User login
When to use mesh in laparoscopic hiatal hernia repair
LAS VEGAS – Routine use of mesh reinforcement when performing laparoscopic repair of hiatal hernia defects 5 cm or larger in diameter is associated with a low recurrence rate, Dr. Chetan V. Aher reported at the annual Minimally Invasive Surgery Week.
His coinvestigators had shown in an earlier randomized controlled trial that mesh reinforcement of primary cruroplasty in patients with a hernia of 8 cm or greater was associated with no recurrences. Repair with simple cruroplasty was associated with a 22% recurrence rate (Arch. Surg. 2002;137:649-52).
However, Dr. Aher and his coinvestigators subsequently observed a high recurrence rate following mesh-free simple cruroplasty for defects in the 5- to 8-cm range. He presented a case series involving 1,094 laparoscopic hiatal hernia repairs performed since he and his colleagues changed their practice by lowering their threshold for polytetrafluoroethylene mesh reinforcement to defects of at least 5 cm from their prior standard of 8 cm or more.
Hernias were less than 5 cm in diameter in 84% of the patients, so mesh wasn’t used for those repairs. In the remaining 178 patients – those with hernias of at least 5 cm – PTFE mesh was utilized to circumferentially reinforce the cruroplasty.
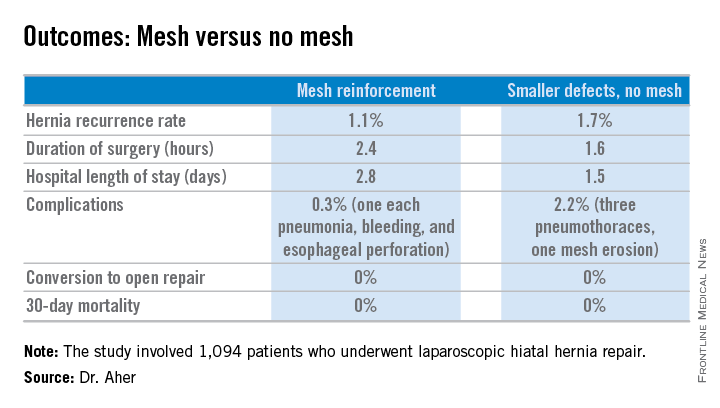
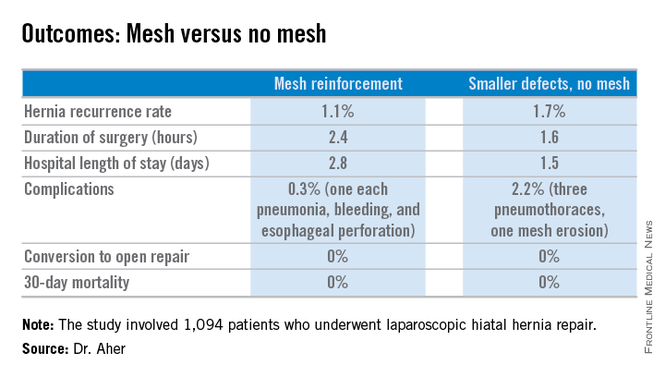
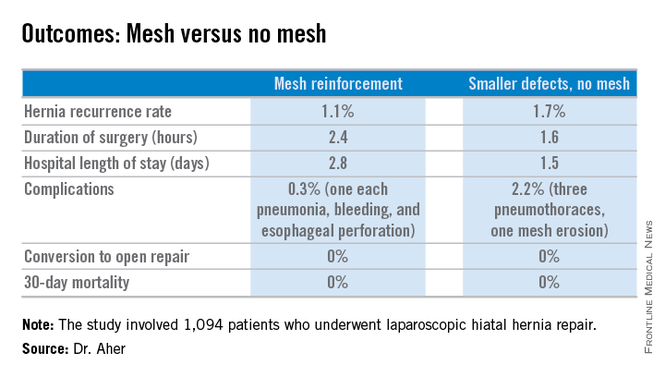
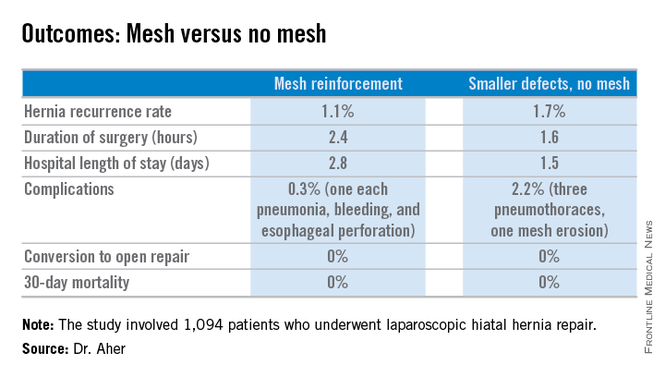
During a mean follow-up of 3.1 years, the hernia recurrence rate was 1.7% in the group with hernia defects of less than 5 cm and similar at 1.1% in those who received mesh reinforcement because their hernias were larger, reported Dr. Aher of Rush University Medical Center in Chicago.
Operative time and length of stay were longer in the mesh reinforcement group (see chart).
“There’s more dissection when using mesh, and obviously the placement of the mesh takes a little longer,” he noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
All repairs were performed using cruroplasty with interrupted nonabsorbable sutures approximating the right and left bundles of the right crura.
Laparoscopic repair has become the standard approach in the primary repair of hiatal hernias. In a 2010 survey of members of the Society of Gastrointestinal and Endoscopic Surgeons conducted by Dr. Aher’s colleagues, respondents indicated they laparoscopically performed 77% of their mesh-reinforced repairs. However, the survey results underscored a lack of consensus within the surgical community regarding mesh usage. Biologic mesh was used by 28% of surgeons; 25% used PTFE (polytetrafluoroethylene), and 21% polypropylene. Mesh placement practices also varied widely: 14% of surgeons utilized anterior placement, 34% posterior, and only 10% circumferential (Surg. Endosc. 2010;24:1017-24).
Asked how he counsels patients about the competing risks of mesh erosion and hernia recurrence in the absence of mesh reinforcement, Dr. Aher pointed to the 22% recurrence risk with large hernias in the earlier randomized trial.
“I would counsel my own family that if you have a large hernia, the risk of mesh erosion is very low and the risk of undergoing a recurrent operation if there is no mesh reinforcement is, I think, overall higher. So I would say they should get the mesh reinforcement,” he concluded.
Dr. Aher reported having no financial conflicts regarding this study.
LAS VEGAS – Routine use of mesh reinforcement when performing laparoscopic repair of hiatal hernia defects 5 cm or larger in diameter is associated with a low recurrence rate, Dr. Chetan V. Aher reported at the annual Minimally Invasive Surgery Week.
His coinvestigators had shown in an earlier randomized controlled trial that mesh reinforcement of primary cruroplasty in patients with a hernia of 8 cm or greater was associated with no recurrences. Repair with simple cruroplasty was associated with a 22% recurrence rate (Arch. Surg. 2002;137:649-52).
However, Dr. Aher and his coinvestigators subsequently observed a high recurrence rate following mesh-free simple cruroplasty for defects in the 5- to 8-cm range. He presented a case series involving 1,094 laparoscopic hiatal hernia repairs performed since he and his colleagues changed their practice by lowering their threshold for polytetrafluoroethylene mesh reinforcement to defects of at least 5 cm from their prior standard of 8 cm or more.
Hernias were less than 5 cm in diameter in 84% of the patients, so mesh wasn’t used for those repairs. In the remaining 178 patients – those with hernias of at least 5 cm – PTFE mesh was utilized to circumferentially reinforce the cruroplasty.
During a mean follow-up of 3.1 years, the hernia recurrence rate was 1.7% in the group with hernia defects of less than 5 cm and similar at 1.1% in those who received mesh reinforcement because their hernias were larger, reported Dr. Aher of Rush University Medical Center in Chicago.
Operative time and length of stay were longer in the mesh reinforcement group (see chart).
“There’s more dissection when using mesh, and obviously the placement of the mesh takes a little longer,” he noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
All repairs were performed using cruroplasty with interrupted nonabsorbable sutures approximating the right and left bundles of the right crura.
Laparoscopic repair has become the standard approach in the primary repair of hiatal hernias. In a 2010 survey of members of the Society of Gastrointestinal and Endoscopic Surgeons conducted by Dr. Aher’s colleagues, respondents indicated they laparoscopically performed 77% of their mesh-reinforced repairs. However, the survey results underscored a lack of consensus within the surgical community regarding mesh usage. Biologic mesh was used by 28% of surgeons; 25% used PTFE (polytetrafluoroethylene), and 21% polypropylene. Mesh placement practices also varied widely: 14% of surgeons utilized anterior placement, 34% posterior, and only 10% circumferential (Surg. Endosc. 2010;24:1017-24).
Asked how he counsels patients about the competing risks of mesh erosion and hernia recurrence in the absence of mesh reinforcement, Dr. Aher pointed to the 22% recurrence risk with large hernias in the earlier randomized trial.
“I would counsel my own family that if you have a large hernia, the risk of mesh erosion is very low and the risk of undergoing a recurrent operation if there is no mesh reinforcement is, I think, overall higher. So I would say they should get the mesh reinforcement,” he concluded.
Dr. Aher reported having no financial conflicts regarding this study.
LAS VEGAS – Routine use of mesh reinforcement when performing laparoscopic repair of hiatal hernia defects 5 cm or larger in diameter is associated with a low recurrence rate, Dr. Chetan V. Aher reported at the annual Minimally Invasive Surgery Week.
His coinvestigators had shown in an earlier randomized controlled trial that mesh reinforcement of primary cruroplasty in patients with a hernia of 8 cm or greater was associated with no recurrences. Repair with simple cruroplasty was associated with a 22% recurrence rate (Arch. Surg. 2002;137:649-52).
However, Dr. Aher and his coinvestigators subsequently observed a high recurrence rate following mesh-free simple cruroplasty for defects in the 5- to 8-cm range. He presented a case series involving 1,094 laparoscopic hiatal hernia repairs performed since he and his colleagues changed their practice by lowering their threshold for polytetrafluoroethylene mesh reinforcement to defects of at least 5 cm from their prior standard of 8 cm or more.
Hernias were less than 5 cm in diameter in 84% of the patients, so mesh wasn’t used for those repairs. In the remaining 178 patients – those with hernias of at least 5 cm – PTFE mesh was utilized to circumferentially reinforce the cruroplasty.
During a mean follow-up of 3.1 years, the hernia recurrence rate was 1.7% in the group with hernia defects of less than 5 cm and similar at 1.1% in those who received mesh reinforcement because their hernias were larger, reported Dr. Aher of Rush University Medical Center in Chicago.
Operative time and length of stay were longer in the mesh reinforcement group (see chart).
“There’s more dissection when using mesh, and obviously the placement of the mesh takes a little longer,” he noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
All repairs were performed using cruroplasty with interrupted nonabsorbable sutures approximating the right and left bundles of the right crura.
Laparoscopic repair has become the standard approach in the primary repair of hiatal hernias. In a 2010 survey of members of the Society of Gastrointestinal and Endoscopic Surgeons conducted by Dr. Aher’s colleagues, respondents indicated they laparoscopically performed 77% of their mesh-reinforced repairs. However, the survey results underscored a lack of consensus within the surgical community regarding mesh usage. Biologic mesh was used by 28% of surgeons; 25% used PTFE (polytetrafluoroethylene), and 21% polypropylene. Mesh placement practices also varied widely: 14% of surgeons utilized anterior placement, 34% posterior, and only 10% circumferential (Surg. Endosc. 2010;24:1017-24).
Asked how he counsels patients about the competing risks of mesh erosion and hernia recurrence in the absence of mesh reinforcement, Dr. Aher pointed to the 22% recurrence risk with large hernias in the earlier randomized trial.
“I would counsel my own family that if you have a large hernia, the risk of mesh erosion is very low and the risk of undergoing a recurrent operation if there is no mesh reinforcement is, I think, overall higher. So I would say they should get the mesh reinforcement,” he concluded.
Dr. Aher reported having no financial conflicts regarding this study.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Using hernia defect size to guide selective use of mesh reinforcement in laparoscopic hiatal hernia repair results in a low recurrence rate and excellent safety.
Major finding: The hernia recurrence rate was 1.7% in patients who underwent primary cruroplasty for hernias less than 5 cm in diameter and 1.1% in those who received mesh reinforcement because their hernias exceeded that size.
Data source: This was a retrospective study of 1,094 patients who underwent laparoscopic hiatal hernia repair since the investigators changed their threshold for utilizing mesh reinforcement from 8- to 5-cm hernia defects.
Disclosures: The presenter reported having no financial conflicts.
More docs need to use available Rx-monitoring programs to help curb opioid abuse
WASHINGTON – The prescription drug–monitoring programs that exist in every state are not going to make a dent in opioid abuse unless physicians use them.
Because each state governs its own prescription drug–monitoring program (PDMP), the efficiency and effectiveness of each varies widely from the others. In the ideal, a PDMP collects information on which prescriptions are being filled by what patients as well as which physicians are prescribing the drugs. Information from the databases is used to help determine which patients might be doctor shopping for opioids as well as identify physicians who might be operating “pill mills” and contributing to the availability of narcotic pain medication that is used for other than clinical purposes.
Data from several studies have shown that in many instances, doctors do not realize the detail and usefulness of data from PDMPs, Allan Coukell, senior director for drugs and medical devices at Pew Charitable Trusts, Washington, said at a panel discussion on prescription drug abuse hosted by the Alliance for Health Reform and the Pharmaceutical Care Management Association, the industry lobby for pharmacy benefit managers.
When shown data on a specific patient, a physician was often “surprised to know how many other physicians that patient was seeing, and having that information changed their prescribing,” Mr. Coukell said, noting that in some cases, the information led to physicians refusing to prescribe pain medication and in others, it eased fears that a patient might be doctor shopping, giving the physician some peace of mind about writing a prescription for a narcotic.
Panelist Dr. Sarah Chouinard, medical director of Community Care of West Virginia, noted that physicians often are surprised when presented with data collected by PDMPs about their own individual prescribing habits.
“Eight out of 10 people were very surprised at the number of hydrocodone prescriptions they had written in the last 3 months,” Dr. Chouinard said.
In addition, the culture of administering pain medicine has gone through a shift in the last 10 years that is contributing to the problem of how many pills are available.
“About 10 years ago, there were doctors wandering around with buttons that said ‘No Pain’ with a red circle and a line through it because we were accused of under treating pain,” she observed. “Now, the pendulum has swung in the opposite direction. They used to say, ‘Hey, we’ll get sued if we don’t write pain medicine for these people,’ and now it’s, ‘Gosh, don’t write anything, or we will be a pill mill.’ I think the real answer is getting back to the middle and allowing the word to be out there that you don’t have to use a narcotic for every bump.”
To that end, Dr. Chouinard shared a solution her community organization has implemented. She said that “none of the [family physicians] are equipped, myself included, to treat chronic pain. Chronic pain is a specialty. ... It requires special training. The training that we as family doctors get now, after residency, is a mandatory 3 hours every 2 years.”
So Community Health of West Virgina hired an anesthetist who is not interested in family medicine but rather has a special interest in addictions medicine and outpatient pain medicine.
“Every one of our patients who has chronic pain [is sent] to this physician first,” Dr. Chouinard explained. “He does the work-up. He looks to see if the patients are amenable to any kind of alternatives and then sends those patients back to us as primary care doctors.”
After that, every patient gets a pain contract that essentially provides consent to have urine tested on a regular basis to track adherence, as well as provide pill counts and office visits as required by the doctors. The physicians also are required to regularly check the PDMP database.
Patients who need this kind of treatment do not complain that the requirements are burdensome, said Dr. Chouinard, who described the program as successful overall. She said 30% have stayed properly adherent to their prescription narcotics and are living within the agreements of their contracts, while another 20% were taken off their medication because they were able to be placed on alternate, nonopioid therapies. About 30% ended up recommended for or enrolled in an addiction program, while 20% failed to maintain their contracts, and thus were unable to get their prescriptions.
Dr. Chouinard said a program like this could easily be rolled out across the country to help address the opioid abuse problem, as well as help remove primary care doctors from the prescribing loop.
“None of these people went into medicine because they had an interest in treating chronic pain,” she said.
In keeping with the overall message of getting doctors to use PDMPs more, Mr. Coukell said that getting this information integrated into electronic health records is “the Holy Grail,” though he added that getting practice alerts are a good short-term fix. He also said that getting consistency of reporting practice uniform across states and getting more states to trade information also was key, as is getting rules in place to allow someone in the office other than the doctor to have access to the PDMP databases (which some states do allow).
Centers for Disease Control and Prevention Director of the Division of Unintentional Injury Prevention Grant Baldwin, Ph.D., concurred.
“Providers have a limited amount of time to see patients,” Dr. Baldwin said. “Integrating all of these fixes will not necessarily extend the amount of time, but it actually makes it easier for the health care team to do their job in an efficient manner in that same 10-15 minute time."
WASHINGTON – The prescription drug–monitoring programs that exist in every state are not going to make a dent in opioid abuse unless physicians use them.
Because each state governs its own prescription drug–monitoring program (PDMP), the efficiency and effectiveness of each varies widely from the others. In the ideal, a PDMP collects information on which prescriptions are being filled by what patients as well as which physicians are prescribing the drugs. Information from the databases is used to help determine which patients might be doctor shopping for opioids as well as identify physicians who might be operating “pill mills” and contributing to the availability of narcotic pain medication that is used for other than clinical purposes.
Data from several studies have shown that in many instances, doctors do not realize the detail and usefulness of data from PDMPs, Allan Coukell, senior director for drugs and medical devices at Pew Charitable Trusts, Washington, said at a panel discussion on prescription drug abuse hosted by the Alliance for Health Reform and the Pharmaceutical Care Management Association, the industry lobby for pharmacy benefit managers.
When shown data on a specific patient, a physician was often “surprised to know how many other physicians that patient was seeing, and having that information changed their prescribing,” Mr. Coukell said, noting that in some cases, the information led to physicians refusing to prescribe pain medication and in others, it eased fears that a patient might be doctor shopping, giving the physician some peace of mind about writing a prescription for a narcotic.
Panelist Dr. Sarah Chouinard, medical director of Community Care of West Virginia, noted that physicians often are surprised when presented with data collected by PDMPs about their own individual prescribing habits.
“Eight out of 10 people were very surprised at the number of hydrocodone prescriptions they had written in the last 3 months,” Dr. Chouinard said.
In addition, the culture of administering pain medicine has gone through a shift in the last 10 years that is contributing to the problem of how many pills are available.
“About 10 years ago, there were doctors wandering around with buttons that said ‘No Pain’ with a red circle and a line through it because we were accused of under treating pain,” she observed. “Now, the pendulum has swung in the opposite direction. They used to say, ‘Hey, we’ll get sued if we don’t write pain medicine for these people,’ and now it’s, ‘Gosh, don’t write anything, or we will be a pill mill.’ I think the real answer is getting back to the middle and allowing the word to be out there that you don’t have to use a narcotic for every bump.”
To that end, Dr. Chouinard shared a solution her community organization has implemented. She said that “none of the [family physicians] are equipped, myself included, to treat chronic pain. Chronic pain is a specialty. ... It requires special training. The training that we as family doctors get now, after residency, is a mandatory 3 hours every 2 years.”
So Community Health of West Virgina hired an anesthetist who is not interested in family medicine but rather has a special interest in addictions medicine and outpatient pain medicine.
“Every one of our patients who has chronic pain [is sent] to this physician first,” Dr. Chouinard explained. “He does the work-up. He looks to see if the patients are amenable to any kind of alternatives and then sends those patients back to us as primary care doctors.”
After that, every patient gets a pain contract that essentially provides consent to have urine tested on a regular basis to track adherence, as well as provide pill counts and office visits as required by the doctors. The physicians also are required to regularly check the PDMP database.
Patients who need this kind of treatment do not complain that the requirements are burdensome, said Dr. Chouinard, who described the program as successful overall. She said 30% have stayed properly adherent to their prescription narcotics and are living within the agreements of their contracts, while another 20% were taken off their medication because they were able to be placed on alternate, nonopioid therapies. About 30% ended up recommended for or enrolled in an addiction program, while 20% failed to maintain their contracts, and thus were unable to get their prescriptions.
Dr. Chouinard said a program like this could easily be rolled out across the country to help address the opioid abuse problem, as well as help remove primary care doctors from the prescribing loop.
“None of these people went into medicine because they had an interest in treating chronic pain,” she said.
In keeping with the overall message of getting doctors to use PDMPs more, Mr. Coukell said that getting this information integrated into electronic health records is “the Holy Grail,” though he added that getting practice alerts are a good short-term fix. He also said that getting consistency of reporting practice uniform across states and getting more states to trade information also was key, as is getting rules in place to allow someone in the office other than the doctor to have access to the PDMP databases (which some states do allow).
Centers for Disease Control and Prevention Director of the Division of Unintentional Injury Prevention Grant Baldwin, Ph.D., concurred.
“Providers have a limited amount of time to see patients,” Dr. Baldwin said. “Integrating all of these fixes will not necessarily extend the amount of time, but it actually makes it easier for the health care team to do their job in an efficient manner in that same 10-15 minute time."
WASHINGTON – The prescription drug–monitoring programs that exist in every state are not going to make a dent in opioid abuse unless physicians use them.
Because each state governs its own prescription drug–monitoring program (PDMP), the efficiency and effectiveness of each varies widely from the others. In the ideal, a PDMP collects information on which prescriptions are being filled by what patients as well as which physicians are prescribing the drugs. Information from the databases is used to help determine which patients might be doctor shopping for opioids as well as identify physicians who might be operating “pill mills” and contributing to the availability of narcotic pain medication that is used for other than clinical purposes.
Data from several studies have shown that in many instances, doctors do not realize the detail and usefulness of data from PDMPs, Allan Coukell, senior director for drugs and medical devices at Pew Charitable Trusts, Washington, said at a panel discussion on prescription drug abuse hosted by the Alliance for Health Reform and the Pharmaceutical Care Management Association, the industry lobby for pharmacy benefit managers.
When shown data on a specific patient, a physician was often “surprised to know how many other physicians that patient was seeing, and having that information changed their prescribing,” Mr. Coukell said, noting that in some cases, the information led to physicians refusing to prescribe pain medication and in others, it eased fears that a patient might be doctor shopping, giving the physician some peace of mind about writing a prescription for a narcotic.
Panelist Dr. Sarah Chouinard, medical director of Community Care of West Virginia, noted that physicians often are surprised when presented with data collected by PDMPs about their own individual prescribing habits.
“Eight out of 10 people were very surprised at the number of hydrocodone prescriptions they had written in the last 3 months,” Dr. Chouinard said.
In addition, the culture of administering pain medicine has gone through a shift in the last 10 years that is contributing to the problem of how many pills are available.
“About 10 years ago, there were doctors wandering around with buttons that said ‘No Pain’ with a red circle and a line through it because we were accused of under treating pain,” she observed. “Now, the pendulum has swung in the opposite direction. They used to say, ‘Hey, we’ll get sued if we don’t write pain medicine for these people,’ and now it’s, ‘Gosh, don’t write anything, or we will be a pill mill.’ I think the real answer is getting back to the middle and allowing the word to be out there that you don’t have to use a narcotic for every bump.”
To that end, Dr. Chouinard shared a solution her community organization has implemented. She said that “none of the [family physicians] are equipped, myself included, to treat chronic pain. Chronic pain is a specialty. ... It requires special training. The training that we as family doctors get now, after residency, is a mandatory 3 hours every 2 years.”
So Community Health of West Virgina hired an anesthetist who is not interested in family medicine but rather has a special interest in addictions medicine and outpatient pain medicine.
“Every one of our patients who has chronic pain [is sent] to this physician first,” Dr. Chouinard explained. “He does the work-up. He looks to see if the patients are amenable to any kind of alternatives and then sends those patients back to us as primary care doctors.”
After that, every patient gets a pain contract that essentially provides consent to have urine tested on a regular basis to track adherence, as well as provide pill counts and office visits as required by the doctors. The physicians also are required to regularly check the PDMP database.
Patients who need this kind of treatment do not complain that the requirements are burdensome, said Dr. Chouinard, who described the program as successful overall. She said 30% have stayed properly adherent to their prescription narcotics and are living within the agreements of their contracts, while another 20% were taken off their medication because they were able to be placed on alternate, nonopioid therapies. About 30% ended up recommended for or enrolled in an addiction program, while 20% failed to maintain their contracts, and thus were unable to get their prescriptions.
Dr. Chouinard said a program like this could easily be rolled out across the country to help address the opioid abuse problem, as well as help remove primary care doctors from the prescribing loop.
“None of these people went into medicine because they had an interest in treating chronic pain,” she said.
In keeping with the overall message of getting doctors to use PDMPs more, Mr. Coukell said that getting this information integrated into electronic health records is “the Holy Grail,” though he added that getting practice alerts are a good short-term fix. He also said that getting consistency of reporting practice uniform across states and getting more states to trade information also was key, as is getting rules in place to allow someone in the office other than the doctor to have access to the PDMP databases (which some states do allow).
Centers for Disease Control and Prevention Director of the Division of Unintentional Injury Prevention Grant Baldwin, Ph.D., concurred.
“Providers have a limited amount of time to see patients,” Dr. Baldwin said. “Integrating all of these fixes will not necessarily extend the amount of time, but it actually makes it easier for the health care team to do their job in an efficient manner in that same 10-15 minute time."
AT A PEW CHARITABLE TRUSTS–HOSTED PANEL
High-dose treatment did not benefit ICU patients with vitamin D deficiency
High-dose vitamin D did not improve outcomes in critically ill, vitamin D–deficient patients, compared with placebo, researchers reported in JAMA and at the annual congress of the European Society of Intensive Care Medicine.
Although the study was adequately powered, length of stay did not differ between the vitamin D and placebo groups, said Dr. Karin Amrein of the Medical University of Graz, Austria, and her associates. “In the overall cohort, hospital and 6-month mortality rates were numerically lower in the vitamin D3 group, but these differences were not significant,” the researchers said.
A subgroup of patients with severe vitamin D deficiency did have significantly lower hospital mortality when treated with vitamin D, compared with placebo, but the effect “should be considered hypothesis generating and requires further study,” the investigators concluded (JAMA 2014 Sept. 29 [doi:10.1001/jama.2014.13204]).
The randomized, double-blind, single-center trial enrolled 492 critically ill medical and surgical patients with serum vitamin D levels of 20 ng/mL or less. Patients received placebo or vitamin D3 at a loading dose of 540,000 IU, followed by a monthly maintenance dose of 90,000 IU for 5 months, the researchers said.
Length of hospital stay averaged 20.1 days for patients who received vitamin D and 19.3 days for the placebo group, the investigators reported.
Among patients who received vitamin D3, 28.3% died in the hospital, compared with 35.3% of the placebo group (hazard ratio, 0.81; 95% confidence interval, 0.58 to 1.11), they said. Six-month mortality was 35.0% for the vitamin D3 group, compared with 42.9% for the placebo group (HR, 0.78; 95% CI, 0.58-1.04), they said.
Among 200 patients with severe vitamin D deficiencies of 12 ng/mL or less, vitamin D3 treatment was linked to a 44% drop in risk of dying in the hospital, the researchers said (28.6% vs. 46.1% for placebo; HR, 0.56; 95% CI, 0.35 to 0.90; P = .04).But length of hospital stay and 6-month mortality rates were similar between the two groups, they reported.
Drug maker Fresenius Kabi provided study medication and a grant to support the research. The European Society for Clinical Nutrition and Metabolism and the Austrian National Bank also funded the study.
Dr Amrein reported and one coauthor reported receiving lecture fees from Fresenius Kabi. The authors reported no other relevant financial conflicts of interest.
High-dose vitamin D did not improve outcomes in critically ill, vitamin D–deficient patients, compared with placebo, researchers reported in JAMA and at the annual congress of the European Society of Intensive Care Medicine.
Although the study was adequately powered, length of stay did not differ between the vitamin D and placebo groups, said Dr. Karin Amrein of the Medical University of Graz, Austria, and her associates. “In the overall cohort, hospital and 6-month mortality rates were numerically lower in the vitamin D3 group, but these differences were not significant,” the researchers said.
A subgroup of patients with severe vitamin D deficiency did have significantly lower hospital mortality when treated with vitamin D, compared with placebo, but the effect “should be considered hypothesis generating and requires further study,” the investigators concluded (JAMA 2014 Sept. 29 [doi:10.1001/jama.2014.13204]).
The randomized, double-blind, single-center trial enrolled 492 critically ill medical and surgical patients with serum vitamin D levels of 20 ng/mL or less. Patients received placebo or vitamin D3 at a loading dose of 540,000 IU, followed by a monthly maintenance dose of 90,000 IU for 5 months, the researchers said.
Length of hospital stay averaged 20.1 days for patients who received vitamin D and 19.3 days for the placebo group, the investigators reported.
Among patients who received vitamin D3, 28.3% died in the hospital, compared with 35.3% of the placebo group (hazard ratio, 0.81; 95% confidence interval, 0.58 to 1.11), they said. Six-month mortality was 35.0% for the vitamin D3 group, compared with 42.9% for the placebo group (HR, 0.78; 95% CI, 0.58-1.04), they said.
Among 200 patients with severe vitamin D deficiencies of 12 ng/mL or less, vitamin D3 treatment was linked to a 44% drop in risk of dying in the hospital, the researchers said (28.6% vs. 46.1% for placebo; HR, 0.56; 95% CI, 0.35 to 0.90; P = .04).But length of hospital stay and 6-month mortality rates were similar between the two groups, they reported.
Drug maker Fresenius Kabi provided study medication and a grant to support the research. The European Society for Clinical Nutrition and Metabolism and the Austrian National Bank also funded the study.
Dr Amrein reported and one coauthor reported receiving lecture fees from Fresenius Kabi. The authors reported no other relevant financial conflicts of interest.
High-dose vitamin D did not improve outcomes in critically ill, vitamin D–deficient patients, compared with placebo, researchers reported in JAMA and at the annual congress of the European Society of Intensive Care Medicine.
Although the study was adequately powered, length of stay did not differ between the vitamin D and placebo groups, said Dr. Karin Amrein of the Medical University of Graz, Austria, and her associates. “In the overall cohort, hospital and 6-month mortality rates were numerically lower in the vitamin D3 group, but these differences were not significant,” the researchers said.
A subgroup of patients with severe vitamin D deficiency did have significantly lower hospital mortality when treated with vitamin D, compared with placebo, but the effect “should be considered hypothesis generating and requires further study,” the investigators concluded (JAMA 2014 Sept. 29 [doi:10.1001/jama.2014.13204]).
The randomized, double-blind, single-center trial enrolled 492 critically ill medical and surgical patients with serum vitamin D levels of 20 ng/mL or less. Patients received placebo or vitamin D3 at a loading dose of 540,000 IU, followed by a monthly maintenance dose of 90,000 IU for 5 months, the researchers said.
Length of hospital stay averaged 20.1 days for patients who received vitamin D and 19.3 days for the placebo group, the investigators reported.
Among patients who received vitamin D3, 28.3% died in the hospital, compared with 35.3% of the placebo group (hazard ratio, 0.81; 95% confidence interval, 0.58 to 1.11), they said. Six-month mortality was 35.0% for the vitamin D3 group, compared with 42.9% for the placebo group (HR, 0.78; 95% CI, 0.58-1.04), they said.
Among 200 patients with severe vitamin D deficiencies of 12 ng/mL or less, vitamin D3 treatment was linked to a 44% drop in risk of dying in the hospital, the researchers said (28.6% vs. 46.1% for placebo; HR, 0.56; 95% CI, 0.35 to 0.90; P = .04).But length of hospital stay and 6-month mortality rates were similar between the two groups, they reported.
Drug maker Fresenius Kabi provided study medication and a grant to support the research. The European Society for Clinical Nutrition and Metabolism and the Austrian National Bank also funded the study.
Dr Amrein reported and one coauthor reported receiving lecture fees from Fresenius Kabi. The authors reported no other relevant financial conflicts of interest.
Key clinical point: Vitamin D3 treatment did not reduce hospital length of stay or mortality in critically ill patients with vitamin D deficiency.
Major finding: Length of hospital stay averaged 20.1 days for patients who received vitamin D and 19.3 days for the placebo group (P = 0.98).
Data source: Randomized, double-blind, placebo-controlled, single-center trial of 492 critically ill medical and surgical patients with vitamin D deficiency of 20 ng per mL or less.
Disclosures: Drug maker Fresenius Kabi provided study medication and a grant to support the research. The European Society for Clinical Nutrition and Metabolism and the Austrian National Bank also funded the study. Dr Amrein reported and one coauthor reported receiving lecture fees from Fresenius Kabi. The authors reported no other relevant financial conflicts of interest.
Hydrocodone rescheduling takes effect Oct. 6
Physicians should ready themselves now for the new set of rules expected when hydrocodone-containing products become subject to tighter regulation on Oct. 6, according to various physician groups.
After a years-long process, the Drug Enforcement Administration announced in late August that it would be moving hydrocodone-containing products from schedule III to schedule II.
That rule takes effect on Oct. 6.
After that date, physicians who want to prescribe HCPs will have to use tamper-proof prescription forms, or use e-prescribing programs. They can call in a 72-hour supply, but must follow that up by mailing the prescription to the pharmacy. Refills by fax or phone are otherwise prohibited.
Patients who are on long term HCP therapy can get up to a 90-day supply through three separate, no-refill prescriptions.
The American Medical Association, which campaigned against the rescheduling of HCPs, is now urging its members to be prepared for the changes in prescribing and work flow that will come with the new landscape.
In a fact sheet, the AMA says that physicians should try to refill prescriptions before Oct. 6, noting that these prescriptions will essentially be grandfathered in under the old rules until Apr. 2015.
The American Society of Clinical Oncology in early September also notified its members of the coming changes, and said that it, too, had opposed rescheduling of HCPs.
Many physician groups have said that moving HCPs to schedule II will not stop abuse or diversion and may hurt patients who have a legitimate need. Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said that “it’s hard to say,” whether upscheduling will make a dent in inappropriate or unnecessary prescribing.
He said in an interview that his practice already requires patients on long-term opioid therapy to come in at least every 3 months for refills and an evaluation. Although physicians may have to change their practice schedules to accommodate refill visits, those visits are good opportunities for education and follow-up, said Dr. Blackwelder.
Requiring face-to-face visits “creates more opportunities to review a treatment plan and make sure it still makes sense,” he said, noting that for many patients, short-acting opioids are the wrong medication.
Dr. Andrew Kolodny, for one, is applauding the rescheduling of HCPs, saying that the explosion in prescriptions for HCPs such as Vicodin (hydrocodone/acetaminophen) has been the single biggest contributor to the rise in opioid addiction.
“I think this is going to have an enormous impact on bringing the epidemic to an end,” Dr. Kolodny, chief medical officer at the Phoenix House Foundation and director of Physicians for Responsible Opioid Prescribing, said in an interview.
He noted that many opioid addicts get their start with HCPs, in part because they are ubiquitous.
The schedule change will bring “a sharp reduction in prescribing of hydrocodone-containing products,” because “it will communicate to prescribers that this drug is every bit as addictive as the other opioids, and needs to be prescribed cautiously,” said Dr. Kolodny.
Dr. Kolodny disclosed that Physicians for Responsible Opioid Prescribing does not accept any industry funding. It is a financed as a Phoenix House program.
On Twitter @aliciaault
Physicians should ready themselves now for the new set of rules expected when hydrocodone-containing products become subject to tighter regulation on Oct. 6, according to various physician groups.
After a years-long process, the Drug Enforcement Administration announced in late August that it would be moving hydrocodone-containing products from schedule III to schedule II.
That rule takes effect on Oct. 6.
After that date, physicians who want to prescribe HCPs will have to use tamper-proof prescription forms, or use e-prescribing programs. They can call in a 72-hour supply, but must follow that up by mailing the prescription to the pharmacy. Refills by fax or phone are otherwise prohibited.
Patients who are on long term HCP therapy can get up to a 90-day supply through three separate, no-refill prescriptions.
The American Medical Association, which campaigned against the rescheduling of HCPs, is now urging its members to be prepared for the changes in prescribing and work flow that will come with the new landscape.
In a fact sheet, the AMA says that physicians should try to refill prescriptions before Oct. 6, noting that these prescriptions will essentially be grandfathered in under the old rules until Apr. 2015.
The American Society of Clinical Oncology in early September also notified its members of the coming changes, and said that it, too, had opposed rescheduling of HCPs.
Many physician groups have said that moving HCPs to schedule II will not stop abuse or diversion and may hurt patients who have a legitimate need. Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said that “it’s hard to say,” whether upscheduling will make a dent in inappropriate or unnecessary prescribing.
He said in an interview that his practice already requires patients on long-term opioid therapy to come in at least every 3 months for refills and an evaluation. Although physicians may have to change their practice schedules to accommodate refill visits, those visits are good opportunities for education and follow-up, said Dr. Blackwelder.
Requiring face-to-face visits “creates more opportunities to review a treatment plan and make sure it still makes sense,” he said, noting that for many patients, short-acting opioids are the wrong medication.
Dr. Andrew Kolodny, for one, is applauding the rescheduling of HCPs, saying that the explosion in prescriptions for HCPs such as Vicodin (hydrocodone/acetaminophen) has been the single biggest contributor to the rise in opioid addiction.
“I think this is going to have an enormous impact on bringing the epidemic to an end,” Dr. Kolodny, chief medical officer at the Phoenix House Foundation and director of Physicians for Responsible Opioid Prescribing, said in an interview.
He noted that many opioid addicts get their start with HCPs, in part because they are ubiquitous.
The schedule change will bring “a sharp reduction in prescribing of hydrocodone-containing products,” because “it will communicate to prescribers that this drug is every bit as addictive as the other opioids, and needs to be prescribed cautiously,” said Dr. Kolodny.
Dr. Kolodny disclosed that Physicians for Responsible Opioid Prescribing does not accept any industry funding. It is a financed as a Phoenix House program.
On Twitter @aliciaault
Physicians should ready themselves now for the new set of rules expected when hydrocodone-containing products become subject to tighter regulation on Oct. 6, according to various physician groups.
After a years-long process, the Drug Enforcement Administration announced in late August that it would be moving hydrocodone-containing products from schedule III to schedule II.
That rule takes effect on Oct. 6.
After that date, physicians who want to prescribe HCPs will have to use tamper-proof prescription forms, or use e-prescribing programs. They can call in a 72-hour supply, but must follow that up by mailing the prescription to the pharmacy. Refills by fax or phone are otherwise prohibited.
Patients who are on long term HCP therapy can get up to a 90-day supply through three separate, no-refill prescriptions.
The American Medical Association, which campaigned against the rescheduling of HCPs, is now urging its members to be prepared for the changes in prescribing and work flow that will come with the new landscape.
In a fact sheet, the AMA says that physicians should try to refill prescriptions before Oct. 6, noting that these prescriptions will essentially be grandfathered in under the old rules until Apr. 2015.
The American Society of Clinical Oncology in early September also notified its members of the coming changes, and said that it, too, had opposed rescheduling of HCPs.
Many physician groups have said that moving HCPs to schedule II will not stop abuse or diversion and may hurt patients who have a legitimate need. Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said that “it’s hard to say,” whether upscheduling will make a dent in inappropriate or unnecessary prescribing.
He said in an interview that his practice already requires patients on long-term opioid therapy to come in at least every 3 months for refills and an evaluation. Although physicians may have to change their practice schedules to accommodate refill visits, those visits are good opportunities for education and follow-up, said Dr. Blackwelder.
Requiring face-to-face visits “creates more opportunities to review a treatment plan and make sure it still makes sense,” he said, noting that for many patients, short-acting opioids are the wrong medication.
Dr. Andrew Kolodny, for one, is applauding the rescheduling of HCPs, saying that the explosion in prescriptions for HCPs such as Vicodin (hydrocodone/acetaminophen) has been the single biggest contributor to the rise in opioid addiction.
“I think this is going to have an enormous impact on bringing the epidemic to an end,” Dr. Kolodny, chief medical officer at the Phoenix House Foundation and director of Physicians for Responsible Opioid Prescribing, said in an interview.
He noted that many opioid addicts get their start with HCPs, in part because they are ubiquitous.
The schedule change will bring “a sharp reduction in prescribing of hydrocodone-containing products,” because “it will communicate to prescribers that this drug is every bit as addictive as the other opioids, and needs to be prescribed cautiously,” said Dr. Kolodny.
Dr. Kolodny disclosed that Physicians for Responsible Opioid Prescribing does not accept any industry funding. It is a financed as a Phoenix House program.
On Twitter @aliciaault
Laparoscopic resection improved short-term outcomes in patients with cirrhotic liver cancer
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resections had lower postoperative morbidity and shorter hospital stays than patients who had open resections.
Major finding: Laparoscopy patients had significantly less postoperative morbidity (10% vs. 26%; P = .0459) and shorter hospital stays (10 vs. 16 days; P = .0008), compared with patients who underwent open resection, with no port site recurrences and no significant differences in long-term survival.
Data source:Retrospective, single-center study of 162 patients with cirrhosis and primary hepatocellular carcinoma who underwent curative hepatic resections, of whom 99 underwent open procedures and 63 underwent laparoscopies.
Disclosures: The authors disclosed no funding sources and reported having no conflicts of interest.
Closing large dermal defects much like a Victorian corset
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EDINBURGH – Barbed absorbable sutures are a useful new tool to facilitate dermal closure of facial and nonfacial defects following tumor resection.
“These are not the bad old sutures that you might of heard about before, that were nonabsorbable sutures and attempted for use in cosmetic procedures,” Dr. John Strasswimmer said at the 15th World Congress on Cancers of the Skin.
Last year, Dr. Strasswimmer, medical director of melanoma and cutaneous oncology at the Lynn Cancer Institute in Boca Raton, Fla., reported his initial experience using a procedure he calls “Corseta” to close a large Mohs defect on the trunk of an 83-year-old man (JAMA Dermatol. 2013;149:853-4).
The procedure employs a barbed, bioabsorbable suture (Ethicon’s Stratafix and Covidien’s V-Loc) that is run in a continuous vertical looping manner in the subcutaneous layer, with minimal to no undermining of the wound. Undermining is typically used in cutaneous surgery to relieve tension or provide structure around anatomical landmarks, but it can increase the risk of bleeding, swelling, and patient discomfort, he said.
Instead, the first suture pass is placed in the deepest portion of the subcutaneous tissue and brought out within the more superficial subcutaneous layer. Each bite of the barbed suture extends peripherally at least 2.0 cm from the edge of the wound, so the point of tension is lateral to the wound margins. At every two passes, tension is placed evenly across the sutures to close the deepest layer of tissue and to engage the barbs, much like closing of a Victorian corset, Dr. Strasswimmer said.
The second arm of the suture is passed in a similar manner in the subcutaneous plane, superficial to the first pass.
“This is a lacing, not a suturing technique,” he said. “You get tissue approximation, but more importantly, because we’re bringing in all that deep tissue, you automatically get beautiful wound-edge eversion and very nice cosmetic results.”
Because the sutures have barbs cut into them, however, a 0-0 weight polydioxane or other absorbable material suture can have a breaking strength of a #2-0 suture. “You have to look very carefully at the manufacturer’s sizing and strength requirements,” Dr. Strasswimmer cautioned.
Since their initial case report, Dr. Strasswimmer and his colleagues have expanded use of the Corseta technique to more than 600 facial and nonfacial reconstructions. The Corseta procedure is not as helpful for curved topography such as the central face or scalp, he said in an interview. Still, of the 600 or so cases, none required conversion to another closure technique.
“The traditional closure technique would not have worked in those challenging cases,” Dr. Strasswimmer said. “In the most difficult situations, such as older patients with severely atrophic skin, even the best suturing won’t work. In that case, the Corseta at least produces a partial closure, thereby reducing the wound and accelerating healing.” The Corseta procedure is often coupled with tumescent anesthesia to decrease the risk of bleeding, particularly in patients on anticoagulation, he noted.
The conference was sponsored by the Skin Cancer Foundation.
EXPERT ANALYSIS FROM WCCS 2014
Same-day combined ERCP and cholecystectomy: achievable and cost effective
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
“Same-day procedures decreased length of stay by 2 days and led to an approximately $30,000 cost savings with no difference in conversion rates or complications between the two cohorts. The success rate of operative ERCP was 100%,” Dr. Jeffrey Wild, of Geisinger Health System in Northeastern Pennsylvania, reported at the annual meeting of the American Association for the Surgery of Trauma.
The Geisinger study validated the findings of two previous European studies (Endoscopy 2006;38:779-86; Am. Surg. 2013;79:1243-7). “These studies found decreased length of stay by 2 to 3 days, they found no difference in the incidence of retained stones, no difference in conversion rates to open cholecystectomy, and there was no difference in complications between the two groups,” Dr. Wild said.
The Geisinger investigators conducted the single-center, retrospective study of 240 patients from 2010 to 2014 comparing same-day and separate-day approaches for patients with choledocholithiasis and cholecystitis. In all, 65 patients had same-day procedures, with an average length of stay of 3 days vs. 5 days for patients who had ERCP and cholecystectomy on separate days, Dr. Wild said.
Like the European studies, the Geisinger experience found no statistical difference in conversion rates to open operation (12% for same-day vs. 14% for separate-day procedures) while the rate of discharge to a skilled nursing facility was half in the same-day cohort: 10% vs. 20% for separate-day patients, Dr. Wild said.
The goal of the Geisinger gallbladder pathway is to facilitate early operations in patients with cholecystitis. “Patients who present with cholecystitis should undergo cholecystectomy within 24 hours of presentation, if appropriate,” Dr. Wild said. “If there is evidence of biliary obstruction and the need for further work-up, our goal is to have gastroenterology work-up and management of the patient and have cholecystectomy done within the first 48 hours.”
The study noted some slight variations between the same-day and separate-day approaches, Dr. Wild said. The success rate of the endoscopist to cannulate the ampulla and perform ERCP was 95% in the same-day group and 100% in the separate-day cohort. ERCP was positive in identifying common bile duct stones or sludge in 97% of the same-day group vs. 91% in separate-day patients. More patients in the separate-day cohort required a second ERCP, usually 3 or 4 weeks after discharge and for removal of biliary stents, Dr. Wild said. Demographics in both groups were similar.
Operating room times varied between the two groups, and even within the same-day group depending on the setting for the ERCP, according to Dr. Wild. For patients in the separate-day group, average operative time was 1 hour, 42 minutes; same-day patients who had ERCP in the endoscopy suite and then transferred to the OR for cholecystectomy averaged 1 hour, 34 minutes; while the same-day cohort who had both ERCP and cholecystectomy done in the OR averaged 2 hours, 12 minutes.
Same-day care required coordination between different departments, Dr. Wild said. “Patients in the same-day group required coordination between the acute care surgical service, anesthesia, and gastroenterology to make sure both procedures could be performed under the same general anesthesia,” he said. The same-day group was almost evenly split between having ERCP in endoscopy before moving to the OR and having both done in the OR, Dr. Wild said.
“The findings of this study are, Number 1, intuitively obvious and easily predicted; and, Number 2, why didn’t I think of that myself?” said discussant Dr. Michael Chang of Wake Forest University Baptist Medical Center, Winston-Salem, N.C.
Dr. Chang also noted that the study provides an example of how to restructure care organizations. “Grouping practitioners by disease process, as opposed to what board they’re certified by or what department they live in, is thought to be a more patient-centered approach to provide cost-effective care,” he said.
Dr. Chang and others asked how the Geisinger surgeons overcame institutional barriers in creating their care model. “Most institutions are still dependent on the gastroenterologists, and lining up that procedure with another service can be difficult,” Dr. Donald Reed Jr. of Lutheran Medical Group in Fort Wayne, Ind., noted.
Dr. Wild acknowledged at first the pathway encountered some resistance. “But what really started this process was that the endoscopy suite was closed on weekends and all the ERCPs were performed in OR,” he said. “And then we were taking patients the following morning back to the OR to take out their gallbladder. Some of my senior partners questioned why aren’t we doing these at the same time.”
At this point, gastroenterology is “very willing” to embrace ERCP in the OR before gallbladder removal, Dr. Wild said.
Dr. Wild reported having no relevant financial disclosures.
FROM THE AAST ANNUAL MEETING
Key clinical point: Scheduling both ERCP and cholecystectomy on the same day reduces hospital stays and saves money.
Major finding: Patients who had preoperative endoscopic retrograde cholangiopancreatography (ERCP) on the same day as cholecystectomy had 3-day hospital stays compared to 5 days for patients who had the procedures on separate days.
Data source: Single-center retrospective study of 240 patients from 2010 to 2014.
Disclosures: Dr. Wild reported having no relevant financial disclosures.
Protocol for small-bowel obstruction
PHILADELPHIA – Closely monitoring patients admitted for small bowel obstruction every 4 hours and starting them on intravenous fluids, bowel rest, and nasogastric tube decompression may aid in quickly differentiating partial and complete SBO and direct them into targeted treatment earlier, according to investigators at the University of Florida Health, Gainesville.
“Despite the prevalence of small bowel obstruction and the fact that we’ve been dealing with it for more than a century, we still do not have a general consensus on how to differentiate between partial bowel obstruction and complete obstruction,” Dr. Janeen Jordan said at the annual meeting of the American Association for the Surgery of Trauma. Dr. Jordan reported on a study involving 91 patients admitted for SBO over 1 year at the University of Florida Health.
Early differentiation of partial vs. complete bowel obstruction and early intervention were goals of the protocol, Dr. Jordan said. “We really wanted to get them to surgery within 3 days with hopes of decreasing our bowel resection rate, hospital length of stay and, of course, mortality,” she said.
She outlined the protocol her institution used in symptomatic patients with x-ray findings positive for SBO: admission for intravenous fluid resuscitation, bowel rest, nasogastric tube decompression, and exams every 4 hours. Once stabilized, patients received a CT scan with only intravenous contrast to confirm the diagnosis. “If there was any suggestion of bowel compromise such as pneumatosis, mesenteric edema, or suggestion of a closed-loop obstruction, they were evaluated immediately for operation,” Dr. Jordan said. “If patients had none of those findings or had fecalization, which suggests a chronic problem instead of an acute issue, those patients were admitted for bowel decompression and IV fluid resuscitation.”
After resuscitation, patients with peritonitis or CT imaging positive for bowel compromise had exploratory surgery. All other patients received an osmotically active, water-soluble contrast agent and diagnostic imaging at 4, 8, 12 and 24 hours. If contrast did not reach the colon in 24 hours, the patient underwent exploratory surgery.
Twenty-six patients went directly to the OR without entering the protocol, 58% of whom required bowel resection, Dr. Jordan said. Among the 75 patients in the protocol, 43% required surgery. The average time to surgery was within 1 day for those not on the protocol and 2 days for those managed with contrast. Demographics between the two groups were similar, although the nonprotocol patients were more likely to have bowel wall thickening on CT scan.
The analysis also compared patients who received contrast and those who did not, and further broke that down into patients who had surgery vs. nonoperative management in each group. “Giving them contrast didn’t increase hospital length of stay,” Dr. Jordan said. “And the patients who didn’t get surgery had an overall hospital length of stay of 3-4 days; if they had surgery, regardless whether or not they received contrast, their hospital length of stay was approximately 10 days.” Additionally, the length of time for the contrast to reach the colon was predictive of who would fail at eating or drinking by mouth or have recurrent symptoms before discharge.
Discussant Dr. Clay Cothren Burlew of Denver Health said she found the concept of a protocol for patients with symptoms of SBO “incredibly appealing.” However, she added, “Patients without overt clinical signs of peritonitis mandating operative intervention are often fraught with challenges. Questions of the timing of intervention to bring about resolution have never really been met. It’s a gray zone in surgery.”
Dr. Martin Schreiber of Oregon Health & Science University, Portland, questioned the cost involved in imaging without contrast. “Instead of doing a CT scan without enteral contrast and then doing an upper GI, why not do the CT with enteral contrast and then do your follow-up x-rays to see if contrast reaches the colon? Skip a step and save lots of money.”
Dr. Ronald Maier of the University of Washington, Seattle, pointed out the protocol seeks to rule out surgery for a patient population that’s unlikely to have surgery anyway. “We know, as many studies have presented, 85% of these people – if you never operate on them – go home without an operation and they do fine,” he said. “So you’re hunting for the 15%, and yet in your protocol you operate on nearly half of them.”
Previously published studies that linked interventions after 3 days in the hospital with higher bowel resection and mortality determined the timing of surgery in the protocol, Dr. Jordan said. However, she admitted that the rate of surgery was lower at the end of the study period than at the beginning.
Dr. Jordan reported having no financial disclosures.
PHILADELPHIA – Closely monitoring patients admitted for small bowel obstruction every 4 hours and starting them on intravenous fluids, bowel rest, and nasogastric tube decompression may aid in quickly differentiating partial and complete SBO and direct them into targeted treatment earlier, according to investigators at the University of Florida Health, Gainesville.
“Despite the prevalence of small bowel obstruction and the fact that we’ve been dealing with it for more than a century, we still do not have a general consensus on how to differentiate between partial bowel obstruction and complete obstruction,” Dr. Janeen Jordan said at the annual meeting of the American Association for the Surgery of Trauma. Dr. Jordan reported on a study involving 91 patients admitted for SBO over 1 year at the University of Florida Health.
Early differentiation of partial vs. complete bowel obstruction and early intervention were goals of the protocol, Dr. Jordan said. “We really wanted to get them to surgery within 3 days with hopes of decreasing our bowel resection rate, hospital length of stay and, of course, mortality,” she said.
She outlined the protocol her institution used in symptomatic patients with x-ray findings positive for SBO: admission for intravenous fluid resuscitation, bowel rest, nasogastric tube decompression, and exams every 4 hours. Once stabilized, patients received a CT scan with only intravenous contrast to confirm the diagnosis. “If there was any suggestion of bowel compromise such as pneumatosis, mesenteric edema, or suggestion of a closed-loop obstruction, they were evaluated immediately for operation,” Dr. Jordan said. “If patients had none of those findings or had fecalization, which suggests a chronic problem instead of an acute issue, those patients were admitted for bowel decompression and IV fluid resuscitation.”
After resuscitation, patients with peritonitis or CT imaging positive for bowel compromise had exploratory surgery. All other patients received an osmotically active, water-soluble contrast agent and diagnostic imaging at 4, 8, 12 and 24 hours. If contrast did not reach the colon in 24 hours, the patient underwent exploratory surgery.
Twenty-six patients went directly to the OR without entering the protocol, 58% of whom required bowel resection, Dr. Jordan said. Among the 75 patients in the protocol, 43% required surgery. The average time to surgery was within 1 day for those not on the protocol and 2 days for those managed with contrast. Demographics between the two groups were similar, although the nonprotocol patients were more likely to have bowel wall thickening on CT scan.
The analysis also compared patients who received contrast and those who did not, and further broke that down into patients who had surgery vs. nonoperative management in each group. “Giving them contrast didn’t increase hospital length of stay,” Dr. Jordan said. “And the patients who didn’t get surgery had an overall hospital length of stay of 3-4 days; if they had surgery, regardless whether or not they received contrast, their hospital length of stay was approximately 10 days.” Additionally, the length of time for the contrast to reach the colon was predictive of who would fail at eating or drinking by mouth or have recurrent symptoms before discharge.
Discussant Dr. Clay Cothren Burlew of Denver Health said she found the concept of a protocol for patients with symptoms of SBO “incredibly appealing.” However, she added, “Patients without overt clinical signs of peritonitis mandating operative intervention are often fraught with challenges. Questions of the timing of intervention to bring about resolution have never really been met. It’s a gray zone in surgery.”
Dr. Martin Schreiber of Oregon Health & Science University, Portland, questioned the cost involved in imaging without contrast. “Instead of doing a CT scan without enteral contrast and then doing an upper GI, why not do the CT with enteral contrast and then do your follow-up x-rays to see if contrast reaches the colon? Skip a step and save lots of money.”
Dr. Ronald Maier of the University of Washington, Seattle, pointed out the protocol seeks to rule out surgery for a patient population that’s unlikely to have surgery anyway. “We know, as many studies have presented, 85% of these people – if you never operate on them – go home without an operation and they do fine,” he said. “So you’re hunting for the 15%, and yet in your protocol you operate on nearly half of them.”
Previously published studies that linked interventions after 3 days in the hospital with higher bowel resection and mortality determined the timing of surgery in the protocol, Dr. Jordan said. However, she admitted that the rate of surgery was lower at the end of the study period than at the beginning.
Dr. Jordan reported having no financial disclosures.
PHILADELPHIA – Closely monitoring patients admitted for small bowel obstruction every 4 hours and starting them on intravenous fluids, bowel rest, and nasogastric tube decompression may aid in quickly differentiating partial and complete SBO and direct them into targeted treatment earlier, according to investigators at the University of Florida Health, Gainesville.
“Despite the prevalence of small bowel obstruction and the fact that we’ve been dealing with it for more than a century, we still do not have a general consensus on how to differentiate between partial bowel obstruction and complete obstruction,” Dr. Janeen Jordan said at the annual meeting of the American Association for the Surgery of Trauma. Dr. Jordan reported on a study involving 91 patients admitted for SBO over 1 year at the University of Florida Health.
Early differentiation of partial vs. complete bowel obstruction and early intervention were goals of the protocol, Dr. Jordan said. “We really wanted to get them to surgery within 3 days with hopes of decreasing our bowel resection rate, hospital length of stay and, of course, mortality,” she said.
She outlined the protocol her institution used in symptomatic patients with x-ray findings positive for SBO: admission for intravenous fluid resuscitation, bowel rest, nasogastric tube decompression, and exams every 4 hours. Once stabilized, patients received a CT scan with only intravenous contrast to confirm the diagnosis. “If there was any suggestion of bowel compromise such as pneumatosis, mesenteric edema, or suggestion of a closed-loop obstruction, they were evaluated immediately for operation,” Dr. Jordan said. “If patients had none of those findings or had fecalization, which suggests a chronic problem instead of an acute issue, those patients were admitted for bowel decompression and IV fluid resuscitation.”
After resuscitation, patients with peritonitis or CT imaging positive for bowel compromise had exploratory surgery. All other patients received an osmotically active, water-soluble contrast agent and diagnostic imaging at 4, 8, 12 and 24 hours. If contrast did not reach the colon in 24 hours, the patient underwent exploratory surgery.
Twenty-six patients went directly to the OR without entering the protocol, 58% of whom required bowel resection, Dr. Jordan said. Among the 75 patients in the protocol, 43% required surgery. The average time to surgery was within 1 day for those not on the protocol and 2 days for those managed with contrast. Demographics between the two groups were similar, although the nonprotocol patients were more likely to have bowel wall thickening on CT scan.
The analysis also compared patients who received contrast and those who did not, and further broke that down into patients who had surgery vs. nonoperative management in each group. “Giving them contrast didn’t increase hospital length of stay,” Dr. Jordan said. “And the patients who didn’t get surgery had an overall hospital length of stay of 3-4 days; if they had surgery, regardless whether or not they received contrast, their hospital length of stay was approximately 10 days.” Additionally, the length of time for the contrast to reach the colon was predictive of who would fail at eating or drinking by mouth or have recurrent symptoms before discharge.
Discussant Dr. Clay Cothren Burlew of Denver Health said she found the concept of a protocol for patients with symptoms of SBO “incredibly appealing.” However, she added, “Patients without overt clinical signs of peritonitis mandating operative intervention are often fraught with challenges. Questions of the timing of intervention to bring about resolution have never really been met. It’s a gray zone in surgery.”
Dr. Martin Schreiber of Oregon Health & Science University, Portland, questioned the cost involved in imaging without contrast. “Instead of doing a CT scan without enteral contrast and then doing an upper GI, why not do the CT with enteral contrast and then do your follow-up x-rays to see if contrast reaches the colon? Skip a step and save lots of money.”
Dr. Ronald Maier of the University of Washington, Seattle, pointed out the protocol seeks to rule out surgery for a patient population that’s unlikely to have surgery anyway. “We know, as many studies have presented, 85% of these people – if you never operate on them – go home without an operation and they do fine,” he said. “So you’re hunting for the 15%, and yet in your protocol you operate on nearly half of them.”
Previously published studies that linked interventions after 3 days in the hospital with higher bowel resection and mortality determined the timing of surgery in the protocol, Dr. Jordan said. However, she admitted that the rate of surgery was lower at the end of the study period than at the beginning.
Dr. Jordan reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Protocol clarifies targeted treatment in SBO management.
Major finding: A quarter of patients with small bowel obstruction went directly to surgery based on imaging or exam findings, half of whom required bowel resection. The remainder were managed on a protocol to differentiate partial and complete bowl obstruction, 45% of whom needed surgery. Those in the protocol went to surgery within 2 days vs. 1 day for those not in the protocol.
Data source: Single-institution experience involved 101 admissions admitted for SBO over 1 year.
Disclosures: Dr. Jordan reported having no financial disclosures.
Most acute VTE therapies yield similar outcomes
For patients with acute venous thromboembolism, both clinical and safety outcomes were similar among seven of eight possible treatment strategies assessed in a network meta-analysis published online Sept. 16 in JAMA.
Clinicians have several treatment options but little guidance for choosing among them when managing acute VTE. Many strategies have shown promising results when assessed in single studies, but there have been few direct comparison studies. So investigators performed a network meta-analysis of 45 articles involving 44,989 patients, which enabled them to compare the safety and efficacy of eight possible approaches. The sample sizes of these studies ranged from 60 to 8,240 participants, with a median of 298. The median follow-up period was 3 months, with a range of 3-8 months.
The currently accepted standard treatment for acute VTE is the use of parenteral low-molecular-weight heparin (LMWH) for a minimum of 5 days, followed by transition to a vitamin K antagonist. This approach was compared against parenteral unfractionated heparin followed by a vitamin K antagonist; parenteral fondaparinux followed by a vitamin K antagonist; parenteral LMWH combined with dabigatran; parenteral LMWH combined with edoxaban; oral rivaroxaban; oral apixaban; and parenteral LMWH alone, said Dr. Lana A. Castellucci of the Ottawa Hospital Research Institute, University of Ottawa, and her associates.
Compared with standard parenteral LMWH plus a vitamin K antagonist, six of these approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding, the investigators said (JAMA 2014 September 16 [doi:10.1001/jama.2014.10538]).
The only strategy that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist. However, “there are clinical circumstances that necessitate the use of unfractionated heparin, including for patients with severe renal insufficiency and those with massive or submassive pulmonary embolism who are potential candidates for thrombolysis or thrombectomy,” Dr. Castellucci and her associates noted.
Oral rivaroxaban and oral apixaban appeared to be associated with the lowest risk of major bleeding. “Future direct comparison trials, patient-level network meta-analyses, or high-quality nonrandomized studies are required to confirm our findings,” they added.
This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
*Correction, 9/17/2014: An earlier version of this article misstated the Key Clinical Point in the Vitals section.
For patients with acute venous thromboembolism, both clinical and safety outcomes were similar among seven of eight possible treatment strategies assessed in a network meta-analysis published online Sept. 16 in JAMA.
Clinicians have several treatment options but little guidance for choosing among them when managing acute VTE. Many strategies have shown promising results when assessed in single studies, but there have been few direct comparison studies. So investigators performed a network meta-analysis of 45 articles involving 44,989 patients, which enabled them to compare the safety and efficacy of eight possible approaches. The sample sizes of these studies ranged from 60 to 8,240 participants, with a median of 298. The median follow-up period was 3 months, with a range of 3-8 months.
The currently accepted standard treatment for acute VTE is the use of parenteral low-molecular-weight heparin (LMWH) for a minimum of 5 days, followed by transition to a vitamin K antagonist. This approach was compared against parenteral unfractionated heparin followed by a vitamin K antagonist; parenteral fondaparinux followed by a vitamin K antagonist; parenteral LMWH combined with dabigatran; parenteral LMWH combined with edoxaban; oral rivaroxaban; oral apixaban; and parenteral LMWH alone, said Dr. Lana A. Castellucci of the Ottawa Hospital Research Institute, University of Ottawa, and her associates.
Compared with standard parenteral LMWH plus a vitamin K antagonist, six of these approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding, the investigators said (JAMA 2014 September 16 [doi:10.1001/jama.2014.10538]).
The only strategy that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist. However, “there are clinical circumstances that necessitate the use of unfractionated heparin, including for patients with severe renal insufficiency and those with massive or submassive pulmonary embolism who are potential candidates for thrombolysis or thrombectomy,” Dr. Castellucci and her associates noted.
Oral rivaroxaban and oral apixaban appeared to be associated with the lowest risk of major bleeding. “Future direct comparison trials, patient-level network meta-analyses, or high-quality nonrandomized studies are required to confirm our findings,” they added.
This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
*Correction, 9/17/2014: An earlier version of this article misstated the Key Clinical Point in the Vitals section.
For patients with acute venous thromboembolism, both clinical and safety outcomes were similar among seven of eight possible treatment strategies assessed in a network meta-analysis published online Sept. 16 in JAMA.
Clinicians have several treatment options but little guidance for choosing among them when managing acute VTE. Many strategies have shown promising results when assessed in single studies, but there have been few direct comparison studies. So investigators performed a network meta-analysis of 45 articles involving 44,989 patients, which enabled them to compare the safety and efficacy of eight possible approaches. The sample sizes of these studies ranged from 60 to 8,240 participants, with a median of 298. The median follow-up period was 3 months, with a range of 3-8 months.
The currently accepted standard treatment for acute VTE is the use of parenteral low-molecular-weight heparin (LMWH) for a minimum of 5 days, followed by transition to a vitamin K antagonist. This approach was compared against parenteral unfractionated heparin followed by a vitamin K antagonist; parenteral fondaparinux followed by a vitamin K antagonist; parenteral LMWH combined with dabigatran; parenteral LMWH combined with edoxaban; oral rivaroxaban; oral apixaban; and parenteral LMWH alone, said Dr. Lana A. Castellucci of the Ottawa Hospital Research Institute, University of Ottawa, and her associates.
Compared with standard parenteral LMWH plus a vitamin K antagonist, six of these approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding, the investigators said (JAMA 2014 September 16 [doi:10.1001/jama.2014.10538]).
The only strategy that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist. However, “there are clinical circumstances that necessitate the use of unfractionated heparin, including for patients with severe renal insufficiency and those with massive or submassive pulmonary embolism who are potential candidates for thrombolysis or thrombectomy,” Dr. Castellucci and her associates noted.
Oral rivaroxaban and oral apixaban appeared to be associated with the lowest risk of major bleeding. “Future direct comparison trials, patient-level network meta-analyses, or high-quality nonrandomized studies are required to confirm our findings,” they added.
This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
*Correction, 9/17/2014: An earlier version of this article misstated the Key Clinical Point in the Vitals section.
FROM JAMA
Key clinical point: Seven of the eight available VTE therapies are equally safe and effective.*
Major finding: Compared with standard parenteral LMWH plus a vitamin K antagonist, six treatment approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding; the only approach that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist.
Data source: A network meta-analysis of 45 articles on studies involving 44,989 patients with acute VTE who were treated using any of eight strategies and followed for a median of 3 months.
Disclosures: This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
E-order sets for Vitamin D testing cut deficiency among elderly
Making physicians aware of their track record assessing vitamin D deficiency and adding computerized order sets to check vitamin D levels and initiate vitamin D supplementation led to "significant improvement" in assessment and treatment of vitamin D deficiency in elderly patients with hip fracture at a North Carolina hospital, according to a study published online in the Journal of Hospital Medicine.
After these interventions, the percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5% (P less than .001), and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68% (P = .008), Dr. John R. Stephens of the University of North Carolina Hospitals and his colleagues reported (J. Hosp. Med. 2014 Sept. 5 [doi:10.1002/jhm.2255]).
The study authors reviewed the literature on the prevalence of vitamin D deficiency in elderly patients and used Endocrine Society guidelines "to define vitamin D deficiency, insufficiency, and recommended treatment dosing for each condition." They presented this information along with a review of data from their hospitalist group practice at a staff meeting.
They also revised the computerized physician order entry (CPOE) set for patients with hip fractures to include two new orders: an automatic order for 25-OH vitamin D level to be drawn the morning after admission and an order for initiation of 1,000 IU daily of vitamin D at admission.
They compared records of 196 patients (mean age 80), with hip fracture treated in the 28 months before these interventions and 107 similar patients treated in the 12 months following the interventions.
Three-quarters of the patients were female and at least 81% of the patients in both the intervention and preintervention groups were white in the single-center study.
"Our study demonstrates a systematic method groups may use to adopt and reliably implement practice guidelines," the authors wrote.
"With safeguards in the electronic system to flag duplicate medications, low toxicity of standard doses of vitamin D, and minimal economic harm with duplicate laboratory therapy in the context of a hospitalization for hip fracture," the researchers wrote, any possible risks "are outweighed by the benefits of screening."
They reported no conflicts of interest.
Making physicians aware of their track record assessing vitamin D deficiency and adding computerized order sets to check vitamin D levels and initiate vitamin D supplementation led to "significant improvement" in assessment and treatment of vitamin D deficiency in elderly patients with hip fracture at a North Carolina hospital, according to a study published online in the Journal of Hospital Medicine.
After these interventions, the percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5% (P less than .001), and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68% (P = .008), Dr. John R. Stephens of the University of North Carolina Hospitals and his colleagues reported (J. Hosp. Med. 2014 Sept. 5 [doi:10.1002/jhm.2255]).
The study authors reviewed the literature on the prevalence of vitamin D deficiency in elderly patients and used Endocrine Society guidelines "to define vitamin D deficiency, insufficiency, and recommended treatment dosing for each condition." They presented this information along with a review of data from their hospitalist group practice at a staff meeting.
They also revised the computerized physician order entry (CPOE) set for patients with hip fractures to include two new orders: an automatic order for 25-OH vitamin D level to be drawn the morning after admission and an order for initiation of 1,000 IU daily of vitamin D at admission.
They compared records of 196 patients (mean age 80), with hip fracture treated in the 28 months before these interventions and 107 similar patients treated in the 12 months following the interventions.
Three-quarters of the patients were female and at least 81% of the patients in both the intervention and preintervention groups were white in the single-center study.
"Our study demonstrates a systematic method groups may use to adopt and reliably implement practice guidelines," the authors wrote.
"With safeguards in the electronic system to flag duplicate medications, low toxicity of standard doses of vitamin D, and minimal economic harm with duplicate laboratory therapy in the context of a hospitalization for hip fracture," the researchers wrote, any possible risks "are outweighed by the benefits of screening."
They reported no conflicts of interest.
Making physicians aware of their track record assessing vitamin D deficiency and adding computerized order sets to check vitamin D levels and initiate vitamin D supplementation led to "significant improvement" in assessment and treatment of vitamin D deficiency in elderly patients with hip fracture at a North Carolina hospital, according to a study published online in the Journal of Hospital Medicine.
After these interventions, the percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5% (P less than .001), and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68% (P = .008), Dr. John R. Stephens of the University of North Carolina Hospitals and his colleagues reported (J. Hosp. Med. 2014 Sept. 5 [doi:10.1002/jhm.2255]).
The study authors reviewed the literature on the prevalence of vitamin D deficiency in elderly patients and used Endocrine Society guidelines "to define vitamin D deficiency, insufficiency, and recommended treatment dosing for each condition." They presented this information along with a review of data from their hospitalist group practice at a staff meeting.
They also revised the computerized physician order entry (CPOE) set for patients with hip fractures to include two new orders: an automatic order for 25-OH vitamin D level to be drawn the morning after admission and an order for initiation of 1,000 IU daily of vitamin D at admission.
They compared records of 196 patients (mean age 80), with hip fracture treated in the 28 months before these interventions and 107 similar patients treated in the 12 months following the interventions.
Three-quarters of the patients were female and at least 81% of the patients in both the intervention and preintervention groups were white in the single-center study.
"Our study demonstrates a systematic method groups may use to adopt and reliably implement practice guidelines," the authors wrote.
"With safeguards in the electronic system to flag duplicate medications, low toxicity of standard doses of vitamin D, and minimal economic harm with duplicate laboratory therapy in the context of a hospitalization for hip fracture," the researchers wrote, any possible risks "are outweighed by the benefits of screening."
They reported no conflicts of interest.
FROM THE JOURNAL OF HOSPITAL MEDICINE
Key clinical point: Having CPOE prompt screening can help reduce vitamin D deficiency in elderly inpatients.
Major finding: The percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5%, and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68%.
Data source: An internal review of hospital records for 196 patients treated before CPOE set interventions and 107 patients treated after interventions.
Disclosures: The authors reported no conflicts of interest.