User login
Polycystic Ovary Syndrome Associated With Midlife Memory, Thinking Problems
TOPLINE:
People with polycystic ovary syndrome (PCOS) may score lower on cognitive tests than people without the condition, a research showed. They also may have worse integrity of brain tissue as evident on an MRI.
METHODOLOGY:
- Researchers used data from the Coronary Artery Risk Development in Young Adults Women’s Study; individuals were 18-30 years old at the beginning of the study and were followed over 30 years.
- A little over 900 women were included in the study, of which 66 had PCOS, which was defined as having elevated androgen levels or self-reported hirsutism and irregular menstrual cycles more than 32 days apart.
- Study participants completed tests measuring verbal learning and memory, processing speed and executive function, attention and cognitive control, and semantics and attention.
- Researchers analyzed brain white matter integrity for 291 of the individuals, including 25 with PCOS, who underwent MRI.
TAKEAWAY:
- Individuals with PCOS had worse memory, attention, and verbal ability scores than those without the disorder.
- MRI scans showed that those with PCOS had lower white matter integrity, an indicator of cognitive deficits, including poorer decision-making abilities.
- Those in the PCOS group were more likely to be White and have diabetes than those in the control group.
IN PRACTICE:
“This report of midlife cognition in PCOS raises a new concern about another potential comorbidity for individuals with this common disorder; given that up to 10% of women may be affected by PCOS, these results have important implications for public health at large,” the authors concluded.
SOURCE:
Heather G. Huddleston, MD, director of the PCOS Clinic at the UCSF Health, San Francisco, California, is the lead author of the study published in Neurology.
LIMITATIONS:
PCOS was determined on the basis of serum androgen levels and self-reporting of hirsutism and oligomenorrhea, so some cases may have been misclassified without the official diagnosis of a clinician.
DISCLOSURES:
The authors did not report any relevant financial conflicts. The study was funded by a grant from the University of California, San Francisco, California.
A version of this article appeared on Medscape.com.
TOPLINE:
People with polycystic ovary syndrome (PCOS) may score lower on cognitive tests than people without the condition, a research showed. They also may have worse integrity of brain tissue as evident on an MRI.
METHODOLOGY:
- Researchers used data from the Coronary Artery Risk Development in Young Adults Women’s Study; individuals were 18-30 years old at the beginning of the study and were followed over 30 years.
- A little over 900 women were included in the study, of which 66 had PCOS, which was defined as having elevated androgen levels or self-reported hirsutism and irregular menstrual cycles more than 32 days apart.
- Study participants completed tests measuring verbal learning and memory, processing speed and executive function, attention and cognitive control, and semantics and attention.
- Researchers analyzed brain white matter integrity for 291 of the individuals, including 25 with PCOS, who underwent MRI.
TAKEAWAY:
- Individuals with PCOS had worse memory, attention, and verbal ability scores than those without the disorder.
- MRI scans showed that those with PCOS had lower white matter integrity, an indicator of cognitive deficits, including poorer decision-making abilities.
- Those in the PCOS group were more likely to be White and have diabetes than those in the control group.
IN PRACTICE:
“This report of midlife cognition in PCOS raises a new concern about another potential comorbidity for individuals with this common disorder; given that up to 10% of women may be affected by PCOS, these results have important implications for public health at large,” the authors concluded.
SOURCE:
Heather G. Huddleston, MD, director of the PCOS Clinic at the UCSF Health, San Francisco, California, is the lead author of the study published in Neurology.
LIMITATIONS:
PCOS was determined on the basis of serum androgen levels and self-reporting of hirsutism and oligomenorrhea, so some cases may have been misclassified without the official diagnosis of a clinician.
DISCLOSURES:
The authors did not report any relevant financial conflicts. The study was funded by a grant from the University of California, San Francisco, California.
A version of this article appeared on Medscape.com.
TOPLINE:
People with polycystic ovary syndrome (PCOS) may score lower on cognitive tests than people without the condition, a research showed. They also may have worse integrity of brain tissue as evident on an MRI.
METHODOLOGY:
- Researchers used data from the Coronary Artery Risk Development in Young Adults Women’s Study; individuals were 18-30 years old at the beginning of the study and were followed over 30 years.
- A little over 900 women were included in the study, of which 66 had PCOS, which was defined as having elevated androgen levels or self-reported hirsutism and irregular menstrual cycles more than 32 days apart.
- Study participants completed tests measuring verbal learning and memory, processing speed and executive function, attention and cognitive control, and semantics and attention.
- Researchers analyzed brain white matter integrity for 291 of the individuals, including 25 with PCOS, who underwent MRI.
TAKEAWAY:
- Individuals with PCOS had worse memory, attention, and verbal ability scores than those without the disorder.
- MRI scans showed that those with PCOS had lower white matter integrity, an indicator of cognitive deficits, including poorer decision-making abilities.
- Those in the PCOS group were more likely to be White and have diabetes than those in the control group.
IN PRACTICE:
“This report of midlife cognition in PCOS raises a new concern about another potential comorbidity for individuals with this common disorder; given that up to 10% of women may be affected by PCOS, these results have important implications for public health at large,” the authors concluded.
SOURCE:
Heather G. Huddleston, MD, director of the PCOS Clinic at the UCSF Health, San Francisco, California, is the lead author of the study published in Neurology.
LIMITATIONS:
PCOS was determined on the basis of serum androgen levels and self-reporting of hirsutism and oligomenorrhea, so some cases may have been misclassified without the official diagnosis of a clinician.
DISCLOSURES:
The authors did not report any relevant financial conflicts. The study was funded by a grant from the University of California, San Francisco, California.
A version of this article appeared on Medscape.com.
CT Poses Risk for Malignant Hematopathies Among Children
More than a million European children undergo a CT scan each year. Ionizing radiation at moderate (> 100 mGy) to high (> 1 Gy) doses is a recognized risk factor for malignant hematopathies. The risk associated with exposure to low doses (< 100 mGy), typically delivered during a CT scan in children or adolescents, is unknown.
Previous studies assessed the risk for malignant hematopathies related to ionizing radiation from CT scans in young patients. Some showed an increased risk for leukemia with repeated scans, but confounding factors resulted in a lack of statistical power or biases in some cases. The EPI-CT study, coordinated by the International Agency for Research on Cancer, aimed to evaluate the cancer risk among children and adolescents after exposure to low doses of ionizing radiation during CT scans.
A European Cohort
A recent article presents an assessment of observed malignant hematopathies following CT scan. The authors followed a multinational European cohort of 948,174 patients who had a CT scan before age 22 years. Ionizing radiation doses to the bone marrow were evaluated based on the scanned body region, patient characteristics, scan year, and the technical parameters of the machine. The analysis involved 876,771 patients who underwent 1,331,896 scans (an average of 1.52 per patient) and were followed for at least 2 years after the first scan.
In total, 790 malignant hematopathies were diagnosed, including 578 lymphoid hematopathies and 203 myeloid hematopathies and acute leukemias. The average follow-up period was 7.8 years. At the time of diagnosis, 51% of patients were under the age of 20 years, and 88.5% were under the age of 30 years. There was an association between cumulative dose and the observed malignant hematopathy, with an observed rate of 1.96 per 100 mGy (790 cases).
This rate corresponds to a 16% increased rate per scan (for a dose observed per scan of 8 mGy). A higher rate for any type of malignant hematopathy was observed for doses > 10 mGy, with an observed rate of 2.66 for doses > 50 mGy, compared with doses < 5 mGy.
The rate of malignant hematopathy increased with older age at the time of radiation exposure, particularly for lymphoid observations. The rate in the 5- to 9-year age group and the > 10-year age group was, respectively, two times and three to four times higher than that in the < 5-year age group. The rate decreased over time, with the highest observed rate between 2 and 5 years after ionizing radiation exposure and the lowest after 10 years.
CT Scans Must Be Warranted
This study, which involved nearly a million patients, has higher statistical power than previous studies, despite missing or approximate data (including that related to actually delivered doses). An association was shown between cumulative dose to the bone marrow and the risk of developing malignant hematopathy, both lymphoid and myeloid, with an increased risk even at low doses (10-15 mGy).
The results suggest that for every 10,000 children examined today (with a dose per scan of 8 mGy), 1-2 could develop a radiation-related malignant hematopathy in the next 12 years (1.4 cases). This study confirms the higher risk for cancer at low radiation doses and emphasizes the importance of justifying each pediatric CT scan and optimizing delivered doses. It is important to recall that an MRI or ultrasound can sometimes be an adequate substitute for a CT scan.
This article was translated from JIM , which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com .
More than a million European children undergo a CT scan each year. Ionizing radiation at moderate (> 100 mGy) to high (> 1 Gy) doses is a recognized risk factor for malignant hematopathies. The risk associated with exposure to low doses (< 100 mGy), typically delivered during a CT scan in children or adolescents, is unknown.
Previous studies assessed the risk for malignant hematopathies related to ionizing radiation from CT scans in young patients. Some showed an increased risk for leukemia with repeated scans, but confounding factors resulted in a lack of statistical power or biases in some cases. The EPI-CT study, coordinated by the International Agency for Research on Cancer, aimed to evaluate the cancer risk among children and adolescents after exposure to low doses of ionizing radiation during CT scans.
A European Cohort
A recent article presents an assessment of observed malignant hematopathies following CT scan. The authors followed a multinational European cohort of 948,174 patients who had a CT scan before age 22 years. Ionizing radiation doses to the bone marrow were evaluated based on the scanned body region, patient characteristics, scan year, and the technical parameters of the machine. The analysis involved 876,771 patients who underwent 1,331,896 scans (an average of 1.52 per patient) and were followed for at least 2 years after the first scan.
In total, 790 malignant hematopathies were diagnosed, including 578 lymphoid hematopathies and 203 myeloid hematopathies and acute leukemias. The average follow-up period was 7.8 years. At the time of diagnosis, 51% of patients were under the age of 20 years, and 88.5% were under the age of 30 years. There was an association between cumulative dose and the observed malignant hematopathy, with an observed rate of 1.96 per 100 mGy (790 cases).
This rate corresponds to a 16% increased rate per scan (for a dose observed per scan of 8 mGy). A higher rate for any type of malignant hematopathy was observed for doses > 10 mGy, with an observed rate of 2.66 for doses > 50 mGy, compared with doses < 5 mGy.
The rate of malignant hematopathy increased with older age at the time of radiation exposure, particularly for lymphoid observations. The rate in the 5- to 9-year age group and the > 10-year age group was, respectively, two times and three to four times higher than that in the < 5-year age group. The rate decreased over time, with the highest observed rate between 2 and 5 years after ionizing radiation exposure and the lowest after 10 years.
CT Scans Must Be Warranted
This study, which involved nearly a million patients, has higher statistical power than previous studies, despite missing or approximate data (including that related to actually delivered doses). An association was shown between cumulative dose to the bone marrow and the risk of developing malignant hematopathy, both lymphoid and myeloid, with an increased risk even at low doses (10-15 mGy).
The results suggest that for every 10,000 children examined today (with a dose per scan of 8 mGy), 1-2 could develop a radiation-related malignant hematopathy in the next 12 years (1.4 cases). This study confirms the higher risk for cancer at low radiation doses and emphasizes the importance of justifying each pediatric CT scan and optimizing delivered doses. It is important to recall that an MRI or ultrasound can sometimes be an adequate substitute for a CT scan.
This article was translated from JIM , which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com .
More than a million European children undergo a CT scan each year. Ionizing radiation at moderate (> 100 mGy) to high (> 1 Gy) doses is a recognized risk factor for malignant hematopathies. The risk associated with exposure to low doses (< 100 mGy), typically delivered during a CT scan in children or adolescents, is unknown.
Previous studies assessed the risk for malignant hematopathies related to ionizing radiation from CT scans in young patients. Some showed an increased risk for leukemia with repeated scans, but confounding factors resulted in a lack of statistical power or biases in some cases. The EPI-CT study, coordinated by the International Agency for Research on Cancer, aimed to evaluate the cancer risk among children and adolescents after exposure to low doses of ionizing radiation during CT scans.
A European Cohort
A recent article presents an assessment of observed malignant hematopathies following CT scan. The authors followed a multinational European cohort of 948,174 patients who had a CT scan before age 22 years. Ionizing radiation doses to the bone marrow were evaluated based on the scanned body region, patient characteristics, scan year, and the technical parameters of the machine. The analysis involved 876,771 patients who underwent 1,331,896 scans (an average of 1.52 per patient) and were followed for at least 2 years after the first scan.
In total, 790 malignant hematopathies were diagnosed, including 578 lymphoid hematopathies and 203 myeloid hematopathies and acute leukemias. The average follow-up period was 7.8 years. At the time of diagnosis, 51% of patients were under the age of 20 years, and 88.5% were under the age of 30 years. There was an association between cumulative dose and the observed malignant hematopathy, with an observed rate of 1.96 per 100 mGy (790 cases).
This rate corresponds to a 16% increased rate per scan (for a dose observed per scan of 8 mGy). A higher rate for any type of malignant hematopathy was observed for doses > 10 mGy, with an observed rate of 2.66 for doses > 50 mGy, compared with doses < 5 mGy.
The rate of malignant hematopathy increased with older age at the time of radiation exposure, particularly for lymphoid observations. The rate in the 5- to 9-year age group and the > 10-year age group was, respectively, two times and three to four times higher than that in the < 5-year age group. The rate decreased over time, with the highest observed rate between 2 and 5 years after ionizing radiation exposure and the lowest after 10 years.
CT Scans Must Be Warranted
This study, which involved nearly a million patients, has higher statistical power than previous studies, despite missing or approximate data (including that related to actually delivered doses). An association was shown between cumulative dose to the bone marrow and the risk of developing malignant hematopathy, both lymphoid and myeloid, with an increased risk even at low doses (10-15 mGy).
The results suggest that for every 10,000 children examined today (with a dose per scan of 8 mGy), 1-2 could develop a radiation-related malignant hematopathy in the next 12 years (1.4 cases). This study confirms the higher risk for cancer at low radiation doses and emphasizes the importance of justifying each pediatric CT scan and optimizing delivered doses. It is important to recall that an MRI or ultrasound can sometimes be an adequate substitute for a CT scan.
This article was translated from JIM , which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com .
Debate grows over facility fees as lawmakers urge greater transparency
Can the US healthcare system learn something about how to operate from car dealerships? Lawrence Kosinski, MD, MBA, a governing board member of American Gastroenterological Association (AGA), believes so.
There’s growing concern in the United States about the lack of clarity surrounding facility fees, which are intended to cover costs of maintaining medical facilities. Dr. Kosinski thinks that Congress should look into the transparency mandate it created for car prices as a model for how to address this.
A 1958 federal law set the stage for the consumer-friendly breakdown of costs and relevant performance data that anyone who has bought a new vehicle in the United States would recognize.
“You look at that and you know exactly what you are paying for,” Dr. Kosinski told this news organization. “In healthcare, we need something like that.”
Novel solutions like Dr. Kosinski’s will be increasingly necessary, as lawmakers on the state and federal level have begun to set their sights on tackling this issue.
The Biden administration in July expressed concern about an increased use of facility fees for healthcare provided at doctors’ offices, saying these additional costs often surprise consumers. House Energy and Commerce Chairwoman Cathy McMorris Rodgers (R-WA) also raised this issue several times this year, including at a May meeting about pending legislation on price transparency for health services, where she mentioned the case of a man who underwent eye surgery in Maine.
“His bill included three separate facility fees totaling $7800 and professional fees totaling $6200,” Ms. Rodgers said. “Why are three facility fees necessary for 1 hour of surgery in one O.R.?”
AGA’s Dr. Kosinski said facility fees cover the additional costs hospitals and clinics face in providing even routine treatments for some patients. For example, colonoscopy for a patient with a body mass index of 50 would pose special challenges for the anesthesiologist.
These factors need to be considered in setting policies on facility fees, he said. But there is no reason hospitals and other sites of medical care can’t make the information about facility fees easy for patients to find and understand, Dr. Kosinski said.
“I’m struggling to see a reason why we can’t be more transparent,” he said.
Big Battles Ahead
There are two connected battles ahead regarding facility fees: Efforts to restrict these additional charges for many medical services and fights over the need for greater transparency in general about health costs.
Senate Health, Education, Labor and Pensions Chairman Bernie Sanders (I-VT) is seeking to broadly restrict facility fees through his pending Primary Care and Health Workforce Act (S. 2840). The measure would block hospitals from charging health plans facility fees for many evaluation, management, and telehealth services.
The American Hospital Association (AHA) opposes it. They argue that the current payment approach rightly accounts for the added costs incurred when hospitals treat patients who are more likely to be ill or have chronic conditions than those seen in independent practices.
AHA said hospitals also need to maintain standby capacity for natural and man-made disasters, public health emergencies, and unexpected traumatic events. In September, AHA launched a television ad campaign to oppose any drive toward site-neutral policies. AHA says reducing the extra payments could cause more hospitals to shut their doors.
But there’s persistent interest in site-neutral payment, the term describing when the same reimbursement is given for care regardless of setting. This would lower pay for hospitals.
Among those pressing for change is an umbrella group of medical organizations known as the Alliance for Site Neutral Payment Reform. Its members include the American Academy of Family Physicians, American Academy of Orthopaedic Surgeons, American College of Physicians, Community Oncology Alliance, and Digestive Health Physicians Association.
And on November 9, Sen. Maggie Hassan (D-NH) argued for eventually including a site-neutral Medicare provision to a major healthcare package that the Senate Finance Committee is putting together.
Sen. Hassan is seeking to end what she called the “the practice of charging patients unfair hospital facility fees for care provided in the off-campus outpatient setting, like at a regular doctor’s office.”
Senate Finance Chairman Ron Wyden (D-OR) and the ranking Republican on the committee, Sen. Mike Crapo (R-ID), told Sen. Hassan they intended to work with her to see if this issue could be addressed in the pending legislative package.
A 2015 budget deal marked the last time Congress took a major step to address the higher cost of services provided in hospital-owned facilities.
Lawmakers then were scrambling to find cuts to offset spending in what became the 2015 Bipartisan Budget Act. This law established site-neutral payments under Medicare for services received at off-campus outpatient departments but exempted hospitals that already ran these kinds of operations or had advanced plans to create them.
Lawmakers are well aware of the potential savings from site-neutral policies and could look in time again to use them as part of a future budget deal.
In fact, in June, Sen. Hassan and Sens. Mike Braun (R-IN) and John Kennedy (R-LA) introduced a bill meant to basically end the exemption given in the 2015 deal to existing hospital outpatient departments, which has allowed higher Medicare payments. In a press release, Braun estimated that their proposed site-neutral change could save taxpayers $40 billion over a decade.
As Debate Continues, States Are Moving Ahead With Changes
Consumer activists have won a few battles this year at the state level about facility fees.
In July, Maine Gov. Janet Mills, a Democrat, signed a law that requires medical organizations to report facility fees to the state, which will share them publicly. Facility fees can pop up after a patient has received an insurance company estimate of the out-of-pocket costs for care.
“Patients receive bills bloated by healthcare providers that overcharge for services and insurance companies that deny claims without explanation,” the Portland Press Herald reported in a 2022 story. “And with little clout to fight back or even negotiate, feeling helpless, they often give up and pay, worn down by a system that is as time-consuming as it is obtuse.”
In May, Colorado enacted a law that will require patient notification about facility fees at many hospitals in the state.
In June, Connecticut expanded its law regarding facility fees and prohibited them for certain routine outpatient healthcare services. A statement from Gov. Ned Lamont’s office said the original intent of these facility fees was to ensure hospitals could maintain the around-the-clock care needed for inpatient and emergency care.
“However, these fees have been increasingly applied to services such as diagnostic testing and other routine services,” the statement said.
But there have been setbacks as well for those seeking to curb facilities.
The Texas Hospital Association (THA) in May said its advocacy defeated a pair of state bills, House bill 1692 and Senate bill 1275, that sought to limit facility fees for outpatient services.
In rallying opposition to these bills, THA said the loss of facility fees would threaten care for patients. Facility fees help cover costs “beyond the doctor’s bill,” such as “lab technicians, interpreters, medical records, security personnel, janitorial staff, and others,” THA said.
More Patients Shopping?
It’s unclear when — or if — Congress and other states will take major steps to reduce additional payments to hospitals for outpatient care.
But the increased use of high deductibles in health plans is driving more consumers to try to understand all of the costs of medical procedures ahead of time and, thus, drawing attention to facility fees, said Charlie Byrge, the chief operating officer of MDsave.
The average annual deductible levels for an individual increased by 3.0% to $2004 from 2020 to 2021 and for a family plan by 3.9% to $3868, according to a federal report. Some people have higher deductibles, exceeding $5000, Mr. Byrge said.
“That’s creating an opportunity for firms that can connect physicians directly with patients who will pay part or all of the costs of a treatment out of pocket,” he told this news organization.
Doctors and hospitals work with MDsave to charge preset prices for certain services, such as colonoscopies and mammograms. Consumers then can shop online to see if they can save. For example, in Nashville, Tennessee, where MDsave is based, the cost of a colonoscopy through MDsave is $2334, about half of the $4714 national average, according to the firm’s website.
This model for pricing routine medical care is akin to those used for other products and services, where companies decide ahead of time what to charge, he said.
“You don’t buy an airline ticket from Southwest or United or Delta and then there’s a bill after the fact because the price of gas went up a little bit on your flight,” Mr. Byrge said.
This will drive more competition among hospitals and clinics, in places where there are several sites of care in a region, Mr. Byrge said. But there are advantages for physicians and hospitals from the MDsave approach, he said.
“They know they’re getting paid upfront. They’re not going through the delays and headaches of the insurance reimbursement process. There are no denials. It’s just an upfront payment, and I think that’s what we’re starting to see the market really moving toward,” he said.
A version of this article appeared on Medscape.com.
Can the US healthcare system learn something about how to operate from car dealerships? Lawrence Kosinski, MD, MBA, a governing board member of American Gastroenterological Association (AGA), believes so.
There’s growing concern in the United States about the lack of clarity surrounding facility fees, which are intended to cover costs of maintaining medical facilities. Dr. Kosinski thinks that Congress should look into the transparency mandate it created for car prices as a model for how to address this.
A 1958 federal law set the stage for the consumer-friendly breakdown of costs and relevant performance data that anyone who has bought a new vehicle in the United States would recognize.
“You look at that and you know exactly what you are paying for,” Dr. Kosinski told this news organization. “In healthcare, we need something like that.”
Novel solutions like Dr. Kosinski’s will be increasingly necessary, as lawmakers on the state and federal level have begun to set their sights on tackling this issue.
The Biden administration in July expressed concern about an increased use of facility fees for healthcare provided at doctors’ offices, saying these additional costs often surprise consumers. House Energy and Commerce Chairwoman Cathy McMorris Rodgers (R-WA) also raised this issue several times this year, including at a May meeting about pending legislation on price transparency for health services, where she mentioned the case of a man who underwent eye surgery in Maine.
“His bill included three separate facility fees totaling $7800 and professional fees totaling $6200,” Ms. Rodgers said. “Why are three facility fees necessary for 1 hour of surgery in one O.R.?”
AGA’s Dr. Kosinski said facility fees cover the additional costs hospitals and clinics face in providing even routine treatments for some patients. For example, colonoscopy for a patient with a body mass index of 50 would pose special challenges for the anesthesiologist.
These factors need to be considered in setting policies on facility fees, he said. But there is no reason hospitals and other sites of medical care can’t make the information about facility fees easy for patients to find and understand, Dr. Kosinski said.
“I’m struggling to see a reason why we can’t be more transparent,” he said.
Big Battles Ahead
There are two connected battles ahead regarding facility fees: Efforts to restrict these additional charges for many medical services and fights over the need for greater transparency in general about health costs.
Senate Health, Education, Labor and Pensions Chairman Bernie Sanders (I-VT) is seeking to broadly restrict facility fees through his pending Primary Care and Health Workforce Act (S. 2840). The measure would block hospitals from charging health plans facility fees for many evaluation, management, and telehealth services.
The American Hospital Association (AHA) opposes it. They argue that the current payment approach rightly accounts for the added costs incurred when hospitals treat patients who are more likely to be ill or have chronic conditions than those seen in independent practices.
AHA said hospitals also need to maintain standby capacity for natural and man-made disasters, public health emergencies, and unexpected traumatic events. In September, AHA launched a television ad campaign to oppose any drive toward site-neutral policies. AHA says reducing the extra payments could cause more hospitals to shut their doors.
But there’s persistent interest in site-neutral payment, the term describing when the same reimbursement is given for care regardless of setting. This would lower pay for hospitals.
Among those pressing for change is an umbrella group of medical organizations known as the Alliance for Site Neutral Payment Reform. Its members include the American Academy of Family Physicians, American Academy of Orthopaedic Surgeons, American College of Physicians, Community Oncology Alliance, and Digestive Health Physicians Association.
And on November 9, Sen. Maggie Hassan (D-NH) argued for eventually including a site-neutral Medicare provision to a major healthcare package that the Senate Finance Committee is putting together.
Sen. Hassan is seeking to end what she called the “the practice of charging patients unfair hospital facility fees for care provided in the off-campus outpatient setting, like at a regular doctor’s office.”
Senate Finance Chairman Ron Wyden (D-OR) and the ranking Republican on the committee, Sen. Mike Crapo (R-ID), told Sen. Hassan they intended to work with her to see if this issue could be addressed in the pending legislative package.
A 2015 budget deal marked the last time Congress took a major step to address the higher cost of services provided in hospital-owned facilities.
Lawmakers then were scrambling to find cuts to offset spending in what became the 2015 Bipartisan Budget Act. This law established site-neutral payments under Medicare for services received at off-campus outpatient departments but exempted hospitals that already ran these kinds of operations or had advanced plans to create them.
Lawmakers are well aware of the potential savings from site-neutral policies and could look in time again to use them as part of a future budget deal.
In fact, in June, Sen. Hassan and Sens. Mike Braun (R-IN) and John Kennedy (R-LA) introduced a bill meant to basically end the exemption given in the 2015 deal to existing hospital outpatient departments, which has allowed higher Medicare payments. In a press release, Braun estimated that their proposed site-neutral change could save taxpayers $40 billion over a decade.
As Debate Continues, States Are Moving Ahead With Changes
Consumer activists have won a few battles this year at the state level about facility fees.
In July, Maine Gov. Janet Mills, a Democrat, signed a law that requires medical organizations to report facility fees to the state, which will share them publicly. Facility fees can pop up after a patient has received an insurance company estimate of the out-of-pocket costs for care.
“Patients receive bills bloated by healthcare providers that overcharge for services and insurance companies that deny claims without explanation,” the Portland Press Herald reported in a 2022 story. “And with little clout to fight back or even negotiate, feeling helpless, they often give up and pay, worn down by a system that is as time-consuming as it is obtuse.”
In May, Colorado enacted a law that will require patient notification about facility fees at many hospitals in the state.
In June, Connecticut expanded its law regarding facility fees and prohibited them for certain routine outpatient healthcare services. A statement from Gov. Ned Lamont’s office said the original intent of these facility fees was to ensure hospitals could maintain the around-the-clock care needed for inpatient and emergency care.
“However, these fees have been increasingly applied to services such as diagnostic testing and other routine services,” the statement said.
But there have been setbacks as well for those seeking to curb facilities.
The Texas Hospital Association (THA) in May said its advocacy defeated a pair of state bills, House bill 1692 and Senate bill 1275, that sought to limit facility fees for outpatient services.
In rallying opposition to these bills, THA said the loss of facility fees would threaten care for patients. Facility fees help cover costs “beyond the doctor’s bill,” such as “lab technicians, interpreters, medical records, security personnel, janitorial staff, and others,” THA said.
More Patients Shopping?
It’s unclear when — or if — Congress and other states will take major steps to reduce additional payments to hospitals for outpatient care.
But the increased use of high deductibles in health plans is driving more consumers to try to understand all of the costs of medical procedures ahead of time and, thus, drawing attention to facility fees, said Charlie Byrge, the chief operating officer of MDsave.
The average annual deductible levels for an individual increased by 3.0% to $2004 from 2020 to 2021 and for a family plan by 3.9% to $3868, according to a federal report. Some people have higher deductibles, exceeding $5000, Mr. Byrge said.
“That’s creating an opportunity for firms that can connect physicians directly with patients who will pay part or all of the costs of a treatment out of pocket,” he told this news organization.
Doctors and hospitals work with MDsave to charge preset prices for certain services, such as colonoscopies and mammograms. Consumers then can shop online to see if they can save. For example, in Nashville, Tennessee, where MDsave is based, the cost of a colonoscopy through MDsave is $2334, about half of the $4714 national average, according to the firm’s website.
This model for pricing routine medical care is akin to those used for other products and services, where companies decide ahead of time what to charge, he said.
“You don’t buy an airline ticket from Southwest or United or Delta and then there’s a bill after the fact because the price of gas went up a little bit on your flight,” Mr. Byrge said.
This will drive more competition among hospitals and clinics, in places where there are several sites of care in a region, Mr. Byrge said. But there are advantages for physicians and hospitals from the MDsave approach, he said.
“They know they’re getting paid upfront. They’re not going through the delays and headaches of the insurance reimbursement process. There are no denials. It’s just an upfront payment, and I think that’s what we’re starting to see the market really moving toward,” he said.
A version of this article appeared on Medscape.com.
Can the US healthcare system learn something about how to operate from car dealerships? Lawrence Kosinski, MD, MBA, a governing board member of American Gastroenterological Association (AGA), believes so.
There’s growing concern in the United States about the lack of clarity surrounding facility fees, which are intended to cover costs of maintaining medical facilities. Dr. Kosinski thinks that Congress should look into the transparency mandate it created for car prices as a model for how to address this.
A 1958 federal law set the stage for the consumer-friendly breakdown of costs and relevant performance data that anyone who has bought a new vehicle in the United States would recognize.
“You look at that and you know exactly what you are paying for,” Dr. Kosinski told this news organization. “In healthcare, we need something like that.”
Novel solutions like Dr. Kosinski’s will be increasingly necessary, as lawmakers on the state and federal level have begun to set their sights on tackling this issue.
The Biden administration in July expressed concern about an increased use of facility fees for healthcare provided at doctors’ offices, saying these additional costs often surprise consumers. House Energy and Commerce Chairwoman Cathy McMorris Rodgers (R-WA) also raised this issue several times this year, including at a May meeting about pending legislation on price transparency for health services, where she mentioned the case of a man who underwent eye surgery in Maine.
“His bill included three separate facility fees totaling $7800 and professional fees totaling $6200,” Ms. Rodgers said. “Why are three facility fees necessary for 1 hour of surgery in one O.R.?”
AGA’s Dr. Kosinski said facility fees cover the additional costs hospitals and clinics face in providing even routine treatments for some patients. For example, colonoscopy for a patient with a body mass index of 50 would pose special challenges for the anesthesiologist.
These factors need to be considered in setting policies on facility fees, he said. But there is no reason hospitals and other sites of medical care can’t make the information about facility fees easy for patients to find and understand, Dr. Kosinski said.
“I’m struggling to see a reason why we can’t be more transparent,” he said.
Big Battles Ahead
There are two connected battles ahead regarding facility fees: Efforts to restrict these additional charges for many medical services and fights over the need for greater transparency in general about health costs.
Senate Health, Education, Labor and Pensions Chairman Bernie Sanders (I-VT) is seeking to broadly restrict facility fees through his pending Primary Care and Health Workforce Act (S. 2840). The measure would block hospitals from charging health plans facility fees for many evaluation, management, and telehealth services.
The American Hospital Association (AHA) opposes it. They argue that the current payment approach rightly accounts for the added costs incurred when hospitals treat patients who are more likely to be ill or have chronic conditions than those seen in independent practices.
AHA said hospitals also need to maintain standby capacity for natural and man-made disasters, public health emergencies, and unexpected traumatic events. In September, AHA launched a television ad campaign to oppose any drive toward site-neutral policies. AHA says reducing the extra payments could cause more hospitals to shut their doors.
But there’s persistent interest in site-neutral payment, the term describing when the same reimbursement is given for care regardless of setting. This would lower pay for hospitals.
Among those pressing for change is an umbrella group of medical organizations known as the Alliance for Site Neutral Payment Reform. Its members include the American Academy of Family Physicians, American Academy of Orthopaedic Surgeons, American College of Physicians, Community Oncology Alliance, and Digestive Health Physicians Association.
And on November 9, Sen. Maggie Hassan (D-NH) argued for eventually including a site-neutral Medicare provision to a major healthcare package that the Senate Finance Committee is putting together.
Sen. Hassan is seeking to end what she called the “the practice of charging patients unfair hospital facility fees for care provided in the off-campus outpatient setting, like at a regular doctor’s office.”
Senate Finance Chairman Ron Wyden (D-OR) and the ranking Republican on the committee, Sen. Mike Crapo (R-ID), told Sen. Hassan they intended to work with her to see if this issue could be addressed in the pending legislative package.
A 2015 budget deal marked the last time Congress took a major step to address the higher cost of services provided in hospital-owned facilities.
Lawmakers then were scrambling to find cuts to offset spending in what became the 2015 Bipartisan Budget Act. This law established site-neutral payments under Medicare for services received at off-campus outpatient departments but exempted hospitals that already ran these kinds of operations or had advanced plans to create them.
Lawmakers are well aware of the potential savings from site-neutral policies and could look in time again to use them as part of a future budget deal.
In fact, in June, Sen. Hassan and Sens. Mike Braun (R-IN) and John Kennedy (R-LA) introduced a bill meant to basically end the exemption given in the 2015 deal to existing hospital outpatient departments, which has allowed higher Medicare payments. In a press release, Braun estimated that their proposed site-neutral change could save taxpayers $40 billion over a decade.
As Debate Continues, States Are Moving Ahead With Changes
Consumer activists have won a few battles this year at the state level about facility fees.
In July, Maine Gov. Janet Mills, a Democrat, signed a law that requires medical organizations to report facility fees to the state, which will share them publicly. Facility fees can pop up after a patient has received an insurance company estimate of the out-of-pocket costs for care.
“Patients receive bills bloated by healthcare providers that overcharge for services and insurance companies that deny claims without explanation,” the Portland Press Herald reported in a 2022 story. “And with little clout to fight back or even negotiate, feeling helpless, they often give up and pay, worn down by a system that is as time-consuming as it is obtuse.”
In May, Colorado enacted a law that will require patient notification about facility fees at many hospitals in the state.
In June, Connecticut expanded its law regarding facility fees and prohibited them for certain routine outpatient healthcare services. A statement from Gov. Ned Lamont’s office said the original intent of these facility fees was to ensure hospitals could maintain the around-the-clock care needed for inpatient and emergency care.
“However, these fees have been increasingly applied to services such as diagnostic testing and other routine services,” the statement said.
But there have been setbacks as well for those seeking to curb facilities.
The Texas Hospital Association (THA) in May said its advocacy defeated a pair of state bills, House bill 1692 and Senate bill 1275, that sought to limit facility fees for outpatient services.
In rallying opposition to these bills, THA said the loss of facility fees would threaten care for patients. Facility fees help cover costs “beyond the doctor’s bill,” such as “lab technicians, interpreters, medical records, security personnel, janitorial staff, and others,” THA said.
More Patients Shopping?
It’s unclear when — or if — Congress and other states will take major steps to reduce additional payments to hospitals for outpatient care.
But the increased use of high deductibles in health plans is driving more consumers to try to understand all of the costs of medical procedures ahead of time and, thus, drawing attention to facility fees, said Charlie Byrge, the chief operating officer of MDsave.
The average annual deductible levels for an individual increased by 3.0% to $2004 from 2020 to 2021 and for a family plan by 3.9% to $3868, according to a federal report. Some people have higher deductibles, exceeding $5000, Mr. Byrge said.
“That’s creating an opportunity for firms that can connect physicians directly with patients who will pay part or all of the costs of a treatment out of pocket,” he told this news organization.
Doctors and hospitals work with MDsave to charge preset prices for certain services, such as colonoscopies and mammograms. Consumers then can shop online to see if they can save. For example, in Nashville, Tennessee, where MDsave is based, the cost of a colonoscopy through MDsave is $2334, about half of the $4714 national average, according to the firm’s website.
This model for pricing routine medical care is akin to those used for other products and services, where companies decide ahead of time what to charge, he said.
“You don’t buy an airline ticket from Southwest or United or Delta and then there’s a bill after the fact because the price of gas went up a little bit on your flight,” Mr. Byrge said.
This will drive more competition among hospitals and clinics, in places where there are several sites of care in a region, Mr. Byrge said. But there are advantages for physicians and hospitals from the MDsave approach, he said.
“They know they’re getting paid upfront. They’re not going through the delays and headaches of the insurance reimbursement process. There are no denials. It’s just an upfront payment, and I think that’s what we’re starting to see the market really moving toward,” he said.
A version of this article appeared on Medscape.com.
PTSD symptoms in women tied to worse heart, brain health
TOPLINE:
METHODOLOGY:
- Researchers conducted a cross-sectional study of 274 women (mean age, 59 years) participating in the MsBrain study of menopause and brain health.
- As part of the study, the women completed the PTSD Checklist–Civilian Version and underwent physical and neuropsychological testing, as well as carotid artery ultrasonography and brain MRI.
- Outcomes of interest were associations of PTSD symptoms with carotid intima media thickness (IMT), brain white matter hyperintensity volume (WMHV), and cognition, assessed in linear regression models.
- Interactions by APOEε4 were assessed; covariates included age, race/ethnicity, education, and CVD risk factors.
TAKEAWAY:
- Higher PTSD symptoms were associated with greater carotid IMT (P = .03); associations of PTSD symptoms with neurocognitive outcomes varied significantly by APOEε4 status.
- Among APOEε4 carriers, PTSD symptoms were associated with greater whole-brain WMHV (P = .009), periventricular WMHV (P = .02), deep WMHV (P = .01), and frontal WMHV (P = .04) in multivariable models.
- APOEε4 carriers with PTSD symptoms also had poorer cognition, specifically attention and working memory (P = .02), semantic fluency (P = .01), perceptual speed (P = .002) and processing speed (P = .002), in multivariable models.
IN PRACTICE:
“This study sheds important insight on the implications of PTSD symptoms to women’s cardiovascular and neurocognitive health. Our findings indicate that the APOEε4 genotype may identify a group of women with PTSD symptoms at particular risk for poor neurocognitive health,” the authors wrote.
SOURCE:
The study, with first author Rebecca Thurston, PhD, of the department of psychiatry, University of Pittsburgh, was published online in JAMA Network Open.
LIMITATIONS:
No diagnostic clinical interviews were conducted, and PTSD treatment was not assessed. All participants identified as cisgender, and most were non-Hispanic Black or White. The study was observational and cross-sectional, precluding assertions about directionality or causality.
DISCLOSURES:
The study was funded by the National Institutes of Health, the University of Pittsburgh Clinical and Translational Science Institute, and the University of Pittsburgh Small Molecule Biomarker Core. Dr. Thurston reported receiving personal fees from Astellas Pharma, Bayer, Hello Therapeutics, Vira Health, and Happify Health outside the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a cross-sectional study of 274 women (mean age, 59 years) participating in the MsBrain study of menopause and brain health.
- As part of the study, the women completed the PTSD Checklist–Civilian Version and underwent physical and neuropsychological testing, as well as carotid artery ultrasonography and brain MRI.
- Outcomes of interest were associations of PTSD symptoms with carotid intima media thickness (IMT), brain white matter hyperintensity volume (WMHV), and cognition, assessed in linear regression models.
- Interactions by APOEε4 were assessed; covariates included age, race/ethnicity, education, and CVD risk factors.
TAKEAWAY:
- Higher PTSD symptoms were associated with greater carotid IMT (P = .03); associations of PTSD symptoms with neurocognitive outcomes varied significantly by APOEε4 status.
- Among APOEε4 carriers, PTSD symptoms were associated with greater whole-brain WMHV (P = .009), periventricular WMHV (P = .02), deep WMHV (P = .01), and frontal WMHV (P = .04) in multivariable models.
- APOEε4 carriers with PTSD symptoms also had poorer cognition, specifically attention and working memory (P = .02), semantic fluency (P = .01), perceptual speed (P = .002) and processing speed (P = .002), in multivariable models.
IN PRACTICE:
“This study sheds important insight on the implications of PTSD symptoms to women’s cardiovascular and neurocognitive health. Our findings indicate that the APOEε4 genotype may identify a group of women with PTSD symptoms at particular risk for poor neurocognitive health,” the authors wrote.
SOURCE:
The study, with first author Rebecca Thurston, PhD, of the department of psychiatry, University of Pittsburgh, was published online in JAMA Network Open.
LIMITATIONS:
No diagnostic clinical interviews were conducted, and PTSD treatment was not assessed. All participants identified as cisgender, and most were non-Hispanic Black or White. The study was observational and cross-sectional, precluding assertions about directionality or causality.
DISCLOSURES:
The study was funded by the National Institutes of Health, the University of Pittsburgh Clinical and Translational Science Institute, and the University of Pittsburgh Small Molecule Biomarker Core. Dr. Thurston reported receiving personal fees from Astellas Pharma, Bayer, Hello Therapeutics, Vira Health, and Happify Health outside the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a cross-sectional study of 274 women (mean age, 59 years) participating in the MsBrain study of menopause and brain health.
- As part of the study, the women completed the PTSD Checklist–Civilian Version and underwent physical and neuropsychological testing, as well as carotid artery ultrasonography and brain MRI.
- Outcomes of interest were associations of PTSD symptoms with carotid intima media thickness (IMT), brain white matter hyperintensity volume (WMHV), and cognition, assessed in linear regression models.
- Interactions by APOEε4 were assessed; covariates included age, race/ethnicity, education, and CVD risk factors.
TAKEAWAY:
- Higher PTSD symptoms were associated with greater carotid IMT (P = .03); associations of PTSD symptoms with neurocognitive outcomes varied significantly by APOEε4 status.
- Among APOEε4 carriers, PTSD symptoms were associated with greater whole-brain WMHV (P = .009), periventricular WMHV (P = .02), deep WMHV (P = .01), and frontal WMHV (P = .04) in multivariable models.
- APOEε4 carriers with PTSD symptoms also had poorer cognition, specifically attention and working memory (P = .02), semantic fluency (P = .01), perceptual speed (P = .002) and processing speed (P = .002), in multivariable models.
IN PRACTICE:
“This study sheds important insight on the implications of PTSD symptoms to women’s cardiovascular and neurocognitive health. Our findings indicate that the APOEε4 genotype may identify a group of women with PTSD symptoms at particular risk for poor neurocognitive health,” the authors wrote.
SOURCE:
The study, with first author Rebecca Thurston, PhD, of the department of psychiatry, University of Pittsburgh, was published online in JAMA Network Open.
LIMITATIONS:
No diagnostic clinical interviews were conducted, and PTSD treatment was not assessed. All participants identified as cisgender, and most were non-Hispanic Black or White. The study was observational and cross-sectional, precluding assertions about directionality or causality.
DISCLOSURES:
The study was funded by the National Institutes of Health, the University of Pittsburgh Clinical and Translational Science Institute, and the University of Pittsburgh Small Molecule Biomarker Core. Dr. Thurston reported receiving personal fees from Astellas Pharma, Bayer, Hello Therapeutics, Vira Health, and Happify Health outside the submitted work.
A version of this article first appeared on Medscape.com.
AI interpretation of CCTA unlocks value of inflammation as CV risk factor
Risk calculations might be transformed
, according to a study that suggests this approach would change treatment about half the time.
In patients with nonobstructive CAD, CCTA measurement of inflammation on the basis of the Fat Attenuation Index (FAI) “predicts fatal and nonfatal cardiac events independently from clinical risk scores and routine CCTA interpretation,” reported Charalambos Antoniades, MD, PhD, professor of cardiology, Radcliffe Department of Medicine, Oxford, England.
This analysis was based on data from ORFAN, an ongoing study that expects to eventually collect data from 250,000 CCTA. There were multiple goals. The first was to evaluate whether there is a need and a role of CCTA to risk stratify patients without obstructive CAD. A second objective was to evaluate if the FAI inflammation score can quantify residual risk in these patients.
Based on the answers to these questions, the investigators then proceeded to determine if an AI risk model that combines data from the FAI score and risk factors is widely generalizable and, in addition, whether it reclassifies patients in a way meaningful to management.
CCTA-based inflammation is promising
The answers to all these questions were yes, according to data presented by Dr. Antoniades in a late-breaker at the American Heart Association scientific sessions.
So far, ORPHAN, which has multiple participating sites in the United Kingdom, Europe, United States, South America, Asia, and Australia, have data on more than 100,000 CCTAs. Approximately 40,000 have been processed. Of these, 82% have had nonobstructive CAD and the remaining obstructive disease.
In long-term follow-up, the numbers of major adverse cardiovascular events (MACE) and cardiac deaths were compared in these two groups. In absolute terms, the nonobstructive CAD group had about twice as many MACE (2,587 vs. 1,450) and cardiac deaths (1,118 vs. 636).
The rate of these events was much lower in the nonobstructive group , which had four times more patients than the obstructive group, but Dr. Antoniades said these data demonstrate substantial rates of events in the nonobstructive group as well as an unmet need to identify and treat risk associated with nonobstructive CAD.
When determining if coronary inflammation as measured with CCTA could be a means identifying risk independent of other factors, the FAI scores were evaluated by quartile in a nested cohort of 3,666 consecutive patients. FAI, which has been validated, is calculated with spatial changes in CCTA-measured perivascular fat composition after standardization for anatomy and other variables.
The discrimination for risk with FAI was impressive. When evaluated across all patients (obstructive or nonobstructive CAD), those in the highest FAI quartile had a hazard ratio (HR) for MACE that was more than six times higher (HR 6.76; P < .001) and a risk of cardiac mortality that was more than 20 times higher (HR 20.20; P < .001) than that of those in the first quartile.
“The prediction was independent of all other risk factors,” Dr. Antoniades reported.
Predictive value greater in nonobstructive CAD
When evaluated in nonobstructive disease, the predictive value of FAI was even greater. In obstructive CAD patients, the increased risk of MACE for the fourth relative to the first quartile was increased threefold (HR 3.15; P < .001), but it was increased almost fivefold among those with nonobstructive CAD (HR 4.77; P < .001). The increases for cardiac mortality were fivefold (HR 5.15; P < .001) and more than 10-fold (HR 10.49; P < .001) in these groups, respectively.
When a risk model based on AI that incorporated FAI plus other cardiovascular risk factors was applied retrospectively to the ORPHAN data, the predicted and actual event graph lines were nearly superimposable over a follow-up to 10 years at risk levels ranging from low to very high.
When this inflammation-based AI model was evaluated against standard risk prediction in patients with nonobstructive CAD, 30% of patients were reclassified to a higher risk category and 10% to a lower risk category.
When the AI-risk calculations were provided to clinicians at four hospitals over a recent 1-year period, it resulted “in changes of management in approximately half of patients,” Dr. Antoniades said.
Overall, Dr. Antoniades said these data provide evidence that coronary inflammation is an important driver of residual risk in patients who have nonobstructive CAD on CCTA, and he believes that the AI-enhanced interpretation of the FAI-based inflammatory burden has the potential to become an important management tool.
“AI-risk assessment may transform risk stratification and management of patients undergoing routine CCTA,” Dr. Antoniades said.
Imaging has potential for expanded risk assessment
The AHA-invited discussant, Viviany R. Taqueti, MD, director of the cardiac stress laboratory at Brigham and Women’s Hospital, Boston, agreed with the promise of evaluating inflammatory infiltrate in the coronary arteries as well as looking at fat in other tissues, such as skeletal muscle, to better risk stratify patients, but she cautioned about the limitations of conclusions based on observational data.
“A registry is not a randomized trial,” she said.
Characterizing AI as a “black box” in terms of understanding methodology, she also recommended further studies to validate the relative contribution of AI to inflammation alone in risk stratification.
Still, she believes that the “explosive growth” in imaging has created new opportunities for more precisely evaluating cardiovascular risk. She said these might be particularly helpful in the context of the “changing landscape” in CAD driven by less smoking, more obesity, and increased statin use. Overall, she endorsed the basic questions Dr. Antoniades is exploring.
“This is an incredibly intriguing idea that deserves continuing research,” she said.
Dr. Antoniades reported financial relationships with Amarin, AstraZeneca, Caristo Diagnostics, Covance, Mitsubishi Tanabe, MedImmune, Novo Nordisk, Sanofi, and Silence Therapeutics. Dr. Taqueti reported no potential conflicts of interest.
Risk calculations might be transformed
Risk calculations might be transformed
, according to a study that suggests this approach would change treatment about half the time.
In patients with nonobstructive CAD, CCTA measurement of inflammation on the basis of the Fat Attenuation Index (FAI) “predicts fatal and nonfatal cardiac events independently from clinical risk scores and routine CCTA interpretation,” reported Charalambos Antoniades, MD, PhD, professor of cardiology, Radcliffe Department of Medicine, Oxford, England.
This analysis was based on data from ORFAN, an ongoing study that expects to eventually collect data from 250,000 CCTA. There were multiple goals. The first was to evaluate whether there is a need and a role of CCTA to risk stratify patients without obstructive CAD. A second objective was to evaluate if the FAI inflammation score can quantify residual risk in these patients.
Based on the answers to these questions, the investigators then proceeded to determine if an AI risk model that combines data from the FAI score and risk factors is widely generalizable and, in addition, whether it reclassifies patients in a way meaningful to management.
CCTA-based inflammation is promising
The answers to all these questions were yes, according to data presented by Dr. Antoniades in a late-breaker at the American Heart Association scientific sessions.
So far, ORPHAN, which has multiple participating sites in the United Kingdom, Europe, United States, South America, Asia, and Australia, have data on more than 100,000 CCTAs. Approximately 40,000 have been processed. Of these, 82% have had nonobstructive CAD and the remaining obstructive disease.
In long-term follow-up, the numbers of major adverse cardiovascular events (MACE) and cardiac deaths were compared in these two groups. In absolute terms, the nonobstructive CAD group had about twice as many MACE (2,587 vs. 1,450) and cardiac deaths (1,118 vs. 636).
The rate of these events was much lower in the nonobstructive group , which had four times more patients than the obstructive group, but Dr. Antoniades said these data demonstrate substantial rates of events in the nonobstructive group as well as an unmet need to identify and treat risk associated with nonobstructive CAD.
When determining if coronary inflammation as measured with CCTA could be a means identifying risk independent of other factors, the FAI scores were evaluated by quartile in a nested cohort of 3,666 consecutive patients. FAI, which has been validated, is calculated with spatial changes in CCTA-measured perivascular fat composition after standardization for anatomy and other variables.
The discrimination for risk with FAI was impressive. When evaluated across all patients (obstructive or nonobstructive CAD), those in the highest FAI quartile had a hazard ratio (HR) for MACE that was more than six times higher (HR 6.76; P < .001) and a risk of cardiac mortality that was more than 20 times higher (HR 20.20; P < .001) than that of those in the first quartile.
“The prediction was independent of all other risk factors,” Dr. Antoniades reported.
Predictive value greater in nonobstructive CAD
When evaluated in nonobstructive disease, the predictive value of FAI was even greater. In obstructive CAD patients, the increased risk of MACE for the fourth relative to the first quartile was increased threefold (HR 3.15; P < .001), but it was increased almost fivefold among those with nonobstructive CAD (HR 4.77; P < .001). The increases for cardiac mortality were fivefold (HR 5.15; P < .001) and more than 10-fold (HR 10.49; P < .001) in these groups, respectively.
When a risk model based on AI that incorporated FAI plus other cardiovascular risk factors was applied retrospectively to the ORPHAN data, the predicted and actual event graph lines were nearly superimposable over a follow-up to 10 years at risk levels ranging from low to very high.
When this inflammation-based AI model was evaluated against standard risk prediction in patients with nonobstructive CAD, 30% of patients were reclassified to a higher risk category and 10% to a lower risk category.
When the AI-risk calculations were provided to clinicians at four hospitals over a recent 1-year period, it resulted “in changes of management in approximately half of patients,” Dr. Antoniades said.
Overall, Dr. Antoniades said these data provide evidence that coronary inflammation is an important driver of residual risk in patients who have nonobstructive CAD on CCTA, and he believes that the AI-enhanced interpretation of the FAI-based inflammatory burden has the potential to become an important management tool.
“AI-risk assessment may transform risk stratification and management of patients undergoing routine CCTA,” Dr. Antoniades said.
Imaging has potential for expanded risk assessment
The AHA-invited discussant, Viviany R. Taqueti, MD, director of the cardiac stress laboratory at Brigham and Women’s Hospital, Boston, agreed with the promise of evaluating inflammatory infiltrate in the coronary arteries as well as looking at fat in other tissues, such as skeletal muscle, to better risk stratify patients, but she cautioned about the limitations of conclusions based on observational data.
“A registry is not a randomized trial,” she said.
Characterizing AI as a “black box” in terms of understanding methodology, she also recommended further studies to validate the relative contribution of AI to inflammation alone in risk stratification.
Still, she believes that the “explosive growth” in imaging has created new opportunities for more precisely evaluating cardiovascular risk. She said these might be particularly helpful in the context of the “changing landscape” in CAD driven by less smoking, more obesity, and increased statin use. Overall, she endorsed the basic questions Dr. Antoniades is exploring.
“This is an incredibly intriguing idea that deserves continuing research,” she said.
Dr. Antoniades reported financial relationships with Amarin, AstraZeneca, Caristo Diagnostics, Covance, Mitsubishi Tanabe, MedImmune, Novo Nordisk, Sanofi, and Silence Therapeutics. Dr. Taqueti reported no potential conflicts of interest.
, according to a study that suggests this approach would change treatment about half the time.
In patients with nonobstructive CAD, CCTA measurement of inflammation on the basis of the Fat Attenuation Index (FAI) “predicts fatal and nonfatal cardiac events independently from clinical risk scores and routine CCTA interpretation,” reported Charalambos Antoniades, MD, PhD, professor of cardiology, Radcliffe Department of Medicine, Oxford, England.
This analysis was based on data from ORFAN, an ongoing study that expects to eventually collect data from 250,000 CCTA. There were multiple goals. The first was to evaluate whether there is a need and a role of CCTA to risk stratify patients without obstructive CAD. A second objective was to evaluate if the FAI inflammation score can quantify residual risk in these patients.
Based on the answers to these questions, the investigators then proceeded to determine if an AI risk model that combines data from the FAI score and risk factors is widely generalizable and, in addition, whether it reclassifies patients in a way meaningful to management.
CCTA-based inflammation is promising
The answers to all these questions were yes, according to data presented by Dr. Antoniades in a late-breaker at the American Heart Association scientific sessions.
So far, ORPHAN, which has multiple participating sites in the United Kingdom, Europe, United States, South America, Asia, and Australia, have data on more than 100,000 CCTAs. Approximately 40,000 have been processed. Of these, 82% have had nonobstructive CAD and the remaining obstructive disease.
In long-term follow-up, the numbers of major adverse cardiovascular events (MACE) and cardiac deaths were compared in these two groups. In absolute terms, the nonobstructive CAD group had about twice as many MACE (2,587 vs. 1,450) and cardiac deaths (1,118 vs. 636).
The rate of these events was much lower in the nonobstructive group , which had four times more patients than the obstructive group, but Dr. Antoniades said these data demonstrate substantial rates of events in the nonobstructive group as well as an unmet need to identify and treat risk associated with nonobstructive CAD.
When determining if coronary inflammation as measured with CCTA could be a means identifying risk independent of other factors, the FAI scores were evaluated by quartile in a nested cohort of 3,666 consecutive patients. FAI, which has been validated, is calculated with spatial changes in CCTA-measured perivascular fat composition after standardization for anatomy and other variables.
The discrimination for risk with FAI was impressive. When evaluated across all patients (obstructive or nonobstructive CAD), those in the highest FAI quartile had a hazard ratio (HR) for MACE that was more than six times higher (HR 6.76; P < .001) and a risk of cardiac mortality that was more than 20 times higher (HR 20.20; P < .001) than that of those in the first quartile.
“The prediction was independent of all other risk factors,” Dr. Antoniades reported.
Predictive value greater in nonobstructive CAD
When evaluated in nonobstructive disease, the predictive value of FAI was even greater. In obstructive CAD patients, the increased risk of MACE for the fourth relative to the first quartile was increased threefold (HR 3.15; P < .001), but it was increased almost fivefold among those with nonobstructive CAD (HR 4.77; P < .001). The increases for cardiac mortality were fivefold (HR 5.15; P < .001) and more than 10-fold (HR 10.49; P < .001) in these groups, respectively.
When a risk model based on AI that incorporated FAI plus other cardiovascular risk factors was applied retrospectively to the ORPHAN data, the predicted and actual event graph lines were nearly superimposable over a follow-up to 10 years at risk levels ranging from low to very high.
When this inflammation-based AI model was evaluated against standard risk prediction in patients with nonobstructive CAD, 30% of patients were reclassified to a higher risk category and 10% to a lower risk category.
When the AI-risk calculations were provided to clinicians at four hospitals over a recent 1-year period, it resulted “in changes of management in approximately half of patients,” Dr. Antoniades said.
Overall, Dr. Antoniades said these data provide evidence that coronary inflammation is an important driver of residual risk in patients who have nonobstructive CAD on CCTA, and he believes that the AI-enhanced interpretation of the FAI-based inflammatory burden has the potential to become an important management tool.
“AI-risk assessment may transform risk stratification and management of patients undergoing routine CCTA,” Dr. Antoniades said.
Imaging has potential for expanded risk assessment
The AHA-invited discussant, Viviany R. Taqueti, MD, director of the cardiac stress laboratory at Brigham and Women’s Hospital, Boston, agreed with the promise of evaluating inflammatory infiltrate in the coronary arteries as well as looking at fat in other tissues, such as skeletal muscle, to better risk stratify patients, but she cautioned about the limitations of conclusions based on observational data.
“A registry is not a randomized trial,” she said.
Characterizing AI as a “black box” in terms of understanding methodology, she also recommended further studies to validate the relative contribution of AI to inflammation alone in risk stratification.
Still, she believes that the “explosive growth” in imaging has created new opportunities for more precisely evaluating cardiovascular risk. She said these might be particularly helpful in the context of the “changing landscape” in CAD driven by less smoking, more obesity, and increased statin use. Overall, she endorsed the basic questions Dr. Antoniades is exploring.
“This is an incredibly intriguing idea that deserves continuing research,” she said.
Dr. Antoniades reported financial relationships with Amarin, AstraZeneca, Caristo Diagnostics, Covance, Mitsubishi Tanabe, MedImmune, Novo Nordisk, Sanofi, and Silence Therapeutics. Dr. Taqueti reported no potential conflicts of interest.
FROM AHA 2023
AI-ECG gets STEMI patients to cath lab sooner
PHILADELPHIA – An artificial intelligence platform that sends alerts based on electrocardiography results enabled cardiologists and emergency department physicians at a major hospital in Taiwan to move patients with ST-elevation myocardial infarction (STEMI) into the catheterization laboratory 9 minutes sooner than the conventional protocol that did not use AI.
“This is the first randomized clinical trial to demonstrate the reduction of electrocardiography to coronary cath lab activation time" from 52.3 to 43.3 minutes (P = .003), Chin Sheng Lin, MD, PhD, director of cardiology at the National Defense Medical Center Tri-Service General Hospital in Taipei City, said in presenting the results at the American Heart Association scientific sessions.
Dr. Lin reported results from the Artificial Intelligence Enabled Rapid Identify of ST-Elevation Myocardial Infarction Using Electrocardiogram (ARISE) trial. The trial included 43,994 patients who came to the hospital’s emergency and inpatient departments with at least one ECG but no history of coronary angiography (CAG) in the previous 3 days between May 2022 and April 2023.
They were randomly assigned by date to either AI-ECG for rapid identification and triage of STEMI or standard care. Overall, 145 patients were finally diagnosed with STEMI based on CAG, 77 in the intervention group and 68 in the control group. All patients were seen by one of 20 cardiologists who participated in the study.
Dr. Lin and his group developed an AI algorithm that captures the ECG readout in the emergency department, analyzes the data and then sends a high-risk alarm to the front-line physician and on-duty cardiologist to activate the primary percutaneous coronary intervention (PCI).
Trial results
The differentiation between groups was even more pronounced in ED patients during regular working hours, Dr. Lin said, at 61.6 minutes for the intervention group vs. 33.1 minutes for controls (P = .001).*
He noted that the AI group showed a trend towards fewer cases of clinically suspected STEMI but not getting CAG, 6.5% vs. 15.8%, for an odds ratio of 0.37 (95% confidence interval, 0.14-0.94).
The AI-ECG model also demonstrated a high diagnostic accuracy. “With this AI-ECG system, because it has a very high accuracy and a high positive predictive variable that reach 88%, we can send a message to the on-duty cardiologists and also the emergency room physician and they can send the patients to receive the operation or the PCI as soon as possible,” Dr. Lin said in an interview.
The time differential is critical, Dr. Lin said. “For the patient with acute myocardial infarction, 1 minute is critical, because the patients can die within minutes,” he said. “If we can save 9 minutes I think we can save more lives, but it needs a larger study to evaluate that.”
Dr. Lin acknowledged a few limitations with the trial, among them its single-center nature, relatively small sample size of STEMI patients and the short-term of follow-up. Future study should involve multiple centers along with a prehospital, emergency medical services AI-ECG model.
‘Novel’ for an AI trial
“This is an incredible application of an AI technology in a real-world problem,” said Brahmajee K. Nallamothu, MD, MPH, an interventional cardiologist at the University of Michigan, Ann Arbor, who did not participate in the study. “What I really love about this study is it’s actually a clinical problem that has large implications, particularly for under-resourced areas.”
Using a randomized clinical trial to evaluate the AI platform is “very, very novel,” he said, and called the time improvement “enormous.” Referencing Dr. Lin’s next steps for studying the AI-ECG platform, Dr. Nallamothu said, “if we could push this up even earlier to paramedics and EMTs and prehospital systems, there would be a lot of excitement there.”
He noted the sensitivity analysis resulted in a rate of 88.8% along with the positive predictive value of 88%. “Missing 1 out of 10 ST-elevation MIs in my eyes can still be considered a big deal, so we need to know if this is happening in particular types of patients, for example women versus men, or other groups.”
However, some investigations reported false activation rates as high as 33%, he said. “So, to say that, the positive predictive value is at 88% is really exciting and I think it can make a real inroads,” Dr. Nallamothu said.
Dr. Lin and Dr. Nallamothu have no relevant disclosures.
*Correction, 11/20/23: An earlier version of this article misstated in both trial arms the time to coronary catheterization lab activation.
PHILADELPHIA – An artificial intelligence platform that sends alerts based on electrocardiography results enabled cardiologists and emergency department physicians at a major hospital in Taiwan to move patients with ST-elevation myocardial infarction (STEMI) into the catheterization laboratory 9 minutes sooner than the conventional protocol that did not use AI.
“This is the first randomized clinical trial to demonstrate the reduction of electrocardiography to coronary cath lab activation time" from 52.3 to 43.3 minutes (P = .003), Chin Sheng Lin, MD, PhD, director of cardiology at the National Defense Medical Center Tri-Service General Hospital in Taipei City, said in presenting the results at the American Heart Association scientific sessions.
Dr. Lin reported results from the Artificial Intelligence Enabled Rapid Identify of ST-Elevation Myocardial Infarction Using Electrocardiogram (ARISE) trial. The trial included 43,994 patients who came to the hospital’s emergency and inpatient departments with at least one ECG but no history of coronary angiography (CAG) in the previous 3 days between May 2022 and April 2023.
They were randomly assigned by date to either AI-ECG for rapid identification and triage of STEMI or standard care. Overall, 145 patients were finally diagnosed with STEMI based on CAG, 77 in the intervention group and 68 in the control group. All patients were seen by one of 20 cardiologists who participated in the study.
Dr. Lin and his group developed an AI algorithm that captures the ECG readout in the emergency department, analyzes the data and then sends a high-risk alarm to the front-line physician and on-duty cardiologist to activate the primary percutaneous coronary intervention (PCI).
Trial results
The differentiation between groups was even more pronounced in ED patients during regular working hours, Dr. Lin said, at 61.6 minutes for the intervention group vs. 33.1 minutes for controls (P = .001).*
He noted that the AI group showed a trend towards fewer cases of clinically suspected STEMI but not getting CAG, 6.5% vs. 15.8%, for an odds ratio of 0.37 (95% confidence interval, 0.14-0.94).
The AI-ECG model also demonstrated a high diagnostic accuracy. “With this AI-ECG system, because it has a very high accuracy and a high positive predictive variable that reach 88%, we can send a message to the on-duty cardiologists and also the emergency room physician and they can send the patients to receive the operation or the PCI as soon as possible,” Dr. Lin said in an interview.
The time differential is critical, Dr. Lin said. “For the patient with acute myocardial infarction, 1 minute is critical, because the patients can die within minutes,” he said. “If we can save 9 minutes I think we can save more lives, but it needs a larger study to evaluate that.”
Dr. Lin acknowledged a few limitations with the trial, among them its single-center nature, relatively small sample size of STEMI patients and the short-term of follow-up. Future study should involve multiple centers along with a prehospital, emergency medical services AI-ECG model.
‘Novel’ for an AI trial
“This is an incredible application of an AI technology in a real-world problem,” said Brahmajee K. Nallamothu, MD, MPH, an interventional cardiologist at the University of Michigan, Ann Arbor, who did not participate in the study. “What I really love about this study is it’s actually a clinical problem that has large implications, particularly for under-resourced areas.”
Using a randomized clinical trial to evaluate the AI platform is “very, very novel,” he said, and called the time improvement “enormous.” Referencing Dr. Lin’s next steps for studying the AI-ECG platform, Dr. Nallamothu said, “if we could push this up even earlier to paramedics and EMTs and prehospital systems, there would be a lot of excitement there.”
He noted the sensitivity analysis resulted in a rate of 88.8% along with the positive predictive value of 88%. “Missing 1 out of 10 ST-elevation MIs in my eyes can still be considered a big deal, so we need to know if this is happening in particular types of patients, for example women versus men, or other groups.”
However, some investigations reported false activation rates as high as 33%, he said. “So, to say that, the positive predictive value is at 88% is really exciting and I think it can make a real inroads,” Dr. Nallamothu said.
Dr. Lin and Dr. Nallamothu have no relevant disclosures.
*Correction, 11/20/23: An earlier version of this article misstated in both trial arms the time to coronary catheterization lab activation.
PHILADELPHIA – An artificial intelligence platform that sends alerts based on electrocardiography results enabled cardiologists and emergency department physicians at a major hospital in Taiwan to move patients with ST-elevation myocardial infarction (STEMI) into the catheterization laboratory 9 minutes sooner than the conventional protocol that did not use AI.
“This is the first randomized clinical trial to demonstrate the reduction of electrocardiography to coronary cath lab activation time" from 52.3 to 43.3 minutes (P = .003), Chin Sheng Lin, MD, PhD, director of cardiology at the National Defense Medical Center Tri-Service General Hospital in Taipei City, said in presenting the results at the American Heart Association scientific sessions.
Dr. Lin reported results from the Artificial Intelligence Enabled Rapid Identify of ST-Elevation Myocardial Infarction Using Electrocardiogram (ARISE) trial. The trial included 43,994 patients who came to the hospital’s emergency and inpatient departments with at least one ECG but no history of coronary angiography (CAG) in the previous 3 days between May 2022 and April 2023.
They were randomly assigned by date to either AI-ECG for rapid identification and triage of STEMI or standard care. Overall, 145 patients were finally diagnosed with STEMI based on CAG, 77 in the intervention group and 68 in the control group. All patients were seen by one of 20 cardiologists who participated in the study.
Dr. Lin and his group developed an AI algorithm that captures the ECG readout in the emergency department, analyzes the data and then sends a high-risk alarm to the front-line physician and on-duty cardiologist to activate the primary percutaneous coronary intervention (PCI).
Trial results
The differentiation between groups was even more pronounced in ED patients during regular working hours, Dr. Lin said, at 61.6 minutes for the intervention group vs. 33.1 minutes for controls (P = .001).*
He noted that the AI group showed a trend towards fewer cases of clinically suspected STEMI but not getting CAG, 6.5% vs. 15.8%, for an odds ratio of 0.37 (95% confidence interval, 0.14-0.94).
The AI-ECG model also demonstrated a high diagnostic accuracy. “With this AI-ECG system, because it has a very high accuracy and a high positive predictive variable that reach 88%, we can send a message to the on-duty cardiologists and also the emergency room physician and they can send the patients to receive the operation or the PCI as soon as possible,” Dr. Lin said in an interview.
The time differential is critical, Dr. Lin said. “For the patient with acute myocardial infarction, 1 minute is critical, because the patients can die within minutes,” he said. “If we can save 9 minutes I think we can save more lives, but it needs a larger study to evaluate that.”
Dr. Lin acknowledged a few limitations with the trial, among them its single-center nature, relatively small sample size of STEMI patients and the short-term of follow-up. Future study should involve multiple centers along with a prehospital, emergency medical services AI-ECG model.
‘Novel’ for an AI trial
“This is an incredible application of an AI technology in a real-world problem,” said Brahmajee K. Nallamothu, MD, MPH, an interventional cardiologist at the University of Michigan, Ann Arbor, who did not participate in the study. “What I really love about this study is it’s actually a clinical problem that has large implications, particularly for under-resourced areas.”
Using a randomized clinical trial to evaluate the AI platform is “very, very novel,” he said, and called the time improvement “enormous.” Referencing Dr. Lin’s next steps for studying the AI-ECG platform, Dr. Nallamothu said, “if we could push this up even earlier to paramedics and EMTs and prehospital systems, there would be a lot of excitement there.”
He noted the sensitivity analysis resulted in a rate of 88.8% along with the positive predictive value of 88%. “Missing 1 out of 10 ST-elevation MIs in my eyes can still be considered a big deal, so we need to know if this is happening in particular types of patients, for example women versus men, or other groups.”
However, some investigations reported false activation rates as high as 33%, he said. “So, to say that, the positive predictive value is at 88% is really exciting and I think it can make a real inroads,” Dr. Nallamothu said.
Dr. Lin and Dr. Nallamothu have no relevant disclosures.
*Correction, 11/20/23: An earlier version of this article misstated in both trial arms the time to coronary catheterization lab activation.
AT AHA 2023
Novel PET tracer for perfusion imaging: What’s the potential?
The emerging advantages of PET myocardial perfusion imaging (MPI) for coronary artery disease (CAD) diagnosis and assessment of cardiovascular event risk has prompted growing use of this technology as an alternative to the more commonly used single photon–emission CT (SPECT) MPI.
The advantages of PET MPI include better diagnostic performance and shorter acquisition times. , including consistent, high-quality images and low radiation exposure. It also allows quantification of myocardial blood flow, and it has “strong prognostic power.”
Tracer availability
Despite these advantages, that position paper and subsequent studies note that PET MPI has been underutilized in the United States, largely owing to issues with the available tracers, which have characteristics that limit widespread use in the clinic.
Rubidium, arguably the most commonly used tracer for PET MPI, is not available in unit dosing and so can be expensive for low-volume centers, plus it also requires an on-site generator, Michael Salerno, MD, PhD, a member of the American College of Cardiology’s Imaging Council and section chief of cardiovascular imaging, Stanford (Calif.) University, told this news organization.
N-ammonia, the other U.S. Food and Drug Administration–approved tracer, is available in unit dosing, but its short half-life means that centers need an onsite cyclotron, Dr. Salerno said.
For cardiac perfusion imaging and myocardial blood flow (MBF) quantification, 15O-water is considered the gold standard, although it’s not approved by the FDA. This tracer also requires an on-site cyclotron and “is challenging to use,” Dr. Salerno said. Use has been largely restricted to research purposes, though efforts are underway to widen its availability.
Enter flurpiridaz F-18 (GE Healthcare), a novel PET MPI tracer labeled with fluorine-18. Its longer half-life – similar to that of fluorodeoxyglucose, a tracer used to detect various cancers – could broaden the number of sites that could perform perfusion PET studies, Dr. Salerno said.
“Flurpiridaz also is supposed to have a more linear relationship between flow and tracer uptake, which could improve the ability to perform quantification of perfusion,” he noted. “It also offers the ability to do exercise PET, which is impossible for rubidium and challenging for ammonia, given its 11-minute half-life.”
Flurpiridaz status
The FDA requires two phase-3 studies that show safety and sufficient diagnostic performance before it will approve a new tracer. The first required study, published in the Journal of the American College of Cardiology, showed that the tracer’s sensitivity for detection of greater than or equal to 50% stenosis by ICA was significantly higher than SPECT; however, the specificity did not meet the prespecified noninferiority criterion.
The second FDA-required study, published online recently, also in the Journal of the American College of Cardiology, was designed differently from the first in that only patients with suspected – not known – CAD were enrolled. The primary efficacy endpoint was sensitivity and specificity of flurpiridaz PET for overall detection of CAD, rather than comparing it to SPECT MPI (which became a secondary endpoint). PET and SPECT studies were both performed before invasive coronary angiography to minimize referral bias; SPECT studies included cadmium zinc telluride cameras.
In that study, which included 578 patients (mean age, 64; 32.5% women) from 48 centers in the United States, Canada, and Europe, flurpiridaz met the efficacy endpoints: Its sensitivity and specificity were significantly higher than the prespecified threshold value by two of the three readers; its sensitivity was higher than SPECT (80.3% vs. 68.7%); and its specificity was noninferior (63.8% vs. 61.7%).
PET areas under the receiver-operating characteristic curves were higher than SPECT in the overall population and in women and obese patients, at half the radiation dose of SPECT.
“Cardiac PET MPI is positioned to serve as the leading modality for the functional evaluation of suspected and known CAD,” Jamieson M. Bourque, MD, MHS, medical director of nuclear cardiology, echocardiography, and the Stress Laboratory, University of Virginia, Charlottesville, wrote in an editorial accompanying the second study . “18F-flurpiridaz will facilitate this upward progression with beneficial tracer characteristics that will increase access and availability, enable exercise stress, and optimize MBF quantification.”
At this point, FDA approval of flurpiridaz is expected sometime in 2024, said James E. Udelson, MD, principal investigator of the recent study, chief of the division of cardiology, and director of the Nuclear Cardiology Laboratory at Tufts University School of Medicine, Boston.
Learning curve
Flurpiridaz comes with “a really interesting and important” learning curve, Dr. Udelson said. “The images are really crisp, and they look very different from what most people are used to. The GE folks are going to have to make sure that the American Society of Nuclear Cardiology and other professional societies are tuned in to help in the education part, because it’s not an easy, automatic switch. Very good image readers can adapt, but it’s not just one day you do one, then switch to the other.”
A “somewhat apt” analogy would be the difference between an echocardiogram and an MRI, he explained. “The MRI is much crisper. You’re seeing edges more crisply. You’re seeing the difference between a thicker and a thinner segment of the wall more crisply, and that’s actually real. You can’t say the thinner segment is abnormal; it’s just that you’re seeing it better. So, with this tracer, normal differences in the thickness of a wall can almost look like a defect if you’re not used to knowing that’s the new normal.”
The expected approval of flurpiridaz “will be a win for cardiac PET, broadening the range of sites that could perform PET,” Dr. Salerno commented. “However, it is worth cautioning that all of the prior data with PET using different agents does not necessarily equate to the same performance with the new agent, given that the performance seems to be lower than that shown in prior PET studies using other agents.”
Dr. Salerno would like to see additional studies comparing flurpiridaz with rubidium or ammonia, as well as studies performing quantification with flurpiridaz, “which theoretically should have some advantages,” he said.
Dr. Udelson noted that MedTrace, a company in Denmark, is working on a radiolabeled water tracer based on 15-O-water that is just starting a pivotal trial. Dr. Udelson is a consultant to the company and is a steering committee member for the pivotal trial.
For now, “the big take-home is that there are a lot of ways these days to test people for CAD,” he said. “As the types of things we can do to test people expand, individuals and centers need to make sure they focus on providing any new service, however they do it, with really superb quality and experience.”
“You don’t just do something new because it’s new,” he added. “It has to be done really well. If you do the new thing badly, you’re not going to get better information.”
Dr. Udelson is a consultant and advisory board member for GE Healthcare, a consultant to MedTrace, and a steering committee member for MedTrace’s pivotal trial. Dr. Bourque has served on a GE Healthcare advisory board for amyloid imaging. Dr. Salerno reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The emerging advantages of PET myocardial perfusion imaging (MPI) for coronary artery disease (CAD) diagnosis and assessment of cardiovascular event risk has prompted growing use of this technology as an alternative to the more commonly used single photon–emission CT (SPECT) MPI.
The advantages of PET MPI include better diagnostic performance and shorter acquisition times. , including consistent, high-quality images and low radiation exposure. It also allows quantification of myocardial blood flow, and it has “strong prognostic power.”
Tracer availability
Despite these advantages, that position paper and subsequent studies note that PET MPI has been underutilized in the United States, largely owing to issues with the available tracers, which have characteristics that limit widespread use in the clinic.
Rubidium, arguably the most commonly used tracer for PET MPI, is not available in unit dosing and so can be expensive for low-volume centers, plus it also requires an on-site generator, Michael Salerno, MD, PhD, a member of the American College of Cardiology’s Imaging Council and section chief of cardiovascular imaging, Stanford (Calif.) University, told this news organization.
N-ammonia, the other U.S. Food and Drug Administration–approved tracer, is available in unit dosing, but its short half-life means that centers need an onsite cyclotron, Dr. Salerno said.
For cardiac perfusion imaging and myocardial blood flow (MBF) quantification, 15O-water is considered the gold standard, although it’s not approved by the FDA. This tracer also requires an on-site cyclotron and “is challenging to use,” Dr. Salerno said. Use has been largely restricted to research purposes, though efforts are underway to widen its availability.
Enter flurpiridaz F-18 (GE Healthcare), a novel PET MPI tracer labeled with fluorine-18. Its longer half-life – similar to that of fluorodeoxyglucose, a tracer used to detect various cancers – could broaden the number of sites that could perform perfusion PET studies, Dr. Salerno said.
“Flurpiridaz also is supposed to have a more linear relationship between flow and tracer uptake, which could improve the ability to perform quantification of perfusion,” he noted. “It also offers the ability to do exercise PET, which is impossible for rubidium and challenging for ammonia, given its 11-minute half-life.”
Flurpiridaz status
The FDA requires two phase-3 studies that show safety and sufficient diagnostic performance before it will approve a new tracer. The first required study, published in the Journal of the American College of Cardiology, showed that the tracer’s sensitivity for detection of greater than or equal to 50% stenosis by ICA was significantly higher than SPECT; however, the specificity did not meet the prespecified noninferiority criterion.
The second FDA-required study, published online recently, also in the Journal of the American College of Cardiology, was designed differently from the first in that only patients with suspected – not known – CAD were enrolled. The primary efficacy endpoint was sensitivity and specificity of flurpiridaz PET for overall detection of CAD, rather than comparing it to SPECT MPI (which became a secondary endpoint). PET and SPECT studies were both performed before invasive coronary angiography to minimize referral bias; SPECT studies included cadmium zinc telluride cameras.
In that study, which included 578 patients (mean age, 64; 32.5% women) from 48 centers in the United States, Canada, and Europe, flurpiridaz met the efficacy endpoints: Its sensitivity and specificity were significantly higher than the prespecified threshold value by two of the three readers; its sensitivity was higher than SPECT (80.3% vs. 68.7%); and its specificity was noninferior (63.8% vs. 61.7%).
PET areas under the receiver-operating characteristic curves were higher than SPECT in the overall population and in women and obese patients, at half the radiation dose of SPECT.
“Cardiac PET MPI is positioned to serve as the leading modality for the functional evaluation of suspected and known CAD,” Jamieson M. Bourque, MD, MHS, medical director of nuclear cardiology, echocardiography, and the Stress Laboratory, University of Virginia, Charlottesville, wrote in an editorial accompanying the second study . “18F-flurpiridaz will facilitate this upward progression with beneficial tracer characteristics that will increase access and availability, enable exercise stress, and optimize MBF quantification.”
At this point, FDA approval of flurpiridaz is expected sometime in 2024, said James E. Udelson, MD, principal investigator of the recent study, chief of the division of cardiology, and director of the Nuclear Cardiology Laboratory at Tufts University School of Medicine, Boston.
Learning curve
Flurpiridaz comes with “a really interesting and important” learning curve, Dr. Udelson said. “The images are really crisp, and they look very different from what most people are used to. The GE folks are going to have to make sure that the American Society of Nuclear Cardiology and other professional societies are tuned in to help in the education part, because it’s not an easy, automatic switch. Very good image readers can adapt, but it’s not just one day you do one, then switch to the other.”
A “somewhat apt” analogy would be the difference between an echocardiogram and an MRI, he explained. “The MRI is much crisper. You’re seeing edges more crisply. You’re seeing the difference between a thicker and a thinner segment of the wall more crisply, and that’s actually real. You can’t say the thinner segment is abnormal; it’s just that you’re seeing it better. So, with this tracer, normal differences in the thickness of a wall can almost look like a defect if you’re not used to knowing that’s the new normal.”
The expected approval of flurpiridaz “will be a win for cardiac PET, broadening the range of sites that could perform PET,” Dr. Salerno commented. “However, it is worth cautioning that all of the prior data with PET using different agents does not necessarily equate to the same performance with the new agent, given that the performance seems to be lower than that shown in prior PET studies using other agents.”
Dr. Salerno would like to see additional studies comparing flurpiridaz with rubidium or ammonia, as well as studies performing quantification with flurpiridaz, “which theoretically should have some advantages,” he said.
Dr. Udelson noted that MedTrace, a company in Denmark, is working on a radiolabeled water tracer based on 15-O-water that is just starting a pivotal trial. Dr. Udelson is a consultant to the company and is a steering committee member for the pivotal trial.
For now, “the big take-home is that there are a lot of ways these days to test people for CAD,” he said. “As the types of things we can do to test people expand, individuals and centers need to make sure they focus on providing any new service, however they do it, with really superb quality and experience.”
“You don’t just do something new because it’s new,” he added. “It has to be done really well. If you do the new thing badly, you’re not going to get better information.”
Dr. Udelson is a consultant and advisory board member for GE Healthcare, a consultant to MedTrace, and a steering committee member for MedTrace’s pivotal trial. Dr. Bourque has served on a GE Healthcare advisory board for amyloid imaging. Dr. Salerno reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The emerging advantages of PET myocardial perfusion imaging (MPI) for coronary artery disease (CAD) diagnosis and assessment of cardiovascular event risk has prompted growing use of this technology as an alternative to the more commonly used single photon–emission CT (SPECT) MPI.
The advantages of PET MPI include better diagnostic performance and shorter acquisition times. , including consistent, high-quality images and low radiation exposure. It also allows quantification of myocardial blood flow, and it has “strong prognostic power.”
Tracer availability
Despite these advantages, that position paper and subsequent studies note that PET MPI has been underutilized in the United States, largely owing to issues with the available tracers, which have characteristics that limit widespread use in the clinic.
Rubidium, arguably the most commonly used tracer for PET MPI, is not available in unit dosing and so can be expensive for low-volume centers, plus it also requires an on-site generator, Michael Salerno, MD, PhD, a member of the American College of Cardiology’s Imaging Council and section chief of cardiovascular imaging, Stanford (Calif.) University, told this news organization.
N-ammonia, the other U.S. Food and Drug Administration–approved tracer, is available in unit dosing, but its short half-life means that centers need an onsite cyclotron, Dr. Salerno said.
For cardiac perfusion imaging and myocardial blood flow (MBF) quantification, 15O-water is considered the gold standard, although it’s not approved by the FDA. This tracer also requires an on-site cyclotron and “is challenging to use,” Dr. Salerno said. Use has been largely restricted to research purposes, though efforts are underway to widen its availability.
Enter flurpiridaz F-18 (GE Healthcare), a novel PET MPI tracer labeled with fluorine-18. Its longer half-life – similar to that of fluorodeoxyglucose, a tracer used to detect various cancers – could broaden the number of sites that could perform perfusion PET studies, Dr. Salerno said.
“Flurpiridaz also is supposed to have a more linear relationship between flow and tracer uptake, which could improve the ability to perform quantification of perfusion,” he noted. “It also offers the ability to do exercise PET, which is impossible for rubidium and challenging for ammonia, given its 11-minute half-life.”
Flurpiridaz status
The FDA requires two phase-3 studies that show safety and sufficient diagnostic performance before it will approve a new tracer. The first required study, published in the Journal of the American College of Cardiology, showed that the tracer’s sensitivity for detection of greater than or equal to 50% stenosis by ICA was significantly higher than SPECT; however, the specificity did not meet the prespecified noninferiority criterion.
The second FDA-required study, published online recently, also in the Journal of the American College of Cardiology, was designed differently from the first in that only patients with suspected – not known – CAD were enrolled. The primary efficacy endpoint was sensitivity and specificity of flurpiridaz PET for overall detection of CAD, rather than comparing it to SPECT MPI (which became a secondary endpoint). PET and SPECT studies were both performed before invasive coronary angiography to minimize referral bias; SPECT studies included cadmium zinc telluride cameras.
In that study, which included 578 patients (mean age, 64; 32.5% women) from 48 centers in the United States, Canada, and Europe, flurpiridaz met the efficacy endpoints: Its sensitivity and specificity were significantly higher than the prespecified threshold value by two of the three readers; its sensitivity was higher than SPECT (80.3% vs. 68.7%); and its specificity was noninferior (63.8% vs. 61.7%).
PET areas under the receiver-operating characteristic curves were higher than SPECT in the overall population and in women and obese patients, at half the radiation dose of SPECT.
“Cardiac PET MPI is positioned to serve as the leading modality for the functional evaluation of suspected and known CAD,” Jamieson M. Bourque, MD, MHS, medical director of nuclear cardiology, echocardiography, and the Stress Laboratory, University of Virginia, Charlottesville, wrote in an editorial accompanying the second study . “18F-flurpiridaz will facilitate this upward progression with beneficial tracer characteristics that will increase access and availability, enable exercise stress, and optimize MBF quantification.”
At this point, FDA approval of flurpiridaz is expected sometime in 2024, said James E. Udelson, MD, principal investigator of the recent study, chief of the division of cardiology, and director of the Nuclear Cardiology Laboratory at Tufts University School of Medicine, Boston.
Learning curve
Flurpiridaz comes with “a really interesting and important” learning curve, Dr. Udelson said. “The images are really crisp, and they look very different from what most people are used to. The GE folks are going to have to make sure that the American Society of Nuclear Cardiology and other professional societies are tuned in to help in the education part, because it’s not an easy, automatic switch. Very good image readers can adapt, but it’s not just one day you do one, then switch to the other.”
A “somewhat apt” analogy would be the difference between an echocardiogram and an MRI, he explained. “The MRI is much crisper. You’re seeing edges more crisply. You’re seeing the difference between a thicker and a thinner segment of the wall more crisply, and that’s actually real. You can’t say the thinner segment is abnormal; it’s just that you’re seeing it better. So, with this tracer, normal differences in the thickness of a wall can almost look like a defect if you’re not used to knowing that’s the new normal.”
The expected approval of flurpiridaz “will be a win for cardiac PET, broadening the range of sites that could perform PET,” Dr. Salerno commented. “However, it is worth cautioning that all of the prior data with PET using different agents does not necessarily equate to the same performance with the new agent, given that the performance seems to be lower than that shown in prior PET studies using other agents.”
Dr. Salerno would like to see additional studies comparing flurpiridaz with rubidium or ammonia, as well as studies performing quantification with flurpiridaz, “which theoretically should have some advantages,” he said.
Dr. Udelson noted that MedTrace, a company in Denmark, is working on a radiolabeled water tracer based on 15-O-water that is just starting a pivotal trial. Dr. Udelson is a consultant to the company and is a steering committee member for the pivotal trial.
For now, “the big take-home is that there are a lot of ways these days to test people for CAD,” he said. “As the types of things we can do to test people expand, individuals and centers need to make sure they focus on providing any new service, however they do it, with really superb quality and experience.”
“You don’t just do something new because it’s new,” he added. “It has to be done really well. If you do the new thing badly, you’re not going to get better information.”
Dr. Udelson is a consultant and advisory board member for GE Healthcare, a consultant to MedTrace, and a steering committee member for MedTrace’s pivotal trial. Dr. Bourque has served on a GE Healthcare advisory board for amyloid imaging. Dr. Salerno reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PET scan at diagnosis may help to predict aneurysm risk in patients with giant cell arteritis
PET scans may serve as both a diagnostic and prognostic tool in giant cell arteritis (GCA), according to a new study.
In over 100 patients with GCA who underwent 18F-fluorodeoxyglucose PET imaging, those with elevated FDG uptake at diagnosis were more likely to develop thoracic aortic aneurysms.
“PET-CT has an excellent diagnostic accuracy for the diagnosis of GCA, certainly if both extracranial and intracranial vessels were assessed. This study shows that performing PET imaging at diagnosis in patients with GCA may also help estimate the future risk for aortic aneurysm formation,” lead author Lien Moreel, MD, of the department of internal medicine at University Hospitals Leuven (Belgium), wrote in an email. “PET imaging at diagnosis can provide both diagnostic and prognostic information in one imaging tool in patients with GCA.”
Previous retrospective studies have found an association between FDG uptake at diagnosis and risk for aortic complications, but “prospective studies confirming these findings are lacking,” the investigators wrote. The study was published online in Annals of Internal Medicine.
In the study, Dr. Moreel and colleagues prospectively followed 106 individuals diagnosed with GCA who received FDG-PET within 3 days after starting glucocorticoids. Patients also had CT imaging at diagnosis and then CT imaging annually for up to 10 years.
A PET scan was considered positive with an FDG uptake of grade 2 or higher in any of seven vascular regions (thoracic and abdominal aorta, subclavian, axillary, carotid, iliac, and femoral arteries). Researchers also used the results to quantify a total vascular score (TVS). Out of the entire cohort, 75 patients had a positive PET scan result.
These patients had a larger increase in the diameter of the ascending aorta and the descending aorta, as well the volume of thoracic aorta after 5 years, compared with those who had a negative PET scan result. These changes were also associated with higher TVS at diagnosis. Of the 23 patients who developed an aortic aneurysm, 18 had a positive PET scan at diagnosis.
The risk of incident thoracic aortic aneurysms was calculated to be 10 times higher in patients with positive PET scans. Fourteen of the 15 patients (93%) with an incident thoracic aortic aneurysm had positive PET results.
Up to now, “we’ve had no way of predicting which patients might be at risk of this potentially serious complication,” Kenneth Warrington, MD, chair of the department of rheumatology and director of the Vasculitis Clinic at the Mayo Clinic in Rochester, Minn., said in an interview. He was not involved with the research.
He hopes that the findings will help inform clinicians on how patients with GCA should be evaluated and monitored. Although the American College of Rheumatology conditionally recommends noninvasive imaging in patients newly diagnosed with GCA, guidance for follow-up on these patients is less clear.
“There are no clear guidelines, but most clinicians who take care of patients with GCA do obtain imaging periodically,” he said. “There is a lot of variability in the practice in terms of which type of scan is used and how often it’s done.”
Although this study did not specifically look at the benefit of screening patients, “we think that follow-up of aortic dimensions seems to be warranted in GCA patients with a positive PET scan result, especially in those with high intensity and broad extent of vascular inflammation,” Dr. Moreel said. “However, the added value of screening and the interval required should be addressed in future studies.”
Applying this study’s protocol in practice in the United States might be difficult, Dr. Warrington noted, as it can be challenging logistically to get imaging done within 3 days of starting steroids. However, Dr. Moreel said it is possible to delay the start of glucocorticoids until the PET scan is performed in patients without visual symptoms or jaw claudication.
PET scans are also expensive, and it can be difficult to get insurance coverage in the United States. However, other imaging modalities could potentially be used in similar ways, Dr. Warrington said. “One could potentially extrapolate to say that if there is difficulty with accessing PET scan, we could use other modalities like CT or MRI basically to see whether the aorta is inflamed or not.”
Dr. Moreel disclosed no relevant financial relationships. Dr. Warrington has received compensation for consulting activities with Sanofi. Eli Lilly, Kiniksa, and Bristol-Myers Squibb have provided support to the Mayo Clinic for clinical trials related to GCA, of which Dr. Warrington served as subinvestigator.
A version of this article appeared on Medscape.com.
PET scans may serve as both a diagnostic and prognostic tool in giant cell arteritis (GCA), according to a new study.
In over 100 patients with GCA who underwent 18F-fluorodeoxyglucose PET imaging, those with elevated FDG uptake at diagnosis were more likely to develop thoracic aortic aneurysms.
“PET-CT has an excellent diagnostic accuracy for the diagnosis of GCA, certainly if both extracranial and intracranial vessels were assessed. This study shows that performing PET imaging at diagnosis in patients with GCA may also help estimate the future risk for aortic aneurysm formation,” lead author Lien Moreel, MD, of the department of internal medicine at University Hospitals Leuven (Belgium), wrote in an email. “PET imaging at diagnosis can provide both diagnostic and prognostic information in one imaging tool in patients with GCA.”
Previous retrospective studies have found an association between FDG uptake at diagnosis and risk for aortic complications, but “prospective studies confirming these findings are lacking,” the investigators wrote. The study was published online in Annals of Internal Medicine.
In the study, Dr. Moreel and colleagues prospectively followed 106 individuals diagnosed with GCA who received FDG-PET within 3 days after starting glucocorticoids. Patients also had CT imaging at diagnosis and then CT imaging annually for up to 10 years.
A PET scan was considered positive with an FDG uptake of grade 2 or higher in any of seven vascular regions (thoracic and abdominal aorta, subclavian, axillary, carotid, iliac, and femoral arteries). Researchers also used the results to quantify a total vascular score (TVS). Out of the entire cohort, 75 patients had a positive PET scan result.
These patients had a larger increase in the diameter of the ascending aorta and the descending aorta, as well the volume of thoracic aorta after 5 years, compared with those who had a negative PET scan result. These changes were also associated with higher TVS at diagnosis. Of the 23 patients who developed an aortic aneurysm, 18 had a positive PET scan at diagnosis.
The risk of incident thoracic aortic aneurysms was calculated to be 10 times higher in patients with positive PET scans. Fourteen of the 15 patients (93%) with an incident thoracic aortic aneurysm had positive PET results.
Up to now, “we’ve had no way of predicting which patients might be at risk of this potentially serious complication,” Kenneth Warrington, MD, chair of the department of rheumatology and director of the Vasculitis Clinic at the Mayo Clinic in Rochester, Minn., said in an interview. He was not involved with the research.
He hopes that the findings will help inform clinicians on how patients with GCA should be evaluated and monitored. Although the American College of Rheumatology conditionally recommends noninvasive imaging in patients newly diagnosed with GCA, guidance for follow-up on these patients is less clear.
“There are no clear guidelines, but most clinicians who take care of patients with GCA do obtain imaging periodically,” he said. “There is a lot of variability in the practice in terms of which type of scan is used and how often it’s done.”
Although this study did not specifically look at the benefit of screening patients, “we think that follow-up of aortic dimensions seems to be warranted in GCA patients with a positive PET scan result, especially in those with high intensity and broad extent of vascular inflammation,” Dr. Moreel said. “However, the added value of screening and the interval required should be addressed in future studies.”
Applying this study’s protocol in practice in the United States might be difficult, Dr. Warrington noted, as it can be challenging logistically to get imaging done within 3 days of starting steroids. However, Dr. Moreel said it is possible to delay the start of glucocorticoids until the PET scan is performed in patients without visual symptoms or jaw claudication.
PET scans are also expensive, and it can be difficult to get insurance coverage in the United States. However, other imaging modalities could potentially be used in similar ways, Dr. Warrington said. “One could potentially extrapolate to say that if there is difficulty with accessing PET scan, we could use other modalities like CT or MRI basically to see whether the aorta is inflamed or not.”
Dr. Moreel disclosed no relevant financial relationships. Dr. Warrington has received compensation for consulting activities with Sanofi. Eli Lilly, Kiniksa, and Bristol-Myers Squibb have provided support to the Mayo Clinic for clinical trials related to GCA, of which Dr. Warrington served as subinvestigator.
A version of this article appeared on Medscape.com.
PET scans may serve as both a diagnostic and prognostic tool in giant cell arteritis (GCA), according to a new study.
In over 100 patients with GCA who underwent 18F-fluorodeoxyglucose PET imaging, those with elevated FDG uptake at diagnosis were more likely to develop thoracic aortic aneurysms.
“PET-CT has an excellent diagnostic accuracy for the diagnosis of GCA, certainly if both extracranial and intracranial vessels were assessed. This study shows that performing PET imaging at diagnosis in patients with GCA may also help estimate the future risk for aortic aneurysm formation,” lead author Lien Moreel, MD, of the department of internal medicine at University Hospitals Leuven (Belgium), wrote in an email. “PET imaging at diagnosis can provide both diagnostic and prognostic information in one imaging tool in patients with GCA.”
Previous retrospective studies have found an association between FDG uptake at diagnosis and risk for aortic complications, but “prospective studies confirming these findings are lacking,” the investigators wrote. The study was published online in Annals of Internal Medicine.
In the study, Dr. Moreel and colleagues prospectively followed 106 individuals diagnosed with GCA who received FDG-PET within 3 days after starting glucocorticoids. Patients also had CT imaging at diagnosis and then CT imaging annually for up to 10 years.
A PET scan was considered positive with an FDG uptake of grade 2 or higher in any of seven vascular regions (thoracic and abdominal aorta, subclavian, axillary, carotid, iliac, and femoral arteries). Researchers also used the results to quantify a total vascular score (TVS). Out of the entire cohort, 75 patients had a positive PET scan result.
These patients had a larger increase in the diameter of the ascending aorta and the descending aorta, as well the volume of thoracic aorta after 5 years, compared with those who had a negative PET scan result. These changes were also associated with higher TVS at diagnosis. Of the 23 patients who developed an aortic aneurysm, 18 had a positive PET scan at diagnosis.
The risk of incident thoracic aortic aneurysms was calculated to be 10 times higher in patients with positive PET scans. Fourteen of the 15 patients (93%) with an incident thoracic aortic aneurysm had positive PET results.
Up to now, “we’ve had no way of predicting which patients might be at risk of this potentially serious complication,” Kenneth Warrington, MD, chair of the department of rheumatology and director of the Vasculitis Clinic at the Mayo Clinic in Rochester, Minn., said in an interview. He was not involved with the research.
He hopes that the findings will help inform clinicians on how patients with GCA should be evaluated and monitored. Although the American College of Rheumatology conditionally recommends noninvasive imaging in patients newly diagnosed with GCA, guidance for follow-up on these patients is less clear.
“There are no clear guidelines, but most clinicians who take care of patients with GCA do obtain imaging periodically,” he said. “There is a lot of variability in the practice in terms of which type of scan is used and how often it’s done.”
Although this study did not specifically look at the benefit of screening patients, “we think that follow-up of aortic dimensions seems to be warranted in GCA patients with a positive PET scan result, especially in those with high intensity and broad extent of vascular inflammation,” Dr. Moreel said. “However, the added value of screening and the interval required should be addressed in future studies.”
Applying this study’s protocol in practice in the United States might be difficult, Dr. Warrington noted, as it can be challenging logistically to get imaging done within 3 days of starting steroids. However, Dr. Moreel said it is possible to delay the start of glucocorticoids until the PET scan is performed in patients without visual symptoms or jaw claudication.
PET scans are also expensive, and it can be difficult to get insurance coverage in the United States. However, other imaging modalities could potentially be used in similar ways, Dr. Warrington said. “One could potentially extrapolate to say that if there is difficulty with accessing PET scan, we could use other modalities like CT or MRI basically to see whether the aorta is inflamed or not.”
Dr. Moreel disclosed no relevant financial relationships. Dr. Warrington has received compensation for consulting activities with Sanofi. Eli Lilly, Kiniksa, and Bristol-Myers Squibb have provided support to the Mayo Clinic for clinical trials related to GCA, of which Dr. Warrington served as subinvestigator.
A version of this article appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Diagnosing pediatric forearm fractures: Radiograph or ultrasound?
TOPLINE:
as well as their waiting time in ED.
METHODOLOGY:
- After the World Health Organization reported a lack of access to any diagnostic imaging in approximately two-thirds of the world population in 2010, ultrasonography has gained popularity in low- and middle-income countries.
- The initial use of ultrasonography is in accordance with the principle of maintaining radiation levels as low as reasonably achievable.
- The BUCKLED trial was conducted, including 270 pediatric patients (age, 5-15 years) who presented to the ED with isolated, acute, clinically nondeformed distal forearm fractures.
- The participants were randomly assigned to receive initial point-of-care ultrasonography (n = 135) or radiography (n = 135) in the ED.
- The primary outcome was the physical function of the affected arm at 4 weeks evaluated using the Pediatric Upper Extremity Short Patient-Reported Outcomes Measurement Information System (PROMIS) tool.
TAKEAWAY:
- At 4 weeks, mean PROMIS scores were 36.4 and 36.3 points in ultrasonography and radiography groups, respectively (mean difference, 0.1 point; 95% confidence interval, − 1.3 to 1.4), indicating noninferiority of ultrasonography over radiography.
- Ultrasonography and radiography groups showed similar efficacy in terms of PROMIS scores at 1 week (MD, 0.7 points; 95% CI, − 1.4 to 2.8) and 8 weeks (MD, 0.1 points; 95% CI, − 0.5 to 0.7).
- Participants in the ultrasonography group had a shorter length of stay in the ED (median difference, 15 minutes; 95% CI, 1-29) and a shorter treatment time (median difference, 28 minutes; 95% CI, 17-40) than those in the radiography group.
- No important fractures were missed with ultrasonography, and no significant difference was observed in the frequency of adverse events or unplanned returns to the ED between the two groups.
IN PRACTICE:
Noting the benefit-risk profile of an ultrasound-first approach in an ED setting, the lead author, Peter J. Snelling, MB, BS, MPH&TM, from Menzies Health Institute Queensland, Gold Coast, Australia, said: “It is highly unlikely that any important fractures would be missed using the protocol that we trained clinicians. The risk is low and the benefit is moderate, such as reducing length of stay and increased level of patient satisfaction.”
He further added that, “with an ultrasound-first approach, clinicians can scan the patient at time of review and may even be able to discharge them immediately (two-thirds of instances in our NEJM trial). This places the patient at the center of care being provided.”
SOURCE:
Authors from the BUCKLED Trial Group published their study in the New England Journal of Medicine.
LIMITATIONS:
PROMIS scores may have been affected by variations in subsequent therapeutic interventions rather than the initial diagnostic method. PROMIS tool was not validated in children younger than 5 years of age.
DISCLOSURES:
The study was funded by the Emergency Medicine Foundation and others. The authors have declared no relevant interests to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
as well as their waiting time in ED.
METHODOLOGY:
- After the World Health Organization reported a lack of access to any diagnostic imaging in approximately two-thirds of the world population in 2010, ultrasonography has gained popularity in low- and middle-income countries.
- The initial use of ultrasonography is in accordance with the principle of maintaining radiation levels as low as reasonably achievable.
- The BUCKLED trial was conducted, including 270 pediatric patients (age, 5-15 years) who presented to the ED with isolated, acute, clinically nondeformed distal forearm fractures.
- The participants were randomly assigned to receive initial point-of-care ultrasonography (n = 135) or radiography (n = 135) in the ED.
- The primary outcome was the physical function of the affected arm at 4 weeks evaluated using the Pediatric Upper Extremity Short Patient-Reported Outcomes Measurement Information System (PROMIS) tool.
TAKEAWAY:
- At 4 weeks, mean PROMIS scores were 36.4 and 36.3 points in ultrasonography and radiography groups, respectively (mean difference, 0.1 point; 95% confidence interval, − 1.3 to 1.4), indicating noninferiority of ultrasonography over radiography.
- Ultrasonography and radiography groups showed similar efficacy in terms of PROMIS scores at 1 week (MD, 0.7 points; 95% CI, − 1.4 to 2.8) and 8 weeks (MD, 0.1 points; 95% CI, − 0.5 to 0.7).
- Participants in the ultrasonography group had a shorter length of stay in the ED (median difference, 15 minutes; 95% CI, 1-29) and a shorter treatment time (median difference, 28 minutes; 95% CI, 17-40) than those in the radiography group.
- No important fractures were missed with ultrasonography, and no significant difference was observed in the frequency of adverse events or unplanned returns to the ED between the two groups.
IN PRACTICE:
Noting the benefit-risk profile of an ultrasound-first approach in an ED setting, the lead author, Peter J. Snelling, MB, BS, MPH&TM, from Menzies Health Institute Queensland, Gold Coast, Australia, said: “It is highly unlikely that any important fractures would be missed using the protocol that we trained clinicians. The risk is low and the benefit is moderate, such as reducing length of stay and increased level of patient satisfaction.”
He further added that, “with an ultrasound-first approach, clinicians can scan the patient at time of review and may even be able to discharge them immediately (two-thirds of instances in our NEJM trial). This places the patient at the center of care being provided.”
SOURCE:
Authors from the BUCKLED Trial Group published their study in the New England Journal of Medicine.
LIMITATIONS:
PROMIS scores may have been affected by variations in subsequent therapeutic interventions rather than the initial diagnostic method. PROMIS tool was not validated in children younger than 5 years of age.
DISCLOSURES:
The study was funded by the Emergency Medicine Foundation and others. The authors have declared no relevant interests to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
as well as their waiting time in ED.
METHODOLOGY:
- After the World Health Organization reported a lack of access to any diagnostic imaging in approximately two-thirds of the world population in 2010, ultrasonography has gained popularity in low- and middle-income countries.
- The initial use of ultrasonography is in accordance with the principle of maintaining radiation levels as low as reasonably achievable.
- The BUCKLED trial was conducted, including 270 pediatric patients (age, 5-15 years) who presented to the ED with isolated, acute, clinically nondeformed distal forearm fractures.
- The participants were randomly assigned to receive initial point-of-care ultrasonography (n = 135) or radiography (n = 135) in the ED.
- The primary outcome was the physical function of the affected arm at 4 weeks evaluated using the Pediatric Upper Extremity Short Patient-Reported Outcomes Measurement Information System (PROMIS) tool.
TAKEAWAY:
- At 4 weeks, mean PROMIS scores were 36.4 and 36.3 points in ultrasonography and radiography groups, respectively (mean difference, 0.1 point; 95% confidence interval, − 1.3 to 1.4), indicating noninferiority of ultrasonography over radiography.
- Ultrasonography and radiography groups showed similar efficacy in terms of PROMIS scores at 1 week (MD, 0.7 points; 95% CI, − 1.4 to 2.8) and 8 weeks (MD, 0.1 points; 95% CI, − 0.5 to 0.7).
- Participants in the ultrasonography group had a shorter length of stay in the ED (median difference, 15 minutes; 95% CI, 1-29) and a shorter treatment time (median difference, 28 minutes; 95% CI, 17-40) than those in the radiography group.
- No important fractures were missed with ultrasonography, and no significant difference was observed in the frequency of adverse events or unplanned returns to the ED between the two groups.
IN PRACTICE:
Noting the benefit-risk profile of an ultrasound-first approach in an ED setting, the lead author, Peter J. Snelling, MB, BS, MPH&TM, from Menzies Health Institute Queensland, Gold Coast, Australia, said: “It is highly unlikely that any important fractures would be missed using the protocol that we trained clinicians. The risk is low and the benefit is moderate, such as reducing length of stay and increased level of patient satisfaction.”
He further added that, “with an ultrasound-first approach, clinicians can scan the patient at time of review and may even be able to discharge them immediately (two-thirds of instances in our NEJM trial). This places the patient at the center of care being provided.”
SOURCE:
Authors from the BUCKLED Trial Group published their study in the New England Journal of Medicine.
LIMITATIONS:
PROMIS scores may have been affected by variations in subsequent therapeutic interventions rather than the initial diagnostic method. PROMIS tool was not validated in children younger than 5 years of age.
DISCLOSURES:
The study was funded by the Emergency Medicine Foundation and others. The authors have declared no relevant interests to disclose.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Should intravascular imaging be almost routine in PCI?
A routine role for intravascular imaging (IVI) guidance for percutaneous coronary intervention (PCI) has long been favored by many of the technology’s researchers and enthusiasts. Now evidence from large, randomized trials may be catching up with such aspirations, though not without caveats.
One way IVI guidance may achieve that, the research suggests, albeit more speculatively, is by cutting risk for stent thrombosis, compared with the risk associated with angiography-only PCI.
The new studies, two large randomized IVI trials plus a meta-analysis of 20 such studies, were presented at the annual congress of the European Society of Cardiology.
In one, called ILUMIEN-4, PCI guided by optical coherence tomography (OCT) was associated with fewer procedural complications and better acute results – that is, larger post-PCI minimum stent area (MSA) – than in angiography-only procedures (P < .001). Poststenting MSA, an established predictor of clinical outcomes, was the primary imaging endpoint of the trial with almost 2,500 patients.
Yet the OCT group’s greater post-PCI MSA did not translate to reduced risk for the primary clinical endpoint of 2-year target-vessel failure. Among secondary endpoints, however, stent thrombosis at some point during the follow-up was 64% less likely (P = .02) with OCT guidance than angiography-only PCI.
ILUMIEN-4, despite its neutral clinical result, still “strongly advocates” for PCI guidance by OCT, at least among patients like those in the trial, said principal investigator Ziad Ali, MD, DPhil. He based that largely on the strategy’s greater postprocedure lumen areas in the trials, which are among “the strongest independent predictors for long term outcomes,” said Dr. Ali, of St. Francis Hospital & Heart Center, Roslyn, N.Y., at a press conference on IVI trials during the ESC Congress.
Selected complex lesion type
In contrast, the OCTOBER trial, presented at the sessions back to back with ILUMIEN-4, saw OCT guidance lead to better clinical outcomes than angiography alone after PCI of bifurcation lesions, which normally can be a special challenge for operators.
In the trial, which entered about 1,200 patients with such complex lesions, the 2-year risk for major adverse cardiac events (MACE) fell 60% after OCT-guided PCI, compared with angiography-only procedures (P = .035).
The finding is novel for showing that OCT guidance in bifurcation PCI can make a significant clinical difference, said OCTOBER investigator Niels R. Holm, MD, at the same media presentation on IVI trials.
“Multiple studies have shown that OCT allows for optimization of bifurcation PCI, and our results confirm that such optimization may improve the patient’s prognosis,” said Dr. Holm of Aarhus (Denmark) University Hospital.
ILUMIEN-4 and OCTOBER, both of which prespecified the Xience (Abbott) everolimus-eluting stent for the procedures, were published in the New England Journal of Medicine in tandem with their respective presentations at the ESC sessions.
Covering the spectrum
A meta-analysis presented at the same ESC session compared IVI using either OCT or intravascular ultrasound (IVUS) with angiography-only PCI across 20 randomized trials with a total of more than 12,000 patients.
Significant outcomes for IVI guidance versus angiography alone included a 31% drop in risk for target-lesion failure, the primary endpoint. And this study, as well, showed a steep 52% reduction in risk for in-stent thrombosis with the IVI-guided approach.
And “for the first time” in IVI studies, “we demonstrated reductions in all-myocardial-infarction and all-cause death, the latter by 25%,” Gregg Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said in presenting the meta-analysis. Dr. Stone is also the ILUMIEN-4 study chairperson.
“The routine use of OCT or IVUS to guide most PCI procedures will substantially improve patient event-free survival,” he predicted, “enhancing both the long-term safety and effectiveness of the procedure.”
Dr. Stone said that IVI guidance “should be standard of care, if not in all patients, then in most patients.” Part of the rationale: PCI is unlikely to be improved much further by incremental gains in drug-eluting stent design. “That technology has almost plateaued.” But there’s yet room for “substantially improved outcomes” from adjunctive treatments and techniques such as IVI guidance.
The 20 studies in the meta-analysis encompassed an array of patients and lesions both complex and noncomplex, Dr. Stone observed, including bifurcation lesions, chronic total occlusions, left-main coronary stenoses, and MI culprit lesions.
“They really covered the spectrum of PCI,” he said. “I’m not recommending that intravascular imaging be used in every single case. But I do think it should be used in the majority of patients” and be standard of care for PCI in left-main lesions and “complex coronary disease, high-risk patients, and high-risk lesions.”
Unique advantage
The IVI-guidance groups in both ILUMIEN-4 and the meta-analysis showed a significant drop in risk for stent thrombosis – that is, abrupt thrombotic vessel closure, which typically occurs in 1% or fewer PCI cases but can trigger an MI and pose a mortality risk up to 45%.
Those risk reductions are consistent with a unique IVI advantage: the ability to guide optimization of stent deployments. When formally presenting ILUMIEN-4 at the ESC sessions, Ali observed that IVUS and OCT imaging allows operators to identify and often correct less-than-ideal results of an initial stent delivery – such as residual gaps between stent struts and vessel wall – that may encroach on the lumen, with possible clinical consequences.
Such imaging, said Dr. Ali, “lets you identify tissue protrusions, malappositions, dissections, and untreated reference-segment disease” that may potentially trigger thrombosis. That makes a strong argument for giving IVI guidance a more common, perhaps even routine role in PCI procedures.
Selling routine IVI-guided PCI in practice
“I think the study results are quite clear,” said Deepak L. Bhatt, MD, MPH, as session comoderator following the OCTOBER presentation. “The challenge, though, will be convincing the average interventional cardiologist worldwide that it was specifically the imaging and not the extra care that the patient getting OCT also inherently receives.”
Did OCT’s better trial outcomes stem from IVI itself or from greater operator attentiveness to procedural results – such as, for example, more high-pressure expansions to optimize stent placement, “the sort of thing that tends to occur when invasive imaging is added on to just plain old angiography?” Dr. Bhatt asked of Lene N. Andreasen, MD, who had just presented the OCTOBER trial. “There’s no way of uncoupling the two things.”
What can be said, “at this point, to convince interventional cardiologists that the extra time, energy, expense, is truly indicated,” that the data are “sufficient to change global practice?” asked Dr. Bhatt, Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai.
That remains an open question,” acknowledged Dr. Andreasen of Aarhus University Hospital. The best argument in favor of selective IVI-guided PCI is that “we actually see a clinical benefit” in the trials. “But of course, it comes with a cost. It comes with longer procedures and more contrast.” How clinical practice responds to the new data remains to be seen, she proposed.
ILUMIEN-4 and OCTOBER in detail
Conducted at 80 centers in 18 countries, ILUMIEN-4 randomly assigned patients with diabetes or complex coronary lesions to undergo PCI guided by OCT or using standard angiography only, 1,233 and 1,254 patients, respectively.
Post-PCI MSA averaged 5.72 mm2 with OCT guidance and 5.36 mm2 in the angiography-only group (P < .001).
Their rates of target-vessel failure at 2 years were not significantly different at 7.4% and 8.2%, respectively. The 2-year composite endpoint included cardiac death, target vessel–related MI, or ischemia-driven target-vessel revascularization.
Definite or probable stent thrombosis was observed over 2 years in 0.5% of the OCT group and 1.4% of those with angiography-only PCI (hazard ratio, 0.36; 95% confidence interval, 0.14-0.91; P = .02) favoring OCT.
The OCTOBER trial, conducted at 38 centers in Europe, entered 1201 patients with stable angina or acute coronary syndromes and angiographically identified complex bifurcation lesions. They involved the left-main coronary artery in about one-fifth of cases.
Patients were randomly assigned to bifurcation PCI guided by OCT or under standard angiography, 600 and 601 patients, respectively. Rates for procedure-related complications were similar at 6.8% and 5.7%, respectively.
Over a median of 2 years, 10.1% of the OCT group and 14.1% of angiography-only patients developed a MACE event, including cardiac death, target-lesion MI, or ischemia-driven target-lesion revascularization. The adjusted HR was 0.71 (95% CI, 0.51-0.98; P = .035) in favor of OCT.
Meta-analysis, trials to date
The meta-analysis presented by Dr. Stone included ILUMIEN-4, OCTOBER, and 18 earlier outcomes trials comparing PCI guided by IVI, either OCT or IVUS, and angiography-only PCI. It covered 12,428 patients with chronic or acute coronary disease and followed them a mean of 26 months; the longest follow-up was 5 years. They were assigned to IVI-guided or angiography-only PCI, 7,038 and 5,390 patients, respectively.
Dr. Stone and colleagues conducted a network meta-analysis of the 20 studies, that is, a combined analysis that allowed both direct and indirect comparisons of standard angiography-only procedures to each of the other studied comparator interventions including OCT, IVUS, and either OCT or IVUS. They then derived network-estimate odds ratios for IVI-guided PCI vs angiography-only procedures.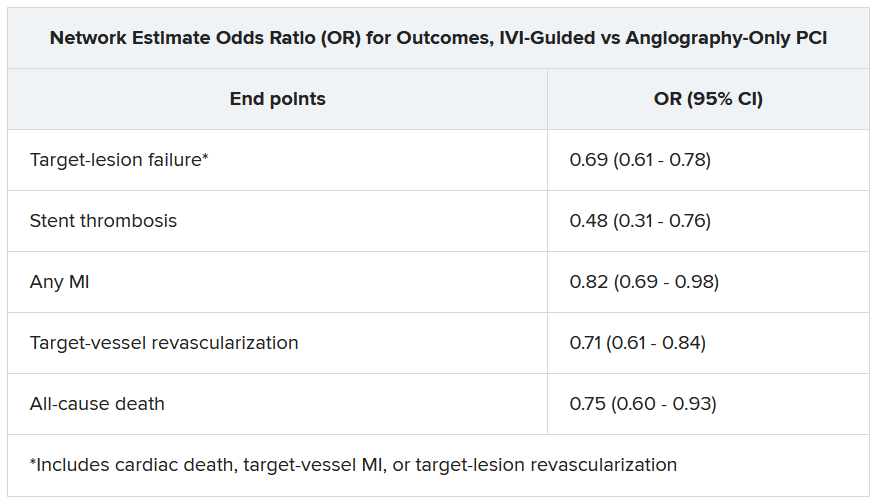
“Hopefully, this will impact the guidelines,” Dr. Stone said of the meta-analysis. Procedures guided by IVI might become more common in clinical practice if they were to garner a Class-I guideline recommendation, the strongest recommendation category.
“That would make a difference, but we’d also need to work to remove impediments to increasing intravascular imaging guidance” for most patients undergoing PCI, he said, referring to challenges in obtaining reimbursement for IVI-guided PCI and training enough operators to handle the projected demand.
ILUMIEN-4 was funded by Abbott. OCTOBER was supported by grants from Abbott Vascular, St. Jude Medical, and Aarhus University. The network meta-analysis received statistical support from Abbott. Dr. Ali disclosed institutional grant support from Abbott, Abiomed, Acist Medical, Boston Scientific, Cardiovascular Systems, Medtronic, the National Institutes of Health, Opsens Medical, Philips, and Teleflex; consulting fees from Astra Zeneca, Philips, Shockwave; and holding equity in Elucid, Spectrawave, Shockwave, and VitalConnect. Dr. Holm and Dr. Bhatt reported numerous conflicts of interest. Dr. Andreasen disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A routine role for intravascular imaging (IVI) guidance for percutaneous coronary intervention (PCI) has long been favored by many of the technology’s researchers and enthusiasts. Now evidence from large, randomized trials may be catching up with such aspirations, though not without caveats.
One way IVI guidance may achieve that, the research suggests, albeit more speculatively, is by cutting risk for stent thrombosis, compared with the risk associated with angiography-only PCI.
The new studies, two large randomized IVI trials plus a meta-analysis of 20 such studies, were presented at the annual congress of the European Society of Cardiology.
In one, called ILUMIEN-4, PCI guided by optical coherence tomography (OCT) was associated with fewer procedural complications and better acute results – that is, larger post-PCI minimum stent area (MSA) – than in angiography-only procedures (P < .001). Poststenting MSA, an established predictor of clinical outcomes, was the primary imaging endpoint of the trial with almost 2,500 patients.
Yet the OCT group’s greater post-PCI MSA did not translate to reduced risk for the primary clinical endpoint of 2-year target-vessel failure. Among secondary endpoints, however, stent thrombosis at some point during the follow-up was 64% less likely (P = .02) with OCT guidance than angiography-only PCI.
ILUMIEN-4, despite its neutral clinical result, still “strongly advocates” for PCI guidance by OCT, at least among patients like those in the trial, said principal investigator Ziad Ali, MD, DPhil. He based that largely on the strategy’s greater postprocedure lumen areas in the trials, which are among “the strongest independent predictors for long term outcomes,” said Dr. Ali, of St. Francis Hospital & Heart Center, Roslyn, N.Y., at a press conference on IVI trials during the ESC Congress.
Selected complex lesion type
In contrast, the OCTOBER trial, presented at the sessions back to back with ILUMIEN-4, saw OCT guidance lead to better clinical outcomes than angiography alone after PCI of bifurcation lesions, which normally can be a special challenge for operators.
In the trial, which entered about 1,200 patients with such complex lesions, the 2-year risk for major adverse cardiac events (MACE) fell 60% after OCT-guided PCI, compared with angiography-only procedures (P = .035).
The finding is novel for showing that OCT guidance in bifurcation PCI can make a significant clinical difference, said OCTOBER investigator Niels R. Holm, MD, at the same media presentation on IVI trials.
“Multiple studies have shown that OCT allows for optimization of bifurcation PCI, and our results confirm that such optimization may improve the patient’s prognosis,” said Dr. Holm of Aarhus (Denmark) University Hospital.
ILUMIEN-4 and OCTOBER, both of which prespecified the Xience (Abbott) everolimus-eluting stent for the procedures, were published in the New England Journal of Medicine in tandem with their respective presentations at the ESC sessions.
Covering the spectrum
A meta-analysis presented at the same ESC session compared IVI using either OCT or intravascular ultrasound (IVUS) with angiography-only PCI across 20 randomized trials with a total of more than 12,000 patients.
Significant outcomes for IVI guidance versus angiography alone included a 31% drop in risk for target-lesion failure, the primary endpoint. And this study, as well, showed a steep 52% reduction in risk for in-stent thrombosis with the IVI-guided approach.
And “for the first time” in IVI studies, “we demonstrated reductions in all-myocardial-infarction and all-cause death, the latter by 25%,” Gregg Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said in presenting the meta-analysis. Dr. Stone is also the ILUMIEN-4 study chairperson.
“The routine use of OCT or IVUS to guide most PCI procedures will substantially improve patient event-free survival,” he predicted, “enhancing both the long-term safety and effectiveness of the procedure.”
Dr. Stone said that IVI guidance “should be standard of care, if not in all patients, then in most patients.” Part of the rationale: PCI is unlikely to be improved much further by incremental gains in drug-eluting stent design. “That technology has almost plateaued.” But there’s yet room for “substantially improved outcomes” from adjunctive treatments and techniques such as IVI guidance.
The 20 studies in the meta-analysis encompassed an array of patients and lesions both complex and noncomplex, Dr. Stone observed, including bifurcation lesions, chronic total occlusions, left-main coronary stenoses, and MI culprit lesions.
“They really covered the spectrum of PCI,” he said. “I’m not recommending that intravascular imaging be used in every single case. But I do think it should be used in the majority of patients” and be standard of care for PCI in left-main lesions and “complex coronary disease, high-risk patients, and high-risk lesions.”
Unique advantage
The IVI-guidance groups in both ILUMIEN-4 and the meta-analysis showed a significant drop in risk for stent thrombosis – that is, abrupt thrombotic vessel closure, which typically occurs in 1% or fewer PCI cases but can trigger an MI and pose a mortality risk up to 45%.
Those risk reductions are consistent with a unique IVI advantage: the ability to guide optimization of stent deployments. When formally presenting ILUMIEN-4 at the ESC sessions, Ali observed that IVUS and OCT imaging allows operators to identify and often correct less-than-ideal results of an initial stent delivery – such as residual gaps between stent struts and vessel wall – that may encroach on the lumen, with possible clinical consequences.
Such imaging, said Dr. Ali, “lets you identify tissue protrusions, malappositions, dissections, and untreated reference-segment disease” that may potentially trigger thrombosis. That makes a strong argument for giving IVI guidance a more common, perhaps even routine role in PCI procedures.
Selling routine IVI-guided PCI in practice
“I think the study results are quite clear,” said Deepak L. Bhatt, MD, MPH, as session comoderator following the OCTOBER presentation. “The challenge, though, will be convincing the average interventional cardiologist worldwide that it was specifically the imaging and not the extra care that the patient getting OCT also inherently receives.”
Did OCT’s better trial outcomes stem from IVI itself or from greater operator attentiveness to procedural results – such as, for example, more high-pressure expansions to optimize stent placement, “the sort of thing that tends to occur when invasive imaging is added on to just plain old angiography?” Dr. Bhatt asked of Lene N. Andreasen, MD, who had just presented the OCTOBER trial. “There’s no way of uncoupling the two things.”
What can be said, “at this point, to convince interventional cardiologists that the extra time, energy, expense, is truly indicated,” that the data are “sufficient to change global practice?” asked Dr. Bhatt, Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai.
That remains an open question,” acknowledged Dr. Andreasen of Aarhus University Hospital. The best argument in favor of selective IVI-guided PCI is that “we actually see a clinical benefit” in the trials. “But of course, it comes with a cost. It comes with longer procedures and more contrast.” How clinical practice responds to the new data remains to be seen, she proposed.
ILUMIEN-4 and OCTOBER in detail
Conducted at 80 centers in 18 countries, ILUMIEN-4 randomly assigned patients with diabetes or complex coronary lesions to undergo PCI guided by OCT or using standard angiography only, 1,233 and 1,254 patients, respectively.
Post-PCI MSA averaged 5.72 mm2 with OCT guidance and 5.36 mm2 in the angiography-only group (P < .001).
Their rates of target-vessel failure at 2 years were not significantly different at 7.4% and 8.2%, respectively. The 2-year composite endpoint included cardiac death, target vessel–related MI, or ischemia-driven target-vessel revascularization.
Definite or probable stent thrombosis was observed over 2 years in 0.5% of the OCT group and 1.4% of those with angiography-only PCI (hazard ratio, 0.36; 95% confidence interval, 0.14-0.91; P = .02) favoring OCT.
The OCTOBER trial, conducted at 38 centers in Europe, entered 1201 patients with stable angina or acute coronary syndromes and angiographically identified complex bifurcation lesions. They involved the left-main coronary artery in about one-fifth of cases.
Patients were randomly assigned to bifurcation PCI guided by OCT or under standard angiography, 600 and 601 patients, respectively. Rates for procedure-related complications were similar at 6.8% and 5.7%, respectively.
Over a median of 2 years, 10.1% of the OCT group and 14.1% of angiography-only patients developed a MACE event, including cardiac death, target-lesion MI, or ischemia-driven target-lesion revascularization. The adjusted HR was 0.71 (95% CI, 0.51-0.98; P = .035) in favor of OCT.
Meta-analysis, trials to date
The meta-analysis presented by Dr. Stone included ILUMIEN-4, OCTOBER, and 18 earlier outcomes trials comparing PCI guided by IVI, either OCT or IVUS, and angiography-only PCI. It covered 12,428 patients with chronic or acute coronary disease and followed them a mean of 26 months; the longest follow-up was 5 years. They were assigned to IVI-guided or angiography-only PCI, 7,038 and 5,390 patients, respectively.
Dr. Stone and colleagues conducted a network meta-analysis of the 20 studies, that is, a combined analysis that allowed both direct and indirect comparisons of standard angiography-only procedures to each of the other studied comparator interventions including OCT, IVUS, and either OCT or IVUS. They then derived network-estimate odds ratios for IVI-guided PCI vs angiography-only procedures.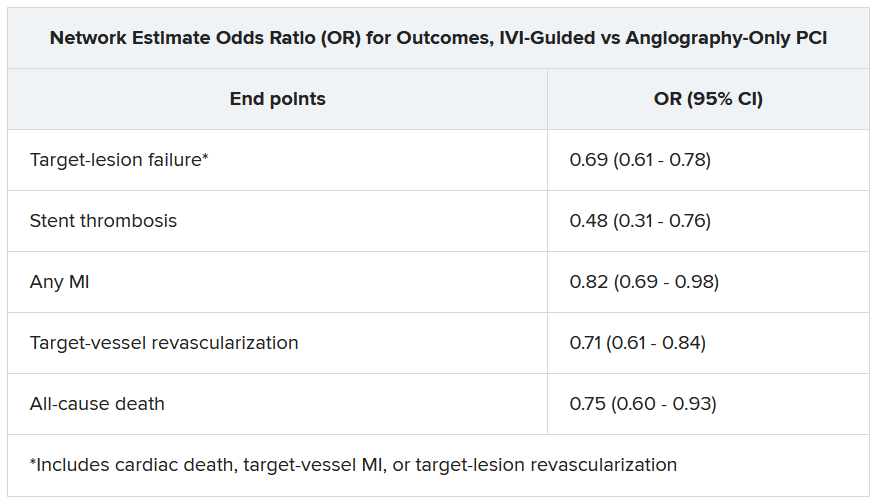
“Hopefully, this will impact the guidelines,” Dr. Stone said of the meta-analysis. Procedures guided by IVI might become more common in clinical practice if they were to garner a Class-I guideline recommendation, the strongest recommendation category.
“That would make a difference, but we’d also need to work to remove impediments to increasing intravascular imaging guidance” for most patients undergoing PCI, he said, referring to challenges in obtaining reimbursement for IVI-guided PCI and training enough operators to handle the projected demand.
ILUMIEN-4 was funded by Abbott. OCTOBER was supported by grants from Abbott Vascular, St. Jude Medical, and Aarhus University. The network meta-analysis received statistical support from Abbott. Dr. Ali disclosed institutional grant support from Abbott, Abiomed, Acist Medical, Boston Scientific, Cardiovascular Systems, Medtronic, the National Institutes of Health, Opsens Medical, Philips, and Teleflex; consulting fees from Astra Zeneca, Philips, Shockwave; and holding equity in Elucid, Spectrawave, Shockwave, and VitalConnect. Dr. Holm and Dr. Bhatt reported numerous conflicts of interest. Dr. Andreasen disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A routine role for intravascular imaging (IVI) guidance for percutaneous coronary intervention (PCI) has long been favored by many of the technology’s researchers and enthusiasts. Now evidence from large, randomized trials may be catching up with such aspirations, though not without caveats.
One way IVI guidance may achieve that, the research suggests, albeit more speculatively, is by cutting risk for stent thrombosis, compared with the risk associated with angiography-only PCI.
The new studies, two large randomized IVI trials plus a meta-analysis of 20 such studies, were presented at the annual congress of the European Society of Cardiology.
In one, called ILUMIEN-4, PCI guided by optical coherence tomography (OCT) was associated with fewer procedural complications and better acute results – that is, larger post-PCI minimum stent area (MSA) – than in angiography-only procedures (P < .001). Poststenting MSA, an established predictor of clinical outcomes, was the primary imaging endpoint of the trial with almost 2,500 patients.
Yet the OCT group’s greater post-PCI MSA did not translate to reduced risk for the primary clinical endpoint of 2-year target-vessel failure. Among secondary endpoints, however, stent thrombosis at some point during the follow-up was 64% less likely (P = .02) with OCT guidance than angiography-only PCI.
ILUMIEN-4, despite its neutral clinical result, still “strongly advocates” for PCI guidance by OCT, at least among patients like those in the trial, said principal investigator Ziad Ali, MD, DPhil. He based that largely on the strategy’s greater postprocedure lumen areas in the trials, which are among “the strongest independent predictors for long term outcomes,” said Dr. Ali, of St. Francis Hospital & Heart Center, Roslyn, N.Y., at a press conference on IVI trials during the ESC Congress.
Selected complex lesion type
In contrast, the OCTOBER trial, presented at the sessions back to back with ILUMIEN-4, saw OCT guidance lead to better clinical outcomes than angiography alone after PCI of bifurcation lesions, which normally can be a special challenge for operators.
In the trial, which entered about 1,200 patients with such complex lesions, the 2-year risk for major adverse cardiac events (MACE) fell 60% after OCT-guided PCI, compared with angiography-only procedures (P = .035).
The finding is novel for showing that OCT guidance in bifurcation PCI can make a significant clinical difference, said OCTOBER investigator Niels R. Holm, MD, at the same media presentation on IVI trials.
“Multiple studies have shown that OCT allows for optimization of bifurcation PCI, and our results confirm that such optimization may improve the patient’s prognosis,” said Dr. Holm of Aarhus (Denmark) University Hospital.
ILUMIEN-4 and OCTOBER, both of which prespecified the Xience (Abbott) everolimus-eluting stent for the procedures, were published in the New England Journal of Medicine in tandem with their respective presentations at the ESC sessions.
Covering the spectrum
A meta-analysis presented at the same ESC session compared IVI using either OCT or intravascular ultrasound (IVUS) with angiography-only PCI across 20 randomized trials with a total of more than 12,000 patients.
Significant outcomes for IVI guidance versus angiography alone included a 31% drop in risk for target-lesion failure, the primary endpoint. And this study, as well, showed a steep 52% reduction in risk for in-stent thrombosis with the IVI-guided approach.
And “for the first time” in IVI studies, “we demonstrated reductions in all-myocardial-infarction and all-cause death, the latter by 25%,” Gregg Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said in presenting the meta-analysis. Dr. Stone is also the ILUMIEN-4 study chairperson.
“The routine use of OCT or IVUS to guide most PCI procedures will substantially improve patient event-free survival,” he predicted, “enhancing both the long-term safety and effectiveness of the procedure.”
Dr. Stone said that IVI guidance “should be standard of care, if not in all patients, then in most patients.” Part of the rationale: PCI is unlikely to be improved much further by incremental gains in drug-eluting stent design. “That technology has almost plateaued.” But there’s yet room for “substantially improved outcomes” from adjunctive treatments and techniques such as IVI guidance.
The 20 studies in the meta-analysis encompassed an array of patients and lesions both complex and noncomplex, Dr. Stone observed, including bifurcation lesions, chronic total occlusions, left-main coronary stenoses, and MI culprit lesions.
“They really covered the spectrum of PCI,” he said. “I’m not recommending that intravascular imaging be used in every single case. But I do think it should be used in the majority of patients” and be standard of care for PCI in left-main lesions and “complex coronary disease, high-risk patients, and high-risk lesions.”
Unique advantage
The IVI-guidance groups in both ILUMIEN-4 and the meta-analysis showed a significant drop in risk for stent thrombosis – that is, abrupt thrombotic vessel closure, which typically occurs in 1% or fewer PCI cases but can trigger an MI and pose a mortality risk up to 45%.
Those risk reductions are consistent with a unique IVI advantage: the ability to guide optimization of stent deployments. When formally presenting ILUMIEN-4 at the ESC sessions, Ali observed that IVUS and OCT imaging allows operators to identify and often correct less-than-ideal results of an initial stent delivery – such as residual gaps between stent struts and vessel wall – that may encroach on the lumen, with possible clinical consequences.
Such imaging, said Dr. Ali, “lets you identify tissue protrusions, malappositions, dissections, and untreated reference-segment disease” that may potentially trigger thrombosis. That makes a strong argument for giving IVI guidance a more common, perhaps even routine role in PCI procedures.
Selling routine IVI-guided PCI in practice
“I think the study results are quite clear,” said Deepak L. Bhatt, MD, MPH, as session comoderator following the OCTOBER presentation. “The challenge, though, will be convincing the average interventional cardiologist worldwide that it was specifically the imaging and not the extra care that the patient getting OCT also inherently receives.”
Did OCT’s better trial outcomes stem from IVI itself or from greater operator attentiveness to procedural results – such as, for example, more high-pressure expansions to optimize stent placement, “the sort of thing that tends to occur when invasive imaging is added on to just plain old angiography?” Dr. Bhatt asked of Lene N. Andreasen, MD, who had just presented the OCTOBER trial. “There’s no way of uncoupling the two things.”
What can be said, “at this point, to convince interventional cardiologists that the extra time, energy, expense, is truly indicated,” that the data are “sufficient to change global practice?” asked Dr. Bhatt, Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai.
That remains an open question,” acknowledged Dr. Andreasen of Aarhus University Hospital. The best argument in favor of selective IVI-guided PCI is that “we actually see a clinical benefit” in the trials. “But of course, it comes with a cost. It comes with longer procedures and more contrast.” How clinical practice responds to the new data remains to be seen, she proposed.
ILUMIEN-4 and OCTOBER in detail
Conducted at 80 centers in 18 countries, ILUMIEN-4 randomly assigned patients with diabetes or complex coronary lesions to undergo PCI guided by OCT or using standard angiography only, 1,233 and 1,254 patients, respectively.
Post-PCI MSA averaged 5.72 mm2 with OCT guidance and 5.36 mm2 in the angiography-only group (P < .001).
Their rates of target-vessel failure at 2 years were not significantly different at 7.4% and 8.2%, respectively. The 2-year composite endpoint included cardiac death, target vessel–related MI, or ischemia-driven target-vessel revascularization.
Definite or probable stent thrombosis was observed over 2 years in 0.5% of the OCT group and 1.4% of those with angiography-only PCI (hazard ratio, 0.36; 95% confidence interval, 0.14-0.91; P = .02) favoring OCT.
The OCTOBER trial, conducted at 38 centers in Europe, entered 1201 patients with stable angina or acute coronary syndromes and angiographically identified complex bifurcation lesions. They involved the left-main coronary artery in about one-fifth of cases.
Patients were randomly assigned to bifurcation PCI guided by OCT or under standard angiography, 600 and 601 patients, respectively. Rates for procedure-related complications were similar at 6.8% and 5.7%, respectively.
Over a median of 2 years, 10.1% of the OCT group and 14.1% of angiography-only patients developed a MACE event, including cardiac death, target-lesion MI, or ischemia-driven target-lesion revascularization. The adjusted HR was 0.71 (95% CI, 0.51-0.98; P = .035) in favor of OCT.
Meta-analysis, trials to date
The meta-analysis presented by Dr. Stone included ILUMIEN-4, OCTOBER, and 18 earlier outcomes trials comparing PCI guided by IVI, either OCT or IVUS, and angiography-only PCI. It covered 12,428 patients with chronic or acute coronary disease and followed them a mean of 26 months; the longest follow-up was 5 years. They were assigned to IVI-guided or angiography-only PCI, 7,038 and 5,390 patients, respectively.
Dr. Stone and colleagues conducted a network meta-analysis of the 20 studies, that is, a combined analysis that allowed both direct and indirect comparisons of standard angiography-only procedures to each of the other studied comparator interventions including OCT, IVUS, and either OCT or IVUS. They then derived network-estimate odds ratios for IVI-guided PCI vs angiography-only procedures.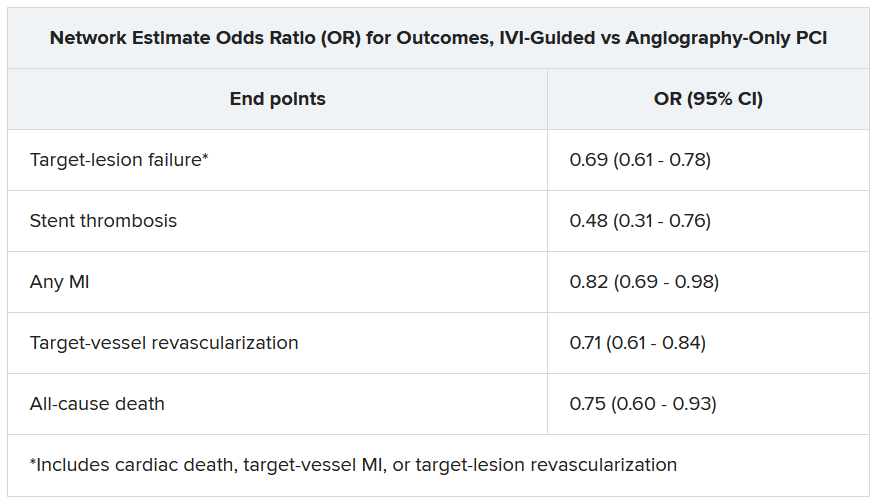
“Hopefully, this will impact the guidelines,” Dr. Stone said of the meta-analysis. Procedures guided by IVI might become more common in clinical practice if they were to garner a Class-I guideline recommendation, the strongest recommendation category.
“That would make a difference, but we’d also need to work to remove impediments to increasing intravascular imaging guidance” for most patients undergoing PCI, he said, referring to challenges in obtaining reimbursement for IVI-guided PCI and training enough operators to handle the projected demand.
ILUMIEN-4 was funded by Abbott. OCTOBER was supported by grants from Abbott Vascular, St. Jude Medical, and Aarhus University. The network meta-analysis received statistical support from Abbott. Dr. Ali disclosed institutional grant support from Abbott, Abiomed, Acist Medical, Boston Scientific, Cardiovascular Systems, Medtronic, the National Institutes of Health, Opsens Medical, Philips, and Teleflex; consulting fees from Astra Zeneca, Philips, Shockwave; and holding equity in Elucid, Spectrawave, Shockwave, and VitalConnect. Dr. Holm and Dr. Bhatt reported numerous conflicts of interest. Dr. Andreasen disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE ESC CONGRESS 2023











