for purity and health.12Although not included in DSM-5, orthorexia nervosa was identified in 1997 as a proposed eating disorder best characterized as an obsession with healthy eating with associated restrictive behaviors.13 Patients with this disorder are rarely focused on losing weight, and orthorexic eating behaviors have been associated with both SSD and OCD.12,14 As in Ms. L’s case, patients with orthorexia nervosa demonstrate intrusive obsessions with nutrition, spend excessive amount of time researching nutrition, and fixate on food quality.12 Throughout Ms. L’s hospitalization, even as her food-related magical thinking symptoms improved, she constantly informed her care team that she had been “eating healthily” even though she was severely cachectic. Patients with SSD and OCD prone to health anxieties are at risk of developing pathologic food beliefs and dangerous eating behaviors. These patients may benefit from psychoeducation regarding nutrition and media literacy, which are components of effective eating disorder programs.15
[polldaddy:11079399]
Continue to: The authors' observations...
The authors’ observations
How do we approach the pharmacologic treatment of patients with co-occurring eating, somatic symptom, and anxiety disorders? Olanzapine facilitates recovery in children and adolescents with ARFID by promoting eating and weight gain, and decreasing symptoms of depression and anxiety.16 Patients with orthorexia nervosa also may benefit from treatment with olanzapine, which has decreased food-related fixations, magical thinking, and delusions regarding food.17 Further, orthorexic patients with ARFID have also been shown to respond to SSRIs due to those agents’ efficacy for treating intrusive thoughts, obsessions, and preoccupations from OCD and SSD.18,19 Thus, treating Ms. L’s symptoms with olanzapine and fluoxetine targeted the intersection of several diagnoses on our differential. Olanzapine’s propensity to cause weight gain is favorable in this population, particularly patients such as Ms. L, who do not exhibit body dysmorphia or fear of gaining weight.
OUTCOME Weight gain and fewer fears
Ms. L is prescribed olanzapine 5 mg/d and fluoxetine 20 mg/d. She gains 20.6 pounds in 4 weeks. Importantly, she endorses fewer fears related to foods and expands her palate to include foods she previously considered to be unhealthy, including white bread and farm-raised salmon. Further, she spends less time thinking about food and says she has less anxiety regarding the recurrence of GI symptoms.
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Murray HB, Bailey AP, Keshishian AC. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995-2002.e1.
3. Görmez A, Kılıç A, Kırpınar İ. Avoidant/restrictive food intake disorder: an adult case responding to cognitive behavioral therapy. Clinical Case Studies. 2018;17(6):443-452.
4. Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016;28(12):1915-1920.
5. Melchior C, Desprez C, Riachi G, et al. Anxiety and depression profile is associated with eating disorders in patients with irritable bowel syndrome. Front Psychiatry. 2020;10:928.
6. Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62 Suppl 8:28-37.
7. Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372-377.
8. Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253-274.
9. Perkins SJ, Keville S, Schmidt U, et al. Eating disorders and irritable bowel syndrome: is there a link? J Psychosom Res. 2005;59(2):57-64.
10. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(2):6024-6030.
11. Masand PS, Keuthen NJ, Gupta S, et al. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11(1):21-25.
12. Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385-394.
13. Bratman S. Health food junkie. Yoga Journal. 1997;136:42-50.
14. Barthels F, Müller R, Schüth T, et al. Orthorexic eating behavior in patients with somatoform disorders. Eat Weight Disord. 2021;26(1):135-143.
15. Ciao AC, Loth K, Neumark-Sztainer D. Preventing eating disorder pathology: common and unique features of successful eating disorders prevention programs. Curr Psychiatry Rep. 2014;16(7):453.
16. Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920-922.
17. Moroze RM, Dunn TM, Craig Holland J, et al. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56(4):397-403.
18. Spettigue W, Norris ML, Santos A, et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord. 2018;6:20.
19. Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health. 2021;18(10):5488. Published 2021 May 20. doi:10.3390/ijerph18105488 Prevalence of orthorexia nervosa and its diagnostic tools-a literature review. Int J Environ Res Public Health. 2021;18(10):5488.
CASE Fixated on health and nutrition
At the insistence of her daughter, Ms. L, age 75, presents to the emergency department (ED) for self-neglect and severe weight loss, with a body mass index (BMI) of 13.5 kg/m2 (normal: 18.5 to 24.9 kg/m2). When asked why she is in the ED, Ms. L says she doesn’t know. She attributes her significant weight loss (approximately 20 pounds in the last few months) to gastroesophageal reflux disease (GERD). She constantly worries about her esophagus. She had been diagnosed with esophageal dysphagia 7 years ago after undergoing radiofrequency ablation for esophageal cancer. Ms. L fixates on the negative effects certain foods and ingredients might have on her stomach and esophagus.
Following transfer from the ED, Ms. L is involuntarily admitted to our inpatient unit. Although she acknowledges weight loss, she minimizes the severity of her illness and indicates she would like to gain weight, but only by eating healthy foods she is comfortable with, including kale, quinoa, and vegetables. Ms. L says that she has always been interested in “healthful foods” and that she “loves sugar,” but “it’s bad for you,” mentioning that “sugar fuels cancer.” She has daily thoughts about sugar causing cancer. Ms. L also mentions that she stopped eating flour, sugar, fried food, and oils because those foods affect her “stomach acid” and cause “pimples on my face and weight loss.” While in the inpatient unit, Ms. L requests a special diet and demands to know the origin and ingredients of the foods she is offered. She emphasizes that her esophageal cancer diagnosis and dysphagia exacerbate worries that certain foods cause cancer, and wants to continue her diet restrictions. Nonetheless, she says she wants to get healthy, and denies an intense fear of gaining weight or feeling fat.
HISTORY Multiple psychiatric diagnoses
Ms. L lives alone and enjoys spending time with her grandchildren, visiting museums, and listening to classical music. However, her family, social workers, and records from a previous psychiatric hospitalization reveal that Ms. L has a history of psychiatric illness and fears regarding certain types of foods for much of her adult life. Ms. L’s family also described a range of compulsive behaviors, including shoplifting, hoarding art, multiple plastic surgeries, and phases where Ms. L ate only frozen yogurt without sugar.
Ms. L’s daughter reported that Ms. L had seen a psychologist in the late 1990s for depression and had been diagnosed with obsessive-compulsive disorder (OCD) and attention deficit/hyperactivity disorder in the early 2000s. In 2006, during a depressive episode after her divorce, Ms. L had a suicide attempt with pills and alcohol, and was hospitalized. Records from that stay described a history of mood dysregulation with fears regarding food and nutrition. Ms. L was treated with aripiprazole 5 mg/d. A trial of trazodone 25 mg/d did not have any effect. When discharged, she was receiving lamotrigine 100 mg/d. However, her daughter believes she stopped taking all psychiatric medications shortly after discharge.
Her daughter says that in the past 2 years, Ms. L has seen multiple doctors for treatment of somatic gastrointestinal (GI) complaints. A 2018 note from a social worker indicated that Ms. L endorsed taking >80 supplements per day and constantly researched nutrition online. In the months leading to her current hospitalization, Ms. L suffered from severe self-neglect and fear regarding foods she felt were not healthy for her. She had stopped leaving her apartment.
Continue to: EVALUATION Poor insight, normal lab results...
EVALUATION Poor insight, normal lab results
During her evaluation, Ms. L appears cachectic and frail. She has a heavily constricted affect and is guarded, dismissive, and vague. Although her thought processes are linear and goal-directed, her insight into her condition is extremely poor and she appears surprised when clinicians inform her that her self-neglect would lead to death. Instead, Ms. L insists she is eating healthily and demonstrates severe anxiety in relation to her GI symptoms.
Ms. L is oriented to person, place, and time. She scores 27/30 on the Montreal Cognitive Assessment, indicating normal cognition. She denies any depressive symptoms or suicidal intent. She does not appear to be internally preoccupied and denies having auditory or visual hallucinations or manic symptoms.
A neurologic examination reveals that her cranial nerves are normal, and cerebellar function, strength, and sensory testing are intact. Her gait is steady and she walks without a walker. Despite her severely low BMI and recent history of self-neglect, Ms. L’s laboratory results are remarkably normal and show no liver, metabolic, or electrolyte abnormalities, no signs of infection, and normal vitamin B12 levels. She has slightly elevated creatinine and blood urea nitrogen levels, but a normal glomerular filtration rate.
Her medical history is significant for squamous cell esophageal cancer, treated with radiofrequency ablation. Although Ms. L is constantly worried about the recurrence of cancer, pathology reports demonstrate no esophageal dysplasia. However, she does show evidence of an approximately 1 cm × 1 cm mild, noncircumferential esophageal stenosis, likely resulting from radiofrequency ablation.
[polldaddy:11079394]
The authors’ observations
Several health- and physical symptom-related psychiatric disorders have overlapping features, which can complicate the differential diagnosis (Table 11). Ms. L presented to the ED with a severely low BMI of 13.5 kg/m2, obsessions regarding specific types of food, and preoccupations regarding her esophagus. Despite her extensive psychiatric history (including intense fears regarding food), we ruled out a primary psychotic disorder because she did not describe auditory or visual hallucinations and never appeared internally preoccupied. While her BMI and persistent minimization of the extent of her disease meet criteria for anorexia nervosa, she denied body dysmorphia and did not have any fear of gaining weight.
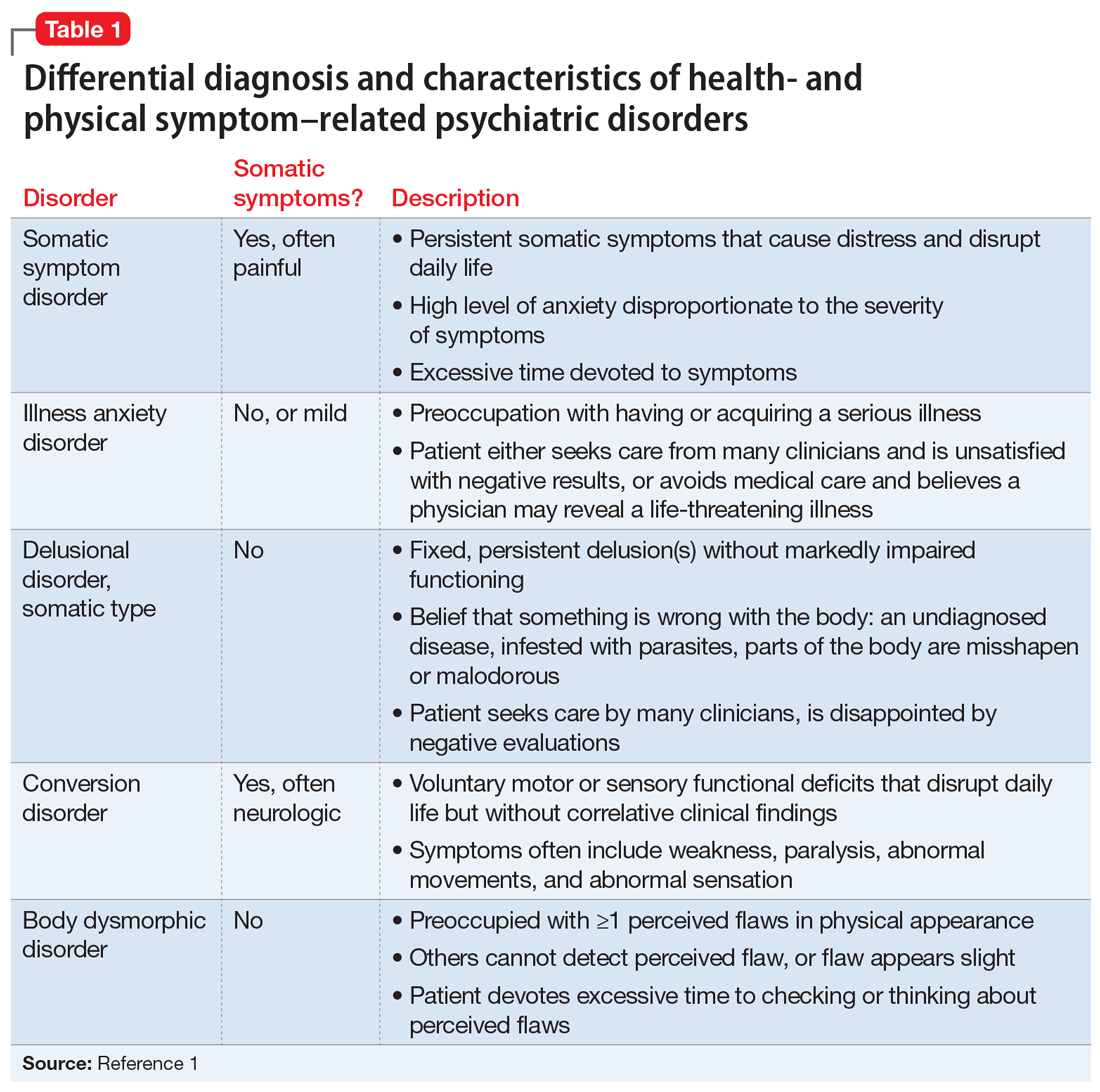
A central element of Ms. L’s presentation was her anxiety regarding how certain types of foods impact her health as well as her anxieties regarding her esophagus. While Ms. L was in remission from esophageal cancer and had a diagnosis of esophageal dysphagia, these preoccupations and obsessions regarding how certain types of foods affect her esophagus drove her to self-neglect and thus represent pathologic thought processes out of proportion to her symptoms. Illness anxiety disorder was considered because Ms. L met many of its criteria: preoccupation with having a serious illness, disproportionate preoccupation with somatic symptoms if they are present, extreme anxiety over health, and performance of health-related behaviors.1 However, illness anxiety disorder is a diagnosis of exclusion, and 1 criterion is that these symptoms cannot be explained by another mental disorder. We felt other diagnoses better fit Ms. L’s condition and ruled out illness anxiety disorder.
Ms. L’s long history of food and non-food–related obsessions and compulsions that interrupted her ability to perform daily activities were strongly suggestive for OCD. Additionally, her intense preoccupation, high level of anxiety, amount of time and energy spent seeking care for her esophagus and GERD symptoms, and the resulting significant disruption of daily life, met criteria for somatic symptom disorder (SSD). However, we did not believe that a diagnosis of OCD and SSD alone explained the entirety of Ms. L’s clinical picture. Despite ruling out anorexia nervosa, Ms. L nonetheless demonstrated disordered eating.
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder in which patients restrict their diet and do not meet nutritional needs for any number of reasons, do not experience body dysmorphia, and do not fear weight gain.1 A common feature of ARFID is a fear of negative consequences from eating specific types of food.2 Table 21,2 summarizes additional clinical features of ARFID. Although ARFID is typically diagnosed in children and adolescents, particularly in individuals with autism with heightened sensory sensitivities, ARFID is also common among adult patients with GI disorders.3 In a retrospective chart review of 410 adults ages 18 to 90 (73% women) referred to a neurogastroenterology care center, 6.3% met the full criteria for ARFID and 17.3% had clinically significant avoidant or restrictive eating behaviors. Among patients with ARFID symptoms, 93% stated that a fear of GI symptoms was the driver of their avoidant or restrictive eating behaviors.2 Patients with GI diseases often develop dietary control and avoidance coping mechanisms to alleviate their symptoms.4 These strategies can exacerbate health anxieties and have a detrimental effect on mental health.5 Patients with GI disorders have a high degree of comorbidity with affective disorders, including anxiety disorders.6 These trends may arise from hypervigilance and the need to gain control over physical symptoms.7 Feeling a need for control, actions driven by anxiety and fear, and the need for compensatory behaviors are cardinal features of OCD and eating disorders.8 Multiple studies have demonstrated comorbidities between irritable bowel syndrome and eating disorders,9 SSD,10 and OCD.11 Taken together with observations that ARFID is also found in patients with GI disorders,2 these findings demonstrate that patients with a history of GI disease are at high risk of developing extreme health anxieties and behavioral coping strategies that can lead to disordered eating.
The rise in “healthy” eating materials online—particularly on social media—has created an atmosphere in which misinformation regarding diet and health is common and widespread. For patients with OCD and a predisposition to health anxiety, such as Ms. L, searching online for nutrition information and healthy living habits can exacerbate food-related anxieties and can lead to a pathological drive for purity and health.12Although not included in DSM-5, orthorexia nervosa was identified in 1997 as a proposed eating disorder best characterized as an obsession with healthy eating with associated restrictive behaviors.13 Patients with this disorder are rarely focused on losing weight, and orthorexic eating behaviors have been associated with both SSD and OCD.12,14 As in Ms. L’s case, patients with orthorexia nervosa demonstrate intrusive obsessions with nutrition, spend excessive amount of time researching nutrition, and fixate on food quality.12 Throughout Ms. L’s hospitalization, even as her food-related magical thinking symptoms improved, she constantly informed her care team that she had been “eating healthily” even though she was severely cachectic. Patients with SSD and OCD prone to health anxieties are at risk of developing pathologic food beliefs and dangerous eating behaviors. These patients may benefit from psychoeducation regarding nutrition and media literacy, which are components of effective eating disorder programs.15
[polldaddy:11079399]
Continue to: The authors' observations...
The authors’ observations
How do we approach the pharmacologic treatment of patients with co-occurring eating, somatic symptom, and anxiety disorders? Olanzapine facilitates recovery in children and adolescents with ARFID by promoting eating and weight gain, and decreasing symptoms of depression and anxiety.16 Patients with orthorexia nervosa also may benefit from treatment with olanzapine, which has decreased food-related fixations, magical thinking, and delusions regarding food.17 Further, orthorexic patients with ARFID have also been shown to respond to SSRIs due to those agents’ efficacy for treating intrusive thoughts, obsessions, and preoccupations from OCD and SSD.18,19 Thus, treating Ms. L’s symptoms with olanzapine and fluoxetine targeted the intersection of several diagnoses on our differential. Olanzapine’s propensity to cause weight gain is favorable in this population, particularly patients such as Ms. L, who do not exhibit body dysmorphia or fear of gaining weight.
OUTCOME Weight gain and fewer fears
Ms. L is prescribed olanzapine 5 mg/d and fluoxetine 20 mg/d. She gains 20.6 pounds in 4 weeks. Importantly, she endorses fewer fears related to foods and expands her palate to include foods she previously considered to be unhealthy, including white bread and farm-raised salmon. Further, she spends less time thinking about food and says she has less anxiety regarding the recurrence of GI symptoms.
CASE Fixated on health and nutrition
At the insistence of her daughter, Ms. L, age 75, presents to the emergency department (ED) for self-neglect and severe weight loss, with a body mass index (BMI) of 13.5 kg/m2 (normal: 18.5 to 24.9 kg/m2). When asked why she is in the ED, Ms. L says she doesn’t know. She attributes her significant weight loss (approximately 20 pounds in the last few months) to gastroesophageal reflux disease (GERD). She constantly worries about her esophagus. She had been diagnosed with esophageal dysphagia 7 years ago after undergoing radiofrequency ablation for esophageal cancer. Ms. L fixates on the negative effects certain foods and ingredients might have on her stomach and esophagus.
Following transfer from the ED, Ms. L is involuntarily admitted to our inpatient unit. Although she acknowledges weight loss, she minimizes the severity of her illness and indicates she would like to gain weight, but only by eating healthy foods she is comfortable with, including kale, quinoa, and vegetables. Ms. L says that she has always been interested in “healthful foods” and that she “loves sugar,” but “it’s bad for you,” mentioning that “sugar fuels cancer.” She has daily thoughts about sugar causing cancer. Ms. L also mentions that she stopped eating flour, sugar, fried food, and oils because those foods affect her “stomach acid” and cause “pimples on my face and weight loss.” While in the inpatient unit, Ms. L requests a special diet and demands to know the origin and ingredients of the foods she is offered. She emphasizes that her esophageal cancer diagnosis and dysphagia exacerbate worries that certain foods cause cancer, and wants to continue her diet restrictions. Nonetheless, she says she wants to get healthy, and denies an intense fear of gaining weight or feeling fat.
HISTORY Multiple psychiatric diagnoses
Ms. L lives alone and enjoys spending time with her grandchildren, visiting museums, and listening to classical music. However, her family, social workers, and records from a previous psychiatric hospitalization reveal that Ms. L has a history of psychiatric illness and fears regarding certain types of foods for much of her adult life. Ms. L’s family also described a range of compulsive behaviors, including shoplifting, hoarding art, multiple plastic surgeries, and phases where Ms. L ate only frozen yogurt without sugar.
Ms. L’s daughter reported that Ms. L had seen a psychologist in the late 1990s for depression and had been diagnosed with obsessive-compulsive disorder (OCD) and attention deficit/hyperactivity disorder in the early 2000s. In 2006, during a depressive episode after her divorce, Ms. L had a suicide attempt with pills and alcohol, and was hospitalized. Records from that stay described a history of mood dysregulation with fears regarding food and nutrition. Ms. L was treated with aripiprazole 5 mg/d. A trial of trazodone 25 mg/d did not have any effect. When discharged, she was receiving lamotrigine 100 mg/d. However, her daughter believes she stopped taking all psychiatric medications shortly after discharge.
Her daughter says that in the past 2 years, Ms. L has seen multiple doctors for treatment of somatic gastrointestinal (GI) complaints. A 2018 note from a social worker indicated that Ms. L endorsed taking >80 supplements per day and constantly researched nutrition online. In the months leading to her current hospitalization, Ms. L suffered from severe self-neglect and fear regarding foods she felt were not healthy for her. She had stopped leaving her apartment.
Continue to: EVALUATION Poor insight, normal lab results...
EVALUATION Poor insight, normal lab results
During her evaluation, Ms. L appears cachectic and frail. She has a heavily constricted affect and is guarded, dismissive, and vague. Although her thought processes are linear and goal-directed, her insight into her condition is extremely poor and she appears surprised when clinicians inform her that her self-neglect would lead to death. Instead, Ms. L insists she is eating healthily and demonstrates severe anxiety in relation to her GI symptoms.
Ms. L is oriented to person, place, and time. She scores 27/30 on the Montreal Cognitive Assessment, indicating normal cognition. She denies any depressive symptoms or suicidal intent. She does not appear to be internally preoccupied and denies having auditory or visual hallucinations or manic symptoms.
A neurologic examination reveals that her cranial nerves are normal, and cerebellar function, strength, and sensory testing are intact. Her gait is steady and she walks without a walker. Despite her severely low BMI and recent history of self-neglect, Ms. L’s laboratory results are remarkably normal and show no liver, metabolic, or electrolyte abnormalities, no signs of infection, and normal vitamin B12 levels. She has slightly elevated creatinine and blood urea nitrogen levels, but a normal glomerular filtration rate.
Her medical history is significant for squamous cell esophageal cancer, treated with radiofrequency ablation. Although Ms. L is constantly worried about the recurrence of cancer, pathology reports demonstrate no esophageal dysplasia. However, she does show evidence of an approximately 1 cm × 1 cm mild, noncircumferential esophageal stenosis, likely resulting from radiofrequency ablation.
[polldaddy:11079394]
The authors’ observations
Several health- and physical symptom-related psychiatric disorders have overlapping features, which can complicate the differential diagnosis (Table 11). Ms. L presented to the ED with a severely low BMI of 13.5 kg/m2, obsessions regarding specific types of food, and preoccupations regarding her esophagus. Despite her extensive psychiatric history (including intense fears regarding food), we ruled out a primary psychotic disorder because she did not describe auditory or visual hallucinations and never appeared internally preoccupied. While her BMI and persistent minimization of the extent of her disease meet criteria for anorexia nervosa, she denied body dysmorphia and did not have any fear of gaining weight.
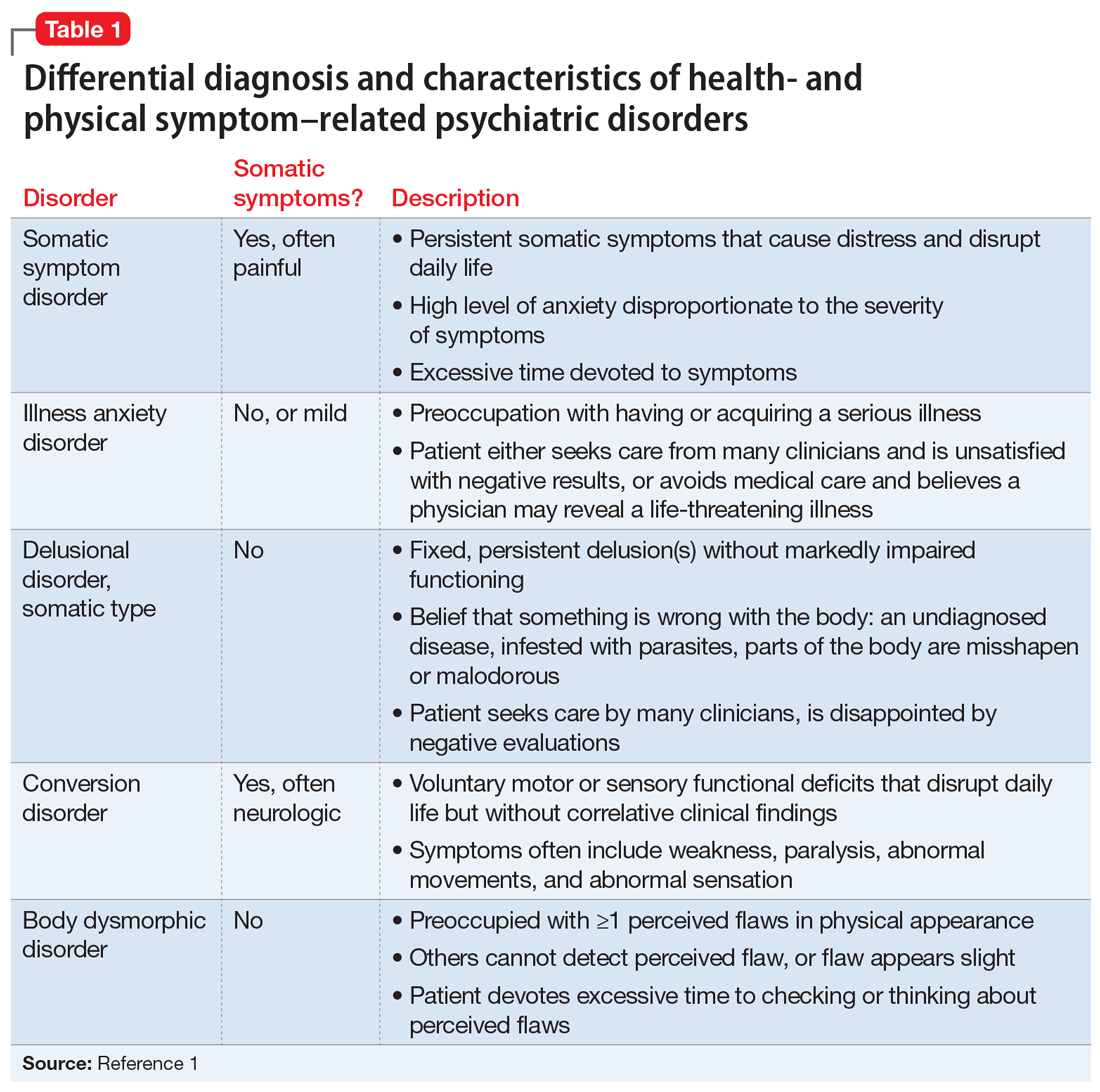
A central element of Ms. L’s presentation was her anxiety regarding how certain types of foods impact her health as well as her anxieties regarding her esophagus. While Ms. L was in remission from esophageal cancer and had a diagnosis of esophageal dysphagia, these preoccupations and obsessions regarding how certain types of foods affect her esophagus drove her to self-neglect and thus represent pathologic thought processes out of proportion to her symptoms. Illness anxiety disorder was considered because Ms. L met many of its criteria: preoccupation with having a serious illness, disproportionate preoccupation with somatic symptoms if they are present, extreme anxiety over health, and performance of health-related behaviors.1 However, illness anxiety disorder is a diagnosis of exclusion, and 1 criterion is that these symptoms cannot be explained by another mental disorder. We felt other diagnoses better fit Ms. L’s condition and ruled out illness anxiety disorder.
Ms. L’s long history of food and non-food–related obsessions and compulsions that interrupted her ability to perform daily activities were strongly suggestive for OCD. Additionally, her intense preoccupation, high level of anxiety, amount of time and energy spent seeking care for her esophagus and GERD symptoms, and the resulting significant disruption of daily life, met criteria for somatic symptom disorder (SSD). However, we did not believe that a diagnosis of OCD and SSD alone explained the entirety of Ms. L’s clinical picture. Despite ruling out anorexia nervosa, Ms. L nonetheless demonstrated disordered eating.
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder in which patients restrict their diet and do not meet nutritional needs for any number of reasons, do not experience body dysmorphia, and do not fear weight gain.1 A common feature of ARFID is a fear of negative consequences from eating specific types of food.2 Table 21,2 summarizes additional clinical features of ARFID. Although ARFID is typically diagnosed in children and adolescents, particularly in individuals with autism with heightened sensory sensitivities, ARFID is also common among adult patients with GI disorders.3 In a retrospective chart review of 410 adults ages 18 to 90 (73% women) referred to a neurogastroenterology care center, 6.3% met the full criteria for ARFID and 17.3% had clinically significant avoidant or restrictive eating behaviors. Among patients with ARFID symptoms, 93% stated that a fear of GI symptoms was the driver of their avoidant or restrictive eating behaviors.2 Patients with GI diseases often develop dietary control and avoidance coping mechanisms to alleviate their symptoms.4 These strategies can exacerbate health anxieties and have a detrimental effect on mental health.5 Patients with GI disorders have a high degree of comorbidity with affective disorders, including anxiety disorders.6 These trends may arise from hypervigilance and the need to gain control over physical symptoms.7 Feeling a need for control, actions driven by anxiety and fear, and the need for compensatory behaviors are cardinal features of OCD and eating disorders.8 Multiple studies have demonstrated comorbidities between irritable bowel syndrome and eating disorders,9 SSD,10 and OCD.11 Taken together with observations that ARFID is also found in patients with GI disorders,2 these findings demonstrate that patients with a history of GI disease are at high risk of developing extreme health anxieties and behavioral coping strategies that can lead to disordered eating.
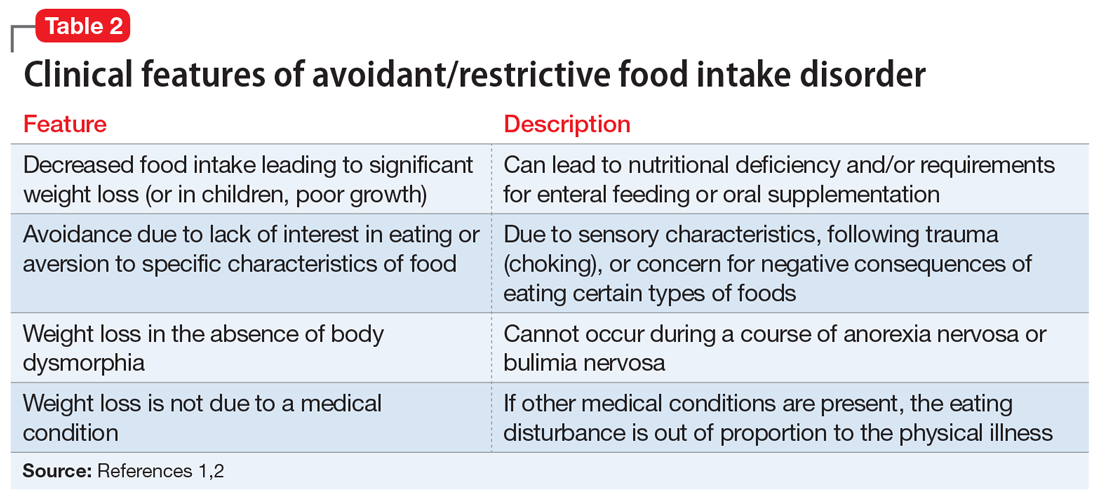
The rise in “healthy” eating materials online—particularly on social media—has created an atmosphere in which misinformation regarding diet and health is common and widespread. For patients with OCD and a predisposition to health anxiety, such as Ms. L, searching online for nutrition information and healthy living habits can exacerbate food-related anxieties and can lead to a pathological drive for purity and health.12Although not included in DSM-5, orthorexia nervosa was identified in 1997 as a proposed eating disorder best characterized as an obsession with healthy eating with associated restrictive behaviors.13 Patients with this disorder are rarely focused on losing weight, and orthorexic eating behaviors have been associated with both SSD and OCD.12,14 As in Ms. L’s case, patients with orthorexia nervosa demonstrate intrusive obsessions with nutrition, spend excessive amount of time researching nutrition, and fixate on food quality.12 Throughout Ms. L’s hospitalization, even as her food-related magical thinking symptoms improved, she constantly informed her care team that she had been “eating healthily” even though she was severely cachectic. Patients with SSD and OCD prone to health anxieties are at risk of developing pathologic food beliefs and dangerous eating behaviors. These patients may benefit from psychoeducation regarding nutrition and media literacy, which are components of effective eating disorder programs.15
[polldaddy:11079399]
Continue to: The authors' observations...
The authors’ observations
How do we approach the pharmacologic treatment of patients with co-occurring eating, somatic symptom, and anxiety disorders? Olanzapine facilitates recovery in children and adolescents with ARFID by promoting eating and weight gain, and decreasing symptoms of depression and anxiety.16 Patients with orthorexia nervosa also may benefit from treatment with olanzapine, which has decreased food-related fixations, magical thinking, and delusions regarding food.17 Further, orthorexic patients with ARFID have also been shown to respond to SSRIs due to those agents’ efficacy for treating intrusive thoughts, obsessions, and preoccupations from OCD and SSD.18,19 Thus, treating Ms. L’s symptoms with olanzapine and fluoxetine targeted the intersection of several diagnoses on our differential. Olanzapine’s propensity to cause weight gain is favorable in this population, particularly patients such as Ms. L, who do not exhibit body dysmorphia or fear of gaining weight.
OUTCOME Weight gain and fewer fears
Ms. L is prescribed olanzapine 5 mg/d and fluoxetine 20 mg/d. She gains 20.6 pounds in 4 weeks. Importantly, she endorses fewer fears related to foods and expands her palate to include foods she previously considered to be unhealthy, including white bread and farm-raised salmon. Further, she spends less time thinking about food and says she has less anxiety regarding the recurrence of GI symptoms.
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Murray HB, Bailey AP, Keshishian AC. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995-2002.e1.
3. Görmez A, Kılıç A, Kırpınar İ. Avoidant/restrictive food intake disorder: an adult case responding to cognitive behavioral therapy. Clinical Case Studies. 2018;17(6):443-452.
4. Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016;28(12):1915-1920.
5. Melchior C, Desprez C, Riachi G, et al. Anxiety and depression profile is associated with eating disorders in patients with irritable bowel syndrome. Front Psychiatry. 2020;10:928.
6. Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62 Suppl 8:28-37.
7. Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372-377.
8. Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253-274.
9. Perkins SJ, Keville S, Schmidt U, et al. Eating disorders and irritable bowel syndrome: is there a link? J Psychosom Res. 2005;59(2):57-64.
10. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(2):6024-6030.
11. Masand PS, Keuthen NJ, Gupta S, et al. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11(1):21-25.
12. Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385-394.
13. Bratman S. Health food junkie. Yoga Journal. 1997;136:42-50.
14. Barthels F, Müller R, Schüth T, et al. Orthorexic eating behavior in patients with somatoform disorders. Eat Weight Disord. 2021;26(1):135-143.
15. Ciao AC, Loth K, Neumark-Sztainer D. Preventing eating disorder pathology: common and unique features of successful eating disorders prevention programs. Curr Psychiatry Rep. 2014;16(7):453.
16. Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920-922.
17. Moroze RM, Dunn TM, Craig Holland J, et al. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56(4):397-403.
18. Spettigue W, Norris ML, Santos A, et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord. 2018;6:20.
19. Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health. 2021;18(10):5488. Published 2021 May 20. doi:10.3390/ijerph18105488 Prevalence of orthorexia nervosa and its diagnostic tools-a literature review. Int J Environ Res Public Health. 2021;18(10):5488.
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Murray HB, Bailey AP, Keshishian AC. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995-2002.e1.
3. Görmez A, Kılıç A, Kırpınar İ. Avoidant/restrictive food intake disorder: an adult case responding to cognitive behavioral therapy. Clinical Case Studies. 2018;17(6):443-452.
4. Reed-Knight B, Squires M, Chitkara DK, et al. Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: a pilot comparison study to healthy adolescents. Neurogastroenterol Motil. 2016;28(12):1915-1920.
5. Melchior C, Desprez C, Riachi G, et al. Anxiety and depression profile is associated with eating disorders in patients with irritable bowel syndrome. Front Psychiatry. 2020;10:928.
6. Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62 Suppl 8:28-37.
7. Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372-377.
8. Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253-274.
9. Perkins SJ, Keville S, Schmidt U, et al. Eating disorders and irritable bowel syndrome: is there a link? J Psychosom Res. 2005;59(2):57-64.
10. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(2):6024-6030.
11. Masand PS, Keuthen NJ, Gupta S, et al. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11(1):21-25.
12. Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385-394.
13. Bratman S. Health food junkie. Yoga Journal. 1997;136:42-50.
14. Barthels F, Müller R, Schüth T, et al. Orthorexic eating behavior in patients with somatoform disorders. Eat Weight Disord. 2021;26(1):135-143.
15. Ciao AC, Loth K, Neumark-Sztainer D. Preventing eating disorder pathology: common and unique features of successful eating disorders prevention programs. Curr Psychiatry Rep. 2014;16(7):453.
16. Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920-922.
17. Moroze RM, Dunn TM, Craig Holland J, et al. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56(4):397-403.
18. Spettigue W, Norris ML, Santos A, et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord. 2018;6:20.
19. Niedzielski A, Kaźmierczak-Wojtaś N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools-A Literature Review. Int J Environ Res Public Health. 2021;18(10):5488. Published 2021 May 20. doi:10.3390/ijerph18105488 Prevalence of orthorexia nervosa and its diagnostic tools-a literature review. Int J Environ Res Public Health. 2021;18(10):5488.
Jury is out on universal screening for eating disorders
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
Eating disorders (binge eating disorder, bulimia nervosa, and anorexia nervosa) can cause “serious harms to physical and psychosocial health and take a tremendous toll on individuals and families,” task force member Lori Pbert, PhD, told this news organization.
“Screening for eating disorders has the potential to improve health by leading to early detection and effective treatment,” said Dr. Pbert, with the department of population and quantitative health sciences, University of Massachusetts, Worcester.
However, a “deep dive” into the available literature failed to turn up adequate evidence to recommend for or against routine screening for eating disorders for children and adolescents aged 10 years and older and for adults who have no signs or symptoms of an eating disorder or concerns about their eating and who have not previously been diagnosed with an eating disorder, Dr. Pbert said.
The task force, therefore, issued an “I” statement (insufficient evidence), meaning it cannot at this time recommend for or against screening for eating disorders.
An “I” statement is “fundamentally a call for more research,” Dr. Pbert noted.
Adolescents and adults who have signs and symptoms of an eating disorder – which include rapid weight loss; weight gain or pronounced deviation from growth trajectory; pubertal delay; bradycardia; oligomenorrhea; and amenorrhea – are not included in this recommendation.
The USPSTF recommendation statement and accompanying evidence report were published online March 15 in JAMA.
Clinical judgment key
In the absence of evidence, clinicians should use their judgment when determining whether or not to screen an individual patient for an eating disorder, Dr. Pbert advised.
One thing to consider is whether the patient is in a group at higher risk for eating disorders, such as athletes, females, young adults aged 18-29, and transgender individuals.
Another is whether the patient reports engaging in unhealthy weight control behaviors, such as fasting or skipping meals, Dr. Pbert said.
Importantly, any patient who has signs or symptoms of an eating disorder or is expressing concerns about their eating should be assessed and referred for appropriate care, Dr. Pbert said.
“The good news is that eating disorders can be treated,” she said.
Several organizations currently recommend screening in the context of monitoring changes in weight and other vital signs or signs and symptoms to determine whether a patient might have an eating disorder.
Dr. Pbert said it’s important to recognize that the USPSTF statement “doesn’t really conflict” with the recommendations of other organizations. “We all agree that patients who present with signs or symptoms of an eating disorder should be assessed further.”
Evidence gaps
The authors of an invited commentary in JAMA) say the task force has identified several “notable deficiencies” in the available data on screening for eating disorders.
“Directing attention to rigorous research to close this evidence gap will be important to find optimal approaches to identify patients with these complex disorders and improve their health outcomes,” write Evelyn Attia, MD, with Weill Cornell Medicine in New York, and Angela Guarda, MD, with Johns Hopkins University, Baltimore.
This “I” statement, they say, “highlights the need to prioritize research aimed at closing the evidence gap identified by USPSTF in a timely manner and underscores the need for new studies that address screening for eating disorders, treatment trials that enroll screen-detected populations from primary care settings, and screening in specific populations.
“Research on screening in primary care also should be paired with development and assessment of early brief intervention strategies for those individuals who screen positive, especially adolescents,” Dr. Attia and Dr. Guarda say.
Members of the USPSTF have disclosed no relevant financial relationships. Dr. Attia has received research support from the National Institute of Mental Health and the Hilda & Preston David Foundation; royalties from UpToDate; and has served as a clinical advisor to Equip Health. Dr. Guarda has received support from the Stephen and Jean Robinson Fund and research funding from the Klarman Family Foundation.
A version of this article first appeared on Medscape.com.
‘Bigorexia’: Why teenage boys are obsessed with bulking up
Why are teenage boys obsessed with bulking up?
While the effects of Instagram on girls’ body image has long been documented – an article in The Wall Street Journal that was published this fall reported that Facebook knew Instagram was toxic for teen girls – teenage boys are under just as much pressure.
For adolescent boys, the goal is often to get superhero-size buff – and this is leading to anxiety, stress, excessive selfies, and, often, obsessive staring in the mirror to assess their “pec” progress.
So-called “bigorexia” – or extreme gym time, excessive focus on protein diets, and intense muscle-building goals – has hit new and concerning levels, according to a recent New York Times report.
Whether it’s the pandemic or TikTok that’s to blame, teen boys are pushing hard to achieve six-pack abs, with one-third of them in the U.S. trying to bulk up, according to a study published in the Journal of Adolescent Health. What’s more, 22% reported they’re engaging in muscle-enhancing behavior, including excess exercise, taking supplements or steroids, or eating more to bulk up, according to a study published in the International Journal of Eating Disorders.
“The pandemic and social media have been a perfect storm for eating disorders and body image issues for all teens, but this has been under-recognized in boys,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Both are directly connected to an increase in muscle dysmorphia.”
While “bigorexia” is a newer term coined by mental health professionals, the concept of muscular dysmorphia isn’t, says Jennifer Bahrman, PhD, a licensed psychologist with McGovern Medical School at UTHealth Houston. This may be why about a third of boys ages 11-18 reported that they aren’t enamored with their bodies, according to a small survey published in 2019 in the Californian Journal of Health Promotion.
“When we think of dysmorphia, we think of girls having it, since we see it more in females,” says Dr. Bahrman, who works extensively with adolescents and athletes. “The interesting thing about muscular dysmorphia is that it’s the only body dysmorphic disorder that’s almost exclusively present in males.”
Social media’s role
Unlike other things in boys’ lives, like movies, TV, or even the uber-buff GI Joe doll, social media has created opportunities for young men to put their bodies on display – and become an influencer or get followers because of it.
“An everyday teen can become a celebrity,” Dr. Nagata says. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example, as well as bodybuilding equipment, and that will further distort reality.”
Before-and-after photos are also known to be quite misleading.
“Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Dr. Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends.”
But as many are aware, photos posted to social media are selected to tell the best story – with the best filters, lighting, and angles possible, however exaggerated.
“A guy will post his worst picture out of a thousand for his before shot and then post the best photo out of a thousand,” Dr. Nagata says. “This, in itself, can really confuse a teenager, because the story of this person’s changed body looks so realistic.”
Worse, these images tend to be damaging to your teenager’s self-esteem.
“When you see images of people you’re aspiring to look like, it can be very upsetting,” Dr. Bahrman says. “After all, it’s easy to think, ‘I’m doing all of these pushups, and I don’t look like this.’ From there, it’s easy to begin internalizing that something is wrong with you.”
Red flags to watch out for
If you’ve noticed that your son is obsessed with his appearance, weight, food, or exercise, take note. Also, notice if he’s asking you to buy protein powder or is spending more time at the gym than with his friends.
“Pay attention if he is withdrawing from friends and family because of his concerns about his appearance,” Dr. Nagata says. “For example, we often hear that a teenager will no longer eat family meals or at a restaurant because the protein content isn’t high enough or the food is too fatty.”
If you’re concerned, always make sure to discuss this with your son’s pediatrician.
“Ultimately, you want to make sure you share your concerns before your teen son becomes even more body-image obsessed,” Dr. Nagata says.
A version of this article first appeared on WebMD.com.
Why are teenage boys obsessed with bulking up?
While the effects of Instagram on girls’ body image has long been documented – an article in The Wall Street Journal that was published this fall reported that Facebook knew Instagram was toxic for teen girls – teenage boys are under just as much pressure.
For adolescent boys, the goal is often to get superhero-size buff – and this is leading to anxiety, stress, excessive selfies, and, often, obsessive staring in the mirror to assess their “pec” progress.
So-called “bigorexia” – or extreme gym time, excessive focus on protein diets, and intense muscle-building goals – has hit new and concerning levels, according to a recent New York Times report.
Whether it’s the pandemic or TikTok that’s to blame, teen boys are pushing hard to achieve six-pack abs, with one-third of them in the U.S. trying to bulk up, according to a study published in the Journal of Adolescent Health. What’s more, 22% reported they’re engaging in muscle-enhancing behavior, including excess exercise, taking supplements or steroids, or eating more to bulk up, according to a study published in the International Journal of Eating Disorders.
“The pandemic and social media have been a perfect storm for eating disorders and body image issues for all teens, but this has been under-recognized in boys,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Both are directly connected to an increase in muscle dysmorphia.”
While “bigorexia” is a newer term coined by mental health professionals, the concept of muscular dysmorphia isn’t, says Jennifer Bahrman, PhD, a licensed psychologist with McGovern Medical School at UTHealth Houston. This may be why about a third of boys ages 11-18 reported that they aren’t enamored with their bodies, according to a small survey published in 2019 in the Californian Journal of Health Promotion.
“When we think of dysmorphia, we think of girls having it, since we see it more in females,” says Dr. Bahrman, who works extensively with adolescents and athletes. “The interesting thing about muscular dysmorphia is that it’s the only body dysmorphic disorder that’s almost exclusively present in males.”
Social media’s role
Unlike other things in boys’ lives, like movies, TV, or even the uber-buff GI Joe doll, social media has created opportunities for young men to put their bodies on display – and become an influencer or get followers because of it.
“An everyday teen can become a celebrity,” Dr. Nagata says. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example, as well as bodybuilding equipment, and that will further distort reality.”
Before-and-after photos are also known to be quite misleading.
“Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Dr. Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends.”
But as many are aware, photos posted to social media are selected to tell the best story – with the best filters, lighting, and angles possible, however exaggerated.
“A guy will post his worst picture out of a thousand for his before shot and then post the best photo out of a thousand,” Dr. Nagata says. “This, in itself, can really confuse a teenager, because the story of this person’s changed body looks so realistic.”
Worse, these images tend to be damaging to your teenager’s self-esteem.
“When you see images of people you’re aspiring to look like, it can be very upsetting,” Dr. Bahrman says. “After all, it’s easy to think, ‘I’m doing all of these pushups, and I don’t look like this.’ From there, it’s easy to begin internalizing that something is wrong with you.”
Red flags to watch out for
If you’ve noticed that your son is obsessed with his appearance, weight, food, or exercise, take note. Also, notice if he’s asking you to buy protein powder or is spending more time at the gym than with his friends.
“Pay attention if he is withdrawing from friends and family because of his concerns about his appearance,” Dr. Nagata says. “For example, we often hear that a teenager will no longer eat family meals or at a restaurant because the protein content isn’t high enough or the food is too fatty.”
If you’re concerned, always make sure to discuss this with your son’s pediatrician.
“Ultimately, you want to make sure you share your concerns before your teen son becomes even more body-image obsessed,” Dr. Nagata says.
A version of this article first appeared on WebMD.com.
Why are teenage boys obsessed with bulking up?
While the effects of Instagram on girls’ body image has long been documented – an article in The Wall Street Journal that was published this fall reported that Facebook knew Instagram was toxic for teen girls – teenage boys are under just as much pressure.
For adolescent boys, the goal is often to get superhero-size buff – and this is leading to anxiety, stress, excessive selfies, and, often, obsessive staring in the mirror to assess their “pec” progress.
So-called “bigorexia” – or extreme gym time, excessive focus on protein diets, and intense muscle-building goals – has hit new and concerning levels, according to a recent New York Times report.
Whether it’s the pandemic or TikTok that’s to blame, teen boys are pushing hard to achieve six-pack abs, with one-third of them in the U.S. trying to bulk up, according to a study published in the Journal of Adolescent Health. What’s more, 22% reported they’re engaging in muscle-enhancing behavior, including excess exercise, taking supplements or steroids, or eating more to bulk up, according to a study published in the International Journal of Eating Disorders.
“The pandemic and social media have been a perfect storm for eating disorders and body image issues for all teens, but this has been under-recognized in boys,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Both are directly connected to an increase in muscle dysmorphia.”
While “bigorexia” is a newer term coined by mental health professionals, the concept of muscular dysmorphia isn’t, says Jennifer Bahrman, PhD, a licensed psychologist with McGovern Medical School at UTHealth Houston. This may be why about a third of boys ages 11-18 reported that they aren’t enamored with their bodies, according to a small survey published in 2019 in the Californian Journal of Health Promotion.
“When we think of dysmorphia, we think of girls having it, since we see it more in females,” says Dr. Bahrman, who works extensively with adolescents and athletes. “The interesting thing about muscular dysmorphia is that it’s the only body dysmorphic disorder that’s almost exclusively present in males.”
Social media’s role
Unlike other things in boys’ lives, like movies, TV, or even the uber-buff GI Joe doll, social media has created opportunities for young men to put their bodies on display – and become an influencer or get followers because of it.
“An everyday teen can become a celebrity,” Dr. Nagata says. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example, as well as bodybuilding equipment, and that will further distort reality.”
Before-and-after photos are also known to be quite misleading.
“Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Dr. Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends.”
But as many are aware, photos posted to social media are selected to tell the best story – with the best filters, lighting, and angles possible, however exaggerated.
“A guy will post his worst picture out of a thousand for his before shot and then post the best photo out of a thousand,” Dr. Nagata says. “This, in itself, can really confuse a teenager, because the story of this person’s changed body looks so realistic.”
Worse, these images tend to be damaging to your teenager’s self-esteem.
“When you see images of people you’re aspiring to look like, it can be very upsetting,” Dr. Bahrman says. “After all, it’s easy to think, ‘I’m doing all of these pushups, and I don’t look like this.’ From there, it’s easy to begin internalizing that something is wrong with you.”
Red flags to watch out for
If you’ve noticed that your son is obsessed with his appearance, weight, food, or exercise, take note. Also, notice if he’s asking you to buy protein powder or is spending more time at the gym than with his friends.
“Pay attention if he is withdrawing from friends and family because of his concerns about his appearance,” Dr. Nagata says. “For example, we often hear that a teenager will no longer eat family meals or at a restaurant because the protein content isn’t high enough or the food is too fatty.”
If you’re concerned, always make sure to discuss this with your son’s pediatrician.
“Ultimately, you want to make sure you share your concerns before your teen son becomes even more body-image obsessed,” Dr. Nagata says.
A version of this article first appeared on WebMD.com.
What is the psychological impact of type 1 diabetes?
“Living with diabetes is not smooth sailing…From the onset of the disease in a child or adolescent through all the days that follow, there is nothing ordinary about it,” according to Aide aux Jeunes Diabétiques (AJD), a French association providing support for children and adolescents with diabetes. What is the psychological impact of the disease on patients and their loved ones? When we look at the life of a person with diabetes, are there key stages that call for more focused attention?
Nadine Hoffmeister, a psychologist at AJD, offers support to patients with diabetes and their parents as they navigate and deal with in-patient treatment for the disease. She recently spoke with this news organization.
Q: Are psychological issues more prevalent in patients with type 1 diabetes (T1D) than in the general population?
Dr. Hoffmeister: Having a chronic disease is not something that should be viewed as automatically making the person more susceptible to psychological issues. When we think about kids with T1D, it’s important to keep in mind that the risk for depression and the risk for eating disorders are, in general, higher in adolescence.
Of course, Clearly, the risk for eating disorders is there, given the constant focus on managing one’s diet. And there’s a greater risk for depression, because life with diabetes can really be trying. That said, how much impact the disease has depends in large part on the environment, the monitoring, and the collaboration of everyone involved.
Q: Are there key stages in the life of patients with T1D that call for targeted psychological support?
Dr. Hoffmeister: The thing about T1D is that it can affect anyone at any age – a small child, a teenager, a young adult. So, in that sense, all ‘firsts’ are key stages. They start, of course, with the first ‘first’: diagnosis. For children diagnosed at an early age, there’s the first day of nursery school or kindergarten, the first piece of birthday cake. Then we get to kids starting middle school and high school, places where they’re now left to their own devices. This is when, for the first time, they’ll have an opportunity to take a trip without their parents and siblings, to go to a party.
And then, there’s the first time using a particular treatment. For example, switching from injections to a pump requires not only an adjustment in terms of physically operating a new device, but a reorientation in terms of mentally settling into a new routine, a new way of administering medication, and so on. They have to learn how to get along with this machine that’s attached to them all the time. They have to view it as being a part of them, view it as a partner, a teammate, a friend. It’s not that easy.
Later on, one of the major stages is, of course, adolescence. Critical developments in the separation–individuation process are taking place. They start to feel the need to break free, to become autonomous, as they seek to fully come to terms with their disease.
Parents usually worry about this stage, adolescence. They’re scared that their child won’t be as vigilant, that they’ll be scatterbrained or careless when it comes to staying on top of all those things that need to be done to keep T1D under control. Most of the time, this stage goes better than they thought. Still, the fact remains that it’s difficult to find a happy medium between adolescence and diabetes. Indeed, there’s a bit of a paradox here. On the one hand, we have adolescence which, by definition, is a time of spontaneity, independence, of trying new things. On the other hand, we have diabetes and its limits and constraints, its care and treatment, day in and day out. We have to pay close attention to how the child navigates and makes their way through this stage of their life.
During adolescence, there’s also a heightened awareness and concern about how others look at you, see you – everywhere, not only in classrooms and hallways. If the way someone looks at them seems aggressive or intrusive, the child may start to feel scared. The risk then becomes that they’ll start feeling awkward or ashamed or embarrassed. We have to keep this in mind and help lead the child away from those feelings. Otherwise, they can end up with low self-esteem, they can start to withdraw.
It can sometimes get to the point where they choose to neglect their treatment so as to conform to the way others see them. Adults can easily lose sight of these kinds of things. So, it’s imperative that we talk to the child. If they’re having trouble following their treatment plan, maybe there’s something going on at school. So, let’s ask them: “How do you like your classes and teachers?” “How are you doing with your injections? Are you finding that they’re getting easier and easier to do?” And always keeping in mind the real possibility that the child may be feeling awkward, ashamed, embarrassed.
Q: Is enough being done to pick up on and address these children’s needs?
Dr. Hoffmeister: I think that these efforts are becoming more and more widespread. Still, there are disparities. When it comes to patients with chronic diseases, it’s not always easy to implement mental health care into the treatment plan. In some cases, there might not be a hospital nearby. And as we know, there are no spots available in medical and psychiatric centers. Of course, outside of hospital settings, we’re seeing the unfortunate situation of fewer and fewer middle schools and high schools having nurses on site.
And then, what options there are for getting support vary greatly from hospital to hospital. Some don’t have psychologists. Others have full schedules and not enough staff. That said, more and more teams are trying to set up regular appointments right from the time of diagnosis. This is a really good approach to take, even though the circumstances may not be ideal. After all, the person has just been told that they have diabetes; they’re not really in the best state of mind to have any kind of discussion.
Q: And so, it makes sense that AJD would offer the kind of mental health support that you’re now providing there.
Dr. Hoffmeister: Exactly. My position was created 4 years ago. I’m not at the hospital. I’m an external. The goal is to be able to offer this psychological support to everyone. I do consultations over the phone so that no matter where a person is in France, they’ll have access to this support. There’s great demand, and the requests are only increasing. I think this has to do with the fact that people are being diagnosed younger and younger. It’s a very complicated situation for the parents. No matter how young their child is, they want to get that support underway as soon as possible.
Q: You speak about the patients getting support. But doesn’t some kind of help have to be given to their parents and loved ones as well?
Dr. Hoffmeister: Yes. I’d say that 60% to 70% of the work I do at AJD is for parents. I also have some older adolescents and some younger kids whom I call to keep up with. But children aren’t very interested in discussing plans over the phone. For parents, the thing about diabetes is that they find themselves in these situations where their child is in the hospital for, say, a week, then is discharged, and all of a sudden, they find themselves at home as the ones in charge of their child’s treatment.
When it’s a little kid, the parents are the ones who are taking care of all the steps, the injections, the pumps. They’re dealing with the distress of a child going through episodes of nocturnal hypoglycemia. They’re experiencing varying degrees of anxiety in carrying out all of these responsibilities and, at the same time, the bond they have with their child is becoming stronger and stronger. So, there’s that anxiety. In this situation, parents may also feel a need for control. And they’re also feeling exhausted; the mental load of dealing with diabetes is very, very intense. To work through all this, many parents reach out for psychological support.
Then later on, when the child has gotten a little older, the parents find it difficult to get to the point of being able to just let go. But once the parents get to know their child better, get to know how their child experiences diabetes, they’ll get to that point. What they come to learn is that the child can take care of things, the child can feel what’s going on in their body, the child can be trusted.
Q: How can we help and support children with diabetes?
Dr. Hoffmeister: One of the most important things is to teach the child to come to terms with the disease and how it affects their body. In other words, the idea here is to adapt diabetes to one’s life, not the other way around. The goal is to not let diabetes take over.
When faced with standardized medical protocols, during a session with a psychologist, the child can talk about their life, give an idea of what a day in their life looks like. For example, the school cafeteria is a place where children get the opportunity to socialize and interact with their peers. We want to have that lunch period be as normal as possible for the child with diabetes. In some schools, lunchtime becomes a challenge. So, not seeing any other solution, mom stops working so the child can come home to eat. These are the kinds of situations where efforts to make the child feel included have failed. They’re tough to deal with, all around. And so this is why we do all we can to keep things as normal as possible for these children.
Q: What would you say is the one initiative out there that’s giving young patients with T1D the most help and support?
Dr. Hoffmeister: AJD offers stays at Care Management and Rehabilitation (SSR) sites. For kids and teenagers with diabetes, these places are like summer camps where every aspect of treatment is taken care of.
There’s a medical team monitoring their disease and a team of counselors always on hand. It’s a time when children may very well bring up things that are on their mind. All in all, the children have a safe and welcoming environment where treatment is provided and they can feel free to open up and talk.
If a problem crops up, I’m always on call to jump online. And throughout the stay, the medical team is keeping in touch to discuss the child’s care.
AJD is also an interdisciplinary association. We regularly organize practice exchange groups that bring together health care professionals and families from all over France. In this way, we’re able to collaborate and come up with resources, such as information packets and kits – for the newly diagnosed, for those starting intensive insulin therapy, and so on. These resources take into account medical protocols related to diabetes. They’re also designed with family life in mind. And having this set of resources works toward standardizing treatments.
A version of this article first appeared on Medscape.com.
“Living with diabetes is not smooth sailing…From the onset of the disease in a child or adolescent through all the days that follow, there is nothing ordinary about it,” according to Aide aux Jeunes Diabétiques (AJD), a French association providing support for children and adolescents with diabetes. What is the psychological impact of the disease on patients and their loved ones? When we look at the life of a person with diabetes, are there key stages that call for more focused attention?
Nadine Hoffmeister, a psychologist at AJD, offers support to patients with diabetes and their parents as they navigate and deal with in-patient treatment for the disease. She recently spoke with this news organization.
Q: Are psychological issues more prevalent in patients with type 1 diabetes (T1D) than in the general population?
Dr. Hoffmeister: Having a chronic disease is not something that should be viewed as automatically making the person more susceptible to psychological issues. When we think about kids with T1D, it’s important to keep in mind that the risk for depression and the risk for eating disorders are, in general, higher in adolescence.
Of course, Clearly, the risk for eating disorders is there, given the constant focus on managing one’s diet. And there’s a greater risk for depression, because life with diabetes can really be trying. That said, how much impact the disease has depends in large part on the environment, the monitoring, and the collaboration of everyone involved.
Q: Are there key stages in the life of patients with T1D that call for targeted psychological support?
Dr. Hoffmeister: The thing about T1D is that it can affect anyone at any age – a small child, a teenager, a young adult. So, in that sense, all ‘firsts’ are key stages. They start, of course, with the first ‘first’: diagnosis. For children diagnosed at an early age, there’s the first day of nursery school or kindergarten, the first piece of birthday cake. Then we get to kids starting middle school and high school, places where they’re now left to their own devices. This is when, for the first time, they’ll have an opportunity to take a trip without their parents and siblings, to go to a party.
And then, there’s the first time using a particular treatment. For example, switching from injections to a pump requires not only an adjustment in terms of physically operating a new device, but a reorientation in terms of mentally settling into a new routine, a new way of administering medication, and so on. They have to learn how to get along with this machine that’s attached to them all the time. They have to view it as being a part of them, view it as a partner, a teammate, a friend. It’s not that easy.
Later on, one of the major stages is, of course, adolescence. Critical developments in the separation–individuation process are taking place. They start to feel the need to break free, to become autonomous, as they seek to fully come to terms with their disease.
Parents usually worry about this stage, adolescence. They’re scared that their child won’t be as vigilant, that they’ll be scatterbrained or careless when it comes to staying on top of all those things that need to be done to keep T1D under control. Most of the time, this stage goes better than they thought. Still, the fact remains that it’s difficult to find a happy medium between adolescence and diabetes. Indeed, there’s a bit of a paradox here. On the one hand, we have adolescence which, by definition, is a time of spontaneity, independence, of trying new things. On the other hand, we have diabetes and its limits and constraints, its care and treatment, day in and day out. We have to pay close attention to how the child navigates and makes their way through this stage of their life.
During adolescence, there’s also a heightened awareness and concern about how others look at you, see you – everywhere, not only in classrooms and hallways. If the way someone looks at them seems aggressive or intrusive, the child may start to feel scared. The risk then becomes that they’ll start feeling awkward or ashamed or embarrassed. We have to keep this in mind and help lead the child away from those feelings. Otherwise, they can end up with low self-esteem, they can start to withdraw.
It can sometimes get to the point where they choose to neglect their treatment so as to conform to the way others see them. Adults can easily lose sight of these kinds of things. So, it’s imperative that we talk to the child. If they’re having trouble following their treatment plan, maybe there’s something going on at school. So, let’s ask them: “How do you like your classes and teachers?” “How are you doing with your injections? Are you finding that they’re getting easier and easier to do?” And always keeping in mind the real possibility that the child may be feeling awkward, ashamed, embarrassed.
Q: Is enough being done to pick up on and address these children’s needs?
Dr. Hoffmeister: I think that these efforts are becoming more and more widespread. Still, there are disparities. When it comes to patients with chronic diseases, it’s not always easy to implement mental health care into the treatment plan. In some cases, there might not be a hospital nearby. And as we know, there are no spots available in medical and psychiatric centers. Of course, outside of hospital settings, we’re seeing the unfortunate situation of fewer and fewer middle schools and high schools having nurses on site.
And then, what options there are for getting support vary greatly from hospital to hospital. Some don’t have psychologists. Others have full schedules and not enough staff. That said, more and more teams are trying to set up regular appointments right from the time of diagnosis. This is a really good approach to take, even though the circumstances may not be ideal. After all, the person has just been told that they have diabetes; they’re not really in the best state of mind to have any kind of discussion.
Q: And so, it makes sense that AJD would offer the kind of mental health support that you’re now providing there.
Dr. Hoffmeister: Exactly. My position was created 4 years ago. I’m not at the hospital. I’m an external. The goal is to be able to offer this psychological support to everyone. I do consultations over the phone so that no matter where a person is in France, they’ll have access to this support. There’s great demand, and the requests are only increasing. I think this has to do with the fact that people are being diagnosed younger and younger. It’s a very complicated situation for the parents. No matter how young their child is, they want to get that support underway as soon as possible.
Q: You speak about the patients getting support. But doesn’t some kind of help have to be given to their parents and loved ones as well?
Dr. Hoffmeister: Yes. I’d say that 60% to 70% of the work I do at AJD is for parents. I also have some older adolescents and some younger kids whom I call to keep up with. But children aren’t very interested in discussing plans over the phone. For parents, the thing about diabetes is that they find themselves in these situations where their child is in the hospital for, say, a week, then is discharged, and all of a sudden, they find themselves at home as the ones in charge of their child’s treatment.
When it’s a little kid, the parents are the ones who are taking care of all the steps, the injections, the pumps. They’re dealing with the distress of a child going through episodes of nocturnal hypoglycemia. They’re experiencing varying degrees of anxiety in carrying out all of these responsibilities and, at the same time, the bond they have with their child is becoming stronger and stronger. So, there’s that anxiety. In this situation, parents may also feel a need for control. And they’re also feeling exhausted; the mental load of dealing with diabetes is very, very intense. To work through all this, many parents reach out for psychological support.
Then later on, when the child has gotten a little older, the parents find it difficult to get to the point of being able to just let go. But once the parents get to know their child better, get to know how their child experiences diabetes, they’ll get to that point. What they come to learn is that the child can take care of things, the child can feel what’s going on in their body, the child can be trusted.
Q: How can we help and support children with diabetes?
Dr. Hoffmeister: One of the most important things is to teach the child to come to terms with the disease and how it affects their body. In other words, the idea here is to adapt diabetes to one’s life, not the other way around. The goal is to not let diabetes take over.
When faced with standardized medical protocols, during a session with a psychologist, the child can talk about their life, give an idea of what a day in their life looks like. For example, the school cafeteria is a place where children get the opportunity to socialize and interact with their peers. We want to have that lunch period be as normal as possible for the child with diabetes. In some schools, lunchtime becomes a challenge. So, not seeing any other solution, mom stops working so the child can come home to eat. These are the kinds of situations where efforts to make the child feel included have failed. They’re tough to deal with, all around. And so this is why we do all we can to keep things as normal as possible for these children.
Q: What would you say is the one initiative out there that’s giving young patients with T1D the most help and support?
Dr. Hoffmeister: AJD offers stays at Care Management and Rehabilitation (SSR) sites. For kids and teenagers with diabetes, these places are like summer camps where every aspect of treatment is taken care of.
There’s a medical team monitoring their disease and a team of counselors always on hand. It’s a time when children may very well bring up things that are on their mind. All in all, the children have a safe and welcoming environment where treatment is provided and they can feel free to open up and talk.
If a problem crops up, I’m always on call to jump online. And throughout the stay, the medical team is keeping in touch to discuss the child’s care.
AJD is also an interdisciplinary association. We regularly organize practice exchange groups that bring together health care professionals and families from all over France. In this way, we’re able to collaborate and come up with resources, such as information packets and kits – for the newly diagnosed, for those starting intensive insulin therapy, and so on. These resources take into account medical protocols related to diabetes. They’re also designed with family life in mind. And having this set of resources works toward standardizing treatments.
A version of this article first appeared on Medscape.com.
“Living with diabetes is not smooth sailing…From the onset of the disease in a child or adolescent through all the days that follow, there is nothing ordinary about it,” according to Aide aux Jeunes Diabétiques (AJD), a French association providing support for children and adolescents with diabetes. What is the psychological impact of the disease on patients and their loved ones? When we look at the life of a person with diabetes, are there key stages that call for more focused attention?
Nadine Hoffmeister, a psychologist at AJD, offers support to patients with diabetes and their parents as they navigate and deal with in-patient treatment for the disease. She recently spoke with this news organization.
Q: Are psychological issues more prevalent in patients with type 1 diabetes (T1D) than in the general population?
Dr. Hoffmeister: Having a chronic disease is not something that should be viewed as automatically making the person more susceptible to psychological issues. When we think about kids with T1D, it’s important to keep in mind that the risk for depression and the risk for eating disorders are, in general, higher in adolescence.
Of course, Clearly, the risk for eating disorders is there, given the constant focus on managing one’s diet. And there’s a greater risk for depression, because life with diabetes can really be trying. That said, how much impact the disease has depends in large part on the environment, the monitoring, and the collaboration of everyone involved.
Q: Are there key stages in the life of patients with T1D that call for targeted psychological support?
Dr. Hoffmeister: The thing about T1D is that it can affect anyone at any age – a small child, a teenager, a young adult. So, in that sense, all ‘firsts’ are key stages. They start, of course, with the first ‘first’: diagnosis. For children diagnosed at an early age, there’s the first day of nursery school or kindergarten, the first piece of birthday cake. Then we get to kids starting middle school and high school, places where they’re now left to their own devices. This is when, for the first time, they’ll have an opportunity to take a trip without their parents and siblings, to go to a party.
And then, there’s the first time using a particular treatment. For example, switching from injections to a pump requires not only an adjustment in terms of physically operating a new device, but a reorientation in terms of mentally settling into a new routine, a new way of administering medication, and so on. They have to learn how to get along with this machine that’s attached to them all the time. They have to view it as being a part of them, view it as a partner, a teammate, a friend. It’s not that easy.
Later on, one of the major stages is, of course, adolescence. Critical developments in the separation–individuation process are taking place. They start to feel the need to break free, to become autonomous, as they seek to fully come to terms with their disease.
Parents usually worry about this stage, adolescence. They’re scared that their child won’t be as vigilant, that they’ll be scatterbrained or careless when it comes to staying on top of all those things that need to be done to keep T1D under control. Most of the time, this stage goes better than they thought. Still, the fact remains that it’s difficult to find a happy medium between adolescence and diabetes. Indeed, there’s a bit of a paradox here. On the one hand, we have adolescence which, by definition, is a time of spontaneity, independence, of trying new things. On the other hand, we have diabetes and its limits and constraints, its care and treatment, day in and day out. We have to pay close attention to how the child navigates and makes their way through this stage of their life.
During adolescence, there’s also a heightened awareness and concern about how others look at you, see you – everywhere, not only in classrooms and hallways. If the way someone looks at them seems aggressive or intrusive, the child may start to feel scared. The risk then becomes that they’ll start feeling awkward or ashamed or embarrassed. We have to keep this in mind and help lead the child away from those feelings. Otherwise, they can end up with low self-esteem, they can start to withdraw.
It can sometimes get to the point where they choose to neglect their treatment so as to conform to the way others see them. Adults can easily lose sight of these kinds of things. So, it’s imperative that we talk to the child. If they’re having trouble following their treatment plan, maybe there’s something going on at school. So, let’s ask them: “How do you like your classes and teachers?” “How are you doing with your injections? Are you finding that they’re getting easier and easier to do?” And always keeping in mind the real possibility that the child may be feeling awkward, ashamed, embarrassed.
Q: Is enough being done to pick up on and address these children’s needs?
Dr. Hoffmeister: I think that these efforts are becoming more and more widespread. Still, there are disparities. When it comes to patients with chronic diseases, it’s not always easy to implement mental health care into the treatment plan. In some cases, there might not be a hospital nearby. And as we know, there are no spots available in medical and psychiatric centers. Of course, outside of hospital settings, we’re seeing the unfortunate situation of fewer and fewer middle schools and high schools having nurses on site.
And then, what options there are for getting support vary greatly from hospital to hospital. Some don’t have psychologists. Others have full schedules and not enough staff. That said, more and more teams are trying to set up regular appointments right from the time of diagnosis. This is a really good approach to take, even though the circumstances may not be ideal. After all, the person has just been told that they have diabetes; they’re not really in the best state of mind to have any kind of discussion.
Q: And so, it makes sense that AJD would offer the kind of mental health support that you’re now providing there.
Dr. Hoffmeister: Exactly. My position was created 4 years ago. I’m not at the hospital. I’m an external. The goal is to be able to offer this psychological support to everyone. I do consultations over the phone so that no matter where a person is in France, they’ll have access to this support. There’s great demand, and the requests are only increasing. I think this has to do with the fact that people are being diagnosed younger and younger. It’s a very complicated situation for the parents. No matter how young their child is, they want to get that support underway as soon as possible.
Q: You speak about the patients getting support. But doesn’t some kind of help have to be given to their parents and loved ones as well?
Dr. Hoffmeister: Yes. I’d say that 60% to 70% of the work I do at AJD is for parents. I also have some older adolescents and some younger kids whom I call to keep up with. But children aren’t very interested in discussing plans over the phone. For parents, the thing about diabetes is that they find themselves in these situations where their child is in the hospital for, say, a week, then is discharged, and all of a sudden, they find themselves at home as the ones in charge of their child’s treatment.
When it’s a little kid, the parents are the ones who are taking care of all the steps, the injections, the pumps. They’re dealing with the distress of a child going through episodes of nocturnal hypoglycemia. They’re experiencing varying degrees of anxiety in carrying out all of these responsibilities and, at the same time, the bond they have with their child is becoming stronger and stronger. So, there’s that anxiety. In this situation, parents may also feel a need for control. And they’re also feeling exhausted; the mental load of dealing with diabetes is very, very intense. To work through all this, many parents reach out for psychological support.
Then later on, when the child has gotten a little older, the parents find it difficult to get to the point of being able to just let go. But once the parents get to know their child better, get to know how their child experiences diabetes, they’ll get to that point. What they come to learn is that the child can take care of things, the child can feel what’s going on in their body, the child can be trusted.
Q: How can we help and support children with diabetes?
Dr. Hoffmeister: One of the most important things is to teach the child to come to terms with the disease and how it affects their body. In other words, the idea here is to adapt diabetes to one’s life, not the other way around. The goal is to not let diabetes take over.
When faced with standardized medical protocols, during a session with a psychologist, the child can talk about their life, give an idea of what a day in their life looks like. For example, the school cafeteria is a place where children get the opportunity to socialize and interact with their peers. We want to have that lunch period be as normal as possible for the child with diabetes. In some schools, lunchtime becomes a challenge. So, not seeing any other solution, mom stops working so the child can come home to eat. These are the kinds of situations where efforts to make the child feel included have failed. They’re tough to deal with, all around. And so this is why we do all we can to keep things as normal as possible for these children.
Q: What would you say is the one initiative out there that’s giving young patients with T1D the most help and support?
Dr. Hoffmeister: AJD offers stays at Care Management and Rehabilitation (SSR) sites. For kids and teenagers with diabetes, these places are like summer camps where every aspect of treatment is taken care of.
There’s a medical team monitoring their disease and a team of counselors always on hand. It’s a time when children may very well bring up things that are on their mind. All in all, the children have a safe and welcoming environment where treatment is provided and they can feel free to open up and talk.
If a problem crops up, I’m always on call to jump online. And throughout the stay, the medical team is keeping in touch to discuss the child’s care.
AJD is also an interdisciplinary association. We regularly organize practice exchange groups that bring together health care professionals and families from all over France. In this way, we’re able to collaborate and come up with resources, such as information packets and kits – for the newly diagnosed, for those starting intensive insulin therapy, and so on. These resources take into account medical protocols related to diabetes. They’re also designed with family life in mind. And having this set of resources works toward standardizing treatments.
A version of this article first appeared on Medscape.com.
Innovative ‘chatbot’ reduces eating disorder risk
Results of a randomized trial show that at-risk women who interacted with the chatbot showed lower concern about their weight and body shape compared to a wait-list control group.
“Chatbots are widely used in industry and have begun to be used in medical settings, although few studies have examined their effectiveness for mental health issues and none address EDs or ED prevention,” senior investigator C. Barr Taylor, MD, a research faculty member at Palo Alto (Calif.) University, said in a press release.
“We found that the group with access to the chatbot had a greater reduction in weight and shape concerns, both right after using it at 3 months and at the 6-month follow-up. The effects had sustainability over time, and we also found indication that the chatbot may reduce ED onset more so than the control group, where there was a greater incidence of EDs,” Dr. Taylor told this news organization.
The study was published online Dec. 28, 2021, in the International Journal of Eating Disorders.
Deadly disorders
“EDs are a common problem with huge risk factors; and, given how widespread they are, we need scalable tools that can reach a lot of people at low cost, reduce risk factors for developing an ED – which is the second most deadly of all psychiatric illnesses – so prevention is of the utmost importance,” Dr. Taylor said.
The investigators developed a targeted Internet-based preventive program called StudentBodies that utilizes cognitive-behavioral therapy approaches. The program was successful in reducing weight/shape concerns in women at high risk for the onset of an ED, and it reduced ED onset in the highest-risk women.
However, it required trained moderators who spent over 45 minutes with participants. Given the large number of people at risk for an ED who might benefit, the researchers noted that it is unlikely that a human-moderated version would be widely disseminated.
A chatbot may represent a “possible solution to reducing delivery costs” because it mimics aspects of human moderation in simulating conversations, the investigators noted.
“We wanted to take the earlier program we developed into this century and program it for delivery in this new format that would allow for bite-size pieces of information for the chatbot to communicate to the user,” lead author Ellen Fitzsimmons-Craft, PhD, assistant professor of psychiatry, Washington University, St. Louis, told this news organization.
“Our ED prevention online version was more effective when there was guidance from a human moderator who could provide feedback on progress, encourage you to go on, and apply the skills in daily life. But that’s not the most scalable. So we thought that a chatbot, in addition to providing content in this perhaps more engaging format, could also provide some aspect of human moderation, although the person is chatting with a robot,” added Dr. Fitzsimmons-Craft, associate director of the Center for Healthy Weight and Wellness.
Tessa will speak to you now
Participants (n = 700 women; mean [SD] age, 21.08 [3.09] years; 84.6% White; 53.8% heterosexual; 31.08% bisexual), were randomized to an intervention group or a wait-list control group (n = 352 and 348, respectively). There were no significant differences between groups in age, race, ethnicity, education, or sexual orientation.
The StudentBodies program was adapted for delivery via a chatbot named Tessa “while retaining the core intervention principles” and referred to as “Body Positive.”
It consisted of several components programmed into the chatbot, which initiated each conversation in a predetermined order. Participants were encouraged to engage in two conversations weekly. The program included an introduction and eight sessions as well as a crisis module that provided users with a referral to a crisis hotline in case of emergency. Referral was triggered on the basis of “recognized keywords,” such as “hurting myself.”
The researchers used the Weight Concerns Scale questionnaire to assess weight and shape concerns and the Internalization: Thin/Low Body Fat subscale of the Sociocultural Attitudes Toward Appearance Questionnaire–4 to “assess the cognitive aspect of thin-ideal internalization.”
Secondary outcomes tested the hypothesis that the chatbot would be more likely to reduce clinical outcomes (ED psychopathology, depression, and anxiety) and prevent ED onset, compared to the control condition.
Ready for prime time
At 3- and 6-month follow-up, there was significantly greater reduction in the intervention group compared with the control group in weight/shape concerns (d = -.20, P = .03 and d = -.19, P = .04, respectively), although there were no differences in thin-ideal internalization change.
The chatbot intervention was associated with significantly greater reductions in overall ED psychopathology at 3 months (d = -.29, P = .003) compared to the control condition, but not at 6 months.
Notably, the intervention group had significantly higher odds than the control group of remaining nonclinical for EDs at 3- and 6-month follow-up (OR, 2.37 [95% confidence interval, 1.37-4.11] and OR, 2.13 [95% CI,1.26-3.59], respectively).
“We were very excited about the study, and frankly, I was surprised by the effectiveness [of the chatbot intervention] because I didn’t think it would have as much of an impact as it did,” said Dr. Taylor. “Prevention gets short shrift everywhere, and I think we succeeded very well.”
Dr. Fitzsimmons-Craft added that the National Eating Disorders Association (NEDA) has agreed to make the chatbot available on its website for people who screen positive for having an ED or for being at high risk, and so their group is working with their industry partner, a company called X2AI, which developed the chatbot, to make this happen.
“This is definitely the fastest research-to-practice translation I’ve ever seen, where we can so quickly show that it works and make it available to tens of thousands almost immediately.”
Dr. Fitzsimmons-Craft is optimistic that it will be available to launch the week of Feb. 21, which is National Eating Disorders Week.
Innovative, creative research
Commenting on the research, Evelyn Attia, MD, professor of psychiatry, Columbia University Medical Center, and director of the Columbia Center for Eating Disorders New York–Presbyterian Hospital, New York, described the study as “innovative and creative.”
Dr. Attia, a member of the Research Advisory Council of the NEDA, noted that the structure of the study is “very preliminary” and that the comparison to a wait-list control makes it hard to know whether this is an effective intervention compared with other types of interventions, rather than compared with no intervention.
“But I’m sure that when the researchers are set up and primed to study this more robustly, they will consider a more active control intervention to see whether this preliminary finding holds up,” she said.
Also commenting on the study, Deborah R. Glasofer, PhD, associate professor of clinical medical psychology (in psychiatry), Columbia Center for Eating Disorders, said, “Higher-than-average concern about appearance – body shape, size, or weight – and a tightly held belief that it is ideal to be thin are known risk factors for the development of an eating disorder.
“This study offers an indication that technology can be leveraged to fill a gap and help folks before unhelpful and sometimes misguided thoughts about food, eating, and appearance evolve into a full-blown eating disorder,” said Dr. Glasofer, who was not involved with the study.
The study was supported by the NEDA Feeding Hope Fund, the National Institute of Mental Health, the National Heart, Lung, and Blood Institute, and the Swedish Research Council. The authors and Dr. Glasofer have disclosed no relevant financial relationships. Dr. Attia is on the board and the Research Advisory Council of NEDA.
A version of this article first appeared on Medscape.com.
Results of a randomized trial show that at-risk women who interacted with the chatbot showed lower concern about their weight and body shape compared to a wait-list control group.
“Chatbots are widely used in industry and have begun to be used in medical settings, although few studies have examined their effectiveness for mental health issues and none address EDs or ED prevention,” senior investigator C. Barr Taylor, MD, a research faculty member at Palo Alto (Calif.) University, said in a press release.
“We found that the group with access to the chatbot had a greater reduction in weight and shape concerns, both right after using it at 3 months and at the 6-month follow-up. The effects had sustainability over time, and we also found indication that the chatbot may reduce ED onset more so than the control group, where there was a greater incidence of EDs,” Dr. Taylor told this news organization.
The study was published online Dec. 28, 2021, in the International Journal of Eating Disorders.
Deadly disorders
“EDs are a common problem with huge risk factors; and, given how widespread they are, we need scalable tools that can reach a lot of people at low cost, reduce risk factors for developing an ED – which is the second most deadly of all psychiatric illnesses – so prevention is of the utmost importance,” Dr. Taylor said.
The investigators developed a targeted Internet-based preventive program called StudentBodies that utilizes cognitive-behavioral therapy approaches. The program was successful in reducing weight/shape concerns in women at high risk for the onset of an ED, and it reduced ED onset in the highest-risk women.
However, it required trained moderators who spent over 45 minutes with participants. Given the large number of people at risk for an ED who might benefit, the researchers noted that it is unlikely that a human-moderated version would be widely disseminated.
A chatbot may represent a “possible solution to reducing delivery costs” because it mimics aspects of human moderation in simulating conversations, the investigators noted.
“We wanted to take the earlier program we developed into this century and program it for delivery in this new format that would allow for bite-size pieces of information for the chatbot to communicate to the user,” lead author Ellen Fitzsimmons-Craft, PhD, assistant professor of psychiatry, Washington University, St. Louis, told this news organization.
“Our ED prevention online version was more effective when there was guidance from a human moderator who could provide feedback on progress, encourage you to go on, and apply the skills in daily life. But that’s not the most scalable. So we thought that a chatbot, in addition to providing content in this perhaps more engaging format, could also provide some aspect of human moderation, although the person is chatting with a robot,” added Dr. Fitzsimmons-Craft, associate director of the Center for Healthy Weight and Wellness.
Tessa will speak to you now
Participants (n = 700 women; mean [SD] age, 21.08 [3.09] years; 84.6% White; 53.8% heterosexual; 31.08% bisexual), were randomized to an intervention group or a wait-list control group (n = 352 and 348, respectively). There were no significant differences between groups in age, race, ethnicity, education, or sexual orientation.
The StudentBodies program was adapted for delivery via a chatbot named Tessa “while retaining the core intervention principles” and referred to as “Body Positive.”
It consisted of several components programmed into the chatbot, which initiated each conversation in a predetermined order. Participants were encouraged to engage in two conversations weekly. The program included an introduction and eight sessions as well as a crisis module that provided users with a referral to a crisis hotline in case of emergency. Referral was triggered on the basis of “recognized keywords,” such as “hurting myself.”
The researchers used the Weight Concerns Scale questionnaire to assess weight and shape concerns and the Internalization: Thin/Low Body Fat subscale of the Sociocultural Attitudes Toward Appearance Questionnaire–4 to “assess the cognitive aspect of thin-ideal internalization.”
Secondary outcomes tested the hypothesis that the chatbot would be more likely to reduce clinical outcomes (ED psychopathology, depression, and anxiety) and prevent ED onset, compared to the control condition.
Ready for prime time
At 3- and 6-month follow-up, there was significantly greater reduction in the intervention group compared with the control group in weight/shape concerns (d = -.20, P = .03 and d = -.19, P = .04, respectively), although there were no differences in thin-ideal internalization change.
The chatbot intervention was associated with significantly greater reductions in overall ED psychopathology at 3 months (d = -.29, P = .003) compared to the control condition, but not at 6 months.
Notably, the intervention group had significantly higher odds than the control group of remaining nonclinical for EDs at 3- and 6-month follow-up (OR, 2.37 [95% confidence interval, 1.37-4.11] and OR, 2.13 [95% CI,1.26-3.59], respectively).
“We were very excited about the study, and frankly, I was surprised by the effectiveness [of the chatbot intervention] because I didn’t think it would have as much of an impact as it did,” said Dr. Taylor. “Prevention gets short shrift everywhere, and I think we succeeded very well.”
Dr. Fitzsimmons-Craft added that the National Eating Disorders Association (NEDA) has agreed to make the chatbot available on its website for people who screen positive for having an ED or for being at high risk, and so their group is working with their industry partner, a company called X2AI, which developed the chatbot, to make this happen.
“This is definitely the fastest research-to-practice translation I’ve ever seen, where we can so quickly show that it works and make it available to tens of thousands almost immediately.”
Dr. Fitzsimmons-Craft is optimistic that it will be available to launch the week of Feb. 21, which is National Eating Disorders Week.
Innovative, creative research
Commenting on the research, Evelyn Attia, MD, professor of psychiatry, Columbia University Medical Center, and director of the Columbia Center for Eating Disorders New York–Presbyterian Hospital, New York, described the study as “innovative and creative.”
Dr. Attia, a member of the Research Advisory Council of the NEDA, noted that the structure of the study is “very preliminary” and that the comparison to a wait-list control makes it hard to know whether this is an effective intervention compared with other types of interventions, rather than compared with no intervention.
“But I’m sure that when the researchers are set up and primed to study this more robustly, they will consider a more active control intervention to see whether this preliminary finding holds up,” she said.
Also commenting on the study, Deborah R. Glasofer, PhD, associate professor of clinical medical psychology (in psychiatry), Columbia Center for Eating Disorders, said, “Higher-than-average concern about appearance – body shape, size, or weight – and a tightly held belief that it is ideal to be thin are known risk factors for the development of an eating disorder.
“This study offers an indication that technology can be leveraged to fill a gap and help folks before unhelpful and sometimes misguided thoughts about food, eating, and appearance evolve into a full-blown eating disorder,” said Dr. Glasofer, who was not involved with the study.
The study was supported by the NEDA Feeding Hope Fund, the National Institute of Mental Health, the National Heart, Lung, and Blood Institute, and the Swedish Research Council. The authors and Dr. Glasofer have disclosed no relevant financial relationships. Dr. Attia is on the board and the Research Advisory Council of NEDA.
A version of this article first appeared on Medscape.com.
Results of a randomized trial show that at-risk women who interacted with the chatbot showed lower concern about their weight and body shape compared to a wait-list control group.
“Chatbots are widely used in industry and have begun to be used in medical settings, although few studies have examined their effectiveness for mental health issues and none address EDs or ED prevention,” senior investigator C. Barr Taylor, MD, a research faculty member at Palo Alto (Calif.) University, said in a press release.
“We found that the group with access to the chatbot had a greater reduction in weight and shape concerns, both right after using it at 3 months and at the 6-month follow-up. The effects had sustainability over time, and we also found indication that the chatbot may reduce ED onset more so than the control group, where there was a greater incidence of EDs,” Dr. Taylor told this news organization.
The study was published online Dec. 28, 2021, in the International Journal of Eating Disorders.
Deadly disorders
“EDs are a common problem with huge risk factors; and, given how widespread they are, we need scalable tools that can reach a lot of people at low cost, reduce risk factors for developing an ED – which is the second most deadly of all psychiatric illnesses – so prevention is of the utmost importance,” Dr. Taylor said.
The investigators developed a targeted Internet-based preventive program called StudentBodies that utilizes cognitive-behavioral therapy approaches. The program was successful in reducing weight/shape concerns in women at high risk for the onset of an ED, and it reduced ED onset in the highest-risk women.
However, it required trained moderators who spent over 45 minutes with participants. Given the large number of people at risk for an ED who might benefit, the researchers noted that it is unlikely that a human-moderated version would be widely disseminated.
A chatbot may represent a “possible solution to reducing delivery costs” because it mimics aspects of human moderation in simulating conversations, the investigators noted.
“We wanted to take the earlier program we developed into this century and program it for delivery in this new format that would allow for bite-size pieces of information for the chatbot to communicate to the user,” lead author Ellen Fitzsimmons-Craft, PhD, assistant professor of psychiatry, Washington University, St. Louis, told this news organization.
“Our ED prevention online version was more effective when there was guidance from a human moderator who could provide feedback on progress, encourage you to go on, and apply the skills in daily life. But that’s not the most scalable. So we thought that a chatbot, in addition to providing content in this perhaps more engaging format, could also provide some aspect of human moderation, although the person is chatting with a robot,” added Dr. Fitzsimmons-Craft, associate director of the Center for Healthy Weight and Wellness.
Tessa will speak to you now
Participants (n = 700 women; mean [SD] age, 21.08 [3.09] years; 84.6% White; 53.8% heterosexual; 31.08% bisexual), were randomized to an intervention group or a wait-list control group (n = 352 and 348, respectively). There were no significant differences between groups in age, race, ethnicity, education, or sexual orientation.
The StudentBodies program was adapted for delivery via a chatbot named Tessa “while retaining the core intervention principles” and referred to as “Body Positive.”
It consisted of several components programmed into the chatbot, which initiated each conversation in a predetermined order. Participants were encouraged to engage in two conversations weekly. The program included an introduction and eight sessions as well as a crisis module that provided users with a referral to a crisis hotline in case of emergency. Referral was triggered on the basis of “recognized keywords,” such as “hurting myself.”
The researchers used the Weight Concerns Scale questionnaire to assess weight and shape concerns and the Internalization: Thin/Low Body Fat subscale of the Sociocultural Attitudes Toward Appearance Questionnaire–4 to “assess the cognitive aspect of thin-ideal internalization.”
Secondary outcomes tested the hypothesis that the chatbot would be more likely to reduce clinical outcomes (ED psychopathology, depression, and anxiety) and prevent ED onset, compared to the control condition.
Ready for prime time
At 3- and 6-month follow-up, there was significantly greater reduction in the intervention group compared with the control group in weight/shape concerns (d = -.20, P = .03 and d = -.19, P = .04, respectively), although there were no differences in thin-ideal internalization change.
The chatbot intervention was associated with significantly greater reductions in overall ED psychopathology at 3 months (d = -.29, P = .003) compared to the control condition, but not at 6 months.
Notably, the intervention group had significantly higher odds than the control group of remaining nonclinical for EDs at 3- and 6-month follow-up (OR, 2.37 [95% confidence interval, 1.37-4.11] and OR, 2.13 [95% CI,1.26-3.59], respectively).
“We were very excited about the study, and frankly, I was surprised by the effectiveness [of the chatbot intervention] because I didn’t think it would have as much of an impact as it did,” said Dr. Taylor. “Prevention gets short shrift everywhere, and I think we succeeded very well.”
Dr. Fitzsimmons-Craft added that the National Eating Disorders Association (NEDA) has agreed to make the chatbot available on its website for people who screen positive for having an ED or for being at high risk, and so their group is working with their industry partner, a company called X2AI, which developed the chatbot, to make this happen.
“This is definitely the fastest research-to-practice translation I’ve ever seen, where we can so quickly show that it works and make it available to tens of thousands almost immediately.”
Dr. Fitzsimmons-Craft is optimistic that it will be available to launch the week of Feb. 21, which is National Eating Disorders Week.
Innovative, creative research
Commenting on the research, Evelyn Attia, MD, professor of psychiatry, Columbia University Medical Center, and director of the Columbia Center for Eating Disorders New York–Presbyterian Hospital, New York, described the study as “innovative and creative.”
Dr. Attia, a member of the Research Advisory Council of the NEDA, noted that the structure of the study is “very preliminary” and that the comparison to a wait-list control makes it hard to know whether this is an effective intervention compared with other types of interventions, rather than compared with no intervention.
“But I’m sure that when the researchers are set up and primed to study this more robustly, they will consider a more active control intervention to see whether this preliminary finding holds up,” she said.
Also commenting on the study, Deborah R. Glasofer, PhD, associate professor of clinical medical psychology (in psychiatry), Columbia Center for Eating Disorders, said, “Higher-than-average concern about appearance – body shape, size, or weight – and a tightly held belief that it is ideal to be thin are known risk factors for the development of an eating disorder.
“This study offers an indication that technology can be leveraged to fill a gap and help folks before unhelpful and sometimes misguided thoughts about food, eating, and appearance evolve into a full-blown eating disorder,” said Dr. Glasofer, who was not involved with the study.
The study was supported by the NEDA Feeding Hope Fund, the National Institute of Mental Health, the National Heart, Lung, and Blood Institute, and the Swedish Research Council. The authors and Dr. Glasofer have disclosed no relevant financial relationships. Dr. Attia is on the board and the Research Advisory Council of NEDA.
A version of this article first appeared on Medscape.com.
ARFID or reasonable food restriction? The jury is out
Problems with eating and nutrition are common among patients with inflammatory bowel disease (IBD) and other gastrointestinal disorders, but clinicians who treat them should be careful not to automatically assume that patients have eating disorders, according to a psychologist who specializes in the psychological and social aspects of chronic digestive diseases.
On the other hand, clinicians must also be aware of the possibility that patients could have a recently identified syndrome cluster called avoidant restrictive food intake disorder (ARFID), said Tiffany Taft, PsyD, a research associate professor of medicine (gastroenterology and hepatology), medical social sciences, and psychiatry and behavioral sciences at Northwestern University, Chicago. In a recent study, she and her colleagues defined ARFID as “failure to meet one’s nutritional needs owing to sensory hypersensitivity, lack of interest in eating, or fear of aversive consequences from eating, and is associated with negative medical and psychosocial outcomes.”
ARFID “is a hot topic that we really don’t understand,” she said in an online presentation at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Nutritional deficiencies
Nutritional deficiencies are common among patients with IBD, “and nutritional deficiencies themselves can lead to symptoms or side effects that can cause people to eat less,” she said.
“As our vitamin B12 goes down, our cognitive functioning starts to decline, and we might not be making clear decisions in how we’re deciding what to eat, when to eat, if we should be eating at all – just something to think about in your patients who have nutritional deficiencies,” she told the audience.
Other common nutritional deficiencies that can affect eating and food choice among patients with IBD include low folate (B9) levels associated with sore tongue and weight loss, low iron levels leading to nausea and loss of appetite, and zinc deficiency leading to loss of appetite and alterations in taste and/or smell, she said.
Newly recognized in GI
She noted that “ARFID actually originates in the pediatric psychiatric literature, mostly in children with sensory issues [such as] autism spectrum disorder, so this is not a construct that started in digestive disease, but has been adapted and applied to patients with digestive disease, including IBD.”
The DSM-5 lists four criteria for ARFID: significant weight loss, significant nutritional deficiency, dependence on enteral nutrition or oral supplements, and marked interference with psychosocial functions.
Helen Burton Murray, PhD, director of the gastrointestinal behavioral health program in the Center for Neurointestinal Health at Massachusetts General Hospital, Boston, who is familiar with Dr. Taft’s work, said in an interview that inclusion of ARFID in DSM-5 has put a name to a syndrome or symptom cluster that in all likelihood already existed.
However, “the jury is still out about whether, if we do diagnose patients who have digestive diseases with ARFID, that then helps them get to a treatment that improves their relationship with food and improves nutritional issues that may have occurred as a result of a restricted food intake,” she said.
“We don’t know yet if the diagnosis will actually improve things. In our clinical practice, anecdotally, it has, both for patients with IBDs and for patients with other GI conditions, particularly GI functional motility disorders. We’re a little bit more confident about making the diagnosis of ARFID in GI functional motility disorders than we are in IBD of course,” she said.
Screening measures
To get a better sense of the prevalence of ARFID, compared with reasonable responses to digestive diseases, Dr. Taft and colleagues conducted their cross-sectional study in 289 adults with achalasia, celiac, eosinophilic esophagitis, or IBD.
They found that 51.3% of the total sample met the diagnostic criteria for ARFID based on the Nine-Item ARFID Screen (NIAS), including 75.7 % of patients with achalasia. But Dr. Taft had cautions
“I can tell you, working with achalasia patients, 75% do not have ARFID,” Dr. Taft said.
She noted that the 51.3% of patients with IBD identified by NIAS or the 53% identified by the ARFID+ scale as having ARFID was also highly doubtful.
Dr. Taft and colleagues determined that nearly half of the variance in the NIAS could be accounted for by GI symptoms rather than psychosocial factors, making it less than ideal for use in the clinic or by researchers.
She also noted, however, that she received an email from one of the creators of NIAS, Hana F. Zickgraf, PhD, from the University of South Alabama, Mobile. Dr. Zickgraf agreed that the scale had drawbacks when applied to patients with GI disease, and pointed instead to the Fear of Food Questionnaire, a newly developed 18-item GI disease-specific instrument. Dr. Taft recommended the new questionnaire for research purposes, and expressed hope that a shorter version could be made available for screening patients in clinic.
Dr. Burton Murray said that while the Fear of Food Questionnaire, perhaps in combination with NIAS, has the potential to be a useful screening tool, cutoffs for it have yet to be established.
“At the end of the day, the diagnosis would be made by a clinician who is able to determine whether the life impairment or if the nutritional impairment or restricted food intake are reasonable in the realm of their digestive disease, or could a treatment for ARFID be warranted to help them to make changes to improve their quality of life and nutrition,” she said.
Check biases at the door
Before arriving at a diagnosis of ARFID, clinicians should also consider biases, Dr. Taft said.
“Eating disorders are highly stigmatized and stereotyped diagnoses,” more often attributed to young White women than to either men or to people of racial or ethnic minorities, she said.
Cultural background may contribute to food restrictions, and the risk may increase with age, with 68% of patients with later-onset IBD restricting diets to control the disease. It’s also possible that beliefs about food and “clean and healthy” eating may influence food and eating choices after a patient receives an IBD diagnosis.
Dr. Taft also pointed out that clinicians and patients may have different ideas about what constitutes significant food avoidance. Clinicians may expect patients with IBD to eat despite feeling nauseated, having abdominal pains, or diarrhea, for example, when the same food avoidance might be deemed reasonable in patients with short-term GI infections.
“Severe IBD symptoms are a significant predictor of posttraumatic stress disorder symptoms, and PTSD is hallmarked by avoidance behaviors,” she added.
She emphasized the need for clinicians to ask the right questions of patients to get at the roots of their nutritional deficiency or eating behavior, and to refer patients to mental health professionals with expertise in disordered eating or GI psychology.
Dr. Taft and Dr. Burton Murray reported having no conflicts of interest to disclose.
This article was updated on Feb. 4, 2022.
Problems with eating and nutrition are common among patients with inflammatory bowel disease (IBD) and other gastrointestinal disorders, but clinicians who treat them should be careful not to automatically assume that patients have eating disorders, according to a psychologist who specializes in the psychological and social aspects of chronic digestive diseases.
On the other hand, clinicians must also be aware of the possibility that patients could have a recently identified syndrome cluster called avoidant restrictive food intake disorder (ARFID), said Tiffany Taft, PsyD, a research associate professor of medicine (gastroenterology and hepatology), medical social sciences, and psychiatry and behavioral sciences at Northwestern University, Chicago. In a recent study, she and her colleagues defined ARFID as “failure to meet one’s nutritional needs owing to sensory hypersensitivity, lack of interest in eating, or fear of aversive consequences from eating, and is associated with negative medical and psychosocial outcomes.”
ARFID “is a hot topic that we really don’t understand,” she said in an online presentation at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Nutritional deficiencies
Nutritional deficiencies are common among patients with IBD, “and nutritional deficiencies themselves can lead to symptoms or side effects that can cause people to eat less,” she said.
“As our vitamin B12 goes down, our cognitive functioning starts to decline, and we might not be making clear decisions in how we’re deciding what to eat, when to eat, if we should be eating at all – just something to think about in your patients who have nutritional deficiencies,” she told the audience.
Other common nutritional deficiencies that can affect eating and food choice among patients with IBD include low folate (B9) levels associated with sore tongue and weight loss, low iron levels leading to nausea and loss of appetite, and zinc deficiency leading to loss of appetite and alterations in taste and/or smell, she said.
Newly recognized in GI
She noted that “ARFID actually originates in the pediatric psychiatric literature, mostly in children with sensory issues [such as] autism spectrum disorder, so this is not a construct that started in digestive disease, but has been adapted and applied to patients with digestive disease, including IBD.”
The DSM-5 lists four criteria for ARFID: significant weight loss, significant nutritional deficiency, dependence on enteral nutrition or oral supplements, and marked interference with psychosocial functions.
Helen Burton Murray, PhD, director of the gastrointestinal behavioral health program in the Center for Neurointestinal Health at Massachusetts General Hospital, Boston, who is familiar with Dr. Taft’s work, said in an interview that inclusion of ARFID in DSM-5 has put a name to a syndrome or symptom cluster that in all likelihood already existed.
However, “the jury is still out about whether, if we do diagnose patients who have digestive diseases with ARFID, that then helps them get to a treatment that improves their relationship with food and improves nutritional issues that may have occurred as a result of a restricted food intake,” she said.
“We don’t know yet if the diagnosis will actually improve things. In our clinical practice, anecdotally, it has, both for patients with IBDs and for patients with other GI conditions, particularly GI functional motility disorders. We’re a little bit more confident about making the diagnosis of ARFID in GI functional motility disorders than we are in IBD of course,” she said.
Screening measures
To get a better sense of the prevalence of ARFID, compared with reasonable responses to digestive diseases, Dr. Taft and colleagues conducted their cross-sectional study in 289 adults with achalasia, celiac, eosinophilic esophagitis, or IBD.
They found that 51.3% of the total sample met the diagnostic criteria for ARFID based on the Nine-Item ARFID Screen (NIAS), including 75.7 % of patients with achalasia. But Dr. Taft had cautions
“I can tell you, working with achalasia patients, 75% do not have ARFID,” Dr. Taft said.
She noted that the 51.3% of patients with IBD identified by NIAS or the 53% identified by the ARFID+ scale as having ARFID was also highly doubtful.
Dr. Taft and colleagues determined that nearly half of the variance in the NIAS could be accounted for by GI symptoms rather than psychosocial factors, making it less than ideal for use in the clinic or by researchers.
She also noted, however, that she received an email from one of the creators of NIAS, Hana F. Zickgraf, PhD, from the University of South Alabama, Mobile. Dr. Zickgraf agreed that the scale had drawbacks when applied to patients with GI disease, and pointed instead to the Fear of Food Questionnaire, a newly developed 18-item GI disease-specific instrument. Dr. Taft recommended the new questionnaire for research purposes, and expressed hope that a shorter version could be made available for screening patients in clinic.
Dr. Burton Murray said that while the Fear of Food Questionnaire, perhaps in combination with NIAS, has the potential to be a useful screening tool, cutoffs for it have yet to be established.
“At the end of the day, the diagnosis would be made by a clinician who is able to determine whether the life impairment or if the nutritional impairment or restricted food intake are reasonable in the realm of their digestive disease, or could a treatment for ARFID be warranted to help them to make changes to improve their quality of life and nutrition,” she said.
Check biases at the door
Before arriving at a diagnosis of ARFID, clinicians should also consider biases, Dr. Taft said.
“Eating disorders are highly stigmatized and stereotyped diagnoses,” more often attributed to young White women than to either men or to people of racial or ethnic minorities, she said.
Cultural background may contribute to food restrictions, and the risk may increase with age, with 68% of patients with later-onset IBD restricting diets to control the disease. It’s also possible that beliefs about food and “clean and healthy” eating may influence food and eating choices after a patient receives an IBD diagnosis.
Dr. Taft also pointed out that clinicians and patients may have different ideas about what constitutes significant food avoidance. Clinicians may expect patients with IBD to eat despite feeling nauseated, having abdominal pains, or diarrhea, for example, when the same food avoidance might be deemed reasonable in patients with short-term GI infections.
“Severe IBD symptoms are a significant predictor of posttraumatic stress disorder symptoms, and PTSD is hallmarked by avoidance behaviors,” she added.
She emphasized the need for clinicians to ask the right questions of patients to get at the roots of their nutritional deficiency or eating behavior, and to refer patients to mental health professionals with expertise in disordered eating or GI psychology.
Dr. Taft and Dr. Burton Murray reported having no conflicts of interest to disclose.
This article was updated on Feb. 4, 2022.
Problems with eating and nutrition are common among patients with inflammatory bowel disease (IBD) and other gastrointestinal disorders, but clinicians who treat them should be careful not to automatically assume that patients have eating disorders, according to a psychologist who specializes in the psychological and social aspects of chronic digestive diseases.
On the other hand, clinicians must also be aware of the possibility that patients could have a recently identified syndrome cluster called avoidant restrictive food intake disorder (ARFID), said Tiffany Taft, PsyD, a research associate professor of medicine (gastroenterology and hepatology), medical social sciences, and psychiatry and behavioral sciences at Northwestern University, Chicago. In a recent study, she and her colleagues defined ARFID as “failure to meet one’s nutritional needs owing to sensory hypersensitivity, lack of interest in eating, or fear of aversive consequences from eating, and is associated with negative medical and psychosocial outcomes.”
ARFID “is a hot topic that we really don’t understand,” she said in an online presentation at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Nutritional deficiencies
Nutritional deficiencies are common among patients with IBD, “and nutritional deficiencies themselves can lead to symptoms or side effects that can cause people to eat less,” she said.
“As our vitamin B12 goes down, our cognitive functioning starts to decline, and we might not be making clear decisions in how we’re deciding what to eat, when to eat, if we should be eating at all – just something to think about in your patients who have nutritional deficiencies,” she told the audience.
Other common nutritional deficiencies that can affect eating and food choice among patients with IBD include low folate (B9) levels associated with sore tongue and weight loss, low iron levels leading to nausea and loss of appetite, and zinc deficiency leading to loss of appetite and alterations in taste and/or smell, she said.
Newly recognized in GI
She noted that “ARFID actually originates in the pediatric psychiatric literature, mostly in children with sensory issues [such as] autism spectrum disorder, so this is not a construct that started in digestive disease, but has been adapted and applied to patients with digestive disease, including IBD.”
The DSM-5 lists four criteria for ARFID: significant weight loss, significant nutritional deficiency, dependence on enteral nutrition or oral supplements, and marked interference with psychosocial functions.
Helen Burton Murray, PhD, director of the gastrointestinal behavioral health program in the Center for Neurointestinal Health at Massachusetts General Hospital, Boston, who is familiar with Dr. Taft’s work, said in an interview that inclusion of ARFID in DSM-5 has put a name to a syndrome or symptom cluster that in all likelihood already existed.
However, “the jury is still out about whether, if we do diagnose patients who have digestive diseases with ARFID, that then helps them get to a treatment that improves their relationship with food and improves nutritional issues that may have occurred as a result of a restricted food intake,” she said.
“We don’t know yet if the diagnosis will actually improve things. In our clinical practice, anecdotally, it has, both for patients with IBDs and for patients with other GI conditions, particularly GI functional motility disorders. We’re a little bit more confident about making the diagnosis of ARFID in GI functional motility disorders than we are in IBD of course,” she said.
Screening measures
To get a better sense of the prevalence of ARFID, compared with reasonable responses to digestive diseases, Dr. Taft and colleagues conducted their cross-sectional study in 289 adults with achalasia, celiac, eosinophilic esophagitis, or IBD.
They found that 51.3% of the total sample met the diagnostic criteria for ARFID based on the Nine-Item ARFID Screen (NIAS), including 75.7 % of patients with achalasia. But Dr. Taft had cautions
“I can tell you, working with achalasia patients, 75% do not have ARFID,” Dr. Taft said.
She noted that the 51.3% of patients with IBD identified by NIAS or the 53% identified by the ARFID+ scale as having ARFID was also highly doubtful.
Dr. Taft and colleagues determined that nearly half of the variance in the NIAS could be accounted for by GI symptoms rather than psychosocial factors, making it less than ideal for use in the clinic or by researchers.
She also noted, however, that she received an email from one of the creators of NIAS, Hana F. Zickgraf, PhD, from the University of South Alabama, Mobile. Dr. Zickgraf agreed that the scale had drawbacks when applied to patients with GI disease, and pointed instead to the Fear of Food Questionnaire, a newly developed 18-item GI disease-specific instrument. Dr. Taft recommended the new questionnaire for research purposes, and expressed hope that a shorter version could be made available for screening patients in clinic.
Dr. Burton Murray said that while the Fear of Food Questionnaire, perhaps in combination with NIAS, has the potential to be a useful screening tool, cutoffs for it have yet to be established.
“At the end of the day, the diagnosis would be made by a clinician who is able to determine whether the life impairment or if the nutritional impairment or restricted food intake are reasonable in the realm of their digestive disease, or could a treatment for ARFID be warranted to help them to make changes to improve their quality of life and nutrition,” she said.
Check biases at the door
Before arriving at a diagnosis of ARFID, clinicians should also consider biases, Dr. Taft said.
“Eating disorders are highly stigmatized and stereotyped diagnoses,” more often attributed to young White women than to either men or to people of racial or ethnic minorities, she said.
Cultural background may contribute to food restrictions, and the risk may increase with age, with 68% of patients with later-onset IBD restricting diets to control the disease. It’s also possible that beliefs about food and “clean and healthy” eating may influence food and eating choices after a patient receives an IBD diagnosis.
Dr. Taft also pointed out that clinicians and patients may have different ideas about what constitutes significant food avoidance. Clinicians may expect patients with IBD to eat despite feeling nauseated, having abdominal pains, or diarrhea, for example, when the same food avoidance might be deemed reasonable in patients with short-term GI infections.
“Severe IBD symptoms are a significant predictor of posttraumatic stress disorder symptoms, and PTSD is hallmarked by avoidance behaviors,” she added.
She emphasized the need for clinicians to ask the right questions of patients to get at the roots of their nutritional deficiency or eating behavior, and to refer patients to mental health professionals with expertise in disordered eating or GI psychology.
Dr. Taft and Dr. Burton Murray reported having no conflicts of interest to disclose.
This article was updated on Feb. 4, 2022.
FROM CROHN’S & COLITIS CONGRESS
Parent group warns of social media/eating disorders link
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.








