User login
Lower Protein Intake In Midlife May Increase Mortality Risk
Lower intake of dietary protein in midlife was a significant independent predictor of all-cause mortality in later life, based on data from a cohort study of more than 8000 men.
The Recommended Dietary Allowance of dietary protein intake is 0.8 g/kg body weight, but previous studies of the effect of dietary protein on all-cause mortality have yielded inconsistent results, Pedro Joaquin Ayau Aguilar, MD, of the University of Hawaii, Honolulu, said in a presentation at the annual meeting of the American Geriatrics Society.
To better examine these effects, Dr. Aguilar and colleagues reviewed data from 7486 participants in the Kuakini Honolulu Heart Program (HHP), a prospective cohort study of Japanese-American men in Hawaii.
Participants underwent a baseline exam in 1965-1968 at ages 45-68 years and were followed for mortality until December 31, 2022. The researchers created quintiles of dietary protein/kg categorized as plant or animal source, trained dietitians worked with participants to complete a 24-hour diet recall, and the primary outcome was all-cause mortality.
Overall, the mean protein intake in the study population was 1.5 g/kg body weight; the mean animal protein and plant protein intakes were 1.1 g/kg and 0.4 g/kg, respectively.
In an age-adjusted analysis, mortality rates per 1,000 person-years were significantly higher with lower total protein intake, with rates of 39.7 per 1,000 person-years and 36.8 per 1,000 person-years in the first and fifth quintiles, respectively (P < .0001).
Data Show Consistency Across Protein Types
Trends were similar for animal protein and plant protein intake, with mortality rates of 39.6 and 36.5 per 1000 person-years for the first and fifth quintiles, respectively.
“All of these categories had a significant trend, with the lowest quintile showing the highest mortality rate,” Dr. Aguilar said in his presentation.
The study was limited by several factors including the homogeneous population of Japanese men, and the inability to make conclusions about cause and effect, Dr. Aguilar said. However, the results were strengthened by the large cohort, long follow-up, and complete mortality surveillance, he added.
As for the study’s clinical implications, “I believe it adds to the body of evidence on how nutrition impacts health and [the data] can help us better advise our patients on their macronutrient intake to better optimize their health,” Dr. Aguilar said in a question-and-answer session following the presentation.
Looking ahead, “More research is needed to more accurately define which type of protein and in which amounts are optimal for health,” as well as how other macronutrients in different stages of life affect health span and life span, he said.
Although a minimum Recommended Daily Allowance of dietary protein is 0.8 g/kg body weight, the relationship between dietary protein intake and all-cause mortality remains unclear, said Shelly Gray, PharmD, professor of pharmacy at the University of Washington School of Pharmacy, said in an interview.
Dr. Gray, who served as a moderator for the session in which the study was presented, agreed that more research is needed before clinical implications can be discussed.
The study was supported by the Department of Geriatric Medicine, John A. Burns School of Medicine, University of Hawaii; Kuakini Medical Center, Honolulu, Hawaii; and the National Institutes of Health. The researchers had no financial conflicts to disclose. Dr. Gray had no financial conflicts to disclose.
Lower intake of dietary protein in midlife was a significant independent predictor of all-cause mortality in later life, based on data from a cohort study of more than 8000 men.
The Recommended Dietary Allowance of dietary protein intake is 0.8 g/kg body weight, but previous studies of the effect of dietary protein on all-cause mortality have yielded inconsistent results, Pedro Joaquin Ayau Aguilar, MD, of the University of Hawaii, Honolulu, said in a presentation at the annual meeting of the American Geriatrics Society.
To better examine these effects, Dr. Aguilar and colleagues reviewed data from 7486 participants in the Kuakini Honolulu Heart Program (HHP), a prospective cohort study of Japanese-American men in Hawaii.
Participants underwent a baseline exam in 1965-1968 at ages 45-68 years and were followed for mortality until December 31, 2022. The researchers created quintiles of dietary protein/kg categorized as plant or animal source, trained dietitians worked with participants to complete a 24-hour diet recall, and the primary outcome was all-cause mortality.
Overall, the mean protein intake in the study population was 1.5 g/kg body weight; the mean animal protein and plant protein intakes were 1.1 g/kg and 0.4 g/kg, respectively.
In an age-adjusted analysis, mortality rates per 1,000 person-years were significantly higher with lower total protein intake, with rates of 39.7 per 1,000 person-years and 36.8 per 1,000 person-years in the first and fifth quintiles, respectively (P < .0001).
Data Show Consistency Across Protein Types
Trends were similar for animal protein and plant protein intake, with mortality rates of 39.6 and 36.5 per 1000 person-years for the first and fifth quintiles, respectively.
“All of these categories had a significant trend, with the lowest quintile showing the highest mortality rate,” Dr. Aguilar said in his presentation.
The study was limited by several factors including the homogeneous population of Japanese men, and the inability to make conclusions about cause and effect, Dr. Aguilar said. However, the results were strengthened by the large cohort, long follow-up, and complete mortality surveillance, he added.
As for the study’s clinical implications, “I believe it adds to the body of evidence on how nutrition impacts health and [the data] can help us better advise our patients on their macronutrient intake to better optimize their health,” Dr. Aguilar said in a question-and-answer session following the presentation.
Looking ahead, “More research is needed to more accurately define which type of protein and in which amounts are optimal for health,” as well as how other macronutrients in different stages of life affect health span and life span, he said.
Although a minimum Recommended Daily Allowance of dietary protein is 0.8 g/kg body weight, the relationship between dietary protein intake and all-cause mortality remains unclear, said Shelly Gray, PharmD, professor of pharmacy at the University of Washington School of Pharmacy, said in an interview.
Dr. Gray, who served as a moderator for the session in which the study was presented, agreed that more research is needed before clinical implications can be discussed.
The study was supported by the Department of Geriatric Medicine, John A. Burns School of Medicine, University of Hawaii; Kuakini Medical Center, Honolulu, Hawaii; and the National Institutes of Health. The researchers had no financial conflicts to disclose. Dr. Gray had no financial conflicts to disclose.
Lower intake of dietary protein in midlife was a significant independent predictor of all-cause mortality in later life, based on data from a cohort study of more than 8000 men.
The Recommended Dietary Allowance of dietary protein intake is 0.8 g/kg body weight, but previous studies of the effect of dietary protein on all-cause mortality have yielded inconsistent results, Pedro Joaquin Ayau Aguilar, MD, of the University of Hawaii, Honolulu, said in a presentation at the annual meeting of the American Geriatrics Society.
To better examine these effects, Dr. Aguilar and colleagues reviewed data from 7486 participants in the Kuakini Honolulu Heart Program (HHP), a prospective cohort study of Japanese-American men in Hawaii.
Participants underwent a baseline exam in 1965-1968 at ages 45-68 years and were followed for mortality until December 31, 2022. The researchers created quintiles of dietary protein/kg categorized as plant or animal source, trained dietitians worked with participants to complete a 24-hour diet recall, and the primary outcome was all-cause mortality.
Overall, the mean protein intake in the study population was 1.5 g/kg body weight; the mean animal protein and plant protein intakes were 1.1 g/kg and 0.4 g/kg, respectively.
In an age-adjusted analysis, mortality rates per 1,000 person-years were significantly higher with lower total protein intake, with rates of 39.7 per 1,000 person-years and 36.8 per 1,000 person-years in the first and fifth quintiles, respectively (P < .0001).
Data Show Consistency Across Protein Types
Trends were similar for animal protein and plant protein intake, with mortality rates of 39.6 and 36.5 per 1000 person-years for the first and fifth quintiles, respectively.
“All of these categories had a significant trend, with the lowest quintile showing the highest mortality rate,” Dr. Aguilar said in his presentation.
The study was limited by several factors including the homogeneous population of Japanese men, and the inability to make conclusions about cause and effect, Dr. Aguilar said. However, the results were strengthened by the large cohort, long follow-up, and complete mortality surveillance, he added.
As for the study’s clinical implications, “I believe it adds to the body of evidence on how nutrition impacts health and [the data] can help us better advise our patients on their macronutrient intake to better optimize their health,” Dr. Aguilar said in a question-and-answer session following the presentation.
Looking ahead, “More research is needed to more accurately define which type of protein and in which amounts are optimal for health,” as well as how other macronutrients in different stages of life affect health span and life span, he said.
Although a minimum Recommended Daily Allowance of dietary protein is 0.8 g/kg body weight, the relationship between dietary protein intake and all-cause mortality remains unclear, said Shelly Gray, PharmD, professor of pharmacy at the University of Washington School of Pharmacy, said in an interview.
Dr. Gray, who served as a moderator for the session in which the study was presented, agreed that more research is needed before clinical implications can be discussed.
The study was supported by the Department of Geriatric Medicine, John A. Burns School of Medicine, University of Hawaii; Kuakini Medical Center, Honolulu, Hawaii; and the National Institutes of Health. The researchers had no financial conflicts to disclose. Dr. Gray had no financial conflicts to disclose.
FROM AGS 2024
Testosterone/CVD Risk Debate Revived by New Meta-Analysis
A new systematic literature review adds complexity to the controversy over testosterone’s relationship to risk for myocardial infarction, stroke, cardiovascular death, and all-cause mortality.
Last year, the TRAVERSE (Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy ResponSE in Hypogonadal Men) trial was the first randomized, placebo-controlled study designed and powered to determine whether testosterone therapy increased risk for major cardiovascular events in men (ages 45-80 years). Its conclusions provided reassurance that modest use of testosterone therapy short term does not increase CVD risk.
But other studies have had different conclusions and TRAVERSE left unanswered questions, so Bu B. Yeap, MBBS, PhD, an endocrinologist at the University of Western Australia in Crawley, and colleagues completed a literature review with 11 prospective cohort studies of community-dwelling men with sex steroid levels measured with mass spectrometry. Nine of the studies provided individual participation data (IPD); two used aggregate data, and all had at least 5 years of follow-up.
The findings were published in Annals of Internal Medicine .
Dr. Yeap’s team concluded that certain groups of men have higher risk for CVD events. In this study, men with very low testosterone, high luteinizing hormone (LH), or very low estradiol concentrations had higher all-cause mortality. Sex hormone–binding globulin (SHBG) concentration was positively associated and dihydrotestosterone (DHT) levels were nonlinearly associated with all-cause mortality and CVD mortality.
The testosterone level below which men had higher risk of death from any cause was 7.4 nmol/L (213 ng/dL), regardless of LH concentration, the researchers concluded, writing, “This adds to information on reference ranges based on distributions of testosterone in selected samples of healthy men.”
The link between higher SHBG concentrations and higher all-cause mortality “may be related to its role as the major binding protein for sex steroids in the circulation,” the authors wrote. “We found a U-shaped association of DHT with all-cause and CVD-related mortality risks, which were higher at lower and very high DHT concentrations. Men with very low DHT concentrations also had increased risk for incident CVD events. Further investigation into potential underlying mechanisms for these associations is warranted.”
Rigorous Methodology Adds Value
Bradley D. Anawalt, MD, with the University of Washington School of Medicine in Seattle, pointed out in an accompanying editorial that the study’s findings are particularly valuable because of the team’s rigorous methodology. The team measured testosterone with the gold standard, mass spectrometry, which can also measure DHT and estradiol more accurately than widely available commercial immunoassays, which “are inaccurate for measurement of these sex steroids in men, who typically have low serum concentrations of these two metabolites of testosterone,” Dr. Anawalt said.
Also, the researchers obtained raw data from the nine IPD studies and reanalyzed the combined data, which allows for more sophisticated analysis when combining data from multiple studies, Dr. Anawalt explained.
The main finding from the Yeap et al. study, he wrote, is that high testosterone concentrations at baseline were not linked with increased deaths from CVD or from all causes “but very low serum total testosterone concentrations at baseline were.
“It is tempting to hypothesize that testosterone therapy might have cardiovascular benefits solely in patients with very low concentrations of serum total testosterone,” Dr. Anawalt wrote.
He pointed out as particularly interesting the findings for DHT and estradiol.
“The finding that a low serum estradiol concentration is associated with higher all-cause mortality adds another reason (in addition to the adverse effects on body fat and bone health) to avoid aromatase inhibitors that are commonly taken by persons who use anabolic steroids,” he wrote. “The prospect of a U-shaped curve for the relationship between serum DHT and higher cardiovascular risk warrants further study.”
The work is funded by the Government of Western Australia and Lawley Pharmaceuticals. The authors’ and editorial writer’s conflicts of interest are listed in the full study.
A new systematic literature review adds complexity to the controversy over testosterone’s relationship to risk for myocardial infarction, stroke, cardiovascular death, and all-cause mortality.
Last year, the TRAVERSE (Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy ResponSE in Hypogonadal Men) trial was the first randomized, placebo-controlled study designed and powered to determine whether testosterone therapy increased risk for major cardiovascular events in men (ages 45-80 years). Its conclusions provided reassurance that modest use of testosterone therapy short term does not increase CVD risk.
But other studies have had different conclusions and TRAVERSE left unanswered questions, so Bu B. Yeap, MBBS, PhD, an endocrinologist at the University of Western Australia in Crawley, and colleagues completed a literature review with 11 prospective cohort studies of community-dwelling men with sex steroid levels measured with mass spectrometry. Nine of the studies provided individual participation data (IPD); two used aggregate data, and all had at least 5 years of follow-up.
The findings were published in Annals of Internal Medicine .
Dr. Yeap’s team concluded that certain groups of men have higher risk for CVD events. In this study, men with very low testosterone, high luteinizing hormone (LH), or very low estradiol concentrations had higher all-cause mortality. Sex hormone–binding globulin (SHBG) concentration was positively associated and dihydrotestosterone (DHT) levels were nonlinearly associated with all-cause mortality and CVD mortality.
The testosterone level below which men had higher risk of death from any cause was 7.4 nmol/L (213 ng/dL), regardless of LH concentration, the researchers concluded, writing, “This adds to information on reference ranges based on distributions of testosterone in selected samples of healthy men.”
The link between higher SHBG concentrations and higher all-cause mortality “may be related to its role as the major binding protein for sex steroids in the circulation,” the authors wrote. “We found a U-shaped association of DHT with all-cause and CVD-related mortality risks, which were higher at lower and very high DHT concentrations. Men with very low DHT concentrations also had increased risk for incident CVD events. Further investigation into potential underlying mechanisms for these associations is warranted.”
Rigorous Methodology Adds Value
Bradley D. Anawalt, MD, with the University of Washington School of Medicine in Seattle, pointed out in an accompanying editorial that the study’s findings are particularly valuable because of the team’s rigorous methodology. The team measured testosterone with the gold standard, mass spectrometry, which can also measure DHT and estradiol more accurately than widely available commercial immunoassays, which “are inaccurate for measurement of these sex steroids in men, who typically have low serum concentrations of these two metabolites of testosterone,” Dr. Anawalt said.
Also, the researchers obtained raw data from the nine IPD studies and reanalyzed the combined data, which allows for more sophisticated analysis when combining data from multiple studies, Dr. Anawalt explained.
The main finding from the Yeap et al. study, he wrote, is that high testosterone concentrations at baseline were not linked with increased deaths from CVD or from all causes “but very low serum total testosterone concentrations at baseline were.
“It is tempting to hypothesize that testosterone therapy might have cardiovascular benefits solely in patients with very low concentrations of serum total testosterone,” Dr. Anawalt wrote.
He pointed out as particularly interesting the findings for DHT and estradiol.
“The finding that a low serum estradiol concentration is associated with higher all-cause mortality adds another reason (in addition to the adverse effects on body fat and bone health) to avoid aromatase inhibitors that are commonly taken by persons who use anabolic steroids,” he wrote. “The prospect of a U-shaped curve for the relationship between serum DHT and higher cardiovascular risk warrants further study.”
The work is funded by the Government of Western Australia and Lawley Pharmaceuticals. The authors’ and editorial writer’s conflicts of interest are listed in the full study.
A new systematic literature review adds complexity to the controversy over testosterone’s relationship to risk for myocardial infarction, stroke, cardiovascular death, and all-cause mortality.
Last year, the TRAVERSE (Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy ResponSE in Hypogonadal Men) trial was the first randomized, placebo-controlled study designed and powered to determine whether testosterone therapy increased risk for major cardiovascular events in men (ages 45-80 years). Its conclusions provided reassurance that modest use of testosterone therapy short term does not increase CVD risk.
But other studies have had different conclusions and TRAVERSE left unanswered questions, so Bu B. Yeap, MBBS, PhD, an endocrinologist at the University of Western Australia in Crawley, and colleagues completed a literature review with 11 prospective cohort studies of community-dwelling men with sex steroid levels measured with mass spectrometry. Nine of the studies provided individual participation data (IPD); two used aggregate data, and all had at least 5 years of follow-up.
The findings were published in Annals of Internal Medicine .
Dr. Yeap’s team concluded that certain groups of men have higher risk for CVD events. In this study, men with very low testosterone, high luteinizing hormone (LH), or very low estradiol concentrations had higher all-cause mortality. Sex hormone–binding globulin (SHBG) concentration was positively associated and dihydrotestosterone (DHT) levels were nonlinearly associated with all-cause mortality and CVD mortality.
The testosterone level below which men had higher risk of death from any cause was 7.4 nmol/L (213 ng/dL), regardless of LH concentration, the researchers concluded, writing, “This adds to information on reference ranges based on distributions of testosterone in selected samples of healthy men.”
The link between higher SHBG concentrations and higher all-cause mortality “may be related to its role as the major binding protein for sex steroids in the circulation,” the authors wrote. “We found a U-shaped association of DHT with all-cause and CVD-related mortality risks, which were higher at lower and very high DHT concentrations. Men with very low DHT concentrations also had increased risk for incident CVD events. Further investigation into potential underlying mechanisms for these associations is warranted.”
Rigorous Methodology Adds Value
Bradley D. Anawalt, MD, with the University of Washington School of Medicine in Seattle, pointed out in an accompanying editorial that the study’s findings are particularly valuable because of the team’s rigorous methodology. The team measured testosterone with the gold standard, mass spectrometry, which can also measure DHT and estradiol more accurately than widely available commercial immunoassays, which “are inaccurate for measurement of these sex steroids in men, who typically have low serum concentrations of these two metabolites of testosterone,” Dr. Anawalt said.
Also, the researchers obtained raw data from the nine IPD studies and reanalyzed the combined data, which allows for more sophisticated analysis when combining data from multiple studies, Dr. Anawalt explained.
The main finding from the Yeap et al. study, he wrote, is that high testosterone concentrations at baseline were not linked with increased deaths from CVD or from all causes “but very low serum total testosterone concentrations at baseline were.
“It is tempting to hypothesize that testosterone therapy might have cardiovascular benefits solely in patients with very low concentrations of serum total testosterone,” Dr. Anawalt wrote.
He pointed out as particularly interesting the findings for DHT and estradiol.
“The finding that a low serum estradiol concentration is associated with higher all-cause mortality adds another reason (in addition to the adverse effects on body fat and bone health) to avoid aromatase inhibitors that are commonly taken by persons who use anabolic steroids,” he wrote. “The prospect of a U-shaped curve for the relationship between serum DHT and higher cardiovascular risk warrants further study.”
The work is funded by the Government of Western Australia and Lawley Pharmaceuticals. The authors’ and editorial writer’s conflicts of interest are listed in the full study.
FROM ANNALS OF INTERNAL MEDICINE
Inappropriate Medication Use Persists in Older Adults With Dementia
Medications that could have a negative effect on cognition are often used by older adults with dementia, according to data from approximately 13 million individuals presented at the annual meeting of the American Geriatrics Society.
Classes of medications including anticholinergics, antipsychotics, benzodiazepines, and non-benzodiazepine sedatives (Z drugs) have been identified as potentially inappropriate medications (PIMs) in patients with dementia, according to The American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults.
The medications that could worsen dementia or cognition are known as CogPIMs, said presenting author Caroline M. Mak, a doctor of pharmacy candidate at the University at Buffalo School of Pharmacy and Pharmaceutical Sciences, New York.
Previous research has characterized the prevalence of use of CogPIMs, but data connecting use of CogPIMs and healthcare use are lacking, Ms. Mak said.
Ms. Mak and colleagues conducted a cross-sectional analysis of data from 2011 to 2015 from the Medical Expenditure Panel Survey (MEPS), a national survey with data on medication and healthcare use. The researchers included approximately 13 million survey respondents older than 65 years with dementia.
Exposure to CogPIMs was defined as filling a prescription for one or more of the CogPIMs during the study period. Population estimates of the prevalence of use of the CogPIMs were created using survey-weighted procedures, and prevalence trends were assessed using the Cochran-Armitage test.
Overall, the prevalence was 15.9%, 11.5%, 7.5%, and 3.8% for use of benzodiazepines, anticholinergics, antipsychotics, and Z drugs, respectively, during the study period.
Of these, benzodiazepines showed a significant trend with an increase in prevalence from 8.9% in 2011 to 16.4% in 2015 (P = .02).
The odds of hospitalization were more than twice as likely in individuals who reported using Z drugs (odds ratio, 2.57; P = .02) based on logistic regression. In addition, exposure to antipsychotics was significantly associated with an increased rate of hospitalization based on a binomial model for incidence rate ratio (IRR, 1.51; P = .02).
The findings were limited by several factors including the cross-sectional design, reliance on self-reports, and the lack of more recent data.
However, the results show that CogPIMs are often used by older adults with dementia, and antipsychotics and Z drugs could be targets for interventions to prevent harm from medication interactions and side effects, the researchers concluded.
Findings Highlight Need for Drug Awareness
The current study is important because of the expansion in the aging population and an increase in the number of patients with dementia, Ms. Mak said in an interview. “In both our older population and dementia patients, there are certain medication considerations that we need to take into account, and certain drugs that should be avoided if possible,” she said. Clinicians have been trying to use the Beers criteria to reduce potential medication harm, she noted. “One group of investigators (Hilmer et al.), has proposed a narrower focus on anticholinergic and sedative/hypnotic medication in the Drug Burden Index (DBI); the CogPIMs are a subset of both approaches (Beers and DBI) and represent a collection of medications that pose potential risks to our patients,” said Ms. Mak.
Continued reassessment is needed on appropriateness of anticholinergics, Z drugs, benzodiazepines, and antipsychotics in older patients with dementia, she added.
“Even though the only group to have a significant increase in prevalence [of use] was the benzodiazepine group, we didn’t see a decrease in any of the other groups,” said Ms. Mak. The current research provides a benchmark for CogPIMs use that can be monitored in the future for increases or, ideally, decreases, she said.
Part of a Bigger Picture
The current study is part of the work of Team Alice, a national deprescribing group affiliated with the University at Buffalo that was inspired by the tragic death of Alice Brennan, triggered by preventable medication harm, Ms. Mak said in an interview. “Team Alice consists of an array of academic, primary care, health plan, and regional health information partners that have designed patient-driven interventions to reduce medication harm, especially within primary care settings,” she said. “Their mission is to save people like Alice by pursuing multiple strategies to deprescribe unsafe medication, reduce harm, and foster successful aging. By characterizing the use of CogPIMs, we can design better intervention strategies,” she said.
Although Ms. Mak was not surprised by the emergence of benzodiazepines as the most commonly used drug groups, she was surprised by the increase during the study period.
“Unfortunately, our dataset was not rich enough to include reasons for this increase,” she said. In practice, “I have seen patients getting short-term, as needed, prescriptions for a benzodiazepine to address the anxiety and/or insomnia after the loss of a loved one; this may account for a small proportion of benzodiazepine use that appears to be inappropriate because of a lack of associated appropriate diagnosis,” she noted.
Also, the findings of increased hospitalization associated with Z drugs raises concerns, Ms. Mak said. Although the findings are consistent with other research, they illustrate the need for further investigation to identify strategies to prevent this harm, she said. “Not finding associations with hospitalization related to benzodiazepine or anticholinergics was a mild surprise,” Ms. Mak said in an interview. “However, while we know that these drugs can have a negative effect on older people, the effects may not have been severe enough to result in hospitalizations,” she said.
Looking ahead, Ms. Mak said she would like to see the study rerun with a more current data set, especially with regard to benzodiazepines and antipsychotics.
Seek Strategies to Reduce Medication Use
The current study was notable for its community-based population and attention to hospitalizations, Shelly Gray, PharmD, a professor of pharmacy at the University of Washington School of Pharmacy, said in an interview.
“Most studies examining potentially inappropriate medications that may impair cognition have been conducted in nursing homes, while this study focuses on community dwelling older adults where most people with dementia live,” said Dr. Gray, who served as a moderator for the session in which the study was presented.
In addition, “A unique aspect of this study was to examine how these medications are related to hospitalizations,” she said.
Given recent efforts to reduce use of potentially inappropriate medications in people with dementia, the increase in prevalence of use over the study period was surprising, especially for benzodiazepines, said Dr. Gray.
In clinical practice, “health care providers should continue to look for opportunities to deprescribe medications that may worsen cognition in people with dementia,” she said. However, more research is needed to examine trends in the years beyond 2015 for a more contemporary picture of medication use in this population, she noted.
The study received no outside funding. The researchers and Dr. Gray had no financial conflicts to disclose.
Medications that could have a negative effect on cognition are often used by older adults with dementia, according to data from approximately 13 million individuals presented at the annual meeting of the American Geriatrics Society.
Classes of medications including anticholinergics, antipsychotics, benzodiazepines, and non-benzodiazepine sedatives (Z drugs) have been identified as potentially inappropriate medications (PIMs) in patients with dementia, according to The American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults.
The medications that could worsen dementia or cognition are known as CogPIMs, said presenting author Caroline M. Mak, a doctor of pharmacy candidate at the University at Buffalo School of Pharmacy and Pharmaceutical Sciences, New York.
Previous research has characterized the prevalence of use of CogPIMs, but data connecting use of CogPIMs and healthcare use are lacking, Ms. Mak said.
Ms. Mak and colleagues conducted a cross-sectional analysis of data from 2011 to 2015 from the Medical Expenditure Panel Survey (MEPS), a national survey with data on medication and healthcare use. The researchers included approximately 13 million survey respondents older than 65 years with dementia.
Exposure to CogPIMs was defined as filling a prescription for one or more of the CogPIMs during the study period. Population estimates of the prevalence of use of the CogPIMs were created using survey-weighted procedures, and prevalence trends were assessed using the Cochran-Armitage test.
Overall, the prevalence was 15.9%, 11.5%, 7.5%, and 3.8% for use of benzodiazepines, anticholinergics, antipsychotics, and Z drugs, respectively, during the study period.
Of these, benzodiazepines showed a significant trend with an increase in prevalence from 8.9% in 2011 to 16.4% in 2015 (P = .02).
The odds of hospitalization were more than twice as likely in individuals who reported using Z drugs (odds ratio, 2.57; P = .02) based on logistic regression. In addition, exposure to antipsychotics was significantly associated with an increased rate of hospitalization based on a binomial model for incidence rate ratio (IRR, 1.51; P = .02).
The findings were limited by several factors including the cross-sectional design, reliance on self-reports, and the lack of more recent data.
However, the results show that CogPIMs are often used by older adults with dementia, and antipsychotics and Z drugs could be targets for interventions to prevent harm from medication interactions and side effects, the researchers concluded.
Findings Highlight Need for Drug Awareness
The current study is important because of the expansion in the aging population and an increase in the number of patients with dementia, Ms. Mak said in an interview. “In both our older population and dementia patients, there are certain medication considerations that we need to take into account, and certain drugs that should be avoided if possible,” she said. Clinicians have been trying to use the Beers criteria to reduce potential medication harm, she noted. “One group of investigators (Hilmer et al.), has proposed a narrower focus on anticholinergic and sedative/hypnotic medication in the Drug Burden Index (DBI); the CogPIMs are a subset of both approaches (Beers and DBI) and represent a collection of medications that pose potential risks to our patients,” said Ms. Mak.
Continued reassessment is needed on appropriateness of anticholinergics, Z drugs, benzodiazepines, and antipsychotics in older patients with dementia, she added.
“Even though the only group to have a significant increase in prevalence [of use] was the benzodiazepine group, we didn’t see a decrease in any of the other groups,” said Ms. Mak. The current research provides a benchmark for CogPIMs use that can be monitored in the future for increases or, ideally, decreases, she said.
Part of a Bigger Picture
The current study is part of the work of Team Alice, a national deprescribing group affiliated with the University at Buffalo that was inspired by the tragic death of Alice Brennan, triggered by preventable medication harm, Ms. Mak said in an interview. “Team Alice consists of an array of academic, primary care, health plan, and regional health information partners that have designed patient-driven interventions to reduce medication harm, especially within primary care settings,” she said. “Their mission is to save people like Alice by pursuing multiple strategies to deprescribe unsafe medication, reduce harm, and foster successful aging. By characterizing the use of CogPIMs, we can design better intervention strategies,” she said.
Although Ms. Mak was not surprised by the emergence of benzodiazepines as the most commonly used drug groups, she was surprised by the increase during the study period.
“Unfortunately, our dataset was not rich enough to include reasons for this increase,” she said. In practice, “I have seen patients getting short-term, as needed, prescriptions for a benzodiazepine to address the anxiety and/or insomnia after the loss of a loved one; this may account for a small proportion of benzodiazepine use that appears to be inappropriate because of a lack of associated appropriate diagnosis,” she noted.
Also, the findings of increased hospitalization associated with Z drugs raises concerns, Ms. Mak said. Although the findings are consistent with other research, they illustrate the need for further investigation to identify strategies to prevent this harm, she said. “Not finding associations with hospitalization related to benzodiazepine or anticholinergics was a mild surprise,” Ms. Mak said in an interview. “However, while we know that these drugs can have a negative effect on older people, the effects may not have been severe enough to result in hospitalizations,” she said.
Looking ahead, Ms. Mak said she would like to see the study rerun with a more current data set, especially with regard to benzodiazepines and antipsychotics.
Seek Strategies to Reduce Medication Use
The current study was notable for its community-based population and attention to hospitalizations, Shelly Gray, PharmD, a professor of pharmacy at the University of Washington School of Pharmacy, said in an interview.
“Most studies examining potentially inappropriate medications that may impair cognition have been conducted in nursing homes, while this study focuses on community dwelling older adults where most people with dementia live,” said Dr. Gray, who served as a moderator for the session in which the study was presented.
In addition, “A unique aspect of this study was to examine how these medications are related to hospitalizations,” she said.
Given recent efforts to reduce use of potentially inappropriate medications in people with dementia, the increase in prevalence of use over the study period was surprising, especially for benzodiazepines, said Dr. Gray.
In clinical practice, “health care providers should continue to look for opportunities to deprescribe medications that may worsen cognition in people with dementia,” she said. However, more research is needed to examine trends in the years beyond 2015 for a more contemporary picture of medication use in this population, she noted.
The study received no outside funding. The researchers and Dr. Gray had no financial conflicts to disclose.
Medications that could have a negative effect on cognition are often used by older adults with dementia, according to data from approximately 13 million individuals presented at the annual meeting of the American Geriatrics Society.
Classes of medications including anticholinergics, antipsychotics, benzodiazepines, and non-benzodiazepine sedatives (Z drugs) have been identified as potentially inappropriate medications (PIMs) in patients with dementia, according to The American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults.
The medications that could worsen dementia or cognition are known as CogPIMs, said presenting author Caroline M. Mak, a doctor of pharmacy candidate at the University at Buffalo School of Pharmacy and Pharmaceutical Sciences, New York.
Previous research has characterized the prevalence of use of CogPIMs, but data connecting use of CogPIMs and healthcare use are lacking, Ms. Mak said.
Ms. Mak and colleagues conducted a cross-sectional analysis of data from 2011 to 2015 from the Medical Expenditure Panel Survey (MEPS), a national survey with data on medication and healthcare use. The researchers included approximately 13 million survey respondents older than 65 years with dementia.
Exposure to CogPIMs was defined as filling a prescription for one or more of the CogPIMs during the study period. Population estimates of the prevalence of use of the CogPIMs were created using survey-weighted procedures, and prevalence trends were assessed using the Cochran-Armitage test.
Overall, the prevalence was 15.9%, 11.5%, 7.5%, and 3.8% for use of benzodiazepines, anticholinergics, antipsychotics, and Z drugs, respectively, during the study period.
Of these, benzodiazepines showed a significant trend with an increase in prevalence from 8.9% in 2011 to 16.4% in 2015 (P = .02).
The odds of hospitalization were more than twice as likely in individuals who reported using Z drugs (odds ratio, 2.57; P = .02) based on logistic regression. In addition, exposure to antipsychotics was significantly associated with an increased rate of hospitalization based on a binomial model for incidence rate ratio (IRR, 1.51; P = .02).
The findings were limited by several factors including the cross-sectional design, reliance on self-reports, and the lack of more recent data.
However, the results show that CogPIMs are often used by older adults with dementia, and antipsychotics and Z drugs could be targets for interventions to prevent harm from medication interactions and side effects, the researchers concluded.
Findings Highlight Need for Drug Awareness
The current study is important because of the expansion in the aging population and an increase in the number of patients with dementia, Ms. Mak said in an interview. “In both our older population and dementia patients, there are certain medication considerations that we need to take into account, and certain drugs that should be avoided if possible,” she said. Clinicians have been trying to use the Beers criteria to reduce potential medication harm, she noted. “One group of investigators (Hilmer et al.), has proposed a narrower focus on anticholinergic and sedative/hypnotic medication in the Drug Burden Index (DBI); the CogPIMs are a subset of both approaches (Beers and DBI) and represent a collection of medications that pose potential risks to our patients,” said Ms. Mak.
Continued reassessment is needed on appropriateness of anticholinergics, Z drugs, benzodiazepines, and antipsychotics in older patients with dementia, she added.
“Even though the only group to have a significant increase in prevalence [of use] was the benzodiazepine group, we didn’t see a decrease in any of the other groups,” said Ms. Mak. The current research provides a benchmark for CogPIMs use that can be monitored in the future for increases or, ideally, decreases, she said.
Part of a Bigger Picture
The current study is part of the work of Team Alice, a national deprescribing group affiliated with the University at Buffalo that was inspired by the tragic death of Alice Brennan, triggered by preventable medication harm, Ms. Mak said in an interview. “Team Alice consists of an array of academic, primary care, health plan, and regional health information partners that have designed patient-driven interventions to reduce medication harm, especially within primary care settings,” she said. “Their mission is to save people like Alice by pursuing multiple strategies to deprescribe unsafe medication, reduce harm, and foster successful aging. By characterizing the use of CogPIMs, we can design better intervention strategies,” she said.
Although Ms. Mak was not surprised by the emergence of benzodiazepines as the most commonly used drug groups, she was surprised by the increase during the study period.
“Unfortunately, our dataset was not rich enough to include reasons for this increase,” she said. In practice, “I have seen patients getting short-term, as needed, prescriptions for a benzodiazepine to address the anxiety and/or insomnia after the loss of a loved one; this may account for a small proportion of benzodiazepine use that appears to be inappropriate because of a lack of associated appropriate diagnosis,” she noted.
Also, the findings of increased hospitalization associated with Z drugs raises concerns, Ms. Mak said. Although the findings are consistent with other research, they illustrate the need for further investigation to identify strategies to prevent this harm, she said. “Not finding associations with hospitalization related to benzodiazepine or anticholinergics was a mild surprise,” Ms. Mak said in an interview. “However, while we know that these drugs can have a negative effect on older people, the effects may not have been severe enough to result in hospitalizations,” she said.
Looking ahead, Ms. Mak said she would like to see the study rerun with a more current data set, especially with regard to benzodiazepines and antipsychotics.
Seek Strategies to Reduce Medication Use
The current study was notable for its community-based population and attention to hospitalizations, Shelly Gray, PharmD, a professor of pharmacy at the University of Washington School of Pharmacy, said in an interview.
“Most studies examining potentially inappropriate medications that may impair cognition have been conducted in nursing homes, while this study focuses on community dwelling older adults where most people with dementia live,” said Dr. Gray, who served as a moderator for the session in which the study was presented.
In addition, “A unique aspect of this study was to examine how these medications are related to hospitalizations,” she said.
Given recent efforts to reduce use of potentially inappropriate medications in people with dementia, the increase in prevalence of use over the study period was surprising, especially for benzodiazepines, said Dr. Gray.
In clinical practice, “health care providers should continue to look for opportunities to deprescribe medications that may worsen cognition in people with dementia,” she said. However, more research is needed to examine trends in the years beyond 2015 for a more contemporary picture of medication use in this population, she noted.
The study received no outside funding. The researchers and Dr. Gray had no financial conflicts to disclose.
FROM AGS 2024
Clinical Guidelines: Start Screening at Age 50 for Age-Related Hearing Loss
Clinical guidelines on age-related hearing loss (ARHL), published in Otolaryngology–Head and Neck Surgery, highlight referral recommendations for all clinicians, including primary care doctors, who often are the first clinicians to screen for and address the condition.
Betty S. Tsai Do, MD, with the department of head & neck surgery at Kaiser Permanente in Walnut Creek, California, is the first author for the guidelines, which recommend screening patients 50 years or older at the time of a healthcare encounter. They also detail when to test and refer.
Three ‘Strong Recommendations’
Three of the action points are labeled “strong recommendations.” They are:
- If screening suggests hearing loss, clinicians should conduct an audiogram or refer to a clinician who can conduct one.
- Clinicians should offer, or refer to a specialist who can offer, appropriately fit amplification, such as hearing aids.
- If patients have appropriately fit amplification and still have trouble with hearing and understanding speech, clinicians should refer patients to see if they are good candidates for a cochlear implant.
The authors note that ARHL is the most common sensory deficit seen in older patients, but it is underdiagnosed and undertreated. “Between ages 65 and 74, one in three adults experience hearing loss and almost 50% of those 75 years of age or older will report hearing loss according to the National Institute on Deafness and Other Communication Disorders.” Consequences of the untreated deficit, in addition to limiting ability to communicate, include higher risk of dementia, cardiovascular disease, depression, falls, and workplace marginalization.
Until now, there have been no evidence-based clinical guidelines on when to screen, test, and refer. Though previously proposed quality improvement measures have defined ARHL as starting at age 60, these guidelines include those 50 and older to promote earlier detection.
Guidelines Only Part of the Solution
While the guidelines are a step in the right direction, they won’t address some persistent barriers to changing practice, said Michael McKee, MD, MPH, a family medicine physician and co-director of the Center for Disability Health and Wellness at the University of Michigan in Ann Arbor, who was not part of the guideline team.
“I think [the guidelines] will raise the awareness on why it’s important to address hearing loss,” he says. “Many primary care providers don’t elevate hearing loss as a priority topic. The problem is that we’re struggling with getting things in place to have a more supportive system to carry out those recommendations.”
Lack of Training and Support
The problems include lack of training on hearing loss for physicians, starting with medical school. Another complication is time: A conversation about hearing loss adds to the multitude of conversations a primary care provider is expected to have with their patients in a short visit.
Additionally, when hearing loss is suspected, an audiologist may be hard to find to perform the audiogram, Dr. McKee says. If patients agree to see an audiologist and that specialist finds hearing loss, patients may not want to wear a device due to stigma or may not be able to afford a device that will fit properly and truly benefit them because Medicare does not cover hearing aids.
“Only about 20-plus percent of those eligible for hearing aids get them,” he said. Hearing aids available over the counter help some people, but may be difficult to fit properly and may be hard for some to use correctly, he added.
“That comes back to the primary care provider, so it’s unfortunately a very unsatisfying course,” he said.
‘Primary Care Providers Do Value Guidelines’
However, “Primary care providers do value guidelines. They do value strong recommendations,” he said. We are trying to figure out how we can support people with unaddressed hearing loss in the primary care setting, Dr. McKee said. “Once we get there, we need to advocate for an expansion of coverage,” he said.
The authors note that the messages in the guidelines are important for all clinicians.
“The impact of hearing loss and screening should not be the sole responsibility of an audiologist, an otolaryngologist, nor primary care provider. Any time and place that a patient interacts with the healthcare system is an opportunity for preventive healthcare, such as hearing screening, to occur,” they write.
Funding for this research was provided by the American Academy of Otolaryngology–Head and Neck Surgery Foundation. Dr. Do and Dr. McKee report no relevant financial relationships. Full disclosures of the co-authors are listed with the full text of the paper.
Clinical guidelines on age-related hearing loss (ARHL), published in Otolaryngology–Head and Neck Surgery, highlight referral recommendations for all clinicians, including primary care doctors, who often are the first clinicians to screen for and address the condition.
Betty S. Tsai Do, MD, with the department of head & neck surgery at Kaiser Permanente in Walnut Creek, California, is the first author for the guidelines, which recommend screening patients 50 years or older at the time of a healthcare encounter. They also detail when to test and refer.
Three ‘Strong Recommendations’
Three of the action points are labeled “strong recommendations.” They are:
- If screening suggests hearing loss, clinicians should conduct an audiogram or refer to a clinician who can conduct one.
- Clinicians should offer, or refer to a specialist who can offer, appropriately fit amplification, such as hearing aids.
- If patients have appropriately fit amplification and still have trouble with hearing and understanding speech, clinicians should refer patients to see if they are good candidates for a cochlear implant.
The authors note that ARHL is the most common sensory deficit seen in older patients, but it is underdiagnosed and undertreated. “Between ages 65 and 74, one in three adults experience hearing loss and almost 50% of those 75 years of age or older will report hearing loss according to the National Institute on Deafness and Other Communication Disorders.” Consequences of the untreated deficit, in addition to limiting ability to communicate, include higher risk of dementia, cardiovascular disease, depression, falls, and workplace marginalization.
Until now, there have been no evidence-based clinical guidelines on when to screen, test, and refer. Though previously proposed quality improvement measures have defined ARHL as starting at age 60, these guidelines include those 50 and older to promote earlier detection.
Guidelines Only Part of the Solution
While the guidelines are a step in the right direction, they won’t address some persistent barriers to changing practice, said Michael McKee, MD, MPH, a family medicine physician and co-director of the Center for Disability Health and Wellness at the University of Michigan in Ann Arbor, who was not part of the guideline team.
“I think [the guidelines] will raise the awareness on why it’s important to address hearing loss,” he says. “Many primary care providers don’t elevate hearing loss as a priority topic. The problem is that we’re struggling with getting things in place to have a more supportive system to carry out those recommendations.”
Lack of Training and Support
The problems include lack of training on hearing loss for physicians, starting with medical school. Another complication is time: A conversation about hearing loss adds to the multitude of conversations a primary care provider is expected to have with their patients in a short visit.
Additionally, when hearing loss is suspected, an audiologist may be hard to find to perform the audiogram, Dr. McKee says. If patients agree to see an audiologist and that specialist finds hearing loss, patients may not want to wear a device due to stigma or may not be able to afford a device that will fit properly and truly benefit them because Medicare does not cover hearing aids.
“Only about 20-plus percent of those eligible for hearing aids get them,” he said. Hearing aids available over the counter help some people, but may be difficult to fit properly and may be hard for some to use correctly, he added.
“That comes back to the primary care provider, so it’s unfortunately a very unsatisfying course,” he said.
‘Primary Care Providers Do Value Guidelines’
However, “Primary care providers do value guidelines. They do value strong recommendations,” he said. We are trying to figure out how we can support people with unaddressed hearing loss in the primary care setting, Dr. McKee said. “Once we get there, we need to advocate for an expansion of coverage,” he said.
The authors note that the messages in the guidelines are important for all clinicians.
“The impact of hearing loss and screening should not be the sole responsibility of an audiologist, an otolaryngologist, nor primary care provider. Any time and place that a patient interacts with the healthcare system is an opportunity for preventive healthcare, such as hearing screening, to occur,” they write.
Funding for this research was provided by the American Academy of Otolaryngology–Head and Neck Surgery Foundation. Dr. Do and Dr. McKee report no relevant financial relationships. Full disclosures of the co-authors are listed with the full text of the paper.
Clinical guidelines on age-related hearing loss (ARHL), published in Otolaryngology–Head and Neck Surgery, highlight referral recommendations for all clinicians, including primary care doctors, who often are the first clinicians to screen for and address the condition.
Betty S. Tsai Do, MD, with the department of head & neck surgery at Kaiser Permanente in Walnut Creek, California, is the first author for the guidelines, which recommend screening patients 50 years or older at the time of a healthcare encounter. They also detail when to test and refer.
Three ‘Strong Recommendations’
Three of the action points are labeled “strong recommendations.” They are:
- If screening suggests hearing loss, clinicians should conduct an audiogram or refer to a clinician who can conduct one.
- Clinicians should offer, or refer to a specialist who can offer, appropriately fit amplification, such as hearing aids.
- If patients have appropriately fit amplification and still have trouble with hearing and understanding speech, clinicians should refer patients to see if they are good candidates for a cochlear implant.
The authors note that ARHL is the most common sensory deficit seen in older patients, but it is underdiagnosed and undertreated. “Between ages 65 and 74, one in three adults experience hearing loss and almost 50% of those 75 years of age or older will report hearing loss according to the National Institute on Deafness and Other Communication Disorders.” Consequences of the untreated deficit, in addition to limiting ability to communicate, include higher risk of dementia, cardiovascular disease, depression, falls, and workplace marginalization.
Until now, there have been no evidence-based clinical guidelines on when to screen, test, and refer. Though previously proposed quality improvement measures have defined ARHL as starting at age 60, these guidelines include those 50 and older to promote earlier detection.
Guidelines Only Part of the Solution
While the guidelines are a step in the right direction, they won’t address some persistent barriers to changing practice, said Michael McKee, MD, MPH, a family medicine physician and co-director of the Center for Disability Health and Wellness at the University of Michigan in Ann Arbor, who was not part of the guideline team.
“I think [the guidelines] will raise the awareness on why it’s important to address hearing loss,” he says. “Many primary care providers don’t elevate hearing loss as a priority topic. The problem is that we’re struggling with getting things in place to have a more supportive system to carry out those recommendations.”
Lack of Training and Support
The problems include lack of training on hearing loss for physicians, starting with medical school. Another complication is time: A conversation about hearing loss adds to the multitude of conversations a primary care provider is expected to have with their patients in a short visit.
Additionally, when hearing loss is suspected, an audiologist may be hard to find to perform the audiogram, Dr. McKee says. If patients agree to see an audiologist and that specialist finds hearing loss, patients may not want to wear a device due to stigma or may not be able to afford a device that will fit properly and truly benefit them because Medicare does not cover hearing aids.
“Only about 20-plus percent of those eligible for hearing aids get them,” he said. Hearing aids available over the counter help some people, but may be difficult to fit properly and may be hard for some to use correctly, he added.
“That comes back to the primary care provider, so it’s unfortunately a very unsatisfying course,” he said.
‘Primary Care Providers Do Value Guidelines’
However, “Primary care providers do value guidelines. They do value strong recommendations,” he said. We are trying to figure out how we can support people with unaddressed hearing loss in the primary care setting, Dr. McKee said. “Once we get there, we need to advocate for an expansion of coverage,” he said.
The authors note that the messages in the guidelines are important for all clinicians.
“The impact of hearing loss and screening should not be the sole responsibility of an audiologist, an otolaryngologist, nor primary care provider. Any time and place that a patient interacts with the healthcare system is an opportunity for preventive healthcare, such as hearing screening, to occur,” they write.
Funding for this research was provided by the American Academy of Otolaryngology–Head and Neck Surgery Foundation. Dr. Do and Dr. McKee report no relevant financial relationships. Full disclosures of the co-authors are listed with the full text of the paper.
FROM OTOLARYNGOLOGY–HEAD AND NECK SURGERY
From Stigma to Support: Raising Awareness of Pelvic Organ Prolapse
Sherrie Palm, a patient advocate in Mukwonago, Wisconsin, learned in her 30s that she needed to educate herself about her own health. So when she discovered a walnut-sized lump coming out of her vagina in her mid-50s, she was stunned when her primary care provider (PCP) told her it was pelvic organ prolapse (POP), where one or more organs descend into the vaginal cavity.
“I was shocked,” Ms. Palm said. After searching online and discovering how prevalent POP was, her shock turned to anger. “I was blown away that it could be this common and I’d never heard of it,” she said. “I knew within 2 weeks that I had to do something to change the status quo.”
Ms. Palm eventually founded the nonprofit Association for Pelvic Organ Prolapse Support, or APOPS, complete with a forum where women can learn about POP and support one another. She said awareness has improved substantially since her diagnosis in 2007, but “we have a long way to go” because POP and vaginal health in general are so stigmatized.
Her website notes that about half of women with incontinence do not seek help, largely because of stigma. “The status quo is that PCPs do not POP screen,” she said. ObGyns may screen but often “because the patient has asked to be screened, they say it’s not that bad, come back and see me in a year, and do your Kegels,” Ms. Palm said.
Doctors who diagnose POP agree that the issue is often off PCPs’ radar.
“Primary care doctors are really in a time crunch, so this is one of the things that may not get addressed,” Jill Rabin, MD, vice chair of education and development in obstetrics and gynecology at Northwell Health in New York, said. Dr. Rabin is also head of urogynecology at Long Island Jewish Medical Center.
Ann Nwabuebo, PT, DPT, owner and founder of Body Connect Physical Therapy in Bethesda, Maryland, said social media has been shifting the attitude that pelvic health is a taboo subject. “It’s empowering people to seek care if they’re not finding physicians who are helping.”
But social media is also a double-edged sword, said Jenny LaCross, PT, DPT, PhD, a physical therapist at MOVE PT in Monroe, Michigan, and a postdoctoral research fellow with Michigan Medicine’s Pelvic Floor Research Group. “Pelvic health in general is talked about a lot more, but there’s also a lot more misinformation,” she said.
Part of that misinformation is the idea that pelvic prolapse is solely about weakness in the pelvic floor when it can also result from a widening of natural openings within the pelvis, Dr. LaCross said. She pointed to the two definitions of pelvic organ prolapse by the International Urogynecologic Consultation and the International Continence Society, both of which have been updated in recent years.
“This is why this is challenging for primary care providers,” Dr. LaCross said. “Even urogynecologists who are the specialists that treat prolapse and incontinence have changed how they assess it and the terminology and criteria that they use.”
What hasn’t changed is the substantial negative impact POP can have on quality of life. “This is the second most common reason that women enter nursing homes,” primarily because of urinary incontinence, Dr. Rabin said. “It’s very debilitating, but a lot of it is preventable and a lot is treatable.”
Dr. Rabin estimated that three out of every five women older than 60 and one or two out of every five women younger than 60 experience POP. Prevalence studies vary widely, from nearly a quarter of women to more than half, and racial and ethnic disparities in diagnosis further complicate the statistics.
PCPs therefore have an important role to play in screening for POP. The evidence shows that “patients want their providers to bring this up,” Dr. LaCross said. “They want to talk about it, but they want the provider to ask the questions first.”
Causes, Risk Factors, and Symptoms
Many causes contribute to POP, with gravity, aging, childbirth, and menopause at the top of the list.
“As people get older, their pelvic muscles and connective tissue get weaker, and the nerves don’t function as well,” Dr. Rabin said. Meanwhile, the body is losing estrogen, which affects how well the muscles contract and how easily the connective tissue can tear, she said.
With menopause, when baseline estrogen is lower, the tissue integrity is not as supportive as it should be and women are going to be at an increased risk of prolapse, Dr. Nwabuebo said.
POP has a range of risk factors:
- Increasing age, as muscle mass decreases and connective tissue hardens.
- Menopause.
- Vaginal delivery with complications, such as long second-stage labor, instrument-assisted delivery, multiple vaginal lacerations, and improperly repaired episiotomy.
- Multiple vaginal deliveries.
- Birthing large babies.
- Family history of pelvic organ prolapse (genetics can play a role in POP risk).
- Previous pelvic/abdominal surgery, including cesarean delivery and hysterectomy.
- Smoking (largely because of associated coughing).
- Chronic lung conditions that cause a lot of coughing.
- Chronic constipation or irritable bowel syndrome.
- Some types of high-impact activity, such as jogging or marathon running.
- Early menopause, for younger women.
- Repetitive heavy lifting in daily activities, such as occupational lifting (though not necessarily weight lifting as an exercise).
- Higher body mass index.
- Connective tissue disorders, such as joint hypermobility syndrome or Ehlers-Danlos syndrome.
Roger Dmochowski, MD, professor of urology and surgery at Vanderbilt University Medical Center, groups POP symptoms into two groups: anatomic and functional ones. A common anatomic symptom is bulging. “They’ll describe sitting on a ball, feeling like their bladder or something’s falling out, feeling a pressure or a heaviness,” Dr. Dmochowski said.
Functional symptoms can include vaginal dryness, vaginal irritation, painful intercourse, contact of the vaginal tissues with underclothes, and associated urinary symptoms, such as stress incontinence, urge incontinence, and incomplete emptying of the bladder. Dr. Dmochowski noted that women who report urinary incontinence may be at risk for being prescribed a medication without the necessary referral to a specialist for a full gynecologic evaluation.
Two other groups of functional symptoms include bowel-related disorders – primarily fecal incontinence and ongoing constipation – and pelvic pain or discomfort.
There can also be asymptomatic cases. “A lot of women have what we call silent prolapse,” Dr. Dmochowski said. That is, “they have some degree of loss of support to the bladder, vagina, or uterus, but they’re not symptomatic.” These women may be particularly good candidates for pelvic health physical therapy.
Screening and Diagnosis
Because many postmenopausal women stop seeing their ob.gyn, it’s often up to their primary care physician to determine whether their patients are experiencing POP symptoms.
“Women sometimes don’t bring this up with their doctor because they think there’s not enough time, or they’ll be laughed at, or their friends told them this is normal,” Dr. Rabin said. But primary care providers are really in a unique position to be able to ask the key symptom questions.
Dr. Rabin recommends a couple of questions to cover all the bases: “Do you leak urine when you cough or sneeze or on the way to the bathroom? Do you notice a bulge coming out of the vagina, or are you bothered by pelvic pressure?”
Dr. Dmochowski offered a single question that can open the conversation to more questions: “Are you bothered by any urinary or bowel or vaginal issues that we should talk about?” He also suggests asking how bothersome the symptoms are, which can help in directing treatment or prevention options. A physical exam can reveal signs of POP as well.
Diagnosis involves a detailed history, a comprehensive physical exam, and assessment with the Pelvic Organ Prolapse Quantification (POP-Q) tool. A urogynecologist can diagnose the type of POP – such as cystocele, rectocele, enterocele, uterine prolapse, or vaginal vault prolapse – and its grade (0-4).
Treatment: Physical Therapy, Pessary, and Surgery
No medications can treat prolapse, though some can treat downstream effects, such as hormonal vaginal creams for vaginal dryness and irritation, and medications for urinary incontinence. However, two mistakes PCPs can make are sending someone straight to surgery or prescribing them medication for symptoms without referring them for a diagnostic evaluation, Dr. Rabin said. “You have to have a diagnosis first to know what type of prolapse is there,” she said.
Because there can be long waiting lists for a urogynecologist or urologist, PCPs should also refer their patients to a pelvic health physical therapist (PT) who can help patients begin addressing the symptoms while they await a specialist who can diagnose them.
Though PT is often thought of as preventive, it’s also a conservative first-line intervention for prolapse, Dr. Nwabuebo said. Strong evidence shows pelvic floor muscle training from pelvic health PT can reduce symptoms of prolapse and reduce the severity by one grade in those with a grade 1 or 2 prolapse. Stage 3 is trickier, where PT may or may not be able to shift the symptom presentation, Dr. Nwabeubo said, and stage 4 is usually a surgical candidate.
“If you have a grade 4 prolapse, or the tissues are really visible outside the body, physical therapy and pelvic floor muscle training is not going to elevate that tissue back up into your body, but it can sometimes help with symptoms,” Dr. LaCross said.
The PT conducts a thorough pelvic muscle assessment, discusses lifestyle, and may teach breathing and bracing strategies for lifting, for example.
“A lot of what we’re talking about with pelvic floor therapy is lifestyle modifications,” Dr. Nwabuebo said. “If I have a patient with a history of chronic constipation, it doesn’t matter how much we do pelvic floor exercises; if we don’t manage the constipation issues by addressing their nutrition, then straining when using the bathroom will keep putting pressure on the pelvic floor.”
PTs can also recommend appropriate vaginal weights and dilators to help with pelvic floor strengthening and teach patients how to use them properly.
Even if women ultimately opt for surgery, PT prior to surgery can be beneficial. Dr. Rabin cited three reasons she recommends first-line PT: It may elevate the bladder enough to reduce stress incontinence and thicken the pelvic muscles, it can improve the effectiveness of a pessary or surgery if the woman chooses one of those options, and it can quiet bladder contractions, potentially obviating the need for pharmacologic treatment for overactive bladder.
The next nonsurgical option is a pessary, a device that fits into the vagina to provide support to the tissues displaced by prolapse. There’s a wide range of pessary types: some are short-term, worn only daily, or disposable, while others can be worn longer. Some women can self-insert and remove the pessary, and others may need a clinician to do so. Dr. Dmochowski recommends patients try a pessary to see if it benefits them. About a third of women will find them comfortable enough to wear regularly, but others will feel more sensitive to the pessary’s presence, he said.
One of the newest, most innovative pessary options for women is Gynethotics, which received Food and Drug Administration (FDA) clearance in March, as the first 3D-printed, customizable pessary capable of nearly 10 million configurations based on a person’s body.
Nearly all stage 4 prolapses and most of stage 3 prolapses can be addressed only through transvaginal or transabdominal surgery.
“We tell patients, if you can get 10 years out of your operation, you’re lucky,” Dr. Dmochowski said. A major reason for the short-lived durability is the poor quality of the tissue that needs to be pulled together. Serious complications resulting from use of polypropylene mesh during prolapse surgery led the FDA to halt sales of the devices and recommend discontinuing their use. However, one type of vaginal mesh is still considered safe to use in sacral colpopexy surgery.
Three things can shorten the durability of the surgery, Dr. Dmochowski said: heavy lifting, particularly anything over 30 pounds; chronic coughing, such as in those with chronic lung conditions; and chronic constipation.
Ms. Palm tried a pessary for her grade 3 prolapse with cystocele, rectocele, and enterocele but didn’t feel she had the time to use it regularly, so she opted for surgery. After a week on the couch recovering, she took it easy for another 12 weeks. Since then, she’s dedicated much of her time to educating and supporting women with POP and combating stigma associated with it. The APOPS website that she started has become a valuable resource for PCPs to send patients to, and the forum includes more 27,000 women from around the world.
“We encourage women to share what they’re experiencing. Tell your family, tell your friends, tell the people you work with about it,” Ms. Palm said. But many still feel uncomfortable speaking up, making PCPs’ role even more important.
*This story was updated on May 14, 2024.
Sherrie Palm, a patient advocate in Mukwonago, Wisconsin, learned in her 30s that she needed to educate herself about her own health. So when she discovered a walnut-sized lump coming out of her vagina in her mid-50s, she was stunned when her primary care provider (PCP) told her it was pelvic organ prolapse (POP), where one or more organs descend into the vaginal cavity.
“I was shocked,” Ms. Palm said. After searching online and discovering how prevalent POP was, her shock turned to anger. “I was blown away that it could be this common and I’d never heard of it,” she said. “I knew within 2 weeks that I had to do something to change the status quo.”
Ms. Palm eventually founded the nonprofit Association for Pelvic Organ Prolapse Support, or APOPS, complete with a forum where women can learn about POP and support one another. She said awareness has improved substantially since her diagnosis in 2007, but “we have a long way to go” because POP and vaginal health in general are so stigmatized.
Her website notes that about half of women with incontinence do not seek help, largely because of stigma. “The status quo is that PCPs do not POP screen,” she said. ObGyns may screen but often “because the patient has asked to be screened, they say it’s not that bad, come back and see me in a year, and do your Kegels,” Ms. Palm said.
Doctors who diagnose POP agree that the issue is often off PCPs’ radar.
“Primary care doctors are really in a time crunch, so this is one of the things that may not get addressed,” Jill Rabin, MD, vice chair of education and development in obstetrics and gynecology at Northwell Health in New York, said. Dr. Rabin is also head of urogynecology at Long Island Jewish Medical Center.
Ann Nwabuebo, PT, DPT, owner and founder of Body Connect Physical Therapy in Bethesda, Maryland, said social media has been shifting the attitude that pelvic health is a taboo subject. “It’s empowering people to seek care if they’re not finding physicians who are helping.”
But social media is also a double-edged sword, said Jenny LaCross, PT, DPT, PhD, a physical therapist at MOVE PT in Monroe, Michigan, and a postdoctoral research fellow with Michigan Medicine’s Pelvic Floor Research Group. “Pelvic health in general is talked about a lot more, but there’s also a lot more misinformation,” she said.
Part of that misinformation is the idea that pelvic prolapse is solely about weakness in the pelvic floor when it can also result from a widening of natural openings within the pelvis, Dr. LaCross said. She pointed to the two definitions of pelvic organ prolapse by the International Urogynecologic Consultation and the International Continence Society, both of which have been updated in recent years.
“This is why this is challenging for primary care providers,” Dr. LaCross said. “Even urogynecologists who are the specialists that treat prolapse and incontinence have changed how they assess it and the terminology and criteria that they use.”
What hasn’t changed is the substantial negative impact POP can have on quality of life. “This is the second most common reason that women enter nursing homes,” primarily because of urinary incontinence, Dr. Rabin said. “It’s very debilitating, but a lot of it is preventable and a lot is treatable.”
Dr. Rabin estimated that three out of every five women older than 60 and one or two out of every five women younger than 60 experience POP. Prevalence studies vary widely, from nearly a quarter of women to more than half, and racial and ethnic disparities in diagnosis further complicate the statistics.
PCPs therefore have an important role to play in screening for POP. The evidence shows that “patients want their providers to bring this up,” Dr. LaCross said. “They want to talk about it, but they want the provider to ask the questions first.”
Causes, Risk Factors, and Symptoms
Many causes contribute to POP, with gravity, aging, childbirth, and menopause at the top of the list.
“As people get older, their pelvic muscles and connective tissue get weaker, and the nerves don’t function as well,” Dr. Rabin said. Meanwhile, the body is losing estrogen, which affects how well the muscles contract and how easily the connective tissue can tear, she said.
With menopause, when baseline estrogen is lower, the tissue integrity is not as supportive as it should be and women are going to be at an increased risk of prolapse, Dr. Nwabuebo said.
POP has a range of risk factors:
- Increasing age, as muscle mass decreases and connective tissue hardens.
- Menopause.
- Vaginal delivery with complications, such as long second-stage labor, instrument-assisted delivery, multiple vaginal lacerations, and improperly repaired episiotomy.
- Multiple vaginal deliveries.
- Birthing large babies.
- Family history of pelvic organ prolapse (genetics can play a role in POP risk).
- Previous pelvic/abdominal surgery, including cesarean delivery and hysterectomy.
- Smoking (largely because of associated coughing).
- Chronic lung conditions that cause a lot of coughing.
- Chronic constipation or irritable bowel syndrome.
- Some types of high-impact activity, such as jogging or marathon running.
- Early menopause, for younger women.
- Repetitive heavy lifting in daily activities, such as occupational lifting (though not necessarily weight lifting as an exercise).
- Higher body mass index.
- Connective tissue disorders, such as joint hypermobility syndrome or Ehlers-Danlos syndrome.
Roger Dmochowski, MD, professor of urology and surgery at Vanderbilt University Medical Center, groups POP symptoms into two groups: anatomic and functional ones. A common anatomic symptom is bulging. “They’ll describe sitting on a ball, feeling like their bladder or something’s falling out, feeling a pressure or a heaviness,” Dr. Dmochowski said.
Functional symptoms can include vaginal dryness, vaginal irritation, painful intercourse, contact of the vaginal tissues with underclothes, and associated urinary symptoms, such as stress incontinence, urge incontinence, and incomplete emptying of the bladder. Dr. Dmochowski noted that women who report urinary incontinence may be at risk for being prescribed a medication without the necessary referral to a specialist for a full gynecologic evaluation.
Two other groups of functional symptoms include bowel-related disorders – primarily fecal incontinence and ongoing constipation – and pelvic pain or discomfort.
There can also be asymptomatic cases. “A lot of women have what we call silent prolapse,” Dr. Dmochowski said. That is, “they have some degree of loss of support to the bladder, vagina, or uterus, but they’re not symptomatic.” These women may be particularly good candidates for pelvic health physical therapy.
Screening and Diagnosis
Because many postmenopausal women stop seeing their ob.gyn, it’s often up to their primary care physician to determine whether their patients are experiencing POP symptoms.
“Women sometimes don’t bring this up with their doctor because they think there’s not enough time, or they’ll be laughed at, or their friends told them this is normal,” Dr. Rabin said. But primary care providers are really in a unique position to be able to ask the key symptom questions.
Dr. Rabin recommends a couple of questions to cover all the bases: “Do you leak urine when you cough or sneeze or on the way to the bathroom? Do you notice a bulge coming out of the vagina, or are you bothered by pelvic pressure?”
Dr. Dmochowski offered a single question that can open the conversation to more questions: “Are you bothered by any urinary or bowel or vaginal issues that we should talk about?” He also suggests asking how bothersome the symptoms are, which can help in directing treatment or prevention options. A physical exam can reveal signs of POP as well.
Diagnosis involves a detailed history, a comprehensive physical exam, and assessment with the Pelvic Organ Prolapse Quantification (POP-Q) tool. A urogynecologist can diagnose the type of POP – such as cystocele, rectocele, enterocele, uterine prolapse, or vaginal vault prolapse – and its grade (0-4).
Treatment: Physical Therapy, Pessary, and Surgery
No medications can treat prolapse, though some can treat downstream effects, such as hormonal vaginal creams for vaginal dryness and irritation, and medications for urinary incontinence. However, two mistakes PCPs can make are sending someone straight to surgery or prescribing them medication for symptoms without referring them for a diagnostic evaluation, Dr. Rabin said. “You have to have a diagnosis first to know what type of prolapse is there,” she said.
Because there can be long waiting lists for a urogynecologist or urologist, PCPs should also refer their patients to a pelvic health physical therapist (PT) who can help patients begin addressing the symptoms while they await a specialist who can diagnose them.
Though PT is often thought of as preventive, it’s also a conservative first-line intervention for prolapse, Dr. Nwabuebo said. Strong evidence shows pelvic floor muscle training from pelvic health PT can reduce symptoms of prolapse and reduce the severity by one grade in those with a grade 1 or 2 prolapse. Stage 3 is trickier, where PT may or may not be able to shift the symptom presentation, Dr. Nwabeubo said, and stage 4 is usually a surgical candidate.
“If you have a grade 4 prolapse, or the tissues are really visible outside the body, physical therapy and pelvic floor muscle training is not going to elevate that tissue back up into your body, but it can sometimes help with symptoms,” Dr. LaCross said.
The PT conducts a thorough pelvic muscle assessment, discusses lifestyle, and may teach breathing and bracing strategies for lifting, for example.
“A lot of what we’re talking about with pelvic floor therapy is lifestyle modifications,” Dr. Nwabuebo said. “If I have a patient with a history of chronic constipation, it doesn’t matter how much we do pelvic floor exercises; if we don’t manage the constipation issues by addressing their nutrition, then straining when using the bathroom will keep putting pressure on the pelvic floor.”
PTs can also recommend appropriate vaginal weights and dilators to help with pelvic floor strengthening and teach patients how to use them properly.
Even if women ultimately opt for surgery, PT prior to surgery can be beneficial. Dr. Rabin cited three reasons she recommends first-line PT: It may elevate the bladder enough to reduce stress incontinence and thicken the pelvic muscles, it can improve the effectiveness of a pessary or surgery if the woman chooses one of those options, and it can quiet bladder contractions, potentially obviating the need for pharmacologic treatment for overactive bladder.
The next nonsurgical option is a pessary, a device that fits into the vagina to provide support to the tissues displaced by prolapse. There’s a wide range of pessary types: some are short-term, worn only daily, or disposable, while others can be worn longer. Some women can self-insert and remove the pessary, and others may need a clinician to do so. Dr. Dmochowski recommends patients try a pessary to see if it benefits them. About a third of women will find them comfortable enough to wear regularly, but others will feel more sensitive to the pessary’s presence, he said.
One of the newest, most innovative pessary options for women is Gynethotics, which received Food and Drug Administration (FDA) clearance in March, as the first 3D-printed, customizable pessary capable of nearly 10 million configurations based on a person’s body.
Nearly all stage 4 prolapses and most of stage 3 prolapses can be addressed only through transvaginal or transabdominal surgery.
“We tell patients, if you can get 10 years out of your operation, you’re lucky,” Dr. Dmochowski said. A major reason for the short-lived durability is the poor quality of the tissue that needs to be pulled together. Serious complications resulting from use of polypropylene mesh during prolapse surgery led the FDA to halt sales of the devices and recommend discontinuing their use. However, one type of vaginal mesh is still considered safe to use in sacral colpopexy surgery.
Three things can shorten the durability of the surgery, Dr. Dmochowski said: heavy lifting, particularly anything over 30 pounds; chronic coughing, such as in those with chronic lung conditions; and chronic constipation.
Ms. Palm tried a pessary for her grade 3 prolapse with cystocele, rectocele, and enterocele but didn’t feel she had the time to use it regularly, so she opted for surgery. After a week on the couch recovering, she took it easy for another 12 weeks. Since then, she’s dedicated much of her time to educating and supporting women with POP and combating stigma associated with it. The APOPS website that she started has become a valuable resource for PCPs to send patients to, and the forum includes more 27,000 women from around the world.
“We encourage women to share what they’re experiencing. Tell your family, tell your friends, tell the people you work with about it,” Ms. Palm said. But many still feel uncomfortable speaking up, making PCPs’ role even more important.
*This story was updated on May 14, 2024.
Sherrie Palm, a patient advocate in Mukwonago, Wisconsin, learned in her 30s that she needed to educate herself about her own health. So when she discovered a walnut-sized lump coming out of her vagina in her mid-50s, she was stunned when her primary care provider (PCP) told her it was pelvic organ prolapse (POP), where one or more organs descend into the vaginal cavity.
“I was shocked,” Ms. Palm said. After searching online and discovering how prevalent POP was, her shock turned to anger. “I was blown away that it could be this common and I’d never heard of it,” she said. “I knew within 2 weeks that I had to do something to change the status quo.”
Ms. Palm eventually founded the nonprofit Association for Pelvic Organ Prolapse Support, or APOPS, complete with a forum where women can learn about POP and support one another. She said awareness has improved substantially since her diagnosis in 2007, but “we have a long way to go” because POP and vaginal health in general are so stigmatized.
Her website notes that about half of women with incontinence do not seek help, largely because of stigma. “The status quo is that PCPs do not POP screen,” she said. ObGyns may screen but often “because the patient has asked to be screened, they say it’s not that bad, come back and see me in a year, and do your Kegels,” Ms. Palm said.
Doctors who diagnose POP agree that the issue is often off PCPs’ radar.
“Primary care doctors are really in a time crunch, so this is one of the things that may not get addressed,” Jill Rabin, MD, vice chair of education and development in obstetrics and gynecology at Northwell Health in New York, said. Dr. Rabin is also head of urogynecology at Long Island Jewish Medical Center.
Ann Nwabuebo, PT, DPT, owner and founder of Body Connect Physical Therapy in Bethesda, Maryland, said social media has been shifting the attitude that pelvic health is a taboo subject. “It’s empowering people to seek care if they’re not finding physicians who are helping.”
But social media is also a double-edged sword, said Jenny LaCross, PT, DPT, PhD, a physical therapist at MOVE PT in Monroe, Michigan, and a postdoctoral research fellow with Michigan Medicine’s Pelvic Floor Research Group. “Pelvic health in general is talked about a lot more, but there’s also a lot more misinformation,” she said.
Part of that misinformation is the idea that pelvic prolapse is solely about weakness in the pelvic floor when it can also result from a widening of natural openings within the pelvis, Dr. LaCross said. She pointed to the two definitions of pelvic organ prolapse by the International Urogynecologic Consultation and the International Continence Society, both of which have been updated in recent years.
“This is why this is challenging for primary care providers,” Dr. LaCross said. “Even urogynecologists who are the specialists that treat prolapse and incontinence have changed how they assess it and the terminology and criteria that they use.”
What hasn’t changed is the substantial negative impact POP can have on quality of life. “This is the second most common reason that women enter nursing homes,” primarily because of urinary incontinence, Dr. Rabin said. “It’s very debilitating, but a lot of it is preventable and a lot is treatable.”
Dr. Rabin estimated that three out of every five women older than 60 and one or two out of every five women younger than 60 experience POP. Prevalence studies vary widely, from nearly a quarter of women to more than half, and racial and ethnic disparities in diagnosis further complicate the statistics.
PCPs therefore have an important role to play in screening for POP. The evidence shows that “patients want their providers to bring this up,” Dr. LaCross said. “They want to talk about it, but they want the provider to ask the questions first.”
Causes, Risk Factors, and Symptoms
Many causes contribute to POP, with gravity, aging, childbirth, and menopause at the top of the list.
“As people get older, their pelvic muscles and connective tissue get weaker, and the nerves don’t function as well,” Dr. Rabin said. Meanwhile, the body is losing estrogen, which affects how well the muscles contract and how easily the connective tissue can tear, she said.
With menopause, when baseline estrogen is lower, the tissue integrity is not as supportive as it should be and women are going to be at an increased risk of prolapse, Dr. Nwabuebo said.
POP has a range of risk factors:
- Increasing age, as muscle mass decreases and connective tissue hardens.
- Menopause.
- Vaginal delivery with complications, such as long second-stage labor, instrument-assisted delivery, multiple vaginal lacerations, and improperly repaired episiotomy.
- Multiple vaginal deliveries.
- Birthing large babies.
- Family history of pelvic organ prolapse (genetics can play a role in POP risk).
- Previous pelvic/abdominal surgery, including cesarean delivery and hysterectomy.
- Smoking (largely because of associated coughing).
- Chronic lung conditions that cause a lot of coughing.
- Chronic constipation or irritable bowel syndrome.
- Some types of high-impact activity, such as jogging or marathon running.
- Early menopause, for younger women.
- Repetitive heavy lifting in daily activities, such as occupational lifting (though not necessarily weight lifting as an exercise).
- Higher body mass index.
- Connective tissue disorders, such as joint hypermobility syndrome or Ehlers-Danlos syndrome.
Roger Dmochowski, MD, professor of urology and surgery at Vanderbilt University Medical Center, groups POP symptoms into two groups: anatomic and functional ones. A common anatomic symptom is bulging. “They’ll describe sitting on a ball, feeling like their bladder or something’s falling out, feeling a pressure or a heaviness,” Dr. Dmochowski said.
Functional symptoms can include vaginal dryness, vaginal irritation, painful intercourse, contact of the vaginal tissues with underclothes, and associated urinary symptoms, such as stress incontinence, urge incontinence, and incomplete emptying of the bladder. Dr. Dmochowski noted that women who report urinary incontinence may be at risk for being prescribed a medication without the necessary referral to a specialist for a full gynecologic evaluation.
Two other groups of functional symptoms include bowel-related disorders – primarily fecal incontinence and ongoing constipation – and pelvic pain or discomfort.
There can also be asymptomatic cases. “A lot of women have what we call silent prolapse,” Dr. Dmochowski said. That is, “they have some degree of loss of support to the bladder, vagina, or uterus, but they’re not symptomatic.” These women may be particularly good candidates for pelvic health physical therapy.
Screening and Diagnosis
Because many postmenopausal women stop seeing their ob.gyn, it’s often up to their primary care physician to determine whether their patients are experiencing POP symptoms.
“Women sometimes don’t bring this up with their doctor because they think there’s not enough time, or they’ll be laughed at, or their friends told them this is normal,” Dr. Rabin said. But primary care providers are really in a unique position to be able to ask the key symptom questions.
Dr. Rabin recommends a couple of questions to cover all the bases: “Do you leak urine when you cough or sneeze or on the way to the bathroom? Do you notice a bulge coming out of the vagina, or are you bothered by pelvic pressure?”
Dr. Dmochowski offered a single question that can open the conversation to more questions: “Are you bothered by any urinary or bowel or vaginal issues that we should talk about?” He also suggests asking how bothersome the symptoms are, which can help in directing treatment or prevention options. A physical exam can reveal signs of POP as well.
Diagnosis involves a detailed history, a comprehensive physical exam, and assessment with the Pelvic Organ Prolapse Quantification (POP-Q) tool. A urogynecologist can diagnose the type of POP – such as cystocele, rectocele, enterocele, uterine prolapse, or vaginal vault prolapse – and its grade (0-4).
Treatment: Physical Therapy, Pessary, and Surgery
No medications can treat prolapse, though some can treat downstream effects, such as hormonal vaginal creams for vaginal dryness and irritation, and medications for urinary incontinence. However, two mistakes PCPs can make are sending someone straight to surgery or prescribing them medication for symptoms without referring them for a diagnostic evaluation, Dr. Rabin said. “You have to have a diagnosis first to know what type of prolapse is there,” she said.
Because there can be long waiting lists for a urogynecologist or urologist, PCPs should also refer their patients to a pelvic health physical therapist (PT) who can help patients begin addressing the symptoms while they await a specialist who can diagnose them.
Though PT is often thought of as preventive, it’s also a conservative first-line intervention for prolapse, Dr. Nwabuebo said. Strong evidence shows pelvic floor muscle training from pelvic health PT can reduce symptoms of prolapse and reduce the severity by one grade in those with a grade 1 or 2 prolapse. Stage 3 is trickier, where PT may or may not be able to shift the symptom presentation, Dr. Nwabeubo said, and stage 4 is usually a surgical candidate.
“If you have a grade 4 prolapse, or the tissues are really visible outside the body, physical therapy and pelvic floor muscle training is not going to elevate that tissue back up into your body, but it can sometimes help with symptoms,” Dr. LaCross said.
The PT conducts a thorough pelvic muscle assessment, discusses lifestyle, and may teach breathing and bracing strategies for lifting, for example.
“A lot of what we’re talking about with pelvic floor therapy is lifestyle modifications,” Dr. Nwabuebo said. “If I have a patient with a history of chronic constipation, it doesn’t matter how much we do pelvic floor exercises; if we don’t manage the constipation issues by addressing their nutrition, then straining when using the bathroom will keep putting pressure on the pelvic floor.”
PTs can also recommend appropriate vaginal weights and dilators to help with pelvic floor strengthening and teach patients how to use them properly.
Even if women ultimately opt for surgery, PT prior to surgery can be beneficial. Dr. Rabin cited three reasons she recommends first-line PT: It may elevate the bladder enough to reduce stress incontinence and thicken the pelvic muscles, it can improve the effectiveness of a pessary or surgery if the woman chooses one of those options, and it can quiet bladder contractions, potentially obviating the need for pharmacologic treatment for overactive bladder.
The next nonsurgical option is a pessary, a device that fits into the vagina to provide support to the tissues displaced by prolapse. There’s a wide range of pessary types: some are short-term, worn only daily, or disposable, while others can be worn longer. Some women can self-insert and remove the pessary, and others may need a clinician to do so. Dr. Dmochowski recommends patients try a pessary to see if it benefits them. About a third of women will find them comfortable enough to wear regularly, but others will feel more sensitive to the pessary’s presence, he said.
One of the newest, most innovative pessary options for women is Gynethotics, which received Food and Drug Administration (FDA) clearance in March, as the first 3D-printed, customizable pessary capable of nearly 10 million configurations based on a person’s body.
Nearly all stage 4 prolapses and most of stage 3 prolapses can be addressed only through transvaginal or transabdominal surgery.
“We tell patients, if you can get 10 years out of your operation, you’re lucky,” Dr. Dmochowski said. A major reason for the short-lived durability is the poor quality of the tissue that needs to be pulled together. Serious complications resulting from use of polypropylene mesh during prolapse surgery led the FDA to halt sales of the devices and recommend discontinuing their use. However, one type of vaginal mesh is still considered safe to use in sacral colpopexy surgery.
Three things can shorten the durability of the surgery, Dr. Dmochowski said: heavy lifting, particularly anything over 30 pounds; chronic coughing, such as in those with chronic lung conditions; and chronic constipation.
Ms. Palm tried a pessary for her grade 3 prolapse with cystocele, rectocele, and enterocele but didn’t feel she had the time to use it regularly, so she opted for surgery. After a week on the couch recovering, she took it easy for another 12 weeks. Since then, she’s dedicated much of her time to educating and supporting women with POP and combating stigma associated with it. The APOPS website that she started has become a valuable resource for PCPs to send patients to, and the forum includes more 27,000 women from around the world.
“We encourage women to share what they’re experiencing. Tell your family, tell your friends, tell the people you work with about it,” Ms. Palm said. But many still feel uncomfortable speaking up, making PCPs’ role even more important.
*This story was updated on May 14, 2024.
Mandatory DMV Reporting Tied to Dementia Underdiagnosis
, new research suggests.
Investigators found that primary care physicians (PCPs) in states with clinician reporting mandates had a 59% higher probability of underdiagnosing dementia compared with their counterparts in states that require patients to self-report or that have no reporting mandates.
“Our findings in this cross-sectional study raise concerns about potential adverse effects of mandatory clinician reporting for dementia diagnosis and underscore the need for careful consideration of the effect of such policies,” wrote the investigators, led by Soeren Mattke, MD, DSc, director of the USC Brain Health Observatory and research professor of economics at the University of Southern California, Los Angeles.
The study was published online in JAMA Network Open.
Lack of Guidance
As the US population ages, the number of older drivers is increasing, with 55.8 million drivers 65 years old or older. Approximately 7 million people in this age group have dementia — an estimate that is expected to increase to nearly 12 million by 2040.
The aging population raises a “critical policy question” about how to ensure road safety. Although the American Medical Association’s Code of Ethics outlines a physician’s obligation to identify drivers with medical impairments that impede safe driving, guidance restricting cognitively impaired drivers from driving is lacking.
In addition, evidence as to whether cognitive impairment indeed poses a threat to driving safety is mixed and has led to a lack of uniform policies with respect to reporting dementia.
Four states explicitly require clinicians to report dementia diagnoses to the DMV, which will then determine the patient’s fitness to drive, whereas 14 states require people with dementia to self-report. The remaining states have no explicit reporting requirements.
The issue of mandatory reporting is controversial, the researchers noted. On the one hand, physicians could protect patients and others by reporting potentially unsafe drivers.
On the other hand, evidence of an association with lower accident risks in patients with dementia is sparse and mandatory reporting may adversely affect physician-patient relationships. Empirical evidence for unintended consequences of reporting laws is lacking.
To examine the potential link between dementia underdiagnosis and mandatory reporting policies, the investigators analyzed the 100% data from the Medicare fee-for-service program and Medicare Advantage plans from 2017 to 2019, which included 223,036 PCPs with a panel of 25 or more Medicare patients.
The researchers examined dementia diagnosis rates in the patient panel of PCPs, rather than neurologists or gerontologists, regardless of who documented the diagnosis. Dr. Mattke said that it is possible that the diagnosis was established after referral to a specialist.
Each physician’s expected number of dementia cases was estimated using a predictive model based on patient characteristics. The researchers then compared the estimate with observed dementia diagnoses, thereby identifying clinicians who underdiagnosed dementia after sampling errors were accounted for.
‘Heavy-Handed Interference’
The researchers adjusted for several covariates potentially associated with a clinician’s probability of underdiagnosing dementia. These included sex, office location, practice specialty, racial/ethnic composition of the patient panel, and percentage of patients dually eligible for Medicare and Medicaid. The table shows PCP characteristics.
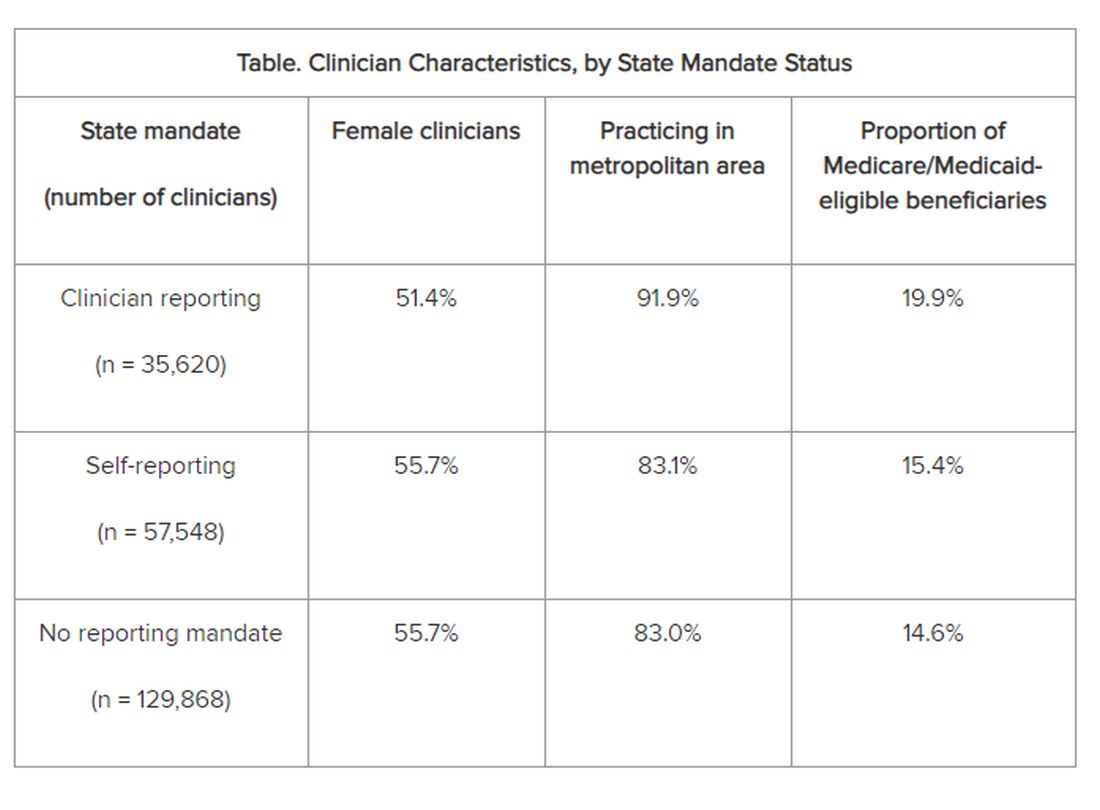
Adjusted results showed that PCPs practicing in states with clinician reporting mandates had a 12.4% (95% confidence interval [CI], 10.5%-14.2%) probability of underdiagnosing dementia versus 7.8% (95% CI, 6.9%-8.7%) in states with self-reporting and 7.7% (95% CI, 6.9%-8.4%) in states with no mandates, translating into a 4–percentage point difference (P < .001).
“Our study is the first to provide empirical evidence for the potential adverse effects of reporting policies,” the researchers noted. “Although we found that some clinicians underdiagnosed dementia regardless of state mandates, the key finding of this study reveals that primary care clinicians who practice in states with clinician reporting mandates were 59% more likely to do so…compared with those states with no reporting requirements…or driver self-reporting requirements.”
The investigators suggested that one potential explanation for underdiagnosis is patient resistance to cognitive testing. If patients were aware that the clinician was obligated by law to report their dementia diagnosis to the DMV, “they might be more inclined to conceal their symptoms or refuse further assessments, in addition to the general stigma and resistance to a formal assessment after a positive dementia screening result.”
“The findings suggest that policymakers might want to rethink those physician reporting mandates, since we also could not find conclusive evidence that they improve road safety,” Dr. Mattke said. “Maybe patients and their physicians can arrive at a sensible approach to determine driving fitness without such heavy-handed interference.”
However, he cautioned that the findings are not definitive and further study is needed before firm recommendations either for or against mandatory reporting.
In addition, the researchers noted several study limitations. One is that dementia underdiagnosis may also be associated with factors not captured in their model, including physician-patient relationships, health literacy, or language barriers.
However, Dr. Mattke noted, “ my sense is that those unobservable factors are not systematically related to state reporting policies and having omitted them would therefore not bias our results.”
Experts Weigh In
Commenting on the research, Morgan Daven, MA, the Alzheimer’s Association vice president of health systems, said that dementia is widely and significantly underdiagnosed, and not only in the states with dementia reporting mandates. Many factors may contribute to underdiagnosis, and although the study shows an association between reporting mandates and underdiagnosis, it does not demonstrate causation.
That said, Mr. Daven added, “fear and stigma related to dementia may inhibit the clinician, the patient, and their family from pursuing detection and diagnosis for dementia. As a society, we need to address dementia fear and stigma for all parties.”
He noted that useful tools include healthcare policies, workforce training, public awareness and education, and public policies to mitigate fear and stigma and their negative effects on diagnosis, care, support, and communication.
A potential study limitation is that it relied only on diagnoses by PCPs. Mr. Daven noted that the diagnosis of Alzheimer’ disease — the most common cause of dementia — is confirmation of amyloid buildup via a biomarker test, using PET or cerebrospinal fluid analysis.
“Both of these tests are extremely limited in their use and accessibility in a primary care setting. Inclusion of diagnoses by dementia specialists would provide a more complete picture,” he said.
Mr. Daven added that the Alzheimer’s Association encourages families to proactively discuss driving and other disease-related safety concerns as soon as possible. The Alzheimer’s Association Dementia and Driving webpage offers tips and strategies to discuss driving concerns with a family member.
In an accompanying editorial, Donald Redelmeier, MD, MS(HSR), and Vidhi Bhatt, BSc, both of the Department of Medicine, University of Toronto, differentiate the mandate for physicians to warn patients with dementia about traffic safety from the mandate for reporting child maltreatment, gunshot victims, or communicable diseases. They noted that mandated warnings “are not easy, can engender patient dissatisfaction, and need to be handled with tact.”
Yet, they pointed out, “breaking bad news is what practicing medicine entails.” They emphasized that, regardless of government mandates, “counseling patients for more road safety is an essential skill for clinicians in diverse states who hope to help their patients avoid becoming more traffic statistics.”
Research reported in this publication was supported by Genentech, a member of the Roche Group, and a grant from the National Institute on Aging of the National Institutes of Health. Dr. Mattke reported receiving grants from Genentech for a research contract with USC during the conduct of the study; personal fees from Eisai, Biogen, C2N, Novo Nordisk, Novartis, and Roche Genentech; and serving on the Senscio Systems board of directors, ALZpath scientific advisory board, AiCure scientific advisory board, and Boston Millennia Partners scientific advisory board outside the submitted work. The other authors’ disclosures are listed on the original paper. The editorial was supported by the Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, Kimel-Schatzky Traumatic Brain Injury Research Fund, and the Graduate Diploma Program in Health Research at the University of Toronto. The editorial authors report no other relevant financial relationships.
A version of this article appeared on Medscape.com.
, new research suggests.
Investigators found that primary care physicians (PCPs) in states with clinician reporting mandates had a 59% higher probability of underdiagnosing dementia compared with their counterparts in states that require patients to self-report or that have no reporting mandates.
“Our findings in this cross-sectional study raise concerns about potential adverse effects of mandatory clinician reporting for dementia diagnosis and underscore the need for careful consideration of the effect of such policies,” wrote the investigators, led by Soeren Mattke, MD, DSc, director of the USC Brain Health Observatory and research professor of economics at the University of Southern California, Los Angeles.
The study was published online in JAMA Network Open.
Lack of Guidance
As the US population ages, the number of older drivers is increasing, with 55.8 million drivers 65 years old or older. Approximately 7 million people in this age group have dementia — an estimate that is expected to increase to nearly 12 million by 2040.
The aging population raises a “critical policy question” about how to ensure road safety. Although the American Medical Association’s Code of Ethics outlines a physician’s obligation to identify drivers with medical impairments that impede safe driving, guidance restricting cognitively impaired drivers from driving is lacking.
In addition, evidence as to whether cognitive impairment indeed poses a threat to driving safety is mixed and has led to a lack of uniform policies with respect to reporting dementia.
Four states explicitly require clinicians to report dementia diagnoses to the DMV, which will then determine the patient’s fitness to drive, whereas 14 states require people with dementia to self-report. The remaining states have no explicit reporting requirements.
The issue of mandatory reporting is controversial, the researchers noted. On the one hand, physicians could protect patients and others by reporting potentially unsafe drivers.
On the other hand, evidence of an association with lower accident risks in patients with dementia is sparse and mandatory reporting may adversely affect physician-patient relationships. Empirical evidence for unintended consequences of reporting laws is lacking.
To examine the potential link between dementia underdiagnosis and mandatory reporting policies, the investigators analyzed the 100% data from the Medicare fee-for-service program and Medicare Advantage plans from 2017 to 2019, which included 223,036 PCPs with a panel of 25 or more Medicare patients.
The researchers examined dementia diagnosis rates in the patient panel of PCPs, rather than neurologists or gerontologists, regardless of who documented the diagnosis. Dr. Mattke said that it is possible that the diagnosis was established after referral to a specialist.
Each physician’s expected number of dementia cases was estimated using a predictive model based on patient characteristics. The researchers then compared the estimate with observed dementia diagnoses, thereby identifying clinicians who underdiagnosed dementia after sampling errors were accounted for.
‘Heavy-Handed Interference’
The researchers adjusted for several covariates potentially associated with a clinician’s probability of underdiagnosing dementia. These included sex, office location, practice specialty, racial/ethnic composition of the patient panel, and percentage of patients dually eligible for Medicare and Medicaid. The table shows PCP characteristics.
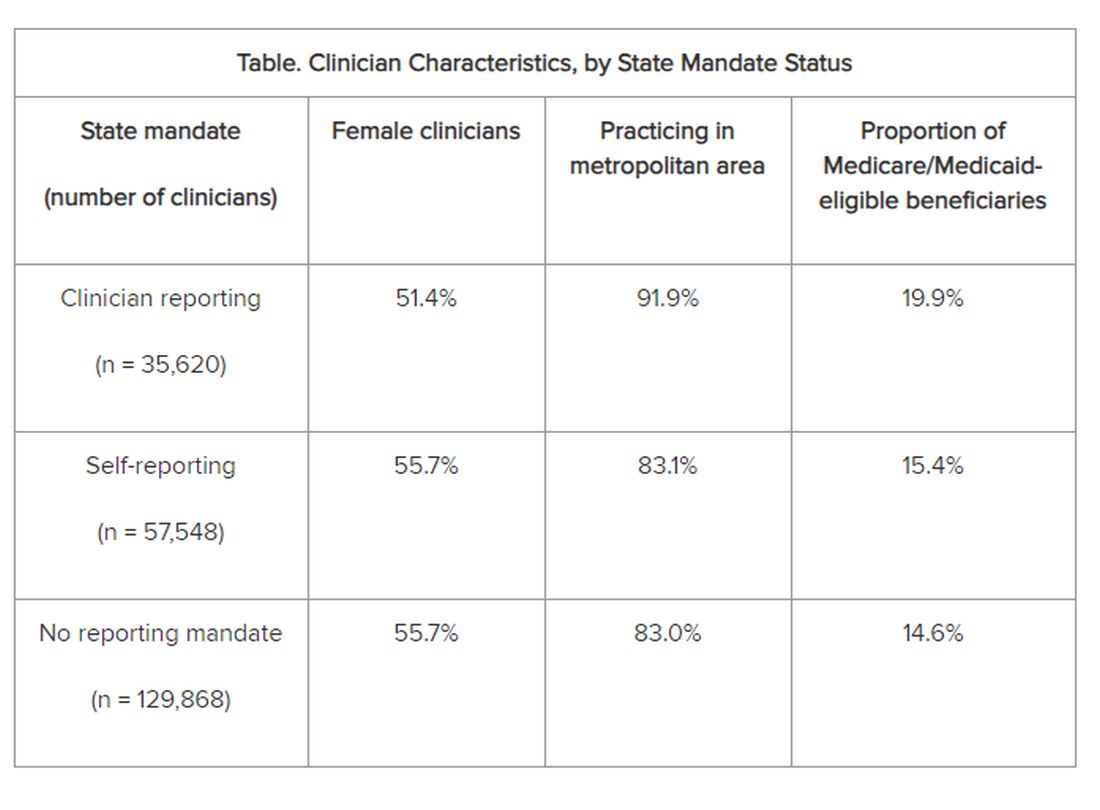
Adjusted results showed that PCPs practicing in states with clinician reporting mandates had a 12.4% (95% confidence interval [CI], 10.5%-14.2%) probability of underdiagnosing dementia versus 7.8% (95% CI, 6.9%-8.7%) in states with self-reporting and 7.7% (95% CI, 6.9%-8.4%) in states with no mandates, translating into a 4–percentage point difference (P < .001).
“Our study is the first to provide empirical evidence for the potential adverse effects of reporting policies,” the researchers noted. “Although we found that some clinicians underdiagnosed dementia regardless of state mandates, the key finding of this study reveals that primary care clinicians who practice in states with clinician reporting mandates were 59% more likely to do so…compared with those states with no reporting requirements…or driver self-reporting requirements.”
The investigators suggested that one potential explanation for underdiagnosis is patient resistance to cognitive testing. If patients were aware that the clinician was obligated by law to report their dementia diagnosis to the DMV, “they might be more inclined to conceal their symptoms or refuse further assessments, in addition to the general stigma and resistance to a formal assessment after a positive dementia screening result.”
“The findings suggest that policymakers might want to rethink those physician reporting mandates, since we also could not find conclusive evidence that they improve road safety,” Dr. Mattke said. “Maybe patients and their physicians can arrive at a sensible approach to determine driving fitness without such heavy-handed interference.”
However, he cautioned that the findings are not definitive and further study is needed before firm recommendations either for or against mandatory reporting.
In addition, the researchers noted several study limitations. One is that dementia underdiagnosis may also be associated with factors not captured in their model, including physician-patient relationships, health literacy, or language barriers.
However, Dr. Mattke noted, “ my sense is that those unobservable factors are not systematically related to state reporting policies and having omitted them would therefore not bias our results.”
Experts Weigh In
Commenting on the research, Morgan Daven, MA, the Alzheimer’s Association vice president of health systems, said that dementia is widely and significantly underdiagnosed, and not only in the states with dementia reporting mandates. Many factors may contribute to underdiagnosis, and although the study shows an association between reporting mandates and underdiagnosis, it does not demonstrate causation.
That said, Mr. Daven added, “fear and stigma related to dementia may inhibit the clinician, the patient, and their family from pursuing detection and diagnosis for dementia. As a society, we need to address dementia fear and stigma for all parties.”
He noted that useful tools include healthcare policies, workforce training, public awareness and education, and public policies to mitigate fear and stigma and their negative effects on diagnosis, care, support, and communication.
A potential study limitation is that it relied only on diagnoses by PCPs. Mr. Daven noted that the diagnosis of Alzheimer’ disease — the most common cause of dementia — is confirmation of amyloid buildup via a biomarker test, using PET or cerebrospinal fluid analysis.
“Both of these tests are extremely limited in their use and accessibility in a primary care setting. Inclusion of diagnoses by dementia specialists would provide a more complete picture,” he said.
Mr. Daven added that the Alzheimer’s Association encourages families to proactively discuss driving and other disease-related safety concerns as soon as possible. The Alzheimer’s Association Dementia and Driving webpage offers tips and strategies to discuss driving concerns with a family member.
In an accompanying editorial, Donald Redelmeier, MD, MS(HSR), and Vidhi Bhatt, BSc, both of the Department of Medicine, University of Toronto, differentiate the mandate for physicians to warn patients with dementia about traffic safety from the mandate for reporting child maltreatment, gunshot victims, or communicable diseases. They noted that mandated warnings “are not easy, can engender patient dissatisfaction, and need to be handled with tact.”
Yet, they pointed out, “breaking bad news is what practicing medicine entails.” They emphasized that, regardless of government mandates, “counseling patients for more road safety is an essential skill for clinicians in diverse states who hope to help their patients avoid becoming more traffic statistics.”
Research reported in this publication was supported by Genentech, a member of the Roche Group, and a grant from the National Institute on Aging of the National Institutes of Health. Dr. Mattke reported receiving grants from Genentech for a research contract with USC during the conduct of the study; personal fees from Eisai, Biogen, C2N, Novo Nordisk, Novartis, and Roche Genentech; and serving on the Senscio Systems board of directors, ALZpath scientific advisory board, AiCure scientific advisory board, and Boston Millennia Partners scientific advisory board outside the submitted work. The other authors’ disclosures are listed on the original paper. The editorial was supported by the Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, Kimel-Schatzky Traumatic Brain Injury Research Fund, and the Graduate Diploma Program in Health Research at the University of Toronto. The editorial authors report no other relevant financial relationships.
A version of this article appeared on Medscape.com.
, new research suggests.
Investigators found that primary care physicians (PCPs) in states with clinician reporting mandates had a 59% higher probability of underdiagnosing dementia compared with their counterparts in states that require patients to self-report or that have no reporting mandates.
“Our findings in this cross-sectional study raise concerns about potential adverse effects of mandatory clinician reporting for dementia diagnosis and underscore the need for careful consideration of the effect of such policies,” wrote the investigators, led by Soeren Mattke, MD, DSc, director of the USC Brain Health Observatory and research professor of economics at the University of Southern California, Los Angeles.
The study was published online in JAMA Network Open.
Lack of Guidance
As the US population ages, the number of older drivers is increasing, with 55.8 million drivers 65 years old or older. Approximately 7 million people in this age group have dementia — an estimate that is expected to increase to nearly 12 million by 2040.
The aging population raises a “critical policy question” about how to ensure road safety. Although the American Medical Association’s Code of Ethics outlines a physician’s obligation to identify drivers with medical impairments that impede safe driving, guidance restricting cognitively impaired drivers from driving is lacking.
In addition, evidence as to whether cognitive impairment indeed poses a threat to driving safety is mixed and has led to a lack of uniform policies with respect to reporting dementia.
Four states explicitly require clinicians to report dementia diagnoses to the DMV, which will then determine the patient’s fitness to drive, whereas 14 states require people with dementia to self-report. The remaining states have no explicit reporting requirements.
The issue of mandatory reporting is controversial, the researchers noted. On the one hand, physicians could protect patients and others by reporting potentially unsafe drivers.
On the other hand, evidence of an association with lower accident risks in patients with dementia is sparse and mandatory reporting may adversely affect physician-patient relationships. Empirical evidence for unintended consequences of reporting laws is lacking.
To examine the potential link between dementia underdiagnosis and mandatory reporting policies, the investigators analyzed the 100% data from the Medicare fee-for-service program and Medicare Advantage plans from 2017 to 2019, which included 223,036 PCPs with a panel of 25 or more Medicare patients.
The researchers examined dementia diagnosis rates in the patient panel of PCPs, rather than neurologists or gerontologists, regardless of who documented the diagnosis. Dr. Mattke said that it is possible that the diagnosis was established after referral to a specialist.
Each physician’s expected number of dementia cases was estimated using a predictive model based on patient characteristics. The researchers then compared the estimate with observed dementia diagnoses, thereby identifying clinicians who underdiagnosed dementia after sampling errors were accounted for.
‘Heavy-Handed Interference’
The researchers adjusted for several covariates potentially associated with a clinician’s probability of underdiagnosing dementia. These included sex, office location, practice specialty, racial/ethnic composition of the patient panel, and percentage of patients dually eligible for Medicare and Medicaid. The table shows PCP characteristics.
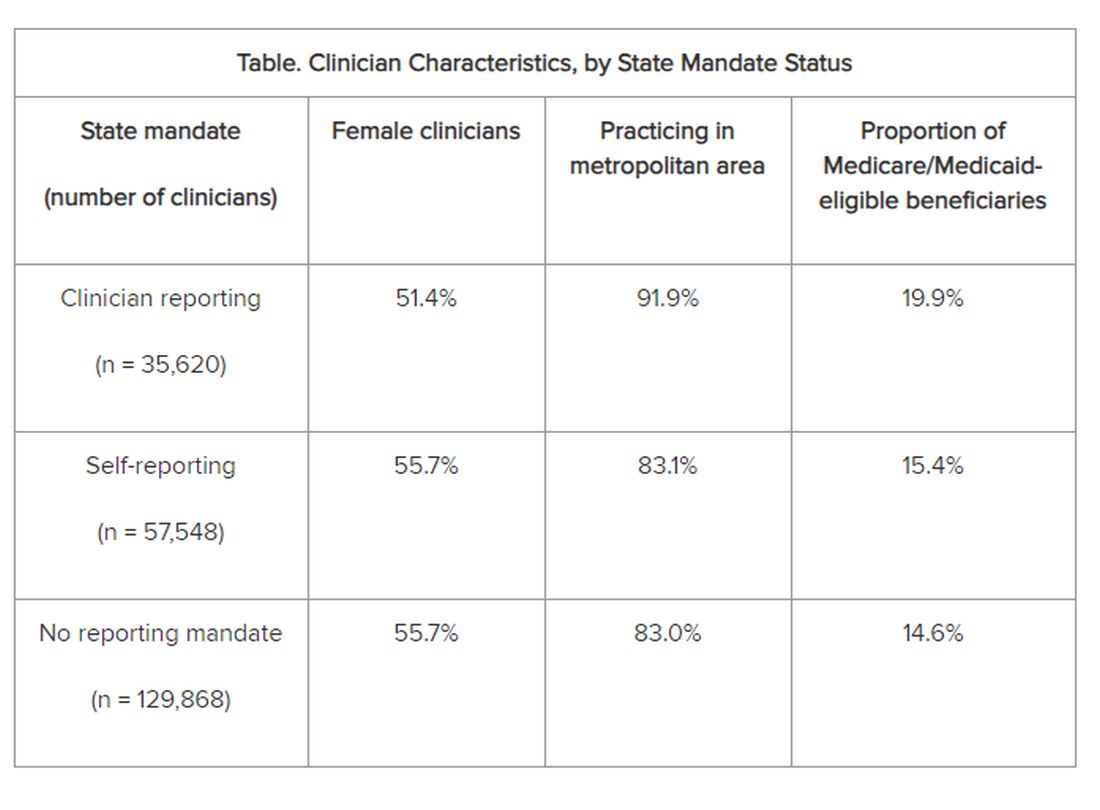
Adjusted results showed that PCPs practicing in states with clinician reporting mandates had a 12.4% (95% confidence interval [CI], 10.5%-14.2%) probability of underdiagnosing dementia versus 7.8% (95% CI, 6.9%-8.7%) in states with self-reporting and 7.7% (95% CI, 6.9%-8.4%) in states with no mandates, translating into a 4–percentage point difference (P < .001).
“Our study is the first to provide empirical evidence for the potential adverse effects of reporting policies,” the researchers noted. “Although we found that some clinicians underdiagnosed dementia regardless of state mandates, the key finding of this study reveals that primary care clinicians who practice in states with clinician reporting mandates were 59% more likely to do so…compared with those states with no reporting requirements…or driver self-reporting requirements.”
The investigators suggested that one potential explanation for underdiagnosis is patient resistance to cognitive testing. If patients were aware that the clinician was obligated by law to report their dementia diagnosis to the DMV, “they might be more inclined to conceal their symptoms or refuse further assessments, in addition to the general stigma and resistance to a formal assessment after a positive dementia screening result.”
“The findings suggest that policymakers might want to rethink those physician reporting mandates, since we also could not find conclusive evidence that they improve road safety,” Dr. Mattke said. “Maybe patients and their physicians can arrive at a sensible approach to determine driving fitness without such heavy-handed interference.”
However, he cautioned that the findings are not definitive and further study is needed before firm recommendations either for or against mandatory reporting.
In addition, the researchers noted several study limitations. One is that dementia underdiagnosis may also be associated with factors not captured in their model, including physician-patient relationships, health literacy, or language barriers.
However, Dr. Mattke noted, “ my sense is that those unobservable factors are not systematically related to state reporting policies and having omitted them would therefore not bias our results.”
Experts Weigh In
Commenting on the research, Morgan Daven, MA, the Alzheimer’s Association vice president of health systems, said that dementia is widely and significantly underdiagnosed, and not only in the states with dementia reporting mandates. Many factors may contribute to underdiagnosis, and although the study shows an association between reporting mandates and underdiagnosis, it does not demonstrate causation.
That said, Mr. Daven added, “fear and stigma related to dementia may inhibit the clinician, the patient, and their family from pursuing detection and diagnosis for dementia. As a society, we need to address dementia fear and stigma for all parties.”
He noted that useful tools include healthcare policies, workforce training, public awareness and education, and public policies to mitigate fear and stigma and their negative effects on diagnosis, care, support, and communication.
A potential study limitation is that it relied only on diagnoses by PCPs. Mr. Daven noted that the diagnosis of Alzheimer’ disease — the most common cause of dementia — is confirmation of amyloid buildup via a biomarker test, using PET or cerebrospinal fluid analysis.
“Both of these tests are extremely limited in their use and accessibility in a primary care setting. Inclusion of diagnoses by dementia specialists would provide a more complete picture,” he said.
Mr. Daven added that the Alzheimer’s Association encourages families to proactively discuss driving and other disease-related safety concerns as soon as possible. The Alzheimer’s Association Dementia and Driving webpage offers tips and strategies to discuss driving concerns with a family member.
In an accompanying editorial, Donald Redelmeier, MD, MS(HSR), and Vidhi Bhatt, BSc, both of the Department of Medicine, University of Toronto, differentiate the mandate for physicians to warn patients with dementia about traffic safety from the mandate for reporting child maltreatment, gunshot victims, or communicable diseases. They noted that mandated warnings “are not easy, can engender patient dissatisfaction, and need to be handled with tact.”
Yet, they pointed out, “breaking bad news is what practicing medicine entails.” They emphasized that, regardless of government mandates, “counseling patients for more road safety is an essential skill for clinicians in diverse states who hope to help their patients avoid becoming more traffic statistics.”
Research reported in this publication was supported by Genentech, a member of the Roche Group, and a grant from the National Institute on Aging of the National Institutes of Health. Dr. Mattke reported receiving grants from Genentech for a research contract with USC during the conduct of the study; personal fees from Eisai, Biogen, C2N, Novo Nordisk, Novartis, and Roche Genentech; and serving on the Senscio Systems board of directors, ALZpath scientific advisory board, AiCure scientific advisory board, and Boston Millennia Partners scientific advisory board outside the submitted work. The other authors’ disclosures are listed on the original paper. The editorial was supported by the Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, Kimel-Schatzky Traumatic Brain Injury Research Fund, and the Graduate Diploma Program in Health Research at the University of Toronto. The editorial authors report no other relevant financial relationships.
A version of this article appeared on Medscape.com.
From JAMA Network Open
Novel Agent Curbs Alzheimer’s-Related Agitation
DENVER —
More than half of participants in the open-label extension period of the randomized clinical trial responded to the medication, which was associated with a 3.6-fold lower risk for relapse compared with placebo.
“The positive efficacy and favorable safety results with AXS-05 support its potential to fulfill a high unmet need for the treatment of Alzheimer’s disease agitation,” said Anton P. Porsteinsson, MD, director of the Alzheimer’s Disease Care, Research and Education Program, University of Rochester, New York.
The findings were presented at the 2024 annual meeting of the American Academy of Neurology.
Common and Disruptive
Agitation is reported in up to 70% of patients with Alzheimer’s disease and is characterized by emotional distress, aggressive behaviors, disruptive irritability, and disinhibition. Alzheimer’s disease-related agitation has been associated with increased caregiver burden, decreased functioning, accelerated cognitive decline, earlier nursing home placement, and increased mortality.
A previous phase 2/3 study of AXS-05 showed that the investigative agent led to rapid and significantly improvement in Alzheimer’s disease agitation, as measured by the Cohen-Mansfield Agitation Inventory (CMAI) total score, compared with placebo.
ACCORD was a phase 3, randomized, double-blind, placebo-controlled withdrawal trial evaluating the efficacy and safety of AXS-05 in patients with Alzheimer’s disease agitation.
In the open-label period, 178 adults with probable Alzheimer’s disease and clinically significant agitation received AXS-05 (titrated to 45 mg dextromethorphan/105 mg bupropion twice daily) for up to 9 weeks.
A total of 108 (61%) patients had a sustained response, with 30% or more improvement from baseline in the CMAI total score and improvement on the Patient Global Impression of Change that were both maintained for 4 or more consecutive weeks. These patients entered the double-blind phase and were randomly allocated to receive twice-daily AXS-05 or placebo for up to 26 weeks.
In the double-blind period, AXS-05 “substantially and statistically” increased the time to relapse of agitation symptoms compared with placebo (hazard ratio [HR], 0.275; P = .014).
“The risk of relapse was 3.6-fold lower with AXS-05 compared with placebo,” Dr. Porsteinsson reported.
AXS-05 was also associated with a significantly lower relapse rate compared with placebo (7.5% vs 25.9%; P = .018).
Rates of discontinuation in the double-blind period owing to adverse events (AEs) were low (0% for AXS-05 and 1.9% for placebo). Three serious AEs were reported: one in the AXS-05 group (fecaloma), which was not related to study medication, and two in the placebo group (cardiac arrest, femur fracture).
Falls were reported in four participants in the AXS-05 group, none of which were related to study medication or associated with serious AEs, and in two participants in the placebo group, one of which was associated with femur fracture.
One death was reported in the placebo group. There was no evidence of cognitive decline with AXS-05, and treatment was not associated with sedation.
Promising Agent
Commenting on this research, Glen R. Finney, MD, director of the Geisinger Memory and Cognition Clinic in Wilkes-Barre, Pennsylvania, said the data “look promising as a safe way to help address acute agitation and reduce agitation reoccurrence.
“Agitation is a common, distressing, and sometimes safety issue for people fighting Alzheimer’s disease, and there’s very little evidence for efficacy and significant side effect issues for current medical management of agitation in Alzheimer’s disease,” said Dr. Finney, who was not part of the study.
He noted that first-line strategies for addressing agitation involve behavioral and environmental interventions.
“See if there’s a reason for the agitation and address that. Look for triggers for agitation and avoid those. Find places, things, and interactions that help people with Alzheimer’s disease avoid agitation: familiar locations, music, simple engaging activities. Reassurance, redirection, and distraction can help de-escalate agitation. Provide a safe environment that reduces safety risks,” Dr. Finney explained.
The next step, when medically appropriate, is trying acetylcholinesterase inhibitors such as donepezil, rivastigmine, and galantamine, and then adding memantine, a weak N-methyl-D-aspartate receptor antagonist.
“These medications can help reduce the risk of agitation,” Dr. Finney said.
“Beyond that, the evidence becomes weaker for any specific treatments, and that is where treatments with emerging evidence of efficacy and safety like dextromethorphan-bupropion become important,” Dr. Finney added.
Last May, the US Food and Drug Administration (FDA) approved the antipsychotic brexpiprazole (Rexulti) for Alzheimer’s disease-related agitation, making it the first FDA-approved drug for this indication.
The drug includes a boxed warning for medications in this class that older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk for death.
“There’s certainly a need to have multiple options for treating agitation in individuals with Alzheimer’s disease,” said Rebecca Edelmayer, PhD, senior director of scientific engagement for the Alzheimer’s Association.
Dr. Edelmayer, who was not part of the study, noted that in the ACCORD study, AXS-05 “significantly delayed the relapse or prevented the relapse with Alzheimer’s disease agitation compared with the placebo group and it was generally well tolerated, but it will be important to make sure that there’s more thorough review of the data overall to be sure that it’s both safe and effective.”
The study was funded by Axsome Therapeutics, the manufacturer of AXS-05. Dr. Porsteinsson has disclosed no relevant conflicts of interest. Dr. Finney and Dr. Edelmayer have no relevant disclosures.
A version of this article appeared on Medscape.com.
DENVER —
More than half of participants in the open-label extension period of the randomized clinical trial responded to the medication, which was associated with a 3.6-fold lower risk for relapse compared with placebo.
“The positive efficacy and favorable safety results with AXS-05 support its potential to fulfill a high unmet need for the treatment of Alzheimer’s disease agitation,” said Anton P. Porsteinsson, MD, director of the Alzheimer’s Disease Care, Research and Education Program, University of Rochester, New York.
The findings were presented at the 2024 annual meeting of the American Academy of Neurology.
Common and Disruptive
Agitation is reported in up to 70% of patients with Alzheimer’s disease and is characterized by emotional distress, aggressive behaviors, disruptive irritability, and disinhibition. Alzheimer’s disease-related agitation has been associated with increased caregiver burden, decreased functioning, accelerated cognitive decline, earlier nursing home placement, and increased mortality.
A previous phase 2/3 study of AXS-05 showed that the investigative agent led to rapid and significantly improvement in Alzheimer’s disease agitation, as measured by the Cohen-Mansfield Agitation Inventory (CMAI) total score, compared with placebo.
ACCORD was a phase 3, randomized, double-blind, placebo-controlled withdrawal trial evaluating the efficacy and safety of AXS-05 in patients with Alzheimer’s disease agitation.
In the open-label period, 178 adults with probable Alzheimer’s disease and clinically significant agitation received AXS-05 (titrated to 45 mg dextromethorphan/105 mg bupropion twice daily) for up to 9 weeks.
A total of 108 (61%) patients had a sustained response, with 30% or more improvement from baseline in the CMAI total score and improvement on the Patient Global Impression of Change that were both maintained for 4 or more consecutive weeks. These patients entered the double-blind phase and were randomly allocated to receive twice-daily AXS-05 or placebo for up to 26 weeks.
In the double-blind period, AXS-05 “substantially and statistically” increased the time to relapse of agitation symptoms compared with placebo (hazard ratio [HR], 0.275; P = .014).
“The risk of relapse was 3.6-fold lower with AXS-05 compared with placebo,” Dr. Porsteinsson reported.
AXS-05 was also associated with a significantly lower relapse rate compared with placebo (7.5% vs 25.9%; P = .018).
Rates of discontinuation in the double-blind period owing to adverse events (AEs) were low (0% for AXS-05 and 1.9% for placebo). Three serious AEs were reported: one in the AXS-05 group (fecaloma), which was not related to study medication, and two in the placebo group (cardiac arrest, femur fracture).
Falls were reported in four participants in the AXS-05 group, none of which were related to study medication or associated with serious AEs, and in two participants in the placebo group, one of which was associated with femur fracture.
One death was reported in the placebo group. There was no evidence of cognitive decline with AXS-05, and treatment was not associated with sedation.
Promising Agent
Commenting on this research, Glen R. Finney, MD, director of the Geisinger Memory and Cognition Clinic in Wilkes-Barre, Pennsylvania, said the data “look promising as a safe way to help address acute agitation and reduce agitation reoccurrence.
“Agitation is a common, distressing, and sometimes safety issue for people fighting Alzheimer’s disease, and there’s very little evidence for efficacy and significant side effect issues for current medical management of agitation in Alzheimer’s disease,” said Dr. Finney, who was not part of the study.
He noted that first-line strategies for addressing agitation involve behavioral and environmental interventions.
“See if there’s a reason for the agitation and address that. Look for triggers for agitation and avoid those. Find places, things, and interactions that help people with Alzheimer’s disease avoid agitation: familiar locations, music, simple engaging activities. Reassurance, redirection, and distraction can help de-escalate agitation. Provide a safe environment that reduces safety risks,” Dr. Finney explained.
The next step, when medically appropriate, is trying acetylcholinesterase inhibitors such as donepezil, rivastigmine, and galantamine, and then adding memantine, a weak N-methyl-D-aspartate receptor antagonist.
“These medications can help reduce the risk of agitation,” Dr. Finney said.
“Beyond that, the evidence becomes weaker for any specific treatments, and that is where treatments with emerging evidence of efficacy and safety like dextromethorphan-bupropion become important,” Dr. Finney added.
Last May, the US Food and Drug Administration (FDA) approved the antipsychotic brexpiprazole (Rexulti) for Alzheimer’s disease-related agitation, making it the first FDA-approved drug for this indication.
The drug includes a boxed warning for medications in this class that older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk for death.
“There’s certainly a need to have multiple options for treating agitation in individuals with Alzheimer’s disease,” said Rebecca Edelmayer, PhD, senior director of scientific engagement for the Alzheimer’s Association.
Dr. Edelmayer, who was not part of the study, noted that in the ACCORD study, AXS-05 “significantly delayed the relapse or prevented the relapse with Alzheimer’s disease agitation compared with the placebo group and it was generally well tolerated, but it will be important to make sure that there’s more thorough review of the data overall to be sure that it’s both safe and effective.”
The study was funded by Axsome Therapeutics, the manufacturer of AXS-05. Dr. Porsteinsson has disclosed no relevant conflicts of interest. Dr. Finney and Dr. Edelmayer have no relevant disclosures.
A version of this article appeared on Medscape.com.
DENVER —
More than half of participants in the open-label extension period of the randomized clinical trial responded to the medication, which was associated with a 3.6-fold lower risk for relapse compared with placebo.
“The positive efficacy and favorable safety results with AXS-05 support its potential to fulfill a high unmet need for the treatment of Alzheimer’s disease agitation,” said Anton P. Porsteinsson, MD, director of the Alzheimer’s Disease Care, Research and Education Program, University of Rochester, New York.
The findings were presented at the 2024 annual meeting of the American Academy of Neurology.
Common and Disruptive
Agitation is reported in up to 70% of patients with Alzheimer’s disease and is characterized by emotional distress, aggressive behaviors, disruptive irritability, and disinhibition. Alzheimer’s disease-related agitation has been associated with increased caregiver burden, decreased functioning, accelerated cognitive decline, earlier nursing home placement, and increased mortality.
A previous phase 2/3 study of AXS-05 showed that the investigative agent led to rapid and significantly improvement in Alzheimer’s disease agitation, as measured by the Cohen-Mansfield Agitation Inventory (CMAI) total score, compared with placebo.
ACCORD was a phase 3, randomized, double-blind, placebo-controlled withdrawal trial evaluating the efficacy and safety of AXS-05 in patients with Alzheimer’s disease agitation.
In the open-label period, 178 adults with probable Alzheimer’s disease and clinically significant agitation received AXS-05 (titrated to 45 mg dextromethorphan/105 mg bupropion twice daily) for up to 9 weeks.
A total of 108 (61%) patients had a sustained response, with 30% or more improvement from baseline in the CMAI total score and improvement on the Patient Global Impression of Change that were both maintained for 4 or more consecutive weeks. These patients entered the double-blind phase and were randomly allocated to receive twice-daily AXS-05 or placebo for up to 26 weeks.
In the double-blind period, AXS-05 “substantially and statistically” increased the time to relapse of agitation symptoms compared with placebo (hazard ratio [HR], 0.275; P = .014).
“The risk of relapse was 3.6-fold lower with AXS-05 compared with placebo,” Dr. Porsteinsson reported.
AXS-05 was also associated with a significantly lower relapse rate compared with placebo (7.5% vs 25.9%; P = .018).
Rates of discontinuation in the double-blind period owing to adverse events (AEs) were low (0% for AXS-05 and 1.9% for placebo). Three serious AEs were reported: one in the AXS-05 group (fecaloma), which was not related to study medication, and two in the placebo group (cardiac arrest, femur fracture).
Falls were reported in four participants in the AXS-05 group, none of which were related to study medication or associated with serious AEs, and in two participants in the placebo group, one of which was associated with femur fracture.
One death was reported in the placebo group. There was no evidence of cognitive decline with AXS-05, and treatment was not associated with sedation.
Promising Agent
Commenting on this research, Glen R. Finney, MD, director of the Geisinger Memory and Cognition Clinic in Wilkes-Barre, Pennsylvania, said the data “look promising as a safe way to help address acute agitation and reduce agitation reoccurrence.
“Agitation is a common, distressing, and sometimes safety issue for people fighting Alzheimer’s disease, and there’s very little evidence for efficacy and significant side effect issues for current medical management of agitation in Alzheimer’s disease,” said Dr. Finney, who was not part of the study.
He noted that first-line strategies for addressing agitation involve behavioral and environmental interventions.
“See if there’s a reason for the agitation and address that. Look for triggers for agitation and avoid those. Find places, things, and interactions that help people with Alzheimer’s disease avoid agitation: familiar locations, music, simple engaging activities. Reassurance, redirection, and distraction can help de-escalate agitation. Provide a safe environment that reduces safety risks,” Dr. Finney explained.
The next step, when medically appropriate, is trying acetylcholinesterase inhibitors such as donepezil, rivastigmine, and galantamine, and then adding memantine, a weak N-methyl-D-aspartate receptor antagonist.
“These medications can help reduce the risk of agitation,” Dr. Finney said.
“Beyond that, the evidence becomes weaker for any specific treatments, and that is where treatments with emerging evidence of efficacy and safety like dextromethorphan-bupropion become important,” Dr. Finney added.
Last May, the US Food and Drug Administration (FDA) approved the antipsychotic brexpiprazole (Rexulti) for Alzheimer’s disease-related agitation, making it the first FDA-approved drug for this indication.
The drug includes a boxed warning for medications in this class that older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk for death.
“There’s certainly a need to have multiple options for treating agitation in individuals with Alzheimer’s disease,” said Rebecca Edelmayer, PhD, senior director of scientific engagement for the Alzheimer’s Association.
Dr. Edelmayer, who was not part of the study, noted that in the ACCORD study, AXS-05 “significantly delayed the relapse or prevented the relapse with Alzheimer’s disease agitation compared with the placebo group and it was generally well tolerated, but it will be important to make sure that there’s more thorough review of the data overall to be sure that it’s both safe and effective.”
The study was funded by Axsome Therapeutics, the manufacturer of AXS-05. Dr. Porsteinsson has disclosed no relevant conflicts of interest. Dr. Finney and Dr. Edelmayer have no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AAN 2024
Adding Life to Your Patients’ Years
Caring for older adults was one of the most rewarding parts of my years practicing as a clinical cardiologist. I appreciated their wisdom, humor, and, very often, their respect and appreciation for physicians. It was always upsetting to see them suffer a mild fall or episode of atrial fibrillation and recognize that it could have major health ramifications.
That is not just a question for geriatric care. With fewer than two practicing geriatricians for every 10,000 older individuals, it is obvious that geriatricians cannot shoulder this responsibility alone. Almost all primary care physicians and subspecialists should prepare to care for older individuals and help them age healthfully.
Susan Friedman, MD, a board-certified geriatrics and lifestyle medicine clinician at the University of Rochester School of Medicine and Dentistry, Rochester, New York, reviewed the literature on the connection between lifestyle and healthy aging and concluded that the integration of lifestyle medicine into medical care for older adults is key to compressing morbidity. The pillars of lifestyle medicine — optimal nutrition, physical activity, stress management, restorative sleep, positive social connections, and avoidance of risky substances — both individually or as a sum are associated with less chronic disease, improved engagement in life, better physical and cognitive function, less frailty, and less sarcopenia. Framing discussions with patients around the six pillars of lifestyle medicine can be an effective strategy.
Optimal Nutrition
For a variety of reasons, older adults, especially those living alone, often lose the desire to prepare a nourishing meal. Older adults require different protein intake than younger patients to offset age-related sarcopenia, but helping them select healthy sources of protein is imperative. Both adequate protein consumption and eating patterns high in vegetables, legumes, fruit, and nuts and low in saturated fat, red meat, and processed meat can lower the risk of developing frailty.
Asking a patient to share a 24-hour food recall, and based upon that, resourcing nutritional guidance, a lifestyle medicine program or specialist, and insurance or community resources for food-as-medicine services, is a good first step.
Physical Activity
Increasing general physical activity can be a tough ask for many older adults, and joint pain is a common reason they demur. Messaging around targeted exercises to mitigate falls, improve muscle strength, and reduce joint pain may be more appealing. Contemporary research demonstrates that exercise, particularly open-skill exercise that requires quick decisions (such as table tennis) can be powerful. Maintaining cognition, mood enhancement, and independence may also be motivating messages.
The first step is curiosity: What does your patient like to do? Referral to a physical therapist or an exercise specialist to provide stepwise guidance along with resourcing community opportunities can then follow.
Restorative Sleep
“I’m old. I don’t need as much sleep.” We’ve probably all heard older patients say this. But the National Sleep Foundation’s report on sleep health and aging indicates that the need to sleep does not decrease with age. The ability to sleep, however, may decline. Assessing and treating disordered sleep is another example of how each lifestyle medicine pillar, such as nutrition and physical activity, is multidimensional and interacts to support the functional integrity of older patients. It’s hard to feel motivated to go for a walk if you lack adequate sleep.
Stress Management
Exploring stress with patients can be very revealing. Do they experience stress that energizes and has a positive effect? How much of their day is spent in negatively impactful distress? Chronic stress has been shown to affect immune function in older individuals. Start conversations with your older patients to normalize the importance of stress as a health measure.
Positive Social Connections
Loneliness puts individuals at higher risk for heart disease, stroke, and dementia and even increases the risk for premature death by up to 60%. Yet, clinicians and patients rarely discuss social connections during medical appointments. Tools such as the UCLA Loneliness Scale exist for health practitioners to assess and identify patients at risk for loneliness, as do resources to integrate social care into the delivery of healthcare.
Avoidance of Risky Substances
Alcohol assessments are not just for younger patients. One study found that 5.6 million adults ages 65 or older engaged in binge drinking in the past month. Because of body changes, the negative effects of alcohol may be greater on older adults, including interactions between alcohol and commonly prescribed medications.
Conducting a lifestyle assessment is an important way to engage with older patients and allows clinicians to identify opportunities to improve health behaviors, understand obstacles, and support patients to make lifestyle changes. It may uncover ways to remove some of the pill and treatment burdens that older adults often experience. The American College of Lifestyle Medicine (ACLM) offers clinical practice resources to support clinicians as well as “Lifestyle Medicine and Food as Medicine Essentials,” a 5.5-hour complimentary CE/CME course on food and lifestyle medicine that introduces clinicians to the therapeutic use of lifestyle medicine. ACLM also offers members interest groups focused on geriatrics, fitness, and mental health, which may be beneficial to clinicians treating older adults.
By engaging with older patients on their lifestyle behaviors, we can ensure that we are doing all we can to help them live longer — and live better.
Dr. Collings is director of lifestyle medicine, Silicon Valley Medical Development, and past president, American College of Lifestyle Medicine, Mountain View, California. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Caring for older adults was one of the most rewarding parts of my years practicing as a clinical cardiologist. I appreciated their wisdom, humor, and, very often, their respect and appreciation for physicians. It was always upsetting to see them suffer a mild fall or episode of atrial fibrillation and recognize that it could have major health ramifications.
That is not just a question for geriatric care. With fewer than two practicing geriatricians for every 10,000 older individuals, it is obvious that geriatricians cannot shoulder this responsibility alone. Almost all primary care physicians and subspecialists should prepare to care for older individuals and help them age healthfully.
Susan Friedman, MD, a board-certified geriatrics and lifestyle medicine clinician at the University of Rochester School of Medicine and Dentistry, Rochester, New York, reviewed the literature on the connection between lifestyle and healthy aging and concluded that the integration of lifestyle medicine into medical care for older adults is key to compressing morbidity. The pillars of lifestyle medicine — optimal nutrition, physical activity, stress management, restorative sleep, positive social connections, and avoidance of risky substances — both individually or as a sum are associated with less chronic disease, improved engagement in life, better physical and cognitive function, less frailty, and less sarcopenia. Framing discussions with patients around the six pillars of lifestyle medicine can be an effective strategy.
Optimal Nutrition
For a variety of reasons, older adults, especially those living alone, often lose the desire to prepare a nourishing meal. Older adults require different protein intake than younger patients to offset age-related sarcopenia, but helping them select healthy sources of protein is imperative. Both adequate protein consumption and eating patterns high in vegetables, legumes, fruit, and nuts and low in saturated fat, red meat, and processed meat can lower the risk of developing frailty.
Asking a patient to share a 24-hour food recall, and based upon that, resourcing nutritional guidance, a lifestyle medicine program or specialist, and insurance or community resources for food-as-medicine services, is a good first step.
Physical Activity
Increasing general physical activity can be a tough ask for many older adults, and joint pain is a common reason they demur. Messaging around targeted exercises to mitigate falls, improve muscle strength, and reduce joint pain may be more appealing. Contemporary research demonstrates that exercise, particularly open-skill exercise that requires quick decisions (such as table tennis) can be powerful. Maintaining cognition, mood enhancement, and independence may also be motivating messages.
The first step is curiosity: What does your patient like to do? Referral to a physical therapist or an exercise specialist to provide stepwise guidance along with resourcing community opportunities can then follow.
Restorative Sleep
“I’m old. I don’t need as much sleep.” We’ve probably all heard older patients say this. But the National Sleep Foundation’s report on sleep health and aging indicates that the need to sleep does not decrease with age. The ability to sleep, however, may decline. Assessing and treating disordered sleep is another example of how each lifestyle medicine pillar, such as nutrition and physical activity, is multidimensional and interacts to support the functional integrity of older patients. It’s hard to feel motivated to go for a walk if you lack adequate sleep.
Stress Management
Exploring stress with patients can be very revealing. Do they experience stress that energizes and has a positive effect? How much of their day is spent in negatively impactful distress? Chronic stress has been shown to affect immune function in older individuals. Start conversations with your older patients to normalize the importance of stress as a health measure.
Positive Social Connections
Loneliness puts individuals at higher risk for heart disease, stroke, and dementia and even increases the risk for premature death by up to 60%. Yet, clinicians and patients rarely discuss social connections during medical appointments. Tools such as the UCLA Loneliness Scale exist for health practitioners to assess and identify patients at risk for loneliness, as do resources to integrate social care into the delivery of healthcare.
Avoidance of Risky Substances
Alcohol assessments are not just for younger patients. One study found that 5.6 million adults ages 65 or older engaged in binge drinking in the past month. Because of body changes, the negative effects of alcohol may be greater on older adults, including interactions between alcohol and commonly prescribed medications.
Conducting a lifestyle assessment is an important way to engage with older patients and allows clinicians to identify opportunities to improve health behaviors, understand obstacles, and support patients to make lifestyle changes. It may uncover ways to remove some of the pill and treatment burdens that older adults often experience. The American College of Lifestyle Medicine (ACLM) offers clinical practice resources to support clinicians as well as “Lifestyle Medicine and Food as Medicine Essentials,” a 5.5-hour complimentary CE/CME course on food and lifestyle medicine that introduces clinicians to the therapeutic use of lifestyle medicine. ACLM also offers members interest groups focused on geriatrics, fitness, and mental health, which may be beneficial to clinicians treating older adults.
By engaging with older patients on their lifestyle behaviors, we can ensure that we are doing all we can to help them live longer — and live better.
Dr. Collings is director of lifestyle medicine, Silicon Valley Medical Development, and past president, American College of Lifestyle Medicine, Mountain View, California. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Caring for older adults was one of the most rewarding parts of my years practicing as a clinical cardiologist. I appreciated their wisdom, humor, and, very often, their respect and appreciation for physicians. It was always upsetting to see them suffer a mild fall or episode of atrial fibrillation and recognize that it could have major health ramifications.
That is not just a question for geriatric care. With fewer than two practicing geriatricians for every 10,000 older individuals, it is obvious that geriatricians cannot shoulder this responsibility alone. Almost all primary care physicians and subspecialists should prepare to care for older individuals and help them age healthfully.
Susan Friedman, MD, a board-certified geriatrics and lifestyle medicine clinician at the University of Rochester School of Medicine and Dentistry, Rochester, New York, reviewed the literature on the connection between lifestyle and healthy aging and concluded that the integration of lifestyle medicine into medical care for older adults is key to compressing morbidity. The pillars of lifestyle medicine — optimal nutrition, physical activity, stress management, restorative sleep, positive social connections, and avoidance of risky substances — both individually or as a sum are associated with less chronic disease, improved engagement in life, better physical and cognitive function, less frailty, and less sarcopenia. Framing discussions with patients around the six pillars of lifestyle medicine can be an effective strategy.
Optimal Nutrition
For a variety of reasons, older adults, especially those living alone, often lose the desire to prepare a nourishing meal. Older adults require different protein intake than younger patients to offset age-related sarcopenia, but helping them select healthy sources of protein is imperative. Both adequate protein consumption and eating patterns high in vegetables, legumes, fruit, and nuts and low in saturated fat, red meat, and processed meat can lower the risk of developing frailty.
Asking a patient to share a 24-hour food recall, and based upon that, resourcing nutritional guidance, a lifestyle medicine program or specialist, and insurance or community resources for food-as-medicine services, is a good first step.
Physical Activity
Increasing general physical activity can be a tough ask for many older adults, and joint pain is a common reason they demur. Messaging around targeted exercises to mitigate falls, improve muscle strength, and reduce joint pain may be more appealing. Contemporary research demonstrates that exercise, particularly open-skill exercise that requires quick decisions (such as table tennis) can be powerful. Maintaining cognition, mood enhancement, and independence may also be motivating messages.
The first step is curiosity: What does your patient like to do? Referral to a physical therapist or an exercise specialist to provide stepwise guidance along with resourcing community opportunities can then follow.
Restorative Sleep
“I’m old. I don’t need as much sleep.” We’ve probably all heard older patients say this. But the National Sleep Foundation’s report on sleep health and aging indicates that the need to sleep does not decrease with age. The ability to sleep, however, may decline. Assessing and treating disordered sleep is another example of how each lifestyle medicine pillar, such as nutrition and physical activity, is multidimensional and interacts to support the functional integrity of older patients. It’s hard to feel motivated to go for a walk if you lack adequate sleep.
Stress Management
Exploring stress with patients can be very revealing. Do they experience stress that energizes and has a positive effect? How much of their day is spent in negatively impactful distress? Chronic stress has been shown to affect immune function in older individuals. Start conversations with your older patients to normalize the importance of stress as a health measure.
Positive Social Connections
Loneliness puts individuals at higher risk for heart disease, stroke, and dementia and even increases the risk for premature death by up to 60%. Yet, clinicians and patients rarely discuss social connections during medical appointments. Tools such as the UCLA Loneliness Scale exist for health practitioners to assess and identify patients at risk for loneliness, as do resources to integrate social care into the delivery of healthcare.
Avoidance of Risky Substances
Alcohol assessments are not just for younger patients. One study found that 5.6 million adults ages 65 or older engaged in binge drinking in the past month. Because of body changes, the negative effects of alcohol may be greater on older adults, including interactions between alcohol and commonly prescribed medications.
Conducting a lifestyle assessment is an important way to engage with older patients and allows clinicians to identify opportunities to improve health behaviors, understand obstacles, and support patients to make lifestyle changes. It may uncover ways to remove some of the pill and treatment burdens that older adults often experience. The American College of Lifestyle Medicine (ACLM) offers clinical practice resources to support clinicians as well as “Lifestyle Medicine and Food as Medicine Essentials,” a 5.5-hour complimentary CE/CME course on food and lifestyle medicine that introduces clinicians to the therapeutic use of lifestyle medicine. ACLM also offers members interest groups focused on geriatrics, fitness, and mental health, which may be beneficial to clinicians treating older adults.
By engaging with older patients on their lifestyle behaviors, we can ensure that we are doing all we can to help them live longer — and live better.
Dr. Collings is director of lifestyle medicine, Silicon Valley Medical Development, and past president, American College of Lifestyle Medicine, Mountain View, California. She has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Antipsychotics for Dementia Pose Wide-Ranging Health Risks
Antipsychotic use in older adults with dementia is associated with a significant increased risk for stroke, myocardial infarction, heart failure, pneumonia, fracture, acute kidney injury, and a range of other health problems compared with nonuse, new research showed.
The adverse events are far broader and pose more severe health risks than previously reported, investigators noted, and suggested greater caution is needed when prescribing antipsychotics to treat psychological symptoms of dementia.
The matched cohort study used patient registry data on nearly 174,000 people with dementia and compared those who were prescribed an antipsychotic on or after their dementia diagnosis with those who had not received a prescription for the drugs.
Any antipsychotic use was associated with double the risk for pneumonia, a 1.7-fold increased risk for acute kidney injury, and 1.6-fold higher odds of venous thromboembolism compared to nonuse.
Investigators found an increased risk for all outcomes studied, except for ventricular arrythmia, and risk was highest for most within the first week of treatment.
“Any potential benefits of antipsychotic treatment therefore need to be weighed against the risk of serious harm across multiple outcomes. Although there may be times when an antipsychotic prescription is the least bad option, clinicians should actively consider the risks, considering patients’ pre-existing comorbidities and living support,” lead investigator Pearl Mok, research fellow at the Centre for Pharmacoepidemiology and Drug Safety, The University of Manchester, Manchester, England, and colleagues wrote.
The findings were published online in The BMJ.
High Risk
Depression, aggression, anxiety, psychosis, and other behavioral and psychological symptoms are common in people with dementia. Despite earlier reports of increased risk for stroke and mortality with antipsychotic use, the drugs are frequently prescribed to treat these symptoms.
While some preliminary studies identified other adverse outcomes from antipsychotic use, results are limited and inconsistent.
Investigators used primary and secondary care data from the Clinical Practice Research Datalink in England. A total of 173,910 adults (63% women) had a dementia diagnosis between January 1998 and May 2018.
Of the total cohort, 35,339 patients were prescribed an antipsychotic on, or after, a dementia diagnosis. Each was matched with up to 15 patients with dementia with no history of antipsychotic use following diagnosis.
Almost 80% of antipsychotic prescriptions were for risperidone, quetiapine, haloperidol, and olanzapine.
Any antipsychotic use was associated with significantly higher risks for pneumonia (hazard ratio [HR], 2.03; 95% CI, 1.96-2.10), acute kidney injury (HR, 1.57; 95% CI, 1.48-1.66), stroke (HR, 1.54; 95% CI, 1.46-1.63), venous thromboembolism (HR, 1.52; 95% CI, 1.38-1.67), fracture (HR, 1.36; 95% CI, 1.30-1.44), myocardial infarction (HR, 1.22; 95% CI, 1.12-1.34), and heart failure (HR, 1.16; 95% CI, 1.09-1.24).
The risk for all conditions was highest within the first 3 months of treatment, with a cumulative incidence of pneumonia among antipsychotic users of 4.48% vs 1.49% among nonusers. At 1 year, this increased to 10.41% for users vs 5.63% for nonusers.
“Given the higher risks of adverse events in the early days after drug initiation, clinical examinations should be taken before, and clinical reviews conducted shortly after, the start of treatment,” the authors wrote. “Our study reaffirms that these drugs should only be prescribed for the shortest period possible.”
‘Serious Harms’
In an accompanying editorial, Raya Elfadel Kheirbek, MD, and Cristina LaFont, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland, said the findings “highlight the need for careful justification of antipsychotic use in dementia care, including a comprehensive assessment of the benefits weighed against a broader range of serious harms than previously acknowledged.”
“Using antipsychotics for the management of dementia-related behaviors requires nuanced decision-making after careful assessment, informed by a personalized approach,” they continued. “Dr. Mok and colleagues call for a critical re-evaluation of antipsychotic use in this clinical setting.”
While the findings add to and expand what was already known, “we need to be clear that they don’t show antipsychotics cause all the adverse outcomes reported,” Masud Husain, DPhil, professor of neurology, University of Oxford, England, said in a statement.
While investigators attempted to use matched controls with dementia who had not received antipsychotics, “the people who were prescribed the drugs may simply have been more vulnerable to some of the conditions that occurred more frequently in them, such as pneumonia and cardiovascular disorders,” said Dr. Husain, who was not part of the research.
Although the study was not designed to explore reverse causality, the findings are important for clinicians who prescribe antipsychotics for patients with dementia, Robert Howard, professor of old age psychiatry, at the University of College London, London, England said in a statement.
“Initiation of these drugs in people with dementia should only ever be under specialist supervision, with involvement of patients and family members in informed discussion and review,” said Dr. Howard, who was not involved in the study.
The study was funded by the National Institute for Health and Care Research. Dr. Mok reported no relevant conflicts. Other authors’ disclosures are included in the original article. Dr. Hussain, Dr. Howard, Dr. Kheirbek, and Dr. LeFon reported no relevant conflicts.
A version of this article appeared on Medscape.com.
Antipsychotic use in older adults with dementia is associated with a significant increased risk for stroke, myocardial infarction, heart failure, pneumonia, fracture, acute kidney injury, and a range of other health problems compared with nonuse, new research showed.
The adverse events are far broader and pose more severe health risks than previously reported, investigators noted, and suggested greater caution is needed when prescribing antipsychotics to treat psychological symptoms of dementia.
The matched cohort study used patient registry data on nearly 174,000 people with dementia and compared those who were prescribed an antipsychotic on or after their dementia diagnosis with those who had not received a prescription for the drugs.
Any antipsychotic use was associated with double the risk for pneumonia, a 1.7-fold increased risk for acute kidney injury, and 1.6-fold higher odds of venous thromboembolism compared to nonuse.
Investigators found an increased risk for all outcomes studied, except for ventricular arrythmia, and risk was highest for most within the first week of treatment.
“Any potential benefits of antipsychotic treatment therefore need to be weighed against the risk of serious harm across multiple outcomes. Although there may be times when an antipsychotic prescription is the least bad option, clinicians should actively consider the risks, considering patients’ pre-existing comorbidities and living support,” lead investigator Pearl Mok, research fellow at the Centre for Pharmacoepidemiology and Drug Safety, The University of Manchester, Manchester, England, and colleagues wrote.
The findings were published online in The BMJ.
High Risk
Depression, aggression, anxiety, psychosis, and other behavioral and psychological symptoms are common in people with dementia. Despite earlier reports of increased risk for stroke and mortality with antipsychotic use, the drugs are frequently prescribed to treat these symptoms.
While some preliminary studies identified other adverse outcomes from antipsychotic use, results are limited and inconsistent.
Investigators used primary and secondary care data from the Clinical Practice Research Datalink in England. A total of 173,910 adults (63% women) had a dementia diagnosis between January 1998 and May 2018.
Of the total cohort, 35,339 patients were prescribed an antipsychotic on, or after, a dementia diagnosis. Each was matched with up to 15 patients with dementia with no history of antipsychotic use following diagnosis.
Almost 80% of antipsychotic prescriptions were for risperidone, quetiapine, haloperidol, and olanzapine.
Any antipsychotic use was associated with significantly higher risks for pneumonia (hazard ratio [HR], 2.03; 95% CI, 1.96-2.10), acute kidney injury (HR, 1.57; 95% CI, 1.48-1.66), stroke (HR, 1.54; 95% CI, 1.46-1.63), venous thromboembolism (HR, 1.52; 95% CI, 1.38-1.67), fracture (HR, 1.36; 95% CI, 1.30-1.44), myocardial infarction (HR, 1.22; 95% CI, 1.12-1.34), and heart failure (HR, 1.16; 95% CI, 1.09-1.24).
The risk for all conditions was highest within the first 3 months of treatment, with a cumulative incidence of pneumonia among antipsychotic users of 4.48% vs 1.49% among nonusers. At 1 year, this increased to 10.41% for users vs 5.63% for nonusers.
“Given the higher risks of adverse events in the early days after drug initiation, clinical examinations should be taken before, and clinical reviews conducted shortly after, the start of treatment,” the authors wrote. “Our study reaffirms that these drugs should only be prescribed for the shortest period possible.”
‘Serious Harms’
In an accompanying editorial, Raya Elfadel Kheirbek, MD, and Cristina LaFont, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland, said the findings “highlight the need for careful justification of antipsychotic use in dementia care, including a comprehensive assessment of the benefits weighed against a broader range of serious harms than previously acknowledged.”
“Using antipsychotics for the management of dementia-related behaviors requires nuanced decision-making after careful assessment, informed by a personalized approach,” they continued. “Dr. Mok and colleagues call for a critical re-evaluation of antipsychotic use in this clinical setting.”
While the findings add to and expand what was already known, “we need to be clear that they don’t show antipsychotics cause all the adverse outcomes reported,” Masud Husain, DPhil, professor of neurology, University of Oxford, England, said in a statement.
While investigators attempted to use matched controls with dementia who had not received antipsychotics, “the people who were prescribed the drugs may simply have been more vulnerable to some of the conditions that occurred more frequently in them, such as pneumonia and cardiovascular disorders,” said Dr. Husain, who was not part of the research.
Although the study was not designed to explore reverse causality, the findings are important for clinicians who prescribe antipsychotics for patients with dementia, Robert Howard, professor of old age psychiatry, at the University of College London, London, England said in a statement.
“Initiation of these drugs in people with dementia should only ever be under specialist supervision, with involvement of patients and family members in informed discussion and review,” said Dr. Howard, who was not involved in the study.
The study was funded by the National Institute for Health and Care Research. Dr. Mok reported no relevant conflicts. Other authors’ disclosures are included in the original article. Dr. Hussain, Dr. Howard, Dr. Kheirbek, and Dr. LeFon reported no relevant conflicts.
A version of this article appeared on Medscape.com.
Antipsychotic use in older adults with dementia is associated with a significant increased risk for stroke, myocardial infarction, heart failure, pneumonia, fracture, acute kidney injury, and a range of other health problems compared with nonuse, new research showed.
The adverse events are far broader and pose more severe health risks than previously reported, investigators noted, and suggested greater caution is needed when prescribing antipsychotics to treat psychological symptoms of dementia.
The matched cohort study used patient registry data on nearly 174,000 people with dementia and compared those who were prescribed an antipsychotic on or after their dementia diagnosis with those who had not received a prescription for the drugs.
Any antipsychotic use was associated with double the risk for pneumonia, a 1.7-fold increased risk for acute kidney injury, and 1.6-fold higher odds of venous thromboembolism compared to nonuse.
Investigators found an increased risk for all outcomes studied, except for ventricular arrythmia, and risk was highest for most within the first week of treatment.
“Any potential benefits of antipsychotic treatment therefore need to be weighed against the risk of serious harm across multiple outcomes. Although there may be times when an antipsychotic prescription is the least bad option, clinicians should actively consider the risks, considering patients’ pre-existing comorbidities and living support,” lead investigator Pearl Mok, research fellow at the Centre for Pharmacoepidemiology and Drug Safety, The University of Manchester, Manchester, England, and colleagues wrote.
The findings were published online in The BMJ.
High Risk
Depression, aggression, anxiety, psychosis, and other behavioral and psychological symptoms are common in people with dementia. Despite earlier reports of increased risk for stroke and mortality with antipsychotic use, the drugs are frequently prescribed to treat these symptoms.
While some preliminary studies identified other adverse outcomes from antipsychotic use, results are limited and inconsistent.
Investigators used primary and secondary care data from the Clinical Practice Research Datalink in England. A total of 173,910 adults (63% women) had a dementia diagnosis between January 1998 and May 2018.
Of the total cohort, 35,339 patients were prescribed an antipsychotic on, or after, a dementia diagnosis. Each was matched with up to 15 patients with dementia with no history of antipsychotic use following diagnosis.
Almost 80% of antipsychotic prescriptions were for risperidone, quetiapine, haloperidol, and olanzapine.
Any antipsychotic use was associated with significantly higher risks for pneumonia (hazard ratio [HR], 2.03; 95% CI, 1.96-2.10), acute kidney injury (HR, 1.57; 95% CI, 1.48-1.66), stroke (HR, 1.54; 95% CI, 1.46-1.63), venous thromboembolism (HR, 1.52; 95% CI, 1.38-1.67), fracture (HR, 1.36; 95% CI, 1.30-1.44), myocardial infarction (HR, 1.22; 95% CI, 1.12-1.34), and heart failure (HR, 1.16; 95% CI, 1.09-1.24).
The risk for all conditions was highest within the first 3 months of treatment, with a cumulative incidence of pneumonia among antipsychotic users of 4.48% vs 1.49% among nonusers. At 1 year, this increased to 10.41% for users vs 5.63% for nonusers.
“Given the higher risks of adverse events in the early days after drug initiation, clinical examinations should be taken before, and clinical reviews conducted shortly after, the start of treatment,” the authors wrote. “Our study reaffirms that these drugs should only be prescribed for the shortest period possible.”
‘Serious Harms’
In an accompanying editorial, Raya Elfadel Kheirbek, MD, and Cristina LaFont, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland, said the findings “highlight the need for careful justification of antipsychotic use in dementia care, including a comprehensive assessment of the benefits weighed against a broader range of serious harms than previously acknowledged.”
“Using antipsychotics for the management of dementia-related behaviors requires nuanced decision-making after careful assessment, informed by a personalized approach,” they continued. “Dr. Mok and colleagues call for a critical re-evaluation of antipsychotic use in this clinical setting.”
While the findings add to and expand what was already known, “we need to be clear that they don’t show antipsychotics cause all the adverse outcomes reported,” Masud Husain, DPhil, professor of neurology, University of Oxford, England, said in a statement.
While investigators attempted to use matched controls with dementia who had not received antipsychotics, “the people who were prescribed the drugs may simply have been more vulnerable to some of the conditions that occurred more frequently in them, such as pneumonia and cardiovascular disorders,” said Dr. Husain, who was not part of the research.
Although the study was not designed to explore reverse causality, the findings are important for clinicians who prescribe antipsychotics for patients with dementia, Robert Howard, professor of old age psychiatry, at the University of College London, London, England said in a statement.
“Initiation of these drugs in people with dementia should only ever be under specialist supervision, with involvement of patients and family members in informed discussion and review,” said Dr. Howard, who was not involved in the study.
The study was funded by the National Institute for Health and Care Research. Dr. Mok reported no relevant conflicts. Other authors’ disclosures are included in the original article. Dr. Hussain, Dr. Howard, Dr. Kheirbek, and Dr. LeFon reported no relevant conflicts.
A version of this article appeared on Medscape.com.
FROM THE BMJ
Heart Failure the Most Common Complication of Atrial Fibrillation, Not Stroke
FROM BMJ
The lifetime risk of atrial fibrillation (AF) increased from 2000 to 2022 from one in four to one in three, a Danish population-based study of temporal trends found.
Heart failure was the most frequent complication linked to this arrhythmia, with a lifetime risk of two in five, twice that of stroke, according to investigators led by Nicklas Vinter, MD, PhD, a postdoctoral researcher at the Danish Center for Health Service Research in the Department of Clinical Medicine at Aalborg University, Denmark.
Published in BMJ, the study found the lifetime risks of post-AF stroke, ischemic stroke, and myocardial infarction improved only modestly over time and remained high, with virtually no improvement in the lifetime risk of heart failure.
“Our work provides novel lifetime risk estimates that are instrumental in facilitating effective risk communication between patients and their physicians,” Dr. Vinter said in an interview. “The knowledge of risks from a lifelong perspective may serve as a motivator for patients to commence or intensify preventive efforts.” AF patients could, for example, adopt healthier lifestyles or adhere to prescribed medications, Dr. Vinter explained.
“The substantial lifetime risk of heart failure following atrial fibrillation necessitates heightened attention to its prevention and early detection,” Dr. Vinter said. “Furthermore, the high lifetime risk of stroke remains a critical complication, which highlights the importance of continuous attention to the initiation and maintenance of oral anticoagulation therapy.”
The Study
The cohort consisted of 3.5 million individuals (51.7% women) who did not have AF as of age 45 or older. These individuals were followed until incident AF, migration, death, or end of follow-up, whichever came first.
All 362,721 individuals with incident AF (53.6% men) but no prevalent complication were further followed over two time periods (2000-2010 and 2011-2020) until incident heart failure, stroke, or myocardial infarction.
Among the findings:
- Lifetime AF risk increased from 24.2% in 2000-2010 to 30.9% in 2011-2022, for a difference of 6.7% (95% confidence interval [CI], 6.5%-6.8%).
- Lifetime AF risk rose across all subgroups over time, with a larger increase in men and individuals with heart failure, myocardial infarction, stroke, diabetes, and chronic kidney disease.
- Lifetime risk of heart failure was 42.9% in 2000-2010 and 42.1% in 2011-2022, for a difference of −0.8% (95% CI, −3.8% to 2.2%).
- The lifetime risks of post-AF stroke and of myocardial infarction decreased slightly between the two periods, from 22.4% to 19.9% for stroke (difference −2.5%, 95% CI, −4.2% to −0.7%) and from 13.7% to 9.8% for myocardial infarction (−3.9%, 95% CI, −5.3% to −2.4%). No differential decrease between men and women emerged.
“Our novel quantification of the long-term downstream consequences of atrial fibrillation highlights the critical need for treatments to further decrease stroke risk as well as for heart failure prevention strategies among patients with atrial fibrillation,” the Danish researchers wrote.
Offering an outsider’s perspective, John P. Higgins, MD, MBA, MPhil, a sports cardiologist at McGovern Medical School at The University of Texas Health Science Center at Houston, said, “Think of atrial fibrillation as a barometer of underlying stress on the heart. When blood pressure is high, or a patient has underlying asymptomatic coronary artery disease or heart failure, they are more likely to have episodes of atrial fibrillation.”
According to Dr. Higgins, risk factors for AF are underappreciated in the United States and elsewhere, and primary care doctors need to be aware of them. “We should try to identify these risk factors and do primary prevention to improve risk factors to reduce the progression to heart failure and myocardial infarction and stroke. But lifelong prevention is even better, he added. “Doing things to prevent actually getting risk factors in the first place. So a healthy lifestyle including exercise, diet, hydration, sleep, relaxation, social contact, and a little sunlight might be the long-term keys and starting them at a young age, too.”
In an accompanying editorial, Jianhua Wu, PhD, a professor of biostatistics and health data science with the Wolfson Institute of Population Health at Queen Mary University of London, and a colleague, cited the study’s robust observational research and called the analysis noteworthy for its quantification of the long-term risks of post-AF sequelae. They cautioned, however, that its grouping into two 10-year periods (2000-2010 and 2011-2020) came at the cost of losing temporal resolution. They also called out the lack of reporting on the ethnic composition of the study population, a factor that influences lifetime AF risk, and the absence of subgroup analysis by socioeconomic status, which affects incidence and outcomes.
The editorialists noted that while interventions to prevent stroke dominated AF research and guidelines during the study time period, no evidence suggests these interventions can prevent incident heart failure. “Alignment of both randomised clinical trials and guidelines to better reflect the needs of the real-world population with atrial fibrillation is necessary because further improvements to patient prognosis are likely to require a broader perspective on atrial fibrillation management beyond prevention of stroke,” they wrote.
In the meantime this study “challenges research priorities and guideline design, and raises critical questions for the research and clinical communities about how the growing burden of atrial fibrillation can be stopped,” they wrote.
This work was supported by the Danish Cardiovascular Academy, which is funded by the Novo Nordisk Foundation, and The Danish Heart Foundation. Dr. Vinter has been an advisory board member and consultant for AstraZeneca and has an institutional research grant from BMS/Pfizer unrelated to the current study. He reported personal consulting fees from BMS and Pfizer. Other coauthors disclosed research support from and/or consulting work for private industry, as well as grants from not-for-profit research-funding organizations. Dr. Higgins had no competing interest to declare. The editorial writers had no relevant financial interests to declare. Dr. Wu is supported by Barts Charity.
FROM BMJ
The lifetime risk of atrial fibrillation (AF) increased from 2000 to 2022 from one in four to one in three, a Danish population-based study of temporal trends found.
Heart failure was the most frequent complication linked to this arrhythmia, with a lifetime risk of two in five, twice that of stroke, according to investigators led by Nicklas Vinter, MD, PhD, a postdoctoral researcher at the Danish Center for Health Service Research in the Department of Clinical Medicine at Aalborg University, Denmark.
Published in BMJ, the study found the lifetime risks of post-AF stroke, ischemic stroke, and myocardial infarction improved only modestly over time and remained high, with virtually no improvement in the lifetime risk of heart failure.
“Our work provides novel lifetime risk estimates that are instrumental in facilitating effective risk communication between patients and their physicians,” Dr. Vinter said in an interview. “The knowledge of risks from a lifelong perspective may serve as a motivator for patients to commence or intensify preventive efforts.” AF patients could, for example, adopt healthier lifestyles or adhere to prescribed medications, Dr. Vinter explained.
“The substantial lifetime risk of heart failure following atrial fibrillation necessitates heightened attention to its prevention and early detection,” Dr. Vinter said. “Furthermore, the high lifetime risk of stroke remains a critical complication, which highlights the importance of continuous attention to the initiation and maintenance of oral anticoagulation therapy.”
The Study
The cohort consisted of 3.5 million individuals (51.7% women) who did not have AF as of age 45 or older. These individuals were followed until incident AF, migration, death, or end of follow-up, whichever came first.
All 362,721 individuals with incident AF (53.6% men) but no prevalent complication were further followed over two time periods (2000-2010 and 2011-2020) until incident heart failure, stroke, or myocardial infarction.
Among the findings:
- Lifetime AF risk increased from 24.2% in 2000-2010 to 30.9% in 2011-2022, for a difference of 6.7% (95% confidence interval [CI], 6.5%-6.8%).
- Lifetime AF risk rose across all subgroups over time, with a larger increase in men and individuals with heart failure, myocardial infarction, stroke, diabetes, and chronic kidney disease.
- Lifetime risk of heart failure was 42.9% in 2000-2010 and 42.1% in 2011-2022, for a difference of −0.8% (95% CI, −3.8% to 2.2%).
- The lifetime risks of post-AF stroke and of myocardial infarction decreased slightly between the two periods, from 22.4% to 19.9% for stroke (difference −2.5%, 95% CI, −4.2% to −0.7%) and from 13.7% to 9.8% for myocardial infarction (−3.9%, 95% CI, −5.3% to −2.4%). No differential decrease between men and women emerged.
“Our novel quantification of the long-term downstream consequences of atrial fibrillation highlights the critical need for treatments to further decrease stroke risk as well as for heart failure prevention strategies among patients with atrial fibrillation,” the Danish researchers wrote.
Offering an outsider’s perspective, John P. Higgins, MD, MBA, MPhil, a sports cardiologist at McGovern Medical School at The University of Texas Health Science Center at Houston, said, “Think of atrial fibrillation as a barometer of underlying stress on the heart. When blood pressure is high, or a patient has underlying asymptomatic coronary artery disease or heart failure, they are more likely to have episodes of atrial fibrillation.”
According to Dr. Higgins, risk factors for AF are underappreciated in the United States and elsewhere, and primary care doctors need to be aware of them. “We should try to identify these risk factors and do primary prevention to improve risk factors to reduce the progression to heart failure and myocardial infarction and stroke. But lifelong prevention is even better, he added. “Doing things to prevent actually getting risk factors in the first place. So a healthy lifestyle including exercise, diet, hydration, sleep, relaxation, social contact, and a little sunlight might be the long-term keys and starting them at a young age, too.”
In an accompanying editorial, Jianhua Wu, PhD, a professor of biostatistics and health data science with the Wolfson Institute of Population Health at Queen Mary University of London, and a colleague, cited the study’s robust observational research and called the analysis noteworthy for its quantification of the long-term risks of post-AF sequelae. They cautioned, however, that its grouping into two 10-year periods (2000-2010 and 2011-2020) came at the cost of losing temporal resolution. They also called out the lack of reporting on the ethnic composition of the study population, a factor that influences lifetime AF risk, and the absence of subgroup analysis by socioeconomic status, which affects incidence and outcomes.
The editorialists noted that while interventions to prevent stroke dominated AF research and guidelines during the study time period, no evidence suggests these interventions can prevent incident heart failure. “Alignment of both randomised clinical trials and guidelines to better reflect the needs of the real-world population with atrial fibrillation is necessary because further improvements to patient prognosis are likely to require a broader perspective on atrial fibrillation management beyond prevention of stroke,” they wrote.
In the meantime this study “challenges research priorities and guideline design, and raises critical questions for the research and clinical communities about how the growing burden of atrial fibrillation can be stopped,” they wrote.
This work was supported by the Danish Cardiovascular Academy, which is funded by the Novo Nordisk Foundation, and The Danish Heart Foundation. Dr. Vinter has been an advisory board member and consultant for AstraZeneca and has an institutional research grant from BMS/Pfizer unrelated to the current study. He reported personal consulting fees from BMS and Pfizer. Other coauthors disclosed research support from and/or consulting work for private industry, as well as grants from not-for-profit research-funding organizations. Dr. Higgins had no competing interest to declare. The editorial writers had no relevant financial interests to declare. Dr. Wu is supported by Barts Charity.
FROM BMJ
The lifetime risk of atrial fibrillation (AF) increased from 2000 to 2022 from one in four to one in three, a Danish population-based study of temporal trends found.
Heart failure was the most frequent complication linked to this arrhythmia, with a lifetime risk of two in five, twice that of stroke, according to investigators led by Nicklas Vinter, MD, PhD, a postdoctoral researcher at the Danish Center for Health Service Research in the Department of Clinical Medicine at Aalborg University, Denmark.
Published in BMJ, the study found the lifetime risks of post-AF stroke, ischemic stroke, and myocardial infarction improved only modestly over time and remained high, with virtually no improvement in the lifetime risk of heart failure.
“Our work provides novel lifetime risk estimates that are instrumental in facilitating effective risk communication between patients and their physicians,” Dr. Vinter said in an interview. “The knowledge of risks from a lifelong perspective may serve as a motivator for patients to commence or intensify preventive efforts.” AF patients could, for example, adopt healthier lifestyles or adhere to prescribed medications, Dr. Vinter explained.
“The substantial lifetime risk of heart failure following atrial fibrillation necessitates heightened attention to its prevention and early detection,” Dr. Vinter said. “Furthermore, the high lifetime risk of stroke remains a critical complication, which highlights the importance of continuous attention to the initiation and maintenance of oral anticoagulation therapy.”
The Study
The cohort consisted of 3.5 million individuals (51.7% women) who did not have AF as of age 45 or older. These individuals were followed until incident AF, migration, death, or end of follow-up, whichever came first.
All 362,721 individuals with incident AF (53.6% men) but no prevalent complication were further followed over two time periods (2000-2010 and 2011-2020) until incident heart failure, stroke, or myocardial infarction.
Among the findings:
- Lifetime AF risk increased from 24.2% in 2000-2010 to 30.9% in 2011-2022, for a difference of 6.7% (95% confidence interval [CI], 6.5%-6.8%).
- Lifetime AF risk rose across all subgroups over time, with a larger increase in men and individuals with heart failure, myocardial infarction, stroke, diabetes, and chronic kidney disease.
- Lifetime risk of heart failure was 42.9% in 2000-2010 and 42.1% in 2011-2022, for a difference of −0.8% (95% CI, −3.8% to 2.2%).
- The lifetime risks of post-AF stroke and of myocardial infarction decreased slightly between the two periods, from 22.4% to 19.9% for stroke (difference −2.5%, 95% CI, −4.2% to −0.7%) and from 13.7% to 9.8% for myocardial infarction (−3.9%, 95% CI, −5.3% to −2.4%). No differential decrease between men and women emerged.
“Our novel quantification of the long-term downstream consequences of atrial fibrillation highlights the critical need for treatments to further decrease stroke risk as well as for heart failure prevention strategies among patients with atrial fibrillation,” the Danish researchers wrote.
Offering an outsider’s perspective, John P. Higgins, MD, MBA, MPhil, a sports cardiologist at McGovern Medical School at The University of Texas Health Science Center at Houston, said, “Think of atrial fibrillation as a barometer of underlying stress on the heart. When blood pressure is high, or a patient has underlying asymptomatic coronary artery disease or heart failure, they are more likely to have episodes of atrial fibrillation.”
According to Dr. Higgins, risk factors for AF are underappreciated in the United States and elsewhere, and primary care doctors need to be aware of them. “We should try to identify these risk factors and do primary prevention to improve risk factors to reduce the progression to heart failure and myocardial infarction and stroke. But lifelong prevention is even better, he added. “Doing things to prevent actually getting risk factors in the first place. So a healthy lifestyle including exercise, diet, hydration, sleep, relaxation, social contact, and a little sunlight might be the long-term keys and starting them at a young age, too.”
In an accompanying editorial, Jianhua Wu, PhD, a professor of biostatistics and health data science with the Wolfson Institute of Population Health at Queen Mary University of London, and a colleague, cited the study’s robust observational research and called the analysis noteworthy for its quantification of the long-term risks of post-AF sequelae. They cautioned, however, that its grouping into two 10-year periods (2000-2010 and 2011-2020) came at the cost of losing temporal resolution. They also called out the lack of reporting on the ethnic composition of the study population, a factor that influences lifetime AF risk, and the absence of subgroup analysis by socioeconomic status, which affects incidence and outcomes.
The editorialists noted that while interventions to prevent stroke dominated AF research and guidelines during the study time period, no evidence suggests these interventions can prevent incident heart failure. “Alignment of both randomised clinical trials and guidelines to better reflect the needs of the real-world population with atrial fibrillation is necessary because further improvements to patient prognosis are likely to require a broader perspective on atrial fibrillation management beyond prevention of stroke,” they wrote.
In the meantime this study “challenges research priorities and guideline design, and raises critical questions for the research and clinical communities about how the growing burden of atrial fibrillation can be stopped,” they wrote.
This work was supported by the Danish Cardiovascular Academy, which is funded by the Novo Nordisk Foundation, and The Danish Heart Foundation. Dr. Vinter has been an advisory board member and consultant for AstraZeneca and has an institutional research grant from BMS/Pfizer unrelated to the current study. He reported personal consulting fees from BMS and Pfizer. Other coauthors disclosed research support from and/or consulting work for private industry, as well as grants from not-for-profit research-funding organizations. Dr. Higgins had no competing interest to declare. The editorial writers had no relevant financial interests to declare. Dr. Wu is supported by Barts Charity.



