User login
Four-antigen vaccine boosts S. aureus antibodies
PHILADELPHIA – A single injection of the investigational 4-antigen SA4Ag vaccine was well tolerated and induced robust antibody responses against Staphylococcusaureus in healthy adults in a phase I/II study.
“The very quick development of antibodies suggest that the vaccine could be used pre-operatively [2-3 weeks] for elective surgeries that are at higher risk of Staph. infection, such as thoracotomy or insertion of rods for scoliosis or spinal fusion,” Dr. Robert W. Frenck Jr. said in an interview at Infectious Diseases Week 2014.
As to the durability of responses, antibody levels for all four antigens in the vaccine rose rapidly and then decayed slowly over the next 12 months, he said. “The results support the continued development of SA4Ag for the prevention of invasive S. aureus disease in at-risk adults, including those undergoing elective surgery.”
There is no licensed vaccine that prevents invasive S. aureus infection, although several multi-antigen vaccines are in development.
SA4Ag vaccine is a second-generation vaccine to Pfizer’s 3-antigen SA3AG candidate vaccine and was granted Fast Track designation by the U.S. Food and Drug Administration in February 2014, according to the manufacturer.
SA4Ag contains capsular polysaccharides serotypes 5 and 8 (CP5 and CP8) individually conjugated to CRM₁₉₇, a recombinant surface protein clumping factor A (rmClfA), with a recombinant manganese transporter protein C known as rP305A. Each component was selected based on the virulence of these antigens in S. aureus infections, Dr. Frenck Jr., professor of pediatrics and interim director of infectious diseases, at Cincinnati (Ohio) Children’s Hospital Medical Center, said.
The study stratified 456 healthy adults by age (18-49 years and 50-64 years) and then randomly assigned them to receive a single injection of placebo or one of three formulations of SA4Ag: fixed doses of 30 μg CP5-CRM₁₉₇, 30 μg CP8-CRM₁₉₇, and 60 μg rmClfA, and either a low- (20 μg), mid- (60 μg), or high- (200 μg) rP305A dose.
The participants average age was 45 years, 57% were female, 73% were white, and 87.5% completed the study through month 12.
Local reactions reported through day 14 were mild or moderate, and systemic events and other adverse events were comparable across all groups, Dr. Frenck Jr. said. No vaccine-related serious adverse events or deaths were reported.
At day 29, all participants vaccinated with SA4Ag achieved the CP5 opsonophagocytic activity (OPA) threshold (≥ 1,000 titers) and 96%–99% met the CP8 OPA threshold (≥ 2,000 titers).
“The percentage of subjects reaching the threshold is equivalent for each one of the vaccine doses, indicating that the rP305A did not affect the immune response to the other components in the vaccine,” Dr. Frenck Jr. said.
Less than 25% of patients given placebo achieved the CP5 or CP8 OPA thresholds.
Immune responses to ClfA were robust by day 15 and did not vary by the dose of rP305A, again suggesting that rP305A does not affect the other three antigens in the vaccine, he observed.
Immune responses to the rP305A antigen were dose dependent, with the percentage of patients with a threshold response increasing step-wise from the low (47%), mid (63.2%), and high (83%) doses.
By day 29, there was a very brisk rise in geometric mean titers for CP5. Responses did not differ by rP305A dose or across age groups, with a similar pattern observed for CP8 and ClfA, Dr. Fenck Jr. said.
Session co-moderator Dr. Walter Orenstein, from Emory University in Atlanta, commented that the rate of decay post-vaccination was promising, particularly compared with that observed with meningococcal vaccines.
The vaccine “program is exciting because it not only relies on just antibody, but it actually looks at functional responses and those functional responses have some correlate with protection against staphylococcal disease,” he said in an interview. High-risk populations, like renal dialysis patients, were not studied and it would be interesting to see how well they would respond. “Previous studies have shown transient benefits for those types of populations.”
PHILADELPHIA – A single injection of the investigational 4-antigen SA4Ag vaccine was well tolerated and induced robust antibody responses against Staphylococcusaureus in healthy adults in a phase I/II study.
“The very quick development of antibodies suggest that the vaccine could be used pre-operatively [2-3 weeks] for elective surgeries that are at higher risk of Staph. infection, such as thoracotomy or insertion of rods for scoliosis or spinal fusion,” Dr. Robert W. Frenck Jr. said in an interview at Infectious Diseases Week 2014.
As to the durability of responses, antibody levels for all four antigens in the vaccine rose rapidly and then decayed slowly over the next 12 months, he said. “The results support the continued development of SA4Ag for the prevention of invasive S. aureus disease in at-risk adults, including those undergoing elective surgery.”
There is no licensed vaccine that prevents invasive S. aureus infection, although several multi-antigen vaccines are in development.
SA4Ag vaccine is a second-generation vaccine to Pfizer’s 3-antigen SA3AG candidate vaccine and was granted Fast Track designation by the U.S. Food and Drug Administration in February 2014, according to the manufacturer.
SA4Ag contains capsular polysaccharides serotypes 5 and 8 (CP5 and CP8) individually conjugated to CRM₁₉₇, a recombinant surface protein clumping factor A (rmClfA), with a recombinant manganese transporter protein C known as rP305A. Each component was selected based on the virulence of these antigens in S. aureus infections, Dr. Frenck Jr., professor of pediatrics and interim director of infectious diseases, at Cincinnati (Ohio) Children’s Hospital Medical Center, said.
The study stratified 456 healthy adults by age (18-49 years and 50-64 years) and then randomly assigned them to receive a single injection of placebo or one of three formulations of SA4Ag: fixed doses of 30 μg CP5-CRM₁₉₇, 30 μg CP8-CRM₁₉₇, and 60 μg rmClfA, and either a low- (20 μg), mid- (60 μg), or high- (200 μg) rP305A dose.
The participants average age was 45 years, 57% were female, 73% were white, and 87.5% completed the study through month 12.
Local reactions reported through day 14 were mild or moderate, and systemic events and other adverse events were comparable across all groups, Dr. Frenck Jr. said. No vaccine-related serious adverse events or deaths were reported.
At day 29, all participants vaccinated with SA4Ag achieved the CP5 opsonophagocytic activity (OPA) threshold (≥ 1,000 titers) and 96%–99% met the CP8 OPA threshold (≥ 2,000 titers).
“The percentage of subjects reaching the threshold is equivalent for each one of the vaccine doses, indicating that the rP305A did not affect the immune response to the other components in the vaccine,” Dr. Frenck Jr. said.
Less than 25% of patients given placebo achieved the CP5 or CP8 OPA thresholds.
Immune responses to ClfA were robust by day 15 and did not vary by the dose of rP305A, again suggesting that rP305A does not affect the other three antigens in the vaccine, he observed.
Immune responses to the rP305A antigen were dose dependent, with the percentage of patients with a threshold response increasing step-wise from the low (47%), mid (63.2%), and high (83%) doses.
By day 29, there was a very brisk rise in geometric mean titers for CP5. Responses did not differ by rP305A dose or across age groups, with a similar pattern observed for CP8 and ClfA, Dr. Fenck Jr. said.
Session co-moderator Dr. Walter Orenstein, from Emory University in Atlanta, commented that the rate of decay post-vaccination was promising, particularly compared with that observed with meningococcal vaccines.
The vaccine “program is exciting because it not only relies on just antibody, but it actually looks at functional responses and those functional responses have some correlate with protection against staphylococcal disease,” he said in an interview. High-risk populations, like renal dialysis patients, were not studied and it would be interesting to see how well they would respond. “Previous studies have shown transient benefits for those types of populations.”
PHILADELPHIA – A single injection of the investigational 4-antigen SA4Ag vaccine was well tolerated and induced robust antibody responses against Staphylococcusaureus in healthy adults in a phase I/II study.
“The very quick development of antibodies suggest that the vaccine could be used pre-operatively [2-3 weeks] for elective surgeries that are at higher risk of Staph. infection, such as thoracotomy or insertion of rods for scoliosis or spinal fusion,” Dr. Robert W. Frenck Jr. said in an interview at Infectious Diseases Week 2014.
As to the durability of responses, antibody levels for all four antigens in the vaccine rose rapidly and then decayed slowly over the next 12 months, he said. “The results support the continued development of SA4Ag for the prevention of invasive S. aureus disease in at-risk adults, including those undergoing elective surgery.”
There is no licensed vaccine that prevents invasive S. aureus infection, although several multi-antigen vaccines are in development.
SA4Ag vaccine is a second-generation vaccine to Pfizer’s 3-antigen SA3AG candidate vaccine and was granted Fast Track designation by the U.S. Food and Drug Administration in February 2014, according to the manufacturer.
SA4Ag contains capsular polysaccharides serotypes 5 and 8 (CP5 and CP8) individually conjugated to CRM₁₉₇, a recombinant surface protein clumping factor A (rmClfA), with a recombinant manganese transporter protein C known as rP305A. Each component was selected based on the virulence of these antigens in S. aureus infections, Dr. Frenck Jr., professor of pediatrics and interim director of infectious diseases, at Cincinnati (Ohio) Children’s Hospital Medical Center, said.
The study stratified 456 healthy adults by age (18-49 years and 50-64 years) and then randomly assigned them to receive a single injection of placebo or one of three formulations of SA4Ag: fixed doses of 30 μg CP5-CRM₁₉₇, 30 μg CP8-CRM₁₉₇, and 60 μg rmClfA, and either a low- (20 μg), mid- (60 μg), or high- (200 μg) rP305A dose.
The participants average age was 45 years, 57% were female, 73% were white, and 87.5% completed the study through month 12.
Local reactions reported through day 14 were mild or moderate, and systemic events and other adverse events were comparable across all groups, Dr. Frenck Jr. said. No vaccine-related serious adverse events or deaths were reported.
At day 29, all participants vaccinated with SA4Ag achieved the CP5 opsonophagocytic activity (OPA) threshold (≥ 1,000 titers) and 96%–99% met the CP8 OPA threshold (≥ 2,000 titers).
“The percentage of subjects reaching the threshold is equivalent for each one of the vaccine doses, indicating that the rP305A did not affect the immune response to the other components in the vaccine,” Dr. Frenck Jr. said.
Less than 25% of patients given placebo achieved the CP5 or CP8 OPA thresholds.
Immune responses to ClfA were robust by day 15 and did not vary by the dose of rP305A, again suggesting that rP305A does not affect the other three antigens in the vaccine, he observed.
Immune responses to the rP305A antigen were dose dependent, with the percentage of patients with a threshold response increasing step-wise from the low (47%), mid (63.2%), and high (83%) doses.
By day 29, there was a very brisk rise in geometric mean titers for CP5. Responses did not differ by rP305A dose or across age groups, with a similar pattern observed for CP8 and ClfA, Dr. Fenck Jr. said.
Session co-moderator Dr. Walter Orenstein, from Emory University in Atlanta, commented that the rate of decay post-vaccination was promising, particularly compared with that observed with meningococcal vaccines.
The vaccine “program is exciting because it not only relies on just antibody, but it actually looks at functional responses and those functional responses have some correlate with protection against staphylococcal disease,” he said in an interview. High-risk populations, like renal dialysis patients, were not studied and it would be interesting to see how well they would respond. “Previous studies have shown transient benefits for those types of populations.”
AT ID WEEK 2014
Key clinical point: A vaccine to prevent invasive Staphylococcus aureus infections is in the early stages of testing.
Major finding: At day 29, all participants who received the active vaccine achieved the CP5 opsonophagocytic activity threshold and 96%–99% met the CP8 threshold.
Data source: Double-blind phase I/II study in 456 healthy adults.
Disclosures: The study was funded by Pfizer. Dr. Frenck Jr. reported receiving grant support from Pfizer to conduct the study. Three co-authors are Pfizer employees.
VIDEO: How to negotiate the robotic surgery learning curve
SAN FRANCISCO– Before attempting robotic surgery, it’s important to be comfortable with both the open and laparoscopic versions of the procedure, according to Dr. Kenneth Meredith, director of robotic surgery at the University of Wisconsin, Madison.
In experienced hands, robotic results can be good. In a case series of 138 robotic-assisted Ivor Lewis esophagectomies at the university for esophageal cancer, the median intensive care unit stay was 2 days and median hospital stay 9 days, Dr. Meredith. Complications occurred in about a quarter of patients.
In a video interview at the American College of Surgeons Clinical Congress, Dr. Meredith explained the significance of the findings and gave tips on how to negotiate the robotic surgery learning curve.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Before attempting robotic surgery, it’s important to be comfortable with both the open and laparoscopic versions of the procedure, according to Dr. Kenneth Meredith, director of robotic surgery at the University of Wisconsin, Madison.
In experienced hands, robotic results can be good. In a case series of 138 robotic-assisted Ivor Lewis esophagectomies at the university for esophageal cancer, the median intensive care unit stay was 2 days and median hospital stay 9 days, Dr. Meredith. Complications occurred in about a quarter of patients.
In a video interview at the American College of Surgeons Clinical Congress, Dr. Meredith explained the significance of the findings and gave tips on how to negotiate the robotic surgery learning curve.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Before attempting robotic surgery, it’s important to be comfortable with both the open and laparoscopic versions of the procedure, according to Dr. Kenneth Meredith, director of robotic surgery at the University of Wisconsin, Madison.
In experienced hands, robotic results can be good. In a case series of 138 robotic-assisted Ivor Lewis esophagectomies at the university for esophageal cancer, the median intensive care unit stay was 2 days and median hospital stay 9 days, Dr. Meredith. Complications occurred in about a quarter of patients.
In a video interview at the American College of Surgeons Clinical Congress, Dr. Meredith explained the significance of the findings and gave tips on how to negotiate the robotic surgery learning curve.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AMERICAN COLLEGE OF SURGEONS CLINICAL CONGRESS
Postdiagnosis imaging common in thyroid cancer
CORONADO, CALIF.– Today’s clinicians are ordering more postdiagnosis imaging tests in patients with thyroid cancer than they did in the early 1990s, results from the largest study of its kind showed.
“There is very little data on surveillance imaging for cancers in general, and especially for thyroid cancer,” lead author Dr. Jaime L. Wiebel said in an interview in advance of at the annual meeting of the American Thyroid Association, where the work was presented. “This study revealed that, over time, there has been an increase in all postdiagnosis imaging studies: ultrasound, I-131 [radioactive iodine] scans, and PET scans.”
Dr. Wiebel of the University of Michigan’s metabolism, endocrinology, and diabetes clinic, Ann Arbor, and her associates used records from the linked database to identify patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009. Next, they reviewed medical claims and determined the use of thyroid ultrasound, I-131 scan, or PET scan within 3 years post diagnosis. The researchers used linear regression analysis to evaluate imaging trends during the study period and multivariate logistic regression to estimate the likelihood of imaging use based on patient characteristics.
In all, 23,669 patients with well-differentiated thyroid cancer were included in the analysis. Most (79%) were younger than age 75 years, and 70% were female. Dr. Wiebel and her associates observed an increased use of both thyroid ultrasound and I-131 among patients with localized disease (P < .001 and P = .003, respectively). Use of the two modalities also increased among patients with regional disease (both P < .001) as well as among patients with distant disease (P = .001 and P = .015).
After controlling for patient characteristics, the researchers found that patients diagnosed during 2001-2009 were 2.15 times more likely to undergo a thyroid ultrasound, compared with those diagnosed during 1991-2000. In addition, PET scan use during 2005-2009, compared with 1996-2004, increased 32.4-fold among those with localized disease, 13.1-fold among those with regional disease, and 33.4-fold among those with distant disease (all significant at P < .001). Patients diagnosed with thyroid cancer after the year 2000 were more likely to have smaller, localized cancer.
“A few of our findings were unexpected,” Dr. Wiebel said. “We had anticipated that since more low-risk thyroid cancer is being diagnosed in the United States, that postdiagnosis surveillance imaging would decrease over time. We found the exact opposite. Despite the rise in low-risk thyroid cancer, there has been an increase in postdiagnosis imaging in the United States. Especially surprising was the very large increase in PET scan use.”
She acknowledged certain limitations of the analysis, including lack of data regarding indications for the imaging studies, “including iodine avidity of the tumor, disease recurrence, or patient preferences,” and the fact that most of the patients were over age 65 years. “However, we suspect that imaging practices in younger patients are similar,” she said.
Dr. Wiebel reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Today’s clinicians are ordering more postdiagnosis imaging tests in patients with thyroid cancer than they did in the early 1990s, results from the largest study of its kind showed.
“There is very little data on surveillance imaging for cancers in general, and especially for thyroid cancer,” lead author Dr. Jaime L. Wiebel said in an interview in advance of at the annual meeting of the American Thyroid Association, where the work was presented. “This study revealed that, over time, there has been an increase in all postdiagnosis imaging studies: ultrasound, I-131 [radioactive iodine] scans, and PET scans.”
Dr. Wiebel of the University of Michigan’s metabolism, endocrinology, and diabetes clinic, Ann Arbor, and her associates used records from the linked database to identify patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009. Next, they reviewed medical claims and determined the use of thyroid ultrasound, I-131 scan, or PET scan within 3 years post diagnosis. The researchers used linear regression analysis to evaluate imaging trends during the study period and multivariate logistic regression to estimate the likelihood of imaging use based on patient characteristics.
In all, 23,669 patients with well-differentiated thyroid cancer were included in the analysis. Most (79%) were younger than age 75 years, and 70% were female. Dr. Wiebel and her associates observed an increased use of both thyroid ultrasound and I-131 among patients with localized disease (P < .001 and P = .003, respectively). Use of the two modalities also increased among patients with regional disease (both P < .001) as well as among patients with distant disease (P = .001 and P = .015).
After controlling for patient characteristics, the researchers found that patients diagnosed during 2001-2009 were 2.15 times more likely to undergo a thyroid ultrasound, compared with those diagnosed during 1991-2000. In addition, PET scan use during 2005-2009, compared with 1996-2004, increased 32.4-fold among those with localized disease, 13.1-fold among those with regional disease, and 33.4-fold among those with distant disease (all significant at P < .001). Patients diagnosed with thyroid cancer after the year 2000 were more likely to have smaller, localized cancer.
“A few of our findings were unexpected,” Dr. Wiebel said. “We had anticipated that since more low-risk thyroid cancer is being diagnosed in the United States, that postdiagnosis surveillance imaging would decrease over time. We found the exact opposite. Despite the rise in low-risk thyroid cancer, there has been an increase in postdiagnosis imaging in the United States. Especially surprising was the very large increase in PET scan use.”
She acknowledged certain limitations of the analysis, including lack of data regarding indications for the imaging studies, “including iodine avidity of the tumor, disease recurrence, or patient preferences,” and the fact that most of the patients were over age 65 years. “However, we suspect that imaging practices in younger patients are similar,” she said.
Dr. Wiebel reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF.– Today’s clinicians are ordering more postdiagnosis imaging tests in patients with thyroid cancer than they did in the early 1990s, results from the largest study of its kind showed.
“There is very little data on surveillance imaging for cancers in general, and especially for thyroid cancer,” lead author Dr. Jaime L. Wiebel said in an interview in advance of at the annual meeting of the American Thyroid Association, where the work was presented. “This study revealed that, over time, there has been an increase in all postdiagnosis imaging studies: ultrasound, I-131 [radioactive iodine] scans, and PET scans.”
Dr. Wiebel of the University of Michigan’s metabolism, endocrinology, and diabetes clinic, Ann Arbor, and her associates used records from the linked database to identify patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009. Next, they reviewed medical claims and determined the use of thyroid ultrasound, I-131 scan, or PET scan within 3 years post diagnosis. The researchers used linear regression analysis to evaluate imaging trends during the study period and multivariate logistic regression to estimate the likelihood of imaging use based on patient characteristics.
In all, 23,669 patients with well-differentiated thyroid cancer were included in the analysis. Most (79%) were younger than age 75 years, and 70% were female. Dr. Wiebel and her associates observed an increased use of both thyroid ultrasound and I-131 among patients with localized disease (P < .001 and P = .003, respectively). Use of the two modalities also increased among patients with regional disease (both P < .001) as well as among patients with distant disease (P = .001 and P = .015).
After controlling for patient characteristics, the researchers found that patients diagnosed during 2001-2009 were 2.15 times more likely to undergo a thyroid ultrasound, compared with those diagnosed during 1991-2000. In addition, PET scan use during 2005-2009, compared with 1996-2004, increased 32.4-fold among those with localized disease, 13.1-fold among those with regional disease, and 33.4-fold among those with distant disease (all significant at P < .001). Patients diagnosed with thyroid cancer after the year 2000 were more likely to have smaller, localized cancer.
“A few of our findings were unexpected,” Dr. Wiebel said. “We had anticipated that since more low-risk thyroid cancer is being diagnosed in the United States, that postdiagnosis surveillance imaging would decrease over time. We found the exact opposite. Despite the rise in low-risk thyroid cancer, there has been an increase in postdiagnosis imaging in the United States. Especially surprising was the very large increase in PET scan use.”
She acknowledged certain limitations of the analysis, including lack of data regarding indications for the imaging studies, “including iodine avidity of the tumor, disease recurrence, or patient preferences,” and the fact that most of the patients were over age 65 years. “However, we suspect that imaging practices in younger patients are similar,” she said.
Dr. Wiebel reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Regardless of stage, clinicians are doing more postdiagnosis imaging of thyroid cancer patients than they were in the 1990s.
Major finding: Between 1991 and 2009, the use of both thyroid ultrasound and I-131 scans increased significantly among patients with localized thyroid disease. Imaging also increased among those with regional and distant disease.
Data source: An analysis of 23,669 patients diagnosed with localized, regional, or distant well-differentiated thyroid cancer between 1991 and 2009 who were identified from the linked SEER-Medicare database.
Disclosures: Dr. Wiebel reported having no financial disclosures.
Three-minute assessment detected most cases of delirium
A shortened version of the Confusion Assessment Method took 3 minutes to administer and identified 95% of patients with delirium, compared with a reference standard that involved 1.5 hours of interviews and medical record reviews by a panel of experts, researchers reported online Oct. 20 in the Annals of Internal Medicine.
The 3-minute CAM (3D-CAM) also had a high estimated specificity (94%; 95% confidence interval, 90%-97%), although specificity was substantially lower (86%) in patients with dementia (95% CI, 67%-96%), probably because it can be difficult to distinguish delirium from dementia, said Dr. Edward Marcantonio of the Beth Israel Deaconess Medical Center in Boston and his associates. “Further research will focus on developing the optimal strategies for translating the 3D-CAM into routine care and determining whether improved detection of delirium can result in improved outcomes for vulnerable hospitalized older persons,” said the researchers (Ann. Intern. Med. 2014 Oct. 20 [doi:10.7326/M14-0865]).
The original CAM has been widely used since the 1990s and is regarded as accurate, but challenging to administer. To create the 3-minute version of the CAM, the investigators used a data set of 4,598 structured delirium assessments from a prior multisite trial in which they had selected the 36 items that best captured the four diagnostic features of the CAM. Those features include acute change or fluctuating course, inattention, disorganized thinking, and altered level of consciousness, said the investigators. They further reduced the 36-item list to 20 by using logistic regression to identify the most useful items for each diagnostic feature, they said.
The researchers then tested the 3D-CAM in a prospective cohort of 201 medical patients with a median age of 84 years. In all, 88% of patients were white, and 21% had been diagnosed with dementia, the researchers reported. An expert panel determined that 42 (21%) of these patients had delirium, of which 88% had hypoactive or normal psychomotor features, said Dr. Marcantonio and his associates.
When compared with this reference standard, the overall sensitivity of the 3D-CAM was 95% (95% CI, 84%-99%), and the test was similarly sensitive in patients with and without dementia, the researchers reported. Among nine false positives, six patients had subsyndromal delirium as determined by the expert panel, the investigators added.
The 3D-CAM took a median of 3 minutes to administer (interquartile range, 2-5 minutes), said the researchers. Because some 95% confidence intervals were wide and the study was conducted at one urban teaching hospital on a single day, they recommended validating the results in settings such as surgical wards and postacute and palliative care facilities.
The National Institute on Aging funded the study. The investigators declared no financial conflicts.
A shortened version of the Confusion Assessment Method took 3 minutes to administer and identified 95% of patients with delirium, compared with a reference standard that involved 1.5 hours of interviews and medical record reviews by a panel of experts, researchers reported online Oct. 20 in the Annals of Internal Medicine.
The 3-minute CAM (3D-CAM) also had a high estimated specificity (94%; 95% confidence interval, 90%-97%), although specificity was substantially lower (86%) in patients with dementia (95% CI, 67%-96%), probably because it can be difficult to distinguish delirium from dementia, said Dr. Edward Marcantonio of the Beth Israel Deaconess Medical Center in Boston and his associates. “Further research will focus on developing the optimal strategies for translating the 3D-CAM into routine care and determining whether improved detection of delirium can result in improved outcomes for vulnerable hospitalized older persons,” said the researchers (Ann. Intern. Med. 2014 Oct. 20 [doi:10.7326/M14-0865]).
The original CAM has been widely used since the 1990s and is regarded as accurate, but challenging to administer. To create the 3-minute version of the CAM, the investigators used a data set of 4,598 structured delirium assessments from a prior multisite trial in which they had selected the 36 items that best captured the four diagnostic features of the CAM. Those features include acute change or fluctuating course, inattention, disorganized thinking, and altered level of consciousness, said the investigators. They further reduced the 36-item list to 20 by using logistic regression to identify the most useful items for each diagnostic feature, they said.
The researchers then tested the 3D-CAM in a prospective cohort of 201 medical patients with a median age of 84 years. In all, 88% of patients were white, and 21% had been diagnosed with dementia, the researchers reported. An expert panel determined that 42 (21%) of these patients had delirium, of which 88% had hypoactive or normal psychomotor features, said Dr. Marcantonio and his associates.
When compared with this reference standard, the overall sensitivity of the 3D-CAM was 95% (95% CI, 84%-99%), and the test was similarly sensitive in patients with and without dementia, the researchers reported. Among nine false positives, six patients had subsyndromal delirium as determined by the expert panel, the investigators added.
The 3D-CAM took a median of 3 minutes to administer (interquartile range, 2-5 minutes), said the researchers. Because some 95% confidence intervals were wide and the study was conducted at one urban teaching hospital on a single day, they recommended validating the results in settings such as surgical wards and postacute and palliative care facilities.
The National Institute on Aging funded the study. The investigators declared no financial conflicts.
A shortened version of the Confusion Assessment Method took 3 minutes to administer and identified 95% of patients with delirium, compared with a reference standard that involved 1.5 hours of interviews and medical record reviews by a panel of experts, researchers reported online Oct. 20 in the Annals of Internal Medicine.
The 3-minute CAM (3D-CAM) also had a high estimated specificity (94%; 95% confidence interval, 90%-97%), although specificity was substantially lower (86%) in patients with dementia (95% CI, 67%-96%), probably because it can be difficult to distinguish delirium from dementia, said Dr. Edward Marcantonio of the Beth Israel Deaconess Medical Center in Boston and his associates. “Further research will focus on developing the optimal strategies for translating the 3D-CAM into routine care and determining whether improved detection of delirium can result in improved outcomes for vulnerable hospitalized older persons,” said the researchers (Ann. Intern. Med. 2014 Oct. 20 [doi:10.7326/M14-0865]).
The original CAM has been widely used since the 1990s and is regarded as accurate, but challenging to administer. To create the 3-minute version of the CAM, the investigators used a data set of 4,598 structured delirium assessments from a prior multisite trial in which they had selected the 36 items that best captured the four diagnostic features of the CAM. Those features include acute change or fluctuating course, inattention, disorganized thinking, and altered level of consciousness, said the investigators. They further reduced the 36-item list to 20 by using logistic regression to identify the most useful items for each diagnostic feature, they said.
The researchers then tested the 3D-CAM in a prospective cohort of 201 medical patients with a median age of 84 years. In all, 88% of patients were white, and 21% had been diagnosed with dementia, the researchers reported. An expert panel determined that 42 (21%) of these patients had delirium, of which 88% had hypoactive or normal psychomotor features, said Dr. Marcantonio and his associates.
When compared with this reference standard, the overall sensitivity of the 3D-CAM was 95% (95% CI, 84%-99%), and the test was similarly sensitive in patients with and without dementia, the researchers reported. Among nine false positives, six patients had subsyndromal delirium as determined by the expert panel, the investigators added.
The 3D-CAM took a median of 3 minutes to administer (interquartile range, 2-5 minutes), said the researchers. Because some 95% confidence intervals were wide and the study was conducted at one urban teaching hospital on a single day, they recommended validating the results in settings such as surgical wards and postacute and palliative care facilities.
The National Institute on Aging funded the study. The investigators declared no financial conflicts.
Key clinical point: A 3-minute version of the Confusion Assessment Method (3D-CAM) detected delirium in elderly patients.
Major finding: Median time to administer the assessment was 3 minutes, estimated sensitivity was 95%, and overall specificity was 94%.
Data source: Single-center, cross-sectional study of 201 patients at an academic medical center.
Disclosures: The National Institute on Aging funded the study. The authors declared no financial conflicts.
Should ductal carcinoma in situ be treated?
Remarks given during a session of the ASCO Breast Cancer Symposium titled Ductal Carcinoma in Situ Debate: Treatment vs. Observation
Dr. Kuerer comments: There has been a marked increase ductal carcinoma in situ (DCIS) in what is being called overdiagnosis, and this is leading to concerns of overtreatment, which has been in the news now for several years. We have more than 60,000 cases of DCIS diagnosed per year in the United States. We’re trying to prevent invasive breast cancer and distant metastases. The problem is identifying which patients will go on to develop invasive disease. That’s really unknown.
At M.D. Anderson, looking at 10-year follow-up of 2,449 patients, the rate of developing distant metastases was 0.1%. The problem with this is that no prominent variables were associated with the development of invasive metastatic disease. Overall, we are doing a good job at preventing death from breast cancer when we treat DCIS, with less than 1% of patients dying of breast cancer (Ann. Surg. Onc. 2011;18:2873-8).
Dr. Shelley E. Hwang and her group very elegantly started exploring preoperative systemic therapy as a way to get a clue about which patients might be safely observed alone (that is, a core biopsy diagnosis of DCIS and then just follow-up without surgery or other treatments). At M.D. Anderson, we studied whether or not we could eradicate DCIS in patients with human epidermal growth factor receptor 2 (HER2) overexpression by treatment with trastuzumab prior to surgery, under the hypothesis that if we could eradicate the DCIS, we might eventually use this drug potentially to prevent HER2-positive invasive breast cancers. We saw very dramatic responses in their immune response with antibody-dependent cellular cytotoxicity mediated by natural killer cells, which is exciting, but there were no histopathologic changes. The most important finding was that 42% of our patients who we thought only had DCIS actually had occult invasive breast cancer (Cancer 2011;117:39-47). This is concerning because without surgery, we may be missing or leaving untreated invasive breast cancers in some patients.
So, we have an underestimation of invasive breast cancer at DCIS diagnosis. A very elegant meta-analysis of 7,350 patients reported that even if we take patients with non–high-grade, very-small DCIS, we’re still looking at an upgrade to invasive cancer of about 20% (Radiology 2011;260:119-28). The best and most recent studies of MRI and DCIS again found a diagnostic upgrade of about 27%. There were no MRI features correlating with invasive breast cancer, and this resulted in a 31% increase in procedures and more biopsies with the use of MRI.
So where are we? In active surveillance of 14 patients with DCIS at the University of California, San Francisco, 8 went on to surgery at a median follow-up of 28 months, and 5 of the 8 (62%) had invasive breast cancer (The Breast 2011;20:529-33).
What’s the cost to the health care system of surveillance if we biopsy only the DCIS and follow it without surgery or other adjuvant therapies? The psychological cost to our patients? What is the natural history of DCIS if left in place? What will be the result of microcalcifications? How are we going to follow this? What are the criteria that we will use for repeat biopsy? This really is not known.
Which are the patients that we’re going to select for observation alone? There are trials in Europe that have begun or will begin to address the safety of just observing DCIS without surgery and other therapies.
The United Kingdom Low-Risk DCIS Trial is randomizing patients with low and intermediate grade DCIS of any size to biopsy alone without surgical intervention (active monitoring) or standard therapy. Another trial, a joint Dutch Breast Cancer Research Group and European Organization for the Research and Treatment of Cancer trial is randomizing women with low-risk, low-grade DCIS to active surveillance or standard treatment. If we look at M.D. Anderson’s data and our National Cancer Database, only about 10%-15% of patients would be eligible for the latter study. I don’t think with these numbers we’d have a great impact, but it is a start.
I submit that the best U.S. patients to study will be patients with a diagnosis of atypical ductal hyperplasia (generally the smallest lesions and perhaps the earliest form of DCIS) because we have about 100,000 cases each year.
What’s the patient’s perspective? What about the need for continued repeat biopsies, and how this will affect their overall quality of life? Do patients in the United States really want to observe the DCIS in an era when our patients are requesting more and more mastectomy with reconstruction and contralateral mastectomy at diagnosis of DCIS? I seriously doubt that our patients in the United States would agree to be randomized in DCIS trials to no treatment at all. I really don’t know.
Dr. Kuerer is a professor of surgery at the University of Texas M.D. Anderson Cancer Center, Houston. He reported financial associations with Gerson Lehrman Group and McGraw-Hill Publishing.
Dr. Hwang comments: Today, about 1/1,300 screening mammograms result in a diagnosis of DCIS. There are two important considerations when we talk about active surveillance or doing less aggressive treatment. First, what is the rate at which progression to invasive cancer can occur, either with or without treatment? Second, what is the fate of these DCIS lesions? These are issues for which we currently don’t have good answers.
We’re treating all disease detected at an early stage, and for the sake of argument, I’ll include DCIS, as if it likely will cause harm if we did absolutely nothing when, in fact, there could be many cancers that progress so slowly and have such a low propensity for developing metastatic disease that they would not likely cause any symptoms or harm during a patient’s lifetime.
In autopsy series, the disease reservoir of unrecognized DCIS is about 9% and the disease reservoir of invasive cancer is about 1%. It’s not that different from prostate cancer, although at a much lower rate. These data show that there certainly are women who die with DCIS rather than of it.
We really don’t have a very solid understanding of the natural history of DCIS. If we do nothing, but maybe surgically biopsy it, what happens to these patients in the long term? In a meta-analysis, the world’s literature included only 151 cases of women who had surgical biopsy of DCIS that initially was misdiagnosed as a benign lesion and therefore didn’t undergo any further therapy, some with up to 31 years of follow-up. The long-term risk of invasive cancer in this cohort is only 22% (Breast Cancer Res. Treat. 2006;97:135-44). The annual risk of breast cancer in women with atypia is 1% per year, so this ends up looking very similar to the risk of progression that you see for atypical ductal hyperplasia or lobular carcinoma in situ.
The most common treatment for DCIS in the United States is lumpectomy with radiation. A meta-analysis by the European Breast Cancer Trialists’ Group found a 50% proportional reduction in local recurrence risk in women treated with lumpectomy and radiation vs. lumpectomy alone. The absolute magnitude of reduction was dependent on baseline recurrence risk. That’s a really important concept, because if your baseline risk is only 5%, then the 50% proportional reduction only translates into a 2.5% reduction in risk in 10 years.
The prospective, randomized Radiation Therapy Oncologists Group 9804 study randomized low-risk women with DCIS, unlike prior randomized trials that included broad eligibility criteria for DCIS. In 5 years of follow-up, the ipsilateral recurrence risk (which includes both invasive cancer and DCIS) was 3.2% in the lumpectomy-only group vs. 0.4% in the lumpectomy and radiation therapy group. The difference is highly statistically significant, however, given the small absolute difference between groups, the clinical significance certainly can be argued. There was no significant difference between groups in contralateral new primary lesions (Radiat. Oncol. 2012;84:S5).
We just presented a study this year looking at DCIS and competing causes of mortality in different age groups with different types of treatment. Among women with DCIS over 70 years of age, there was a significant difference in overall survival but none of the treatments conferred any benefit in disease-specific survival.
Active surveillance alone may be reasonable to consider in some patients. We can learn a lot from our colleagues who treat prostate cancer. They’re at least 10 years ahead of us in thinking about reducing the harms that have been introduced by screening for prostate cancer. When you look at breast cancer–specific and other-cause mortality in the setting of DCIS, the mortality curves look very similar to those with early-stage prostate cancer. Women with DCIS, regardless of what they are treated with, die of other causes and very rarely die of breast cancer.
When we compare such different options as mastectomy to active surveillance only, it’s really hard for a patient to feel that both of those approaches can offer them the same outcomes. But when you look at the actual data and evidence, the differences in recurrence or progression to invasive cancer don’t translate easily into a large difference in breast cancer mortality provided that patients are diagnosed at stage I or II, with more than a 90% survival from breast cancer.
We have an opportunity to take a big step back and redefine our goals of DCIS “treatment” from “curing” DCIS to trying to reduce breast cancer-specific mortality. This will help us reduce the harms that can result from screening and will reserve our aggressive treatments for those most likely to benefit from them.
Dr. Hwang is a professor of surgery at Duke University, Durham, N.C. She serves as a consultant for Genomic Health.
Remarks given during a session of the ASCO Breast Cancer Symposium titled Ductal Carcinoma in Situ Debate: Treatment vs. Observation
Dr. Kuerer comments: There has been a marked increase ductal carcinoma in situ (DCIS) in what is being called overdiagnosis, and this is leading to concerns of overtreatment, which has been in the news now for several years. We have more than 60,000 cases of DCIS diagnosed per year in the United States. We’re trying to prevent invasive breast cancer and distant metastases. The problem is identifying which patients will go on to develop invasive disease. That’s really unknown.
At M.D. Anderson, looking at 10-year follow-up of 2,449 patients, the rate of developing distant metastases was 0.1%. The problem with this is that no prominent variables were associated with the development of invasive metastatic disease. Overall, we are doing a good job at preventing death from breast cancer when we treat DCIS, with less than 1% of patients dying of breast cancer (Ann. Surg. Onc. 2011;18:2873-8).
Dr. Shelley E. Hwang and her group very elegantly started exploring preoperative systemic therapy as a way to get a clue about which patients might be safely observed alone (that is, a core biopsy diagnosis of DCIS and then just follow-up without surgery or other treatments). At M.D. Anderson, we studied whether or not we could eradicate DCIS in patients with human epidermal growth factor receptor 2 (HER2) overexpression by treatment with trastuzumab prior to surgery, under the hypothesis that if we could eradicate the DCIS, we might eventually use this drug potentially to prevent HER2-positive invasive breast cancers. We saw very dramatic responses in their immune response with antibody-dependent cellular cytotoxicity mediated by natural killer cells, which is exciting, but there were no histopathologic changes. The most important finding was that 42% of our patients who we thought only had DCIS actually had occult invasive breast cancer (Cancer 2011;117:39-47). This is concerning because without surgery, we may be missing or leaving untreated invasive breast cancers in some patients.
So, we have an underestimation of invasive breast cancer at DCIS diagnosis. A very elegant meta-analysis of 7,350 patients reported that even if we take patients with non–high-grade, very-small DCIS, we’re still looking at an upgrade to invasive cancer of about 20% (Radiology 2011;260:119-28). The best and most recent studies of MRI and DCIS again found a diagnostic upgrade of about 27%. There were no MRI features correlating with invasive breast cancer, and this resulted in a 31% increase in procedures and more biopsies with the use of MRI.
So where are we? In active surveillance of 14 patients with DCIS at the University of California, San Francisco, 8 went on to surgery at a median follow-up of 28 months, and 5 of the 8 (62%) had invasive breast cancer (The Breast 2011;20:529-33).
What’s the cost to the health care system of surveillance if we biopsy only the DCIS and follow it without surgery or other adjuvant therapies? The psychological cost to our patients? What is the natural history of DCIS if left in place? What will be the result of microcalcifications? How are we going to follow this? What are the criteria that we will use for repeat biopsy? This really is not known.
Which are the patients that we’re going to select for observation alone? There are trials in Europe that have begun or will begin to address the safety of just observing DCIS without surgery and other therapies.
The United Kingdom Low-Risk DCIS Trial is randomizing patients with low and intermediate grade DCIS of any size to biopsy alone without surgical intervention (active monitoring) or standard therapy. Another trial, a joint Dutch Breast Cancer Research Group and European Organization for the Research and Treatment of Cancer trial is randomizing women with low-risk, low-grade DCIS to active surveillance or standard treatment. If we look at M.D. Anderson’s data and our National Cancer Database, only about 10%-15% of patients would be eligible for the latter study. I don’t think with these numbers we’d have a great impact, but it is a start.
I submit that the best U.S. patients to study will be patients with a diagnosis of atypical ductal hyperplasia (generally the smallest lesions and perhaps the earliest form of DCIS) because we have about 100,000 cases each year.
What’s the patient’s perspective? What about the need for continued repeat biopsies, and how this will affect their overall quality of life? Do patients in the United States really want to observe the DCIS in an era when our patients are requesting more and more mastectomy with reconstruction and contralateral mastectomy at diagnosis of DCIS? I seriously doubt that our patients in the United States would agree to be randomized in DCIS trials to no treatment at all. I really don’t know.
Dr. Kuerer is a professor of surgery at the University of Texas M.D. Anderson Cancer Center, Houston. He reported financial associations with Gerson Lehrman Group and McGraw-Hill Publishing.
Dr. Hwang comments: Today, about 1/1,300 screening mammograms result in a diagnosis of DCIS. There are two important considerations when we talk about active surveillance or doing less aggressive treatment. First, what is the rate at which progression to invasive cancer can occur, either with or without treatment? Second, what is the fate of these DCIS lesions? These are issues for which we currently don’t have good answers.
We’re treating all disease detected at an early stage, and for the sake of argument, I’ll include DCIS, as if it likely will cause harm if we did absolutely nothing when, in fact, there could be many cancers that progress so slowly and have such a low propensity for developing metastatic disease that they would not likely cause any symptoms or harm during a patient’s lifetime.
In autopsy series, the disease reservoir of unrecognized DCIS is about 9% and the disease reservoir of invasive cancer is about 1%. It’s not that different from prostate cancer, although at a much lower rate. These data show that there certainly are women who die with DCIS rather than of it.
We really don’t have a very solid understanding of the natural history of DCIS. If we do nothing, but maybe surgically biopsy it, what happens to these patients in the long term? In a meta-analysis, the world’s literature included only 151 cases of women who had surgical biopsy of DCIS that initially was misdiagnosed as a benign lesion and therefore didn’t undergo any further therapy, some with up to 31 years of follow-up. The long-term risk of invasive cancer in this cohort is only 22% (Breast Cancer Res. Treat. 2006;97:135-44). The annual risk of breast cancer in women with atypia is 1% per year, so this ends up looking very similar to the risk of progression that you see for atypical ductal hyperplasia or lobular carcinoma in situ.
The most common treatment for DCIS in the United States is lumpectomy with radiation. A meta-analysis by the European Breast Cancer Trialists’ Group found a 50% proportional reduction in local recurrence risk in women treated with lumpectomy and radiation vs. lumpectomy alone. The absolute magnitude of reduction was dependent on baseline recurrence risk. That’s a really important concept, because if your baseline risk is only 5%, then the 50% proportional reduction only translates into a 2.5% reduction in risk in 10 years.
The prospective, randomized Radiation Therapy Oncologists Group 9804 study randomized low-risk women with DCIS, unlike prior randomized trials that included broad eligibility criteria for DCIS. In 5 years of follow-up, the ipsilateral recurrence risk (which includes both invasive cancer and DCIS) was 3.2% in the lumpectomy-only group vs. 0.4% in the lumpectomy and radiation therapy group. The difference is highly statistically significant, however, given the small absolute difference between groups, the clinical significance certainly can be argued. There was no significant difference between groups in contralateral new primary lesions (Radiat. Oncol. 2012;84:S5).
We just presented a study this year looking at DCIS and competing causes of mortality in different age groups with different types of treatment. Among women with DCIS over 70 years of age, there was a significant difference in overall survival but none of the treatments conferred any benefit in disease-specific survival.
Active surveillance alone may be reasonable to consider in some patients. We can learn a lot from our colleagues who treat prostate cancer. They’re at least 10 years ahead of us in thinking about reducing the harms that have been introduced by screening for prostate cancer. When you look at breast cancer–specific and other-cause mortality in the setting of DCIS, the mortality curves look very similar to those with early-stage prostate cancer. Women with DCIS, regardless of what they are treated with, die of other causes and very rarely die of breast cancer.
When we compare such different options as mastectomy to active surveillance only, it’s really hard for a patient to feel that both of those approaches can offer them the same outcomes. But when you look at the actual data and evidence, the differences in recurrence or progression to invasive cancer don’t translate easily into a large difference in breast cancer mortality provided that patients are diagnosed at stage I or II, with more than a 90% survival from breast cancer.
We have an opportunity to take a big step back and redefine our goals of DCIS “treatment” from “curing” DCIS to trying to reduce breast cancer-specific mortality. This will help us reduce the harms that can result from screening and will reserve our aggressive treatments for those most likely to benefit from them.
Dr. Hwang is a professor of surgery at Duke University, Durham, N.C. She serves as a consultant for Genomic Health.
Remarks given during a session of the ASCO Breast Cancer Symposium titled Ductal Carcinoma in Situ Debate: Treatment vs. Observation
Dr. Kuerer comments: There has been a marked increase ductal carcinoma in situ (DCIS) in what is being called overdiagnosis, and this is leading to concerns of overtreatment, which has been in the news now for several years. We have more than 60,000 cases of DCIS diagnosed per year in the United States. We’re trying to prevent invasive breast cancer and distant metastases. The problem is identifying which patients will go on to develop invasive disease. That’s really unknown.
At M.D. Anderson, looking at 10-year follow-up of 2,449 patients, the rate of developing distant metastases was 0.1%. The problem with this is that no prominent variables were associated with the development of invasive metastatic disease. Overall, we are doing a good job at preventing death from breast cancer when we treat DCIS, with less than 1% of patients dying of breast cancer (Ann. Surg. Onc. 2011;18:2873-8).
Dr. Shelley E. Hwang and her group very elegantly started exploring preoperative systemic therapy as a way to get a clue about which patients might be safely observed alone (that is, a core biopsy diagnosis of DCIS and then just follow-up without surgery or other treatments). At M.D. Anderson, we studied whether or not we could eradicate DCIS in patients with human epidermal growth factor receptor 2 (HER2) overexpression by treatment with trastuzumab prior to surgery, under the hypothesis that if we could eradicate the DCIS, we might eventually use this drug potentially to prevent HER2-positive invasive breast cancers. We saw very dramatic responses in their immune response with antibody-dependent cellular cytotoxicity mediated by natural killer cells, which is exciting, but there were no histopathologic changes. The most important finding was that 42% of our patients who we thought only had DCIS actually had occult invasive breast cancer (Cancer 2011;117:39-47). This is concerning because without surgery, we may be missing or leaving untreated invasive breast cancers in some patients.
So, we have an underestimation of invasive breast cancer at DCIS diagnosis. A very elegant meta-analysis of 7,350 patients reported that even if we take patients with non–high-grade, very-small DCIS, we’re still looking at an upgrade to invasive cancer of about 20% (Radiology 2011;260:119-28). The best and most recent studies of MRI and DCIS again found a diagnostic upgrade of about 27%. There were no MRI features correlating with invasive breast cancer, and this resulted in a 31% increase in procedures and more biopsies with the use of MRI.
So where are we? In active surveillance of 14 patients with DCIS at the University of California, San Francisco, 8 went on to surgery at a median follow-up of 28 months, and 5 of the 8 (62%) had invasive breast cancer (The Breast 2011;20:529-33).
What’s the cost to the health care system of surveillance if we biopsy only the DCIS and follow it without surgery or other adjuvant therapies? The psychological cost to our patients? What is the natural history of DCIS if left in place? What will be the result of microcalcifications? How are we going to follow this? What are the criteria that we will use for repeat biopsy? This really is not known.
Which are the patients that we’re going to select for observation alone? There are trials in Europe that have begun or will begin to address the safety of just observing DCIS without surgery and other therapies.
The United Kingdom Low-Risk DCIS Trial is randomizing patients with low and intermediate grade DCIS of any size to biopsy alone without surgical intervention (active monitoring) or standard therapy. Another trial, a joint Dutch Breast Cancer Research Group and European Organization for the Research and Treatment of Cancer trial is randomizing women with low-risk, low-grade DCIS to active surveillance or standard treatment. If we look at M.D. Anderson’s data and our National Cancer Database, only about 10%-15% of patients would be eligible for the latter study. I don’t think with these numbers we’d have a great impact, but it is a start.
I submit that the best U.S. patients to study will be patients with a diagnosis of atypical ductal hyperplasia (generally the smallest lesions and perhaps the earliest form of DCIS) because we have about 100,000 cases each year.
What’s the patient’s perspective? What about the need for continued repeat biopsies, and how this will affect their overall quality of life? Do patients in the United States really want to observe the DCIS in an era when our patients are requesting more and more mastectomy with reconstruction and contralateral mastectomy at diagnosis of DCIS? I seriously doubt that our patients in the United States would agree to be randomized in DCIS trials to no treatment at all. I really don’t know.
Dr. Kuerer is a professor of surgery at the University of Texas M.D. Anderson Cancer Center, Houston. He reported financial associations with Gerson Lehrman Group and McGraw-Hill Publishing.
Dr. Hwang comments: Today, about 1/1,300 screening mammograms result in a diagnosis of DCIS. There are two important considerations when we talk about active surveillance or doing less aggressive treatment. First, what is the rate at which progression to invasive cancer can occur, either with or without treatment? Second, what is the fate of these DCIS lesions? These are issues for which we currently don’t have good answers.
We’re treating all disease detected at an early stage, and for the sake of argument, I’ll include DCIS, as if it likely will cause harm if we did absolutely nothing when, in fact, there could be many cancers that progress so slowly and have such a low propensity for developing metastatic disease that they would not likely cause any symptoms or harm during a patient’s lifetime.
In autopsy series, the disease reservoir of unrecognized DCIS is about 9% and the disease reservoir of invasive cancer is about 1%. It’s not that different from prostate cancer, although at a much lower rate. These data show that there certainly are women who die with DCIS rather than of it.
We really don’t have a very solid understanding of the natural history of DCIS. If we do nothing, but maybe surgically biopsy it, what happens to these patients in the long term? In a meta-analysis, the world’s literature included only 151 cases of women who had surgical biopsy of DCIS that initially was misdiagnosed as a benign lesion and therefore didn’t undergo any further therapy, some with up to 31 years of follow-up. The long-term risk of invasive cancer in this cohort is only 22% (Breast Cancer Res. Treat. 2006;97:135-44). The annual risk of breast cancer in women with atypia is 1% per year, so this ends up looking very similar to the risk of progression that you see for atypical ductal hyperplasia or lobular carcinoma in situ.
The most common treatment for DCIS in the United States is lumpectomy with radiation. A meta-analysis by the European Breast Cancer Trialists’ Group found a 50% proportional reduction in local recurrence risk in women treated with lumpectomy and radiation vs. lumpectomy alone. The absolute magnitude of reduction was dependent on baseline recurrence risk. That’s a really important concept, because if your baseline risk is only 5%, then the 50% proportional reduction only translates into a 2.5% reduction in risk in 10 years.
The prospective, randomized Radiation Therapy Oncologists Group 9804 study randomized low-risk women with DCIS, unlike prior randomized trials that included broad eligibility criteria for DCIS. In 5 years of follow-up, the ipsilateral recurrence risk (which includes both invasive cancer and DCIS) was 3.2% in the lumpectomy-only group vs. 0.4% in the lumpectomy and radiation therapy group. The difference is highly statistically significant, however, given the small absolute difference between groups, the clinical significance certainly can be argued. There was no significant difference between groups in contralateral new primary lesions (Radiat. Oncol. 2012;84:S5).
We just presented a study this year looking at DCIS and competing causes of mortality in different age groups with different types of treatment. Among women with DCIS over 70 years of age, there was a significant difference in overall survival but none of the treatments conferred any benefit in disease-specific survival.
Active surveillance alone may be reasonable to consider in some patients. We can learn a lot from our colleagues who treat prostate cancer. They’re at least 10 years ahead of us in thinking about reducing the harms that have been introduced by screening for prostate cancer. When you look at breast cancer–specific and other-cause mortality in the setting of DCIS, the mortality curves look very similar to those with early-stage prostate cancer. Women with DCIS, regardless of what they are treated with, die of other causes and very rarely die of breast cancer.
When we compare such different options as mastectomy to active surveillance only, it’s really hard for a patient to feel that both of those approaches can offer them the same outcomes. But when you look at the actual data and evidence, the differences in recurrence or progression to invasive cancer don’t translate easily into a large difference in breast cancer mortality provided that patients are diagnosed at stage I or II, with more than a 90% survival from breast cancer.
We have an opportunity to take a big step back and redefine our goals of DCIS “treatment” from “curing” DCIS to trying to reduce breast cancer-specific mortality. This will help us reduce the harms that can result from screening and will reserve our aggressive treatments for those most likely to benefit from them.
Dr. Hwang is a professor of surgery at Duke University, Durham, N.C. She serves as a consultant for Genomic Health.
Laparoscopic splenectomy underutilized in the U.S.
LAS VEGAS – Laparoscopic splenectomy has become the preferred surgical approach in the literature, but the number of such procedures performed in the United States remains relatively low, according to Dr. John Afthinos.
National data for 2005-2010 showed a total of 37,006 elective total splenectomies were performed. Only 4,938 of them, or 13.3%, began as laparoscopic procedures, of which 40% had to be converted to open splenectomies, he reported at the annual Minimally Invasive Surgery Week.
“Laparoscopic splenectomy remains underutilized,” Dr. Afthinos commented. “This is one of the lowest recorded rates of laparoscopic completion of any advanced procedure that we know of.”
For example, other investigators have demonstrated that laparoscopic colectomies and bariatric surgical procedures are typically completed laparoscopically in 85%-95% of cases, noted Dr. Afthinos of Staten Island (N.Y.) University Hospital.
The laparoscopic approach has convincingly been shown to result in less pain, shorter hospital length of stay, faster recovery, and improved cosmetic results, compared with the open surgical versions of various operations.
“In the U.S., laparoscopic splenectomy is not well incorporated into the armamentarium of the average general surgeon. We can speculate that the underutilization of this approach around the country prevents development of the familiarity and skill that you need to perform the operation safely without conversion,” he said at the meeting, presented by the Society of Laparoscopic Surgeons and affiliated societies.
Dr. Afthinos’s data were drawn from the Nationwide Inpatient Sample maintained by the U.S. Agency for Healthcare Research and Quality. In this database, patients who had a laparoscopic splenectomy had the shortest average hospital length of stay: 5.6 days, compared with 7.5 in those who underwent open splenectomy and 7.1 for conversion procedures. The overall morbidity rate was significantly lower in the laparoscopic group, too: 7.4%, compared with 10.4% in the open splenectomy group.
In a multivariate analysis, he and his coworkers identified three independent risk factors for conversion from laparoscopic to open splenectomy: hemorrhage, with a 3.23-fold increased risk; splenomegaly, with a 1.3-fold increased risk; and autoimmune hemolytic anemia, with an associated 1.36-fold elevated risk of conversion.
Dr. Catalin Vasilescu of Carol Davila University in Bucharest, Romania, rose from the audience to voice his incredulity at the American data: “I am really surprised at your national conversion rate of well over 30%. That is really a problem. Earlier at this meeting, we presented 520 laparoscopic splenectomy patients with a conversion rate over 20 years of 4%-5%,” the Romanian general surgeon said.
“How do you explain this? I have a hypothesis: Perhaps there are so many surgeons each performing very few of these procedures, instead of referring patients to an experienced center,” he said.
“It was surprising to us, too,” Dr. Afthinos replied. “I mean, I was expecting the conversion rate to be high, but not that high.”
He said Dr. Vasilescu was right on the mark. In addition, he explained, it’s important to understand that there are vast rural areas of the United States, and some rural patients are reluctant to travel hundreds of miles to undergo laparoscopic splenectomy at a large experienced center, especially in the winter or if their family can’t come along for support. And a rural general surgeon is not going to risk a patient’s life if he or she isn’t comfortable with a laparoscopic approach.
There is hope that the situation will improve, however, as more fellowship-trained minimally invasive surgeons enter clinical practice, according to Dr. Afthinos. He cited a recent report from a Columbus, Ohio, general surgery practice that after a fellowship-trained minimally invasive surgeon joined the practice, the group – excluding their fellowship-trained recent hire – increased its rate of various advanced procedures being performed laparoscopically from 12% to 48%. The five established surgeons indicated they found mentoring by a colleague with minimally invasive surgery training was a better way to learn the procedures than via weekend courses, videos, traveling proctors, and other methods (Surg. Endosc. 2013;27:1267-72).
Dr. Afthinos reported having no relevant financial conflicts.
LAS VEGAS – Laparoscopic splenectomy has become the preferred surgical approach in the literature, but the number of such procedures performed in the United States remains relatively low, according to Dr. John Afthinos.
National data for 2005-2010 showed a total of 37,006 elective total splenectomies were performed. Only 4,938 of them, or 13.3%, began as laparoscopic procedures, of which 40% had to be converted to open splenectomies, he reported at the annual Minimally Invasive Surgery Week.
“Laparoscopic splenectomy remains underutilized,” Dr. Afthinos commented. “This is one of the lowest recorded rates of laparoscopic completion of any advanced procedure that we know of.”
For example, other investigators have demonstrated that laparoscopic colectomies and bariatric surgical procedures are typically completed laparoscopically in 85%-95% of cases, noted Dr. Afthinos of Staten Island (N.Y.) University Hospital.
The laparoscopic approach has convincingly been shown to result in less pain, shorter hospital length of stay, faster recovery, and improved cosmetic results, compared with the open surgical versions of various operations.
“In the U.S., laparoscopic splenectomy is not well incorporated into the armamentarium of the average general surgeon. We can speculate that the underutilization of this approach around the country prevents development of the familiarity and skill that you need to perform the operation safely without conversion,” he said at the meeting, presented by the Society of Laparoscopic Surgeons and affiliated societies.
Dr. Afthinos’s data were drawn from the Nationwide Inpatient Sample maintained by the U.S. Agency for Healthcare Research and Quality. In this database, patients who had a laparoscopic splenectomy had the shortest average hospital length of stay: 5.6 days, compared with 7.5 in those who underwent open splenectomy and 7.1 for conversion procedures. The overall morbidity rate was significantly lower in the laparoscopic group, too: 7.4%, compared with 10.4% in the open splenectomy group.
In a multivariate analysis, he and his coworkers identified three independent risk factors for conversion from laparoscopic to open splenectomy: hemorrhage, with a 3.23-fold increased risk; splenomegaly, with a 1.3-fold increased risk; and autoimmune hemolytic anemia, with an associated 1.36-fold elevated risk of conversion.
Dr. Catalin Vasilescu of Carol Davila University in Bucharest, Romania, rose from the audience to voice his incredulity at the American data: “I am really surprised at your national conversion rate of well over 30%. That is really a problem. Earlier at this meeting, we presented 520 laparoscopic splenectomy patients with a conversion rate over 20 years of 4%-5%,” the Romanian general surgeon said.
“How do you explain this? I have a hypothesis: Perhaps there are so many surgeons each performing very few of these procedures, instead of referring patients to an experienced center,” he said.
“It was surprising to us, too,” Dr. Afthinos replied. “I mean, I was expecting the conversion rate to be high, but not that high.”
He said Dr. Vasilescu was right on the mark. In addition, he explained, it’s important to understand that there are vast rural areas of the United States, and some rural patients are reluctant to travel hundreds of miles to undergo laparoscopic splenectomy at a large experienced center, especially in the winter or if their family can’t come along for support. And a rural general surgeon is not going to risk a patient’s life if he or she isn’t comfortable with a laparoscopic approach.
There is hope that the situation will improve, however, as more fellowship-trained minimally invasive surgeons enter clinical practice, according to Dr. Afthinos. He cited a recent report from a Columbus, Ohio, general surgery practice that after a fellowship-trained minimally invasive surgeon joined the practice, the group – excluding their fellowship-trained recent hire – increased its rate of various advanced procedures being performed laparoscopically from 12% to 48%. The five established surgeons indicated they found mentoring by a colleague with minimally invasive surgery training was a better way to learn the procedures than via weekend courses, videos, traveling proctors, and other methods (Surg. Endosc. 2013;27:1267-72).
Dr. Afthinos reported having no relevant financial conflicts.
LAS VEGAS – Laparoscopic splenectomy has become the preferred surgical approach in the literature, but the number of such procedures performed in the United States remains relatively low, according to Dr. John Afthinos.
National data for 2005-2010 showed a total of 37,006 elective total splenectomies were performed. Only 4,938 of them, or 13.3%, began as laparoscopic procedures, of which 40% had to be converted to open splenectomies, he reported at the annual Minimally Invasive Surgery Week.
“Laparoscopic splenectomy remains underutilized,” Dr. Afthinos commented. “This is one of the lowest recorded rates of laparoscopic completion of any advanced procedure that we know of.”
For example, other investigators have demonstrated that laparoscopic colectomies and bariatric surgical procedures are typically completed laparoscopically in 85%-95% of cases, noted Dr. Afthinos of Staten Island (N.Y.) University Hospital.
The laparoscopic approach has convincingly been shown to result in less pain, shorter hospital length of stay, faster recovery, and improved cosmetic results, compared with the open surgical versions of various operations.
“In the U.S., laparoscopic splenectomy is not well incorporated into the armamentarium of the average general surgeon. We can speculate that the underutilization of this approach around the country prevents development of the familiarity and skill that you need to perform the operation safely without conversion,” he said at the meeting, presented by the Society of Laparoscopic Surgeons and affiliated societies.
Dr. Afthinos’s data were drawn from the Nationwide Inpatient Sample maintained by the U.S. Agency for Healthcare Research and Quality. In this database, patients who had a laparoscopic splenectomy had the shortest average hospital length of stay: 5.6 days, compared with 7.5 in those who underwent open splenectomy and 7.1 for conversion procedures. The overall morbidity rate was significantly lower in the laparoscopic group, too: 7.4%, compared with 10.4% in the open splenectomy group.
In a multivariate analysis, he and his coworkers identified three independent risk factors for conversion from laparoscopic to open splenectomy: hemorrhage, with a 3.23-fold increased risk; splenomegaly, with a 1.3-fold increased risk; and autoimmune hemolytic anemia, with an associated 1.36-fold elevated risk of conversion.
Dr. Catalin Vasilescu of Carol Davila University in Bucharest, Romania, rose from the audience to voice his incredulity at the American data: “I am really surprised at your national conversion rate of well over 30%. That is really a problem. Earlier at this meeting, we presented 520 laparoscopic splenectomy patients with a conversion rate over 20 years of 4%-5%,” the Romanian general surgeon said.
“How do you explain this? I have a hypothesis: Perhaps there are so many surgeons each performing very few of these procedures, instead of referring patients to an experienced center,” he said.
“It was surprising to us, too,” Dr. Afthinos replied. “I mean, I was expecting the conversion rate to be high, but not that high.”
He said Dr. Vasilescu was right on the mark. In addition, he explained, it’s important to understand that there are vast rural areas of the United States, and some rural patients are reluctant to travel hundreds of miles to undergo laparoscopic splenectomy at a large experienced center, especially in the winter or if their family can’t come along for support. And a rural general surgeon is not going to risk a patient’s life if he or she isn’t comfortable with a laparoscopic approach.
There is hope that the situation will improve, however, as more fellowship-trained minimally invasive surgeons enter clinical practice, according to Dr. Afthinos. He cited a recent report from a Columbus, Ohio, general surgery practice that after a fellowship-trained minimally invasive surgeon joined the practice, the group – excluding their fellowship-trained recent hire – increased its rate of various advanced procedures being performed laparoscopically from 12% to 48%. The five established surgeons indicated they found mentoring by a colleague with minimally invasive surgery training was a better way to learn the procedures than via weekend courses, videos, traveling proctors, and other methods (Surg. Endosc. 2013;27:1267-72).
Dr. Afthinos reported having no relevant financial conflicts.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: American general surgeons lag far behind their foreign colleagues in their rate of laparoscopically completed splenectomies.
Major finding: Only 13.3% of elective splenectomies performed in the United States started out as laparoscopic procedures – and of those, 40% were converted to open splenectomy.
Data source: A retrospective study of the Nationwide Inpatient Sample for 2005-2010, during which 37,006 elective total splenectomies were performed.
Disclosures: The presenter reported having no relevant financial conflicts.
Study finds lap approach to bariatric revision safe, effective
LAS VEGAS– As the volume of bariatric surgery climbs sharply in response to the obesity epidemic, the need for revision procedures due to weight regain is also on the rise.
Laparoscopic revision bariatric surgery, while more technically challenging, is safe and effective, and it entails less morbidity than typically seen with open revisions, Dr. Rana M. Ballo said at the annual Minimally Invasive Surgery Week.
Dr. Ballo, a fifth-year general surgery resident at Rush University Medical Center in Chicago, presented a retrospective single-center study involving 227 patients who during 2001-2011 underwent laparoscopic revision of bariatric procedures that had failed because of weight regain. The goal of the revision bariatric surgery was to restore the restrictive component and/or add a malabsorptive component in order to improve long-term weight loss.
The patients fell into four groups. Group 1 consisted of 53 patients who initially had a laparoscopic adjustable gastric band procedure which was converted to a gastric bypass. Group 2, the largest group, initially had a Roux-en-Y gastric bypass in which the pouch eventually became dilated, which is the No. 1 cause of failure of this operation in the literature; their revision surgery entailed laparoscopic pouch reduction. The 38 patients who comprised Group 3 had a Roux-en-Y gastric bypass with subsequent pouch reduction and elongation of the biliopancreatic limb. Group 4 consisted of 17 patients who initially had a vertical banded gastroplasty – a procedure with a restrictive component only – and subsequently underwent laparoscopic conversion to a gastric bypass.
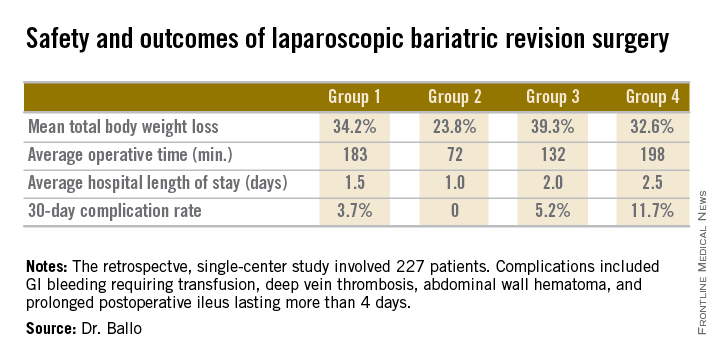
After a median follow-up of 3.9 years, Group 2 had significantly less total body weight loss than the rest of the groups, all of which had similar weight losses. On the other hand, Group 2 also had a shorter operative time and briefer average hospital length of stay than the other three groups, and it was the only group with zero complications. Still, the lengths of stay and 30-day morbidity rates across the board in this laparoscopic revision series were impressively low in comparison to those previously reported in series involving open revision, Dr. Ballo noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
There was no mortality in this study. This is one of the largest series reported to date of laparoscopic revision of failed bariatric surgery. Most prior studies have involved 30-100 patients, according to Dr. Ballo.
In the 1990s, roughly 13,000 bariatric procedures were performed annually in the United States. Today that figure is in excess of 200,000 annually.
Dr. Ballo reported having no financial conflicts with regard to this study.
LAS VEGAS– As the volume of bariatric surgery climbs sharply in response to the obesity epidemic, the need for revision procedures due to weight regain is also on the rise.
Laparoscopic revision bariatric surgery, while more technically challenging, is safe and effective, and it entails less morbidity than typically seen with open revisions, Dr. Rana M. Ballo said at the annual Minimally Invasive Surgery Week.
Dr. Ballo, a fifth-year general surgery resident at Rush University Medical Center in Chicago, presented a retrospective single-center study involving 227 patients who during 2001-2011 underwent laparoscopic revision of bariatric procedures that had failed because of weight regain. The goal of the revision bariatric surgery was to restore the restrictive component and/or add a malabsorptive component in order to improve long-term weight loss.
The patients fell into four groups. Group 1 consisted of 53 patients who initially had a laparoscopic adjustable gastric band procedure which was converted to a gastric bypass. Group 2, the largest group, initially had a Roux-en-Y gastric bypass in which the pouch eventually became dilated, which is the No. 1 cause of failure of this operation in the literature; their revision surgery entailed laparoscopic pouch reduction. The 38 patients who comprised Group 3 had a Roux-en-Y gastric bypass with subsequent pouch reduction and elongation of the biliopancreatic limb. Group 4 consisted of 17 patients who initially had a vertical banded gastroplasty – a procedure with a restrictive component only – and subsequently underwent laparoscopic conversion to a gastric bypass.
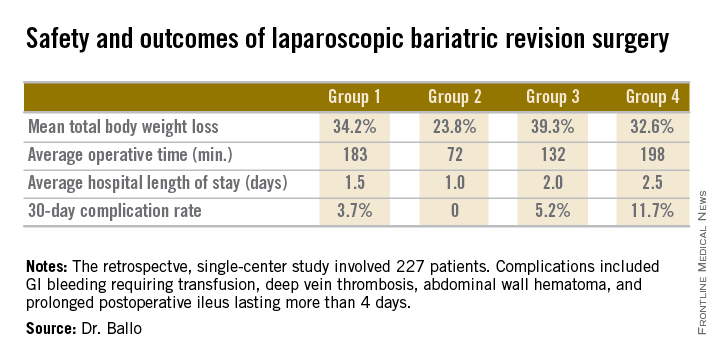
After a median follow-up of 3.9 years, Group 2 had significantly less total body weight loss than the rest of the groups, all of which had similar weight losses. On the other hand, Group 2 also had a shorter operative time and briefer average hospital length of stay than the other three groups, and it was the only group with zero complications. Still, the lengths of stay and 30-day morbidity rates across the board in this laparoscopic revision series were impressively low in comparison to those previously reported in series involving open revision, Dr. Ballo noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
There was no mortality in this study. This is one of the largest series reported to date of laparoscopic revision of failed bariatric surgery. Most prior studies have involved 30-100 patients, according to Dr. Ballo.
In the 1990s, roughly 13,000 bariatric procedures were performed annually in the United States. Today that figure is in excess of 200,000 annually.
Dr. Ballo reported having no financial conflicts with regard to this study.
LAS VEGAS– As the volume of bariatric surgery climbs sharply in response to the obesity epidemic, the need for revision procedures due to weight regain is also on the rise.
Laparoscopic revision bariatric surgery, while more technically challenging, is safe and effective, and it entails less morbidity than typically seen with open revisions, Dr. Rana M. Ballo said at the annual Minimally Invasive Surgery Week.
Dr. Ballo, a fifth-year general surgery resident at Rush University Medical Center in Chicago, presented a retrospective single-center study involving 227 patients who during 2001-2011 underwent laparoscopic revision of bariatric procedures that had failed because of weight regain. The goal of the revision bariatric surgery was to restore the restrictive component and/or add a malabsorptive component in order to improve long-term weight loss.
The patients fell into four groups. Group 1 consisted of 53 patients who initially had a laparoscopic adjustable gastric band procedure which was converted to a gastric bypass. Group 2, the largest group, initially had a Roux-en-Y gastric bypass in which the pouch eventually became dilated, which is the No. 1 cause of failure of this operation in the literature; their revision surgery entailed laparoscopic pouch reduction. The 38 patients who comprised Group 3 had a Roux-en-Y gastric bypass with subsequent pouch reduction and elongation of the biliopancreatic limb. Group 4 consisted of 17 patients who initially had a vertical banded gastroplasty – a procedure with a restrictive component only – and subsequently underwent laparoscopic conversion to a gastric bypass.
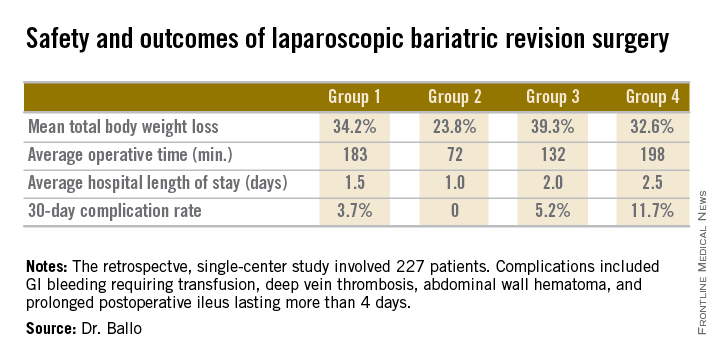
After a median follow-up of 3.9 years, Group 2 had significantly less total body weight loss than the rest of the groups, all of which had similar weight losses. On the other hand, Group 2 also had a shorter operative time and briefer average hospital length of stay than the other three groups, and it was the only group with zero complications. Still, the lengths of stay and 30-day morbidity rates across the board in this laparoscopic revision series were impressively low in comparison to those previously reported in series involving open revision, Dr. Ballo noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
There was no mortality in this study. This is one of the largest series reported to date of laparoscopic revision of failed bariatric surgery. Most prior studies have involved 30-100 patients, according to Dr. Ballo.
In the 1990s, roughly 13,000 bariatric procedures were performed annually in the United States. Today that figure is in excess of 200,000 annually.
Dr. Ballo reported having no financial conflicts with regard to this study.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Laparoscopic revision of failed bariatric surgery is safe and effective.
Major finding: Patients experienced a mean total body weight loss of 24%-39% at a median of 3.9 years after laparoscopic revision of failed bariatric surgery. The weight loss depended upon the primary procedure and type of revision.
Data source: This was a retrospective single-center series involving 227 patients who underwent laparoscopic revisional bariatric surgery in response to weight regain.
Disclosures: The presenter reported having no financial conflicts regarding this study.
Rethinking the postop patient-surgeon visit
LAS VEGAS– Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a possible alternative to the traditional surgeon-patient clinic visit, a pilot study indicates.
“It is feasible and seems effective. It is well received by patients, and it’s especially attractive for patients traveling long distances to receive their medical care. It may well prove to be the most efficient method for follow-up after laparoscopic inguinal hernia repair. It frees up clinic time: More than 80% of patients in our study were spared a clinic visit, and this allowed us to increase the number of our outpatient encounters,” Dr. Dan Eisenberg said at the annual Minimally Invasive Surgery Week.
He presented a prospective study of 62 consecutive patients who underwent laparoscopic inguinal hernia repair at the Veterans Affairs Palo Alto (Calif.) Health Care System and agreed to follow-up by a physician assistant 2-3 weeks after surgery in lieu of the traditional face-to-face clinic visit with the surgeon. The phone interview involved a predetermined nine-question script. A single “yes” answer prompted an appointment for a clinic visit.
Of the 62 patients, 3 were lost to follow-up. Because of a scheduling error, another four showed up at the VA clinic for a follow-up visit before the planned phone call. Of the remaining 55 patients, 50 (91%) were satisfied with their telephone follow-up experience.
Five patients were seen face to face at the clinic as a result of their telephone follow-up. Three did so because of self-limited groin discomfort, one for a large seroma, and one for early hernia recurrence treated by the total extraperitoneal approach, reported Dr. Eisenberg, a general surgeon at the Palo Alto VA.
Session chair Vincenzo Neri voiced a misgiving about the study.
“The only problem I see is that it contributes to the dehumanization of surgery,” commented Dr. Neri, professor and director of the division of general surgery at the University of Foggia (Italy). “The follow-up contact that you have in the clinic when you actually see the patient can be important because so many things can happen to the patient that he has no awareness of. Your way, the follow-up is basically gone.”
Dr. Eisenberg was quick to concur that the patient-surgeon relationship is basic to clinical medicine, and that the postop clinic visit is a fundamental part of this relationship.
“It is unfortunate to see that in the U.S., external constraints are changing the way we practice medicine,” he added, “but these external pressures are demanding more time efficiency and more resource efficiency, ultimately culminating, hopefully, in cost efficiency. The VA system is single payer. At the Palo Alto VA, we’ve noticed an increase in resource constraint limiting clinic access, and financial constraints going along with it.”
The Palo Alto VA Health Care System serves an enormous geographic area running north to the Oregon border and east into Nevada. The average roundtrip distance to the VA hospital for the study participants was 122 miles, and they were happy to forgo the journey.
“In Bay Area traffic, that corresponds to 3 to 3 1/2 hours on the road,” Dr. Eisenberg noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
His future research plans include randomizing patients to telephone follow-up or a face-to-face clinic visit after laparoscopic inguinal hernia repair in order to quantify the impact of the novel alternative on clinic flow and patient satisfaction. He also plans to extend the practice of telephone follow-up by a midlevel provider to other surgical procedures. He and his coworkers have already applied it to patients after laparoscopic cholecystectomy, where it also appears to be safe and efficient.
“It raises the question of how much further we can push this. Maybe it doesn’t have to be just for outpatient surgery,” according to Dr. Eisenberg.
Dr. Eisenberg reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
The nine yes/no telephone follow-up questions
Do you feel unwell?
Are you requiring frequent analgesics?
Are you having trouble returning to your normal activities?
Do you have fever or chills?
Is there increasing redness or swelling at the incision site?
Do you have testicular swelling or pain?
Are you having trouble tolerating a regular diet?
Do you have any concerns?
Would you like a face-to-face clinic visit?
A “yes” answer to any of the above triggers a clinic visit.
Source: Dr. Eisenberg
LAS VEGAS– Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a possible alternative to the traditional surgeon-patient clinic visit, a pilot study indicates.
“It is feasible and seems effective. It is well received by patients, and it’s especially attractive for patients traveling long distances to receive their medical care. It may well prove to be the most efficient method for follow-up after laparoscopic inguinal hernia repair. It frees up clinic time: More than 80% of patients in our study were spared a clinic visit, and this allowed us to increase the number of our outpatient encounters,” Dr. Dan Eisenberg said at the annual Minimally Invasive Surgery Week.
He presented a prospective study of 62 consecutive patients who underwent laparoscopic inguinal hernia repair at the Veterans Affairs Palo Alto (Calif.) Health Care System and agreed to follow-up by a physician assistant 2-3 weeks after surgery in lieu of the traditional face-to-face clinic visit with the surgeon. The phone interview involved a predetermined nine-question script. A single “yes” answer prompted an appointment for a clinic visit.
Of the 62 patients, 3 were lost to follow-up. Because of a scheduling error, another four showed up at the VA clinic for a follow-up visit before the planned phone call. Of the remaining 55 patients, 50 (91%) were satisfied with their telephone follow-up experience.
Five patients were seen face to face at the clinic as a result of their telephone follow-up. Three did so because of self-limited groin discomfort, one for a large seroma, and one for early hernia recurrence treated by the total extraperitoneal approach, reported Dr. Eisenberg, a general surgeon at the Palo Alto VA.
Session chair Vincenzo Neri voiced a misgiving about the study.
“The only problem I see is that it contributes to the dehumanization of surgery,” commented Dr. Neri, professor and director of the division of general surgery at the University of Foggia (Italy). “The follow-up contact that you have in the clinic when you actually see the patient can be important because so many things can happen to the patient that he has no awareness of. Your way, the follow-up is basically gone.”
Dr. Eisenberg was quick to concur that the patient-surgeon relationship is basic to clinical medicine, and that the postop clinic visit is a fundamental part of this relationship.
“It is unfortunate to see that in the U.S., external constraints are changing the way we practice medicine,” he added, “but these external pressures are demanding more time efficiency and more resource efficiency, ultimately culminating, hopefully, in cost efficiency. The VA system is single payer. At the Palo Alto VA, we’ve noticed an increase in resource constraint limiting clinic access, and financial constraints going along with it.”
The Palo Alto VA Health Care System serves an enormous geographic area running north to the Oregon border and east into Nevada. The average roundtrip distance to the VA hospital for the study participants was 122 miles, and they were happy to forgo the journey.
“In Bay Area traffic, that corresponds to 3 to 3 1/2 hours on the road,” Dr. Eisenberg noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
His future research plans include randomizing patients to telephone follow-up or a face-to-face clinic visit after laparoscopic inguinal hernia repair in order to quantify the impact of the novel alternative on clinic flow and patient satisfaction. He also plans to extend the practice of telephone follow-up by a midlevel provider to other surgical procedures. He and his coworkers have already applied it to patients after laparoscopic cholecystectomy, where it also appears to be safe and efficient.
“It raises the question of how much further we can push this. Maybe it doesn’t have to be just for outpatient surgery,” according to Dr. Eisenberg.
Dr. Eisenberg reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
The nine yes/no telephone follow-up questions
Do you feel unwell?
Are you requiring frequent analgesics?
Are you having trouble returning to your normal activities?
Do you have fever or chills?
Is there increasing redness or swelling at the incision site?
Do you have testicular swelling or pain?
Are you having trouble tolerating a regular diet?
Do you have any concerns?
Would you like a face-to-face clinic visit?
A “yes” answer to any of the above triggers a clinic visit.
Source: Dr. Eisenberg
LAS VEGAS– Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a possible alternative to the traditional surgeon-patient clinic visit, a pilot study indicates.
“It is feasible and seems effective. It is well received by patients, and it’s especially attractive for patients traveling long distances to receive their medical care. It may well prove to be the most efficient method for follow-up after laparoscopic inguinal hernia repair. It frees up clinic time: More than 80% of patients in our study were spared a clinic visit, and this allowed us to increase the number of our outpatient encounters,” Dr. Dan Eisenberg said at the annual Minimally Invasive Surgery Week.
He presented a prospective study of 62 consecutive patients who underwent laparoscopic inguinal hernia repair at the Veterans Affairs Palo Alto (Calif.) Health Care System and agreed to follow-up by a physician assistant 2-3 weeks after surgery in lieu of the traditional face-to-face clinic visit with the surgeon. The phone interview involved a predetermined nine-question script. A single “yes” answer prompted an appointment for a clinic visit.
Of the 62 patients, 3 were lost to follow-up. Because of a scheduling error, another four showed up at the VA clinic for a follow-up visit before the planned phone call. Of the remaining 55 patients, 50 (91%) were satisfied with their telephone follow-up experience.
Five patients were seen face to face at the clinic as a result of their telephone follow-up. Three did so because of self-limited groin discomfort, one for a large seroma, and one for early hernia recurrence treated by the total extraperitoneal approach, reported Dr. Eisenberg, a general surgeon at the Palo Alto VA.
Session chair Vincenzo Neri voiced a misgiving about the study.
“The only problem I see is that it contributes to the dehumanization of surgery,” commented Dr. Neri, professor and director of the division of general surgery at the University of Foggia (Italy). “The follow-up contact that you have in the clinic when you actually see the patient can be important because so many things can happen to the patient that he has no awareness of. Your way, the follow-up is basically gone.”
Dr. Eisenberg was quick to concur that the patient-surgeon relationship is basic to clinical medicine, and that the postop clinic visit is a fundamental part of this relationship.
“It is unfortunate to see that in the U.S., external constraints are changing the way we practice medicine,” he added, “but these external pressures are demanding more time efficiency and more resource efficiency, ultimately culminating, hopefully, in cost efficiency. The VA system is single payer. At the Palo Alto VA, we’ve noticed an increase in resource constraint limiting clinic access, and financial constraints going along with it.”
The Palo Alto VA Health Care System serves an enormous geographic area running north to the Oregon border and east into Nevada. The average roundtrip distance to the VA hospital for the study participants was 122 miles, and they were happy to forgo the journey.
“In Bay Area traffic, that corresponds to 3 to 3 1/2 hours on the road,” Dr. Eisenberg noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
His future research plans include randomizing patients to telephone follow-up or a face-to-face clinic visit after laparoscopic inguinal hernia repair in order to quantify the impact of the novel alternative on clinic flow and patient satisfaction. He also plans to extend the practice of telephone follow-up by a midlevel provider to other surgical procedures. He and his coworkers have already applied it to patients after laparoscopic cholecystectomy, where it also appears to be safe and efficient.
“It raises the question of how much further we can push this. Maybe it doesn’t have to be just for outpatient surgery,” according to Dr. Eisenberg.
Dr. Eisenberg reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
The nine yes/no telephone follow-up questions
Do you feel unwell?
Are you requiring frequent analgesics?
Are you having trouble returning to your normal activities?
Do you have fever or chills?
Is there increasing redness or swelling at the incision site?
Do you have testicular swelling or pain?
Are you having trouble tolerating a regular diet?
Do you have any concerns?
Would you like a face-to-face clinic visit?
A “yes” answer to any of the above triggers a clinic visit.
Source: Dr. Eisenberg
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Scripted telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a safe, effective, and resource-sparing alternative to the traditional face-to-face surgeon-patient follow-up visit.
Major finding: Fifty of 55 patients who underwent laparoscopic inguinal hernia repair were safely able to be spared a follow-up clinic visit as a result of telephone follow-up by a physician assistant several weeks after surgery.
Data source: This was a prospective observational study in which patients who had laparoscopic repair of an inguinal hernia agreed to a scripted telephone follow-up by a physician assistant instead of returning to the clinic for the traditional surgeon-patient face-to-face encounter.
Disclosures: The presenter reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
Antimicrobial use varies across hospital units
Patients in surgical critical care units were most likely to receive antimicrobial medication, while those in nursery wards were least likely to receive it, according to a recent study.
Nearly 78% of patients who used a surgical critical care unit (CCU) received antimicrobials in 2011, with 71% of patients in medical-surgical pediatric CCUs receiving antimicrobials and patients in cardiothoracic CCUs receiving antimicrobials at a 68% rate, according to Dr. Shelley S. Magill of the Centers for Disease Control and Prevention, Atlanta, and her associates (JAMA 2014;312:1438-46).
With only 3% of patients receiving antimicrobials, nursery wards had the lowest rate of medication, with labor, delivery, recovery, and postpartum wards giving antimicrobials to 20% of patients and 22% of patients receiving antimicrobials in special care nurseries, they reported.
Of the 5,635 patients who received antimicrobials, 4,278 received them for the treatment of infection. Lower respiratory tract infections were the most commonly treated type of infection, with 35% of patients receiving antimicrobials. Urinary tract and skin and soft tissue infections also were commonly treated with antimicrobials at a rate of 22% and 16%, respectively.
Overall (including prophylaxis,noninfection-related reasons, and undocumented rationale), vancomycin was the most commonly received antimicrobial, followed by cefazolin and ceftriaxone, according to Dr. Magill and her associates.
The study used data collected during 1-day prevalence surveys at 183 U.S. acute care hospitals and involving 11,282 patients.

Patients in surgical critical care units were most likely to receive antimicrobial medication, while those in nursery wards were least likely to receive it, according to a recent study.
Nearly 78% of patients who used a surgical critical care unit (CCU) received antimicrobials in 2011, with 71% of patients in medical-surgical pediatric CCUs receiving antimicrobials and patients in cardiothoracic CCUs receiving antimicrobials at a 68% rate, according to Dr. Shelley S. Magill of the Centers for Disease Control and Prevention, Atlanta, and her associates (JAMA 2014;312:1438-46).
With only 3% of patients receiving antimicrobials, nursery wards had the lowest rate of medication, with labor, delivery, recovery, and postpartum wards giving antimicrobials to 20% of patients and 22% of patients receiving antimicrobials in special care nurseries, they reported.
Of the 5,635 patients who received antimicrobials, 4,278 received them for the treatment of infection. Lower respiratory tract infections were the most commonly treated type of infection, with 35% of patients receiving antimicrobials. Urinary tract and skin and soft tissue infections also were commonly treated with antimicrobials at a rate of 22% and 16%, respectively.
Overall (including prophylaxis,noninfection-related reasons, and undocumented rationale), vancomycin was the most commonly received antimicrobial, followed by cefazolin and ceftriaxone, according to Dr. Magill and her associates.
The study used data collected during 1-day prevalence surveys at 183 U.S. acute care hospitals and involving 11,282 patients.

Patients in surgical critical care units were most likely to receive antimicrobial medication, while those in nursery wards were least likely to receive it, according to a recent study.
Nearly 78% of patients who used a surgical critical care unit (CCU) received antimicrobials in 2011, with 71% of patients in medical-surgical pediatric CCUs receiving antimicrobials and patients in cardiothoracic CCUs receiving antimicrobials at a 68% rate, according to Dr. Shelley S. Magill of the Centers for Disease Control and Prevention, Atlanta, and her associates (JAMA 2014;312:1438-46).
With only 3% of patients receiving antimicrobials, nursery wards had the lowest rate of medication, with labor, delivery, recovery, and postpartum wards giving antimicrobials to 20% of patients and 22% of patients receiving antimicrobials in special care nurseries, they reported.
Of the 5,635 patients who received antimicrobials, 4,278 received them for the treatment of infection. Lower respiratory tract infections were the most commonly treated type of infection, with 35% of patients receiving antimicrobials. Urinary tract and skin and soft tissue infections also were commonly treated with antimicrobials at a rate of 22% and 16%, respectively.
Overall (including prophylaxis,noninfection-related reasons, and undocumented rationale), vancomycin was the most commonly received antimicrobial, followed by cefazolin and ceftriaxone, according to Dr. Magill and her associates.
The study used data collected during 1-day prevalence surveys at 183 U.S. acute care hospitals and involving 11,282 patients.

FROM JAMA
When to use mesh in laparoscopic hiatal hernia repair
LAS VEGAS – Routine use of mesh reinforcement when performing laparoscopic repair of hiatal hernia defects 5 cm or larger in diameter is associated with a low recurrence rate, Dr. Chetan V. Aher reported at the annual Minimally Invasive Surgery Week.
His coinvestigators had shown in an earlier randomized controlled trial that mesh reinforcement of primary cruroplasty in patients with a hernia of 8 cm or greater was associated with no recurrences. Repair with simple cruroplasty was associated with a 22% recurrence rate (Arch. Surg. 2002;137:649-52).
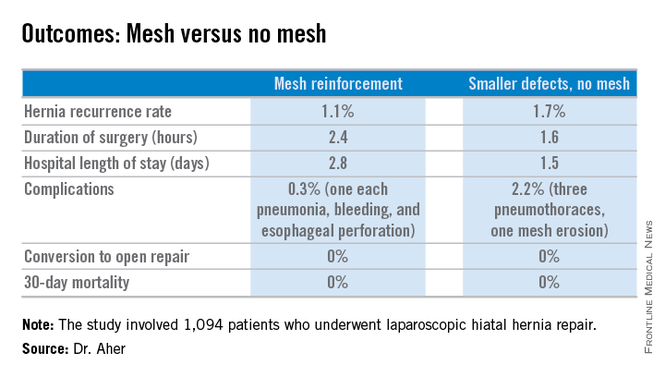
However, Dr. Aher and his coinvestigators subsequently observed a high recurrence rate following mesh-free simple cruroplasty for defects in the 5- to 8-cm range. He presented a case series involving 1,094 laparoscopic hiatal hernia repairs performed since he and his colleagues changed their practice by lowering their threshold for polytetrafluoroethylene mesh reinforcement to defects of at least 5 cm from their prior standard of 8 cm or more.
Hernias were less than 5 cm in diameter in 84% of the patients, so mesh wasn’t used for those repairs. In the remaining 178 patients – those with hernias of at least 5 cm – PTFE mesh was utilized to circumferentially reinforce the cruroplasty.
During a mean follow-up of 3.1 years, the hernia recurrence rate was 1.7% in the group with hernia defects of less than 5 cm and similar at 1.1% in those who received mesh reinforcement because their hernias were larger, reported Dr. Aher of Rush University Medical Center in Chicago.
Operative time and length of stay were longer in the mesh reinforcement group (see chart).
“There’s more dissection when using mesh, and obviously the placement of the mesh takes a little longer,” he noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
All repairs were performed using cruroplasty with interrupted nonabsorbable sutures approximating the right and left bundles of the right crura.
Laparoscopic repair has become the standard approach in the primary repair of hiatal hernias. In a 2010 survey of members of the Society of Gastrointestinal and Endoscopic Surgeons conducted by Dr. Aher’s colleagues, respondents indicated they laparoscopically performed 77% of their mesh-reinforced repairs. However, the survey results underscored a lack of consensus within the surgical community regarding mesh usage. Biologic mesh was used by 28% of surgeons; 25% used PTFE (polytetrafluoroethylene), and 21% polypropylene. Mesh placement practices also varied widely: 14% of surgeons utilized anterior placement, 34% posterior, and only 10% circumferential (Surg. Endosc. 2010;24:1017-24).
Asked how he counsels patients about the competing risks of mesh erosion and hernia recurrence in the absence of mesh reinforcement, Dr. Aher pointed to the 22% recurrence risk with large hernias in the earlier randomized trial.
“I would counsel my own family that if you have a large hernia, the risk of mesh erosion is very low and the risk of undergoing a recurrent operation if there is no mesh reinforcement is, I think, overall higher. So I would say they should get the mesh reinforcement,” he concluded.
Dr. Aher reported having no financial conflicts regarding this study.
LAS VEGAS – Routine use of mesh reinforcement when performing laparoscopic repair of hiatal hernia defects 5 cm or larger in diameter is associated with a low recurrence rate, Dr. Chetan V. Aher reported at the annual Minimally Invasive Surgery Week.
His coinvestigators had shown in an earlier randomized controlled trial that mesh reinforcement of primary cruroplasty in patients with a hernia of 8 cm or greater was associated with no recurrences. Repair with simple cruroplasty was associated with a 22% recurrence rate (Arch. Surg. 2002;137:649-52).
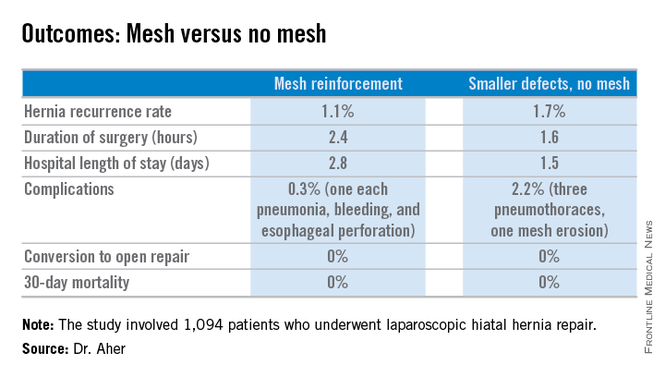
However, Dr. Aher and his coinvestigators subsequently observed a high recurrence rate following mesh-free simple cruroplasty for defects in the 5- to 8-cm range. He presented a case series involving 1,094 laparoscopic hiatal hernia repairs performed since he and his colleagues changed their practice by lowering their threshold for polytetrafluoroethylene mesh reinforcement to defects of at least 5 cm from their prior standard of 8 cm or more.
Hernias were less than 5 cm in diameter in 84% of the patients, so mesh wasn’t used for those repairs. In the remaining 178 patients – those with hernias of at least 5 cm – PTFE mesh was utilized to circumferentially reinforce the cruroplasty.
During a mean follow-up of 3.1 years, the hernia recurrence rate was 1.7% in the group with hernia defects of less than 5 cm and similar at 1.1% in those who received mesh reinforcement because their hernias were larger, reported Dr. Aher of Rush University Medical Center in Chicago.
Operative time and length of stay were longer in the mesh reinforcement group (see chart).
“There’s more dissection when using mesh, and obviously the placement of the mesh takes a little longer,” he noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
All repairs were performed using cruroplasty with interrupted nonabsorbable sutures approximating the right and left bundles of the right crura.
Laparoscopic repair has become the standard approach in the primary repair of hiatal hernias. In a 2010 survey of members of the Society of Gastrointestinal and Endoscopic Surgeons conducted by Dr. Aher’s colleagues, respondents indicated they laparoscopically performed 77% of their mesh-reinforced repairs. However, the survey results underscored a lack of consensus within the surgical community regarding mesh usage. Biologic mesh was used by 28% of surgeons; 25% used PTFE (polytetrafluoroethylene), and 21% polypropylene. Mesh placement practices also varied widely: 14% of surgeons utilized anterior placement, 34% posterior, and only 10% circumferential (Surg. Endosc. 2010;24:1017-24).
Asked how he counsels patients about the competing risks of mesh erosion and hernia recurrence in the absence of mesh reinforcement, Dr. Aher pointed to the 22% recurrence risk with large hernias in the earlier randomized trial.
“I would counsel my own family that if you have a large hernia, the risk of mesh erosion is very low and the risk of undergoing a recurrent operation if there is no mesh reinforcement is, I think, overall higher. So I would say they should get the mesh reinforcement,” he concluded.
Dr. Aher reported having no financial conflicts regarding this study.
LAS VEGAS – Routine use of mesh reinforcement when performing laparoscopic repair of hiatal hernia defects 5 cm or larger in diameter is associated with a low recurrence rate, Dr. Chetan V. Aher reported at the annual Minimally Invasive Surgery Week.
His coinvestigators had shown in an earlier randomized controlled trial that mesh reinforcement of primary cruroplasty in patients with a hernia of 8 cm or greater was associated with no recurrences. Repair with simple cruroplasty was associated with a 22% recurrence rate (Arch. Surg. 2002;137:649-52).
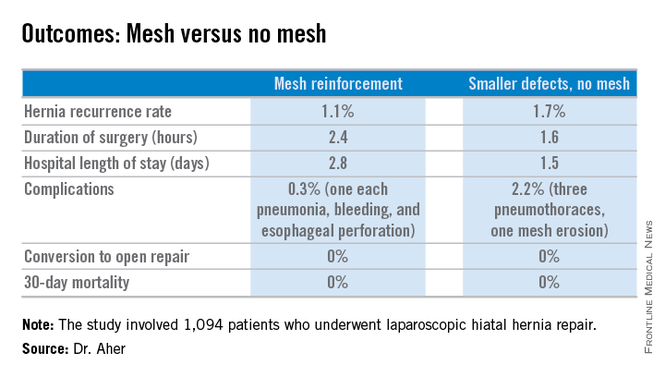
However, Dr. Aher and his coinvestigators subsequently observed a high recurrence rate following mesh-free simple cruroplasty for defects in the 5- to 8-cm range. He presented a case series involving 1,094 laparoscopic hiatal hernia repairs performed since he and his colleagues changed their practice by lowering their threshold for polytetrafluoroethylene mesh reinforcement to defects of at least 5 cm from their prior standard of 8 cm or more.
Hernias were less than 5 cm in diameter in 84% of the patients, so mesh wasn’t used for those repairs. In the remaining 178 patients – those with hernias of at least 5 cm – PTFE mesh was utilized to circumferentially reinforce the cruroplasty.
During a mean follow-up of 3.1 years, the hernia recurrence rate was 1.7% in the group with hernia defects of less than 5 cm and similar at 1.1% in those who received mesh reinforcement because their hernias were larger, reported Dr. Aher of Rush University Medical Center in Chicago.
Operative time and length of stay were longer in the mesh reinforcement group (see chart).
“There’s more dissection when using mesh, and obviously the placement of the mesh takes a little longer,” he noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
All repairs were performed using cruroplasty with interrupted nonabsorbable sutures approximating the right and left bundles of the right crura.
Laparoscopic repair has become the standard approach in the primary repair of hiatal hernias. In a 2010 survey of members of the Society of Gastrointestinal and Endoscopic Surgeons conducted by Dr. Aher’s colleagues, respondents indicated they laparoscopically performed 77% of their mesh-reinforced repairs. However, the survey results underscored a lack of consensus within the surgical community regarding mesh usage. Biologic mesh was used by 28% of surgeons; 25% used PTFE (polytetrafluoroethylene), and 21% polypropylene. Mesh placement practices also varied widely: 14% of surgeons utilized anterior placement, 34% posterior, and only 10% circumferential (Surg. Endosc. 2010;24:1017-24).
Asked how he counsels patients about the competing risks of mesh erosion and hernia recurrence in the absence of mesh reinforcement, Dr. Aher pointed to the 22% recurrence risk with large hernias in the earlier randomized trial.
“I would counsel my own family that if you have a large hernia, the risk of mesh erosion is very low and the risk of undergoing a recurrent operation if there is no mesh reinforcement is, I think, overall higher. So I would say they should get the mesh reinforcement,” he concluded.
Dr. Aher reported having no financial conflicts regarding this study.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Using hernia defect size to guide selective use of mesh reinforcement in laparoscopic hiatal hernia repair results in a low recurrence rate and excellent safety.
Major finding: The hernia recurrence rate was 1.7% in patients who underwent primary cruroplasty for hernias less than 5 cm in diameter and 1.1% in those who received mesh reinforcement because their hernias exceeded that size.
Data source: This was a retrospective study of 1,094 patients who underwent laparoscopic hiatal hernia repair since the investigators changed their threshold for utilizing mesh reinforcement from 8- to 5-cm hernia defects.
Disclosures: The presenter reported having no financial conflicts.