User login
In Lecanemab Alzheimer Extension Study, Placebo Roll-Over Group Does Not Catch Up
DENVER — , according to a first report of 6-month OLE data.
Due to the steady disease progression observed after the switch of placebo to active therapy, the message of these data is that “early initiation of lecanemab is important,” according to Michael Irizarry, MD, the senior vice president of clinical research at Eisai Ltd, which markets lecanemab.
The 6-month OLE data along with data from a tau PET substudy were presented by Dr. Irizarry at the 2024 annual meeting of the American Academy of Neurology.
From the start of the OLE through the 6-month follow-up, the downward trajectory of cognitive function, as measured with the Clinical Dementia Rating – Sum of Boxes (CDR-SB), has been parallel for the lecanemab-start and switch arms. As a result, the degree of separation between active and placebo groups over the course of the OLE has remained unchanged from the end of the randomized trial.
This does not rule out any benefit in the switch arm, according to Dr. Irizarry. Although there was no discernible change in the trajectory of decline among placebo patients after they were switched to lecanemab, Dr. Irizarry postulated that this might overlook the greater likely decline over time with no treatment.
“There was no placebo group in the OLE to compare with those on active treatment,” he pointed out. He then juxtaposed data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Over the same 6-month timeframe, these data show a hypothetical separation of the curves if no treatment had been received.
The 6-month OLE data provide a preliminary look at outcomes in a planned 4-year follow-up. At the end of the randomized CLARITY trial, the mean decline from the baseline CDR-SB score of 3.2, was 1.21 in the lecanemab group, translating into a 38% decline, and 1.66 in the placebo group, translating into about a 50% decline. Over the 6 months of OLE, there has been a further mean CDR-SB reduction of approximately 0.6 in both arms, suggesting a further 18% decline from baseline.
Additional Data
In the pivotal CLARITY trial, which was published a few months prior to regulatory approval early last year, 1785 patients were randomized to 10 mg/kg lecanemab or placebo infused every 2 weeks. At the end of 18 months, the superiority of lecanemab for the primary endpoint of adverse change in CDR-SB was highly significant (P < .001) as were the differences in key secondary endpoints, such as Alzheimer’s Disease Composite Score (P < .001).
Of those who participated in CLARITY, 1385 patients entered the OLE. Placebo patients were switched to lecanemab which is being maintained in all patients on the trial schedule of 10 mg/kg administered by intravenous infusion every 2 weeks.
In addition to the overall OLE 6-month data, which has not raised any new safety signals, Dr. Irizarry provided a new look at the PET TAU substudy with a focus on patients who entered the study with a low relative tau burden. Of the three classifications, which also included medium and high tau, as measured with positron-emission tomography (PET), the low tau group represented 41.2% of the 342 tau PET substudy participants. With only 2.9% entering the study with a high tau burden, almost all the others fell in the medium stratification.
Due to the potential for a lower therapeutic response, “patients with low Tau are often excluded from trials,” Dr. Irizarry said. But the sizable proportion of low tau patients has permitted an assessment of relative response with lecanemab, which turned out to be substantial.
“Consistent rates of clinical stability or improvements were observed regardless of baseline tau levels with the highest rates of improvements observed for the low tau group after 24 months of follow-up,” Dr. Irizarry reported.
In previously reported results from the tau PET substudy, lecanemab was shown to slow tau spread at least numerically in every section of the brain evaluated, including the frontal, cingulate, parietal, and whole cortical gray matter areas. The reductions reached significance for the medial temporal (P = .0024), meta temporal (P = .012), and temporal (P = .16) portions.
When most recently evaluated in the OLE, the CDR-SB score declined 38% less among those treated with lecanemab than those treated with placebo in the subgroup enrolled in the tau PET substudy.
Relative to those with intermediate or high tau, patients in the low tau had an even greater reduction in cognitive decline than those with higher tau burdens. Although Dr. Irizarry cautioned that greater baseline CDR-SB scores exaggerated the treatment effect in the low tau group, the message is that “a lecanemab treatment effect is seen even when baseline tau levels are low.”
Now, with the recent market withdrawal of aducanumab, another anti-amyloid monoclonal antibody that was previously approved for Alzheimer’s disease, lecanemab is the only therapy currently available for the goal of changing disease progression, not just modifying symptoms.
Looking Long Term
Both sets of data provide important messages for clinicians, according to Marcelo Matiello, MD, a physician investigator at Mass General Hospital and associate professor of neurology at Harvard Medical School, Boston.
“Clinicians are really looking for more data because this remains a relatively new drug,” he said. Both sets of findings presented by Dr. Irizarry “look good but the follow-up is still short, so I think everyone is still looking closely at long-term safety and efficacy.”
The need for continuous indefinite therapy is one concern that Dr. Matiello expressed. As moderator of the session in which these data were presented, Dr. Matiello specifically asked Dr. Irizarry if there are plans to explore whether periods without treatment might be a means to reduce the cost and burden of frequent infusions while preserving cognitive gains.
In response, Dr. Irizarry said that earlier studies showed rapid progression when lecanemab was stopped. On this basis, he thinks therapy must be maintained, but he did say that there are plans to look at less frequent dosing, such as once per month. He also said that a subcutaneous formulation in development might also reduce the burden of prolonged treatment.
Dr. Irizarry is an employee of Eisai Ltd., which manufacturers lecanemab. Dr. Matiello reports no potential conflicts of interest.
DENVER — , according to a first report of 6-month OLE data.
Due to the steady disease progression observed after the switch of placebo to active therapy, the message of these data is that “early initiation of lecanemab is important,” according to Michael Irizarry, MD, the senior vice president of clinical research at Eisai Ltd, which markets lecanemab.
The 6-month OLE data along with data from a tau PET substudy were presented by Dr. Irizarry at the 2024 annual meeting of the American Academy of Neurology.
From the start of the OLE through the 6-month follow-up, the downward trajectory of cognitive function, as measured with the Clinical Dementia Rating – Sum of Boxes (CDR-SB), has been parallel for the lecanemab-start and switch arms. As a result, the degree of separation between active and placebo groups over the course of the OLE has remained unchanged from the end of the randomized trial.
This does not rule out any benefit in the switch arm, according to Dr. Irizarry. Although there was no discernible change in the trajectory of decline among placebo patients after they were switched to lecanemab, Dr. Irizarry postulated that this might overlook the greater likely decline over time with no treatment.
“There was no placebo group in the OLE to compare with those on active treatment,” he pointed out. He then juxtaposed data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Over the same 6-month timeframe, these data show a hypothetical separation of the curves if no treatment had been received.
The 6-month OLE data provide a preliminary look at outcomes in a planned 4-year follow-up. At the end of the randomized CLARITY trial, the mean decline from the baseline CDR-SB score of 3.2, was 1.21 in the lecanemab group, translating into a 38% decline, and 1.66 in the placebo group, translating into about a 50% decline. Over the 6 months of OLE, there has been a further mean CDR-SB reduction of approximately 0.6 in both arms, suggesting a further 18% decline from baseline.
Additional Data
In the pivotal CLARITY trial, which was published a few months prior to regulatory approval early last year, 1785 patients were randomized to 10 mg/kg lecanemab or placebo infused every 2 weeks. At the end of 18 months, the superiority of lecanemab for the primary endpoint of adverse change in CDR-SB was highly significant (P < .001) as were the differences in key secondary endpoints, such as Alzheimer’s Disease Composite Score (P < .001).
Of those who participated in CLARITY, 1385 patients entered the OLE. Placebo patients were switched to lecanemab which is being maintained in all patients on the trial schedule of 10 mg/kg administered by intravenous infusion every 2 weeks.
In addition to the overall OLE 6-month data, which has not raised any new safety signals, Dr. Irizarry provided a new look at the PET TAU substudy with a focus on patients who entered the study with a low relative tau burden. Of the three classifications, which also included medium and high tau, as measured with positron-emission tomography (PET), the low tau group represented 41.2% of the 342 tau PET substudy participants. With only 2.9% entering the study with a high tau burden, almost all the others fell in the medium stratification.
Due to the potential for a lower therapeutic response, “patients with low Tau are often excluded from trials,” Dr. Irizarry said. But the sizable proportion of low tau patients has permitted an assessment of relative response with lecanemab, which turned out to be substantial.
“Consistent rates of clinical stability or improvements were observed regardless of baseline tau levels with the highest rates of improvements observed for the low tau group after 24 months of follow-up,” Dr. Irizarry reported.
In previously reported results from the tau PET substudy, lecanemab was shown to slow tau spread at least numerically in every section of the brain evaluated, including the frontal, cingulate, parietal, and whole cortical gray matter areas. The reductions reached significance for the medial temporal (P = .0024), meta temporal (P = .012), and temporal (P = .16) portions.
When most recently evaluated in the OLE, the CDR-SB score declined 38% less among those treated with lecanemab than those treated with placebo in the subgroup enrolled in the tau PET substudy.
Relative to those with intermediate or high tau, patients in the low tau had an even greater reduction in cognitive decline than those with higher tau burdens. Although Dr. Irizarry cautioned that greater baseline CDR-SB scores exaggerated the treatment effect in the low tau group, the message is that “a lecanemab treatment effect is seen even when baseline tau levels are low.”
Now, with the recent market withdrawal of aducanumab, another anti-amyloid monoclonal antibody that was previously approved for Alzheimer’s disease, lecanemab is the only therapy currently available for the goal of changing disease progression, not just modifying symptoms.
Looking Long Term
Both sets of data provide important messages for clinicians, according to Marcelo Matiello, MD, a physician investigator at Mass General Hospital and associate professor of neurology at Harvard Medical School, Boston.
“Clinicians are really looking for more data because this remains a relatively new drug,” he said. Both sets of findings presented by Dr. Irizarry “look good but the follow-up is still short, so I think everyone is still looking closely at long-term safety and efficacy.”
The need for continuous indefinite therapy is one concern that Dr. Matiello expressed. As moderator of the session in which these data were presented, Dr. Matiello specifically asked Dr. Irizarry if there are plans to explore whether periods without treatment might be a means to reduce the cost and burden of frequent infusions while preserving cognitive gains.
In response, Dr. Irizarry said that earlier studies showed rapid progression when lecanemab was stopped. On this basis, he thinks therapy must be maintained, but he did say that there are plans to look at less frequent dosing, such as once per month. He also said that a subcutaneous formulation in development might also reduce the burden of prolonged treatment.
Dr. Irizarry is an employee of Eisai Ltd., which manufacturers lecanemab. Dr. Matiello reports no potential conflicts of interest.
DENVER — , according to a first report of 6-month OLE data.
Due to the steady disease progression observed after the switch of placebo to active therapy, the message of these data is that “early initiation of lecanemab is important,” according to Michael Irizarry, MD, the senior vice president of clinical research at Eisai Ltd, which markets lecanemab.
The 6-month OLE data along with data from a tau PET substudy were presented by Dr. Irizarry at the 2024 annual meeting of the American Academy of Neurology.
From the start of the OLE through the 6-month follow-up, the downward trajectory of cognitive function, as measured with the Clinical Dementia Rating – Sum of Boxes (CDR-SB), has been parallel for the lecanemab-start and switch arms. As a result, the degree of separation between active and placebo groups over the course of the OLE has remained unchanged from the end of the randomized trial.
This does not rule out any benefit in the switch arm, according to Dr. Irizarry. Although there was no discernible change in the trajectory of decline among placebo patients after they were switched to lecanemab, Dr. Irizarry postulated that this might overlook the greater likely decline over time with no treatment.
“There was no placebo group in the OLE to compare with those on active treatment,” he pointed out. He then juxtaposed data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Over the same 6-month timeframe, these data show a hypothetical separation of the curves if no treatment had been received.
The 6-month OLE data provide a preliminary look at outcomes in a planned 4-year follow-up. At the end of the randomized CLARITY trial, the mean decline from the baseline CDR-SB score of 3.2, was 1.21 in the lecanemab group, translating into a 38% decline, and 1.66 in the placebo group, translating into about a 50% decline. Over the 6 months of OLE, there has been a further mean CDR-SB reduction of approximately 0.6 in both arms, suggesting a further 18% decline from baseline.
Additional Data
In the pivotal CLARITY trial, which was published a few months prior to regulatory approval early last year, 1785 patients were randomized to 10 mg/kg lecanemab or placebo infused every 2 weeks. At the end of 18 months, the superiority of lecanemab for the primary endpoint of adverse change in CDR-SB was highly significant (P < .001) as were the differences in key secondary endpoints, such as Alzheimer’s Disease Composite Score (P < .001).
Of those who participated in CLARITY, 1385 patients entered the OLE. Placebo patients were switched to lecanemab which is being maintained in all patients on the trial schedule of 10 mg/kg administered by intravenous infusion every 2 weeks.
In addition to the overall OLE 6-month data, which has not raised any new safety signals, Dr. Irizarry provided a new look at the PET TAU substudy with a focus on patients who entered the study with a low relative tau burden. Of the three classifications, which also included medium and high tau, as measured with positron-emission tomography (PET), the low tau group represented 41.2% of the 342 tau PET substudy participants. With only 2.9% entering the study with a high tau burden, almost all the others fell in the medium stratification.
Due to the potential for a lower therapeutic response, “patients with low Tau are often excluded from trials,” Dr. Irizarry said. But the sizable proportion of low tau patients has permitted an assessment of relative response with lecanemab, which turned out to be substantial.
“Consistent rates of clinical stability or improvements were observed regardless of baseline tau levels with the highest rates of improvements observed for the low tau group after 24 months of follow-up,” Dr. Irizarry reported.
In previously reported results from the tau PET substudy, lecanemab was shown to slow tau spread at least numerically in every section of the brain evaluated, including the frontal, cingulate, parietal, and whole cortical gray matter areas. The reductions reached significance for the medial temporal (P = .0024), meta temporal (P = .012), and temporal (P = .16) portions.
When most recently evaluated in the OLE, the CDR-SB score declined 38% less among those treated with lecanemab than those treated with placebo in the subgroup enrolled in the tau PET substudy.
Relative to those with intermediate or high tau, patients in the low tau had an even greater reduction in cognitive decline than those with higher tau burdens. Although Dr. Irizarry cautioned that greater baseline CDR-SB scores exaggerated the treatment effect in the low tau group, the message is that “a lecanemab treatment effect is seen even when baseline tau levels are low.”
Now, with the recent market withdrawal of aducanumab, another anti-amyloid monoclonal antibody that was previously approved for Alzheimer’s disease, lecanemab is the only therapy currently available for the goal of changing disease progression, not just modifying symptoms.
Looking Long Term
Both sets of data provide important messages for clinicians, according to Marcelo Matiello, MD, a physician investigator at Mass General Hospital and associate professor of neurology at Harvard Medical School, Boston.
“Clinicians are really looking for more data because this remains a relatively new drug,” he said. Both sets of findings presented by Dr. Irizarry “look good but the follow-up is still short, so I think everyone is still looking closely at long-term safety and efficacy.”
The need for continuous indefinite therapy is one concern that Dr. Matiello expressed. As moderator of the session in which these data were presented, Dr. Matiello specifically asked Dr. Irizarry if there are plans to explore whether periods without treatment might be a means to reduce the cost and burden of frequent infusions while preserving cognitive gains.
In response, Dr. Irizarry said that earlier studies showed rapid progression when lecanemab was stopped. On this basis, he thinks therapy must be maintained, but he did say that there are plans to look at less frequent dosing, such as once per month. He also said that a subcutaneous formulation in development might also reduce the burden of prolonged treatment.
Dr. Irizarry is an employee of Eisai Ltd., which manufacturers lecanemab. Dr. Matiello reports no potential conflicts of interest.
FROM AAN 2024
Salt Substitutes May Cut All-Cause And Cardiovascular Mortality
Large-scale salt substitution holds promise for reducing mortality with no elevated risk of serious harms, especially for older people at increased cardiovascular disease (CVD) risk, a systematic review and meta-analysis by Australian researchers suggested.
The study, published in Annals of Internal Medicine, adds more evidence that broad adoption of potassium-rich salt substitutes for food preparation could have a significant effect on population health.
Although the supporting evidence was of low certainty, the analysis of 16 international randomized controlled trials of various interventions with 35,321 participants found salt substitution to be associated with an absolute reduction of 5 in 1000 in all-cause mortality (confidence interval, –3 to –7) and 3 in 1000 in CVD mortality (CI, –1 to –5).
Led by Hannah Greenwood, BPsychSc, a cardiovascular researcher at the Institute for Evidence-Based Healthcare at Bond University in Gold Coast, Queensland, the investigators also found very low certainty evidence of an absolute reduction of 8 in 1000 in major adverse cardiovascular events (CI, 0 to –15), with a 1 in 1000 decrease in more serious adverse events (CI, 4 to –2) in the same population.
Seven of the 16 studies were conducted in China and Taiwan and seven were conducted in populations of older age (mean age 62 years) and/or at higher cardiovascular risk.
With most of the data deriving from populations of older age at higher-than-average CV risk and/or eating an Asian diet, the findings’ generalizability to populations following a Western diet and/or at average CVD risk is limited, the researchers acknowledged.
“We are less certain about the effects in Western, younger, and healthy population groups,” corresponding author Loai Albarqouni, MD, MSc, PhD, assistant professor at the Institute for Evidence-Based Healthcare, said in an interview. “While we saw small, clinically meaningful reductions in cardiovascular deaths and events, effectiveness should be better established before salt substitutes are recommended more broadly, though they are promising.”
In addition, he said, since the longest follow-up of substitute use was 10 years, “we can’t speak to benefits or harms beyond this time frame.”
Still, recommending salt substitutes may be an effective way for physicians to help patients reduce CVD risk, especially those hesitant to start medication, he said. “But physicians should take into account individual circumstances and other factors like kidney disease before recommending salt substitutes. Other non-drug methods of reducing cardiovascular risk, such as diet or exercise, may also be considered.”
Dr. Albarqouni stressed that sodium intake is not the only driver of CVD and reducing intake is just one piece of the puzzle. He cautioned that substitutes themselves can contain high levels of sodium, “so if people are using them in large volumes, they may still present similar risks to the sodium in regular salt.”
While the substitutes appear safe as evidenced by low incidence of hyperkalemia or renal dysfunction, the evidence is scarce, heterogeneous, and weak, the authors stressed.
“They can pose a health risk among people who have kidney disease, diabetes, and heart failure or who take certain medications, including ACE inhibitors and potassium-sparing diuretics,” said Emma Laing, PhD, RDN, director of dietetics at the University of Georgia in Athens. And while their salty flavor makes these a reasonable alternate to sodium chloride, “the downsides include a higher cost and bitter or metallic taste in high amounts. These salt substitutes tend to be better accepted by patients if they contain less than 30% potassium chloride.”
She noted that flavorful salt-free spices, herbs, lemon and lime juices, and vinegars can be effective in lowering dietary sodium when used in lieu of cooking salt.
In similar findings, a recent Chinese study of elderly normotensive people in residential care facilities observed a decrease in the incidence of hypertension with salt substitution.
Approximately one-third of otherwise health individuals are salt-sensitive, rising to more than 50% those with hypertension, and excessive salt intake is estimated to be responsible for nearly 5 million deaths per year globally.
How much impact could household food preparation with salt substitutes really have in North America where sodium consumption is largely driven by processed and takeout food? “While someone may make the switch to a salt substitute for home cooking, their sodium intake might still be very high if a lot of processed or takeaway foods are eaten,” Dr. Albarqouni said. “To see large population impacts, we will likely need policy and institutional-level change as to how sodium is used in food processing, alongside individuals’ switching from regular salt to salt substitutes.”
In agreement, an accompanying editorial by researchers from the universities of Sydney, New South Wales, and California, San Diego, noted the failure of governments and industry to address the World Health Organization’s call for a 30% reduction in global sodium consumption by 2025. With hypertension a major global health burden, the editorialists, led by J. Jaime Miranda, MD, MSc, PhD, of the Sydney School of Public Health at the University of Sydney, believe salt substitutes could be an accessible path toward that goal for food production companies.
“Although the benefits of reducing salt intake have been known for decades, little progress has been made in the quest to lower salt intake on the industry and commercial fronts with existing regulatory tools,” they wrote. “Consequently, we must turn our attention to effective evidence-based alternatives, such as the use of potassium-enriched salts.”
Given the high rates of nonadherence to antihypertensive medication, nonpharmacologic measures to improve blood pressure control are required, they added. “Expanding the routine use of potassium-enriched salts across households and the food industry would benefit not only persons with existing hypertension but all members of the household and communities. An entire shift of the population’s blood pressure curve is possible.”
The study authors called for research to determine the cost-effectiveness of salt substitution in older Asian populations and its efficacy in groups at average cardiovascular risk or following a Western diet.
This research was supported by the National Health and Medical Research Council of Australia and an Australian Government Research Training Program Scholarship. Coauthor Dr. Lauren Ball disclosed support from the National Health and Medical Research Council of Australia. Ms. Hannah Greenwood received support from the Australian government and Bond University. Dr. Miranda disclosed numerous consulting, advisory, and research-funding relationships with government, academic, philanthropic, and nonprofit organizations. Editorial commentator Dr. Kathy Trieu reported research support from multiple government and non-profit research-funding organizations. Dr. Cheryl Anderson disclosed ties to Weight Watchers and the McCormick Science Institute, as well support from numerous government, academic, and nonprofit research-funding agencies.
Large-scale salt substitution holds promise for reducing mortality with no elevated risk of serious harms, especially for older people at increased cardiovascular disease (CVD) risk, a systematic review and meta-analysis by Australian researchers suggested.
The study, published in Annals of Internal Medicine, adds more evidence that broad adoption of potassium-rich salt substitutes for food preparation could have a significant effect on population health.
Although the supporting evidence was of low certainty, the analysis of 16 international randomized controlled trials of various interventions with 35,321 participants found salt substitution to be associated with an absolute reduction of 5 in 1000 in all-cause mortality (confidence interval, –3 to –7) and 3 in 1000 in CVD mortality (CI, –1 to –5).
Led by Hannah Greenwood, BPsychSc, a cardiovascular researcher at the Institute for Evidence-Based Healthcare at Bond University in Gold Coast, Queensland, the investigators also found very low certainty evidence of an absolute reduction of 8 in 1000 in major adverse cardiovascular events (CI, 0 to –15), with a 1 in 1000 decrease in more serious adverse events (CI, 4 to –2) in the same population.
Seven of the 16 studies were conducted in China and Taiwan and seven were conducted in populations of older age (mean age 62 years) and/or at higher cardiovascular risk.
With most of the data deriving from populations of older age at higher-than-average CV risk and/or eating an Asian diet, the findings’ generalizability to populations following a Western diet and/or at average CVD risk is limited, the researchers acknowledged.
“We are less certain about the effects in Western, younger, and healthy population groups,” corresponding author Loai Albarqouni, MD, MSc, PhD, assistant professor at the Institute for Evidence-Based Healthcare, said in an interview. “While we saw small, clinically meaningful reductions in cardiovascular deaths and events, effectiveness should be better established before salt substitutes are recommended more broadly, though they are promising.”
In addition, he said, since the longest follow-up of substitute use was 10 years, “we can’t speak to benefits or harms beyond this time frame.”
Still, recommending salt substitutes may be an effective way for physicians to help patients reduce CVD risk, especially those hesitant to start medication, he said. “But physicians should take into account individual circumstances and other factors like kidney disease before recommending salt substitutes. Other non-drug methods of reducing cardiovascular risk, such as diet or exercise, may also be considered.”
Dr. Albarqouni stressed that sodium intake is not the only driver of CVD and reducing intake is just one piece of the puzzle. He cautioned that substitutes themselves can contain high levels of sodium, “so if people are using them in large volumes, they may still present similar risks to the sodium in regular salt.”
While the substitutes appear safe as evidenced by low incidence of hyperkalemia or renal dysfunction, the evidence is scarce, heterogeneous, and weak, the authors stressed.
“They can pose a health risk among people who have kidney disease, diabetes, and heart failure or who take certain medications, including ACE inhibitors and potassium-sparing diuretics,” said Emma Laing, PhD, RDN, director of dietetics at the University of Georgia in Athens. And while their salty flavor makes these a reasonable alternate to sodium chloride, “the downsides include a higher cost and bitter or metallic taste in high amounts. These salt substitutes tend to be better accepted by patients if they contain less than 30% potassium chloride.”
She noted that flavorful salt-free spices, herbs, lemon and lime juices, and vinegars can be effective in lowering dietary sodium when used in lieu of cooking salt.
In similar findings, a recent Chinese study of elderly normotensive people in residential care facilities observed a decrease in the incidence of hypertension with salt substitution.
Approximately one-third of otherwise health individuals are salt-sensitive, rising to more than 50% those with hypertension, and excessive salt intake is estimated to be responsible for nearly 5 million deaths per year globally.
How much impact could household food preparation with salt substitutes really have in North America where sodium consumption is largely driven by processed and takeout food? “While someone may make the switch to a salt substitute for home cooking, their sodium intake might still be very high if a lot of processed or takeaway foods are eaten,” Dr. Albarqouni said. “To see large population impacts, we will likely need policy and institutional-level change as to how sodium is used in food processing, alongside individuals’ switching from regular salt to salt substitutes.”
In agreement, an accompanying editorial by researchers from the universities of Sydney, New South Wales, and California, San Diego, noted the failure of governments and industry to address the World Health Organization’s call for a 30% reduction in global sodium consumption by 2025. With hypertension a major global health burden, the editorialists, led by J. Jaime Miranda, MD, MSc, PhD, of the Sydney School of Public Health at the University of Sydney, believe salt substitutes could be an accessible path toward that goal for food production companies.
“Although the benefits of reducing salt intake have been known for decades, little progress has been made in the quest to lower salt intake on the industry and commercial fronts with existing regulatory tools,” they wrote. “Consequently, we must turn our attention to effective evidence-based alternatives, such as the use of potassium-enriched salts.”
Given the high rates of nonadherence to antihypertensive medication, nonpharmacologic measures to improve blood pressure control are required, they added. “Expanding the routine use of potassium-enriched salts across households and the food industry would benefit not only persons with existing hypertension but all members of the household and communities. An entire shift of the population’s blood pressure curve is possible.”
The study authors called for research to determine the cost-effectiveness of salt substitution in older Asian populations and its efficacy in groups at average cardiovascular risk or following a Western diet.
This research was supported by the National Health and Medical Research Council of Australia and an Australian Government Research Training Program Scholarship. Coauthor Dr. Lauren Ball disclosed support from the National Health and Medical Research Council of Australia. Ms. Hannah Greenwood received support from the Australian government and Bond University. Dr. Miranda disclosed numerous consulting, advisory, and research-funding relationships with government, academic, philanthropic, and nonprofit organizations. Editorial commentator Dr. Kathy Trieu reported research support from multiple government and non-profit research-funding organizations. Dr. Cheryl Anderson disclosed ties to Weight Watchers and the McCormick Science Institute, as well support from numerous government, academic, and nonprofit research-funding agencies.
Large-scale salt substitution holds promise for reducing mortality with no elevated risk of serious harms, especially for older people at increased cardiovascular disease (CVD) risk, a systematic review and meta-analysis by Australian researchers suggested.
The study, published in Annals of Internal Medicine, adds more evidence that broad adoption of potassium-rich salt substitutes for food preparation could have a significant effect on population health.
Although the supporting evidence was of low certainty, the analysis of 16 international randomized controlled trials of various interventions with 35,321 participants found salt substitution to be associated with an absolute reduction of 5 in 1000 in all-cause mortality (confidence interval, –3 to –7) and 3 in 1000 in CVD mortality (CI, –1 to –5).
Led by Hannah Greenwood, BPsychSc, a cardiovascular researcher at the Institute for Evidence-Based Healthcare at Bond University in Gold Coast, Queensland, the investigators also found very low certainty evidence of an absolute reduction of 8 in 1000 in major adverse cardiovascular events (CI, 0 to –15), with a 1 in 1000 decrease in more serious adverse events (CI, 4 to –2) in the same population.
Seven of the 16 studies were conducted in China and Taiwan and seven were conducted in populations of older age (mean age 62 years) and/or at higher cardiovascular risk.
With most of the data deriving from populations of older age at higher-than-average CV risk and/or eating an Asian diet, the findings’ generalizability to populations following a Western diet and/or at average CVD risk is limited, the researchers acknowledged.
“We are less certain about the effects in Western, younger, and healthy population groups,” corresponding author Loai Albarqouni, MD, MSc, PhD, assistant professor at the Institute for Evidence-Based Healthcare, said in an interview. “While we saw small, clinically meaningful reductions in cardiovascular deaths and events, effectiveness should be better established before salt substitutes are recommended more broadly, though they are promising.”
In addition, he said, since the longest follow-up of substitute use was 10 years, “we can’t speak to benefits or harms beyond this time frame.”
Still, recommending salt substitutes may be an effective way for physicians to help patients reduce CVD risk, especially those hesitant to start medication, he said. “But physicians should take into account individual circumstances and other factors like kidney disease before recommending salt substitutes. Other non-drug methods of reducing cardiovascular risk, such as diet or exercise, may also be considered.”
Dr. Albarqouni stressed that sodium intake is not the only driver of CVD and reducing intake is just one piece of the puzzle. He cautioned that substitutes themselves can contain high levels of sodium, “so if people are using them in large volumes, they may still present similar risks to the sodium in regular salt.”
While the substitutes appear safe as evidenced by low incidence of hyperkalemia or renal dysfunction, the evidence is scarce, heterogeneous, and weak, the authors stressed.
“They can pose a health risk among people who have kidney disease, diabetes, and heart failure or who take certain medications, including ACE inhibitors and potassium-sparing diuretics,” said Emma Laing, PhD, RDN, director of dietetics at the University of Georgia in Athens. And while their salty flavor makes these a reasonable alternate to sodium chloride, “the downsides include a higher cost and bitter or metallic taste in high amounts. These salt substitutes tend to be better accepted by patients if they contain less than 30% potassium chloride.”
She noted that flavorful salt-free spices, herbs, lemon and lime juices, and vinegars can be effective in lowering dietary sodium when used in lieu of cooking salt.
In similar findings, a recent Chinese study of elderly normotensive people in residential care facilities observed a decrease in the incidence of hypertension with salt substitution.
Approximately one-third of otherwise health individuals are salt-sensitive, rising to more than 50% those with hypertension, and excessive salt intake is estimated to be responsible for nearly 5 million deaths per year globally.
How much impact could household food preparation with salt substitutes really have in North America where sodium consumption is largely driven by processed and takeout food? “While someone may make the switch to a salt substitute for home cooking, their sodium intake might still be very high if a lot of processed or takeaway foods are eaten,” Dr. Albarqouni said. “To see large population impacts, we will likely need policy and institutional-level change as to how sodium is used in food processing, alongside individuals’ switching from regular salt to salt substitutes.”
In agreement, an accompanying editorial by researchers from the universities of Sydney, New South Wales, and California, San Diego, noted the failure of governments and industry to address the World Health Organization’s call for a 30% reduction in global sodium consumption by 2025. With hypertension a major global health burden, the editorialists, led by J. Jaime Miranda, MD, MSc, PhD, of the Sydney School of Public Health at the University of Sydney, believe salt substitutes could be an accessible path toward that goal for food production companies.
“Although the benefits of reducing salt intake have been known for decades, little progress has been made in the quest to lower salt intake on the industry and commercial fronts with existing regulatory tools,” they wrote. “Consequently, we must turn our attention to effective evidence-based alternatives, such as the use of potassium-enriched salts.”
Given the high rates of nonadherence to antihypertensive medication, nonpharmacologic measures to improve blood pressure control are required, they added. “Expanding the routine use of potassium-enriched salts across households and the food industry would benefit not only persons with existing hypertension but all members of the household and communities. An entire shift of the population’s blood pressure curve is possible.”
The study authors called for research to determine the cost-effectiveness of salt substitution in older Asian populations and its efficacy in groups at average cardiovascular risk or following a Western diet.
This research was supported by the National Health and Medical Research Council of Australia and an Australian Government Research Training Program Scholarship. Coauthor Dr. Lauren Ball disclosed support from the National Health and Medical Research Council of Australia. Ms. Hannah Greenwood received support from the Australian government and Bond University. Dr. Miranda disclosed numerous consulting, advisory, and research-funding relationships with government, academic, philanthropic, and nonprofit organizations. Editorial commentator Dr. Kathy Trieu reported research support from multiple government and non-profit research-funding organizations. Dr. Cheryl Anderson disclosed ties to Weight Watchers and the McCormick Science Institute, as well support from numerous government, academic, and nonprofit research-funding agencies.
FROM ANNALS OF INTERNAL MEDICINE
Hormone Therapy After 65 a Good Option for Most Women
Hormone Therapy (HT) is a good option for most women over age 65, despite entrenched fears about HT safety, according to findings from a new study published in Menopause.
The study, led by Seo H. Baik, PhD, of Lister Hill National Center for Biomedical Communications, National Library of Medicine, in Bethesda, Maryland, and colleagues is based on the health records of 10 million senior women on Medicare from 2007 to 2020. It concludes there are important health benefits with HT beyond age 65 and the effects of using HT after age 65 vary by type of therapy, route of administration, and dose.
Controversial Since Women’s Health Initiative
Use of HT after age 65 has been controversial in light of the findings of the Women’s Health Initiative (WHI) study in 2002. Since that study, many women have decided against HT, especially after age 65, because of fears of increased risks for cancers and heart disease.
Baik et al. concluded that, compared with never using or stopping use of HT before the age of 65 years, the use of estrogen alone beyond age 65 years was associated with the following significant risk reductions: mortality (19%); breast cancer (16%); lung cancer (13%); colorectal cancer (12%); congestive heart failure (5%); venous thromboembolism (5%); atrial fibrillation (4%); acute myocardial infarction (11%); and dementia (2%).
The authors further found that estrogen plus progestin was associated with significant risk reductions in endometrial cancer (45%); ovarian cancer (21%); ischemic heart disease (5%); congestive heart failure (5%); and venous thromboembolism (5%).
Estrogen plus progesterone, however, was linked with risk reduction only in congestive heart failure (4%).
Reassuring Results
“These results should provide additional reassurance to women about hormone therapy,” said Lisa C, Larkin, MD, president of The Menopause Society. “This data is largely consistent with the WHI data as we understand it today — that for the majority of women with symptoms transitioning through menopause, hormone therapy is the most effective treatment and has benefits that outweigh risks.”
There may be some exceptions, she noted, particularly in older women with high risk for cardiovascular disease and stroke. Among those women, she explained, the risks of HT may outweigh the benefits and it may be appropriate to stop hormone therapy.
“In these older women with specific risk factors, the discussion of continuing or stopping HT is nuanced and complex and must involve shared decision-making,” she said.
Elevated Breast Cancer Risk Can be Mitigated
With a therapy combining estrogen and progestogen, both estrogen plus progestin and estrogen plus progesterone were associated with a 10%-19% increased risk of breast cancer, but the authors say that risk can be mitigated using low doses of transdermal or vaginal estrogen plus progestin.
“In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (estradiol) rather than conjugated estrogen,” the authors write.
The authors report that over 14 years of follow-up (from 2007 to 2020), the proportion of senior women taking any HT-containing estrogen dropped by half, from 11.4% to 5.5%. E2 has largely replaced conjugated estrogen (CEE); and vaginal administration largely replaced oral.
Controversy Remains
Even with these results, hormone use will remain controversial, Dr. Larkin said, without enormous efforts to educate. Menopausal HT therapy in young 50-year-old women having symptoms is still controversial — despite the large body of evidence supporting safety and benefit in the majority of women, she said.
“For the last 25 years we have completely neglected education of clinicians about menopause and the data on hormone therapy,” she said. “As a result, most of the clinicians practicing do not understand the data and remain very negative about hormones even in younger women. The decades of lack of education of clinicians about menopause is one of the major reasons far too many young, healthy, 50-year-old women with symptoms are not getting the care they need [hormone therapy] at menopause.” Instead, she says, women are told to take supplements because some providers think hormone therapy is too dangerous.
Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine, and founding director of the Northwestern Medical Center for Sexual Medicine and Menopause, both in Chicago, says, “In the WHI, 70% of the women were over the age of 65 when they initiated therapy, which partially accounts for the negative outcomes. In addition, in WHI, everyone was taking oral [HT]. This (current) data is very reassuring — and validating — for women who would like to continue taking HT.”
Dr. Streicher says women who would like to start HT after 65 should be counseled on individual risks and after cardiac health is evaluated. But, she notes, this study did not address that.
‘Best Time to Stop HT is When You Die’
She says in her practice she will counsel women who are on HT and would like to continue after age 65 the way she always has: “If someone is taking HT and has no specific reason to stop, there is no reason to stop at some arbitrary age or time and that if they do, they will lose many of the benefits,” particularly bone, cognitive, cardiovascular, and vulvovaginal benefits, she explained. “The best time to stop HT is when you die,” Dr. Streicher said, “And, given the reduction in mortality in women who take HT, that will be at a much older age than women who don’t take HT.”
So will these new data be convincing?
“It will convince the already convinced — menopause experts who follow the data. It is the rare menopause expert that tells women to stop HT,” Dr. Streicher said.
However, she said, “The overwhelming majority of clinicians in the US currently do not prescribe HT. Sadly, I don’t think this will change much.”
The authors report no relevant financial relationships. Dr. Larkin consults for several women’s health companies including Mayne Pharma, Astellas, Johnson & Johnson, Grail, Pfizer, and Solv Wellness. Dr. Streicher reports no relevant financial relationships.
Hormone Therapy (HT) is a good option for most women over age 65, despite entrenched fears about HT safety, according to findings from a new study published in Menopause.
The study, led by Seo H. Baik, PhD, of Lister Hill National Center for Biomedical Communications, National Library of Medicine, in Bethesda, Maryland, and colleagues is based on the health records of 10 million senior women on Medicare from 2007 to 2020. It concludes there are important health benefits with HT beyond age 65 and the effects of using HT after age 65 vary by type of therapy, route of administration, and dose.
Controversial Since Women’s Health Initiative
Use of HT after age 65 has been controversial in light of the findings of the Women’s Health Initiative (WHI) study in 2002. Since that study, many women have decided against HT, especially after age 65, because of fears of increased risks for cancers and heart disease.
Baik et al. concluded that, compared with never using or stopping use of HT before the age of 65 years, the use of estrogen alone beyond age 65 years was associated with the following significant risk reductions: mortality (19%); breast cancer (16%); lung cancer (13%); colorectal cancer (12%); congestive heart failure (5%); venous thromboembolism (5%); atrial fibrillation (4%); acute myocardial infarction (11%); and dementia (2%).
The authors further found that estrogen plus progestin was associated with significant risk reductions in endometrial cancer (45%); ovarian cancer (21%); ischemic heart disease (5%); congestive heart failure (5%); and venous thromboembolism (5%).
Estrogen plus progesterone, however, was linked with risk reduction only in congestive heart failure (4%).
Reassuring Results
“These results should provide additional reassurance to women about hormone therapy,” said Lisa C, Larkin, MD, president of The Menopause Society. “This data is largely consistent with the WHI data as we understand it today — that for the majority of women with symptoms transitioning through menopause, hormone therapy is the most effective treatment and has benefits that outweigh risks.”
There may be some exceptions, she noted, particularly in older women with high risk for cardiovascular disease and stroke. Among those women, she explained, the risks of HT may outweigh the benefits and it may be appropriate to stop hormone therapy.
“In these older women with specific risk factors, the discussion of continuing or stopping HT is nuanced and complex and must involve shared decision-making,” she said.
Elevated Breast Cancer Risk Can be Mitigated
With a therapy combining estrogen and progestogen, both estrogen plus progestin and estrogen plus progesterone were associated with a 10%-19% increased risk of breast cancer, but the authors say that risk can be mitigated using low doses of transdermal or vaginal estrogen plus progestin.
“In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (estradiol) rather than conjugated estrogen,” the authors write.
The authors report that over 14 years of follow-up (from 2007 to 2020), the proportion of senior women taking any HT-containing estrogen dropped by half, from 11.4% to 5.5%. E2 has largely replaced conjugated estrogen (CEE); and vaginal administration largely replaced oral.
Controversy Remains
Even with these results, hormone use will remain controversial, Dr. Larkin said, without enormous efforts to educate. Menopausal HT therapy in young 50-year-old women having symptoms is still controversial — despite the large body of evidence supporting safety and benefit in the majority of women, she said.
“For the last 25 years we have completely neglected education of clinicians about menopause and the data on hormone therapy,” she said. “As a result, most of the clinicians practicing do not understand the data and remain very negative about hormones even in younger women. The decades of lack of education of clinicians about menopause is one of the major reasons far too many young, healthy, 50-year-old women with symptoms are not getting the care they need [hormone therapy] at menopause.” Instead, she says, women are told to take supplements because some providers think hormone therapy is too dangerous.
Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine, and founding director of the Northwestern Medical Center for Sexual Medicine and Menopause, both in Chicago, says, “In the WHI, 70% of the women were over the age of 65 when they initiated therapy, which partially accounts for the negative outcomes. In addition, in WHI, everyone was taking oral [HT]. This (current) data is very reassuring — and validating — for women who would like to continue taking HT.”
Dr. Streicher says women who would like to start HT after 65 should be counseled on individual risks and after cardiac health is evaluated. But, she notes, this study did not address that.
‘Best Time to Stop HT is When You Die’
She says in her practice she will counsel women who are on HT and would like to continue after age 65 the way she always has: “If someone is taking HT and has no specific reason to stop, there is no reason to stop at some arbitrary age or time and that if they do, they will lose many of the benefits,” particularly bone, cognitive, cardiovascular, and vulvovaginal benefits, she explained. “The best time to stop HT is when you die,” Dr. Streicher said, “And, given the reduction in mortality in women who take HT, that will be at a much older age than women who don’t take HT.”
So will these new data be convincing?
“It will convince the already convinced — menopause experts who follow the data. It is the rare menopause expert that tells women to stop HT,” Dr. Streicher said.
However, she said, “The overwhelming majority of clinicians in the US currently do not prescribe HT. Sadly, I don’t think this will change much.”
The authors report no relevant financial relationships. Dr. Larkin consults for several women’s health companies including Mayne Pharma, Astellas, Johnson & Johnson, Grail, Pfizer, and Solv Wellness. Dr. Streicher reports no relevant financial relationships.
Hormone Therapy (HT) is a good option for most women over age 65, despite entrenched fears about HT safety, according to findings from a new study published in Menopause.
The study, led by Seo H. Baik, PhD, of Lister Hill National Center for Biomedical Communications, National Library of Medicine, in Bethesda, Maryland, and colleagues is based on the health records of 10 million senior women on Medicare from 2007 to 2020. It concludes there are important health benefits with HT beyond age 65 and the effects of using HT after age 65 vary by type of therapy, route of administration, and dose.
Controversial Since Women’s Health Initiative
Use of HT after age 65 has been controversial in light of the findings of the Women’s Health Initiative (WHI) study in 2002. Since that study, many women have decided against HT, especially after age 65, because of fears of increased risks for cancers and heart disease.
Baik et al. concluded that, compared with never using or stopping use of HT before the age of 65 years, the use of estrogen alone beyond age 65 years was associated with the following significant risk reductions: mortality (19%); breast cancer (16%); lung cancer (13%); colorectal cancer (12%); congestive heart failure (5%); venous thromboembolism (5%); atrial fibrillation (4%); acute myocardial infarction (11%); and dementia (2%).
The authors further found that estrogen plus progestin was associated with significant risk reductions in endometrial cancer (45%); ovarian cancer (21%); ischemic heart disease (5%); congestive heart failure (5%); and venous thromboembolism (5%).
Estrogen plus progesterone, however, was linked with risk reduction only in congestive heart failure (4%).
Reassuring Results
“These results should provide additional reassurance to women about hormone therapy,” said Lisa C, Larkin, MD, president of The Menopause Society. “This data is largely consistent with the WHI data as we understand it today — that for the majority of women with symptoms transitioning through menopause, hormone therapy is the most effective treatment and has benefits that outweigh risks.”
There may be some exceptions, she noted, particularly in older women with high risk for cardiovascular disease and stroke. Among those women, she explained, the risks of HT may outweigh the benefits and it may be appropriate to stop hormone therapy.
“In these older women with specific risk factors, the discussion of continuing or stopping HT is nuanced and complex and must involve shared decision-making,” she said.
Elevated Breast Cancer Risk Can be Mitigated
With a therapy combining estrogen and progestogen, both estrogen plus progestin and estrogen plus progesterone were associated with a 10%-19% increased risk of breast cancer, but the authors say that risk can be mitigated using low doses of transdermal or vaginal estrogen plus progestin.
“In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (estradiol) rather than conjugated estrogen,” the authors write.
The authors report that over 14 years of follow-up (from 2007 to 2020), the proportion of senior women taking any HT-containing estrogen dropped by half, from 11.4% to 5.5%. E2 has largely replaced conjugated estrogen (CEE); and vaginal administration largely replaced oral.
Controversy Remains
Even with these results, hormone use will remain controversial, Dr. Larkin said, without enormous efforts to educate. Menopausal HT therapy in young 50-year-old women having symptoms is still controversial — despite the large body of evidence supporting safety and benefit in the majority of women, she said.
“For the last 25 years we have completely neglected education of clinicians about menopause and the data on hormone therapy,” she said. “As a result, most of the clinicians practicing do not understand the data and remain very negative about hormones even in younger women. The decades of lack of education of clinicians about menopause is one of the major reasons far too many young, healthy, 50-year-old women with symptoms are not getting the care they need [hormone therapy] at menopause.” Instead, she says, women are told to take supplements because some providers think hormone therapy is too dangerous.
Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine, and founding director of the Northwestern Medical Center for Sexual Medicine and Menopause, both in Chicago, says, “In the WHI, 70% of the women were over the age of 65 when they initiated therapy, which partially accounts for the negative outcomes. In addition, in WHI, everyone was taking oral [HT]. This (current) data is very reassuring — and validating — for women who would like to continue taking HT.”
Dr. Streicher says women who would like to start HT after 65 should be counseled on individual risks and after cardiac health is evaluated. But, she notes, this study did not address that.
‘Best Time to Stop HT is When You Die’
She says in her practice she will counsel women who are on HT and would like to continue after age 65 the way she always has: “If someone is taking HT and has no specific reason to stop, there is no reason to stop at some arbitrary age or time and that if they do, they will lose many of the benefits,” particularly bone, cognitive, cardiovascular, and vulvovaginal benefits, she explained. “The best time to stop HT is when you die,” Dr. Streicher said, “And, given the reduction in mortality in women who take HT, that will be at a much older age than women who don’t take HT.”
So will these new data be convincing?
“It will convince the already convinced — menopause experts who follow the data. It is the rare menopause expert that tells women to stop HT,” Dr. Streicher said.
However, she said, “The overwhelming majority of clinicians in the US currently do not prescribe HT. Sadly, I don’t think this will change much.”
The authors report no relevant financial relationships. Dr. Larkin consults for several women’s health companies including Mayne Pharma, Astellas, Johnson & Johnson, Grail, Pfizer, and Solv Wellness. Dr. Streicher reports no relevant financial relationships.
FROM MENOPAUSE
Higher BMI More CVD Protective in Older Adults With T2D?
Among adults with type 2 diabetes (T2D) older than 65 years, a body mass index (BMI) in the moderate overweight category (26-28) appears to offer better protection from cardiovascular death than does a BMI in the “normal” range, new data suggested.
On the other hand, the study findings also suggest that the “normal” range of 23-25 is optimal for middle-aged adults with T2D.
The findings reflect a previously demonstrated phenomenon called the “obesity paradox,” in which older people with overweight may have better outcomes than leaner people due to factors such as bone loss, frailty, and nutritional deficits, study lead author Shaoyong Xu, of Xiangyang Central Hospital, Affiliated Hospital of Hubei University of Arts and Science, Xiangyang, China, told this news organization.
“In this era of population growth and aging, the question arises as to whether obesity or overweight can be beneficial in improving survival rates for older individuals with diabetes. This topic holds significant relevance due to the potential implications it has on weight management strategies for older adults. If overweight does not pose an increased risk of cardiovascular mortality, it may suggest that older individuals are not necessarily required to strive for weight loss to achieve so-called normal values.”
Moreover, Dr. Xu added, “inappropriate weight loss and being underweight could potentially elevate the risk of cardiovascular events, myocardial infarction, cerebral infarction, and all-cause mortality.”
Thus, he said, “while there are general guidelines recommending a BMI below 25, our findings suggest that personalized BMI targets may be more beneficial, particularly for different age groups and individuals with specific health conditions.”
Asked to comment, Ian J. Neeland, MD, director of cardiovascular prevention, University Hospitals Harrington Heart & Vascular Institute, Case Western Reserve University, Cleveland, Ohio, pointed out that older people who are underweight or in lower weight categories may be more likely to smoke or have undiagnosed cancer, or that “their BMI is not so much reflective of fat mass as of low muscle mass, or sarcopenia, and that is definitely a risk factor for adverse outcomes and risks. ... And those who have slightly higher BMIs may be maintaining muscle mass, even though they’re older, and therefore they have less risk.”
However, Dr. Neeland disagreed with the authors’ conclusions regarding “optimal” BMI. “Just because you have different risk categories based on BMI doesn’t mean that’s ‘optimal’ BMI. The way I would interpret this paper is that there’s an association of mildly overweight with better outcomes in adults who are over 65 with type 2 diabetes. We need to try to understand the mechanisms underlying that observation.”
Dr. Neeland advised that for an older person with T2D who has low muscle mass and frailty, “I wouldn’t recommend necessarily targeted weight loss in that person. But I would potentially recommend weight loss in addition to resistance training, muscle building, and endurance training, and therefore reducing fat mass. The goal would be not so much weight loss but reduction of body fat and maintaining and improving muscle health.”
U-Shaped Relationship Found Between Age, BMI, and Cardiovascular Disease (CVD) Risk
The data come from the UK Biobank, a population-based prospective cohort study of adults in the United Kingdom. A total of 22,874 participants with baseline T2D were included in the current study. Baseline surveys were conducted between 2006 and 2010, and follow-up was a median of 12.52 years. During that time, 891 people died of CVD.
Hazard ratios were adjusted for baseline variables including age, sex, smoking history, alcohol consumption, level of physical exercise, and history of CVDs.
Compared with people with BMI a < 25 in the group who were aged 65 years or younger, those with a BMI of 25.0-29.9 had a 13% higher risk for cardiovascular death. However, among those older than 65 years, a BMI between 25.0 and 29.9 was associated with an 18% lower risk.
A U-shaped relationship was found between BMI and the risk for cardiovascular death, with an optimal BMI cutoff of 24.0 in the under-65 group and a 27.0 cutoff in the older group. Ranges of 23.0-25.0 in the under-65 group and 26.0-28 in the older group were associated with the lowest cardiovascular risk.
In contrast, there was a linear relationship between both waist circumference and waist-to-height ratio and the risk for cardiovascular death, making those more direct measures of adiposity, Dr. Xu told this news organization.
“For clinicians, our data underscores the importance of considering age when assessing BMI targets for cardiovascular health. Personalized treatment plans that account for age-specific BMI cutoffs and other risk factors may enhance patient outcomes and reduce CVD mortality,” Dr. Xu said.
However, he added, “while these findings suggest an optimal BMI range, it is crucial to acknowledge that these cutoff points may vary based on gender, race, and other factors. Our future studies will validate these findings in different populations and attempt to explain the mechanism by which the optimal nodal values exist in people with diabetes at different ages.”
Dr. Neeland cautioned, “I think more work needs to be done in terms of not just identifying the risk differences but understanding why and how to better risk stratify individuals and do personalized medicine. I think that’s important, but you have to have good data to support the strategies you’re going to use. These data are observational, and they’re a good start, but they wouldn’t directly impact practice at this point.”
The data will be presented at the European Congress on Obesity taking place May 12-15 in Venice, Italy.
The authors declared no competing interests. Study funding came from several sources, including the Young Talents Project of Hubei Provincial Health Commission, China, Hubei Provincial Natural Science Foundation of China, the Science and Technology Research Key Project of the Education Department of Hubei Province China, and the Sanuo Diabetes Charity Foundation, China, and the Xiangyang Science and Technology Plan Project, China. Dr. Neeland is a speaker and/or consultant for Boehringer Ingelheim, Novo Nordisk, Bayer, and Eli Lilly and Company.
A version of this article appeared on Medscape.com.
Among adults with type 2 diabetes (T2D) older than 65 years, a body mass index (BMI) in the moderate overweight category (26-28) appears to offer better protection from cardiovascular death than does a BMI in the “normal” range, new data suggested.
On the other hand, the study findings also suggest that the “normal” range of 23-25 is optimal for middle-aged adults with T2D.
The findings reflect a previously demonstrated phenomenon called the “obesity paradox,” in which older people with overweight may have better outcomes than leaner people due to factors such as bone loss, frailty, and nutritional deficits, study lead author Shaoyong Xu, of Xiangyang Central Hospital, Affiliated Hospital of Hubei University of Arts and Science, Xiangyang, China, told this news organization.
“In this era of population growth and aging, the question arises as to whether obesity or overweight can be beneficial in improving survival rates for older individuals with diabetes. This topic holds significant relevance due to the potential implications it has on weight management strategies for older adults. If overweight does not pose an increased risk of cardiovascular mortality, it may suggest that older individuals are not necessarily required to strive for weight loss to achieve so-called normal values.”
Moreover, Dr. Xu added, “inappropriate weight loss and being underweight could potentially elevate the risk of cardiovascular events, myocardial infarction, cerebral infarction, and all-cause mortality.”
Thus, he said, “while there are general guidelines recommending a BMI below 25, our findings suggest that personalized BMI targets may be more beneficial, particularly for different age groups and individuals with specific health conditions.”
Asked to comment, Ian J. Neeland, MD, director of cardiovascular prevention, University Hospitals Harrington Heart & Vascular Institute, Case Western Reserve University, Cleveland, Ohio, pointed out that older people who are underweight or in lower weight categories may be more likely to smoke or have undiagnosed cancer, or that “their BMI is not so much reflective of fat mass as of low muscle mass, or sarcopenia, and that is definitely a risk factor for adverse outcomes and risks. ... And those who have slightly higher BMIs may be maintaining muscle mass, even though they’re older, and therefore they have less risk.”
However, Dr. Neeland disagreed with the authors’ conclusions regarding “optimal” BMI. “Just because you have different risk categories based on BMI doesn’t mean that’s ‘optimal’ BMI. The way I would interpret this paper is that there’s an association of mildly overweight with better outcomes in adults who are over 65 with type 2 diabetes. We need to try to understand the mechanisms underlying that observation.”
Dr. Neeland advised that for an older person with T2D who has low muscle mass and frailty, “I wouldn’t recommend necessarily targeted weight loss in that person. But I would potentially recommend weight loss in addition to resistance training, muscle building, and endurance training, and therefore reducing fat mass. The goal would be not so much weight loss but reduction of body fat and maintaining and improving muscle health.”
U-Shaped Relationship Found Between Age, BMI, and Cardiovascular Disease (CVD) Risk
The data come from the UK Biobank, a population-based prospective cohort study of adults in the United Kingdom. A total of 22,874 participants with baseline T2D were included in the current study. Baseline surveys were conducted between 2006 and 2010, and follow-up was a median of 12.52 years. During that time, 891 people died of CVD.
Hazard ratios were adjusted for baseline variables including age, sex, smoking history, alcohol consumption, level of physical exercise, and history of CVDs.
Compared with people with BMI a < 25 in the group who were aged 65 years or younger, those with a BMI of 25.0-29.9 had a 13% higher risk for cardiovascular death. However, among those older than 65 years, a BMI between 25.0 and 29.9 was associated with an 18% lower risk.
A U-shaped relationship was found between BMI and the risk for cardiovascular death, with an optimal BMI cutoff of 24.0 in the under-65 group and a 27.0 cutoff in the older group. Ranges of 23.0-25.0 in the under-65 group and 26.0-28 in the older group were associated with the lowest cardiovascular risk.
In contrast, there was a linear relationship between both waist circumference and waist-to-height ratio and the risk for cardiovascular death, making those more direct measures of adiposity, Dr. Xu told this news organization.
“For clinicians, our data underscores the importance of considering age when assessing BMI targets for cardiovascular health. Personalized treatment plans that account for age-specific BMI cutoffs and other risk factors may enhance patient outcomes and reduce CVD mortality,” Dr. Xu said.
However, he added, “while these findings suggest an optimal BMI range, it is crucial to acknowledge that these cutoff points may vary based on gender, race, and other factors. Our future studies will validate these findings in different populations and attempt to explain the mechanism by which the optimal nodal values exist in people with diabetes at different ages.”
Dr. Neeland cautioned, “I think more work needs to be done in terms of not just identifying the risk differences but understanding why and how to better risk stratify individuals and do personalized medicine. I think that’s important, but you have to have good data to support the strategies you’re going to use. These data are observational, and they’re a good start, but they wouldn’t directly impact practice at this point.”
The data will be presented at the European Congress on Obesity taking place May 12-15 in Venice, Italy.
The authors declared no competing interests. Study funding came from several sources, including the Young Talents Project of Hubei Provincial Health Commission, China, Hubei Provincial Natural Science Foundation of China, the Science and Technology Research Key Project of the Education Department of Hubei Province China, and the Sanuo Diabetes Charity Foundation, China, and the Xiangyang Science and Technology Plan Project, China. Dr. Neeland is a speaker and/or consultant for Boehringer Ingelheim, Novo Nordisk, Bayer, and Eli Lilly and Company.
A version of this article appeared on Medscape.com.
Among adults with type 2 diabetes (T2D) older than 65 years, a body mass index (BMI) in the moderate overweight category (26-28) appears to offer better protection from cardiovascular death than does a BMI in the “normal” range, new data suggested.
On the other hand, the study findings also suggest that the “normal” range of 23-25 is optimal for middle-aged adults with T2D.
The findings reflect a previously demonstrated phenomenon called the “obesity paradox,” in which older people with overweight may have better outcomes than leaner people due to factors such as bone loss, frailty, and nutritional deficits, study lead author Shaoyong Xu, of Xiangyang Central Hospital, Affiliated Hospital of Hubei University of Arts and Science, Xiangyang, China, told this news organization.
“In this era of population growth and aging, the question arises as to whether obesity or overweight can be beneficial in improving survival rates for older individuals with diabetes. This topic holds significant relevance due to the potential implications it has on weight management strategies for older adults. If overweight does not pose an increased risk of cardiovascular mortality, it may suggest that older individuals are not necessarily required to strive for weight loss to achieve so-called normal values.”
Moreover, Dr. Xu added, “inappropriate weight loss and being underweight could potentially elevate the risk of cardiovascular events, myocardial infarction, cerebral infarction, and all-cause mortality.”
Thus, he said, “while there are general guidelines recommending a BMI below 25, our findings suggest that personalized BMI targets may be more beneficial, particularly for different age groups and individuals with specific health conditions.”
Asked to comment, Ian J. Neeland, MD, director of cardiovascular prevention, University Hospitals Harrington Heart & Vascular Institute, Case Western Reserve University, Cleveland, Ohio, pointed out that older people who are underweight or in lower weight categories may be more likely to smoke or have undiagnosed cancer, or that “their BMI is not so much reflective of fat mass as of low muscle mass, or sarcopenia, and that is definitely a risk factor for adverse outcomes and risks. ... And those who have slightly higher BMIs may be maintaining muscle mass, even though they’re older, and therefore they have less risk.”
However, Dr. Neeland disagreed with the authors’ conclusions regarding “optimal” BMI. “Just because you have different risk categories based on BMI doesn’t mean that’s ‘optimal’ BMI. The way I would interpret this paper is that there’s an association of mildly overweight with better outcomes in adults who are over 65 with type 2 diabetes. We need to try to understand the mechanisms underlying that observation.”
Dr. Neeland advised that for an older person with T2D who has low muscle mass and frailty, “I wouldn’t recommend necessarily targeted weight loss in that person. But I would potentially recommend weight loss in addition to resistance training, muscle building, and endurance training, and therefore reducing fat mass. The goal would be not so much weight loss but reduction of body fat and maintaining and improving muscle health.”
U-Shaped Relationship Found Between Age, BMI, and Cardiovascular Disease (CVD) Risk
The data come from the UK Biobank, a population-based prospective cohort study of adults in the United Kingdom. A total of 22,874 participants with baseline T2D were included in the current study. Baseline surveys were conducted between 2006 and 2010, and follow-up was a median of 12.52 years. During that time, 891 people died of CVD.
Hazard ratios were adjusted for baseline variables including age, sex, smoking history, alcohol consumption, level of physical exercise, and history of CVDs.
Compared with people with BMI a < 25 in the group who were aged 65 years or younger, those with a BMI of 25.0-29.9 had a 13% higher risk for cardiovascular death. However, among those older than 65 years, a BMI between 25.0 and 29.9 was associated with an 18% lower risk.
A U-shaped relationship was found between BMI and the risk for cardiovascular death, with an optimal BMI cutoff of 24.0 in the under-65 group and a 27.0 cutoff in the older group. Ranges of 23.0-25.0 in the under-65 group and 26.0-28 in the older group were associated with the lowest cardiovascular risk.
In contrast, there was a linear relationship between both waist circumference and waist-to-height ratio and the risk for cardiovascular death, making those more direct measures of adiposity, Dr. Xu told this news organization.
“For clinicians, our data underscores the importance of considering age when assessing BMI targets for cardiovascular health. Personalized treatment plans that account for age-specific BMI cutoffs and other risk factors may enhance patient outcomes and reduce CVD mortality,” Dr. Xu said.
However, he added, “while these findings suggest an optimal BMI range, it is crucial to acknowledge that these cutoff points may vary based on gender, race, and other factors. Our future studies will validate these findings in different populations and attempt to explain the mechanism by which the optimal nodal values exist in people with diabetes at different ages.”
Dr. Neeland cautioned, “I think more work needs to be done in terms of not just identifying the risk differences but understanding why and how to better risk stratify individuals and do personalized medicine. I think that’s important, but you have to have good data to support the strategies you’re going to use. These data are observational, and they’re a good start, but they wouldn’t directly impact practice at this point.”
The data will be presented at the European Congress on Obesity taking place May 12-15 in Venice, Italy.
The authors declared no competing interests. Study funding came from several sources, including the Young Talents Project of Hubei Provincial Health Commission, China, Hubei Provincial Natural Science Foundation of China, the Science and Technology Research Key Project of the Education Department of Hubei Province China, and the Sanuo Diabetes Charity Foundation, China, and the Xiangyang Science and Technology Plan Project, China. Dr. Neeland is a speaker and/or consultant for Boehringer Ingelheim, Novo Nordisk, Bayer, and Eli Lilly and Company.
A version of this article appeared on Medscape.com.
A Prescription Checklist for Older Adults in ED
TOPLINE:
The geriatric emergency medication safety recommendations (GEMS-Rx) is the first expert consensus-based list identifying high-risk medication classes that should not be prescribed to older patients visiting the emergency department (ED).
METHODOLOGY:
- The American Geriatrics Society (AGS) has already established guidelines to identify potentially inappropriate medications in older adults; however, the criteria are centered on chronic conditions and long-term medication use and are unsuitable for managing ED prescriptions.
- In this study, the GEMS-Rx high-risk prescription list was prepared with a panel of 10 ED physicians with expertise in geriatrics and quality measurement and a pharmacist with expertise in geriatric pharmacotherapy and emergency medicine.
- They reviewed over 30 medication classes from the 2019 AGS Beers Criteria that were deemed inappropriate for use in older patients. Despite their not being included in the Beers list, the use of short- and long-acting opioids was also discussed.
- After three rounds of review and discussion, the panelists ranked each class of medication on a 5-point Likert scale, with a score of 1 indicating the lowest and 5 indicating the greatest need for avoiding a drug in an ED prescription.
TAKEAWAY:
- The first round suggested that first-generation antihistamines, metoclopramide, short-acting opioids, antipsychotics, barbiturates, skeletal muscle relaxants, and benzodiazepines should be avoided, with mean Likert scores ranging from 3.7 to 4.6.
- Although nonbenzodiazepine and benzodiazepine receptor agonist hypnotics (“Z-drugs”) were not initially considered owing to their low frequency of prescription in ED settings, the panelists finally included “Z” drugs and sulfonylureas in the GEMS-Rx list after the second and third rounds.
- The final list of high-risk medications to be avoided in ED settings that were prioritized included benzodiazepines, skeletal muscle relaxants, barbiturates, first-generation antipsychotics, first-generation antihistamines, “Z” drugs, metoclopramide, and sulfonylureas.
- However, seizure disorders, benzodiazepine withdrawal, ethanol withdrawal, severe generalized anxiety disorder, end-of-life care, allergic reactions, and ED visits for prescription refilling were deemed exceptional cases in which these high-risk medications could be prescribed.
IN PRACTICE:
“By combining expert consensus and evidence-based criteria, this list can serve as a resource to guide prescribing decisions and mitigate potential risks associated with medications at this crucial care transition. The incorporation of this emergency medicine-specific geriatric prescription list in a national quality measure has the potential to improve patient safety and enhance the quality of care for the millions of older adults who seek care in EDs each year,” the authors said.
SOURCE:
This study was led by Rachel M. Skains, MD, MSPH, Department of Emergency Medicine, University of Alabama at Birmingham, and published online in Annals of Emergency Medicine.
LIMITATIONS:
The GEMS-Rx list was prepared by physicians and pharmacists and may not have fully captured data regarding individual patient preferences, comorbidities, or other contextual factors. During the meetings, the panelists’ identities were not concealed from one another, which may have affected the conversations owing to response and social desirability bias. Furthermore, this list may not be generalizable to other settings because it was produced and intended for usage in US EDs.
DISCLOSURES:
This work was supported by the American College of Emergency Physicians. Some of the authors, including the lead author, declared being supported by various funding agencies. Few authors also declared serving in leadership positions for several sources.
A version of this article appeared on Medscape.com.
TOPLINE:
The geriatric emergency medication safety recommendations (GEMS-Rx) is the first expert consensus-based list identifying high-risk medication classes that should not be prescribed to older patients visiting the emergency department (ED).
METHODOLOGY:
- The American Geriatrics Society (AGS) has already established guidelines to identify potentially inappropriate medications in older adults; however, the criteria are centered on chronic conditions and long-term medication use and are unsuitable for managing ED prescriptions.
- In this study, the GEMS-Rx high-risk prescription list was prepared with a panel of 10 ED physicians with expertise in geriatrics and quality measurement and a pharmacist with expertise in geriatric pharmacotherapy and emergency medicine.
- They reviewed over 30 medication classes from the 2019 AGS Beers Criteria that were deemed inappropriate for use in older patients. Despite their not being included in the Beers list, the use of short- and long-acting opioids was also discussed.
- After three rounds of review and discussion, the panelists ranked each class of medication on a 5-point Likert scale, with a score of 1 indicating the lowest and 5 indicating the greatest need for avoiding a drug in an ED prescription.
TAKEAWAY:
- The first round suggested that first-generation antihistamines, metoclopramide, short-acting opioids, antipsychotics, barbiturates, skeletal muscle relaxants, and benzodiazepines should be avoided, with mean Likert scores ranging from 3.7 to 4.6.
- Although nonbenzodiazepine and benzodiazepine receptor agonist hypnotics (“Z-drugs”) were not initially considered owing to their low frequency of prescription in ED settings, the panelists finally included “Z” drugs and sulfonylureas in the GEMS-Rx list after the second and third rounds.
- The final list of high-risk medications to be avoided in ED settings that were prioritized included benzodiazepines, skeletal muscle relaxants, barbiturates, first-generation antipsychotics, first-generation antihistamines, “Z” drugs, metoclopramide, and sulfonylureas.
- However, seizure disorders, benzodiazepine withdrawal, ethanol withdrawal, severe generalized anxiety disorder, end-of-life care, allergic reactions, and ED visits for prescription refilling were deemed exceptional cases in which these high-risk medications could be prescribed.
IN PRACTICE:
“By combining expert consensus and evidence-based criteria, this list can serve as a resource to guide prescribing decisions and mitigate potential risks associated with medications at this crucial care transition. The incorporation of this emergency medicine-specific geriatric prescription list in a national quality measure has the potential to improve patient safety and enhance the quality of care for the millions of older adults who seek care in EDs each year,” the authors said.
SOURCE:
This study was led by Rachel M. Skains, MD, MSPH, Department of Emergency Medicine, University of Alabama at Birmingham, and published online in Annals of Emergency Medicine.
LIMITATIONS:
The GEMS-Rx list was prepared by physicians and pharmacists and may not have fully captured data regarding individual patient preferences, comorbidities, or other contextual factors. During the meetings, the panelists’ identities were not concealed from one another, which may have affected the conversations owing to response and social desirability bias. Furthermore, this list may not be generalizable to other settings because it was produced and intended for usage in US EDs.
DISCLOSURES:
This work was supported by the American College of Emergency Physicians. Some of the authors, including the lead author, declared being supported by various funding agencies. Few authors also declared serving in leadership positions for several sources.
A version of this article appeared on Medscape.com.
TOPLINE:
The geriatric emergency medication safety recommendations (GEMS-Rx) is the first expert consensus-based list identifying high-risk medication classes that should not be prescribed to older patients visiting the emergency department (ED).
METHODOLOGY:
- The American Geriatrics Society (AGS) has already established guidelines to identify potentially inappropriate medications in older adults; however, the criteria are centered on chronic conditions and long-term medication use and are unsuitable for managing ED prescriptions.
- In this study, the GEMS-Rx high-risk prescription list was prepared with a panel of 10 ED physicians with expertise in geriatrics and quality measurement and a pharmacist with expertise in geriatric pharmacotherapy and emergency medicine.
- They reviewed over 30 medication classes from the 2019 AGS Beers Criteria that were deemed inappropriate for use in older patients. Despite their not being included in the Beers list, the use of short- and long-acting opioids was also discussed.
- After three rounds of review and discussion, the panelists ranked each class of medication on a 5-point Likert scale, with a score of 1 indicating the lowest and 5 indicating the greatest need for avoiding a drug in an ED prescription.
TAKEAWAY:
- The first round suggested that first-generation antihistamines, metoclopramide, short-acting opioids, antipsychotics, barbiturates, skeletal muscle relaxants, and benzodiazepines should be avoided, with mean Likert scores ranging from 3.7 to 4.6.
- Although nonbenzodiazepine and benzodiazepine receptor agonist hypnotics (“Z-drugs”) were not initially considered owing to their low frequency of prescription in ED settings, the panelists finally included “Z” drugs and sulfonylureas in the GEMS-Rx list after the second and third rounds.
- The final list of high-risk medications to be avoided in ED settings that were prioritized included benzodiazepines, skeletal muscle relaxants, barbiturates, first-generation antipsychotics, first-generation antihistamines, “Z” drugs, metoclopramide, and sulfonylureas.
- However, seizure disorders, benzodiazepine withdrawal, ethanol withdrawal, severe generalized anxiety disorder, end-of-life care, allergic reactions, and ED visits for prescription refilling were deemed exceptional cases in which these high-risk medications could be prescribed.
IN PRACTICE:
“By combining expert consensus and evidence-based criteria, this list can serve as a resource to guide prescribing decisions and mitigate potential risks associated with medications at this crucial care transition. The incorporation of this emergency medicine-specific geriatric prescription list in a national quality measure has the potential to improve patient safety and enhance the quality of care for the millions of older adults who seek care in EDs each year,” the authors said.
SOURCE:
This study was led by Rachel M. Skains, MD, MSPH, Department of Emergency Medicine, University of Alabama at Birmingham, and published online in Annals of Emergency Medicine.
LIMITATIONS:
The GEMS-Rx list was prepared by physicians and pharmacists and may not have fully captured data regarding individual patient preferences, comorbidities, or other contextual factors. During the meetings, the panelists’ identities were not concealed from one another, which may have affected the conversations owing to response and social desirability bias. Furthermore, this list may not be generalizable to other settings because it was produced and intended for usage in US EDs.
DISCLOSURES:
This work was supported by the American College of Emergency Physicians. Some of the authors, including the lead author, declared being supported by various funding agencies. Few authors also declared serving in leadership positions for several sources.
A version of this article appeared on Medscape.com.
This Could Be Key to Motivating Older Patients to Exercise
Starting an exercise regimen with others can be a powerful fitness motivator, and new research spotlights the strategy’s particular importance for older adults.
In a randomized clinical trial published in JAMA Network Open, older adults who talked with peers about their exercise program were able to increase and sustain physical activity levels much better than those who focused on self-motivation and setting fitness goals.
Such self-focused — or “intrapersonal” — strategies tend to be more common in health and fitness than interactive, or “interpersonal,” ones, the study authors noted. Yet, research on their effectiveness is limited.
“We’re not saying that intrapersonal strategies should not be used,” said study author Siobhan McMahon, PhD, associate professor and codirector of the Center on Aging Science and Care at the University of Minnesota, in Minneapolis, Minnesota, “but this study shows that interpersonal strategies are really important.”
Low physical activity among older adults is linked with “disability, difficulty managing chronic conditions, and increased falls and related injuries,” the authors wrote. Exercise can be the antidote, yet fewer than 16% of older adults meet the recommended guidelines (150 minutes of moderate aerobic activity and two muscle-strengthening sessions per week).
The study builds on previous research that suggests interpersonal strategies could help change that by encouraging more older adults to move.
Intrapersonal vs Interpersonal Behavior Change Strategies
More than 300 participants aged 70 years and older who did not meet physical activity guidelines were given a wearable fitness tracker and an exercise program and randomly split into four groups:
- One using intrapersonal behavior change strategies
- Another using interpersonal strategies
- A group combining both intrapersonal and interpersonal strategies
- A control group that received neither intervention
For 8 weeks, all participants exercised in meet-ups and discussed their progress in their groups. Afterward, they were left to their own devices and monitored for the remainder of the year.
“The intrapersonal strategies group involved personal reflection,” said Dr. McMahon. They set personal goals (increasing daily step count or exercise repetitions) and developed action plans for implementing physical activity into their daily routines.
“The interpersonal group involved more peer-to-peer conversation, collaborative learning, and sharing,” said Dr. McMahon. Participants talked among themselves about how they could sustain doing the prescribed exercises at home. “Through those conversations, they learned and experimented,” Dr. McMahon said. They problem-solved, determining what barriers might stop them from exercising and brainstorming ways around them.
The researchers evaluated the participants after 1 week, 6 months, and 12 months. The interpersonal group exhibited significant increases in physical activity — including light, moderate, and vigorous activity — for the entire year. They increased their average physical activity per day by 21-28 minutes and their daily step count by 776-1058.
The intrapersonal group, meanwhile, exhibited no significant changes in total physical activity. (The third experimental group, the intrapersonal plus interpersonal condition, had results similar to the interpersonal one.)
The results echoed the findings of a similar study Dr. McMahon conducted in 2017. “We followed people over a longer period of time in this [new] study,” she said, “12 months instead of 6 months. This is important in physical activity studies because a lot of evidence shows that after 6 months, people’s activity drops off.”
How Socializing Promotes Exercise Compliance
Research on the effectiveness of exercise in social groups dates back as far as the 19th century. It’s called the social facilitation theory: The idea that people will make an increased effort as a result of the real, imagined, or implied presence of others.
“Norman Triplett was a scientist who studied indoor cyclists, and he came up with the social facilitation theory in 1898,” said Robert Linkul, CSCS*D, who sits on the National Strength and Conditioning Association’s board of directors and specializes in exercise for older adults. “He noticed that during relays, the first cyclist would get slower as he fatigued, but as soon as his teammate came out, his last lap would be faster than his previous two laps. People try harder when there’s some other person present. They tend to feel pressure to perform because they don’t want to look bad.”
Dr. McMahon said the exact psychology of why socializing supports exercise isn’t clear yet but noted that talking to other people builds relationships and makes one feel connected to and involved with a community.
“I think connections between peers are really important,” said Dr. McMahon. “It goes beyond just being in the same room and doing the exercises together. It’s taking a little bit of time to talk about it. To acknowledge what they’re doing and their progress. To encourage each other and provide support.”
Some of the study participants even became friends and continued to meet on their own time over the course of the trial.
“They stayed in touch,” said Dr. McMahon. “One thing that people talked about after the study, even if they weren’t friends, was that the conversations within the meetings made them feel kind of a fellowship that helped them learn about themselves or people like them.”
Help Patients Find Their Own Fellowship of Active People
- Communicate the importance of exercise. During appointments, ask how the patient is doing with their exercise and listen for any obstacles to compliance, Dr. McMahon said.
- See if they have access to fitness classes. Many community-dwelling older adults do, Mr. Linkul said. If not, consider local or state agencies on aging — “in Minnesota, we have a program, Juniper,” Dr. McMahon said, that maintains a list of physical activity programs — or AARP’s free online group classes, or Silver Sneakers (free for those with eligible Medicare Advantage plans).
- Reach out to local qualified fitness professionals. Trainers with the Training the Older Adult certification (founded by Mr. Linkul) can be found here. Other qualified trainers can be found through the Functional Aging Institute, American Council on Exercise, and National Academy of Sports Medicine, Mr. Linkul said. “Many of these trainers will offer semiprivate sessions,” said Mr. Linkul, “which is usually four to eight people.” Groups of this size often facilitate better participation than larger classes. “You get more personalized attention from the instructor along with an environment that allows social engagement,” said Mr. Linkul. If you have exercise or rehab professionals in your network, you might consider reaching out to them. Some physical therapists lead activity groups, though reimbursement challenges mean they aren’t common, Dr. McMahon said.
- Prescribe short walks with a friend, family member, or neighbor. Have the person start with 30 minutes of walking or rucking (walking with a weighted backpack) most days, Mr. Linkul suggested, a recommendation that is echoed by the American College of Sports Medicine.
- Encourage patients to talk about their exercise. Even for those who prefer to exercise solo, “our studies suggest it might be helpful to have conversations with others about movement, and motivations for movement,” Dr. McMahon said. They can simply mention one idea, question, or observation related to physical activity during casual catchups or chats.
- Recommend resistance training. That goes for patients with preexisting health conditions too, Mr. Linkul said. Physicians “find out a patient has low bone mineral density, and they’ll often tell them not to pick up anything heavy because they’ll hurt themselves — and that’s the exact wrong answer,” Mr. Linkul said. A total of 32% of the participants in the JAMA Network study had cardiovascular disease, nearly 34% had osteoporosis, 70% had arthritis, and more than 20% were living with diabetes.
- Expect pushback. Encouraging older adults to exercise is hard because many are resistant to it, Mr. Linkul acknowledged. Do it anyway. Some will listen and that makes the effort worthwhile. “I try to provide as much information as I can about what happens to aging bodies if they don’t train,” said Mr. Linkul. “These people are more likely to fall, they’ll die earlier, and have a poorer quality of life. But when they start exercising, they feel better immediately.”
A version of this article appeared on Medscape.com.
Starting an exercise regimen with others can be a powerful fitness motivator, and new research spotlights the strategy’s particular importance for older adults.
In a randomized clinical trial published in JAMA Network Open, older adults who talked with peers about their exercise program were able to increase and sustain physical activity levels much better than those who focused on self-motivation and setting fitness goals.
Such self-focused — or “intrapersonal” — strategies tend to be more common in health and fitness than interactive, or “interpersonal,” ones, the study authors noted. Yet, research on their effectiveness is limited.
“We’re not saying that intrapersonal strategies should not be used,” said study author Siobhan McMahon, PhD, associate professor and codirector of the Center on Aging Science and Care at the University of Minnesota, in Minneapolis, Minnesota, “but this study shows that interpersonal strategies are really important.”
Low physical activity among older adults is linked with “disability, difficulty managing chronic conditions, and increased falls and related injuries,” the authors wrote. Exercise can be the antidote, yet fewer than 16% of older adults meet the recommended guidelines (150 minutes of moderate aerobic activity and two muscle-strengthening sessions per week).
The study builds on previous research that suggests interpersonal strategies could help change that by encouraging more older adults to move.
Intrapersonal vs Interpersonal Behavior Change Strategies
More than 300 participants aged 70 years and older who did not meet physical activity guidelines were given a wearable fitness tracker and an exercise program and randomly split into four groups:
- One using intrapersonal behavior change strategies
- Another using interpersonal strategies
- A group combining both intrapersonal and interpersonal strategies
- A control group that received neither intervention
For 8 weeks, all participants exercised in meet-ups and discussed their progress in their groups. Afterward, they were left to their own devices and monitored for the remainder of the year.
“The intrapersonal strategies group involved personal reflection,” said Dr. McMahon. They set personal goals (increasing daily step count or exercise repetitions) and developed action plans for implementing physical activity into their daily routines.
“The interpersonal group involved more peer-to-peer conversation, collaborative learning, and sharing,” said Dr. McMahon. Participants talked among themselves about how they could sustain doing the prescribed exercises at home. “Through those conversations, they learned and experimented,” Dr. McMahon said. They problem-solved, determining what barriers might stop them from exercising and brainstorming ways around them.
The researchers evaluated the participants after 1 week, 6 months, and 12 months. The interpersonal group exhibited significant increases in physical activity — including light, moderate, and vigorous activity — for the entire year. They increased their average physical activity per day by 21-28 minutes and their daily step count by 776-1058.
The intrapersonal group, meanwhile, exhibited no significant changes in total physical activity. (The third experimental group, the intrapersonal plus interpersonal condition, had results similar to the interpersonal one.)
The results echoed the findings of a similar study Dr. McMahon conducted in 2017. “We followed people over a longer period of time in this [new] study,” she said, “12 months instead of 6 months. This is important in physical activity studies because a lot of evidence shows that after 6 months, people’s activity drops off.”
How Socializing Promotes Exercise Compliance
Research on the effectiveness of exercise in social groups dates back as far as the 19th century. It’s called the social facilitation theory: The idea that people will make an increased effort as a result of the real, imagined, or implied presence of others.
“Norman Triplett was a scientist who studied indoor cyclists, and he came up with the social facilitation theory in 1898,” said Robert Linkul, CSCS*D, who sits on the National Strength and Conditioning Association’s board of directors and specializes in exercise for older adults. “He noticed that during relays, the first cyclist would get slower as he fatigued, but as soon as his teammate came out, his last lap would be faster than his previous two laps. People try harder when there’s some other person present. They tend to feel pressure to perform because they don’t want to look bad.”
Dr. McMahon said the exact psychology of why socializing supports exercise isn’t clear yet but noted that talking to other people builds relationships and makes one feel connected to and involved with a community.
“I think connections between peers are really important,” said Dr. McMahon. “It goes beyond just being in the same room and doing the exercises together. It’s taking a little bit of time to talk about it. To acknowledge what they’re doing and their progress. To encourage each other and provide support.”
Some of the study participants even became friends and continued to meet on their own time over the course of the trial.
“They stayed in touch,” said Dr. McMahon. “One thing that people talked about after the study, even if they weren’t friends, was that the conversations within the meetings made them feel kind of a fellowship that helped them learn about themselves or people like them.”
Help Patients Find Their Own Fellowship of Active People
- Communicate the importance of exercise. During appointments, ask how the patient is doing with their exercise and listen for any obstacles to compliance, Dr. McMahon said.
- See if they have access to fitness classes. Many community-dwelling older adults do, Mr. Linkul said. If not, consider local or state agencies on aging — “in Minnesota, we have a program, Juniper,” Dr. McMahon said, that maintains a list of physical activity programs — or AARP’s free online group classes, or Silver Sneakers (free for those with eligible Medicare Advantage plans).
- Reach out to local qualified fitness professionals. Trainers with the Training the Older Adult certification (founded by Mr. Linkul) can be found here. Other qualified trainers can be found through the Functional Aging Institute, American Council on Exercise, and National Academy of Sports Medicine, Mr. Linkul said. “Many of these trainers will offer semiprivate sessions,” said Mr. Linkul, “which is usually four to eight people.” Groups of this size often facilitate better participation than larger classes. “You get more personalized attention from the instructor along with an environment that allows social engagement,” said Mr. Linkul. If you have exercise or rehab professionals in your network, you might consider reaching out to them. Some physical therapists lead activity groups, though reimbursement challenges mean they aren’t common, Dr. McMahon said.
- Prescribe short walks with a friend, family member, or neighbor. Have the person start with 30 minutes of walking or rucking (walking with a weighted backpack) most days, Mr. Linkul suggested, a recommendation that is echoed by the American College of Sports Medicine.
- Encourage patients to talk about their exercise. Even for those who prefer to exercise solo, “our studies suggest it might be helpful to have conversations with others about movement, and motivations for movement,” Dr. McMahon said. They can simply mention one idea, question, or observation related to physical activity during casual catchups or chats.
- Recommend resistance training. That goes for patients with preexisting health conditions too, Mr. Linkul said. Physicians “find out a patient has low bone mineral density, and they’ll often tell them not to pick up anything heavy because they’ll hurt themselves — and that’s the exact wrong answer,” Mr. Linkul said. A total of 32% of the participants in the JAMA Network study had cardiovascular disease, nearly 34% had osteoporosis, 70% had arthritis, and more than 20% were living with diabetes.
- Expect pushback. Encouraging older adults to exercise is hard because many are resistant to it, Mr. Linkul acknowledged. Do it anyway. Some will listen and that makes the effort worthwhile. “I try to provide as much information as I can about what happens to aging bodies if they don’t train,” said Mr. Linkul. “These people are more likely to fall, they’ll die earlier, and have a poorer quality of life. But when they start exercising, they feel better immediately.”
A version of this article appeared on Medscape.com.
Starting an exercise regimen with others can be a powerful fitness motivator, and new research spotlights the strategy’s particular importance for older adults.
In a randomized clinical trial published in JAMA Network Open, older adults who talked with peers about their exercise program were able to increase and sustain physical activity levels much better than those who focused on self-motivation and setting fitness goals.
Such self-focused — or “intrapersonal” — strategies tend to be more common in health and fitness than interactive, or “interpersonal,” ones, the study authors noted. Yet, research on their effectiveness is limited.
“We’re not saying that intrapersonal strategies should not be used,” said study author Siobhan McMahon, PhD, associate professor and codirector of the Center on Aging Science and Care at the University of Minnesota, in Minneapolis, Minnesota, “but this study shows that interpersonal strategies are really important.”
Low physical activity among older adults is linked with “disability, difficulty managing chronic conditions, and increased falls and related injuries,” the authors wrote. Exercise can be the antidote, yet fewer than 16% of older adults meet the recommended guidelines (150 minutes of moderate aerobic activity and two muscle-strengthening sessions per week).
The study builds on previous research that suggests interpersonal strategies could help change that by encouraging more older adults to move.
Intrapersonal vs Interpersonal Behavior Change Strategies
More than 300 participants aged 70 years and older who did not meet physical activity guidelines were given a wearable fitness tracker and an exercise program and randomly split into four groups:
- One using intrapersonal behavior change strategies
- Another using interpersonal strategies
- A group combining both intrapersonal and interpersonal strategies
- A control group that received neither intervention
For 8 weeks, all participants exercised in meet-ups and discussed their progress in their groups. Afterward, they were left to their own devices and monitored for the remainder of the year.
“The intrapersonal strategies group involved personal reflection,” said Dr. McMahon. They set personal goals (increasing daily step count or exercise repetitions) and developed action plans for implementing physical activity into their daily routines.
“The interpersonal group involved more peer-to-peer conversation, collaborative learning, and sharing,” said Dr. McMahon. Participants talked among themselves about how they could sustain doing the prescribed exercises at home. “Through those conversations, they learned and experimented,” Dr. McMahon said. They problem-solved, determining what barriers might stop them from exercising and brainstorming ways around them.
The researchers evaluated the participants after 1 week, 6 months, and 12 months. The interpersonal group exhibited significant increases in physical activity — including light, moderate, and vigorous activity — for the entire year. They increased their average physical activity per day by 21-28 minutes and their daily step count by 776-1058.
The intrapersonal group, meanwhile, exhibited no significant changes in total physical activity. (The third experimental group, the intrapersonal plus interpersonal condition, had results similar to the interpersonal one.)
The results echoed the findings of a similar study Dr. McMahon conducted in 2017. “We followed people over a longer period of time in this [new] study,” she said, “12 months instead of 6 months. This is important in physical activity studies because a lot of evidence shows that after 6 months, people’s activity drops off.”
How Socializing Promotes Exercise Compliance
Research on the effectiveness of exercise in social groups dates back as far as the 19th century. It’s called the social facilitation theory: The idea that people will make an increased effort as a result of the real, imagined, or implied presence of others.
“Norman Triplett was a scientist who studied indoor cyclists, and he came up with the social facilitation theory in 1898,” said Robert Linkul, CSCS*D, who sits on the National Strength and Conditioning Association’s board of directors and specializes in exercise for older adults. “He noticed that during relays, the first cyclist would get slower as he fatigued, but as soon as his teammate came out, his last lap would be faster than his previous two laps. People try harder when there’s some other person present. They tend to feel pressure to perform because they don’t want to look bad.”
Dr. McMahon said the exact psychology of why socializing supports exercise isn’t clear yet but noted that talking to other people builds relationships and makes one feel connected to and involved with a community.
“I think connections between peers are really important,” said Dr. McMahon. “It goes beyond just being in the same room and doing the exercises together. It’s taking a little bit of time to talk about it. To acknowledge what they’re doing and their progress. To encourage each other and provide support.”
Some of the study participants even became friends and continued to meet on their own time over the course of the trial.
“They stayed in touch,” said Dr. McMahon. “One thing that people talked about after the study, even if they weren’t friends, was that the conversations within the meetings made them feel kind of a fellowship that helped them learn about themselves or people like them.”
Help Patients Find Their Own Fellowship of Active People
- Communicate the importance of exercise. During appointments, ask how the patient is doing with their exercise and listen for any obstacles to compliance, Dr. McMahon said.
- See if they have access to fitness classes. Many community-dwelling older adults do, Mr. Linkul said. If not, consider local or state agencies on aging — “in Minnesota, we have a program, Juniper,” Dr. McMahon said, that maintains a list of physical activity programs — or AARP’s free online group classes, or Silver Sneakers (free for those with eligible Medicare Advantage plans).
- Reach out to local qualified fitness professionals. Trainers with the Training the Older Adult certification (founded by Mr. Linkul) can be found here. Other qualified trainers can be found through the Functional Aging Institute, American Council on Exercise, and National Academy of Sports Medicine, Mr. Linkul said. “Many of these trainers will offer semiprivate sessions,” said Mr. Linkul, “which is usually four to eight people.” Groups of this size often facilitate better participation than larger classes. “You get more personalized attention from the instructor along with an environment that allows social engagement,” said Mr. Linkul. If you have exercise or rehab professionals in your network, you might consider reaching out to them. Some physical therapists lead activity groups, though reimbursement challenges mean they aren’t common, Dr. McMahon said.
- Prescribe short walks with a friend, family member, or neighbor. Have the person start with 30 minutes of walking or rucking (walking with a weighted backpack) most days, Mr. Linkul suggested, a recommendation that is echoed by the American College of Sports Medicine.
- Encourage patients to talk about their exercise. Even for those who prefer to exercise solo, “our studies suggest it might be helpful to have conversations with others about movement, and motivations for movement,” Dr. McMahon said. They can simply mention one idea, question, or observation related to physical activity during casual catchups or chats.
- Recommend resistance training. That goes for patients with preexisting health conditions too, Mr. Linkul said. Physicians “find out a patient has low bone mineral density, and they’ll often tell them not to pick up anything heavy because they’ll hurt themselves — and that’s the exact wrong answer,” Mr. Linkul said. A total of 32% of the participants in the JAMA Network study had cardiovascular disease, nearly 34% had osteoporosis, 70% had arthritis, and more than 20% were living with diabetes.
- Expect pushback. Encouraging older adults to exercise is hard because many are resistant to it, Mr. Linkul acknowledged. Do it anyway. Some will listen and that makes the effort worthwhile. “I try to provide as much information as I can about what happens to aging bodies if they don’t train,” said Mr. Linkul. “These people are more likely to fall, they’ll die earlier, and have a poorer quality of life. But when they start exercising, they feel better immediately.”
A version of this article appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Statins Tied to Lower Mortality, Even With Comorbid Dementia
Use of statin drugs was associated with improved mortality in older nursing home residents, regardless of dementia status, a new study showed.
The study is among the first to explore whether statin use in older nursing home residents offers a mortality benefit, especially among individuals with dementia, a group largely excluded from earlier statin trials.
Investigators’ analysis of 4 years of data on nearly 300,000 nursing home residents revealed that statin use was associated with a 40% lower risk for all-cause mortality than statin nonuse in those without dementia and a 20% lower risk in those with dementia.
“These findings may provide evidence that supports the continued use of statins in older nursing home patients with multiple medical conditions,” wrote lead author Julie Lorraine O’Sullivan, PhD, of the Charité–Universitätsmedizin Berlin, Freie Universität Berlin, German Center for Mental Health, Berlin, and colleagues.
The study was published online on February 27 in Neurology.
Understudied Population
Statins are the first-line treatment for preventing atherosclerotic cardiovascular disease (ASCVD), but they are also known to carry risks to patients who are frail or care-dependent. Many prior clinical trials excluded older participants with multiple comorbidities, especially those with dementia. So, evidence regarding the drugs’ efficacy in this population was lacking.
Investigators retrospectively examined 5 years of claims data from a German health and long-term care insurance provider on 282,693 nursing home residents (mean age, 83 years) who had used statins consecutively for ≥ 6 months.
Researchers used propensity score matching in 96,162 individuals to adjust for potential imbalances in the distribution of covariates (eg, age, sex, atrial fibrillation, ASCVD, and other conditions, as well as medications) and to reduce bias. Cox regression models were similarly adjusted for these factors, as well as care level. Residents were followed for an average of 2 years.
There were 54,269 recorded deaths during the study period, with most patients requiring a high level of care and 65% with dementia.
Statin use was associated with lower all-cause mortality in residents with dementia (hazard ratio [HR], 0.80, P < .001) and those without dementia (HR, 0.73; P < .001) compared with nonusers. The benefits remained consistent even after excluding participants with a history of ASCVD and across subgroups stratified by age sex, care level, and dementia type.
Limitations included the potential for unknown confounders and a lack of information about previous statin use, smoking and sedentary behavior, and the cause of mortality.
“Although our findings suggest the benefits of statins ... it is vital to acknowledge the need for further research to understand the underlying mechanism and the need for replication of our results to understand the potential risks before making recommendations to clinicians and families regarding statin therapy,” investigators wrote.
‘First Step’
In an accompanying editorial, Ariela R. Orkaby, MD, MPH, assistant professor of medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, called the study a “first step” to a better understanding of statin use in an understudied population.
“These findings build on a limited body of observational evidence for statin use in high-risk older adults, which has generally demonstrated protective associations for statins and mortality, including those with dementia and frailty, although nursing home status has not been specifically explored,” Dr. Orkaby wrote.
Perhaps more important than gaining information about statins’ effect on mortality risk in older people with dementia may be a better understanding of how the drugs might improve quality of life by reducing the risk for stroke or other cardiovascular events.
“It may be time to reconsider the broad recommendations to avoid or deprescribe statins in nursing home residents and rather invest in high-quality evidence to guide the care of this vulnerable population. After all, a lack of evidence does not imply benefit or harm, rather a need for more data,” Dr. Orkaby added.
The research was funded by Stiftung Charité; Dr. O’Sullivan and coauthors reported no relevant financial relationships. Dr. Orkaby received funding from a VA CSR&D CDA-2 award.
A version of this article appeared on Medscape.com.
Use of statin drugs was associated with improved mortality in older nursing home residents, regardless of dementia status, a new study showed.
The study is among the first to explore whether statin use in older nursing home residents offers a mortality benefit, especially among individuals with dementia, a group largely excluded from earlier statin trials.
Investigators’ analysis of 4 years of data on nearly 300,000 nursing home residents revealed that statin use was associated with a 40% lower risk for all-cause mortality than statin nonuse in those without dementia and a 20% lower risk in those with dementia.
“These findings may provide evidence that supports the continued use of statins in older nursing home patients with multiple medical conditions,” wrote lead author Julie Lorraine O’Sullivan, PhD, of the Charité–Universitätsmedizin Berlin, Freie Universität Berlin, German Center for Mental Health, Berlin, and colleagues.
The study was published online on February 27 in Neurology.
Understudied Population
Statins are the first-line treatment for preventing atherosclerotic cardiovascular disease (ASCVD), but they are also known to carry risks to patients who are frail or care-dependent. Many prior clinical trials excluded older participants with multiple comorbidities, especially those with dementia. So, evidence regarding the drugs’ efficacy in this population was lacking.
Investigators retrospectively examined 5 years of claims data from a German health and long-term care insurance provider on 282,693 nursing home residents (mean age, 83 years) who had used statins consecutively for ≥ 6 months.
Researchers used propensity score matching in 96,162 individuals to adjust for potential imbalances in the distribution of covariates (eg, age, sex, atrial fibrillation, ASCVD, and other conditions, as well as medications) and to reduce bias. Cox regression models were similarly adjusted for these factors, as well as care level. Residents were followed for an average of 2 years.
There were 54,269 recorded deaths during the study period, with most patients requiring a high level of care and 65% with dementia.
Statin use was associated with lower all-cause mortality in residents with dementia (hazard ratio [HR], 0.80, P < .001) and those without dementia (HR, 0.73; P < .001) compared with nonusers. The benefits remained consistent even after excluding participants with a history of ASCVD and across subgroups stratified by age sex, care level, and dementia type.
Limitations included the potential for unknown confounders and a lack of information about previous statin use, smoking and sedentary behavior, and the cause of mortality.
“Although our findings suggest the benefits of statins ... it is vital to acknowledge the need for further research to understand the underlying mechanism and the need for replication of our results to understand the potential risks before making recommendations to clinicians and families regarding statin therapy,” investigators wrote.
‘First Step’
In an accompanying editorial, Ariela R. Orkaby, MD, MPH, assistant professor of medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, called the study a “first step” to a better understanding of statin use in an understudied population.
“These findings build on a limited body of observational evidence for statin use in high-risk older adults, which has generally demonstrated protective associations for statins and mortality, including those with dementia and frailty, although nursing home status has not been specifically explored,” Dr. Orkaby wrote.
Perhaps more important than gaining information about statins’ effect on mortality risk in older people with dementia may be a better understanding of how the drugs might improve quality of life by reducing the risk for stroke or other cardiovascular events.
“It may be time to reconsider the broad recommendations to avoid or deprescribe statins in nursing home residents and rather invest in high-quality evidence to guide the care of this vulnerable population. After all, a lack of evidence does not imply benefit or harm, rather a need for more data,” Dr. Orkaby added.
The research was funded by Stiftung Charité; Dr. O’Sullivan and coauthors reported no relevant financial relationships. Dr. Orkaby received funding from a VA CSR&D CDA-2 award.
A version of this article appeared on Medscape.com.
Use of statin drugs was associated with improved mortality in older nursing home residents, regardless of dementia status, a new study showed.
The study is among the first to explore whether statin use in older nursing home residents offers a mortality benefit, especially among individuals with dementia, a group largely excluded from earlier statin trials.
Investigators’ analysis of 4 years of data on nearly 300,000 nursing home residents revealed that statin use was associated with a 40% lower risk for all-cause mortality than statin nonuse in those without dementia and a 20% lower risk in those with dementia.
“These findings may provide evidence that supports the continued use of statins in older nursing home patients with multiple medical conditions,” wrote lead author Julie Lorraine O’Sullivan, PhD, of the Charité–Universitätsmedizin Berlin, Freie Universität Berlin, German Center for Mental Health, Berlin, and colleagues.
The study was published online on February 27 in Neurology.
Understudied Population
Statins are the first-line treatment for preventing atherosclerotic cardiovascular disease (ASCVD), but they are also known to carry risks to patients who are frail or care-dependent. Many prior clinical trials excluded older participants with multiple comorbidities, especially those with dementia. So, evidence regarding the drugs’ efficacy in this population was lacking.
Investigators retrospectively examined 5 years of claims data from a German health and long-term care insurance provider on 282,693 nursing home residents (mean age, 83 years) who had used statins consecutively for ≥ 6 months.
Researchers used propensity score matching in 96,162 individuals to adjust for potential imbalances in the distribution of covariates (eg, age, sex, atrial fibrillation, ASCVD, and other conditions, as well as medications) and to reduce bias. Cox regression models were similarly adjusted for these factors, as well as care level. Residents were followed for an average of 2 years.
There were 54,269 recorded deaths during the study period, with most patients requiring a high level of care and 65% with dementia.
Statin use was associated with lower all-cause mortality in residents with dementia (hazard ratio [HR], 0.80, P < .001) and those without dementia (HR, 0.73; P < .001) compared with nonusers. The benefits remained consistent even after excluding participants with a history of ASCVD and across subgroups stratified by age sex, care level, and dementia type.
Limitations included the potential for unknown confounders and a lack of information about previous statin use, smoking and sedentary behavior, and the cause of mortality.
“Although our findings suggest the benefits of statins ... it is vital to acknowledge the need for further research to understand the underlying mechanism and the need for replication of our results to understand the potential risks before making recommendations to clinicians and families regarding statin therapy,” investigators wrote.
‘First Step’
In an accompanying editorial, Ariela R. Orkaby, MD, MPH, assistant professor of medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, called the study a “first step” to a better understanding of statin use in an understudied population.
“These findings build on a limited body of observational evidence for statin use in high-risk older adults, which has generally demonstrated protective associations for statins and mortality, including those with dementia and frailty, although nursing home status has not been specifically explored,” Dr. Orkaby wrote.
Perhaps more important than gaining information about statins’ effect on mortality risk in older people with dementia may be a better understanding of how the drugs might improve quality of life by reducing the risk for stroke or other cardiovascular events.
“It may be time to reconsider the broad recommendations to avoid or deprescribe statins in nursing home residents and rather invest in high-quality evidence to guide the care of this vulnerable population. After all, a lack of evidence does not imply benefit or harm, rather a need for more data,” Dr. Orkaby added.
The research was funded by Stiftung Charité; Dr. O’Sullivan and coauthors reported no relevant financial relationships. Dr. Orkaby received funding from a VA CSR&D CDA-2 award.
A version of this article appeared on Medscape.com.
Practicing Medicine in Canada’s Far North
In 2019, we interviewed Andrea Prince, MD, who was completing her internship in the Inuit village of Puvirnituq, a town of 2000 inhabitants located in Nunavik, in the Canadian Far North. Five years later, still in her position, what perspective does she have on her practice? Have the challenges of practicing medicine in a remote region within the Inuit community affected her vocation? Would she recommend this experience to young doctors?
Question: What position do you currently hold?
Dr. Prince: I am a full-time general practitioner at Puvirnituq Hospital. My responsibilities range from following up on hospitalized patients to those seen in outpatient clinics for chronic illnesses. Within our medical team, I receive patients in the emergency department (day and night shifts), and I travel to smaller dispensaries nearby, especially to the village of Akulivik. So, it’s quite a varied practice.
More recently, I have been involved in remote continuing medical education projects in collaboration with specialists based in Montreal. In this context, we are increasingly trying to collaborate with doctors from other indigenous communities, such as the Grand Council of the Cree, because our practices are quite similar.
Q: What is the patient volume you see?
Dr. Prince: We see approximately 20-30 patients per day in the clinic, plus about 10 by appointment, and dozens of calls from dispensaries, in addition to patients transferred from other villages. There are four daytime doctors (one at night) and about 15 nurses stationed full-time at Puvirnituq Hospital.
Our practice relies heavily on collaboration with the nursing team, which has an expanded role — they can manage certain patients according to the treatment plan established by the doctor and prescribe treatments (eg, antibiotics for uncomplicated otitis).
Q: Access to care in these isolated regions is considered difficult. Have you observed any improvement in the situation over the past 5 years? What about new material and human resources?
Dr. Prince: For the past year, we have had a Starlink internet connection at the hospital, which facilitates telemedicine exchanges with specialists; we can now send data and medical images to Montreal to obtain expertise much more easily. Previously, everything was done by phone or with significant delays. We do not yet have a cellular network, and all records are currently in paper format.
But the challenges remain numerous. Progress is very slow. Like everywhere in the country, we are experiencing a shortage of staff, particularly an insufficient number of nurses. But the impact is even more dramatic in these isolated territories. We have had to close dispensaries on the coast due to a lack of personnel and only offer emergency services. However, patients have no other options; they cannot drive to another hospital. In Nunavik, the road network is practically nonexistent, and travel to other regions is by plane (about a 2.5-hour medical evacuation trip).
So, sometimes, patients do not seek care in time, and when we finally see them, unfortunately, the issue can be quite advanced.
Q: What are the most pressing logistical needs?
Dr. Prince: We still do not have a scanner in the Far North. This has a significant impact on mortality, especially in the case of accidents and trauma, which are very common in these regions. “Residents of Nunavik are four times more likely to suffer trauma than the rest of Quebec’s population and 40 times more likely to die from it,” as recently reported in La Presse.
There has also been much discussion about cancer mortality, with a risk for death about 70% higher following a lung cancer diagnosis (reported by Medscape Medical News). We do not have a mammogram machine to diagnose breast cancer. Before the COVID-19 pandemic, equipped diagnostic teams sometimes traveled to the region, but this is no longer the case. Today, a patient needing a mammogram will have to travel to Montreal. The same goes for colonoscopies, but visits are becoming less frequent. Therefore, campaigns to screen for certain common types of cancer are practically nonexistent.
As for urgent surgeries (appendicitis, cesarean sections, trauma, etc.), patients must be transferred to Montreal by medical evacuation. We have a visiting surgeon twice a year.
Q: What improvement strategies do you foresee despite the lack of resources?
Dr. Prince: The saying “prevention is better than cure” makes perfect sense in such remote regions under extreme conditions (it is impossible to fly a medevac when it is too windy or during a snowstorm!). That’s why my colleagues and I believe that prevention should be the top priority in terms of healthcare intervention. It may seem obvious, but nothing is simple in the Far North.
Q: In which areas should prevention campaigns be prioritized in your opinion?
Dr. Prince: An example is wearing helmets. Practically no one wears this type of protection in the Far North. They use all-terrain vehicles that are dangerous and for which helmet use is crucial. But they are simply not available in stores. So, communication is difficult: We tell people, “you need a helmet for the ATV, another for the bike, for the snowmobile, for playing hockey, etc.” when it is difficult to obtain one. With traumatologists in Montreal, we had a project to create multifunctional helmets for children — to protect them but also to develop a culture of helmet use, which is not common practice in the community — but these are projects that take a lot of time and are more complex than they seem.
Villages still do not have running water. Therefore, it is difficult to give recommendations to patients as they live in sanitary conditions that are unseen elsewhere in Canada. Without clean water, we cannot ensure that wound care is done properly. Not to mention the occurrence of hepatitis A epidemics, like the one we had to face.
Residents also grapple with significant alcohol and smoking problems, but there is no detox center or dedicated psychological help on site. To follow a detox program, patients would have to leave, move away from their families, and that can be psychologically very destabilizing. I try, in my practice, to talk to my patients about this, especially pregnant women — because many continue to smoke or drink during their pregnancy — but we need more resources.
Q: What about women’s health in this region?
Dr. Prince: We are fortunate to have a team of midwives, several of whom are Inuit, who are of great help in accessing contraception, performing cervical cancer screening tests, etc. But some patients with high-risk pregnancies who should be transferred to Montreal refuse to give birth away from their families. Again, if we had the means to allow high-risk women — or those for whom continuous monitoring or a cesarean section may be necessary — to give birth here safely, it would be a big step. As for abortion, it is feasible but remains a very taboo subject in the community.
Regarding violence against women, I have not observed any particularly encouraging developments in the past 5 years, but recently, we met with the mayor about this, hoping that concrete actions will be taken to help victims of violence.
Q: What is the predominant feeling in your daily life in a situation that is slow to evolve?
Dr. Prince: I remain hopeful for my patients. We must continue to fight! Initiatives must also come from the communities themselves; they must be involved in developing solutions. Because patients, too, need to have hope. They have the right to be cared for like other inhabitants of Canada.
On my part, I try to find a balance between feeling good about my caregiving profession and not burning out professionally. But burnout is a subject that concerns many doctors around the world and is increasingly being discussed. We should all have psychological support when entering medicine!
Q: Would you recommend colleagues to come and work in the Far North? What would you tell them?
Dr. Prince: I would tell them they will have no regrets! Yes, it’s difficult, but it’s a unique type of practice and very rewarding on a human level.
Professionally, it is a general practice that is no longer seen in the city today. The spectrum is very broad, ranging from neonatology to geriatrics, from the simplest to the most complex. It’s very stimulating. Diagnostically, practice is also very different from what is done in the metropolis. Without a scanner, you really have to question and investigate to evaluate whether a patient should be evacuated by plane to Montreal or not. It’s not trivial. Decisions must be made judiciously and quickly.
The human experience is also unique. Inuit communities are little known, and the aspects relayed in the media are often negative due to their increased risk for addiction. However, they are cheerful and very warm people, with an extraordinary culture. I have learned a lot from them, including reconsidering the notion of time, reviewing my priorities, and approaching life one day at a time.
I am very grateful to them for accepting me. I am sometimes even greeted with a “Welcome home!” when I return from vacation...Being told that in Nunavik, I am also “at home,” touches me immensely. I have seen children grow up, adolescents become adults. A bond of trust has developed.
Of course, all of this comes with sacrifices like being away from family and loved ones. We miss birthdays, weddings, etc. But without hesitation, it’s worth it!
Q: What are the next steps in your career in Nunavik? Will you stay for a long time?
Dr. Prince: I take it one day at a time, especially since I am about to take maternity leave very soon. But if a full-time return to Nunavik is difficult with a newborn, I know that the Nunavummiuts [inhabitants of Nunavik] will always be part of my life and my practice.
I want to remain involved with these communities, whether on-site (by practicing there a few months a year) or in Montreal where many patients are transferred. Coming to be treated in a big city (Montreal, 1.7M inhabitants), in very large hospitals, can be very stressful for them. They express themselves much less verbally than Westerners, so we must know how to listen to them, dedicate the necessary time to them, consider their culture and beliefs. I would like to be the familiar face they will encounter when they are cared for away from home. It’s a bond I want to preserve.
This story was translated from Medscape France using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
In 2019, we interviewed Andrea Prince, MD, who was completing her internship in the Inuit village of Puvirnituq, a town of 2000 inhabitants located in Nunavik, in the Canadian Far North. Five years later, still in her position, what perspective does she have on her practice? Have the challenges of practicing medicine in a remote region within the Inuit community affected her vocation? Would she recommend this experience to young doctors?
Question: What position do you currently hold?
Dr. Prince: I am a full-time general practitioner at Puvirnituq Hospital. My responsibilities range from following up on hospitalized patients to those seen in outpatient clinics for chronic illnesses. Within our medical team, I receive patients in the emergency department (day and night shifts), and I travel to smaller dispensaries nearby, especially to the village of Akulivik. So, it’s quite a varied practice.
More recently, I have been involved in remote continuing medical education projects in collaboration with specialists based in Montreal. In this context, we are increasingly trying to collaborate with doctors from other indigenous communities, such as the Grand Council of the Cree, because our practices are quite similar.
Q: What is the patient volume you see?
Dr. Prince: We see approximately 20-30 patients per day in the clinic, plus about 10 by appointment, and dozens of calls from dispensaries, in addition to patients transferred from other villages. There are four daytime doctors (one at night) and about 15 nurses stationed full-time at Puvirnituq Hospital.
Our practice relies heavily on collaboration with the nursing team, which has an expanded role — they can manage certain patients according to the treatment plan established by the doctor and prescribe treatments (eg, antibiotics for uncomplicated otitis).
Q: Access to care in these isolated regions is considered difficult. Have you observed any improvement in the situation over the past 5 years? What about new material and human resources?
Dr. Prince: For the past year, we have had a Starlink internet connection at the hospital, which facilitates telemedicine exchanges with specialists; we can now send data and medical images to Montreal to obtain expertise much more easily. Previously, everything was done by phone or with significant delays. We do not yet have a cellular network, and all records are currently in paper format.
But the challenges remain numerous. Progress is very slow. Like everywhere in the country, we are experiencing a shortage of staff, particularly an insufficient number of nurses. But the impact is even more dramatic in these isolated territories. We have had to close dispensaries on the coast due to a lack of personnel and only offer emergency services. However, patients have no other options; they cannot drive to another hospital. In Nunavik, the road network is practically nonexistent, and travel to other regions is by plane (about a 2.5-hour medical evacuation trip).
So, sometimes, patients do not seek care in time, and when we finally see them, unfortunately, the issue can be quite advanced.
Q: What are the most pressing logistical needs?
Dr. Prince: We still do not have a scanner in the Far North. This has a significant impact on mortality, especially in the case of accidents and trauma, which are very common in these regions. “Residents of Nunavik are four times more likely to suffer trauma than the rest of Quebec’s population and 40 times more likely to die from it,” as recently reported in La Presse.
There has also been much discussion about cancer mortality, with a risk for death about 70% higher following a lung cancer diagnosis (reported by Medscape Medical News). We do not have a mammogram machine to diagnose breast cancer. Before the COVID-19 pandemic, equipped diagnostic teams sometimes traveled to the region, but this is no longer the case. Today, a patient needing a mammogram will have to travel to Montreal. The same goes for colonoscopies, but visits are becoming less frequent. Therefore, campaigns to screen for certain common types of cancer are practically nonexistent.
As for urgent surgeries (appendicitis, cesarean sections, trauma, etc.), patients must be transferred to Montreal by medical evacuation. We have a visiting surgeon twice a year.
Q: What improvement strategies do you foresee despite the lack of resources?
Dr. Prince: The saying “prevention is better than cure” makes perfect sense in such remote regions under extreme conditions (it is impossible to fly a medevac when it is too windy or during a snowstorm!). That’s why my colleagues and I believe that prevention should be the top priority in terms of healthcare intervention. It may seem obvious, but nothing is simple in the Far North.
Q: In which areas should prevention campaigns be prioritized in your opinion?
Dr. Prince: An example is wearing helmets. Practically no one wears this type of protection in the Far North. They use all-terrain vehicles that are dangerous and for which helmet use is crucial. But they are simply not available in stores. So, communication is difficult: We tell people, “you need a helmet for the ATV, another for the bike, for the snowmobile, for playing hockey, etc.” when it is difficult to obtain one. With traumatologists in Montreal, we had a project to create multifunctional helmets for children — to protect them but also to develop a culture of helmet use, which is not common practice in the community — but these are projects that take a lot of time and are more complex than they seem.
Villages still do not have running water. Therefore, it is difficult to give recommendations to patients as they live in sanitary conditions that are unseen elsewhere in Canada. Without clean water, we cannot ensure that wound care is done properly. Not to mention the occurrence of hepatitis A epidemics, like the one we had to face.
Residents also grapple with significant alcohol and smoking problems, but there is no detox center or dedicated psychological help on site. To follow a detox program, patients would have to leave, move away from their families, and that can be psychologically very destabilizing. I try, in my practice, to talk to my patients about this, especially pregnant women — because many continue to smoke or drink during their pregnancy — but we need more resources.
Q: What about women’s health in this region?
Dr. Prince: We are fortunate to have a team of midwives, several of whom are Inuit, who are of great help in accessing contraception, performing cervical cancer screening tests, etc. But some patients with high-risk pregnancies who should be transferred to Montreal refuse to give birth away from their families. Again, if we had the means to allow high-risk women — or those for whom continuous monitoring or a cesarean section may be necessary — to give birth here safely, it would be a big step. As for abortion, it is feasible but remains a very taboo subject in the community.
Regarding violence against women, I have not observed any particularly encouraging developments in the past 5 years, but recently, we met with the mayor about this, hoping that concrete actions will be taken to help victims of violence.
Q: What is the predominant feeling in your daily life in a situation that is slow to evolve?
Dr. Prince: I remain hopeful for my patients. We must continue to fight! Initiatives must also come from the communities themselves; they must be involved in developing solutions. Because patients, too, need to have hope. They have the right to be cared for like other inhabitants of Canada.
On my part, I try to find a balance between feeling good about my caregiving profession and not burning out professionally. But burnout is a subject that concerns many doctors around the world and is increasingly being discussed. We should all have psychological support when entering medicine!
Q: Would you recommend colleagues to come and work in the Far North? What would you tell them?
Dr. Prince: I would tell them they will have no regrets! Yes, it’s difficult, but it’s a unique type of practice and very rewarding on a human level.
Professionally, it is a general practice that is no longer seen in the city today. The spectrum is very broad, ranging from neonatology to geriatrics, from the simplest to the most complex. It’s very stimulating. Diagnostically, practice is also very different from what is done in the metropolis. Without a scanner, you really have to question and investigate to evaluate whether a patient should be evacuated by plane to Montreal or not. It’s not trivial. Decisions must be made judiciously and quickly.
The human experience is also unique. Inuit communities are little known, and the aspects relayed in the media are often negative due to their increased risk for addiction. However, they are cheerful and very warm people, with an extraordinary culture. I have learned a lot from them, including reconsidering the notion of time, reviewing my priorities, and approaching life one day at a time.
I am very grateful to them for accepting me. I am sometimes even greeted with a “Welcome home!” when I return from vacation...Being told that in Nunavik, I am also “at home,” touches me immensely. I have seen children grow up, adolescents become adults. A bond of trust has developed.
Of course, all of this comes with sacrifices like being away from family and loved ones. We miss birthdays, weddings, etc. But without hesitation, it’s worth it!
Q: What are the next steps in your career in Nunavik? Will you stay for a long time?
Dr. Prince: I take it one day at a time, especially since I am about to take maternity leave very soon. But if a full-time return to Nunavik is difficult with a newborn, I know that the Nunavummiuts [inhabitants of Nunavik] will always be part of my life and my practice.
I want to remain involved with these communities, whether on-site (by practicing there a few months a year) or in Montreal where many patients are transferred. Coming to be treated in a big city (Montreal, 1.7M inhabitants), in very large hospitals, can be very stressful for them. They express themselves much less verbally than Westerners, so we must know how to listen to them, dedicate the necessary time to them, consider their culture and beliefs. I would like to be the familiar face they will encounter when they are cared for away from home. It’s a bond I want to preserve.
This story was translated from Medscape France using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
In 2019, we interviewed Andrea Prince, MD, who was completing her internship in the Inuit village of Puvirnituq, a town of 2000 inhabitants located in Nunavik, in the Canadian Far North. Five years later, still in her position, what perspective does she have on her practice? Have the challenges of practicing medicine in a remote region within the Inuit community affected her vocation? Would she recommend this experience to young doctors?
Question: What position do you currently hold?
Dr. Prince: I am a full-time general practitioner at Puvirnituq Hospital. My responsibilities range from following up on hospitalized patients to those seen in outpatient clinics for chronic illnesses. Within our medical team, I receive patients in the emergency department (day and night shifts), and I travel to smaller dispensaries nearby, especially to the village of Akulivik. So, it’s quite a varied practice.
More recently, I have been involved in remote continuing medical education projects in collaboration with specialists based in Montreal. In this context, we are increasingly trying to collaborate with doctors from other indigenous communities, such as the Grand Council of the Cree, because our practices are quite similar.
Q: What is the patient volume you see?
Dr. Prince: We see approximately 20-30 patients per day in the clinic, plus about 10 by appointment, and dozens of calls from dispensaries, in addition to patients transferred from other villages. There are four daytime doctors (one at night) and about 15 nurses stationed full-time at Puvirnituq Hospital.
Our practice relies heavily on collaboration with the nursing team, which has an expanded role — they can manage certain patients according to the treatment plan established by the doctor and prescribe treatments (eg, antibiotics for uncomplicated otitis).
Q: Access to care in these isolated regions is considered difficult. Have you observed any improvement in the situation over the past 5 years? What about new material and human resources?
Dr. Prince: For the past year, we have had a Starlink internet connection at the hospital, which facilitates telemedicine exchanges with specialists; we can now send data and medical images to Montreal to obtain expertise much more easily. Previously, everything was done by phone or with significant delays. We do not yet have a cellular network, and all records are currently in paper format.
But the challenges remain numerous. Progress is very slow. Like everywhere in the country, we are experiencing a shortage of staff, particularly an insufficient number of nurses. But the impact is even more dramatic in these isolated territories. We have had to close dispensaries on the coast due to a lack of personnel and only offer emergency services. However, patients have no other options; they cannot drive to another hospital. In Nunavik, the road network is practically nonexistent, and travel to other regions is by plane (about a 2.5-hour medical evacuation trip).
So, sometimes, patients do not seek care in time, and when we finally see them, unfortunately, the issue can be quite advanced.
Q: What are the most pressing logistical needs?
Dr. Prince: We still do not have a scanner in the Far North. This has a significant impact on mortality, especially in the case of accidents and trauma, which are very common in these regions. “Residents of Nunavik are four times more likely to suffer trauma than the rest of Quebec’s population and 40 times more likely to die from it,” as recently reported in La Presse.
There has also been much discussion about cancer mortality, with a risk for death about 70% higher following a lung cancer diagnosis (reported by Medscape Medical News). We do not have a mammogram machine to diagnose breast cancer. Before the COVID-19 pandemic, equipped diagnostic teams sometimes traveled to the region, but this is no longer the case. Today, a patient needing a mammogram will have to travel to Montreal. The same goes for colonoscopies, but visits are becoming less frequent. Therefore, campaigns to screen for certain common types of cancer are practically nonexistent.
As for urgent surgeries (appendicitis, cesarean sections, trauma, etc.), patients must be transferred to Montreal by medical evacuation. We have a visiting surgeon twice a year.
Q: What improvement strategies do you foresee despite the lack of resources?
Dr. Prince: The saying “prevention is better than cure” makes perfect sense in such remote regions under extreme conditions (it is impossible to fly a medevac when it is too windy or during a snowstorm!). That’s why my colleagues and I believe that prevention should be the top priority in terms of healthcare intervention. It may seem obvious, but nothing is simple in the Far North.
Q: In which areas should prevention campaigns be prioritized in your opinion?
Dr. Prince: An example is wearing helmets. Practically no one wears this type of protection in the Far North. They use all-terrain vehicles that are dangerous and for which helmet use is crucial. But they are simply not available in stores. So, communication is difficult: We tell people, “you need a helmet for the ATV, another for the bike, for the snowmobile, for playing hockey, etc.” when it is difficult to obtain one. With traumatologists in Montreal, we had a project to create multifunctional helmets for children — to protect them but also to develop a culture of helmet use, which is not common practice in the community — but these are projects that take a lot of time and are more complex than they seem.
Villages still do not have running water. Therefore, it is difficult to give recommendations to patients as they live in sanitary conditions that are unseen elsewhere in Canada. Without clean water, we cannot ensure that wound care is done properly. Not to mention the occurrence of hepatitis A epidemics, like the one we had to face.
Residents also grapple with significant alcohol and smoking problems, but there is no detox center or dedicated psychological help on site. To follow a detox program, patients would have to leave, move away from their families, and that can be psychologically very destabilizing. I try, in my practice, to talk to my patients about this, especially pregnant women — because many continue to smoke or drink during their pregnancy — but we need more resources.
Q: What about women’s health in this region?
Dr. Prince: We are fortunate to have a team of midwives, several of whom are Inuit, who are of great help in accessing contraception, performing cervical cancer screening tests, etc. But some patients with high-risk pregnancies who should be transferred to Montreal refuse to give birth away from their families. Again, if we had the means to allow high-risk women — or those for whom continuous monitoring or a cesarean section may be necessary — to give birth here safely, it would be a big step. As for abortion, it is feasible but remains a very taboo subject in the community.
Regarding violence against women, I have not observed any particularly encouraging developments in the past 5 years, but recently, we met with the mayor about this, hoping that concrete actions will be taken to help victims of violence.
Q: What is the predominant feeling in your daily life in a situation that is slow to evolve?
Dr. Prince: I remain hopeful for my patients. We must continue to fight! Initiatives must also come from the communities themselves; they must be involved in developing solutions. Because patients, too, need to have hope. They have the right to be cared for like other inhabitants of Canada.
On my part, I try to find a balance between feeling good about my caregiving profession and not burning out professionally. But burnout is a subject that concerns many doctors around the world and is increasingly being discussed. We should all have psychological support when entering medicine!
Q: Would you recommend colleagues to come and work in the Far North? What would you tell them?
Dr. Prince: I would tell them they will have no regrets! Yes, it’s difficult, but it’s a unique type of practice and very rewarding on a human level.
Professionally, it is a general practice that is no longer seen in the city today. The spectrum is very broad, ranging from neonatology to geriatrics, from the simplest to the most complex. It’s very stimulating. Diagnostically, practice is also very different from what is done in the metropolis. Without a scanner, you really have to question and investigate to evaluate whether a patient should be evacuated by plane to Montreal or not. It’s not trivial. Decisions must be made judiciously and quickly.
The human experience is also unique. Inuit communities are little known, and the aspects relayed in the media are often negative due to their increased risk for addiction. However, they are cheerful and very warm people, with an extraordinary culture. I have learned a lot from them, including reconsidering the notion of time, reviewing my priorities, and approaching life one day at a time.
I am very grateful to them for accepting me. I am sometimes even greeted with a “Welcome home!” when I return from vacation...Being told that in Nunavik, I am also “at home,” touches me immensely. I have seen children grow up, adolescents become adults. A bond of trust has developed.
Of course, all of this comes with sacrifices like being away from family and loved ones. We miss birthdays, weddings, etc. But without hesitation, it’s worth it!
Q: What are the next steps in your career in Nunavik? Will you stay for a long time?
Dr. Prince: I take it one day at a time, especially since I am about to take maternity leave very soon. But if a full-time return to Nunavik is difficult with a newborn, I know that the Nunavummiuts [inhabitants of Nunavik] will always be part of my life and my practice.
I want to remain involved with these communities, whether on-site (by practicing there a few months a year) or in Montreal where many patients are transferred. Coming to be treated in a big city (Montreal, 1.7M inhabitants), in very large hospitals, can be very stressful for them. They express themselves much less verbally than Westerners, so we must know how to listen to them, dedicate the necessary time to them, consider their culture and beliefs. I would like to be the familiar face they will encounter when they are cared for away from home. It’s a bond I want to preserve.
This story was translated from Medscape France using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Vitamin D Supplements May Be a Double-Edged Sword
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Imagine, if you will, the great Cathedral of Our Lady of Correlation. You walk through the majestic oak doors depicting the link between ice cream sales and shark attacks, past the rose window depicting the cardiovascular benefits of red wine, and down the aisles frescoed in dramatic images showing how Facebook usage is associated with less life satisfaction. And then you reach the altar, the holy of holies where, emblazoned in shimmering pyrite, you see the patron saint of this church: vitamin D.
Yes, if you’ve watched this space, then you know that I have little truck with the wildly popular supplement. In all of clinical research, I believe that there is no molecule with stronger data for correlation and weaker data for causation.
Low serum vitamin D levels have been linked to higher risks for heart disease, cancer, falls, COVID, dementia, C diff, and others. And yet, when we do randomized trials of vitamin D supplementation — the thing that can prove that the low level was causally linked to the outcome of interest — we get negative results.
Trials aren’t perfect, of course, and we’ll talk in a moment about a big one that had some issues. But we are at a point where we need to either be vitamin D apologists, saying, “Forget what those lying RCTs tell you and buy this supplement” — an $800 million-a-year industry, by the way — or conclude that vitamin D levels are a convenient marker of various lifestyle factors that are associated with better outcomes: markers of exercise, getting outside, eating a varied diet.
Or perhaps vitamin D supplements have real effects. It’s just that the beneficial effects are matched by the harmful ones. Stay tuned.
The Women’s Health Initiative remains among the largest randomized trials of vitamin D and calcium supplementation ever conducted — and a major contributor to the negative outcomes of vitamin D trials.
But if you dig into the inclusion and exclusion criteria for this trial, you’ll find that individuals were allowed to continue taking vitamins and supplements while they were in the trial, regardless of their randomization status. In fact, the majority took supplements at baseline, and more took supplements over time.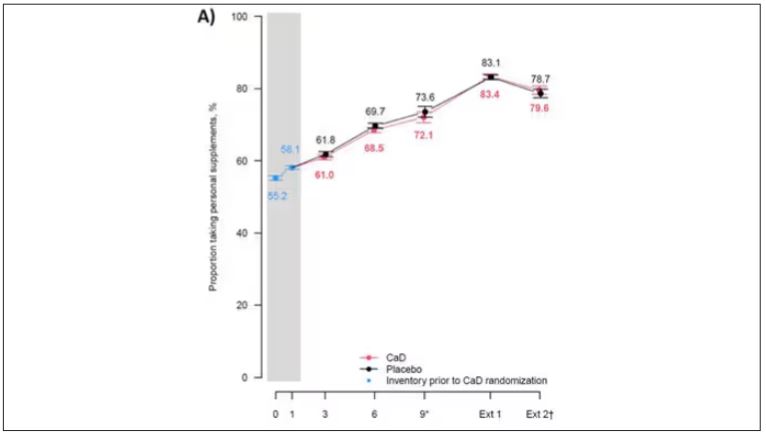
That means, of course, that people in the placebo group, who were getting sugar pills instead of vitamin D and calcium, may have been taking vitamin D and calcium on the side. That would certainly bias the results of the trial toward the null, which is what the primary analyses showed. To wit, the original analysis of the Women’s Health Initiative trial showed no effect of randomization to vitamin D supplementation on improving cancer or cardiovascular outcomes.
But the Women’s Health Initiative trial started 30 years ago. Today, with the benefit of decades of follow-up, we can re-investigate — and perhaps re-litigate — those findings, courtesy of this study, “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women” appearing in Annals of Internal Medicine.
Dr Cynthia Thomson, of the Mel and Enid Zuckerman College of Public Health at the University of Arizona, and colleagues led this updated analysis focused on two findings that had been hinted at, but not statistically confirmed, in other vitamin D studies: a potential for the supplement to reduce the risk for cancer, and a potential for it to increase the risk for heart disease.
The randomized trial itself only lasted 7 years. What we are seeing in this analysis of 36,282 women is outcomes that happened at any time from randomization to the end of 2023 — around 20 years after the randomization to supplementation stopped. But, the researchers would argue, that’s probably okay. Cancer and heart disease take time to develop; we see lung cancer long after people stop smoking. So a history of consistent vitamin D supplementation may indeed be protective — or harmful.
Here are the top-line results. Those randomized to vitamin D and calcium supplementation had a 7% reduction in the rate of death from cancer, driven primarily by a reduction in colorectal cancer. This was statistically significant. Also statistically significant? Those randomized to supplementation had a 6% increase in the rate of death from cardiovascular disease. Put those findings together and what do you get? Stone-cold nothing, in terms of overall mortality.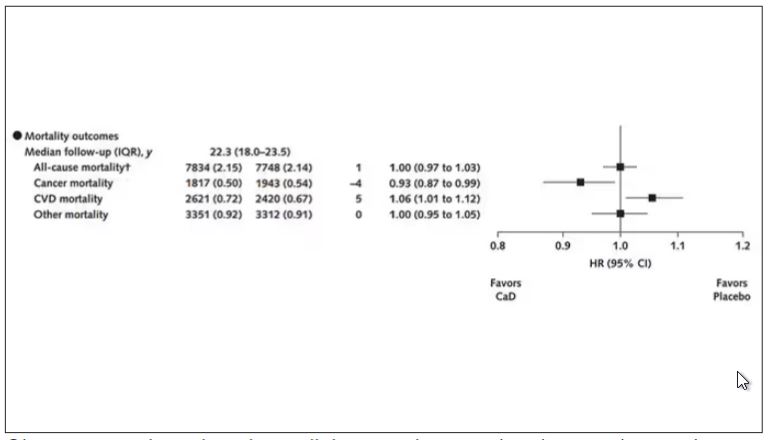
Okay, you say, but what about all that supplementation that was happening outside of the context of the trial, biasing our results toward the null?
The researchers finally clue us in.
First of all, I’ll tell you that, yes, people who were supplementing outside of the trial had higher baseline vitamin D levels — a median of 54.5 nmol/L vs 32.8 nmol/L. This may be because they were supplementing with vitamin D, but it could also be because people who take supplements tend to do other healthy things — another correlation to add to the great cathedral.
To get a better view of the real effects of randomization, the authors restricted the analysis to just those who did not use outside supplements. If vitamin D supplements help, then these are the people they should help. This group had about a 11% reduction in the incidence of cancer — statistically significant — and a 7% reduction in cancer mortality that did not meet the bar for statistical significance.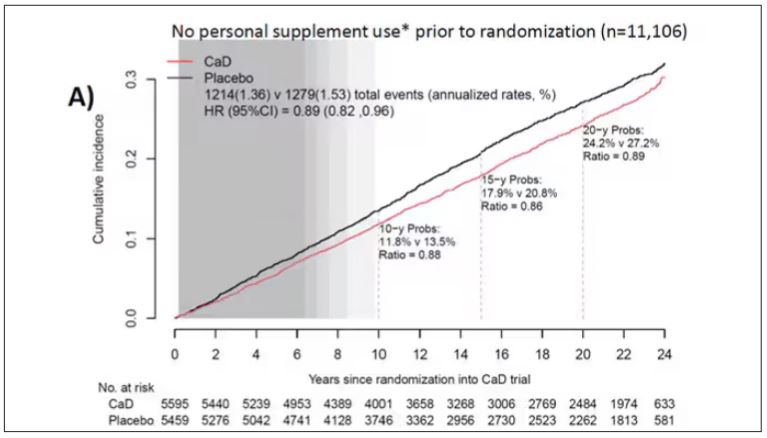
There was no increase in cardiovascular disease among this group. But this small effect on cancer was nowhere near enough to significantly reduce the rate of all-cause mortality.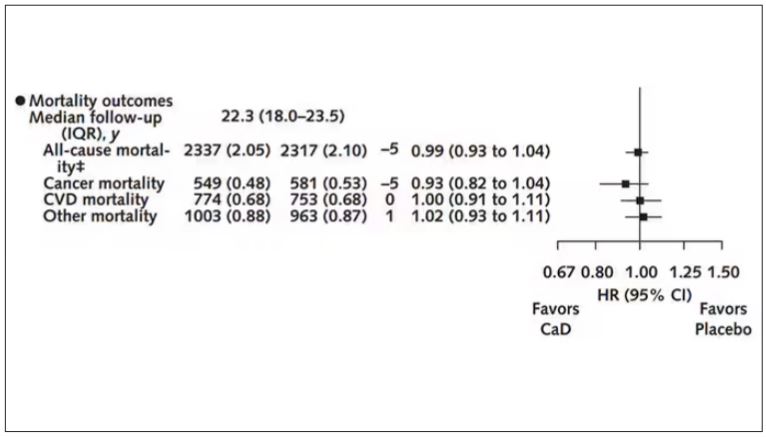
Among those using supplements, vitamin D supplementation didn’t really move the needle on any outcome.
I know what you’re thinking: How many of these women were vitamin D deficient when we got started? These results may simply be telling us that people who have normal vitamin D levels are fine to go without supplementation.
Nearly three fourths of women who were not taking supplements entered the trial with vitamin D levels below the 50 nmol/L cutoff that the authors suggest would qualify for deficiency. Around half of those who used supplements were deficient. And yet, frustratingly, I could not find data on the effect of randomization to supplementation stratified by baseline vitamin D level. I even reached out to Dr Thomson to ask about this. She replied, “We did not stratify on baseline values because the numbers are too small statistically to test this.” Sorry.
In the meantime, I can tell you that for your “average woman,” vitamin D supplementation likely has no effect on mortality. It might modestly reduce the risk for certain cancers while increasing the risk for heart disease (probably through coronary calcification). So, there might be some room for personalization here. Perhaps women with a strong family history of cancer or other risk factors would do better with supplements, and those with a high risk for heart disease would do worse. Seems like a strategy that could be tested in a clinical trial. But maybe we could ask the participants to give up their extracurricular supplement use before they enter the trial. F. Perry Wilson, MD, MSCE, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his book, How Medicine Works and When It Doesn’t, is available now.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Imagine, if you will, the great Cathedral of Our Lady of Correlation. You walk through the majestic oak doors depicting the link between ice cream sales and shark attacks, past the rose window depicting the cardiovascular benefits of red wine, and down the aisles frescoed in dramatic images showing how Facebook usage is associated with less life satisfaction. And then you reach the altar, the holy of holies where, emblazoned in shimmering pyrite, you see the patron saint of this church: vitamin D.
Yes, if you’ve watched this space, then you know that I have little truck with the wildly popular supplement. In all of clinical research, I believe that there is no molecule with stronger data for correlation and weaker data for causation.
Low serum vitamin D levels have been linked to higher risks for heart disease, cancer, falls, COVID, dementia, C diff, and others. And yet, when we do randomized trials of vitamin D supplementation — the thing that can prove that the low level was causally linked to the outcome of interest — we get negative results.
Trials aren’t perfect, of course, and we’ll talk in a moment about a big one that had some issues. But we are at a point where we need to either be vitamin D apologists, saying, “Forget what those lying RCTs tell you and buy this supplement” — an $800 million-a-year industry, by the way — or conclude that vitamin D levels are a convenient marker of various lifestyle factors that are associated with better outcomes: markers of exercise, getting outside, eating a varied diet.
Or perhaps vitamin D supplements have real effects. It’s just that the beneficial effects are matched by the harmful ones. Stay tuned.
The Women’s Health Initiative remains among the largest randomized trials of vitamin D and calcium supplementation ever conducted — and a major contributor to the negative outcomes of vitamin D trials.
But if you dig into the inclusion and exclusion criteria for this trial, you’ll find that individuals were allowed to continue taking vitamins and supplements while they were in the trial, regardless of their randomization status. In fact, the majority took supplements at baseline, and more took supplements over time.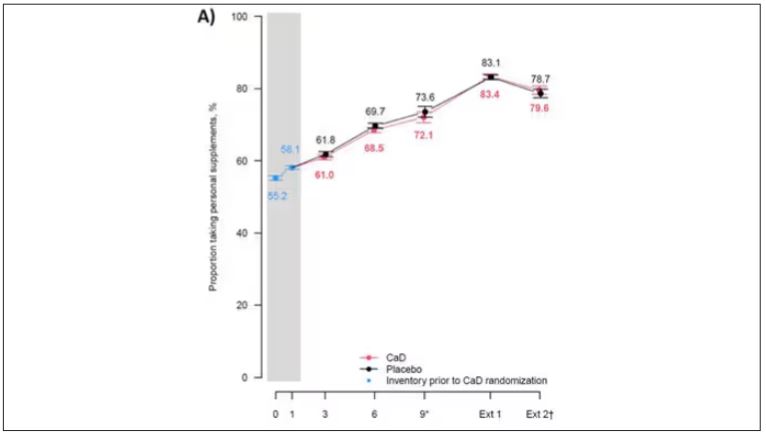
That means, of course, that people in the placebo group, who were getting sugar pills instead of vitamin D and calcium, may have been taking vitamin D and calcium on the side. That would certainly bias the results of the trial toward the null, which is what the primary analyses showed. To wit, the original analysis of the Women’s Health Initiative trial showed no effect of randomization to vitamin D supplementation on improving cancer or cardiovascular outcomes.
But the Women’s Health Initiative trial started 30 years ago. Today, with the benefit of decades of follow-up, we can re-investigate — and perhaps re-litigate — those findings, courtesy of this study, “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women” appearing in Annals of Internal Medicine.
Dr Cynthia Thomson, of the Mel and Enid Zuckerman College of Public Health at the University of Arizona, and colleagues led this updated analysis focused on two findings that had been hinted at, but not statistically confirmed, in other vitamin D studies: a potential for the supplement to reduce the risk for cancer, and a potential for it to increase the risk for heart disease.
The randomized trial itself only lasted 7 years. What we are seeing in this analysis of 36,282 women is outcomes that happened at any time from randomization to the end of 2023 — around 20 years after the randomization to supplementation stopped. But, the researchers would argue, that’s probably okay. Cancer and heart disease take time to develop; we see lung cancer long after people stop smoking. So a history of consistent vitamin D supplementation may indeed be protective — or harmful.
Here are the top-line results. Those randomized to vitamin D and calcium supplementation had a 7% reduction in the rate of death from cancer, driven primarily by a reduction in colorectal cancer. This was statistically significant. Also statistically significant? Those randomized to supplementation had a 6% increase in the rate of death from cardiovascular disease. Put those findings together and what do you get? Stone-cold nothing, in terms of overall mortality.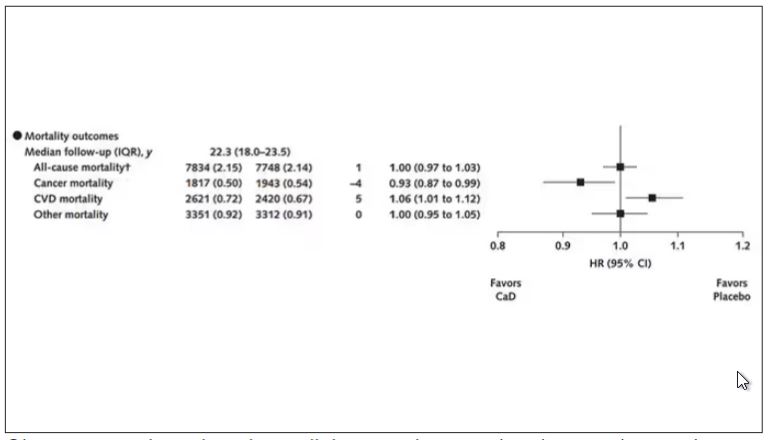
Okay, you say, but what about all that supplementation that was happening outside of the context of the trial, biasing our results toward the null?
The researchers finally clue us in.
First of all, I’ll tell you that, yes, people who were supplementing outside of the trial had higher baseline vitamin D levels — a median of 54.5 nmol/L vs 32.8 nmol/L. This may be because they were supplementing with vitamin D, but it could also be because people who take supplements tend to do other healthy things — another correlation to add to the great cathedral.
To get a better view of the real effects of randomization, the authors restricted the analysis to just those who did not use outside supplements. If vitamin D supplements help, then these are the people they should help. This group had about a 11% reduction in the incidence of cancer — statistically significant — and a 7% reduction in cancer mortality that did not meet the bar for statistical significance.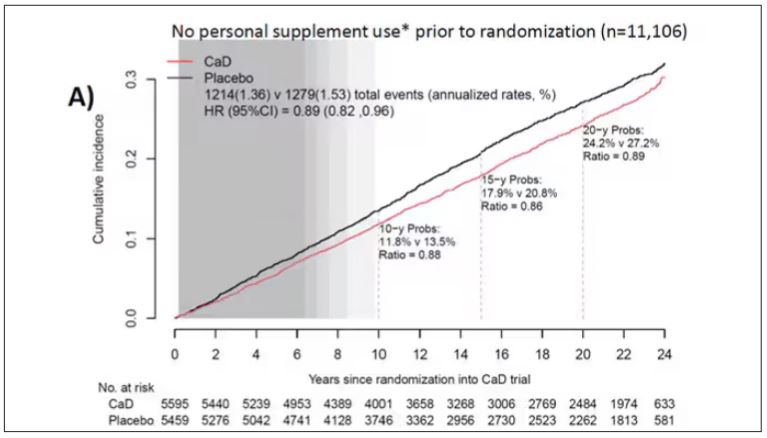
There was no increase in cardiovascular disease among this group. But this small effect on cancer was nowhere near enough to significantly reduce the rate of all-cause mortality.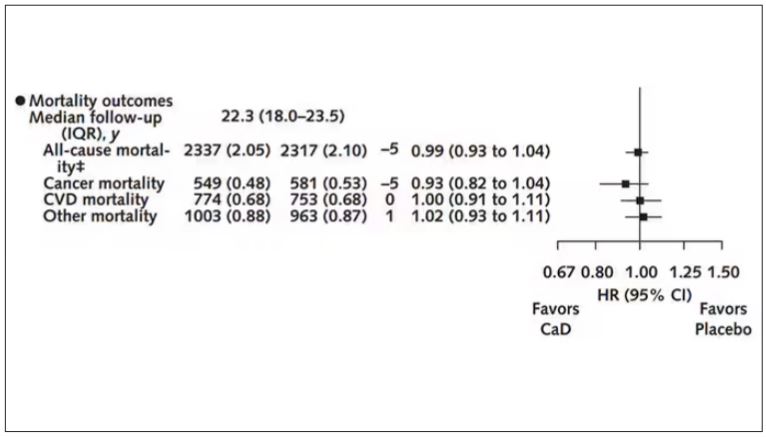
Among those using supplements, vitamin D supplementation didn’t really move the needle on any outcome.
I know what you’re thinking: How many of these women were vitamin D deficient when we got started? These results may simply be telling us that people who have normal vitamin D levels are fine to go without supplementation.
Nearly three fourths of women who were not taking supplements entered the trial with vitamin D levels below the 50 nmol/L cutoff that the authors suggest would qualify for deficiency. Around half of those who used supplements were deficient. And yet, frustratingly, I could not find data on the effect of randomization to supplementation stratified by baseline vitamin D level. I even reached out to Dr Thomson to ask about this. She replied, “We did not stratify on baseline values because the numbers are too small statistically to test this.” Sorry.
In the meantime, I can tell you that for your “average woman,” vitamin D supplementation likely has no effect on mortality. It might modestly reduce the risk for certain cancers while increasing the risk for heart disease (probably through coronary calcification). So, there might be some room for personalization here. Perhaps women with a strong family history of cancer or other risk factors would do better with supplements, and those with a high risk for heart disease would do worse. Seems like a strategy that could be tested in a clinical trial. But maybe we could ask the participants to give up their extracurricular supplement use before they enter the trial. F. Perry Wilson, MD, MSCE, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his book, How Medicine Works and When It Doesn’t, is available now.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Imagine, if you will, the great Cathedral of Our Lady of Correlation. You walk through the majestic oak doors depicting the link between ice cream sales and shark attacks, past the rose window depicting the cardiovascular benefits of red wine, and down the aisles frescoed in dramatic images showing how Facebook usage is associated with less life satisfaction. And then you reach the altar, the holy of holies where, emblazoned in shimmering pyrite, you see the patron saint of this church: vitamin D.
Yes, if you’ve watched this space, then you know that I have little truck with the wildly popular supplement. In all of clinical research, I believe that there is no molecule with stronger data for correlation and weaker data for causation.
Low serum vitamin D levels have been linked to higher risks for heart disease, cancer, falls, COVID, dementia, C diff, and others. And yet, when we do randomized trials of vitamin D supplementation — the thing that can prove that the low level was causally linked to the outcome of interest — we get negative results.
Trials aren’t perfect, of course, and we’ll talk in a moment about a big one that had some issues. But we are at a point where we need to either be vitamin D apologists, saying, “Forget what those lying RCTs tell you and buy this supplement” — an $800 million-a-year industry, by the way — or conclude that vitamin D levels are a convenient marker of various lifestyle factors that are associated with better outcomes: markers of exercise, getting outside, eating a varied diet.
Or perhaps vitamin D supplements have real effects. It’s just that the beneficial effects are matched by the harmful ones. Stay tuned.
The Women’s Health Initiative remains among the largest randomized trials of vitamin D and calcium supplementation ever conducted — and a major contributor to the negative outcomes of vitamin D trials.
But if you dig into the inclusion and exclusion criteria for this trial, you’ll find that individuals were allowed to continue taking vitamins and supplements while they were in the trial, regardless of their randomization status. In fact, the majority took supplements at baseline, and more took supplements over time.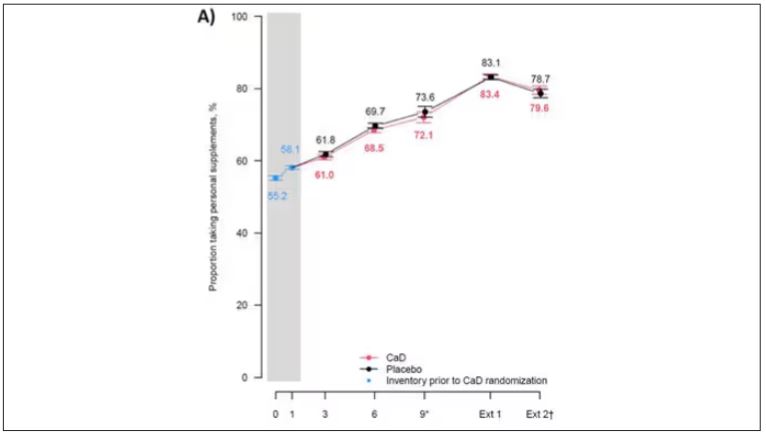
That means, of course, that people in the placebo group, who were getting sugar pills instead of vitamin D and calcium, may have been taking vitamin D and calcium on the side. That would certainly bias the results of the trial toward the null, which is what the primary analyses showed. To wit, the original analysis of the Women’s Health Initiative trial showed no effect of randomization to vitamin D supplementation on improving cancer or cardiovascular outcomes.
But the Women’s Health Initiative trial started 30 years ago. Today, with the benefit of decades of follow-up, we can re-investigate — and perhaps re-litigate — those findings, courtesy of this study, “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women” appearing in Annals of Internal Medicine.
Dr Cynthia Thomson, of the Mel and Enid Zuckerman College of Public Health at the University of Arizona, and colleagues led this updated analysis focused on two findings that had been hinted at, but not statistically confirmed, in other vitamin D studies: a potential for the supplement to reduce the risk for cancer, and a potential for it to increase the risk for heart disease.
The randomized trial itself only lasted 7 years. What we are seeing in this analysis of 36,282 women is outcomes that happened at any time from randomization to the end of 2023 — around 20 years after the randomization to supplementation stopped. But, the researchers would argue, that’s probably okay. Cancer and heart disease take time to develop; we see lung cancer long after people stop smoking. So a history of consistent vitamin D supplementation may indeed be protective — or harmful.
Here are the top-line results. Those randomized to vitamin D and calcium supplementation had a 7% reduction in the rate of death from cancer, driven primarily by a reduction in colorectal cancer. This was statistically significant. Also statistically significant? Those randomized to supplementation had a 6% increase in the rate of death from cardiovascular disease. Put those findings together and what do you get? Stone-cold nothing, in terms of overall mortality.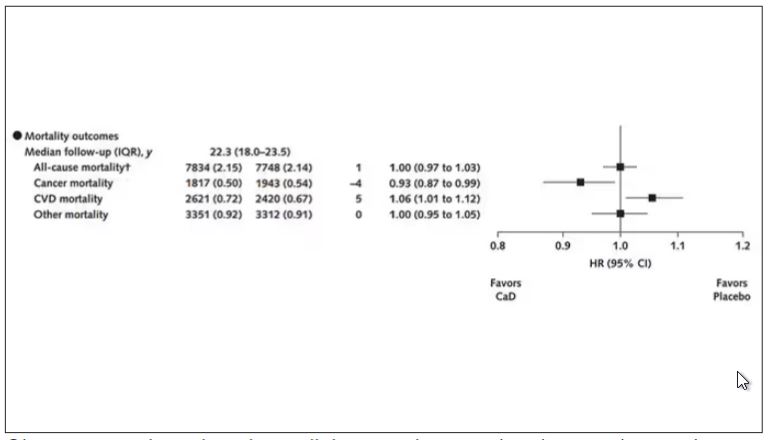
Okay, you say, but what about all that supplementation that was happening outside of the context of the trial, biasing our results toward the null?
The researchers finally clue us in.
First of all, I’ll tell you that, yes, people who were supplementing outside of the trial had higher baseline vitamin D levels — a median of 54.5 nmol/L vs 32.8 nmol/L. This may be because they were supplementing with vitamin D, but it could also be because people who take supplements tend to do other healthy things — another correlation to add to the great cathedral.
To get a better view of the real effects of randomization, the authors restricted the analysis to just those who did not use outside supplements. If vitamin D supplements help, then these are the people they should help. This group had about a 11% reduction in the incidence of cancer — statistically significant — and a 7% reduction in cancer mortality that did not meet the bar for statistical significance.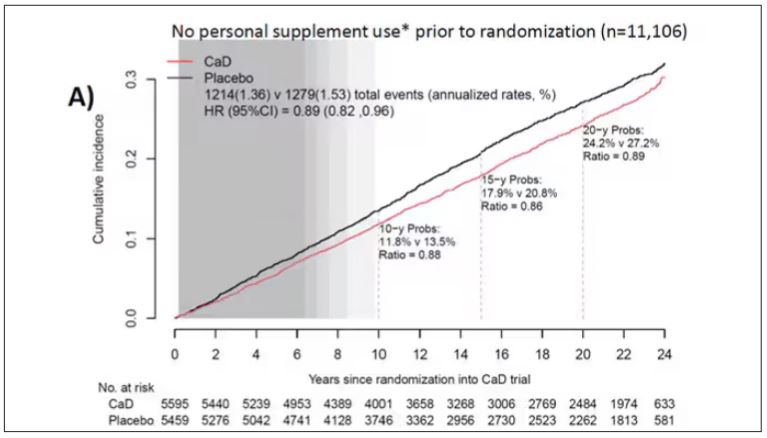
There was no increase in cardiovascular disease among this group. But this small effect on cancer was nowhere near enough to significantly reduce the rate of all-cause mortality.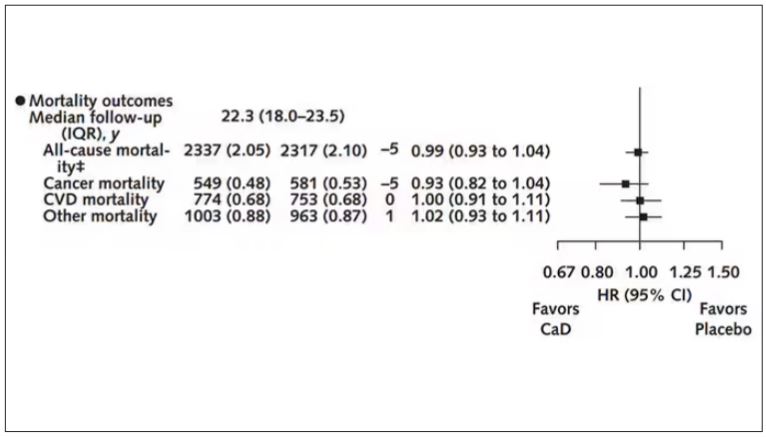
Among those using supplements, vitamin D supplementation didn’t really move the needle on any outcome.
I know what you’re thinking: How many of these women were vitamin D deficient when we got started? These results may simply be telling us that people who have normal vitamin D levels are fine to go without supplementation.
Nearly three fourths of women who were not taking supplements entered the trial with vitamin D levels below the 50 nmol/L cutoff that the authors suggest would qualify for deficiency. Around half of those who used supplements were deficient. And yet, frustratingly, I could not find data on the effect of randomization to supplementation stratified by baseline vitamin D level. I even reached out to Dr Thomson to ask about this. She replied, “We did not stratify on baseline values because the numbers are too small statistically to test this.” Sorry.
In the meantime, I can tell you that for your “average woman,” vitamin D supplementation likely has no effect on mortality. It might modestly reduce the risk for certain cancers while increasing the risk for heart disease (probably through coronary calcification). So, there might be some room for personalization here. Perhaps women with a strong family history of cancer or other risk factors would do better with supplements, and those with a high risk for heart disease would do worse. Seems like a strategy that could be tested in a clinical trial. But maybe we could ask the participants to give up their extracurricular supplement use before they enter the trial. F. Perry Wilson, MD, MSCE, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his book, How Medicine Works and When It Doesn’t, is available now.
Long-Term Calcium and Vitamin D: Cancer Deaths Down, CVD Deaths Up in Older Women?
Some doctors may be scratching their heads over a new analysis reporting that combined calcium and vitamin D (CaD) supplements appear to be associated with a slight 6% increase in cardiovascular (CVD) mortality, a slight 7% decrease in cancer risk, and no effect on osteoporotic fracture in postmenopausal women.
The study, in Annals of Internal Medicine, found no effect of supplementation on all-cause mortality.
The findings emerged from an analysis of more than 20 years’ follow-up data on a randomized trial in postmenopausal women conducted as part of the Women’s Health Initiative (WHI).
Cynthia A. Thomson, PhD, RD, first author and cancer prevention scientist at the Arizona Cancer Center and a professor of health promotion sciences at the University of Arizona in Tucson said the findings recommend individualized assessment of the need for supplements for older women as they consider them in hopes of preventing fractures.
“Evaluate your patients individually and understand that there are some who may benefit from supplementation, for example, in terms of reducing colorectal cancer mortality,” Dr. Thomson said in an interview. The approach should be nuanced. “If you check the adequacy of vitamin D and calcium in their diets, supplementation may not be needed.” She added that supplementation is best considered in the context of a woman’s overall health profile, including risk factors for fracture, heart disease, and cancer, especially colorectal cancer (CRC).
Study Details
The investigators conducted postintervention follow-up of the WHI’s 7-year multicenter randomized intervention trial of CaD vs placebo.
Since existing evidence of long-term health outcomes was limited, the trial, begun in 1999 and closed in 2005, enrolled 36,282 postmenopausal women (mean age 62) with no history of breast or colorectal cancer. They were randomly assigned 1:1 to supplementation with 1000 mg of calcium carbonate (400 mg elemental calcium) plus 400 IU of vitamin D3 daily or placebo, taken twice daily in half doses.
Study outcomes were incidence of CRC, total and invasive breast cancer; disease-specific and all-cause mortality; total CVD; and hip fracture measured through December 2020, with analyses stratified by personal supplement usage.
Cancer. CaD was associated with reduced incident total cancer, CRC, and invasive breast cancer — notably among participants not taking CaD before randomization. Cancer incidence estimates varied widely, the authors noted, when stratified by supplement use before randomization. Noting that CaD seemed to have more cancer-related impact in those without prior supplementation, the authors suggested supplementation may affect cancer biology primarily by augmenting nutrient insufficiency.
An estimated 7% reduction in cancer mortality was observed after a median cumulative follow-up of 22.3 years: 1817 vs 1943 deaths (hazard ratio, 0.93; 95% CI, 0.87-0.99).
CVD. An estimated 6% increase in CVD mortality was seen in the CaD group: 2621 vs 2420 deaths (HR, 1.06; 95% CI, 1.01-1.12). Pretrial supplement users were found to be at higher CVD risk.
Hip fracture. No effect on hip fracture risk was measured, but the authors cautioned that hip fracture and CVD outcomes were available only for a subset of participants, and the effects of calcium alone vs vitamin D alone vs the combination could not be disentangled.
In a small subgroup analysis, some CaD users were seen to respond in terms of bone mineral density but since only 4 of the study’s 40 sites collected such information, the study was underpowered to examine the effect. ”Many other studies, however, show a response to supplementation in women who already have bone mineral deficits,” Dr. Thomson said.
The Calcification Question
One of the possible mechanisms of harm is that high-dose calcium supplements can increase the rate of blood coagulation and promote vascular calcification, said Emma Laing, PhD, RD, director of dietetics at the University of Georgia in Athens and a spokesperson for the Chicago-based Academy of Nutrition and Dietetics.
“Other factors that should be considered when determining a patient’s CVD risk are race, genetic predisposition, medical and social history, response to stress, and lifestyle behaviors, as well as the length of time supplements have been consumed,” added Dr. Laing, who was not involved in the WHI analysis.
“We asked ourselves if CaD supplements might contribute to calcification of the coronary arteries, since some believe this to be the case, although the literature is mixed,” said Dr. Thomson.
“So we did a shorter ancillary study in a small sample of several hundred [women] to see if there was any increase in calcification” and no difference was seen on imaging across the two arms. “However, women who were already on supplements before entering the study seemed to be at higher CVD risk,” she said.
Added study coauthor JoAnn E. Manson, MD, DrPH, chief of the division of preventive medicine at Brigham and Women’s Hospital and professor of women’s health at Harvard Medical School, both in Boston: “With no increase or decrease in coronary artery calcium at the end of the trial, we don’t believe starting or continuing calcium/vitamin D supplements should require screening for coronary artery disease.”
Some randomized trials and systematic reviews, however, have observed an increased risk of CVD in healthy patients on calcium supplements, with one Korean meta-analysis reporting a 15% increase in CVD risk in healthy postmenopausal women taking calcium supplements. Another meta-analysis found a link between calcium supplements and a greater risk of various cardiovascular outcomes, especially myocardial infarction.
Vitamin D Supplementation
As for vitamin D only supplementation, an updated meta-analysis including more than 83,000 individuals showed that it confers no cardiovascular protection and is therefore not indicated for this purpose.
Practice Considerations
Offering an outsider’s perspective, Sarah G. Candler, MD, MPH, an internist in Houston specializing in primary care for older high-risk adults, said: “Unfortunately, this latest study continues the trend of creating more questions than answers. If the adverse outcome of CVD death is a result of supplementation, it is unclear if this is due to the vitamin D, the calcium, or both. And it is unclear if this is dose dependent, time dependent, or due to concurrent risk factors unique to certain populations.
“It is recommended that patients at risk of osteoporosis based on age, sex, medications, and lifestyle be screened for osteoporosis and treated accordingly, including supplementation with CaD,” Dr. Candler said. “It remains unclear whether supplementation with CaD in the absence of osteoporosis and osteopenia is net beneficial or harmful, and at this time I would not recommend it to my patients.”
Added Dr. Manson: “The very small increase seen in cardiovascular mortality wouldn’t be a reason to discontinue supplementation among women who have been advised by their healthcare providers to take these supplements for bone health or other purposes.
“Among those at usual risk of fracture, we recommend trying to obtain adequate calcium and vitamin D from food sources first and to use supplements only for the purpose of filling gaps in intake,” Dr. Manson continued. Overall, the findings support the national recommended dietary allowances for daily calcium intake of 1200 mg and daily vitamin D intake of 600-800 IU among postmenopausal women for maintenance of bone health, she said.
While a 2022 study found that vitamin D supplementation alone did not prevent fractures in healthy adults, other research has shown that a calcium/vitamin D combination is more likely to protect the skeleton.
“Patients at risk for fractures will probably benefit from calcium and/or vitamin D supplementation if they do not meet dietary intake requirements, have malabsorption syndromes, are taking medications that affect nutrient absorption, or if they are older and not regularly exposed to sunlight,” said Dr. Laing. “A combination of biochemical, imaging, functional, and dietary intake data can help determine if a supplement is warranted.”
She stressed that additional research is needed in more diverse populations before changing practice guidelines. “However, doctors should continue to weigh the risks and benefits of prescribing supplements for each patient.”
The WHI program is funded by the National Heart, Lung, and Blood Institute. Dr. Thomson disclosed no competing interests. Dr. Manson reported a relationship with Mars Edge. Multiple authors reported grant support from government funding agencies. The outside commentators had no relevant competing interests to disclose.
Some doctors may be scratching their heads over a new analysis reporting that combined calcium and vitamin D (CaD) supplements appear to be associated with a slight 6% increase in cardiovascular (CVD) mortality, a slight 7% decrease in cancer risk, and no effect on osteoporotic fracture in postmenopausal women.
The study, in Annals of Internal Medicine, found no effect of supplementation on all-cause mortality.
The findings emerged from an analysis of more than 20 years’ follow-up data on a randomized trial in postmenopausal women conducted as part of the Women’s Health Initiative (WHI).
Cynthia A. Thomson, PhD, RD, first author and cancer prevention scientist at the Arizona Cancer Center and a professor of health promotion sciences at the University of Arizona in Tucson said the findings recommend individualized assessment of the need for supplements for older women as they consider them in hopes of preventing fractures.
“Evaluate your patients individually and understand that there are some who may benefit from supplementation, for example, in terms of reducing colorectal cancer mortality,” Dr. Thomson said in an interview. The approach should be nuanced. “If you check the adequacy of vitamin D and calcium in their diets, supplementation may not be needed.” She added that supplementation is best considered in the context of a woman’s overall health profile, including risk factors for fracture, heart disease, and cancer, especially colorectal cancer (CRC).
Study Details
The investigators conducted postintervention follow-up of the WHI’s 7-year multicenter randomized intervention trial of CaD vs placebo.
Since existing evidence of long-term health outcomes was limited, the trial, begun in 1999 and closed in 2005, enrolled 36,282 postmenopausal women (mean age 62) with no history of breast or colorectal cancer. They were randomly assigned 1:1 to supplementation with 1000 mg of calcium carbonate (400 mg elemental calcium) plus 400 IU of vitamin D3 daily or placebo, taken twice daily in half doses.
Study outcomes were incidence of CRC, total and invasive breast cancer; disease-specific and all-cause mortality; total CVD; and hip fracture measured through December 2020, with analyses stratified by personal supplement usage.
Cancer. CaD was associated with reduced incident total cancer, CRC, and invasive breast cancer — notably among participants not taking CaD before randomization. Cancer incidence estimates varied widely, the authors noted, when stratified by supplement use before randomization. Noting that CaD seemed to have more cancer-related impact in those without prior supplementation, the authors suggested supplementation may affect cancer biology primarily by augmenting nutrient insufficiency.
An estimated 7% reduction in cancer mortality was observed after a median cumulative follow-up of 22.3 years: 1817 vs 1943 deaths (hazard ratio, 0.93; 95% CI, 0.87-0.99).
CVD. An estimated 6% increase in CVD mortality was seen in the CaD group: 2621 vs 2420 deaths (HR, 1.06; 95% CI, 1.01-1.12). Pretrial supplement users were found to be at higher CVD risk.
Hip fracture. No effect on hip fracture risk was measured, but the authors cautioned that hip fracture and CVD outcomes were available only for a subset of participants, and the effects of calcium alone vs vitamin D alone vs the combination could not be disentangled.
In a small subgroup analysis, some CaD users were seen to respond in terms of bone mineral density but since only 4 of the study’s 40 sites collected such information, the study was underpowered to examine the effect. ”Many other studies, however, show a response to supplementation in women who already have bone mineral deficits,” Dr. Thomson said.
The Calcification Question
One of the possible mechanisms of harm is that high-dose calcium supplements can increase the rate of blood coagulation and promote vascular calcification, said Emma Laing, PhD, RD, director of dietetics at the University of Georgia in Athens and a spokesperson for the Chicago-based Academy of Nutrition and Dietetics.
“Other factors that should be considered when determining a patient’s CVD risk are race, genetic predisposition, medical and social history, response to stress, and lifestyle behaviors, as well as the length of time supplements have been consumed,” added Dr. Laing, who was not involved in the WHI analysis.
“We asked ourselves if CaD supplements might contribute to calcification of the coronary arteries, since some believe this to be the case, although the literature is mixed,” said Dr. Thomson.
“So we did a shorter ancillary study in a small sample of several hundred [women] to see if there was any increase in calcification” and no difference was seen on imaging across the two arms. “However, women who were already on supplements before entering the study seemed to be at higher CVD risk,” she said.
Added study coauthor JoAnn E. Manson, MD, DrPH, chief of the division of preventive medicine at Brigham and Women’s Hospital and professor of women’s health at Harvard Medical School, both in Boston: “With no increase or decrease in coronary artery calcium at the end of the trial, we don’t believe starting or continuing calcium/vitamin D supplements should require screening for coronary artery disease.”
Some randomized trials and systematic reviews, however, have observed an increased risk of CVD in healthy patients on calcium supplements, with one Korean meta-analysis reporting a 15% increase in CVD risk in healthy postmenopausal women taking calcium supplements. Another meta-analysis found a link between calcium supplements and a greater risk of various cardiovascular outcomes, especially myocardial infarction.
Vitamin D Supplementation
As for vitamin D only supplementation, an updated meta-analysis including more than 83,000 individuals showed that it confers no cardiovascular protection and is therefore not indicated for this purpose.
Practice Considerations
Offering an outsider’s perspective, Sarah G. Candler, MD, MPH, an internist in Houston specializing in primary care for older high-risk adults, said: “Unfortunately, this latest study continues the trend of creating more questions than answers. If the adverse outcome of CVD death is a result of supplementation, it is unclear if this is due to the vitamin D, the calcium, or both. And it is unclear if this is dose dependent, time dependent, or due to concurrent risk factors unique to certain populations.
“It is recommended that patients at risk of osteoporosis based on age, sex, medications, and lifestyle be screened for osteoporosis and treated accordingly, including supplementation with CaD,” Dr. Candler said. “It remains unclear whether supplementation with CaD in the absence of osteoporosis and osteopenia is net beneficial or harmful, and at this time I would not recommend it to my patients.”
Added Dr. Manson: “The very small increase seen in cardiovascular mortality wouldn’t be a reason to discontinue supplementation among women who have been advised by their healthcare providers to take these supplements for bone health or other purposes.
“Among those at usual risk of fracture, we recommend trying to obtain adequate calcium and vitamin D from food sources first and to use supplements only for the purpose of filling gaps in intake,” Dr. Manson continued. Overall, the findings support the national recommended dietary allowances for daily calcium intake of 1200 mg and daily vitamin D intake of 600-800 IU among postmenopausal women for maintenance of bone health, she said.
While a 2022 study found that vitamin D supplementation alone did not prevent fractures in healthy adults, other research has shown that a calcium/vitamin D combination is more likely to protect the skeleton.
“Patients at risk for fractures will probably benefit from calcium and/or vitamin D supplementation if they do not meet dietary intake requirements, have malabsorption syndromes, are taking medications that affect nutrient absorption, or if they are older and not regularly exposed to sunlight,” said Dr. Laing. “A combination of biochemical, imaging, functional, and dietary intake data can help determine if a supplement is warranted.”
She stressed that additional research is needed in more diverse populations before changing practice guidelines. “However, doctors should continue to weigh the risks and benefits of prescribing supplements for each patient.”
The WHI program is funded by the National Heart, Lung, and Blood Institute. Dr. Thomson disclosed no competing interests. Dr. Manson reported a relationship with Mars Edge. Multiple authors reported grant support from government funding agencies. The outside commentators had no relevant competing interests to disclose.
Some doctors may be scratching their heads over a new analysis reporting that combined calcium and vitamin D (CaD) supplements appear to be associated with a slight 6% increase in cardiovascular (CVD) mortality, a slight 7% decrease in cancer risk, and no effect on osteoporotic fracture in postmenopausal women.
The study, in Annals of Internal Medicine, found no effect of supplementation on all-cause mortality.
The findings emerged from an analysis of more than 20 years’ follow-up data on a randomized trial in postmenopausal women conducted as part of the Women’s Health Initiative (WHI).
Cynthia A. Thomson, PhD, RD, first author and cancer prevention scientist at the Arizona Cancer Center and a professor of health promotion sciences at the University of Arizona in Tucson said the findings recommend individualized assessment of the need for supplements for older women as they consider them in hopes of preventing fractures.
“Evaluate your patients individually and understand that there are some who may benefit from supplementation, for example, in terms of reducing colorectal cancer mortality,” Dr. Thomson said in an interview. The approach should be nuanced. “If you check the adequacy of vitamin D and calcium in their diets, supplementation may not be needed.” She added that supplementation is best considered in the context of a woman’s overall health profile, including risk factors for fracture, heart disease, and cancer, especially colorectal cancer (CRC).
Study Details
The investigators conducted postintervention follow-up of the WHI’s 7-year multicenter randomized intervention trial of CaD vs placebo.
Since existing evidence of long-term health outcomes was limited, the trial, begun in 1999 and closed in 2005, enrolled 36,282 postmenopausal women (mean age 62) with no history of breast or colorectal cancer. They were randomly assigned 1:1 to supplementation with 1000 mg of calcium carbonate (400 mg elemental calcium) plus 400 IU of vitamin D3 daily or placebo, taken twice daily in half doses.
Study outcomes were incidence of CRC, total and invasive breast cancer; disease-specific and all-cause mortality; total CVD; and hip fracture measured through December 2020, with analyses stratified by personal supplement usage.
Cancer. CaD was associated with reduced incident total cancer, CRC, and invasive breast cancer — notably among participants not taking CaD before randomization. Cancer incidence estimates varied widely, the authors noted, when stratified by supplement use before randomization. Noting that CaD seemed to have more cancer-related impact in those without prior supplementation, the authors suggested supplementation may affect cancer biology primarily by augmenting nutrient insufficiency.
An estimated 7% reduction in cancer mortality was observed after a median cumulative follow-up of 22.3 years: 1817 vs 1943 deaths (hazard ratio, 0.93; 95% CI, 0.87-0.99).
CVD. An estimated 6% increase in CVD mortality was seen in the CaD group: 2621 vs 2420 deaths (HR, 1.06; 95% CI, 1.01-1.12). Pretrial supplement users were found to be at higher CVD risk.
Hip fracture. No effect on hip fracture risk was measured, but the authors cautioned that hip fracture and CVD outcomes were available only for a subset of participants, and the effects of calcium alone vs vitamin D alone vs the combination could not be disentangled.
In a small subgroup analysis, some CaD users were seen to respond in terms of bone mineral density but since only 4 of the study’s 40 sites collected such information, the study was underpowered to examine the effect. ”Many other studies, however, show a response to supplementation in women who already have bone mineral deficits,” Dr. Thomson said.
The Calcification Question
One of the possible mechanisms of harm is that high-dose calcium supplements can increase the rate of blood coagulation and promote vascular calcification, said Emma Laing, PhD, RD, director of dietetics at the University of Georgia in Athens and a spokesperson for the Chicago-based Academy of Nutrition and Dietetics.
“Other factors that should be considered when determining a patient’s CVD risk are race, genetic predisposition, medical and social history, response to stress, and lifestyle behaviors, as well as the length of time supplements have been consumed,” added Dr. Laing, who was not involved in the WHI analysis.
“We asked ourselves if CaD supplements might contribute to calcification of the coronary arteries, since some believe this to be the case, although the literature is mixed,” said Dr. Thomson.
“So we did a shorter ancillary study in a small sample of several hundred [women] to see if there was any increase in calcification” and no difference was seen on imaging across the two arms. “However, women who were already on supplements before entering the study seemed to be at higher CVD risk,” she said.
Added study coauthor JoAnn E. Manson, MD, DrPH, chief of the division of preventive medicine at Brigham and Women’s Hospital and professor of women’s health at Harvard Medical School, both in Boston: “With no increase or decrease in coronary artery calcium at the end of the trial, we don’t believe starting or continuing calcium/vitamin D supplements should require screening for coronary artery disease.”
Some randomized trials and systematic reviews, however, have observed an increased risk of CVD in healthy patients on calcium supplements, with one Korean meta-analysis reporting a 15% increase in CVD risk in healthy postmenopausal women taking calcium supplements. Another meta-analysis found a link between calcium supplements and a greater risk of various cardiovascular outcomes, especially myocardial infarction.
Vitamin D Supplementation
As for vitamin D only supplementation, an updated meta-analysis including more than 83,000 individuals showed that it confers no cardiovascular protection and is therefore not indicated for this purpose.
Practice Considerations
Offering an outsider’s perspective, Sarah G. Candler, MD, MPH, an internist in Houston specializing in primary care for older high-risk adults, said: “Unfortunately, this latest study continues the trend of creating more questions than answers. If the adverse outcome of CVD death is a result of supplementation, it is unclear if this is due to the vitamin D, the calcium, or both. And it is unclear if this is dose dependent, time dependent, or due to concurrent risk factors unique to certain populations.
“It is recommended that patients at risk of osteoporosis based on age, sex, medications, and lifestyle be screened for osteoporosis and treated accordingly, including supplementation with CaD,” Dr. Candler said. “It remains unclear whether supplementation with CaD in the absence of osteoporosis and osteopenia is net beneficial or harmful, and at this time I would not recommend it to my patients.”
Added Dr. Manson: “The very small increase seen in cardiovascular mortality wouldn’t be a reason to discontinue supplementation among women who have been advised by their healthcare providers to take these supplements for bone health or other purposes.
“Among those at usual risk of fracture, we recommend trying to obtain adequate calcium and vitamin D from food sources first and to use supplements only for the purpose of filling gaps in intake,” Dr. Manson continued. Overall, the findings support the national recommended dietary allowances for daily calcium intake of 1200 mg and daily vitamin D intake of 600-800 IU among postmenopausal women for maintenance of bone health, she said.
While a 2022 study found that vitamin D supplementation alone did not prevent fractures in healthy adults, other research has shown that a calcium/vitamin D combination is more likely to protect the skeleton.
“Patients at risk for fractures will probably benefit from calcium and/or vitamin D supplementation if they do not meet dietary intake requirements, have malabsorption syndromes, are taking medications that affect nutrient absorption, or if they are older and not regularly exposed to sunlight,” said Dr. Laing. “A combination of biochemical, imaging, functional, and dietary intake data can help determine if a supplement is warranted.”
She stressed that additional research is needed in more diverse populations before changing practice guidelines. “However, doctors should continue to weigh the risks and benefits of prescribing supplements for each patient.”
The WHI program is funded by the National Heart, Lung, and Blood Institute. Dr. Thomson disclosed no competing interests. Dr. Manson reported a relationship with Mars Edge. Multiple authors reported grant support from government funding agencies. The outside commentators had no relevant competing interests to disclose.
FROM ANNALS OF INTERNAL MEDICINE







