User login
Lack of Knowledge About Surgical Smoke, Masks, and Respirators Among US Dermatology Residents and Fellows in the Era of COVID-19
During dermatologic surgery, surgical smoke created by electrocautery is known to contain not only nanoparticles and carcinogenic compounds but also infectious particles.1 Poor awareness of the risks associated with breathing surgical smoke and lack of safety practices among US dermatology residents has been documented.2 In this era of the novel coronavirus disease 2019 (COVID-19) pandemic, these issues are particularly pertinent due to the theoretical risk of viral transmission through aerosolized particles. There are few studies investigating viral transmission during surgery, but large numbers of health care workers in close contact with the upper aerodigestive tract during diagnostic and therapeutic procedures have become infected with COVID-19, leading to the recommendation of added safety measures for surgeons in other fields.3 Recommendations do not yet exist for dermatologic surgeons, and it is not yet known if this population is at higher risk for COVID-19 infection due to aerosolized viral particles in the air or in surgical smoke. Nonetheless, we feel that additional safety measures during dermatologic surgery are warranted, particularly when operating on areas of higher viral load such as the nasal or oral mucosae, and understanding of safety equipment is paramount. Thus, we aimed to assess the awareness of safety measures among training dermatologists and dermatologic surgeons during the COVID-19 pandemic.
In April 2020, one of the authors (S.I.B.J.) gave a lecture to residents and fellows of accredited dermatology residency or fellowship programs in the United States on surgical masks and surgical smoke in dermatologic surgery on an online videoconferencing platform through our institution. During the lecture, participants were polled regarding their understanding of these topics. Forty-one attendees were included in this analysis, with a 100% response rate. Results showed that 54% (22/41) of respondents indicated they had not had formal lectures on surgical smoke content and management, and 51% (21/41) responded that they do not use a smoke evacuator during surgical procedures. When asked why smoke evacuators are not used, 27% (11/41) responded that the equipment is too cumbersome, 12% (5/41) reported that smoke evacuators are not available at their practice or institution, 7% did not believe that smoke evacuators are necessary, and 5% did not know they are used in dermatology. Additionally, 66% (27/41) said they had not had formal presentations on personal protective equipment (PPE) or masks, though 93% (38/41) said they wear a surgical mask during surgery. Despite the high percentage of respondents using masks, 82% (31/38) did not know what type of mask they were wearing, and the remainder wore a variety of American Society for Testing and Materials–rated (levels 1, 2, or 3) and European Standards type II (EN14683) masks. Following the presentation, 100% of respondents said they were likely to use a smoke evacuator if made available, and 100% reported that they had a better understanding of respirators and masks.
In summary, more than 50% of dermatology trainees in our study had not been formally educated regarding PPE despite its importance during the COVID-19 pandemic. The majority of respondents were unaware of the dangers of surgical smoke, and a small number of respondents believed that smoke evacuators were not necessary or did not know that they were even used in dermatology. Based on the results of this quick survey during a lecture to dermatology trainees, we believe it is important to alert educators to this knowledge gap regarding PPE in the dermatology teaching curriculum. We have shown that even a short lecture format was an effective way of disseminating information about PPE and surgical safety. We believe that safety measures are more important now during a time when risk for infection with a potentially fatal virus is high. We encourage clinical educators to emphasize the importance of personal safety to trainees during residency, especially during the COVID-19 pandemic.
- Georgesen C, Lipner SR. Surgical smoke: risk assessment and mitigation strategies. J Am Acad Dermatol. 2018;79:746-755.
- Chapman LW, Korta DZ, Lee PK, et al. Awareness of surgical smoke risks and assessment of safety practices during electrosurgery among US dermatology residents. JAMA Dermatol. 2017;153:467.
- Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic [published online March 31, 2020]. JAMA Otolaryngol Neck Surg. doi:10.1001/jamaoto.2020.0780.
During dermatologic surgery, surgical smoke created by electrocautery is known to contain not only nanoparticles and carcinogenic compounds but also infectious particles.1 Poor awareness of the risks associated with breathing surgical smoke and lack of safety practices among US dermatology residents has been documented.2 In this era of the novel coronavirus disease 2019 (COVID-19) pandemic, these issues are particularly pertinent due to the theoretical risk of viral transmission through aerosolized particles. There are few studies investigating viral transmission during surgery, but large numbers of health care workers in close contact with the upper aerodigestive tract during diagnostic and therapeutic procedures have become infected with COVID-19, leading to the recommendation of added safety measures for surgeons in other fields.3 Recommendations do not yet exist for dermatologic surgeons, and it is not yet known if this population is at higher risk for COVID-19 infection due to aerosolized viral particles in the air or in surgical smoke. Nonetheless, we feel that additional safety measures during dermatologic surgery are warranted, particularly when operating on areas of higher viral load such as the nasal or oral mucosae, and understanding of safety equipment is paramount. Thus, we aimed to assess the awareness of safety measures among training dermatologists and dermatologic surgeons during the COVID-19 pandemic.
In April 2020, one of the authors (S.I.B.J.) gave a lecture to residents and fellows of accredited dermatology residency or fellowship programs in the United States on surgical masks and surgical smoke in dermatologic surgery on an online videoconferencing platform through our institution. During the lecture, participants were polled regarding their understanding of these topics. Forty-one attendees were included in this analysis, with a 100% response rate. Results showed that 54% (22/41) of respondents indicated they had not had formal lectures on surgical smoke content and management, and 51% (21/41) responded that they do not use a smoke evacuator during surgical procedures. When asked why smoke evacuators are not used, 27% (11/41) responded that the equipment is too cumbersome, 12% (5/41) reported that smoke evacuators are not available at their practice or institution, 7% did not believe that smoke evacuators are necessary, and 5% did not know they are used in dermatology. Additionally, 66% (27/41) said they had not had formal presentations on personal protective equipment (PPE) or masks, though 93% (38/41) said they wear a surgical mask during surgery. Despite the high percentage of respondents using masks, 82% (31/38) did not know what type of mask they were wearing, and the remainder wore a variety of American Society for Testing and Materials–rated (levels 1, 2, or 3) and European Standards type II (EN14683) masks. Following the presentation, 100% of respondents said they were likely to use a smoke evacuator if made available, and 100% reported that they had a better understanding of respirators and masks.
In summary, more than 50% of dermatology trainees in our study had not been formally educated regarding PPE despite its importance during the COVID-19 pandemic. The majority of respondents were unaware of the dangers of surgical smoke, and a small number of respondents believed that smoke evacuators were not necessary or did not know that they were even used in dermatology. Based on the results of this quick survey during a lecture to dermatology trainees, we believe it is important to alert educators to this knowledge gap regarding PPE in the dermatology teaching curriculum. We have shown that even a short lecture format was an effective way of disseminating information about PPE and surgical safety. We believe that safety measures are more important now during a time when risk for infection with a potentially fatal virus is high. We encourage clinical educators to emphasize the importance of personal safety to trainees during residency, especially during the COVID-19 pandemic.
During dermatologic surgery, surgical smoke created by electrocautery is known to contain not only nanoparticles and carcinogenic compounds but also infectious particles.1 Poor awareness of the risks associated with breathing surgical smoke and lack of safety practices among US dermatology residents has been documented.2 In this era of the novel coronavirus disease 2019 (COVID-19) pandemic, these issues are particularly pertinent due to the theoretical risk of viral transmission through aerosolized particles. There are few studies investigating viral transmission during surgery, but large numbers of health care workers in close contact with the upper aerodigestive tract during diagnostic and therapeutic procedures have become infected with COVID-19, leading to the recommendation of added safety measures for surgeons in other fields.3 Recommendations do not yet exist for dermatologic surgeons, and it is not yet known if this population is at higher risk for COVID-19 infection due to aerosolized viral particles in the air or in surgical smoke. Nonetheless, we feel that additional safety measures during dermatologic surgery are warranted, particularly when operating on areas of higher viral load such as the nasal or oral mucosae, and understanding of safety equipment is paramount. Thus, we aimed to assess the awareness of safety measures among training dermatologists and dermatologic surgeons during the COVID-19 pandemic.
In April 2020, one of the authors (S.I.B.J.) gave a lecture to residents and fellows of accredited dermatology residency or fellowship programs in the United States on surgical masks and surgical smoke in dermatologic surgery on an online videoconferencing platform through our institution. During the lecture, participants were polled regarding their understanding of these topics. Forty-one attendees were included in this analysis, with a 100% response rate. Results showed that 54% (22/41) of respondents indicated they had not had formal lectures on surgical smoke content and management, and 51% (21/41) responded that they do not use a smoke evacuator during surgical procedures. When asked why smoke evacuators are not used, 27% (11/41) responded that the equipment is too cumbersome, 12% (5/41) reported that smoke evacuators are not available at their practice or institution, 7% did not believe that smoke evacuators are necessary, and 5% did not know they are used in dermatology. Additionally, 66% (27/41) said they had not had formal presentations on personal protective equipment (PPE) or masks, though 93% (38/41) said they wear a surgical mask during surgery. Despite the high percentage of respondents using masks, 82% (31/38) did not know what type of mask they were wearing, and the remainder wore a variety of American Society for Testing and Materials–rated (levels 1, 2, or 3) and European Standards type II (EN14683) masks. Following the presentation, 100% of respondents said they were likely to use a smoke evacuator if made available, and 100% reported that they had a better understanding of respirators and masks.
In summary, more than 50% of dermatology trainees in our study had not been formally educated regarding PPE despite its importance during the COVID-19 pandemic. The majority of respondents were unaware of the dangers of surgical smoke, and a small number of respondents believed that smoke evacuators were not necessary or did not know that they were even used in dermatology. Based on the results of this quick survey during a lecture to dermatology trainees, we believe it is important to alert educators to this knowledge gap regarding PPE in the dermatology teaching curriculum. We have shown that even a short lecture format was an effective way of disseminating information about PPE and surgical safety. We believe that safety measures are more important now during a time when risk for infection with a potentially fatal virus is high. We encourage clinical educators to emphasize the importance of personal safety to trainees during residency, especially during the COVID-19 pandemic.
- Georgesen C, Lipner SR. Surgical smoke: risk assessment and mitigation strategies. J Am Acad Dermatol. 2018;79:746-755.
- Chapman LW, Korta DZ, Lee PK, et al. Awareness of surgical smoke risks and assessment of safety practices during electrosurgery among US dermatology residents. JAMA Dermatol. 2017;153:467.
- Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic [published online March 31, 2020]. JAMA Otolaryngol Neck Surg. doi:10.1001/jamaoto.2020.0780.
- Georgesen C, Lipner SR. Surgical smoke: risk assessment and mitigation strategies. J Am Acad Dermatol. 2018;79:746-755.
- Chapman LW, Korta DZ, Lee PK, et al. Awareness of surgical smoke risks and assessment of safety practices during electrosurgery among US dermatology residents. JAMA Dermatol. 2017;153:467.
- Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic [published online March 31, 2020]. JAMA Otolaryngol Neck Surg. doi:10.1001/jamaoto.2020.0780.
Practice Points
- Harmful surgical smoke is created with electrocautery. Smoke evacuators and approved surgical masks can help mitigate the harmful effects of smoke on the health of dermatologic surgeons.
- Dermatology curricula for residents and medical students should include information on surgical smoke safety.
Dual therapy serves as well as triple for most HIV patients
based on a meta-analysis including data from more than 5,000 patients.
Although triple therapy remains the standard of care, the availability of more potent drugs has revived interest in dual and mono therapies, wrote Pisaturo Mariantonietta, MD, of the University of Campania Luigi Vanvitelli, Naples, Italy, and colleagues.
In a study published in Clinical Microbiology and Infection, the researchers identified 14 articles including 5,205 treatment-naive HIV adults. The studies were published between 2008 and 2020; 13 were randomized, controlled trials.
The dual therapies used in the studies included atazanavir/r plus maraviroc; lopinavir/r plus lamivudine; raltegravir plus darunavir/r; lopinavir/r plus tenofovir, raltegravir, efavirenz, or maraviroc; atazanavir/r plus raltegravir and darunavir/r plus maraviroc; and dolutegravir plus lamivudine.
Overall, no significant differences occurred in the primary endpoint of treatment failure across 10 studies between dual therapy and triple therapy patients based on data at 48 weeks (relative risk 1.20). “The rate of treatment failure did not differ among the two groups when stratifying the patients according to the drug used in the dual regimen,” the researchers said.
Low viral load’s link to treatment failure
Among 2,398 patients with a low HIV viral load (less than 100,000 copies/mL), dual therapy patients were significantly more likely to experience treatment failure than were triple therapy patients (RR, 1.47, P = .007). No differences were noted between dual and triple therapy failure among patients with high HIV viral loads at baseline. Patterns were similar at 96 weeks, but only three studies included 96-week data, the researchers said.
The rate of discontinuation because of adverse events was not significantly different between the groups at 48 weeks.
The study findings were limited by several factors, including the use of different regimens in the dual strategies, some of which are no longer in use, as well as there being insufficient data to fully compare outcomes at 96 weeks, and lack of information on cerebrospinal fluid viral load, the researchers noted.
However, the results suggest that dual therapy might be considered for HIV-naive patients with a low viral load, they said.
“Further RCTs that will evaluate the efficacy of antiretroviral regimens in use today among difficult-to-treat populations, such as patients with high viral load, including both intention-to-treat and per-protocol analysis, are needed to address this topic,” they concluded.
Consider range of patient factors when choosing therapies
Conducting the study at this time was important because of the expanding options for treating HIV patients, Donna E. Sweet, MD, an HIV specialist and professor of medicine at the University of Kansas, Wichita, said in an interview.
“We now have two single tablet formulations that are dual rather than triple therapy, and as treaters we are all trying to know when to use them,” she explained.
Dr. Sweet said she was not surprised by the study findings, given that well-conducted, randomized, controlled trials allowed the combination therapies to be approved.
Some of the key challenges to identifying the optimal treatment for HIV patients include factoring in the use of concomitant medications that could lead to drug-drug interactions, noted Dr. Sweet, who serves an editorial advisory board member of Internal Medicine News.
The take-home message for clinicians, in her opinion, is that “less drugs may mean less toxicity, but we don’t want to sacrifice efficacy,” she said. “There may be patients who are better suited than others for two vs. three drugs,” Dr. Sweet emphasized.
The next steps for research on the value of dual vs. triple therapy should include longer term efficacy studies, especially in those with lower CD4 counts and higher viral loads, said Dr. Sweet. In addition to factors such as CD4 counts and viral load, the food requirements of certain ART regimens could affect adherence and therefore a clinician decision to use two drugs rather than three, she noted.
Dr. Sweet disclosed past relationships with ViiV, Gilead, Merck, and Janssen on their speakers bureaus, and current advisory roles with Gilead and ViiV.
The study received no outside funding. Lead author Dr. Mariantonietta and several coauthors disclosed relationships with companies including ViiV Healthcare, AbbVie, Janssen-Cilag and Gilead Science, and Merck Sharp & Dohme, but no conflicts in connection with this study.
SOURCE: Mariantonietta P et al. Clin Microbiol Infect. 2020 Oct 5. doi: 10.1016/j.cmi.2020.09.048.
based on a meta-analysis including data from more than 5,000 patients.
Although triple therapy remains the standard of care, the availability of more potent drugs has revived interest in dual and mono therapies, wrote Pisaturo Mariantonietta, MD, of the University of Campania Luigi Vanvitelli, Naples, Italy, and colleagues.
In a study published in Clinical Microbiology and Infection, the researchers identified 14 articles including 5,205 treatment-naive HIV adults. The studies were published between 2008 and 2020; 13 were randomized, controlled trials.
The dual therapies used in the studies included atazanavir/r plus maraviroc; lopinavir/r plus lamivudine; raltegravir plus darunavir/r; lopinavir/r plus tenofovir, raltegravir, efavirenz, or maraviroc; atazanavir/r plus raltegravir and darunavir/r plus maraviroc; and dolutegravir plus lamivudine.
Overall, no significant differences occurred in the primary endpoint of treatment failure across 10 studies between dual therapy and triple therapy patients based on data at 48 weeks (relative risk 1.20). “The rate of treatment failure did not differ among the two groups when stratifying the patients according to the drug used in the dual regimen,” the researchers said.
Low viral load’s link to treatment failure
Among 2,398 patients with a low HIV viral load (less than 100,000 copies/mL), dual therapy patients were significantly more likely to experience treatment failure than were triple therapy patients (RR, 1.47, P = .007). No differences were noted between dual and triple therapy failure among patients with high HIV viral loads at baseline. Patterns were similar at 96 weeks, but only three studies included 96-week data, the researchers said.
The rate of discontinuation because of adverse events was not significantly different between the groups at 48 weeks.
The study findings were limited by several factors, including the use of different regimens in the dual strategies, some of which are no longer in use, as well as there being insufficient data to fully compare outcomes at 96 weeks, and lack of information on cerebrospinal fluid viral load, the researchers noted.
However, the results suggest that dual therapy might be considered for HIV-naive patients with a low viral load, they said.
“Further RCTs that will evaluate the efficacy of antiretroviral regimens in use today among difficult-to-treat populations, such as patients with high viral load, including both intention-to-treat and per-protocol analysis, are needed to address this topic,” they concluded.
Consider range of patient factors when choosing therapies
Conducting the study at this time was important because of the expanding options for treating HIV patients, Donna E. Sweet, MD, an HIV specialist and professor of medicine at the University of Kansas, Wichita, said in an interview.
“We now have two single tablet formulations that are dual rather than triple therapy, and as treaters we are all trying to know when to use them,” she explained.
Dr. Sweet said she was not surprised by the study findings, given that well-conducted, randomized, controlled trials allowed the combination therapies to be approved.
Some of the key challenges to identifying the optimal treatment for HIV patients include factoring in the use of concomitant medications that could lead to drug-drug interactions, noted Dr. Sweet, who serves an editorial advisory board member of Internal Medicine News.
The take-home message for clinicians, in her opinion, is that “less drugs may mean less toxicity, but we don’t want to sacrifice efficacy,” she said. “There may be patients who are better suited than others for two vs. three drugs,” Dr. Sweet emphasized.
The next steps for research on the value of dual vs. triple therapy should include longer term efficacy studies, especially in those with lower CD4 counts and higher viral loads, said Dr. Sweet. In addition to factors such as CD4 counts and viral load, the food requirements of certain ART regimens could affect adherence and therefore a clinician decision to use two drugs rather than three, she noted.
Dr. Sweet disclosed past relationships with ViiV, Gilead, Merck, and Janssen on their speakers bureaus, and current advisory roles with Gilead and ViiV.
The study received no outside funding. Lead author Dr. Mariantonietta and several coauthors disclosed relationships with companies including ViiV Healthcare, AbbVie, Janssen-Cilag and Gilead Science, and Merck Sharp & Dohme, but no conflicts in connection with this study.
SOURCE: Mariantonietta P et al. Clin Microbiol Infect. 2020 Oct 5. doi: 10.1016/j.cmi.2020.09.048.
based on a meta-analysis including data from more than 5,000 patients.
Although triple therapy remains the standard of care, the availability of more potent drugs has revived interest in dual and mono therapies, wrote Pisaturo Mariantonietta, MD, of the University of Campania Luigi Vanvitelli, Naples, Italy, and colleagues.
In a study published in Clinical Microbiology and Infection, the researchers identified 14 articles including 5,205 treatment-naive HIV adults. The studies were published between 2008 and 2020; 13 were randomized, controlled trials.
The dual therapies used in the studies included atazanavir/r plus maraviroc; lopinavir/r plus lamivudine; raltegravir plus darunavir/r; lopinavir/r plus tenofovir, raltegravir, efavirenz, or maraviroc; atazanavir/r plus raltegravir and darunavir/r plus maraviroc; and dolutegravir plus lamivudine.
Overall, no significant differences occurred in the primary endpoint of treatment failure across 10 studies between dual therapy and triple therapy patients based on data at 48 weeks (relative risk 1.20). “The rate of treatment failure did not differ among the two groups when stratifying the patients according to the drug used in the dual regimen,” the researchers said.
Low viral load’s link to treatment failure
Among 2,398 patients with a low HIV viral load (less than 100,000 copies/mL), dual therapy patients were significantly more likely to experience treatment failure than were triple therapy patients (RR, 1.47, P = .007). No differences were noted between dual and triple therapy failure among patients with high HIV viral loads at baseline. Patterns were similar at 96 weeks, but only three studies included 96-week data, the researchers said.
The rate of discontinuation because of adverse events was not significantly different between the groups at 48 weeks.
The study findings were limited by several factors, including the use of different regimens in the dual strategies, some of which are no longer in use, as well as there being insufficient data to fully compare outcomes at 96 weeks, and lack of information on cerebrospinal fluid viral load, the researchers noted.
However, the results suggest that dual therapy might be considered for HIV-naive patients with a low viral load, they said.
“Further RCTs that will evaluate the efficacy of antiretroviral regimens in use today among difficult-to-treat populations, such as patients with high viral load, including both intention-to-treat and per-protocol analysis, are needed to address this topic,” they concluded.
Consider range of patient factors when choosing therapies
Conducting the study at this time was important because of the expanding options for treating HIV patients, Donna E. Sweet, MD, an HIV specialist and professor of medicine at the University of Kansas, Wichita, said in an interview.
“We now have two single tablet formulations that are dual rather than triple therapy, and as treaters we are all trying to know when to use them,” she explained.
Dr. Sweet said she was not surprised by the study findings, given that well-conducted, randomized, controlled trials allowed the combination therapies to be approved.
Some of the key challenges to identifying the optimal treatment for HIV patients include factoring in the use of concomitant medications that could lead to drug-drug interactions, noted Dr. Sweet, who serves an editorial advisory board member of Internal Medicine News.
The take-home message for clinicians, in her opinion, is that “less drugs may mean less toxicity, but we don’t want to sacrifice efficacy,” she said. “There may be patients who are better suited than others for two vs. three drugs,” Dr. Sweet emphasized.
The next steps for research on the value of dual vs. triple therapy should include longer term efficacy studies, especially in those with lower CD4 counts and higher viral loads, said Dr. Sweet. In addition to factors such as CD4 counts and viral load, the food requirements of certain ART regimens could affect adherence and therefore a clinician decision to use two drugs rather than three, she noted.
Dr. Sweet disclosed past relationships with ViiV, Gilead, Merck, and Janssen on their speakers bureaus, and current advisory roles with Gilead and ViiV.
The study received no outside funding. Lead author Dr. Mariantonietta and several coauthors disclosed relationships with companies including ViiV Healthcare, AbbVie, Janssen-Cilag and Gilead Science, and Merck Sharp & Dohme, but no conflicts in connection with this study.
SOURCE: Mariantonietta P et al. Clin Microbiol Infect. 2020 Oct 5. doi: 10.1016/j.cmi.2020.09.048.
FROM CLINICAL MICROBIOLOGY AND INFECTION
Being HIV positive increases risk of death from COVID-19
compared with people without HIV.
A comparison of outcomes of people with HIV to people without HIV who were hospitalized in the United Kingdom with COVID-19 from Jan. 17 to June 4 showed that HIV-positive status was associated with a 63% increased risk of day 28 mortality.
This was especially true for HIV+ patients younger than 70 years of age, said Anna Maria Geretti, MD, PhD, professor of virology and infectious diseases, University of Liverpool, England.
The results are from an analysis of data from the ISARIC World Health Organization (WHO) Clinical Characterisation Protocol (UK) study, and were presented at the HIV Glasgow annual meeting, held virtually this year because of the pandemic.
“We investigated whether HIV status could be important in COVID-19 outcomes because there was anxiety on the part of our patients, and we wanted to gather some evidence-based information in order to help guide them,” Dr. Geretti said in an interview.
“ISARIC is an international protocol and the UK is one of the nations participating. We applied for access to its very large database, which connects data from all patients who are hospitalized with either known or suspected COVID-19. We wanted to see specifically how the presentation and outcomes of patients with HIV compared with the rest of the population without HIV. It afforded us an ideal opportunity to start to answer this question, and this is our first analysis in what will be an ongoing process. Importantly, we showed that there is a need to really look more carefully at the population with HIV,” she said.
Out of a total of 47,539 patients in the database, 115 (0.24%) had confirmed HIV-positive status, and 103 of those 115, or 89.6%, had a record of being on antiretroviral therapy.
On admission, the patients with HIV were younger, with a median age of 55 compared with 74 for patients without HIV (P < .001). They also had a higher prevalence of obesity, moderate to severe liver disease, higher lymphocyte counts and C-reactive protein, as well as more systemic symptoms.
There were no differences in respiratory rate, need for oxygen, or prevalence of chest infiltrates.
The cumulative incidence of mortality at day 28 was 25.2% in HIV-positive patients compared with 32.1% in HIV-negative patients (P = .12).
But when the researchers looked more closely, they noticed that the mortality rate was actually higher in younger HIV+ patients compared with HIV-negative patients.
Stratified by age, 28-day mortality was significantly higher in HIV+ patients aged <50 years (P =.004); and those aged 50 to 59 years (P = .05).
“So below the age of 70, the risk of mortality was double in people with HIV. The people with HIV who died often had diabetes with complications and also more frequent obesity, but this was not the only explanation,” Dr. Geretti said. “There is something to do with the HIV status per se.”
Next steps will be to expand the data set and repeat the analysis with an additional 100 patients “at least” she said.
The researchers also hope to zero in on what about being HIV+ is increasing the mortality risk from COVID-19.
“Right now we need greater numbers and we hope that the research community will be stimulated to take a closer look at this information, and merge other data so that we can strengthen confidence in the data and tease out what factors are causing this increased risk for mortality,” Dr. Geretti said.
She also emphasized that all patients admitted to hospital with COVID-19 should be asked about their HIV status.
“It is important that the HIV status be recorded if we want to increase our ability to understand how HIV impacts survival,” she stressed. “In our experience we found that most of the hospital records were not doing that. Since HIV+ patients seem to be at increased risk, HIV status should be factored into the clinical management. Ask patients if they are HIV+, and if it is not known, then do a test. That would be good practice.”
Dr. Geretti reported no relevant financial relationships. The work was supported by grants from the National Institute of Health Research, the Medical Research Council, the Wellcome Trust, the Department for International Development, and the Bill and Melinda Gates Foundation.
A version of this article originally appeared on Medscape.com.
compared with people without HIV.
A comparison of outcomes of people with HIV to people without HIV who were hospitalized in the United Kingdom with COVID-19 from Jan. 17 to June 4 showed that HIV-positive status was associated with a 63% increased risk of day 28 mortality.
This was especially true for HIV+ patients younger than 70 years of age, said Anna Maria Geretti, MD, PhD, professor of virology and infectious diseases, University of Liverpool, England.
The results are from an analysis of data from the ISARIC World Health Organization (WHO) Clinical Characterisation Protocol (UK) study, and were presented at the HIV Glasgow annual meeting, held virtually this year because of the pandemic.
“We investigated whether HIV status could be important in COVID-19 outcomes because there was anxiety on the part of our patients, and we wanted to gather some evidence-based information in order to help guide them,” Dr. Geretti said in an interview.
“ISARIC is an international protocol and the UK is one of the nations participating. We applied for access to its very large database, which connects data from all patients who are hospitalized with either known or suspected COVID-19. We wanted to see specifically how the presentation and outcomes of patients with HIV compared with the rest of the population without HIV. It afforded us an ideal opportunity to start to answer this question, and this is our first analysis in what will be an ongoing process. Importantly, we showed that there is a need to really look more carefully at the population with HIV,” she said.
Out of a total of 47,539 patients in the database, 115 (0.24%) had confirmed HIV-positive status, and 103 of those 115, or 89.6%, had a record of being on antiretroviral therapy.
On admission, the patients with HIV were younger, with a median age of 55 compared with 74 for patients without HIV (P < .001). They also had a higher prevalence of obesity, moderate to severe liver disease, higher lymphocyte counts and C-reactive protein, as well as more systemic symptoms.
There were no differences in respiratory rate, need for oxygen, or prevalence of chest infiltrates.
The cumulative incidence of mortality at day 28 was 25.2% in HIV-positive patients compared with 32.1% in HIV-negative patients (P = .12).
But when the researchers looked more closely, they noticed that the mortality rate was actually higher in younger HIV+ patients compared with HIV-negative patients.
Stratified by age, 28-day mortality was significantly higher in HIV+ patients aged <50 years (P =.004); and those aged 50 to 59 years (P = .05).
“So below the age of 70, the risk of mortality was double in people with HIV. The people with HIV who died often had diabetes with complications and also more frequent obesity, but this was not the only explanation,” Dr. Geretti said. “There is something to do with the HIV status per se.”
Next steps will be to expand the data set and repeat the analysis with an additional 100 patients “at least” she said.
The researchers also hope to zero in on what about being HIV+ is increasing the mortality risk from COVID-19.
“Right now we need greater numbers and we hope that the research community will be stimulated to take a closer look at this information, and merge other data so that we can strengthen confidence in the data and tease out what factors are causing this increased risk for mortality,” Dr. Geretti said.
She also emphasized that all patients admitted to hospital with COVID-19 should be asked about their HIV status.
“It is important that the HIV status be recorded if we want to increase our ability to understand how HIV impacts survival,” she stressed. “In our experience we found that most of the hospital records were not doing that. Since HIV+ patients seem to be at increased risk, HIV status should be factored into the clinical management. Ask patients if they are HIV+, and if it is not known, then do a test. That would be good practice.”
Dr. Geretti reported no relevant financial relationships. The work was supported by grants from the National Institute of Health Research, the Medical Research Council, the Wellcome Trust, the Department for International Development, and the Bill and Melinda Gates Foundation.
A version of this article originally appeared on Medscape.com.
compared with people without HIV.
A comparison of outcomes of people with HIV to people without HIV who were hospitalized in the United Kingdom with COVID-19 from Jan. 17 to June 4 showed that HIV-positive status was associated with a 63% increased risk of day 28 mortality.
This was especially true for HIV+ patients younger than 70 years of age, said Anna Maria Geretti, MD, PhD, professor of virology and infectious diseases, University of Liverpool, England.
The results are from an analysis of data from the ISARIC World Health Organization (WHO) Clinical Characterisation Protocol (UK) study, and were presented at the HIV Glasgow annual meeting, held virtually this year because of the pandemic.
“We investigated whether HIV status could be important in COVID-19 outcomes because there was anxiety on the part of our patients, and we wanted to gather some evidence-based information in order to help guide them,” Dr. Geretti said in an interview.
“ISARIC is an international protocol and the UK is one of the nations participating. We applied for access to its very large database, which connects data from all patients who are hospitalized with either known or suspected COVID-19. We wanted to see specifically how the presentation and outcomes of patients with HIV compared with the rest of the population without HIV. It afforded us an ideal opportunity to start to answer this question, and this is our first analysis in what will be an ongoing process. Importantly, we showed that there is a need to really look more carefully at the population with HIV,” she said.
Out of a total of 47,539 patients in the database, 115 (0.24%) had confirmed HIV-positive status, and 103 of those 115, or 89.6%, had a record of being on antiretroviral therapy.
On admission, the patients with HIV were younger, with a median age of 55 compared with 74 for patients without HIV (P < .001). They also had a higher prevalence of obesity, moderate to severe liver disease, higher lymphocyte counts and C-reactive protein, as well as more systemic symptoms.
There were no differences in respiratory rate, need for oxygen, or prevalence of chest infiltrates.
The cumulative incidence of mortality at day 28 was 25.2% in HIV-positive patients compared with 32.1% in HIV-negative patients (P = .12).
But when the researchers looked more closely, they noticed that the mortality rate was actually higher in younger HIV+ patients compared with HIV-negative patients.
Stratified by age, 28-day mortality was significantly higher in HIV+ patients aged <50 years (P =.004); and those aged 50 to 59 years (P = .05).
“So below the age of 70, the risk of mortality was double in people with HIV. The people with HIV who died often had diabetes with complications and also more frequent obesity, but this was not the only explanation,” Dr. Geretti said. “There is something to do with the HIV status per se.”
Next steps will be to expand the data set and repeat the analysis with an additional 100 patients “at least” she said.
The researchers also hope to zero in on what about being HIV+ is increasing the mortality risk from COVID-19.
“Right now we need greater numbers and we hope that the research community will be stimulated to take a closer look at this information, and merge other data so that we can strengthen confidence in the data and tease out what factors are causing this increased risk for mortality,” Dr. Geretti said.
She also emphasized that all patients admitted to hospital with COVID-19 should be asked about their HIV status.
“It is important that the HIV status be recorded if we want to increase our ability to understand how HIV impacts survival,” she stressed. “In our experience we found that most of the hospital records were not doing that. Since HIV+ patients seem to be at increased risk, HIV status should be factored into the clinical management. Ask patients if they are HIV+, and if it is not known, then do a test. That would be good practice.”
Dr. Geretti reported no relevant financial relationships. The work was supported by grants from the National Institute of Health Research, the Medical Research Council, the Wellcome Trust, the Department for International Development, and the Bill and Melinda Gates Foundation.
A version of this article originally appeared on Medscape.com.
Switch to integrase inhibitor regimen safe and effective
data from a randomized trial indicate.
Among 212 women with successful HIV virologic suppression following 48 weeks of treatment with ritonavir-boosted atazanavir plus tenofovir disoproxil fumarate (ATV/r +TDF), among those who were switched to continued therapy with an integrase inhibitor–based regimen of elvitegravir/cobicistat/emtricitabine and tenofovir alafenamide (E/C/F/TAF), mean increases in lumbar spine bone mineral density (BMD) were greater and renal function was improved compared with patients who were maintained with ATV/r + TDF, reported Monica Thormann, MD, from Salvador B. Gautier Hospital in Santo Domingo, Dominican Republic, and colleagues at the HIV Glasgow drug therapy meeting, which was held online in 2020.
Although the E/C/F/TAF regimen was associated with a significantly greater increase in lipids, there was no significant change in the total cholesterol to high-density lipoprotein (HDL) cholesterol ratio.
The patients in the study had previously participated in a blinded randomized trial comparing the integrase inhibitor combination plus TDF with ATV/r + TDF in treatment-naive women.
In the current study, patients were randomly assigned in a 3:1 ratio to maintenance with either E/C/F/TAF (159 patients) or ATV/r + TDF (53 patients).
Forty-eight weeks after the switch, virologic suppression (to fewer than 50 copies/mL) was maintained among 94.3% of those on the integrase inhibitor–based regimen, compared with 86.8% of those on the protease inhibitor–based regimen. Virologic failure was seen in 1.9% of those on the integrase inhibitor–based regimen and in 3.8% of those on the protease inhibitor–based regimen.
In addition, virologic suppression below 20 c/mL at week 48 was more common among women maintained on E/C/F/TAF, at 84.9% vs 71.7% (P = .041). No treatment-emergent resistance was seen with either regimen.
As noted, there were higher mean percentage increases in BMD in the E/C/F/TAF group for both total hip and lumbar spine, but only the latter measure improved significantly in comparison with patients treated with ATV/r + TDF (2.82% vs 0%, P < .001).
Markers of renal tubule damage, including the beta-2 microglobulin to creatinine ratio and the rentinol-binding protein to creatinine ratio, were significantly improved with the integrase inhibitor regimen.
Increases in total cholesterol, LDL cholesterol, and HDL cholesterol were 27 vs 5 mg/dL, 16 vs 8 mg/dL, and 5 vs 0 mg/dL in each case comparing the integrase inhibitor–based regimen to the protease inhibitor–based regimen. All of those comparisons were statistically significant.
As noted, however, the total cholesterol to HDL cholesterol ratio was not significantly different between the treatment arms. The rate or initiation of lipid-modifying agents was 1.3% in the E/C/F/TAF group vs 0 in the ATV/r + TDF group, but this difference was not statistically significant.
“These data demonstrate that women who switch to an integrase inhibitor + TAF‐based regimen maintain high levels of virologic suppression with improvement in BMD and renal function biomarkers, as compared with those remaining on their ritonavir boosted atazanavir + TDF‐based regimen,” the authors wrote.
This article first appeared on Medscape.com.
data from a randomized trial indicate.
Among 212 women with successful HIV virologic suppression following 48 weeks of treatment with ritonavir-boosted atazanavir plus tenofovir disoproxil fumarate (ATV/r +TDF), among those who were switched to continued therapy with an integrase inhibitor–based regimen of elvitegravir/cobicistat/emtricitabine and tenofovir alafenamide (E/C/F/TAF), mean increases in lumbar spine bone mineral density (BMD) were greater and renal function was improved compared with patients who were maintained with ATV/r + TDF, reported Monica Thormann, MD, from Salvador B. Gautier Hospital in Santo Domingo, Dominican Republic, and colleagues at the HIV Glasgow drug therapy meeting, which was held online in 2020.
Although the E/C/F/TAF regimen was associated with a significantly greater increase in lipids, there was no significant change in the total cholesterol to high-density lipoprotein (HDL) cholesterol ratio.
The patients in the study had previously participated in a blinded randomized trial comparing the integrase inhibitor combination plus TDF with ATV/r + TDF in treatment-naive women.
In the current study, patients were randomly assigned in a 3:1 ratio to maintenance with either E/C/F/TAF (159 patients) or ATV/r + TDF (53 patients).
Forty-eight weeks after the switch, virologic suppression (to fewer than 50 copies/mL) was maintained among 94.3% of those on the integrase inhibitor–based regimen, compared with 86.8% of those on the protease inhibitor–based regimen. Virologic failure was seen in 1.9% of those on the integrase inhibitor–based regimen and in 3.8% of those on the protease inhibitor–based regimen.
In addition, virologic suppression below 20 c/mL at week 48 was more common among women maintained on E/C/F/TAF, at 84.9% vs 71.7% (P = .041). No treatment-emergent resistance was seen with either regimen.
As noted, there were higher mean percentage increases in BMD in the E/C/F/TAF group for both total hip and lumbar spine, but only the latter measure improved significantly in comparison with patients treated with ATV/r + TDF (2.82% vs 0%, P < .001).
Markers of renal tubule damage, including the beta-2 microglobulin to creatinine ratio and the rentinol-binding protein to creatinine ratio, were significantly improved with the integrase inhibitor regimen.
Increases in total cholesterol, LDL cholesterol, and HDL cholesterol were 27 vs 5 mg/dL, 16 vs 8 mg/dL, and 5 vs 0 mg/dL in each case comparing the integrase inhibitor–based regimen to the protease inhibitor–based regimen. All of those comparisons were statistically significant.
As noted, however, the total cholesterol to HDL cholesterol ratio was not significantly different between the treatment arms. The rate or initiation of lipid-modifying agents was 1.3% in the E/C/F/TAF group vs 0 in the ATV/r + TDF group, but this difference was not statistically significant.
“These data demonstrate that women who switch to an integrase inhibitor + TAF‐based regimen maintain high levels of virologic suppression with improvement in BMD and renal function biomarkers, as compared with those remaining on their ritonavir boosted atazanavir + TDF‐based regimen,” the authors wrote.
This article first appeared on Medscape.com.
data from a randomized trial indicate.
Among 212 women with successful HIV virologic suppression following 48 weeks of treatment with ritonavir-boosted atazanavir plus tenofovir disoproxil fumarate (ATV/r +TDF), among those who were switched to continued therapy with an integrase inhibitor–based regimen of elvitegravir/cobicistat/emtricitabine and tenofovir alafenamide (E/C/F/TAF), mean increases in lumbar spine bone mineral density (BMD) were greater and renal function was improved compared with patients who were maintained with ATV/r + TDF, reported Monica Thormann, MD, from Salvador B. Gautier Hospital in Santo Domingo, Dominican Republic, and colleagues at the HIV Glasgow drug therapy meeting, which was held online in 2020.
Although the E/C/F/TAF regimen was associated with a significantly greater increase in lipids, there was no significant change in the total cholesterol to high-density lipoprotein (HDL) cholesterol ratio.
The patients in the study had previously participated in a blinded randomized trial comparing the integrase inhibitor combination plus TDF with ATV/r + TDF in treatment-naive women.
In the current study, patients were randomly assigned in a 3:1 ratio to maintenance with either E/C/F/TAF (159 patients) or ATV/r + TDF (53 patients).
Forty-eight weeks after the switch, virologic suppression (to fewer than 50 copies/mL) was maintained among 94.3% of those on the integrase inhibitor–based regimen, compared with 86.8% of those on the protease inhibitor–based regimen. Virologic failure was seen in 1.9% of those on the integrase inhibitor–based regimen and in 3.8% of those on the protease inhibitor–based regimen.
In addition, virologic suppression below 20 c/mL at week 48 was more common among women maintained on E/C/F/TAF, at 84.9% vs 71.7% (P = .041). No treatment-emergent resistance was seen with either regimen.
As noted, there were higher mean percentage increases in BMD in the E/C/F/TAF group for both total hip and lumbar spine, but only the latter measure improved significantly in comparison with patients treated with ATV/r + TDF (2.82% vs 0%, P < .001).
Markers of renal tubule damage, including the beta-2 microglobulin to creatinine ratio and the rentinol-binding protein to creatinine ratio, were significantly improved with the integrase inhibitor regimen.
Increases in total cholesterol, LDL cholesterol, and HDL cholesterol were 27 vs 5 mg/dL, 16 vs 8 mg/dL, and 5 vs 0 mg/dL in each case comparing the integrase inhibitor–based regimen to the protease inhibitor–based regimen. All of those comparisons were statistically significant.
As noted, however, the total cholesterol to HDL cholesterol ratio was not significantly different between the treatment arms. The rate or initiation of lipid-modifying agents was 1.3% in the E/C/F/TAF group vs 0 in the ATV/r + TDF group, but this difference was not statistically significant.
“These data demonstrate that women who switch to an integrase inhibitor + TAF‐based regimen maintain high levels of virologic suppression with improvement in BMD and renal function biomarkers, as compared with those remaining on their ritonavir boosted atazanavir + TDF‐based regimen,” the authors wrote.
This article first appeared on Medscape.com.
Islatravir + doravirine maintains HIV viral suppression
according to new data.
ISL is a first-in-class nucleoside reverse transcriptase translocation inhibitor (NRTTI), Jean-Michel Molina, MD, PhD, of Saint‐Louis and Lariboisière Hospitals in Paris, explained at the annual HIV drug therapy meeting in Glasgow, Scotland. The randomized, double-blind, dose‐ranging trial compared ISL+DOR to a fixed‐dose combination of DOR, lamivudine, and tenofovir disoproxil fumarate (DOR/3TC/TDF) daily in 121 patients.
Patients in the ISL+DOR group initially received 0.25, 0.75, or 2.25 mg of ISL along with 100 mg of DOR and 200 mg of 3TC. Beginning at week 20, participants achieving HIV viral loads of 50 copies/mL or less discontinued 3TC but continued on their assigned dose of ISL+DOR for at least 24 weeks. At that point the investigators noted a greater number of discontinuations in the 2.25-mg group and settled on the 0.75-mg ISL dose. All patients in the ISL group were transitioned to that dose between weeks 60 and 72.
At week 96, 81.1% of the patients in the combined ISL group maintained viral loads <50 copies/mL, comparable to the 80.6% of those in the DOR/3TC/TDF group.
ISL+DOR appeared to be “well tolerated,” the investigators noted. They found drug-related adverse events in 7.8% of the patients in the ISL+DOR group compared with 22.6% of patients in the DOR/3TC/TDF group. In addition, among the 90 patients in the ISL+DOR group, no more than 5% of participants experienced any specific drug-related adverse event.
Source: HIV Glasgow 2020 Virtual Conference: Abstract O415. Oct. 5-8, 2020.
A version of this article originally appeared on Medscape.com.
according to new data.
ISL is a first-in-class nucleoside reverse transcriptase translocation inhibitor (NRTTI), Jean-Michel Molina, MD, PhD, of Saint‐Louis and Lariboisière Hospitals in Paris, explained at the annual HIV drug therapy meeting in Glasgow, Scotland. The randomized, double-blind, dose‐ranging trial compared ISL+DOR to a fixed‐dose combination of DOR, lamivudine, and tenofovir disoproxil fumarate (DOR/3TC/TDF) daily in 121 patients.
Patients in the ISL+DOR group initially received 0.25, 0.75, or 2.25 mg of ISL along with 100 mg of DOR and 200 mg of 3TC. Beginning at week 20, participants achieving HIV viral loads of 50 copies/mL or less discontinued 3TC but continued on their assigned dose of ISL+DOR for at least 24 weeks. At that point the investigators noted a greater number of discontinuations in the 2.25-mg group and settled on the 0.75-mg ISL dose. All patients in the ISL group were transitioned to that dose between weeks 60 and 72.
At week 96, 81.1% of the patients in the combined ISL group maintained viral loads <50 copies/mL, comparable to the 80.6% of those in the DOR/3TC/TDF group.
ISL+DOR appeared to be “well tolerated,” the investigators noted. They found drug-related adverse events in 7.8% of the patients in the ISL+DOR group compared with 22.6% of patients in the DOR/3TC/TDF group. In addition, among the 90 patients in the ISL+DOR group, no more than 5% of participants experienced any specific drug-related adverse event.
Source: HIV Glasgow 2020 Virtual Conference: Abstract O415. Oct. 5-8, 2020.
A version of this article originally appeared on Medscape.com.
according to new data.
ISL is a first-in-class nucleoside reverse transcriptase translocation inhibitor (NRTTI), Jean-Michel Molina, MD, PhD, of Saint‐Louis and Lariboisière Hospitals in Paris, explained at the annual HIV drug therapy meeting in Glasgow, Scotland. The randomized, double-blind, dose‐ranging trial compared ISL+DOR to a fixed‐dose combination of DOR, lamivudine, and tenofovir disoproxil fumarate (DOR/3TC/TDF) daily in 121 patients.
Patients in the ISL+DOR group initially received 0.25, 0.75, or 2.25 mg of ISL along with 100 mg of DOR and 200 mg of 3TC. Beginning at week 20, participants achieving HIV viral loads of 50 copies/mL or less discontinued 3TC but continued on their assigned dose of ISL+DOR for at least 24 weeks. At that point the investigators noted a greater number of discontinuations in the 2.25-mg group and settled on the 0.75-mg ISL dose. All patients in the ISL group were transitioned to that dose between weeks 60 and 72.
At week 96, 81.1% of the patients in the combined ISL group maintained viral loads <50 copies/mL, comparable to the 80.6% of those in the DOR/3TC/TDF group.
ISL+DOR appeared to be “well tolerated,” the investigators noted. They found drug-related adverse events in 7.8% of the patients in the ISL+DOR group compared with 22.6% of patients in the DOR/3TC/TDF group. In addition, among the 90 patients in the ISL+DOR group, no more than 5% of participants experienced any specific drug-related adverse event.
Source: HIV Glasgow 2020 Virtual Conference: Abstract O415. Oct. 5-8, 2020.
A version of this article originally appeared on Medscape.com.
C. difficile linked to surgery risk in pediatric Crohn’s
In pediatric Crohn’s disease, a Clostridioides difficile infection detected within the first year after diagnosis is associated with a shorter time to first bowel resection surgery, according to a study that included both a retrospective and prospective analysis. The researchers also found evidence that changes in methionine biosynthesis and depletion of beneficial bacteria may contribute to risk of surgery.
C. difficile infection (CDI) disproportionately affects individuals with inflammatory bowel disease (IBD). Pediatric IBD patients have a 34% risk of recurrent CDI infection, compared with 7.5% in the general population. Previous research found that adults with ulcerative colitis and CDI are at more risk of colectomy, but the finding has not been replicated in children.
In a study published in Inflammatory Bowel Diseases, researchers led by Jennifer Hellmann and Lee Denson of the University of Cincinnati conducted a single-center retrospective analysis of 75 pediatric Crohn’s disease patients. They also conducted a prospective study of 70 pediatric Crohn’s disease patients, using shotgun metagenome sequencing to examine the relationship between microbiota composition and C. difficile carriage or surgery history.
Nineteen percent of patients tested positive for C. difficile. Use of antibiotics was associated with C. difficile (odds ratio, 7.9; P = .02). Of patients who underwent C. difficile testing in the first year, 23 went on to have surgery: 21% who were C. difficile negative required surgery, compared with 67% of those who were positive (hazard ratio, 4.4; P = .0003). The mean time to surgery was 527 days for C. difficile–positive patients and 1,268 days for those who were negative.
A multivariate regression analysis on 54 patients with complete data sets showed that the presence of C. difficile was associated with increased risk of surgery (OR, 16.2; P = .0006). When the analysis was run on all 73 patients, using null value for missing data, the results were similar (OR, 9.17; P = .008).
Shotgun sequencing found that 47 of 114 bacterial species that were associated with the presence of C. difficile were also associated with prior surgery for Crohn’s disease. Species included some that may play a role in mucosal homeostasis, such as Bifidobacterium breve and several Alistipes and Ruminococcus species. That suggests that a reduction in the numbers of these taxa may be associated with C. difficile presence and surgical risk.
The researchers also found that methionine synthesis pathways were depressed in C. difficile–positive and surgery patients. Methionine may bolster antioxidant capacity and improve villus morphology. IBD patients with dysbiosis and those experiencing Crohn’s disease exacerbations have been shown to have decreased methionine pathway activity, suggesting methionine biosynthesis changes have clinical relevance.
The study was funded by the National Institutes of Health.
SOURCE: Hellmann J et al. Inflamm Bowel Dis. 2020. doi: 10.1093/ibd/izz263.
In pediatric Crohn’s disease, a Clostridioides difficile infection detected within the first year after diagnosis is associated with a shorter time to first bowel resection surgery, according to a study that included both a retrospective and prospective analysis. The researchers also found evidence that changes in methionine biosynthesis and depletion of beneficial bacteria may contribute to risk of surgery.
C. difficile infection (CDI) disproportionately affects individuals with inflammatory bowel disease (IBD). Pediatric IBD patients have a 34% risk of recurrent CDI infection, compared with 7.5% in the general population. Previous research found that adults with ulcerative colitis and CDI are at more risk of colectomy, but the finding has not been replicated in children.
In a study published in Inflammatory Bowel Diseases, researchers led by Jennifer Hellmann and Lee Denson of the University of Cincinnati conducted a single-center retrospective analysis of 75 pediatric Crohn’s disease patients. They also conducted a prospective study of 70 pediatric Crohn’s disease patients, using shotgun metagenome sequencing to examine the relationship between microbiota composition and C. difficile carriage or surgery history.
Nineteen percent of patients tested positive for C. difficile. Use of antibiotics was associated with C. difficile (odds ratio, 7.9; P = .02). Of patients who underwent C. difficile testing in the first year, 23 went on to have surgery: 21% who were C. difficile negative required surgery, compared with 67% of those who were positive (hazard ratio, 4.4; P = .0003). The mean time to surgery was 527 days for C. difficile–positive patients and 1,268 days for those who were negative.
A multivariate regression analysis on 54 patients with complete data sets showed that the presence of C. difficile was associated with increased risk of surgery (OR, 16.2; P = .0006). When the analysis was run on all 73 patients, using null value for missing data, the results were similar (OR, 9.17; P = .008).
Shotgun sequencing found that 47 of 114 bacterial species that were associated with the presence of C. difficile were also associated with prior surgery for Crohn’s disease. Species included some that may play a role in mucosal homeostasis, such as Bifidobacterium breve and several Alistipes and Ruminococcus species. That suggests that a reduction in the numbers of these taxa may be associated with C. difficile presence and surgical risk.
The researchers also found that methionine synthesis pathways were depressed in C. difficile–positive and surgery patients. Methionine may bolster antioxidant capacity and improve villus morphology. IBD patients with dysbiosis and those experiencing Crohn’s disease exacerbations have been shown to have decreased methionine pathway activity, suggesting methionine biosynthesis changes have clinical relevance.
The study was funded by the National Institutes of Health.
SOURCE: Hellmann J et al. Inflamm Bowel Dis. 2020. doi: 10.1093/ibd/izz263.
In pediatric Crohn’s disease, a Clostridioides difficile infection detected within the first year after diagnosis is associated with a shorter time to first bowel resection surgery, according to a study that included both a retrospective and prospective analysis. The researchers also found evidence that changes in methionine biosynthesis and depletion of beneficial bacteria may contribute to risk of surgery.
C. difficile infection (CDI) disproportionately affects individuals with inflammatory bowel disease (IBD). Pediatric IBD patients have a 34% risk of recurrent CDI infection, compared with 7.5% in the general population. Previous research found that adults with ulcerative colitis and CDI are at more risk of colectomy, but the finding has not been replicated in children.
In a study published in Inflammatory Bowel Diseases, researchers led by Jennifer Hellmann and Lee Denson of the University of Cincinnati conducted a single-center retrospective analysis of 75 pediatric Crohn’s disease patients. They also conducted a prospective study of 70 pediatric Crohn’s disease patients, using shotgun metagenome sequencing to examine the relationship between microbiota composition and C. difficile carriage or surgery history.
Nineteen percent of patients tested positive for C. difficile. Use of antibiotics was associated with C. difficile (odds ratio, 7.9; P = .02). Of patients who underwent C. difficile testing in the first year, 23 went on to have surgery: 21% who were C. difficile negative required surgery, compared with 67% of those who were positive (hazard ratio, 4.4; P = .0003). The mean time to surgery was 527 days for C. difficile–positive patients and 1,268 days for those who were negative.
A multivariate regression analysis on 54 patients with complete data sets showed that the presence of C. difficile was associated with increased risk of surgery (OR, 16.2; P = .0006). When the analysis was run on all 73 patients, using null value for missing data, the results were similar (OR, 9.17; P = .008).
Shotgun sequencing found that 47 of 114 bacterial species that were associated with the presence of C. difficile were also associated with prior surgery for Crohn’s disease. Species included some that may play a role in mucosal homeostasis, such as Bifidobacterium breve and several Alistipes and Ruminococcus species. That suggests that a reduction in the numbers of these taxa may be associated with C. difficile presence and surgical risk.
The researchers also found that methionine synthesis pathways were depressed in C. difficile–positive and surgery patients. Methionine may bolster antioxidant capacity and improve villus morphology. IBD patients with dysbiosis and those experiencing Crohn’s disease exacerbations have been shown to have decreased methionine pathway activity, suggesting methionine biosynthesis changes have clinical relevance.
The study was funded by the National Institutes of Health.
SOURCE: Hellmann J et al. Inflamm Bowel Dis. 2020. doi: 10.1093/ibd/izz263.
Fecal transplant linked to reduced C. difficile mortality
Vancomycin followed by fecal microbiota transplant (FMT) was associated with reduced Clostridioides difficile (C. diff)-related mortality in patients hospitalized with refractory severe or fulminant C. diff infection (CDI) at a single center. The improvements came after Indiana University implemented an FMT option in 2013.
About 8% of C. diff patients develop severe or fulminant CDI (SFCDI), which can lead to toxic colon and multiorgan failure. Surgery is the current recommended treatment for these patients if they are refractory to vancomycin, but 30-day mortality is above 40%. FMT is recommended for recurrent CDI, and it achieves cure rates greater than 80%, along with fewer relapses compared with anti-CDI antibiotic therapy.
FMT has been shown to be effective for SFCDI, with a 91% cure rate for serious CDI and 66% for fulminant CDI.
In the study published in the September issue of Clinical Gastroenterology and Hepatology, researchers led by Yao-Wen Cheng, MD, and Monika Fischer, MD, of Indiana University, assessed the effect of FMT on SFCDI after their institution adopted it as a treatment protocol for SFCDI. Patients could receive FMT if there was evidence that their SFCDI was refractory, or if they had two or more CDI recurrences. The treatment includes oral vancomycin and pseudomembrane-driven sequential FMT.
Two hundred five patients were admitted before FMT implementation, 225 after. Fifty patients received FMT because of refractory SFCDI. A median of two FMTs was conducted per patient. 21 other patients received FMT for nonrefractory SFCDI or other conditions, including 18 patients with multiple recurrent CDI.
Thirty-day CDI-related mortality dropped after FMT implementation (4.4% versus 10.2%; P =.02). This was true in both the fulminant subset (9.1% versus 21.3%; P =.015) and the refractory group (12.1% versus 43.2%; P < .001).
The researchers used segmented logistic regression to determine if the improved outcomes could be due to nontreatment factors that varied over time, and found that the difference in CDI-related mortality was eliminated except for refractory SFCDI patients (odds of mortality after FMT implementation, 0.09; P =.023). There was no significant difference between those receiving non-CDI antibiotics (4.8%) and those who did not (6.9%; P =.75).
FMT was associated with lower frequency of CDI-related colectomy overall (2.7% versus 6.8%; P =.041), as well as in the fulminant (5.5% versus 15.7%; P =.017) and refractory subgroups (7.6% versus 31.8%; P =.001).
The findings follow another study that showed improved 3-month mortality for FMT among patients hospitalized with severe CDI (12.1% versus 42.2%; P < .003).
The results underscore the utility of FMT for SFCDI, and suggest it might have the most benefit in refractory SFCDI. The authors believe that FMT should be an alternative to colectomy when first-line anti-CDI antibiotics are partially or completely ineffective. In the absence of FMT, patients who go on to fail vancomycin or fidaxomicin will likely continue to be managed medically, with up to 80% mortality, or through salvage colectomy, with postsurgical morality rates of 30-40%.
Although a randomized trial could answer the question of FMT efficacy more definitively, it is unlikely to be conducted for ethical reasons.
“Further investigation is required to clearly define FMT’s role and timing in the clinical course of severe and fulminant CDI. However, our study suggests that FMT should be offered to patients with severe and fulminant CDI who do not respond to a 5-day course of anti-CDI antibiotics and may be considered in lieu of or before colectomy,” the researchers wrote.
No source of funding was disclosed.
SOURCE: Cheng YW et al. Clin Gastroenterol Hepatol. 2020;18:2234-43. doi: 10.1016/j.cgh.2019.12.029.
Vancomycin followed by fecal microbiota transplant (FMT) was associated with reduced Clostridioides difficile (C. diff)-related mortality in patients hospitalized with refractory severe or fulminant C. diff infection (CDI) at a single center. The improvements came after Indiana University implemented an FMT option in 2013.
About 8% of C. diff patients develop severe or fulminant CDI (SFCDI), which can lead to toxic colon and multiorgan failure. Surgery is the current recommended treatment for these patients if they are refractory to vancomycin, but 30-day mortality is above 40%. FMT is recommended for recurrent CDI, and it achieves cure rates greater than 80%, along with fewer relapses compared with anti-CDI antibiotic therapy.
FMT has been shown to be effective for SFCDI, with a 91% cure rate for serious CDI and 66% for fulminant CDI.
In the study published in the September issue of Clinical Gastroenterology and Hepatology, researchers led by Yao-Wen Cheng, MD, and Monika Fischer, MD, of Indiana University, assessed the effect of FMT on SFCDI after their institution adopted it as a treatment protocol for SFCDI. Patients could receive FMT if there was evidence that their SFCDI was refractory, or if they had two or more CDI recurrences. The treatment includes oral vancomycin and pseudomembrane-driven sequential FMT.
Two hundred five patients were admitted before FMT implementation, 225 after. Fifty patients received FMT because of refractory SFCDI. A median of two FMTs was conducted per patient. 21 other patients received FMT for nonrefractory SFCDI or other conditions, including 18 patients with multiple recurrent CDI.
Thirty-day CDI-related mortality dropped after FMT implementation (4.4% versus 10.2%; P =.02). This was true in both the fulminant subset (9.1% versus 21.3%; P =.015) and the refractory group (12.1% versus 43.2%; P < .001).
The researchers used segmented logistic regression to determine if the improved outcomes could be due to nontreatment factors that varied over time, and found that the difference in CDI-related mortality was eliminated except for refractory SFCDI patients (odds of mortality after FMT implementation, 0.09; P =.023). There was no significant difference between those receiving non-CDI antibiotics (4.8%) and those who did not (6.9%; P =.75).
FMT was associated with lower frequency of CDI-related colectomy overall (2.7% versus 6.8%; P =.041), as well as in the fulminant (5.5% versus 15.7%; P =.017) and refractory subgroups (7.6% versus 31.8%; P =.001).
The findings follow another study that showed improved 3-month mortality for FMT among patients hospitalized with severe CDI (12.1% versus 42.2%; P < .003).
The results underscore the utility of FMT for SFCDI, and suggest it might have the most benefit in refractory SFCDI. The authors believe that FMT should be an alternative to colectomy when first-line anti-CDI antibiotics are partially or completely ineffective. In the absence of FMT, patients who go on to fail vancomycin or fidaxomicin will likely continue to be managed medically, with up to 80% mortality, or through salvage colectomy, with postsurgical morality rates of 30-40%.
Although a randomized trial could answer the question of FMT efficacy more definitively, it is unlikely to be conducted for ethical reasons.
“Further investigation is required to clearly define FMT’s role and timing in the clinical course of severe and fulminant CDI. However, our study suggests that FMT should be offered to patients with severe and fulminant CDI who do not respond to a 5-day course of anti-CDI antibiotics and may be considered in lieu of or before colectomy,” the researchers wrote.
No source of funding was disclosed.
SOURCE: Cheng YW et al. Clin Gastroenterol Hepatol. 2020;18:2234-43. doi: 10.1016/j.cgh.2019.12.029.
Vancomycin followed by fecal microbiota transplant (FMT) was associated with reduced Clostridioides difficile (C. diff)-related mortality in patients hospitalized with refractory severe or fulminant C. diff infection (CDI) at a single center. The improvements came after Indiana University implemented an FMT option in 2013.
About 8% of C. diff patients develop severe or fulminant CDI (SFCDI), which can lead to toxic colon and multiorgan failure. Surgery is the current recommended treatment for these patients if they are refractory to vancomycin, but 30-day mortality is above 40%. FMT is recommended for recurrent CDI, and it achieves cure rates greater than 80%, along with fewer relapses compared with anti-CDI antibiotic therapy.
FMT has been shown to be effective for SFCDI, with a 91% cure rate for serious CDI and 66% for fulminant CDI.
In the study published in the September issue of Clinical Gastroenterology and Hepatology, researchers led by Yao-Wen Cheng, MD, and Monika Fischer, MD, of Indiana University, assessed the effect of FMT on SFCDI after their institution adopted it as a treatment protocol for SFCDI. Patients could receive FMT if there was evidence that their SFCDI was refractory, or if they had two or more CDI recurrences. The treatment includes oral vancomycin and pseudomembrane-driven sequential FMT.
Two hundred five patients were admitted before FMT implementation, 225 after. Fifty patients received FMT because of refractory SFCDI. A median of two FMTs was conducted per patient. 21 other patients received FMT for nonrefractory SFCDI or other conditions, including 18 patients with multiple recurrent CDI.
Thirty-day CDI-related mortality dropped after FMT implementation (4.4% versus 10.2%; P =.02). This was true in both the fulminant subset (9.1% versus 21.3%; P =.015) and the refractory group (12.1% versus 43.2%; P < .001).
The researchers used segmented logistic regression to determine if the improved outcomes could be due to nontreatment factors that varied over time, and found that the difference in CDI-related mortality was eliminated except for refractory SFCDI patients (odds of mortality after FMT implementation, 0.09; P =.023). There was no significant difference between those receiving non-CDI antibiotics (4.8%) and those who did not (6.9%; P =.75).
FMT was associated with lower frequency of CDI-related colectomy overall (2.7% versus 6.8%; P =.041), as well as in the fulminant (5.5% versus 15.7%; P =.017) and refractory subgroups (7.6% versus 31.8%; P =.001).
The findings follow another study that showed improved 3-month mortality for FMT among patients hospitalized with severe CDI (12.1% versus 42.2%; P < .003).
The results underscore the utility of FMT for SFCDI, and suggest it might have the most benefit in refractory SFCDI. The authors believe that FMT should be an alternative to colectomy when first-line anti-CDI antibiotics are partially or completely ineffective. In the absence of FMT, patients who go on to fail vancomycin or fidaxomicin will likely continue to be managed medically, with up to 80% mortality, or through salvage colectomy, with postsurgical morality rates of 30-40%.
Although a randomized trial could answer the question of FMT efficacy more definitively, it is unlikely to be conducted for ethical reasons.
“Further investigation is required to clearly define FMT’s role and timing in the clinical course of severe and fulminant CDI. However, our study suggests that FMT should be offered to patients with severe and fulminant CDI who do not respond to a 5-day course of anti-CDI antibiotics and may be considered in lieu of or before colectomy,” the researchers wrote.
No source of funding was disclosed.
SOURCE: Cheng YW et al. Clin Gastroenterol Hepatol. 2020;18:2234-43. doi: 10.1016/j.cgh.2019.12.029.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Influenza Vaccination Recommendations During Use of Select Immunosuppressants for Psoriasis
A 42-year-old woman with psoriasis presents for a checkup at the dermatology clinic. Her psoriasis has been fairly stable on methotrexate with no recent flares. She presents her concern of the coronavirus pandemic continuing into the flu season and mentions she would like to minimize her chances of having a respiratory illness. The influenza vaccine has just become available, and she inquires when she can get the vaccine and whether it will interfere with her treatment. What are your recommendations for the patient?
Psoriasis is an immune-mediated, inflammatory skin condition stemming from hyperproliferation of keratinocytes that classically involves erythematous skin plaques with overlying scale. Treatment options vary widely and include topical modalities, phototherapy, immunosuppressants, and biologic agents. Selection of treatment largely depends on the severity and extent of body surface area involvement; systemic therapy generally is indicated when the affected body surface area is greater than 5% to 10%. In patients on systemic therapy, increased susceptibility to infection is a priority concern for prescribing physicians. In the context of continuing immunosuppressive medications, vaccines that reduce susceptibility to infectious diseases can play an important role in reducing morbidity and mortality for these patients; however, an important consideration is that in patients with chronic conditions and frequent hospital visits, vaccines may be administered by various clinicians who may not be familiar with the management of immunosuppressive treatments. It is pivotal for prescribing dermatologists to provide appropriate vaccination instructions for the patient and any future clinicians to ensure vaccine efficacy in these patients.
The intramuscular influenza vaccine is a killed vaccine that is administered annually and has been shown to be safe for use in both immunocompetent and immunocompromised patients.1,2 Despite its safety, questions remain regarding the efficacy of vaccines while a patient is unable to mount a normal immune response and whether the treatment must be altered to maximize immunogenicity. The common systemic treatment options for psoriasis and any recommendations that can be made regarding administration of the influenza vaccine in that context are outlined in the Table. Given the sparsity of clinical data measuring vaccine immunogenicity in patients with psoriasis, vaccine guidelines are drawn from patients with various conditions who are receiving the same dose of medication as indicated for psoriasis.

Immunosuppressants and biologics commonly are used in dermatology for the management of many conditions, including psoriasis. As flu season approaches in the setting of a global pandemic, it is critical to understand the effects of commonly used psoriasis medications on the influenza vaccine. Through a brief review of the latest data concerning their interactions, dermatologists will be able to provide appropriate recommendations that maximize a patient’s immune response to the vaccine while minimizing adverse effects from holding medication.
- Zbinden D, Manuel O. Influenza vaccination in immunocompromised patients: efficacy and safety. Immunotherapy. 2014;6:131-139.
- Milanovic M, Stojanovich L, Djokovic A, et al. Influenza vaccination in autoimmune rheumatic disease patients. Tohoku J Exp Med. 2013;229:29-34.
- Dengler TJ, Strnad N, Bühring I, et al. Differential immune response to influenza and pneumococcal vaccination in immunosuppressed patients after heart transplantation. Transplantation. 1998;66:1340-1347.
- Willcocks LC, Chaudhry AN, Smith JC, et al. The effect of sirolimus therapy on vaccine responses in transplant recipients. Am J Transplant. 2007;7:2006-2011.
- Chioato A, Noseda E, Stevens M, et al. Treatment with the interleukin-17A-blocking antibody secukinumab does not interfere with the efficacy of influenza and meningococcal vaccinations in healthy subjects: results of an open-label, parallel-group, randomized single-center study. Clin Vaccine Immunol. 2012;19:1597-1602.
- Richi P, Martín MD, de Ory F, et al. Secukinumab does not impair the immunogenic response to the influenza vaccine in patients. RMD Open. 2019;5:e001018.
- Furer V, Zisman D, Kaufman I, et al. Immunogenicity and safety of vaccination against seasonal influenza vaccine in patients with psoriatic arthritis treated with secukinumab. Vaccine. 2020;38:847-851.
- Hua C, Barnetche T, Combe B, et al. Effect of methotrexate, anti-tumor necrosis factor α, and rituximab on the immune response to influenza and pneumococcal vaccines in patients with rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res. 2014;66:1016-1026.
- Park JK, Choi Y, Winthrop KL, et al. Optimal time between the last methotrexate administration and seasonal influenza vaccination in rheumatoid arthritis: post hoc analysis of a randomised clinical trial. Ann Rheum Dis. 2019;78:1283-1284.
- Park JK, Lee MA, Lee EY, et al. Effect of methotrexate discontinuation on efficacy of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2017;76:1559-1565.
- Park JK, Lee YJ, Shin K, et al. Impact of temporary methotrexate discontinuation for 2 weeks on immunogenicity of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2018;77:898-904.
- Shirai S, Hara M, Sakata Y, et al. Immunogenicity of quadrivalent influenza vaccine for patients with inflammatory bowel disease undergoing immunosuppressive therapy. Inflamm Bowel Dis. 2018;24:1082-1091.
- Fomin I. Vaccination against influenza in rheumatoid arthritis: the effect of disease modifying drugs, including TNF blockers. Ann Rheum Dis. 2006;65:191-194.
- Bosaeed M, Kumar D. Seasonal influenza vaccine in immunocompromised persons. Hum Vaccin Immunother. 2018;14:1311-1322.
- Kaine JL, Kivitz AJ, Birbara C, et al. Immune responses following administration of influenza and pneumococcal vaccines to patients with rheumatoid arthritis receiving adalimumab. J Rheumatol. 2007;34:272-279.
A 42-year-old woman with psoriasis presents for a checkup at the dermatology clinic. Her psoriasis has been fairly stable on methotrexate with no recent flares. She presents her concern of the coronavirus pandemic continuing into the flu season and mentions she would like to minimize her chances of having a respiratory illness. The influenza vaccine has just become available, and she inquires when she can get the vaccine and whether it will interfere with her treatment. What are your recommendations for the patient?
Psoriasis is an immune-mediated, inflammatory skin condition stemming from hyperproliferation of keratinocytes that classically involves erythematous skin plaques with overlying scale. Treatment options vary widely and include topical modalities, phototherapy, immunosuppressants, and biologic agents. Selection of treatment largely depends on the severity and extent of body surface area involvement; systemic therapy generally is indicated when the affected body surface area is greater than 5% to 10%. In patients on systemic therapy, increased susceptibility to infection is a priority concern for prescribing physicians. In the context of continuing immunosuppressive medications, vaccines that reduce susceptibility to infectious diseases can play an important role in reducing morbidity and mortality for these patients; however, an important consideration is that in patients with chronic conditions and frequent hospital visits, vaccines may be administered by various clinicians who may not be familiar with the management of immunosuppressive treatments. It is pivotal for prescribing dermatologists to provide appropriate vaccination instructions for the patient and any future clinicians to ensure vaccine efficacy in these patients.
The intramuscular influenza vaccine is a killed vaccine that is administered annually and has been shown to be safe for use in both immunocompetent and immunocompromised patients.1,2 Despite its safety, questions remain regarding the efficacy of vaccines while a patient is unable to mount a normal immune response and whether the treatment must be altered to maximize immunogenicity. The common systemic treatment options for psoriasis and any recommendations that can be made regarding administration of the influenza vaccine in that context are outlined in the Table. Given the sparsity of clinical data measuring vaccine immunogenicity in patients with psoriasis, vaccine guidelines are drawn from patients with various conditions who are receiving the same dose of medication as indicated for psoriasis.

Immunosuppressants and biologics commonly are used in dermatology for the management of many conditions, including psoriasis. As flu season approaches in the setting of a global pandemic, it is critical to understand the effects of commonly used psoriasis medications on the influenza vaccine. Through a brief review of the latest data concerning their interactions, dermatologists will be able to provide appropriate recommendations that maximize a patient’s immune response to the vaccine while minimizing adverse effects from holding medication.
A 42-year-old woman with psoriasis presents for a checkup at the dermatology clinic. Her psoriasis has been fairly stable on methotrexate with no recent flares. She presents her concern of the coronavirus pandemic continuing into the flu season and mentions she would like to minimize her chances of having a respiratory illness. The influenza vaccine has just become available, and she inquires when she can get the vaccine and whether it will interfere with her treatment. What are your recommendations for the patient?
Psoriasis is an immune-mediated, inflammatory skin condition stemming from hyperproliferation of keratinocytes that classically involves erythematous skin plaques with overlying scale. Treatment options vary widely and include topical modalities, phototherapy, immunosuppressants, and biologic agents. Selection of treatment largely depends on the severity and extent of body surface area involvement; systemic therapy generally is indicated when the affected body surface area is greater than 5% to 10%. In patients on systemic therapy, increased susceptibility to infection is a priority concern for prescribing physicians. In the context of continuing immunosuppressive medications, vaccines that reduce susceptibility to infectious diseases can play an important role in reducing morbidity and mortality for these patients; however, an important consideration is that in patients with chronic conditions and frequent hospital visits, vaccines may be administered by various clinicians who may not be familiar with the management of immunosuppressive treatments. It is pivotal for prescribing dermatologists to provide appropriate vaccination instructions for the patient and any future clinicians to ensure vaccine efficacy in these patients.
The intramuscular influenza vaccine is a killed vaccine that is administered annually and has been shown to be safe for use in both immunocompetent and immunocompromised patients.1,2 Despite its safety, questions remain regarding the efficacy of vaccines while a patient is unable to mount a normal immune response and whether the treatment must be altered to maximize immunogenicity. The common systemic treatment options for psoriasis and any recommendations that can be made regarding administration of the influenza vaccine in that context are outlined in the Table. Given the sparsity of clinical data measuring vaccine immunogenicity in patients with psoriasis, vaccine guidelines are drawn from patients with various conditions who are receiving the same dose of medication as indicated for psoriasis.

Immunosuppressants and biologics commonly are used in dermatology for the management of many conditions, including psoriasis. As flu season approaches in the setting of a global pandemic, it is critical to understand the effects of commonly used psoriasis medications on the influenza vaccine. Through a brief review of the latest data concerning their interactions, dermatologists will be able to provide appropriate recommendations that maximize a patient’s immune response to the vaccine while minimizing adverse effects from holding medication.
- Zbinden D, Manuel O. Influenza vaccination in immunocompromised patients: efficacy and safety. Immunotherapy. 2014;6:131-139.
- Milanovic M, Stojanovich L, Djokovic A, et al. Influenza vaccination in autoimmune rheumatic disease patients. Tohoku J Exp Med. 2013;229:29-34.
- Dengler TJ, Strnad N, Bühring I, et al. Differential immune response to influenza and pneumococcal vaccination in immunosuppressed patients after heart transplantation. Transplantation. 1998;66:1340-1347.
- Willcocks LC, Chaudhry AN, Smith JC, et al. The effect of sirolimus therapy on vaccine responses in transplant recipients. Am J Transplant. 2007;7:2006-2011.
- Chioato A, Noseda E, Stevens M, et al. Treatment with the interleukin-17A-blocking antibody secukinumab does not interfere with the efficacy of influenza and meningococcal vaccinations in healthy subjects: results of an open-label, parallel-group, randomized single-center study. Clin Vaccine Immunol. 2012;19:1597-1602.
- Richi P, Martín MD, de Ory F, et al. Secukinumab does not impair the immunogenic response to the influenza vaccine in patients. RMD Open. 2019;5:e001018.
- Furer V, Zisman D, Kaufman I, et al. Immunogenicity and safety of vaccination against seasonal influenza vaccine in patients with psoriatic arthritis treated with secukinumab. Vaccine. 2020;38:847-851.
- Hua C, Barnetche T, Combe B, et al. Effect of methotrexate, anti-tumor necrosis factor α, and rituximab on the immune response to influenza and pneumococcal vaccines in patients with rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res. 2014;66:1016-1026.
- Park JK, Choi Y, Winthrop KL, et al. Optimal time between the last methotrexate administration and seasonal influenza vaccination in rheumatoid arthritis: post hoc analysis of a randomised clinical trial. Ann Rheum Dis. 2019;78:1283-1284.
- Park JK, Lee MA, Lee EY, et al. Effect of methotrexate discontinuation on efficacy of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2017;76:1559-1565.
- Park JK, Lee YJ, Shin K, et al. Impact of temporary methotrexate discontinuation for 2 weeks on immunogenicity of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2018;77:898-904.
- Shirai S, Hara M, Sakata Y, et al. Immunogenicity of quadrivalent influenza vaccine for patients with inflammatory bowel disease undergoing immunosuppressive therapy. Inflamm Bowel Dis. 2018;24:1082-1091.
- Fomin I. Vaccination against influenza in rheumatoid arthritis: the effect of disease modifying drugs, including TNF blockers. Ann Rheum Dis. 2006;65:191-194.
- Bosaeed M, Kumar D. Seasonal influenza vaccine in immunocompromised persons. Hum Vaccin Immunother. 2018;14:1311-1322.
- Kaine JL, Kivitz AJ, Birbara C, et al. Immune responses following administration of influenza and pneumococcal vaccines to patients with rheumatoid arthritis receiving adalimumab. J Rheumatol. 2007;34:272-279.
- Zbinden D, Manuel O. Influenza vaccination in immunocompromised patients: efficacy and safety. Immunotherapy. 2014;6:131-139.
- Milanovic M, Stojanovich L, Djokovic A, et al. Influenza vaccination in autoimmune rheumatic disease patients. Tohoku J Exp Med. 2013;229:29-34.
- Dengler TJ, Strnad N, Bühring I, et al. Differential immune response to influenza and pneumococcal vaccination in immunosuppressed patients after heart transplantation. Transplantation. 1998;66:1340-1347.
- Willcocks LC, Chaudhry AN, Smith JC, et al. The effect of sirolimus therapy on vaccine responses in transplant recipients. Am J Transplant. 2007;7:2006-2011.
- Chioato A, Noseda E, Stevens M, et al. Treatment with the interleukin-17A-blocking antibody secukinumab does not interfere with the efficacy of influenza and meningococcal vaccinations in healthy subjects: results of an open-label, parallel-group, randomized single-center study. Clin Vaccine Immunol. 2012;19:1597-1602.
- Richi P, Martín MD, de Ory F, et al. Secukinumab does not impair the immunogenic response to the influenza vaccine in patients. RMD Open. 2019;5:e001018.
- Furer V, Zisman D, Kaufman I, et al. Immunogenicity and safety of vaccination against seasonal influenza vaccine in patients with psoriatic arthritis treated with secukinumab. Vaccine. 2020;38:847-851.
- Hua C, Barnetche T, Combe B, et al. Effect of methotrexate, anti-tumor necrosis factor α, and rituximab on the immune response to influenza and pneumococcal vaccines in patients with rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res. 2014;66:1016-1026.
- Park JK, Choi Y, Winthrop KL, et al. Optimal time between the last methotrexate administration and seasonal influenza vaccination in rheumatoid arthritis: post hoc analysis of a randomised clinical trial. Ann Rheum Dis. 2019;78:1283-1284.
- Park JK, Lee MA, Lee EY, et al. Effect of methotrexate discontinuation on efficacy of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2017;76:1559-1565.
- Park JK, Lee YJ, Shin K, et al. Impact of temporary methotrexate discontinuation for 2 weeks on immunogenicity of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2018;77:898-904.
- Shirai S, Hara M, Sakata Y, et al. Immunogenicity of quadrivalent influenza vaccine for patients with inflammatory bowel disease undergoing immunosuppressive therapy. Inflamm Bowel Dis. 2018;24:1082-1091.
- Fomin I. Vaccination against influenza in rheumatoid arthritis: the effect of disease modifying drugs, including TNF blockers. Ann Rheum Dis. 2006;65:191-194.
- Bosaeed M, Kumar D. Seasonal influenza vaccine in immunocompromised persons. Hum Vaccin Immunother. 2018;14:1311-1322.
- Kaine JL, Kivitz AJ, Birbara C, et al. Immune responses following administration of influenza and pneumococcal vaccines to patients with rheumatoid arthritis receiving adalimumab. J Rheumatol. 2007;34:272-279.
Practice Points
- Patients receiving methotrexate appear to benefit from suspending treatment for 2 weeks following influenza vaccination, as it maximizes the seroprotective response.
- Patients receiving tumor necrosis factor α inhibitors and low-dose IL-17 inhibitors have an unaltered humoral response to vaccination and attain protection equal to that of the general population.
- Patients treated with cyclosporine should be closely monitored for influenza symptoms even after vaccination, as approximately half of patients do not achieve a seroprotective response.
- Consider the increased risk for psoriatic flare during treatment suspension and the possibility of failed seroprotection, warranting close monitoring and clinical judgement tailored to each individual.
What’s in a number? 697,633 children with COVID-19
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
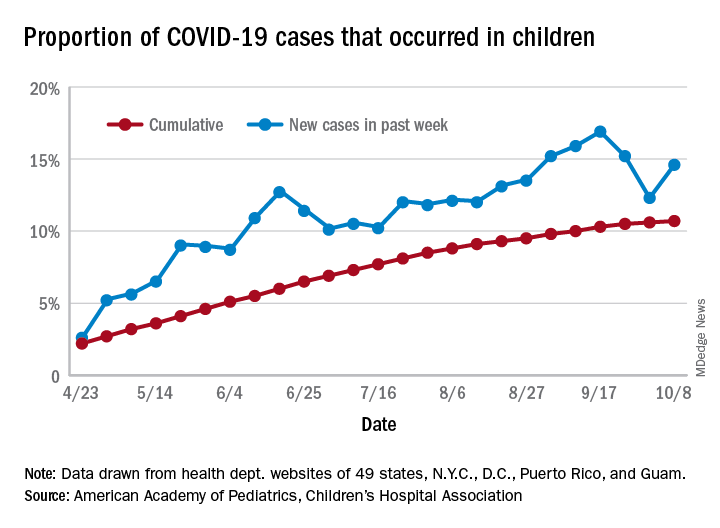
For the week, 14.6% of all COVID-19 cases reported in the United States occurred in children, after 2 consecutive weeks of declines that saw the proportion drop from 16.9% to 12.3%. The cumulative rate of child cases for the entire pandemic is 10.7%, with total child cases in the United States now up to 697,633 and cases among all ages at just over 6.5 million, the AAP and the CHA said Oct. 12 in their weekly COVID-19 report.
Nationally, there were 927 cases reported per 100,000 children as of Oct. 8, with rates at the state level varying from 176 per 100,000 in Vermont to 2,221 per 100,000 in North Dakota. Two other states were over 2,000 cases per 100,000 children: Tennessee (2,155) and South Carolina (2,116), based on data from the health departments of 49 states (New York does not report age distribution), as well as the District of Columbia, New York City, Puerto Rico, and Guam.
Severe illness continues to be rare in children, and national (25 states and New York City) hospitalization rates dropped in the last week. The proportion of hospitalizations occurring in children slipped from a pandemic high of 1.8% the previous week to 1.7% during the week of Oct. 8, and the rate of hospitalizations for children with COVID-19 was down to 1.4% from 1.6% the week before and 1.9% on Sept. 3, the AAP and the CHA said.
Mortality data from 42 states and New York City also show a decline. For the third consecutive week, children represented just 0.06% of all COVID-19 deaths in the United States, down from a high of 0.07% on Sept. 17. Only 0.02% of all cases in children have resulted in death, and that figure has been dropping since early June, when it reached 0.06%, according to the AAP/CHA report. As of Oct. 8, there have been 115 total deaths reported in children.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
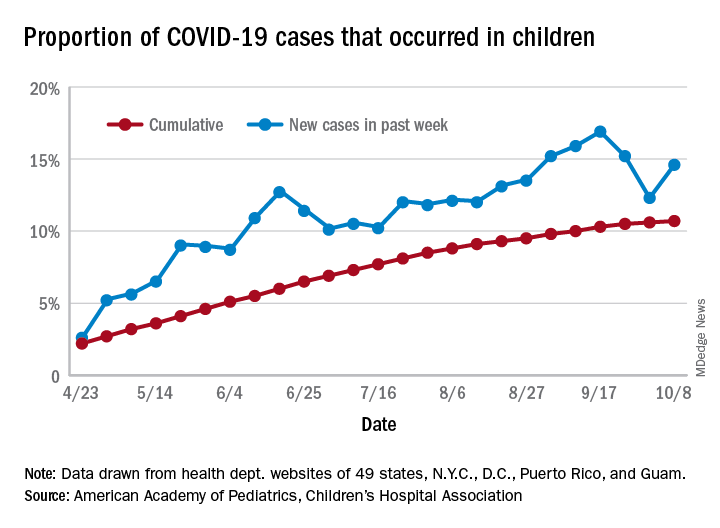
For the week, 14.6% of all COVID-19 cases reported in the United States occurred in children, after 2 consecutive weeks of declines that saw the proportion drop from 16.9% to 12.3%. The cumulative rate of child cases for the entire pandemic is 10.7%, with total child cases in the United States now up to 697,633 and cases among all ages at just over 6.5 million, the AAP and the CHA said Oct. 12 in their weekly COVID-19 report.
Nationally, there were 927 cases reported per 100,000 children as of Oct. 8, with rates at the state level varying from 176 per 100,000 in Vermont to 2,221 per 100,000 in North Dakota. Two other states were over 2,000 cases per 100,000 children: Tennessee (2,155) and South Carolina (2,116), based on data from the health departments of 49 states (New York does not report age distribution), as well as the District of Columbia, New York City, Puerto Rico, and Guam.
Severe illness continues to be rare in children, and national (25 states and New York City) hospitalization rates dropped in the last week. The proportion of hospitalizations occurring in children slipped from a pandemic high of 1.8% the previous week to 1.7% during the week of Oct. 8, and the rate of hospitalizations for children with COVID-19 was down to 1.4% from 1.6% the week before and 1.9% on Sept. 3, the AAP and the CHA said.
Mortality data from 42 states and New York City also show a decline. For the third consecutive week, children represented just 0.06% of all COVID-19 deaths in the United States, down from a high of 0.07% on Sept. 17. Only 0.02% of all cases in children have resulted in death, and that figure has been dropping since early June, when it reached 0.06%, according to the AAP/CHA report. As of Oct. 8, there have been 115 total deaths reported in children.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
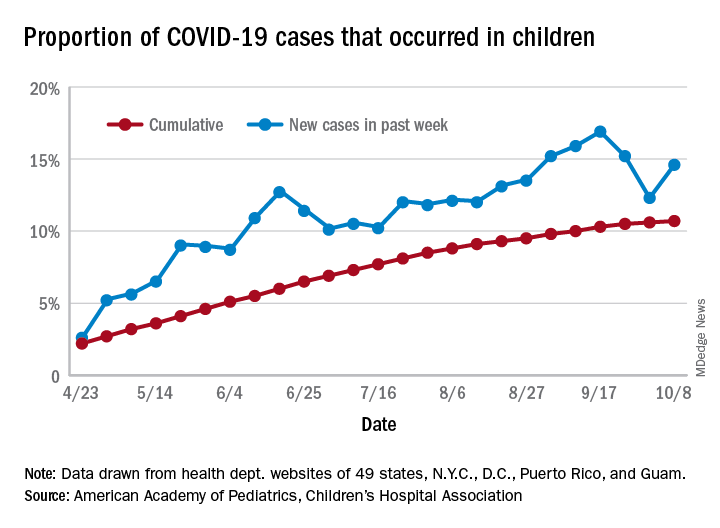
For the week, 14.6% of all COVID-19 cases reported in the United States occurred in children, after 2 consecutive weeks of declines that saw the proportion drop from 16.9% to 12.3%. The cumulative rate of child cases for the entire pandemic is 10.7%, with total child cases in the United States now up to 697,633 and cases among all ages at just over 6.5 million, the AAP and the CHA said Oct. 12 in their weekly COVID-19 report.
Nationally, there were 927 cases reported per 100,000 children as of Oct. 8, with rates at the state level varying from 176 per 100,000 in Vermont to 2,221 per 100,000 in North Dakota. Two other states were over 2,000 cases per 100,000 children: Tennessee (2,155) and South Carolina (2,116), based on data from the health departments of 49 states (New York does not report age distribution), as well as the District of Columbia, New York City, Puerto Rico, and Guam.
Severe illness continues to be rare in children, and national (25 states and New York City) hospitalization rates dropped in the last week. The proportion of hospitalizations occurring in children slipped from a pandemic high of 1.8% the previous week to 1.7% during the week of Oct. 8, and the rate of hospitalizations for children with COVID-19 was down to 1.4% from 1.6% the week before and 1.9% on Sept. 3, the AAP and the CHA said.
Mortality data from 42 states and New York City also show a decline. For the third consecutive week, children represented just 0.06% of all COVID-19 deaths in the United States, down from a high of 0.07% on Sept. 17. Only 0.02% of all cases in children have resulted in death, and that figure has been dropping since early June, when it reached 0.06%, according to the AAP/CHA report. As of Oct. 8, there have been 115 total deaths reported in children.
Flu vaccine significantly cuts pediatric hospitalizations
Unlike previous studies focused on vaccine effectiveness (VE) in ambulatory care office visits, Angela P. Campbell, MD, MPH, and associates have uncovered evidence of the overall benefit influenza vaccines play in reducing hospitalizations and emergency department visits in pediatric influenza patients.
“Our data provide important VE estimates against severe influenza in children,” the researchers noted in Pediatrics, adding that the findings “provide important evidence supporting the annual recommendation that all children 6 months and older should receive influenza vaccination.”
Dr. Campbell and colleagues collected ongoing surveillance data from the New Vaccine Surveillance Network (NVSN), which is a network of pediatric hospitals across seven cities, including Kansas City, Mo.; Rochester, N.Y.; Cincinnati; Pittsburgh; Nashville, Tenn.; Houston; and Seattle. The influenza season encompassed the period Nov. 7, 2018 to June 21, 2019.
A total of 2,748 hospitalized children and 2,676 children who had completed ED visits that did not lead to hospitalization were included. Once those under 6 months were excluded, 1,792 hospitalized children were included in the VE analysis; of these, 226 (13%) tested positive for influenza infection, including 211 (93%) with influenza A viruses and 15 (7%) with influenza B viruses. Fully 1,611 of the patients (90%), had verified vaccine status, while 181 (10%) had solely parental reported vaccine status. The researchers reported 88 (5%) of the patients received mechanical ventilation and 7 (<1%) died.
Most noteworthy, They further estimated a significant reduction in hospitalizations linked to A(H3N2) and A(H1N1)pdm09 viruses, even in the presence of circulating A(H3N2) viruses that differed from the A(H3N2) vaccine component.
Studies from other countries during the same time period showed that while “significant protection against influenza-associated ambulatory care visits and hospitalizations among children infected with A(H1N1)pdm09 viruses” was observed, the same could not be said for protection against A(H3N2) viruses, which varied among pediatric outpatients in the United States (24%), in England (17% outpatient; 31% inpatient), Europe (46%), and Canada (48%). They explained that such variation in vaccine protection is multifactorial, and includes virus-, host-, and environment-related factors. They also noted that regional variations in circulating viruses, host factors including age, imprinting, and previous vaccination could explain the study’s finding of vaccine protection against both A(H1N1)pdm09 and A(H3N2) viruses.
When comparing VE estimates between ED visits and hospitalizations, the researchers observed one significant difference, that “hospitalized children likely represent more medically complex patients, with 58% having underlying medical conditions and 38% reporting at lease one hospitalization in the past year, compared with 28% and 14% respectively, among ED participants.”
Strengths of the study included the prospective multisite enrollment that provided data across diverse locations and representation from pediatric hospitalizations and ED care, which were not previously strongly represented in the literature. The single-season study with small sample size was considered a limitation, as was the inability to evaluate full and partial vaccine status. Vaccine data also were limited for many of the ED patients observed.
Dr. Campbell and colleagues did caution that while they consider their test-negative design optimal for evaluating both hospitalized and ED patients, they feel their results should not be “interpreted as VE against influenza-associated ambulatory care visits or infections that are not medically attended.”
In a separate interview, Michael E. Pichichero, MD, director of the Rochester General Hospital Research Institute and a clinical professor of pediatrics at the University of Rochester (N.Y.), observed: “There are really no surprises here. A well done contemporary study confirms again the benefits of annual influenza vaccinations for children. Viral coinfections involving SARS-CoV-2 and influenza have been reported from Australia to cause heightened illnesses. That observation provides further impetus for parents to have their children receive influenza vaccinations.”
The researchers cited multiple sources of financial support for their ongoing work, including Sanofi, Quidel, Moderna, Karius, GlaxoSmithKline, Merck, AstraZeneca, and Pfizer. Funding for this study was supported by the Centers for Disease Control and Prevention. Dr. Pichichero said he had no relevant financial disclosures.
SOURCE: Campbell AP et al. Pediatrics. 2020. doi: 10.1542/peds.2020-1368.
Unlike previous studies focused on vaccine effectiveness (VE) in ambulatory care office visits, Angela P. Campbell, MD, MPH, and associates have uncovered evidence of the overall benefit influenza vaccines play in reducing hospitalizations and emergency department visits in pediatric influenza patients.
“Our data provide important VE estimates against severe influenza in children,” the researchers noted in Pediatrics, adding that the findings “provide important evidence supporting the annual recommendation that all children 6 months and older should receive influenza vaccination.”
Dr. Campbell and colleagues collected ongoing surveillance data from the New Vaccine Surveillance Network (NVSN), which is a network of pediatric hospitals across seven cities, including Kansas City, Mo.; Rochester, N.Y.; Cincinnati; Pittsburgh; Nashville, Tenn.; Houston; and Seattle. The influenza season encompassed the period Nov. 7, 2018 to June 21, 2019.
A total of 2,748 hospitalized children and 2,676 children who had completed ED visits that did not lead to hospitalization were included. Once those under 6 months were excluded, 1,792 hospitalized children were included in the VE analysis; of these, 226 (13%) tested positive for influenza infection, including 211 (93%) with influenza A viruses and 15 (7%) with influenza B viruses. Fully 1,611 of the patients (90%), had verified vaccine status, while 181 (10%) had solely parental reported vaccine status. The researchers reported 88 (5%) of the patients received mechanical ventilation and 7 (<1%) died.
Most noteworthy, They further estimated a significant reduction in hospitalizations linked to A(H3N2) and A(H1N1)pdm09 viruses, even in the presence of circulating A(H3N2) viruses that differed from the A(H3N2) vaccine component.
Studies from other countries during the same time period showed that while “significant protection against influenza-associated ambulatory care visits and hospitalizations among children infected with A(H1N1)pdm09 viruses” was observed, the same could not be said for protection against A(H3N2) viruses, which varied among pediatric outpatients in the United States (24%), in England (17% outpatient; 31% inpatient), Europe (46%), and Canada (48%). They explained that such variation in vaccine protection is multifactorial, and includes virus-, host-, and environment-related factors. They also noted that regional variations in circulating viruses, host factors including age, imprinting, and previous vaccination could explain the study’s finding of vaccine protection against both A(H1N1)pdm09 and A(H3N2) viruses.
When comparing VE estimates between ED visits and hospitalizations, the researchers observed one significant difference, that “hospitalized children likely represent more medically complex patients, with 58% having underlying medical conditions and 38% reporting at lease one hospitalization in the past year, compared with 28% and 14% respectively, among ED participants.”
Strengths of the study included the prospective multisite enrollment that provided data across diverse locations and representation from pediatric hospitalizations and ED care, which were not previously strongly represented in the literature. The single-season study with small sample size was considered a limitation, as was the inability to evaluate full and partial vaccine status. Vaccine data also were limited for many of the ED patients observed.
Dr. Campbell and colleagues did caution that while they consider their test-negative design optimal for evaluating both hospitalized and ED patients, they feel their results should not be “interpreted as VE against influenza-associated ambulatory care visits or infections that are not medically attended.”
In a separate interview, Michael E. Pichichero, MD, director of the Rochester General Hospital Research Institute and a clinical professor of pediatrics at the University of Rochester (N.Y.), observed: “There are really no surprises here. A well done contemporary study confirms again the benefits of annual influenza vaccinations for children. Viral coinfections involving SARS-CoV-2 and influenza have been reported from Australia to cause heightened illnesses. That observation provides further impetus for parents to have their children receive influenza vaccinations.”
The researchers cited multiple sources of financial support for their ongoing work, including Sanofi, Quidel, Moderna, Karius, GlaxoSmithKline, Merck, AstraZeneca, and Pfizer. Funding for this study was supported by the Centers for Disease Control and Prevention. Dr. Pichichero said he had no relevant financial disclosures.
SOURCE: Campbell AP et al. Pediatrics. 2020. doi: 10.1542/peds.2020-1368.
Unlike previous studies focused on vaccine effectiveness (VE) in ambulatory care office visits, Angela P. Campbell, MD, MPH, and associates have uncovered evidence of the overall benefit influenza vaccines play in reducing hospitalizations and emergency department visits in pediatric influenza patients.
“Our data provide important VE estimates against severe influenza in children,” the researchers noted in Pediatrics, adding that the findings “provide important evidence supporting the annual recommendation that all children 6 months and older should receive influenza vaccination.”
Dr. Campbell and colleagues collected ongoing surveillance data from the New Vaccine Surveillance Network (NVSN), which is a network of pediatric hospitals across seven cities, including Kansas City, Mo.; Rochester, N.Y.; Cincinnati; Pittsburgh; Nashville, Tenn.; Houston; and Seattle. The influenza season encompassed the period Nov. 7, 2018 to June 21, 2019.
A total of 2,748 hospitalized children and 2,676 children who had completed ED visits that did not lead to hospitalization were included. Once those under 6 months were excluded, 1,792 hospitalized children were included in the VE analysis; of these, 226 (13%) tested positive for influenza infection, including 211 (93%) with influenza A viruses and 15 (7%) with influenza B viruses. Fully 1,611 of the patients (90%), had verified vaccine status, while 181 (10%) had solely parental reported vaccine status. The researchers reported 88 (5%) of the patients received mechanical ventilation and 7 (<1%) died.
Most noteworthy, They further estimated a significant reduction in hospitalizations linked to A(H3N2) and A(H1N1)pdm09 viruses, even in the presence of circulating A(H3N2) viruses that differed from the A(H3N2) vaccine component.
Studies from other countries during the same time period showed that while “significant protection against influenza-associated ambulatory care visits and hospitalizations among children infected with A(H1N1)pdm09 viruses” was observed, the same could not be said for protection against A(H3N2) viruses, which varied among pediatric outpatients in the United States (24%), in England (17% outpatient; 31% inpatient), Europe (46%), and Canada (48%). They explained that such variation in vaccine protection is multifactorial, and includes virus-, host-, and environment-related factors. They also noted that regional variations in circulating viruses, host factors including age, imprinting, and previous vaccination could explain the study’s finding of vaccine protection against both A(H1N1)pdm09 and A(H3N2) viruses.
When comparing VE estimates between ED visits and hospitalizations, the researchers observed one significant difference, that “hospitalized children likely represent more medically complex patients, with 58% having underlying medical conditions and 38% reporting at lease one hospitalization in the past year, compared with 28% and 14% respectively, among ED participants.”
Strengths of the study included the prospective multisite enrollment that provided data across diverse locations and representation from pediatric hospitalizations and ED care, which were not previously strongly represented in the literature. The single-season study with small sample size was considered a limitation, as was the inability to evaluate full and partial vaccine status. Vaccine data also were limited for many of the ED patients observed.
Dr. Campbell and colleagues did caution that while they consider their test-negative design optimal for evaluating both hospitalized and ED patients, they feel their results should not be “interpreted as VE against influenza-associated ambulatory care visits or infections that are not medically attended.”
In a separate interview, Michael E. Pichichero, MD, director of the Rochester General Hospital Research Institute and a clinical professor of pediatrics at the University of Rochester (N.Y.), observed: “There are really no surprises here. A well done contemporary study confirms again the benefits of annual influenza vaccinations for children. Viral coinfections involving SARS-CoV-2 and influenza have been reported from Australia to cause heightened illnesses. That observation provides further impetus for parents to have their children receive influenza vaccinations.”
The researchers cited multiple sources of financial support for their ongoing work, including Sanofi, Quidel, Moderna, Karius, GlaxoSmithKline, Merck, AstraZeneca, and Pfizer. Funding for this study was supported by the Centers for Disease Control and Prevention. Dr. Pichichero said he had no relevant financial disclosures.
SOURCE: Campbell AP et al. Pediatrics. 2020. doi: 10.1542/peds.2020-1368.
FROM PEDIATRICS



