User login
Fewer transplants for MM with quadruplet therapy?
“It is not a big leap of faith to imagine that, in the near future, with the availability of quadruplets and T-cell therapies, the role of high-dose melphalan and autologous stem cell transplant will be diminished,” said Dickran Kazandjian, MD, and Ola Landgren, MD, PhD, of the myeloma division, Sylvester Comprehensive Cancer Center, University of Miami.
They commented in a editorial in JAMA Oncology, prompted by a paper describing new results with a novel quadruple combination of therapies. These treatments included the monoclonal antibody elotuzumab (Empliciti) added onto the established backbone of carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (known as KRd).
“Regardless of what the future holds for elotuzumab-based combinations, it is clear that the new treatment paradigm of newly diagnosed MM will incorporate antibody-based quadruplet regimens,” the editorialists commented.
“Novel immunotherapies are here to stay,” they added, “as they are already transforming the lives of patients with multiple MM and bringing a bright horizon to the treatment landscape.”
Study details
The trial of the novel quadruplet regimen was a multicenter, single-arm, phase 2 study that involved 46 patients with newly diagnosed multiple myeloma, explain first author Benjamin A. Derman, MD, of the University of Chicago Medical Center, and colleagues.
These patients had a median age of 62; more than two-thirds were male (72%) and White (70%). About half (48%) had high-risk cytogenetic abnormalities.
All patients were treated with 12 cycles of the quadruple therapy Elo-KRd regimen. They underwent bone marrow assessment of measurable residual disease (MRD; with 10-5 sensitivity) after cycle 8 and cycle 12.
“An MRD-adapted treatment approach is rational because it may identify which patients can be administered shorter courses of intensive therapy without compromising efficacy,” the authors explained.
Patients who had MRD negativity at both time points did not receive further Elo-KRd, while patients who converted from MRD positivity to negativity in between cycles 8 and 12 received 6 additional cycles of Elo-KRd. Those who remained MRD positive or converted to positivity after 12 cycles received an additional 12 cycles of Elo-KRd.
Following Elo-KRd treatment, all patients transitioned to triple therapy with Elo-Rd (with no carfilzomib), for indefinite maintenance therapy or until disease progression.
For the primary endpoint, the rate of stringent complete response and/or MRD-negativity after cycle 8 was 58% (26 of 45), meeting the predefined definition of efficacy.
Importantly, 26% of patients converted from MRD positivity after cycle 8 to negativity at a later time point, while 50% of patients reached 1-year sustained MRD negativity.
Overall, the estimated 3-year, progression-free survival was 72%, and the rate was 92% for patients with MRD-negativity at cycle 8. The overall survival rate was 78%.
The most common grade 3 or 4 adverse events were lung and nonpulmonary infections (13% and 11%, respectively), and one patient had a grade 5 MI. Three patients discontinued the treatment because of intolerance.
“An MRD-adapted design using elotuzumab and weekly KRd without autologous stem cell transplantation showed a high rate of stringent complete response (sCR) and/or MRD-negativity and durable responses,” the authors wrote.
“This approach provides support for further evaluation of MRD-guided de-escalation of therapy to decrease treatment exposure while sustaining deep responses.”
To better assess the difference of the therapy versus treatment including stem cell transplantation, a phase 3, randomized trial is currently underway to compare the Elo-KRd regimen against KRd with autologous stem cell transplant in newly diagnosed MM.
“If Elo-KRd proves superior, a randomized comparison of Elo versus anti-CD38 mAb-based quadruplets would help determine the optimal combination of therapies in the frontline setting,” the authors noted.
Randomized trial anticipated to clarify benefit
In their editorial, Dr. Kazandjian and Dr. Landgren agreed with the authors that the role of elotuzumab needs to be better clarified in a randomized trial setting.
Elotuzumab received FDA approval in 2015 based on results from the ELOQUENT-2 study, which showed improved progression-free survival and overall survival with the addition of elotuzumab to lenalidomide and dexamethasone in patients with multiple myeloma who have previously received one to three other therapies.
However, the editorialists pointed out that recently published results from the randomized ELOQUENT-1 trial of lenalidomide and dexamethasone with and without elotuzumab showed the addition of elotuzumab was not associated with a statistically significant difference in progression-free survival.
The editorialists also pointed out that, in the setting of newly diagnosed multiple myeloma, another recent, similarly designed study found that the backbone regimen of carfilzomib, lenalidomide, and dexamethasone – on its own – was also associated with a favorable MRD-negative rate of 62%.
In addition, several studies involving novel quadruple treatments with the monoclonal antibody daratumumab (Darzalex) instead of elotuzumab, have also shown benefit in newly diagnosed multiple myeloma, resulting in high rates of MRD negativity.
Collectively, the findings bode well for the quadruple regimens in the treatment of MM, the editorialists emphasized.
“Importantly, with the rate of deep remissions observed with antibody-based quadruplet therapies, one may question the role of using early high-dose melphalan and autologous stem cell transplant in every patient, especially in those who have achieved MRD negativity with the quadruplet alone,” they added.
The study was sponsored in part by Amgen, Bristol-Myers Squibb, and the Multiple Myeloma Research Consortium. Dr. Derman reported advisory board fees from Sanofi, Janssen, and COTA Healthcare; honoraria from PleXus Communications and MJH Life Sciences. Dr. Kazandjian declares receiving advisory board or consulting fees from Bristol-Myers Squibb, Sanofi, and Arcellx outside the submitted work. Dr. Landgren has received grant support from numerous organizations and pharmaceutical companies. Dr. Landgren has also received honoraria for scientific talks/participated in advisory boards for Adaptive Biotech, Amgen, Binding Site, Bristol-Myers Squibb, Celgene, Cellectis, Glenmark, Janssen, Juno, and Pfizer, and served on independent data monitoring committees for international randomized trials by Takeda, Merck, Janssen, and Theradex.
A version of this article first appeared on Medscape.com.
“It is not a big leap of faith to imagine that, in the near future, with the availability of quadruplets and T-cell therapies, the role of high-dose melphalan and autologous stem cell transplant will be diminished,” said Dickran Kazandjian, MD, and Ola Landgren, MD, PhD, of the myeloma division, Sylvester Comprehensive Cancer Center, University of Miami.
They commented in a editorial in JAMA Oncology, prompted by a paper describing new results with a novel quadruple combination of therapies. These treatments included the monoclonal antibody elotuzumab (Empliciti) added onto the established backbone of carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (known as KRd).
“Regardless of what the future holds for elotuzumab-based combinations, it is clear that the new treatment paradigm of newly diagnosed MM will incorporate antibody-based quadruplet regimens,” the editorialists commented.
“Novel immunotherapies are here to stay,” they added, “as they are already transforming the lives of patients with multiple MM and bringing a bright horizon to the treatment landscape.”
Study details
The trial of the novel quadruplet regimen was a multicenter, single-arm, phase 2 study that involved 46 patients with newly diagnosed multiple myeloma, explain first author Benjamin A. Derman, MD, of the University of Chicago Medical Center, and colleagues.
These patients had a median age of 62; more than two-thirds were male (72%) and White (70%). About half (48%) had high-risk cytogenetic abnormalities.
All patients were treated with 12 cycles of the quadruple therapy Elo-KRd regimen. They underwent bone marrow assessment of measurable residual disease (MRD; with 10-5 sensitivity) after cycle 8 and cycle 12.
“An MRD-adapted treatment approach is rational because it may identify which patients can be administered shorter courses of intensive therapy without compromising efficacy,” the authors explained.
Patients who had MRD negativity at both time points did not receive further Elo-KRd, while patients who converted from MRD positivity to negativity in between cycles 8 and 12 received 6 additional cycles of Elo-KRd. Those who remained MRD positive or converted to positivity after 12 cycles received an additional 12 cycles of Elo-KRd.
Following Elo-KRd treatment, all patients transitioned to triple therapy with Elo-Rd (with no carfilzomib), for indefinite maintenance therapy or until disease progression.
For the primary endpoint, the rate of stringent complete response and/or MRD-negativity after cycle 8 was 58% (26 of 45), meeting the predefined definition of efficacy.
Importantly, 26% of patients converted from MRD positivity after cycle 8 to negativity at a later time point, while 50% of patients reached 1-year sustained MRD negativity.
Overall, the estimated 3-year, progression-free survival was 72%, and the rate was 92% for patients with MRD-negativity at cycle 8. The overall survival rate was 78%.
The most common grade 3 or 4 adverse events were lung and nonpulmonary infections (13% and 11%, respectively), and one patient had a grade 5 MI. Three patients discontinued the treatment because of intolerance.
“An MRD-adapted design using elotuzumab and weekly KRd without autologous stem cell transplantation showed a high rate of stringent complete response (sCR) and/or MRD-negativity and durable responses,” the authors wrote.
“This approach provides support for further evaluation of MRD-guided de-escalation of therapy to decrease treatment exposure while sustaining deep responses.”
To better assess the difference of the therapy versus treatment including stem cell transplantation, a phase 3, randomized trial is currently underway to compare the Elo-KRd regimen against KRd with autologous stem cell transplant in newly diagnosed MM.
“If Elo-KRd proves superior, a randomized comparison of Elo versus anti-CD38 mAb-based quadruplets would help determine the optimal combination of therapies in the frontline setting,” the authors noted.
Randomized trial anticipated to clarify benefit
In their editorial, Dr. Kazandjian and Dr. Landgren agreed with the authors that the role of elotuzumab needs to be better clarified in a randomized trial setting.
Elotuzumab received FDA approval in 2015 based on results from the ELOQUENT-2 study, which showed improved progression-free survival and overall survival with the addition of elotuzumab to lenalidomide and dexamethasone in patients with multiple myeloma who have previously received one to three other therapies.
However, the editorialists pointed out that recently published results from the randomized ELOQUENT-1 trial of lenalidomide and dexamethasone with and without elotuzumab showed the addition of elotuzumab was not associated with a statistically significant difference in progression-free survival.
The editorialists also pointed out that, in the setting of newly diagnosed multiple myeloma, another recent, similarly designed study found that the backbone regimen of carfilzomib, lenalidomide, and dexamethasone – on its own – was also associated with a favorable MRD-negative rate of 62%.
In addition, several studies involving novel quadruple treatments with the monoclonal antibody daratumumab (Darzalex) instead of elotuzumab, have also shown benefit in newly diagnosed multiple myeloma, resulting in high rates of MRD negativity.
Collectively, the findings bode well for the quadruple regimens in the treatment of MM, the editorialists emphasized.
“Importantly, with the rate of deep remissions observed with antibody-based quadruplet therapies, one may question the role of using early high-dose melphalan and autologous stem cell transplant in every patient, especially in those who have achieved MRD negativity with the quadruplet alone,” they added.
The study was sponsored in part by Amgen, Bristol-Myers Squibb, and the Multiple Myeloma Research Consortium. Dr. Derman reported advisory board fees from Sanofi, Janssen, and COTA Healthcare; honoraria from PleXus Communications and MJH Life Sciences. Dr. Kazandjian declares receiving advisory board or consulting fees from Bristol-Myers Squibb, Sanofi, and Arcellx outside the submitted work. Dr. Landgren has received grant support from numerous organizations and pharmaceutical companies. Dr. Landgren has also received honoraria for scientific talks/participated in advisory boards for Adaptive Biotech, Amgen, Binding Site, Bristol-Myers Squibb, Celgene, Cellectis, Glenmark, Janssen, Juno, and Pfizer, and served on independent data monitoring committees for international randomized trials by Takeda, Merck, Janssen, and Theradex.
A version of this article first appeared on Medscape.com.
“It is not a big leap of faith to imagine that, in the near future, with the availability of quadruplets and T-cell therapies, the role of high-dose melphalan and autologous stem cell transplant will be diminished,” said Dickran Kazandjian, MD, and Ola Landgren, MD, PhD, of the myeloma division, Sylvester Comprehensive Cancer Center, University of Miami.
They commented in a editorial in JAMA Oncology, prompted by a paper describing new results with a novel quadruple combination of therapies. These treatments included the monoclonal antibody elotuzumab (Empliciti) added onto the established backbone of carfilzomib (Kyprolis), lenalidomide (Revlimid), and dexamethasone (known as KRd).
“Regardless of what the future holds for elotuzumab-based combinations, it is clear that the new treatment paradigm of newly diagnosed MM will incorporate antibody-based quadruplet regimens,” the editorialists commented.
“Novel immunotherapies are here to stay,” they added, “as they are already transforming the lives of patients with multiple MM and bringing a bright horizon to the treatment landscape.”
Study details
The trial of the novel quadruplet regimen was a multicenter, single-arm, phase 2 study that involved 46 patients with newly diagnosed multiple myeloma, explain first author Benjamin A. Derman, MD, of the University of Chicago Medical Center, and colleagues.
These patients had a median age of 62; more than two-thirds were male (72%) and White (70%). About half (48%) had high-risk cytogenetic abnormalities.
All patients were treated with 12 cycles of the quadruple therapy Elo-KRd regimen. They underwent bone marrow assessment of measurable residual disease (MRD; with 10-5 sensitivity) after cycle 8 and cycle 12.
“An MRD-adapted treatment approach is rational because it may identify which patients can be administered shorter courses of intensive therapy without compromising efficacy,” the authors explained.
Patients who had MRD negativity at both time points did not receive further Elo-KRd, while patients who converted from MRD positivity to negativity in between cycles 8 and 12 received 6 additional cycles of Elo-KRd. Those who remained MRD positive or converted to positivity after 12 cycles received an additional 12 cycles of Elo-KRd.
Following Elo-KRd treatment, all patients transitioned to triple therapy with Elo-Rd (with no carfilzomib), for indefinite maintenance therapy or until disease progression.
For the primary endpoint, the rate of stringent complete response and/or MRD-negativity after cycle 8 was 58% (26 of 45), meeting the predefined definition of efficacy.
Importantly, 26% of patients converted from MRD positivity after cycle 8 to negativity at a later time point, while 50% of patients reached 1-year sustained MRD negativity.
Overall, the estimated 3-year, progression-free survival was 72%, and the rate was 92% for patients with MRD-negativity at cycle 8. The overall survival rate was 78%.
The most common grade 3 or 4 adverse events were lung and nonpulmonary infections (13% and 11%, respectively), and one patient had a grade 5 MI. Three patients discontinued the treatment because of intolerance.
“An MRD-adapted design using elotuzumab and weekly KRd without autologous stem cell transplantation showed a high rate of stringent complete response (sCR) and/or MRD-negativity and durable responses,” the authors wrote.
“This approach provides support for further evaluation of MRD-guided de-escalation of therapy to decrease treatment exposure while sustaining deep responses.”
To better assess the difference of the therapy versus treatment including stem cell transplantation, a phase 3, randomized trial is currently underway to compare the Elo-KRd regimen against KRd with autologous stem cell transplant in newly diagnosed MM.
“If Elo-KRd proves superior, a randomized comparison of Elo versus anti-CD38 mAb-based quadruplets would help determine the optimal combination of therapies in the frontline setting,” the authors noted.
Randomized trial anticipated to clarify benefit
In their editorial, Dr. Kazandjian and Dr. Landgren agreed with the authors that the role of elotuzumab needs to be better clarified in a randomized trial setting.
Elotuzumab received FDA approval in 2015 based on results from the ELOQUENT-2 study, which showed improved progression-free survival and overall survival with the addition of elotuzumab to lenalidomide and dexamethasone in patients with multiple myeloma who have previously received one to three other therapies.
However, the editorialists pointed out that recently published results from the randomized ELOQUENT-1 trial of lenalidomide and dexamethasone with and without elotuzumab showed the addition of elotuzumab was not associated with a statistically significant difference in progression-free survival.
The editorialists also pointed out that, in the setting of newly diagnosed multiple myeloma, another recent, similarly designed study found that the backbone regimen of carfilzomib, lenalidomide, and dexamethasone – on its own – was also associated with a favorable MRD-negative rate of 62%.
In addition, several studies involving novel quadruple treatments with the monoclonal antibody daratumumab (Darzalex) instead of elotuzumab, have also shown benefit in newly diagnosed multiple myeloma, resulting in high rates of MRD negativity.
Collectively, the findings bode well for the quadruple regimens in the treatment of MM, the editorialists emphasized.
“Importantly, with the rate of deep remissions observed with antibody-based quadruplet therapies, one may question the role of using early high-dose melphalan and autologous stem cell transplant in every patient, especially in those who have achieved MRD negativity with the quadruplet alone,” they added.
The study was sponsored in part by Amgen, Bristol-Myers Squibb, and the Multiple Myeloma Research Consortium. Dr. Derman reported advisory board fees from Sanofi, Janssen, and COTA Healthcare; honoraria from PleXus Communications and MJH Life Sciences. Dr. Kazandjian declares receiving advisory board or consulting fees from Bristol-Myers Squibb, Sanofi, and Arcellx outside the submitted work. Dr. Landgren has received grant support from numerous organizations and pharmaceutical companies. Dr. Landgren has also received honoraria for scientific talks/participated in advisory boards for Adaptive Biotech, Amgen, Binding Site, Bristol-Myers Squibb, Celgene, Cellectis, Glenmark, Janssen, Juno, and Pfizer, and served on independent data monitoring committees for international randomized trials by Takeda, Merck, Janssen, and Theradex.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
No more injections after one-off gene therapy in hemophilia B
Patients with hemophilia B face a lifelong need for regular factor IX injections.
“Removing the need for hemophilia patients to regularly inject themselves with the missing protein is an important step in improving their quality of life,” lead author Pratima Chowdary, MD, of the Royal Free Hospital, University College London Cancer Institute, commented in a press statement.
The team reported new results with the investigational gene therapy FLT180a in a study published in the New England Journal of Medicine.
“We found that normal factor IX levels can be achieved in patients with severe or moderately severe hemophilia B with the use of relatively low vector doses of FLT180a,” the authors reported. “In all but one patient, gene therapy led to durable factor IX expression, eliminated the need for factor IX prophylaxis, and eliminated spontaneous bleeding leading to factor IX replacement.”
FLT180a (Freeline Therapeutics) is a liver-directed, adeno-associated virus (AAV) gene therapy designed to normalize levels of the factor IX protein that is needed for coagulation; however, it is produced in dangerously low levels in people with hemophilia B as a result of gene mutations.
Under the current standard of care, patients with hemophilia B require lifelong prophylaxis of regular intravenous injections with recombinant factor IX replacement therapy, and they commonly continue to experience potentially severe joint pain.
While factor-replacement therapies with longer half-lives have emerged, the prophylaxis is still invasive and extremely expensive, with the average price tag in the United States of $397,491 a year for the conventional treatment and an average of $788,861 a year for an extended half-life treatment, according to a 2019 report.
Novel gene therapy
Hemophilia B is a rare and inherited genetic bleeding disorder caused by defects in the gene responsible for factor IX protein, which is needed for blood clotting.
AAV gene therapy delivers a functional copy of this gene directly to patient tissues to compensate for one that is not working properly. It leads to the synthesis of factor IX proteins and a one-time gene therapy infusion can achieve long-lasting effects, the team explained in a press release.
The results they reported come from the phase 1/2 multicenter B-AMAZE open-label trial. It involved 10 patients (all age 18 and older) with severe or moderately severe hemophilia B, defined as having a factor IX level of 2% or less that of normal values.
All patients received one-off gene therapy infusion, at one of four FLT180a doses.
All patients also received immunosuppression to prevent the body from rejecting the vector gene therapy. This consisted of glucocorticoids with or without tacrolimus for a period of ranging from several weeks to several months.
Following the FLT180a infusion, all patients showed dose-dependent increases in factor IX levels. After a median follow-up of 27.2 months (range, 19.1-42.4 months), nearly all the patients (9 of 10) continued to show sustained factor IX activity.
Steady production of factor IX activity started at month 12, with low bleeding frequency that allowed these nine patients to no longer require weekly injections of the protein.
Five of the patients had factor IX levels in the normal range, from 51% to 78%; three patients had lower increases of 23%-43% of the normal range, and one patient who had received the highest dose, had a level that was 260% of normal.
The exception was one patient who required a return to factor IX prophylaxis. He had experienced a failure in the immunosuppression regimen due to a delay in the recognition of an immune response at approximately 22 weeks after treatment, the authors reported.
The therapy was generally well tolerated, with no infusion reactions or discontinuations of infusions. As of the study cutoff, no inhibitors of factor IX were detected.
Of the adverse events, about 10% were determined to be related to the gene therapy. The most common event associated with the gene therapy was increases in liver aminotransferase, which is a concern with AAV gene therapies, the authors commented.
Otherwise, 24% of adverse events were determined to be related to the immunosuppression, and were consistent with the known safety profiles of glucocorticoids and tacrolimus.
Late increases in aminotransferase levels were reported among patients who had received prolonged tacrolimus beyond the tapering of glucocorticoid treatment.
The one serious adverse event that was reported involved an arteriovenous fistula thrombosis, which occurred in the patient who had received the highest dose of gene therapy and who showed the highest factor IX levels.
The current findings, along with data from another recent study involving gene therapy for patients with hemophilia A, emphasized that “immune responses can occur later than previously expected and may coincide with the withdrawal of immunosuppression,” the authors cautioned.
“Consistent best practices for monitoring aminotransferase levels and deciding when ALT increases warrant intervention remain a critical topic for the field,” they noted.
Meanwhile, the patients in this B-AMAZE trial all remain enrolled in a long-term follow-up study to assess the safety and durability of FLT180a over 15 years.
The trial was sponsored by University College London and funded by Freeline Therapeutics. Dr. Chowdary disclosed various relationships with industry.
A version of this article first appeared on Medscape.com.
Patients with hemophilia B face a lifelong need for regular factor IX injections.
“Removing the need for hemophilia patients to regularly inject themselves with the missing protein is an important step in improving their quality of life,” lead author Pratima Chowdary, MD, of the Royal Free Hospital, University College London Cancer Institute, commented in a press statement.
The team reported new results with the investigational gene therapy FLT180a in a study published in the New England Journal of Medicine.
“We found that normal factor IX levels can be achieved in patients with severe or moderately severe hemophilia B with the use of relatively low vector doses of FLT180a,” the authors reported. “In all but one patient, gene therapy led to durable factor IX expression, eliminated the need for factor IX prophylaxis, and eliminated spontaneous bleeding leading to factor IX replacement.”
FLT180a (Freeline Therapeutics) is a liver-directed, adeno-associated virus (AAV) gene therapy designed to normalize levels of the factor IX protein that is needed for coagulation; however, it is produced in dangerously low levels in people with hemophilia B as a result of gene mutations.
Under the current standard of care, patients with hemophilia B require lifelong prophylaxis of regular intravenous injections with recombinant factor IX replacement therapy, and they commonly continue to experience potentially severe joint pain.
While factor-replacement therapies with longer half-lives have emerged, the prophylaxis is still invasive and extremely expensive, with the average price tag in the United States of $397,491 a year for the conventional treatment and an average of $788,861 a year for an extended half-life treatment, according to a 2019 report.
Novel gene therapy
Hemophilia B is a rare and inherited genetic bleeding disorder caused by defects in the gene responsible for factor IX protein, which is needed for blood clotting.
AAV gene therapy delivers a functional copy of this gene directly to patient tissues to compensate for one that is not working properly. It leads to the synthesis of factor IX proteins and a one-time gene therapy infusion can achieve long-lasting effects, the team explained in a press release.
The results they reported come from the phase 1/2 multicenter B-AMAZE open-label trial. It involved 10 patients (all age 18 and older) with severe or moderately severe hemophilia B, defined as having a factor IX level of 2% or less that of normal values.
All patients received one-off gene therapy infusion, at one of four FLT180a doses.
All patients also received immunosuppression to prevent the body from rejecting the vector gene therapy. This consisted of glucocorticoids with or without tacrolimus for a period of ranging from several weeks to several months.
Following the FLT180a infusion, all patients showed dose-dependent increases in factor IX levels. After a median follow-up of 27.2 months (range, 19.1-42.4 months), nearly all the patients (9 of 10) continued to show sustained factor IX activity.
Steady production of factor IX activity started at month 12, with low bleeding frequency that allowed these nine patients to no longer require weekly injections of the protein.
Five of the patients had factor IX levels in the normal range, from 51% to 78%; three patients had lower increases of 23%-43% of the normal range, and one patient who had received the highest dose, had a level that was 260% of normal.
The exception was one patient who required a return to factor IX prophylaxis. He had experienced a failure in the immunosuppression regimen due to a delay in the recognition of an immune response at approximately 22 weeks after treatment, the authors reported.
The therapy was generally well tolerated, with no infusion reactions or discontinuations of infusions. As of the study cutoff, no inhibitors of factor IX were detected.
Of the adverse events, about 10% were determined to be related to the gene therapy. The most common event associated with the gene therapy was increases in liver aminotransferase, which is a concern with AAV gene therapies, the authors commented.
Otherwise, 24% of adverse events were determined to be related to the immunosuppression, and were consistent with the known safety profiles of glucocorticoids and tacrolimus.
Late increases in aminotransferase levels were reported among patients who had received prolonged tacrolimus beyond the tapering of glucocorticoid treatment.
The one serious adverse event that was reported involved an arteriovenous fistula thrombosis, which occurred in the patient who had received the highest dose of gene therapy and who showed the highest factor IX levels.
The current findings, along with data from another recent study involving gene therapy for patients with hemophilia A, emphasized that “immune responses can occur later than previously expected and may coincide with the withdrawal of immunosuppression,” the authors cautioned.
“Consistent best practices for monitoring aminotransferase levels and deciding when ALT increases warrant intervention remain a critical topic for the field,” they noted.
Meanwhile, the patients in this B-AMAZE trial all remain enrolled in a long-term follow-up study to assess the safety and durability of FLT180a over 15 years.
The trial was sponsored by University College London and funded by Freeline Therapeutics. Dr. Chowdary disclosed various relationships with industry.
A version of this article first appeared on Medscape.com.
Patients with hemophilia B face a lifelong need for regular factor IX injections.
“Removing the need for hemophilia patients to regularly inject themselves with the missing protein is an important step in improving their quality of life,” lead author Pratima Chowdary, MD, of the Royal Free Hospital, University College London Cancer Institute, commented in a press statement.
The team reported new results with the investigational gene therapy FLT180a in a study published in the New England Journal of Medicine.
“We found that normal factor IX levels can be achieved in patients with severe or moderately severe hemophilia B with the use of relatively low vector doses of FLT180a,” the authors reported. “In all but one patient, gene therapy led to durable factor IX expression, eliminated the need for factor IX prophylaxis, and eliminated spontaneous bleeding leading to factor IX replacement.”
FLT180a (Freeline Therapeutics) is a liver-directed, adeno-associated virus (AAV) gene therapy designed to normalize levels of the factor IX protein that is needed for coagulation; however, it is produced in dangerously low levels in people with hemophilia B as a result of gene mutations.
Under the current standard of care, patients with hemophilia B require lifelong prophylaxis of regular intravenous injections with recombinant factor IX replacement therapy, and they commonly continue to experience potentially severe joint pain.
While factor-replacement therapies with longer half-lives have emerged, the prophylaxis is still invasive and extremely expensive, with the average price tag in the United States of $397,491 a year for the conventional treatment and an average of $788,861 a year for an extended half-life treatment, according to a 2019 report.
Novel gene therapy
Hemophilia B is a rare and inherited genetic bleeding disorder caused by defects in the gene responsible for factor IX protein, which is needed for blood clotting.
AAV gene therapy delivers a functional copy of this gene directly to patient tissues to compensate for one that is not working properly. It leads to the synthesis of factor IX proteins and a one-time gene therapy infusion can achieve long-lasting effects, the team explained in a press release.
The results they reported come from the phase 1/2 multicenter B-AMAZE open-label trial. It involved 10 patients (all age 18 and older) with severe or moderately severe hemophilia B, defined as having a factor IX level of 2% or less that of normal values.
All patients received one-off gene therapy infusion, at one of four FLT180a doses.
All patients also received immunosuppression to prevent the body from rejecting the vector gene therapy. This consisted of glucocorticoids with or without tacrolimus for a period of ranging from several weeks to several months.
Following the FLT180a infusion, all patients showed dose-dependent increases in factor IX levels. After a median follow-up of 27.2 months (range, 19.1-42.4 months), nearly all the patients (9 of 10) continued to show sustained factor IX activity.
Steady production of factor IX activity started at month 12, with low bleeding frequency that allowed these nine patients to no longer require weekly injections of the protein.
Five of the patients had factor IX levels in the normal range, from 51% to 78%; three patients had lower increases of 23%-43% of the normal range, and one patient who had received the highest dose, had a level that was 260% of normal.
The exception was one patient who required a return to factor IX prophylaxis. He had experienced a failure in the immunosuppression regimen due to a delay in the recognition of an immune response at approximately 22 weeks after treatment, the authors reported.
The therapy was generally well tolerated, with no infusion reactions or discontinuations of infusions. As of the study cutoff, no inhibitors of factor IX were detected.
Of the adverse events, about 10% were determined to be related to the gene therapy. The most common event associated with the gene therapy was increases in liver aminotransferase, which is a concern with AAV gene therapies, the authors commented.
Otherwise, 24% of adverse events were determined to be related to the immunosuppression, and were consistent with the known safety profiles of glucocorticoids and tacrolimus.
Late increases in aminotransferase levels were reported among patients who had received prolonged tacrolimus beyond the tapering of glucocorticoid treatment.
The one serious adverse event that was reported involved an arteriovenous fistula thrombosis, which occurred in the patient who had received the highest dose of gene therapy and who showed the highest factor IX levels.
The current findings, along with data from another recent study involving gene therapy for patients with hemophilia A, emphasized that “immune responses can occur later than previously expected and may coincide with the withdrawal of immunosuppression,” the authors cautioned.
“Consistent best practices for monitoring aminotransferase levels and deciding when ALT increases warrant intervention remain a critical topic for the field,” they noted.
Meanwhile, the patients in this B-AMAZE trial all remain enrolled in a long-term follow-up study to assess the safety and durability of FLT180a over 15 years.
The trial was sponsored by University College London and funded by Freeline Therapeutics. Dr. Chowdary disclosed various relationships with industry.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
CAR T-cell therapy turns 10 and finally earns the word ‘cure’
Ten years ago, Stephan Grupp, MD, PhD, plunged into an unexplored area of pediatric cancer treatment with a 6-year-old patient for whom every treatment available for her acute lymphoblastic leukemia (ALL) had been exhausted.
Dr. Grupp, a pioneer in cellular immunotherapy at Children’s Hospital of Philadelphia, had just got the green light to launch the first phase 1 trial of chimeric antigen receptor (CAR) T-cell therapy for children.
“The trial opened at the absolute last possible moment that it could have been helpful to her,” he said in an interview. “There was nothing else to do to temporize her further. ... It had to open then or never.”
The patient was Emily Whitehead, who has since become a poster girl for the dramatic results that can be achieved with these novel therapies. After that one CAR T-cell treatment back in 2012, she has been free of her leukemia and has remained in remission for more than 10 years.
Dr. Grupp said that he is, at last, starting to use the “cure” word.
“I’m not just a doctor, I’m a scientist – and one case isn’t enough to have confidence about anything,” he said. “We wanted more patients to be out longer to be able to say that thing which we have for a long time called the ‘c word.’
“CAR T-cell therapy has now been given to hundreds of patients at CHOP, and – we are unique in this – we have a couple dozen patients who are 5, 6, 7, 9 years out or more without further therapy. That feels like a cure to me,” he commented.
First patient with ALL
Emily was the first patient with ALL to receive the novel treatment, and also the first child.
There was a precedent, however. After having been “stuck” for decades, the CAR T-cell field had recently made a breakthrough, thanks to research by Dr. Grupp’s colleague Carl June, MD, and associates at the University of Pennsylvania, Philadelphia. By tweaking two key steps in the genetic modification of T cells, Dr. June’s team had successfully treated three adults with chronic lymphocytic leukemia (CLL), two of whom were in complete remission.
But using the treatment for a child and for a different type of leukemia was a daunting prospect. Dr. Grupp said that he was candid with Emily’s parents, Tom and Kari Whitehead, emphasizing that there are no guarantees in cancer treatment, particularly in a phase 1 trial.
But the Whiteheads had no time to waste and nowhere else to turn. Her father, Tom, recalled saying: “This is something outside the box, this is going to give her a chance.”
Dr. Grupp, who described himself as being “on the cowboy end” of oncology care, was ready to take the plunge.
Little did any of them know that the treatment would make Emily even sicker than she already was, putting her in intensive care. But thanks to a combination of several lucky breaks and a lot of brain power, she would make a breathtakingly rapid recovery.
The ‘magic formula’
CAR T-cell therapy involves harvesting a patient’s T cells and modifying them in the lab with a chimeric antigen receptor to target CD19, a protein found on the surface of ALL cancer cells.
Before the University of Pennsylvania team tweaked the process, clinical trials of the therapy yielded only modest results because the modified T cells “were very powerful in the short term but had almost no proliferative capacity” once they were infused back into the patient, Dr. Grupp explained.
“It does not matter how many cells you give to a patient, what matters is that the cells grow in the patient to the level needed to control the leukemia,” he said.
Dr. June’s team came up with what Dr. Grupp calls “the magic formula”: A bead-based manufacturing process that produced younger T-cell phenotypes with “enormous” proliferative capacity, and a lentiviral approach to the genetic modification, enabling prolonged expression of the CAR-T molecule.
“Was it rogue? Absolutely, positively not,” said Dr. Grupp, thinking back to the day he enrolled Emily in the trial. “Was it risky? Obviously ... we all dived into this pool without knowing what was under the water, so I would say, rogue, no, risky, yes. And I would say we didn’t know nearly enough about the risks.”
Cytokine storm
The gravest risk that Dr. Grupp and his team encountered was something they had not anticipated. At the time, they had no name for it.
The three adults with CLL who had received CAR T-cell therapy had experienced a mild version that the researchers referred to as “tumor lysis syndrome”.
But for Emily, on day 3 of her CAR T-cell infusion, there was a ferocious reaction storm that later came to be called cytokine release syndrome.
“The wheels just came off then,” said Mr. Whitehead. “I remember her blood pressure was 53 over 29. They took her to the ICU, induced a coma, and put her on a ventilator. It was brutal to watch. The oscillatory ventilator just pounds on you, and there was blood bubbling out around the hose in her mouth.
“I remember the third or fourth night, a doctor took me in the hallway and said, ‘There’s a one-in-a-thousand chance your daughter is alive when the sun comes up,’” Mr. Whitehead said in an interview. “And I said: ‘All right, I’ll see you at rounds tomorrow, because she’ll still be here.’ ”
“We had some vague notion of toxicity ... but it turned out not nearly enough,” said Dr. Grupp. The ICU “worked flat out” to save her life. “They had deployed everything they had to keep a human being alive and they had nothing more to add. At some point, you run out of things that you can do, and we had run out.”
On the fly
It was then that the team ran into some good luck. The first break was when they decided to look at her cytokines. “Our whole knowledge base came together in the moment, on the fly, at the exact moment when Emily was so very sick,” he recalled. “Could we get the result fast enough? The lab dropped everything to run the test.”
They ordered a broad cytokine panel that included 30 analytes. The results showed that a number of cytokines “were just unbelievably elevated,” he said. Among them was interleukin-6.
“IL-6 isn’t even made by T cells, so nobody in the world would have guessed that this would have mattered. If we’d ordered a smaller panel, it might not even have been on it. Yet this was the one cytokine we had a drug for – tocilizumab – so that was chance. And then, another chance was that the drug was at the hospital, because there are rheumatology patients who get it.
“So, we went from making the determination that IL-6 was high and figuring out there was a drug for it at 3:00 o’clock to giving the drug to her at 8:00 o’clock, and then her clinical situation turned around so quickly – I mean hours later.”
Emily woke up from a 14-day medically induced coma on her seventh birthday.
Eight days later, her bone marrow showed complete remission. “The doctors said, ‘We’ve never seen anyone this sick get better any faster,’ ” Mr. Whitehead said.
She had already been through a battery of treatments for her leukemia. “It was 22 months of failed, standard treatment, and then just 23 days after they gave her the first dose of CAR T-cells that she was cancer free,” he added.
Talking about ‘cure’
Now that Emily, 17, has remained in remission for 10 years, Dr. Grupp is finally willing to use the word “cure” – but it has taken him a long time.
Now, he says, the challenge from the bedside is to keep parents’ and patients’ expectations realistic about what they see as a miracle cure.
“It’s not a miracle. We can get patients into remission 90-plus percent of the time – but some patients do relapse – and then there are the risks [of the cytokine storm, which can be life-threatening].
“Right now, our experience is that about 12% of patients end up in the ICU, but they hardly ever end up as sick as Emily ... because now we’re giving the tocilizumab much earlier,” Dr. Grupp said.
Hearing whispers
Since their daughter’s recovery, Tom and Kari Whitehead have dedicated much of their time to spreading the word about the treatment that saved Emily’s life. Mr. Whitehead testified at the Food and Drug Administration’s advisory committee meeting in 2017 when approval was being considered for the CAR T-cell product that Emily received. The product was tisagenlecleucel-T (Novartis); at that meeting, there was a unanimous vote to recommend approval. This was the first CAR T cell to reach the market.
As cofounders of the Emily Whitehead Foundation, Emily’s parents have helped raise more than $2 million to support research in the field, and they travel around the world telling their story to “move this revolution forward.”
Despite their fierce belief in the science that saved Emily, they also acknowledge there was luck – and faith. Early in their journey, when Emily experienced relapse after her initial treatments, Mr. Whitehead drew comfort from two visions, which he calls “whispers,” that guided them through several forks in the road and through tough decisions about Emily’s treatment.
Several times the parents refused treatment that was offered to Emily, and once they had her discharged against medical advice. “I told Kari she’s definitely going to beat her cancer – I saw it. I don’t know how it’s going to happen, but we’re going to be in the bone marrow transplant hallway [at CHOP] teaching her to walk again. I know a lot of doctors don’t want to hear anything about ‘a sign,’ or what guided us, but I don’t think you have to separate faith and science, I think it takes everything to make something like this to happen.”
Enduring effect
The key to the CAR T-cell breakthrough that gave rise to Emily’s therapy was cell proliferation, and the effect is enduring, beyond all expectations, said Dr. Grupp. The modified T cells are still detectable in Emily and other patients in long-term remission.
“The fundamental question is, are the cells still working, or are the patients cured and they don’t need them?” said Dr. Grupp. “I think it’s the latter. The data that we have from several large datasets that we developed with Novartis are that, if you get to a year and your minimal residual disease testing both by flow and by next-generation sequencing is negative and you still have B-cell aplasia, the relapse risk is close to zero at that point.”
While it’s still not clear if and when that risk will ever get to zero, Emily and Dr. Grupp have successfully closed the chapter.
“Oncologists have different notions of what the word ‘cure’ means. If your attitude is you’re not cured until you’ve basically reached the end of your life and you haven’t relapsed, well, that’s an impossible bar to hit. My attitude is, if your likelihood of having a disease recurrence is lower than the other risks in your life, like getting into your car and driving to your appointment, then that’s what a functional cure looks like,” he said.
“I’m probably the doctor that still sees her the most, but honestly, the whole conversation is not about leukemia at all. She has B-cell aplasia, so we have to treat that, and then it’s about making sure there’s no long-term side effects from the totality of her treatment. Generally, for a patient who’s gotten a moderate amount of chemotherapy and CAR T, that should not interfere with fertility. Has any patient in the history of the world ever relapsed more than 5 years out from their therapy? Of course. Is that incredibly rare? Yes, it is. You can be paralyzed by that, or you can compartmentalize it.”
As for the Whiteheads, they are focused on Emily’s college applications, her new driver’s license, and her project to cowrite a film about her story with a Hollywood filmmaker.
Mr. Whitehead said the one thing he hopes clinicians take away from their story is that sometimes a parent’s instinct transcends science.
A version of this article first appeared on Medscape.com.
Ten years ago, Stephan Grupp, MD, PhD, plunged into an unexplored area of pediatric cancer treatment with a 6-year-old patient for whom every treatment available for her acute lymphoblastic leukemia (ALL) had been exhausted.
Dr. Grupp, a pioneer in cellular immunotherapy at Children’s Hospital of Philadelphia, had just got the green light to launch the first phase 1 trial of chimeric antigen receptor (CAR) T-cell therapy for children.
“The trial opened at the absolute last possible moment that it could have been helpful to her,” he said in an interview. “There was nothing else to do to temporize her further. ... It had to open then or never.”
The patient was Emily Whitehead, who has since become a poster girl for the dramatic results that can be achieved with these novel therapies. After that one CAR T-cell treatment back in 2012, she has been free of her leukemia and has remained in remission for more than 10 years.
Dr. Grupp said that he is, at last, starting to use the “cure” word.
“I’m not just a doctor, I’m a scientist – and one case isn’t enough to have confidence about anything,” he said. “We wanted more patients to be out longer to be able to say that thing which we have for a long time called the ‘c word.’
“CAR T-cell therapy has now been given to hundreds of patients at CHOP, and – we are unique in this – we have a couple dozen patients who are 5, 6, 7, 9 years out or more without further therapy. That feels like a cure to me,” he commented.
First patient with ALL
Emily was the first patient with ALL to receive the novel treatment, and also the first child.
There was a precedent, however. After having been “stuck” for decades, the CAR T-cell field had recently made a breakthrough, thanks to research by Dr. Grupp’s colleague Carl June, MD, and associates at the University of Pennsylvania, Philadelphia. By tweaking two key steps in the genetic modification of T cells, Dr. June’s team had successfully treated three adults with chronic lymphocytic leukemia (CLL), two of whom were in complete remission.
But using the treatment for a child and for a different type of leukemia was a daunting prospect. Dr. Grupp said that he was candid with Emily’s parents, Tom and Kari Whitehead, emphasizing that there are no guarantees in cancer treatment, particularly in a phase 1 trial.
But the Whiteheads had no time to waste and nowhere else to turn. Her father, Tom, recalled saying: “This is something outside the box, this is going to give her a chance.”
Dr. Grupp, who described himself as being “on the cowboy end” of oncology care, was ready to take the plunge.
Little did any of them know that the treatment would make Emily even sicker than she already was, putting her in intensive care. But thanks to a combination of several lucky breaks and a lot of brain power, she would make a breathtakingly rapid recovery.
The ‘magic formula’
CAR T-cell therapy involves harvesting a patient’s T cells and modifying them in the lab with a chimeric antigen receptor to target CD19, a protein found on the surface of ALL cancer cells.
Before the University of Pennsylvania team tweaked the process, clinical trials of the therapy yielded only modest results because the modified T cells “were very powerful in the short term but had almost no proliferative capacity” once they were infused back into the patient, Dr. Grupp explained.
“It does not matter how many cells you give to a patient, what matters is that the cells grow in the patient to the level needed to control the leukemia,” he said.
Dr. June’s team came up with what Dr. Grupp calls “the magic formula”: A bead-based manufacturing process that produced younger T-cell phenotypes with “enormous” proliferative capacity, and a lentiviral approach to the genetic modification, enabling prolonged expression of the CAR-T molecule.
“Was it rogue? Absolutely, positively not,” said Dr. Grupp, thinking back to the day he enrolled Emily in the trial. “Was it risky? Obviously ... we all dived into this pool without knowing what was under the water, so I would say, rogue, no, risky, yes. And I would say we didn’t know nearly enough about the risks.”
Cytokine storm
The gravest risk that Dr. Grupp and his team encountered was something they had not anticipated. At the time, they had no name for it.
The three adults with CLL who had received CAR T-cell therapy had experienced a mild version that the researchers referred to as “tumor lysis syndrome”.
But for Emily, on day 3 of her CAR T-cell infusion, there was a ferocious reaction storm that later came to be called cytokine release syndrome.
“The wheels just came off then,” said Mr. Whitehead. “I remember her blood pressure was 53 over 29. They took her to the ICU, induced a coma, and put her on a ventilator. It was brutal to watch. The oscillatory ventilator just pounds on you, and there was blood bubbling out around the hose in her mouth.
“I remember the third or fourth night, a doctor took me in the hallway and said, ‘There’s a one-in-a-thousand chance your daughter is alive when the sun comes up,’” Mr. Whitehead said in an interview. “And I said: ‘All right, I’ll see you at rounds tomorrow, because she’ll still be here.’ ”
“We had some vague notion of toxicity ... but it turned out not nearly enough,” said Dr. Grupp. The ICU “worked flat out” to save her life. “They had deployed everything they had to keep a human being alive and they had nothing more to add. At some point, you run out of things that you can do, and we had run out.”
On the fly
It was then that the team ran into some good luck. The first break was when they decided to look at her cytokines. “Our whole knowledge base came together in the moment, on the fly, at the exact moment when Emily was so very sick,” he recalled. “Could we get the result fast enough? The lab dropped everything to run the test.”
They ordered a broad cytokine panel that included 30 analytes. The results showed that a number of cytokines “were just unbelievably elevated,” he said. Among them was interleukin-6.
“IL-6 isn’t even made by T cells, so nobody in the world would have guessed that this would have mattered. If we’d ordered a smaller panel, it might not even have been on it. Yet this was the one cytokine we had a drug for – tocilizumab – so that was chance. And then, another chance was that the drug was at the hospital, because there are rheumatology patients who get it.
“So, we went from making the determination that IL-6 was high and figuring out there was a drug for it at 3:00 o’clock to giving the drug to her at 8:00 o’clock, and then her clinical situation turned around so quickly – I mean hours later.”
Emily woke up from a 14-day medically induced coma on her seventh birthday.
Eight days later, her bone marrow showed complete remission. “The doctors said, ‘We’ve never seen anyone this sick get better any faster,’ ” Mr. Whitehead said.
She had already been through a battery of treatments for her leukemia. “It was 22 months of failed, standard treatment, and then just 23 days after they gave her the first dose of CAR T-cells that she was cancer free,” he added.
Talking about ‘cure’
Now that Emily, 17, has remained in remission for 10 years, Dr. Grupp is finally willing to use the word “cure” – but it has taken him a long time.
Now, he says, the challenge from the bedside is to keep parents’ and patients’ expectations realistic about what they see as a miracle cure.
“It’s not a miracle. We can get patients into remission 90-plus percent of the time – but some patients do relapse – and then there are the risks [of the cytokine storm, which can be life-threatening].
“Right now, our experience is that about 12% of patients end up in the ICU, but they hardly ever end up as sick as Emily ... because now we’re giving the tocilizumab much earlier,” Dr. Grupp said.
Hearing whispers
Since their daughter’s recovery, Tom and Kari Whitehead have dedicated much of their time to spreading the word about the treatment that saved Emily’s life. Mr. Whitehead testified at the Food and Drug Administration’s advisory committee meeting in 2017 when approval was being considered for the CAR T-cell product that Emily received. The product was tisagenlecleucel-T (Novartis); at that meeting, there was a unanimous vote to recommend approval. This was the first CAR T cell to reach the market.
As cofounders of the Emily Whitehead Foundation, Emily’s parents have helped raise more than $2 million to support research in the field, and they travel around the world telling their story to “move this revolution forward.”
Despite their fierce belief in the science that saved Emily, they also acknowledge there was luck – and faith. Early in their journey, when Emily experienced relapse after her initial treatments, Mr. Whitehead drew comfort from two visions, which he calls “whispers,” that guided them through several forks in the road and through tough decisions about Emily’s treatment.
Several times the parents refused treatment that was offered to Emily, and once they had her discharged against medical advice. “I told Kari she’s definitely going to beat her cancer – I saw it. I don’t know how it’s going to happen, but we’re going to be in the bone marrow transplant hallway [at CHOP] teaching her to walk again. I know a lot of doctors don’t want to hear anything about ‘a sign,’ or what guided us, but I don’t think you have to separate faith and science, I think it takes everything to make something like this to happen.”
Enduring effect
The key to the CAR T-cell breakthrough that gave rise to Emily’s therapy was cell proliferation, and the effect is enduring, beyond all expectations, said Dr. Grupp. The modified T cells are still detectable in Emily and other patients in long-term remission.
“The fundamental question is, are the cells still working, or are the patients cured and they don’t need them?” said Dr. Grupp. “I think it’s the latter. The data that we have from several large datasets that we developed with Novartis are that, if you get to a year and your minimal residual disease testing both by flow and by next-generation sequencing is negative and you still have B-cell aplasia, the relapse risk is close to zero at that point.”
While it’s still not clear if and when that risk will ever get to zero, Emily and Dr. Grupp have successfully closed the chapter.
“Oncologists have different notions of what the word ‘cure’ means. If your attitude is you’re not cured until you’ve basically reached the end of your life and you haven’t relapsed, well, that’s an impossible bar to hit. My attitude is, if your likelihood of having a disease recurrence is lower than the other risks in your life, like getting into your car and driving to your appointment, then that’s what a functional cure looks like,” he said.
“I’m probably the doctor that still sees her the most, but honestly, the whole conversation is not about leukemia at all. She has B-cell aplasia, so we have to treat that, and then it’s about making sure there’s no long-term side effects from the totality of her treatment. Generally, for a patient who’s gotten a moderate amount of chemotherapy and CAR T, that should not interfere with fertility. Has any patient in the history of the world ever relapsed more than 5 years out from their therapy? Of course. Is that incredibly rare? Yes, it is. You can be paralyzed by that, or you can compartmentalize it.”
As for the Whiteheads, they are focused on Emily’s college applications, her new driver’s license, and her project to cowrite a film about her story with a Hollywood filmmaker.
Mr. Whitehead said the one thing he hopes clinicians take away from their story is that sometimes a parent’s instinct transcends science.
A version of this article first appeared on Medscape.com.
Ten years ago, Stephan Grupp, MD, PhD, plunged into an unexplored area of pediatric cancer treatment with a 6-year-old patient for whom every treatment available for her acute lymphoblastic leukemia (ALL) had been exhausted.
Dr. Grupp, a pioneer in cellular immunotherapy at Children’s Hospital of Philadelphia, had just got the green light to launch the first phase 1 trial of chimeric antigen receptor (CAR) T-cell therapy for children.
“The trial opened at the absolute last possible moment that it could have been helpful to her,” he said in an interview. “There was nothing else to do to temporize her further. ... It had to open then or never.”
The patient was Emily Whitehead, who has since become a poster girl for the dramatic results that can be achieved with these novel therapies. After that one CAR T-cell treatment back in 2012, she has been free of her leukemia and has remained in remission for more than 10 years.
Dr. Grupp said that he is, at last, starting to use the “cure” word.
“I’m not just a doctor, I’m a scientist – and one case isn’t enough to have confidence about anything,” he said. “We wanted more patients to be out longer to be able to say that thing which we have for a long time called the ‘c word.’
“CAR T-cell therapy has now been given to hundreds of patients at CHOP, and – we are unique in this – we have a couple dozen patients who are 5, 6, 7, 9 years out or more without further therapy. That feels like a cure to me,” he commented.
First patient with ALL
Emily was the first patient with ALL to receive the novel treatment, and also the first child.
There was a precedent, however. After having been “stuck” for decades, the CAR T-cell field had recently made a breakthrough, thanks to research by Dr. Grupp’s colleague Carl June, MD, and associates at the University of Pennsylvania, Philadelphia. By tweaking two key steps in the genetic modification of T cells, Dr. June’s team had successfully treated three adults with chronic lymphocytic leukemia (CLL), two of whom were in complete remission.
But using the treatment for a child and for a different type of leukemia was a daunting prospect. Dr. Grupp said that he was candid with Emily’s parents, Tom and Kari Whitehead, emphasizing that there are no guarantees in cancer treatment, particularly in a phase 1 trial.
But the Whiteheads had no time to waste and nowhere else to turn. Her father, Tom, recalled saying: “This is something outside the box, this is going to give her a chance.”
Dr. Grupp, who described himself as being “on the cowboy end” of oncology care, was ready to take the plunge.
Little did any of them know that the treatment would make Emily even sicker than she already was, putting her in intensive care. But thanks to a combination of several lucky breaks and a lot of brain power, she would make a breathtakingly rapid recovery.
The ‘magic formula’
CAR T-cell therapy involves harvesting a patient’s T cells and modifying them in the lab with a chimeric antigen receptor to target CD19, a protein found on the surface of ALL cancer cells.
Before the University of Pennsylvania team tweaked the process, clinical trials of the therapy yielded only modest results because the modified T cells “were very powerful in the short term but had almost no proliferative capacity” once they were infused back into the patient, Dr. Grupp explained.
“It does not matter how many cells you give to a patient, what matters is that the cells grow in the patient to the level needed to control the leukemia,” he said.
Dr. June’s team came up with what Dr. Grupp calls “the magic formula”: A bead-based manufacturing process that produced younger T-cell phenotypes with “enormous” proliferative capacity, and a lentiviral approach to the genetic modification, enabling prolonged expression of the CAR-T molecule.
“Was it rogue? Absolutely, positively not,” said Dr. Grupp, thinking back to the day he enrolled Emily in the trial. “Was it risky? Obviously ... we all dived into this pool without knowing what was under the water, so I would say, rogue, no, risky, yes. And I would say we didn’t know nearly enough about the risks.”
Cytokine storm
The gravest risk that Dr. Grupp and his team encountered was something they had not anticipated. At the time, they had no name for it.
The three adults with CLL who had received CAR T-cell therapy had experienced a mild version that the researchers referred to as “tumor lysis syndrome”.
But for Emily, on day 3 of her CAR T-cell infusion, there was a ferocious reaction storm that later came to be called cytokine release syndrome.
“The wheels just came off then,” said Mr. Whitehead. “I remember her blood pressure was 53 over 29. They took her to the ICU, induced a coma, and put her on a ventilator. It was brutal to watch. The oscillatory ventilator just pounds on you, and there was blood bubbling out around the hose in her mouth.
“I remember the third or fourth night, a doctor took me in the hallway and said, ‘There’s a one-in-a-thousand chance your daughter is alive when the sun comes up,’” Mr. Whitehead said in an interview. “And I said: ‘All right, I’ll see you at rounds tomorrow, because she’ll still be here.’ ”
“We had some vague notion of toxicity ... but it turned out not nearly enough,” said Dr. Grupp. The ICU “worked flat out” to save her life. “They had deployed everything they had to keep a human being alive and they had nothing more to add. At some point, you run out of things that you can do, and we had run out.”
On the fly
It was then that the team ran into some good luck. The first break was when they decided to look at her cytokines. “Our whole knowledge base came together in the moment, on the fly, at the exact moment when Emily was so very sick,” he recalled. “Could we get the result fast enough? The lab dropped everything to run the test.”
They ordered a broad cytokine panel that included 30 analytes. The results showed that a number of cytokines “were just unbelievably elevated,” he said. Among them was interleukin-6.
“IL-6 isn’t even made by T cells, so nobody in the world would have guessed that this would have mattered. If we’d ordered a smaller panel, it might not even have been on it. Yet this was the one cytokine we had a drug for – tocilizumab – so that was chance. And then, another chance was that the drug was at the hospital, because there are rheumatology patients who get it.
“So, we went from making the determination that IL-6 was high and figuring out there was a drug for it at 3:00 o’clock to giving the drug to her at 8:00 o’clock, and then her clinical situation turned around so quickly – I mean hours later.”
Emily woke up from a 14-day medically induced coma on her seventh birthday.
Eight days later, her bone marrow showed complete remission. “The doctors said, ‘We’ve never seen anyone this sick get better any faster,’ ” Mr. Whitehead said.
She had already been through a battery of treatments for her leukemia. “It was 22 months of failed, standard treatment, and then just 23 days after they gave her the first dose of CAR T-cells that she was cancer free,” he added.
Talking about ‘cure’
Now that Emily, 17, has remained in remission for 10 years, Dr. Grupp is finally willing to use the word “cure” – but it has taken him a long time.
Now, he says, the challenge from the bedside is to keep parents’ and patients’ expectations realistic about what they see as a miracle cure.
“It’s not a miracle. We can get patients into remission 90-plus percent of the time – but some patients do relapse – and then there are the risks [of the cytokine storm, which can be life-threatening].
“Right now, our experience is that about 12% of patients end up in the ICU, but they hardly ever end up as sick as Emily ... because now we’re giving the tocilizumab much earlier,” Dr. Grupp said.
Hearing whispers
Since their daughter’s recovery, Tom and Kari Whitehead have dedicated much of their time to spreading the word about the treatment that saved Emily’s life. Mr. Whitehead testified at the Food and Drug Administration’s advisory committee meeting in 2017 when approval was being considered for the CAR T-cell product that Emily received. The product was tisagenlecleucel-T (Novartis); at that meeting, there was a unanimous vote to recommend approval. This was the first CAR T cell to reach the market.
As cofounders of the Emily Whitehead Foundation, Emily’s parents have helped raise more than $2 million to support research in the field, and they travel around the world telling their story to “move this revolution forward.”
Despite their fierce belief in the science that saved Emily, they also acknowledge there was luck – and faith. Early in their journey, when Emily experienced relapse after her initial treatments, Mr. Whitehead drew comfort from two visions, which he calls “whispers,” that guided them through several forks in the road and through tough decisions about Emily’s treatment.
Several times the parents refused treatment that was offered to Emily, and once they had her discharged against medical advice. “I told Kari she’s definitely going to beat her cancer – I saw it. I don’t know how it’s going to happen, but we’re going to be in the bone marrow transplant hallway [at CHOP] teaching her to walk again. I know a lot of doctors don’t want to hear anything about ‘a sign,’ or what guided us, but I don’t think you have to separate faith and science, I think it takes everything to make something like this to happen.”
Enduring effect
The key to the CAR T-cell breakthrough that gave rise to Emily’s therapy was cell proliferation, and the effect is enduring, beyond all expectations, said Dr. Grupp. The modified T cells are still detectable in Emily and other patients in long-term remission.
“The fundamental question is, are the cells still working, or are the patients cured and they don’t need them?” said Dr. Grupp. “I think it’s the latter. The data that we have from several large datasets that we developed with Novartis are that, if you get to a year and your minimal residual disease testing both by flow and by next-generation sequencing is negative and you still have B-cell aplasia, the relapse risk is close to zero at that point.”
While it’s still not clear if and when that risk will ever get to zero, Emily and Dr. Grupp have successfully closed the chapter.
“Oncologists have different notions of what the word ‘cure’ means. If your attitude is you’re not cured until you’ve basically reached the end of your life and you haven’t relapsed, well, that’s an impossible bar to hit. My attitude is, if your likelihood of having a disease recurrence is lower than the other risks in your life, like getting into your car and driving to your appointment, then that’s what a functional cure looks like,” he said.
“I’m probably the doctor that still sees her the most, but honestly, the whole conversation is not about leukemia at all. She has B-cell aplasia, so we have to treat that, and then it’s about making sure there’s no long-term side effects from the totality of her treatment. Generally, for a patient who’s gotten a moderate amount of chemotherapy and CAR T, that should not interfere with fertility. Has any patient in the history of the world ever relapsed more than 5 years out from their therapy? Of course. Is that incredibly rare? Yes, it is. You can be paralyzed by that, or you can compartmentalize it.”
As for the Whiteheads, they are focused on Emily’s college applications, her new driver’s license, and her project to cowrite a film about her story with a Hollywood filmmaker.
Mr. Whitehead said the one thing he hopes clinicians take away from their story is that sometimes a parent’s instinct transcends science.
A version of this article first appeared on Medscape.com.
Essential strategies and tactics for managing sickle cell disease
The group of disorders known as sickle cell disease (SCD) is one of the more common genetic hemoglobinopathies. Homozygous production of the S variant of hemoglobin (Hb) in red blood cells (RBCs) results in profound sickling under conditions of physiologic stress, a condition known as Hb SS disease. People with Hb SS disease are at risk of chronic hemolytic anemia, tissue ischemia that causes vaso-occlusive pain syndrome, and other vaso-occlusive complications.1 They also experience a > 20-year reduction in life expectancy, compared to age-matched controls; onset of risk of early death is usually after age 25 years.
People with heterozygous expression of the Hb S variant—that is, from one parent, and expression of Hb A from the other parent—are said to have sickle cell trait (SCT). They typically do not have symptoms of SCD, although they can experience vaso-occlusive pain under severe physiologic stress and suffer sudden death more often than age-matched controls. People who are heterozygous for Hb S but have another hemoglobinopathy (eg,
Alleviating the harsh burden of illness. All patients with SCD are more likely than age-matched counterparts to experience income loss because of their disability; the same loss is true for their caregivers. Such loss, when combined with time spent in the health care system, can be catastrophic.2,3 But this loss can be mitigated with access to regular, comprehensive health care that includes the steps described here to detect SCD early and reduce the likelihood of complications.4,5
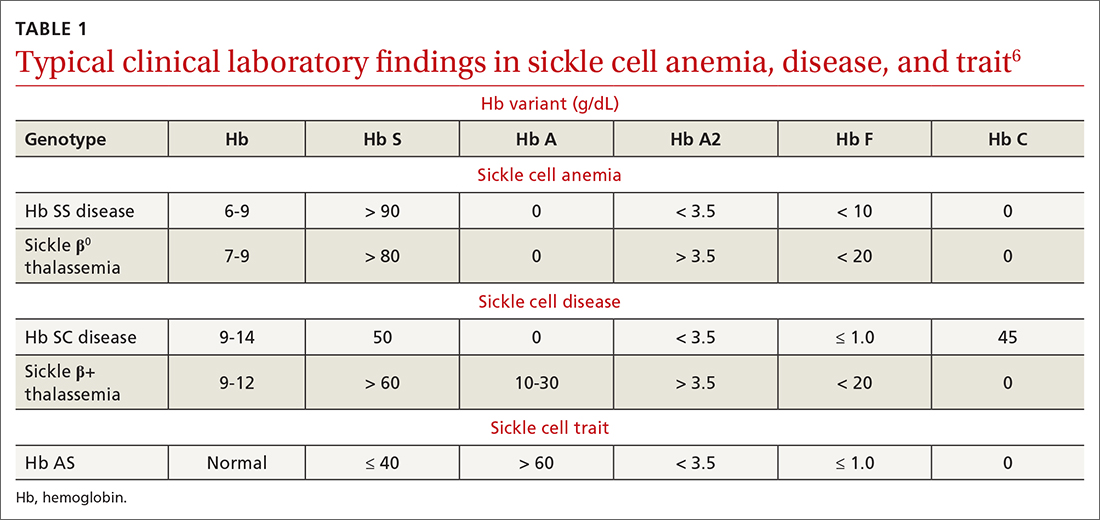
To begin, TABLE 16 lists typical laboratory findings and classifications in patients who are homozygous or heterozygous for Hb S, and therefore experience more severe Hb SS disease or milder SCD, respectively.
Who should be screened for hemoglobinopathy?
Because of the presence of the fetal Hb (Hb F) in newborns and infants, clinical signs of Hb SS before age 2 months are uncommon. Neonatal clinical laboratory testing is necessary for prompt identification of Hb SS; universal screening is now required by all states (although parents can opt out by claiming a religious exemption). A positive test result requires confirmatory testing: most often, Hb electrophoresis or DNA testing.
A confirmed positive homozygous (Hb SS) or heterozygous (Hb S) result is reported to the patient’s identified medical home for subsequent management. Thus, pediatric patients with SCD can be identified, and prophylactic treatment initiated, as early as possible. Later in the patient’s life, repeat screening for SCD and SCT is recommended at the initiation of pregnancy care7 and prior to the start of high-intensity physical training, as occurs in college and professional athletics and in certain branches of the military.8
Putting prevention into practice
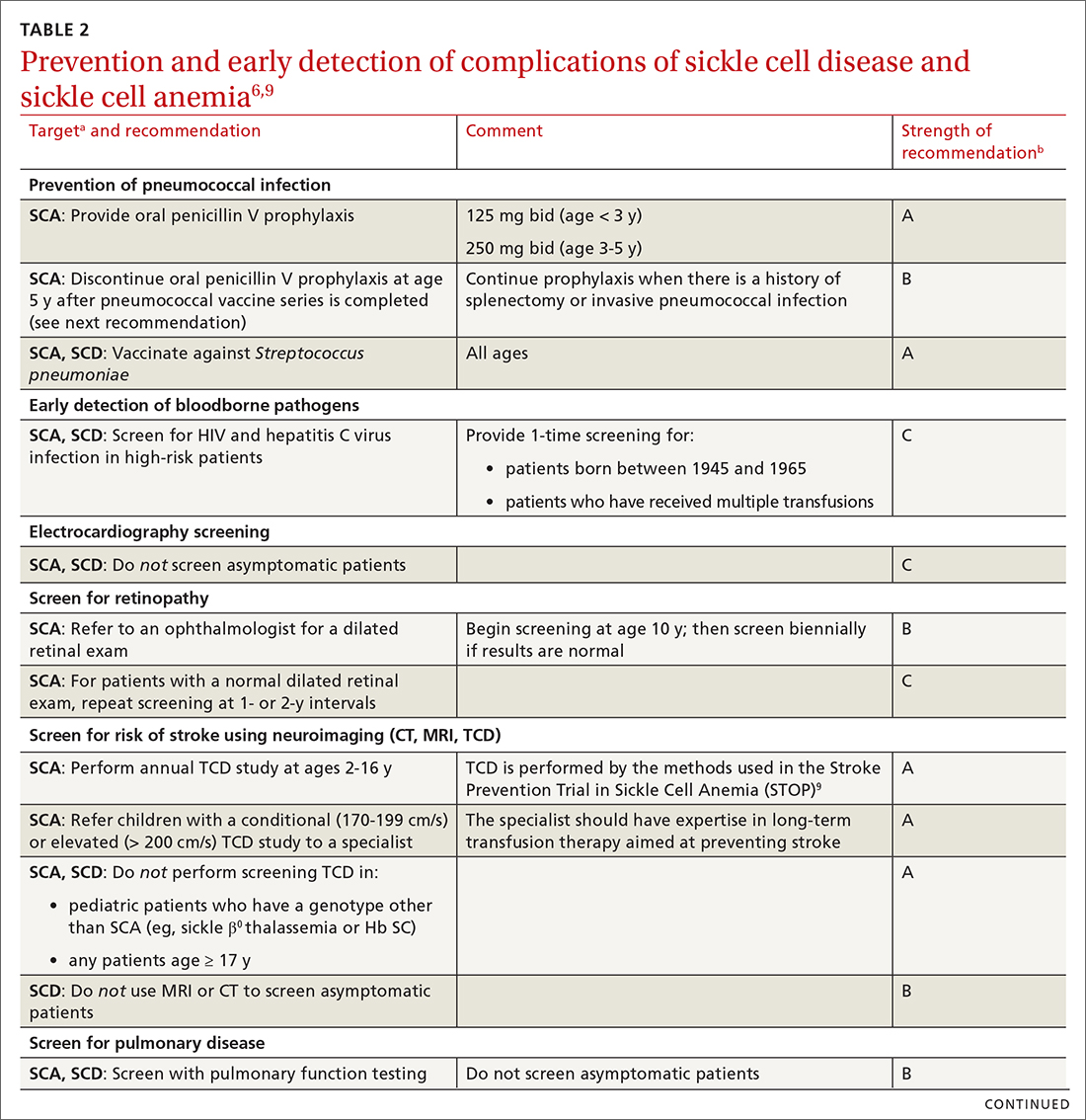
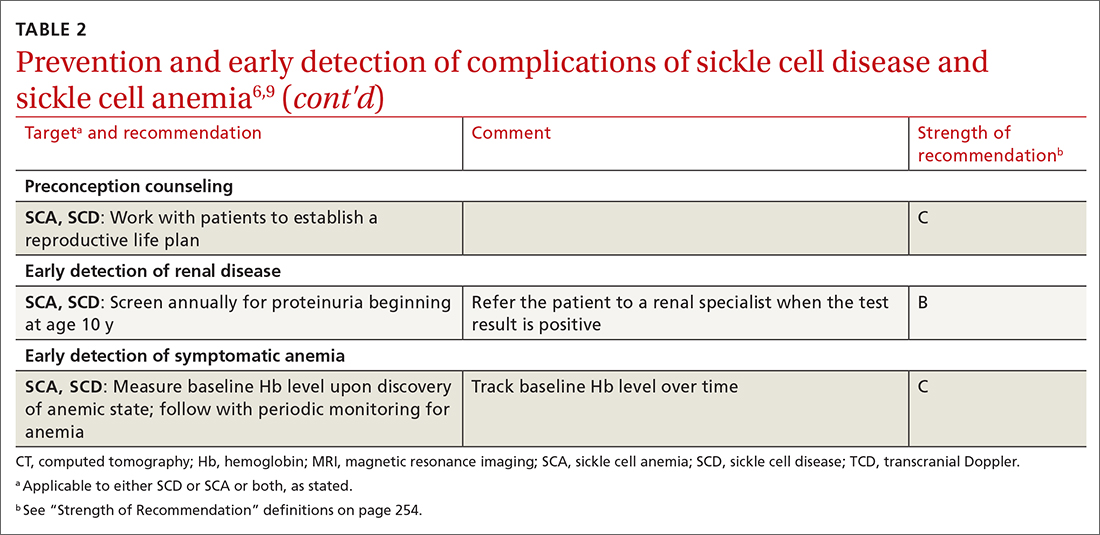
Some of the recommendations we make to prevent complications of SCD are directed only at patients with severe disease—ie, those who have Hb SS SCD or sickle β0 thalassemia (SCA); the rest apply to all patients with SCD (TABLE 26,9). (For patients with SCT, follow guidelines as you would for patients who do not have SCD, unless otherwise noted.)
Continue to: In addition, keep in mind...
In addition, keep in mind that preventive recommendations made by the US Preventive Services Task Force (Exhibit 5 in the Expert Panel Report)6 apply to all patients with SCD and SCT.
Prevention of invasive pneumococcal disease
All patients with SCD are assumed to have lifelong splenic dysfunction that begins in childhood. This is particularly true for those with SCA. In the absence of vaccination, the lifetime incidence of pneumococcal bacteremia resulting in serious complications is as high as 16% in SCD.10 In multiple randomized clinical trials, prophylactic penicillin dosing has proved beneficial in these patients, demonstrating a decrease in the risk of (1) pneumococcal infection and (2) early death during the study period, with minimal adverse effects.5
Prophylactic penicillin dosing should be initiated during infancy in patients with SCA. From ages 3 months to 3 years, the dosage of penicillin V is 125 mg twice daily; from 3 to 5 years, 250 mg twice daily. After age 5 years, the decision to continue penicillin is individualized, with consideration of prior severe pneumococcal infection and general preventive health maintenance. Penicillin-allergic patients can be given erythromycin. All patients with SCD who have had surgical splenectomy should be placed on antibiotic prophylaxis (ie, penicillin as dosed above).5
The polyvalent pneumococcal vaccine has resulted in significant protection against invasive pneumococcal disease; mortality from pneumococcal disease among patients with SCD who are younger than 14 years has decreased dramatically since the vaccine was introduced.6 For all patients with SCD, the standard PCV13 series should be administered beginning at age 6 weeks. A 2-dose series of the PPSV23 vaccine, which includes more Streptococcus pneumoniae serotypes than the PCV13 vaccine, should be administered beginning at age 2 years or 8 weeks after completion of the PCV13 series, whichever comes first.
Prevention of flu, COVID-19, and other vaccine-preventable illness
Influenza. Beginning at age 6 months, all patients with SCD should receive inactivated influenza vaccine annually at the beginning of the influenza season. Avoid using the live attenuated vaccine (Flumist) because of an associated increased risk of severe or complicated infection.11
Continue to: COVID-19, caused by severe...
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is especially problematic in patients with SCD12; infection causes mortality at a rate as high as 7%.5 The SARS-CoV-2 mRNA vaccine series is potentially lifesaving for these patients.12 In addition, at times of high community prevalence, make an effort to minimize patients’ exposure to SARS-CoV-2, by providing telemedicine visits.
Follow the immunization schedule. Patients with SCD should receive all standard recommended vaccinations (ie, those recommended by the Advisory Committee on Immunization Practices.a) Inactivated virus vaccines are preferred in SCD, when available. For patients who are behind on vaccinations, use a standard vaccine catch-up schedule.
Screening and prevention of complications such as stroke
Determining the risk of stroke. Patients with SCA who are not monitored have a 10% to 11% lifetime prevalence of stroke.5,6,10 An abnormal transcranial Doppler (TCD) study (defined as a time-averaged mean maximum velocity ≥ 200 cm/s in the distal internal carotid artery or proximal middle cerebral artery) is predictive of a 40% risk of stroke in patients with SCA. With chronic transfusion therapy, a 92% reduction in the risk of stroke is achievable.10
All patients with SCA should undergo annual screening with TCD ultrasonography from ages 2 to 16 years.6 Those who have an abnormal TCD study should receive chronic transfusion therapy. Screening is not recommended for patients with SCD or SCT.
Other complications. Screen and manage as follows:
- Proteinuria. Left untreated, SCD can affect the kidneys and lead to renal failure. Annual screening for proteinuria is recommended beginning at age 10 years, with referral when the test is positive and reproducible.
- Lung disease and cardiovascular disease. Screening for progression of lung disease and for cardiovascular disease is not recommended in asymptomatic patients with SCD, except through the history.
- Blood pressure screening and management of hypertension are based on Joint National Committee (JNC 8) guidelines.13
- Screening for ocular complications by an eye care provider is recommended beginning at age 10 years.
TABLE 26,9 summarizes recommendations on the prevention and early detection of complications of SCD.
Continue to: Pregnancy planning
Pregnancy planning
The Centers for Disease Control and Prevention recommends that a “reproductive life plan” be part of every person’s health journey (TABLE 2).6,9 The plan is especially relevant for female patients who have a known heritable concern, such as SCD, in which a pregnancy is more likely to be complicated by growth restriction, preterm delivery, and fetal demise. These risks are reduced—but not eliminated—with intensive surveillance of the pregnancy. Pregnancy in patients with SCD is also more likely to be complicated by preeclampsia, venous thromboembolism, infection, and maternal death.
Other recommendations:
- Every patient with SCD should receive genetic counselling before conceiving, when possible.
- Pregnancy should be considered high risk in women who have SCD, and monitored as such.
- Women with SCD can use any method of contraception—none of which put them at increased risk of complications, compared to the general population. Rather, it is pregnancy that puts them at greater risk of morbidity and mortality in every age group.
Ambulatory management of acute complications
Vaso-occlusive pain crisis. The hallmark of SCD is the acute pain crisis. Almost all patients with SCD (and the occasional patient with SCT) will experience a pain crisis. In more affluent countries, management of an acute pain crisis almost always includes opioid analgesia.6
For the most part, pain crises manifest in a predictable pattern. Although patients with SCD might have acute pain, other causes of acute pain, such as an acute intra-abdominal process or (in older patients) a cardiac process, should be considered as well.
For patients having a vaso-occlusive pain crisis, achieving rapid analgesia is key to management. Ready availability of narcotics, at home or under observation, prevents subsequent hospitalization; nonsteroidal anti-inflammatory drugs can be used as adjuvant treatment in patients without contraindications.5,6 An individualized treatment plan, including access to analgesia at an appropriate dosage, should be negotiated, and adhered to, by the patient and the care team.
Continue to: Rapid access to higher-level care...
Rapid access to higher-level care, including parenteral analgesia, is important if outpatient management is desired. In addition, escalation to a higher level of care should occur if there is hypoxia (or another reason to suspect acute chest syndrome [ACS; discussed in a bit]) or dehydration that requires parenteral therapy. Use of nondrug therapy, such as heat, should be encouraged. The care team should work with the patient’s school or employer to negotiate time away through the federal Family Medical Leave Act of 1993, or other means, because a pain crisis is not a planned event.
Fever. Because of the risk of serious infection as a consequence of functional asplenia, fever is particularly worrisome in patients with SCA and problematic in patients with SCD. The increased risk begins as the physiologic level of Hb F declines beginning at age 2 months.
ACS, characterized by a combination of respiratory symptoms or new infiltrates, often manifests initially with fever, and can progress rapidly to death if treatment is delayed. The initial signs and symptoms may be subtle; suspicion should remain high in any patient with respiratory symptoms who is newly hypoxic, even those who do not have fever. Osteomyelitis, another febrile illness, is also potentially life threatening if not treated promptly.
All patients with SCD whose body temperature is > 101.3 °F should be evaluated with appropriate clinical laboratory testing (complete blood count; inflammatory markers, such as C-reactive protein; basic chemistry parameters; and other tests as indicated, including serum lactate and urine culture), blood culture, and chest radiography. Empiric parenteral antibiotics are required until the patient is known to be nonbacteremic, regardless of vaccination status. Outpatient follow-up and even outpatient management with ceftriaxone can be offered in select circumstances (eg, if the patient so desires or is nontoxic, and if close follow-up can be assured).14 If ACS is a possibility based on symptoms or radiographic findings, outpatient management is not an option.
Anemia. Patients with SCA, and some with SCD, have an Hb level that is chronically, sometimes critically, low. A baseline Hb level should be established for a patient with SCD and then monitored periodically. A drop in the Hb level > 2 g/dL from baseline (or an initial Hb level of 6 g/dL if the baseline is unknown) constitutes acute anemia. Patients in whom anemia has been diagnosed should be emergently evaluated for acute splenic sequestration, an aplastic episode, a delayed hemolytic transfusion reaction, ACS, or infection, and should be treated appropriately.
Continue to: Simple transfusion can be used...
Simple transfusion can be used in an acute setting to restore and maintain Hb at a safe level. Iron overload and formation of RBC alloantigen are associated with multiple transfusions; once either of these conditions is established, subsequent transfusion therapy can be harmful. Care must be taken to prescribe transfusion appropriately; leukocyte-depleted RBCs should be used when available.
It is important to define specific goals of transfusion to optimize its use. Patients who have received multiple transfusions should have enhanced monitoring for bloodborne infection, such as hepatitis C virus. Acute aplastic crises are caused by parvovirus B19; when other members of the household who have SCD are present, they should be monitored for this viral infection with serial measurement of Hb and white blood cell count.6
Other acute problems. Should stroke, acute renal failure, priapism, or hepatobiliary complications develop, evaluate the patient rapidly and refer them to the appropriate care team for management.
Management of chronic complications
Chronic pain is a problem for many patients with SCD. The etiology of this symptom should be investigated fully because a vaso-occlusive crisis is characterized by acute pain. Avascular necrosis or ulcers due to chronic vaso-occlusion should be managed definitively when possible. Adjuvant therapy for chronic pain, such as heat or massage, should be encouraged.
In some patients, chronic pain without objective findings develops over time and becomes unresponsive to nonopioid pharmacotherapy. Such patients might require chronic opioid therapy, the need for which is dictated by the ability of the patient to perform their activities of daily living. For patients who require long-term daily narcotic drugs, best practices—obtaining informed consent, using registries and contracts, random drug testing, and providing naloxone [Narcan] for overdose emergency use—should be employed.15
Continue to: Chronic anemia
Chronic anemia can be managed with transfusion when elevating the Hb level is required (eg, preoperatively, to prevent stroke, to manage priapism). For some patients, ongoing transfusion is required; care should be taken to avoid iron overload and hemolysis due to antibody formation. Ongoing surveillance for these complications is required.6
Other chronic problems. Patients with SCD who develop avascular necrosis, vaso-occlusive ulcers, pulmonary hypertension, renal disease, recurrent priapism, or ophthalmologic complications should be co-managed with a care team.6
Pharmacotherapy and SCA
A principal goal in the management of patients with SCA is prevention of vaso-occlusive events, including ACS and acute pain crises.
Hydroxyurea, a key component of SCA treatment, is a ribonucleotide reductase inhibitor that increases the level of Hb F, thus reducing the absolute number of symptomatic vaso-occlusive events and increasing arterial blood flow. It is most useful for patients who have multiple crises. The drug prolongs survival and reduces the need for transfusion and hospitalization.4,5
Hydroxyurea can be started in patients at age 9 months; blood testing should be performed at the start of treatment and the dosage titrated based on blood counts. Initial blood work includes:
- Hb level;
- Hb electrophoresis with the quantitative percentage of Hb F;
- complete blood count with differential and reticulocyte counts;
- chemistry profile (electrolytes, lactate dehydrogenase, total protein, albumin, total bilirubin);
- liver function tests (aspartate aminotransferase, alanine aminotransferase);
- measurement of renal function (blood urea nitrogen, creatinine);
- serum vitamin B12 and folate;
- serum iron, total iron-binding capacity, and ferritin;
- hepatitis B, hepatitis C, and parvovirus B19 antigen; and
- serologic testing for HIV.
Continue to: Testing should also...
Testing should also include a pregnancy test for postmenarchal females because hydroxyurea is in US Food and Drug Administration pregnancy risk category X.
Avoid hydroxyurea in lactating women; dose the drug renally in the setting of renal disease. Because hydroxyurea has a high rate of serious adverse effects and drug-drug interactions, it should be offered in conjunction with an individualized care plan.
Hydroxyurea can also be offered to patients with other forms of SCD who have recurrent vaso-occlusive symptoms.
Two newer medications improve oxygen delivery in patients with SCD. Voxelotor, approved in 2019, works to reduce Hb S polymerization by binding to the alpha chain of Hb S and, subsequently, increasing its oxygen affinity. The drug is generally well tolerated and can be used in patients with SCD who are ≥ 12 years.16 Crizanlizumab is a monoclonal antibody directed against P-selectin, an adhesion molecule located on endothelial cells and activated platelets. The efficacy of crizanlizumab was demonstrated in the SUSTAIN trial, in which it reduced vaso-occlusive pain in patients ≥ 16 years.17
All of these medications have a narrow toxic–therapeutic window. They should therefore be administered with the participation of a multidisciplinary care team.
Continue to: The need to coordinated, comprehensive care
The need for coordinated, comprehensive care
Patients with SCD report how challenging their disease is. All patients with SCD are more likely than age-matched counterparts to experience loss, including workdays for disability, educational potential, workdays for caregivers of affected children, and time spent in the hospital or the emergency department.4,5 These losses, with the concomitant stress associated with chronic illness and the struggle to manage recurrent pain crises and chronic complications, are often overwhelming.
Comprehensive care can, as we have illustrated in this discussion, mitigate these losses. Such care should include extensive education, genetic counseling, infection prevention, pain management, and implementation of evidence-based management guidelines.3,4,6 Patients with SCD report that their illness outlook would be better with
- greater provider knowledge of SCD,
- destigmatization of narcotics for SCD vaso-occlusive pain management,
- optimal coordination among members of the health care team, and
- improved transportation for appointments.
Patients also report that barriers associated with the unique US health care financing system are often insurmountable. As patients with SCD live longer, improved care management should focus on reducing these barriers and enhancing their quality of life.2,18,19
CORRESPONDENCE
Robert Allen Perkins, MD, MPH, Department of Family Medicine, University of South Alabama College of Medicine, 1601 Center Street, 2N, Mobile, AL 36604; perkins@health. southalabama.edu
1. Lubeck D, Agodoa I, Bhakta N, et al. Estimated life expectancy and income of patients with sickle cell disease compared with those without sickle cell disease. JAMA Netw Open. 2019;2:e1915374. doi:10.1001/jamanetworkopen.2019.15374
2. Swanson ME, Grosse SD, Kulkarni R. Disability among individuals with sickle cell disease: literature review from a public health perspective. Am J Prev Med. 2011;41(6 suppl 4):S390-S397. doi: 10.1016/j.amepre.2011.09.006
3. Moskowitz JT, Butensky E, Harmatz P, et al. Caregiving time in sickle cell disease: psychological effects in maternal caregivers. Pediatr Blood Cancer. 2007;48:64-71. doi:10.1002/pbc.20792
4. Mehta SR, Afenyi-Annan A, Lottenberg R. Opportunities to improve outcomes in sickle cell disease. Am Fam Phys. 2006;74:303-310.
5. Yawn BP, John-Sowah J. Management of sickle cell disease: recommendations from the 2014 Expert Panel Report. Am Fam Phys. 2015;92:1069-1077.
6. National Heart, Lung, and Blood Institute, National Institutes of Health. Evidence-based management of sickle cell disease. Expert Panel Report, 2014. Accessed June 9, 2022. www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines
7. Committee Opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40. doi: 10.1097/AOG.0000000000001951
8. Jordan LB, Smith-Whitley K, Treadwell MJ, et al. Screening U.S. college athletes for their sickle cell disease carrier status. Am J Prev Med. 2011;41:S406-S412. doi: 10.1016/j.amepre.2011.09.014
9. Adams RJ, McKie VC, Brambilla D, et al. Stroke prevention trial in sickle cell anemia. Control Clin Trials. 1998;19:110-129. doi: 10.1016/s0197-2456(97)00099-8
10. Alzahrani F, Alaidarous K, Alqarni S, et al. Incidence and predictors of bacterial infections in febrile children with sickle cell disease. Int J Pediatr Adolesc Med. 2021;8:236-238 doi: 10.1016/j.ijpam.2020.12.005
11. Committee on Infectious Diseases. Recommendations for prevention and control of influenza in children, 2021-2022. Pediatrics. 2021;148: e2021053745. doi: 10.1542/peds.2021-053745
12. Centers for Disease Control and Prevention. Study finds people with sickle cell disease who developed coronavirus disease have high rates of hospitalization, intensive care unit admission, and death. October 20, 2020. Accessed June 9, 2022. www.cdc.gov/ncbddd/sicklecell/features/scd-and-covid-19.html
13. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
14. Baskin MN, Goh XL, Heeney MM, et al. Bacteremia risk and outpatient management of febrile patients with sickle cell disease. Pediatrics. 2013;131:1035-1041. doi: 10.1542/peds.2012-2139
15. Osunkwo I, Veeramreddy P, Arnall J, et al. Use of buprenorphine/naloxone in amelio rating acute care utilization and chronic opioid use in adults with sickle cell disease. Blood. 2019;134 (suppl 1):790. doi: 10.1182/blood-2019-126589
16. Vichinsky E, Hoppe CC, Ataga KI, et al; HOPE Trial Investigators. A phase 3 randomized trial of voxelotor in sickle cell disease. N Engl J Med. 2019;381:509-519. doi: 10.1056/NEJMoa1903212
17. Ataga KI, Kutlar A, Kanter J, et al. Crizanlizumab for the prevention of pain crises in sickle cell disease. N Engl J Med. 2017;376:429-439. doi: 10.1056/NEJMoa1611770
18. Dixit R, Nettem S, Madan SS, et al. Folate supplementation in people with sickle cell disease. Cochrane Database Syst Rev. 2016;2:CD011130. doi: 10.1002/14651858.CD011130.pub2
19. Brennan-Cook J, Bonnabeau E, Aponte R, et al. Barriers to care for persons with sickle cell disease: the case manager’s opportunity to improve patient outcomes. Prof Case Manag. 2018;23:213-219. doi: 10.1097/NCM.0000000000000260
The group of disorders known as sickle cell disease (SCD) is one of the more common genetic hemoglobinopathies. Homozygous production of the S variant of hemoglobin (Hb) in red blood cells (RBCs) results in profound sickling under conditions of physiologic stress, a condition known as Hb SS disease. People with Hb SS disease are at risk of chronic hemolytic anemia, tissue ischemia that causes vaso-occlusive pain syndrome, and other vaso-occlusive complications.1 They also experience a > 20-year reduction in life expectancy, compared to age-matched controls; onset of risk of early death is usually after age 25 years.
People with heterozygous expression of the Hb S variant—that is, from one parent, and expression of Hb A from the other parent—are said to have sickle cell trait (SCT). They typically do not have symptoms of SCD, although they can experience vaso-occlusive pain under severe physiologic stress and suffer sudden death more often than age-matched controls. People who are heterozygous for Hb S but have another hemoglobinopathy (eg,
Alleviating the harsh burden of illness. All patients with SCD are more likely than age-matched counterparts to experience income loss because of their disability; the same loss is true for their caregivers. Such loss, when combined with time spent in the health care system, can be catastrophic.2,3 But this loss can be mitigated with access to regular, comprehensive health care that includes the steps described here to detect SCD early and reduce the likelihood of complications.4,5
To begin, TABLE 16 lists typical laboratory findings and classifications in patients who are homozygous or heterozygous for Hb S, and therefore experience more severe Hb SS disease or milder SCD, respectively.
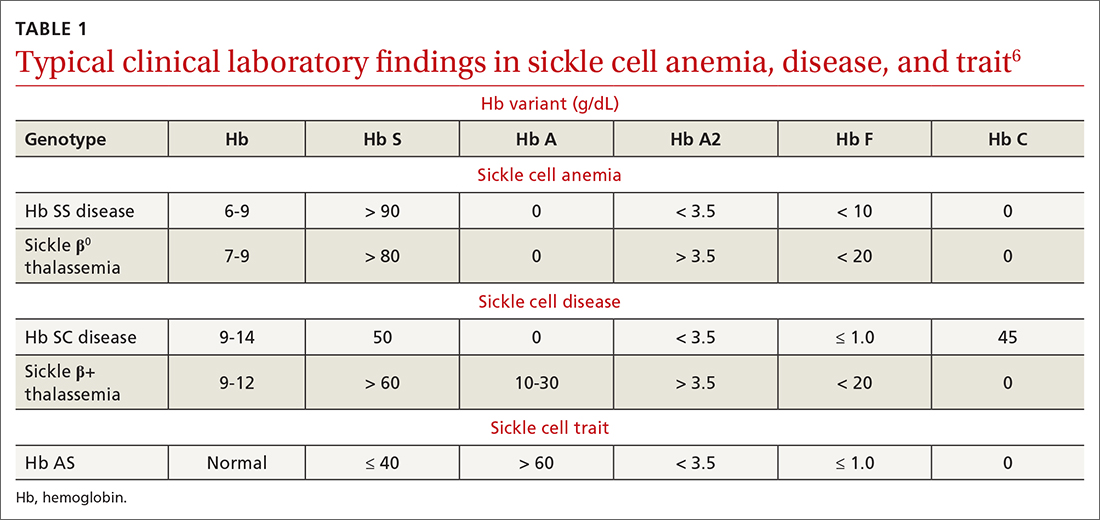
Who should be screened for hemoglobinopathy?
Because of the presence of the fetal Hb (Hb F) in newborns and infants, clinical signs of Hb SS before age 2 months are uncommon. Neonatal clinical laboratory testing is necessary for prompt identification of Hb SS; universal screening is now required by all states (although parents can opt out by claiming a religious exemption). A positive test result requires confirmatory testing: most often, Hb electrophoresis or DNA testing.
A confirmed positive homozygous (Hb SS) or heterozygous (Hb S) result is reported to the patient’s identified medical home for subsequent management. Thus, pediatric patients with SCD can be identified, and prophylactic treatment initiated, as early as possible. Later in the patient’s life, repeat screening for SCD and SCT is recommended at the initiation of pregnancy care7 and prior to the start of high-intensity physical training, as occurs in college and professional athletics and in certain branches of the military.8
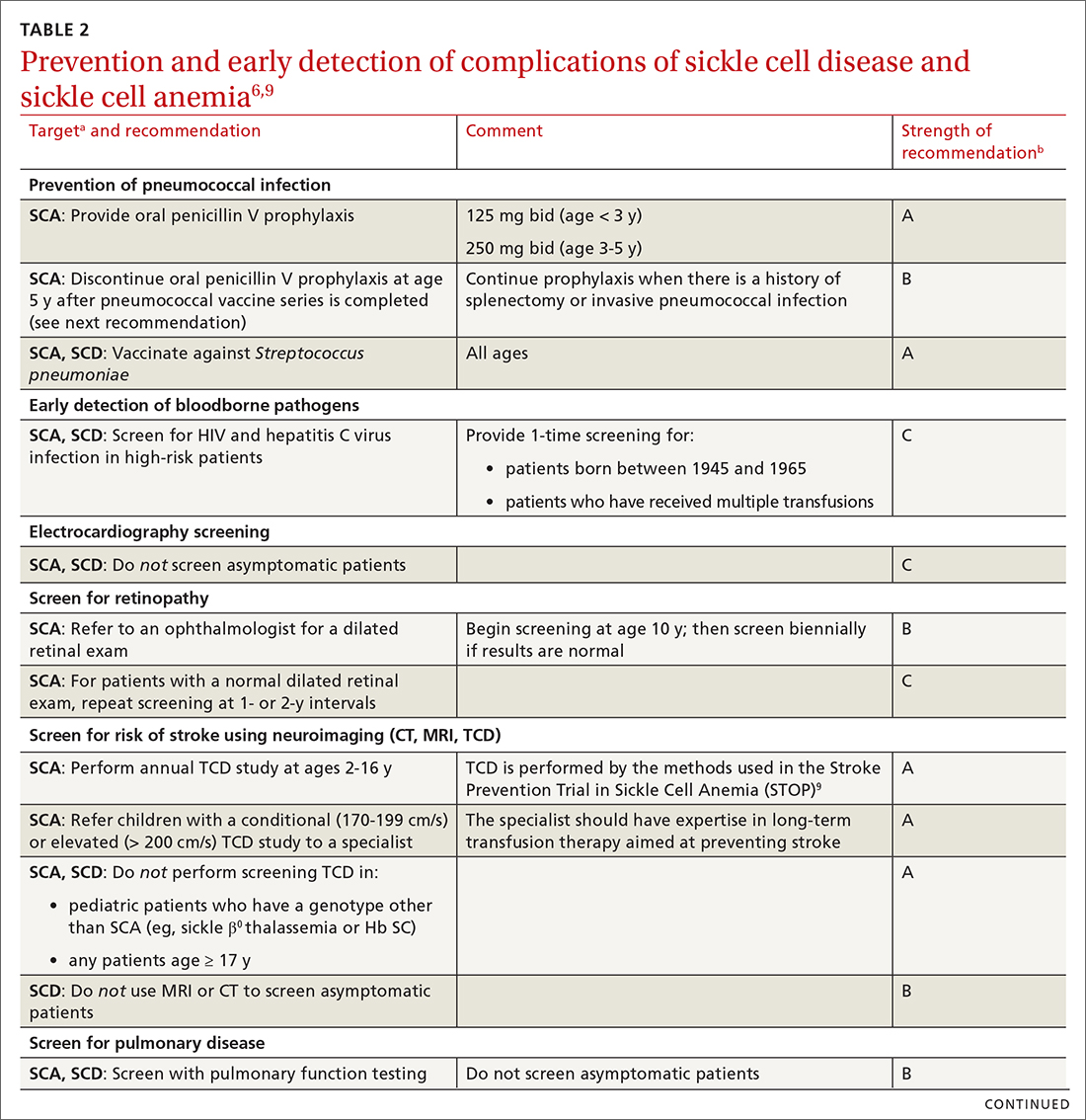
Putting prevention into practice
Some of the recommendations we make to prevent complications of SCD are directed only at patients with severe disease—ie, those who have Hb SS SCD or sickle β0 thalassemia (SCA); the rest apply to all patients with SCD (TABLE 26,9). (For patients with SCT, follow guidelines as you would for patients who do not have SCD, unless otherwise noted.)
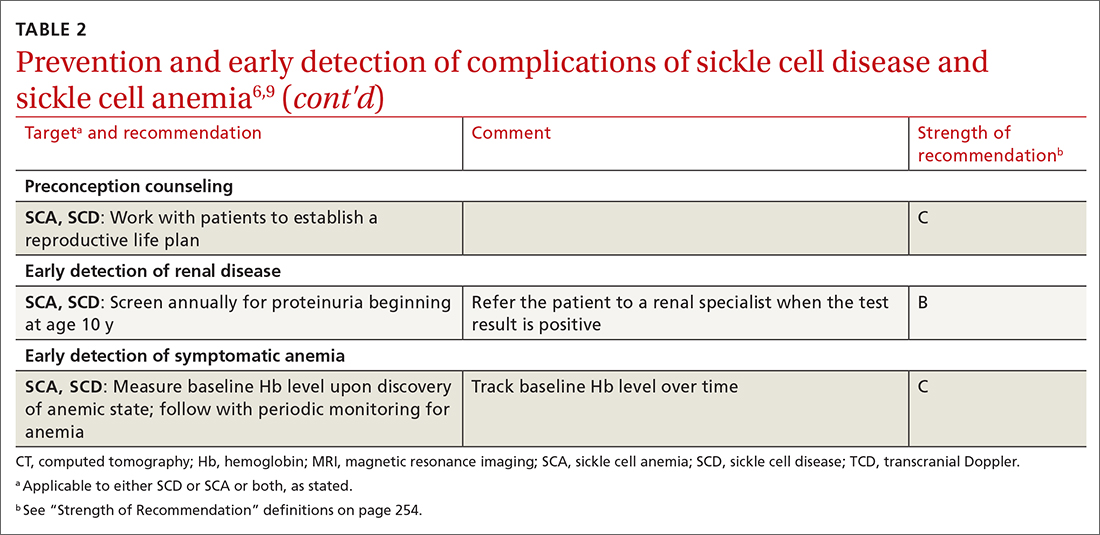
Continue to: In addition, keep in mind...
In addition, keep in mind that preventive recommendations made by the US Preventive Services Task Force (Exhibit 5 in the Expert Panel Report)6 apply to all patients with SCD and SCT.
Prevention of invasive pneumococcal disease
All patients with SCD are assumed to have lifelong splenic dysfunction that begins in childhood. This is particularly true for those with SCA. In the absence of vaccination, the lifetime incidence of pneumococcal bacteremia resulting in serious complications is as high as 16% in SCD.10 In multiple randomized clinical trials, prophylactic penicillin dosing has proved beneficial in these patients, demonstrating a decrease in the risk of (1) pneumococcal infection and (2) early death during the study period, with minimal adverse effects.5
Prophylactic penicillin dosing should be initiated during infancy in patients with SCA. From ages 3 months to 3 years, the dosage of penicillin V is 125 mg twice daily; from 3 to 5 years, 250 mg twice daily. After age 5 years, the decision to continue penicillin is individualized, with consideration of prior severe pneumococcal infection and general preventive health maintenance. Penicillin-allergic patients can be given erythromycin. All patients with SCD who have had surgical splenectomy should be placed on antibiotic prophylaxis (ie, penicillin as dosed above).5
The polyvalent pneumococcal vaccine has resulted in significant protection against invasive pneumococcal disease; mortality from pneumococcal disease among patients with SCD who are younger than 14 years has decreased dramatically since the vaccine was introduced.6 For all patients with SCD, the standard PCV13 series should be administered beginning at age 6 weeks. A 2-dose series of the PPSV23 vaccine, which includes more Streptococcus pneumoniae serotypes than the PCV13 vaccine, should be administered beginning at age 2 years or 8 weeks after completion of the PCV13 series, whichever comes first.
Prevention of flu, COVID-19, and other vaccine-preventable illness
Influenza. Beginning at age 6 months, all patients with SCD should receive inactivated influenza vaccine annually at the beginning of the influenza season. Avoid using the live attenuated vaccine (Flumist) because of an associated increased risk of severe or complicated infection.11
Continue to: COVID-19, caused by severe...
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is especially problematic in patients with SCD12; infection causes mortality at a rate as high as 7%.5 The SARS-CoV-2 mRNA vaccine series is potentially lifesaving for these patients.12 In addition, at times of high community prevalence, make an effort to minimize patients’ exposure to SARS-CoV-2, by providing telemedicine visits.
Follow the immunization schedule. Patients with SCD should receive all standard recommended vaccinations (ie, those recommended by the Advisory Committee on Immunization Practices.a) Inactivated virus vaccines are preferred in SCD, when available. For patients who are behind on vaccinations, use a standard vaccine catch-up schedule.
Screening and prevention of complications such as stroke
Determining the risk of stroke. Patients with SCA who are not monitored have a 10% to 11% lifetime prevalence of stroke.5,6,10 An abnormal transcranial Doppler (TCD) study (defined as a time-averaged mean maximum velocity ≥ 200 cm/s in the distal internal carotid artery or proximal middle cerebral artery) is predictive of a 40% risk of stroke in patients with SCA. With chronic transfusion therapy, a 92% reduction in the risk of stroke is achievable.10
All patients with SCA should undergo annual screening with TCD ultrasonography from ages 2 to 16 years.6 Those who have an abnormal TCD study should receive chronic transfusion therapy. Screening is not recommended for patients with SCD or SCT.
Other complications. Screen and manage as follows:
- Proteinuria. Left untreated, SCD can affect the kidneys and lead to renal failure. Annual screening for proteinuria is recommended beginning at age 10 years, with referral when the test is positive and reproducible.
- Lung disease and cardiovascular disease. Screening for progression of lung disease and for cardiovascular disease is not recommended in asymptomatic patients with SCD, except through the history.
- Blood pressure screening and management of hypertension are based on Joint National Committee (JNC 8) guidelines.13
- Screening for ocular complications by an eye care provider is recommended beginning at age 10 years.
TABLE 26,9 summarizes recommendations on the prevention and early detection of complications of SCD.
Continue to: Pregnancy planning
Pregnancy planning
The Centers for Disease Control and Prevention recommends that a “reproductive life plan” be part of every person’s health journey (TABLE 2).6,9 The plan is especially relevant for female patients who have a known heritable concern, such as SCD, in which a pregnancy is more likely to be complicated by growth restriction, preterm delivery, and fetal demise. These risks are reduced—but not eliminated—with intensive surveillance of the pregnancy. Pregnancy in patients with SCD is also more likely to be complicated by preeclampsia, venous thromboembolism, infection, and maternal death.
Other recommendations:
- Every patient with SCD should receive genetic counselling before conceiving, when possible.
- Pregnancy should be considered high risk in women who have SCD, and monitored as such.
- Women with SCD can use any method of contraception—none of which put them at increased risk of complications, compared to the general population. Rather, it is pregnancy that puts them at greater risk of morbidity and mortality in every age group.
Ambulatory management of acute complications
Vaso-occlusive pain crisis. The hallmark of SCD is the acute pain crisis. Almost all patients with SCD (and the occasional patient with SCT) will experience a pain crisis. In more affluent countries, management of an acute pain crisis almost always includes opioid analgesia.6
For the most part, pain crises manifest in a predictable pattern. Although patients with SCD might have acute pain, other causes of acute pain, such as an acute intra-abdominal process or (in older patients) a cardiac process, should be considered as well.
For patients having a vaso-occlusive pain crisis, achieving rapid analgesia is key to management. Ready availability of narcotics, at home or under observation, prevents subsequent hospitalization; nonsteroidal anti-inflammatory drugs can be used as adjuvant treatment in patients without contraindications.5,6 An individualized treatment plan, including access to analgesia at an appropriate dosage, should be negotiated, and adhered to, by the patient and the care team.
Continue to: Rapid access to higher-level care...
Rapid access to higher-level care, including parenteral analgesia, is important if outpatient management is desired. In addition, escalation to a higher level of care should occur if there is hypoxia (or another reason to suspect acute chest syndrome [ACS; discussed in a bit]) or dehydration that requires parenteral therapy. Use of nondrug therapy, such as heat, should be encouraged. The care team should work with the patient’s school or employer to negotiate time away through the federal Family Medical Leave Act of 1993, or other means, because a pain crisis is not a planned event.
Fever. Because of the risk of serious infection as a consequence of functional asplenia, fever is particularly worrisome in patients with SCA and problematic in patients with SCD. The increased risk begins as the physiologic level of Hb F declines beginning at age 2 months.
ACS, characterized by a combination of respiratory symptoms or new infiltrates, often manifests initially with fever, and can progress rapidly to death if treatment is delayed. The initial signs and symptoms may be subtle; suspicion should remain high in any patient with respiratory symptoms who is newly hypoxic, even those who do not have fever. Osteomyelitis, another febrile illness, is also potentially life threatening if not treated promptly.
All patients with SCD whose body temperature is > 101.3 °F should be evaluated with appropriate clinical laboratory testing (complete blood count; inflammatory markers, such as C-reactive protein; basic chemistry parameters; and other tests as indicated, including serum lactate and urine culture), blood culture, and chest radiography. Empiric parenteral antibiotics are required until the patient is known to be nonbacteremic, regardless of vaccination status. Outpatient follow-up and even outpatient management with ceftriaxone can be offered in select circumstances (eg, if the patient so desires or is nontoxic, and if close follow-up can be assured).14 If ACS is a possibility based on symptoms or radiographic findings, outpatient management is not an option.
Anemia. Patients with SCA, and some with SCD, have an Hb level that is chronically, sometimes critically, low. A baseline Hb level should be established for a patient with SCD and then monitored periodically. A drop in the Hb level > 2 g/dL from baseline (or an initial Hb level of 6 g/dL if the baseline is unknown) constitutes acute anemia. Patients in whom anemia has been diagnosed should be emergently evaluated for acute splenic sequestration, an aplastic episode, a delayed hemolytic transfusion reaction, ACS, or infection, and should be treated appropriately.
Continue to: Simple transfusion can be used...
Simple transfusion can be used in an acute setting to restore and maintain Hb at a safe level. Iron overload and formation of RBC alloantigen are associated with multiple transfusions; once either of these conditions is established, subsequent transfusion therapy can be harmful. Care must be taken to prescribe transfusion appropriately; leukocyte-depleted RBCs should be used when available.
It is important to define specific goals of transfusion to optimize its use. Patients who have received multiple transfusions should have enhanced monitoring for bloodborne infection, such as hepatitis C virus. Acute aplastic crises are caused by parvovirus B19; when other members of the household who have SCD are present, they should be monitored for this viral infection with serial measurement of Hb and white blood cell count.6
Other acute problems. Should stroke, acute renal failure, priapism, or hepatobiliary complications develop, evaluate the patient rapidly and refer them to the appropriate care team for management.
Management of chronic complications
Chronic pain is a problem for many patients with SCD. The etiology of this symptom should be investigated fully because a vaso-occlusive crisis is characterized by acute pain. Avascular necrosis or ulcers due to chronic vaso-occlusion should be managed definitively when possible. Adjuvant therapy for chronic pain, such as heat or massage, should be encouraged.
In some patients, chronic pain without objective findings develops over time and becomes unresponsive to nonopioid pharmacotherapy. Such patients might require chronic opioid therapy, the need for which is dictated by the ability of the patient to perform their activities of daily living. For patients who require long-term daily narcotic drugs, best practices—obtaining informed consent, using registries and contracts, random drug testing, and providing naloxone [Narcan] for overdose emergency use—should be employed.15
Continue to: Chronic anemia
Chronic anemia can be managed with transfusion when elevating the Hb level is required (eg, preoperatively, to prevent stroke, to manage priapism). For some patients, ongoing transfusion is required; care should be taken to avoid iron overload and hemolysis due to antibody formation. Ongoing surveillance for these complications is required.6
Other chronic problems. Patients with SCD who develop avascular necrosis, vaso-occlusive ulcers, pulmonary hypertension, renal disease, recurrent priapism, or ophthalmologic complications should be co-managed with a care team.6
Pharmacotherapy and SCA
A principal goal in the management of patients with SCA is prevention of vaso-occlusive events, including ACS and acute pain crises.
Hydroxyurea, a key component of SCA treatment, is a ribonucleotide reductase inhibitor that increases the level of Hb F, thus reducing the absolute number of symptomatic vaso-occlusive events and increasing arterial blood flow. It is most useful for patients who have multiple crises. The drug prolongs survival and reduces the need for transfusion and hospitalization.4,5
Hydroxyurea can be started in patients at age 9 months; blood testing should be performed at the start of treatment and the dosage titrated based on blood counts. Initial blood work includes:
- Hb level;
- Hb electrophoresis with the quantitative percentage of Hb F;
- complete blood count with differential and reticulocyte counts;
- chemistry profile (electrolytes, lactate dehydrogenase, total protein, albumin, total bilirubin);
- liver function tests (aspartate aminotransferase, alanine aminotransferase);
- measurement of renal function (blood urea nitrogen, creatinine);
- serum vitamin B12 and folate;
- serum iron, total iron-binding capacity, and ferritin;
- hepatitis B, hepatitis C, and parvovirus B19 antigen; and
- serologic testing for HIV.
Continue to: Testing should also...
Testing should also include a pregnancy test for postmenarchal females because hydroxyurea is in US Food and Drug Administration pregnancy risk category X.
Avoid hydroxyurea in lactating women; dose the drug renally in the setting of renal disease. Because hydroxyurea has a high rate of serious adverse effects and drug-drug interactions, it should be offered in conjunction with an individualized care plan.
Hydroxyurea can also be offered to patients with other forms of SCD who have recurrent vaso-occlusive symptoms.
Two newer medications improve oxygen delivery in patients with SCD. Voxelotor, approved in 2019, works to reduce Hb S polymerization by binding to the alpha chain of Hb S and, subsequently, increasing its oxygen affinity. The drug is generally well tolerated and can be used in patients with SCD who are ≥ 12 years.16 Crizanlizumab is a monoclonal antibody directed against P-selectin, an adhesion molecule located on endothelial cells and activated platelets. The efficacy of crizanlizumab was demonstrated in the SUSTAIN trial, in which it reduced vaso-occlusive pain in patients ≥ 16 years.17
All of these medications have a narrow toxic–therapeutic window. They should therefore be administered with the participation of a multidisciplinary care team.
Continue to: The need to coordinated, comprehensive care
The need for coordinated, comprehensive care
Patients with SCD report how challenging their disease is. All patients with SCD are more likely than age-matched counterparts to experience loss, including workdays for disability, educational potential, workdays for caregivers of affected children, and time spent in the hospital or the emergency department.4,5 These losses, with the concomitant stress associated with chronic illness and the struggle to manage recurrent pain crises and chronic complications, are often overwhelming.
Comprehensive care can, as we have illustrated in this discussion, mitigate these losses. Such care should include extensive education, genetic counseling, infection prevention, pain management, and implementation of evidence-based management guidelines.3,4,6 Patients with SCD report that their illness outlook would be better with
- greater provider knowledge of SCD,
- destigmatization of narcotics for SCD vaso-occlusive pain management,
- optimal coordination among members of the health care team, and
- improved transportation for appointments.
Patients also report that barriers associated with the unique US health care financing system are often insurmountable. As patients with SCD live longer, improved care management should focus on reducing these barriers and enhancing their quality of life.2,18,19
CORRESPONDENCE
Robert Allen Perkins, MD, MPH, Department of Family Medicine, University of South Alabama College of Medicine, 1601 Center Street, 2N, Mobile, AL 36604; perkins@health. southalabama.edu
The group of disorders known as sickle cell disease (SCD) is one of the more common genetic hemoglobinopathies. Homozygous production of the S variant of hemoglobin (Hb) in red blood cells (RBCs) results in profound sickling under conditions of physiologic stress, a condition known as Hb SS disease. People with Hb SS disease are at risk of chronic hemolytic anemia, tissue ischemia that causes vaso-occlusive pain syndrome, and other vaso-occlusive complications.1 They also experience a > 20-year reduction in life expectancy, compared to age-matched controls; onset of risk of early death is usually after age 25 years.
People with heterozygous expression of the Hb S variant—that is, from one parent, and expression of Hb A from the other parent—are said to have sickle cell trait (SCT). They typically do not have symptoms of SCD, although they can experience vaso-occlusive pain under severe physiologic stress and suffer sudden death more often than age-matched controls. People who are heterozygous for Hb S but have another hemoglobinopathy (eg,
Alleviating the harsh burden of illness. All patients with SCD are more likely than age-matched counterparts to experience income loss because of their disability; the same loss is true for their caregivers. Such loss, when combined with time spent in the health care system, can be catastrophic.2,3 But this loss can be mitigated with access to regular, comprehensive health care that includes the steps described here to detect SCD early and reduce the likelihood of complications.4,5
To begin, TABLE 16 lists typical laboratory findings and classifications in patients who are homozygous or heterozygous for Hb S, and therefore experience more severe Hb SS disease or milder SCD, respectively.
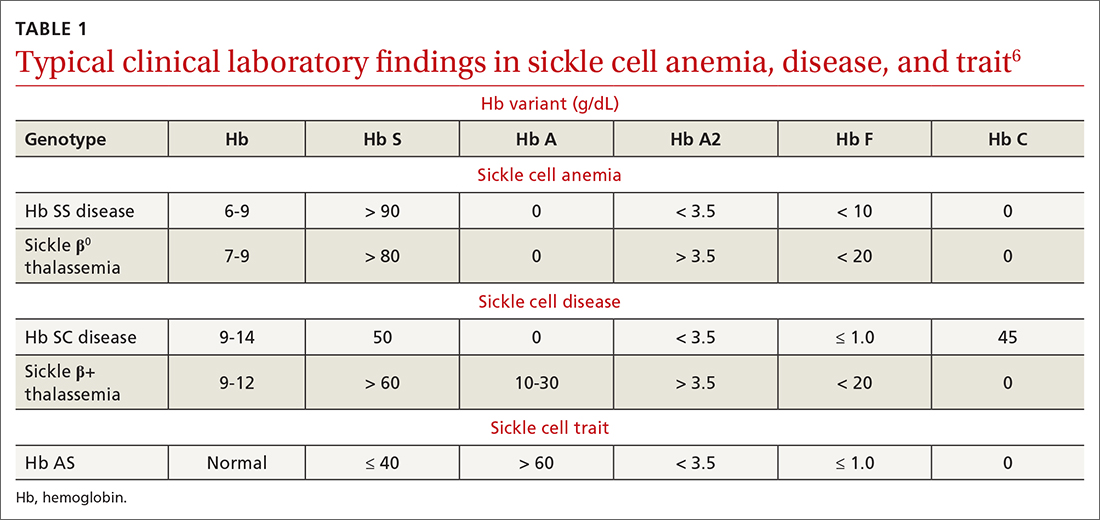
Who should be screened for hemoglobinopathy?
Because of the presence of the fetal Hb (Hb F) in newborns and infants, clinical signs of Hb SS before age 2 months are uncommon. Neonatal clinical laboratory testing is necessary for prompt identification of Hb SS; universal screening is now required by all states (although parents can opt out by claiming a religious exemption). A positive test result requires confirmatory testing: most often, Hb electrophoresis or DNA testing.
A confirmed positive homozygous (Hb SS) or heterozygous (Hb S) result is reported to the patient’s identified medical home for subsequent management. Thus, pediatric patients with SCD can be identified, and prophylactic treatment initiated, as early as possible. Later in the patient’s life, repeat screening for SCD and SCT is recommended at the initiation of pregnancy care7 and prior to the start of high-intensity physical training, as occurs in college and professional athletics and in certain branches of the military.8
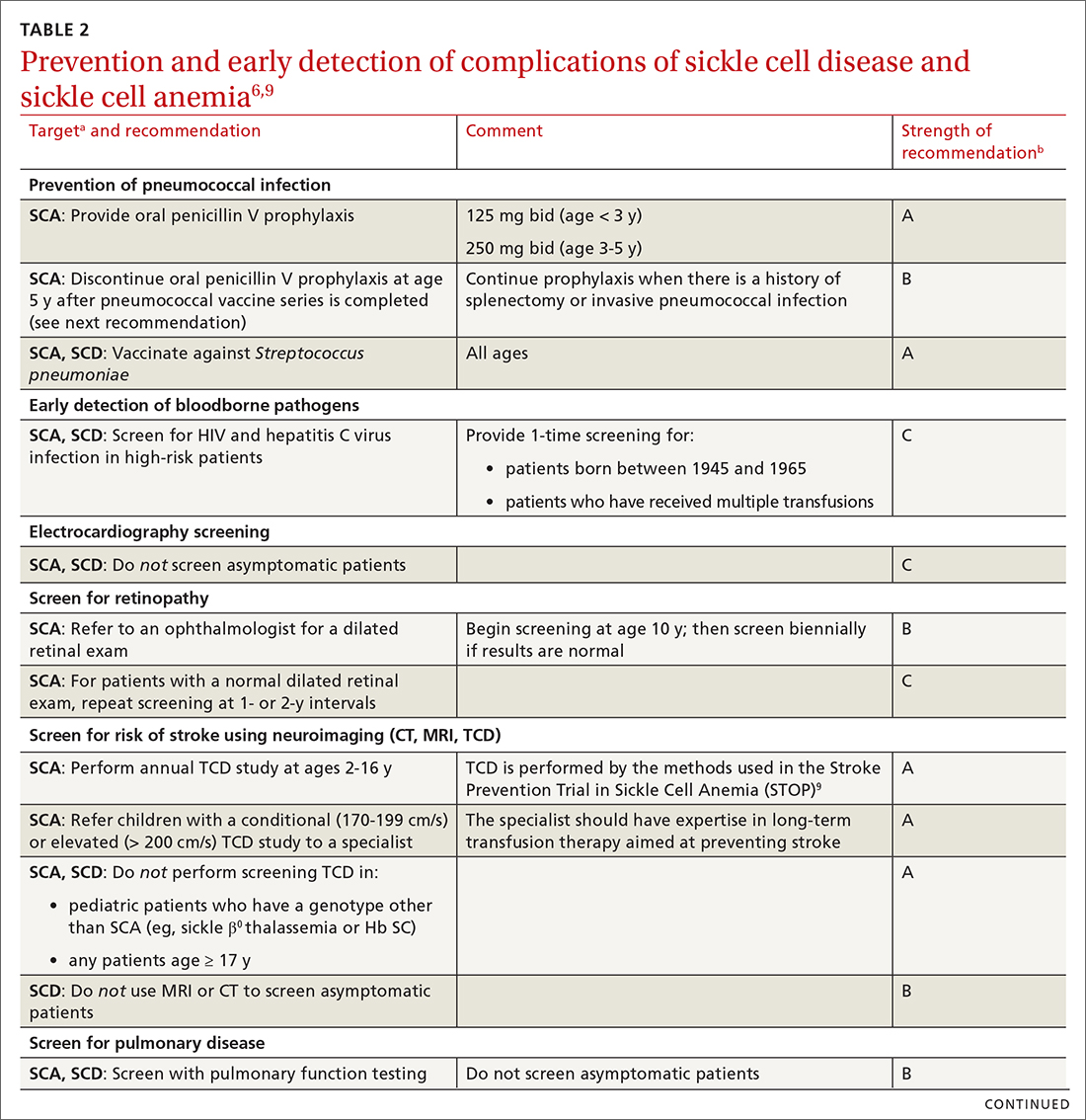
Putting prevention into practice
Some of the recommendations we make to prevent complications of SCD are directed only at patients with severe disease—ie, those who have Hb SS SCD or sickle β0 thalassemia (SCA); the rest apply to all patients with SCD (TABLE 26,9). (For patients with SCT, follow guidelines as you would for patients who do not have SCD, unless otherwise noted.)
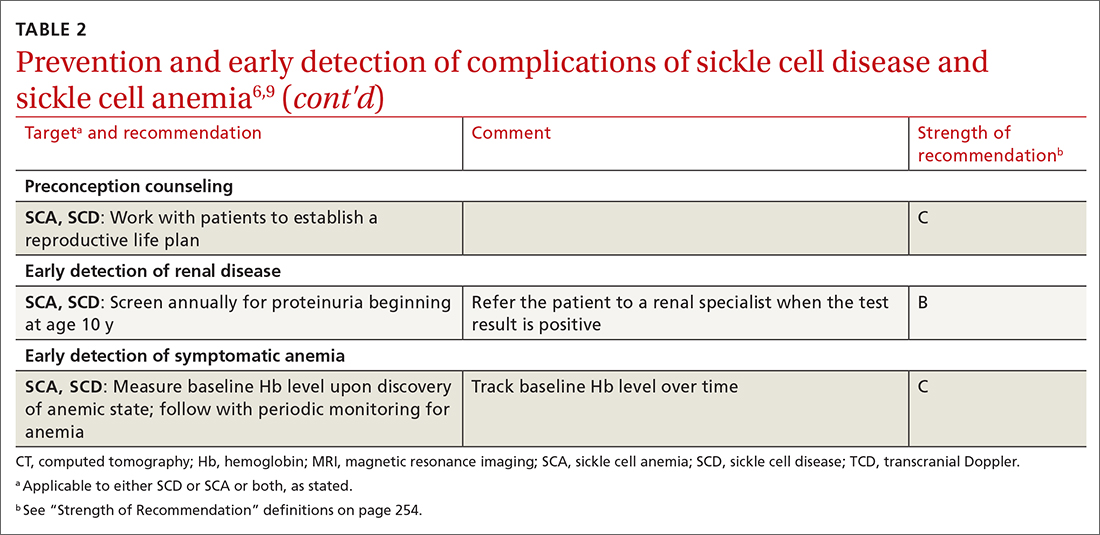
Continue to: In addition, keep in mind...
In addition, keep in mind that preventive recommendations made by the US Preventive Services Task Force (Exhibit 5 in the Expert Panel Report)6 apply to all patients with SCD and SCT.
Prevention of invasive pneumococcal disease
All patients with SCD are assumed to have lifelong splenic dysfunction that begins in childhood. This is particularly true for those with SCA. In the absence of vaccination, the lifetime incidence of pneumococcal bacteremia resulting in serious complications is as high as 16% in SCD.10 In multiple randomized clinical trials, prophylactic penicillin dosing has proved beneficial in these patients, demonstrating a decrease in the risk of (1) pneumococcal infection and (2) early death during the study period, with minimal adverse effects.5
Prophylactic penicillin dosing should be initiated during infancy in patients with SCA. From ages 3 months to 3 years, the dosage of penicillin V is 125 mg twice daily; from 3 to 5 years, 250 mg twice daily. After age 5 years, the decision to continue penicillin is individualized, with consideration of prior severe pneumococcal infection and general preventive health maintenance. Penicillin-allergic patients can be given erythromycin. All patients with SCD who have had surgical splenectomy should be placed on antibiotic prophylaxis (ie, penicillin as dosed above).5
The polyvalent pneumococcal vaccine has resulted in significant protection against invasive pneumococcal disease; mortality from pneumococcal disease among patients with SCD who are younger than 14 years has decreased dramatically since the vaccine was introduced.6 For all patients with SCD, the standard PCV13 series should be administered beginning at age 6 weeks. A 2-dose series of the PPSV23 vaccine, which includes more Streptococcus pneumoniae serotypes than the PCV13 vaccine, should be administered beginning at age 2 years or 8 weeks after completion of the PCV13 series, whichever comes first.
Prevention of flu, COVID-19, and other vaccine-preventable illness
Influenza. Beginning at age 6 months, all patients with SCD should receive inactivated influenza vaccine annually at the beginning of the influenza season. Avoid using the live attenuated vaccine (Flumist) because of an associated increased risk of severe or complicated infection.11
Continue to: COVID-19, caused by severe...
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is especially problematic in patients with SCD12; infection causes mortality at a rate as high as 7%.5 The SARS-CoV-2 mRNA vaccine series is potentially lifesaving for these patients.12 In addition, at times of high community prevalence, make an effort to minimize patients’ exposure to SARS-CoV-2, by providing telemedicine visits.
Follow the immunization schedule. Patients with SCD should receive all standard recommended vaccinations (ie, those recommended by the Advisory Committee on Immunization Practices.a) Inactivated virus vaccines are preferred in SCD, when available. For patients who are behind on vaccinations, use a standard vaccine catch-up schedule.
Screening and prevention of complications such as stroke
Determining the risk of stroke. Patients with SCA who are not monitored have a 10% to 11% lifetime prevalence of stroke.5,6,10 An abnormal transcranial Doppler (TCD) study (defined as a time-averaged mean maximum velocity ≥ 200 cm/s in the distal internal carotid artery or proximal middle cerebral artery) is predictive of a 40% risk of stroke in patients with SCA. With chronic transfusion therapy, a 92% reduction in the risk of stroke is achievable.10
All patients with SCA should undergo annual screening with TCD ultrasonography from ages 2 to 16 years.6 Those who have an abnormal TCD study should receive chronic transfusion therapy. Screening is not recommended for patients with SCD or SCT.
Other complications. Screen and manage as follows:
- Proteinuria. Left untreated, SCD can affect the kidneys and lead to renal failure. Annual screening for proteinuria is recommended beginning at age 10 years, with referral when the test is positive and reproducible.
- Lung disease and cardiovascular disease. Screening for progression of lung disease and for cardiovascular disease is not recommended in asymptomatic patients with SCD, except through the history.
- Blood pressure screening and management of hypertension are based on Joint National Committee (JNC 8) guidelines.13
- Screening for ocular complications by an eye care provider is recommended beginning at age 10 years.
TABLE 26,9 summarizes recommendations on the prevention and early detection of complications of SCD.
Continue to: Pregnancy planning
Pregnancy planning
The Centers for Disease Control and Prevention recommends that a “reproductive life plan” be part of every person’s health journey (TABLE 2).6,9 The plan is especially relevant for female patients who have a known heritable concern, such as SCD, in which a pregnancy is more likely to be complicated by growth restriction, preterm delivery, and fetal demise. These risks are reduced—but not eliminated—with intensive surveillance of the pregnancy. Pregnancy in patients with SCD is also more likely to be complicated by preeclampsia, venous thromboembolism, infection, and maternal death.
Other recommendations:
- Every patient with SCD should receive genetic counselling before conceiving, when possible.
- Pregnancy should be considered high risk in women who have SCD, and monitored as such.
- Women with SCD can use any method of contraception—none of which put them at increased risk of complications, compared to the general population. Rather, it is pregnancy that puts them at greater risk of morbidity and mortality in every age group.
Ambulatory management of acute complications
Vaso-occlusive pain crisis. The hallmark of SCD is the acute pain crisis. Almost all patients with SCD (and the occasional patient with SCT) will experience a pain crisis. In more affluent countries, management of an acute pain crisis almost always includes opioid analgesia.6
For the most part, pain crises manifest in a predictable pattern. Although patients with SCD might have acute pain, other causes of acute pain, such as an acute intra-abdominal process or (in older patients) a cardiac process, should be considered as well.
For patients having a vaso-occlusive pain crisis, achieving rapid analgesia is key to management. Ready availability of narcotics, at home or under observation, prevents subsequent hospitalization; nonsteroidal anti-inflammatory drugs can be used as adjuvant treatment in patients without contraindications.5,6 An individualized treatment plan, including access to analgesia at an appropriate dosage, should be negotiated, and adhered to, by the patient and the care team.
Continue to: Rapid access to higher-level care...
Rapid access to higher-level care, including parenteral analgesia, is important if outpatient management is desired. In addition, escalation to a higher level of care should occur if there is hypoxia (or another reason to suspect acute chest syndrome [ACS; discussed in a bit]) or dehydration that requires parenteral therapy. Use of nondrug therapy, such as heat, should be encouraged. The care team should work with the patient’s school or employer to negotiate time away through the federal Family Medical Leave Act of 1993, or other means, because a pain crisis is not a planned event.
Fever. Because of the risk of serious infection as a consequence of functional asplenia, fever is particularly worrisome in patients with SCA and problematic in patients with SCD. The increased risk begins as the physiologic level of Hb F declines beginning at age 2 months.
ACS, characterized by a combination of respiratory symptoms or new infiltrates, often manifests initially with fever, and can progress rapidly to death if treatment is delayed. The initial signs and symptoms may be subtle; suspicion should remain high in any patient with respiratory symptoms who is newly hypoxic, even those who do not have fever. Osteomyelitis, another febrile illness, is also potentially life threatening if not treated promptly.
All patients with SCD whose body temperature is > 101.3 °F should be evaluated with appropriate clinical laboratory testing (complete blood count; inflammatory markers, such as C-reactive protein; basic chemistry parameters; and other tests as indicated, including serum lactate and urine culture), blood culture, and chest radiography. Empiric parenteral antibiotics are required until the patient is known to be nonbacteremic, regardless of vaccination status. Outpatient follow-up and even outpatient management with ceftriaxone can be offered in select circumstances (eg, if the patient so desires or is nontoxic, and if close follow-up can be assured).14 If ACS is a possibility based on symptoms or radiographic findings, outpatient management is not an option.
Anemia. Patients with SCA, and some with SCD, have an Hb level that is chronically, sometimes critically, low. A baseline Hb level should be established for a patient with SCD and then monitored periodically. A drop in the Hb level > 2 g/dL from baseline (or an initial Hb level of 6 g/dL if the baseline is unknown) constitutes acute anemia. Patients in whom anemia has been diagnosed should be emergently evaluated for acute splenic sequestration, an aplastic episode, a delayed hemolytic transfusion reaction, ACS, or infection, and should be treated appropriately.
Continue to: Simple transfusion can be used...
Simple transfusion can be used in an acute setting to restore and maintain Hb at a safe level. Iron overload and formation of RBC alloantigen are associated with multiple transfusions; once either of these conditions is established, subsequent transfusion therapy can be harmful. Care must be taken to prescribe transfusion appropriately; leukocyte-depleted RBCs should be used when available.
It is important to define specific goals of transfusion to optimize its use. Patients who have received multiple transfusions should have enhanced monitoring for bloodborne infection, such as hepatitis C virus. Acute aplastic crises are caused by parvovirus B19; when other members of the household who have SCD are present, they should be monitored for this viral infection with serial measurement of Hb and white blood cell count.6
Other acute problems. Should stroke, acute renal failure, priapism, or hepatobiliary complications develop, evaluate the patient rapidly and refer them to the appropriate care team for management.
Management of chronic complications
Chronic pain is a problem for many patients with SCD. The etiology of this symptom should be investigated fully because a vaso-occlusive crisis is characterized by acute pain. Avascular necrosis or ulcers due to chronic vaso-occlusion should be managed definitively when possible. Adjuvant therapy for chronic pain, such as heat or massage, should be encouraged.
In some patients, chronic pain without objective findings develops over time and becomes unresponsive to nonopioid pharmacotherapy. Such patients might require chronic opioid therapy, the need for which is dictated by the ability of the patient to perform their activities of daily living. For patients who require long-term daily narcotic drugs, best practices—obtaining informed consent, using registries and contracts, random drug testing, and providing naloxone [Narcan] for overdose emergency use—should be employed.15
Continue to: Chronic anemia
Chronic anemia can be managed with transfusion when elevating the Hb level is required (eg, preoperatively, to prevent stroke, to manage priapism). For some patients, ongoing transfusion is required; care should be taken to avoid iron overload and hemolysis due to antibody formation. Ongoing surveillance for these complications is required.6
Other chronic problems. Patients with SCD who develop avascular necrosis, vaso-occlusive ulcers, pulmonary hypertension, renal disease, recurrent priapism, or ophthalmologic complications should be co-managed with a care team.6
Pharmacotherapy and SCA
A principal goal in the management of patients with SCA is prevention of vaso-occlusive events, including ACS and acute pain crises.
Hydroxyurea, a key component of SCA treatment, is a ribonucleotide reductase inhibitor that increases the level of Hb F, thus reducing the absolute number of symptomatic vaso-occlusive events and increasing arterial blood flow. It is most useful for patients who have multiple crises. The drug prolongs survival and reduces the need for transfusion and hospitalization.4,5
Hydroxyurea can be started in patients at age 9 months; blood testing should be performed at the start of treatment and the dosage titrated based on blood counts. Initial blood work includes:
- Hb level;
- Hb electrophoresis with the quantitative percentage of Hb F;
- complete blood count with differential and reticulocyte counts;
- chemistry profile (electrolytes, lactate dehydrogenase, total protein, albumin, total bilirubin);
- liver function tests (aspartate aminotransferase, alanine aminotransferase);
- measurement of renal function (blood urea nitrogen, creatinine);
- serum vitamin B12 and folate;
- serum iron, total iron-binding capacity, and ferritin;
- hepatitis B, hepatitis C, and parvovirus B19 antigen; and
- serologic testing for HIV.
Continue to: Testing should also...
Testing should also include a pregnancy test for postmenarchal females because hydroxyurea is in US Food and Drug Administration pregnancy risk category X.
Avoid hydroxyurea in lactating women; dose the drug renally in the setting of renal disease. Because hydroxyurea has a high rate of serious adverse effects and drug-drug interactions, it should be offered in conjunction with an individualized care plan.
Hydroxyurea can also be offered to patients with other forms of SCD who have recurrent vaso-occlusive symptoms.
Two newer medications improve oxygen delivery in patients with SCD. Voxelotor, approved in 2019, works to reduce Hb S polymerization by binding to the alpha chain of Hb S and, subsequently, increasing its oxygen affinity. The drug is generally well tolerated and can be used in patients with SCD who are ≥ 12 years.16 Crizanlizumab is a monoclonal antibody directed against P-selectin, an adhesion molecule located on endothelial cells and activated platelets. The efficacy of crizanlizumab was demonstrated in the SUSTAIN trial, in which it reduced vaso-occlusive pain in patients ≥ 16 years.17
All of these medications have a narrow toxic–therapeutic window. They should therefore be administered with the participation of a multidisciplinary care team.
Continue to: The need to coordinated, comprehensive care
The need for coordinated, comprehensive care
Patients with SCD report how challenging their disease is. All patients with SCD are more likely than age-matched counterparts to experience loss, including workdays for disability, educational potential, workdays for caregivers of affected children, and time spent in the hospital or the emergency department.4,5 These losses, with the concomitant stress associated with chronic illness and the struggle to manage recurrent pain crises and chronic complications, are often overwhelming.
Comprehensive care can, as we have illustrated in this discussion, mitigate these losses. Such care should include extensive education, genetic counseling, infection prevention, pain management, and implementation of evidence-based management guidelines.3,4,6 Patients with SCD report that their illness outlook would be better with
- greater provider knowledge of SCD,
- destigmatization of narcotics for SCD vaso-occlusive pain management,
- optimal coordination among members of the health care team, and
- improved transportation for appointments.
Patients also report that barriers associated with the unique US health care financing system are often insurmountable. As patients with SCD live longer, improved care management should focus on reducing these barriers and enhancing their quality of life.2,18,19
CORRESPONDENCE
Robert Allen Perkins, MD, MPH, Department of Family Medicine, University of South Alabama College of Medicine, 1601 Center Street, 2N, Mobile, AL 36604; perkins@health. southalabama.edu
1. Lubeck D, Agodoa I, Bhakta N, et al. Estimated life expectancy and income of patients with sickle cell disease compared with those without sickle cell disease. JAMA Netw Open. 2019;2:e1915374. doi:10.1001/jamanetworkopen.2019.15374
2. Swanson ME, Grosse SD, Kulkarni R. Disability among individuals with sickle cell disease: literature review from a public health perspective. Am J Prev Med. 2011;41(6 suppl 4):S390-S397. doi: 10.1016/j.amepre.2011.09.006
3. Moskowitz JT, Butensky E, Harmatz P, et al. Caregiving time in sickle cell disease: psychological effects in maternal caregivers. Pediatr Blood Cancer. 2007;48:64-71. doi:10.1002/pbc.20792
4. Mehta SR, Afenyi-Annan A, Lottenberg R. Opportunities to improve outcomes in sickle cell disease. Am Fam Phys. 2006;74:303-310.
5. Yawn BP, John-Sowah J. Management of sickle cell disease: recommendations from the 2014 Expert Panel Report. Am Fam Phys. 2015;92:1069-1077.
6. National Heart, Lung, and Blood Institute, National Institutes of Health. Evidence-based management of sickle cell disease. Expert Panel Report, 2014. Accessed June 9, 2022. www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines
7. Committee Opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40. doi: 10.1097/AOG.0000000000001951
8. Jordan LB, Smith-Whitley K, Treadwell MJ, et al. Screening U.S. college athletes for their sickle cell disease carrier status. Am J Prev Med. 2011;41:S406-S412. doi: 10.1016/j.amepre.2011.09.014
9. Adams RJ, McKie VC, Brambilla D, et al. Stroke prevention trial in sickle cell anemia. Control Clin Trials. 1998;19:110-129. doi: 10.1016/s0197-2456(97)00099-8
10. Alzahrani F, Alaidarous K, Alqarni S, et al. Incidence and predictors of bacterial infections in febrile children with sickle cell disease. Int J Pediatr Adolesc Med. 2021;8:236-238 doi: 10.1016/j.ijpam.2020.12.005
11. Committee on Infectious Diseases. Recommendations for prevention and control of influenza in children, 2021-2022. Pediatrics. 2021;148: e2021053745. doi: 10.1542/peds.2021-053745
12. Centers for Disease Control and Prevention. Study finds people with sickle cell disease who developed coronavirus disease have high rates of hospitalization, intensive care unit admission, and death. October 20, 2020. Accessed June 9, 2022. www.cdc.gov/ncbddd/sicklecell/features/scd-and-covid-19.html
13. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
14. Baskin MN, Goh XL, Heeney MM, et al. Bacteremia risk and outpatient management of febrile patients with sickle cell disease. Pediatrics. 2013;131:1035-1041. doi: 10.1542/peds.2012-2139
15. Osunkwo I, Veeramreddy P, Arnall J, et al. Use of buprenorphine/naloxone in amelio rating acute care utilization and chronic opioid use in adults with sickle cell disease. Blood. 2019;134 (suppl 1):790. doi: 10.1182/blood-2019-126589
16. Vichinsky E, Hoppe CC, Ataga KI, et al; HOPE Trial Investigators. A phase 3 randomized trial of voxelotor in sickle cell disease. N Engl J Med. 2019;381:509-519. doi: 10.1056/NEJMoa1903212
17. Ataga KI, Kutlar A, Kanter J, et al. Crizanlizumab for the prevention of pain crises in sickle cell disease. N Engl J Med. 2017;376:429-439. doi: 10.1056/NEJMoa1611770
18. Dixit R, Nettem S, Madan SS, et al. Folate supplementation in people with sickle cell disease. Cochrane Database Syst Rev. 2016;2:CD011130. doi: 10.1002/14651858.CD011130.pub2
19. Brennan-Cook J, Bonnabeau E, Aponte R, et al. Barriers to care for persons with sickle cell disease: the case manager’s opportunity to improve patient outcomes. Prof Case Manag. 2018;23:213-219. doi: 10.1097/NCM.0000000000000260
1. Lubeck D, Agodoa I, Bhakta N, et al. Estimated life expectancy and income of patients with sickle cell disease compared with those without sickle cell disease. JAMA Netw Open. 2019;2:e1915374. doi:10.1001/jamanetworkopen.2019.15374
2. Swanson ME, Grosse SD, Kulkarni R. Disability among individuals with sickle cell disease: literature review from a public health perspective. Am J Prev Med. 2011;41(6 suppl 4):S390-S397. doi: 10.1016/j.amepre.2011.09.006
3. Moskowitz JT, Butensky E, Harmatz P, et al. Caregiving time in sickle cell disease: psychological effects in maternal caregivers. Pediatr Blood Cancer. 2007;48:64-71. doi:10.1002/pbc.20792
4. Mehta SR, Afenyi-Annan A, Lottenberg R. Opportunities to improve outcomes in sickle cell disease. Am Fam Phys. 2006;74:303-310.
5. Yawn BP, John-Sowah J. Management of sickle cell disease: recommendations from the 2014 Expert Panel Report. Am Fam Phys. 2015;92:1069-1077.
6. National Heart, Lung, and Blood Institute, National Institutes of Health. Evidence-based management of sickle cell disease. Expert Panel Report, 2014. Accessed June 9, 2022. www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines
7. Committee Opinion No. 690: Carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40. doi: 10.1097/AOG.0000000000001951
8. Jordan LB, Smith-Whitley K, Treadwell MJ, et al. Screening U.S. college athletes for their sickle cell disease carrier status. Am J Prev Med. 2011;41:S406-S412. doi: 10.1016/j.amepre.2011.09.014
9. Adams RJ, McKie VC, Brambilla D, et al. Stroke prevention trial in sickle cell anemia. Control Clin Trials. 1998;19:110-129. doi: 10.1016/s0197-2456(97)00099-8
10. Alzahrani F, Alaidarous K, Alqarni S, et al. Incidence and predictors of bacterial infections in febrile children with sickle cell disease. Int J Pediatr Adolesc Med. 2021;8:236-238 doi: 10.1016/j.ijpam.2020.12.005
11. Committee on Infectious Diseases. Recommendations for prevention and control of influenza in children, 2021-2022. Pediatrics. 2021;148: e2021053745. doi: 10.1542/peds.2021-053745
12. Centers for Disease Control and Prevention. Study finds people with sickle cell disease who developed coronavirus disease have high rates of hospitalization, intensive care unit admission, and death. October 20, 2020. Accessed June 9, 2022. www.cdc.gov/ncbddd/sicklecell/features/scd-and-covid-19.html
13. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
14. Baskin MN, Goh XL, Heeney MM, et al. Bacteremia risk and outpatient management of febrile patients with sickle cell disease. Pediatrics. 2013;131:1035-1041. doi: 10.1542/peds.2012-2139
15. Osunkwo I, Veeramreddy P, Arnall J, et al. Use of buprenorphine/naloxone in amelio rating acute care utilization and chronic opioid use in adults with sickle cell disease. Blood. 2019;134 (suppl 1):790. doi: 10.1182/blood-2019-126589
16. Vichinsky E, Hoppe CC, Ataga KI, et al; HOPE Trial Investigators. A phase 3 randomized trial of voxelotor in sickle cell disease. N Engl J Med. 2019;381:509-519. doi: 10.1056/NEJMoa1903212
17. Ataga KI, Kutlar A, Kanter J, et al. Crizanlizumab for the prevention of pain crises in sickle cell disease. N Engl J Med. 2017;376:429-439. doi: 10.1056/NEJMoa1611770
18. Dixit R, Nettem S, Madan SS, et al. Folate supplementation in people with sickle cell disease. Cochrane Database Syst Rev. 2016;2:CD011130. doi: 10.1002/14651858.CD011130.pub2
19. Brennan-Cook J, Bonnabeau E, Aponte R, et al. Barriers to care for persons with sickle cell disease: the case manager’s opportunity to improve patient outcomes. Prof Case Manag. 2018;23:213-219. doi: 10.1097/NCM.0000000000000260
PRACTICE RECOMMENDATIONS
› Offer rapid access to narcotic analgesia for patients with sickle cell disease (SCD) who have recurrent vaso-occlusive crises, to prevent unnecessary hospitalization. A
› Provide oral penicillin prophylaxis against pneumococcal disease in patients < 5 years of age who have sickle cell anemia (SCA), but not in children whose SCD is less severe. A
› Screen all patients with SCA annually, beginning at age 2 years until age 16 years, for their risk of stroke, using a transcranial Doppler study. A
› Administer the COVID-19 mRNA vaccine series to all patients with SCD, unless contraindicated. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
FDA warning: Lymphoma drug heightens risk of death
The U.S. Food and Drug Administration issued a warning today that the cancer drug duvelisib (Copiktra, Verastem), a PI3 kinase inhibitor, may increase the risk of death and serious side effects.
Duvelisib was approved in 2018 to treat adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) who had received at least two prior therapies that did not work or stopped working.
However, more recent 5-year overall survival results from the randomized phase 3 DUO clinical trial found a possible increased risk of death with duvelisib, compared with another drug used to treat leukemia and lymphoma, according to an FDA Drug Safety Communication.
“The trial also found Copiktra was associated with a higher risk of serious side effects, including infections, diarrhea, inflammation of the intestines and lungs, skin reactions, and high liver enzyme levels in the blood,” states the warning, which advises prescribers to weigh the risks and benefits of continued use versus use of other treatments.
More specifically, median 5-year overall survival among 319 patients with CLL or SLL in the DUO trial was 52.3 months with duvelisib versus 63.3 months with the monoclonal antibody ofatumumab (hazard ratio, 1.09 overall and 1.06 among patients who received at least two prior lines of therapy).
Serious adverse events of grade 3 or higher were also more common in those treated with duvelisib.
Of note, in April, the FDA also announced that it was withdrawing approval of the relapsed or refractory follicular lymphoma indication for duvelisib following a voluntary request by the drug manufacturer Secura Bio.
A public meeting will be scheduled to discuss the findings of the trial and whether the drug should continue to be prescribed.
This FDA warning follows the agency’s June 1 withdrawal of approval for umbralisib (Ukoniq), another PI3 kinase inhibitor, following an investigation into a “possible increased risk of death.”
As reported by this news organization, umbralisib had received accelerated approval in February 2021 to treat adults with relapsed or refractory marginal zone lymphoma following at least one prior therapy and those with relapsed or refractory follicular lymphoma who had received at least three prior therapies.
“These safety findings were similar for other medicines in the same PI3 kinase inhibitor class, which were discussed at an advisory committee meeting of non-FDA experts in April 2022,” according to the FDA warning.
The FDA urges patients and health care professionals to report side effects involving duvelisib or other medicines to the FDA MedWatch program.
A version of this article first appeared on Medscape.com
The U.S. Food and Drug Administration issued a warning today that the cancer drug duvelisib (Copiktra, Verastem), a PI3 kinase inhibitor, may increase the risk of death and serious side effects.
Duvelisib was approved in 2018 to treat adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) who had received at least two prior therapies that did not work or stopped working.
However, more recent 5-year overall survival results from the randomized phase 3 DUO clinical trial found a possible increased risk of death with duvelisib, compared with another drug used to treat leukemia and lymphoma, according to an FDA Drug Safety Communication.
“The trial also found Copiktra was associated with a higher risk of serious side effects, including infections, diarrhea, inflammation of the intestines and lungs, skin reactions, and high liver enzyme levels in the blood,” states the warning, which advises prescribers to weigh the risks and benefits of continued use versus use of other treatments.
More specifically, median 5-year overall survival among 319 patients with CLL or SLL in the DUO trial was 52.3 months with duvelisib versus 63.3 months with the monoclonal antibody ofatumumab (hazard ratio, 1.09 overall and 1.06 among patients who received at least two prior lines of therapy).
Serious adverse events of grade 3 or higher were also more common in those treated with duvelisib.
Of note, in April, the FDA also announced that it was withdrawing approval of the relapsed or refractory follicular lymphoma indication for duvelisib following a voluntary request by the drug manufacturer Secura Bio.
A public meeting will be scheduled to discuss the findings of the trial and whether the drug should continue to be prescribed.
This FDA warning follows the agency’s June 1 withdrawal of approval for umbralisib (Ukoniq), another PI3 kinase inhibitor, following an investigation into a “possible increased risk of death.”
As reported by this news organization, umbralisib had received accelerated approval in February 2021 to treat adults with relapsed or refractory marginal zone lymphoma following at least one prior therapy and those with relapsed or refractory follicular lymphoma who had received at least three prior therapies.
“These safety findings were similar for other medicines in the same PI3 kinase inhibitor class, which were discussed at an advisory committee meeting of non-FDA experts in April 2022,” according to the FDA warning.
The FDA urges patients and health care professionals to report side effects involving duvelisib or other medicines to the FDA MedWatch program.
A version of this article first appeared on Medscape.com
The U.S. Food and Drug Administration issued a warning today that the cancer drug duvelisib (Copiktra, Verastem), a PI3 kinase inhibitor, may increase the risk of death and serious side effects.
Duvelisib was approved in 2018 to treat adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) who had received at least two prior therapies that did not work or stopped working.
However, more recent 5-year overall survival results from the randomized phase 3 DUO clinical trial found a possible increased risk of death with duvelisib, compared with another drug used to treat leukemia and lymphoma, according to an FDA Drug Safety Communication.
“The trial also found Copiktra was associated with a higher risk of serious side effects, including infections, diarrhea, inflammation of the intestines and lungs, skin reactions, and high liver enzyme levels in the blood,” states the warning, which advises prescribers to weigh the risks and benefits of continued use versus use of other treatments.
More specifically, median 5-year overall survival among 319 patients with CLL or SLL in the DUO trial was 52.3 months with duvelisib versus 63.3 months with the monoclonal antibody ofatumumab (hazard ratio, 1.09 overall and 1.06 among patients who received at least two prior lines of therapy).
Serious adverse events of grade 3 or higher were also more common in those treated with duvelisib.
Of note, in April, the FDA also announced that it was withdrawing approval of the relapsed or refractory follicular lymphoma indication for duvelisib following a voluntary request by the drug manufacturer Secura Bio.
A public meeting will be scheduled to discuss the findings of the trial and whether the drug should continue to be prescribed.
This FDA warning follows the agency’s June 1 withdrawal of approval for umbralisib (Ukoniq), another PI3 kinase inhibitor, following an investigation into a “possible increased risk of death.”
As reported by this news organization, umbralisib had received accelerated approval in February 2021 to treat adults with relapsed or refractory marginal zone lymphoma following at least one prior therapy and those with relapsed or refractory follicular lymphoma who had received at least three prior therapies.
“These safety findings were similar for other medicines in the same PI3 kinase inhibitor class, which were discussed at an advisory committee meeting of non-FDA experts in April 2022,” according to the FDA warning.
The FDA urges patients and health care professionals to report side effects involving duvelisib or other medicines to the FDA MedWatch program.
A version of this article first appeared on Medscape.com
Evidence still lacking that vitamins prevent CVD, cancer: USPSTF
There is not enough evidence to recommend for or against taking most vitamin and mineral supplements to prevent heart disease, stroke, and cancer, a new report by the U.S. Preventive Services Task Force concludes.
However, there are two vitamins – vitamin E and beta-carotene – that the task force recommends against for the prevention of heart disease, stroke, and cancer. Evidence shows that there is no benefit to taking vitamin E and that beta-carotene can increase the risk for lung cancer in people already at risk, such as smokers and those with occupational exposure to asbestos.
These are the main findings of the USPSTF’s final recommendation statement on vitamin, mineral, and multivitamin supplementation to prevent cardiovascular disease and cancer. The statement was published in JAMA.
“This is essentially the same recommendation that the task force made in 2014,” USPSTF member John Wong, MD, professor of medicine at Tufts University, Boston, said in an interview.
“We recognize that over half of people in the U.S. take a vitamin supplement of some sort every day and 30% take a vitamin/mineral combination. We wanted to review the evidence again to see if there was any benefit in terms of reducing the risk of cardiovascular disease or cancer or increasing the chances of living longer,” Dr. Wong explained.
“We looked hard for evidence, reviewing 84 studies in total. But we did not find sufficient evidence in favor of taking or not taking vitamins, with the two exceptions of beta-carotene and vitamin E, which we recommend against taking,” he noted.
Although there is evidence of some harm with beta-carotene, the main reason behind the recommendation against taking vitamin E is the consistent evidence of no benefit, Dr. Wong explained.
“While the evidence for some other vitamins is conflicting, there is more consistent evidence of no benefit for vitamin E,” he said.
The bulk of new evidence since the last review in 2014 was predominately for vitamin D supplementation, but despite the inclusion of 32 new randomized, controlled trials and two cohort studies, pooled estimates for all-cause mortality were similar to those in the previous review, with confidence intervals only slightly crossing 1, and point estimates that suggest at most a very small benefit, the task force noted.
“Apart from beta-carotene and vitamin E, after reviewing 84 studies – including 78 randomized controlled trials – in over a million patients, we can find no clear demonstration of benefit or harm of taking vitamins in terms of developing cardiovascular disease or cancer or the effect on all-cause mortality. So, we don’t know whether people should take vitamins or not, and we need more research,” Dr. Wong added.
On the use of a multivitamin supplement, Dr. Wong noted that the complete body of evidence did not find any benefit of taking a multivitamin on cardiovascular or cancer mortality. But there was a small reduction in cancer incidence.
However, he pointed out that the three studies that suggested a reduction in cancer incidence all had issues regarding generalizability.
“The recently published COSMOS trial had an average follow-up of only 3.6 years, which isn’t really long enough when thinking about the prevention of cancer, one of the other studies only used antioxidants, and the third study was conducted only in U.S. male physicians. So those limitations regarding generalizability limited our confidence in making recommendations about multivitamins,” Dr. Wong explained.
But he noted that the task force did not find any significant harms from taking multivitamins.
“There are possible harms from taking high doses of vitamin A and vitamin D, but generally the doses contained in a multivitamin tablet are lower than these. But if the goal for taking a multivitamin is to lower your risk of cancer or cardiovascular disease, we didn’t find sufficient evidence to be able to make a recommendation,” he said.
Asked what he would say to all the people currently taking multivitamins, Dr. Wong responded that he would advise them to have a conversation with a trusted health care professional about their particular circumstances.
“Our statement has quite a narrow focus. It is directed toward community-dwelling, nonpregnant adults. This recommendation does not apply to children, persons who are pregnant or may become pregnant, or persons who are chronically ill, are hospitalized, or have a known nutritional deficiency,” he commented.
‘Any benefit likely to be small’
In an editorial accompanying the publication of the USPSTF statement, Jenny Jia, MD; Natalie Cameron, MD; and Jeffrey Linder, MD – all from Northwestern University, Chicago – noted that the current evidence base includes 52 additional studies not available when the last USPSTF recommendation on this topic was published in 2014.
The editorialists pointed out that for multivitamins, proving the absence of a benefit is challenging, but at best, current evidence suggests that any potential benefits of a multivitamin to reduce mortality are likely to be small.
They gave an example of a healthy 65-year-old woman with a 9-year estimated mortality risk of about 8%, and note that taking a multivitamin for 5-10 years might reduce her estimated mortality risk to 7.5% (based on an odds ratio of 0.94).
“In addition to showing small potential benefit, this estimate is based on imperfect evidence, is imprecise, and is highly sensitive to how the data are interpreted and analyzed,” they said.
The editorialists recommended that lifestyle counseling to prevent chronic diseases should continue to focus on evidence-based approaches, including balanced diets that are high in fruits and vegetables and physical activity.
However, they added that healthy eating can be a challenge when the American industrialized food system does not prioritize health, and healthy foods tend to be more expensive, leading to access problems and food insecurity.
The editorialists suggested that, rather than focusing money, time, and attention on supplements, it would be better to emphasize lower-risk, higher-benefit activities, such as getting exercise, maintaining a healthy weight, and avoiding smoking, in addition to following a healthful diet.
Possible benefit for older adults?
Commenting on the USPSTF statement, JoAnn Manson, MD, chief, division of preventive medicine, Brigham and Women’s Hospital, Boston, who led the recent COSMOS study, said that vitamin and mineral supplements should not be perceived as a substitute for a healthful diet.
“The emphasis needs to be on getting nutritional needs from a healthy diet that is high in plant-based and whole foods that don’t strip the vitamins and minerals through excessive processing,” she said. “Although it’s easier to pop a pill each day than to focus on healthful dietary patterns, the mixture of phytochemicals, fiber, and all the other nutrients in actual foods just can’t be packaged into a pill. Also, vitamins and minerals tend to be better absorbed from food than from supplements and healthy foods can replace calories from less healthy foods, such as red meat and processed foods.”
However, Dr. Manson noted that the evidence is mounting that taking a tablet containing moderate doses of a wide range of vitamins and minerals is safe and may actually have benefits for some people.
She pointed out that the COSMOS and COSMOS-Mind studies showed benefits of multivitamins in slowing cognitive decline in older adults, but the findings need to be replicated.
“The USPSTF did see a statistically significant 7% reduction in cancer with multivitamins in their meta-analysis of four randomized trials and a borderline 6% reduction in all-cause mortality,” she noted. “Plus, multivitamins have been shown to be quite safe in several large and long-term randomized trials. I agree the evidence is not sufficient to make a blanket recommendation for everyone to take multivitamins, but the evidence is mounting that this would be a prudent approach for many older adults,” Dr. Manson said.
“Many people view multivitamins as a form of insurance, as a way to hedge their bets,” she added. “Although this is a rational approach, especially for those who have concerns about the adequacy of their diet, it’s important that this mindset not lead to complacency about following healthy lifestyle practices, including healthy eating, regular physical activity, not smoking, making sure that blood pressure and cholesterol levels are well controlled, and many other practices that critically important for health but are more challenging than simply popping a pill each day.”
A version of this article first appeared on Medscape.com.
There is not enough evidence to recommend for or against taking most vitamin and mineral supplements to prevent heart disease, stroke, and cancer, a new report by the U.S. Preventive Services Task Force concludes.
However, there are two vitamins – vitamin E and beta-carotene – that the task force recommends against for the prevention of heart disease, stroke, and cancer. Evidence shows that there is no benefit to taking vitamin E and that beta-carotene can increase the risk for lung cancer in people already at risk, such as smokers and those with occupational exposure to asbestos.
These are the main findings of the USPSTF’s final recommendation statement on vitamin, mineral, and multivitamin supplementation to prevent cardiovascular disease and cancer. The statement was published in JAMA.
“This is essentially the same recommendation that the task force made in 2014,” USPSTF member John Wong, MD, professor of medicine at Tufts University, Boston, said in an interview.
“We recognize that over half of people in the U.S. take a vitamin supplement of some sort every day and 30% take a vitamin/mineral combination. We wanted to review the evidence again to see if there was any benefit in terms of reducing the risk of cardiovascular disease or cancer or increasing the chances of living longer,” Dr. Wong explained.
“We looked hard for evidence, reviewing 84 studies in total. But we did not find sufficient evidence in favor of taking or not taking vitamins, with the two exceptions of beta-carotene and vitamin E, which we recommend against taking,” he noted.
Although there is evidence of some harm with beta-carotene, the main reason behind the recommendation against taking vitamin E is the consistent evidence of no benefit, Dr. Wong explained.
“While the evidence for some other vitamins is conflicting, there is more consistent evidence of no benefit for vitamin E,” he said.
The bulk of new evidence since the last review in 2014 was predominately for vitamin D supplementation, but despite the inclusion of 32 new randomized, controlled trials and two cohort studies, pooled estimates for all-cause mortality were similar to those in the previous review, with confidence intervals only slightly crossing 1, and point estimates that suggest at most a very small benefit, the task force noted.
“Apart from beta-carotene and vitamin E, after reviewing 84 studies – including 78 randomized controlled trials – in over a million patients, we can find no clear demonstration of benefit or harm of taking vitamins in terms of developing cardiovascular disease or cancer or the effect on all-cause mortality. So, we don’t know whether people should take vitamins or not, and we need more research,” Dr. Wong added.
On the use of a multivitamin supplement, Dr. Wong noted that the complete body of evidence did not find any benefit of taking a multivitamin on cardiovascular or cancer mortality. But there was a small reduction in cancer incidence.
However, he pointed out that the three studies that suggested a reduction in cancer incidence all had issues regarding generalizability.
“The recently published COSMOS trial had an average follow-up of only 3.6 years, which isn’t really long enough when thinking about the prevention of cancer, one of the other studies only used antioxidants, and the third study was conducted only in U.S. male physicians. So those limitations regarding generalizability limited our confidence in making recommendations about multivitamins,” Dr. Wong explained.
But he noted that the task force did not find any significant harms from taking multivitamins.
“There are possible harms from taking high doses of vitamin A and vitamin D, but generally the doses contained in a multivitamin tablet are lower than these. But if the goal for taking a multivitamin is to lower your risk of cancer or cardiovascular disease, we didn’t find sufficient evidence to be able to make a recommendation,” he said.
Asked what he would say to all the people currently taking multivitamins, Dr. Wong responded that he would advise them to have a conversation with a trusted health care professional about their particular circumstances.
“Our statement has quite a narrow focus. It is directed toward community-dwelling, nonpregnant adults. This recommendation does not apply to children, persons who are pregnant or may become pregnant, or persons who are chronically ill, are hospitalized, or have a known nutritional deficiency,” he commented.
‘Any benefit likely to be small’
In an editorial accompanying the publication of the USPSTF statement, Jenny Jia, MD; Natalie Cameron, MD; and Jeffrey Linder, MD – all from Northwestern University, Chicago – noted that the current evidence base includes 52 additional studies not available when the last USPSTF recommendation on this topic was published in 2014.
The editorialists pointed out that for multivitamins, proving the absence of a benefit is challenging, but at best, current evidence suggests that any potential benefits of a multivitamin to reduce mortality are likely to be small.
They gave an example of a healthy 65-year-old woman with a 9-year estimated mortality risk of about 8%, and note that taking a multivitamin for 5-10 years might reduce her estimated mortality risk to 7.5% (based on an odds ratio of 0.94).
“In addition to showing small potential benefit, this estimate is based on imperfect evidence, is imprecise, and is highly sensitive to how the data are interpreted and analyzed,” they said.
The editorialists recommended that lifestyle counseling to prevent chronic diseases should continue to focus on evidence-based approaches, including balanced diets that are high in fruits and vegetables and physical activity.
However, they added that healthy eating can be a challenge when the American industrialized food system does not prioritize health, and healthy foods tend to be more expensive, leading to access problems and food insecurity.
The editorialists suggested that, rather than focusing money, time, and attention on supplements, it would be better to emphasize lower-risk, higher-benefit activities, such as getting exercise, maintaining a healthy weight, and avoiding smoking, in addition to following a healthful diet.
Possible benefit for older adults?
Commenting on the USPSTF statement, JoAnn Manson, MD, chief, division of preventive medicine, Brigham and Women’s Hospital, Boston, who led the recent COSMOS study, said that vitamin and mineral supplements should not be perceived as a substitute for a healthful diet.
“The emphasis needs to be on getting nutritional needs from a healthy diet that is high in plant-based and whole foods that don’t strip the vitamins and minerals through excessive processing,” she said. “Although it’s easier to pop a pill each day than to focus on healthful dietary patterns, the mixture of phytochemicals, fiber, and all the other nutrients in actual foods just can’t be packaged into a pill. Also, vitamins and minerals tend to be better absorbed from food than from supplements and healthy foods can replace calories from less healthy foods, such as red meat and processed foods.”
However, Dr. Manson noted that the evidence is mounting that taking a tablet containing moderate doses of a wide range of vitamins and minerals is safe and may actually have benefits for some people.
She pointed out that the COSMOS and COSMOS-Mind studies showed benefits of multivitamins in slowing cognitive decline in older adults, but the findings need to be replicated.
“The USPSTF did see a statistically significant 7% reduction in cancer with multivitamins in their meta-analysis of four randomized trials and a borderline 6% reduction in all-cause mortality,” she noted. “Plus, multivitamins have been shown to be quite safe in several large and long-term randomized trials. I agree the evidence is not sufficient to make a blanket recommendation for everyone to take multivitamins, but the evidence is mounting that this would be a prudent approach for many older adults,” Dr. Manson said.
“Many people view multivitamins as a form of insurance, as a way to hedge their bets,” she added. “Although this is a rational approach, especially for those who have concerns about the adequacy of their diet, it’s important that this mindset not lead to complacency about following healthy lifestyle practices, including healthy eating, regular physical activity, not smoking, making sure that blood pressure and cholesterol levels are well controlled, and many other practices that critically important for health but are more challenging than simply popping a pill each day.”
A version of this article first appeared on Medscape.com.
There is not enough evidence to recommend for or against taking most vitamin and mineral supplements to prevent heart disease, stroke, and cancer, a new report by the U.S. Preventive Services Task Force concludes.
However, there are two vitamins – vitamin E and beta-carotene – that the task force recommends against for the prevention of heart disease, stroke, and cancer. Evidence shows that there is no benefit to taking vitamin E and that beta-carotene can increase the risk for lung cancer in people already at risk, such as smokers and those with occupational exposure to asbestos.
These are the main findings of the USPSTF’s final recommendation statement on vitamin, mineral, and multivitamin supplementation to prevent cardiovascular disease and cancer. The statement was published in JAMA.
“This is essentially the same recommendation that the task force made in 2014,” USPSTF member John Wong, MD, professor of medicine at Tufts University, Boston, said in an interview.
“We recognize that over half of people in the U.S. take a vitamin supplement of some sort every day and 30% take a vitamin/mineral combination. We wanted to review the evidence again to see if there was any benefit in terms of reducing the risk of cardiovascular disease or cancer or increasing the chances of living longer,” Dr. Wong explained.
“We looked hard for evidence, reviewing 84 studies in total. But we did not find sufficient evidence in favor of taking or not taking vitamins, with the two exceptions of beta-carotene and vitamin E, which we recommend against taking,” he noted.
Although there is evidence of some harm with beta-carotene, the main reason behind the recommendation against taking vitamin E is the consistent evidence of no benefit, Dr. Wong explained.
“While the evidence for some other vitamins is conflicting, there is more consistent evidence of no benefit for vitamin E,” he said.
The bulk of new evidence since the last review in 2014 was predominately for vitamin D supplementation, but despite the inclusion of 32 new randomized, controlled trials and two cohort studies, pooled estimates for all-cause mortality were similar to those in the previous review, with confidence intervals only slightly crossing 1, and point estimates that suggest at most a very small benefit, the task force noted.
“Apart from beta-carotene and vitamin E, after reviewing 84 studies – including 78 randomized controlled trials – in over a million patients, we can find no clear demonstration of benefit or harm of taking vitamins in terms of developing cardiovascular disease or cancer or the effect on all-cause mortality. So, we don’t know whether people should take vitamins or not, and we need more research,” Dr. Wong added.
On the use of a multivitamin supplement, Dr. Wong noted that the complete body of evidence did not find any benefit of taking a multivitamin on cardiovascular or cancer mortality. But there was a small reduction in cancer incidence.
However, he pointed out that the three studies that suggested a reduction in cancer incidence all had issues regarding generalizability.
“The recently published COSMOS trial had an average follow-up of only 3.6 years, which isn’t really long enough when thinking about the prevention of cancer, one of the other studies only used antioxidants, and the third study was conducted only in U.S. male physicians. So those limitations regarding generalizability limited our confidence in making recommendations about multivitamins,” Dr. Wong explained.
But he noted that the task force did not find any significant harms from taking multivitamins.
“There are possible harms from taking high doses of vitamin A and vitamin D, but generally the doses contained in a multivitamin tablet are lower than these. But if the goal for taking a multivitamin is to lower your risk of cancer or cardiovascular disease, we didn’t find sufficient evidence to be able to make a recommendation,” he said.
Asked what he would say to all the people currently taking multivitamins, Dr. Wong responded that he would advise them to have a conversation with a trusted health care professional about their particular circumstances.
“Our statement has quite a narrow focus. It is directed toward community-dwelling, nonpregnant adults. This recommendation does not apply to children, persons who are pregnant or may become pregnant, or persons who are chronically ill, are hospitalized, or have a known nutritional deficiency,” he commented.
‘Any benefit likely to be small’
In an editorial accompanying the publication of the USPSTF statement, Jenny Jia, MD; Natalie Cameron, MD; and Jeffrey Linder, MD – all from Northwestern University, Chicago – noted that the current evidence base includes 52 additional studies not available when the last USPSTF recommendation on this topic was published in 2014.
The editorialists pointed out that for multivitamins, proving the absence of a benefit is challenging, but at best, current evidence suggests that any potential benefits of a multivitamin to reduce mortality are likely to be small.
They gave an example of a healthy 65-year-old woman with a 9-year estimated mortality risk of about 8%, and note that taking a multivitamin for 5-10 years might reduce her estimated mortality risk to 7.5% (based on an odds ratio of 0.94).
“In addition to showing small potential benefit, this estimate is based on imperfect evidence, is imprecise, and is highly sensitive to how the data are interpreted and analyzed,” they said.
The editorialists recommended that lifestyle counseling to prevent chronic diseases should continue to focus on evidence-based approaches, including balanced diets that are high in fruits and vegetables and physical activity.
However, they added that healthy eating can be a challenge when the American industrialized food system does not prioritize health, and healthy foods tend to be more expensive, leading to access problems and food insecurity.
The editorialists suggested that, rather than focusing money, time, and attention on supplements, it would be better to emphasize lower-risk, higher-benefit activities, such as getting exercise, maintaining a healthy weight, and avoiding smoking, in addition to following a healthful diet.
Possible benefit for older adults?
Commenting on the USPSTF statement, JoAnn Manson, MD, chief, division of preventive medicine, Brigham and Women’s Hospital, Boston, who led the recent COSMOS study, said that vitamin and mineral supplements should not be perceived as a substitute for a healthful diet.
“The emphasis needs to be on getting nutritional needs from a healthy diet that is high in plant-based and whole foods that don’t strip the vitamins and minerals through excessive processing,” she said. “Although it’s easier to pop a pill each day than to focus on healthful dietary patterns, the mixture of phytochemicals, fiber, and all the other nutrients in actual foods just can’t be packaged into a pill. Also, vitamins and minerals tend to be better absorbed from food than from supplements and healthy foods can replace calories from less healthy foods, such as red meat and processed foods.”
However, Dr. Manson noted that the evidence is mounting that taking a tablet containing moderate doses of a wide range of vitamins and minerals is safe and may actually have benefits for some people.
She pointed out that the COSMOS and COSMOS-Mind studies showed benefits of multivitamins in slowing cognitive decline in older adults, but the findings need to be replicated.
“The USPSTF did see a statistically significant 7% reduction in cancer with multivitamins in their meta-analysis of four randomized trials and a borderline 6% reduction in all-cause mortality,” she noted. “Plus, multivitamins have been shown to be quite safe in several large and long-term randomized trials. I agree the evidence is not sufficient to make a blanket recommendation for everyone to take multivitamins, but the evidence is mounting that this would be a prudent approach for many older adults,” Dr. Manson said.
“Many people view multivitamins as a form of insurance, as a way to hedge their bets,” she added. “Although this is a rational approach, especially for those who have concerns about the adequacy of their diet, it’s important that this mindset not lead to complacency about following healthy lifestyle practices, including healthy eating, regular physical activity, not smoking, making sure that blood pressure and cholesterol levels are well controlled, and many other practices that critically important for health but are more challenging than simply popping a pill each day.”
A version of this article first appeared on Medscape.com.
FROM JAMA
Patients with blood cancers underutilize palliative care
I used to attend the Supportive Care in Oncology Symposium every year, but to my dismay, the American Society for Clinical Oncology stopped hosting the symposium a few years ago. Instead, ASCO now incorporates palliative care research fully into its annual meeting which was held in early June in Chicago. Being integrated into the annual meeting means greater exposure to a broader audience that may not otherwise see this work. In this column, I highlight some presentations that stood out to me.
Palliative care studies for patients with hematologic malignancies
There continues to be low uptake of outpatient palliative care services among patients with hematologic malignancies. Fortunately, there are efforts underway to study the impact of integrating early palliative care into the routine care of hematology patients. In a study presented by Mazie Tsang, MD, a clinical fellow at the University of California, San Francisco, researchers embedded a palliative care nurse practitioner in a hematology clinic and studied the impact this single NP had over 4 years of integration. They found that patients were less likely to be hospitalized or visit the emergency department after integrating the NP. They also found that advance directives were more likely to be completed following NP integration. The results were limited by small sample size and lack of a true control group, but generally trended toward significance when compared with historical controls.
Other studies highlighted the relatively high symptom burden among patients with hematologic malignancies, such as myeloma, leukemia, and lymphoma. In a study presented by Sarah E. Monick, MD, of the University of Chicago, researchers found that, among adolescents and young adults with hematologic malignancies seen in a clinic where a palliative care provider was embedded, symptom burden was high across the board regardless of where patients were in their disease trajectory or their demographic characteristics. Due to the presence of high symptom burden among adolescents and young adults, the authors suggest that patients undergo screening at every visit and that supportive care be incorporated throughout the patient’s journey.
Kyle Fitzgibbon of the Princess Margaret Cancer Centre in Toronto shared details of an ongoing multicenter, randomized, controlled, phase 3 trial designed to evaluate the effect of a novel psychosocial/palliative care intervention for patients with acute leukemia hospitalized for induction chemotherapy. The intervention will consist of 8 weeks of psychological support as well as access to palliative care for physical symptoms. Participants will be randomized to receive either intervention or standard of care at the beginning of their hospitalization. Researchers plan to study the impact of the intervention on physical and psychological symptom severity, quality of life, and patient satisfaction at multiple time points. It will be exciting to see the results of this study given that there are very few research clinical trials examining early palliative care with patients who have hematologic malignancies.
Trends in palliative care integration with oncology care
One key trend that I am elated to see is the integration of palliative care throughout the entire patient journey. A secondary analysis of oncology practice data from the National Cancer Institute Community Oncology Research Program found that more than three-quarters of outpatient oncology practices surveyed in 2015 have integrated palliative care inpatient and outpatient services. 36% said they had an outpatient palliative care clinic. More availability of services typically translates to better access to care and improved outcomes for patients, so it is always nice to see these quality metrics continue to move in a positive direction. The analysis was presented by Tiffany M. Statler, PA, of Atrium Health Wake Forest Baptist, Winston Salem, N.C.
It turns out that patients are also advocating for integrated palliative care. A unique qualitative project brought together patient advocates from several countries to hold a moderated discussion about quality of life and treatment side effects. The advocates focused on the importance of maintaining independence with activities of daily living as a significant quality of life goal, particularly as treatments tend to cause cumulative mental and physical fatigue. They highlighted the importance of palliative care for helping achieve quality of life goals, especially in latter part of the disease trajectory. The project was presented by Paul Wheatley-Price, MD, of the Ottawa Hospital Cancer Centre, University of Ottawa.
In 2010, a study by Temel and colleagues was published, finding that patients with metastatic non–small cell lung cancer who received palliative care early had significant improvements in quality of life and mood as compared with patients who received standard care. It was a landmark study and is frequently cited. The Temel group reports on the planning process for a new randomized controlled trial of palliative care with metastatic lung cancer patients who have targetable mutations. With next generation sequencing of tumor tissue, many patients with metastatic lung cancer are identified at diagnosis as having a targetable mutation. As such, they may receive a targeted therapy as first-line treatment instead of traditional chemotherapy. This has lengthened survival considerably, but the disease remains incurable and ultimately fatal, and the trajectory can resemble a roller-coaster ride.
In this new randomized controlled trial, patients in the experimental arm will receive four monthly visits with a palliative care clinician who is specially trained to help patients manage the uncertainties of prolonged illness. The researchers plan to evaluate patients’ distress levels and prognostic awareness, as well as evidence of advance care planning in the chart.
And, a study presented by Roberto Enrique Ochoa Planchart, MD, of Chen Medical Centers, Miami, found that when primary care providers used declines in functional status as a trigger for referring advanced cancer patients to palliative care, those patients were less likely to be admitted to the hospital near the end of life, translating to an 86% cost savings. This study reiterated the importance of partnering with a patient’s nononcologic providers, that is, primary care and palliative care clinicians to improve outcomes at the end of life.
Use of technology in palliative care
Numerous studies were reported on innovative uses of technology for various functions relevant to palliative care. They included everything from capturing patient-reported outcomes through patient-facing smartphone apps, to using artificial intelligence and/or machine learning to build prognostication tools and to generate earlier referrals to palliative care. There were presentations on the use of online tools to assist with and document goals of care conversations.
As a clinician who is always looking for new ways to capture patient symptom information and motivate patients to engage in advance care planning, I am excited about the prospect of using some of these tools in real time.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I used to attend the Supportive Care in Oncology Symposium every year, but to my dismay, the American Society for Clinical Oncology stopped hosting the symposium a few years ago. Instead, ASCO now incorporates palliative care research fully into its annual meeting which was held in early June in Chicago. Being integrated into the annual meeting means greater exposure to a broader audience that may not otherwise see this work. In this column, I highlight some presentations that stood out to me.
Palliative care studies for patients with hematologic malignancies
There continues to be low uptake of outpatient palliative care services among patients with hematologic malignancies. Fortunately, there are efforts underway to study the impact of integrating early palliative care into the routine care of hematology patients. In a study presented by Mazie Tsang, MD, a clinical fellow at the University of California, San Francisco, researchers embedded a palliative care nurse practitioner in a hematology clinic and studied the impact this single NP had over 4 years of integration. They found that patients were less likely to be hospitalized or visit the emergency department after integrating the NP. They also found that advance directives were more likely to be completed following NP integration. The results were limited by small sample size and lack of a true control group, but generally trended toward significance when compared with historical controls.
Other studies highlighted the relatively high symptom burden among patients with hematologic malignancies, such as myeloma, leukemia, and lymphoma. In a study presented by Sarah E. Monick, MD, of the University of Chicago, researchers found that, among adolescents and young adults with hematologic malignancies seen in a clinic where a palliative care provider was embedded, symptom burden was high across the board regardless of where patients were in their disease trajectory or their demographic characteristics. Due to the presence of high symptom burden among adolescents and young adults, the authors suggest that patients undergo screening at every visit and that supportive care be incorporated throughout the patient’s journey.
Kyle Fitzgibbon of the Princess Margaret Cancer Centre in Toronto shared details of an ongoing multicenter, randomized, controlled, phase 3 trial designed to evaluate the effect of a novel psychosocial/palliative care intervention for patients with acute leukemia hospitalized for induction chemotherapy. The intervention will consist of 8 weeks of psychological support as well as access to palliative care for physical symptoms. Participants will be randomized to receive either intervention or standard of care at the beginning of their hospitalization. Researchers plan to study the impact of the intervention on physical and psychological symptom severity, quality of life, and patient satisfaction at multiple time points. It will be exciting to see the results of this study given that there are very few research clinical trials examining early palliative care with patients who have hematologic malignancies.
Trends in palliative care integration with oncology care
One key trend that I am elated to see is the integration of palliative care throughout the entire patient journey. A secondary analysis of oncology practice data from the National Cancer Institute Community Oncology Research Program found that more than three-quarters of outpatient oncology practices surveyed in 2015 have integrated palliative care inpatient and outpatient services. 36% said they had an outpatient palliative care clinic. More availability of services typically translates to better access to care and improved outcomes for patients, so it is always nice to see these quality metrics continue to move in a positive direction. The analysis was presented by Tiffany M. Statler, PA, of Atrium Health Wake Forest Baptist, Winston Salem, N.C.
It turns out that patients are also advocating for integrated palliative care. A unique qualitative project brought together patient advocates from several countries to hold a moderated discussion about quality of life and treatment side effects. The advocates focused on the importance of maintaining independence with activities of daily living as a significant quality of life goal, particularly as treatments tend to cause cumulative mental and physical fatigue. They highlighted the importance of palliative care for helping achieve quality of life goals, especially in latter part of the disease trajectory. The project was presented by Paul Wheatley-Price, MD, of the Ottawa Hospital Cancer Centre, University of Ottawa.
In 2010, a study by Temel and colleagues was published, finding that patients with metastatic non–small cell lung cancer who received palliative care early had significant improvements in quality of life and mood as compared with patients who received standard care. It was a landmark study and is frequently cited. The Temel group reports on the planning process for a new randomized controlled trial of palliative care with metastatic lung cancer patients who have targetable mutations. With next generation sequencing of tumor tissue, many patients with metastatic lung cancer are identified at diagnosis as having a targetable mutation. As such, they may receive a targeted therapy as first-line treatment instead of traditional chemotherapy. This has lengthened survival considerably, but the disease remains incurable and ultimately fatal, and the trajectory can resemble a roller-coaster ride.
In this new randomized controlled trial, patients in the experimental arm will receive four monthly visits with a palliative care clinician who is specially trained to help patients manage the uncertainties of prolonged illness. The researchers plan to evaluate patients’ distress levels and prognostic awareness, as well as evidence of advance care planning in the chart.
And, a study presented by Roberto Enrique Ochoa Planchart, MD, of Chen Medical Centers, Miami, found that when primary care providers used declines in functional status as a trigger for referring advanced cancer patients to palliative care, those patients were less likely to be admitted to the hospital near the end of life, translating to an 86% cost savings. This study reiterated the importance of partnering with a patient’s nononcologic providers, that is, primary care and palliative care clinicians to improve outcomes at the end of life.
Use of technology in palliative care
Numerous studies were reported on innovative uses of technology for various functions relevant to palliative care. They included everything from capturing patient-reported outcomes through patient-facing smartphone apps, to using artificial intelligence and/or machine learning to build prognostication tools and to generate earlier referrals to palliative care. There were presentations on the use of online tools to assist with and document goals of care conversations.
As a clinician who is always looking for new ways to capture patient symptom information and motivate patients to engage in advance care planning, I am excited about the prospect of using some of these tools in real time.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I used to attend the Supportive Care in Oncology Symposium every year, but to my dismay, the American Society for Clinical Oncology stopped hosting the symposium a few years ago. Instead, ASCO now incorporates palliative care research fully into its annual meeting which was held in early June in Chicago. Being integrated into the annual meeting means greater exposure to a broader audience that may not otherwise see this work. In this column, I highlight some presentations that stood out to me.
Palliative care studies for patients with hematologic malignancies
There continues to be low uptake of outpatient palliative care services among patients with hematologic malignancies. Fortunately, there are efforts underway to study the impact of integrating early palliative care into the routine care of hematology patients. In a study presented by Mazie Tsang, MD, a clinical fellow at the University of California, San Francisco, researchers embedded a palliative care nurse practitioner in a hematology clinic and studied the impact this single NP had over 4 years of integration. They found that patients were less likely to be hospitalized or visit the emergency department after integrating the NP. They also found that advance directives were more likely to be completed following NP integration. The results were limited by small sample size and lack of a true control group, but generally trended toward significance when compared with historical controls.
Other studies highlighted the relatively high symptom burden among patients with hematologic malignancies, such as myeloma, leukemia, and lymphoma. In a study presented by Sarah E. Monick, MD, of the University of Chicago, researchers found that, among adolescents and young adults with hematologic malignancies seen in a clinic where a palliative care provider was embedded, symptom burden was high across the board regardless of where patients were in their disease trajectory or their demographic characteristics. Due to the presence of high symptom burden among adolescents and young adults, the authors suggest that patients undergo screening at every visit and that supportive care be incorporated throughout the patient’s journey.
Kyle Fitzgibbon of the Princess Margaret Cancer Centre in Toronto shared details of an ongoing multicenter, randomized, controlled, phase 3 trial designed to evaluate the effect of a novel psychosocial/palliative care intervention for patients with acute leukemia hospitalized for induction chemotherapy. The intervention will consist of 8 weeks of psychological support as well as access to palliative care for physical symptoms. Participants will be randomized to receive either intervention or standard of care at the beginning of their hospitalization. Researchers plan to study the impact of the intervention on physical and psychological symptom severity, quality of life, and patient satisfaction at multiple time points. It will be exciting to see the results of this study given that there are very few research clinical trials examining early palliative care with patients who have hematologic malignancies.
Trends in palliative care integration with oncology care
One key trend that I am elated to see is the integration of palliative care throughout the entire patient journey. A secondary analysis of oncology practice data from the National Cancer Institute Community Oncology Research Program found that more than three-quarters of outpatient oncology practices surveyed in 2015 have integrated palliative care inpatient and outpatient services. 36% said they had an outpatient palliative care clinic. More availability of services typically translates to better access to care and improved outcomes for patients, so it is always nice to see these quality metrics continue to move in a positive direction. The analysis was presented by Tiffany M. Statler, PA, of Atrium Health Wake Forest Baptist, Winston Salem, N.C.
It turns out that patients are also advocating for integrated palliative care. A unique qualitative project brought together patient advocates from several countries to hold a moderated discussion about quality of life and treatment side effects. The advocates focused on the importance of maintaining independence with activities of daily living as a significant quality of life goal, particularly as treatments tend to cause cumulative mental and physical fatigue. They highlighted the importance of palliative care for helping achieve quality of life goals, especially in latter part of the disease trajectory. The project was presented by Paul Wheatley-Price, MD, of the Ottawa Hospital Cancer Centre, University of Ottawa.
In 2010, a study by Temel and colleagues was published, finding that patients with metastatic non–small cell lung cancer who received palliative care early had significant improvements in quality of life and mood as compared with patients who received standard care. It was a landmark study and is frequently cited. The Temel group reports on the planning process for a new randomized controlled trial of palliative care with metastatic lung cancer patients who have targetable mutations. With next generation sequencing of tumor tissue, many patients with metastatic lung cancer are identified at diagnosis as having a targetable mutation. As such, they may receive a targeted therapy as first-line treatment instead of traditional chemotherapy. This has lengthened survival considerably, but the disease remains incurable and ultimately fatal, and the trajectory can resemble a roller-coaster ride.
In this new randomized controlled trial, patients in the experimental arm will receive four monthly visits with a palliative care clinician who is specially trained to help patients manage the uncertainties of prolonged illness. The researchers plan to evaluate patients’ distress levels and prognostic awareness, as well as evidence of advance care planning in the chart.
And, a study presented by Roberto Enrique Ochoa Planchart, MD, of Chen Medical Centers, Miami, found that when primary care providers used declines in functional status as a trigger for referring advanced cancer patients to palliative care, those patients were less likely to be admitted to the hospital near the end of life, translating to an 86% cost savings. This study reiterated the importance of partnering with a patient’s nononcologic providers, that is, primary care and palliative care clinicians to improve outcomes at the end of life.
Use of technology in palliative care
Numerous studies were reported on innovative uses of technology for various functions relevant to palliative care. They included everything from capturing patient-reported outcomes through patient-facing smartphone apps, to using artificial intelligence and/or machine learning to build prognostication tools and to generate earlier referrals to palliative care. There were presentations on the use of online tools to assist with and document goals of care conversations.
As a clinician who is always looking for new ways to capture patient symptom information and motivate patients to engage in advance care planning, I am excited about the prospect of using some of these tools in real time.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
FROM ASCO 2022
Updated AHA/ASA guideline changes care for spontaneous intracerebral hemorrhage
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Cancer patients unaware of their increased thrombosis risk
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
FROM CANCER TREATMENT AND RESEARCH COMMUNICATIONS
Novel COVID-19 vaccine could fill the void for patients with blood cancers
according to study results presented at the annual meeting of the American Association for Cancer Research.
The phase 1/2 trial included 54 patients with a B-cell deficiency (mean age, 63 years; 28% female): 4 had congenital B-cell deficiency and 50 had a blood cancer (lymphocytic leukemia or lymphoma). T-cell immune responses were observed in 86% of patients 28 days after vaccination with a single CoVac-1 dose. The potency of CoVac-1–induced T-cell responses exceeded those seen typically with B cell–deficient patient responses after mRNA vaccine treatment and were comparable with those seen among nonimmunocompromised COVID-19 patients.
In the majority of individuals, currently approved SARS-CoV-2 vaccines induce a robust immune response, however, their efficacy, has been shown to be decreased among individuals who are immunocompromised. Patients treated for hematologic cancers, in particular, receive treatment regimens that damage healthy immune cells, particularly B cells, said Juliane Walz, MD, the study’s senior author and professor of medicine at University Hospital Tübingen (Germany).
“In the clinic, we see many cancer patients who do not mount sufficient humoral immune responses after vaccination with available SARS-CoV-2 vaccines,” Dr. Walz said. “These patients are at a high risk for a severe course of COVID-19.”
B-cell deficiency, she stated, can be compensated for by enhancing T-cell responses against SARS-CoV-2, which can then combat infections in the absence of neutralizing antibodies.
In a prior study of CoVac-1 among 36 adults without immune deficiency, the vaccine elicited T-cell responses that were still robust 3 months post vaccination, and that included responses against omicron and other key SARS-CoV-2 variants.
While mRNA-based or adenoviral vector-based vaccines are limited to the spike protein and are thus prone to loss of activity because of viral mutations, CoVac-1–induced T-cell immunity is far more intense and broader, Dr. Walz said.
CoVac-1 is a peptide vaccine that is injected directly rather than being encoded via mRNA and targets different viral components. It would not be given, however, to healthy, immunocompetent adults because it is important for them to have both B-cell antibody and T-cell response.
The patients with B-cell deficiency recruited for the study were given a single dose of CoVac-1 and assessed for safety and immunogenicity until day 56. Prior vaccinations with an approved SARS-CoV-2 vaccine had failed to elicit a humoral response in 87% of the subjects.
“Our vaccine does not induce antibody responses,” Dr. Walz said. “However, it could be used to induce broad T-cell responses as a complementary or additive vaccine for elderly adults. In the elderly, antibody responses decline very, very fast after vaccination.”
Dr. Walz said that CoVac-1 could find application in various syndromes associated with congenital B-cell deficiencies, in autoimmune diseases such as rheumatoid arthritis and multiple sclerosis, or diseases treated with rituximab or other B cell–depleting therapies (for example, ofatumumab, blinatumomab, or chimeric antigen receptor T cells), and in transplant patients.
A phase 3 study of CoVac-1 versus placebo is under discussion and would require about 300-500 subjects, Dr. Walz said.
“CoVac-1 is designed to induce broad and long-lasting SARS-CoV-2 T-cell immunity, even in individuals who have impaired ability to mount sufficient immunity from a currently approved vaccine, and thus protect these high-risk patients from a severe course of COVID-19,” Dr. Walz said.
“Having an option for these patients is just critical – so this is significant work,” said Ana Maria Lopez, MD, MPH, of the Sidney Kimmel Cancer Center–Jefferson Health, Philadelphia.
Limitations of this study included the small sample size with low racial and ethnic diversity, Dr. Walz stated.
Funding was provided by the Ministry of Science, Research and the Arts of the state of Baden-Württemberg; the Federal Ministry of Research and Education in Germany; the German Research Foundation under Germany’s Excellence Strategy; and the Clinical Cooperation Unit Translational Immunology at University Hospital Tübingen. Dr. Walz holds the CoVac-1 patent.
according to study results presented at the annual meeting of the American Association for Cancer Research.
The phase 1/2 trial included 54 patients with a B-cell deficiency (mean age, 63 years; 28% female): 4 had congenital B-cell deficiency and 50 had a blood cancer (lymphocytic leukemia or lymphoma). T-cell immune responses were observed in 86% of patients 28 days after vaccination with a single CoVac-1 dose. The potency of CoVac-1–induced T-cell responses exceeded those seen typically with B cell–deficient patient responses after mRNA vaccine treatment and were comparable with those seen among nonimmunocompromised COVID-19 patients.
In the majority of individuals, currently approved SARS-CoV-2 vaccines induce a robust immune response, however, their efficacy, has been shown to be decreased among individuals who are immunocompromised. Patients treated for hematologic cancers, in particular, receive treatment regimens that damage healthy immune cells, particularly B cells, said Juliane Walz, MD, the study’s senior author and professor of medicine at University Hospital Tübingen (Germany).
“In the clinic, we see many cancer patients who do not mount sufficient humoral immune responses after vaccination with available SARS-CoV-2 vaccines,” Dr. Walz said. “These patients are at a high risk for a severe course of COVID-19.”
B-cell deficiency, she stated, can be compensated for by enhancing T-cell responses against SARS-CoV-2, which can then combat infections in the absence of neutralizing antibodies.
In a prior study of CoVac-1 among 36 adults without immune deficiency, the vaccine elicited T-cell responses that were still robust 3 months post vaccination, and that included responses against omicron and other key SARS-CoV-2 variants.
While mRNA-based or adenoviral vector-based vaccines are limited to the spike protein and are thus prone to loss of activity because of viral mutations, CoVac-1–induced T-cell immunity is far more intense and broader, Dr. Walz said.
CoVac-1 is a peptide vaccine that is injected directly rather than being encoded via mRNA and targets different viral components. It would not be given, however, to healthy, immunocompetent adults because it is important for them to have both B-cell antibody and T-cell response.
The patients with B-cell deficiency recruited for the study were given a single dose of CoVac-1 and assessed for safety and immunogenicity until day 56. Prior vaccinations with an approved SARS-CoV-2 vaccine had failed to elicit a humoral response in 87% of the subjects.
“Our vaccine does not induce antibody responses,” Dr. Walz said. “However, it could be used to induce broad T-cell responses as a complementary or additive vaccine for elderly adults. In the elderly, antibody responses decline very, very fast after vaccination.”
Dr. Walz said that CoVac-1 could find application in various syndromes associated with congenital B-cell deficiencies, in autoimmune diseases such as rheumatoid arthritis and multiple sclerosis, or diseases treated with rituximab or other B cell–depleting therapies (for example, ofatumumab, blinatumomab, or chimeric antigen receptor T cells), and in transplant patients.
A phase 3 study of CoVac-1 versus placebo is under discussion and would require about 300-500 subjects, Dr. Walz said.
“CoVac-1 is designed to induce broad and long-lasting SARS-CoV-2 T-cell immunity, even in individuals who have impaired ability to mount sufficient immunity from a currently approved vaccine, and thus protect these high-risk patients from a severe course of COVID-19,” Dr. Walz said.
“Having an option for these patients is just critical – so this is significant work,” said Ana Maria Lopez, MD, MPH, of the Sidney Kimmel Cancer Center–Jefferson Health, Philadelphia.
Limitations of this study included the small sample size with low racial and ethnic diversity, Dr. Walz stated.
Funding was provided by the Ministry of Science, Research and the Arts of the state of Baden-Württemberg; the Federal Ministry of Research and Education in Germany; the German Research Foundation under Germany’s Excellence Strategy; and the Clinical Cooperation Unit Translational Immunology at University Hospital Tübingen. Dr. Walz holds the CoVac-1 patent.
according to study results presented at the annual meeting of the American Association for Cancer Research.
The phase 1/2 trial included 54 patients with a B-cell deficiency (mean age, 63 years; 28% female): 4 had congenital B-cell deficiency and 50 had a blood cancer (lymphocytic leukemia or lymphoma). T-cell immune responses were observed in 86% of patients 28 days after vaccination with a single CoVac-1 dose. The potency of CoVac-1–induced T-cell responses exceeded those seen typically with B cell–deficient patient responses after mRNA vaccine treatment and were comparable with those seen among nonimmunocompromised COVID-19 patients.
In the majority of individuals, currently approved SARS-CoV-2 vaccines induce a robust immune response, however, their efficacy, has been shown to be decreased among individuals who are immunocompromised. Patients treated for hematologic cancers, in particular, receive treatment regimens that damage healthy immune cells, particularly B cells, said Juliane Walz, MD, the study’s senior author and professor of medicine at University Hospital Tübingen (Germany).
“In the clinic, we see many cancer patients who do not mount sufficient humoral immune responses after vaccination with available SARS-CoV-2 vaccines,” Dr. Walz said. “These patients are at a high risk for a severe course of COVID-19.”
B-cell deficiency, she stated, can be compensated for by enhancing T-cell responses against SARS-CoV-2, which can then combat infections in the absence of neutralizing antibodies.
In a prior study of CoVac-1 among 36 adults without immune deficiency, the vaccine elicited T-cell responses that were still robust 3 months post vaccination, and that included responses against omicron and other key SARS-CoV-2 variants.
While mRNA-based or adenoviral vector-based vaccines are limited to the spike protein and are thus prone to loss of activity because of viral mutations, CoVac-1–induced T-cell immunity is far more intense and broader, Dr. Walz said.
CoVac-1 is a peptide vaccine that is injected directly rather than being encoded via mRNA and targets different viral components. It would not be given, however, to healthy, immunocompetent adults because it is important for them to have both B-cell antibody and T-cell response.
The patients with B-cell deficiency recruited for the study were given a single dose of CoVac-1 and assessed for safety and immunogenicity until day 56. Prior vaccinations with an approved SARS-CoV-2 vaccine had failed to elicit a humoral response in 87% of the subjects.
“Our vaccine does not induce antibody responses,” Dr. Walz said. “However, it could be used to induce broad T-cell responses as a complementary or additive vaccine for elderly adults. In the elderly, antibody responses decline very, very fast after vaccination.”
Dr. Walz said that CoVac-1 could find application in various syndromes associated with congenital B-cell deficiencies, in autoimmune diseases such as rheumatoid arthritis and multiple sclerosis, or diseases treated with rituximab or other B cell–depleting therapies (for example, ofatumumab, blinatumomab, or chimeric antigen receptor T cells), and in transplant patients.
A phase 3 study of CoVac-1 versus placebo is under discussion and would require about 300-500 subjects, Dr. Walz said.
“CoVac-1 is designed to induce broad and long-lasting SARS-CoV-2 T-cell immunity, even in individuals who have impaired ability to mount sufficient immunity from a currently approved vaccine, and thus protect these high-risk patients from a severe course of COVID-19,” Dr. Walz said.
“Having an option for these patients is just critical – so this is significant work,” said Ana Maria Lopez, MD, MPH, of the Sidney Kimmel Cancer Center–Jefferson Health, Philadelphia.
Limitations of this study included the small sample size with low racial and ethnic diversity, Dr. Walz stated.
Funding was provided by the Ministry of Science, Research and the Arts of the state of Baden-Württemberg; the Federal Ministry of Research and Education in Germany; the German Research Foundation under Germany’s Excellence Strategy; and the Clinical Cooperation Unit Translational Immunology at University Hospital Tübingen. Dr. Walz holds the CoVac-1 patent.
FROM AACR 2022




