User login
CDC reports Burkholderia cepacia and B. pseudomallei outbreaks
The Centers for Disease Control and Prevention and Food and Drug Administration have announced an outbreak of at least 15 Burkholderia cepacia infections associated with contaminated ultrasound gel used to guide invasive procedures as well as an unrelated outbreak of Burkholderia pseudomallei that caused two deaths.
The procedures involved in the B. cepacia outbreak included placement of both central and peripheral intravenous catheters and paracentesis (removal of peritoneal fluid from the abdominal cavity). Cases have occurred in several states.
Further testing has shown the presence of Burkholderia stabilis, a member of B. cepacia complex (Bcc), in four lots of unopened bottles of MediChoice M500812 ultrasound gel. Eco-Med Pharmaceuticals of Etobicoke, Ont., the parent manufacturer, has issued a recall of MediChoice M500812 or Eco-Gel 200 with the following lot numbers: B029, B030, B031, B032, B040, B041, B048, B055. A similar outbreak occurred in Canada.
Some of these cases resulted in bloodstream infections. Further details are not yet available. Bcc infections have ranged from asymptomatic to life-threatening pneumonias, particularly in patients with cystic fibrosis. Other risk factors include immunosuppression, mechanical ventilation, and the use of other invasive venous or urinary catheters.
Kiran M. Perkins, MD, MPH, outbreak lead with the CDC’s Prevention Research Branch, said in an interview via email that automated systems such as Vitek might have trouble identifying the organism as “the system may only reveal the microbial species at the genus level but not at the species level, and/or it may have difficulty distinguishing between members of closely related group members.”
In the CDC’s experience, “most facilities do not conduct further species identification.” The agency added that it cannot tell if there has been any increase in cases associated with COVID-19, as they are not notifiable diseases and the “CDC does not systematically collect information on B. cepacia complex infections.”
Rodney Rohde, PhD, professor of clinical laboratory science and chair of the clinical laboratory science program, Texas State University, San Marcos, told this news organization via email that Burkholderia’s “detection in the manufacturing process is difficult, and product recalls are frequent.” He added, “A recent review by the Food and Drug Administration in the U.S. found that almost 40% of contamination reports in both sterile and nonsterile pharmaceutical products were caused by Bcc bacteria.” Another problem is that they often create biofilms, so “they are tenacious environmental colonizers of medical equipment and surfaces in general.”
There have been many other outbreaks as a result to B. cepacia complex. Because it is often in the water supply used in pharmaceutical manufacturing and is resistant to preservatives, the FDA cautions that it poses a risk of contamination in all nonsterile, water-based drug products.
Recalls have included contaminated antiseptics, such as povidone iodine, benzalkonium chloride, and chlorhexidine gluconate. Contamination in manufacturing may not be uniform, and only some samples may be affected. Antiseptic mouthwashes have also been affected. So have nonbacterial soaps and docusate (a stool softener) solutions, and various personal care products, including nasal sprays, lotions, simethicone gas relief drops (Mylicon), and baby wipes.
Although Bcc are considered “objectionable organisms,” there have been no strong or consistent standards for their detection from the U.S. Pharmacopeia, and some manufacturers reportedly underestimate the consequences of contamination. The FDA issued a guidance to manufacturers in 2017 on quality assurance and cleaning procedures. This is particularly important since preservatives are ineffective against Bcc, and sterility has to be insured at each step of production.
Burkholderia isolates are generally resistant to commonly used antibiotics. Treatment might therefore include a combination of two drugs (to try to limit the emergence of more resistance) such as ceftazidime, piperacillin, meropenem with trimethoprim-sulfamethoxazole, or a beta-lactam plus aminoglycoside.
Interestingly, an outbreak of Burkholderia pseudomallei was just reported by the CDC as well. This is a related gram-negative bacillus which is quite uncommon in the United States. It causes melioidosis, usually a tropical infection, which presents with nonspecific symptoms or serious pneumonia, abscesses, or bloodstream infections.
Four cases have been identified this year in Georgia, Kansas, Minnesota, and Texas, two of them fatal. It is usually acquired from soil or water. By genomic analysis, the four cases are felt to be related, but no common source of exposure has been identified. They also appear to be closely related to South Asian strains, although none of the patients had traveled internationally. Prolonged antibiotic therapy with ceftazidime or meropenem, followed by 3-6 months of trimethoprim-sulfamethoxazole, is often required.
In his email, Dr. Rohde stated, “Melioidosis causes cough, chest pain, high fever, headache or unexplained weight loss, but it may take 2-3 weeks for symptoms of melioidosis to appear after a person’s initial exposure to the bacteria. So, one could see how this might be overlooked as COVID per symptoms and per the limitations of laboratory identification.”
It’s essential for clinicians to recognize that automated microbiology identification systems can misidentify B. pseudomallei as B. cepacia and to ask the lab for more specialized molecular diagnostics, particularly when relatively unusual organisms are isolated.
Candice Hoffmann, a public affairs specialist at the CDC, told this news organization that “clinicians should consider melioidosis as a differential diagnosis in both adult and pediatric patients who are suspected to have a bacterial infection (pneumonia, sepsis, meningitis, wound) and are not responding to antibacterial treatment, even if they have not traveled outside of the continental United States.”
Dr. Rohde has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention and Food and Drug Administration have announced an outbreak of at least 15 Burkholderia cepacia infections associated with contaminated ultrasound gel used to guide invasive procedures as well as an unrelated outbreak of Burkholderia pseudomallei that caused two deaths.
The procedures involved in the B. cepacia outbreak included placement of both central and peripheral intravenous catheters and paracentesis (removal of peritoneal fluid from the abdominal cavity). Cases have occurred in several states.
Further testing has shown the presence of Burkholderia stabilis, a member of B. cepacia complex (Bcc), in four lots of unopened bottles of MediChoice M500812 ultrasound gel. Eco-Med Pharmaceuticals of Etobicoke, Ont., the parent manufacturer, has issued a recall of MediChoice M500812 or Eco-Gel 200 with the following lot numbers: B029, B030, B031, B032, B040, B041, B048, B055. A similar outbreak occurred in Canada.
Some of these cases resulted in bloodstream infections. Further details are not yet available. Bcc infections have ranged from asymptomatic to life-threatening pneumonias, particularly in patients with cystic fibrosis. Other risk factors include immunosuppression, mechanical ventilation, and the use of other invasive venous or urinary catheters.
Kiran M. Perkins, MD, MPH, outbreak lead with the CDC’s Prevention Research Branch, said in an interview via email that automated systems such as Vitek might have trouble identifying the organism as “the system may only reveal the microbial species at the genus level but not at the species level, and/or it may have difficulty distinguishing between members of closely related group members.”
In the CDC’s experience, “most facilities do not conduct further species identification.” The agency added that it cannot tell if there has been any increase in cases associated with COVID-19, as they are not notifiable diseases and the “CDC does not systematically collect information on B. cepacia complex infections.”
Rodney Rohde, PhD, professor of clinical laboratory science and chair of the clinical laboratory science program, Texas State University, San Marcos, told this news organization via email that Burkholderia’s “detection in the manufacturing process is difficult, and product recalls are frequent.” He added, “A recent review by the Food and Drug Administration in the U.S. found that almost 40% of contamination reports in both sterile and nonsterile pharmaceutical products were caused by Bcc bacteria.” Another problem is that they often create biofilms, so “they are tenacious environmental colonizers of medical equipment and surfaces in general.”
There have been many other outbreaks as a result to B. cepacia complex. Because it is often in the water supply used in pharmaceutical manufacturing and is resistant to preservatives, the FDA cautions that it poses a risk of contamination in all nonsterile, water-based drug products.
Recalls have included contaminated antiseptics, such as povidone iodine, benzalkonium chloride, and chlorhexidine gluconate. Contamination in manufacturing may not be uniform, and only some samples may be affected. Antiseptic mouthwashes have also been affected. So have nonbacterial soaps and docusate (a stool softener) solutions, and various personal care products, including nasal sprays, lotions, simethicone gas relief drops (Mylicon), and baby wipes.
Although Bcc are considered “objectionable organisms,” there have been no strong or consistent standards for their detection from the U.S. Pharmacopeia, and some manufacturers reportedly underestimate the consequences of contamination. The FDA issued a guidance to manufacturers in 2017 on quality assurance and cleaning procedures. This is particularly important since preservatives are ineffective against Bcc, and sterility has to be insured at each step of production.
Burkholderia isolates are generally resistant to commonly used antibiotics. Treatment might therefore include a combination of two drugs (to try to limit the emergence of more resistance) such as ceftazidime, piperacillin, meropenem with trimethoprim-sulfamethoxazole, or a beta-lactam plus aminoglycoside.
Interestingly, an outbreak of Burkholderia pseudomallei was just reported by the CDC as well. This is a related gram-negative bacillus which is quite uncommon in the United States. It causes melioidosis, usually a tropical infection, which presents with nonspecific symptoms or serious pneumonia, abscesses, or bloodstream infections.
Four cases have been identified this year in Georgia, Kansas, Minnesota, and Texas, two of them fatal. It is usually acquired from soil or water. By genomic analysis, the four cases are felt to be related, but no common source of exposure has been identified. They also appear to be closely related to South Asian strains, although none of the patients had traveled internationally. Prolonged antibiotic therapy with ceftazidime or meropenem, followed by 3-6 months of trimethoprim-sulfamethoxazole, is often required.
In his email, Dr. Rohde stated, “Melioidosis causes cough, chest pain, high fever, headache or unexplained weight loss, but it may take 2-3 weeks for symptoms of melioidosis to appear after a person’s initial exposure to the bacteria. So, one could see how this might be overlooked as COVID per symptoms and per the limitations of laboratory identification.”
It’s essential for clinicians to recognize that automated microbiology identification systems can misidentify B. pseudomallei as B. cepacia and to ask the lab for more specialized molecular diagnostics, particularly when relatively unusual organisms are isolated.
Candice Hoffmann, a public affairs specialist at the CDC, told this news organization that “clinicians should consider melioidosis as a differential diagnosis in both adult and pediatric patients who are suspected to have a bacterial infection (pneumonia, sepsis, meningitis, wound) and are not responding to antibacterial treatment, even if they have not traveled outside of the continental United States.”
Dr. Rohde has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention and Food and Drug Administration have announced an outbreak of at least 15 Burkholderia cepacia infections associated with contaminated ultrasound gel used to guide invasive procedures as well as an unrelated outbreak of Burkholderia pseudomallei that caused two deaths.
The procedures involved in the B. cepacia outbreak included placement of both central and peripheral intravenous catheters and paracentesis (removal of peritoneal fluid from the abdominal cavity). Cases have occurred in several states.
Further testing has shown the presence of Burkholderia stabilis, a member of B. cepacia complex (Bcc), in four lots of unopened bottles of MediChoice M500812 ultrasound gel. Eco-Med Pharmaceuticals of Etobicoke, Ont., the parent manufacturer, has issued a recall of MediChoice M500812 or Eco-Gel 200 with the following lot numbers: B029, B030, B031, B032, B040, B041, B048, B055. A similar outbreak occurred in Canada.
Some of these cases resulted in bloodstream infections. Further details are not yet available. Bcc infections have ranged from asymptomatic to life-threatening pneumonias, particularly in patients with cystic fibrosis. Other risk factors include immunosuppression, mechanical ventilation, and the use of other invasive venous or urinary catheters.
Kiran M. Perkins, MD, MPH, outbreak lead with the CDC’s Prevention Research Branch, said in an interview via email that automated systems such as Vitek might have trouble identifying the organism as “the system may only reveal the microbial species at the genus level but not at the species level, and/or it may have difficulty distinguishing between members of closely related group members.”
In the CDC’s experience, “most facilities do not conduct further species identification.” The agency added that it cannot tell if there has been any increase in cases associated with COVID-19, as they are not notifiable diseases and the “CDC does not systematically collect information on B. cepacia complex infections.”
Rodney Rohde, PhD, professor of clinical laboratory science and chair of the clinical laboratory science program, Texas State University, San Marcos, told this news organization via email that Burkholderia’s “detection in the manufacturing process is difficult, and product recalls are frequent.” He added, “A recent review by the Food and Drug Administration in the U.S. found that almost 40% of contamination reports in both sterile and nonsterile pharmaceutical products were caused by Bcc bacteria.” Another problem is that they often create biofilms, so “they are tenacious environmental colonizers of medical equipment and surfaces in general.”
There have been many other outbreaks as a result to B. cepacia complex. Because it is often in the water supply used in pharmaceutical manufacturing and is resistant to preservatives, the FDA cautions that it poses a risk of contamination in all nonsterile, water-based drug products.
Recalls have included contaminated antiseptics, such as povidone iodine, benzalkonium chloride, and chlorhexidine gluconate. Contamination in manufacturing may not be uniform, and only some samples may be affected. Antiseptic mouthwashes have also been affected. So have nonbacterial soaps and docusate (a stool softener) solutions, and various personal care products, including nasal sprays, lotions, simethicone gas relief drops (Mylicon), and baby wipes.
Although Bcc are considered “objectionable organisms,” there have been no strong or consistent standards for their detection from the U.S. Pharmacopeia, and some manufacturers reportedly underestimate the consequences of contamination. The FDA issued a guidance to manufacturers in 2017 on quality assurance and cleaning procedures. This is particularly important since preservatives are ineffective against Bcc, and sterility has to be insured at each step of production.
Burkholderia isolates are generally resistant to commonly used antibiotics. Treatment might therefore include a combination of two drugs (to try to limit the emergence of more resistance) such as ceftazidime, piperacillin, meropenem with trimethoprim-sulfamethoxazole, or a beta-lactam plus aminoglycoside.
Interestingly, an outbreak of Burkholderia pseudomallei was just reported by the CDC as well. This is a related gram-negative bacillus which is quite uncommon in the United States. It causes melioidosis, usually a tropical infection, which presents with nonspecific symptoms or serious pneumonia, abscesses, or bloodstream infections.
Four cases have been identified this year in Georgia, Kansas, Minnesota, and Texas, two of them fatal. It is usually acquired from soil or water. By genomic analysis, the four cases are felt to be related, but no common source of exposure has been identified. They also appear to be closely related to South Asian strains, although none of the patients had traveled internationally. Prolonged antibiotic therapy with ceftazidime or meropenem, followed by 3-6 months of trimethoprim-sulfamethoxazole, is often required.
In his email, Dr. Rohde stated, “Melioidosis causes cough, chest pain, high fever, headache or unexplained weight loss, but it may take 2-3 weeks for symptoms of melioidosis to appear after a person’s initial exposure to the bacteria. So, one could see how this might be overlooked as COVID per symptoms and per the limitations of laboratory identification.”
It’s essential for clinicians to recognize that automated microbiology identification systems can misidentify B. pseudomallei as B. cepacia and to ask the lab for more specialized molecular diagnostics, particularly when relatively unusual organisms are isolated.
Candice Hoffmann, a public affairs specialist at the CDC, told this news organization that “clinicians should consider melioidosis as a differential diagnosis in both adult and pediatric patients who are suspected to have a bacterial infection (pneumonia, sepsis, meningitis, wound) and are not responding to antibacterial treatment, even if they have not traveled outside of the continental United States.”
Dr. Rohde has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Infective endocarditis with stroke after TAVR has ‘dismal’ prognosis
Patients who suffer a stroke during hospitalization for infective endocarditis (IE) after transcatheter aortic valve replacement (TAVR) have a dismal prognosis, with more than half dying during the index hospitalization and two-thirds within the first year, a new study shows.
The study – the first to evaluate stroke as an IE-related complication following TAVR in a large multicenter cohort – is published in the May 11 issue of the Journal of the American College of Cardiology.
The authors, led by David del Val, MD, Quebec Heart & Lung Institute, Quebec City, explain that IE after TAVR is a rare but serious complication associated with a high mortality rate. Neurologic events, especially stroke, remain one of the most common and potentially disabling IE-related complications, but until now, no study has attempted to evaluate the predictors of stroke and outcomes in patients with IE following TAVR.
For the current study, the authors analyzed data from the Infectious Endocarditis after TAVR International Registry, including 569 patients who developed definite IE following TAVR from 59 centers in 11 countries.
Patients who experienced a stroke during IE admission were compared with patients who did not have a stroke.
Results showed that 57 patients (10%) had a stroke during IE hospitalization, with no differences in the causative microorganism between groups. Stroke patients had higher rates of acute renal failure, systemic embolization, and persistent bacteremia.
Factors associated with a higher risk for stroke during the index IE hospitalization included stroke before IE, moderate or higher residual aortic regurgitation after TAVR, balloon-expandable valves, IE within 30 days after TAVR, and vegetation size greater than 8 mm.
The stroke rate was 3.1% in patients with none of these risk factors; 6.1% with one risk factor; 13.1% with two risk factors; 28.9% with three risk factors, and 60% with four risk factors.
“The presence of such factors (particularly in combination) may be considered for determining an earlier and more aggressive (medical or surgical) treatment in these patients,” the researchers say.
IE patients with stroke had higher rates of in-hospital mortality (54.4% vs. 28.7%) and overall mortality at 1 year (66.3% vs. 45.6%).
Surgery rates were low (25%) even in the presence of stroke and failed to improve outcomes in this population.
Noting that consensus guidelines for managing patients with IE recommend surgery along with antibiotic treatment for patients developing systemic embolism, particularly stroke, the researchers say their findings suggest that such surgery recommendations may not be extrapolated to TAVR-IE patients, and specific guidelines are warranted for this particular population.
Furthermore, the possibility of early surgery in those patients with factors increasing the risk for stroke should be evaluated in future studies.
The authors note that TAVR has revolutionized the treatment of aortic stenosis and is currently moving toward less complex and younger patients with lower surgical risk. Despite the relatively low incidence of IE after TAVR, the number of procedures is expected to grow exponentially, increasing the number of patients at risk of developing this life-threatening complication. Therefore, detailed knowledge of this disease and its complications is essential to improve outcomes.
They point out that the 10% rate of stroke found in this study is substantially lower, compared with the largest surgical prosthetic-valve infective endocarditis registries, but they suggest that the unique clinical profile of TAVR patients may lead to an underdiagnosis of stroke, with a high proportion of elderly patients who more frequently present with nonspecific symptoms.
They conclude that “IE post-TAVR is associated with a poor prognosis with high in-hospital and late mortality rates. Our study reveals that patients with IE after TAVR complicated by stroke showed an even worse prognosis.”
“The progressive implementation of advanced imaging modalities for early IE diagnosis, especially nuclear imaging, may translate into a better prognosis in coming years. Close attention should be paid to early recognition of stroke-associated factors to improve clinical outcomes,” they add.
In an accompanying editorial, Vuyisile Nkomo, MD, Daniel DeSimone, MD, and William Miranda, MD, Mayo Clinic, Rochester, Minn., say the current study “highlights the devastating consequences of IE after TAVR and the even worse consequences when IE was associated with stroke.”
This points to the critical importance of efforts to prevent IE with appropriate antibiotic prophylaxis and addressing potential sources of infection (for example, dental screening) before invasive cardiac procedures.
“Patient education is critical in regard to recognizing early signs and symptoms of IE. In particular, patients must be informed to obtain blood cultures with any episode of fever, as identification of bacteremia is critical in the diagnosis of IE,” the editorialists comment.
Endocarditis should also be suspected in afebrile patients with increasing transcatheter heart valve gradients or new or worsening regurgitation, they state.
Multimodality imaging is important for the early diagnosis of IE to facilitate prompt antibiotic treatment and potentially decrease the risk for IE complications, especially systemic embolization, they add.
“Despite the unequivocal advances in the safety and periprocedural complications of TAVR, IE with and without stroke in this TAVR population remains a dreadful complication,” they conclude.
Dr. Del Val was supported by a research grant from the Fundación Alfonso Martin Escudero. The editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients who suffer a stroke during hospitalization for infective endocarditis (IE) after transcatheter aortic valve replacement (TAVR) have a dismal prognosis, with more than half dying during the index hospitalization and two-thirds within the first year, a new study shows.
The study – the first to evaluate stroke as an IE-related complication following TAVR in a large multicenter cohort – is published in the May 11 issue of the Journal of the American College of Cardiology.
The authors, led by David del Val, MD, Quebec Heart & Lung Institute, Quebec City, explain that IE after TAVR is a rare but serious complication associated with a high mortality rate. Neurologic events, especially stroke, remain one of the most common and potentially disabling IE-related complications, but until now, no study has attempted to evaluate the predictors of stroke and outcomes in patients with IE following TAVR.
For the current study, the authors analyzed data from the Infectious Endocarditis after TAVR International Registry, including 569 patients who developed definite IE following TAVR from 59 centers in 11 countries.
Patients who experienced a stroke during IE admission were compared with patients who did not have a stroke.
Results showed that 57 patients (10%) had a stroke during IE hospitalization, with no differences in the causative microorganism between groups. Stroke patients had higher rates of acute renal failure, systemic embolization, and persistent bacteremia.
Factors associated with a higher risk for stroke during the index IE hospitalization included stroke before IE, moderate or higher residual aortic regurgitation after TAVR, balloon-expandable valves, IE within 30 days after TAVR, and vegetation size greater than 8 mm.
The stroke rate was 3.1% in patients with none of these risk factors; 6.1% with one risk factor; 13.1% with two risk factors; 28.9% with three risk factors, and 60% with four risk factors.
“The presence of such factors (particularly in combination) may be considered for determining an earlier and more aggressive (medical or surgical) treatment in these patients,” the researchers say.
IE patients with stroke had higher rates of in-hospital mortality (54.4% vs. 28.7%) and overall mortality at 1 year (66.3% vs. 45.6%).
Surgery rates were low (25%) even in the presence of stroke and failed to improve outcomes in this population.
Noting that consensus guidelines for managing patients with IE recommend surgery along with antibiotic treatment for patients developing systemic embolism, particularly stroke, the researchers say their findings suggest that such surgery recommendations may not be extrapolated to TAVR-IE patients, and specific guidelines are warranted for this particular population.
Furthermore, the possibility of early surgery in those patients with factors increasing the risk for stroke should be evaluated in future studies.
The authors note that TAVR has revolutionized the treatment of aortic stenosis and is currently moving toward less complex and younger patients with lower surgical risk. Despite the relatively low incidence of IE after TAVR, the number of procedures is expected to grow exponentially, increasing the number of patients at risk of developing this life-threatening complication. Therefore, detailed knowledge of this disease and its complications is essential to improve outcomes.
They point out that the 10% rate of stroke found in this study is substantially lower, compared with the largest surgical prosthetic-valve infective endocarditis registries, but they suggest that the unique clinical profile of TAVR patients may lead to an underdiagnosis of stroke, with a high proportion of elderly patients who more frequently present with nonspecific symptoms.
They conclude that “IE post-TAVR is associated with a poor prognosis with high in-hospital and late mortality rates. Our study reveals that patients with IE after TAVR complicated by stroke showed an even worse prognosis.”
“The progressive implementation of advanced imaging modalities for early IE diagnosis, especially nuclear imaging, may translate into a better prognosis in coming years. Close attention should be paid to early recognition of stroke-associated factors to improve clinical outcomes,” they add.
In an accompanying editorial, Vuyisile Nkomo, MD, Daniel DeSimone, MD, and William Miranda, MD, Mayo Clinic, Rochester, Minn., say the current study “highlights the devastating consequences of IE after TAVR and the even worse consequences when IE was associated with stroke.”
This points to the critical importance of efforts to prevent IE with appropriate antibiotic prophylaxis and addressing potential sources of infection (for example, dental screening) before invasive cardiac procedures.
“Patient education is critical in regard to recognizing early signs and symptoms of IE. In particular, patients must be informed to obtain blood cultures with any episode of fever, as identification of bacteremia is critical in the diagnosis of IE,” the editorialists comment.
Endocarditis should also be suspected in afebrile patients with increasing transcatheter heart valve gradients or new or worsening regurgitation, they state.
Multimodality imaging is important for the early diagnosis of IE to facilitate prompt antibiotic treatment and potentially decrease the risk for IE complications, especially systemic embolization, they add.
“Despite the unequivocal advances in the safety and periprocedural complications of TAVR, IE with and without stroke in this TAVR population remains a dreadful complication,” they conclude.
Dr. Del Val was supported by a research grant from the Fundación Alfonso Martin Escudero. The editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients who suffer a stroke during hospitalization for infective endocarditis (IE) after transcatheter aortic valve replacement (TAVR) have a dismal prognosis, with more than half dying during the index hospitalization and two-thirds within the first year, a new study shows.
The study – the first to evaluate stroke as an IE-related complication following TAVR in a large multicenter cohort – is published in the May 11 issue of the Journal of the American College of Cardiology.
The authors, led by David del Val, MD, Quebec Heart & Lung Institute, Quebec City, explain that IE after TAVR is a rare but serious complication associated with a high mortality rate. Neurologic events, especially stroke, remain one of the most common and potentially disabling IE-related complications, but until now, no study has attempted to evaluate the predictors of stroke and outcomes in patients with IE following TAVR.
For the current study, the authors analyzed data from the Infectious Endocarditis after TAVR International Registry, including 569 patients who developed definite IE following TAVR from 59 centers in 11 countries.
Patients who experienced a stroke during IE admission were compared with patients who did not have a stroke.
Results showed that 57 patients (10%) had a stroke during IE hospitalization, with no differences in the causative microorganism between groups. Stroke patients had higher rates of acute renal failure, systemic embolization, and persistent bacteremia.
Factors associated with a higher risk for stroke during the index IE hospitalization included stroke before IE, moderate or higher residual aortic regurgitation after TAVR, balloon-expandable valves, IE within 30 days after TAVR, and vegetation size greater than 8 mm.
The stroke rate was 3.1% in patients with none of these risk factors; 6.1% with one risk factor; 13.1% with two risk factors; 28.9% with three risk factors, and 60% with four risk factors.
“The presence of such factors (particularly in combination) may be considered for determining an earlier and more aggressive (medical or surgical) treatment in these patients,” the researchers say.
IE patients with stroke had higher rates of in-hospital mortality (54.4% vs. 28.7%) and overall mortality at 1 year (66.3% vs. 45.6%).
Surgery rates were low (25%) even in the presence of stroke and failed to improve outcomes in this population.
Noting that consensus guidelines for managing patients with IE recommend surgery along with antibiotic treatment for patients developing systemic embolism, particularly stroke, the researchers say their findings suggest that such surgery recommendations may not be extrapolated to TAVR-IE patients, and specific guidelines are warranted for this particular population.
Furthermore, the possibility of early surgery in those patients with factors increasing the risk for stroke should be evaluated in future studies.
The authors note that TAVR has revolutionized the treatment of aortic stenosis and is currently moving toward less complex and younger patients with lower surgical risk. Despite the relatively low incidence of IE after TAVR, the number of procedures is expected to grow exponentially, increasing the number of patients at risk of developing this life-threatening complication. Therefore, detailed knowledge of this disease and its complications is essential to improve outcomes.
They point out that the 10% rate of stroke found in this study is substantially lower, compared with the largest surgical prosthetic-valve infective endocarditis registries, but they suggest that the unique clinical profile of TAVR patients may lead to an underdiagnosis of stroke, with a high proportion of elderly patients who more frequently present with nonspecific symptoms.
They conclude that “IE post-TAVR is associated with a poor prognosis with high in-hospital and late mortality rates. Our study reveals that patients with IE after TAVR complicated by stroke showed an even worse prognosis.”
“The progressive implementation of advanced imaging modalities for early IE diagnosis, especially nuclear imaging, may translate into a better prognosis in coming years. Close attention should be paid to early recognition of stroke-associated factors to improve clinical outcomes,” they add.
In an accompanying editorial, Vuyisile Nkomo, MD, Daniel DeSimone, MD, and William Miranda, MD, Mayo Clinic, Rochester, Minn., say the current study “highlights the devastating consequences of IE after TAVR and the even worse consequences when IE was associated with stroke.”
This points to the critical importance of efforts to prevent IE with appropriate antibiotic prophylaxis and addressing potential sources of infection (for example, dental screening) before invasive cardiac procedures.
“Patient education is critical in regard to recognizing early signs and symptoms of IE. In particular, patients must be informed to obtain blood cultures with any episode of fever, as identification of bacteremia is critical in the diagnosis of IE,” the editorialists comment.
Endocarditis should also be suspected in afebrile patients with increasing transcatheter heart valve gradients or new or worsening regurgitation, they state.
Multimodality imaging is important for the early diagnosis of IE to facilitate prompt antibiotic treatment and potentially decrease the risk for IE complications, especially systemic embolization, they add.
“Despite the unequivocal advances in the safety and periprocedural complications of TAVR, IE with and without stroke in this TAVR population remains a dreadful complication,” they conclude.
Dr. Del Val was supported by a research grant from the Fundación Alfonso Martin Escudero. The editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Deaths tied to reprocessed urologic endoscopes, FDA warns
The U.S. Food and Drug Administration is warning health care providers about the risk for potentially life-threatening infections associated with reprocessed endoscopes used for viewing the urinary tract, including cystoscopes, cystouerthroscopes, and ureteroscopes.
The federal agency is investigating more than 450 medical device reports, including three reports of deaths, received between Jan. 1, 2017, and Feb. 20, 2021, that describe post-procedure infections and other possible contamination problems associated with the reprocessing or cleaning and sterilization of the devices.
Although it’s early in the investigation, on the basis of available data, the FDA believes the risk for infection is low.
“We are very concerned about the three reported deaths – outside of the United States – associated with these infections, and we’re acting fast to communicate with health care providers and the public about what we know and what is still an emerging issue,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement released on April 1.
Manufacturer Olympus Corporation submitted three reports of deaths attributed to a bacterial infection. In two of those reports, the infection was linked to a forceps/irrigation plug, an accessory component used to control water flow and enable access to the working channel of the endoscope. Lab tests confirmed that the bacteria that caused the infection was present in the forceps/irrigation plug.
The FDA said the third victim’s death involved a cystoscope that did not pass a leak test. It is possible that the damaged device was a factor in the patient’s becoming infected.
It’s not known to what degree the reported infections or patient comorbidities played a part in the patient deaths. The FDA also hasn’t concluded that any specific manufacturer or brand of these devices is associated with higher risks than others.
The FDA released recommendations for processing and using these devices and emphasized the importance of following manufacturers’ labeling and reprocessing instructions to minimize the risk for infection.
In addition to following reprocessing instructions, the recommendations include not using a device that has failed a leak test, developing schedules for routine device inspection and maintenance, and discussing the potential benefits and risks associated with procedures involving reprocessed urologic endoscopes with patients.
The newly reported concerns with urologic endoscopes are similar to problems associated with reprocessed duodenoscopes. In 2018, the FDA warned about higher-than-expected contamination rates for reprocessed duodenoscopes. The FDA has taken action on infections related to the reprocessing of duodenoscopes. In 2015, it required postmarket safety studies and the updating of sampling and culturing protocols. In 2019, the FDA approved single-use duodenoscopes in an effort to curb infections.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration is warning health care providers about the risk for potentially life-threatening infections associated with reprocessed endoscopes used for viewing the urinary tract, including cystoscopes, cystouerthroscopes, and ureteroscopes.
The federal agency is investigating more than 450 medical device reports, including three reports of deaths, received between Jan. 1, 2017, and Feb. 20, 2021, that describe post-procedure infections and other possible contamination problems associated with the reprocessing or cleaning and sterilization of the devices.
Although it’s early in the investigation, on the basis of available data, the FDA believes the risk for infection is low.
“We are very concerned about the three reported deaths – outside of the United States – associated with these infections, and we’re acting fast to communicate with health care providers and the public about what we know and what is still an emerging issue,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement released on April 1.
Manufacturer Olympus Corporation submitted three reports of deaths attributed to a bacterial infection. In two of those reports, the infection was linked to a forceps/irrigation plug, an accessory component used to control water flow and enable access to the working channel of the endoscope. Lab tests confirmed that the bacteria that caused the infection was present in the forceps/irrigation plug.
The FDA said the third victim’s death involved a cystoscope that did not pass a leak test. It is possible that the damaged device was a factor in the patient’s becoming infected.
It’s not known to what degree the reported infections or patient comorbidities played a part in the patient deaths. The FDA also hasn’t concluded that any specific manufacturer or brand of these devices is associated with higher risks than others.
The FDA released recommendations for processing and using these devices and emphasized the importance of following manufacturers’ labeling and reprocessing instructions to minimize the risk for infection.
In addition to following reprocessing instructions, the recommendations include not using a device that has failed a leak test, developing schedules for routine device inspection and maintenance, and discussing the potential benefits and risks associated with procedures involving reprocessed urologic endoscopes with patients.
The newly reported concerns with urologic endoscopes are similar to problems associated with reprocessed duodenoscopes. In 2018, the FDA warned about higher-than-expected contamination rates for reprocessed duodenoscopes. The FDA has taken action on infections related to the reprocessing of duodenoscopes. In 2015, it required postmarket safety studies and the updating of sampling and culturing protocols. In 2019, the FDA approved single-use duodenoscopes in an effort to curb infections.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration is warning health care providers about the risk for potentially life-threatening infections associated with reprocessed endoscopes used for viewing the urinary tract, including cystoscopes, cystouerthroscopes, and ureteroscopes.
The federal agency is investigating more than 450 medical device reports, including three reports of deaths, received between Jan. 1, 2017, and Feb. 20, 2021, that describe post-procedure infections and other possible contamination problems associated with the reprocessing or cleaning and sterilization of the devices.
Although it’s early in the investigation, on the basis of available data, the FDA believes the risk for infection is low.
“We are very concerned about the three reported deaths – outside of the United States – associated with these infections, and we’re acting fast to communicate with health care providers and the public about what we know and what is still an emerging issue,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement released on April 1.
Manufacturer Olympus Corporation submitted three reports of deaths attributed to a bacterial infection. In two of those reports, the infection was linked to a forceps/irrigation plug, an accessory component used to control water flow and enable access to the working channel of the endoscope. Lab tests confirmed that the bacteria that caused the infection was present in the forceps/irrigation plug.
The FDA said the third victim’s death involved a cystoscope that did not pass a leak test. It is possible that the damaged device was a factor in the patient’s becoming infected.
It’s not known to what degree the reported infections or patient comorbidities played a part in the patient deaths. The FDA also hasn’t concluded that any specific manufacturer or brand of these devices is associated with higher risks than others.
The FDA released recommendations for processing and using these devices and emphasized the importance of following manufacturers’ labeling and reprocessing instructions to minimize the risk for infection.
In addition to following reprocessing instructions, the recommendations include not using a device that has failed a leak test, developing schedules for routine device inspection and maintenance, and discussing the potential benefits and risks associated with procedures involving reprocessed urologic endoscopes with patients.
The newly reported concerns with urologic endoscopes are similar to problems associated with reprocessed duodenoscopes. In 2018, the FDA warned about higher-than-expected contamination rates for reprocessed duodenoscopes. The FDA has taken action on infections related to the reprocessing of duodenoscopes. In 2015, it required postmarket safety studies and the updating of sampling and culturing protocols. In 2019, the FDA approved single-use duodenoscopes in an effort to curb infections.
A version of this article first appeared on Medscape.com.
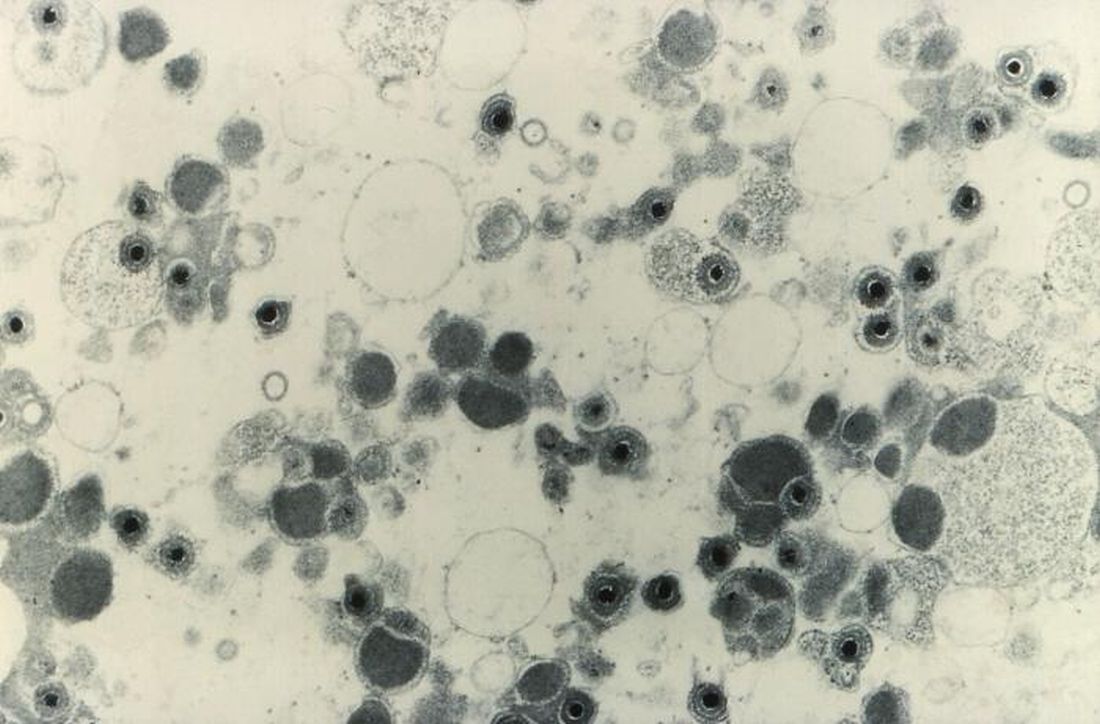
Maribavir seen as superior to other antivirals for CMV clearance post transplant
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
FROM TCT 2021
Hand hygiene in pediatric ICUs: Identifying areas for improvement
A multidisciplinary team seeking to measure compliance with hand hygiene (HH) practices in pediatric ICUs across Europe found compliance was comparable and relatively high among unit doctors and nurses, but not as high in nonunit doctors and nurses.
Ioannis Kopsidas, MD, presented these results from the RANIN-KIDS Network during the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. RANIN-KIDS (Reducing Antimicrobial Use and Nosocomial Infections in Kids) is a European network with the aim of preventing hospital-associated infections and promoting judicial antimicrobial use in pediatric patients using a common sustainable methodology across Europe.
Infections kill. This is especially the case in pediatric ICUs, where young age and an immunocompromised status make patients particularly vulnerable to infections. Poor HH is a major cause for disease transmission. To reduce the risk, the World Health Organization recommends attention to five moments of hand hygiene and nine steps for hand washing. Various tools are available to improve adherence, but whether these measures are being followed is unclear. The researchers sought to assess the degree of compliance with HH practices in pediatric ICUs and to identify targets for improvement.
Dr. Kopsidas, of the Center of Clinical Epidemiology and Outcomes Research, the National and Kapodistrian University of Athens, and colleagues examined practices in nine pediatric ICUs across six European countries (Estonia, Germany, Greece, Italy, Spain, and Switzerland) by means of prospective observational study. All organizations were part of the RANIN-KIDS network. Over a 6-month period starting in March 2019, observations were conducted in every unit by observers using a data collection tool developed based on WHO guidelines. Training for observers was provided using a self-paced teaching kit comprising PowerPoint and video presentations, followed by the completion of a test observation form after observing staged hand hygiene exercises. Results were then compared with WHO guidance, and irregularities were explained in order to achieve interrater reliability.
Researchers observed 1,715 HH opportunities. Across all pediatric ICUs, the median HH compliance rate was 82% (interquartile range, 72%-95%). Stratified by type of professional, median compliance was comparable among unit doctors (90%) and nurses (87%), but lower for nonunit doctors and nurses (81%) and also for nondoctors and nonnurses (67%). Alcohol-based hand rub was substantially preferred to soap and water, being used in 84% of the observations (IQR, 69%-87%). Cleaning and drying technique was considered appropriate in a median of 93% of observations (IQR, 86%-96%).
Compliance to moment 5 (after touching patient surroundings) was the lowest across hospitals (median 71%), compared with a median 100% for moment 2 (before clean/aseptic procedures) and a median 93% for moment 3 (after body fluid exposure/risk). For moment 1, median compliance was 87% (before touching a patient), and for moment 4, median compliance was 82% (after touching a patient).
Dr. Kopsidas concluded that the overall level of HH compliance among doctors and nurses working in European pediatric ICUs appears to be high, with moment 5 being the most frequently missed opportunity. Nonunit doctors and nurses and other personnel show lower WHO guidelines adherence. He stated that “these results will be used to design tailor-made interventions in participating units with the aim of reducing HAIs [health care–associated infections] and spread of multidrug resistant infections.”
He also said that “unified surveillance in Europe is possible and achievable, and allows for benchmarking among countries, institutions and wards.”
For some units, improving HH is a missed opportunity. The next stop for the RANIN-KIDS network is to look at the effects of interventions on reducing spread.
Dr. Kopsidas had no relevant financial disclosures.
A multidisciplinary team seeking to measure compliance with hand hygiene (HH) practices in pediatric ICUs across Europe found compliance was comparable and relatively high among unit doctors and nurses, but not as high in nonunit doctors and nurses.
Ioannis Kopsidas, MD, presented these results from the RANIN-KIDS Network during the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. RANIN-KIDS (Reducing Antimicrobial Use and Nosocomial Infections in Kids) is a European network with the aim of preventing hospital-associated infections and promoting judicial antimicrobial use in pediatric patients using a common sustainable methodology across Europe.
Infections kill. This is especially the case in pediatric ICUs, where young age and an immunocompromised status make patients particularly vulnerable to infections. Poor HH is a major cause for disease transmission. To reduce the risk, the World Health Organization recommends attention to five moments of hand hygiene and nine steps for hand washing. Various tools are available to improve adherence, but whether these measures are being followed is unclear. The researchers sought to assess the degree of compliance with HH practices in pediatric ICUs and to identify targets for improvement.
Dr. Kopsidas, of the Center of Clinical Epidemiology and Outcomes Research, the National and Kapodistrian University of Athens, and colleagues examined practices in nine pediatric ICUs across six European countries (Estonia, Germany, Greece, Italy, Spain, and Switzerland) by means of prospective observational study. All organizations were part of the RANIN-KIDS network. Over a 6-month period starting in March 2019, observations were conducted in every unit by observers using a data collection tool developed based on WHO guidelines. Training for observers was provided using a self-paced teaching kit comprising PowerPoint and video presentations, followed by the completion of a test observation form after observing staged hand hygiene exercises. Results were then compared with WHO guidance, and irregularities were explained in order to achieve interrater reliability.
Researchers observed 1,715 HH opportunities. Across all pediatric ICUs, the median HH compliance rate was 82% (interquartile range, 72%-95%). Stratified by type of professional, median compliance was comparable among unit doctors (90%) and nurses (87%), but lower for nonunit doctors and nurses (81%) and also for nondoctors and nonnurses (67%). Alcohol-based hand rub was substantially preferred to soap and water, being used in 84% of the observations (IQR, 69%-87%). Cleaning and drying technique was considered appropriate in a median of 93% of observations (IQR, 86%-96%).
Compliance to moment 5 (after touching patient surroundings) was the lowest across hospitals (median 71%), compared with a median 100% for moment 2 (before clean/aseptic procedures) and a median 93% for moment 3 (after body fluid exposure/risk). For moment 1, median compliance was 87% (before touching a patient), and for moment 4, median compliance was 82% (after touching a patient).
Dr. Kopsidas concluded that the overall level of HH compliance among doctors and nurses working in European pediatric ICUs appears to be high, with moment 5 being the most frequently missed opportunity. Nonunit doctors and nurses and other personnel show lower WHO guidelines adherence. He stated that “these results will be used to design tailor-made interventions in participating units with the aim of reducing HAIs [health care–associated infections] and spread of multidrug resistant infections.”
He also said that “unified surveillance in Europe is possible and achievable, and allows for benchmarking among countries, institutions and wards.”
For some units, improving HH is a missed opportunity. The next stop for the RANIN-KIDS network is to look at the effects of interventions on reducing spread.
Dr. Kopsidas had no relevant financial disclosures.
A multidisciplinary team seeking to measure compliance with hand hygiene (HH) practices in pediatric ICUs across Europe found compliance was comparable and relatively high among unit doctors and nurses, but not as high in nonunit doctors and nurses.
Ioannis Kopsidas, MD, presented these results from the RANIN-KIDS Network during the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. RANIN-KIDS (Reducing Antimicrobial Use and Nosocomial Infections in Kids) is a European network with the aim of preventing hospital-associated infections and promoting judicial antimicrobial use in pediatric patients using a common sustainable methodology across Europe.
Infections kill. This is especially the case in pediatric ICUs, where young age and an immunocompromised status make patients particularly vulnerable to infections. Poor HH is a major cause for disease transmission. To reduce the risk, the World Health Organization recommends attention to five moments of hand hygiene and nine steps for hand washing. Various tools are available to improve adherence, but whether these measures are being followed is unclear. The researchers sought to assess the degree of compliance with HH practices in pediatric ICUs and to identify targets for improvement.
Dr. Kopsidas, of the Center of Clinical Epidemiology and Outcomes Research, the National and Kapodistrian University of Athens, and colleagues examined practices in nine pediatric ICUs across six European countries (Estonia, Germany, Greece, Italy, Spain, and Switzerland) by means of prospective observational study. All organizations were part of the RANIN-KIDS network. Over a 6-month period starting in March 2019, observations were conducted in every unit by observers using a data collection tool developed based on WHO guidelines. Training for observers was provided using a self-paced teaching kit comprising PowerPoint and video presentations, followed by the completion of a test observation form after observing staged hand hygiene exercises. Results were then compared with WHO guidance, and irregularities were explained in order to achieve interrater reliability.
Researchers observed 1,715 HH opportunities. Across all pediatric ICUs, the median HH compliance rate was 82% (interquartile range, 72%-95%). Stratified by type of professional, median compliance was comparable among unit doctors (90%) and nurses (87%), but lower for nonunit doctors and nurses (81%) and also for nondoctors and nonnurses (67%). Alcohol-based hand rub was substantially preferred to soap and water, being used in 84% of the observations (IQR, 69%-87%). Cleaning and drying technique was considered appropriate in a median of 93% of observations (IQR, 86%-96%).
Compliance to moment 5 (after touching patient surroundings) was the lowest across hospitals (median 71%), compared with a median 100% for moment 2 (before clean/aseptic procedures) and a median 93% for moment 3 (after body fluid exposure/risk). For moment 1, median compliance was 87% (before touching a patient), and for moment 4, median compliance was 82% (after touching a patient).
Dr. Kopsidas concluded that the overall level of HH compliance among doctors and nurses working in European pediatric ICUs appears to be high, with moment 5 being the most frequently missed opportunity. Nonunit doctors and nurses and other personnel show lower WHO guidelines adherence. He stated that “these results will be used to design tailor-made interventions in participating units with the aim of reducing HAIs [health care–associated infections] and spread of multidrug resistant infections.”
He also said that “unified surveillance in Europe is possible and achievable, and allows for benchmarking among countries, institutions and wards.”
For some units, improving HH is a missed opportunity. The next stop for the RANIN-KIDS network is to look at the effects of interventions on reducing spread.
Dr. Kopsidas had no relevant financial disclosures.
FROM ESPID 2020
C. difficile control could require integrated approach
Clostridioides difficile (C. diff) infection (CDI) is a pathogen of both humans and animals, and to control it will require an integrated approach that encompasses human health care, veterinary health care, environmental regulation, and public policy. That is the conclusion of a group led by Su-Chen Lim, MD, and Tom Riley, MD, of Edith Cowan University in Australia, who published a review in Clinical Microbiology and Infection.
CDI was generally considered a nuisance infection until the early 21st century, when a hypervirulent fluoroquinolone-resistant strain emerged in North America. The strain is now documented In the United States, Canada, and most countries in Europe.
Another new feature of CDI is increased evidence of community transmission, which was previously rare. This is defined as cases where the patient experienced symptom onset outside the hospital, and had no history of hospitalization in the previous 12 weeks or symptom onset within 48 hours of hospital admission. Community-associated CDI now accounts for 41% of U.S. cases, nearly 30% of Australian cases, and about 14% in Europe, according to recent studies.
Several features of CDI suggest a need for an integrated management plan. The preferred habitat of C. diff is the gastrointestinal track of mammals, and likely colonizes all mammalian neonates. Over time, colonization by other microbes likely crowd it out and prevent overgrowth. But widespread use of antimicrobials in animal production can lead to the creation of an environment resembling that of the neonate, allowing C. diff to expand. That has led to food animals becoming a major C. diff reservoir, and whole-genome studies showed that strains found in humans, food, animals, and the environment are closely related and sometimes genetically indistinguishable, suggesting transmission between humans and animals that may be attributable to contaminated food and environments.
The authors suggest that C. diff infection control should be guided by the One Health initiative, which seeks cooperation between physicians, osteopathic physicians, veterinarians, dentists, nurses, and other scientific and environmental disciplines. The goal is to enhance surveillance and interdisciplinary communication, as well as integrated policies. The authors note that C. diff is often thought of by physicians as primarily a hospital problem, who may be unaware of the increased prevalence of community-acquired disease. It is also a significant problem in agriculture, since as many as 50% of piglets succumb to the disease. Other studies have recently shown that asymptomatic carriers of toxigenic strains are likely to transmit the bacteria to C. diff-negative patients. Asymptomatic carriers cluster with symptomatic patients. In one Cleveland hospital, more than 25% of hospital-associated CDI cases were found to have been colonized prior to admission, suggesting that these were not true hospital-associated cases.
C. diff has been isolated from a wide range of sources, including food animals, meat, seafood, vegetables, household environments, and natural environments like rivers, lakes, and soil. About 20% of calves and 70% of piglets are colonized with C. diff. It has a high prevalence in meat products in the United States, but lower in the Europe, possibly because of different slaughtering practices.
The authors suggest that zoonotic C. diff spread is unlikely to be confined to any geographic region or population, and that widespread C. diff contamination is occurring through food or the environment. This could be occurring because spores can withstand cooking temperatures and disseminate through the air, and even through manure from food animals made into compost or fertilizer.
Veterinary efforts mimicking hospital measures have reduced animal CDI, but there are no rapid diagnostic tests for CDI in animals, making it challenging to control its spread in this context.
The authors call for enhanced antimicrobial stewardship in both human and animal settings, including banning of antimicrobial agents as growth promoters. This has been done in the United States and Europe, but not in Brazil, China, Canada, India, and Australia. They also call for research on inactivation of C. diff spores during waste treatment.
Even better, the authors suggest that vaccines should be developed and employed in both animals and humans. No such vaccine exists in animals, but Pfizer has one for humans in a phase 3 clinical trial, but it does not prevent colonization. Others are in development.
The epidemiology of CDI is an ongoing challenge, with emerging new strains and changing social and environmental conditions. “However, it is with the collaborative efforts of industry partners, policymakers, veterinarians, clinicians, and researchers that CDI needs to be approached, a perfect example of One Health. Opening an interdisciplinary dialogue to address CDI and One Health issues has to be the focus of future studies,” the authors concluded.
SOURCE: SC Lim et al. Clinical Microbiology and Infection. 2020;26:85-863.
Clostridioides difficile (C. diff) infection (CDI) is a pathogen of both humans and animals, and to control it will require an integrated approach that encompasses human health care, veterinary health care, environmental regulation, and public policy. That is the conclusion of a group led by Su-Chen Lim, MD, and Tom Riley, MD, of Edith Cowan University in Australia, who published a review in Clinical Microbiology and Infection.
CDI was generally considered a nuisance infection until the early 21st century, when a hypervirulent fluoroquinolone-resistant strain emerged in North America. The strain is now documented In the United States, Canada, and most countries in Europe.
Another new feature of CDI is increased evidence of community transmission, which was previously rare. This is defined as cases where the patient experienced symptom onset outside the hospital, and had no history of hospitalization in the previous 12 weeks or symptom onset within 48 hours of hospital admission. Community-associated CDI now accounts for 41% of U.S. cases, nearly 30% of Australian cases, and about 14% in Europe, according to recent studies.
Several features of CDI suggest a need for an integrated management plan. The preferred habitat of C. diff is the gastrointestinal track of mammals, and likely colonizes all mammalian neonates. Over time, colonization by other microbes likely crowd it out and prevent overgrowth. But widespread use of antimicrobials in animal production can lead to the creation of an environment resembling that of the neonate, allowing C. diff to expand. That has led to food animals becoming a major C. diff reservoir, and whole-genome studies showed that strains found in humans, food, animals, and the environment are closely related and sometimes genetically indistinguishable, suggesting transmission between humans and animals that may be attributable to contaminated food and environments.
The authors suggest that C. diff infection control should be guided by the One Health initiative, which seeks cooperation between physicians, osteopathic physicians, veterinarians, dentists, nurses, and other scientific and environmental disciplines. The goal is to enhance surveillance and interdisciplinary communication, as well as integrated policies. The authors note that C. diff is often thought of by physicians as primarily a hospital problem, who may be unaware of the increased prevalence of community-acquired disease. It is also a significant problem in agriculture, since as many as 50% of piglets succumb to the disease. Other studies have recently shown that asymptomatic carriers of toxigenic strains are likely to transmit the bacteria to C. diff-negative patients. Asymptomatic carriers cluster with symptomatic patients. In one Cleveland hospital, more than 25% of hospital-associated CDI cases were found to have been colonized prior to admission, suggesting that these were not true hospital-associated cases.
C. diff has been isolated from a wide range of sources, including food animals, meat, seafood, vegetables, household environments, and natural environments like rivers, lakes, and soil. About 20% of calves and 70% of piglets are colonized with C. diff. It has a high prevalence in meat products in the United States, but lower in the Europe, possibly because of different slaughtering practices.
The authors suggest that zoonotic C. diff spread is unlikely to be confined to any geographic region or population, and that widespread C. diff contamination is occurring through food or the environment. This could be occurring because spores can withstand cooking temperatures and disseminate through the air, and even through manure from food animals made into compost or fertilizer.
Veterinary efforts mimicking hospital measures have reduced animal CDI, but there are no rapid diagnostic tests for CDI in animals, making it challenging to control its spread in this context.
The authors call for enhanced antimicrobial stewardship in both human and animal settings, including banning of antimicrobial agents as growth promoters. This has been done in the United States and Europe, but not in Brazil, China, Canada, India, and Australia. They also call for research on inactivation of C. diff spores during waste treatment.
Even better, the authors suggest that vaccines should be developed and employed in both animals and humans. No such vaccine exists in animals, but Pfizer has one for humans in a phase 3 clinical trial, but it does not prevent colonization. Others are in development.
The epidemiology of CDI is an ongoing challenge, with emerging new strains and changing social and environmental conditions. “However, it is with the collaborative efforts of industry partners, policymakers, veterinarians, clinicians, and researchers that CDI needs to be approached, a perfect example of One Health. Opening an interdisciplinary dialogue to address CDI and One Health issues has to be the focus of future studies,” the authors concluded.
SOURCE: SC Lim et al. Clinical Microbiology and Infection. 2020;26:85-863.
Clostridioides difficile (C. diff) infection (CDI) is a pathogen of both humans and animals, and to control it will require an integrated approach that encompasses human health care, veterinary health care, environmental regulation, and public policy. That is the conclusion of a group led by Su-Chen Lim, MD, and Tom Riley, MD, of Edith Cowan University in Australia, who published a review in Clinical Microbiology and Infection.
CDI was generally considered a nuisance infection until the early 21st century, when a hypervirulent fluoroquinolone-resistant strain emerged in North America. The strain is now documented In the United States, Canada, and most countries in Europe.
Another new feature of CDI is increased evidence of community transmission, which was previously rare. This is defined as cases where the patient experienced symptom onset outside the hospital, and had no history of hospitalization in the previous 12 weeks or symptom onset within 48 hours of hospital admission. Community-associated CDI now accounts for 41% of U.S. cases, nearly 30% of Australian cases, and about 14% in Europe, according to recent studies.
Several features of CDI suggest a need for an integrated management plan. The preferred habitat of C. diff is the gastrointestinal track of mammals, and likely colonizes all mammalian neonates. Over time, colonization by other microbes likely crowd it out and prevent overgrowth. But widespread use of antimicrobials in animal production can lead to the creation of an environment resembling that of the neonate, allowing C. diff to expand. That has led to food animals becoming a major C. diff reservoir, and whole-genome studies showed that strains found in humans, food, animals, and the environment are closely related and sometimes genetically indistinguishable, suggesting transmission between humans and animals that may be attributable to contaminated food and environments.
The authors suggest that C. diff infection control should be guided by the One Health initiative, which seeks cooperation between physicians, osteopathic physicians, veterinarians, dentists, nurses, and other scientific and environmental disciplines. The goal is to enhance surveillance and interdisciplinary communication, as well as integrated policies. The authors note that C. diff is often thought of by physicians as primarily a hospital problem, who may be unaware of the increased prevalence of community-acquired disease. It is also a significant problem in agriculture, since as many as 50% of piglets succumb to the disease. Other studies have recently shown that asymptomatic carriers of toxigenic strains are likely to transmit the bacteria to C. diff-negative patients. Asymptomatic carriers cluster with symptomatic patients. In one Cleveland hospital, more than 25% of hospital-associated CDI cases were found to have been colonized prior to admission, suggesting that these were not true hospital-associated cases.
C. diff has been isolated from a wide range of sources, including food animals, meat, seafood, vegetables, household environments, and natural environments like rivers, lakes, and soil. About 20% of calves and 70% of piglets are colonized with C. diff. It has a high prevalence in meat products in the United States, but lower in the Europe, possibly because of different slaughtering practices.
The authors suggest that zoonotic C. diff spread is unlikely to be confined to any geographic region or population, and that widespread C. diff contamination is occurring through food or the environment. This could be occurring because spores can withstand cooking temperatures and disseminate through the air, and even through manure from food animals made into compost or fertilizer.
Veterinary efforts mimicking hospital measures have reduced animal CDI, but there are no rapid diagnostic tests for CDI in animals, making it challenging to control its spread in this context.
The authors call for enhanced antimicrobial stewardship in both human and animal settings, including banning of antimicrobial agents as growth promoters. This has been done in the United States and Europe, but not in Brazil, China, Canada, India, and Australia. They also call for research on inactivation of C. diff spores during waste treatment.
Even better, the authors suggest that vaccines should be developed and employed in both animals and humans. No such vaccine exists in animals, but Pfizer has one for humans in a phase 3 clinical trial, but it does not prevent colonization. Others are in development.
The epidemiology of CDI is an ongoing challenge, with emerging new strains and changing social and environmental conditions. “However, it is with the collaborative efforts of industry partners, policymakers, veterinarians, clinicians, and researchers that CDI needs to be approached, a perfect example of One Health. Opening an interdisciplinary dialogue to address CDI and One Health issues has to be the focus of future studies,” the authors concluded.
SOURCE: SC Lim et al. Clinical Microbiology and Infection. 2020;26:85-863.
FROM CLINICAL MICROBIOLOGY AND INFECTION
Fulminant C. diff debate: Fecal transplants or antibiotics?
Two experts at IDWeek 2020 debated the best treatment for patients with the most severe type of Clostridioides difficile infection – fulminant C. diff. The discussion pitted fecal microbiota transplants (FMT) from the stool of healthy donors against traditional antibiotics.
Fulminant C. diff infection (CDI) represents about 8% of all CDI cases and is often fatal. Patients frequently don’t respond to maximum antibiotic therapy.
Should these patients be treated with FMT before surgery is considered?
“Unequivocally, yes,” said Jessica R. Allegretti, MD, MPH, associate director of the Crohn’s and Colitis Center at Brigham and Women’s Hospital in Boston.
Patients face full colectomy
Fulminant infection, she says, typically requires a total abdominal colectomy with end ileostomy.
“Patients have a quite high perioperative and intraoperative mortality because this is typically an older population with significant comorbidities,” she said.
Often the patients are poor candidates for surgery, she added.
She pointed to the efficacy of FMT in studies such as one published in Gut Microbes in 2017. The study, by Monika Fischer, MD, of Indiana University, Indianapolis, and colleagues showed a 91% cure rate at 1 month in severe patients with an average of 1.5 fecal transplants, noting that was “quite remarkable” in this very sick population.
Though FMT is not approved by the US Food and Drug Administration for fulminant CDI, Dr. Allegretti said, the FDA does allow treatment under “enforcement discretion,” which means no investigational new drug license is needed specifically if treating CDI patients who haven’t responded to standard therapy, as long as proper consent has been obtained.
“This is a patient population that is likely going to die,” she said. “If you were the one in the ICU with fulminant C. diff and you’ve been on maximum therapy for 3-5 days and you’re not getting better, wouldn’t you want somebody to offer you a fecal transplant and give you the chance to recover and leave the hospital with your colon intact? The data suggest that is possible, with a high likelihood and a good safety profile.”
She said the most recent guidelines have supported FMT, and emerging guidelines coming within months “will support this as well.”
Unknowns with FMT
Taking the other side of the debate, Kevin Garey, PharmD, chair of the department of pharmacy practice and translational research at University of Houston College of Pharmacy, warned against trading traditional antibiotics, such as vancomycin and fidaxomicin, for the novelty of FMT.
“With the science of the microbiome and the novelty of fecal microbiota transplantation in expanding use, I think people have somewhat forgotten pharmacotherapy,” he said.
He pointed out safety concerns with FMT reported in June 2019, after which the FDA issued an alert. Two immunocompromised patients who received FMT, both from the same donor, developed invasive infections caused by extended-spectrum beta-lactamase (ESBL)–producing Escherichia coli. One died.
The FDA explained that the donated FMT samples the patients received were not tested for ESBL-producing gram-negative organisms before use.
Dr. Allegretti agreed antibiotics play a role in treatment with FMT, but she argued that the safety profile of FMT remains strong and that the safety issues came from isolated incidents at a single center.
Dr. Garey countered that there are just too many unknowns with FMT.
“We will never know what the next superbug that’s going to land in an FMT is until we’ve identified that superbug in somebody – the next Candida auris, the next CRE [carbapenem-resistant Enterobacteriaceae], the next thing that’s going to show up in FMT – until we get rid of the ‘F,’ “ Dr. Garey said.
“[Until] we get microbial therapy that’s generated without the need for healthy donors, I think we’re always going to be in this problem.”
He said although FMT “has an amazing ability to alter a microbiome” it “pales in comparison” to vancomycin’s ability to do so.
Disruption of the microbiome is, without a doubt, a hallmark of C. diff, but we don’t have to run to FMT,” Dr. Garey said. “We can think about prophylaxis strategies, we can think about new drug development that spares the microbiota. The need for FMT might be a consequence of poor pharmacotherapy management, not a part of pharmacotherapy management.”
Moderator Sam Aitken, PharmD, MPH, a clinical pharmacy specialist in infectious disease at MD Anderson Cancer Center in Houston, said in an interview the speakers found some common ground.
“I think there was a general consensus between both Dr. Allegretti and Dr. Garey that both traditional therapeutics and fecal microbiota transplantation have a role to play in these patients, although there is still quite a bit of discussion around where those might be best positioned,” Dr. Aitken said.
He added, “There’s also a general consensus that there is not likely to be one right answer for all patients with multiple recurrent CDI.”
Dr. Allegretti, Dr. Garey, and Dr. Aitken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two experts at IDWeek 2020 debated the best treatment for patients with the most severe type of Clostridioides difficile infection – fulminant C. diff. The discussion pitted fecal microbiota transplants (FMT) from the stool of healthy donors against traditional antibiotics.
Fulminant C. diff infection (CDI) represents about 8% of all CDI cases and is often fatal. Patients frequently don’t respond to maximum antibiotic therapy.
Should these patients be treated with FMT before surgery is considered?
“Unequivocally, yes,” said Jessica R. Allegretti, MD, MPH, associate director of the Crohn’s and Colitis Center at Brigham and Women’s Hospital in Boston.
Patients face full colectomy
Fulminant infection, she says, typically requires a total abdominal colectomy with end ileostomy.
“Patients have a quite high perioperative and intraoperative mortality because this is typically an older population with significant comorbidities,” she said.
Often the patients are poor candidates for surgery, she added.
She pointed to the efficacy of FMT in studies such as one published in Gut Microbes in 2017. The study, by Monika Fischer, MD, of Indiana University, Indianapolis, and colleagues showed a 91% cure rate at 1 month in severe patients with an average of 1.5 fecal transplants, noting that was “quite remarkable” in this very sick population.
Though FMT is not approved by the US Food and Drug Administration for fulminant CDI, Dr. Allegretti said, the FDA does allow treatment under “enforcement discretion,” which means no investigational new drug license is needed specifically if treating CDI patients who haven’t responded to standard therapy, as long as proper consent has been obtained.
“This is a patient population that is likely going to die,” she said. “If you were the one in the ICU with fulminant C. diff and you’ve been on maximum therapy for 3-5 days and you’re not getting better, wouldn’t you want somebody to offer you a fecal transplant and give you the chance to recover and leave the hospital with your colon intact? The data suggest that is possible, with a high likelihood and a good safety profile.”
She said the most recent guidelines have supported FMT, and emerging guidelines coming within months “will support this as well.”
Unknowns with FMT
Taking the other side of the debate, Kevin Garey, PharmD, chair of the department of pharmacy practice and translational research at University of Houston College of Pharmacy, warned against trading traditional antibiotics, such as vancomycin and fidaxomicin, for the novelty of FMT.
“With the science of the microbiome and the novelty of fecal microbiota transplantation in expanding use, I think people have somewhat forgotten pharmacotherapy,” he said.
He pointed out safety concerns with FMT reported in June 2019, after which the FDA issued an alert. Two immunocompromised patients who received FMT, both from the same donor, developed invasive infections caused by extended-spectrum beta-lactamase (ESBL)–producing Escherichia coli. One died.
The FDA explained that the donated FMT samples the patients received were not tested for ESBL-producing gram-negative organisms before use.
Dr. Allegretti agreed antibiotics play a role in treatment with FMT, but she argued that the safety profile of FMT remains strong and that the safety issues came from isolated incidents at a single center.
Dr. Garey countered that there are just too many unknowns with FMT.
“We will never know what the next superbug that’s going to land in an FMT is until we’ve identified that superbug in somebody – the next Candida auris, the next CRE [carbapenem-resistant Enterobacteriaceae], the next thing that’s going to show up in FMT – until we get rid of the ‘F,’ “ Dr. Garey said.
“[Until] we get microbial therapy that’s generated without the need for healthy donors, I think we’re always going to be in this problem.”
He said although FMT “has an amazing ability to alter a microbiome” it “pales in comparison” to vancomycin’s ability to do so.
Disruption of the microbiome is, without a doubt, a hallmark of C. diff, but we don’t have to run to FMT,” Dr. Garey said. “We can think about prophylaxis strategies, we can think about new drug development that spares the microbiota. The need for FMT might be a consequence of poor pharmacotherapy management, not a part of pharmacotherapy management.”
Moderator Sam Aitken, PharmD, MPH, a clinical pharmacy specialist in infectious disease at MD Anderson Cancer Center in Houston, said in an interview the speakers found some common ground.
“I think there was a general consensus between both Dr. Allegretti and Dr. Garey that both traditional therapeutics and fecal microbiota transplantation have a role to play in these patients, although there is still quite a bit of discussion around where those might be best positioned,” Dr. Aitken said.
He added, “There’s also a general consensus that there is not likely to be one right answer for all patients with multiple recurrent CDI.”
Dr. Allegretti, Dr. Garey, and Dr. Aitken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two experts at IDWeek 2020 debated the best treatment for patients with the most severe type of Clostridioides difficile infection – fulminant C. diff. The discussion pitted fecal microbiota transplants (FMT) from the stool of healthy donors against traditional antibiotics.
Fulminant C. diff infection (CDI) represents about 8% of all CDI cases and is often fatal. Patients frequently don’t respond to maximum antibiotic therapy.
Should these patients be treated with FMT before surgery is considered?
“Unequivocally, yes,” said Jessica R. Allegretti, MD, MPH, associate director of the Crohn’s and Colitis Center at Brigham and Women’s Hospital in Boston.
Patients face full colectomy
Fulminant infection, she says, typically requires a total abdominal colectomy with end ileostomy.
“Patients have a quite high perioperative and intraoperative mortality because this is typically an older population with significant comorbidities,” she said.
Often the patients are poor candidates for surgery, she added.
She pointed to the efficacy of FMT in studies such as one published in Gut Microbes in 2017. The study, by Monika Fischer, MD, of Indiana University, Indianapolis, and colleagues showed a 91% cure rate at 1 month in severe patients with an average of 1.5 fecal transplants, noting that was “quite remarkable” in this very sick population.
Though FMT is not approved by the US Food and Drug Administration for fulminant CDI, Dr. Allegretti said, the FDA does allow treatment under “enforcement discretion,” which means no investigational new drug license is needed specifically if treating CDI patients who haven’t responded to standard therapy, as long as proper consent has been obtained.
“This is a patient population that is likely going to die,” she said. “If you were the one in the ICU with fulminant C. diff and you’ve been on maximum therapy for 3-5 days and you’re not getting better, wouldn’t you want somebody to offer you a fecal transplant and give you the chance to recover and leave the hospital with your colon intact? The data suggest that is possible, with a high likelihood and a good safety profile.”
She said the most recent guidelines have supported FMT, and emerging guidelines coming within months “will support this as well.”
Unknowns with FMT
Taking the other side of the debate, Kevin Garey, PharmD, chair of the department of pharmacy practice and translational research at University of Houston College of Pharmacy, warned against trading traditional antibiotics, such as vancomycin and fidaxomicin, for the novelty of FMT.
“With the science of the microbiome and the novelty of fecal microbiota transplantation in expanding use, I think people have somewhat forgotten pharmacotherapy,” he said.
He pointed out safety concerns with FMT reported in June 2019, after which the FDA issued an alert. Two immunocompromised patients who received FMT, both from the same donor, developed invasive infections caused by extended-spectrum beta-lactamase (ESBL)–producing Escherichia coli. One died.
The FDA explained that the donated FMT samples the patients received were not tested for ESBL-producing gram-negative organisms before use.
Dr. Allegretti agreed antibiotics play a role in treatment with FMT, but she argued that the safety profile of FMT remains strong and that the safety issues came from isolated incidents at a single center.
Dr. Garey countered that there are just too many unknowns with FMT.
“We will never know what the next superbug that’s going to land in an FMT is until we’ve identified that superbug in somebody – the next Candida auris, the next CRE [carbapenem-resistant Enterobacteriaceae], the next thing that’s going to show up in FMT – until we get rid of the ‘F,’ “ Dr. Garey said.
“[Until] we get microbial therapy that’s generated without the need for healthy donors, I think we’re always going to be in this problem.”
He said although FMT “has an amazing ability to alter a microbiome” it “pales in comparison” to vancomycin’s ability to do so.
Disruption of the microbiome is, without a doubt, a hallmark of C. diff, but we don’t have to run to FMT,” Dr. Garey said. “We can think about prophylaxis strategies, we can think about new drug development that spares the microbiota. The need for FMT might be a consequence of poor pharmacotherapy management, not a part of pharmacotherapy management.”
Moderator Sam Aitken, PharmD, MPH, a clinical pharmacy specialist in infectious disease at MD Anderson Cancer Center in Houston, said in an interview the speakers found some common ground.
“I think there was a general consensus between both Dr. Allegretti and Dr. Garey that both traditional therapeutics and fecal microbiota transplantation have a role to play in these patients, although there is still quite a bit of discussion around where those might be best positioned,” Dr. Aitken said.
He added, “There’s also a general consensus that there is not likely to be one right answer for all patients with multiple recurrent CDI.”
Dr. Allegretti, Dr. Garey, and Dr. Aitken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FDA warns of serious infection risk after FMT
The Food and Drug Administration has issued a Safety Alert warning of the potential risk of serious, life-threatening infection in patients who receive fecal microbiota transplant for Clostridioides difficile infection.
The FDA has received six reports of infection associated with fecal microbiota transplant from a stool bank company based in the United States: Two patients had enteropathogenic Escherichia coli (EPEC) infection, and four had shiga toxin–producing E. coli (STEC). The two EPEC infections came from two separate donors, but the four STEC infections came from a single donor, according to the FDA.
In addition, two patients died after receiving fecal microbiota transplant from the donor associated with the STEC infections. These patients died before any of the STEC infections were reported to the FDA; as their stool was not tested for STEC, it is unclear whether it contributed to their deaths.
The use of fecal microbiota transplant is still investigational, and as such, patients should be made aware by health care providers of the risks, which include the potential for transmission of pathogenic bacteria and the resultant adverse events, the FDA said in the press release.
The Food and Drug Administration has issued a Safety Alert warning of the potential risk of serious, life-threatening infection in patients who receive fecal microbiota transplant for Clostridioides difficile infection.
The FDA has received six reports of infection associated with fecal microbiota transplant from a stool bank company based in the United States: Two patients had enteropathogenic Escherichia coli (EPEC) infection, and four had shiga toxin–producing E. coli (STEC). The two EPEC infections came from two separate donors, but the four STEC infections came from a single donor, according to the FDA.
In addition, two patients died after receiving fecal microbiota transplant from the donor associated with the STEC infections. These patients died before any of the STEC infections were reported to the FDA; as their stool was not tested for STEC, it is unclear whether it contributed to their deaths.
The use of fecal microbiota transplant is still investigational, and as such, patients should be made aware by health care providers of the risks, which include the potential for transmission of pathogenic bacteria and the resultant adverse events, the FDA said in the press release.
The Food and Drug Administration has issued a Safety Alert warning of the potential risk of serious, life-threatening infection in patients who receive fecal microbiota transplant for Clostridioides difficile infection.
The FDA has received six reports of infection associated with fecal microbiota transplant from a stool bank company based in the United States: Two patients had enteropathogenic Escherichia coli (EPEC) infection, and four had shiga toxin–producing E. coli (STEC). The two EPEC infections came from two separate donors, but the four STEC infections came from a single donor, according to the FDA.
In addition, two patients died after receiving fecal microbiota transplant from the donor associated with the STEC infections. These patients died before any of the STEC infections were reported to the FDA; as their stool was not tested for STEC, it is unclear whether it contributed to their deaths.
The use of fecal microbiota transplant is still investigational, and as such, patients should be made aware by health care providers of the risks, which include the potential for transmission of pathogenic bacteria and the resultant adverse events, the FDA said in the press release.
FDA clears first fully disposable duodenoscope
The Food and Drug Administration on Dec. 13 cleared Boston Scientific’s single-use duodenoscope, the Exalt Model D, for endoscopic retrograde cholangiopancreatography.
It’s the first disposable duodenoscope to hit the market in the wake of the agency’s August call for manufacturers and health care facilities to move to partially or fully disposable duodenoscopes. The goal is to eliminate the risk of spreading infections between patients from incomplete sterilization of traditional, multi-use scopes. The FDA also recently approved a Pentax duodenoscope with a disposable elevator, the most difficult part to clean.
The agency reported in April that 5.4% of samples from multi-use scopes test postive for Escherichia coli, Pseudomonas aeruginosa, or other “high-concern” organisms.
Boston Scientific spokesperson Kate Haranis said the Exalt Model D will be available in the first quarter of 2020, but the company is still working out how much it will charge.
Cost effectiveness will depend largely on the degree to which the price of the device is offset by the infections it prevents. It might prove particularly attractive to high-volume centers with higher than usual infection rates. It might also be of interest to smaller practices where the price of a multi-use scope doesn’t make sense for only a few procedures a year, said Gyanprakash Ketwaroo, MD, an interventional endoscopist and assistant professor of gastroenterology at Baylor University, Houston.
“The feel is a little different,” said Dr. Ketwaroo, who’s tried the new device, but “it’s pretty functional and probably okay to use in almost all endoscopic procedures that require ERCP.”
In a study funded by Boston Scientific, endoscopists reported a median overall satisfaction score of 9 out of 10 with the new scope (Clin Gastroenterol Hepatol. 2019 Nov 6. doi: 10.1016/j.cgh.2019.10.052).
As for using it at Baylor, Dr. Ketwaroo said, “we’re not sure yet; we are still evaluating it” and want to see if any problems emerge once it’s on the market. It’s also not clear if infection risks would be lower than with the disposable elevator model from Pentax, he added.
The Exalt Model D was granted breakthrough status by the FDA, and the agency worked closely with Boston Scientific to bring it to market.
“The availability of a fully disposable duodenoscope represents another major step forward for improving the safety of these devices, which are used in more than 500,000 procedures in the United States each year. The FDA continues to encourage innovative ways to improve the safety and effectiveness of these devices,” Jeff Shuren, MD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
Dr. Ketwaroo had no relevant financial disclosures.
The Food and Drug Administration on Dec. 13 cleared Boston Scientific’s single-use duodenoscope, the Exalt Model D, for endoscopic retrograde cholangiopancreatography.
It’s the first disposable duodenoscope to hit the market in the wake of the agency’s August call for manufacturers and health care facilities to move to partially or fully disposable duodenoscopes. The goal is to eliminate the risk of spreading infections between patients from incomplete sterilization of traditional, multi-use scopes. The FDA also recently approved a Pentax duodenoscope with a disposable elevator, the most difficult part to clean.
The agency reported in April that 5.4% of samples from multi-use scopes test postive for Escherichia coli, Pseudomonas aeruginosa, or other “high-concern” organisms.
Boston Scientific spokesperson Kate Haranis said the Exalt Model D will be available in the first quarter of 2020, but the company is still working out how much it will charge.
Cost effectiveness will depend largely on the degree to which the price of the device is offset by the infections it prevents. It might prove particularly attractive to high-volume centers with higher than usual infection rates. It might also be of interest to smaller practices where the price of a multi-use scope doesn’t make sense for only a few procedures a year, said Gyanprakash Ketwaroo, MD, an interventional endoscopist and assistant professor of gastroenterology at Baylor University, Houston.
“The feel is a little different,” said Dr. Ketwaroo, who’s tried the new device, but “it’s pretty functional and probably okay to use in almost all endoscopic procedures that require ERCP.”
In a study funded by Boston Scientific, endoscopists reported a median overall satisfaction score of 9 out of 10 with the new scope (Clin Gastroenterol Hepatol. 2019 Nov 6. doi: 10.1016/j.cgh.2019.10.052).
As for using it at Baylor, Dr. Ketwaroo said, “we’re not sure yet; we are still evaluating it” and want to see if any problems emerge once it’s on the market. It’s also not clear if infection risks would be lower than with the disposable elevator model from Pentax, he added.
The Exalt Model D was granted breakthrough status by the FDA, and the agency worked closely with Boston Scientific to bring it to market.
“The availability of a fully disposable duodenoscope represents another major step forward for improving the safety of these devices, which are used in more than 500,000 procedures in the United States each year. The FDA continues to encourage innovative ways to improve the safety and effectiveness of these devices,” Jeff Shuren, MD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
Dr. Ketwaroo had no relevant financial disclosures.
The Food and Drug Administration on Dec. 13 cleared Boston Scientific’s single-use duodenoscope, the Exalt Model D, for endoscopic retrograde cholangiopancreatography.
It’s the first disposable duodenoscope to hit the market in the wake of the agency’s August call for manufacturers and health care facilities to move to partially or fully disposable duodenoscopes. The goal is to eliminate the risk of spreading infections between patients from incomplete sterilization of traditional, multi-use scopes. The FDA also recently approved a Pentax duodenoscope with a disposable elevator, the most difficult part to clean.
The agency reported in April that 5.4% of samples from multi-use scopes test postive for Escherichia coli, Pseudomonas aeruginosa, or other “high-concern” organisms.
Boston Scientific spokesperson Kate Haranis said the Exalt Model D will be available in the first quarter of 2020, but the company is still working out how much it will charge.
Cost effectiveness will depend largely on the degree to which the price of the device is offset by the infections it prevents. It might prove particularly attractive to high-volume centers with higher than usual infection rates. It might also be of interest to smaller practices where the price of a multi-use scope doesn’t make sense for only a few procedures a year, said Gyanprakash Ketwaroo, MD, an interventional endoscopist and assistant professor of gastroenterology at Baylor University, Houston.
“The feel is a little different,” said Dr. Ketwaroo, who’s tried the new device, but “it’s pretty functional and probably okay to use in almost all endoscopic procedures that require ERCP.”
In a study funded by Boston Scientific, endoscopists reported a median overall satisfaction score of 9 out of 10 with the new scope (Clin Gastroenterol Hepatol. 2019 Nov 6. doi: 10.1016/j.cgh.2019.10.052).
As for using it at Baylor, Dr. Ketwaroo said, “we’re not sure yet; we are still evaluating it” and want to see if any problems emerge once it’s on the market. It’s also not clear if infection risks would be lower than with the disposable elevator model from Pentax, he added.
The Exalt Model D was granted breakthrough status by the FDA, and the agency worked closely with Boston Scientific to bring it to market.
“The availability of a fully disposable duodenoscope represents another major step forward for improving the safety of these devices, which are used in more than 500,000 procedures in the United States each year. The FDA continues to encourage innovative ways to improve the safety and effectiveness of these devices,” Jeff Shuren, MD, director of the FDA’s Center for Devices and Radiological Health, said in a statement.
Dr. Ketwaroo had no relevant financial disclosures.
FROM THE FDA
Perioperative antirheumatic drug use does not impact postsurgery infection rate in RA patients
ATLANTA – Patients with rheumatoid arthritis were more at risk of postoperative infection because of a high Charlson Comorbidity Index or longer surgery time than because of perioperative use of antirheumatic medications, according to a presentation at the annual meeting of the American College of Rheumatology.
Anna Shmagel, MD, of the University of Minnesota in Minneapolis and colleagues performed a retrospective cohort study of 154 patients with seropositive RA who were in the Fairview Health System between Jan. 2010 and Dec. 2017 and underwent either orthopedic or major organ surgery. The patients were classified based on their use of disease-modifying antirheumatic drugs (DMARDs) and biologics alone or in combination, with patients divided into “no DMARD or biologic,” “DMARD but no biologic” and “biologic with or without DMARD” groups.
The question of whether to discontinue antirheumatic medications before surgery is still controversial, with conflicting evidence across studies, Dr. Shmagel said in her presentation. A study by Giles and colleagues found 10 of 91 patients (11%) RA who underwent an orthopedic surgical procedure developed a postoperative infection, with patients receiving tumor necrosis factor (TNF) inhibitors more likely to develop an infection, compared with patients who were not receiving TNF inhibitors (Arthritis Care Res. 2006. doi: 10.1002/art.21841).
However, other studies have challenged that idea, and a 2018 study from Goodman and colleagues raised the issue of whether patients stopping biologics prior to surgery are at increased risk of flares. Of 120 RA patients in their study who underwent total hip or total knee arthroplasty, 75% of patients flared at 6 weeks after surgery. While patients who halted biologics before surgery were more likely to flare, stopping biologics did not predict flaring after surgery (J Rheumatol. 2018. doi: 10.3899/jrheum.170366).
“It’s not entirely clear whether these theories are related to what we do with antirheumatic medications, but we felt that it was pertinent to further study this question.” Dr. Shmagel said.
Dr. Shmagel and colleagues examined the 30-day infection rate of RA patients postoperatively, with 30-day readmission and 30-day mortality rates as secondary outcomes. Patient-associated factors such as age, gender, race, body mass index, smoking status, Charlson Comorbidity Index, income, and use of corticosteroids were analyzed as covariates in addition to factors involving surgery such as expected surgery time, perioperative antibiotic use, and whether the procedure was elective or emergency surgery.
A majority of the patients in the study across all groups were white women about 63 years old with a body mass index above 30 kg/m2 and almost all undergoing electing surgery compared with emergency surgery. While patients in each group were similar with regard to Charlson Comorbidity Index, expected length of surgery, and percentage of patients undergoing elective surgery, patients in the biologic with or without DMARD group had a significantly lower median income level compared with those in the other two groups (P = .01).
Overall, there were 244 surgeries in 154 patients, with 117 surgeries in the group not receiving biologics or DMARDs, 95 surgeries in the group receiving DMARDs but no biologics, and 32 surgeries in the biologics with or without DMARD group. In the DMARD but no biologics group, most patients were receiving methotrexate (45%) or hydroxychloroquine (44%), while the most common biologics in the biologics with or without DMARD group were infliximab (25%), tocilizumab (19%), abatacept (16%), etanercept (13%), rituximab (9%), and tofacitinib (9%).
There was an 11% overall rate of infection, with a similar rate of infection across all groups (P = .09). While there was a higher rate of surgical site infections among patients in the biologics with or without DMARD group (9%) and a higher percentage of urinary tract infections in the no DMARD and no biologics group (4%), the results were not statistically significant. When the rate of infections was examined by type of surgery, there were no significant differences between infections from musculoskeletal surgery (P = .7) and major organ surgery (P = .8).
The overall 30-day readmission rate was 12%, but there were no statistically significant differences between groups. Although there were five deaths in the study, four deaths were in the group not receiving DMARDs or biologics, and one death was in the biologic with or without DMARD group.
Higher Charlson Comorbidity Index did predict infection risk, with an odds ratio of 1.37 per 1-point increase in the index (95% confidence interval, 1.10-1.70). Length of surgery also increased the risk of infection, with an OR of 1.16 per 15-minute increase in surgery time (95% CI, 1.09-1.23).
Dr. Shmagel noted that the retrospective nature of the study and the midwestern cohort may mean the results are not generalizable to other populations and that larger randomized trials should be considered. “Certainly, a larger study with more events would be needed,” she said.
This study was funded by the University of Minnesota. Dr. Shmagel reported no relevant conflicts of interest.
SOURCE: Kerski M et al. Arthritis Rheumatol. 2019;71 (suppl 10), Abstract 1805.
ATLANTA – Patients with rheumatoid arthritis were more at risk of postoperative infection because of a high Charlson Comorbidity Index or longer surgery time than because of perioperative use of antirheumatic medications, according to a presentation at the annual meeting of the American College of Rheumatology.
Anna Shmagel, MD, of the University of Minnesota in Minneapolis and colleagues performed a retrospective cohort study of 154 patients with seropositive RA who were in the Fairview Health System between Jan. 2010 and Dec. 2017 and underwent either orthopedic or major organ surgery. The patients were classified based on their use of disease-modifying antirheumatic drugs (DMARDs) and biologics alone or in combination, with patients divided into “no DMARD or biologic,” “DMARD but no biologic” and “biologic with or without DMARD” groups.
The question of whether to discontinue antirheumatic medications before surgery is still controversial, with conflicting evidence across studies, Dr. Shmagel said in her presentation. A study by Giles and colleagues found 10 of 91 patients (11%) RA who underwent an orthopedic surgical procedure developed a postoperative infection, with patients receiving tumor necrosis factor (TNF) inhibitors more likely to develop an infection, compared with patients who were not receiving TNF inhibitors (Arthritis Care Res. 2006. doi: 10.1002/art.21841).
However, other studies have challenged that idea, and a 2018 study from Goodman and colleagues raised the issue of whether patients stopping biologics prior to surgery are at increased risk of flares. Of 120 RA patients in their study who underwent total hip or total knee arthroplasty, 75% of patients flared at 6 weeks after surgery. While patients who halted biologics before surgery were more likely to flare, stopping biologics did not predict flaring after surgery (J Rheumatol. 2018. doi: 10.3899/jrheum.170366).
“It’s not entirely clear whether these theories are related to what we do with antirheumatic medications, but we felt that it was pertinent to further study this question.” Dr. Shmagel said.
Dr. Shmagel and colleagues examined the 30-day infection rate of RA patients postoperatively, with 30-day readmission and 30-day mortality rates as secondary outcomes. Patient-associated factors such as age, gender, race, body mass index, smoking status, Charlson Comorbidity Index, income, and use of corticosteroids were analyzed as covariates in addition to factors involving surgery such as expected surgery time, perioperative antibiotic use, and whether the procedure was elective or emergency surgery.
A majority of the patients in the study across all groups were white women about 63 years old with a body mass index above 30 kg/m2 and almost all undergoing electing surgery compared with emergency surgery. While patients in each group were similar with regard to Charlson Comorbidity Index, expected length of surgery, and percentage of patients undergoing elective surgery, patients in the biologic with or without DMARD group had a significantly lower median income level compared with those in the other two groups (P = .01).
Overall, there were 244 surgeries in 154 patients, with 117 surgeries in the group not receiving biologics or DMARDs, 95 surgeries in the group receiving DMARDs but no biologics, and 32 surgeries in the biologics with or without DMARD group. In the DMARD but no biologics group, most patients were receiving methotrexate (45%) or hydroxychloroquine (44%), while the most common biologics in the biologics with or without DMARD group were infliximab (25%), tocilizumab (19%), abatacept (16%), etanercept (13%), rituximab (9%), and tofacitinib (9%).
There was an 11% overall rate of infection, with a similar rate of infection across all groups (P = .09). While there was a higher rate of surgical site infections among patients in the biologics with or without DMARD group (9%) and a higher percentage of urinary tract infections in the no DMARD and no biologics group (4%), the results were not statistically significant. When the rate of infections was examined by type of surgery, there were no significant differences between infections from musculoskeletal surgery (P = .7) and major organ surgery (P = .8).
The overall 30-day readmission rate was 12%, but there were no statistically significant differences between groups. Although there were five deaths in the study, four deaths were in the group not receiving DMARDs or biologics, and one death was in the biologic with or without DMARD group.
Higher Charlson Comorbidity Index did predict infection risk, with an odds ratio of 1.37 per 1-point increase in the index (95% confidence interval, 1.10-1.70). Length of surgery also increased the risk of infection, with an OR of 1.16 per 15-minute increase in surgery time (95% CI, 1.09-1.23).
Dr. Shmagel noted that the retrospective nature of the study and the midwestern cohort may mean the results are not generalizable to other populations and that larger randomized trials should be considered. “Certainly, a larger study with more events would be needed,” she said.
This study was funded by the University of Minnesota. Dr. Shmagel reported no relevant conflicts of interest.
SOURCE: Kerski M et al. Arthritis Rheumatol. 2019;71 (suppl 10), Abstract 1805.
ATLANTA – Patients with rheumatoid arthritis were more at risk of postoperative infection because of a high Charlson Comorbidity Index or longer surgery time than because of perioperative use of antirheumatic medications, according to a presentation at the annual meeting of the American College of Rheumatology.
Anna Shmagel, MD, of the University of Minnesota in Minneapolis and colleagues performed a retrospective cohort study of 154 patients with seropositive RA who were in the Fairview Health System between Jan. 2010 and Dec. 2017 and underwent either orthopedic or major organ surgery. The patients were classified based on their use of disease-modifying antirheumatic drugs (DMARDs) and biologics alone or in combination, with patients divided into “no DMARD or biologic,” “DMARD but no biologic” and “biologic with or without DMARD” groups.
The question of whether to discontinue antirheumatic medications before surgery is still controversial, with conflicting evidence across studies, Dr. Shmagel said in her presentation. A study by Giles and colleagues found 10 of 91 patients (11%) RA who underwent an orthopedic surgical procedure developed a postoperative infection, with patients receiving tumor necrosis factor (TNF) inhibitors more likely to develop an infection, compared with patients who were not receiving TNF inhibitors (Arthritis Care Res. 2006. doi: 10.1002/art.21841).
However, other studies have challenged that idea, and a 2018 study from Goodman and colleagues raised the issue of whether patients stopping biologics prior to surgery are at increased risk of flares. Of 120 RA patients in their study who underwent total hip or total knee arthroplasty, 75% of patients flared at 6 weeks after surgery. While patients who halted biologics before surgery were more likely to flare, stopping biologics did not predict flaring after surgery (J Rheumatol. 2018. doi: 10.3899/jrheum.170366).
“It’s not entirely clear whether these theories are related to what we do with antirheumatic medications, but we felt that it was pertinent to further study this question.” Dr. Shmagel said.
Dr. Shmagel and colleagues examined the 30-day infection rate of RA patients postoperatively, with 30-day readmission and 30-day mortality rates as secondary outcomes. Patient-associated factors such as age, gender, race, body mass index, smoking status, Charlson Comorbidity Index, income, and use of corticosteroids were analyzed as covariates in addition to factors involving surgery such as expected surgery time, perioperative antibiotic use, and whether the procedure was elective or emergency surgery.
A majority of the patients in the study across all groups were white women about 63 years old with a body mass index above 30 kg/m2 and almost all undergoing electing surgery compared with emergency surgery. While patients in each group were similar with regard to Charlson Comorbidity Index, expected length of surgery, and percentage of patients undergoing elective surgery, patients in the biologic with or without DMARD group had a significantly lower median income level compared with those in the other two groups (P = .01).
Overall, there were 244 surgeries in 154 patients, with 117 surgeries in the group not receiving biologics or DMARDs, 95 surgeries in the group receiving DMARDs but no biologics, and 32 surgeries in the biologics with or without DMARD group. In the DMARD but no biologics group, most patients were receiving methotrexate (45%) or hydroxychloroquine (44%), while the most common biologics in the biologics with or without DMARD group were infliximab (25%), tocilizumab (19%), abatacept (16%), etanercept (13%), rituximab (9%), and tofacitinib (9%).
There was an 11% overall rate of infection, with a similar rate of infection across all groups (P = .09). While there was a higher rate of surgical site infections among patients in the biologics with or without DMARD group (9%) and a higher percentage of urinary tract infections in the no DMARD and no biologics group (4%), the results were not statistically significant. When the rate of infections was examined by type of surgery, there were no significant differences between infections from musculoskeletal surgery (P = .7) and major organ surgery (P = .8).
The overall 30-day readmission rate was 12%, but there were no statistically significant differences between groups. Although there were five deaths in the study, four deaths were in the group not receiving DMARDs or biologics, and one death was in the biologic with or without DMARD group.
Higher Charlson Comorbidity Index did predict infection risk, with an odds ratio of 1.37 per 1-point increase in the index (95% confidence interval, 1.10-1.70). Length of surgery also increased the risk of infection, with an OR of 1.16 per 15-minute increase in surgery time (95% CI, 1.09-1.23).
Dr. Shmagel noted that the retrospective nature of the study and the midwestern cohort may mean the results are not generalizable to other populations and that larger randomized trials should be considered. “Certainly, a larger study with more events would be needed,” she said.
This study was funded by the University of Minnesota. Dr. Shmagel reported no relevant conflicts of interest.
SOURCE: Kerski M et al. Arthritis Rheumatol. 2019;71 (suppl 10), Abstract 1805.
REPORTING FROM ACR 2019