User login
Four-part ‘safety bundle’ targets gynecologic surgery infections
In a new consensus safety bundle designed to reduce the frequency of infections related to gynecologic surgery, an expert panel is calling for preoperative evaluation of infection risk in every patient and surgical timeouts in every case.
The bundle, from the Council on Patient Safety in Women & Mother’s Health Care, seeks to compile existing guidelines and evidence-based recommendations in a way that can be easily implemented with whatever resources an individual institution has available.
The safety bundle covers four domains:
1. Readiness (every facility). The statement calls for standardized preoperative and postoperative care instructions and clearly defined roles for each surgical team member.
Standards should also be established regarding skin preparation, use of prophylactic antibiotics (terminate them within 24 hours after surgery completion unless medical indications are present), and temperature, such as ambient operating room temperature.
“Although the effect of temperature maintenance on surgical site infection is not definitive,” the consensus statement says, “there is no denying other benefits of normothermia; foremost among these is overall patient satisfaction and comfort.”
2. Recognition and prevention (every patient). Every patient should undergo a preoperative evaluation of infection risk based on blood glucose level, body mass index, immunodeficiency, methicillin-resistant Staphylococcus aureus (MRSA) status, nutritional status, and smoking status.
3. Response (every case). Develop “timeouts” during operations, as mandated by the Joint Commission, to address antibiotic dosage and timing, and reassess risk for infection following the procedure based on the length of surgery and blood loss.
4. Reporting and systems learning (every facility). Develop “huddles” – brief team meetings of less than 15 minutes – for high-risk patients. Surgeons and hospital officials should also create a system to report and analyze data about surgical site infections and share physician-specific infection data with all surgeons as part of ongoing professional practice evaluation.
The statement appeared in Obstetrics & Gynecology (2017;129:50-61) and was published concurrently in Anesthesia & Analgesia, the Journal of Obstetric, Gynecologic & Neonatal Nursing, and the AANA Journal.
The authors reported having no potential conflicts of interest.
In a new consensus safety bundle designed to reduce the frequency of infections related to gynecologic surgery, an expert panel is calling for preoperative evaluation of infection risk in every patient and surgical timeouts in every case.
The bundle, from the Council on Patient Safety in Women & Mother’s Health Care, seeks to compile existing guidelines and evidence-based recommendations in a way that can be easily implemented with whatever resources an individual institution has available.
The safety bundle covers four domains:
1. Readiness (every facility). The statement calls for standardized preoperative and postoperative care instructions and clearly defined roles for each surgical team member.
Standards should also be established regarding skin preparation, use of prophylactic antibiotics (terminate them within 24 hours after surgery completion unless medical indications are present), and temperature, such as ambient operating room temperature.
“Although the effect of temperature maintenance on surgical site infection is not definitive,” the consensus statement says, “there is no denying other benefits of normothermia; foremost among these is overall patient satisfaction and comfort.”
2. Recognition and prevention (every patient). Every patient should undergo a preoperative evaluation of infection risk based on blood glucose level, body mass index, immunodeficiency, methicillin-resistant Staphylococcus aureus (MRSA) status, nutritional status, and smoking status.
3. Response (every case). Develop “timeouts” during operations, as mandated by the Joint Commission, to address antibiotic dosage and timing, and reassess risk for infection following the procedure based on the length of surgery and blood loss.
4. Reporting and systems learning (every facility). Develop “huddles” – brief team meetings of less than 15 minutes – for high-risk patients. Surgeons and hospital officials should also create a system to report and analyze data about surgical site infections and share physician-specific infection data with all surgeons as part of ongoing professional practice evaluation.
The statement appeared in Obstetrics & Gynecology (2017;129:50-61) and was published concurrently in Anesthesia & Analgesia, the Journal of Obstetric, Gynecologic & Neonatal Nursing, and the AANA Journal.
The authors reported having no potential conflicts of interest.
In a new consensus safety bundle designed to reduce the frequency of infections related to gynecologic surgery, an expert panel is calling for preoperative evaluation of infection risk in every patient and surgical timeouts in every case.
The bundle, from the Council on Patient Safety in Women & Mother’s Health Care, seeks to compile existing guidelines and evidence-based recommendations in a way that can be easily implemented with whatever resources an individual institution has available.
The safety bundle covers four domains:
1. Readiness (every facility). The statement calls for standardized preoperative and postoperative care instructions and clearly defined roles for each surgical team member.
Standards should also be established regarding skin preparation, use of prophylactic antibiotics (terminate them within 24 hours after surgery completion unless medical indications are present), and temperature, such as ambient operating room temperature.
“Although the effect of temperature maintenance on surgical site infection is not definitive,” the consensus statement says, “there is no denying other benefits of normothermia; foremost among these is overall patient satisfaction and comfort.”
2. Recognition and prevention (every patient). Every patient should undergo a preoperative evaluation of infection risk based on blood glucose level, body mass index, immunodeficiency, methicillin-resistant Staphylococcus aureus (MRSA) status, nutritional status, and smoking status.
3. Response (every case). Develop “timeouts” during operations, as mandated by the Joint Commission, to address antibiotic dosage and timing, and reassess risk for infection following the procedure based on the length of surgery and blood loss.
4. Reporting and systems learning (every facility). Develop “huddles” – brief team meetings of less than 15 minutes – for high-risk patients. Surgeons and hospital officials should also create a system to report and analyze data about surgical site infections and share physician-specific infection data with all surgeons as part of ongoing professional practice evaluation.
The statement appeared in Obstetrics & Gynecology (2017;129:50-61) and was published concurrently in Anesthesia & Analgesia, the Journal of Obstetric, Gynecologic & Neonatal Nursing, and the AANA Journal.
The authors reported having no potential conflicts of interest.
FROM OBSTETRICS & GYNECOLOGY
Rate of resistant P. aeruginosa in children rising steadily
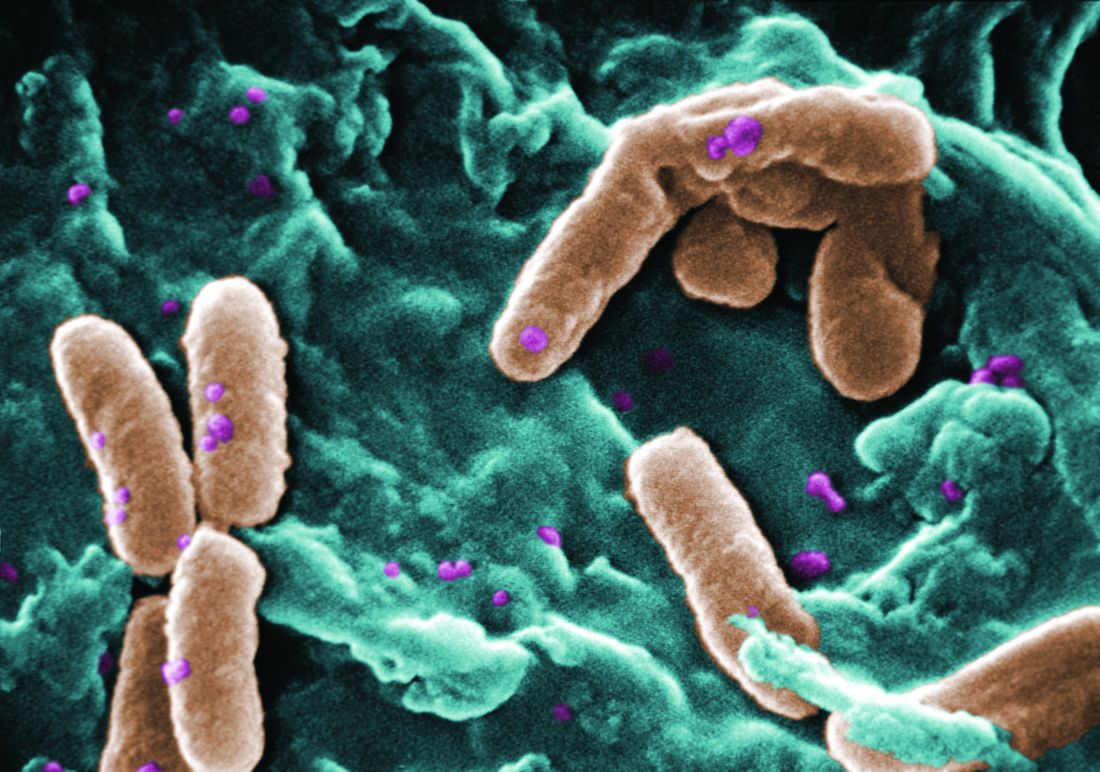
The rate of infection with resistant Pseudomonas aeruginosa among children has risen steadily about 4% per year since 1999, according to a report.
Infections with P aeruginosa in children occur most often associated with pulmonary disease in patients with cystic fibrosis, but healthy children also can experience a variety of P aeruginosa infection types.
They focused on 77,349 P. aeruginosa isolates that were tested for resistance for all five antibiotic classes: cephalosporins, beta-lactam and beta-lactamase inhibitors, carbapenems, fluoroquinolones, and aminoglycosides. The investigators were specifically interested in multidrug- and carbapenem-resistant P. aeruginosa. They described the organism as “arguably the most resistance-prone health care–related pathogen.”
The study samples were obtained from the respiratory tract, urinary tract, ear, sinuses, wounds, skin, and connective tissues of children aged 1-17 years who were treated in 1999-2012; 2012 was the last year for which this information was collected in this database. Patients were treated in ambulatory, inpatient, ICU, and long-term-care settings. The study excluded children with cystic fibrosis and children under 1 year of age, so as to improve the applicability of the results to the general pediatric population.
The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%. This represents an average annual increase of approximately 4% for both types of resistance, Dr. Logan and her associates said (J Ped Infect Dis. 2016 Nov 16. doi: 10.1093/jpids/piw064).
These increases were consistent across all but one age group and all but one treatment setting, the exception being inpatients aged 13-17 years. The prevalence of resistant P. aeruginosa was highest among adolescents in ambulatory, ICU, or long-term-care settings; their rates were three times higher than those in children aged 1 year and two times higher than those in children aged 5 years. It is possible that this pattern reflects “an increasing number of older children with a medically complex condition who have frequent exposure to the health care environment,” the investigators noted.
“The results of our study highlight the need for bacterial surveillance, strategies for implementing effective infection prevention, and antimicrobial stewardship programs.” In addition, all health care facilities should consider using rapid molecular diagnostic platforms to guide antibiotic treatment decisions, “to reduce the burden of the persistent and continually evolving global threat of extensively drug-resistant organisms,” Dr. Logan and her associates added.
This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
The rate of infection with resistant Pseudomonas aeruginosa among children has risen steadily about 4% per year since 1999, according to a report.
Infections with P aeruginosa in children occur most often associated with pulmonary disease in patients with cystic fibrosis, but healthy children also can experience a variety of P aeruginosa infection types.
They focused on 77,349 P. aeruginosa isolates that were tested for resistance for all five antibiotic classes: cephalosporins, beta-lactam and beta-lactamase inhibitors, carbapenems, fluoroquinolones, and aminoglycosides. The investigators were specifically interested in multidrug- and carbapenem-resistant P. aeruginosa. They described the organism as “arguably the most resistance-prone health care–related pathogen.”
The study samples were obtained from the respiratory tract, urinary tract, ear, sinuses, wounds, skin, and connective tissues of children aged 1-17 years who were treated in 1999-2012; 2012 was the last year for which this information was collected in this database. Patients were treated in ambulatory, inpatient, ICU, and long-term-care settings. The study excluded children with cystic fibrosis and children under 1 year of age, so as to improve the applicability of the results to the general pediatric population.
The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%. This represents an average annual increase of approximately 4% for both types of resistance, Dr. Logan and her associates said (J Ped Infect Dis. 2016 Nov 16. doi: 10.1093/jpids/piw064).
These increases were consistent across all but one age group and all but one treatment setting, the exception being inpatients aged 13-17 years. The prevalence of resistant P. aeruginosa was highest among adolescents in ambulatory, ICU, or long-term-care settings; their rates were three times higher than those in children aged 1 year and two times higher than those in children aged 5 years. It is possible that this pattern reflects “an increasing number of older children with a medically complex condition who have frequent exposure to the health care environment,” the investigators noted.
“The results of our study highlight the need for bacterial surveillance, strategies for implementing effective infection prevention, and antimicrobial stewardship programs.” In addition, all health care facilities should consider using rapid molecular diagnostic platforms to guide antibiotic treatment decisions, “to reduce the burden of the persistent and continually evolving global threat of extensively drug-resistant organisms,” Dr. Logan and her associates added.
This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
The rate of infection with resistant Pseudomonas aeruginosa among children has risen steadily about 4% per year since 1999, according to a report.
Infections with P aeruginosa in children occur most often associated with pulmonary disease in patients with cystic fibrosis, but healthy children also can experience a variety of P aeruginosa infection types.
They focused on 77,349 P. aeruginosa isolates that were tested for resistance for all five antibiotic classes: cephalosporins, beta-lactam and beta-lactamase inhibitors, carbapenems, fluoroquinolones, and aminoglycosides. The investigators were specifically interested in multidrug- and carbapenem-resistant P. aeruginosa. They described the organism as “arguably the most resistance-prone health care–related pathogen.”
The study samples were obtained from the respiratory tract, urinary tract, ear, sinuses, wounds, skin, and connective tissues of children aged 1-17 years who were treated in 1999-2012; 2012 was the last year for which this information was collected in this database. Patients were treated in ambulatory, inpatient, ICU, and long-term-care settings. The study excluded children with cystic fibrosis and children under 1 year of age, so as to improve the applicability of the results to the general pediatric population.
The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%. This represents an average annual increase of approximately 4% for both types of resistance, Dr. Logan and her associates said (J Ped Infect Dis. 2016 Nov 16. doi: 10.1093/jpids/piw064).
These increases were consistent across all but one age group and all but one treatment setting, the exception being inpatients aged 13-17 years. The prevalence of resistant P. aeruginosa was highest among adolescents in ambulatory, ICU, or long-term-care settings; their rates were three times higher than those in children aged 1 year and two times higher than those in children aged 5 years. It is possible that this pattern reflects “an increasing number of older children with a medically complex condition who have frequent exposure to the health care environment,” the investigators noted.
“The results of our study highlight the need for bacterial surveillance, strategies for implementing effective infection prevention, and antimicrobial stewardship programs.” In addition, all health care facilities should consider using rapid molecular diagnostic platforms to guide antibiotic treatment decisions, “to reduce the burden of the persistent and continually evolving global threat of extensively drug-resistant organisms,” Dr. Logan and her associates added.
This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
FROM THE JOURNAL OF PEDIATRIC INFECTIOUS DISEASES
Key clinical point:
Major finding: The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%.
Data source: A longitudinal analysis of information in a nationally representative database of microbiology laboratories serving approximately 300 U.S. hospitals.
Disclosures: This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
Should surgeons change gloves during total laparoscopic hysterectomy?
ORLANDO – Many gynecologic surgeons change gloves, gowns, and even surgical drapes during total laparoscopic hysterectomy to prevent bacterial infections, but little data support the practice.
In a small study of women undergoing total laparoscopic hysterectomy, investigators found that the overall risk of infection from contaminated gowns, gloves, and instruments was very low, with bacterial growth below the infection threshold in 98.9% of samples and no surgical site infections reported during 6 weeks of follow-up after surgery.
“Tradition dictates that even after both fields have been prepped, we refer to the perineum and vagina as ‘dirty,’ and the abdomen as ‘clean,’ ” Dr. Shockley said, “And surgeons habitually change their gown and gloves when inadvertent contact with the perineum or vagina occurs.”
To elucidate the true pathogen picture, Dr. Shockley and her colleagues assessed 31 women undergoing total laparoscopic hysterectomy for a benign indication during 2016. They evaluated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus.
All patients received perioperative antibiotic prophylaxis and standard, separate perineovaginal and abdominal prep with chlorhexidine. Investigators swabbed the vaginal fornices and abdomen at six sites, as well as the surgeon’s gloves following placement of the uterine manipulator, tips of instruments used to close the vaginal cuff, uterine fundus after extraction, and surgeon’s gloves following removal of the uterus.
They detected no anaerobic bacterial growth from samples taken from the abdomen, in the vagina, or on the tips of instruments used for cuff closure. Similarly, there was no aerobic growth observed in the vagina of any patient. However, they did detect aerobic bacterial growth in the abdomen, which in all cases was consistent with skin flora.
Three patients demonstrated some growth with the surgeon’s gloves following manipulator placement. Nearly one-third – 32% – of surgeon’s gloves cultured bacteria after removal of the uterus. One sample yielded cumulative growth for a bacterial count considered high enough to potentially cause infection, defined as more than 5,000 colony-forming units (CFU) per milliliter. This was the highest growth sample out of the 180 samples collected.
Additionally, 39% of samples from the uterine fundus were positive, a higher percentage than at any other site, Dr. Shockley reported. “And the one sample with growth exceeding 5,000 CFU/mL – you guessed it – was from the same patient.”
Bacterial growth was scant on the instrument tips used to close the vaginal cuffs.
Overall, bacterial growth in 98.9% of samples was below the infection threshold. “We did not identify any post–surgical site infections during 6 weeks of follow-up,” Dr. Shockley said at the meeting sponsored by AAGL.
“This study does provide a good description and count of the bacteria encountered during total laparoscopic hysterectomy. They are unlikely to cause surgical site infections … but based on concentration and frequency of bacterial growth on the surgeon’s gloves after specimen extraction, we would recommend if you are going to change gloves, do it after this step, before turning your attention back to the abdomen for vaginal cuff closure,” she said.
But changing gloves after placing the Foley and uterine manipulator “seems to be a wasted exercise,” Dr. Shockley said. “There was no growth on the vaginal fornices of any patient.”
The bacteria on the gloves in those three cases developed very low colony counts. “Yes, there was growth after the removal of the specimen, but with the exception of one patient, the colony counts were all below 5,000,” she said. “I think we need more data to reassure ourselves [attire changes are] unnecessary at every step of the [total laparoscopic hysterectomy].”
The study was supported by an educational grant from the Foundation of the AAGL Jerome J. Hoffman Endowment. Dr. Shockley reported having no relevant financial disclosures.
ORLANDO – Many gynecologic surgeons change gloves, gowns, and even surgical drapes during total laparoscopic hysterectomy to prevent bacterial infections, but little data support the practice.
In a small study of women undergoing total laparoscopic hysterectomy, investigators found that the overall risk of infection from contaminated gowns, gloves, and instruments was very low, with bacterial growth below the infection threshold in 98.9% of samples and no surgical site infections reported during 6 weeks of follow-up after surgery.
“Tradition dictates that even after both fields have been prepped, we refer to the perineum and vagina as ‘dirty,’ and the abdomen as ‘clean,’ ” Dr. Shockley said, “And surgeons habitually change their gown and gloves when inadvertent contact with the perineum or vagina occurs.”
To elucidate the true pathogen picture, Dr. Shockley and her colleagues assessed 31 women undergoing total laparoscopic hysterectomy for a benign indication during 2016. They evaluated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus.
All patients received perioperative antibiotic prophylaxis and standard, separate perineovaginal and abdominal prep with chlorhexidine. Investigators swabbed the vaginal fornices and abdomen at six sites, as well as the surgeon’s gloves following placement of the uterine manipulator, tips of instruments used to close the vaginal cuff, uterine fundus after extraction, and surgeon’s gloves following removal of the uterus.
They detected no anaerobic bacterial growth from samples taken from the abdomen, in the vagina, or on the tips of instruments used for cuff closure. Similarly, there was no aerobic growth observed in the vagina of any patient. However, they did detect aerobic bacterial growth in the abdomen, which in all cases was consistent with skin flora.
Three patients demonstrated some growth with the surgeon’s gloves following manipulator placement. Nearly one-third – 32% – of surgeon’s gloves cultured bacteria after removal of the uterus. One sample yielded cumulative growth for a bacterial count considered high enough to potentially cause infection, defined as more than 5,000 colony-forming units (CFU) per milliliter. This was the highest growth sample out of the 180 samples collected.
Additionally, 39% of samples from the uterine fundus were positive, a higher percentage than at any other site, Dr. Shockley reported. “And the one sample with growth exceeding 5,000 CFU/mL – you guessed it – was from the same patient.”
Bacterial growth was scant on the instrument tips used to close the vaginal cuffs.
Overall, bacterial growth in 98.9% of samples was below the infection threshold. “We did not identify any post–surgical site infections during 6 weeks of follow-up,” Dr. Shockley said at the meeting sponsored by AAGL.
“This study does provide a good description and count of the bacteria encountered during total laparoscopic hysterectomy. They are unlikely to cause surgical site infections … but based on concentration and frequency of bacterial growth on the surgeon’s gloves after specimen extraction, we would recommend if you are going to change gloves, do it after this step, before turning your attention back to the abdomen for vaginal cuff closure,” she said.
But changing gloves after placing the Foley and uterine manipulator “seems to be a wasted exercise,” Dr. Shockley said. “There was no growth on the vaginal fornices of any patient.”
The bacteria on the gloves in those three cases developed very low colony counts. “Yes, there was growth after the removal of the specimen, but with the exception of one patient, the colony counts were all below 5,000,” she said. “I think we need more data to reassure ourselves [attire changes are] unnecessary at every step of the [total laparoscopic hysterectomy].”
The study was supported by an educational grant from the Foundation of the AAGL Jerome J. Hoffman Endowment. Dr. Shockley reported having no relevant financial disclosures.
ORLANDO – Many gynecologic surgeons change gloves, gowns, and even surgical drapes during total laparoscopic hysterectomy to prevent bacterial infections, but little data support the practice.
In a small study of women undergoing total laparoscopic hysterectomy, investigators found that the overall risk of infection from contaminated gowns, gloves, and instruments was very low, with bacterial growth below the infection threshold in 98.9% of samples and no surgical site infections reported during 6 weeks of follow-up after surgery.
“Tradition dictates that even after both fields have been prepped, we refer to the perineum and vagina as ‘dirty,’ and the abdomen as ‘clean,’ ” Dr. Shockley said, “And surgeons habitually change their gown and gloves when inadvertent contact with the perineum or vagina occurs.”
To elucidate the true pathogen picture, Dr. Shockley and her colleagues assessed 31 women undergoing total laparoscopic hysterectomy for a benign indication during 2016. They evaluated the type and quantity of bacteria found intraoperatively on the abdomen, vagina, surgical gloves, instrument tips, and uterus.
All patients received perioperative antibiotic prophylaxis and standard, separate perineovaginal and abdominal prep with chlorhexidine. Investigators swabbed the vaginal fornices and abdomen at six sites, as well as the surgeon’s gloves following placement of the uterine manipulator, tips of instruments used to close the vaginal cuff, uterine fundus after extraction, and surgeon’s gloves following removal of the uterus.
They detected no anaerobic bacterial growth from samples taken from the abdomen, in the vagina, or on the tips of instruments used for cuff closure. Similarly, there was no aerobic growth observed in the vagina of any patient. However, they did detect aerobic bacterial growth in the abdomen, which in all cases was consistent with skin flora.
Three patients demonstrated some growth with the surgeon’s gloves following manipulator placement. Nearly one-third – 32% – of surgeon’s gloves cultured bacteria after removal of the uterus. One sample yielded cumulative growth for a bacterial count considered high enough to potentially cause infection, defined as more than 5,000 colony-forming units (CFU) per milliliter. This was the highest growth sample out of the 180 samples collected.
Additionally, 39% of samples from the uterine fundus were positive, a higher percentage than at any other site, Dr. Shockley reported. “And the one sample with growth exceeding 5,000 CFU/mL – you guessed it – was from the same patient.”
Bacterial growth was scant on the instrument tips used to close the vaginal cuffs.
Overall, bacterial growth in 98.9% of samples was below the infection threshold. “We did not identify any post–surgical site infections during 6 weeks of follow-up,” Dr. Shockley said at the meeting sponsored by AAGL.
“This study does provide a good description and count of the bacteria encountered during total laparoscopic hysterectomy. They are unlikely to cause surgical site infections … but based on concentration and frequency of bacterial growth on the surgeon’s gloves after specimen extraction, we would recommend if you are going to change gloves, do it after this step, before turning your attention back to the abdomen for vaginal cuff closure,” she said.
But changing gloves after placing the Foley and uterine manipulator “seems to be a wasted exercise,” Dr. Shockley said. “There was no growth on the vaginal fornices of any patient.”
The bacteria on the gloves in those three cases developed very low colony counts. “Yes, there was growth after the removal of the specimen, but with the exception of one patient, the colony counts were all below 5,000,” she said. “I think we need more data to reassure ourselves [attire changes are] unnecessary at every step of the [total laparoscopic hysterectomy].”
The study was supported by an educational grant from the Foundation of the AAGL Jerome J. Hoffman Endowment. Dr. Shockley reported having no relevant financial disclosures.
AT THE AAGL GLOBAL CONGRESS
Key clinical point:
Major finding: Bacterial concentrations did not exceed thresholds required to trigger potential infection in almost 99% of cultures.
Data source: A study of 31 women undergoing total laparoscopic hysterectomy for benign indications in 2016.
Disclosures: The study was supported by an educational grant from the Foundation of the AAGL Jerome J. Hoffman Endowment. Dr. Shockley reported having no relevant financial disclosures.
Hypervirulent Mycobacterium clone infecting cystic fibrosis patients worldwide
A recently evolved strain of Mycobacterium is circulating in hospitals worldwide, causing nearly impossible-to-treat lung infections among patients with cystic fibrosis.
A genome-wide study has determined that Mycobacterium abscessus is not transmitted through soil and water, as once thought, but is a nosocomial infection transmitted person to person through droplet and surface contamination, Andres Floto, MD, reported in Science (2016 Nov 11;354[6313]:751-7).
“The bug initially seems to have entered the patient population from the environment, but we think it has recently evolved to become capable of jumping from patient to patient, getting more virulent as it does so,” Dr. Floto of the University of Cambridge, England, wrote in a press statement.
The path of global transmission is not yet entirely clear, the authors noted. But since it first appeared, around 1978, M. abscessus has spread globally, strongly suggesting that asymptomatic carriers may be one source of transmission.
“We found no evidence of cystic fibrosis patients or of equipment moving between centers in different countries, indicating that the global spread of M. abscessus may be driven by alternative human, zoonotic, or environmental vectors of transmission,” the researchers wrote.
The team conducted whole-genome sequencing on 1,080 samples of M. abscessus obtained from 517 cystic fibrosis patients in clinics and hospitals within the United States, the United Kingdom, Europe, and Australia. They identified three subspecies, some of which contained nearly genetically identical strains, “suggesting widespread transmission of circulating clones within the global cystic fibrosis patient community.”
Most patients (74%) were infected with these genetically identical strains despite their diverse geographic locations. The isolates were amazingly similar, the authors noted: 90% differed by less than 20 single nucleotide polymorphisms.
Using these strains, the researchers were able to construct several possible transmission chains in most of the cystic fibrosis centers included in the study. The three dominant circulating clones were all observed in the United States, European, and Australian samples, indicating transcontinental transmission.
“We also detected numerous examples of identical or near-identical isolates infecting groups of patients in different cystic fibrosis centers and, indeed, across different countries, indicating the recent global spread of M. abscessus clones throughout the international cystic fibrosis patient community.”
The team also determined that the common ancestor of these strains probably emerged around 1978.
Another sequencing series tracked specific isolates among individual patients. This strongly suggests person-to-person transmission. Adding this to their previous work on M. abscessus transmission, the authors postulated that spread was probably by surface contamination by droplet contamination and by cough aerosol from infected patients.
The team then looked at clinical outcomes associated with the bacteria and treatment with amikacin and macrolides – antibiotics typically used to fight this very-challenging infection. “We did observe increased rates of chronic infection in individuals,” infected with the clones, which were resistant to both those medications, they said.
In immunodeficient mice, the strains were more likely to cause granulomatous and inflammatory lung changes. And the bacteria tended to survive even after being consumed by macrophages, “suggesting that the establishment of transmission chains may have permitted multiple rounds of within-host genetic adaptation to allow M. abscessus to evolve from an environmental organism to a true lung pathogen.”
The research was funded by the Wellcome Trust and the Cystic Fibrosis Trust in the United Kingdom. There were no financial disclosures.
[email protected]
On Twitter @alz_gal
Approximately 30,000 American adults, children, and infants have cystic fibrosis. Nontuberculous mycobacteria (NTM) are ubiquitous environmental microorganisms, and it has been known for some time that these infections can be transmitted person to person. Any patient, actually, who has preexisting lung disease – and especially those with poor mucociliary clearance – are at risk for a nontuberculous mycobacterial infection. This type of lung infection also can be difficult to diagnose and hard to treat. The U.S. Cystic Fibrosis Foundation in conjunction with the European Cystic Fibrosis Society has developed consensus guidelines for infection control, evaluation, and treatment of this problem. This executive summary was published last January (Floto et al. Thorax.2016;71:i1-i22).
At our center, in addition to the standard contact precautions we use for every CF patient, patients with confirmed NTM infections are seen at every clinic visit in an airborne infection isolation room. We also require all CF patients to wear an isolation mask when entering the hospital or clinic facility, when going to a laboratory, or even when going to the bathroom down the hall. Finally, we stress the significant importance of good hand hygiene.
Susan Millard, MD, FCCP, is a pediatric pulmonologist with Spectrum Health/Butterworth Hospital in Grand Rapids, Mich.
Approximately 30,000 American adults, children, and infants have cystic fibrosis. Nontuberculous mycobacteria (NTM) are ubiquitous environmental microorganisms, and it has been known for some time that these infections can be transmitted person to person. Any patient, actually, who has preexisting lung disease – and especially those with poor mucociliary clearance – are at risk for a nontuberculous mycobacterial infection. This type of lung infection also can be difficult to diagnose and hard to treat. The U.S. Cystic Fibrosis Foundation in conjunction with the European Cystic Fibrosis Society has developed consensus guidelines for infection control, evaluation, and treatment of this problem. This executive summary was published last January (Floto et al. Thorax.2016;71:i1-i22).
At our center, in addition to the standard contact precautions we use for every CF patient, patients with confirmed NTM infections are seen at every clinic visit in an airborne infection isolation room. We also require all CF patients to wear an isolation mask when entering the hospital or clinic facility, when going to a laboratory, or even when going to the bathroom down the hall. Finally, we stress the significant importance of good hand hygiene.
Susan Millard, MD, FCCP, is a pediatric pulmonologist with Spectrum Health/Butterworth Hospital in Grand Rapids, Mich.
Approximately 30,000 American adults, children, and infants have cystic fibrosis. Nontuberculous mycobacteria (NTM) are ubiquitous environmental microorganisms, and it has been known for some time that these infections can be transmitted person to person. Any patient, actually, who has preexisting lung disease – and especially those with poor mucociliary clearance – are at risk for a nontuberculous mycobacterial infection. This type of lung infection also can be difficult to diagnose and hard to treat. The U.S. Cystic Fibrosis Foundation in conjunction with the European Cystic Fibrosis Society has developed consensus guidelines for infection control, evaluation, and treatment of this problem. This executive summary was published last January (Floto et al. Thorax.2016;71:i1-i22).
At our center, in addition to the standard contact precautions we use for every CF patient, patients with confirmed NTM infections are seen at every clinic visit in an airborne infection isolation room. We also require all CF patients to wear an isolation mask when entering the hospital or clinic facility, when going to a laboratory, or even when going to the bathroom down the hall. Finally, we stress the significant importance of good hand hygiene.
Susan Millard, MD, FCCP, is a pediatric pulmonologist with Spectrum Health/Butterworth Hospital in Grand Rapids, Mich.
A recently evolved strain of Mycobacterium is circulating in hospitals worldwide, causing nearly impossible-to-treat lung infections among patients with cystic fibrosis.
A genome-wide study has determined that Mycobacterium abscessus is not transmitted through soil and water, as once thought, but is a nosocomial infection transmitted person to person through droplet and surface contamination, Andres Floto, MD, reported in Science (2016 Nov 11;354[6313]:751-7).
“The bug initially seems to have entered the patient population from the environment, but we think it has recently evolved to become capable of jumping from patient to patient, getting more virulent as it does so,” Dr. Floto of the University of Cambridge, England, wrote in a press statement.
The path of global transmission is not yet entirely clear, the authors noted. But since it first appeared, around 1978, M. abscessus has spread globally, strongly suggesting that asymptomatic carriers may be one source of transmission.
“We found no evidence of cystic fibrosis patients or of equipment moving between centers in different countries, indicating that the global spread of M. abscessus may be driven by alternative human, zoonotic, or environmental vectors of transmission,” the researchers wrote.
The team conducted whole-genome sequencing on 1,080 samples of M. abscessus obtained from 517 cystic fibrosis patients in clinics and hospitals within the United States, the United Kingdom, Europe, and Australia. They identified three subspecies, some of which contained nearly genetically identical strains, “suggesting widespread transmission of circulating clones within the global cystic fibrosis patient community.”
Most patients (74%) were infected with these genetically identical strains despite their diverse geographic locations. The isolates were amazingly similar, the authors noted: 90% differed by less than 20 single nucleotide polymorphisms.
Using these strains, the researchers were able to construct several possible transmission chains in most of the cystic fibrosis centers included in the study. The three dominant circulating clones were all observed in the United States, European, and Australian samples, indicating transcontinental transmission.
“We also detected numerous examples of identical or near-identical isolates infecting groups of patients in different cystic fibrosis centers and, indeed, across different countries, indicating the recent global spread of M. abscessus clones throughout the international cystic fibrosis patient community.”
The team also determined that the common ancestor of these strains probably emerged around 1978.
Another sequencing series tracked specific isolates among individual patients. This strongly suggests person-to-person transmission. Adding this to their previous work on M. abscessus transmission, the authors postulated that spread was probably by surface contamination by droplet contamination and by cough aerosol from infected patients.
The team then looked at clinical outcomes associated with the bacteria and treatment with amikacin and macrolides – antibiotics typically used to fight this very-challenging infection. “We did observe increased rates of chronic infection in individuals,” infected with the clones, which were resistant to both those medications, they said.
In immunodeficient mice, the strains were more likely to cause granulomatous and inflammatory lung changes. And the bacteria tended to survive even after being consumed by macrophages, “suggesting that the establishment of transmission chains may have permitted multiple rounds of within-host genetic adaptation to allow M. abscessus to evolve from an environmental organism to a true lung pathogen.”
The research was funded by the Wellcome Trust and the Cystic Fibrosis Trust in the United Kingdom. There were no financial disclosures.
[email protected]
On Twitter @alz_gal
A recently evolved strain of Mycobacterium is circulating in hospitals worldwide, causing nearly impossible-to-treat lung infections among patients with cystic fibrosis.
A genome-wide study has determined that Mycobacterium abscessus is not transmitted through soil and water, as once thought, but is a nosocomial infection transmitted person to person through droplet and surface contamination, Andres Floto, MD, reported in Science (2016 Nov 11;354[6313]:751-7).
“The bug initially seems to have entered the patient population from the environment, but we think it has recently evolved to become capable of jumping from patient to patient, getting more virulent as it does so,” Dr. Floto of the University of Cambridge, England, wrote in a press statement.
The path of global transmission is not yet entirely clear, the authors noted. But since it first appeared, around 1978, M. abscessus has spread globally, strongly suggesting that asymptomatic carriers may be one source of transmission.
“We found no evidence of cystic fibrosis patients or of equipment moving between centers in different countries, indicating that the global spread of M. abscessus may be driven by alternative human, zoonotic, or environmental vectors of transmission,” the researchers wrote.
The team conducted whole-genome sequencing on 1,080 samples of M. abscessus obtained from 517 cystic fibrosis patients in clinics and hospitals within the United States, the United Kingdom, Europe, and Australia. They identified three subspecies, some of which contained nearly genetically identical strains, “suggesting widespread transmission of circulating clones within the global cystic fibrosis patient community.”
Most patients (74%) were infected with these genetically identical strains despite their diverse geographic locations. The isolates were amazingly similar, the authors noted: 90% differed by less than 20 single nucleotide polymorphisms.
Using these strains, the researchers were able to construct several possible transmission chains in most of the cystic fibrosis centers included in the study. The three dominant circulating clones were all observed in the United States, European, and Australian samples, indicating transcontinental transmission.
“We also detected numerous examples of identical or near-identical isolates infecting groups of patients in different cystic fibrosis centers and, indeed, across different countries, indicating the recent global spread of M. abscessus clones throughout the international cystic fibrosis patient community.”
The team also determined that the common ancestor of these strains probably emerged around 1978.
Another sequencing series tracked specific isolates among individual patients. This strongly suggests person-to-person transmission. Adding this to their previous work on M. abscessus transmission, the authors postulated that spread was probably by surface contamination by droplet contamination and by cough aerosol from infected patients.
The team then looked at clinical outcomes associated with the bacteria and treatment with amikacin and macrolides – antibiotics typically used to fight this very-challenging infection. “We did observe increased rates of chronic infection in individuals,” infected with the clones, which were resistant to both those medications, they said.
In immunodeficient mice, the strains were more likely to cause granulomatous and inflammatory lung changes. And the bacteria tended to survive even after being consumed by macrophages, “suggesting that the establishment of transmission chains may have permitted multiple rounds of within-host genetic adaptation to allow M. abscessus to evolve from an environmental organism to a true lung pathogen.”
The research was funded by the Wellcome Trust and the Cystic Fibrosis Trust in the United Kingdom. There were no financial disclosures.
[email protected]
On Twitter @alz_gal
FROM SCIENCE
Key clinical point:
Major finding: Hypervirulent clones of Mycobacterium abscessus with apparent person-to-person transmission, are appearing in cystic fibrosis centers worldwide.
Data source: Gene sequencing was performed on 1,080 samples of M. abscessus from the United States, the United Kingdom, Europe, and Australia.
Disclosures: The research was funded by the Wellcome Trust and the Cystic Fibrosis Trust in the United Kingdom.
Continue DMARDs, biologics in RA surgery patients
WASHINGTON – The perioperative use of disease-modifying antirheumatic drug monotherapy or combined therapy with methotrexate and a tumor necrosis factor (TNF) inhibitor is not associated with increased rates of postoperative infectious complications or wound infections in patients with rheumatoid arthritis, according to findings from a retrospective review of more than 9,000 surgeries.
With respect to monotherapy, treatment was continued in 1,951 of 2,601 surgeries among patients receiving methotrexate, in 1,496 of 2,012 surgeries among patients receiving hydroxychloroquine, and in 508 of 652 surgeries among patient receiving leflunomide. The odds ratios for postoperative infection (including urinary tract, pneumonia, or sepsis) and postoperative wound infection, respectively, were 0.79 and 0.77 with methotrexate continuation, 0.93 and 0.86 with hydroxychloroquine continuation, and 0.78 and 0.87 with leflunomide continuation, Hsin-Hsuan Juo, MD, reported at the annual meeting of the American College of Rheumatology.
Data for this study were derived from the U.S. Department of Veterans Affairs administrative database and surgical quality registry. Rheumatoid arthritis patients who underwent a surgical procedure and who were on at least one disease-modifying antirheumatic drug (DMARD) or one biologic agent in the perioperative period during the study period of Oct. 1, 1999, through Sept. 30, 2009, were included. Subjects had a mean age of 67 years, and 91% were men.
The finding that the continuation of DMARD monotherapy or the combination of methotrexate and TNF inhibitor therapy for RA in the perioperative setting was not associated with increased rates of overall postoperative infectious complications and wound infections is important, because many patients are advised to stop taking these drugs prior to surgery because of concerns about increased susceptibility to infection. Discontinuing RA medication can increase the risk of disease flares requiring treatment with prednisone, which can further increase the risk of postsurgical complications, Dr. Juo said.
Clear, consistent guidance on the continuation of treatment among RA patients undergoing surgery has been lacking, she said, noting that guidelines over the years from the ACR, the British Society for Rheumatology, and the Canadian Rheumatology Association have differed in their recommendations.
A new draft guideline reported the morning of Dr. Juo’s presentation at the ACR annual meeting recommended continuing DMARDs but discontinuing biologics prior to surgery, but that guideline is limited to orthopedic surgery among patients with various rheumatic diseases.
“With literature review, the results are conflicting as well; some recommend continuing medication, and others recommend discontinuing medications prior to surgery,” she said.
The current findings, though limited by the study’s observational design and generally older, male population, suggest that continuing antirheumatic medications during the perioperative period is not associated with increased rates of postoperative complications.
“Our study results suggest that discontinuing DMARDs and biologic agents prior to surgery may not be necessary. Therefore, being on DMARDs or biologic agents should not preclude patients from receiving urgent surgeries,” Dr. Juo concluded.
Dr. Juo reported having no disclosures.
WASHINGTON – The perioperative use of disease-modifying antirheumatic drug monotherapy or combined therapy with methotrexate and a tumor necrosis factor (TNF) inhibitor is not associated with increased rates of postoperative infectious complications or wound infections in patients with rheumatoid arthritis, according to findings from a retrospective review of more than 9,000 surgeries.
With respect to monotherapy, treatment was continued in 1,951 of 2,601 surgeries among patients receiving methotrexate, in 1,496 of 2,012 surgeries among patients receiving hydroxychloroquine, and in 508 of 652 surgeries among patient receiving leflunomide. The odds ratios for postoperative infection (including urinary tract, pneumonia, or sepsis) and postoperative wound infection, respectively, were 0.79 and 0.77 with methotrexate continuation, 0.93 and 0.86 with hydroxychloroquine continuation, and 0.78 and 0.87 with leflunomide continuation, Hsin-Hsuan Juo, MD, reported at the annual meeting of the American College of Rheumatology.
Data for this study were derived from the U.S. Department of Veterans Affairs administrative database and surgical quality registry. Rheumatoid arthritis patients who underwent a surgical procedure and who were on at least one disease-modifying antirheumatic drug (DMARD) or one biologic agent in the perioperative period during the study period of Oct. 1, 1999, through Sept. 30, 2009, were included. Subjects had a mean age of 67 years, and 91% were men.
The finding that the continuation of DMARD monotherapy or the combination of methotrexate and TNF inhibitor therapy for RA in the perioperative setting was not associated with increased rates of overall postoperative infectious complications and wound infections is important, because many patients are advised to stop taking these drugs prior to surgery because of concerns about increased susceptibility to infection. Discontinuing RA medication can increase the risk of disease flares requiring treatment with prednisone, which can further increase the risk of postsurgical complications, Dr. Juo said.
Clear, consistent guidance on the continuation of treatment among RA patients undergoing surgery has been lacking, she said, noting that guidelines over the years from the ACR, the British Society for Rheumatology, and the Canadian Rheumatology Association have differed in their recommendations.
A new draft guideline reported the morning of Dr. Juo’s presentation at the ACR annual meeting recommended continuing DMARDs but discontinuing biologics prior to surgery, but that guideline is limited to orthopedic surgery among patients with various rheumatic diseases.
“With literature review, the results are conflicting as well; some recommend continuing medication, and others recommend discontinuing medications prior to surgery,” she said.
The current findings, though limited by the study’s observational design and generally older, male population, suggest that continuing antirheumatic medications during the perioperative period is not associated with increased rates of postoperative complications.
“Our study results suggest that discontinuing DMARDs and biologic agents prior to surgery may not be necessary. Therefore, being on DMARDs or biologic agents should not preclude patients from receiving urgent surgeries,” Dr. Juo concluded.
Dr. Juo reported having no disclosures.
WASHINGTON – The perioperative use of disease-modifying antirheumatic drug monotherapy or combined therapy with methotrexate and a tumor necrosis factor (TNF) inhibitor is not associated with increased rates of postoperative infectious complications or wound infections in patients with rheumatoid arthritis, according to findings from a retrospective review of more than 9,000 surgeries.
With respect to monotherapy, treatment was continued in 1,951 of 2,601 surgeries among patients receiving methotrexate, in 1,496 of 2,012 surgeries among patients receiving hydroxychloroquine, and in 508 of 652 surgeries among patient receiving leflunomide. The odds ratios for postoperative infection (including urinary tract, pneumonia, or sepsis) and postoperative wound infection, respectively, were 0.79 and 0.77 with methotrexate continuation, 0.93 and 0.86 with hydroxychloroquine continuation, and 0.78 and 0.87 with leflunomide continuation, Hsin-Hsuan Juo, MD, reported at the annual meeting of the American College of Rheumatology.
Data for this study were derived from the U.S. Department of Veterans Affairs administrative database and surgical quality registry. Rheumatoid arthritis patients who underwent a surgical procedure and who were on at least one disease-modifying antirheumatic drug (DMARD) or one biologic agent in the perioperative period during the study period of Oct. 1, 1999, through Sept. 30, 2009, were included. Subjects had a mean age of 67 years, and 91% were men.
The finding that the continuation of DMARD monotherapy or the combination of methotrexate and TNF inhibitor therapy for RA in the perioperative setting was not associated with increased rates of overall postoperative infectious complications and wound infections is important, because many patients are advised to stop taking these drugs prior to surgery because of concerns about increased susceptibility to infection. Discontinuing RA medication can increase the risk of disease flares requiring treatment with prednisone, which can further increase the risk of postsurgical complications, Dr. Juo said.
Clear, consistent guidance on the continuation of treatment among RA patients undergoing surgery has been lacking, she said, noting that guidelines over the years from the ACR, the British Society for Rheumatology, and the Canadian Rheumatology Association have differed in their recommendations.
A new draft guideline reported the morning of Dr. Juo’s presentation at the ACR annual meeting recommended continuing DMARDs but discontinuing biologics prior to surgery, but that guideline is limited to orthopedic surgery among patients with various rheumatic diseases.
“With literature review, the results are conflicting as well; some recommend continuing medication, and others recommend discontinuing medications prior to surgery,” she said.
The current findings, though limited by the study’s observational design and generally older, male population, suggest that continuing antirheumatic medications during the perioperative period is not associated with increased rates of postoperative complications.
“Our study results suggest that discontinuing DMARDs and biologic agents prior to surgery may not be necessary. Therefore, being on DMARDs or biologic agents should not preclude patients from receiving urgent surgeries,” Dr. Juo concluded.
Dr. Juo reported having no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point:
Major finding: Odds ratios for postoperative infection and postoperative wound infection, respectively, were 0.79 and 0.77 with methotrexate continuation, 0.93 and 0.86 with hydroxychloroquine continuation, 0.78 and 0.87 with leflunomide continuation, and 0.35 and 0.38 with combined methotrexate/TNF inhibitor continuation.
Data source: A retrospective review of more than 9,000 surgeries.
Disclosures: Dr. Juo reported having no disclosures.
Robotic surgery instruments ‘virtually impossible’ to clean completely
Instruments used for robotic surgery are “virtually impossible” to clean completely, according to a report published in Infection Control & Hospital Epidemiology.
“A new standard for the cleaning of complex surgical instruments needs to be established, especially for those used in robotic surgery,” wrote Yuhei Saito of the surgical center at the University of Tokyo Hospital and associates.
They assessed the residual contamination of both robotic and regular surgical instruments at their medical center because “hospital staff in central sterile supply departments are troubled by the reprocessing of robotic instruments because they cannot be disassembled for cleaning like other endoscopic instruments. Their complex structure impairs brushing the inner surface of narrow lumens, resulting in failure to [completely] remove contaminants,” the researchers wrote.
In the first phase of the study, the researchers examined 41 instruments immediately after they were used in robotic surgery (7 radical prostatectomies and 2 anterior resections of the rectum) and 27 regular instruments immediately after they were used for open surgery (gastrectomy and colectomy). The robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on the regular instruments, the investigators reported (Infect Control Hosp Epidemiol. 2016 Oct 31. doi: 10.1017/ice.2016.249).
In the second phase of the study, the researchers examined another 24 robotic instruments and 40 regular instruments after they were used in surgery and then cleaned according to the manufacturers’ instructions three successive times. For the robotic instruments, this involved manually brushing the outer surface while moving the instrument “wrists” through their full range of motion, followed by 15 minutes of ultrasonication with enzymatic detergent, flushing the lumen with a water gun through flush ports, and rinsing the entire instrument. For regular instruments, cleaning involved washer-disinfectors and included 5 minutes of ultrasonication, 10 minutes of spraying with an alkaline detergent, and 10 minutes of disinfection via heating.
The level of contamination declined with each successive cleaning but still remained comparatively high for the robotic instruments. The amount of protein contaminants released in the three cleanings was 650, 550, and 530 mcg per robotic instrument, compared with 16, 17, and 17 mcg per ordinary instrument.
The efficacy of cleaning was 97.6% for robotic instruments and 99.1% for regular instruments, the researchers reported.
This study was not designed to assess whether residual contamination is associated with adverse events such as infection in subsequent patients, and there are few data available on this topic.
“We have to recognize that there might be a considerable volume of insufficient cleaning or occult surgical site infections,” the investigators wrote.
New instrument washers equipped with a specific cleaning function for narrow lumens are becoming available, they noted, and “further study should be conducted using these washers with improved cleaning efficacy.”
The study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
Instruments used for robotic surgery are “virtually impossible” to clean completely, according to a report published in Infection Control & Hospital Epidemiology.
“A new standard for the cleaning of complex surgical instruments needs to be established, especially for those used in robotic surgery,” wrote Yuhei Saito of the surgical center at the University of Tokyo Hospital and associates.
They assessed the residual contamination of both robotic and regular surgical instruments at their medical center because “hospital staff in central sterile supply departments are troubled by the reprocessing of robotic instruments because they cannot be disassembled for cleaning like other endoscopic instruments. Their complex structure impairs brushing the inner surface of narrow lumens, resulting in failure to [completely] remove contaminants,” the researchers wrote.
In the first phase of the study, the researchers examined 41 instruments immediately after they were used in robotic surgery (7 radical prostatectomies and 2 anterior resections of the rectum) and 27 regular instruments immediately after they were used for open surgery (gastrectomy and colectomy). The robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on the regular instruments, the investigators reported (Infect Control Hosp Epidemiol. 2016 Oct 31. doi: 10.1017/ice.2016.249).
In the second phase of the study, the researchers examined another 24 robotic instruments and 40 regular instruments after they were used in surgery and then cleaned according to the manufacturers’ instructions three successive times. For the robotic instruments, this involved manually brushing the outer surface while moving the instrument “wrists” through their full range of motion, followed by 15 minutes of ultrasonication with enzymatic detergent, flushing the lumen with a water gun through flush ports, and rinsing the entire instrument. For regular instruments, cleaning involved washer-disinfectors and included 5 minutes of ultrasonication, 10 minutes of spraying with an alkaline detergent, and 10 minutes of disinfection via heating.
The level of contamination declined with each successive cleaning but still remained comparatively high for the robotic instruments. The amount of protein contaminants released in the three cleanings was 650, 550, and 530 mcg per robotic instrument, compared with 16, 17, and 17 mcg per ordinary instrument.
The efficacy of cleaning was 97.6% for robotic instruments and 99.1% for regular instruments, the researchers reported.
This study was not designed to assess whether residual contamination is associated with adverse events such as infection in subsequent patients, and there are few data available on this topic.
“We have to recognize that there might be a considerable volume of insufficient cleaning or occult surgical site infections,” the investigators wrote.
New instrument washers equipped with a specific cleaning function for narrow lumens are becoming available, they noted, and “further study should be conducted using these washers with improved cleaning efficacy.”
The study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
Instruments used for robotic surgery are “virtually impossible” to clean completely, according to a report published in Infection Control & Hospital Epidemiology.
“A new standard for the cleaning of complex surgical instruments needs to be established, especially for those used in robotic surgery,” wrote Yuhei Saito of the surgical center at the University of Tokyo Hospital and associates.
They assessed the residual contamination of both robotic and regular surgical instruments at their medical center because “hospital staff in central sterile supply departments are troubled by the reprocessing of robotic instruments because they cannot be disassembled for cleaning like other endoscopic instruments. Their complex structure impairs brushing the inner surface of narrow lumens, resulting in failure to [completely] remove contaminants,” the researchers wrote.
In the first phase of the study, the researchers examined 41 instruments immediately after they were used in robotic surgery (7 radical prostatectomies and 2 anterior resections of the rectum) and 27 regular instruments immediately after they were used for open surgery (gastrectomy and colectomy). The robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on the regular instruments, the investigators reported (Infect Control Hosp Epidemiol. 2016 Oct 31. doi: 10.1017/ice.2016.249).
In the second phase of the study, the researchers examined another 24 robotic instruments and 40 regular instruments after they were used in surgery and then cleaned according to the manufacturers’ instructions three successive times. For the robotic instruments, this involved manually brushing the outer surface while moving the instrument “wrists” through their full range of motion, followed by 15 minutes of ultrasonication with enzymatic detergent, flushing the lumen with a water gun through flush ports, and rinsing the entire instrument. For regular instruments, cleaning involved washer-disinfectors and included 5 minutes of ultrasonication, 10 minutes of spraying with an alkaline detergent, and 10 minutes of disinfection via heating.
The level of contamination declined with each successive cleaning but still remained comparatively high for the robotic instruments. The amount of protein contaminants released in the three cleanings was 650, 550, and 530 mcg per robotic instrument, compared with 16, 17, and 17 mcg per ordinary instrument.
The efficacy of cleaning was 97.6% for robotic instruments and 99.1% for regular instruments, the researchers reported.
This study was not designed to assess whether residual contamination is associated with adverse events such as infection in subsequent patients, and there are few data available on this topic.
“We have to recognize that there might be a considerable volume of insufficient cleaning or occult surgical site infections,” the investigators wrote.
New instrument washers equipped with a specific cleaning function for narrow lumens are becoming available, they noted, and “further study should be conducted using these washers with improved cleaning efficacy.”
The study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
FROM INFECTION CONTROL AND HOSPITAL EPIDEMIOLOGY
Key clinical point:
Major finding: Immediately after surgery, robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on regular instruments.
Data source: A single-center analysis of protein contamination before and after three successive cleanings on 65 instruments used for robotic surgery and 67 regular instruments used for open surgery.
Disclosures: This study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
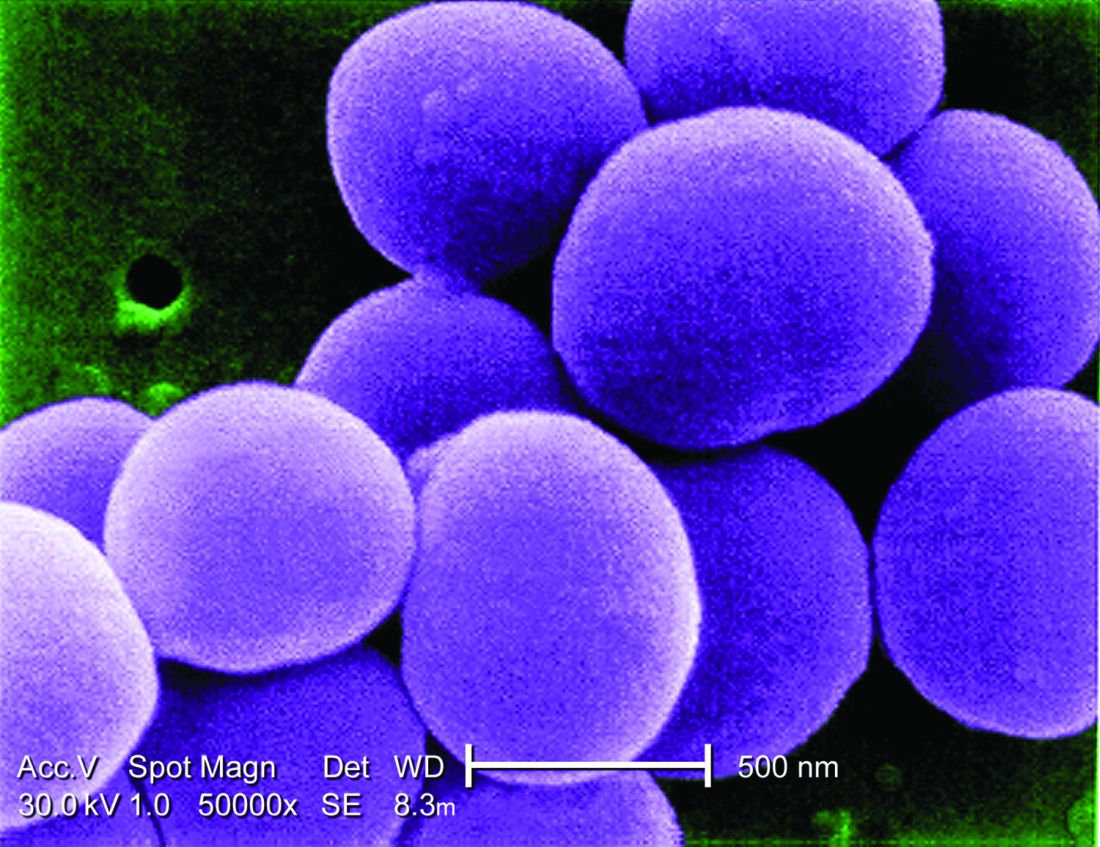
‘Skip phenomenon’ could explain fluctuating positivity for S. aureus bacteremia
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: No effect of donor on FMT outcomes in C. difficile patients
NEW ORLEANS – Fecal microbiota transplantation, or FMT, is a highly effective treatment for Clostridium difficile infection (CDI) and other digestive and autoimmune disorders, but little is known about the role of donor characteristics with respect to outcomes in patients with recurrent CDI.
A study of nearly 1,999 patients with an 83.9% cure rate showed no significant difference between 28 donors in terms of clinical outcomes at 8 weeks, according to Majdi Osman, MD, of OpenBiome, a not-for-profit stool bank in the Boston area.
Studies in inflammatory bowel diseases have suggested that donors do matter, but that does not appear to be the case when it comes to recurrent CDI, Dr. Osman said at an annual scientific meeting on infectious diseases.
“Broadly speaking, it seems like the efficacy rate is the same amongst all of our donors,” he said in a video interview at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Potential donors are subject to a rigorous screening process, and less than 3% are accepted, but given that donors were shown in previous studies to play a role in effectiveness in some other conditions, Dr. Osman said it was worth checking to see if outcomes in CDI could be further improved through donor selection.
In fact, it appears that “the donor doesn’t matter,” he said, noting that it may be that “we are selecting for a fairly narrow spectrum of the population, and actually the stool that we’re selecting is fairly similar in composition.”
Efforts are underway to look more closely at that possibility, and Dr. Osman said he hopes to see more standardized clinical trials and clinical follow-up. He also said he is excited about an FMT registry – a joint project of the American Gastroenterology Association and the Infectious Diseases Society of America – that will follow 4,000 patients for 10 years.
“We will be working closely with them to provide material and get some really good robust clinical data going forward,” he said.
Dr. Osman reported having no disclosures.
NEW ORLEANS – Fecal microbiota transplantation, or FMT, is a highly effective treatment for Clostridium difficile infection (CDI) and other digestive and autoimmune disorders, but little is known about the role of donor characteristics with respect to outcomes in patients with recurrent CDI.
A study of nearly 1,999 patients with an 83.9% cure rate showed no significant difference between 28 donors in terms of clinical outcomes at 8 weeks, according to Majdi Osman, MD, of OpenBiome, a not-for-profit stool bank in the Boston area.
Studies in inflammatory bowel diseases have suggested that donors do matter, but that does not appear to be the case when it comes to recurrent CDI, Dr. Osman said at an annual scientific meeting on infectious diseases.
“Broadly speaking, it seems like the efficacy rate is the same amongst all of our donors,” he said in a video interview at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Potential donors are subject to a rigorous screening process, and less than 3% are accepted, but given that donors were shown in previous studies to play a role in effectiveness in some other conditions, Dr. Osman said it was worth checking to see if outcomes in CDI could be further improved through donor selection.
In fact, it appears that “the donor doesn’t matter,” he said, noting that it may be that “we are selecting for a fairly narrow spectrum of the population, and actually the stool that we’re selecting is fairly similar in composition.”
Efforts are underway to look more closely at that possibility, and Dr. Osman said he hopes to see more standardized clinical trials and clinical follow-up. He also said he is excited about an FMT registry – a joint project of the American Gastroenterology Association and the Infectious Diseases Society of America – that will follow 4,000 patients for 10 years.
“We will be working closely with them to provide material and get some really good robust clinical data going forward,” he said.
Dr. Osman reported having no disclosures.
NEW ORLEANS – Fecal microbiota transplantation, or FMT, is a highly effective treatment for Clostridium difficile infection (CDI) and other digestive and autoimmune disorders, but little is known about the role of donor characteristics with respect to outcomes in patients with recurrent CDI.
A study of nearly 1,999 patients with an 83.9% cure rate showed no significant difference between 28 donors in terms of clinical outcomes at 8 weeks, according to Majdi Osman, MD, of OpenBiome, a not-for-profit stool bank in the Boston area.
Studies in inflammatory bowel diseases have suggested that donors do matter, but that does not appear to be the case when it comes to recurrent CDI, Dr. Osman said at an annual scientific meeting on infectious diseases.
“Broadly speaking, it seems like the efficacy rate is the same amongst all of our donors,” he said in a video interview at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Potential donors are subject to a rigorous screening process, and less than 3% are accepted, but given that donors were shown in previous studies to play a role in effectiveness in some other conditions, Dr. Osman said it was worth checking to see if outcomes in CDI could be further improved through donor selection.
In fact, it appears that “the donor doesn’t matter,” he said, noting that it may be that “we are selecting for a fairly narrow spectrum of the population, and actually the stool that we’re selecting is fairly similar in composition.”
Efforts are underway to look more closely at that possibility, and Dr. Osman said he hopes to see more standardized clinical trials and clinical follow-up. He also said he is excited about an FMT registry – a joint project of the American Gastroenterology Association and the Infectious Diseases Society of America – that will follow 4,000 patients for 10 years.
“We will be working closely with them to provide material and get some really good robust clinical data going forward,” he said.
Dr. Osman reported having no disclosures.
Treated bacteremia that clears, then recurs, termed ‘skip phenomenon’
NEW ORLEANS – When Mayo Clinic physicians noticed some patients on appropriate antibiotic treatment for Staphylococcus aureus bacteremia cleared the infection, only to see it recur a few days later, Justin A. Fiala, MD and his colleagues grew curious.
Dr. Fiala, an infectious diseases internist at Mayo Clinic, Rochester, Minn., was intrigued by the possibility of fluctuating blood culture positivity in this subset of bacteremia patients.
“We wanted first to see whether or not this is a real entity and determine the prevalence of this ‘skip pattern,’” Dr. Fiala said at IDWeek 2016, the annual combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association and the Pediatric Infectious Diseases Society. He said identifying predictors and finding any differences in clinical outcomes compared to control S. aureus bacteremia (SAB) patients were additional aims.
Dr. Fiala and his colleagues assessed a hospitalized cohort of 726 adults with SAB at Mayo Clinic between July 2006 and June 2011. Patients with one or more negative blood cultures followed by a positive culture were identified within this group, and compared with 2 to 4 patients matched for age, sex and duration of bacteremia who served as controls.
The investigators found 29 patients – or 4% – of the 726 had this ‘skip pattern’ of infection, clearance, and reinfection. Those with the phenomenon were 90% male and tended to be older, with a mean age of 69 years, compared to the controls. They had index bacteremia about two days longer than controls. The study also revealed a significant difference in mean number of central venous catheters: 2.7 in the skip phenomenon group versus 1.7 in controls.
Given the predominance of the skip phenomenon in older, immunosuppressed males, “the takeaway … is that serial negative blood cultures may be warranted in these patient groups,” Dr. Fiala said.
The groups did not differ significantly by presence of implants or foreign bodies or by whether SAB was nosocomial or acquired in the community. “We thought it was interesting that 90% had immune suppression, although it was not statistically significant,” Dr. Fiala said.
With no prior reports in the medical literature, the researchers named this clinical entity “skip phenomenon.” Dr. Fiala noted that published studies have assessed recurrence of SAB after completion of antibiotics, but not specifically during treatment.
“We think this is a topic that is quite clinically prevalent and applicable,” Dr. Fiala said. He pointed out that SAB is common, accounting for about 20% of all nosocomial bacteremia cases. SAB also highly virulent with a mortality rate estimated between 20% and 35%. Although the study did not reveal significant mortality differences in the subgroup with skip phenomenon, “we can say there is increased morbidity.”
The most recent IDSA guidelines state that a single set of negative blood cultures is sufficient to demonstrate clearance of SAB, Dr. Fiala said. “Could this be falsely reassuring if Staphylococcus aureus does have a tendency to exhibit this fluctuating pattern?”
The retrospective design of the study and the relatively small number of patients with the skip phenomenon were limitations, the investigators acknowledged. Dr. Fiala had no relevant disclosures.
NEW ORLEANS – When Mayo Clinic physicians noticed some patients on appropriate antibiotic treatment for Staphylococcus aureus bacteremia cleared the infection, only to see it recur a few days later, Justin A. Fiala, MD and his colleagues grew curious.
Dr. Fiala, an infectious diseases internist at Mayo Clinic, Rochester, Minn., was intrigued by the possibility of fluctuating blood culture positivity in this subset of bacteremia patients.
“We wanted first to see whether or not this is a real entity and determine the prevalence of this ‘skip pattern,’” Dr. Fiala said at IDWeek 2016, the annual combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association and the Pediatric Infectious Diseases Society. He said identifying predictors and finding any differences in clinical outcomes compared to control S. aureus bacteremia (SAB) patients were additional aims.
Dr. Fiala and his colleagues assessed a hospitalized cohort of 726 adults with SAB at Mayo Clinic between July 2006 and June 2011. Patients with one or more negative blood cultures followed by a positive culture were identified within this group, and compared with 2 to 4 patients matched for age, sex and duration of bacteremia who served as controls.
The investigators found 29 patients – or 4% – of the 726 had this ‘skip pattern’ of infection, clearance, and reinfection. Those with the phenomenon were 90% male and tended to be older, with a mean age of 69 years, compared to the controls. They had index bacteremia about two days longer than controls. The study also revealed a significant difference in mean number of central venous catheters: 2.7 in the skip phenomenon group versus 1.7 in controls.
Given the predominance of the skip phenomenon in older, immunosuppressed males, “the takeaway … is that serial negative blood cultures may be warranted in these patient groups,” Dr. Fiala said.
The groups did not differ significantly by presence of implants or foreign bodies or by whether SAB was nosocomial or acquired in the community. “We thought it was interesting that 90% had immune suppression, although it was not statistically significant,” Dr. Fiala said.
With no prior reports in the medical literature, the researchers named this clinical entity “skip phenomenon.” Dr. Fiala noted that published studies have assessed recurrence of SAB after completion of antibiotics, but not specifically during treatment.
“We think this is a topic that is quite clinically prevalent and applicable,” Dr. Fiala said. He pointed out that SAB is common, accounting for about 20% of all nosocomial bacteremia cases. SAB also highly virulent with a mortality rate estimated between 20% and 35%. Although the study did not reveal significant mortality differences in the subgroup with skip phenomenon, “we can say there is increased morbidity.”
The most recent IDSA guidelines state that a single set of negative blood cultures is sufficient to demonstrate clearance of SAB, Dr. Fiala said. “Could this be falsely reassuring if Staphylococcus aureus does have a tendency to exhibit this fluctuating pattern?”
The retrospective design of the study and the relatively small number of patients with the skip phenomenon were limitations, the investigators acknowledged. Dr. Fiala had no relevant disclosures.
NEW ORLEANS – When Mayo Clinic physicians noticed some patients on appropriate antibiotic treatment for Staphylococcus aureus bacteremia cleared the infection, only to see it recur a few days later, Justin A. Fiala, MD and his colleagues grew curious.
Dr. Fiala, an infectious diseases internist at Mayo Clinic, Rochester, Minn., was intrigued by the possibility of fluctuating blood culture positivity in this subset of bacteremia patients.
“We wanted first to see whether or not this is a real entity and determine the prevalence of this ‘skip pattern,’” Dr. Fiala said at IDWeek 2016, the annual combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association and the Pediatric Infectious Diseases Society. He said identifying predictors and finding any differences in clinical outcomes compared to control S. aureus bacteremia (SAB) patients were additional aims.
Dr. Fiala and his colleagues assessed a hospitalized cohort of 726 adults with SAB at Mayo Clinic between July 2006 and June 2011. Patients with one or more negative blood cultures followed by a positive culture were identified within this group, and compared with 2 to 4 patients matched for age, sex and duration of bacteremia who served as controls.
The investigators found 29 patients – or 4% – of the 726 had this ‘skip pattern’ of infection, clearance, and reinfection. Those with the phenomenon were 90% male and tended to be older, with a mean age of 69 years, compared to the controls. They had index bacteremia about two days longer than controls. The study also revealed a significant difference in mean number of central venous catheters: 2.7 in the skip phenomenon group versus 1.7 in controls.
Given the predominance of the skip phenomenon in older, immunosuppressed males, “the takeaway … is that serial negative blood cultures may be warranted in these patient groups,” Dr. Fiala said.
The groups did not differ significantly by presence of implants or foreign bodies or by whether SAB was nosocomial or acquired in the community. “We thought it was interesting that 90% had immune suppression, although it was not statistically significant,” Dr. Fiala said.
With no prior reports in the medical literature, the researchers named this clinical entity “skip phenomenon.” Dr. Fiala noted that published studies have assessed recurrence of SAB after completion of antibiotics, but not specifically during treatment.
“We think this is a topic that is quite clinically prevalent and applicable,” Dr. Fiala said. He pointed out that SAB is common, accounting for about 20% of all nosocomial bacteremia cases. SAB also highly virulent with a mortality rate estimated between 20% and 35%. Although the study did not reveal significant mortality differences in the subgroup with skip phenomenon, “we can say there is increased morbidity.”
The most recent IDSA guidelines state that a single set of negative blood cultures is sufficient to demonstrate clearance of SAB, Dr. Fiala said. “Could this be falsely reassuring if Staphylococcus aureus does have a tendency to exhibit this fluctuating pattern?”
The retrospective design of the study and the relatively small number of patients with the skip phenomenon were limitations, the investigators acknowledged. Dr. Fiala had no relevant disclosures.
Key clinical point:
Major finding: About 4% of S. aureus bacteremia cases may not clear completely, as judged by one negative blood culture, contrary to recent IDSA guidelines.
Data source: Nested case-control study of 726 adult inpatients at Mayo Clinic between July 2006 and June 2011 with ≥3 days of S. aureus bacteremia.
Disclosures: Dr. Fiala had no relevant disclosures.
Surgical treatment tops medical management of prosthetic valve endocarditis
NEW ORLEANS – Over the years patients with prosthetic valve endocarditis treated at Cleveland Clinic tended to fare better with surgery compared to medical management, some clinicians noted. However, there was no data to confirm their observations.
“It was not recognized widely. A lot of our colleagues continued to believe it could be adequately treated with the right antibiotic,” Nabin K. Shrestha, MD, said at the IDWeek 2016 annual meeting on infectious diseases.
So Dr Shrestha and his colleagues conducted a retrospective cohort study to compare outcomes between 253 surgically treated adults and 77 others treated medically between April 2008 and December 2012. Survival from the time of treatment decision was the primary outcome.
The groups differed on some demographic and clinical factors. For example, the medically treated group was older, had fewer men, and more patients with mitral valves. “We might think the medical patients might be too sick for surgery, and that could certainly be true, but … they could have been too well for surgery too,” Dr. Shrestha said. To control for these differences between groups, the investigators performed a number of statistical analyses, including a propensity score adjusted model and reduced Cox proportion hazards model.
“Patients with PVE have a high hazard of death if treated medically,” Dr. Shrestha said, based on a 6.68 hazard ratio. The higher risk of death associated with medical treatment remained significant when adjusted for age, sex, and other factors. “Compared to surgical treatment, medical treatment was associated with a seven-fold higher hazard of death overall,” Dr. Shrestha said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The medical treatment group also fared worse on a number of secondary outcomes. For example, this group had a five-fold higher risk of death during hospitalization compared to the surgery group (odds ratio, 4.65); a 12-fold higher risk of death within one year (OR, 11.70); a seven-fold higher risk of subsequent surgery for infective endocarditis (OR, 6.57); and an eight-fold higher odds of surgery for the same episode of infective endocarditis at a subsequent hospitalization (OR, 8.02).
A large sample size and setting the date of management decision as time zero to avoid survival selection bias “give us confidence in our findings.” Limitations include an inability to look at some important variables because of the retrospective design.
A meeting attendee commented that surgeons often request a patient be optimized medically prior to surgery, and asked if investigators looked at time from hospitalization to the operation.
“The median date from admission to surgery was six days in our database,” said Dr. Shrestha, who is a staff physician at the Cleveland Clinic in Ohio.
“Medical treatment overall is associated with significantly poorer outcomes in patients with PVE compared with surgical treatment,” Dr. Shrestha said. “Although some patients are not candidates for surgery, a definite diagnosis of PVE should prompt a surgical evaluation in the majority of patients.”
Dr. Shrestha reported having no disclosures.
NEW ORLEANS – Over the years patients with prosthetic valve endocarditis treated at Cleveland Clinic tended to fare better with surgery compared to medical management, some clinicians noted. However, there was no data to confirm their observations.
“It was not recognized widely. A lot of our colleagues continued to believe it could be adequately treated with the right antibiotic,” Nabin K. Shrestha, MD, said at the IDWeek 2016 annual meeting on infectious diseases.
So Dr Shrestha and his colleagues conducted a retrospective cohort study to compare outcomes between 253 surgically treated adults and 77 others treated medically between April 2008 and December 2012. Survival from the time of treatment decision was the primary outcome.
The groups differed on some demographic and clinical factors. For example, the medically treated group was older, had fewer men, and more patients with mitral valves. “We might think the medical patients might be too sick for surgery, and that could certainly be true, but … they could have been too well for surgery too,” Dr. Shrestha said. To control for these differences between groups, the investigators performed a number of statistical analyses, including a propensity score adjusted model and reduced Cox proportion hazards model.
“Patients with PVE have a high hazard of death if treated medically,” Dr. Shrestha said, based on a 6.68 hazard ratio. The higher risk of death associated with medical treatment remained significant when adjusted for age, sex, and other factors. “Compared to surgical treatment, medical treatment was associated with a seven-fold higher hazard of death overall,” Dr. Shrestha said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The medical treatment group also fared worse on a number of secondary outcomes. For example, this group had a five-fold higher risk of death during hospitalization compared to the surgery group (odds ratio, 4.65); a 12-fold higher risk of death within one year (OR, 11.70); a seven-fold higher risk of subsequent surgery for infective endocarditis (OR, 6.57); and an eight-fold higher odds of surgery for the same episode of infective endocarditis at a subsequent hospitalization (OR, 8.02).
A large sample size and setting the date of management decision as time zero to avoid survival selection bias “give us confidence in our findings.” Limitations include an inability to look at some important variables because of the retrospective design.
A meeting attendee commented that surgeons often request a patient be optimized medically prior to surgery, and asked if investigators looked at time from hospitalization to the operation.
“The median date from admission to surgery was six days in our database,” said Dr. Shrestha, who is a staff physician at the Cleveland Clinic in Ohio.
“Medical treatment overall is associated with significantly poorer outcomes in patients with PVE compared with surgical treatment,” Dr. Shrestha said. “Although some patients are not candidates for surgery, a definite diagnosis of PVE should prompt a surgical evaluation in the majority of patients.”
Dr. Shrestha reported having no disclosures.
NEW ORLEANS – Over the years patients with prosthetic valve endocarditis treated at Cleveland Clinic tended to fare better with surgery compared to medical management, some clinicians noted. However, there was no data to confirm their observations.
“It was not recognized widely. A lot of our colleagues continued to believe it could be adequately treated with the right antibiotic,” Nabin K. Shrestha, MD, said at the IDWeek 2016 annual meeting on infectious diseases.
So Dr Shrestha and his colleagues conducted a retrospective cohort study to compare outcomes between 253 surgically treated adults and 77 others treated medically between April 2008 and December 2012. Survival from the time of treatment decision was the primary outcome.
The groups differed on some demographic and clinical factors. For example, the medically treated group was older, had fewer men, and more patients with mitral valves. “We might think the medical patients might be too sick for surgery, and that could certainly be true, but … they could have been too well for surgery too,” Dr. Shrestha said. To control for these differences between groups, the investigators performed a number of statistical analyses, including a propensity score adjusted model and reduced Cox proportion hazards model.
“Patients with PVE have a high hazard of death if treated medically,” Dr. Shrestha said, based on a 6.68 hazard ratio. The higher risk of death associated with medical treatment remained significant when adjusted for age, sex, and other factors. “Compared to surgical treatment, medical treatment was associated with a seven-fold higher hazard of death overall,” Dr. Shrestha said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The medical treatment group also fared worse on a number of secondary outcomes. For example, this group had a five-fold higher risk of death during hospitalization compared to the surgery group (odds ratio, 4.65); a 12-fold higher risk of death within one year (OR, 11.70); a seven-fold higher risk of subsequent surgery for infective endocarditis (OR, 6.57); and an eight-fold higher odds of surgery for the same episode of infective endocarditis at a subsequent hospitalization (OR, 8.02).
A large sample size and setting the date of management decision as time zero to avoid survival selection bias “give us confidence in our findings.” Limitations include an inability to look at some important variables because of the retrospective design.
A meeting attendee commented that surgeons often request a patient be optimized medically prior to surgery, and asked if investigators looked at time from hospitalization to the operation.
“The median date from admission to surgery was six days in our database,” said Dr. Shrestha, who is a staff physician at the Cleveland Clinic in Ohio.
“Medical treatment overall is associated with significantly poorer outcomes in patients with PVE compared with surgical treatment,” Dr. Shrestha said. “Although some patients are not candidates for surgery, a definite diagnosis of PVE should prompt a surgical evaluation in the majority of patients.”
Dr. Shrestha reported having no disclosures.
Key clinical point:
Major finding: Compared to surgery, odds of death within one year higher were almost 7 times greater with medical treatment (hazard ratio, 6.68).
Data source: Presentation at IDWeek 2016
Disclosures: Dr. Nabin K. Shrestha had no relevant disclosures.