User login
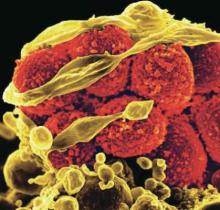
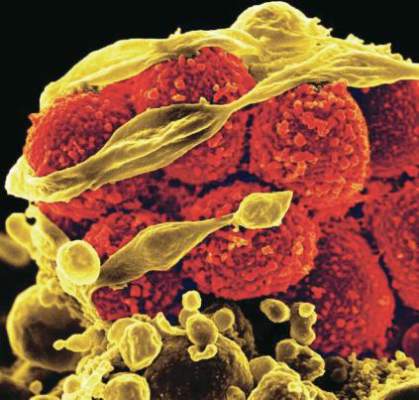
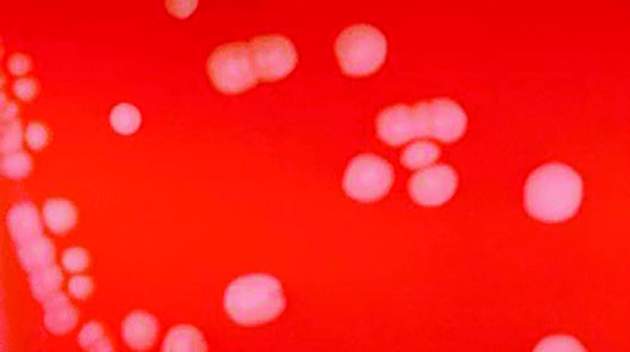
Diabetes, stroke linked to recurrent C. difficile
LAS VEGAS – Diabetes and stroke are risk factors for recurrent Clostridium difficile infection (CDI), with stroke patients at about 10 times the risk of recurrence.
The underlying cause for the association is a mystery, but one-sided paralysis is one possibility. “A lot of stroke patients may be hemiplegic, and they may be bedridden, so that may be a risk factor by itself. It’s something that may need to be studied in the future,” Alan Putrus, MD, a gastroenterology fellow at St. John Providence Hospital, Detroit, said in an interview.
CDI recurrence rates range from 5% to 47%, depending on the institution. Although risk factors of initial CDI have been well defined, few studies have looked at risk factors associated with recurrence.
In order to get at the question, the researchers conducted a study of 108 initial CDIs and 113 recurrences at two urban and one suburban hospital. Patients who experienced recurrence were matched 1:1 to age- and gender-matched controls with no recurrent CDI.
CDI recurrence rates were 16.5% and 15.9% in the two urban hospitals, and 14.9% in the suburban hospital.
Logistic regression revealed risk factors associated with CDI recurrence, including diabetes (odds ratio, 1.91; 95% confidence interval, 1.05-3.47; P = .04), stroke (OR, 9.73; 95% CI, 1.15-82.35; P = .04), exposure to proton pump inhibitors in the past 3 months (OR, 1.82; 95% CI, 1.03-3.23; P = .04), and admission to an intensive care unit in the past 3 months (OR, 1.95; 95% CI, 1.0-3.83; P = .04).
The results suggest that diabetes and especially stroke may be important risk factors for CDI recurrence, and their presence should prompt physicians to alter patient care accordingly, according to Dr. Putrus.
He stressed the importance of antibiotic stewardship. “Once you find a certain bug or pathogen, try to deescalate the antibiotics as soon as you can. If a patient is diabetic, controlling their blood sugar may also help,” Dr. Putrus said.
Finally, physicians should consider whether proton pump inhibitors are really necessary. Some patients start on PPIs but remain on the drugs long after symptoms have abated. “A lot of patients just have some discomfort in their abdomen, and they never stop taking it. They keep refilling it. So that’s a problem,” said Dr. Putrus.
Dr. Putrus has declared no conflicts of interest.
LAS VEGAS – Diabetes and stroke are risk factors for recurrent Clostridium difficile infection (CDI), with stroke patients at about 10 times the risk of recurrence.
The underlying cause for the association is a mystery, but one-sided paralysis is one possibility. “A lot of stroke patients may be hemiplegic, and they may be bedridden, so that may be a risk factor by itself. It’s something that may need to be studied in the future,” Alan Putrus, MD, a gastroenterology fellow at St. John Providence Hospital, Detroit, said in an interview.
CDI recurrence rates range from 5% to 47%, depending on the institution. Although risk factors of initial CDI have been well defined, few studies have looked at risk factors associated with recurrence.
In order to get at the question, the researchers conducted a study of 108 initial CDIs and 113 recurrences at two urban and one suburban hospital. Patients who experienced recurrence were matched 1:1 to age- and gender-matched controls with no recurrent CDI.
CDI recurrence rates were 16.5% and 15.9% in the two urban hospitals, and 14.9% in the suburban hospital.
Logistic regression revealed risk factors associated with CDI recurrence, including diabetes (odds ratio, 1.91; 95% confidence interval, 1.05-3.47; P = .04), stroke (OR, 9.73; 95% CI, 1.15-82.35; P = .04), exposure to proton pump inhibitors in the past 3 months (OR, 1.82; 95% CI, 1.03-3.23; P = .04), and admission to an intensive care unit in the past 3 months (OR, 1.95; 95% CI, 1.0-3.83; P = .04).
The results suggest that diabetes and especially stroke may be important risk factors for CDI recurrence, and their presence should prompt physicians to alter patient care accordingly, according to Dr. Putrus.
He stressed the importance of antibiotic stewardship. “Once you find a certain bug or pathogen, try to deescalate the antibiotics as soon as you can. If a patient is diabetic, controlling their blood sugar may also help,” Dr. Putrus said.
Finally, physicians should consider whether proton pump inhibitors are really necessary. Some patients start on PPIs but remain on the drugs long after symptoms have abated. “A lot of patients just have some discomfort in their abdomen, and they never stop taking it. They keep refilling it. So that’s a problem,” said Dr. Putrus.
Dr. Putrus has declared no conflicts of interest.
LAS VEGAS – Diabetes and stroke are risk factors for recurrent Clostridium difficile infection (CDI), with stroke patients at about 10 times the risk of recurrence.
The underlying cause for the association is a mystery, but one-sided paralysis is one possibility. “A lot of stroke patients may be hemiplegic, and they may be bedridden, so that may be a risk factor by itself. It’s something that may need to be studied in the future,” Alan Putrus, MD, a gastroenterology fellow at St. John Providence Hospital, Detroit, said in an interview.
CDI recurrence rates range from 5% to 47%, depending on the institution. Although risk factors of initial CDI have been well defined, few studies have looked at risk factors associated with recurrence.
In order to get at the question, the researchers conducted a study of 108 initial CDIs and 113 recurrences at two urban and one suburban hospital. Patients who experienced recurrence were matched 1:1 to age- and gender-matched controls with no recurrent CDI.
CDI recurrence rates were 16.5% and 15.9% in the two urban hospitals, and 14.9% in the suburban hospital.
Logistic regression revealed risk factors associated with CDI recurrence, including diabetes (odds ratio, 1.91; 95% confidence interval, 1.05-3.47; P = .04), stroke (OR, 9.73; 95% CI, 1.15-82.35; P = .04), exposure to proton pump inhibitors in the past 3 months (OR, 1.82; 95% CI, 1.03-3.23; P = .04), and admission to an intensive care unit in the past 3 months (OR, 1.95; 95% CI, 1.0-3.83; P = .04).
The results suggest that diabetes and especially stroke may be important risk factors for CDI recurrence, and their presence should prompt physicians to alter patient care accordingly, according to Dr. Putrus.
He stressed the importance of antibiotic stewardship. “Once you find a certain bug or pathogen, try to deescalate the antibiotics as soon as you can. If a patient is diabetic, controlling their blood sugar may also help,” Dr. Putrus said.
Finally, physicians should consider whether proton pump inhibitors are really necessary. Some patients start on PPIs but remain on the drugs long after symptoms have abated. “A lot of patients just have some discomfort in their abdomen, and they never stop taking it. They keep refilling it. So that’s a problem,” said Dr. Putrus.
Dr. Putrus has declared no conflicts of interest.
AT ACG 2016
Key clinical point:
Major finding: Diabetes, stroke, and a history of PPI use were all associated with higher risks of recurrence.
Data source: Case-control, retrospective study.
Disclosures: Dr. Putrus has declared no conflicts of interest.
C. difficile risk linked to antibiotic use in prior hospital bed occupant
Inpatients are at increased risk for Clostridium difficile infection if the previous occupant of their hospital bed received antibiotics, according to a report published online October 10 in JAMA Internal Medicine.
The increase in risk was characterized as “modest,” but it is important because the use of antibiotics in hospitals is so common. “Our results show that antibiotics can potentially cause harm to patients who do not themselves receive the antibiotics and thus emphasize the value of antibiotic stewardship,” said Daniel E. Freedberg, MD, a gastroenterologist at Columbia University, New York, and his associates (JAMA Intern Med. 2016 Oct 10. doi: 10.1001/jamainternmed.2016.6193).
They performed a large retrospective cohort study of sequentially hospitalized adults at four New York City area hospitals between 2010 and 2015. They focused on 100,615 pairs of patients in which the first patient was hospitalized for at least 24 hours and was discharged less than 1 week before the second patient was hospitalized in the same bed for at least 48 hours. A total of 576 “second patients” developed C. difficile infection 2 to14 days after hospitalization.
There were no C. difficile outbreaks during the study period, and the incidence of C. difficile infections remained constant. The “first patient” occupied the bed for a median of 3.0 days, and the median interval before the “second patient” arrived at the bed was 10 hours. Among those who developed a C. difficile infection, the median time from admission into the bed to the development of the infection was 6.4 days.
The cumulative incidence of C. difficile infections was significantly higher among second patients when the prior bed occupants had received antibiotics (0.72%) than when the prior bed occupants had not received antibiotics (0.43%). This correlation remained strong and significant when the data were adjusted to account for potential confounders such as the second patient’s comorbidities and use of antibiotics, the number of nearby patients who already had a C. difficile infection, and the type of hospital ward involved.
The strong association also persisted through numerous sensitivity analyses, including one that excluded the 1,497 patient pairs in which the first patient had had a recent C. difficile infection (adjusted hazard ratio, 1.20). In a further analysis examining multiple risk factors for infection, receipt of antibiotics by the “first patient” was the only factor associated with subsequent patients’ infection risk. The investigators noted that the four hospitals involved in this study were among the many that routinely single out the rooms of patients with C. difficile infection for intensive cleaning, including UV radiation.
These findings “support the hypothesis that antibiotics given to one patient may alter the local microenvironment to influence a different patients’ risk” for C. difficile infection, the investigators concluded.
The study was supported in part by the American Gastroenterological Association and the National Center for Advancing Translational Sciences. Dr. Freedberg and his associates reported having no relevant financial disclosures.
Inpatients are at increased risk for Clostridium difficile infection if the previous occupant of their hospital bed received antibiotics, according to a report published online October 10 in JAMA Internal Medicine.
The increase in risk was characterized as “modest,” but it is important because the use of antibiotics in hospitals is so common. “Our results show that antibiotics can potentially cause harm to patients who do not themselves receive the antibiotics and thus emphasize the value of antibiotic stewardship,” said Daniel E. Freedberg, MD, a gastroenterologist at Columbia University, New York, and his associates (JAMA Intern Med. 2016 Oct 10. doi: 10.1001/jamainternmed.2016.6193).
They performed a large retrospective cohort study of sequentially hospitalized adults at four New York City area hospitals between 2010 and 2015. They focused on 100,615 pairs of patients in which the first patient was hospitalized for at least 24 hours and was discharged less than 1 week before the second patient was hospitalized in the same bed for at least 48 hours. A total of 576 “second patients” developed C. difficile infection 2 to14 days after hospitalization.
There were no C. difficile outbreaks during the study period, and the incidence of C. difficile infections remained constant. The “first patient” occupied the bed for a median of 3.0 days, and the median interval before the “second patient” arrived at the bed was 10 hours. Among those who developed a C. difficile infection, the median time from admission into the bed to the development of the infection was 6.4 days.
The cumulative incidence of C. difficile infections was significantly higher among second patients when the prior bed occupants had received antibiotics (0.72%) than when the prior bed occupants had not received antibiotics (0.43%). This correlation remained strong and significant when the data were adjusted to account for potential confounders such as the second patient’s comorbidities and use of antibiotics, the number of nearby patients who already had a C. difficile infection, and the type of hospital ward involved.
The strong association also persisted through numerous sensitivity analyses, including one that excluded the 1,497 patient pairs in which the first patient had had a recent C. difficile infection (adjusted hazard ratio, 1.20). In a further analysis examining multiple risk factors for infection, receipt of antibiotics by the “first patient” was the only factor associated with subsequent patients’ infection risk. The investigators noted that the four hospitals involved in this study were among the many that routinely single out the rooms of patients with C. difficile infection for intensive cleaning, including UV radiation.
These findings “support the hypothesis that antibiotics given to one patient may alter the local microenvironment to influence a different patients’ risk” for C. difficile infection, the investigators concluded.
The study was supported in part by the American Gastroenterological Association and the National Center for Advancing Translational Sciences. Dr. Freedberg and his associates reported having no relevant financial disclosures.
Inpatients are at increased risk for Clostridium difficile infection if the previous occupant of their hospital bed received antibiotics, according to a report published online October 10 in JAMA Internal Medicine.
The increase in risk was characterized as “modest,” but it is important because the use of antibiotics in hospitals is so common. “Our results show that antibiotics can potentially cause harm to patients who do not themselves receive the antibiotics and thus emphasize the value of antibiotic stewardship,” said Daniel E. Freedberg, MD, a gastroenterologist at Columbia University, New York, and his associates (JAMA Intern Med. 2016 Oct 10. doi: 10.1001/jamainternmed.2016.6193).
They performed a large retrospective cohort study of sequentially hospitalized adults at four New York City area hospitals between 2010 and 2015. They focused on 100,615 pairs of patients in which the first patient was hospitalized for at least 24 hours and was discharged less than 1 week before the second patient was hospitalized in the same bed for at least 48 hours. A total of 576 “second patients” developed C. difficile infection 2 to14 days after hospitalization.
There were no C. difficile outbreaks during the study period, and the incidence of C. difficile infections remained constant. The “first patient” occupied the bed for a median of 3.0 days, and the median interval before the “second patient” arrived at the bed was 10 hours. Among those who developed a C. difficile infection, the median time from admission into the bed to the development of the infection was 6.4 days.
The cumulative incidence of C. difficile infections was significantly higher among second patients when the prior bed occupants had received antibiotics (0.72%) than when the prior bed occupants had not received antibiotics (0.43%). This correlation remained strong and significant when the data were adjusted to account for potential confounders such as the second patient’s comorbidities and use of antibiotics, the number of nearby patients who already had a C. difficile infection, and the type of hospital ward involved.
The strong association also persisted through numerous sensitivity analyses, including one that excluded the 1,497 patient pairs in which the first patient had had a recent C. difficile infection (adjusted hazard ratio, 1.20). In a further analysis examining multiple risk factors for infection, receipt of antibiotics by the “first patient” was the only factor associated with subsequent patients’ infection risk. The investigators noted that the four hospitals involved in this study were among the many that routinely single out the rooms of patients with C. difficile infection for intensive cleaning, including UV radiation.
These findings “support the hypothesis that antibiotics given to one patient may alter the local microenvironment to influence a different patients’ risk” for C. difficile infection, the investigators concluded.
The study was supported in part by the American Gastroenterological Association and the National Center for Advancing Translational Sciences. Dr. Freedberg and his associates reported having no relevant financial disclosures.
FROM JAMA INTERNAL MEDICINE
Levosimendan does not reduce organ dysfunction risk in sepsis
Levosimendan does not reduce the likelihood of severe organ dysfunction in adults with sepsis, nor does it lower the mortality rate, according to research presented at the annual congress of the European Society of Intensive Care Medicine and published in the New England Journal of Medicine.
Levosimendan is a calcium-sensitizing drug with inotropic and vasodilatory properties, which is commonly used to treat decompensated heart failure. “Small studies that have investigated the use of levosimendan in patients with septic shock have shown improvements in hemodynamic variables, microcirculatory flow, and renal and hepatic function, as compared with dobutamine,” wrote Anthony C. Gordon, MD, of Imperial College London and Imperial College Healthcare NHS Trust and his coauthors.
In the Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis (LeoPARDS) trial, 516 patients were randomized to 24 hours of a blinded infusion either of levosimendan (.05-0.2 mcg per kilogram of body weight per minute) or placebo in addition to standard care.
Researchers saw no significant difference in the mean daily Sequential Organ Failure Assessment (SOFA) score between the two groups (mean difference, 0.61; 95% confidence interval, −0.07 to 1.29; P = .053). When the SOFA score was analyzed by system, the mean daily cardiovascular score was significantly higher in the levosimendan group, compared with the placebo group, indicating greater dysfunction in that system.
“The cardiovascular SOFA score was higher in the levosimendan group than in the placebo group, which reflects the higher doses of norepinephrine that were required to maintain the mean arterial pressure,” researchers reported.
There was no significant difference in 28-day mortality between the levosimendan and placebo groups (34.5% vs. 30.9%; 95% CI, −4.5 to 11.7; P = .43), and both groups had a similar number of catecholamine-free days. However, among the patients who required ventilation at baseline, those treated with levosimendan were less likely than those given placebo to be successfully weaned from ventilation over the 28-day follow-up.
Patients treated with levosimendan also had a higher incidence of serious adverse events, and supraventricular tachyarrhythmia was significantly more common in the levosimendan group than in the placebo group (3.1% vs. 0.4%; 95% CI, 0.1- 5.3; P = .04).
The two groups showed similar cardiac index, stroke volume, central venous oxygen saturations or pressure, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, and serum creatinine and bilirubin levels.
The authors drew attention to several limitations of the study, including the fact that levosimendan was added to standard care rather than being compared with an alternative inotrope such as dobutamine.
“Less than 10% of the patients in the placebo group received dobutamine, although the rate of use in the placebo group was higher than in the levosimendan group and may explain in part why the cardiac index and stroke volume were not higher in the levosimendan group than in the placebo group,” they wrote.
The study did not include echocardiographic analysis to discover any changes in myocardial function with levosimendan, and there were only a small number of patients with low cardiac index.
“Therefore, this trial cannot provide guidance as to which inotrope is best to use in the management of sepsis if a low cardiac index is present,” the authors said. “The target mean arterial pressure of 65-70 mm Hg, which was recommended in the protocol and reiterated at investigator meetings, was frequently exceeded (as in other trials involving patients with shock), which suggests that the norepinephrine doses that were administered could have been reduced in the two trial groups.”
The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions, and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Levosimendan does not reduce the likelihood of severe organ dysfunction in adults with sepsis, nor does it lower the mortality rate, according to research presented at the annual congress of the European Society of Intensive Care Medicine and published in the New England Journal of Medicine.
Levosimendan is a calcium-sensitizing drug with inotropic and vasodilatory properties, which is commonly used to treat decompensated heart failure. “Small studies that have investigated the use of levosimendan in patients with septic shock have shown improvements in hemodynamic variables, microcirculatory flow, and renal and hepatic function, as compared with dobutamine,” wrote Anthony C. Gordon, MD, of Imperial College London and Imperial College Healthcare NHS Trust and his coauthors.
In the Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis (LeoPARDS) trial, 516 patients were randomized to 24 hours of a blinded infusion either of levosimendan (.05-0.2 mcg per kilogram of body weight per minute) or placebo in addition to standard care.
Researchers saw no significant difference in the mean daily Sequential Organ Failure Assessment (SOFA) score between the two groups (mean difference, 0.61; 95% confidence interval, −0.07 to 1.29; P = .053). When the SOFA score was analyzed by system, the mean daily cardiovascular score was significantly higher in the levosimendan group, compared with the placebo group, indicating greater dysfunction in that system.
“The cardiovascular SOFA score was higher in the levosimendan group than in the placebo group, which reflects the higher doses of norepinephrine that were required to maintain the mean arterial pressure,” researchers reported.
There was no significant difference in 28-day mortality between the levosimendan and placebo groups (34.5% vs. 30.9%; 95% CI, −4.5 to 11.7; P = .43), and both groups had a similar number of catecholamine-free days. However, among the patients who required ventilation at baseline, those treated with levosimendan were less likely than those given placebo to be successfully weaned from ventilation over the 28-day follow-up.
Patients treated with levosimendan also had a higher incidence of serious adverse events, and supraventricular tachyarrhythmia was significantly more common in the levosimendan group than in the placebo group (3.1% vs. 0.4%; 95% CI, 0.1- 5.3; P = .04).
The two groups showed similar cardiac index, stroke volume, central venous oxygen saturations or pressure, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, and serum creatinine and bilirubin levels.
The authors drew attention to several limitations of the study, including the fact that levosimendan was added to standard care rather than being compared with an alternative inotrope such as dobutamine.
“Less than 10% of the patients in the placebo group received dobutamine, although the rate of use in the placebo group was higher than in the levosimendan group and may explain in part why the cardiac index and stroke volume were not higher in the levosimendan group than in the placebo group,” they wrote.
The study did not include echocardiographic analysis to discover any changes in myocardial function with levosimendan, and there were only a small number of patients with low cardiac index.
“Therefore, this trial cannot provide guidance as to which inotrope is best to use in the management of sepsis if a low cardiac index is present,” the authors said. “The target mean arterial pressure of 65-70 mm Hg, which was recommended in the protocol and reiterated at investigator meetings, was frequently exceeded (as in other trials involving patients with shock), which suggests that the norepinephrine doses that were administered could have been reduced in the two trial groups.”
The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions, and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Levosimendan does not reduce the likelihood of severe organ dysfunction in adults with sepsis, nor does it lower the mortality rate, according to research presented at the annual congress of the European Society of Intensive Care Medicine and published in the New England Journal of Medicine.
Levosimendan is a calcium-sensitizing drug with inotropic and vasodilatory properties, which is commonly used to treat decompensated heart failure. “Small studies that have investigated the use of levosimendan in patients with septic shock have shown improvements in hemodynamic variables, microcirculatory flow, and renal and hepatic function, as compared with dobutamine,” wrote Anthony C. Gordon, MD, of Imperial College London and Imperial College Healthcare NHS Trust and his coauthors.
In the Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis (LeoPARDS) trial, 516 patients were randomized to 24 hours of a blinded infusion either of levosimendan (.05-0.2 mcg per kilogram of body weight per minute) or placebo in addition to standard care.
Researchers saw no significant difference in the mean daily Sequential Organ Failure Assessment (SOFA) score between the two groups (mean difference, 0.61; 95% confidence interval, −0.07 to 1.29; P = .053). When the SOFA score was analyzed by system, the mean daily cardiovascular score was significantly higher in the levosimendan group, compared with the placebo group, indicating greater dysfunction in that system.
“The cardiovascular SOFA score was higher in the levosimendan group than in the placebo group, which reflects the higher doses of norepinephrine that were required to maintain the mean arterial pressure,” researchers reported.
There was no significant difference in 28-day mortality between the levosimendan and placebo groups (34.5% vs. 30.9%; 95% CI, −4.5 to 11.7; P = .43), and both groups had a similar number of catecholamine-free days. However, among the patients who required ventilation at baseline, those treated with levosimendan were less likely than those given placebo to be successfully weaned from ventilation over the 28-day follow-up.
Patients treated with levosimendan also had a higher incidence of serious adverse events, and supraventricular tachyarrhythmia was significantly more common in the levosimendan group than in the placebo group (3.1% vs. 0.4%; 95% CI, 0.1- 5.3; P = .04).
The two groups showed similar cardiac index, stroke volume, central venous oxygen saturations or pressure, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, and serum creatinine and bilirubin levels.
The authors drew attention to several limitations of the study, including the fact that levosimendan was added to standard care rather than being compared with an alternative inotrope such as dobutamine.
“Less than 10% of the patients in the placebo group received dobutamine, although the rate of use in the placebo group was higher than in the levosimendan group and may explain in part why the cardiac index and stroke volume were not higher in the levosimendan group than in the placebo group,” they wrote.
The study did not include echocardiographic analysis to discover any changes in myocardial function with levosimendan, and there were only a small number of patients with low cardiac index.
“Therefore, this trial cannot provide guidance as to which inotrope is best to use in the management of sepsis if a low cardiac index is present,” the authors said. “The target mean arterial pressure of 65-70 mm Hg, which was recommended in the protocol and reiterated at investigator meetings, was frequently exceeded (as in other trials involving patients with shock), which suggests that the norepinephrine doses that were administered could have been reduced in the two trial groups.”
The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions, and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Key clinical point: Levosimendan does not reduce the likelihood of severe organ dysfunction or lower the mortality rate in adults with sepsis.
Major finding: There were no significant differences in mean daily Sequential Organ Failure Assessment score or mortality between patients treated with levosimendan or placebo in addition to standard care.
Data source: Randomized, placebo-controlled LeoPARDS trial in 516 adults with sepsis.
Disclosures: The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Striking the balance: Who should be screened for CP-CRE acquisition?
Carbapenem-resistant Enterobacteriaceae (CRE) are extremely drug-resistant organisms. According to the Centers for Disease Control and Prevention’s National Healthcare Safety Network, in 2014 in the United States, 3.6% of Enterobacteriaceae causing hospital-acquired infections were resistant to carbapenems.1 Antibiotic treatment options for CRE infections are severely limited, and mortality for invasive infections can be as high as 40%-50%.2
Resistance to carbapenems can be mediated by several mechanisms. From an epidemiologic standpoint, production of carbapenemases is the most-threatening mechanism because Enterobacteriaceae-harboring carbapenemases are highly transmissible.
Carbapenemase-producing CRE (CP-CRE) have caused large outbreaks throughout the world. Israel experienced a nationwide outbreak of CP-CRE, primarily Klebsiella pneumoniae carbapenemase–producing Klebsiella pneumoniae, in the mid-2000s. At the peak of the outbreak in 2007, there were 185 new cases per month (55.5/100,000 patient-days). A successful intervention at the national level dramatically decreased the incidence to 4.8/100,000 patient days in 2012.3
One component of the intervention (which is still ongoing) is active surveillance of high-risk groups using rectal swabs. Upon admission to the hospital, we screen patients who were recently in other hospitals or long-term care facilities. In addition, when a patient is newly diagnosed with CP-CRE (either asymptomatic carriage or clinical infection), we screen patients who had contact with that index case before isolation measures were implemented.
We recently published a study in Infection Control and Hospital Epidemiology that draws on our experience with CP-CRE screening of contacts at Tel Aviv Sourasky Medical Center.4 Both Israeli and International guidelines do not precisely define which contacts of a CP-CRE index case warrant screening. For example, should only roommates of index cases be screened or should we screen all patients on the same ward as the index case? Likewise, is there a minimum time of contact that should trigger screening?
Identifying which contacts are at high risk of acquiring CP-CRE is important for two reasons: We want to detect contacts who acquired CP-CRE so that they can be isolated before further transmission occurs, and we don’t want to waste resources and screen those at low risk. In our hospital, the criteria for being a contact are staying in the same ward and being treated by the same nursing staff as a newly identified CP-CRE patient.
This strategy appears to lead to overscreening, as we found that from October 2008 to June 2012, 3,158 screening tests were performed to detect 53 positive contacts (a yield of less than 2%). In order to screen more efficiently, our study aimed to determine risk factors for CP-CRE acquisition among patients exposed to a CP-CRE index patient.
We used a matched case-control design. The case group consisted of the 53 contacts who screened positive for CP-CRE. For each case we chose 2 controls: contacts who screened negative for CP-CRE. The basis for matching between the case and the 2 controls was that they were exposed to the same index patient. The benefit of matching this way was that it eliminated the question of whether a contact became positive because the index patient was more likely to transmit CP-CRE (e.g., because of diarrhea), and not because of characteristics of the contact patients themselves.
We found three factors that increased the risk that a contact would screen positive:
• Contact period of at least 3 days with the index case.
• Being on mechanical ventilation.
• Having a history of carriage or infection with another multidrug-resistant organism (such as methicillin-resistant Staphylococcus aureus).
Unexpectedly, sharing a room with the index patient or being debilitated did not significantly increase the risk of acquiring CP-CRE.
Many studies have identified antibiotic use as a risk factor for acquiring CP-CRE. In our study, no class of antibiotic increased the risk of CP-CRE acquisition, probably because only a small number of patients received each class. We were surprised to find that contacts who had taken cephalosporins were less likely to acquire CP-CRE. On further examination, when we compared patients who received only cephalosporins with patients who received no antibiotic, this protective effect disappeared. Nevertheless, compared with other antibiotics, it appears that cephalosporins might pose less of a risk for CP-CRE acquisition. More studies are needed to confirm our findings.
Our findings have practical implications for infection control. Using the risk factors we identified could help us to avoid excessive screening. We calculated that selective screening, based on our three risk factors, would have decreased the number of contacts screened by 30%, but 2 out of 53 positive contacts would have been missed. Institutions need to decide whether that is a trade-off they are willing to make.
Another way to apply our findings could be to add an additional layer of infection control by preemptively implementing contact precautions for patients at highest risk, for example, those with more than one risk factor.
1. Weiner LM, Fridkin SK, Aponte-Torres Z, Avery L, Coffin N, Dudeck MA, Edwards JR, Jernigan JA, Konnor R, Soe MM, Peterson K, Clifford McDonald L. Vital signs: preventing antibiotic-resistant infections in hospitals - United States, 2014. Am J Transplant. 2016 Jul;16(7):2224-30.
2. Centers for Disease Control and Prevention. Facility guidance for control of carbapenem-resistant Enterobacteriaceae (CRE): November 2015 update – CRE Toolkit.
3. Schwaber MJ, Carmeli Y. An ongoing national intervention to contain the spread of carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2014 Mar;58(5):697-703.
Schwartz-Neiderman A, Braun T, Fallach N, Schwartz D, Carmeli Y, Schechner V. Risk factors for carbapenemase-producing carbapenem-resistant Enterobacteriaceae (CP-CRE) acquisition among contacts of newly diagnosed CP-CRE patients. Infect Control Hosp Epidemiol. 2016 Jul 25:1-7.
Vered Schechner, MD, MSc, is an infection control physician in the department of epidemiology at Tel Aviv Sourasky Medical Center.
Carbapenem-resistant Enterobacteriaceae (CRE) are extremely drug-resistant organisms. According to the Centers for Disease Control and Prevention’s National Healthcare Safety Network, in 2014 in the United States, 3.6% of Enterobacteriaceae causing hospital-acquired infections were resistant to carbapenems.1 Antibiotic treatment options for CRE infections are severely limited, and mortality for invasive infections can be as high as 40%-50%.2
Resistance to carbapenems can be mediated by several mechanisms. From an epidemiologic standpoint, production of carbapenemases is the most-threatening mechanism because Enterobacteriaceae-harboring carbapenemases are highly transmissible.
Carbapenemase-producing CRE (CP-CRE) have caused large outbreaks throughout the world. Israel experienced a nationwide outbreak of CP-CRE, primarily Klebsiella pneumoniae carbapenemase–producing Klebsiella pneumoniae, in the mid-2000s. At the peak of the outbreak in 2007, there were 185 new cases per month (55.5/100,000 patient-days). A successful intervention at the national level dramatically decreased the incidence to 4.8/100,000 patient days in 2012.3
One component of the intervention (which is still ongoing) is active surveillance of high-risk groups using rectal swabs. Upon admission to the hospital, we screen patients who were recently in other hospitals or long-term care facilities. In addition, when a patient is newly diagnosed with CP-CRE (either asymptomatic carriage or clinical infection), we screen patients who had contact with that index case before isolation measures were implemented.
We recently published a study in Infection Control and Hospital Epidemiology that draws on our experience with CP-CRE screening of contacts at Tel Aviv Sourasky Medical Center.4 Both Israeli and International guidelines do not precisely define which contacts of a CP-CRE index case warrant screening. For example, should only roommates of index cases be screened or should we screen all patients on the same ward as the index case? Likewise, is there a minimum time of contact that should trigger screening?
Identifying which contacts are at high risk of acquiring CP-CRE is important for two reasons: We want to detect contacts who acquired CP-CRE so that they can be isolated before further transmission occurs, and we don’t want to waste resources and screen those at low risk. In our hospital, the criteria for being a contact are staying in the same ward and being treated by the same nursing staff as a newly identified CP-CRE patient.
This strategy appears to lead to overscreening, as we found that from October 2008 to June 2012, 3,158 screening tests were performed to detect 53 positive contacts (a yield of less than 2%). In order to screen more efficiently, our study aimed to determine risk factors for CP-CRE acquisition among patients exposed to a CP-CRE index patient.
We used a matched case-control design. The case group consisted of the 53 contacts who screened positive for CP-CRE. For each case we chose 2 controls: contacts who screened negative for CP-CRE. The basis for matching between the case and the 2 controls was that they were exposed to the same index patient. The benefit of matching this way was that it eliminated the question of whether a contact became positive because the index patient was more likely to transmit CP-CRE (e.g., because of diarrhea), and not because of characteristics of the contact patients themselves.
We found three factors that increased the risk that a contact would screen positive:
• Contact period of at least 3 days with the index case.
• Being on mechanical ventilation.
• Having a history of carriage or infection with another multidrug-resistant organism (such as methicillin-resistant Staphylococcus aureus).
Unexpectedly, sharing a room with the index patient or being debilitated did not significantly increase the risk of acquiring CP-CRE.
Many studies have identified antibiotic use as a risk factor for acquiring CP-CRE. In our study, no class of antibiotic increased the risk of CP-CRE acquisition, probably because only a small number of patients received each class. We were surprised to find that contacts who had taken cephalosporins were less likely to acquire CP-CRE. On further examination, when we compared patients who received only cephalosporins with patients who received no antibiotic, this protective effect disappeared. Nevertheless, compared with other antibiotics, it appears that cephalosporins might pose less of a risk for CP-CRE acquisition. More studies are needed to confirm our findings.
Our findings have practical implications for infection control. Using the risk factors we identified could help us to avoid excessive screening. We calculated that selective screening, based on our three risk factors, would have decreased the number of contacts screened by 30%, but 2 out of 53 positive contacts would have been missed. Institutions need to decide whether that is a trade-off they are willing to make.
Another way to apply our findings could be to add an additional layer of infection control by preemptively implementing contact precautions for patients at highest risk, for example, those with more than one risk factor.
1. Weiner LM, Fridkin SK, Aponte-Torres Z, Avery L, Coffin N, Dudeck MA, Edwards JR, Jernigan JA, Konnor R, Soe MM, Peterson K, Clifford McDonald L. Vital signs: preventing antibiotic-resistant infections in hospitals - United States, 2014. Am J Transplant. 2016 Jul;16(7):2224-30.
2. Centers for Disease Control and Prevention. Facility guidance for control of carbapenem-resistant Enterobacteriaceae (CRE): November 2015 update – CRE Toolkit.
3. Schwaber MJ, Carmeli Y. An ongoing national intervention to contain the spread of carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2014 Mar;58(5):697-703.
Schwartz-Neiderman A, Braun T, Fallach N, Schwartz D, Carmeli Y, Schechner V. Risk factors for carbapenemase-producing carbapenem-resistant Enterobacteriaceae (CP-CRE) acquisition among contacts of newly diagnosed CP-CRE patients. Infect Control Hosp Epidemiol. 2016 Jul 25:1-7.
Vered Schechner, MD, MSc, is an infection control physician in the department of epidemiology at Tel Aviv Sourasky Medical Center.
Carbapenem-resistant Enterobacteriaceae (CRE) are extremely drug-resistant organisms. According to the Centers for Disease Control and Prevention’s National Healthcare Safety Network, in 2014 in the United States, 3.6% of Enterobacteriaceae causing hospital-acquired infections were resistant to carbapenems.1 Antibiotic treatment options for CRE infections are severely limited, and mortality for invasive infections can be as high as 40%-50%.2
Resistance to carbapenems can be mediated by several mechanisms. From an epidemiologic standpoint, production of carbapenemases is the most-threatening mechanism because Enterobacteriaceae-harboring carbapenemases are highly transmissible.
Carbapenemase-producing CRE (CP-CRE) have caused large outbreaks throughout the world. Israel experienced a nationwide outbreak of CP-CRE, primarily Klebsiella pneumoniae carbapenemase–producing Klebsiella pneumoniae, in the mid-2000s. At the peak of the outbreak in 2007, there were 185 new cases per month (55.5/100,000 patient-days). A successful intervention at the national level dramatically decreased the incidence to 4.8/100,000 patient days in 2012.3
One component of the intervention (which is still ongoing) is active surveillance of high-risk groups using rectal swabs. Upon admission to the hospital, we screen patients who were recently in other hospitals or long-term care facilities. In addition, when a patient is newly diagnosed with CP-CRE (either asymptomatic carriage or clinical infection), we screen patients who had contact with that index case before isolation measures were implemented.
We recently published a study in Infection Control and Hospital Epidemiology that draws on our experience with CP-CRE screening of contacts at Tel Aviv Sourasky Medical Center.4 Both Israeli and International guidelines do not precisely define which contacts of a CP-CRE index case warrant screening. For example, should only roommates of index cases be screened or should we screen all patients on the same ward as the index case? Likewise, is there a minimum time of contact that should trigger screening?
Identifying which contacts are at high risk of acquiring CP-CRE is important for two reasons: We want to detect contacts who acquired CP-CRE so that they can be isolated before further transmission occurs, and we don’t want to waste resources and screen those at low risk. In our hospital, the criteria for being a contact are staying in the same ward and being treated by the same nursing staff as a newly identified CP-CRE patient.
This strategy appears to lead to overscreening, as we found that from October 2008 to June 2012, 3,158 screening tests were performed to detect 53 positive contacts (a yield of less than 2%). In order to screen more efficiently, our study aimed to determine risk factors for CP-CRE acquisition among patients exposed to a CP-CRE index patient.
We used a matched case-control design. The case group consisted of the 53 contacts who screened positive for CP-CRE. For each case we chose 2 controls: contacts who screened negative for CP-CRE. The basis for matching between the case and the 2 controls was that they were exposed to the same index patient. The benefit of matching this way was that it eliminated the question of whether a contact became positive because the index patient was more likely to transmit CP-CRE (e.g., because of diarrhea), and not because of characteristics of the contact patients themselves.
We found three factors that increased the risk that a contact would screen positive:
• Contact period of at least 3 days with the index case.
• Being on mechanical ventilation.
• Having a history of carriage or infection with another multidrug-resistant organism (such as methicillin-resistant Staphylococcus aureus).
Unexpectedly, sharing a room with the index patient or being debilitated did not significantly increase the risk of acquiring CP-CRE.
Many studies have identified antibiotic use as a risk factor for acquiring CP-CRE. In our study, no class of antibiotic increased the risk of CP-CRE acquisition, probably because only a small number of patients received each class. We were surprised to find that contacts who had taken cephalosporins were less likely to acquire CP-CRE. On further examination, when we compared patients who received only cephalosporins with patients who received no antibiotic, this protective effect disappeared. Nevertheless, compared with other antibiotics, it appears that cephalosporins might pose less of a risk for CP-CRE acquisition. More studies are needed to confirm our findings.
Our findings have practical implications for infection control. Using the risk factors we identified could help us to avoid excessive screening. We calculated that selective screening, based on our three risk factors, would have decreased the number of contacts screened by 30%, but 2 out of 53 positive contacts would have been missed. Institutions need to decide whether that is a trade-off they are willing to make.
Another way to apply our findings could be to add an additional layer of infection control by preemptively implementing contact precautions for patients at highest risk, for example, those with more than one risk factor.
1. Weiner LM, Fridkin SK, Aponte-Torres Z, Avery L, Coffin N, Dudeck MA, Edwards JR, Jernigan JA, Konnor R, Soe MM, Peterson K, Clifford McDonald L. Vital signs: preventing antibiotic-resistant infections in hospitals - United States, 2014. Am J Transplant. 2016 Jul;16(7):2224-30.
2. Centers for Disease Control and Prevention. Facility guidance for control of carbapenem-resistant Enterobacteriaceae (CRE): November 2015 update – CRE Toolkit.
3. Schwaber MJ, Carmeli Y. An ongoing national intervention to contain the spread of carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2014 Mar;58(5):697-703.
Schwartz-Neiderman A, Braun T, Fallach N, Schwartz D, Carmeli Y, Schechner V. Risk factors for carbapenemase-producing carbapenem-resistant Enterobacteriaceae (CP-CRE) acquisition among contacts of newly diagnosed CP-CRE patients. Infect Control Hosp Epidemiol. 2016 Jul 25:1-7.
Vered Schechner, MD, MSc, is an infection control physician in the department of epidemiology at Tel Aviv Sourasky Medical Center.
Steroids could reduce death rate for TB patients with acute respiratory failure
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Key clinical point: Corticosteroids used in combination with anti-TB treatment appeared to lower 90-day mortality in TB patients with ARF.
Major finding: Reduced 90-day mortality was associated with corticosteroid use (odds ratio, 0.47; 95% CI, 0.22-0.98; P = .049).
Data source: A retrospective cohort study of 124 patients admitted to intensive care units with TB and ARF in a single Korean center from 1989 to 2014.
Disclosures: The investigators reported no outside funding or conflicts of interest.
Seven days of antibiotics sufficient for most hospital-acquired pneumonia
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology of the infection, according to an updated Clinical Practice Guidelines for managing adults with these disorders.
In addition, every hospital should develop its own antibiogram to align clinicians’ choice of treatments with the local distribution of likely pathogens and their antimicrobial susceptibilities. Both of these recommendations, as well as others that are also new to the updated guidelines, are intended to minimize patient exposure to unnecessary antibiotics and reduce antibiotic resistance, said Andre C. Kalil, MD, and Mark L. Metersky, MD, cochairs of the guidelines panel of 18 experts in infectious diseases, pulmonary medicine, critical care medicine, laboratory medicine, microbiology, pharmacology, and guideline methodology.
The guidelines, an update of the last version issued in 2005 and developed jointly by representatives of the Infectious Disease Society of America (including Dr. Kalil) and the American Thoracic Society (including Dr. Metersky), are intended for use by all clinicians who care for patients at risk for hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP), including surgeons, anesthesiologists, and hospitalists as well as specialists in infectious diseases, pulmonary diseases, and critical care. The guidelines no longer use the concept of health care–associated pneumonia (HCAP), chiefly because new evidence shows that designation is too general: HCAP patients are not at high risk for multidrug-resistant organisms simply because of their contact with the health care system, the guidelines panel wrote (Clin Infect Dis. 2016 Sep 1;63[5]:e61-e111).
The IDSA/ATS Guidelines strongly recommend short-course (1-week) antibiotic therapy instead of longer courses for both HAP and VAP and assert that antibiotic doses should be de-escalated rather than fixed. It advises that serum procalcitonin level plus clinical criteria, not just clinical criteria alone, should be used to guide antibiotic discontinuation, and suggests that the Clinical Pulmonary Infection Score not be used to guide discontinuation.
The guidelines also address empiric treatments when MRSA is suspected and give detailed guidance for selecting antibiotics once the causative organism is identified, including Pseudomonas aeruginosa, extended-spectrum beta-lactamase–producing gram-negative bacilli, Acinetobacter species, and pathogens resistant to carbapenem.
The guidelines include numerous other recommendations concerning the diagnosis of HAP and VAP, the optimal initial treatments, the pharmacokinetic and pharmacodynamic optimization of antibiotic therapies, and the use of inhaled antibiotics. All the recommendations “are a compromise between the competing goals of providing early appropriate antibiotic coverage and avoiding superfluous treatment that may lead to adverse drug effects, Clostridium difficile infections, antibiotic resistance, and increased costs,” the guidelines panel noted.
The full-text guidelines, including details about the panel’s methodology in reviewing the current literature and the summaries of evidence that support each recommendation, is available free on the Clinical Infectious Diseases website.
The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
Key clinical point: A 1-week course of antibiotics is sufficient for most hospital-acquired and ventilator-associated pneumonia, regardless of the microbial etiology.
Major finding: The joint IDSA/ATS Guidelines include 25 recommendations regarding diagnosis, empiric therapy, and pathogen-targeted antibiotics for HAP and VAP.
Data source: An update to the 2005 Clinical Practice Guidelines for managing adults with HAP or VAP.
Disclosures: The Infectious Diseases Society of America and the American Thoracic Society provided financial and administrative support to develop the guidelines. No industry funding was permitted. Dr. Kalil reported having no potential conflicts of interest; Dr. Metersky reported ties to Aradigm, Gilead, Pfizer, Bayer, and their associates reported ties to numerous industry sources.
MRSA patients report signs of stigma tied to illness
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF HOSPITAL INFECTION
Key clinical point: Adults with methicillin-resistant Staphylococcus aureus (MRSA) are susceptible to stigma.
Major finding: Approximately half (56%) of adults being treated for MRSA reported stigma associated with their illness.
Data source: A cross-sectional study including 61 adults with MRSA.
Disclosures: The researchers had no financial conflicts to disclose.
Update on the third international consensus definitions for sepsis and septic shock
Sepsis is the primary cause of death from infection. Early identification and treatment of sepsis is important in improving patient outcomes. The consensus conference sought to differentiate sepsis, which is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” from uncomplicated infection.
Sepsis was last classified in a 2001 guideline that based its definition on the presence of two or more systemic inflammatory response syndrome (SIRS) criteria, which included an elevated temperature, heart rate higher than 90 bpm, respiratory rate higher than 20 breaths per minute, and a white blood cell count greater than greater than 12,000 mcL or less than 4,000 mcL or greater than 10% immature bands.
The problem with the SIRS definition of sepsis is that while it reflects a response to infection, it does not sufficiently distinguish between individuals with infections and those with a dysregulated response that leads to a poor prognosis, which is the definition of sepsis. The current consensus conference redefines sepsis with a more direct emphasis on organ dysfunction, as this is the aspect of sepsis that is most clearly linked to patient outcomes.
In the consensus conference document, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.” The guidelines recommend using the quick version of the sequential (sepsis-related) organ failure assessment score (qSOFA) to identify patients with sepsis. In its long form, the SOFA used seven clinical and laboratory data points for completion, and is best suited to use in an intensive care setting where detailed data are available. The qSOFA score has only three criteria and by being easier to use can aid in rapid identification of sepsis and the patients most likely to deteriorate from sepsis.
The qSOFA criteria predict poor outcome in patients with infection who have two or more of the following: respiratory rate greater than or equal to 22 breaths/min, new or worsened altered mentation, or systolic blood pressure less than or equal to 100 mm Hg. Unlike the full SOFA score, the qSOFA does not require any laboratory testing and so can be performed in the office or bedside on a hospital floor. The qSOFA does not necessarily define sepsis, rather it identifies patients at a higher risk of hospital death or prolonged ICU stay. The consensus conference suggests that “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, initiate or escalate therapy as appropriate, and consider referral to critical care or increase the frequency of monitoring, if such actions have not already been undertaken.” The task force suggested that the qSOFA score may be a helpful adjunct to best clinical judgment for identifying patients who might benefit from a higher level of care.
Septic shock is defined as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk for death than sepsis alone. Septic shock can be identified when, after adequate fluid resuscitation, the patient requires vasopressor therapy to maintain mean arterial pressure of at least 65 mm Hg and has a serum lactate level greater than 2 mmol/L.
Once sepsis is suspected, prompt therapy needs to be started as per the Surviving Sepsis Campaign Guidelines. The qSOFA criteria can be used to identify patients at high risk for morbidity and mortality. Within 3 hours, a lactate level should be obtained as well as blood cultures from two separate sites drawn prior to administration of antibiotics (but do not delay antibiotic administration). Empiric broad-spectrum antibiotics should be given within 45 minutes of the identification of sepsis. Antibiotic choice will vary per clinician/institution preference, but should likely include coverage for Pseudomonas and MRSA (piperacillin/tazobactam and vancomycin, for example). Antibiotics should be reassessed daily for de-escalation. Administer 30 mL/kg crystalloid for hypotension or lactate greater than or equal to 4 mmol/L. Within 6 hours, vasopressors should be given for hypotension that does not respond to initial fluid resuscitation to maintain a mean arterial pressure (MAP) of at least 65mm Hg. In the event of persistent hypotension after initial fluid administration (MAP under 65 mm Hg) or if initial lactate was greater than or equal to 4 mmol/L, volume status and tissue perfusion should be reassessed and lactate should be rechecked if it was initially elevated.
The bottom line
A 2016 international task force recommended that the definition of sepsis should be changed to emphasize organ dysfunction rather than a systemic inflammatory response. Use of the qSOFA score, which relies only on clinically observable data rather than laboratory evaluation, is recommended to identify patients at high risk for morbidity and mortality. Early recognition of sepsis and evaluation with qSOFT should facilitate early treatment and improve survival.
References
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) FRCP; JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6.
Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004 Mar;32(3):858-73.
Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Sepsis is the primary cause of death from infection. Early identification and treatment of sepsis is important in improving patient outcomes. The consensus conference sought to differentiate sepsis, which is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” from uncomplicated infection.
Sepsis was last classified in a 2001 guideline that based its definition on the presence of two or more systemic inflammatory response syndrome (SIRS) criteria, which included an elevated temperature, heart rate higher than 90 bpm, respiratory rate higher than 20 breaths per minute, and a white blood cell count greater than greater than 12,000 mcL or less than 4,000 mcL or greater than 10% immature bands.
The problem with the SIRS definition of sepsis is that while it reflects a response to infection, it does not sufficiently distinguish between individuals with infections and those with a dysregulated response that leads to a poor prognosis, which is the definition of sepsis. The current consensus conference redefines sepsis with a more direct emphasis on organ dysfunction, as this is the aspect of sepsis that is most clearly linked to patient outcomes.
In the consensus conference document, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.” The guidelines recommend using the quick version of the sequential (sepsis-related) organ failure assessment score (qSOFA) to identify patients with sepsis. In its long form, the SOFA used seven clinical and laboratory data points for completion, and is best suited to use in an intensive care setting where detailed data are available. The qSOFA score has only three criteria and by being easier to use can aid in rapid identification of sepsis and the patients most likely to deteriorate from sepsis.
The qSOFA criteria predict poor outcome in patients with infection who have two or more of the following: respiratory rate greater than or equal to 22 breaths/min, new or worsened altered mentation, or systolic blood pressure less than or equal to 100 mm Hg. Unlike the full SOFA score, the qSOFA does not require any laboratory testing and so can be performed in the office or bedside on a hospital floor. The qSOFA does not necessarily define sepsis, rather it identifies patients at a higher risk of hospital death or prolonged ICU stay. The consensus conference suggests that “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, initiate or escalate therapy as appropriate, and consider referral to critical care or increase the frequency of monitoring, if such actions have not already been undertaken.” The task force suggested that the qSOFA score may be a helpful adjunct to best clinical judgment for identifying patients who might benefit from a higher level of care.
Septic shock is defined as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk for death than sepsis alone. Septic shock can be identified when, after adequate fluid resuscitation, the patient requires vasopressor therapy to maintain mean arterial pressure of at least 65 mm Hg and has a serum lactate level greater than 2 mmol/L.
Once sepsis is suspected, prompt therapy needs to be started as per the Surviving Sepsis Campaign Guidelines. The qSOFA criteria can be used to identify patients at high risk for morbidity and mortality. Within 3 hours, a lactate level should be obtained as well as blood cultures from two separate sites drawn prior to administration of antibiotics (but do not delay antibiotic administration). Empiric broad-spectrum antibiotics should be given within 45 minutes of the identification of sepsis. Antibiotic choice will vary per clinician/institution preference, but should likely include coverage for Pseudomonas and MRSA (piperacillin/tazobactam and vancomycin, for example). Antibiotics should be reassessed daily for de-escalation. Administer 30 mL/kg crystalloid for hypotension or lactate greater than or equal to 4 mmol/L. Within 6 hours, vasopressors should be given for hypotension that does not respond to initial fluid resuscitation to maintain a mean arterial pressure (MAP) of at least 65mm Hg. In the event of persistent hypotension after initial fluid administration (MAP under 65 mm Hg) or if initial lactate was greater than or equal to 4 mmol/L, volume status and tissue perfusion should be reassessed and lactate should be rechecked if it was initially elevated.
The bottom line
A 2016 international task force recommended that the definition of sepsis should be changed to emphasize organ dysfunction rather than a systemic inflammatory response. Use of the qSOFA score, which relies only on clinically observable data rather than laboratory evaluation, is recommended to identify patients at high risk for morbidity and mortality. Early recognition of sepsis and evaluation with qSOFT should facilitate early treatment and improve survival.
References
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) FRCP; JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6.
Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004 Mar;32(3):858-73.
Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Sepsis is the primary cause of death from infection. Early identification and treatment of sepsis is important in improving patient outcomes. The consensus conference sought to differentiate sepsis, which is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” from uncomplicated infection.
Sepsis was last classified in a 2001 guideline that based its definition on the presence of two or more systemic inflammatory response syndrome (SIRS) criteria, which included an elevated temperature, heart rate higher than 90 bpm, respiratory rate higher than 20 breaths per minute, and a white blood cell count greater than greater than 12,000 mcL or less than 4,000 mcL or greater than 10% immature bands.
The problem with the SIRS definition of sepsis is that while it reflects a response to infection, it does not sufficiently distinguish between individuals with infections and those with a dysregulated response that leads to a poor prognosis, which is the definition of sepsis. The current consensus conference redefines sepsis with a more direct emphasis on organ dysfunction, as this is the aspect of sepsis that is most clearly linked to patient outcomes.
In the consensus conference document, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.” The guidelines recommend using the quick version of the sequential (sepsis-related) organ failure assessment score (qSOFA) to identify patients with sepsis. In its long form, the SOFA used seven clinical and laboratory data points for completion, and is best suited to use in an intensive care setting where detailed data are available. The qSOFA score has only three criteria and by being easier to use can aid in rapid identification of sepsis and the patients most likely to deteriorate from sepsis.
The qSOFA criteria predict poor outcome in patients with infection who have two or more of the following: respiratory rate greater than or equal to 22 breaths/min, new or worsened altered mentation, or systolic blood pressure less than or equal to 100 mm Hg. Unlike the full SOFA score, the qSOFA does not require any laboratory testing and so can be performed in the office or bedside on a hospital floor. The qSOFA does not necessarily define sepsis, rather it identifies patients at a higher risk of hospital death or prolonged ICU stay. The consensus conference suggests that “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, initiate or escalate therapy as appropriate, and consider referral to critical care or increase the frequency of monitoring, if such actions have not already been undertaken.” The task force suggested that the qSOFA score may be a helpful adjunct to best clinical judgment for identifying patients who might benefit from a higher level of care.
Septic shock is defined as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk for death than sepsis alone. Septic shock can be identified when, after adequate fluid resuscitation, the patient requires vasopressor therapy to maintain mean arterial pressure of at least 65 mm Hg and has a serum lactate level greater than 2 mmol/L.
Once sepsis is suspected, prompt therapy needs to be started as per the Surviving Sepsis Campaign Guidelines. The qSOFA criteria can be used to identify patients at high risk for morbidity and mortality. Within 3 hours, a lactate level should be obtained as well as blood cultures from two separate sites drawn prior to administration of antibiotics (but do not delay antibiotic administration). Empiric broad-spectrum antibiotics should be given within 45 minutes of the identification of sepsis. Antibiotic choice will vary per clinician/institution preference, but should likely include coverage for Pseudomonas and MRSA (piperacillin/tazobactam and vancomycin, for example). Antibiotics should be reassessed daily for de-escalation. Administer 30 mL/kg crystalloid for hypotension or lactate greater than or equal to 4 mmol/L. Within 6 hours, vasopressors should be given for hypotension that does not respond to initial fluid resuscitation to maintain a mean arterial pressure (MAP) of at least 65mm Hg. In the event of persistent hypotension after initial fluid administration (MAP under 65 mm Hg) or if initial lactate was greater than or equal to 4 mmol/L, volume status and tissue perfusion should be reassessed and lactate should be rechecked if it was initially elevated.
The bottom line
A 2016 international task force recommended that the definition of sepsis should be changed to emphasize organ dysfunction rather than a systemic inflammatory response. Use of the qSOFA score, which relies only on clinically observable data rather than laboratory evaluation, is recommended to identify patients at high risk for morbidity and mortality. Early recognition of sepsis and evaluation with qSOFT should facilitate early treatment and improve survival.
References
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) FRCP; JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6.
Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004 Mar;32(3):858-73.
Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Cytokine shows promise as biomarker for sepsis outcomes
LONDON – A cytokine known as tumor necrosis factor–related apoptosis-inducing ligand (TRAIL) is showing potential as a biomarker for evaluating the severity of sepsis and septic shock, according to results of a prospective study presented at the annual congress of the European Respiratory Society.
In a prospective study undertaken in patients administered to an intensive care unit, “lower levels of plasma TRAIL correlated with both organ system dysfunction and mortality,” reported Thomas Nicholson, MD, of Cornell University, New York.
A series of studies associating low levels of TRAIL with increased sepsis severity have attracted attention to this potential biomarker, according to Dr. Nicholson. In a mouse model of sepsis, for example, exogenous administration of TRAIL was associated with improved survival. In a clinical study conducted in CHINA that was cited by Dr. Nicholson, low levels of TRAIL correlated with lower rates of survival.
In the data presented at the ERS Congress, plasma TRAIL was collected from 108 patients on the first day of ICU admission. Of these patients 59 (54%) had sepsis and 23 (21%) had septic shock. Those with a noninfectious critical illness served as controls.
All patients with sepsis or septic shock were required to meet diagnostic criteria from the recently published Third International Consensus Definitions for Sepsis and Septic Shock (JAMA. 2016;315[8]:801-10). This is important because the newer criteria, relative to previous criteria, have “moved conceptually away from a condition defined by inflammatory biomarkers toward one that emphasizes signs of organ dysfunction,” Dr. Nicholson reported.
Although a dysregulated host response to infection is still a fundamental concept to the newer definition of sepsis, the importance of biomarkers of inflammation has been deemphasized, a change that would not be expected to favor an inflammatory cytokine as a biomarker.
Despite this, plasma TRAIL levels, which were measured with commercially available ELISA kits, were significantly lower for those with sepsis (P = .038) and for those with septic shock (P less than .001) relative to those with a noninfectious critical illness. There was a trend (P = .077) for lower plasma levels of TRAIL in patients with septic shock relative to sepsis.
In addition, there was a positive and significant correlation (r = –0.1983; P = .0397) between plasma TRAIL and degree of organ dysfunction as measured with the Sequential Organ Failure Assessment (SOFA) score. Higher plasma TRAIL levels also predicted survival at 28 days (P = .016). Although the overall mortality for patients with sepsis or septic shock in this series was 23%, there were no deaths among sepsis or septic shock patients with a TRAIL above the mean, which was 26.8 pg/mL.
“For every 10 mg/mL increase in TRAIL the odds ratio for survival increased by 1.9-fold,” Dr. Nicholson reported.
TRAIL is implicated in several processes that may explain these observations, according to Dr. Nicholson. For example, he reported that there is evidence that TRAIL induces apoptosis in neutrophils, a suspected mediator of sepsis-related injury.
“The observations in our study are consistent with a growing literature suggesting that TRAIL is an important mediator of inflammatory cells, such as neutrophils, tempering the degree of inflammation,” Dr. Nicholson explained.
More data are needed to verify that TRAIL is a clinically useful biomarker, but Dr. Nicholson emphasized that this is a promising area of research. He said the biomarker is being developed as a potential tool for evaluating sepsis severity.
Dr. Nicholson reported no relevant financial relationships.
LONDON – A cytokine known as tumor necrosis factor–related apoptosis-inducing ligand (TRAIL) is showing potential as a biomarker for evaluating the severity of sepsis and septic shock, according to results of a prospective study presented at the annual congress of the European Respiratory Society.
In a prospective study undertaken in patients administered to an intensive care unit, “lower levels of plasma TRAIL correlated with both organ system dysfunction and mortality,” reported Thomas Nicholson, MD, of Cornell University, New York.
A series of studies associating low levels of TRAIL with increased sepsis severity have attracted attention to this potential biomarker, according to Dr. Nicholson. In a mouse model of sepsis, for example, exogenous administration of TRAIL was associated with improved survival. In a clinical study conducted in CHINA that was cited by Dr. Nicholson, low levels of TRAIL correlated with lower rates of survival.
In the data presented at the ERS Congress, plasma TRAIL was collected from 108 patients on the first day of ICU admission. Of these patients 59 (54%) had sepsis and 23 (21%) had septic shock. Those with a noninfectious critical illness served as controls.
All patients with sepsis or septic shock were required to meet diagnostic criteria from the recently published Third International Consensus Definitions for Sepsis and Septic Shock (JAMA. 2016;315[8]:801-10). This is important because the newer criteria, relative to previous criteria, have “moved conceptually away from a condition defined by inflammatory biomarkers toward one that emphasizes signs of organ dysfunction,” Dr. Nicholson reported.
Although a dysregulated host response to infection is still a fundamental concept to the newer definition of sepsis, the importance of biomarkers of inflammation has been deemphasized, a change that would not be expected to favor an inflammatory cytokine as a biomarker.
Despite this, plasma TRAIL levels, which were measured with commercially available ELISA kits, were significantly lower for those with sepsis (P = .038) and for those with septic shock (P less than .001) relative to those with a noninfectious critical illness. There was a trend (P = .077) for lower plasma levels of TRAIL in patients with septic shock relative to sepsis.
In addition, there was a positive and significant correlation (r = –0.1983; P = .0397) between plasma TRAIL and degree of organ dysfunction as measured with the Sequential Organ Failure Assessment (SOFA) score. Higher plasma TRAIL levels also predicted survival at 28 days (P = .016). Although the overall mortality for patients with sepsis or septic shock in this series was 23%, there were no deaths among sepsis or septic shock patients with a TRAIL above the mean, which was 26.8 pg/mL.
“For every 10 mg/mL increase in TRAIL the odds ratio for survival increased by 1.9-fold,” Dr. Nicholson reported.
TRAIL is implicated in several processes that may explain these observations, according to Dr. Nicholson. For example, he reported that there is evidence that TRAIL induces apoptosis in neutrophils, a suspected mediator of sepsis-related injury.
“The observations in our study are consistent with a growing literature suggesting that TRAIL is an important mediator of inflammatory cells, such as neutrophils, tempering the degree of inflammation,” Dr. Nicholson explained.
More data are needed to verify that TRAIL is a clinically useful biomarker, but Dr. Nicholson emphasized that this is a promising area of research. He said the biomarker is being developed as a potential tool for evaluating sepsis severity.
Dr. Nicholson reported no relevant financial relationships.
LONDON – A cytokine known as tumor necrosis factor–related apoptosis-inducing ligand (TRAIL) is showing potential as a biomarker for evaluating the severity of sepsis and septic shock, according to results of a prospective study presented at the annual congress of the European Respiratory Society.
In a prospective study undertaken in patients administered to an intensive care unit, “lower levels of plasma TRAIL correlated with both organ system dysfunction and mortality,” reported Thomas Nicholson, MD, of Cornell University, New York.
A series of studies associating low levels of TRAIL with increased sepsis severity have attracted attention to this potential biomarker, according to Dr. Nicholson. In a mouse model of sepsis, for example, exogenous administration of TRAIL was associated with improved survival. In a clinical study conducted in CHINA that was cited by Dr. Nicholson, low levels of TRAIL correlated with lower rates of survival.
In the data presented at the ERS Congress, plasma TRAIL was collected from 108 patients on the first day of ICU admission. Of these patients 59 (54%) had sepsis and 23 (21%) had septic shock. Those with a noninfectious critical illness served as controls.
All patients with sepsis or septic shock were required to meet diagnostic criteria from the recently published Third International Consensus Definitions for Sepsis and Septic Shock (JAMA. 2016;315[8]:801-10). This is important because the newer criteria, relative to previous criteria, have “moved conceptually away from a condition defined by inflammatory biomarkers toward one that emphasizes signs of organ dysfunction,” Dr. Nicholson reported.
Although a dysregulated host response to infection is still a fundamental concept to the newer definition of sepsis, the importance of biomarkers of inflammation has been deemphasized, a change that would not be expected to favor an inflammatory cytokine as a biomarker.
Despite this, plasma TRAIL levels, which were measured with commercially available ELISA kits, were significantly lower for those with sepsis (P = .038) and for those with septic shock (P less than .001) relative to those with a noninfectious critical illness. There was a trend (P = .077) for lower plasma levels of TRAIL in patients with septic shock relative to sepsis.
In addition, there was a positive and significant correlation (r = –0.1983; P = .0397) between plasma TRAIL and degree of organ dysfunction as measured with the Sequential Organ Failure Assessment (SOFA) score. Higher plasma TRAIL levels also predicted survival at 28 days (P = .016). Although the overall mortality for patients with sepsis or septic shock in this series was 23%, there were no deaths among sepsis or septic shock patients with a TRAIL above the mean, which was 26.8 pg/mL.
“For every 10 mg/mL increase in TRAIL the odds ratio for survival increased by 1.9-fold,” Dr. Nicholson reported.
TRAIL is implicated in several processes that may explain these observations, according to Dr. Nicholson. For example, he reported that there is evidence that TRAIL induces apoptosis in neutrophils, a suspected mediator of sepsis-related injury.
“The observations in our study are consistent with a growing literature suggesting that TRAIL is an important mediator of inflammatory cells, such as neutrophils, tempering the degree of inflammation,” Dr. Nicholson explained.
More data are needed to verify that TRAIL is a clinically useful biomarker, but Dr. Nicholson emphasized that this is a promising area of research. He said the biomarker is being developed as a potential tool for evaluating sepsis severity.
Dr. Nicholson reported no relevant financial relationships.
AT THE ERS CONGRESS 2016
Key clinical point: A biomarker – TRAIL – is demonstrating promise as a tool to evaluate the presence and severity of sepsis and septic shock.
Major finding: In a prospective evaluation, low levels of TRAIL correlated with sepsis and organ dysfunction and higher levels of TRAIL were associated with survival.
Data source: Ongoing prospective cohort study.
Disclosures: Dr. Nicholson reported no relevant financial relationships.
CSF lactate concentration identifies postneurosurgical bacterial meningitis
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
FROM BMC INFECTIOUS DISEASES
Key clinical point: CSF lactate concentration accurately identifies bacterial meningitis that develops after neurosurgery.
Major finding: CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%.
Data source: A meta-analysis of five published studies involving 404 patients during a 15-year period.
Disclosures: This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.