User login
DDNA19: The NASH conundrum
Zobair Younossi, MD, MPH, chairman of the department of medicine at Inova Fairfax (Va.) Medical Campus, discusses the progressive form of NAFLD -- NASH -- and its optimal treatment.

Zobair Younossi, MD, MPH, chairman of the department of medicine at Inova Fairfax (Va.) Medical Campus, discusses the progressive form of NAFLD -- NASH -- and its optimal treatment.

Zobair Younossi, MD, MPH, chairman of the department of medicine at Inova Fairfax (Va.) Medical Campus, discusses the progressive form of NAFLD -- NASH -- and its optimal treatment.

AT DIGESTIVE DISEASES: NEW ADVANCES 2019
Cirrhosis model predicts decompensation across diverse populations
A prognostic model that uses serum albumin-bilirubin (ALBI) and Fibrosis-4 (FIB-4) scores can identify patients with cirrhosis who are at high risk of liver decompensation, according to investigators.
During validation testing, the scoring system performed well among European and Middle Eastern patients, which supports prognostic value across diverse populations, reported lead author Neil Guha, MRCP, PhD, of the University of Nottingham (U.K.) and his colleagues, who suggested that the scoring system could fix an important practice gap.
“Identification of patients [with chronic liver disease] that need intensive monitoring and timely intervention is challenging,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Robust prognostic tools using simple laboratory variables, with potential for implementation in nonspecialist settings and across different health care systems, have significant appeal.”
Although existing scoring systems have been used for decades, they have clear limitations, the investigators noted, referring to predictive ability that may be too little, too late.
“[T]hese scoring systems provide value after synthetic liver function has become significantly deranged and provide only short-term prognostic value,” the investigators wrote. “Presently, there are no scores, performed in routine clinical practice, that provide robust prognostic stratification within early, compensated cirrhosis over the medium/long term.”
To fulfill this need, the investigators developed and validated a prognostic model that incorporates data from the ALBI and FIB-4 scoring systems because these tests measure both fibrosis and function. The development phase involved 145 patients with compensated cirrhosis from Nottingham. Almost half of the cohort had liver disease because of alcohol (44.8%), while about one out of three patients had nonalcoholic fatty liver disease (29.7%). After investigators collected baseline clinical features and scores, patients were followed for a median of 4.59 years, during which time decompensation events were recorded (ascites, variceal bleeding, and encephalopathy). Decompensation occurred in about one out of five patients (19.3%) in the U.K. group, with ascites being the most common (71.4%). Using these findings, the investigators created the prognostic model, which classified patients as having either low or high risk of decompensation. In the development cohort, patients with high risk scores had a hazard ratio for decompensation of 7.10.
In the second part of the study, the investigators validated their model with two clinically distinct groups in Dublin, Ireland (prospective; n = 141), and Menoufia, Egypt (retrospective; n = 93).
In the Dublin cohort, the most common etiologies were alcohol (39.7%) and hepatitis C (29.8%). Over a maximum observational period of 6.4 years, the decompensation rate was lower than the development group, at 12.1%. Types of decompensation also differed, with variceal bleeding being the most common (47.1%). Patients with high risk scores had a higher HR for decompensation than the U.K. cohort, at 12.54.
In the Egypt group, the most common causes of liver disease were nonalcoholic fatty liver disease (47.3%) and hepatitis C (34.4%). The maximum follow-up period was 10.6 years, during which time 38.7% of patients experienced decompensation, with ascites being the most common form (57.1%). The HR of 5.10 was the lowest of all cohorts.
The investigators noted that the cohorts represented unique patient populations with different etiological patterns. “This provides reassurance that the model has generalizability for stratifying liver disease at an international level,” the investigators wrote, suggesting that ALBI and FIB-4 can be used in low-resource and community settings.
“A frequently leveled criticism of algorithms such as ALBI-FIB-4 is that they are too complicated to be applied routinely in the clinical setting,” the investigators wrote. “To overcome this problem we developed a simple online calculator which can be accessed using the following link: https://jscalc.io/calc/gdEJj89Wz5PirkSL.”
“We have shown that routinely available laboratory variables, combined in a novel algorithm, ALBI-FIB-4, can stratify patients with cirrhosis for future risk of liver decompensation,” the investigators concluded. “The ability to do this in the context of early, compensated cirrhosis with preserved liver synthetic function whilst also predicting long-term clinical outcomes has clinical utility for international health care systems.”
The study was funded by National Institute for Health Research (NIHR) Nottingham Digestive Diseases Biomedical Research Centre based at Nottingham University Hospitals NHS Trust and the University of Nottingham. The investigators declared no conflicts of interest.
SOURCE: Guha N et al. CGH. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.042.
A prognostic model that uses serum albumin-bilirubin (ALBI) and Fibrosis-4 (FIB-4) scores can identify patients with cirrhosis who are at high risk of liver decompensation, according to investigators.
During validation testing, the scoring system performed well among European and Middle Eastern patients, which supports prognostic value across diverse populations, reported lead author Neil Guha, MRCP, PhD, of the University of Nottingham (U.K.) and his colleagues, who suggested that the scoring system could fix an important practice gap.
“Identification of patients [with chronic liver disease] that need intensive monitoring and timely intervention is challenging,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Robust prognostic tools using simple laboratory variables, with potential for implementation in nonspecialist settings and across different health care systems, have significant appeal.”
Although existing scoring systems have been used for decades, they have clear limitations, the investigators noted, referring to predictive ability that may be too little, too late.
“[T]hese scoring systems provide value after synthetic liver function has become significantly deranged and provide only short-term prognostic value,” the investigators wrote. “Presently, there are no scores, performed in routine clinical practice, that provide robust prognostic stratification within early, compensated cirrhosis over the medium/long term.”
To fulfill this need, the investigators developed and validated a prognostic model that incorporates data from the ALBI and FIB-4 scoring systems because these tests measure both fibrosis and function. The development phase involved 145 patients with compensated cirrhosis from Nottingham. Almost half of the cohort had liver disease because of alcohol (44.8%), while about one out of three patients had nonalcoholic fatty liver disease (29.7%). After investigators collected baseline clinical features and scores, patients were followed for a median of 4.59 years, during which time decompensation events were recorded (ascites, variceal bleeding, and encephalopathy). Decompensation occurred in about one out of five patients (19.3%) in the U.K. group, with ascites being the most common (71.4%). Using these findings, the investigators created the prognostic model, which classified patients as having either low or high risk of decompensation. In the development cohort, patients with high risk scores had a hazard ratio for decompensation of 7.10.
In the second part of the study, the investigators validated their model with two clinically distinct groups in Dublin, Ireland (prospective; n = 141), and Menoufia, Egypt (retrospective; n = 93).
In the Dublin cohort, the most common etiologies were alcohol (39.7%) and hepatitis C (29.8%). Over a maximum observational period of 6.4 years, the decompensation rate was lower than the development group, at 12.1%. Types of decompensation also differed, with variceal bleeding being the most common (47.1%). Patients with high risk scores had a higher HR for decompensation than the U.K. cohort, at 12.54.
In the Egypt group, the most common causes of liver disease were nonalcoholic fatty liver disease (47.3%) and hepatitis C (34.4%). The maximum follow-up period was 10.6 years, during which time 38.7% of patients experienced decompensation, with ascites being the most common form (57.1%). The HR of 5.10 was the lowest of all cohorts.
The investigators noted that the cohorts represented unique patient populations with different etiological patterns. “This provides reassurance that the model has generalizability for stratifying liver disease at an international level,” the investigators wrote, suggesting that ALBI and FIB-4 can be used in low-resource and community settings.
“A frequently leveled criticism of algorithms such as ALBI-FIB-4 is that they are too complicated to be applied routinely in the clinical setting,” the investigators wrote. “To overcome this problem we developed a simple online calculator which can be accessed using the following link: https://jscalc.io/calc/gdEJj89Wz5PirkSL.”
“We have shown that routinely available laboratory variables, combined in a novel algorithm, ALBI-FIB-4, can stratify patients with cirrhosis for future risk of liver decompensation,” the investigators concluded. “The ability to do this in the context of early, compensated cirrhosis with preserved liver synthetic function whilst also predicting long-term clinical outcomes has clinical utility for international health care systems.”
The study was funded by National Institute for Health Research (NIHR) Nottingham Digestive Diseases Biomedical Research Centre based at Nottingham University Hospitals NHS Trust and the University of Nottingham. The investigators declared no conflicts of interest.
SOURCE: Guha N et al. CGH. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.042.
A prognostic model that uses serum albumin-bilirubin (ALBI) and Fibrosis-4 (FIB-4) scores can identify patients with cirrhosis who are at high risk of liver decompensation, according to investigators.
During validation testing, the scoring system performed well among European and Middle Eastern patients, which supports prognostic value across diverse populations, reported lead author Neil Guha, MRCP, PhD, of the University of Nottingham (U.K.) and his colleagues, who suggested that the scoring system could fix an important practice gap.
“Identification of patients [with chronic liver disease] that need intensive monitoring and timely intervention is challenging,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Robust prognostic tools using simple laboratory variables, with potential for implementation in nonspecialist settings and across different health care systems, have significant appeal.”
Although existing scoring systems have been used for decades, they have clear limitations, the investigators noted, referring to predictive ability that may be too little, too late.
“[T]hese scoring systems provide value after synthetic liver function has become significantly deranged and provide only short-term prognostic value,” the investigators wrote. “Presently, there are no scores, performed in routine clinical practice, that provide robust prognostic stratification within early, compensated cirrhosis over the medium/long term.”
To fulfill this need, the investigators developed and validated a prognostic model that incorporates data from the ALBI and FIB-4 scoring systems because these tests measure both fibrosis and function. The development phase involved 145 patients with compensated cirrhosis from Nottingham. Almost half of the cohort had liver disease because of alcohol (44.8%), while about one out of three patients had nonalcoholic fatty liver disease (29.7%). After investigators collected baseline clinical features and scores, patients were followed for a median of 4.59 years, during which time decompensation events were recorded (ascites, variceal bleeding, and encephalopathy). Decompensation occurred in about one out of five patients (19.3%) in the U.K. group, with ascites being the most common (71.4%). Using these findings, the investigators created the prognostic model, which classified patients as having either low or high risk of decompensation. In the development cohort, patients with high risk scores had a hazard ratio for decompensation of 7.10.
In the second part of the study, the investigators validated their model with two clinically distinct groups in Dublin, Ireland (prospective; n = 141), and Menoufia, Egypt (retrospective; n = 93).
In the Dublin cohort, the most common etiologies were alcohol (39.7%) and hepatitis C (29.8%). Over a maximum observational period of 6.4 years, the decompensation rate was lower than the development group, at 12.1%. Types of decompensation also differed, with variceal bleeding being the most common (47.1%). Patients with high risk scores had a higher HR for decompensation than the U.K. cohort, at 12.54.
In the Egypt group, the most common causes of liver disease were nonalcoholic fatty liver disease (47.3%) and hepatitis C (34.4%). The maximum follow-up period was 10.6 years, during which time 38.7% of patients experienced decompensation, with ascites being the most common form (57.1%). The HR of 5.10 was the lowest of all cohorts.
The investigators noted that the cohorts represented unique patient populations with different etiological patterns. “This provides reassurance that the model has generalizability for stratifying liver disease at an international level,” the investigators wrote, suggesting that ALBI and FIB-4 can be used in low-resource and community settings.
“A frequently leveled criticism of algorithms such as ALBI-FIB-4 is that they are too complicated to be applied routinely in the clinical setting,” the investigators wrote. “To overcome this problem we developed a simple online calculator which can be accessed using the following link: https://jscalc.io/calc/gdEJj89Wz5PirkSL.”
“We have shown that routinely available laboratory variables, combined in a novel algorithm, ALBI-FIB-4, can stratify patients with cirrhosis for future risk of liver decompensation,” the investigators concluded. “The ability to do this in the context of early, compensated cirrhosis with preserved liver synthetic function whilst also predicting long-term clinical outcomes has clinical utility for international health care systems.”
The study was funded by National Institute for Health Research (NIHR) Nottingham Digestive Diseases Biomedical Research Centre based at Nottingham University Hospitals NHS Trust and the University of Nottingham. The investigators declared no conflicts of interest.
SOURCE: Guha N et al. CGH. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.042.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Will inpatient albumin help in decompensated cirrhosis?
PHILADELPHIA – , according to Vijay Shah, MD, chair of the division of gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
“These are interesting studies, but I don’t think we’re ready yet to use this broadly,” Dr. Shah said at the meeting jointly provided by Rutgers and Global Academy for Medical Education.
Current guidelines do describe the use of albumin for large-volume paracentesis and other specific inpatient situations; however, extrapolating its long-term use has been explored in two major studies that recently came out with contradictory findings.
In the ANSWER trial, as reported in the Lancet, investigators at 33 centers randomized patients with cirrhosis and uncomplicated ascites to either standard medical treatment with or without human albumin, at 40 g twice weekly for 2 weeks, followed by 40 g weekly for up to 18 months.
Those investigators found that long-term albumin prolonged overall survival, with a 38% reduction in the mortality hazard ratio, with similar rates of serious, nonliver adverse events, leading them to conclude that this intervention may act as a disease-modifying treatment in decompensated cirrhosis patients.
By contrast, however, a recent randomized, placebo-controlled trial reported in the Journal of Hepatology showed that albumin plus midodrine, an alpha-adrenergic vasoconstrictor, did not improve survival among patients with decompensated cirrhosis on the liver transplant waiting list, at least at the doses administered (midodrine 15-30 mg/day and albumin 40 g every 15 days for a year).
While this particular combination of albumin plus midodrine did decrease renin and aldosterone levels, the intervention did not prevent complications or improve survival, investigators said at the time. Complication rates were 37% and 43% for treatment and placebo, respectively (P = .402), with low rates of death in both groups and no significant difference in mortality at 1 year (P = .527).
Dr. Shah said the discrepant results may be attributable to specific differences in study design or enrollment.
“It’s just hand waving, but it may be related to the dose of albumin, or may be related to the types of patients – the second study was in patients who are waiting for liver transplantation,” he told attendees. “But I don’t think that there’s currently enough evidence to use albumin in your patients in the outpatient setting.”
There is a third study, recently published in the American Journal of Gastroenterology, looking at data for a large end-stage liver disease cohort with hyponatremia. Investigators observed a higher rate of hyponatremia resolution and improved 30-day survival in those who had received albumin (total mean amount, 225 g) versus those who had not.
Considering all of this evidence taken together, Dr. Shah said he would not favor using outpatient albumin at this point – though he advised attendees to watch for a currently recruiting phase 3 randomized study, known as PRECIOSA, which is evaluating long-term administration of human albumin 20% injectable solution, dosed by body weight, in patients with decompensated cirrhosis and ascites.
Dr. Shah indicated that he is a consultant for Afimmune, Durect Corporation, Enterome, GRI Bio, Merck Research Laboratories, Novartis Pharma, and Vital Therapeutics. Global Academy and this news organization are owned by the same company.
PHILADELPHIA – , according to Vijay Shah, MD, chair of the division of gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
“These are interesting studies, but I don’t think we’re ready yet to use this broadly,” Dr. Shah said at the meeting jointly provided by Rutgers and Global Academy for Medical Education.
Current guidelines do describe the use of albumin for large-volume paracentesis and other specific inpatient situations; however, extrapolating its long-term use has been explored in two major studies that recently came out with contradictory findings.
In the ANSWER trial, as reported in the Lancet, investigators at 33 centers randomized patients with cirrhosis and uncomplicated ascites to either standard medical treatment with or without human albumin, at 40 g twice weekly for 2 weeks, followed by 40 g weekly for up to 18 months.
Those investigators found that long-term albumin prolonged overall survival, with a 38% reduction in the mortality hazard ratio, with similar rates of serious, nonliver adverse events, leading them to conclude that this intervention may act as a disease-modifying treatment in decompensated cirrhosis patients.
By contrast, however, a recent randomized, placebo-controlled trial reported in the Journal of Hepatology showed that albumin plus midodrine, an alpha-adrenergic vasoconstrictor, did not improve survival among patients with decompensated cirrhosis on the liver transplant waiting list, at least at the doses administered (midodrine 15-30 mg/day and albumin 40 g every 15 days for a year).
While this particular combination of albumin plus midodrine did decrease renin and aldosterone levels, the intervention did not prevent complications or improve survival, investigators said at the time. Complication rates were 37% and 43% for treatment and placebo, respectively (P = .402), with low rates of death in both groups and no significant difference in mortality at 1 year (P = .527).
Dr. Shah said the discrepant results may be attributable to specific differences in study design or enrollment.
“It’s just hand waving, but it may be related to the dose of albumin, or may be related to the types of patients – the second study was in patients who are waiting for liver transplantation,” he told attendees. “But I don’t think that there’s currently enough evidence to use albumin in your patients in the outpatient setting.”
There is a third study, recently published in the American Journal of Gastroenterology, looking at data for a large end-stage liver disease cohort with hyponatremia. Investigators observed a higher rate of hyponatremia resolution and improved 30-day survival in those who had received albumin (total mean amount, 225 g) versus those who had not.
Considering all of this evidence taken together, Dr. Shah said he would not favor using outpatient albumin at this point – though he advised attendees to watch for a currently recruiting phase 3 randomized study, known as PRECIOSA, which is evaluating long-term administration of human albumin 20% injectable solution, dosed by body weight, in patients with decompensated cirrhosis and ascites.
Dr. Shah indicated that he is a consultant for Afimmune, Durect Corporation, Enterome, GRI Bio, Merck Research Laboratories, Novartis Pharma, and Vital Therapeutics. Global Academy and this news organization are owned by the same company.
PHILADELPHIA – , according to Vijay Shah, MD, chair of the division of gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
“These are interesting studies, but I don’t think we’re ready yet to use this broadly,” Dr. Shah said at the meeting jointly provided by Rutgers and Global Academy for Medical Education.
Current guidelines do describe the use of albumin for large-volume paracentesis and other specific inpatient situations; however, extrapolating its long-term use has been explored in two major studies that recently came out with contradictory findings.
In the ANSWER trial, as reported in the Lancet, investigators at 33 centers randomized patients with cirrhosis and uncomplicated ascites to either standard medical treatment with or without human albumin, at 40 g twice weekly for 2 weeks, followed by 40 g weekly for up to 18 months.
Those investigators found that long-term albumin prolonged overall survival, with a 38% reduction in the mortality hazard ratio, with similar rates of serious, nonliver adverse events, leading them to conclude that this intervention may act as a disease-modifying treatment in decompensated cirrhosis patients.
By contrast, however, a recent randomized, placebo-controlled trial reported in the Journal of Hepatology showed that albumin plus midodrine, an alpha-adrenergic vasoconstrictor, did not improve survival among patients with decompensated cirrhosis on the liver transplant waiting list, at least at the doses administered (midodrine 15-30 mg/day and albumin 40 g every 15 days for a year).
While this particular combination of albumin plus midodrine did decrease renin and aldosterone levels, the intervention did not prevent complications or improve survival, investigators said at the time. Complication rates were 37% and 43% for treatment and placebo, respectively (P = .402), with low rates of death in both groups and no significant difference in mortality at 1 year (P = .527).
Dr. Shah said the discrepant results may be attributable to specific differences in study design or enrollment.
“It’s just hand waving, but it may be related to the dose of albumin, or may be related to the types of patients – the second study was in patients who are waiting for liver transplantation,” he told attendees. “But I don’t think that there’s currently enough evidence to use albumin in your patients in the outpatient setting.”
There is a third study, recently published in the American Journal of Gastroenterology, looking at data for a large end-stage liver disease cohort with hyponatremia. Investigators observed a higher rate of hyponatremia resolution and improved 30-day survival in those who had received albumin (total mean amount, 225 g) versus those who had not.
Considering all of this evidence taken together, Dr. Shah said he would not favor using outpatient albumin at this point – though he advised attendees to watch for a currently recruiting phase 3 randomized study, known as PRECIOSA, which is evaluating long-term administration of human albumin 20% injectable solution, dosed by body weight, in patients with decompensated cirrhosis and ascites.
Dr. Shah indicated that he is a consultant for Afimmune, Durect Corporation, Enterome, GRI Bio, Merck Research Laboratories, Novartis Pharma, and Vital Therapeutics. Global Academy and this news organization are owned by the same company.
REPORTING FROM DIGESTIVE DISEASES: NEW ADVANCES
DDNA19: Cardiac Complications in Liver Disease Patients

Dr. Marc Klapholz of Rutgers University, Newark, N.J., explains the latest developments in portopulmonary arterial hypertension, hepatopulmonary syndrome, and cirrhotic cardiomyopathy, as well as the emerging field and association between non-alcoholic fatty liver disease and cardiovascular disease.

Dr. Marc Klapholz of Rutgers University, Newark, N.J., explains the latest developments in portopulmonary arterial hypertension, hepatopulmonary syndrome, and cirrhotic cardiomyopathy, as well as the emerging field and association between non-alcoholic fatty liver disease and cardiovascular disease.

Dr. Marc Klapholz of Rutgers University, Newark, N.J., explains the latest developments in portopulmonary arterial hypertension, hepatopulmonary syndrome, and cirrhotic cardiomyopathy, as well as the emerging field and association between non-alcoholic fatty liver disease and cardiovascular disease.
AT DIGESTIVE DISEASES: NEW ADVANCES
One-time, universal hepatitis C testing cost effective, researchers say
Universal one-time screening for hepatitis C virus infection is cost effective, compared with birth cohort screening alone, according to the results of a study published in Clinical Gastroenterology and Hepatology.
The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force recommend testing all individuals born between 1945 and 1965 in addition to injection drug users and other high-risk individuals. But so-called birth cohort screening does not reflect the recent spike in hepatitis C virus (HCV) cases among younger persons in the United States, nor the current recommendation to treat nearly all chronic HCV cases, wrote Mark H. Eckman, MD, of the University of Cincinnati, and his associates.
Using a computer program called Decision Maker, they modeled the cost-effectiveness of universal one-time testing, birth cohort screening, and no screening based on quality-adjusted life-years (QALYS) and 2017 U.S. dollars. They assumed that all HCV-infected patients were treatment naive, treatment eligible, and asymptomatic (for example, had no decompensated cirrhosis). They used efficacy data from the ASTRAL trials of sofosbuvir-velpatasvir as well as the ENDURANCE, SURVEYOR, and EXPEDITION trials of glecaprevir-pibrentasvir. In the model, patients who did not achieve a sustained viral response to treatment went on to complete a 12-week triple direct-acting antiviral (DAA) regimen (sofosbuvir, velpatasvir, and voxilaprevir).
Based on these assumptions, universal one-time screening and treatment of infected individuals cost less than $50,000 per QALY gained, making it highly cost effective, compared with no screening, the investigators wrote. Universal screening also was highly cost effective when compared with birth cohort screening, costing $11,378 for each QALY gained.
“Analyses performed during the era of first-generation DAAs and interferon-based treatment regimens found birth-cohort screening to be ‘cost effective,’ ” the researchers wrote. “However, the availability of a new generation of highly effective, non–interferon-based oral regimens, with fewer side effects and shorter treatment courses, has altered the dynamic around the question of screening.” They pointed to another recent study in which universal one-time HCV testing was more cost effective than birth cohort screening.
Such findings have spurred experts to revisit guidelines on HCV screening, but universal testing is controversial when some states, counties, and communities have a low HCV prevalence. In the model, universal one-time HCV screening was cost effective (less than $50,000 per QALY gained), compared with birth cohort screening as long as prevalence exceeded 0.07% among adults not born between 1945 and 1965. The current prevalence estimate in this group is 0.29%, which is probably low because it does not account for the rising incidence among younger adults, the researchers wrote. In an ideal world, all clinics and hospitals would implement an HCV testing program, but in the real world of scarce resources, “data regarding the cost-effectiveness threshold can guide local policy decisions by directing testing services to settings in which they generate sufficient benefit for the cost.”
Partial funding came from the National Foundation for the Centers for Disease Control and Prevention (CDC Foundation), with funding provided through multiple donors to the CDC Foundation’s Viral Hepatitis Action Coalition. Dr. Eckman reported grant support from Merck and one coinvestigator reported ties to AbbVie, Gilead, Merck, and several other pharmaceutical companies.
SOURCE: Eckman MH et al. Clin Gastroenterol Hepatol. 2018 Sep 7. doi: 10.1016/j.cgh.2018.08.080.
Universal one-time screening for hepatitis C virus infection is cost effective, compared with birth cohort screening alone, according to the results of a study published in Clinical Gastroenterology and Hepatology.
The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force recommend testing all individuals born between 1945 and 1965 in addition to injection drug users and other high-risk individuals. But so-called birth cohort screening does not reflect the recent spike in hepatitis C virus (HCV) cases among younger persons in the United States, nor the current recommendation to treat nearly all chronic HCV cases, wrote Mark H. Eckman, MD, of the University of Cincinnati, and his associates.
Using a computer program called Decision Maker, they modeled the cost-effectiveness of universal one-time testing, birth cohort screening, and no screening based on quality-adjusted life-years (QALYS) and 2017 U.S. dollars. They assumed that all HCV-infected patients were treatment naive, treatment eligible, and asymptomatic (for example, had no decompensated cirrhosis). They used efficacy data from the ASTRAL trials of sofosbuvir-velpatasvir as well as the ENDURANCE, SURVEYOR, and EXPEDITION trials of glecaprevir-pibrentasvir. In the model, patients who did not achieve a sustained viral response to treatment went on to complete a 12-week triple direct-acting antiviral (DAA) regimen (sofosbuvir, velpatasvir, and voxilaprevir).
Based on these assumptions, universal one-time screening and treatment of infected individuals cost less than $50,000 per QALY gained, making it highly cost effective, compared with no screening, the investigators wrote. Universal screening also was highly cost effective when compared with birth cohort screening, costing $11,378 for each QALY gained.
“Analyses performed during the era of first-generation DAAs and interferon-based treatment regimens found birth-cohort screening to be ‘cost effective,’ ” the researchers wrote. “However, the availability of a new generation of highly effective, non–interferon-based oral regimens, with fewer side effects and shorter treatment courses, has altered the dynamic around the question of screening.” They pointed to another recent study in which universal one-time HCV testing was more cost effective than birth cohort screening.
Such findings have spurred experts to revisit guidelines on HCV screening, but universal testing is controversial when some states, counties, and communities have a low HCV prevalence. In the model, universal one-time HCV screening was cost effective (less than $50,000 per QALY gained), compared with birth cohort screening as long as prevalence exceeded 0.07% among adults not born between 1945 and 1965. The current prevalence estimate in this group is 0.29%, which is probably low because it does not account for the rising incidence among younger adults, the researchers wrote. In an ideal world, all clinics and hospitals would implement an HCV testing program, but in the real world of scarce resources, “data regarding the cost-effectiveness threshold can guide local policy decisions by directing testing services to settings in which they generate sufficient benefit for the cost.”
Partial funding came from the National Foundation for the Centers for Disease Control and Prevention (CDC Foundation), with funding provided through multiple donors to the CDC Foundation’s Viral Hepatitis Action Coalition. Dr. Eckman reported grant support from Merck and one coinvestigator reported ties to AbbVie, Gilead, Merck, and several other pharmaceutical companies.
SOURCE: Eckman MH et al. Clin Gastroenterol Hepatol. 2018 Sep 7. doi: 10.1016/j.cgh.2018.08.080.
Universal one-time screening for hepatitis C virus infection is cost effective, compared with birth cohort screening alone, according to the results of a study published in Clinical Gastroenterology and Hepatology.
The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force recommend testing all individuals born between 1945 and 1965 in addition to injection drug users and other high-risk individuals. But so-called birth cohort screening does not reflect the recent spike in hepatitis C virus (HCV) cases among younger persons in the United States, nor the current recommendation to treat nearly all chronic HCV cases, wrote Mark H. Eckman, MD, of the University of Cincinnati, and his associates.
Using a computer program called Decision Maker, they modeled the cost-effectiveness of universal one-time testing, birth cohort screening, and no screening based on quality-adjusted life-years (QALYS) and 2017 U.S. dollars. They assumed that all HCV-infected patients were treatment naive, treatment eligible, and asymptomatic (for example, had no decompensated cirrhosis). They used efficacy data from the ASTRAL trials of sofosbuvir-velpatasvir as well as the ENDURANCE, SURVEYOR, and EXPEDITION trials of glecaprevir-pibrentasvir. In the model, patients who did not achieve a sustained viral response to treatment went on to complete a 12-week triple direct-acting antiviral (DAA) regimen (sofosbuvir, velpatasvir, and voxilaprevir).
Based on these assumptions, universal one-time screening and treatment of infected individuals cost less than $50,000 per QALY gained, making it highly cost effective, compared with no screening, the investigators wrote. Universal screening also was highly cost effective when compared with birth cohort screening, costing $11,378 for each QALY gained.
“Analyses performed during the era of first-generation DAAs and interferon-based treatment regimens found birth-cohort screening to be ‘cost effective,’ ” the researchers wrote. “However, the availability of a new generation of highly effective, non–interferon-based oral regimens, with fewer side effects and shorter treatment courses, has altered the dynamic around the question of screening.” They pointed to another recent study in which universal one-time HCV testing was more cost effective than birth cohort screening.
Such findings have spurred experts to revisit guidelines on HCV screening, but universal testing is controversial when some states, counties, and communities have a low HCV prevalence. In the model, universal one-time HCV screening was cost effective (less than $50,000 per QALY gained), compared with birth cohort screening as long as prevalence exceeded 0.07% among adults not born between 1945 and 1965. The current prevalence estimate in this group is 0.29%, which is probably low because it does not account for the rising incidence among younger adults, the researchers wrote. In an ideal world, all clinics and hospitals would implement an HCV testing program, but in the real world of scarce resources, “data regarding the cost-effectiveness threshold can guide local policy decisions by directing testing services to settings in which they generate sufficient benefit for the cost.”
Partial funding came from the National Foundation for the Centers for Disease Control and Prevention (CDC Foundation), with funding provided through multiple donors to the CDC Foundation’s Viral Hepatitis Action Coalition. Dr. Eckman reported grant support from Merck and one coinvestigator reported ties to AbbVie, Gilead, Merck, and several other pharmaceutical companies.
SOURCE: Eckman MH et al. Clin Gastroenterol Hepatol. 2018 Sep 7. doi: 10.1016/j.cgh.2018.08.080.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Women survive more often than men do when hospitalized with cirrhosis
Women hospitalized with cirrhosis are less likely to die in the hospital than are men, according to a retrospective analysis of more than half a million patients.
Although women more often had infections and comorbidities, men more often had liver decompensation, which contributed most significantly to their higher mortality rate, reported lead author Jessica Rubin, MD, of the University of California, San Francisco, and her colleagues.
Their findings add to an existing body of knowledge about sex-related differences in chronic liver disease. Women are less likely to develop chronic liver disease; however, when women do develop disease, it often follows a unique clinical course, with milder early disease followed by more severe end-stage disease, meaning many women are too sick for a transplant, or die on the waiting list.
“The reasons behind this ‘reversal’ in [sex] disparities is unknown,” the investigators wrote in Journal of Clinical Gastroenterology.
Considering recent findings that showed a correlation between hospitalization and mortality rates in chronic liver disease, the investigators believed that a comparison of hospital-related outcomes in men and women could explain why women apparently fare worse when dealing with end-stage disease.
The retrospective, cross-sectional study involved 553,017 patients (median age, 57 years) who were hospitalized for cirrhosis between 2009 and 2013. Data were drawn from the National Inpatient Sample (NIS). Inpatient mortality was the primary outcome.
In agreement with previous findings, the minority of patients were women (39%). Against expectations, however, women had a significantly lower mortality rate than that of men (5.7% vs. 6.4%; multivariable analysis odds ratio, 0.86). Better survival was associated with lower rates of decompensation (Baveno IV criteria; 34% vs. 38.8%) and other cirrhosis complications, such as hepatorenal syndrome, variceal bleeding, ascites, and spontaneous bacterial peritonitis. The only cirrhosis complication more common in women than men was hepatic encephalopathy (17.8% vs. 16.8%). Owing to fewer complications, fewer women required liver-related interventions, including transjugular intrahepatic portosystemic shunt (0.8% vs. 1.0%), upper endoscopy (12.8% vs. 13.0%), or paracentesis (17.6% vs. 20.6%).
While less frequent complications and a lower mortality rate might suggest that women were admitted with better overall clinical pictures, not all data supported this conclusion. For instance, women were more likely to have noncirrhosis comorbidities, including diabetes, hypertension, heart failure, stroke, and cancer. Furthermore, women had a higher rate of acute bacterial infection than that of men (34.9% vs. 28.2%), although this disparity should be considered in light of urinary tract infections (UTIs), which were significantly more common among women (18.8% vs. 8.0%).
“Interestingly, infections were a stronger predictor of inpatient mortality in women than men,” the investigators wrote. “Despite this, women in our cohort were less likely to die in the hospital than men.”
Additional analysis revealed etiological differences that may have contributed to differences in mortality rates. For instance, women less often had liver disease due to viral hepatitis (27.6% vs. 35.2%) or alcohol (24.1% vs. 38.7%). In contrast, women more often had autoimmune hepatitis (2.5% vs. 0.4%) or cirrhosis due to unspecified or miscellaneous reasons (45.7% vs. 25.7%).
“Our data suggest that differential rates of ongoing liver injury – including by cofactors such as active alcohol use – explain some but not all of the [sex] difference we observed in hepatic decompensation,” the investigators wrote, before redirecting focus to a clearer clinical finding. “The poor prognosis of decompensated cirrhosis ... provides a reasonable explanation for the higher rates of in-hospital mortality seen among men versus women,” they concluded.
Considering the surprising findings and previously known sex disparities, Dr. Rubin and her colleagues suggested that more research in this area is needed, along with efforts to deliver sex-appropriate care.
“The development of [sex]-specific cirrhosis management programs – focused on interventions to manage the interaction between cirrhosis and other common comorbidities, improving physical function both before and during hospitalization, and postacute discharge programs to facilitate resumption of independent living – would target differential needs of women and men living with cirrhosis, with the ultimate goal of improving long-term outcomes in these patients,” the investigators wrote.
The study was funded by a National Institute on Aging Paul B. Beeson Career Development Award in Aging and a National Institute of Diabetes and Digestive and Kidney Diseases National Research Service Award hepatology training grant. The investigators declared no conflicts of interest.
SOURCE: Rubin et al. J Clin Gastroenterol. 2019 Feb 22. doi: 10.1097/MCG.0000000000001192.
Women hospitalized with cirrhosis are less likely to die in the hospital than are men, according to a retrospective analysis of more than half a million patients.
Although women more often had infections and comorbidities, men more often had liver decompensation, which contributed most significantly to their higher mortality rate, reported lead author Jessica Rubin, MD, of the University of California, San Francisco, and her colleagues.
Their findings add to an existing body of knowledge about sex-related differences in chronic liver disease. Women are less likely to develop chronic liver disease; however, when women do develop disease, it often follows a unique clinical course, with milder early disease followed by more severe end-stage disease, meaning many women are too sick for a transplant, or die on the waiting list.
“The reasons behind this ‘reversal’ in [sex] disparities is unknown,” the investigators wrote in Journal of Clinical Gastroenterology.
Considering recent findings that showed a correlation between hospitalization and mortality rates in chronic liver disease, the investigators believed that a comparison of hospital-related outcomes in men and women could explain why women apparently fare worse when dealing with end-stage disease.
The retrospective, cross-sectional study involved 553,017 patients (median age, 57 years) who were hospitalized for cirrhosis between 2009 and 2013. Data were drawn from the National Inpatient Sample (NIS). Inpatient mortality was the primary outcome.
In agreement with previous findings, the minority of patients were women (39%). Against expectations, however, women had a significantly lower mortality rate than that of men (5.7% vs. 6.4%; multivariable analysis odds ratio, 0.86). Better survival was associated with lower rates of decompensation (Baveno IV criteria; 34% vs. 38.8%) and other cirrhosis complications, such as hepatorenal syndrome, variceal bleeding, ascites, and spontaneous bacterial peritonitis. The only cirrhosis complication more common in women than men was hepatic encephalopathy (17.8% vs. 16.8%). Owing to fewer complications, fewer women required liver-related interventions, including transjugular intrahepatic portosystemic shunt (0.8% vs. 1.0%), upper endoscopy (12.8% vs. 13.0%), or paracentesis (17.6% vs. 20.6%).
While less frequent complications and a lower mortality rate might suggest that women were admitted with better overall clinical pictures, not all data supported this conclusion. For instance, women were more likely to have noncirrhosis comorbidities, including diabetes, hypertension, heart failure, stroke, and cancer. Furthermore, women had a higher rate of acute bacterial infection than that of men (34.9% vs. 28.2%), although this disparity should be considered in light of urinary tract infections (UTIs), which were significantly more common among women (18.8% vs. 8.0%).
“Interestingly, infections were a stronger predictor of inpatient mortality in women than men,” the investigators wrote. “Despite this, women in our cohort were less likely to die in the hospital than men.”
Additional analysis revealed etiological differences that may have contributed to differences in mortality rates. For instance, women less often had liver disease due to viral hepatitis (27.6% vs. 35.2%) or alcohol (24.1% vs. 38.7%). In contrast, women more often had autoimmune hepatitis (2.5% vs. 0.4%) or cirrhosis due to unspecified or miscellaneous reasons (45.7% vs. 25.7%).
“Our data suggest that differential rates of ongoing liver injury – including by cofactors such as active alcohol use – explain some but not all of the [sex] difference we observed in hepatic decompensation,” the investigators wrote, before redirecting focus to a clearer clinical finding. “The poor prognosis of decompensated cirrhosis ... provides a reasonable explanation for the higher rates of in-hospital mortality seen among men versus women,” they concluded.
Considering the surprising findings and previously known sex disparities, Dr. Rubin and her colleagues suggested that more research in this area is needed, along with efforts to deliver sex-appropriate care.
“The development of [sex]-specific cirrhosis management programs – focused on interventions to manage the interaction between cirrhosis and other common comorbidities, improving physical function both before and during hospitalization, and postacute discharge programs to facilitate resumption of independent living – would target differential needs of women and men living with cirrhosis, with the ultimate goal of improving long-term outcomes in these patients,” the investigators wrote.
The study was funded by a National Institute on Aging Paul B. Beeson Career Development Award in Aging and a National Institute of Diabetes and Digestive and Kidney Diseases National Research Service Award hepatology training grant. The investigators declared no conflicts of interest.
SOURCE: Rubin et al. J Clin Gastroenterol. 2019 Feb 22. doi: 10.1097/MCG.0000000000001192.
Women hospitalized with cirrhosis are less likely to die in the hospital than are men, according to a retrospective analysis of more than half a million patients.
Although women more often had infections and comorbidities, men more often had liver decompensation, which contributed most significantly to their higher mortality rate, reported lead author Jessica Rubin, MD, of the University of California, San Francisco, and her colleagues.
Their findings add to an existing body of knowledge about sex-related differences in chronic liver disease. Women are less likely to develop chronic liver disease; however, when women do develop disease, it often follows a unique clinical course, with milder early disease followed by more severe end-stage disease, meaning many women are too sick for a transplant, or die on the waiting list.
“The reasons behind this ‘reversal’ in [sex] disparities is unknown,” the investigators wrote in Journal of Clinical Gastroenterology.
Considering recent findings that showed a correlation between hospitalization and mortality rates in chronic liver disease, the investigators believed that a comparison of hospital-related outcomes in men and women could explain why women apparently fare worse when dealing with end-stage disease.
The retrospective, cross-sectional study involved 553,017 patients (median age, 57 years) who were hospitalized for cirrhosis between 2009 and 2013. Data were drawn from the National Inpatient Sample (NIS). Inpatient mortality was the primary outcome.
In agreement with previous findings, the minority of patients were women (39%). Against expectations, however, women had a significantly lower mortality rate than that of men (5.7% vs. 6.4%; multivariable analysis odds ratio, 0.86). Better survival was associated with lower rates of decompensation (Baveno IV criteria; 34% vs. 38.8%) and other cirrhosis complications, such as hepatorenal syndrome, variceal bleeding, ascites, and spontaneous bacterial peritonitis. The only cirrhosis complication more common in women than men was hepatic encephalopathy (17.8% vs. 16.8%). Owing to fewer complications, fewer women required liver-related interventions, including transjugular intrahepatic portosystemic shunt (0.8% vs. 1.0%), upper endoscopy (12.8% vs. 13.0%), or paracentesis (17.6% vs. 20.6%).
While less frequent complications and a lower mortality rate might suggest that women were admitted with better overall clinical pictures, not all data supported this conclusion. For instance, women were more likely to have noncirrhosis comorbidities, including diabetes, hypertension, heart failure, stroke, and cancer. Furthermore, women had a higher rate of acute bacterial infection than that of men (34.9% vs. 28.2%), although this disparity should be considered in light of urinary tract infections (UTIs), which were significantly more common among women (18.8% vs. 8.0%).
“Interestingly, infections were a stronger predictor of inpatient mortality in women than men,” the investigators wrote. “Despite this, women in our cohort were less likely to die in the hospital than men.”
Additional analysis revealed etiological differences that may have contributed to differences in mortality rates. For instance, women less often had liver disease due to viral hepatitis (27.6% vs. 35.2%) or alcohol (24.1% vs. 38.7%). In contrast, women more often had autoimmune hepatitis (2.5% vs. 0.4%) or cirrhosis due to unspecified or miscellaneous reasons (45.7% vs. 25.7%).
“Our data suggest that differential rates of ongoing liver injury – including by cofactors such as active alcohol use – explain some but not all of the [sex] difference we observed in hepatic decompensation,” the investigators wrote, before redirecting focus to a clearer clinical finding. “The poor prognosis of decompensated cirrhosis ... provides a reasonable explanation for the higher rates of in-hospital mortality seen among men versus women,” they concluded.
Considering the surprising findings and previously known sex disparities, Dr. Rubin and her colleagues suggested that more research in this area is needed, along with efforts to deliver sex-appropriate care.
“The development of [sex]-specific cirrhosis management programs – focused on interventions to manage the interaction between cirrhosis and other common comorbidities, improving physical function both before and during hospitalization, and postacute discharge programs to facilitate resumption of independent living – would target differential needs of women and men living with cirrhosis, with the ultimate goal of improving long-term outcomes in these patients,” the investigators wrote.
The study was funded by a National Institute on Aging Paul B. Beeson Career Development Award in Aging and a National Institute of Diabetes and Digestive and Kidney Diseases National Research Service Award hepatology training grant. The investigators declared no conflicts of interest.
SOURCE: Rubin et al. J Clin Gastroenterol. 2019 Feb 22. doi: 10.1097/MCG.0000000000001192.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
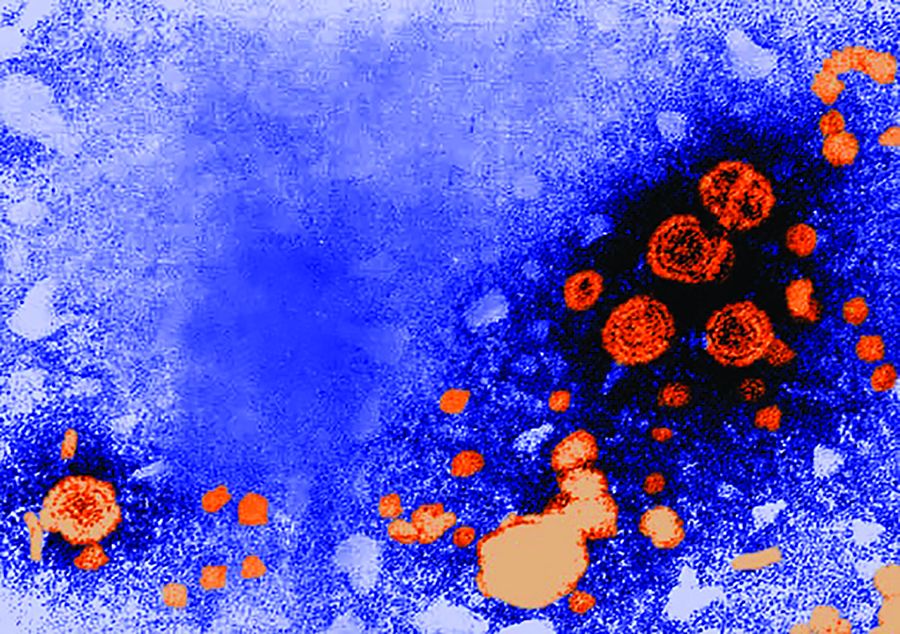
Developing an HCV vaccine faces significant challenges
The development of a prophylactic hepatitis C vaccine faces significant challenges, according to a Justin R. Bailey, MD, of Johns Hopkins University, Baltimore, and his colleagues.
Barriers to developing a prophylactic HCV vaccine include the great diversity of the virus, the limited models that are available for vaccine testing, and the currently incomplete understanding of protective immune responses, according to their review published in Gastroenterology.
Functionally, the inability to culture HCV, until recently, and continuing limitations of HCV culture systems pose challenges to standard production of a live-attenuated or inactivated whole HCV vaccine. In addition, there is the risk of causing HCV infection with live-attenuated vaccines.
On a practical level for all forms of vaccine development, a principal challenge “is the extraordinary genetic diversity of the virus. With 7 known genotypes and more than 80 subtypes, the genetic diversity of HCV exceeds that of human immunodeficiency virus-1,” according to the authors (Gastroenterology 2019;156[2]:418-30).
With regard to vaccine testing, there are also significant difficulties: There is a lack of in vitro systems and immunocompetent small-animal models useful for determining whether vaccination induces protective immunity. Although a use of an HCV-like virus, the rat Hepacivirus, provides a new small-animal model for vaccine testing, this virus has limited sequence analogy to HCV.
The development of immunity to HCV in humans is complex and under broad investigation. However, decades of research have revealed that HCV-specific CD4+ helper T cells, CD8+ cytotoxic T cells, and antibodies all play a role in protection against persistent HCV infection, according to the authors, and vaccine strategies to induce all three adaptive immune responses are in development.
“A prophylactic HCV vaccine is an important part of a successful strategy for global control. Although development is not easy, the quest is a worthy challenge,” the authors concluded.
Dr. Bailey and his colleagues reported that they had no conflicts.
SOURCE: Bailey JR et al. Gastroenterology 2019(2);156:418-30.
The development of a prophylactic hepatitis C vaccine faces significant challenges, according to a Justin R. Bailey, MD, of Johns Hopkins University, Baltimore, and his colleagues.
Barriers to developing a prophylactic HCV vaccine include the great diversity of the virus, the limited models that are available for vaccine testing, and the currently incomplete understanding of protective immune responses, according to their review published in Gastroenterology.
Functionally, the inability to culture HCV, until recently, and continuing limitations of HCV culture systems pose challenges to standard production of a live-attenuated or inactivated whole HCV vaccine. In addition, there is the risk of causing HCV infection with live-attenuated vaccines.
On a practical level for all forms of vaccine development, a principal challenge “is the extraordinary genetic diversity of the virus. With 7 known genotypes and more than 80 subtypes, the genetic diversity of HCV exceeds that of human immunodeficiency virus-1,” according to the authors (Gastroenterology 2019;156[2]:418-30).
With regard to vaccine testing, there are also significant difficulties: There is a lack of in vitro systems and immunocompetent small-animal models useful for determining whether vaccination induces protective immunity. Although a use of an HCV-like virus, the rat Hepacivirus, provides a new small-animal model for vaccine testing, this virus has limited sequence analogy to HCV.
The development of immunity to HCV in humans is complex and under broad investigation. However, decades of research have revealed that HCV-specific CD4+ helper T cells, CD8+ cytotoxic T cells, and antibodies all play a role in protection against persistent HCV infection, according to the authors, and vaccine strategies to induce all three adaptive immune responses are in development.
“A prophylactic HCV vaccine is an important part of a successful strategy for global control. Although development is not easy, the quest is a worthy challenge,” the authors concluded.
Dr. Bailey and his colleagues reported that they had no conflicts.
SOURCE: Bailey JR et al. Gastroenterology 2019(2);156:418-30.
The development of a prophylactic hepatitis C vaccine faces significant challenges, according to a Justin R. Bailey, MD, of Johns Hopkins University, Baltimore, and his colleagues.
Barriers to developing a prophylactic HCV vaccine include the great diversity of the virus, the limited models that are available for vaccine testing, and the currently incomplete understanding of protective immune responses, according to their review published in Gastroenterology.
Functionally, the inability to culture HCV, until recently, and continuing limitations of HCV culture systems pose challenges to standard production of a live-attenuated or inactivated whole HCV vaccine. In addition, there is the risk of causing HCV infection with live-attenuated vaccines.
On a practical level for all forms of vaccine development, a principal challenge “is the extraordinary genetic diversity of the virus. With 7 known genotypes and more than 80 subtypes, the genetic diversity of HCV exceeds that of human immunodeficiency virus-1,” according to the authors (Gastroenterology 2019;156[2]:418-30).
With regard to vaccine testing, there are also significant difficulties: There is a lack of in vitro systems and immunocompetent small-animal models useful for determining whether vaccination induces protective immunity. Although a use of an HCV-like virus, the rat Hepacivirus, provides a new small-animal model for vaccine testing, this virus has limited sequence analogy to HCV.
The development of immunity to HCV in humans is complex and under broad investigation. However, decades of research have revealed that HCV-specific CD4+ helper T cells, CD8+ cytotoxic T cells, and antibodies all play a role in protection against persistent HCV infection, according to the authors, and vaccine strategies to induce all three adaptive immune responses are in development.
“A prophylactic HCV vaccine is an important part of a successful strategy for global control. Although development is not easy, the quest is a worthy challenge,” the authors concluded.
Dr. Bailey and his colleagues reported that they had no conflicts.
SOURCE: Bailey JR et al. Gastroenterology 2019(2);156:418-30.
FROM GASTROENTEROLOGY
Possible biomarkers found for progression to liver cancer in chronic HCV infection
according to the results of a biochemical analysis of human blood samples performed by PhD student Paywast J. Jalal of the University of Sulaimani (Iraq) and colleagues.
Archived HCV-positive serum samples, including those from 31 patients who had developed HCC, were retrieved from the Trent HCV clinical cohort. They were compared with each other over time and against samples from HCV-infected individuals in the cohort who did not develop HCC. In addition, HCV-negative serum samples were obtained commercially and assessed identically. Circulating liver-expressed lectins, ficolin-2, ficolin-3, and MBL were all examined as potential biomarkers for the development of HCC, the authors wrote in Virology.
Binding of ficolin-3 to reference ligands was greater in chronic HCV infection, while ficolin-2 and MBL were significantly elevated in individuals who develop HCC, compared with HCV-infected individuals without HCC. Ficolin-2 and MBL were found to be elevated at 1 and 3 years prior to HCC diagnosis, respectively, suggesting they could be used as prognostic serum markers for the development of HCC.
“The strong evidence for an association between elevated MBL binding activity and the development of HCC is supportive for a larger prospective study of these biomarkers in HCV-induced liver cancer,” the researchers concluded.
This study was funded by a split-site PhD scholarship between the University of Sulaimani and the University of Nottingham (England). The authors reported they had no conflicts.
SOURCE: Jalal PJ et al. Virology. 2019;530:99-106.
according to the results of a biochemical analysis of human blood samples performed by PhD student Paywast J. Jalal of the University of Sulaimani (Iraq) and colleagues.
Archived HCV-positive serum samples, including those from 31 patients who had developed HCC, were retrieved from the Trent HCV clinical cohort. They were compared with each other over time and against samples from HCV-infected individuals in the cohort who did not develop HCC. In addition, HCV-negative serum samples were obtained commercially and assessed identically. Circulating liver-expressed lectins, ficolin-2, ficolin-3, and MBL were all examined as potential biomarkers for the development of HCC, the authors wrote in Virology.
Binding of ficolin-3 to reference ligands was greater in chronic HCV infection, while ficolin-2 and MBL were significantly elevated in individuals who develop HCC, compared with HCV-infected individuals without HCC. Ficolin-2 and MBL were found to be elevated at 1 and 3 years prior to HCC diagnosis, respectively, suggesting they could be used as prognostic serum markers for the development of HCC.
“The strong evidence for an association between elevated MBL binding activity and the development of HCC is supportive for a larger prospective study of these biomarkers in HCV-induced liver cancer,” the researchers concluded.
This study was funded by a split-site PhD scholarship between the University of Sulaimani and the University of Nottingham (England). The authors reported they had no conflicts.
SOURCE: Jalal PJ et al. Virology. 2019;530:99-106.
according to the results of a biochemical analysis of human blood samples performed by PhD student Paywast J. Jalal of the University of Sulaimani (Iraq) and colleagues.
Archived HCV-positive serum samples, including those from 31 patients who had developed HCC, were retrieved from the Trent HCV clinical cohort. They were compared with each other over time and against samples from HCV-infected individuals in the cohort who did not develop HCC. In addition, HCV-negative serum samples were obtained commercially and assessed identically. Circulating liver-expressed lectins, ficolin-2, ficolin-3, and MBL were all examined as potential biomarkers for the development of HCC, the authors wrote in Virology.
Binding of ficolin-3 to reference ligands was greater in chronic HCV infection, while ficolin-2 and MBL were significantly elevated in individuals who develop HCC, compared with HCV-infected individuals without HCC. Ficolin-2 and MBL were found to be elevated at 1 and 3 years prior to HCC diagnosis, respectively, suggesting they could be used as prognostic serum markers for the development of HCC.
“The strong evidence for an association between elevated MBL binding activity and the development of HCC is supportive for a larger prospective study of these biomarkers in HCV-induced liver cancer,” the researchers concluded.
This study was funded by a split-site PhD scholarship between the University of Sulaimani and the University of Nottingham (England). The authors reported they had no conflicts.
SOURCE: Jalal PJ et al. Virology. 2019;530:99-106.
FROM VIROLOGY
Novel capsid assembly modulator shows promise in HBV
For adults with chronic hepatitis B virus infection, treatment with a novel investigational capsid assembly modulator was well tolerated and showed antiviral activity against HBV, according to the results of a phase 1 study of 73 patients.
“Substantial and correlated reductions in serum HBV DNA and HBV RNA levels were observed consistently with the higher-dose cohorts and were notably greatest for combination treatment with NVR 3-778 and pegIFN [pegylated interferon],” Man Fung Yuen, MD, of the University of Hong Kong, and his associates wrote in a report published in Gastroenterology. Hence, this first-in-class capsid assembly modulator might help prolong treatment responses, “most likely as a component of new combination treatment regimens for HBV-infected patients.” However, one patient developed severe rash immediately after completing treatment that took 6 months of intensive outpatient treatment to resolve, they noted.
Chronic viral hepatitis due to HBV is a major cause of early death worldwide, and new therapies are needed to help prevent severe liver disease and liver death from this infection. Current treatments for HBV infection consist of nucleoside or nucleotide analogs or pegylated interferon. These suppress HBV replication in many patients, but most patients do not achieve durable responses. Consequently, most patients require long-term treatment with HBV nucleosides and nucleotide analogs, which they may find difficult to tolerate or adhere to and to which their infections can become resistant, the researchers said.
The HBV virion contains a viral core protein (HBc) that is required to encapsidate viral polymerase and pregenomic HBV RNA into a nucleocapsid. To target this process, researchers developed NVR 3-778, a first-in-class, orally bioavailable small molecule that binds HBc so that HBc forms a defective capsid that lacks nuclear material. Hence, NVR 3-778 is intended to stop the production of HBV nucleocapsids and keep infected cells from releasing the enveloped infectious viral particles that perpetuate HBV infection.
To assess the safety, pharmacokinetics, and antiviral activity of NVR 3-778, the researchers conducted a phase 1 study of 73 patients with chronic HBV infection who tested positive for hepatitis B e-antigen (HBeAg) and had no detectable cirrhosis. Patients were randomly assigned to receive oral NVR 3-778 (100 mg, 200 mg, or 400 mg daily or 600 mg or 1,000 mg twice daily ) or placebo for 28 days. Some patients received combination therapy with pegylated interferon plus either NVR 3-778 (600 mg twice daily) or placebo. Treatment was generally well tolerated, and adverse events were usually mild and deemed unrelated to therapy. No patient stopped treatment for adverse effects.
The only serious adverse event in the study consisted of grade 3 rash that developed in a 42-year-old male after 22 days of treatment at the lowest dose of NVR 3-778 (100 mg per day). This patient completed treatment and ultimately developed a severe papulovesicular rash with a predominantly acral distribution over the hands, arm, side of neck, and one leg (palmar plantar erythrodysesthesia), the researchers said. “There were no perioral or mucosal lesions, no ecchymotic skin involvement, no bullae, and no systemic manifestations or hematological abnormalities,” they wrote. “The rash was subsequently managed with a psoriasis-like treatment regimen of psoralen, ultraviolet light, and topical steroid ointment during outpatient follow-up and resolved after approximately 6 months.”
Another three cases of “minor” skin rash were considered probably related to treatment in the cohort that received 600 mg NVR 3-778 b.i.d. plus pegylated interferon, the investigators said. Two additional cases of mild rash were deemed unrelated to treatment.
“The observed reductions in HBV RNA confirmed the novel mechanism of NVR 3-778,” the researchers concluded. “This class of compounds can also inhibit replenishment of intranuclear covalently closed circular DNA over time and may have immunomodulatory properties.” Longer treatment periods would be needed to study these mechanisms and to quantify reductions in serum HBsAg and HBeAG, they noted.
Novira Therapeutics developed NVR 3-778 and is a Janssen Pharmaceutical Company. Janssen provided funding for editorial support. Dr. Yuen disclosed relationships with AbbVie, Biocartis, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Ionis, Roche, Vir Biotechnology, and several other pharmaceutical companies. Other coinvestigators disclosed ties to pharmaceutical companies; eight reported employment by Novira or a Janssen company.
SOURCE: Yuen MF et al. Gastroenterology. 2019 Jan 5. doi: 10.1053/j.gastro.2018.12.023.
For adults with chronic hepatitis B virus infection, treatment with a novel investigational capsid assembly modulator was well tolerated and showed antiviral activity against HBV, according to the results of a phase 1 study of 73 patients.
“Substantial and correlated reductions in serum HBV DNA and HBV RNA levels were observed consistently with the higher-dose cohorts and were notably greatest for combination treatment with NVR 3-778 and pegIFN [pegylated interferon],” Man Fung Yuen, MD, of the University of Hong Kong, and his associates wrote in a report published in Gastroenterology. Hence, this first-in-class capsid assembly modulator might help prolong treatment responses, “most likely as a component of new combination treatment regimens for HBV-infected patients.” However, one patient developed severe rash immediately after completing treatment that took 6 months of intensive outpatient treatment to resolve, they noted.
Chronic viral hepatitis due to HBV is a major cause of early death worldwide, and new therapies are needed to help prevent severe liver disease and liver death from this infection. Current treatments for HBV infection consist of nucleoside or nucleotide analogs or pegylated interferon. These suppress HBV replication in many patients, but most patients do not achieve durable responses. Consequently, most patients require long-term treatment with HBV nucleosides and nucleotide analogs, which they may find difficult to tolerate or adhere to and to which their infections can become resistant, the researchers said.
The HBV virion contains a viral core protein (HBc) that is required to encapsidate viral polymerase and pregenomic HBV RNA into a nucleocapsid. To target this process, researchers developed NVR 3-778, a first-in-class, orally bioavailable small molecule that binds HBc so that HBc forms a defective capsid that lacks nuclear material. Hence, NVR 3-778 is intended to stop the production of HBV nucleocapsids and keep infected cells from releasing the enveloped infectious viral particles that perpetuate HBV infection.
To assess the safety, pharmacokinetics, and antiviral activity of NVR 3-778, the researchers conducted a phase 1 study of 73 patients with chronic HBV infection who tested positive for hepatitis B e-antigen (HBeAg) and had no detectable cirrhosis. Patients were randomly assigned to receive oral NVR 3-778 (100 mg, 200 mg, or 400 mg daily or 600 mg or 1,000 mg twice daily ) or placebo for 28 days. Some patients received combination therapy with pegylated interferon plus either NVR 3-778 (600 mg twice daily) or placebo. Treatment was generally well tolerated, and adverse events were usually mild and deemed unrelated to therapy. No patient stopped treatment for adverse effects.
The only serious adverse event in the study consisted of grade 3 rash that developed in a 42-year-old male after 22 days of treatment at the lowest dose of NVR 3-778 (100 mg per day). This patient completed treatment and ultimately developed a severe papulovesicular rash with a predominantly acral distribution over the hands, arm, side of neck, and one leg (palmar plantar erythrodysesthesia), the researchers said. “There were no perioral or mucosal lesions, no ecchymotic skin involvement, no bullae, and no systemic manifestations or hematological abnormalities,” they wrote. “The rash was subsequently managed with a psoriasis-like treatment regimen of psoralen, ultraviolet light, and topical steroid ointment during outpatient follow-up and resolved after approximately 6 months.”
Another three cases of “minor” skin rash were considered probably related to treatment in the cohort that received 600 mg NVR 3-778 b.i.d. plus pegylated interferon, the investigators said. Two additional cases of mild rash were deemed unrelated to treatment.
“The observed reductions in HBV RNA confirmed the novel mechanism of NVR 3-778,” the researchers concluded. “This class of compounds can also inhibit replenishment of intranuclear covalently closed circular DNA over time and may have immunomodulatory properties.” Longer treatment periods would be needed to study these mechanisms and to quantify reductions in serum HBsAg and HBeAG, they noted.
Novira Therapeutics developed NVR 3-778 and is a Janssen Pharmaceutical Company. Janssen provided funding for editorial support. Dr. Yuen disclosed relationships with AbbVie, Biocartis, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Ionis, Roche, Vir Biotechnology, and several other pharmaceutical companies. Other coinvestigators disclosed ties to pharmaceutical companies; eight reported employment by Novira or a Janssen company.
SOURCE: Yuen MF et al. Gastroenterology. 2019 Jan 5. doi: 10.1053/j.gastro.2018.12.023.
For adults with chronic hepatitis B virus infection, treatment with a novel investigational capsid assembly modulator was well tolerated and showed antiviral activity against HBV, according to the results of a phase 1 study of 73 patients.
“Substantial and correlated reductions in serum HBV DNA and HBV RNA levels were observed consistently with the higher-dose cohorts and were notably greatest for combination treatment with NVR 3-778 and pegIFN [pegylated interferon],” Man Fung Yuen, MD, of the University of Hong Kong, and his associates wrote in a report published in Gastroenterology. Hence, this first-in-class capsid assembly modulator might help prolong treatment responses, “most likely as a component of new combination treatment regimens for HBV-infected patients.” However, one patient developed severe rash immediately after completing treatment that took 6 months of intensive outpatient treatment to resolve, they noted.
Chronic viral hepatitis due to HBV is a major cause of early death worldwide, and new therapies are needed to help prevent severe liver disease and liver death from this infection. Current treatments for HBV infection consist of nucleoside or nucleotide analogs or pegylated interferon. These suppress HBV replication in many patients, but most patients do not achieve durable responses. Consequently, most patients require long-term treatment with HBV nucleosides and nucleotide analogs, which they may find difficult to tolerate or adhere to and to which their infections can become resistant, the researchers said.
The HBV virion contains a viral core protein (HBc) that is required to encapsidate viral polymerase and pregenomic HBV RNA into a nucleocapsid. To target this process, researchers developed NVR 3-778, a first-in-class, orally bioavailable small molecule that binds HBc so that HBc forms a defective capsid that lacks nuclear material. Hence, NVR 3-778 is intended to stop the production of HBV nucleocapsids and keep infected cells from releasing the enveloped infectious viral particles that perpetuate HBV infection.
To assess the safety, pharmacokinetics, and antiviral activity of NVR 3-778, the researchers conducted a phase 1 study of 73 patients with chronic HBV infection who tested positive for hepatitis B e-antigen (HBeAg) and had no detectable cirrhosis. Patients were randomly assigned to receive oral NVR 3-778 (100 mg, 200 mg, or 400 mg daily or 600 mg or 1,000 mg twice daily ) or placebo for 28 days. Some patients received combination therapy with pegylated interferon plus either NVR 3-778 (600 mg twice daily) or placebo. Treatment was generally well tolerated, and adverse events were usually mild and deemed unrelated to therapy. No patient stopped treatment for adverse effects.
The only serious adverse event in the study consisted of grade 3 rash that developed in a 42-year-old male after 22 days of treatment at the lowest dose of NVR 3-778 (100 mg per day). This patient completed treatment and ultimately developed a severe papulovesicular rash with a predominantly acral distribution over the hands, arm, side of neck, and one leg (palmar plantar erythrodysesthesia), the researchers said. “There were no perioral or mucosal lesions, no ecchymotic skin involvement, no bullae, and no systemic manifestations or hematological abnormalities,” they wrote. “The rash was subsequently managed with a psoriasis-like treatment regimen of psoralen, ultraviolet light, and topical steroid ointment during outpatient follow-up and resolved after approximately 6 months.”
Another three cases of “minor” skin rash were considered probably related to treatment in the cohort that received 600 mg NVR 3-778 b.i.d. plus pegylated interferon, the investigators said. Two additional cases of mild rash were deemed unrelated to treatment.
“The observed reductions in HBV RNA confirmed the novel mechanism of NVR 3-778,” the researchers concluded. “This class of compounds can also inhibit replenishment of intranuclear covalently closed circular DNA over time and may have immunomodulatory properties.” Longer treatment periods would be needed to study these mechanisms and to quantify reductions in serum HBsAg and HBeAG, they noted.
Novira Therapeutics developed NVR 3-778 and is a Janssen Pharmaceutical Company. Janssen provided funding for editorial support. Dr. Yuen disclosed relationships with AbbVie, Biocartis, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Ionis, Roche, Vir Biotechnology, and several other pharmaceutical companies. Other coinvestigators disclosed ties to pharmaceutical companies; eight reported employment by Novira or a Janssen company.
SOURCE: Yuen MF et al. Gastroenterology. 2019 Jan 5. doi: 10.1053/j.gastro.2018.12.023.
FROM GASTROENTEROLOGY
Assessing liver fibrosis without biopsy in patients with HCV or NAFLD
Staging of liver fibrosis, important for determining prognosis in patients with chronic liver disease and for the need to start screening for complications of cirrhosis, was traditionally done only by liver biopsy. While biopsy is still the gold standard method to stage fibrosis, noninvasive methods have been developed that can also assess disease severity.
This article briefly reviews the epidemiology and physiology of chronic liver disease and the traditional role of liver biopsy. Pros and cons of alternative fibrosis assessment methods are discussed, with a focus on their utility for patients with nonalcoholic fatty liver disease (NAFLD) and hepatitis C virus (HCV) infection.
CHRONIC LIVER DISEASE: A HUGE HEALTH BURDEN
Chronic liver disease is associated with enormous health and financial costs in the United States. Its prevalence is about 15%,1 and it is the 12th leading cause of death.2 Hospital costs are estimated at about $4 billion annually.3
The most common causes of chronic liver disease are NAFLD (which may be present in up to one-third of the US population and is increasing with the epidemic of obesity), its aggressive variant, nonalcoholic steatohepatitis (NASH) (present in about 3% of the population), and HCV infection (1%).4,5
Since direct-acting antiviral agents were introduced, HCV infection dropped from being the leading cause of liver transplant to third place.6 But at the same time, the number of patients on the transplant waiting list who have NASH has risen faster than for any other cause of chronic liver disease.7
FIBROSIS: A KEY INDICATOR OF DISEASE SEVERITY
In HCV infection, advanced fibrosis is defined as either stage 4 to 6 using the Ishak system10 or stage 3 to 4 using the Meta-analysis of Histological Data in Viral Hepatitis (METAVIR) system.11
In NAFLD, advanced fibrosis is defined as stage 3 to 4 using the NASH Clinical Research Network system.12
Staging fibrosis is also important so that patients with cirrhosis can be identified early to begin screening for hepatocellular carcinoma and esophageal varices to reduce the risks of illness and death. In addition, insurance companies often require documentation of fibrosis stage before treating HCV with the new direct-acting antiviral agents.
LIVER BIOPSY IS STILL THE GOLD STANDARD
Although invasive, liver biopsy remains the gold standard for determining fibrosis stage. Liver biopsies were performed “blindly” (without imaging) until the 1990s, but imaging-guided biopsy using ultrasonography was then developed, which entailed less pain and lower complication and hospitalization rates. Slightly more hepatic tissue is obtained with guided liver biopsy, but the difference was deemed clinically insignificant.13 Concern initially arose about the added cost involved with imaging, but imaging-guided biopsy was actually found to be more cost-effective.14
In the 2000s, transjugular liver biopsy via the right internal jugular vein became available. This method was originally used primarily in patients with ascites or significant coagulopathy. At first, there were concerns about the adequacy of specimens obtained to make an accurate diagnosis or establish fibrosis stage, but this limitation was overcome with improved techniques.15,16 Transjugular liver biopsy has the additional advantage of enabling one to measure the hepatic venous pressure gradient, which also has prognostic significance; a gradient greater than 10 mm Hg is associated with worse prognosis.17
Disadvantages of biopsy: Complications, sampling errors
Liver biopsy has disadvantages. Reported rates of complications necessitating hospitalization using the blind method were as high as 6% in the 1970s,18 dropping to 3.2% in a 1993 study.19 Bleeding remains the most worrisome complication. With the transjugular method, major and minor complication rates are less than 1% and 7%, respectively.15,16 Complication rates with imaging-guided biopsy are also low.
Liver biopsy is also prone to sampling error. The number of portal tracts obtained in the biopsy correlates with the accuracy of fibrosis staging, and smaller samples may lead to underestimating fibrosis stage. In patients with HCV, samples more than 15 mm long led to accurate staging diagnosis in 65% of patients, and those longer than 25 mm conferred 75% accuracy.20 Also, different stages can be diagnosed from samples obtained from separate locations in the liver, although rarely is the difference more than a single stage.21
Histologic evaluation of liver biopsies is operator-dependent. Although significant interobserver variation has been reported for degree of inflammation, there tends to be good concordance for fibrosis staging.22,23
STAGING BASED ON DEMOGRAPHIC AND LABORATORY VARIABLES
Several scores based on patient characteristics and laboratory values have been developed for assessing liver fibrosis and have been specifically validated for HCV infection, NAFLD, or both. They can serve as inexpensive initial screening tests for the presence or absence of advanced fibrosis.
FIB-4 index for HCV, NAFLD
The FIB-4 index predicts the presence of advanced fibrosis using, as its name indicates, a combination of 4 factors in fibrosis: age, platelet count, and the levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT), according to the formula:
FIB-4 index = (age × AST [U/L]) /
(platelet count [× 109/L] × √ALT [U/L]).
The index was derived from data from 832 patients co-infected with HCV and human immunodeficiency virus.24 The Ishak staging system10 for fibrosis on liver biopsy was used for confirmation, with stage 4 to 6 defined as advanced fibrosis. A cutoff value of more than 3.25 had a positive predictive value of 65% for advanced fibrosis, and to exclude advanced fibrosis, a cutoff value of less than 1.45 had a negative predictive value of 90%.
The FIB-4 index has since been validated in patients with HCV infection25 and NAFLD.26 In a subsequent study in 142 patients with NAFLD, the FIB-4 index was more accurate in diagnosing advanced fibrosis than the other noninvasive prediction models discussed below.27
NAFLD fibrosis score
The NAFLD fibrosis score, constructed and validated only in patients with biopsy-confirmed NAFLD, incorporates age, body mass index, presence of diabetes or prediabetes, albumin level, platelet count, and AST and ALT levels.
A group of 480 patients was used to construct the score, and 253 patients were used to validate it. Using the high cutoff value of 0.676, the presence of advanced fibrosis was diagnosed with a positive predictive value of 90% in the group used to construct the model (82% in the validation group). Using the low cutoff score of –1.455, advanced fibrosis could be excluded with a negative predictive value of 93% in the construction group and 88% in the validation group.28 A score between the cutoff values merits liver biopsy to determine fibrosis stage. The score is more accurate in patients with diabetes.29 When used by primary care physicians, the NAFLD fibrosis score is more cost-effective than transient elastography and liver biopsy for accurately predicting advanced fibrosis.30
AST-to-platelet ratio index score for HCV, NAFLD
The AST-to-platelet ratio index (APRI) score was developed in 2003 using a cohort of 270 patients with HCV and liver biopsy as the standard. A cutoff value of less than or equal to 0.5 had a negative predictive value of 86% for the absence of significant fibrosis, while a score of more than 1.5 detected the presence of significant fibrosis with a positive predictive value of 88%.31 The APRI score was subsequently validated for NAFLD.27,32
FibroSure uses a patented formula
FibroSure (LabCorp; labcorp.com) uses a patented mathematical formula that takes into account age, sex, and levels of gamma-glutamyl transferase, total bilirubin, haptoglobin, apolipoprotein-A, and alpha-2 macroglobulin to assess fibrosis. Developed in 2001 for use in patients with HCV infection, it was reported to have a positive predictive value of greater than 90% and a negative predictive value of 100% for clinically significant fibrosis, defined as stage 2 to 4 based on the METAVIR staging system in the prediction model.33 The use of FibroSure in patients with HCV was subsequently validated in various meta-analyses and systematic reviews.34,35 It is less accurate in patients with normal ALT levels.36
FibroSure also has good accuracy for predicting fibrosis stage in chronic liver disease due to other causes, including NAFLD.37
The prediction models discussed above use routine laboratory tests for chronic liver disease and thus are inexpensive. The high cost of additional testing needed for FibroSure, coupled with the risk of misdiagnosis, makes its cost-effectiveness questionable.38
IMAGING TO PREDICT FIBROSIS STAGE
Conventional ultrasonography (with or without vascular imaging) and computed tomography can detect cirrhosis on the basis of certain imaging characteristics,39,40 including the nodular contour of the liver, caudate lobe hypertrophy, ascites, reversal of blood flow in the portal vein, and splenomegaly. However, they cannot detect fibrosis in its early stages.
The 3 methods discussed below provide more accurate fibrosis staging by measuring the velocity of shear waves sent across hepatic tissue. Because shear-wave velocity increases with liver stiffness, the fibrosis stage can be estimated from this information.41
Transient elastography
Transient elastography uses a special ultrasound transducer. It is highly accurate for predicting advanced fibrosis for almost all causes of chronic liver disease, including HCV infection42,43 and NAFLD.44 The cutoff values of wave velocity to estimate fibrosis stage differ by liver disease etiology.
Transient elastography should not be used to evaluate fibrosis in patients with acute hepatitis, which transiently increases liver stiffness, resulting in a falsely high fibrosis stage diagnosis.45 It is also not a good method for evaluating fibrosis in patients with biliary obstruction or extrahepatic venous congestion. Because liver stiffness can increase after eating,46 the test should be done under fasting conditions.
A significant limitation of transient elastography has been its poor accuracy in patients with obesity.47 This has been largely overcome with the use of a more powerful (XL) probe but is still a limitation for those with morbid obesity.48 Because many patients with NAFLD are obese, this limitation can be significant.
Transient elastography has gained popularity for evaluating fibrosis in patients with chronic liver disease for multiple reasons: it is cost-effective and results are highly reproducible, with low variation in results among different observers and in individual observers.49 Combined with a platelet count, it can also be used to detect the development of clinically significant portal hypertension in patients with cirrhosis, thus determining the need to screen for esophageal varices using endoscopy.50 Screening endoscopy can be avoided in patients whose liver stiffness remains below 20 kPa or whose platelet count is above 150 × 109/L.
Acoustic radiation force imaging
Unlike transient elastography, which requires a separate transducer probe to assess shear- wave velocity, acoustic radiation force imaging uses the same transducer for both this function and imaging. Different image modes are available when testing for liver stiffness, so a region of interest that is optimal for avoiding vascular structures or masses can be selected, increasing accuracy.51
Acoustic radiation force imaging has been tested in different causes of chronic liver disease, including HCV and NAFLD,52 with accuracy similar to that of transient elastography.53 For overweight and obese patients, acoustic radiation force imaging is more accurate than transient elastography using the XL probe.54 However, this method is still new, and we need more data to support using one method over the other.
Magnetic resonance elastography
Magnetic resonance elastography uses a special transducer placed under the rib cage to transmit shear waves concurrently with magnetic resonance imaging. It has been tested in patients with HCV and NAFLD and has been found to have better diagnostic accuracy than transient elastography and acoustic radiation force imaging.55,56 Patients must be fasting for better diagnostic accuracy57 and must hold their breath while elastography is performed. The need for breath-holding and the high cost limit the use of this method for assessing fibrosis.
BOTTOM LINE FOR ASSESSING FIBROSIS
- Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol 2011; 9(6):524–530.e1. doi:10.1016/j.cgh.2011.03.020
- Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung H-C. Deaths: final data for 2009. Natl Vital Stat Rep 2011; 60(3):1–116. pmid:24974587
- Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol 2012; 107(2):247–252. doi:10.1038/ajg.2011.314
- Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011; 34(3):274–285. doi:10.1111/j.1365-2036.2011.04724.x
- Udompap P, Kim D, Kim WR. Current and future burden of chronic nonmalignant liver disease. Clin Gastroenterol Hepatol 2015; 13(12):2031–2041. doi:10.1016/j.cgh.2015.08.015
- Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 annual data report: liver. Am J Transplant 2018; 18(suppl 1):172–253. doi:10.1111/ajt.14559
- Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148(3):547–555. doi:10.1053/j.gastro.2014.11.039
- Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol 1995; 22(6):696–699. pmid:7560864
- Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. Hepatology 1996; 24(2):289–293. doi:10.1002/hep.510240201
- Kleiner DE, Brunt EM, Van Natta M, et al; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005; 41(6):1313–1321. doi:10.1002/hep.20701
- Everhart JE, Wright EC, Goodman ZD, et al; HALT-C Trial Group. Prognostic value of Ishak fibrosis stage: findings from the hepatitis C antiviral long-term treatment against cirrhosis trial. Hepatology 2010; 51(2):585–594. doi:10.1002/hep.23315
- Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015; 149(2):389–397.e10. doi:10.1053/j.gastro.2015.04.043
- Lindor KD, Bru C, Jorgensen RA, et al. The role of ultrasonography and automatic-needle biopsy in outpatient percutaneous liver biopsy. Hepatology 1996; 23(5):1079–1083. doi:10.1002/hep.510230522
- Pasha T, Gabriel S, Therneau T, Dickson ER, Lindor KD. Cost-effectiveness of ultrasound-guided liver biopsy. Hepatology 1998; 27(5):1220–1226. doi:10.1002/hep.510270506
- Alessandria C, Debernardi-Venon W, Rizzetto M, Marzano A. Transjugular liver biopsy: a relatively simple procedure with an indefinite past and an expected brilliant future. J Hepatol 2008; 48(1):171–173. doi:10.1016/j.jhep.2007.10.001
- Kalambokis G, Manousou P, Vibhakorn S, et al. Transjugular liver biopsy—indications, adequacy, quality of specimens, and complications—a systematic review. J Hepatol 2007; 47(2):284–294. doi:10.1016/j.jhep.2007.05.001
- Ripoll C, Groszmann R, Garcia-Tsao G, et al; Portal Hypertension Collaborative Group. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 2007; 133(2):481–488. doi:10.1053/j.gastro.2007.05.024
- Perrault J, McGill DB, Ott BJ, Taylor WF. Liver biopsy: complications in 1000 inpatients and outpatients. Gastroenterology 1978; 74(1):103–106. pmid:618417
- Janes CH, Lindor KD. Outcome of patients hospitalized for complications after outpatient liver biopsy. Ann Intern Med 1993; 118(2):96–98. pmid:8416324
- Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 2003; 38(6):1449–1457. doi:10.1016/j.hep.2003.09.022
- Regev A, Berho M, Jeffers LJ, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 2002; 97(10):2614–2618. doi:10.1111/j.1572-0241.2002.06038.x
- Goldin RD, Goldin JG, Burt AD, et al. Intra-observer and inter-observer variation in the histopathological assessment of chronic viral hepatitis. J Hepatol 1996; 25(5):649–654. pmid:8938541
- Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. The French METAVIR Cooperative Study Group. Hepatology 1994; 20(1 Pt 1):15–20. pmid:8020885
- Sterling RK, Lissen E, Clumeck N, et al; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006; 43(6):1317–1325. doi:10.1002/hep.21178
- Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology 2007; 46(1):32–36. doi:10.1002/hep.21669
- Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2009; 7(10):1104–1112. doi:10.1016/j.cgh.2009.05.033
- McPherson S, Stewart SF, Henderson E, Burt AD, Day CP. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut 2010; 59(9):1265–1269. doi:10.1136/gut.2010.216077
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45(4):846–854. doi:10.1002/hep.21496
- Goh GB, Pagadala MR, Dasarathy J, et al. Clinical spectrum of non-alcoholic fatty liver disease in diabetic and non-diabetic patients. BBA Clin 2015; 3:141–145. doi:10.1016/j.bbacli.2014.09.001
- Tapper EB, Hunink MG, Afdhal NH, Lai M, Sengupta N. Cost-effectiveness analysis: risk stratification of nonalcoholic fatty liver disease (NAFLD) by the primary care physician using the NAFLD fibrosis score. PLoS One 2016; 11(2):e0147237. doi:10.1371/journal.pone.0147237
- Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003; 38(2):518–526. doi:10.1053/jhep.2003.50346
- Calès P, Lainé F, Boursier J, et al. Comparison of blood tests for liver fibrosis specific or not to NAFLD. J Hepatol 2009; 50(1):165–173. doi:10.1016/j.jhep.2008.07.035
- Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T; MULTIVIRC Group. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet 2001; 357(9262):1069–1075. doi:10.1016/S0140-6736(00)04258-6
- Shaheen AA, Wan AF, Myers RP. FibroTest and FibroScan for the prediction of hepatitis C-related fibrosis: a systematic review of diagnostic test accuracy. Am J Gastroenterol 2007; 102(11):2589–2600. doi:10.1111/j.1572-0241.2007.01466.x
- Smith JO, Sterling RK. Systematic review: non-invasive methods of fibrosis analysis in chronic hepatitis C. Aliment Pharmacol Ther 2009; 30(6):557–576. doi:10.1111/j.1365-2036.2009.04062.x
- Sebastiani G, Vario A, Guido M, Alberti A. Performance of noninvasive markers for liver fibrosis is reduced in chronic hepatitis C with normal transaminases. J Viral Hepat 2007; 15(3):212–218. doi:10.1111/j.1365-2893.2007.00932.x
- Poynard T, Morra R, Halfon P, et al. Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol 2007; 7:40. doi:10.1186/1471-230X-7-40
- Carlson JJ, Kowdley KV, Sullivan SD, Ramsey SD, Veenstra DL. An evaluation of the potential cost-effectiveness of non-invasive testing strategies in the diagnosis of significant liver fibrosis. J Gastroenterol Hepatol 2009; 24(5):786–791. doi:10.1111/j.1440-1746.2009.05778.x
- Aubé C, Oberti F, Korali N, et al. Ultrasonographic diagnosis of hepatic fibrosis or cirrhosis. J Hepatol 1999; 30(3):472–478. pmid:10190731
- Di Lelio A, Cestari C, Lomazzi A, Beretta L. Cirrhosis: diagnosis with sonographic study of the liver surface. Radiology 1989; 172(2):389–392. doi:10.1148/radiology.172.2.2526349
- Wong VW, Chan HL. Transient elastography. J Gastroenterol Hepatol 2010; 25(11):1726–1731. doi:10.1111/j.1440-1746.2010.06437.x
- Arena U, Vizzutti F, Abraldes JG, et al. Reliability of transient elastography for the diagnosis of advanced fibrosis in chronic hepatitis C. Gut 2008; 57(9):1288–1293. doi:10.1136/gut.2008.149708
- Ziol M, Handra-Luca A, Kettaneh A, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology 2005; 41(1):48–54. doi:10.1002/hep.20506
- Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology 2010; 51(2):454–462. doi:10.1002/hep.23312
- Sagir A, Erhardt A, Schmitt M, Häussinger D. Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology 2007; 48(2):592–595. doi:10.1002/hep.22056
- Mederacke I, Wursthorn K, Kirschner J, et al. Food intake increases liver stiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int 2009; 29(10):1500–1506. doi:10.1111/j.1478-3231.2009.02100.x
- Castéra L, Foucher J, Bernard PH, et al. Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology 2010; 51(3):828–835. doi:10.1002/hep.23425
- Wong VW, Vergniol J, Wong GL, et al. Liver stiffness measurement using XL probe in patients with nonalcoholic fatty liver disease. Am J Gastroenterol 2012; 107(12):1862–1871. doi:10.1038/ajg.2012.331
- Fraquelli M, Rigamonti C, Casazza G, et al. Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut 2007; 56(7):968–973. doi:10.1136/gut.2006.111302
- de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol 2015; 63(3):743–752. doi:10.1016/j.jhep.2015.05.022
- Friedrich-Rust M, Wunder K, Kriener S, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology 2009; 252(2):595–604. doi:10.1148/radiol.2523081928
- Yoneda M, Suzuki K, Kato S, et al. Nonalcoholic fatty liver disease: US-based acoustic radiation force impulse elastography. Radiology 2010; 256(2):640–647. doi:10.1148/radiol.10091662
- Bota S, Herkner H, Sporea I, et al. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int 2013; 33(8):1138–1147. doi:10.1111/liv.12240
- Attia D, Bantel H, Lenzen H, Manns MP, Gebel MJ, Potthoff A. Liver stiffness measurement using acoustic radiation force impulse elastography in overweight and obese patients. Aliment Pharmacol Ther 2016; 44(4):366–379. doi:10.1111/apt.13710
- Cui J, Heba E, Hernandez C, et al. Magnetic resonance elastography is superior to acoustic radiation force impulse for the diagnosis of fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease: a prospective study. Hepatology 2016; 63(2):453–461. doi:10.1002/hep.28337
- Huwart L, Sempoux C, Vicaut E, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology 2008; 135(1):32–40. doi:10.1053/j.gastro.2008.03.076
- Jajamovich GH, Dyvorne H, Donnerhack C, Taouli B. Quantitative liver MRI combining phase contrast imaging, elastography, and DWI: assessment of reproducibility and postprandial effect at 3.0 T. PLoS One 2014; 9(5):e97355. doi:10.1371/journal.pone.0097355
- Lim JK, Flamm SL, Singh S, Falck-Ytter YT; Clinical Guidelines Committee of the American Gastroenterological Association. American Gastroenterological Association Institute guideline on the role of elastography in the evaluation of liver fibrosis. Gastroenterology 2017; 152(6):1536–1543. doi:10.1053/j.gastro.2017.03.017
- N, Feldstein AE. Noninvasive diagnosis of nonalcoholic fatty liver disease: are we there yet? Metabolism 2016; 65(8):1087–1095. doi:10.1016/j.metabol.2016.01.013
Staging of liver fibrosis, important for determining prognosis in patients with chronic liver disease and for the need to start screening for complications of cirrhosis, was traditionally done only by liver biopsy. While biopsy is still the gold standard method to stage fibrosis, noninvasive methods have been developed that can also assess disease severity.
This article briefly reviews the epidemiology and physiology of chronic liver disease and the traditional role of liver biopsy. Pros and cons of alternative fibrosis assessment methods are discussed, with a focus on their utility for patients with nonalcoholic fatty liver disease (NAFLD) and hepatitis C virus (HCV) infection.
CHRONIC LIVER DISEASE: A HUGE HEALTH BURDEN
Chronic liver disease is associated with enormous health and financial costs in the United States. Its prevalence is about 15%,1 and it is the 12th leading cause of death.2 Hospital costs are estimated at about $4 billion annually.3
The most common causes of chronic liver disease are NAFLD (which may be present in up to one-third of the US population and is increasing with the epidemic of obesity), its aggressive variant, nonalcoholic steatohepatitis (NASH) (present in about 3% of the population), and HCV infection (1%).4,5
Since direct-acting antiviral agents were introduced, HCV infection dropped from being the leading cause of liver transplant to third place.6 But at the same time, the number of patients on the transplant waiting list who have NASH has risen faster than for any other cause of chronic liver disease.7
FIBROSIS: A KEY INDICATOR OF DISEASE SEVERITY
In HCV infection, advanced fibrosis is defined as either stage 4 to 6 using the Ishak system10 or stage 3 to 4 using the Meta-analysis of Histological Data in Viral Hepatitis (METAVIR) system.11
In NAFLD, advanced fibrosis is defined as stage 3 to 4 using the NASH Clinical Research Network system.12
Staging fibrosis is also important so that patients with cirrhosis can be identified early to begin screening for hepatocellular carcinoma and esophageal varices to reduce the risks of illness and death. In addition, insurance companies often require documentation of fibrosis stage before treating HCV with the new direct-acting antiviral agents.
LIVER BIOPSY IS STILL THE GOLD STANDARD
Although invasive, liver biopsy remains the gold standard for determining fibrosis stage. Liver biopsies were performed “blindly” (without imaging) until the 1990s, but imaging-guided biopsy using ultrasonography was then developed, which entailed less pain and lower complication and hospitalization rates. Slightly more hepatic tissue is obtained with guided liver biopsy, but the difference was deemed clinically insignificant.13 Concern initially arose about the added cost involved with imaging, but imaging-guided biopsy was actually found to be more cost-effective.14
In the 2000s, transjugular liver biopsy via the right internal jugular vein became available. This method was originally used primarily in patients with ascites or significant coagulopathy. At first, there were concerns about the adequacy of specimens obtained to make an accurate diagnosis or establish fibrosis stage, but this limitation was overcome with improved techniques.15,16 Transjugular liver biopsy has the additional advantage of enabling one to measure the hepatic venous pressure gradient, which also has prognostic significance; a gradient greater than 10 mm Hg is associated with worse prognosis.17
Disadvantages of biopsy: Complications, sampling errors
Liver biopsy has disadvantages. Reported rates of complications necessitating hospitalization using the blind method were as high as 6% in the 1970s,18 dropping to 3.2% in a 1993 study.19 Bleeding remains the most worrisome complication. With the transjugular method, major and minor complication rates are less than 1% and 7%, respectively.15,16 Complication rates with imaging-guided biopsy are also low.
Liver biopsy is also prone to sampling error. The number of portal tracts obtained in the biopsy correlates with the accuracy of fibrosis staging, and smaller samples may lead to underestimating fibrosis stage. In patients with HCV, samples more than 15 mm long led to accurate staging diagnosis in 65% of patients, and those longer than 25 mm conferred 75% accuracy.20 Also, different stages can be diagnosed from samples obtained from separate locations in the liver, although rarely is the difference more than a single stage.21
Histologic evaluation of liver biopsies is operator-dependent. Although significant interobserver variation has been reported for degree of inflammation, there tends to be good concordance for fibrosis staging.22,23
STAGING BASED ON DEMOGRAPHIC AND LABORATORY VARIABLES
Several scores based on patient characteristics and laboratory values have been developed for assessing liver fibrosis and have been specifically validated for HCV infection, NAFLD, or both. They can serve as inexpensive initial screening tests for the presence or absence of advanced fibrosis.
FIB-4 index for HCV, NAFLD
The FIB-4 index predicts the presence of advanced fibrosis using, as its name indicates, a combination of 4 factors in fibrosis: age, platelet count, and the levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT), according to the formula:
FIB-4 index = (age × AST [U/L]) /
(platelet count [× 109/L] × √ALT [U/L]).
The index was derived from data from 832 patients co-infected with HCV and human immunodeficiency virus.24 The Ishak staging system10 for fibrosis on liver biopsy was used for confirmation, with stage 4 to 6 defined as advanced fibrosis. A cutoff value of more than 3.25 had a positive predictive value of 65% for advanced fibrosis, and to exclude advanced fibrosis, a cutoff value of less than 1.45 had a negative predictive value of 90%.
The FIB-4 index has since been validated in patients with HCV infection25 and NAFLD.26 In a subsequent study in 142 patients with NAFLD, the FIB-4 index was more accurate in diagnosing advanced fibrosis than the other noninvasive prediction models discussed below.27
NAFLD fibrosis score
The NAFLD fibrosis score, constructed and validated only in patients with biopsy-confirmed NAFLD, incorporates age, body mass index, presence of diabetes or prediabetes, albumin level, platelet count, and AST and ALT levels.
A group of 480 patients was used to construct the score, and 253 patients were used to validate it. Using the high cutoff value of 0.676, the presence of advanced fibrosis was diagnosed with a positive predictive value of 90% in the group used to construct the model (82% in the validation group). Using the low cutoff score of –1.455, advanced fibrosis could be excluded with a negative predictive value of 93% in the construction group and 88% in the validation group.28 A score between the cutoff values merits liver biopsy to determine fibrosis stage. The score is more accurate in patients with diabetes.29 When used by primary care physicians, the NAFLD fibrosis score is more cost-effective than transient elastography and liver biopsy for accurately predicting advanced fibrosis.30
AST-to-platelet ratio index score for HCV, NAFLD
The AST-to-platelet ratio index (APRI) score was developed in 2003 using a cohort of 270 patients with HCV and liver biopsy as the standard. A cutoff value of less than or equal to 0.5 had a negative predictive value of 86% for the absence of significant fibrosis, while a score of more than 1.5 detected the presence of significant fibrosis with a positive predictive value of 88%.31 The APRI score was subsequently validated for NAFLD.27,32
FibroSure uses a patented formula
FibroSure (LabCorp; labcorp.com) uses a patented mathematical formula that takes into account age, sex, and levels of gamma-glutamyl transferase, total bilirubin, haptoglobin, apolipoprotein-A, and alpha-2 macroglobulin to assess fibrosis. Developed in 2001 for use in patients with HCV infection, it was reported to have a positive predictive value of greater than 90% and a negative predictive value of 100% for clinically significant fibrosis, defined as stage 2 to 4 based on the METAVIR staging system in the prediction model.33 The use of FibroSure in patients with HCV was subsequently validated in various meta-analyses and systematic reviews.34,35 It is less accurate in patients with normal ALT levels.36
FibroSure also has good accuracy for predicting fibrosis stage in chronic liver disease due to other causes, including NAFLD.37
The prediction models discussed above use routine laboratory tests for chronic liver disease and thus are inexpensive. The high cost of additional testing needed for FibroSure, coupled with the risk of misdiagnosis, makes its cost-effectiveness questionable.38
IMAGING TO PREDICT FIBROSIS STAGE
Conventional ultrasonography (with or without vascular imaging) and computed tomography can detect cirrhosis on the basis of certain imaging characteristics,39,40 including the nodular contour of the liver, caudate lobe hypertrophy, ascites, reversal of blood flow in the portal vein, and splenomegaly. However, they cannot detect fibrosis in its early stages.
The 3 methods discussed below provide more accurate fibrosis staging by measuring the velocity of shear waves sent across hepatic tissue. Because shear-wave velocity increases with liver stiffness, the fibrosis stage can be estimated from this information.41
Transient elastography
Transient elastography uses a special ultrasound transducer. It is highly accurate for predicting advanced fibrosis for almost all causes of chronic liver disease, including HCV infection42,43 and NAFLD.44 The cutoff values of wave velocity to estimate fibrosis stage differ by liver disease etiology.
Transient elastography should not be used to evaluate fibrosis in patients with acute hepatitis, which transiently increases liver stiffness, resulting in a falsely high fibrosis stage diagnosis.45 It is also not a good method for evaluating fibrosis in patients with biliary obstruction or extrahepatic venous congestion. Because liver stiffness can increase after eating,46 the test should be done under fasting conditions.
A significant limitation of transient elastography has been its poor accuracy in patients with obesity.47 This has been largely overcome with the use of a more powerful (XL) probe but is still a limitation for those with morbid obesity.48 Because many patients with NAFLD are obese, this limitation can be significant.
Transient elastography has gained popularity for evaluating fibrosis in patients with chronic liver disease for multiple reasons: it is cost-effective and results are highly reproducible, with low variation in results among different observers and in individual observers.49 Combined with a platelet count, it can also be used to detect the development of clinically significant portal hypertension in patients with cirrhosis, thus determining the need to screen for esophageal varices using endoscopy.50 Screening endoscopy can be avoided in patients whose liver stiffness remains below 20 kPa or whose platelet count is above 150 × 109/L.
Acoustic radiation force imaging
Unlike transient elastography, which requires a separate transducer probe to assess shear- wave velocity, acoustic radiation force imaging uses the same transducer for both this function and imaging. Different image modes are available when testing for liver stiffness, so a region of interest that is optimal for avoiding vascular structures or masses can be selected, increasing accuracy.51
Acoustic radiation force imaging has been tested in different causes of chronic liver disease, including HCV and NAFLD,52 with accuracy similar to that of transient elastography.53 For overweight and obese patients, acoustic radiation force imaging is more accurate than transient elastography using the XL probe.54 However, this method is still new, and we need more data to support using one method over the other.
Magnetic resonance elastography
Magnetic resonance elastography uses a special transducer placed under the rib cage to transmit shear waves concurrently with magnetic resonance imaging. It has been tested in patients with HCV and NAFLD and has been found to have better diagnostic accuracy than transient elastography and acoustic radiation force imaging.55,56 Patients must be fasting for better diagnostic accuracy57 and must hold their breath while elastography is performed. The need for breath-holding and the high cost limit the use of this method for assessing fibrosis.
BOTTOM LINE FOR ASSESSING FIBROSIS
Staging of liver fibrosis, important for determining prognosis in patients with chronic liver disease and for the need to start screening for complications of cirrhosis, was traditionally done only by liver biopsy. While biopsy is still the gold standard method to stage fibrosis, noninvasive methods have been developed that can also assess disease severity.
This article briefly reviews the epidemiology and physiology of chronic liver disease and the traditional role of liver biopsy. Pros and cons of alternative fibrosis assessment methods are discussed, with a focus on their utility for patients with nonalcoholic fatty liver disease (NAFLD) and hepatitis C virus (HCV) infection.
CHRONIC LIVER DISEASE: A HUGE HEALTH BURDEN
Chronic liver disease is associated with enormous health and financial costs in the United States. Its prevalence is about 15%,1 and it is the 12th leading cause of death.2 Hospital costs are estimated at about $4 billion annually.3
The most common causes of chronic liver disease are NAFLD (which may be present in up to one-third of the US population and is increasing with the epidemic of obesity), its aggressive variant, nonalcoholic steatohepatitis (NASH) (present in about 3% of the population), and HCV infection (1%).4,5
Since direct-acting antiviral agents were introduced, HCV infection dropped from being the leading cause of liver transplant to third place.6 But at the same time, the number of patients on the transplant waiting list who have NASH has risen faster than for any other cause of chronic liver disease.7
FIBROSIS: A KEY INDICATOR OF DISEASE SEVERITY
In HCV infection, advanced fibrosis is defined as either stage 4 to 6 using the Ishak system10 or stage 3 to 4 using the Meta-analysis of Histological Data in Viral Hepatitis (METAVIR) system.11
In NAFLD, advanced fibrosis is defined as stage 3 to 4 using the NASH Clinical Research Network system.12
Staging fibrosis is also important so that patients with cirrhosis can be identified early to begin screening for hepatocellular carcinoma and esophageal varices to reduce the risks of illness and death. In addition, insurance companies often require documentation of fibrosis stage before treating HCV with the new direct-acting antiviral agents.
LIVER BIOPSY IS STILL THE GOLD STANDARD
Although invasive, liver biopsy remains the gold standard for determining fibrosis stage. Liver biopsies were performed “blindly” (without imaging) until the 1990s, but imaging-guided biopsy using ultrasonography was then developed, which entailed less pain and lower complication and hospitalization rates. Slightly more hepatic tissue is obtained with guided liver biopsy, but the difference was deemed clinically insignificant.13 Concern initially arose about the added cost involved with imaging, but imaging-guided biopsy was actually found to be more cost-effective.14
In the 2000s, transjugular liver biopsy via the right internal jugular vein became available. This method was originally used primarily in patients with ascites or significant coagulopathy. At first, there were concerns about the adequacy of specimens obtained to make an accurate diagnosis or establish fibrosis stage, but this limitation was overcome with improved techniques.15,16 Transjugular liver biopsy has the additional advantage of enabling one to measure the hepatic venous pressure gradient, which also has prognostic significance; a gradient greater than 10 mm Hg is associated with worse prognosis.17
Disadvantages of biopsy: Complications, sampling errors
Liver biopsy has disadvantages. Reported rates of complications necessitating hospitalization using the blind method were as high as 6% in the 1970s,18 dropping to 3.2% in a 1993 study.19 Bleeding remains the most worrisome complication. With the transjugular method, major and minor complication rates are less than 1% and 7%, respectively.15,16 Complication rates with imaging-guided biopsy are also low.
Liver biopsy is also prone to sampling error. The number of portal tracts obtained in the biopsy correlates with the accuracy of fibrosis staging, and smaller samples may lead to underestimating fibrosis stage. In patients with HCV, samples more than 15 mm long led to accurate staging diagnosis in 65% of patients, and those longer than 25 mm conferred 75% accuracy.20 Also, different stages can be diagnosed from samples obtained from separate locations in the liver, although rarely is the difference more than a single stage.21
Histologic evaluation of liver biopsies is operator-dependent. Although significant interobserver variation has been reported for degree of inflammation, there tends to be good concordance for fibrosis staging.22,23
STAGING BASED ON DEMOGRAPHIC AND LABORATORY VARIABLES
Several scores based on patient characteristics and laboratory values have been developed for assessing liver fibrosis and have been specifically validated for HCV infection, NAFLD, or both. They can serve as inexpensive initial screening tests for the presence or absence of advanced fibrosis.
FIB-4 index for HCV, NAFLD
The FIB-4 index predicts the presence of advanced fibrosis using, as its name indicates, a combination of 4 factors in fibrosis: age, platelet count, and the levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT), according to the formula:
FIB-4 index = (age × AST [U/L]) /
(platelet count [× 109/L] × √ALT [U/L]).
The index was derived from data from 832 patients co-infected with HCV and human immunodeficiency virus.24 The Ishak staging system10 for fibrosis on liver biopsy was used for confirmation, with stage 4 to 6 defined as advanced fibrosis. A cutoff value of more than 3.25 had a positive predictive value of 65% for advanced fibrosis, and to exclude advanced fibrosis, a cutoff value of less than 1.45 had a negative predictive value of 90%.
The FIB-4 index has since been validated in patients with HCV infection25 and NAFLD.26 In a subsequent study in 142 patients with NAFLD, the FIB-4 index was more accurate in diagnosing advanced fibrosis than the other noninvasive prediction models discussed below.27
NAFLD fibrosis score
The NAFLD fibrosis score, constructed and validated only in patients with biopsy-confirmed NAFLD, incorporates age, body mass index, presence of diabetes or prediabetes, albumin level, platelet count, and AST and ALT levels.
A group of 480 patients was used to construct the score, and 253 patients were used to validate it. Using the high cutoff value of 0.676, the presence of advanced fibrosis was diagnosed with a positive predictive value of 90% in the group used to construct the model (82% in the validation group). Using the low cutoff score of –1.455, advanced fibrosis could be excluded with a negative predictive value of 93% in the construction group and 88% in the validation group.28 A score between the cutoff values merits liver biopsy to determine fibrosis stage. The score is more accurate in patients with diabetes.29 When used by primary care physicians, the NAFLD fibrosis score is more cost-effective than transient elastography and liver biopsy for accurately predicting advanced fibrosis.30
AST-to-platelet ratio index score for HCV, NAFLD
The AST-to-platelet ratio index (APRI) score was developed in 2003 using a cohort of 270 patients with HCV and liver biopsy as the standard. A cutoff value of less than or equal to 0.5 had a negative predictive value of 86% for the absence of significant fibrosis, while a score of more than 1.5 detected the presence of significant fibrosis with a positive predictive value of 88%.31 The APRI score was subsequently validated for NAFLD.27,32
FibroSure uses a patented formula
FibroSure (LabCorp; labcorp.com) uses a patented mathematical formula that takes into account age, sex, and levels of gamma-glutamyl transferase, total bilirubin, haptoglobin, apolipoprotein-A, and alpha-2 macroglobulin to assess fibrosis. Developed in 2001 for use in patients with HCV infection, it was reported to have a positive predictive value of greater than 90% and a negative predictive value of 100% for clinically significant fibrosis, defined as stage 2 to 4 based on the METAVIR staging system in the prediction model.33 The use of FibroSure in patients with HCV was subsequently validated in various meta-analyses and systematic reviews.34,35 It is less accurate in patients with normal ALT levels.36
FibroSure also has good accuracy for predicting fibrosis stage in chronic liver disease due to other causes, including NAFLD.37
The prediction models discussed above use routine laboratory tests for chronic liver disease and thus are inexpensive. The high cost of additional testing needed for FibroSure, coupled with the risk of misdiagnosis, makes its cost-effectiveness questionable.38
IMAGING TO PREDICT FIBROSIS STAGE
Conventional ultrasonography (with or without vascular imaging) and computed tomography can detect cirrhosis on the basis of certain imaging characteristics,39,40 including the nodular contour of the liver, caudate lobe hypertrophy, ascites, reversal of blood flow in the portal vein, and splenomegaly. However, they cannot detect fibrosis in its early stages.
The 3 methods discussed below provide more accurate fibrosis staging by measuring the velocity of shear waves sent across hepatic tissue. Because shear-wave velocity increases with liver stiffness, the fibrosis stage can be estimated from this information.41
Transient elastography
Transient elastography uses a special ultrasound transducer. It is highly accurate for predicting advanced fibrosis for almost all causes of chronic liver disease, including HCV infection42,43 and NAFLD.44 The cutoff values of wave velocity to estimate fibrosis stage differ by liver disease etiology.
Transient elastography should not be used to evaluate fibrosis in patients with acute hepatitis, which transiently increases liver stiffness, resulting in a falsely high fibrosis stage diagnosis.45 It is also not a good method for evaluating fibrosis in patients with biliary obstruction or extrahepatic venous congestion. Because liver stiffness can increase after eating,46 the test should be done under fasting conditions.
A significant limitation of transient elastography has been its poor accuracy in patients with obesity.47 This has been largely overcome with the use of a more powerful (XL) probe but is still a limitation for those with morbid obesity.48 Because many patients with NAFLD are obese, this limitation can be significant.
Transient elastography has gained popularity for evaluating fibrosis in patients with chronic liver disease for multiple reasons: it is cost-effective and results are highly reproducible, with low variation in results among different observers and in individual observers.49 Combined with a platelet count, it can also be used to detect the development of clinically significant portal hypertension in patients with cirrhosis, thus determining the need to screen for esophageal varices using endoscopy.50 Screening endoscopy can be avoided in patients whose liver stiffness remains below 20 kPa or whose platelet count is above 150 × 109/L.
Acoustic radiation force imaging
Unlike transient elastography, which requires a separate transducer probe to assess shear- wave velocity, acoustic radiation force imaging uses the same transducer for both this function and imaging. Different image modes are available when testing for liver stiffness, so a region of interest that is optimal for avoiding vascular structures or masses can be selected, increasing accuracy.51
Acoustic radiation force imaging has been tested in different causes of chronic liver disease, including HCV and NAFLD,52 with accuracy similar to that of transient elastography.53 For overweight and obese patients, acoustic radiation force imaging is more accurate than transient elastography using the XL probe.54 However, this method is still new, and we need more data to support using one method over the other.
Magnetic resonance elastography
Magnetic resonance elastography uses a special transducer placed under the rib cage to transmit shear waves concurrently with magnetic resonance imaging. It has been tested in patients with HCV and NAFLD and has been found to have better diagnostic accuracy than transient elastography and acoustic radiation force imaging.55,56 Patients must be fasting for better diagnostic accuracy57 and must hold their breath while elastography is performed. The need for breath-holding and the high cost limit the use of this method for assessing fibrosis.
BOTTOM LINE FOR ASSESSING FIBROSIS
- Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol 2011; 9(6):524–530.e1. doi:10.1016/j.cgh.2011.03.020
- Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung H-C. Deaths: final data for 2009. Natl Vital Stat Rep 2011; 60(3):1–116. pmid:24974587
- Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol 2012; 107(2):247–252. doi:10.1038/ajg.2011.314
- Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011; 34(3):274–285. doi:10.1111/j.1365-2036.2011.04724.x
- Udompap P, Kim D, Kim WR. Current and future burden of chronic nonmalignant liver disease. Clin Gastroenterol Hepatol 2015; 13(12):2031–2041. doi:10.1016/j.cgh.2015.08.015
- Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 annual data report: liver. Am J Transplant 2018; 18(suppl 1):172–253. doi:10.1111/ajt.14559
- Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148(3):547–555. doi:10.1053/j.gastro.2014.11.039
- Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol 1995; 22(6):696–699. pmid:7560864
- Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. Hepatology 1996; 24(2):289–293. doi:10.1002/hep.510240201
- Kleiner DE, Brunt EM, Van Natta M, et al; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005; 41(6):1313–1321. doi:10.1002/hep.20701
- Everhart JE, Wright EC, Goodman ZD, et al; HALT-C Trial Group. Prognostic value of Ishak fibrosis stage: findings from the hepatitis C antiviral long-term treatment against cirrhosis trial. Hepatology 2010; 51(2):585–594. doi:10.1002/hep.23315
- Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015; 149(2):389–397.e10. doi:10.1053/j.gastro.2015.04.043
- Lindor KD, Bru C, Jorgensen RA, et al. The role of ultrasonography and automatic-needle biopsy in outpatient percutaneous liver biopsy. Hepatology 1996; 23(5):1079–1083. doi:10.1002/hep.510230522
- Pasha T, Gabriel S, Therneau T, Dickson ER, Lindor KD. Cost-effectiveness of ultrasound-guided liver biopsy. Hepatology 1998; 27(5):1220–1226. doi:10.1002/hep.510270506
- Alessandria C, Debernardi-Venon W, Rizzetto M, Marzano A. Transjugular liver biopsy: a relatively simple procedure with an indefinite past and an expected brilliant future. J Hepatol 2008; 48(1):171–173. doi:10.1016/j.jhep.2007.10.001
- Kalambokis G, Manousou P, Vibhakorn S, et al. Transjugular liver biopsy—indications, adequacy, quality of specimens, and complications—a systematic review. J Hepatol 2007; 47(2):284–294. doi:10.1016/j.jhep.2007.05.001
- Ripoll C, Groszmann R, Garcia-Tsao G, et al; Portal Hypertension Collaborative Group. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 2007; 133(2):481–488. doi:10.1053/j.gastro.2007.05.024
- Perrault J, McGill DB, Ott BJ, Taylor WF. Liver biopsy: complications in 1000 inpatients and outpatients. Gastroenterology 1978; 74(1):103–106. pmid:618417
- Janes CH, Lindor KD. Outcome of patients hospitalized for complications after outpatient liver biopsy. Ann Intern Med 1993; 118(2):96–98. pmid:8416324
- Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 2003; 38(6):1449–1457. doi:10.1016/j.hep.2003.09.022
- Regev A, Berho M, Jeffers LJ, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 2002; 97(10):2614–2618. doi:10.1111/j.1572-0241.2002.06038.x
- Goldin RD, Goldin JG, Burt AD, et al. Intra-observer and inter-observer variation in the histopathological assessment of chronic viral hepatitis. J Hepatol 1996; 25(5):649–654. pmid:8938541
- Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. The French METAVIR Cooperative Study Group. Hepatology 1994; 20(1 Pt 1):15–20. pmid:8020885
- Sterling RK, Lissen E, Clumeck N, et al; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006; 43(6):1317–1325. doi:10.1002/hep.21178
- Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology 2007; 46(1):32–36. doi:10.1002/hep.21669
- Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2009; 7(10):1104–1112. doi:10.1016/j.cgh.2009.05.033
- McPherson S, Stewart SF, Henderson E, Burt AD, Day CP. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut 2010; 59(9):1265–1269. doi:10.1136/gut.2010.216077
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45(4):846–854. doi:10.1002/hep.21496
- Goh GB, Pagadala MR, Dasarathy J, et al. Clinical spectrum of non-alcoholic fatty liver disease in diabetic and non-diabetic patients. BBA Clin 2015; 3:141–145. doi:10.1016/j.bbacli.2014.09.001
- Tapper EB, Hunink MG, Afdhal NH, Lai M, Sengupta N. Cost-effectiveness analysis: risk stratification of nonalcoholic fatty liver disease (NAFLD) by the primary care physician using the NAFLD fibrosis score. PLoS One 2016; 11(2):e0147237. doi:10.1371/journal.pone.0147237
- Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003; 38(2):518–526. doi:10.1053/jhep.2003.50346
- Calès P, Lainé F, Boursier J, et al. Comparison of blood tests for liver fibrosis specific or not to NAFLD. J Hepatol 2009; 50(1):165–173. doi:10.1016/j.jhep.2008.07.035
- Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T; MULTIVIRC Group. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet 2001; 357(9262):1069–1075. doi:10.1016/S0140-6736(00)04258-6
- Shaheen AA, Wan AF, Myers RP. FibroTest and FibroScan for the prediction of hepatitis C-related fibrosis: a systematic review of diagnostic test accuracy. Am J Gastroenterol 2007; 102(11):2589–2600. doi:10.1111/j.1572-0241.2007.01466.x
- Smith JO, Sterling RK. Systematic review: non-invasive methods of fibrosis analysis in chronic hepatitis C. Aliment Pharmacol Ther 2009; 30(6):557–576. doi:10.1111/j.1365-2036.2009.04062.x
- Sebastiani G, Vario A, Guido M, Alberti A. Performance of noninvasive markers for liver fibrosis is reduced in chronic hepatitis C with normal transaminases. J Viral Hepat 2007; 15(3):212–218. doi:10.1111/j.1365-2893.2007.00932.x
- Poynard T, Morra R, Halfon P, et al. Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol 2007; 7:40. doi:10.1186/1471-230X-7-40
- Carlson JJ, Kowdley KV, Sullivan SD, Ramsey SD, Veenstra DL. An evaluation of the potential cost-effectiveness of non-invasive testing strategies in the diagnosis of significant liver fibrosis. J Gastroenterol Hepatol 2009; 24(5):786–791. doi:10.1111/j.1440-1746.2009.05778.x
- Aubé C, Oberti F, Korali N, et al. Ultrasonographic diagnosis of hepatic fibrosis or cirrhosis. J Hepatol 1999; 30(3):472–478. pmid:10190731
- Di Lelio A, Cestari C, Lomazzi A, Beretta L. Cirrhosis: diagnosis with sonographic study of the liver surface. Radiology 1989; 172(2):389–392. doi:10.1148/radiology.172.2.2526349
- Wong VW, Chan HL. Transient elastography. J Gastroenterol Hepatol 2010; 25(11):1726–1731. doi:10.1111/j.1440-1746.2010.06437.x
- Arena U, Vizzutti F, Abraldes JG, et al. Reliability of transient elastography for the diagnosis of advanced fibrosis in chronic hepatitis C. Gut 2008; 57(9):1288–1293. doi:10.1136/gut.2008.149708
- Ziol M, Handra-Luca A, Kettaneh A, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology 2005; 41(1):48–54. doi:10.1002/hep.20506
- Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology 2010; 51(2):454–462. doi:10.1002/hep.23312
- Sagir A, Erhardt A, Schmitt M, Häussinger D. Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology 2007; 48(2):592–595. doi:10.1002/hep.22056
- Mederacke I, Wursthorn K, Kirschner J, et al. Food intake increases liver stiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int 2009; 29(10):1500–1506. doi:10.1111/j.1478-3231.2009.02100.x
- Castéra L, Foucher J, Bernard PH, et al. Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology 2010; 51(3):828–835. doi:10.1002/hep.23425
- Wong VW, Vergniol J, Wong GL, et al. Liver stiffness measurement using XL probe in patients with nonalcoholic fatty liver disease. Am J Gastroenterol 2012; 107(12):1862–1871. doi:10.1038/ajg.2012.331
- Fraquelli M, Rigamonti C, Casazza G, et al. Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut 2007; 56(7):968–973. doi:10.1136/gut.2006.111302
- de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol 2015; 63(3):743–752. doi:10.1016/j.jhep.2015.05.022
- Friedrich-Rust M, Wunder K, Kriener S, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology 2009; 252(2):595–604. doi:10.1148/radiol.2523081928
- Yoneda M, Suzuki K, Kato S, et al. Nonalcoholic fatty liver disease: US-based acoustic radiation force impulse elastography. Radiology 2010; 256(2):640–647. doi:10.1148/radiol.10091662
- Bota S, Herkner H, Sporea I, et al. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int 2013; 33(8):1138–1147. doi:10.1111/liv.12240
- Attia D, Bantel H, Lenzen H, Manns MP, Gebel MJ, Potthoff A. Liver stiffness measurement using acoustic radiation force impulse elastography in overweight and obese patients. Aliment Pharmacol Ther 2016; 44(4):366–379. doi:10.1111/apt.13710
- Cui J, Heba E, Hernandez C, et al. Magnetic resonance elastography is superior to acoustic radiation force impulse for the diagnosis of fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease: a prospective study. Hepatology 2016; 63(2):453–461. doi:10.1002/hep.28337
- Huwart L, Sempoux C, Vicaut E, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology 2008; 135(1):32–40. doi:10.1053/j.gastro.2008.03.076
- Jajamovich GH, Dyvorne H, Donnerhack C, Taouli B. Quantitative liver MRI combining phase contrast imaging, elastography, and DWI: assessment of reproducibility and postprandial effect at 3.0 T. PLoS One 2014; 9(5):e97355. doi:10.1371/journal.pone.0097355
- Lim JK, Flamm SL, Singh S, Falck-Ytter YT; Clinical Guidelines Committee of the American Gastroenterological Association. American Gastroenterological Association Institute guideline on the role of elastography in the evaluation of liver fibrosis. Gastroenterology 2017; 152(6):1536–1543. doi:10.1053/j.gastro.2017.03.017
- N, Feldstein AE. Noninvasive diagnosis of nonalcoholic fatty liver disease: are we there yet? Metabolism 2016; 65(8):1087–1095. doi:10.1016/j.metabol.2016.01.013
- Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol 2011; 9(6):524–530.e1. doi:10.1016/j.cgh.2011.03.020
- Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung H-C. Deaths: final data for 2009. Natl Vital Stat Rep 2011; 60(3):1–116. pmid:24974587
- Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol 2012; 107(2):247–252. doi:10.1038/ajg.2011.314
- Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011; 34(3):274–285. doi:10.1111/j.1365-2036.2011.04724.x
- Udompap P, Kim D, Kim WR. Current and future burden of chronic nonmalignant liver disease. Clin Gastroenterol Hepatol 2015; 13(12):2031–2041. doi:10.1016/j.cgh.2015.08.015
- Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 annual data report: liver. Am J Transplant 2018; 18(suppl 1):172–253. doi:10.1111/ajt.14559
- Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148(3):547–555. doi:10.1053/j.gastro.2014.11.039
- Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol 1995; 22(6):696–699. pmid:7560864
- Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. Hepatology 1996; 24(2):289–293. doi:10.1002/hep.510240201
- Kleiner DE, Brunt EM, Van Natta M, et al; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005; 41(6):1313–1321. doi:10.1002/hep.20701
- Everhart JE, Wright EC, Goodman ZD, et al; HALT-C Trial Group. Prognostic value of Ishak fibrosis stage: findings from the hepatitis C antiviral long-term treatment against cirrhosis trial. Hepatology 2010; 51(2):585–594. doi:10.1002/hep.23315
- Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015; 149(2):389–397.e10. doi:10.1053/j.gastro.2015.04.043
- Lindor KD, Bru C, Jorgensen RA, et al. The role of ultrasonography and automatic-needle biopsy in outpatient percutaneous liver biopsy. Hepatology 1996; 23(5):1079–1083. doi:10.1002/hep.510230522
- Pasha T, Gabriel S, Therneau T, Dickson ER, Lindor KD. Cost-effectiveness of ultrasound-guided liver biopsy. Hepatology 1998; 27(5):1220–1226. doi:10.1002/hep.510270506
- Alessandria C, Debernardi-Venon W, Rizzetto M, Marzano A. Transjugular liver biopsy: a relatively simple procedure with an indefinite past and an expected brilliant future. J Hepatol 2008; 48(1):171–173. doi:10.1016/j.jhep.2007.10.001
- Kalambokis G, Manousou P, Vibhakorn S, et al. Transjugular liver biopsy—indications, adequacy, quality of specimens, and complications—a systematic review. J Hepatol 2007; 47(2):284–294. doi:10.1016/j.jhep.2007.05.001
- Ripoll C, Groszmann R, Garcia-Tsao G, et al; Portal Hypertension Collaborative Group. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 2007; 133(2):481–488. doi:10.1053/j.gastro.2007.05.024
- Perrault J, McGill DB, Ott BJ, Taylor WF. Liver biopsy: complications in 1000 inpatients and outpatients. Gastroenterology 1978; 74(1):103–106. pmid:618417
- Janes CH, Lindor KD. Outcome of patients hospitalized for complications after outpatient liver biopsy. Ann Intern Med 1993; 118(2):96–98. pmid:8416324
- Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 2003; 38(6):1449–1457. doi:10.1016/j.hep.2003.09.022
- Regev A, Berho M, Jeffers LJ, et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 2002; 97(10):2614–2618. doi:10.1111/j.1572-0241.2002.06038.x
- Goldin RD, Goldin JG, Burt AD, et al. Intra-observer and inter-observer variation in the histopathological assessment of chronic viral hepatitis. J Hepatol 1996; 25(5):649–654. pmid:8938541
- Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. The French METAVIR Cooperative Study Group. Hepatology 1994; 20(1 Pt 1):15–20. pmid:8020885
- Sterling RK, Lissen E, Clumeck N, et al; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006; 43(6):1317–1325. doi:10.1002/hep.21178
- Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology 2007; 46(1):32–36. doi:10.1002/hep.21669
- Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2009; 7(10):1104–1112. doi:10.1016/j.cgh.2009.05.033
- McPherson S, Stewart SF, Henderson E, Burt AD, Day CP. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut 2010; 59(9):1265–1269. doi:10.1136/gut.2010.216077
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45(4):846–854. doi:10.1002/hep.21496
- Goh GB, Pagadala MR, Dasarathy J, et al. Clinical spectrum of non-alcoholic fatty liver disease in diabetic and non-diabetic patients. BBA Clin 2015; 3:141–145. doi:10.1016/j.bbacli.2014.09.001
- Tapper EB, Hunink MG, Afdhal NH, Lai M, Sengupta N. Cost-effectiveness analysis: risk stratification of nonalcoholic fatty liver disease (NAFLD) by the primary care physician using the NAFLD fibrosis score. PLoS One 2016; 11(2):e0147237. doi:10.1371/journal.pone.0147237
- Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003; 38(2):518–526. doi:10.1053/jhep.2003.50346
- Calès P, Lainé F, Boursier J, et al. Comparison of blood tests for liver fibrosis specific or not to NAFLD. J Hepatol 2009; 50(1):165–173. doi:10.1016/j.jhep.2008.07.035
- Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T; MULTIVIRC Group. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet 2001; 357(9262):1069–1075. doi:10.1016/S0140-6736(00)04258-6
- Shaheen AA, Wan AF, Myers RP. FibroTest and FibroScan for the prediction of hepatitis C-related fibrosis: a systematic review of diagnostic test accuracy. Am J Gastroenterol 2007; 102(11):2589–2600. doi:10.1111/j.1572-0241.2007.01466.x
- Smith JO, Sterling RK. Systematic review: non-invasive methods of fibrosis analysis in chronic hepatitis C. Aliment Pharmacol Ther 2009; 30(6):557–576. doi:10.1111/j.1365-2036.2009.04062.x
- Sebastiani G, Vario A, Guido M, Alberti A. Performance of noninvasive markers for liver fibrosis is reduced in chronic hepatitis C with normal transaminases. J Viral Hepat 2007; 15(3):212–218. doi:10.1111/j.1365-2893.2007.00932.x
- Poynard T, Morra R, Halfon P, et al. Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol 2007; 7:40. doi:10.1186/1471-230X-7-40
- Carlson JJ, Kowdley KV, Sullivan SD, Ramsey SD, Veenstra DL. An evaluation of the potential cost-effectiveness of non-invasive testing strategies in the diagnosis of significant liver fibrosis. J Gastroenterol Hepatol 2009; 24(5):786–791. doi:10.1111/j.1440-1746.2009.05778.x
- Aubé C, Oberti F, Korali N, et al. Ultrasonographic diagnosis of hepatic fibrosis or cirrhosis. J Hepatol 1999; 30(3):472–478. pmid:10190731
- Di Lelio A, Cestari C, Lomazzi A, Beretta L. Cirrhosis: diagnosis with sonographic study of the liver surface. Radiology 1989; 172(2):389–392. doi:10.1148/radiology.172.2.2526349
- Wong VW, Chan HL. Transient elastography. J Gastroenterol Hepatol 2010; 25(11):1726–1731. doi:10.1111/j.1440-1746.2010.06437.x
- Arena U, Vizzutti F, Abraldes JG, et al. Reliability of transient elastography for the diagnosis of advanced fibrosis in chronic hepatitis C. Gut 2008; 57(9):1288–1293. doi:10.1136/gut.2008.149708
- Ziol M, Handra-Luca A, Kettaneh A, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology 2005; 41(1):48–54. doi:10.1002/hep.20506
- Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology 2010; 51(2):454–462. doi:10.1002/hep.23312
- Sagir A, Erhardt A, Schmitt M, Häussinger D. Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology 2007; 48(2):592–595. doi:10.1002/hep.22056
- Mederacke I, Wursthorn K, Kirschner J, et al. Food intake increases liver stiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int 2009; 29(10):1500–1506. doi:10.1111/j.1478-3231.2009.02100.x
- Castéra L, Foucher J, Bernard PH, et al. Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology 2010; 51(3):828–835. doi:10.1002/hep.23425
- Wong VW, Vergniol J, Wong GL, et al. Liver stiffness measurement using XL probe in patients with nonalcoholic fatty liver disease. Am J Gastroenterol 2012; 107(12):1862–1871. doi:10.1038/ajg.2012.331
- Fraquelli M, Rigamonti C, Casazza G, et al. Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut 2007; 56(7):968–973. doi:10.1136/gut.2006.111302
- de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol 2015; 63(3):743–752. doi:10.1016/j.jhep.2015.05.022
- Friedrich-Rust M, Wunder K, Kriener S, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology 2009; 252(2):595–604. doi:10.1148/radiol.2523081928
- Yoneda M, Suzuki K, Kato S, et al. Nonalcoholic fatty liver disease: US-based acoustic radiation force impulse elastography. Radiology 2010; 256(2):640–647. doi:10.1148/radiol.10091662
- Bota S, Herkner H, Sporea I, et al. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int 2013; 33(8):1138–1147. doi:10.1111/liv.12240
- Attia D, Bantel H, Lenzen H, Manns MP, Gebel MJ, Potthoff A. Liver stiffness measurement using acoustic radiation force impulse elastography in overweight and obese patients. Aliment Pharmacol Ther 2016; 44(4):366–379. doi:10.1111/apt.13710
- Cui J, Heba E, Hernandez C, et al. Magnetic resonance elastography is superior to acoustic radiation force impulse for the diagnosis of fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease: a prospective study. Hepatology 2016; 63(2):453–461. doi:10.1002/hep.28337
- Huwart L, Sempoux C, Vicaut E, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology 2008; 135(1):32–40. doi:10.1053/j.gastro.2008.03.076
- Jajamovich GH, Dyvorne H, Donnerhack C, Taouli B. Quantitative liver MRI combining phase contrast imaging, elastography, and DWI: assessment of reproducibility and postprandial effect at 3.0 T. PLoS One 2014; 9(5):e97355. doi:10.1371/journal.pone.0097355
- Lim JK, Flamm SL, Singh S, Falck-Ytter YT; Clinical Guidelines Committee of the American Gastroenterological Association. American Gastroenterological Association Institute guideline on the role of elastography in the evaluation of liver fibrosis. Gastroenterology 2017; 152(6):1536–1543. doi:10.1053/j.gastro.2017.03.017
- N, Feldstein AE. Noninvasive diagnosis of nonalcoholic fatty liver disease: are we there yet? Metabolism 2016; 65(8):1087–1095. doi:10.1016/j.metabol.2016.01.013
KEY POINTS
- Liver biopsy remains the gold standard for determining fibrosis stage but is expensive and entails risk of complications.
- For patients infected with HCV, fibrosis stage should be determined with transient elastography, a transthoracic ultrasonographic technique that measures shear-wave velocity.
- For patients with cirrhosis, transient elastography combined with a platelet count can detect developing portal hypertension and determine whether to screen for esophageal varices.
- For NAFLD, combined elastography and NAFLD fibrosis score—which incorporates patient characteristics and laboratory test results—should be used to determine the need for liver biopsy.