User login
Nonmotor symptoms common in Parkinson’s
The hallmark of Parkinson’s disease is the accompanying motor symptoms, but the condition can bring other challenges. Among those are nonmotor symptoms, including depression, dementia, and even psychosis.
The culprit is Lewy bodies, which are also responsible for Lewy body dementia. “What we call Lewy body dementia and Parkinson’s disease are caused by the same pathological process – the formation of Lewy bodies in the brain,” Leslie Citrome, MD, MPH, said in an interview. Dr. Citrome discussed some of the psychiatric comorbidities associated with Parkinson’s disease at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In fact, the association goes both ways. “Many people with Parkinson’s disease develop a dementia. Many people with Lewy body dementia develop motor symptoms that look just like Parkinson’s disease,” said Dr. Citrome, professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, and president of the American Society for Clinical Psychopharmacology.
The motor symptoms of Parkinson’s disease are generally attributable to loss of striatal dopaminergic neurons, while nonmotor symptoms can be traced to loss of neurons in nondopaminergic regions. Nonmotor symptoms – often including sleep disorders, depression, cognitive changes, and psychosis – may occur before motor symptoms. Other problems may include autonomic dysfunction, such as constipation, sexual dysfunction, sweating, or urinary retention.
Patients might not be aware that nonmotor symptoms can occur with Parkinson’s disease and may not even consider mentioning mood changes or hallucinations to their neurologist. Family members may also be unaware.
Sleep problems are common in Parkinson’s disease, including rapid eye-movement sleep behavior disorders, vivid dreams, restless legs syndrome, insomnia, and daytime somnolence. Dopamine agonists may also cause unintended sleep.
Depression is extremely common, affecting up to 90% of Parkinson’s disease patients, and this may be related to dopaminergic losses. Antidepressant medications can worsen Parkinson’s disease symptoms: Tricyclic antidepressants increase risk of adverse events from anticholinergic drugs. Selective serotonin reuptake inhibitors (SSRIs) can exacerbate tremor and may increase risk of serotonin syndrome when combined with MAO‐B inhibitors.
Dr. Citrome was not aware of any antidepressant drugs that have been tested specifically in Parkinson’s disease patients, though “I’d be surprised if there wasn’t,” he said during the Q&A session. “There’s no one perfect antidepressant for people with depression associated with Parkinson’s disease. I would make sure to select one that they would tolerate and be willing to take and that doesn’t interfere with their treatment of their movement disorder, and (I would make sure) that there’s no drug-drug interaction,” he said.
This can include reduced working memory, learning, and planning, and generally does not manifest until at least 1 year after motor symptoms have begun. Rivastigmine is Food and Drug Administration–approved for treatment of cognitive impairment in Parkinson’s disease.
As many as 60% of Parkinson’s disease patients suffer from psychosis at some point, often visual hallucinations or delusions, which can include beliefs of spousal infidelity.
Many clinicians prescribe quetiapine off label, but there are not compelling data to support that it reduces intensity and frequency of hallucinations and delusions, according to Dr. Citrome. However, it is relatively easy to prescribe, requiring no preauthorizations, it is inexpensive, and it may improve sleep.
The FDA approved pimavanserin in 2016 for hallucinations and delusions in Parkinson’s disease, and it doesn’t worsen motor symptoms, Dr. Citrome said. That’s because pimavanserin is a highly selective antagonist of the 5-HT2A receptor, with no effect on dopaminergic, histaminergic, adrenergic, or muscarinic receptors.
The drug improves positive symptoms beginning at days 29 and 43, compared with placebo. An analysis by Dr. Citrome’s group found a number needed to treat (NNT) of 7 to gain a benefit over placebo if the metric is a ≥ 30% reduction in baseline symptom score. The drug had an NNT of 9 to achieve a ≥ 50% reduction, and an NNT of 5 to achieve a score of much improved or very much improved on the Clinical Global Impression–Improvement (CGI-I) scale. In general, an NNT less than 10 suggests that a drug is clinically useful.
In contrast, the number needed to harm (NNH) represents the number of patients who would need to receive a therapy to add one adverse event, compared with placebo. A number greater than 10 indicates that the therapy may be tolerable.
Using various measures, the NNH was well over 10 for pimavanserin. With respect to somnolence, the NNH over placebo was 138, and for a weight gain of 7% or more, the NNH was 594.
Overall, the study found that 4 patients would need to be treated to achieve a benefit over placebo with respect to a ≥ 3–point improvement in the Scale of Positive Symptoms–Parkinson’s Disease (SAPS-PD), while 21 would need to receive the drug to lead to one additional discontinuation because of an adverse event, compared to placebo.
When researchers compared pimavanserin to off-label use of quetiapine, olanzapine, and clozapine, they found a Cohen’s d value of 0.50, which was better than quetiapine and olanzapine, but lower than for clozapine. However, there is no requirement of blood monitoring, and clozapine can potentially worsen motor symptoms.
Dr. Citrome’s presentation should be a reminder to neurologists that psychiatric disorders are an important patient concern, said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati, who moderated the session.
“I think this serves as a model to recognize that many neurological disorders actually present with numerous psychiatric disorders,” Dr. Nasrallah said during the meeting, presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Dr. Citrome has consulted for AbbVie, Acadia, Alkermes, Allergan, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer-Ingelheim, Cadent Therapeutics, Eisai, Impel, Intra-Cellular, Janssen, Karuna, Lundbeck, Lyndra, MedAvante-ProPhase, Merck, Neurocrine, Noven, Otsuka, Ovid, Relmada, Sage, Sunovion, and Teva. He has been a speaker for most of those companies, and he holds stock in Bristol Myers Squibb, Eli Lilly, J&J, Merck, and Pfizer.
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has served on a speakers bureau for most of those companies, in addition to that of Noven.
The hallmark of Parkinson’s disease is the accompanying motor symptoms, but the condition can bring other challenges. Among those are nonmotor symptoms, including depression, dementia, and even psychosis.
The culprit is Lewy bodies, which are also responsible for Lewy body dementia. “What we call Lewy body dementia and Parkinson’s disease are caused by the same pathological process – the formation of Lewy bodies in the brain,” Leslie Citrome, MD, MPH, said in an interview. Dr. Citrome discussed some of the psychiatric comorbidities associated with Parkinson’s disease at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In fact, the association goes both ways. “Many people with Parkinson’s disease develop a dementia. Many people with Lewy body dementia develop motor symptoms that look just like Parkinson’s disease,” said Dr. Citrome, professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, and president of the American Society for Clinical Psychopharmacology.
The motor symptoms of Parkinson’s disease are generally attributable to loss of striatal dopaminergic neurons, while nonmotor symptoms can be traced to loss of neurons in nondopaminergic regions. Nonmotor symptoms – often including sleep disorders, depression, cognitive changes, and psychosis – may occur before motor symptoms. Other problems may include autonomic dysfunction, such as constipation, sexual dysfunction, sweating, or urinary retention.
Patients might not be aware that nonmotor symptoms can occur with Parkinson’s disease and may not even consider mentioning mood changes or hallucinations to their neurologist. Family members may also be unaware.
Sleep problems are common in Parkinson’s disease, including rapid eye-movement sleep behavior disorders, vivid dreams, restless legs syndrome, insomnia, and daytime somnolence. Dopamine agonists may also cause unintended sleep.
Depression is extremely common, affecting up to 90% of Parkinson’s disease patients, and this may be related to dopaminergic losses. Antidepressant medications can worsen Parkinson’s disease symptoms: Tricyclic antidepressants increase risk of adverse events from anticholinergic drugs. Selective serotonin reuptake inhibitors (SSRIs) can exacerbate tremor and may increase risk of serotonin syndrome when combined with MAO‐B inhibitors.
Dr. Citrome was not aware of any antidepressant drugs that have been tested specifically in Parkinson’s disease patients, though “I’d be surprised if there wasn’t,” he said during the Q&A session. “There’s no one perfect antidepressant for people with depression associated with Parkinson’s disease. I would make sure to select one that they would tolerate and be willing to take and that doesn’t interfere with their treatment of their movement disorder, and (I would make sure) that there’s no drug-drug interaction,” he said.
This can include reduced working memory, learning, and planning, and generally does not manifest until at least 1 year after motor symptoms have begun. Rivastigmine is Food and Drug Administration–approved for treatment of cognitive impairment in Parkinson’s disease.
As many as 60% of Parkinson’s disease patients suffer from psychosis at some point, often visual hallucinations or delusions, which can include beliefs of spousal infidelity.
Many clinicians prescribe quetiapine off label, but there are not compelling data to support that it reduces intensity and frequency of hallucinations and delusions, according to Dr. Citrome. However, it is relatively easy to prescribe, requiring no preauthorizations, it is inexpensive, and it may improve sleep.
The FDA approved pimavanserin in 2016 for hallucinations and delusions in Parkinson’s disease, and it doesn’t worsen motor symptoms, Dr. Citrome said. That’s because pimavanserin is a highly selective antagonist of the 5-HT2A receptor, with no effect on dopaminergic, histaminergic, adrenergic, or muscarinic receptors.
The drug improves positive symptoms beginning at days 29 and 43, compared with placebo. An analysis by Dr. Citrome’s group found a number needed to treat (NNT) of 7 to gain a benefit over placebo if the metric is a ≥ 30% reduction in baseline symptom score. The drug had an NNT of 9 to achieve a ≥ 50% reduction, and an NNT of 5 to achieve a score of much improved or very much improved on the Clinical Global Impression–Improvement (CGI-I) scale. In general, an NNT less than 10 suggests that a drug is clinically useful.
In contrast, the number needed to harm (NNH) represents the number of patients who would need to receive a therapy to add one adverse event, compared with placebo. A number greater than 10 indicates that the therapy may be tolerable.
Using various measures, the NNH was well over 10 for pimavanserin. With respect to somnolence, the NNH over placebo was 138, and for a weight gain of 7% or more, the NNH was 594.
Overall, the study found that 4 patients would need to be treated to achieve a benefit over placebo with respect to a ≥ 3–point improvement in the Scale of Positive Symptoms–Parkinson’s Disease (SAPS-PD), while 21 would need to receive the drug to lead to one additional discontinuation because of an adverse event, compared to placebo.
When researchers compared pimavanserin to off-label use of quetiapine, olanzapine, and clozapine, they found a Cohen’s d value of 0.50, which was better than quetiapine and olanzapine, but lower than for clozapine. However, there is no requirement of blood monitoring, and clozapine can potentially worsen motor symptoms.
Dr. Citrome’s presentation should be a reminder to neurologists that psychiatric disorders are an important patient concern, said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati, who moderated the session.
“I think this serves as a model to recognize that many neurological disorders actually present with numerous psychiatric disorders,” Dr. Nasrallah said during the meeting, presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Dr. Citrome has consulted for AbbVie, Acadia, Alkermes, Allergan, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer-Ingelheim, Cadent Therapeutics, Eisai, Impel, Intra-Cellular, Janssen, Karuna, Lundbeck, Lyndra, MedAvante-ProPhase, Merck, Neurocrine, Noven, Otsuka, Ovid, Relmada, Sage, Sunovion, and Teva. He has been a speaker for most of those companies, and he holds stock in Bristol Myers Squibb, Eli Lilly, J&J, Merck, and Pfizer.
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has served on a speakers bureau for most of those companies, in addition to that of Noven.
The hallmark of Parkinson’s disease is the accompanying motor symptoms, but the condition can bring other challenges. Among those are nonmotor symptoms, including depression, dementia, and even psychosis.
The culprit is Lewy bodies, which are also responsible for Lewy body dementia. “What we call Lewy body dementia and Parkinson’s disease are caused by the same pathological process – the formation of Lewy bodies in the brain,” Leslie Citrome, MD, MPH, said in an interview. Dr. Citrome discussed some of the psychiatric comorbidities associated with Parkinson’s disease at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In fact, the association goes both ways. “Many people with Parkinson’s disease develop a dementia. Many people with Lewy body dementia develop motor symptoms that look just like Parkinson’s disease,” said Dr. Citrome, professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, and president of the American Society for Clinical Psychopharmacology.
The motor symptoms of Parkinson’s disease are generally attributable to loss of striatal dopaminergic neurons, while nonmotor symptoms can be traced to loss of neurons in nondopaminergic regions. Nonmotor symptoms – often including sleep disorders, depression, cognitive changes, and psychosis – may occur before motor symptoms. Other problems may include autonomic dysfunction, such as constipation, sexual dysfunction, sweating, or urinary retention.
Patients might not be aware that nonmotor symptoms can occur with Parkinson’s disease and may not even consider mentioning mood changes or hallucinations to their neurologist. Family members may also be unaware.
Sleep problems are common in Parkinson’s disease, including rapid eye-movement sleep behavior disorders, vivid dreams, restless legs syndrome, insomnia, and daytime somnolence. Dopamine agonists may also cause unintended sleep.
Depression is extremely common, affecting up to 90% of Parkinson’s disease patients, and this may be related to dopaminergic losses. Antidepressant medications can worsen Parkinson’s disease symptoms: Tricyclic antidepressants increase risk of adverse events from anticholinergic drugs. Selective serotonin reuptake inhibitors (SSRIs) can exacerbate tremor and may increase risk of serotonin syndrome when combined with MAO‐B inhibitors.
Dr. Citrome was not aware of any antidepressant drugs that have been tested specifically in Parkinson’s disease patients, though “I’d be surprised if there wasn’t,” he said during the Q&A session. “There’s no one perfect antidepressant for people with depression associated with Parkinson’s disease. I would make sure to select one that they would tolerate and be willing to take and that doesn’t interfere with their treatment of their movement disorder, and (I would make sure) that there’s no drug-drug interaction,” he said.
This can include reduced working memory, learning, and planning, and generally does not manifest until at least 1 year after motor symptoms have begun. Rivastigmine is Food and Drug Administration–approved for treatment of cognitive impairment in Parkinson’s disease.
As many as 60% of Parkinson’s disease patients suffer from psychosis at some point, often visual hallucinations or delusions, which can include beliefs of spousal infidelity.
Many clinicians prescribe quetiapine off label, but there are not compelling data to support that it reduces intensity and frequency of hallucinations and delusions, according to Dr. Citrome. However, it is relatively easy to prescribe, requiring no preauthorizations, it is inexpensive, and it may improve sleep.
The FDA approved pimavanserin in 2016 for hallucinations and delusions in Parkinson’s disease, and it doesn’t worsen motor symptoms, Dr. Citrome said. That’s because pimavanserin is a highly selective antagonist of the 5-HT2A receptor, with no effect on dopaminergic, histaminergic, adrenergic, or muscarinic receptors.
The drug improves positive symptoms beginning at days 29 and 43, compared with placebo. An analysis by Dr. Citrome’s group found a number needed to treat (NNT) of 7 to gain a benefit over placebo if the metric is a ≥ 30% reduction in baseline symptom score. The drug had an NNT of 9 to achieve a ≥ 50% reduction, and an NNT of 5 to achieve a score of much improved or very much improved on the Clinical Global Impression–Improvement (CGI-I) scale. In general, an NNT less than 10 suggests that a drug is clinically useful.
In contrast, the number needed to harm (NNH) represents the number of patients who would need to receive a therapy to add one adverse event, compared with placebo. A number greater than 10 indicates that the therapy may be tolerable.
Using various measures, the NNH was well over 10 for pimavanserin. With respect to somnolence, the NNH over placebo was 138, and for a weight gain of 7% or more, the NNH was 594.
Overall, the study found that 4 patients would need to be treated to achieve a benefit over placebo with respect to a ≥ 3–point improvement in the Scale of Positive Symptoms–Parkinson’s Disease (SAPS-PD), while 21 would need to receive the drug to lead to one additional discontinuation because of an adverse event, compared to placebo.
When researchers compared pimavanserin to off-label use of quetiapine, olanzapine, and clozapine, they found a Cohen’s d value of 0.50, which was better than quetiapine and olanzapine, but lower than for clozapine. However, there is no requirement of blood monitoring, and clozapine can potentially worsen motor symptoms.
Dr. Citrome’s presentation should be a reminder to neurologists that psychiatric disorders are an important patient concern, said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati, who moderated the session.
“I think this serves as a model to recognize that many neurological disorders actually present with numerous psychiatric disorders,” Dr. Nasrallah said during the meeting, presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Dr. Citrome has consulted for AbbVie, Acadia, Alkermes, Allergan, Angelini, Astellas, Avanir, Axsome, BioXcel, Boehringer-Ingelheim, Cadent Therapeutics, Eisai, Impel, Intra-Cellular, Janssen, Karuna, Lundbeck, Lyndra, MedAvante-ProPhase, Merck, Neurocrine, Noven, Otsuka, Ovid, Relmada, Sage, Sunovion, and Teva. He has been a speaker for most of those companies, and he holds stock in Bristol Myers Squibb, Eli Lilly, J&J, Merck, and Pfizer.
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has served on a speakers bureau for most of those companies, in addition to that of Noven.
FROM FOCUS ON NEUROPSYCHIATRY 2021
Pandemic unveils growing suicide crisis for communities of color
This story is a collaboration between KHN and “Science Friday.”
Rafiah Maxie has been a licensed clinical social worker in the Chicago area for a decade. Throughout that time, she’d viewed suicide as a problem most prevalent among middle-aged white men.
Until May 27, 2020.
That day, Maxie’s 19-year-old son, Jamal Clay – who loved playing the trumpet and participating in theater, who would help her unload groceries from the car and raise funds for the March of the Dimes – killed himself in their garage.
“Now I cannot blink without seeing my son hanging,” said Maxie, who is Black.
Clay’s death, along with the suicides of more than 100 other Black residents in Illinois last year, has led locals to call for new prevention efforts focused on Black communities. In 2020, during the pandemic’s first year, suicides among White residents decreased compared with previous years, while they increased among Black residents, according to state data.
But this is not a local problem. Nor is it limited to the pandemic.
Interviews with a dozen suicide researchers, data collected from states across the country, and a review of decades of research revealed that suicide is a growing crisis for communities of color – one that plagued them well before the pandemic and has only been exacerbated since.
Overall suicide rates in the U.S. decreased in 2019 and 2020. National and local studies attribute the trend to a drop among White Americans, who make up the majority of suicide deaths. Meanwhile, rates for Black, Hispanic, and Asian Americans – though lower than those of their white peers – continued to climb in many states. (Suicide rates have been consistently high for Native Americans.)
“COVID created more transparency regarding what we already knew was happening,” said Sonyia Richardson, a licensed clinical social worker who focuses on serving people of color, and assistant professor at the University of North Carolina–Charlotte, where she researches suicide. When you put the suicide rates of all communities in one bucket, “that bucket says it’s getting better and what we’re doing is working,” she said. “But that’s not the case for communities of color.”
Losing generations
Although the suicide rate is highest among middle-aged White men, young people of color are emerging as particularly at risk.
Research shows Black kids younger than 13 die by suicide at nearly twice the rate of White kids and, over time, their suicide rates have grown even as rates have decreased for White children. Among teenagers and young adults, suicide deaths have increased more than 45% for Black Americans and about 40% for Asian Americans in the 7 years ending in 2019. Other concerning trends in suicide attempts date to the ’90s.
“We have to pay attention now because if you’re out of the first decade of life and think life is not worth pursuing, that’s a signal to say something is going really wrong.”
These statistics also refute traditional ideas that suicide doesn’t happen in certain ethnic or minority populations because they’re “protected” and “resilient” or the “model minority,” said Kiara Alvarez, a researcher and psychologist at Massachusetts General Hospital who focuses on suicide among Hispanic and immigrant populations.
Although these groups may have had low suicide rates historically, that’s changing, she said.
Paul Chin lost his 17-year-old brother, Chris, to suicide in 2009. A poem Chris wrote in high school about his heritage has left Chin, 8 years his senior, wondering if his brother struggled to feel accepted in the U.S., despite being born and raised in New York.
Growing up, Asian Americans weren’t represented in lessons at school or in pop culture, said Chin, now 37. Even in clinical research on suicide as well as other health topics, kids like Chris are underrepresented, with less than 1% of federal research funding focused on Asian Americans.
It wasn’t until the pandemic, and the concurrent rise in hate crimes against Asian Americans, that Chin saw national attention on the community’s mental health. He hopes the interest is not short-lived.
Suicide is the leading cause of death for Asian Americans ages 15 to 24, yet “that doesn’t get enough attention,” Chin said. “It’s important to continue to share these stories.”
Kathy Williams, who is Black, has been on a similar mission since her 15-year-old son, Torian Graves, died by suicide in 1996. People didn’t talk about suicide in the Black community then, she said. So she started raising the topic at her church in Durham, N.C., and in local schools. She wanted Black families to know the warning signs and society at large to recognize the seriousness of the problem.
The pandemic may have highlighted this, Williams said, but “it has always happened. Always.”
Pandemic sheds light on the triggers
Pinpointing the root causes of rising suicide within communities of color has proved difficult. How much stems from mental illness? How much from socioeconomic changes like job losses or social isolation? Now, COVID-19 may offer some clues.
Recent decades have been marked by growing economic instability, a widening racial wealth gap, and more public attention on police killings of unarmed Black and Brown people, said Michael Lindsey, executive director of the New York University McSilver Institute for Poverty Policy and Research.
With social media, youths face racism on more fronts than their parents did, said Leslie Adams, assistant professor in the department of mental health at Johns Hopkins Bloomberg School of Public Health.
Each of these factors has been shown to affect suicide risk. For example, experiencing racism and sexism together is linked to a threefold increase in suicidal thoughts for Asian American women, said Brian Keum, assistant professor at UCLA, based on preliminary research findings.
COVID-19 intensified these hardships among communities of color, with disproportionate numbers of lost loved ones, lost jobs, and lost housing. The murder of George Floyd prompted widespread racial unrest, and Asian Americans saw an increase in hate crimes.
At the same time, studies in Connecticut and Maryland found that suicide rates rose within these populations and dropped for their White counterparts.
“It’s not just a problem within the person, but societal issues that need to be addressed,” said Shari Jager-Hyman, assistant professor of psychiatry at the University of Pennsylvania.
Lessons from Texas
In Texas, COVID-19 hit Hispanics especially hard. As of July 2021, they accounted for 45% of all COVID-19 deaths and disproportionately lost jobs. Individuals living in the U.S. without authorization were generally not eligible for unemployment benefits or federal stimulus checks.
During this time, suicide deaths among Hispanic Texans climbed from 847 deaths in 2019 to 962 deaths in 2020, according to preliminary state data. Suicide deaths rose for Black Texans and residents classified as “other” races or ethnicities, but decreased for White Texans.
The numbers didn’t surprise Marc Mendiola. The 20-year-old grew up in a majority-Hispanic community on the south side of San Antonio. Even before the pandemic, he often heard classmates say they were suicidal. Many faced dire finances at home, sometimes living without electricity, food, or water. Those who sought mental health treatment often found services prohibitively expensive or inaccessible because they weren’t offered in Spanish.
“These are conditions the community has always been in,” Mendiola said. “But with the pandemic, it’s even worse.”
Four years ago, Mendiola and his classmates at South San High School began advocating for mental health services. In late 2019, just months before COVID-19 struck, their vision became reality. Six community agencies partnered to offer free services to students and their families across three school districts.
Richard Davidson, chief operating officer of Family Service, one of the groups in the collaborative, said the number of students discussing economic stressors has been on the rise since April 2020. More than 90% of the students who received services in the first half of 2021 were Hispanic, and nearly 10% reported thoughts of suicide or self-harm, program data show. None died by suicide.
Many students are so worried about what’s for dinner the next day that they’re not able to see a future beyond that, Davidson said. That’s when suicide can feel like a viable option.
“One of the things we do is help them see … that despite this situation now, you can create a vision for your future,” Davidson said.
A good future
Researchers say the promise of a good future is often overlooked in suicide prevention, perhaps because achieving it is so challenging. It requires economic and social growth and breaking systemic barriers.
Tevis Simon works to address all those fronts. As a child in West Baltimore, Simon, who is Black, faced poverty and trauma. As an adult, she attempted suicide three times. But now she shares her story with youths across the city to inspire them to overcome challenges. She also talks to politicians, law enforcement agencies, and public policy officials about their responsibilities.
“We can’t not talk about race,” said Simon, 43. “We can’t not talk about systematic oppression. We cannot not talk about these conditions that affect our mental well-being and our feeling and desire to live.”
For Jamal Clay in Illinois, the systemic barriers started early. Before his suicide last year, he had tried to harm himself when he was 12 and the victim of bullies. At that time, he was hospitalized for a few days and told to follow up with outpatient therapy, said his mother, Maxie.
But it was difficult to find therapists who accepted Medicaid, she said. When Maxie finally found one, there was a 60-day wait. Other therapists canceled appointments, she said.
“So we worked on our own,” Maxie said, relying on church and community. Her son seemed to improve. “We thought we closed that chapter in our lives.”
But when the pandemic hit, everything got worse, she said. Clay came home from college and worked at an Amazon warehouse. On drives to and from work, he was frequently pulled over by police. He stopped wearing hats so officers would consider him less intimidating, Maxie said.
“He felt uncomfortable being out in the street,” she said.
Maxie is still trying to make sense of what happened the day Clay died. But she’s found meaning in starting a nonprofit called Soul Survivors of Chicago. Through the organization, she provides education, scholarships and shoes – including Jamal’s old ones – to those impacted by violence, suicide, and trauma.
“My son won’t be able to have a first interview in [those] shoes. He won’t be able to have a nice jump shot or go to church or even meet his wife,” Maxie said.
But she hopes his shoes will carry someone else to a good future.
[Editor’s note: For the purposes of this story, “people of color” or “communities of color” refers to any racial or ethnic populations whose members do not identify as White, including those who are multiracial. Hispanics can be of any race or combination of races.]
KHN senior correspondent JoNel Aleccia contributed to this report. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
This story is a collaboration between KHN and “Science Friday.”
Rafiah Maxie has been a licensed clinical social worker in the Chicago area for a decade. Throughout that time, she’d viewed suicide as a problem most prevalent among middle-aged white men.
Until May 27, 2020.
That day, Maxie’s 19-year-old son, Jamal Clay – who loved playing the trumpet and participating in theater, who would help her unload groceries from the car and raise funds for the March of the Dimes – killed himself in their garage.
“Now I cannot blink without seeing my son hanging,” said Maxie, who is Black.
Clay’s death, along with the suicides of more than 100 other Black residents in Illinois last year, has led locals to call for new prevention efforts focused on Black communities. In 2020, during the pandemic’s first year, suicides among White residents decreased compared with previous years, while they increased among Black residents, according to state data.
But this is not a local problem. Nor is it limited to the pandemic.
Interviews with a dozen suicide researchers, data collected from states across the country, and a review of decades of research revealed that suicide is a growing crisis for communities of color – one that plagued them well before the pandemic and has only been exacerbated since.
Overall suicide rates in the U.S. decreased in 2019 and 2020. National and local studies attribute the trend to a drop among White Americans, who make up the majority of suicide deaths. Meanwhile, rates for Black, Hispanic, and Asian Americans – though lower than those of their white peers – continued to climb in many states. (Suicide rates have been consistently high for Native Americans.)
“COVID created more transparency regarding what we already knew was happening,” said Sonyia Richardson, a licensed clinical social worker who focuses on serving people of color, and assistant professor at the University of North Carolina–Charlotte, where she researches suicide. When you put the suicide rates of all communities in one bucket, “that bucket says it’s getting better and what we’re doing is working,” she said. “But that’s not the case for communities of color.”
Losing generations
Although the suicide rate is highest among middle-aged White men, young people of color are emerging as particularly at risk.
Research shows Black kids younger than 13 die by suicide at nearly twice the rate of White kids and, over time, their suicide rates have grown even as rates have decreased for White children. Among teenagers and young adults, suicide deaths have increased more than 45% for Black Americans and about 40% for Asian Americans in the 7 years ending in 2019. Other concerning trends in suicide attempts date to the ’90s.
“We have to pay attention now because if you’re out of the first decade of life and think life is not worth pursuing, that’s a signal to say something is going really wrong.”
These statistics also refute traditional ideas that suicide doesn’t happen in certain ethnic or minority populations because they’re “protected” and “resilient” or the “model minority,” said Kiara Alvarez, a researcher and psychologist at Massachusetts General Hospital who focuses on suicide among Hispanic and immigrant populations.
Although these groups may have had low suicide rates historically, that’s changing, she said.
Paul Chin lost his 17-year-old brother, Chris, to suicide in 2009. A poem Chris wrote in high school about his heritage has left Chin, 8 years his senior, wondering if his brother struggled to feel accepted in the U.S., despite being born and raised in New York.
Growing up, Asian Americans weren’t represented in lessons at school or in pop culture, said Chin, now 37. Even in clinical research on suicide as well as other health topics, kids like Chris are underrepresented, with less than 1% of federal research funding focused on Asian Americans.
It wasn’t until the pandemic, and the concurrent rise in hate crimes against Asian Americans, that Chin saw national attention on the community’s mental health. He hopes the interest is not short-lived.
Suicide is the leading cause of death for Asian Americans ages 15 to 24, yet “that doesn’t get enough attention,” Chin said. “It’s important to continue to share these stories.”
Kathy Williams, who is Black, has been on a similar mission since her 15-year-old son, Torian Graves, died by suicide in 1996. People didn’t talk about suicide in the Black community then, she said. So she started raising the topic at her church in Durham, N.C., and in local schools. She wanted Black families to know the warning signs and society at large to recognize the seriousness of the problem.
The pandemic may have highlighted this, Williams said, but “it has always happened. Always.”
Pandemic sheds light on the triggers
Pinpointing the root causes of rising suicide within communities of color has proved difficult. How much stems from mental illness? How much from socioeconomic changes like job losses or social isolation? Now, COVID-19 may offer some clues.
Recent decades have been marked by growing economic instability, a widening racial wealth gap, and more public attention on police killings of unarmed Black and Brown people, said Michael Lindsey, executive director of the New York University McSilver Institute for Poverty Policy and Research.
With social media, youths face racism on more fronts than their parents did, said Leslie Adams, assistant professor in the department of mental health at Johns Hopkins Bloomberg School of Public Health.
Each of these factors has been shown to affect suicide risk. For example, experiencing racism and sexism together is linked to a threefold increase in suicidal thoughts for Asian American women, said Brian Keum, assistant professor at UCLA, based on preliminary research findings.
COVID-19 intensified these hardships among communities of color, with disproportionate numbers of lost loved ones, lost jobs, and lost housing. The murder of George Floyd prompted widespread racial unrest, and Asian Americans saw an increase in hate crimes.
At the same time, studies in Connecticut and Maryland found that suicide rates rose within these populations and dropped for their White counterparts.
“It’s not just a problem within the person, but societal issues that need to be addressed,” said Shari Jager-Hyman, assistant professor of psychiatry at the University of Pennsylvania.
Lessons from Texas
In Texas, COVID-19 hit Hispanics especially hard. As of July 2021, they accounted for 45% of all COVID-19 deaths and disproportionately lost jobs. Individuals living in the U.S. without authorization were generally not eligible for unemployment benefits or federal stimulus checks.
During this time, suicide deaths among Hispanic Texans climbed from 847 deaths in 2019 to 962 deaths in 2020, according to preliminary state data. Suicide deaths rose for Black Texans and residents classified as “other” races or ethnicities, but decreased for White Texans.
The numbers didn’t surprise Marc Mendiola. The 20-year-old grew up in a majority-Hispanic community on the south side of San Antonio. Even before the pandemic, he often heard classmates say they were suicidal. Many faced dire finances at home, sometimes living without electricity, food, or water. Those who sought mental health treatment often found services prohibitively expensive or inaccessible because they weren’t offered in Spanish.
“These are conditions the community has always been in,” Mendiola said. “But with the pandemic, it’s even worse.”
Four years ago, Mendiola and his classmates at South San High School began advocating for mental health services. In late 2019, just months before COVID-19 struck, their vision became reality. Six community agencies partnered to offer free services to students and their families across three school districts.
Richard Davidson, chief operating officer of Family Service, one of the groups in the collaborative, said the number of students discussing economic stressors has been on the rise since April 2020. More than 90% of the students who received services in the first half of 2021 were Hispanic, and nearly 10% reported thoughts of suicide or self-harm, program data show. None died by suicide.
Many students are so worried about what’s for dinner the next day that they’re not able to see a future beyond that, Davidson said. That’s when suicide can feel like a viable option.
“One of the things we do is help them see … that despite this situation now, you can create a vision for your future,” Davidson said.
A good future
Researchers say the promise of a good future is often overlooked in suicide prevention, perhaps because achieving it is so challenging. It requires economic and social growth and breaking systemic barriers.
Tevis Simon works to address all those fronts. As a child in West Baltimore, Simon, who is Black, faced poverty and trauma. As an adult, she attempted suicide three times. But now she shares her story with youths across the city to inspire them to overcome challenges. She also talks to politicians, law enforcement agencies, and public policy officials about their responsibilities.
“We can’t not talk about race,” said Simon, 43. “We can’t not talk about systematic oppression. We cannot not talk about these conditions that affect our mental well-being and our feeling and desire to live.”
For Jamal Clay in Illinois, the systemic barriers started early. Before his suicide last year, he had tried to harm himself when he was 12 and the victim of bullies. At that time, he was hospitalized for a few days and told to follow up with outpatient therapy, said his mother, Maxie.
But it was difficult to find therapists who accepted Medicaid, she said. When Maxie finally found one, there was a 60-day wait. Other therapists canceled appointments, she said.
“So we worked on our own,” Maxie said, relying on church and community. Her son seemed to improve. “We thought we closed that chapter in our lives.”
But when the pandemic hit, everything got worse, she said. Clay came home from college and worked at an Amazon warehouse. On drives to and from work, he was frequently pulled over by police. He stopped wearing hats so officers would consider him less intimidating, Maxie said.
“He felt uncomfortable being out in the street,” she said.
Maxie is still trying to make sense of what happened the day Clay died. But she’s found meaning in starting a nonprofit called Soul Survivors of Chicago. Through the organization, she provides education, scholarships and shoes – including Jamal’s old ones – to those impacted by violence, suicide, and trauma.
“My son won’t be able to have a first interview in [those] shoes. He won’t be able to have a nice jump shot or go to church or even meet his wife,” Maxie said.
But she hopes his shoes will carry someone else to a good future.
[Editor’s note: For the purposes of this story, “people of color” or “communities of color” refers to any racial or ethnic populations whose members do not identify as White, including those who are multiracial. Hispanics can be of any race or combination of races.]
KHN senior correspondent JoNel Aleccia contributed to this report. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
This story is a collaboration between KHN and “Science Friday.”
Rafiah Maxie has been a licensed clinical social worker in the Chicago area for a decade. Throughout that time, she’d viewed suicide as a problem most prevalent among middle-aged white men.
Until May 27, 2020.
That day, Maxie’s 19-year-old son, Jamal Clay – who loved playing the trumpet and participating in theater, who would help her unload groceries from the car and raise funds for the March of the Dimes – killed himself in their garage.
“Now I cannot blink without seeing my son hanging,” said Maxie, who is Black.
Clay’s death, along with the suicides of more than 100 other Black residents in Illinois last year, has led locals to call for new prevention efforts focused on Black communities. In 2020, during the pandemic’s first year, suicides among White residents decreased compared with previous years, while they increased among Black residents, according to state data.
But this is not a local problem. Nor is it limited to the pandemic.
Interviews with a dozen suicide researchers, data collected from states across the country, and a review of decades of research revealed that suicide is a growing crisis for communities of color – one that plagued them well before the pandemic and has only been exacerbated since.
Overall suicide rates in the U.S. decreased in 2019 and 2020. National and local studies attribute the trend to a drop among White Americans, who make up the majority of suicide deaths. Meanwhile, rates for Black, Hispanic, and Asian Americans – though lower than those of their white peers – continued to climb in many states. (Suicide rates have been consistently high for Native Americans.)
“COVID created more transparency regarding what we already knew was happening,” said Sonyia Richardson, a licensed clinical social worker who focuses on serving people of color, and assistant professor at the University of North Carolina–Charlotte, where she researches suicide. When you put the suicide rates of all communities in one bucket, “that bucket says it’s getting better and what we’re doing is working,” she said. “But that’s not the case for communities of color.”
Losing generations
Although the suicide rate is highest among middle-aged White men, young people of color are emerging as particularly at risk.
Research shows Black kids younger than 13 die by suicide at nearly twice the rate of White kids and, over time, their suicide rates have grown even as rates have decreased for White children. Among teenagers and young adults, suicide deaths have increased more than 45% for Black Americans and about 40% for Asian Americans in the 7 years ending in 2019. Other concerning trends in suicide attempts date to the ’90s.
“We have to pay attention now because if you’re out of the first decade of life and think life is not worth pursuing, that’s a signal to say something is going really wrong.”
These statistics also refute traditional ideas that suicide doesn’t happen in certain ethnic or minority populations because they’re “protected” and “resilient” or the “model minority,” said Kiara Alvarez, a researcher and psychologist at Massachusetts General Hospital who focuses on suicide among Hispanic and immigrant populations.
Although these groups may have had low suicide rates historically, that’s changing, she said.
Paul Chin lost his 17-year-old brother, Chris, to suicide in 2009. A poem Chris wrote in high school about his heritage has left Chin, 8 years his senior, wondering if his brother struggled to feel accepted in the U.S., despite being born and raised in New York.
Growing up, Asian Americans weren’t represented in lessons at school or in pop culture, said Chin, now 37. Even in clinical research on suicide as well as other health topics, kids like Chris are underrepresented, with less than 1% of federal research funding focused on Asian Americans.
It wasn’t until the pandemic, and the concurrent rise in hate crimes against Asian Americans, that Chin saw national attention on the community’s mental health. He hopes the interest is not short-lived.
Suicide is the leading cause of death for Asian Americans ages 15 to 24, yet “that doesn’t get enough attention,” Chin said. “It’s important to continue to share these stories.”
Kathy Williams, who is Black, has been on a similar mission since her 15-year-old son, Torian Graves, died by suicide in 1996. People didn’t talk about suicide in the Black community then, she said. So she started raising the topic at her church in Durham, N.C., and in local schools. She wanted Black families to know the warning signs and society at large to recognize the seriousness of the problem.
The pandemic may have highlighted this, Williams said, but “it has always happened. Always.”
Pandemic sheds light on the triggers
Pinpointing the root causes of rising suicide within communities of color has proved difficult. How much stems from mental illness? How much from socioeconomic changes like job losses or social isolation? Now, COVID-19 may offer some clues.
Recent decades have been marked by growing economic instability, a widening racial wealth gap, and more public attention on police killings of unarmed Black and Brown people, said Michael Lindsey, executive director of the New York University McSilver Institute for Poverty Policy and Research.
With social media, youths face racism on more fronts than their parents did, said Leslie Adams, assistant professor in the department of mental health at Johns Hopkins Bloomberg School of Public Health.
Each of these factors has been shown to affect suicide risk. For example, experiencing racism and sexism together is linked to a threefold increase in suicidal thoughts for Asian American women, said Brian Keum, assistant professor at UCLA, based on preliminary research findings.
COVID-19 intensified these hardships among communities of color, with disproportionate numbers of lost loved ones, lost jobs, and lost housing. The murder of George Floyd prompted widespread racial unrest, and Asian Americans saw an increase in hate crimes.
At the same time, studies in Connecticut and Maryland found that suicide rates rose within these populations and dropped for their White counterparts.
“It’s not just a problem within the person, but societal issues that need to be addressed,” said Shari Jager-Hyman, assistant professor of psychiatry at the University of Pennsylvania.
Lessons from Texas
In Texas, COVID-19 hit Hispanics especially hard. As of July 2021, they accounted for 45% of all COVID-19 deaths and disproportionately lost jobs. Individuals living in the U.S. without authorization were generally not eligible for unemployment benefits or federal stimulus checks.
During this time, suicide deaths among Hispanic Texans climbed from 847 deaths in 2019 to 962 deaths in 2020, according to preliminary state data. Suicide deaths rose for Black Texans and residents classified as “other” races or ethnicities, but decreased for White Texans.
The numbers didn’t surprise Marc Mendiola. The 20-year-old grew up in a majority-Hispanic community on the south side of San Antonio. Even before the pandemic, he often heard classmates say they were suicidal. Many faced dire finances at home, sometimes living without electricity, food, or water. Those who sought mental health treatment often found services prohibitively expensive or inaccessible because they weren’t offered in Spanish.
“These are conditions the community has always been in,” Mendiola said. “But with the pandemic, it’s even worse.”
Four years ago, Mendiola and his classmates at South San High School began advocating for mental health services. In late 2019, just months before COVID-19 struck, their vision became reality. Six community agencies partnered to offer free services to students and their families across three school districts.
Richard Davidson, chief operating officer of Family Service, one of the groups in the collaborative, said the number of students discussing economic stressors has been on the rise since April 2020. More than 90% of the students who received services in the first half of 2021 were Hispanic, and nearly 10% reported thoughts of suicide or self-harm, program data show. None died by suicide.
Many students are so worried about what’s for dinner the next day that they’re not able to see a future beyond that, Davidson said. That’s when suicide can feel like a viable option.
“One of the things we do is help them see … that despite this situation now, you can create a vision for your future,” Davidson said.
A good future
Researchers say the promise of a good future is often overlooked in suicide prevention, perhaps because achieving it is so challenging. It requires economic and social growth and breaking systemic barriers.
Tevis Simon works to address all those fronts. As a child in West Baltimore, Simon, who is Black, faced poverty and trauma. As an adult, she attempted suicide three times. But now she shares her story with youths across the city to inspire them to overcome challenges. She also talks to politicians, law enforcement agencies, and public policy officials about their responsibilities.
“We can’t not talk about race,” said Simon, 43. “We can’t not talk about systematic oppression. We cannot not talk about these conditions that affect our mental well-being and our feeling and desire to live.”
For Jamal Clay in Illinois, the systemic barriers started early. Before his suicide last year, he had tried to harm himself when he was 12 and the victim of bullies. At that time, he was hospitalized for a few days and told to follow up with outpatient therapy, said his mother, Maxie.
But it was difficult to find therapists who accepted Medicaid, she said. When Maxie finally found one, there was a 60-day wait. Other therapists canceled appointments, she said.
“So we worked on our own,” Maxie said, relying on church and community. Her son seemed to improve. “We thought we closed that chapter in our lives.”
But when the pandemic hit, everything got worse, she said. Clay came home from college and worked at an Amazon warehouse. On drives to and from work, he was frequently pulled over by police. He stopped wearing hats so officers would consider him less intimidating, Maxie said.
“He felt uncomfortable being out in the street,” she said.
Maxie is still trying to make sense of what happened the day Clay died. But she’s found meaning in starting a nonprofit called Soul Survivors of Chicago. Through the organization, she provides education, scholarships and shoes – including Jamal’s old ones – to those impacted by violence, suicide, and trauma.
“My son won’t be able to have a first interview in [those] shoes. He won’t be able to have a nice jump shot or go to church or even meet his wife,” Maxie said.
But she hopes his shoes will carry someone else to a good future.
[Editor’s note: For the purposes of this story, “people of color” or “communities of color” refers to any racial or ethnic populations whose members do not identify as White, including those who are multiracial. Hispanics can be of any race or combination of races.]
KHN senior correspondent JoNel Aleccia contributed to this report. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Healing Haiti: The emotional trauma of repeat crises
Steeve Verdieu was at his workstation in his bedroom when the shaking started the morning of Aug. 14. He jumped under his desk and held on as a 7.2-magnitude earthquake tore through his childhood home in southern Haiti.
Mr. Verdieu, 25, said all he could think about was 2010, when a strong earthquake hit the country and left more than 200,000 people dead.
“Most of these adults that are in their mid-20s and 30s have vivid memories,” according to John Fitts, assistant director of Sent To Serve. He started working in the nonprofit sector in Haiti after the 2010 earthquake.
“I can’t even relate to it,” Mr. Fitts said. “If you didn’t live through it, you cannot relate.”
Mr. Verdieu emerged to find his family alive and his home in crumbles.
“In the neighborhood, we have only one child who died the day of the earthquake, but mentally, everybody feels bad,” he said. “Also, we are really frustrated right now because it tends to rain, and everybody is outside right now. So, we are a little bit afraid.”
Mr. Verdieu said that his community has not seen or heard of government authorities coming to offer guidance on next steps.
So, he started posting photos and videos to his Twitter account to seek help.
Surviving to heal
Many Haitians are forced to quickly turn the page after major crises, said Mr. Fitts.
“Survival overrides emotional shock,” he said. “They’re not going to have time. They’re not going to think emotional wellness at this point. It’s not addressed because they don’t have the opportunity to address it. So, it gets buried.”
More rural areas of Haiti were hit hardest by the recent earthquake, which killed over 2,000 people.
Many people were left without shelter and had limited access to food, clean drinking water, and medical help for those severely injured.
But current problems in Haiti, like shaky leadership after the recent assassination of the country’s president, left many people with no direction on what to do next.
With no information coming in, many, like Mr. Verdieu, took to social media or tried calling family and friends to find help on their own.
Having access to basic needs, like food and water, lessens the emotional trauma after these types of disasters, according to Betty Jean, a licensed professional counselor and global mental health and trauma consultant.
“When there is a crisis like an earthquake, the number one thing people need is a sense of safety and that there are entities that are concerned about their overall well-being,” said Ms. Jean, who is Haitian. “The emotional and mental support that we have to provide to people begins first with attending to those primary needs.”
But that’s not always possible in Haiti, mostly because of poor infrastructure, according to Caleb Lucien, founder of Hosean International Ministries.
“For example, the earthquake took place in the south of Haiti,” said Mr. Lucien, who is Haitian. “There has been some gang violence blocking passage from Port-au-Prince [the capital] to the south. Because of the gang fighting, it has been difficult to take the risk of traveling by road. So, airplanes from the capital city have been trying to get supplies there.”
More than resilient
Haitians are usually applauded for their inner strength to keep pushing amid crises. But it’s important to understand that there is often grief behind their resiliency, according to Ms. Jean.
“Sometimes I struggle with that word,” she said. “When I say resilient, I mean they will survive. But we are talking about a traumatized people. I definitely believe the people of Haiti are a people that have PTSD. The Haitian people have not yet fully healed from the first earthquake. I don’t think there was time. And many Haitians are suffering silently right now.”
The trauma shows itself in various ways, said Wilford Marous, entrepreneur and founder of the Haitian Chamber of Commerce in Great Britain.
“I went traveling in Europe with some colleagues of mine to attend some conferences, and one of them, who is Haitian, refused to sleep in a building because he believed it was too high,” he said. “He still had this fear of the earthquake.”
Children are often most affected, Mr. Fitts said.
“They don’t know what to do with it,” he said. “Their parents are not there necessarily to give them the emotional support that they need because they’re just trying to survive when things like this happen. So, a lot of things don’t get addressed and they’re taught early on to move on.”
Hosean International Ministries evacuated 1,500 people after the earthquake in 2010, and 750 of them were kids. The group stayed on the charity’s campground, and children had the chance to continue their education through its school system.
“Kids had issues sleeping,” Mr. Lucien said. “They are dealing with the loss of their loved ones. Some of them lost their moms. Some lost their brothers and sisters. So, we had to work with them and try to get them through that process.”
The charity offered children and their parents counseling sessions to lessen some of the emotional impact after the earthquake.
Common trauma responses
But keep in mind that symptoms like depression and sleeplessness would be common for most people going through mental health crises, such as major natural disasters or war, said Guglielmo Schininà, head of mental health and psychosocial support at the International Organization for Migration.
“It’s important not to jump to conclusions with diagnoses for mental illness or disorders,” Mr. Schininà said. In other situations, psychological effects like these could be symptoms of mental disorders. But in this situation, these are just normal reactions.”
Alongside trauma from natural disasters, many Haitians are angry about the chaos in the country, given the number of resources brought to Haiti over the past decade, according to Ms. Jean.
“We should have had better infrastructure, better roads, lights, emergency plans, trauma hospitals,” she said. “The resources were there.”
The constant lack of safety and security within the country can have ugly outcomes, she said.
“A lot of the political instability, rebels, gang activity, and war within those in politics has been because oppositions feel that those who are in power have not done a very good job of upgrading the Haitian lifestyle,” Ms. Jean said.
Unity and public togetherness are key in times like these, Mr. Marous said. He suggests finding creative ways to promote widespread healing.
“Even if it’s trying to start some sort of healing process through the media,” he said. “Having someone talk to the population, even on TV, 1 hour in the morning. That might be a way to offer some sort of help to the population at large.”
Strategic rebuilding
Haitians across the world are rallying together to keep spirits high, while also helping with recovery efforts, Ms. Jean said.
“We have to step in for the morale of the young people,” she said. “They’re tired. They’re hungry. They want to be cared for. So, our role in the diaspora is really critical in helping Haitians come out of this very traumatic time.”
Hosean International Ministries is organizing and sending supplies to parts of Haiti hardest hit by the earthquake. The ministry is also helping to rebuild some of the homes destroyed by the earthquake.
It’s important to keep in mind lessons learned from past recovery efforts, said Mr. Lucien.
“What we need to do is work with local leaders, asking them exactly what it is that they need,” he said. “The tendency is to rush and say what you’re going to bring. People brought things in 2010 that were not needed. Look for people on the ground, and work with them to provide the help.”
“My call to the international community is how can we come alongside of this resilient nation to alleviate some of the pressure,” Jean said. “But whether or not the help comes, I do believe the Haitian people, yet again, will rise day to day, until we restore and rebuild again.”
This is certainly true for Mr. Verdieu.
He has already launched an online campaign to rebuild his home.
A version of this article first appeared on WebMD.com.
Steeve Verdieu was at his workstation in his bedroom when the shaking started the morning of Aug. 14. He jumped under his desk and held on as a 7.2-magnitude earthquake tore through his childhood home in southern Haiti.
Mr. Verdieu, 25, said all he could think about was 2010, when a strong earthquake hit the country and left more than 200,000 people dead.
“Most of these adults that are in their mid-20s and 30s have vivid memories,” according to John Fitts, assistant director of Sent To Serve. He started working in the nonprofit sector in Haiti after the 2010 earthquake.
“I can’t even relate to it,” Mr. Fitts said. “If you didn’t live through it, you cannot relate.”
Mr. Verdieu emerged to find his family alive and his home in crumbles.
“In the neighborhood, we have only one child who died the day of the earthquake, but mentally, everybody feels bad,” he said. “Also, we are really frustrated right now because it tends to rain, and everybody is outside right now. So, we are a little bit afraid.”
Mr. Verdieu said that his community has not seen or heard of government authorities coming to offer guidance on next steps.
So, he started posting photos and videos to his Twitter account to seek help.
Surviving to heal
Many Haitians are forced to quickly turn the page after major crises, said Mr. Fitts.
“Survival overrides emotional shock,” he said. “They’re not going to have time. They’re not going to think emotional wellness at this point. It’s not addressed because they don’t have the opportunity to address it. So, it gets buried.”
More rural areas of Haiti were hit hardest by the recent earthquake, which killed over 2,000 people.
Many people were left without shelter and had limited access to food, clean drinking water, and medical help for those severely injured.
But current problems in Haiti, like shaky leadership after the recent assassination of the country’s president, left many people with no direction on what to do next.
With no information coming in, many, like Mr. Verdieu, took to social media or tried calling family and friends to find help on their own.
Having access to basic needs, like food and water, lessens the emotional trauma after these types of disasters, according to Betty Jean, a licensed professional counselor and global mental health and trauma consultant.
“When there is a crisis like an earthquake, the number one thing people need is a sense of safety and that there are entities that are concerned about their overall well-being,” said Ms. Jean, who is Haitian. “The emotional and mental support that we have to provide to people begins first with attending to those primary needs.”
But that’s not always possible in Haiti, mostly because of poor infrastructure, according to Caleb Lucien, founder of Hosean International Ministries.
“For example, the earthquake took place in the south of Haiti,” said Mr. Lucien, who is Haitian. “There has been some gang violence blocking passage from Port-au-Prince [the capital] to the south. Because of the gang fighting, it has been difficult to take the risk of traveling by road. So, airplanes from the capital city have been trying to get supplies there.”
More than resilient
Haitians are usually applauded for their inner strength to keep pushing amid crises. But it’s important to understand that there is often grief behind their resiliency, according to Ms. Jean.
“Sometimes I struggle with that word,” she said. “When I say resilient, I mean they will survive. But we are talking about a traumatized people. I definitely believe the people of Haiti are a people that have PTSD. The Haitian people have not yet fully healed from the first earthquake. I don’t think there was time. And many Haitians are suffering silently right now.”
The trauma shows itself in various ways, said Wilford Marous, entrepreneur and founder of the Haitian Chamber of Commerce in Great Britain.
“I went traveling in Europe with some colleagues of mine to attend some conferences, and one of them, who is Haitian, refused to sleep in a building because he believed it was too high,” he said. “He still had this fear of the earthquake.”
Children are often most affected, Mr. Fitts said.
“They don’t know what to do with it,” he said. “Their parents are not there necessarily to give them the emotional support that they need because they’re just trying to survive when things like this happen. So, a lot of things don’t get addressed and they’re taught early on to move on.”
Hosean International Ministries evacuated 1,500 people after the earthquake in 2010, and 750 of them were kids. The group stayed on the charity’s campground, and children had the chance to continue their education through its school system.
“Kids had issues sleeping,” Mr. Lucien said. “They are dealing with the loss of their loved ones. Some of them lost their moms. Some lost their brothers and sisters. So, we had to work with them and try to get them through that process.”
The charity offered children and their parents counseling sessions to lessen some of the emotional impact after the earthquake.
Common trauma responses
But keep in mind that symptoms like depression and sleeplessness would be common for most people going through mental health crises, such as major natural disasters or war, said Guglielmo Schininà, head of mental health and psychosocial support at the International Organization for Migration.
“It’s important not to jump to conclusions with diagnoses for mental illness or disorders,” Mr. Schininà said. In other situations, psychological effects like these could be symptoms of mental disorders. But in this situation, these are just normal reactions.”
Alongside trauma from natural disasters, many Haitians are angry about the chaos in the country, given the number of resources brought to Haiti over the past decade, according to Ms. Jean.
“We should have had better infrastructure, better roads, lights, emergency plans, trauma hospitals,” she said. “The resources were there.”
The constant lack of safety and security within the country can have ugly outcomes, she said.
“A lot of the political instability, rebels, gang activity, and war within those in politics has been because oppositions feel that those who are in power have not done a very good job of upgrading the Haitian lifestyle,” Ms. Jean said.
Unity and public togetherness are key in times like these, Mr. Marous said. He suggests finding creative ways to promote widespread healing.
“Even if it’s trying to start some sort of healing process through the media,” he said. “Having someone talk to the population, even on TV, 1 hour in the morning. That might be a way to offer some sort of help to the population at large.”
Strategic rebuilding
Haitians across the world are rallying together to keep spirits high, while also helping with recovery efforts, Ms. Jean said.
“We have to step in for the morale of the young people,” she said. “They’re tired. They’re hungry. They want to be cared for. So, our role in the diaspora is really critical in helping Haitians come out of this very traumatic time.”
Hosean International Ministries is organizing and sending supplies to parts of Haiti hardest hit by the earthquake. The ministry is also helping to rebuild some of the homes destroyed by the earthquake.
It’s important to keep in mind lessons learned from past recovery efforts, said Mr. Lucien.
“What we need to do is work with local leaders, asking them exactly what it is that they need,” he said. “The tendency is to rush and say what you’re going to bring. People brought things in 2010 that were not needed. Look for people on the ground, and work with them to provide the help.”
“My call to the international community is how can we come alongside of this resilient nation to alleviate some of the pressure,” Jean said. “But whether or not the help comes, I do believe the Haitian people, yet again, will rise day to day, until we restore and rebuild again.”
This is certainly true for Mr. Verdieu.
He has already launched an online campaign to rebuild his home.
A version of this article first appeared on WebMD.com.
Steeve Verdieu was at his workstation in his bedroom when the shaking started the morning of Aug. 14. He jumped under his desk and held on as a 7.2-magnitude earthquake tore through his childhood home in southern Haiti.
Mr. Verdieu, 25, said all he could think about was 2010, when a strong earthquake hit the country and left more than 200,000 people dead.
“Most of these adults that are in their mid-20s and 30s have vivid memories,” according to John Fitts, assistant director of Sent To Serve. He started working in the nonprofit sector in Haiti after the 2010 earthquake.
“I can’t even relate to it,” Mr. Fitts said. “If you didn’t live through it, you cannot relate.”
Mr. Verdieu emerged to find his family alive and his home in crumbles.
“In the neighborhood, we have only one child who died the day of the earthquake, but mentally, everybody feels bad,” he said. “Also, we are really frustrated right now because it tends to rain, and everybody is outside right now. So, we are a little bit afraid.”
Mr. Verdieu said that his community has not seen or heard of government authorities coming to offer guidance on next steps.
So, he started posting photos and videos to his Twitter account to seek help.
Surviving to heal
Many Haitians are forced to quickly turn the page after major crises, said Mr. Fitts.
“Survival overrides emotional shock,” he said. “They’re not going to have time. They’re not going to think emotional wellness at this point. It’s not addressed because they don’t have the opportunity to address it. So, it gets buried.”
More rural areas of Haiti were hit hardest by the recent earthquake, which killed over 2,000 people.
Many people were left without shelter and had limited access to food, clean drinking water, and medical help for those severely injured.
But current problems in Haiti, like shaky leadership after the recent assassination of the country’s president, left many people with no direction on what to do next.
With no information coming in, many, like Mr. Verdieu, took to social media or tried calling family and friends to find help on their own.
Having access to basic needs, like food and water, lessens the emotional trauma after these types of disasters, according to Betty Jean, a licensed professional counselor and global mental health and trauma consultant.
“When there is a crisis like an earthquake, the number one thing people need is a sense of safety and that there are entities that are concerned about their overall well-being,” said Ms. Jean, who is Haitian. “The emotional and mental support that we have to provide to people begins first with attending to those primary needs.”
But that’s not always possible in Haiti, mostly because of poor infrastructure, according to Caleb Lucien, founder of Hosean International Ministries.
“For example, the earthquake took place in the south of Haiti,” said Mr. Lucien, who is Haitian. “There has been some gang violence blocking passage from Port-au-Prince [the capital] to the south. Because of the gang fighting, it has been difficult to take the risk of traveling by road. So, airplanes from the capital city have been trying to get supplies there.”
More than resilient
Haitians are usually applauded for their inner strength to keep pushing amid crises. But it’s important to understand that there is often grief behind their resiliency, according to Ms. Jean.
“Sometimes I struggle with that word,” she said. “When I say resilient, I mean they will survive. But we are talking about a traumatized people. I definitely believe the people of Haiti are a people that have PTSD. The Haitian people have not yet fully healed from the first earthquake. I don’t think there was time. And many Haitians are suffering silently right now.”
The trauma shows itself in various ways, said Wilford Marous, entrepreneur and founder of the Haitian Chamber of Commerce in Great Britain.
“I went traveling in Europe with some colleagues of mine to attend some conferences, and one of them, who is Haitian, refused to sleep in a building because he believed it was too high,” he said. “He still had this fear of the earthquake.”
Children are often most affected, Mr. Fitts said.
“They don’t know what to do with it,” he said. “Their parents are not there necessarily to give them the emotional support that they need because they’re just trying to survive when things like this happen. So, a lot of things don’t get addressed and they’re taught early on to move on.”
Hosean International Ministries evacuated 1,500 people after the earthquake in 2010, and 750 of them were kids. The group stayed on the charity’s campground, and children had the chance to continue their education through its school system.
“Kids had issues sleeping,” Mr. Lucien said. “They are dealing with the loss of their loved ones. Some of them lost their moms. Some lost their brothers and sisters. So, we had to work with them and try to get them through that process.”
The charity offered children and their parents counseling sessions to lessen some of the emotional impact after the earthquake.
Common trauma responses
But keep in mind that symptoms like depression and sleeplessness would be common for most people going through mental health crises, such as major natural disasters or war, said Guglielmo Schininà, head of mental health and psychosocial support at the International Organization for Migration.
“It’s important not to jump to conclusions with diagnoses for mental illness or disorders,” Mr. Schininà said. In other situations, psychological effects like these could be symptoms of mental disorders. But in this situation, these are just normal reactions.”
Alongside trauma from natural disasters, many Haitians are angry about the chaos in the country, given the number of resources brought to Haiti over the past decade, according to Ms. Jean.
“We should have had better infrastructure, better roads, lights, emergency plans, trauma hospitals,” she said. “The resources were there.”
The constant lack of safety and security within the country can have ugly outcomes, she said.
“A lot of the political instability, rebels, gang activity, and war within those in politics has been because oppositions feel that those who are in power have not done a very good job of upgrading the Haitian lifestyle,” Ms. Jean said.
Unity and public togetherness are key in times like these, Mr. Marous said. He suggests finding creative ways to promote widespread healing.
“Even if it’s trying to start some sort of healing process through the media,” he said. “Having someone talk to the population, even on TV, 1 hour in the morning. That might be a way to offer some sort of help to the population at large.”
Strategic rebuilding
Haitians across the world are rallying together to keep spirits high, while also helping with recovery efforts, Ms. Jean said.
“We have to step in for the morale of the young people,” she said. “They’re tired. They’re hungry. They want to be cared for. So, our role in the diaspora is really critical in helping Haitians come out of this very traumatic time.”
Hosean International Ministries is organizing and sending supplies to parts of Haiti hardest hit by the earthquake. The ministry is also helping to rebuild some of the homes destroyed by the earthquake.
It’s important to keep in mind lessons learned from past recovery efforts, said Mr. Lucien.
“What we need to do is work with local leaders, asking them exactly what it is that they need,” he said. “The tendency is to rush and say what you’re going to bring. People brought things in 2010 that were not needed. Look for people on the ground, and work with them to provide the help.”
“My call to the international community is how can we come alongside of this resilient nation to alleviate some of the pressure,” Jean said. “But whether or not the help comes, I do believe the Haitian people, yet again, will rise day to day, until we restore and rebuild again.”
This is certainly true for Mr. Verdieu.
He has already launched an online campaign to rebuild his home.
A version of this article first appeared on WebMD.com.
Psychotic features among older adults tied to Parkinson’s
Adults aged 65 years and older who develop psychotic manifestations are significantly more likely than those without such manifestations to develop prodromal Parkinson’s disease, data from 925 individuals suggest.
“The presence of perceptual abnormalities and/or delusional ideation among community-dwelling elderly individuals is more widespread than considered in the past,” wrote Ioanna Pachi, MD, of National and Kapodistrian University of Athens Medical School and colleagues. However, those psychoses and their potential impact on prodromal Parkinson’s disease (PD) have not been well studied in community-dwelling populations, they noted in the study, published in Parkinsonism and Related Disorders.
In the study, Dr. Pachi and colleagues reviewed data from 914 participants in the Hellenic Longitudinal Investigation of Aging and Diet study (HELIAD), a cross-sectional, population-based cohort study of older adults in Greece. The average age of the participants was 76 years, and 41% were men. Participants had no delusional features at baseline; delusional features were assessed using the Neuropsychiatric Inventory scale and the Columbia University Scale for Psychopathology in Alzheimer’s disease. The researchers calculated the probability of prodromal PD (pPD) for each participant based on the 2019 International Parkinson and Movement Disorders Society research criteria for prodromal PD.
Over a 3-year follow-up period, 20 participants developed psychotic manifestations and were 1.3 times more likely to have pPD, compared with those without psychoses (P = .006). Those with new-onset psychotic features were categorized together as the NPSY group, regardless of symptom severity or frequency; those with no symptoms at either baseline or during follow-up were categorized as unaffected (UPSY). Most of the NPSY participants showed isolated delusional features, although some expressed hallucinations. Most symptoms were mild.
New-onset psychosis was associated with a fivefold increased risk of both subthreshold parkinsonism and depression (adjusted odds ratios, 4.5 and 5.0, respectively) and with a threefold increased risk of constipation (aOR 2.6). Other factors, including nonsmoking, global cognitive deficit, and anxiety were not significantly associated with new-onset psychotic symptoms after adjusting for confounding factors.
Although the mechanism behind the association remains unclear,
The study findings were limited by several factors, including the administration of neuropsychiatric questionnaires by nonpsychiatrists, and lack of detailed psychiatric history, including complete information on medication use, the researchers noted. The small size of the NPSY group also prevented evaluation of the potential associations between pPD and different modalities of hallucinations, they said.
However, the results were strengthened by the overall large and population-based sample size, and the comprehensive evaluation of psychotic features, they wrote. More follow-up evaluations in the HELIAD cohort are planned to further explore the underlying mechanism of the association between late-life psychosis and pPD.
“Provided that these results are confirmed in other community cohorts of elderly subjects, psychotic features may be added to the list of manifestations of pPD,” they concluded.
The study was supported in part by grants from the Alzheimer’s Association, ARISTEIA, and the ESPA-EU program Excellence Grant. It was cofunded by the European Social Fund and Greek National resources, the Ministry for Health and Social Solidarity, Greece, and the Greek State Scholarships Foundation. Dr. Pachi had no disclosures.
Adults aged 65 years and older who develop psychotic manifestations are significantly more likely than those without such manifestations to develop prodromal Parkinson’s disease, data from 925 individuals suggest.
“The presence of perceptual abnormalities and/or delusional ideation among community-dwelling elderly individuals is more widespread than considered in the past,” wrote Ioanna Pachi, MD, of National and Kapodistrian University of Athens Medical School and colleagues. However, those psychoses and their potential impact on prodromal Parkinson’s disease (PD) have not been well studied in community-dwelling populations, they noted in the study, published in Parkinsonism and Related Disorders.
In the study, Dr. Pachi and colleagues reviewed data from 914 participants in the Hellenic Longitudinal Investigation of Aging and Diet study (HELIAD), a cross-sectional, population-based cohort study of older adults in Greece. The average age of the participants was 76 years, and 41% were men. Participants had no delusional features at baseline; delusional features were assessed using the Neuropsychiatric Inventory scale and the Columbia University Scale for Psychopathology in Alzheimer’s disease. The researchers calculated the probability of prodromal PD (pPD) for each participant based on the 2019 International Parkinson and Movement Disorders Society research criteria for prodromal PD.
Over a 3-year follow-up period, 20 participants developed psychotic manifestations and were 1.3 times more likely to have pPD, compared with those without psychoses (P = .006). Those with new-onset psychotic features were categorized together as the NPSY group, regardless of symptom severity or frequency; those with no symptoms at either baseline or during follow-up were categorized as unaffected (UPSY). Most of the NPSY participants showed isolated delusional features, although some expressed hallucinations. Most symptoms were mild.
New-onset psychosis was associated with a fivefold increased risk of both subthreshold parkinsonism and depression (adjusted odds ratios, 4.5 and 5.0, respectively) and with a threefold increased risk of constipation (aOR 2.6). Other factors, including nonsmoking, global cognitive deficit, and anxiety were not significantly associated with new-onset psychotic symptoms after adjusting for confounding factors.
Although the mechanism behind the association remains unclear,
The study findings were limited by several factors, including the administration of neuropsychiatric questionnaires by nonpsychiatrists, and lack of detailed psychiatric history, including complete information on medication use, the researchers noted. The small size of the NPSY group also prevented evaluation of the potential associations between pPD and different modalities of hallucinations, they said.
However, the results were strengthened by the overall large and population-based sample size, and the comprehensive evaluation of psychotic features, they wrote. More follow-up evaluations in the HELIAD cohort are planned to further explore the underlying mechanism of the association between late-life psychosis and pPD.
“Provided that these results are confirmed in other community cohorts of elderly subjects, psychotic features may be added to the list of manifestations of pPD,” they concluded.
The study was supported in part by grants from the Alzheimer’s Association, ARISTEIA, and the ESPA-EU program Excellence Grant. It was cofunded by the European Social Fund and Greek National resources, the Ministry for Health and Social Solidarity, Greece, and the Greek State Scholarships Foundation. Dr. Pachi had no disclosures.
Adults aged 65 years and older who develop psychotic manifestations are significantly more likely than those without such manifestations to develop prodromal Parkinson’s disease, data from 925 individuals suggest.
“The presence of perceptual abnormalities and/or delusional ideation among community-dwelling elderly individuals is more widespread than considered in the past,” wrote Ioanna Pachi, MD, of National and Kapodistrian University of Athens Medical School and colleagues. However, those psychoses and their potential impact on prodromal Parkinson’s disease (PD) have not been well studied in community-dwelling populations, they noted in the study, published in Parkinsonism and Related Disorders.
In the study, Dr. Pachi and colleagues reviewed data from 914 participants in the Hellenic Longitudinal Investigation of Aging and Diet study (HELIAD), a cross-sectional, population-based cohort study of older adults in Greece. The average age of the participants was 76 years, and 41% were men. Participants had no delusional features at baseline; delusional features were assessed using the Neuropsychiatric Inventory scale and the Columbia University Scale for Psychopathology in Alzheimer’s disease. The researchers calculated the probability of prodromal PD (pPD) for each participant based on the 2019 International Parkinson and Movement Disorders Society research criteria for prodromal PD.
Over a 3-year follow-up period, 20 participants developed psychotic manifestations and were 1.3 times more likely to have pPD, compared with those without psychoses (P = .006). Those with new-onset psychotic features were categorized together as the NPSY group, regardless of symptom severity or frequency; those with no symptoms at either baseline or during follow-up were categorized as unaffected (UPSY). Most of the NPSY participants showed isolated delusional features, although some expressed hallucinations. Most symptoms were mild.
New-onset psychosis was associated with a fivefold increased risk of both subthreshold parkinsonism and depression (adjusted odds ratios, 4.5 and 5.0, respectively) and with a threefold increased risk of constipation (aOR 2.6). Other factors, including nonsmoking, global cognitive deficit, and anxiety were not significantly associated with new-onset psychotic symptoms after adjusting for confounding factors.
Although the mechanism behind the association remains unclear,
The study findings were limited by several factors, including the administration of neuropsychiatric questionnaires by nonpsychiatrists, and lack of detailed psychiatric history, including complete information on medication use, the researchers noted. The small size of the NPSY group also prevented evaluation of the potential associations between pPD and different modalities of hallucinations, they said.
However, the results were strengthened by the overall large and population-based sample size, and the comprehensive evaluation of psychotic features, they wrote. More follow-up evaluations in the HELIAD cohort are planned to further explore the underlying mechanism of the association between late-life psychosis and pPD.
“Provided that these results are confirmed in other community cohorts of elderly subjects, psychotic features may be added to the list of manifestations of pPD,” they concluded.
The study was supported in part by grants from the Alzheimer’s Association, ARISTEIA, and the ESPA-EU program Excellence Grant. It was cofunded by the European Social Fund and Greek National resources, the Ministry for Health and Social Solidarity, Greece, and the Greek State Scholarships Foundation. Dr. Pachi had no disclosures.
FROM PARKINSONISM AND RELATED DISORDERS
Low depression scores may miss seniors with suicidal intent
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
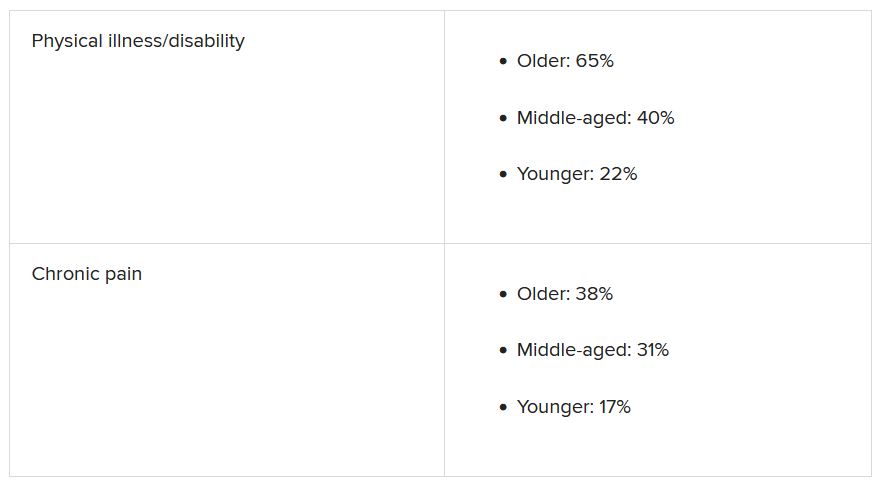
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
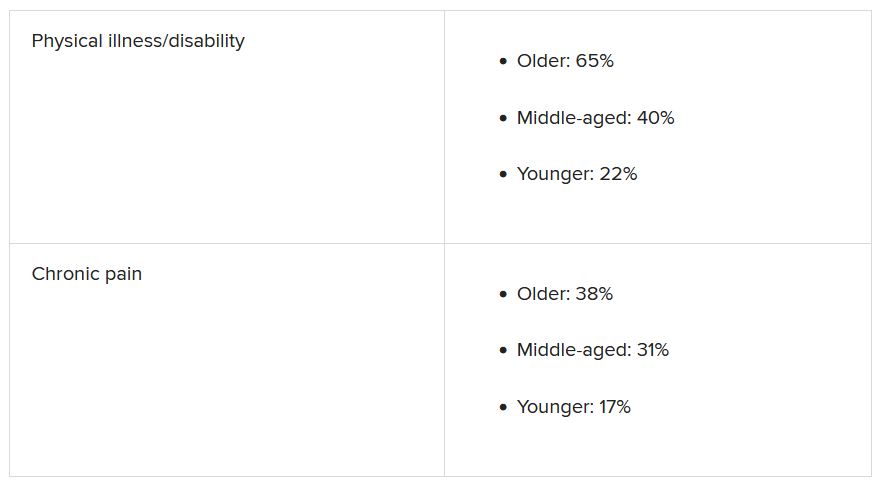
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
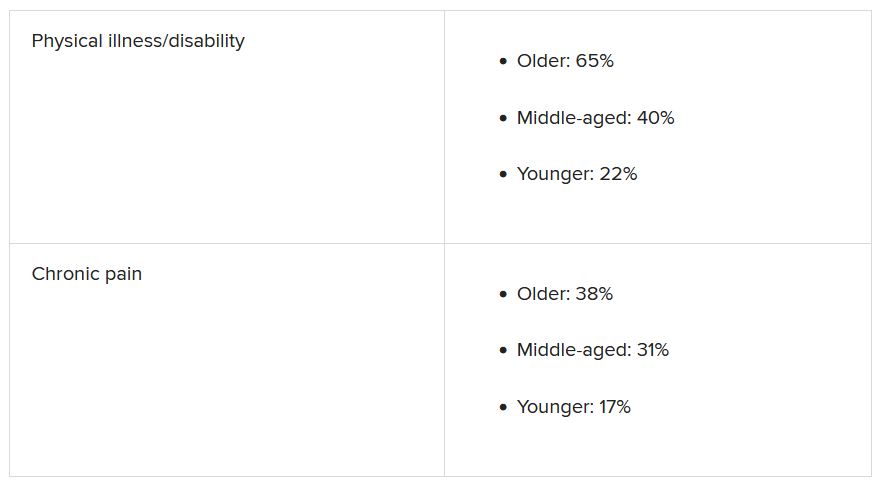
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The hateful patient
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
FDA OKs stimulation device for anxiety in depression
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.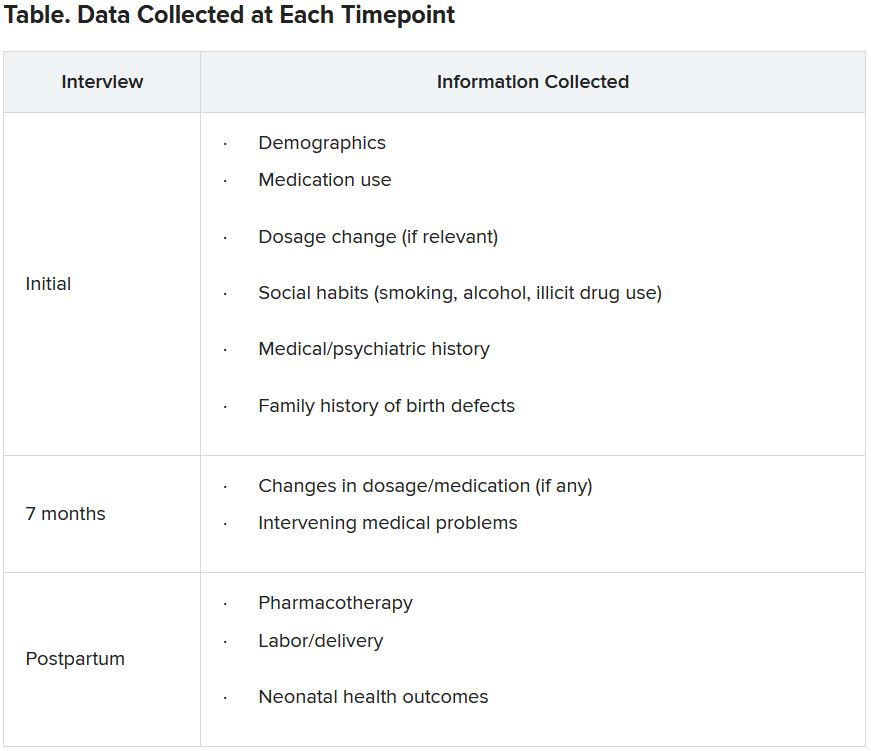
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.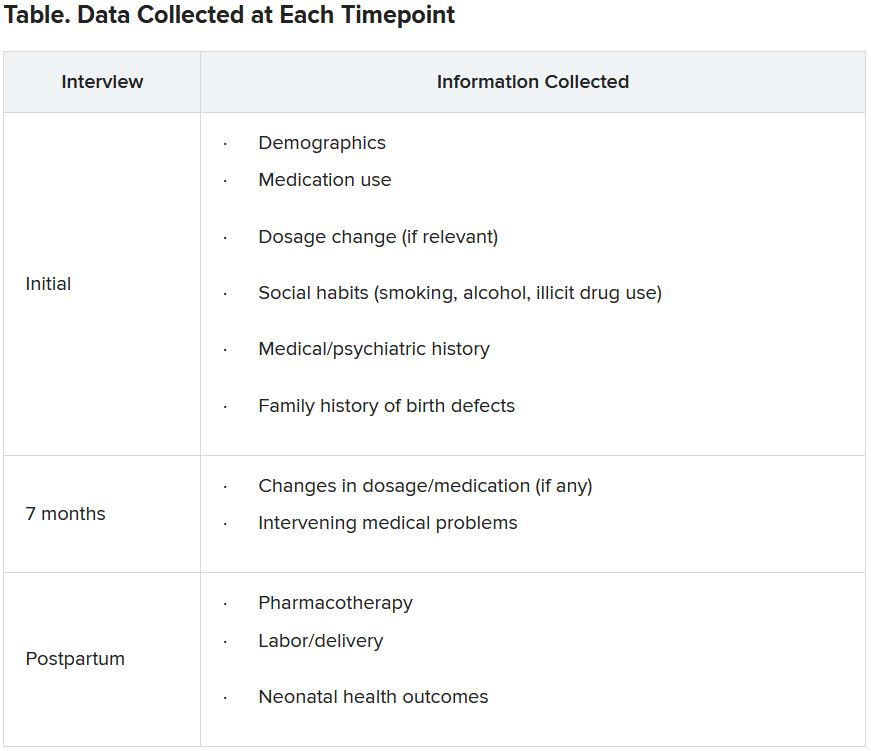
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.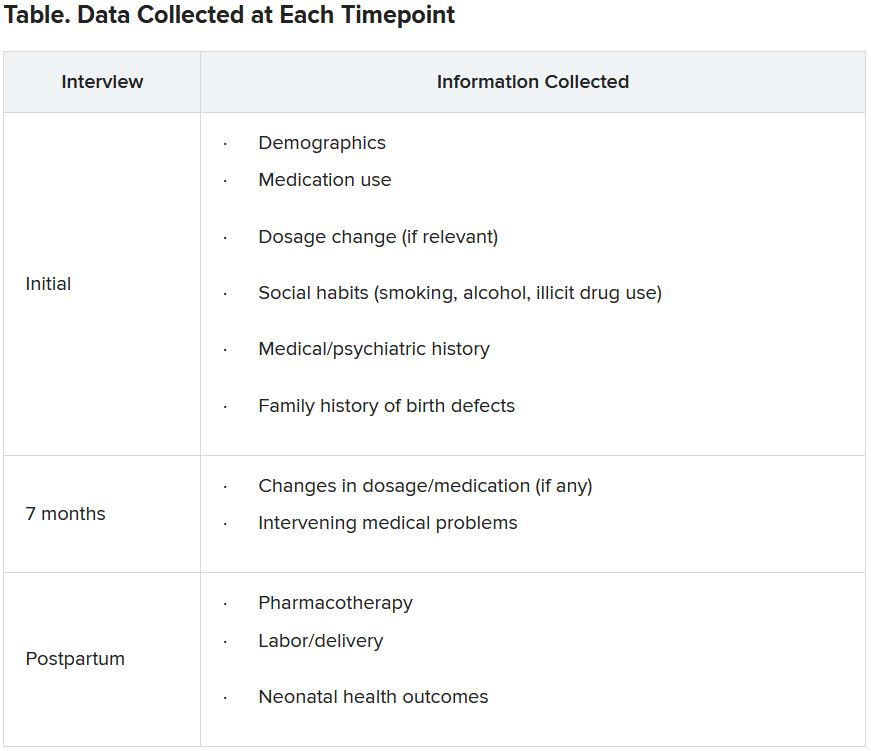
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Shedding the super-doctor myth requires an honest look at systemic racism
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Is this a psychiatric emergency? How to screen, assess, and triage safety concerns from the primary care office
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.












