User login
Long-term ceftaroline use associated with neutropenia
SAN DIEGO – The long-term use of ceftaroline is associated with neutropenia, results from a single-center retrospective study showed.
A fifth-generation cephalosporin antibiotic with activity against methicillin-resistant Staphylococcus aureus, ceftaroline is approved for the treatment of community-acquired pneumonia and skin and skin structure infections. It’s also an option for treating orthopedic and endovascular infections when primary therapy fails or is contraindicated, according to one of the study authors, Dr. Hollis R. O’Neal Jr. “There are small case reports of associations between ceftaroline use and neutropenia, and we were noticing that many patients in our clinical practice were developing neutropenia,” Dr. O’Neal, a pulmonologist at Louisiana State University Health Baton Rouge, said in an interview at the Interscience Conference on Antimicrobial Agents and Chemotherapy.
In an effort to determine the incidence, severity, and outcome of neutropenia in patients receiving long-term ceftaroline therapy, Dr. O’Neal and his associates retrospectively evaluated 38 patients who received at least 7 days of ceftaroline initiated at LSU Health Baton Rouge between June 2012 and December 2014. They defined clinically significant neutropenia as having an absolute neutrophil count (ANC) below 2500 cells/mm3 and gathered pertinent data from medical records including comorbidities, chronic medications, and diagnoses.
The median age of the 38 patients was 47 years and their median body mass index was 28 kg/m2. Of the 38 patients, 10 (26%) developed neutropenia. “That was surprising to me,” Dr. O’Neal said. “I thought we would find three or four cases.” Compared with those who were nonneutropenic, those who developed neutropenia tended to be younger (a median of 44 years vs. 51 years), have a lower body mass index (a median of 25 kg/m2 vs. 32 kg/m2), and be more likely to have a longer duration of ceftaroline therapy (a median of 36 days vs. 26 days).
Of the 10 neutropenic patients, 7 had an ANC below 1,500 cells/mm3, and 4 had an ANC below 500 cells/mm3. The median time to first neutropenic day was day 21, with a median nadir of 1,156 cells/mm3. One hospitalization occurred that was believed to be due to neutropenia, but all 30 patients were alive at least 30 days after completing ceftaroline therapy.
“Once the ANC falls below 2,500 cells/mm3, the risk of developing true neutropenia is high,” Dr. O’Neal said. “So what we’re doing is monitoring ANC levels weekly. When they fall below 2,500 we monitor [ANC levels] twice weekly. When they reach 1,500 we stop the drug. So it’s really changed how we monitor the drug’s use.”
The study’s lead author is Dr. Katherine W. Lavie, an infectious diseases fellow at LSU Health Baton Rouge. The researchers reported having no financial disclosures.
SAN DIEGO – The long-term use of ceftaroline is associated with neutropenia, results from a single-center retrospective study showed.
A fifth-generation cephalosporin antibiotic with activity against methicillin-resistant Staphylococcus aureus, ceftaroline is approved for the treatment of community-acquired pneumonia and skin and skin structure infections. It’s also an option for treating orthopedic and endovascular infections when primary therapy fails or is contraindicated, according to one of the study authors, Dr. Hollis R. O’Neal Jr. “There are small case reports of associations between ceftaroline use and neutropenia, and we were noticing that many patients in our clinical practice were developing neutropenia,” Dr. O’Neal, a pulmonologist at Louisiana State University Health Baton Rouge, said in an interview at the Interscience Conference on Antimicrobial Agents and Chemotherapy.
In an effort to determine the incidence, severity, and outcome of neutropenia in patients receiving long-term ceftaroline therapy, Dr. O’Neal and his associates retrospectively evaluated 38 patients who received at least 7 days of ceftaroline initiated at LSU Health Baton Rouge between June 2012 and December 2014. They defined clinically significant neutropenia as having an absolute neutrophil count (ANC) below 2500 cells/mm3 and gathered pertinent data from medical records including comorbidities, chronic medications, and diagnoses.
The median age of the 38 patients was 47 years and their median body mass index was 28 kg/m2. Of the 38 patients, 10 (26%) developed neutropenia. “That was surprising to me,” Dr. O’Neal said. “I thought we would find three or four cases.” Compared with those who were nonneutropenic, those who developed neutropenia tended to be younger (a median of 44 years vs. 51 years), have a lower body mass index (a median of 25 kg/m2 vs. 32 kg/m2), and be more likely to have a longer duration of ceftaroline therapy (a median of 36 days vs. 26 days).
Of the 10 neutropenic patients, 7 had an ANC below 1,500 cells/mm3, and 4 had an ANC below 500 cells/mm3. The median time to first neutropenic day was day 21, with a median nadir of 1,156 cells/mm3. One hospitalization occurred that was believed to be due to neutropenia, but all 30 patients were alive at least 30 days after completing ceftaroline therapy.
“Once the ANC falls below 2,500 cells/mm3, the risk of developing true neutropenia is high,” Dr. O’Neal said. “So what we’re doing is monitoring ANC levels weekly. When they fall below 2,500 we monitor [ANC levels] twice weekly. When they reach 1,500 we stop the drug. So it’s really changed how we monitor the drug’s use.”
The study’s lead author is Dr. Katherine W. Lavie, an infectious diseases fellow at LSU Health Baton Rouge. The researchers reported having no financial disclosures.
SAN DIEGO – The long-term use of ceftaroline is associated with neutropenia, results from a single-center retrospective study showed.
A fifth-generation cephalosporin antibiotic with activity against methicillin-resistant Staphylococcus aureus, ceftaroline is approved for the treatment of community-acquired pneumonia and skin and skin structure infections. It’s also an option for treating orthopedic and endovascular infections when primary therapy fails or is contraindicated, according to one of the study authors, Dr. Hollis R. O’Neal Jr. “There are small case reports of associations between ceftaroline use and neutropenia, and we were noticing that many patients in our clinical practice were developing neutropenia,” Dr. O’Neal, a pulmonologist at Louisiana State University Health Baton Rouge, said in an interview at the Interscience Conference on Antimicrobial Agents and Chemotherapy.
In an effort to determine the incidence, severity, and outcome of neutropenia in patients receiving long-term ceftaroline therapy, Dr. O’Neal and his associates retrospectively evaluated 38 patients who received at least 7 days of ceftaroline initiated at LSU Health Baton Rouge between June 2012 and December 2014. They defined clinically significant neutropenia as having an absolute neutrophil count (ANC) below 2500 cells/mm3 and gathered pertinent data from medical records including comorbidities, chronic medications, and diagnoses.
The median age of the 38 patients was 47 years and their median body mass index was 28 kg/m2. Of the 38 patients, 10 (26%) developed neutropenia. “That was surprising to me,” Dr. O’Neal said. “I thought we would find three or four cases.” Compared with those who were nonneutropenic, those who developed neutropenia tended to be younger (a median of 44 years vs. 51 years), have a lower body mass index (a median of 25 kg/m2 vs. 32 kg/m2), and be more likely to have a longer duration of ceftaroline therapy (a median of 36 days vs. 26 days).
Of the 10 neutropenic patients, 7 had an ANC below 1,500 cells/mm3, and 4 had an ANC below 500 cells/mm3. The median time to first neutropenic day was day 21, with a median nadir of 1,156 cells/mm3. One hospitalization occurred that was believed to be due to neutropenia, but all 30 patients were alive at least 30 days after completing ceftaroline therapy.
“Once the ANC falls below 2,500 cells/mm3, the risk of developing true neutropenia is high,” Dr. O’Neal said. “So what we’re doing is monitoring ANC levels weekly. When they fall below 2,500 we monitor [ANC levels] twice weekly. When they reach 1,500 we stop the drug. So it’s really changed how we monitor the drug’s use.”
The study’s lead author is Dr. Katherine W. Lavie, an infectious diseases fellow at LSU Health Baton Rouge. The researchers reported having no financial disclosures.
AT ICAAC 2015
Key clinical point: Long-term ceftaroline use is associated with neutropenia.
Major finding: Of 38 patients who received at least 7 days of ceftaroline, 10 (26%) developed neutropenia.
Data source: A retrospective cohort study of 38 patients who received long-term ceftaroline therapy between June 2012 and December 2014.
Disclosures: The researchers reported having no financial disclosures.
New assay may be a game changer in invasive candidiasis
SAN DIEGO – The T2 magnetic resonance assay for rapid diagnosis or rule-out of invasive candidiasis has the potential to significantly change the management and outcome of this common, deadly, and expensive disease, Dr. Peter G. Pappas asserted at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
This novel diagnostic instrument addresses a longstanding major unmet need in the field of infectious diseases: namely, the necessity for a substantially faster and more accurate test for invasive candidiasis than the decades-old current standard, which is automated blood cultures.
Blood cultures are notoriously insensitive. Indeed, they are negative in roughly 50% of patients with invasive candidiasis, mainly those with deep-seated, noncandidemic invasive candidiasis. And blood cultures are far too slow, taking 2-5 days to finalize results, explained Dr. Pappas, professor of medicine at the University of Alabama, Birmingham. “Management of invasive candidiasis involves time-critical decision making. The earlier we can approach the patient with specific therapy, the better the outcomes. That actually hasn’t been shown prospectively, but it’s a reasonable assumption based upon the available retrospective studies. We would like to be able to initiate effective treatment within 12-24 hours; that’s seldom possible with blood cultures,” he continued.
Dr. Pappas was principal investigator in the direct T2 pivotal clinical trial which led to Food and Drug Administration approval of the T2 magnetic resonance assay, known as the T2Candida platform. In this 1,801-patient multicenter study, the assay provided results in a mean of just over 4 hours with 91.4% sensitivity, 99.4% specificity, and a negative predictive value of 99.2%. In contrast, blood cultures, which were obtained in all participants, required an average of more than 120 hours to provide results (Clin Infect Dis. 2015 Mar 15;60[6]:892-9. doi: 10.1093/cid/ciu959).
At ICAAC 2015, the clinical trial was named one of the top 10 papers of the year in mycology.
Invasive candidiasis is a huge problem that’s seen little in the way of progress over the past 2 decades. Candida infections account for 6% of all hospital-acquired infections in the United States. More than 400,000 cases of invasive candidiasis occur annually worldwide. Attributable mortality rates of up to 49% have been reported. The disease is an important cause of prolonged hospitalization, with episodes adding an average of about $40,000 to the cost of a hospital stay.
The T2Candida test not only enables physicians to get effective antifungal agents started quickly, but a negative result will allow a drastic cutback in the now-routine use of empiric antifungal therapy prescribed during the lengthy wait for blood culture results. This will reduce needless exposure to drug side effects among uninfected patients, discourage the rise of resistant Candida strains, and substantially reduce health care costs.
Extrapolating from this trial’s data, and from other studies, Dr. Pappas said “the sweet spot” for the assay, where it has an impressively high 75%-85% positive predictive value, occurs when it is applied to patients with a pretest probability of invasive candidiasis in the 3%-10% range based upon well-known high-risk factors, including current cancer, neutropenia, organ or stem cell transplantation, having a central venous catheter, or being on steroid therapy.
The new assay bypasses blood cultures entirely, instead employing molecular diagnostics to directly analyze a whole blood sample. It can identify C. albicans and four other clinically relevant Candida species which collectively account for the vast majority of cases of invasive candidiasis. One of the reasons panelists at ICAAC 2015 named the T2Candida pivotal trial to their top-10 list of major papers in mycology is that the T2 magnetic resonance technology is a platform capable of also being applied to the diagnosis of other pathogens whose prompt diagnosis is critical.
Another advantage of the T2Candida platform is that the results are unaffected by antifungal therapy. In contrast, blood cultures become unreliable if a patient has empiric antifungal therapy onboard. In a separate presentation at ICAAC 2015, Dr. Pappas and coworkers presented interim results from an ongoing study that capitalizes on this advantage of the new technology.
To date, the study has enrolled 23 patients with culture-proven candidemia, all of whom underwent daily testing via both blood cultures and T2Candida during their first 7 days on antifungal therapy. Blood cultures remained positive for only two patients on-treatment, whereas T2Candida remained positive for nine patients on all 7 days and also detected one new case of intra-abdominal candidiasis missed by blood cultures.
Thus, the T2Candida platform may be an effective method not only for diagnosis of invasive candidiasis, Dr. Pappas observed, but for monitoring the response to therapy in the form of antifungal agents and/or removal of an offending contaminated catheter.
Dr. Pappas reported receiving research grants from and serving as an advisor to T2 Biosystems, which markets the assay. He has also received research support from Astellas, Gilead, and Merck.
SAN DIEGO – The T2 magnetic resonance assay for rapid diagnosis or rule-out of invasive candidiasis has the potential to significantly change the management and outcome of this common, deadly, and expensive disease, Dr. Peter G. Pappas asserted at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
This novel diagnostic instrument addresses a longstanding major unmet need in the field of infectious diseases: namely, the necessity for a substantially faster and more accurate test for invasive candidiasis than the decades-old current standard, which is automated blood cultures.
Blood cultures are notoriously insensitive. Indeed, they are negative in roughly 50% of patients with invasive candidiasis, mainly those with deep-seated, noncandidemic invasive candidiasis. And blood cultures are far too slow, taking 2-5 days to finalize results, explained Dr. Pappas, professor of medicine at the University of Alabama, Birmingham. “Management of invasive candidiasis involves time-critical decision making. The earlier we can approach the patient with specific therapy, the better the outcomes. That actually hasn’t been shown prospectively, but it’s a reasonable assumption based upon the available retrospective studies. We would like to be able to initiate effective treatment within 12-24 hours; that’s seldom possible with blood cultures,” he continued.
Dr. Pappas was principal investigator in the direct T2 pivotal clinical trial which led to Food and Drug Administration approval of the T2 magnetic resonance assay, known as the T2Candida platform. In this 1,801-patient multicenter study, the assay provided results in a mean of just over 4 hours with 91.4% sensitivity, 99.4% specificity, and a negative predictive value of 99.2%. In contrast, blood cultures, which were obtained in all participants, required an average of more than 120 hours to provide results (Clin Infect Dis. 2015 Mar 15;60[6]:892-9. doi: 10.1093/cid/ciu959).
At ICAAC 2015, the clinical trial was named one of the top 10 papers of the year in mycology.
Invasive candidiasis is a huge problem that’s seen little in the way of progress over the past 2 decades. Candida infections account for 6% of all hospital-acquired infections in the United States. More than 400,000 cases of invasive candidiasis occur annually worldwide. Attributable mortality rates of up to 49% have been reported. The disease is an important cause of prolonged hospitalization, with episodes adding an average of about $40,000 to the cost of a hospital stay.
The T2Candida test not only enables physicians to get effective antifungal agents started quickly, but a negative result will allow a drastic cutback in the now-routine use of empiric antifungal therapy prescribed during the lengthy wait for blood culture results. This will reduce needless exposure to drug side effects among uninfected patients, discourage the rise of resistant Candida strains, and substantially reduce health care costs.
Extrapolating from this trial’s data, and from other studies, Dr. Pappas said “the sweet spot” for the assay, where it has an impressively high 75%-85% positive predictive value, occurs when it is applied to patients with a pretest probability of invasive candidiasis in the 3%-10% range based upon well-known high-risk factors, including current cancer, neutropenia, organ or stem cell transplantation, having a central venous catheter, or being on steroid therapy.
The new assay bypasses blood cultures entirely, instead employing molecular diagnostics to directly analyze a whole blood sample. It can identify C. albicans and four other clinically relevant Candida species which collectively account for the vast majority of cases of invasive candidiasis. One of the reasons panelists at ICAAC 2015 named the T2Candida pivotal trial to their top-10 list of major papers in mycology is that the T2 magnetic resonance technology is a platform capable of also being applied to the diagnosis of other pathogens whose prompt diagnosis is critical.
Another advantage of the T2Candida platform is that the results are unaffected by antifungal therapy. In contrast, blood cultures become unreliable if a patient has empiric antifungal therapy onboard. In a separate presentation at ICAAC 2015, Dr. Pappas and coworkers presented interim results from an ongoing study that capitalizes on this advantage of the new technology.
To date, the study has enrolled 23 patients with culture-proven candidemia, all of whom underwent daily testing via both blood cultures and T2Candida during their first 7 days on antifungal therapy. Blood cultures remained positive for only two patients on-treatment, whereas T2Candida remained positive for nine patients on all 7 days and also detected one new case of intra-abdominal candidiasis missed by blood cultures.
Thus, the T2Candida platform may be an effective method not only for diagnosis of invasive candidiasis, Dr. Pappas observed, but for monitoring the response to therapy in the form of antifungal agents and/or removal of an offending contaminated catheter.
Dr. Pappas reported receiving research grants from and serving as an advisor to T2 Biosystems, which markets the assay. He has also received research support from Astellas, Gilead, and Merck.
SAN DIEGO – The T2 magnetic resonance assay for rapid diagnosis or rule-out of invasive candidiasis has the potential to significantly change the management and outcome of this common, deadly, and expensive disease, Dr. Peter G. Pappas asserted at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
This novel diagnostic instrument addresses a longstanding major unmet need in the field of infectious diseases: namely, the necessity for a substantially faster and more accurate test for invasive candidiasis than the decades-old current standard, which is automated blood cultures.
Blood cultures are notoriously insensitive. Indeed, they are negative in roughly 50% of patients with invasive candidiasis, mainly those with deep-seated, noncandidemic invasive candidiasis. And blood cultures are far too slow, taking 2-5 days to finalize results, explained Dr. Pappas, professor of medicine at the University of Alabama, Birmingham. “Management of invasive candidiasis involves time-critical decision making. The earlier we can approach the patient with specific therapy, the better the outcomes. That actually hasn’t been shown prospectively, but it’s a reasonable assumption based upon the available retrospective studies. We would like to be able to initiate effective treatment within 12-24 hours; that’s seldom possible with blood cultures,” he continued.
Dr. Pappas was principal investigator in the direct T2 pivotal clinical trial which led to Food and Drug Administration approval of the T2 magnetic resonance assay, known as the T2Candida platform. In this 1,801-patient multicenter study, the assay provided results in a mean of just over 4 hours with 91.4% sensitivity, 99.4% specificity, and a negative predictive value of 99.2%. In contrast, blood cultures, which were obtained in all participants, required an average of more than 120 hours to provide results (Clin Infect Dis. 2015 Mar 15;60[6]:892-9. doi: 10.1093/cid/ciu959).
At ICAAC 2015, the clinical trial was named one of the top 10 papers of the year in mycology.
Invasive candidiasis is a huge problem that’s seen little in the way of progress over the past 2 decades. Candida infections account for 6% of all hospital-acquired infections in the United States. More than 400,000 cases of invasive candidiasis occur annually worldwide. Attributable mortality rates of up to 49% have been reported. The disease is an important cause of prolonged hospitalization, with episodes adding an average of about $40,000 to the cost of a hospital stay.
The T2Candida test not only enables physicians to get effective antifungal agents started quickly, but a negative result will allow a drastic cutback in the now-routine use of empiric antifungal therapy prescribed during the lengthy wait for blood culture results. This will reduce needless exposure to drug side effects among uninfected patients, discourage the rise of resistant Candida strains, and substantially reduce health care costs.
Extrapolating from this trial’s data, and from other studies, Dr. Pappas said “the sweet spot” for the assay, where it has an impressively high 75%-85% positive predictive value, occurs when it is applied to patients with a pretest probability of invasive candidiasis in the 3%-10% range based upon well-known high-risk factors, including current cancer, neutropenia, organ or stem cell transplantation, having a central venous catheter, or being on steroid therapy.
The new assay bypasses blood cultures entirely, instead employing molecular diagnostics to directly analyze a whole blood sample. It can identify C. albicans and four other clinically relevant Candida species which collectively account for the vast majority of cases of invasive candidiasis. One of the reasons panelists at ICAAC 2015 named the T2Candida pivotal trial to their top-10 list of major papers in mycology is that the T2 magnetic resonance technology is a platform capable of also being applied to the diagnosis of other pathogens whose prompt diagnosis is critical.
Another advantage of the T2Candida platform is that the results are unaffected by antifungal therapy. In contrast, blood cultures become unreliable if a patient has empiric antifungal therapy onboard. In a separate presentation at ICAAC 2015, Dr. Pappas and coworkers presented interim results from an ongoing study that capitalizes on this advantage of the new technology.
To date, the study has enrolled 23 patients with culture-proven candidemia, all of whom underwent daily testing via both blood cultures and T2Candida during their first 7 days on antifungal therapy. Blood cultures remained positive for only two patients on-treatment, whereas T2Candida remained positive for nine patients on all 7 days and also detected one new case of intra-abdominal candidiasis missed by blood cultures.
Thus, the T2Candida platform may be an effective method not only for diagnosis of invasive candidiasis, Dr. Pappas observed, but for monitoring the response to therapy in the form of antifungal agents and/or removal of an offending contaminated catheter.
Dr. Pappas reported receiving research grants from and serving as an advisor to T2 Biosystems, which markets the assay. He has also received research support from Astellas, Gilead, and Merck.
EXPERT ANALYSIS FROM ICAAC 2015
Hospitalization driving bariatric surgery cost differences
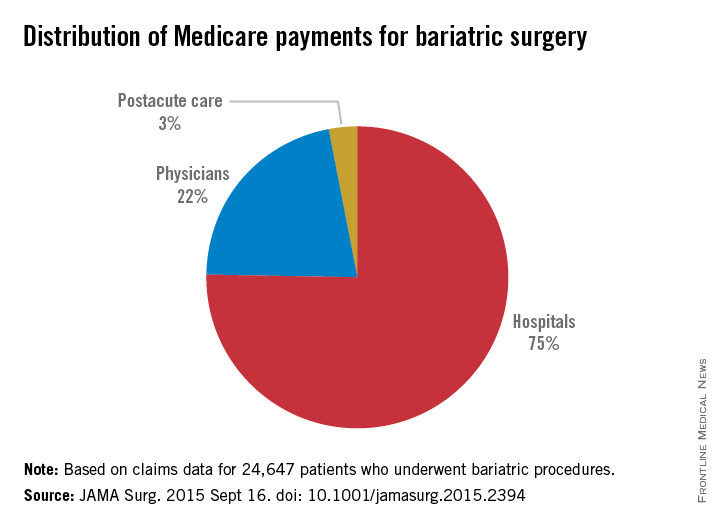
Medicare payments to hospitals for bariatric operations varied by nearly $2,000 per episode of care, mostly because of differences in costs incurred in the initial – or index – hospitalization.
The findings, published online Sept. 16 in JAMA Surgery, offer hospitals a guide to where cost variation is highest (doi:10.1001/jamasurg.2015.2394) for these procedures.
Knowing where costs vary the most is particularly important if hospitals opt to accept bundled Medicare payments for bariatric procedures, which are a proposed addition to 48 other episodes of care that can currently be reimbursed in this way. Under bundled care payment programs, hospitals receive a single payment for all services related to a surgery or other episode of care, thereby accepting more risk when inefficiencies occur.
For their research, Dr. Tyler R. Grenda and his colleagues at University of Michigan, Ann Arbor, Center for Healthcare Outcomes and Policy, looked at claims data for 24,647 patients receiving bariatric procedures at 463 hospitals during 2011-2012.
Operations included laparoscopic gastric banding, laparoscopic Roux-en-Y gastric bypass, and open Roux-en-Y gastric bypass, with fewer than 5% of patients receiving other interventions. Mean total payments varied from $11,086 to $13,073 per episode of care, defined as index hospitalization through 30 days postdischarge, for a 16.5% difference between the lowest and highest hospital quartiles.
The index hospitalization was responsible for the largest portion of total payments (75%), seen in the study, followed by physician services (21%) and postacute care services (2.8%).
The large share of costs incurred during the index hospitalization was “likely owing to inpatient complications that drive [diagnosis-related group] up-coding,” the authors wrote, noting that DRG with complications result in higher Medicare payments.
Dr. Grenda and his colleagues concluded that bariatric surgery “appears to have a distinct pattern of hospital cost variation” unlike that seen in other procedures that have been studied to identify drivers of cost differences. “This difference in the pattern of variation emphasizes the importance of understanding cost variation specific to each procedure,” they wrote.
For example, a study that looked at hip fracture repair found that postacute care accounted for a large portion of variation in payments, while less variation was seen for the index hospitalization (Health Serv Res. 2010;45[6, pt 1]:1783-95).
In the current policy environment, in which bundled payments are seen as a way to shift cost accountability to hospitals, “a detailed understanding of variation in the costs for bariatric surgery will be essential for hospitals to identify areas of risk and opportunities for improvement,” the researchers wrote in their analysis.
Dr. Grenda and his colleagues’ research was funded by Agency for Healthcare Research and Quality. One coauthor and the supervisor of the study, Dr. Justin Dimnick, disclosed a financial relationship with ArborMetrix, a health care analytics firm not involved with the study; he is also an editor of JAMA Surgery, which published the study.
Medicare payments to hospitals for bariatric operations varied by nearly $2,000 per episode of care, mostly because of differences in costs incurred in the initial – or index – hospitalization.
The findings, published online Sept. 16 in JAMA Surgery, offer hospitals a guide to where cost variation is highest (doi:10.1001/jamasurg.2015.2394) for these procedures.
Knowing where costs vary the most is particularly important if hospitals opt to accept bundled Medicare payments for bariatric procedures, which are a proposed addition to 48 other episodes of care that can currently be reimbursed in this way. Under bundled care payment programs, hospitals receive a single payment for all services related to a surgery or other episode of care, thereby accepting more risk when inefficiencies occur.
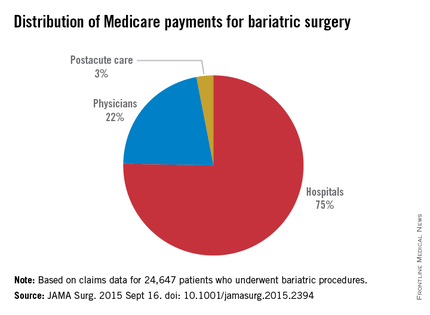
For their research, Dr. Tyler R. Grenda and his colleagues at University of Michigan, Ann Arbor, Center for Healthcare Outcomes and Policy, looked at claims data for 24,647 patients receiving bariatric procedures at 463 hospitals during 2011-2012.
Operations included laparoscopic gastric banding, laparoscopic Roux-en-Y gastric bypass, and open Roux-en-Y gastric bypass, with fewer than 5% of patients receiving other interventions. Mean total payments varied from $11,086 to $13,073 per episode of care, defined as index hospitalization through 30 days postdischarge, for a 16.5% difference between the lowest and highest hospital quartiles.
The index hospitalization was responsible for the largest portion of total payments (75%), seen in the study, followed by physician services (21%) and postacute care services (2.8%).
The large share of costs incurred during the index hospitalization was “likely owing to inpatient complications that drive [diagnosis-related group] up-coding,” the authors wrote, noting that DRG with complications result in higher Medicare payments.
Dr. Grenda and his colleagues concluded that bariatric surgery “appears to have a distinct pattern of hospital cost variation” unlike that seen in other procedures that have been studied to identify drivers of cost differences. “This difference in the pattern of variation emphasizes the importance of understanding cost variation specific to each procedure,” they wrote.
For example, a study that looked at hip fracture repair found that postacute care accounted for a large portion of variation in payments, while less variation was seen for the index hospitalization (Health Serv Res. 2010;45[6, pt 1]:1783-95).
In the current policy environment, in which bundled payments are seen as a way to shift cost accountability to hospitals, “a detailed understanding of variation in the costs for bariatric surgery will be essential for hospitals to identify areas of risk and opportunities for improvement,” the researchers wrote in their analysis.
Dr. Grenda and his colleagues’ research was funded by Agency for Healthcare Research and Quality. One coauthor and the supervisor of the study, Dr. Justin Dimnick, disclosed a financial relationship with ArborMetrix, a health care analytics firm not involved with the study; he is also an editor of JAMA Surgery, which published the study.
Medicare payments to hospitals for bariatric operations varied by nearly $2,000 per episode of care, mostly because of differences in costs incurred in the initial – or index – hospitalization.
The findings, published online Sept. 16 in JAMA Surgery, offer hospitals a guide to where cost variation is highest (doi:10.1001/jamasurg.2015.2394) for these procedures.
Knowing where costs vary the most is particularly important if hospitals opt to accept bundled Medicare payments for bariatric procedures, which are a proposed addition to 48 other episodes of care that can currently be reimbursed in this way. Under bundled care payment programs, hospitals receive a single payment for all services related to a surgery or other episode of care, thereby accepting more risk when inefficiencies occur.
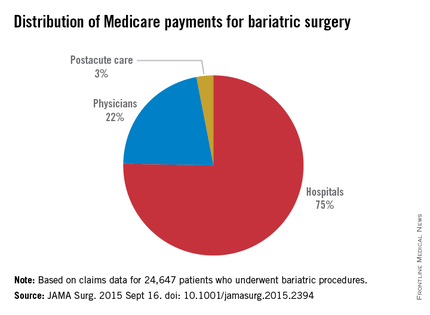
For their research, Dr. Tyler R. Grenda and his colleagues at University of Michigan, Ann Arbor, Center for Healthcare Outcomes and Policy, looked at claims data for 24,647 patients receiving bariatric procedures at 463 hospitals during 2011-2012.
Operations included laparoscopic gastric banding, laparoscopic Roux-en-Y gastric bypass, and open Roux-en-Y gastric bypass, with fewer than 5% of patients receiving other interventions. Mean total payments varied from $11,086 to $13,073 per episode of care, defined as index hospitalization through 30 days postdischarge, for a 16.5% difference between the lowest and highest hospital quartiles.
The index hospitalization was responsible for the largest portion of total payments (75%), seen in the study, followed by physician services (21%) and postacute care services (2.8%).
The large share of costs incurred during the index hospitalization was “likely owing to inpatient complications that drive [diagnosis-related group] up-coding,” the authors wrote, noting that DRG with complications result in higher Medicare payments.
Dr. Grenda and his colleagues concluded that bariatric surgery “appears to have a distinct pattern of hospital cost variation” unlike that seen in other procedures that have been studied to identify drivers of cost differences. “This difference in the pattern of variation emphasizes the importance of understanding cost variation specific to each procedure,” they wrote.
For example, a study that looked at hip fracture repair found that postacute care accounted for a large portion of variation in payments, while less variation was seen for the index hospitalization (Health Serv Res. 2010;45[6, pt 1]:1783-95).
In the current policy environment, in which bundled payments are seen as a way to shift cost accountability to hospitals, “a detailed understanding of variation in the costs for bariatric surgery will be essential for hospitals to identify areas of risk and opportunities for improvement,” the researchers wrote in their analysis.
Dr. Grenda and his colleagues’ research was funded by Agency for Healthcare Research and Quality. One coauthor and the supervisor of the study, Dr. Justin Dimnick, disclosed a financial relationship with ArborMetrix, a health care analytics firm not involved with the study; he is also an editor of JAMA Surgery, which published the study.
FROM JAMA SURGERY
Key clinical point: Initial hospitalization costs account for the lion’s share of cost variation for bariatric operations covered under Medicare.
Major finding: Mean total costs varied from $11,086 to about $13,073 per care episode, a 16.5% difference between the lowest- and highest-quartile hospitals; index hospitalizations accounted for 75% of payments, with less spent on physician fees and aftercare.
Data source: Medicare claims data for nearly 25,000 bariatric procedures performed at U.S. hospitals during 2011-2012.
Disclosures: Study was sponsored by the Agency for Healthcare Research and Quality; one coauthor disclosed financial relationship with a health analytics firm and journal editorship.
Diabetic foot ulcer: Early closure post debridement best
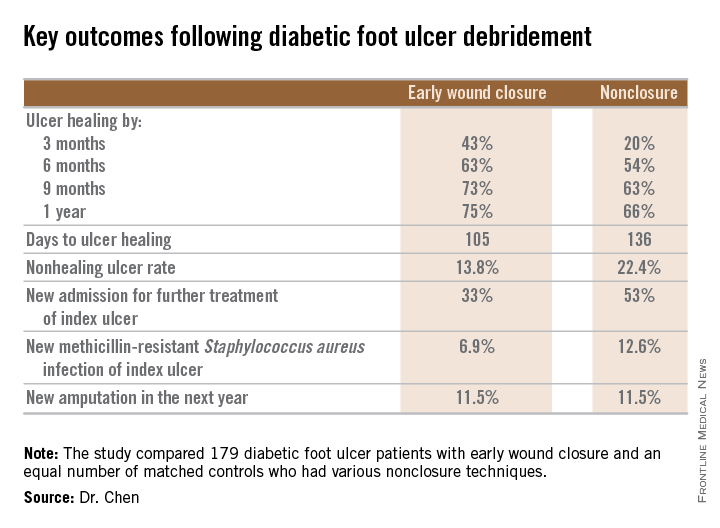
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, Dr. Shey-Ying Chen reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.

He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings. The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 52% of the nonclosure group. Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in patients with peripheral vascular disease, with an OR of 0.62; neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, he continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up. Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported having no financial conflicts with regard to this study, conducted without commercial sponsorship.
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, Dr. Shey-Ying Chen reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.

He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings. The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 52% of the nonclosure group. Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in patients with peripheral vascular disease, with an OR of 0.62; neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, he continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up. Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported having no financial conflicts with regard to this study, conducted without commercial sponsorship.
SAN DIEGO – Early wound closure prior to hospital discharge after surgical debridement of infected diabetic foot ulcers yields higher ulcer healing rates and a shorter time to healing, compared with various nonclosure wound management methods, according to a propensity-matched study.
How best to manage the open wound following nonamputative surgery of infected diabetic foot ulcers has been controversial. But early wound closure during the index hospitalization was the clear winner in this comparative study, Dr. Shey-Ying Chen reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.

He presented a retrospective comparison between 179 diabetic foot ulcer (DFU) patients with early wound closure after surgical debridement and an equal number of matched controls treated with various nonclosure techniques, including negative pressure wound therapy and the repeated application of moist dressings. The two study groups were matched first on the basis of DFU location – toe, forefoot, midfoot, or rear foot – and then further propensity matched based on demographics, comorbid conditions, the presence of neuropathy, ulcer status by Wagner classification, infection severity, revascularization procedures, and other variables.
During 1 year of follow-up post discharge, ulcer healing occurred in 75% of the early wound closure group, compared with 66% of the nonclosure patients. Readmission for further treatment of the index ulcer occurred in 33% of the early closure group and 52% of the nonclosure group. Other outcomes were also superior in the early wound closure group, noted Dr. Chen of Beth Israel Deaconess Medical Center, Boston.
Two independent predictors of DFU healing during the follow-up period emerged from a Cox regression analysis: early wound closure, with an adjusted odds ratio of 1.63, and acute as opposed to chronic DFU, with an OR of 1.35.
Ulcer healing was significantly less likely in patients with peripheral vascular disease, with an OR of 0.62; neuropathy, with an OR of 0.53; and methicillin-resistant Staphylococcus aureus wound infection, with an OR of 0.59, he continued.
Underscoring the longer-term difficulties faced by patients with DFUs, it’s noteworthy that 11.5% of patients in both study arms underwent new amputations during the year of follow-up. Moreover, a new diagnosis of osteomyelitis was made in 20% of the early wound closure group and 26% of the nonclosure group, a nonsignificant difference.
Dr. Adolf W. Karchmer, Dr. Chen’s senior coinvestigator, said the outcome data are too new to be able to gauge how vascular, orthopedic, and podiatric surgeons will react.
The investigators reported having no financial conflicts with regard to this study, conducted without commercial sponsorship.
AT ICAAC 2015
Key clinical point: Diabetic foot ulcers are more likely to heal with early wound closure following surgical debridement than with nonclosure techniques.
Major finding: Healing of diabetic foot ulcers after surgical debridement took an average of 105 days in patients who underwent early wound closure prior to hospital discharge, compared with 136 days in those whose wounds were managed with nonclosure techniques.
Data source: A retrospective, nonrandomized study featuring two propensity score–matched groups, with 179 patients in each, who were followed for 1 year post discharge for surgical debridement of a diabetic foot ulcer.
Disclosures: The presenter reported having no financial conflicts regarding this study, conducted free of commercial support.
No difference in long-term cost for diabetes treatment with bariatric surgery
There was no difference in long-term health care cost between conventional treatment and bariatric surgery in patients with diabetes, according to a study published in the Lancet online Sept. 17.
Elevated body mass index is associated with an increased risk of diabetes. However, devising effective lifestyle interventions to reduce weight in the severely obese remains a challenge. Data from the Swedish Obese Subjects (SOS) study have demonstrated prevention and remission of type 2 diabetes after bariatric surgery.
Catherine Keating, Ph.D., of the Deakin Health Economics and Baker IDI Heart and Diabetes Institute in Melbourne, and her associates sought to quantify the health care costs during a 15-year period for obese patients treated with bariatric surgery versus conventional treatment.
Data on prescription drug costs were obtained by questionnaires from participants in the SOS study and the Swedish Prescribed Drug Register. The Swedish National Patient Register was used to obtain data on the outpatient and inpatient visits. The participants were followed for up to 15 years.
The original SOS study was a prospective study that compared treatment outcomes and costs in two groups of obese adults: those who underwent bariatric surgery versus a control cohort who received conventional obesity management. The participants ranged from 37 to 60 years old with BMIs of greater than 34 kg/m2 in men and greater than 38 in women. Conventional treatment included behavior modification, lifestyle intervention, or no treatment.
The definition of diabetes was based on a self-report of taking diabetes drugs or a fasting glucose measurement.
After exclusions, 4,030 participants were included; of these, 2,836 were euglycemic, 591 had prediabetes, and 603 were diabetic, the investigators reported (Lancet 2015 Sep 16 [doi: 10.1016/
S2213-8587(15)00290-9]).
Patients in the bariatric surgery groups were on average 6.2 kg heavier (P less than .0001) and 1.5 years younger (P less than .0001) than were the controls. After the 15-year follow-up, weight loss was 16 kg greater in the diabetes subgroup, 18 kg greater in the prediabetes subgroup, and 20 kg greater in the euglycemia subgroup who had bariatric surgery versus conventional treatment (P less than .0001 for all).
After 15 years, the aggregated drug costs were not different between the conventional treatment group and the bariatric surgery group in patients with euglycemia. However, drug costs were lower in the prediabetic participants who had surgery versus conventional treatment (P = .007). Similarly, patients with diabetes who underwent bariatric surgery incurred lower drug costs after 15 years (P less than .0001).
The inpatient hospital costs after 15 years were greater in the surgery group for all glucose levels versus conventional treatment (mean, $51,225 vs. $25,313; P less than .0001).
There were no differences in outpatient costs demonstrated between the glucose subgroups. However, in the diabetes group, there were wide confidence intervals associated with outpatient costs that were thought to be secondary to end-stage renal disease visits.
Finally, the total cost of health care for the euglycemic group was higher in those who underwent surgery versus conventional treatment (P less than .0001). The prediabetic subgroup also incurred a higher total health care cost for surgery versus conventional treatment (P less than .0001). However, there were no differences in total health care cost for patients with diabetes who had surgery versus conventional treatment ($88,572 vs. $79,967, P less than .090).
The total cost was also higher in patients with diabetes for more than 1 year who had surgical intervention versus those who got conventional treatment (P less than .011). However, patients with diabetes for less than 1 year did not show differences in total cost when treated with surgery versus conventional treatments (P less than .476)
“In this study, we show that for obese patients with type 2 diabetes, the upfront costs of bariatric surgery seem to be largely offset by prevention of future health care and drug use,” the authors wrote. In addition, “long-term health care cost results support prioritization of patients with obesity and type 2 diabetes for bariatric surgery.”
This study was supported by a grant from AFA Forsakring. The authors reported multiple disclosures.
Bariatric surgery should be considered, irrespective of body mas index, in patients whose diabetes is not under control, despite the use of medications and lifestyle interventions.
Since the start of the SOS study, bariatric surgery has changed, and present day surgical costs would be lower.
Dr. Ricardo Cohen is affiliated with the Center for Obesity and Diabetes in Sao Paulo, Brazil. These comments were taken from an accompanying editorial (Lancet 2015 Sep 16 [doi: 10.1016/S2213-8587(15)00320-4]). No conflicts of interests were declared.
Bariatric surgery should be considered, irrespective of body mas index, in patients whose diabetes is not under control, despite the use of medications and lifestyle interventions.
Since the start of the SOS study, bariatric surgery has changed, and present day surgical costs would be lower.
Dr. Ricardo Cohen is affiliated with the Center for Obesity and Diabetes in Sao Paulo, Brazil. These comments were taken from an accompanying editorial (Lancet 2015 Sep 16 [doi: 10.1016/S2213-8587(15)00320-4]). No conflicts of interests were declared.
Bariatric surgery should be considered, irrespective of body mas index, in patients whose diabetes is not under control, despite the use of medications and lifestyle interventions.
Since the start of the SOS study, bariatric surgery has changed, and present day surgical costs would be lower.
Dr. Ricardo Cohen is affiliated with the Center for Obesity and Diabetes in Sao Paulo, Brazil. These comments were taken from an accompanying editorial (Lancet 2015 Sep 16 [doi: 10.1016/S2213-8587(15)00320-4]). No conflicts of interests were declared.
There was no difference in long-term health care cost between conventional treatment and bariatric surgery in patients with diabetes, according to a study published in the Lancet online Sept. 17.
Elevated body mass index is associated with an increased risk of diabetes. However, devising effective lifestyle interventions to reduce weight in the severely obese remains a challenge. Data from the Swedish Obese Subjects (SOS) study have demonstrated prevention and remission of type 2 diabetes after bariatric surgery.
Catherine Keating, Ph.D., of the Deakin Health Economics and Baker IDI Heart and Diabetes Institute in Melbourne, and her associates sought to quantify the health care costs during a 15-year period for obese patients treated with bariatric surgery versus conventional treatment.
Data on prescription drug costs were obtained by questionnaires from participants in the SOS study and the Swedish Prescribed Drug Register. The Swedish National Patient Register was used to obtain data on the outpatient and inpatient visits. The participants were followed for up to 15 years.
The original SOS study was a prospective study that compared treatment outcomes and costs in two groups of obese adults: those who underwent bariatric surgery versus a control cohort who received conventional obesity management. The participants ranged from 37 to 60 years old with BMIs of greater than 34 kg/m2 in men and greater than 38 in women. Conventional treatment included behavior modification, lifestyle intervention, or no treatment.
The definition of diabetes was based on a self-report of taking diabetes drugs or a fasting glucose measurement.
After exclusions, 4,030 participants were included; of these, 2,836 were euglycemic, 591 had prediabetes, and 603 were diabetic, the investigators reported (Lancet 2015 Sep 16 [doi: 10.1016/
S2213-8587(15)00290-9]).
Patients in the bariatric surgery groups were on average 6.2 kg heavier (P less than .0001) and 1.5 years younger (P less than .0001) than were the controls. After the 15-year follow-up, weight loss was 16 kg greater in the diabetes subgroup, 18 kg greater in the prediabetes subgroup, and 20 kg greater in the euglycemia subgroup who had bariatric surgery versus conventional treatment (P less than .0001 for all).
After 15 years, the aggregated drug costs were not different between the conventional treatment group and the bariatric surgery group in patients with euglycemia. However, drug costs were lower in the prediabetic participants who had surgery versus conventional treatment (P = .007). Similarly, patients with diabetes who underwent bariatric surgery incurred lower drug costs after 15 years (P less than .0001).
The inpatient hospital costs after 15 years were greater in the surgery group for all glucose levels versus conventional treatment (mean, $51,225 vs. $25,313; P less than .0001).
There were no differences in outpatient costs demonstrated between the glucose subgroups. However, in the diabetes group, there were wide confidence intervals associated with outpatient costs that were thought to be secondary to end-stage renal disease visits.
Finally, the total cost of health care for the euglycemic group was higher in those who underwent surgery versus conventional treatment (P less than .0001). The prediabetic subgroup also incurred a higher total health care cost for surgery versus conventional treatment (P less than .0001). However, there were no differences in total health care cost for patients with diabetes who had surgery versus conventional treatment ($88,572 vs. $79,967, P less than .090).
The total cost was also higher in patients with diabetes for more than 1 year who had surgical intervention versus those who got conventional treatment (P less than .011). However, patients with diabetes for less than 1 year did not show differences in total cost when treated with surgery versus conventional treatments (P less than .476)
“In this study, we show that for obese patients with type 2 diabetes, the upfront costs of bariatric surgery seem to be largely offset by prevention of future health care and drug use,” the authors wrote. In addition, “long-term health care cost results support prioritization of patients with obesity and type 2 diabetes for bariatric surgery.”
This study was supported by a grant from AFA Forsakring. The authors reported multiple disclosures.
There was no difference in long-term health care cost between conventional treatment and bariatric surgery in patients with diabetes, according to a study published in the Lancet online Sept. 17.
Elevated body mass index is associated with an increased risk of diabetes. However, devising effective lifestyle interventions to reduce weight in the severely obese remains a challenge. Data from the Swedish Obese Subjects (SOS) study have demonstrated prevention and remission of type 2 diabetes after bariatric surgery.
Catherine Keating, Ph.D., of the Deakin Health Economics and Baker IDI Heart and Diabetes Institute in Melbourne, and her associates sought to quantify the health care costs during a 15-year period for obese patients treated with bariatric surgery versus conventional treatment.
Data on prescription drug costs were obtained by questionnaires from participants in the SOS study and the Swedish Prescribed Drug Register. The Swedish National Patient Register was used to obtain data on the outpatient and inpatient visits. The participants were followed for up to 15 years.
The original SOS study was a prospective study that compared treatment outcomes and costs in two groups of obese adults: those who underwent bariatric surgery versus a control cohort who received conventional obesity management. The participants ranged from 37 to 60 years old with BMIs of greater than 34 kg/m2 in men and greater than 38 in women. Conventional treatment included behavior modification, lifestyle intervention, or no treatment.
The definition of diabetes was based on a self-report of taking diabetes drugs or a fasting glucose measurement.
After exclusions, 4,030 participants were included; of these, 2,836 were euglycemic, 591 had prediabetes, and 603 were diabetic, the investigators reported (Lancet 2015 Sep 16 [doi: 10.1016/
S2213-8587(15)00290-9]).
Patients in the bariatric surgery groups were on average 6.2 kg heavier (P less than .0001) and 1.5 years younger (P less than .0001) than were the controls. After the 15-year follow-up, weight loss was 16 kg greater in the diabetes subgroup, 18 kg greater in the prediabetes subgroup, and 20 kg greater in the euglycemia subgroup who had bariatric surgery versus conventional treatment (P less than .0001 for all).
After 15 years, the aggregated drug costs were not different between the conventional treatment group and the bariatric surgery group in patients with euglycemia. However, drug costs were lower in the prediabetic participants who had surgery versus conventional treatment (P = .007). Similarly, patients with diabetes who underwent bariatric surgery incurred lower drug costs after 15 years (P less than .0001).
The inpatient hospital costs after 15 years were greater in the surgery group for all glucose levels versus conventional treatment (mean, $51,225 vs. $25,313; P less than .0001).
There were no differences in outpatient costs demonstrated between the glucose subgroups. However, in the diabetes group, there were wide confidence intervals associated with outpatient costs that were thought to be secondary to end-stage renal disease visits.
Finally, the total cost of health care for the euglycemic group was higher in those who underwent surgery versus conventional treatment (P less than .0001). The prediabetic subgroup also incurred a higher total health care cost for surgery versus conventional treatment (P less than .0001). However, there were no differences in total health care cost for patients with diabetes who had surgery versus conventional treatment ($88,572 vs. $79,967, P less than .090).
The total cost was also higher in patients with diabetes for more than 1 year who had surgical intervention versus those who got conventional treatment (P less than .011). However, patients with diabetes for less than 1 year did not show differences in total cost when treated with surgery versus conventional treatments (P less than .476)
“In this study, we show that for obese patients with type 2 diabetes, the upfront costs of bariatric surgery seem to be largely offset by prevention of future health care and drug use,” the authors wrote. In addition, “long-term health care cost results support prioritization of patients with obesity and type 2 diabetes for bariatric surgery.”
This study was supported by a grant from AFA Forsakring. The authors reported multiple disclosures.
THE LANCET
Key clinical point: There was no difference in long-term health care cost between conventional treatment and bariatric surgery in patients with diabetes.
Major finding: There was no difference in total health care cost for patients with diabetes who received surgery versus conventional treatment ($88,572 vs. $79,967, P = .090).
Data source: A 15-year follow-up of Swedish Obese Subjects study participants with additional data obtained on drug costs and inpatient and outpatient visits.
Disclosures: This study was supported by a grant from AFA Forsakring. The authors reported multiple disclosures.
ESC: Noncardiac surgery in HCM patients warrants special attention
LONDON – Hypertrophic cardiomyopathy patients undergoing noncardiac surgery posted significantly worse 30-day composite outcomes than did closely matched controls undergoing the same sorts of surgical procedures.
“Our recommendation is that when hypertrophic cardiomyopathy patients need noncardiac surgery they should be evaluated and treated at an experienced center,” Dr. Milind Y. Desai concluded at the annual congress of the European Society of Cardiology.
There is a dearth of data on outcomes of noncardiac surgery in patients with hypertrophic cardiomyopathy (HCM). This was the impetus for Dr. Desai and his coinvestigators at the Cleveland Clinic to conduct a case-control study involving 92 consecutive adults with HCM undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 controls matched for age, gender, and type of surgery. Enrollment was restricted to HCM patients who hadn’t previously undergone septal myectomy or alcohol ablation.
The primary outcome was the 30-day composite of postoperative death, MI, stroke, or heart failure. The incidence was 10% in the HCM group, significantly greater than the 3% rate in controls. Moreover, 4% of HCM patients developed postoperative atrial fibrillation, compared with none of the controls. Three deaths occurred among the 92 HCM patients, an incidence twice that in the control group.
The special challenge of noncardiac surgery in HCM patients is that their heart condition is characterized by systolic anterior motion of the mitral valve, dynamic left ventricular outflow tract obstruction, diastolic dysfunction, and mitral regurgitation. The rapid blood pressure and fluid shifts that occur during noncardiac surgery require special attention in such patients, Dr. Desai observed.
The HCM patients in this series received such attention, he added. They were more likely than controls to be on beta-blocker therapy at surgery, they received lower doses of ephedrine intraoperatively so as to avoid aggravating outflow tract obstruction, and they spent half as much time as controls with a systolic blood pressure below 90 mm Hg or a heart rate greater than 100 bpm.
“Care was taken to make sure these patients did not decompensate,” he noted.
Dr. Desai reported no financial conflicts regarding this study, conducted free of commercial support.
LONDON – Hypertrophic cardiomyopathy patients undergoing noncardiac surgery posted significantly worse 30-day composite outcomes than did closely matched controls undergoing the same sorts of surgical procedures.
“Our recommendation is that when hypertrophic cardiomyopathy patients need noncardiac surgery they should be evaluated and treated at an experienced center,” Dr. Milind Y. Desai concluded at the annual congress of the European Society of Cardiology.
There is a dearth of data on outcomes of noncardiac surgery in patients with hypertrophic cardiomyopathy (HCM). This was the impetus for Dr. Desai and his coinvestigators at the Cleveland Clinic to conduct a case-control study involving 92 consecutive adults with HCM undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 controls matched for age, gender, and type of surgery. Enrollment was restricted to HCM patients who hadn’t previously undergone septal myectomy or alcohol ablation.
The primary outcome was the 30-day composite of postoperative death, MI, stroke, or heart failure. The incidence was 10% in the HCM group, significantly greater than the 3% rate in controls. Moreover, 4% of HCM patients developed postoperative atrial fibrillation, compared with none of the controls. Three deaths occurred among the 92 HCM patients, an incidence twice that in the control group.
The special challenge of noncardiac surgery in HCM patients is that their heart condition is characterized by systolic anterior motion of the mitral valve, dynamic left ventricular outflow tract obstruction, diastolic dysfunction, and mitral regurgitation. The rapid blood pressure and fluid shifts that occur during noncardiac surgery require special attention in such patients, Dr. Desai observed.
The HCM patients in this series received such attention, he added. They were more likely than controls to be on beta-blocker therapy at surgery, they received lower doses of ephedrine intraoperatively so as to avoid aggravating outflow tract obstruction, and they spent half as much time as controls with a systolic blood pressure below 90 mm Hg or a heart rate greater than 100 bpm.
“Care was taken to make sure these patients did not decompensate,” he noted.
Dr. Desai reported no financial conflicts regarding this study, conducted free of commercial support.
LONDON – Hypertrophic cardiomyopathy patients undergoing noncardiac surgery posted significantly worse 30-day composite outcomes than did closely matched controls undergoing the same sorts of surgical procedures.
“Our recommendation is that when hypertrophic cardiomyopathy patients need noncardiac surgery they should be evaluated and treated at an experienced center,” Dr. Milind Y. Desai concluded at the annual congress of the European Society of Cardiology.
There is a dearth of data on outcomes of noncardiac surgery in patients with hypertrophic cardiomyopathy (HCM). This was the impetus for Dr. Desai and his coinvestigators at the Cleveland Clinic to conduct a case-control study involving 92 consecutive adults with HCM undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 controls matched for age, gender, and type of surgery. Enrollment was restricted to HCM patients who hadn’t previously undergone septal myectomy or alcohol ablation.
The primary outcome was the 30-day composite of postoperative death, MI, stroke, or heart failure. The incidence was 10% in the HCM group, significantly greater than the 3% rate in controls. Moreover, 4% of HCM patients developed postoperative atrial fibrillation, compared with none of the controls. Three deaths occurred among the 92 HCM patients, an incidence twice that in the control group.
The special challenge of noncardiac surgery in HCM patients is that their heart condition is characterized by systolic anterior motion of the mitral valve, dynamic left ventricular outflow tract obstruction, diastolic dysfunction, and mitral regurgitation. The rapid blood pressure and fluid shifts that occur during noncardiac surgery require special attention in such patients, Dr. Desai observed.
The HCM patients in this series received such attention, he added. They were more likely than controls to be on beta-blocker therapy at surgery, they received lower doses of ephedrine intraoperatively so as to avoid aggravating outflow tract obstruction, and they spent half as much time as controls with a systolic blood pressure below 90 mm Hg or a heart rate greater than 100 bpm.
“Care was taken to make sure these patients did not decompensate,” he noted.
Dr. Desai reported no financial conflicts regarding this study, conducted free of commercial support.
AT THE ESC CONGRESS 2015
Key clinical point: Hypertrophic cardiomyopathy patients undergoing noncardiac surgery have significantly worse outcomes than do matched controls undergoing similar operations.
Major finding: The 30-day composite endpoint of death, MI, stroke, or heart failure occurred in 10% of hypertrophic cardiomyopathy patients who underwent noncardiac surgery, compared with 3% of matched controls.
Data source: A case-control study comparing 30-day outcomes in 92 consecutive hypertrophic cardiomyopathy patients undergoing intermediate- or high-cardiovascular-risk noncardiac surgery and 184 matched controls.
Disclosures: This study was conducted free of commercial support, and the presenter reported having no financial conflicts.
White board in the OR adds a layer of safety
NEW YORK – Displaying a low-tech, low-cost white board in the operating room during the “time out” before surgery can significantly improve memory retention among members of the surgical team, a new study suggests.
“We found that providing a white board that you can buy at any office supply store gives a visual stimulus on top of the verbal stimulus [that] improves retention of important information,” Dr. Aryan Meknat, the study author, said at the annual Minimally Invasive Surgery Week.
A surgical pause or “time out” performed before any operative procedure is a major component of the Joint Commission’s Universal Protocol to prevent wrong site, wrong procedure, and wrong person surgery. Retention of information presented during the surgical pause is essential, at the beginning of the case and for the duration of the procedure, he said.
During the study, surgical teams were randomly divided into two groups: in the first group, 30 team members were given information verbally during the surgical pause; while a second group of 29 team members was provided with verbal information that was read from the white board. The white board was displayed in the operating room throughout the surgical procedure for the second group.
After the conclusion of the procedure, the white board was removed and both groups were given a short written questionnaire. Each team was tested only once in order to keep the study blinded. Also, participants had no prior knowledge that they would be tested after the procedure.
Study participants were asked to recall several facts about the patient, including the patient’s first and last name, age, sex, weight, site of IV placement, allergies, medications, relation of accompanying guardian, and the signature on the consent form.
Team members in the first study group answered a total of 300 questions, and 200 questions (66.7%) were correctly answered. Participants in the second group – which used the white board – answered 290 questions, and 239 (82.4%) were correctly answered. The white board group had a 23.6% overall increase in correctly answered questions. The difference between retention in the two groups was statistically significant (P less than .05) in every category tested.
“These findings apply to operating rooms everywhere, especially in cases where there may be long delays before starting the procedure, changes in anesthesia midcase, situations where two procedures are scheduled in one patient, or in intraoperative emergency situations. We need to be sure that the surgical team retains information, as well as [listens] to verbal instructions,” said Dr. Meknat of MobiSurg, a mobile surgical unit based in Laguna Hills, Calif.
Dr. Meknat reported having no financial disclosures.
NEW YORK – Displaying a low-tech, low-cost white board in the operating room during the “time out” before surgery can significantly improve memory retention among members of the surgical team, a new study suggests.
“We found that providing a white board that you can buy at any office supply store gives a visual stimulus on top of the verbal stimulus [that] improves retention of important information,” Dr. Aryan Meknat, the study author, said at the annual Minimally Invasive Surgery Week.
A surgical pause or “time out” performed before any operative procedure is a major component of the Joint Commission’s Universal Protocol to prevent wrong site, wrong procedure, and wrong person surgery. Retention of information presented during the surgical pause is essential, at the beginning of the case and for the duration of the procedure, he said.
During the study, surgical teams were randomly divided into two groups: in the first group, 30 team members were given information verbally during the surgical pause; while a second group of 29 team members was provided with verbal information that was read from the white board. The white board was displayed in the operating room throughout the surgical procedure for the second group.
After the conclusion of the procedure, the white board was removed and both groups were given a short written questionnaire. Each team was tested only once in order to keep the study blinded. Also, participants had no prior knowledge that they would be tested after the procedure.
Study participants were asked to recall several facts about the patient, including the patient’s first and last name, age, sex, weight, site of IV placement, allergies, medications, relation of accompanying guardian, and the signature on the consent form.
Team members in the first study group answered a total of 300 questions, and 200 questions (66.7%) were correctly answered. Participants in the second group – which used the white board – answered 290 questions, and 239 (82.4%) were correctly answered. The white board group had a 23.6% overall increase in correctly answered questions. The difference between retention in the two groups was statistically significant (P less than .05) in every category tested.
“These findings apply to operating rooms everywhere, especially in cases where there may be long delays before starting the procedure, changes in anesthesia midcase, situations where two procedures are scheduled in one patient, or in intraoperative emergency situations. We need to be sure that the surgical team retains information, as well as [listens] to verbal instructions,” said Dr. Meknat of MobiSurg, a mobile surgical unit based in Laguna Hills, Calif.
Dr. Meknat reported having no financial disclosures.
NEW YORK – Displaying a low-tech, low-cost white board in the operating room during the “time out” before surgery can significantly improve memory retention among members of the surgical team, a new study suggests.
“We found that providing a white board that you can buy at any office supply store gives a visual stimulus on top of the verbal stimulus [that] improves retention of important information,” Dr. Aryan Meknat, the study author, said at the annual Minimally Invasive Surgery Week.
A surgical pause or “time out” performed before any operative procedure is a major component of the Joint Commission’s Universal Protocol to prevent wrong site, wrong procedure, and wrong person surgery. Retention of information presented during the surgical pause is essential, at the beginning of the case and for the duration of the procedure, he said.
During the study, surgical teams were randomly divided into two groups: in the first group, 30 team members were given information verbally during the surgical pause; while a second group of 29 team members was provided with verbal information that was read from the white board. The white board was displayed in the operating room throughout the surgical procedure for the second group.
After the conclusion of the procedure, the white board was removed and both groups were given a short written questionnaire. Each team was tested only once in order to keep the study blinded. Also, participants had no prior knowledge that they would be tested after the procedure.
Study participants were asked to recall several facts about the patient, including the patient’s first and last name, age, sex, weight, site of IV placement, allergies, medications, relation of accompanying guardian, and the signature on the consent form.
Team members in the first study group answered a total of 300 questions, and 200 questions (66.7%) were correctly answered. Participants in the second group – which used the white board – answered 290 questions, and 239 (82.4%) were correctly answered. The white board group had a 23.6% overall increase in correctly answered questions. The difference between retention in the two groups was statistically significant (P less than .05) in every category tested.
“These findings apply to operating rooms everywhere, especially in cases where there may be long delays before starting the procedure, changes in anesthesia midcase, situations where two procedures are scheduled in one patient, or in intraoperative emergency situations. We need to be sure that the surgical team retains information, as well as [listens] to verbal instructions,” said Dr. Meknat of MobiSurg, a mobile surgical unit based in Laguna Hills, Calif.
Dr. Meknat reported having no financial disclosures.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Displaying a white board during the “time out” before surgery significantly improves memory retention.
Major finding: Surgical team members using a white board achieved a 23.6% improvement in recall of patient information after surgery.
Data source: A prospective blinded study of 59 surgical team members.
Disclosures: Dr. Meknat reported having no financial disclosures.
Postop delirium heightens risk of other dangerous complications
Delirium is not only the most common major complication of elective surgery in older adults, it also markedly raises the risk of all adverse outcomes, including prolonged length of stay, discharge to an institution rather than home, and readmission within 30 days, according to a report published online Sept. 9 in JAMA Surgery.
“Given its high prevalence and negative effect, delirium should be considered as the leading postoperative complication contributing to adverse outcomes” in this patient population, wrote Dr. Lauren J. Gleason of the department of medicine at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her associates.
Delirium is typically considered a less serious event than other major postoperative complications, even though its association with higher in-hospital mortality, 6-month mortality, functional decline, and higher health care costs has been well documented. To assess whether delirium should be considered equivalent to other major life-altering or life-threatening complications, the investigators studied 566 patients aged 70 years and older who underwent elective orthopedic, general, or vascular procedures at Beth Israel Deaconess or Brigham and Women’s Hospital in a 3-year period. The data were collected for the Successful Aging after Elective Surgery (SAGES) study.
Operations included total hip or knee replacement, lumbar or cervical laminectomy, lower-extremity bypass, open abdominal aortic aneurysm repair, open colectomyt, and laparoscopic colectomy. In general, these patients were highly functional and highly educated. The mean age was 76.7 years, and 93% of the study participants were white.
Delirium developed in 135 patients (24%) – much more frequently than all other major complications combined (47 patients, or 8%). This is comparable with rates of delirium reported in other studies of elective noncardiac surgeries, Dr. Gleason and her associates noted. Other major complications included unstable arrhythmias, respiratory failure, abscess requiring incision and drainage, abdominal compartment syndrome, anastomotic leak, deep surgical site infection, and hernia repair.
Compared with patients who didn’t develop delirium, those who did had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission, the investigators reported (JAMA Surg. 2015 Sept 9. doi: 10.1001/jamasurg.2015.2606).
Since delirium is often preventable, clinicians should try harder to implement preventive strategies before surgery and continue them afterward. The Hospital Elder Life Program, proactive geriatric consultation, and comanagement services all have proved effective in this regard, they added.
This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation. The authors reported no relevant disclosures.
Delirium is not only the most common major complication of elective surgery in older adults, it also markedly raises the risk of all adverse outcomes, including prolonged length of stay, discharge to an institution rather than home, and readmission within 30 days, according to a report published online Sept. 9 in JAMA Surgery.
“Given its high prevalence and negative effect, delirium should be considered as the leading postoperative complication contributing to adverse outcomes” in this patient population, wrote Dr. Lauren J. Gleason of the department of medicine at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her associates.
Delirium is typically considered a less serious event than other major postoperative complications, even though its association with higher in-hospital mortality, 6-month mortality, functional decline, and higher health care costs has been well documented. To assess whether delirium should be considered equivalent to other major life-altering or life-threatening complications, the investigators studied 566 patients aged 70 years and older who underwent elective orthopedic, general, or vascular procedures at Beth Israel Deaconess or Brigham and Women’s Hospital in a 3-year period. The data were collected for the Successful Aging after Elective Surgery (SAGES) study.
Operations included total hip or knee replacement, lumbar or cervical laminectomy, lower-extremity bypass, open abdominal aortic aneurysm repair, open colectomyt, and laparoscopic colectomy. In general, these patients were highly functional and highly educated. The mean age was 76.7 years, and 93% of the study participants were white.
Delirium developed in 135 patients (24%) – much more frequently than all other major complications combined (47 patients, or 8%). This is comparable with rates of delirium reported in other studies of elective noncardiac surgeries, Dr. Gleason and her associates noted. Other major complications included unstable arrhythmias, respiratory failure, abscess requiring incision and drainage, abdominal compartment syndrome, anastomotic leak, deep surgical site infection, and hernia repair.
Compared with patients who didn’t develop delirium, those who did had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission, the investigators reported (JAMA Surg. 2015 Sept 9. doi: 10.1001/jamasurg.2015.2606).
Since delirium is often preventable, clinicians should try harder to implement preventive strategies before surgery and continue them afterward. The Hospital Elder Life Program, proactive geriatric consultation, and comanagement services all have proved effective in this regard, they added.
This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation. The authors reported no relevant disclosures.
Delirium is not only the most common major complication of elective surgery in older adults, it also markedly raises the risk of all adverse outcomes, including prolonged length of stay, discharge to an institution rather than home, and readmission within 30 days, according to a report published online Sept. 9 in JAMA Surgery.
“Given its high prevalence and negative effect, delirium should be considered as the leading postoperative complication contributing to adverse outcomes” in this patient population, wrote Dr. Lauren J. Gleason of the department of medicine at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her associates.
Delirium is typically considered a less serious event than other major postoperative complications, even though its association with higher in-hospital mortality, 6-month mortality, functional decline, and higher health care costs has been well documented. To assess whether delirium should be considered equivalent to other major life-altering or life-threatening complications, the investigators studied 566 patients aged 70 years and older who underwent elective orthopedic, general, or vascular procedures at Beth Israel Deaconess or Brigham and Women’s Hospital in a 3-year period. The data were collected for the Successful Aging after Elective Surgery (SAGES) study.
Operations included total hip or knee replacement, lumbar or cervical laminectomy, lower-extremity bypass, open abdominal aortic aneurysm repair, open colectomyt, and laparoscopic colectomy. In general, these patients were highly functional and highly educated. The mean age was 76.7 years, and 93% of the study participants were white.
Delirium developed in 135 patients (24%) – much more frequently than all other major complications combined (47 patients, or 8%). This is comparable with rates of delirium reported in other studies of elective noncardiac surgeries, Dr. Gleason and her associates noted. Other major complications included unstable arrhythmias, respiratory failure, abscess requiring incision and drainage, abdominal compartment syndrome, anastomotic leak, deep surgical site infection, and hernia repair.
Compared with patients who didn’t develop delirium, those who did had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission, the investigators reported (JAMA Surg. 2015 Sept 9. doi: 10.1001/jamasurg.2015.2606).
Since delirium is often preventable, clinicians should try harder to implement preventive strategies before surgery and continue them afterward. The Hospital Elder Life Program, proactive geriatric consultation, and comanagement services all have proved effective in this regard, they added.
This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation. The authors reported no relevant disclosures.
FROM JAMA SURGERY
Key clinical point: Delirium is the most common and among the most harmful of complications of elective surgery in older adults.
Major finding: Elderly patients who developed delirium had a twofold higher risk of prolonged length of stay, a 50% higher risk of discharge to an institution, and more than double the risk of 30-day readmission.
Data source: A prospective cohort study involving 566 older adults undergoing elective surgery at two hospitals in a 3-year period.
Disclosures: This study was supported by the National Institute on Aging, the Health and Resources Services Administration, and the John A. Hartford Foundation.
VIDEO: Consistency is key to monitoring patients on opioids
ORLANDO – Take a consistent approach with all patients on opioid therapy, regardless of a patient’s perceived potential for abuse, Dr. Melissa B. Weimer advised.
“This is an area of medicine where I feel we need to apply universal precautions to all patients,” noted Dr. Weimer, assistant professor of medicine, Oregon Health and Science University, Portland. “We’re treating all patients as at some level of potential harm from this medication.”
In an interview at a meeting held by the American Pain Society and Global Academy for Medical Education, Dr. Weimer outlined a strategy that employs the same protocol to monitor therapy, even when the abuse potential is considered to be low.
Global Academy and this news organization are owned by the same company. Dr. Weimer reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Take a consistent approach with all patients on opioid therapy, regardless of a patient’s perceived potential for abuse, Dr. Melissa B. Weimer advised.
“This is an area of medicine where I feel we need to apply universal precautions to all patients,” noted Dr. Weimer, assistant professor of medicine, Oregon Health and Science University, Portland. “We’re treating all patients as at some level of potential harm from this medication.”
In an interview at a meeting held by the American Pain Society and Global Academy for Medical Education, Dr. Weimer outlined a strategy that employs the same protocol to monitor therapy, even when the abuse potential is considered to be low.
Global Academy and this news organization are owned by the same company. Dr. Weimer reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – Take a consistent approach with all patients on opioid therapy, regardless of a patient’s perceived potential for abuse, Dr. Melissa B. Weimer advised.
“This is an area of medicine where I feel we need to apply universal precautions to all patients,” noted Dr. Weimer, assistant professor of medicine, Oregon Health and Science University, Portland. “We’re treating all patients as at some level of potential harm from this medication.”
In an interview at a meeting held by the American Pain Society and Global Academy for Medical Education, Dr. Weimer outlined a strategy that employs the same protocol to monitor therapy, even when the abuse potential is considered to be low.
Global Academy and this news organization are owned by the same company. Dr. Weimer reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM PAIN CARE FOR PRIMARY CARE
Prescription opioid overdoses targeted in new CDC program
The Centers for Disease Control and Prevention has launched a program aimed at helping states combat and prevent opioid drug overdoses.
The Prescription Drug Overdose: Prevention for States program will be launching in 16 states chosen in a competitive application process. The CDC is committing $20 million in fiscal year 2015, and each state will receive $750,000 to $1 million each year for the next 4 years to advance prevention in several areas, such as enhancing prescription drug–monitoring programs, putting prevention into action in communities nationwide, and investigating the connection between prescription opioid abuse and heroin use, the CDC said in a press release.
In 2013, 16,000 people died from prescription opioid overdoses, four times more than in 1999, with prescription of opioids increasing at the same rate over the same time. Despite more opioids being prescribed, the amount of pain Americans report has not changed. In addition, heroin deaths also have spiked, with the 8,000 heroin overdose deaths nearly three times as many as in 2010.
“The prescription drug overdose epidemic requires a multifaceted approach, and states are key partners in our efforts on the front lines to prevent overdose deaths. With this funding, states can improve their ability to track the problem, work with insurers to help providers make informed prescribing decisions, and take action to combat this epidemic,” U.S. Department of Health & Human Services Secretary Sylvia M. Burwell said in the release.
Find the full CDC press release here.
The Centers for Disease Control and Prevention has launched a program aimed at helping states combat and prevent opioid drug overdoses.
The Prescription Drug Overdose: Prevention for States program will be launching in 16 states chosen in a competitive application process. The CDC is committing $20 million in fiscal year 2015, and each state will receive $750,000 to $1 million each year for the next 4 years to advance prevention in several areas, such as enhancing prescription drug–monitoring programs, putting prevention into action in communities nationwide, and investigating the connection between prescription opioid abuse and heroin use, the CDC said in a press release.
In 2013, 16,000 people died from prescription opioid overdoses, four times more than in 1999, with prescription of opioids increasing at the same rate over the same time. Despite more opioids being prescribed, the amount of pain Americans report has not changed. In addition, heroin deaths also have spiked, with the 8,000 heroin overdose deaths nearly three times as many as in 2010.
“The prescription drug overdose epidemic requires a multifaceted approach, and states are key partners in our efforts on the front lines to prevent overdose deaths. With this funding, states can improve their ability to track the problem, work with insurers to help providers make informed prescribing decisions, and take action to combat this epidemic,” U.S. Department of Health & Human Services Secretary Sylvia M. Burwell said in the release.
Find the full CDC press release here.
The Centers for Disease Control and Prevention has launched a program aimed at helping states combat and prevent opioid drug overdoses.
The Prescription Drug Overdose: Prevention for States program will be launching in 16 states chosen in a competitive application process. The CDC is committing $20 million in fiscal year 2015, and each state will receive $750,000 to $1 million each year for the next 4 years to advance prevention in several areas, such as enhancing prescription drug–monitoring programs, putting prevention into action in communities nationwide, and investigating the connection between prescription opioid abuse and heroin use, the CDC said in a press release.
In 2013, 16,000 people died from prescription opioid overdoses, four times more than in 1999, with prescription of opioids increasing at the same rate over the same time. Despite more opioids being prescribed, the amount of pain Americans report has not changed. In addition, heroin deaths also have spiked, with the 8,000 heroin overdose deaths nearly three times as many as in 2010.
“The prescription drug overdose epidemic requires a multifaceted approach, and states are key partners in our efforts on the front lines to prevent overdose deaths. With this funding, states can improve their ability to track the problem, work with insurers to help providers make informed prescribing decisions, and take action to combat this epidemic,” U.S. Department of Health & Human Services Secretary Sylvia M. Burwell said in the release.
Find the full CDC press release here.