User login
Core behaviors enhance communication about neonatal death
Clinicians can improve communications with parents during neonatal end-of-life situations by adopting key behaviors such as sitting down to talk to parents and using the infant’s name, according to data from a simulation study.
“Empirical evidence regarding communication with parents during and after a child’s critical instability or death is scarce,” wrote Marie-Hélène Lizotte, MD, of Centre Hospitalier Universitaire Sainte-Justine, Montréal, and colleagues. Noting that realistic simulation has been shown to help clinicians improve their communication skills, the investigators recruited clinicians to participate in a simulated unsuccessful neonatal resuscitation to identify behaviors associated with optimal parent communication.
Behaviors associated with high scores for clinicians deemed “good communicators” included introducing themselves to parents, using the infant’s name (if known), sitting down to speak to parents, not leaving the infant alone on the bed after death, and allowing time for silence, the researchers reported in Pediatrics.
The investigators presented the video simulations to evaluators, including clinicians and bereaved parents. In the simulation, a term infant was born after an emergency cesarean delivery for fetal distress and died after an unsuccessful attempt at resuscitation. A manikin infant was programmed to remain pulseless, and two actors played the roles of the parents in the video.
Evaluators scored the videos for overall performance and for communication with the parent actors during and after the resuscitation.
Overall, parent evaluators and parent actors agreed with clinicians on what actions exemplified optimal communication in about 81% of evaluations. Discrepancies were mainly related to the language participants used related to death, as some parent evaluators said they had trouble understanding certain sentences or found them insensitive, such as “her heart never came back” and “allowing natural death.”
A total of 31 participants were recruited for the simulation, including 15 pediatric residents, 5 neonatal fellows, 3 neonatologists, 3 neonatal nurse practitioners, and 5 transport and resuscitation team providers. Videos of the simulations were examined by 21 evaluators, including bereaved parents, the parent actors, a neonatologist, a maternal-fetal medicine specialist, a psychologist, and a respiratory therapist. There were 651 evaluations.
The study findings were limited by several factors including the use of a single center, use of videos for evaluations, and the use of a single infant-resuscitation scenario, the researchers noted. The results were strengthened, however, by the large number of evaluations, and they support the core behaviors as “a skeleton on which to build additional skills with practice and training” with attention to cultural differences in their application, such as recognizing that infants are not named until after birth in some cultures, they said.
The existing literature on strategies for providing empathy and support to parents facing the death of a child is limited, but this simulation study provides a design model to help address this issue, Chris Feudtner, MD, of the Children’s Hospital of Philadelphia wrote in an accompanying editorial. “Overall, this study, in terms of design and methodologic rigor, is a great advance toward answering our key question: how to best support parents in such circumstances,” he said.
Dr. Feudtner said that he would divide the clinician behaviors into two groups. The first, “Calm kind politeness,” includes acknowledging the parents, introducing themselves, using the infant’s name, and remaining calm. The second set of behaviors, which he called “Skillful situational leadership,” includes preparing parents for the resuscitation activities and providing verbal milestones that prepared them for the fatal outcome.
“Picking up on a metaphor offered by the authors of the study, training and repetitive drills on these specific behaviors cannot be emphasized enough because they are not only the skeleton of excellent communication; they are likely also the muscles, the heart, and even the soul,” he concluded.
The study was supported by a grant from the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and Dr. Feudtner reported no financial conflicts.
SOURCE: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
Clinicians can improve communications with parents during neonatal end-of-life situations by adopting key behaviors such as sitting down to talk to parents and using the infant’s name, according to data from a simulation study.
“Empirical evidence regarding communication with parents during and after a child’s critical instability or death is scarce,” wrote Marie-Hélène Lizotte, MD, of Centre Hospitalier Universitaire Sainte-Justine, Montréal, and colleagues. Noting that realistic simulation has been shown to help clinicians improve their communication skills, the investigators recruited clinicians to participate in a simulated unsuccessful neonatal resuscitation to identify behaviors associated with optimal parent communication.
Behaviors associated with high scores for clinicians deemed “good communicators” included introducing themselves to parents, using the infant’s name (if known), sitting down to speak to parents, not leaving the infant alone on the bed after death, and allowing time for silence, the researchers reported in Pediatrics.
The investigators presented the video simulations to evaluators, including clinicians and bereaved parents. In the simulation, a term infant was born after an emergency cesarean delivery for fetal distress and died after an unsuccessful attempt at resuscitation. A manikin infant was programmed to remain pulseless, and two actors played the roles of the parents in the video.
Evaluators scored the videos for overall performance and for communication with the parent actors during and after the resuscitation.
Overall, parent evaluators and parent actors agreed with clinicians on what actions exemplified optimal communication in about 81% of evaluations. Discrepancies were mainly related to the language participants used related to death, as some parent evaluators said they had trouble understanding certain sentences or found them insensitive, such as “her heart never came back” and “allowing natural death.”
A total of 31 participants were recruited for the simulation, including 15 pediatric residents, 5 neonatal fellows, 3 neonatologists, 3 neonatal nurse practitioners, and 5 transport and resuscitation team providers. Videos of the simulations were examined by 21 evaluators, including bereaved parents, the parent actors, a neonatologist, a maternal-fetal medicine specialist, a psychologist, and a respiratory therapist. There were 651 evaluations.
The study findings were limited by several factors including the use of a single center, use of videos for evaluations, and the use of a single infant-resuscitation scenario, the researchers noted. The results were strengthened, however, by the large number of evaluations, and they support the core behaviors as “a skeleton on which to build additional skills with practice and training” with attention to cultural differences in their application, such as recognizing that infants are not named until after birth in some cultures, they said.
The existing literature on strategies for providing empathy and support to parents facing the death of a child is limited, but this simulation study provides a design model to help address this issue, Chris Feudtner, MD, of the Children’s Hospital of Philadelphia wrote in an accompanying editorial. “Overall, this study, in terms of design and methodologic rigor, is a great advance toward answering our key question: how to best support parents in such circumstances,” he said.
Dr. Feudtner said that he would divide the clinician behaviors into two groups. The first, “Calm kind politeness,” includes acknowledging the parents, introducing themselves, using the infant’s name, and remaining calm. The second set of behaviors, which he called “Skillful situational leadership,” includes preparing parents for the resuscitation activities and providing verbal milestones that prepared them for the fatal outcome.
“Picking up on a metaphor offered by the authors of the study, training and repetitive drills on these specific behaviors cannot be emphasized enough because they are not only the skeleton of excellent communication; they are likely also the muscles, the heart, and even the soul,” he concluded.
The study was supported by a grant from the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and Dr. Feudtner reported no financial conflicts.
SOURCE: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
Clinicians can improve communications with parents during neonatal end-of-life situations by adopting key behaviors such as sitting down to talk to parents and using the infant’s name, according to data from a simulation study.
“Empirical evidence regarding communication with parents during and after a child’s critical instability or death is scarce,” wrote Marie-Hélène Lizotte, MD, of Centre Hospitalier Universitaire Sainte-Justine, Montréal, and colleagues. Noting that realistic simulation has been shown to help clinicians improve their communication skills, the investigators recruited clinicians to participate in a simulated unsuccessful neonatal resuscitation to identify behaviors associated with optimal parent communication.
Behaviors associated with high scores for clinicians deemed “good communicators” included introducing themselves to parents, using the infant’s name (if known), sitting down to speak to parents, not leaving the infant alone on the bed after death, and allowing time for silence, the researchers reported in Pediatrics.
The investigators presented the video simulations to evaluators, including clinicians and bereaved parents. In the simulation, a term infant was born after an emergency cesarean delivery for fetal distress and died after an unsuccessful attempt at resuscitation. A manikin infant was programmed to remain pulseless, and two actors played the roles of the parents in the video.
Evaluators scored the videos for overall performance and for communication with the parent actors during and after the resuscitation.
Overall, parent evaluators and parent actors agreed with clinicians on what actions exemplified optimal communication in about 81% of evaluations. Discrepancies were mainly related to the language participants used related to death, as some parent evaluators said they had trouble understanding certain sentences or found them insensitive, such as “her heart never came back” and “allowing natural death.”
A total of 31 participants were recruited for the simulation, including 15 pediatric residents, 5 neonatal fellows, 3 neonatologists, 3 neonatal nurse practitioners, and 5 transport and resuscitation team providers. Videos of the simulations were examined by 21 evaluators, including bereaved parents, the parent actors, a neonatologist, a maternal-fetal medicine specialist, a psychologist, and a respiratory therapist. There were 651 evaluations.
The study findings were limited by several factors including the use of a single center, use of videos for evaluations, and the use of a single infant-resuscitation scenario, the researchers noted. The results were strengthened, however, by the large number of evaluations, and they support the core behaviors as “a skeleton on which to build additional skills with practice and training” with attention to cultural differences in their application, such as recognizing that infants are not named until after birth in some cultures, they said.
The existing literature on strategies for providing empathy and support to parents facing the death of a child is limited, but this simulation study provides a design model to help address this issue, Chris Feudtner, MD, of the Children’s Hospital of Philadelphia wrote in an accompanying editorial. “Overall, this study, in terms of design and methodologic rigor, is a great advance toward answering our key question: how to best support parents in such circumstances,” he said.
Dr. Feudtner said that he would divide the clinician behaviors into two groups. The first, “Calm kind politeness,” includes acknowledging the parents, introducing themselves, using the infant’s name, and remaining calm. The second set of behaviors, which he called “Skillful situational leadership,” includes preparing parents for the resuscitation activities and providing verbal milestones that prepared them for the fatal outcome.
“Picking up on a metaphor offered by the authors of the study, training and repetitive drills on these specific behaviors cannot be emphasized enough because they are not only the skeleton of excellent communication; they are likely also the muscles, the heart, and even the soul,” he concluded.
The study was supported by a grant from the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and Dr. Feudtner reported no financial conflicts.
SOURCE: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
FROM PEDIATRICS
Key clinical point: Clinicians who took steps such as sitting down and using the infant’s name were seen by parents as good communicators.
Major finding: Evaluators of a simulation agreed 81% of the time on defining optimal communication.
Study details: The data come from a simulation study of 31 participants and 21 evaluators and a total of 651 evaluations.
Disclosures: The study was supported in part by the Fonds de Recherche en Santé du Québec and the Medical Education Grant from Centre Hospitalier Universitaire Sainte-Justine. The researchers and editorialist said they had no financial conflicts.
Source: Lizotte M-H et al. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-1925; Feudtner C. Pediatrics. 2020 Jan 27. doi: 10.1542/peds.2019-3116.
Infant deaths from birth defects decline, but some disparities widen
according to the Centers for Disease Control and Prevention.
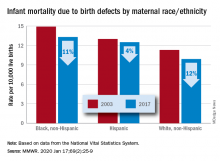
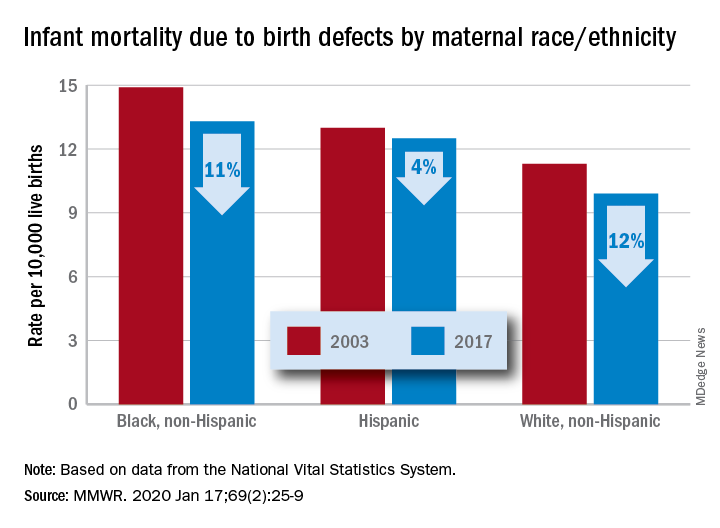
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
FROM MMWR
Cognitive problems after extremely preterm birth persist
Cognitive and neuropsychological impairment associated with extremely preterm (EP) birth persists into young adulthood, according to findings from the 1995 EPICure cohort.
Of note, intellectual impairment increased significantly after the age of 11 years among 19-year-olds in the cohort of individuals born EP, Helen O’Reilly, PhD, of the Institute for Women’s Health at University College London and colleagues reported in Pediatrics.
Neuropsychological assessment to examine general cognitive abilities, visuomotor abilities, prospective memory, and certain aspects of executive functioning and language in 127 cases and 64 term-born controls showed significantly lower scores across all tests in those born EP.
Impairment in at least one neuropsychological domain was present in 60% of EP birth cases (compared with 21% of controls), with 35% having impairment in at least four domains. Most deficits occurred in general cognitive function and/or visuomotor abilities.
Further, and those with cognitive impairment at 11 years were at increased risk of deficit at 19 years (RR, 3.56), even after adjustment for sex and socioeconomic status, the authors wrote.
None of the term-born controls had a cognitive impairment at 11 years, and two (3%) had impairment at 19 years.
Studies of adults born very preterm have revealed that these individuals are at risk for neuropsychological impairment, but the extent of such impairment in individuals with EP birth, defined as birth before 26 weeks’ gestation, had not previously been studied in the long term.
Assessments in the EPICure cohort of individuals born EP in 1995 previously showed scores at 1.1-1.6 standard deviations lower on measures of general cognitive function, compared with standardized norms and/or term-born controls, at age 2.5, 6, and 11 years, Dr. O’Reilly and colleagues explained.
The current findings indicate that general cognitive and neuropsychological functioning problems associated with EP birth persist and can increase into early adulthood, and they “highlight the need for early and ongoing neuropsychological and educational assessment in EP children to ensure these children receive appropriate support in school and for planned educational pathways,” the investigators concluded.
In an accompanying editorial, Louis A. Schmidt, PhD, and Saroj Saigal, MD, of McMaster University, Hamilton, Ont., wrote that these findings “provide compelling evidence for persistent effects of cognitive impairments” in individuals born EP.
They highlighted three lessons from the study:
- It is important to control for anxiety in future studies like this “to eliminate potential confounding influences of anxiety when examining performance-based measures in the laboratory setting,” as individuals born EP are known to exhibit anxiety.
- Group heterogeneity also should be considered, as all survivors of prematurity are not alike.
- Measurement equivalency should be established between groups.
With respect to the latter, “although many of the measures used by O’Reilly et al. have been normed, issues of measurement invariance have not been established between EP and control groups on some of the measures reported,” Dr. Schmidt and Dr. Saigal wrote, noting that “many other studies [also] fail to consider this fundamental measurement property.”
“Considering issues of measurement equivalency is of critical importance to ensuring unbiased interpretations of findings,” they added, concluding that the findings by O’Reilly et al. represent an important contribution and confirm findings from many prior studies of extreme prematurity, which “informs how we effectively manage these problems.”
“As the percentage of preterm birth continues to rise worldwide, coupled with reduced morbidity and mortality, and with more EP infants reaching adulthood, there is a need for prospective, long-term outcome studies of extreme prematurity,” Dr. Schmidt and Dr. Saigal added.
The study was funded by the Medical Research Council United Kingdom. The authors reported having no relevant financial disclosures. The editorial by Dr. Schmidt and Dr. Saigal, who also reported having no relevant financial disclosures, was supported by the Canadian Institutes of Health Research.
SOURCES: O’Reilly H et al. Pediatrics. 2020;145(2):e20192087; Schmidt LA, Saigal S. Pediatrics. 2020;145(2):e20193359.
Cognitive and neuropsychological impairment associated with extremely preterm (EP) birth persists into young adulthood, according to findings from the 1995 EPICure cohort.
Of note, intellectual impairment increased significantly after the age of 11 years among 19-year-olds in the cohort of individuals born EP, Helen O’Reilly, PhD, of the Institute for Women’s Health at University College London and colleagues reported in Pediatrics.
Neuropsychological assessment to examine general cognitive abilities, visuomotor abilities, prospective memory, and certain aspects of executive functioning and language in 127 cases and 64 term-born controls showed significantly lower scores across all tests in those born EP.
Impairment in at least one neuropsychological domain was present in 60% of EP birth cases (compared with 21% of controls), with 35% having impairment in at least four domains. Most deficits occurred in general cognitive function and/or visuomotor abilities.
Further, and those with cognitive impairment at 11 years were at increased risk of deficit at 19 years (RR, 3.56), even after adjustment for sex and socioeconomic status, the authors wrote.
None of the term-born controls had a cognitive impairment at 11 years, and two (3%) had impairment at 19 years.
Studies of adults born very preterm have revealed that these individuals are at risk for neuropsychological impairment, but the extent of such impairment in individuals with EP birth, defined as birth before 26 weeks’ gestation, had not previously been studied in the long term.
Assessments in the EPICure cohort of individuals born EP in 1995 previously showed scores at 1.1-1.6 standard deviations lower on measures of general cognitive function, compared with standardized norms and/or term-born controls, at age 2.5, 6, and 11 years, Dr. O’Reilly and colleagues explained.
The current findings indicate that general cognitive and neuropsychological functioning problems associated with EP birth persist and can increase into early adulthood, and they “highlight the need for early and ongoing neuropsychological and educational assessment in EP children to ensure these children receive appropriate support in school and for planned educational pathways,” the investigators concluded.
In an accompanying editorial, Louis A. Schmidt, PhD, and Saroj Saigal, MD, of McMaster University, Hamilton, Ont., wrote that these findings “provide compelling evidence for persistent effects of cognitive impairments” in individuals born EP.
They highlighted three lessons from the study:
- It is important to control for anxiety in future studies like this “to eliminate potential confounding influences of anxiety when examining performance-based measures in the laboratory setting,” as individuals born EP are known to exhibit anxiety.
- Group heterogeneity also should be considered, as all survivors of prematurity are not alike.
- Measurement equivalency should be established between groups.
With respect to the latter, “although many of the measures used by O’Reilly et al. have been normed, issues of measurement invariance have not been established between EP and control groups on some of the measures reported,” Dr. Schmidt and Dr. Saigal wrote, noting that “many other studies [also] fail to consider this fundamental measurement property.”
“Considering issues of measurement equivalency is of critical importance to ensuring unbiased interpretations of findings,” they added, concluding that the findings by O’Reilly et al. represent an important contribution and confirm findings from many prior studies of extreme prematurity, which “informs how we effectively manage these problems.”
“As the percentage of preterm birth continues to rise worldwide, coupled with reduced morbidity and mortality, and with more EP infants reaching adulthood, there is a need for prospective, long-term outcome studies of extreme prematurity,” Dr. Schmidt and Dr. Saigal added.
The study was funded by the Medical Research Council United Kingdom. The authors reported having no relevant financial disclosures. The editorial by Dr. Schmidt and Dr. Saigal, who also reported having no relevant financial disclosures, was supported by the Canadian Institutes of Health Research.
SOURCES: O’Reilly H et al. Pediatrics. 2020;145(2):e20192087; Schmidt LA, Saigal S. Pediatrics. 2020;145(2):e20193359.
Cognitive and neuropsychological impairment associated with extremely preterm (EP) birth persists into young adulthood, according to findings from the 1995 EPICure cohort.
Of note, intellectual impairment increased significantly after the age of 11 years among 19-year-olds in the cohort of individuals born EP, Helen O’Reilly, PhD, of the Institute for Women’s Health at University College London and colleagues reported in Pediatrics.
Neuropsychological assessment to examine general cognitive abilities, visuomotor abilities, prospective memory, and certain aspects of executive functioning and language in 127 cases and 64 term-born controls showed significantly lower scores across all tests in those born EP.
Impairment in at least one neuropsychological domain was present in 60% of EP birth cases (compared with 21% of controls), with 35% having impairment in at least four domains. Most deficits occurred in general cognitive function and/or visuomotor abilities.
Further, and those with cognitive impairment at 11 years were at increased risk of deficit at 19 years (RR, 3.56), even after adjustment for sex and socioeconomic status, the authors wrote.
None of the term-born controls had a cognitive impairment at 11 years, and two (3%) had impairment at 19 years.
Studies of adults born very preterm have revealed that these individuals are at risk for neuropsychological impairment, but the extent of such impairment in individuals with EP birth, defined as birth before 26 weeks’ gestation, had not previously been studied in the long term.
Assessments in the EPICure cohort of individuals born EP in 1995 previously showed scores at 1.1-1.6 standard deviations lower on measures of general cognitive function, compared with standardized norms and/or term-born controls, at age 2.5, 6, and 11 years, Dr. O’Reilly and colleagues explained.
The current findings indicate that general cognitive and neuropsychological functioning problems associated with EP birth persist and can increase into early adulthood, and they “highlight the need for early and ongoing neuropsychological and educational assessment in EP children to ensure these children receive appropriate support in school and for planned educational pathways,” the investigators concluded.
In an accompanying editorial, Louis A. Schmidt, PhD, and Saroj Saigal, MD, of McMaster University, Hamilton, Ont., wrote that these findings “provide compelling evidence for persistent effects of cognitive impairments” in individuals born EP.
They highlighted three lessons from the study:
- It is important to control for anxiety in future studies like this “to eliminate potential confounding influences of anxiety when examining performance-based measures in the laboratory setting,” as individuals born EP are known to exhibit anxiety.
- Group heterogeneity also should be considered, as all survivors of prematurity are not alike.
- Measurement equivalency should be established between groups.
With respect to the latter, “although many of the measures used by O’Reilly et al. have been normed, issues of measurement invariance have not been established between EP and control groups on some of the measures reported,” Dr. Schmidt and Dr. Saigal wrote, noting that “many other studies [also] fail to consider this fundamental measurement property.”
“Considering issues of measurement equivalency is of critical importance to ensuring unbiased interpretations of findings,” they added, concluding that the findings by O’Reilly et al. represent an important contribution and confirm findings from many prior studies of extreme prematurity, which “informs how we effectively manage these problems.”
“As the percentage of preterm birth continues to rise worldwide, coupled with reduced morbidity and mortality, and with more EP infants reaching adulthood, there is a need for prospective, long-term outcome studies of extreme prematurity,” Dr. Schmidt and Dr. Saigal added.
The study was funded by the Medical Research Council United Kingdom. The authors reported having no relevant financial disclosures. The editorial by Dr. Schmidt and Dr. Saigal, who also reported having no relevant financial disclosures, was supported by the Canadian Institutes of Health Research.
SOURCES: O’Reilly H et al. Pediatrics. 2020;145(2):e20192087; Schmidt LA, Saigal S. Pediatrics. 2020;145(2):e20193359.
FROM PEDIATRICS
AED exposure from breastfeeding appears to be low
, according to a study published online ahead of print Dec. 30, 2019, in JAMA Neurology. The results may explain why previous research failed to find adverse neurodevelopmental effects of breastfeeding in infants whose mothers are undergoing AED treatment, said the authors.
“The results of this study add support to the general safety of breastfeeding by mothers with epilepsy who take AEDs,” wrote Angela K. Birnbaum, PhD, professor of experimental and clinical pharmacology at the University of Minnesota in Minneapolis, and colleagues.
Investigators measured infants’ blood AED concentrations
To date, medical consensus about the safety of breastfeeding while the mother is taking AEDs has been elusive. Researchers have investigated breast milk concentrations of AEDs as surrogate markers of AED concentrations in children. Breast milk concentrations, however, do not account for differences in infant pharmacokinetic processes and thus could misrepresent AED exposure in children through breastfeeding.
Dr. Birnbaum and colleagues sought to measure blood concentrations of AEDs in mothers with epilepsy and the infants that they breastfed to achieve an objective measure of AED exposure through breastfeeding. They examined data collected from December 2012 to October 2016 in the prospective Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study. Eligible participants were pregnant women with epilepsy between the ages of 14 and 45 years whose pregnancies had progressed to fewer than 20 weeks’ gestational age and who had IQ scores greater than 70 points. Participants were followed up throughout pregnancy and for 9 months post partum. Children were enrolled at birth.
The investigators collected blood samples from mothers and infants who were breastfed at the same visit, which occurred at between 5 and 20 weeks after birth. The volume of ingested breast milk delivered through graduated feeding bottles each day and the total duration of all daily breastfeeding sessions were recorded. For infants, blood samples were collected from the plantar surface of the heel and stored as dried blood spots on filter paper. The study’s primary endpoint was the percentage of infant-to-mother concentration of AEDs. Concentrations of AEDs in infants at less than the lower limit of quantification were assessed as half of the lower limit.
Exposure in utero may be greater than exposure through breast milk
In all, the researchers enrolled 351 pregnant women with epilepsy into the study and collected data on 345 infants. Two hundred twenty-two (64.3%) of the infants were breastfed, and 146 (42.3%) had AED concentrations available. After excluding outliers and mothers with missing concentration data, Dr. Birnbaum and colleagues included 164 matching infant-mother concentration pairs in their analysis (i.e., of 135 mothers and 138 infants). Approximately 52% of the infants were female, and their median age at blood collection was 13 weeks. The mothers’ median age was 32 years. About 82% of mothers were receiving monotherapy. The investigators found no demographic differences between groups of mothers taking various AEDs.
Sixty-eight infants (49.3%) had AED concentrations that were less than the lower limit of quantification. AED concentration was not greater than the lower limit of quantification for any infants breastfed by mothers taking carbamazepine, oxcarbazepine, valproic acid, or topiramate. Most levetiracetam (71.4%) and zonisamide (60.0%) concentrations in infants were less than the lower limit of quantification. Most lamotrigine concentrations in infants (88.6%) were greater than the lower limit of quantification.
The median percentage of infant-to-mother concentration was 28.9% for lamotrigine, 5.3% for levetiracetam, 44.2% for zonisamide, 5.7% for carbamazepine, 5.4% for carbamazepine epoxide, 0.3% for oxcarbazepine, 17.2% for topiramate, and 21.4% for valproic acid. Multiple linear regression models indicated that maternal concentration was significantly associated with lamotrigine concentration in infants, but not levetiracetam concentration in infants.
“Prior studies at delivery demonstrated that umbilical-cord concentrations were nearly equal to maternal concentrations, suggesting extensive placental passage to the fetus,” wrote Dr. Birnbaum and colleagues. “Therefore, the amount of AED exposure via breast milk is likely substantially lower than fetal exposure during pregnancy and appears unlikely to confer any additional risks beyond those that might be associated with exposure in pregnancy, especially given prior studies showing no adverse neurodevelopmental effects of breastfeeding while taking AEDs.”
The investigators acknowledged several limitations of their research, including the observational design of the MONEAD study. The amount of AED in participants’ breast milk is unknown, and the investigators could not calculate relative infant dosages. Only one blood sample was taken per infant, thus the results may not reflect infants’ total exposure over time.
The National Institute of Neurological Disorders and Stroke and the National Institute of Child Health and Development funded the research. The authors reported receiving research support from various pharmaceutical companies.
SOURCE: Birnbaum AK et al. JAMA Neurol. 2019 Dec 30. doi: 10.1001/jamaneurol.2019.4443.
, according to a study published online ahead of print Dec. 30, 2019, in JAMA Neurology. The results may explain why previous research failed to find adverse neurodevelopmental effects of breastfeeding in infants whose mothers are undergoing AED treatment, said the authors.
“The results of this study add support to the general safety of breastfeeding by mothers with epilepsy who take AEDs,” wrote Angela K. Birnbaum, PhD, professor of experimental and clinical pharmacology at the University of Minnesota in Minneapolis, and colleagues.
Investigators measured infants’ blood AED concentrations
To date, medical consensus about the safety of breastfeeding while the mother is taking AEDs has been elusive. Researchers have investigated breast milk concentrations of AEDs as surrogate markers of AED concentrations in children. Breast milk concentrations, however, do not account for differences in infant pharmacokinetic processes and thus could misrepresent AED exposure in children through breastfeeding.
Dr. Birnbaum and colleagues sought to measure blood concentrations of AEDs in mothers with epilepsy and the infants that they breastfed to achieve an objective measure of AED exposure through breastfeeding. They examined data collected from December 2012 to October 2016 in the prospective Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study. Eligible participants were pregnant women with epilepsy between the ages of 14 and 45 years whose pregnancies had progressed to fewer than 20 weeks’ gestational age and who had IQ scores greater than 70 points. Participants were followed up throughout pregnancy and for 9 months post partum. Children were enrolled at birth.
The investigators collected blood samples from mothers and infants who were breastfed at the same visit, which occurred at between 5 and 20 weeks after birth. The volume of ingested breast milk delivered through graduated feeding bottles each day and the total duration of all daily breastfeeding sessions were recorded. For infants, blood samples were collected from the plantar surface of the heel and stored as dried blood spots on filter paper. The study’s primary endpoint was the percentage of infant-to-mother concentration of AEDs. Concentrations of AEDs in infants at less than the lower limit of quantification were assessed as half of the lower limit.
Exposure in utero may be greater than exposure through breast milk
In all, the researchers enrolled 351 pregnant women with epilepsy into the study and collected data on 345 infants. Two hundred twenty-two (64.3%) of the infants were breastfed, and 146 (42.3%) had AED concentrations available. After excluding outliers and mothers with missing concentration data, Dr. Birnbaum and colleagues included 164 matching infant-mother concentration pairs in their analysis (i.e., of 135 mothers and 138 infants). Approximately 52% of the infants were female, and their median age at blood collection was 13 weeks. The mothers’ median age was 32 years. About 82% of mothers were receiving monotherapy. The investigators found no demographic differences between groups of mothers taking various AEDs.
Sixty-eight infants (49.3%) had AED concentrations that were less than the lower limit of quantification. AED concentration was not greater than the lower limit of quantification for any infants breastfed by mothers taking carbamazepine, oxcarbazepine, valproic acid, or topiramate. Most levetiracetam (71.4%) and zonisamide (60.0%) concentrations in infants were less than the lower limit of quantification. Most lamotrigine concentrations in infants (88.6%) were greater than the lower limit of quantification.
The median percentage of infant-to-mother concentration was 28.9% for lamotrigine, 5.3% for levetiracetam, 44.2% for zonisamide, 5.7% for carbamazepine, 5.4% for carbamazepine epoxide, 0.3% for oxcarbazepine, 17.2% for topiramate, and 21.4% for valproic acid. Multiple linear regression models indicated that maternal concentration was significantly associated with lamotrigine concentration in infants, but not levetiracetam concentration in infants.
“Prior studies at delivery demonstrated that umbilical-cord concentrations were nearly equal to maternal concentrations, suggesting extensive placental passage to the fetus,” wrote Dr. Birnbaum and colleagues. “Therefore, the amount of AED exposure via breast milk is likely substantially lower than fetal exposure during pregnancy and appears unlikely to confer any additional risks beyond those that might be associated with exposure in pregnancy, especially given prior studies showing no adverse neurodevelopmental effects of breastfeeding while taking AEDs.”
The investigators acknowledged several limitations of their research, including the observational design of the MONEAD study. The amount of AED in participants’ breast milk is unknown, and the investigators could not calculate relative infant dosages. Only one blood sample was taken per infant, thus the results may not reflect infants’ total exposure over time.
The National Institute of Neurological Disorders and Stroke and the National Institute of Child Health and Development funded the research. The authors reported receiving research support from various pharmaceutical companies.
SOURCE: Birnbaum AK et al. JAMA Neurol. 2019 Dec 30. doi: 10.1001/jamaneurol.2019.4443.
, according to a study published online ahead of print Dec. 30, 2019, in JAMA Neurology. The results may explain why previous research failed to find adverse neurodevelopmental effects of breastfeeding in infants whose mothers are undergoing AED treatment, said the authors.
“The results of this study add support to the general safety of breastfeeding by mothers with epilepsy who take AEDs,” wrote Angela K. Birnbaum, PhD, professor of experimental and clinical pharmacology at the University of Minnesota in Minneapolis, and colleagues.
Investigators measured infants’ blood AED concentrations
To date, medical consensus about the safety of breastfeeding while the mother is taking AEDs has been elusive. Researchers have investigated breast milk concentrations of AEDs as surrogate markers of AED concentrations in children. Breast milk concentrations, however, do not account for differences in infant pharmacokinetic processes and thus could misrepresent AED exposure in children through breastfeeding.
Dr. Birnbaum and colleagues sought to measure blood concentrations of AEDs in mothers with epilepsy and the infants that they breastfed to achieve an objective measure of AED exposure through breastfeeding. They examined data collected from December 2012 to October 2016 in the prospective Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study. Eligible participants were pregnant women with epilepsy between the ages of 14 and 45 years whose pregnancies had progressed to fewer than 20 weeks’ gestational age and who had IQ scores greater than 70 points. Participants were followed up throughout pregnancy and for 9 months post partum. Children were enrolled at birth.
The investigators collected blood samples from mothers and infants who were breastfed at the same visit, which occurred at between 5 and 20 weeks after birth. The volume of ingested breast milk delivered through graduated feeding bottles each day and the total duration of all daily breastfeeding sessions were recorded. For infants, blood samples were collected from the plantar surface of the heel and stored as dried blood spots on filter paper. The study’s primary endpoint was the percentage of infant-to-mother concentration of AEDs. Concentrations of AEDs in infants at less than the lower limit of quantification were assessed as half of the lower limit.
Exposure in utero may be greater than exposure through breast milk
In all, the researchers enrolled 351 pregnant women with epilepsy into the study and collected data on 345 infants. Two hundred twenty-two (64.3%) of the infants were breastfed, and 146 (42.3%) had AED concentrations available. After excluding outliers and mothers with missing concentration data, Dr. Birnbaum and colleagues included 164 matching infant-mother concentration pairs in their analysis (i.e., of 135 mothers and 138 infants). Approximately 52% of the infants were female, and their median age at blood collection was 13 weeks. The mothers’ median age was 32 years. About 82% of mothers were receiving monotherapy. The investigators found no demographic differences between groups of mothers taking various AEDs.
Sixty-eight infants (49.3%) had AED concentrations that were less than the lower limit of quantification. AED concentration was not greater than the lower limit of quantification for any infants breastfed by mothers taking carbamazepine, oxcarbazepine, valproic acid, or topiramate. Most levetiracetam (71.4%) and zonisamide (60.0%) concentrations in infants were less than the lower limit of quantification. Most lamotrigine concentrations in infants (88.6%) were greater than the lower limit of quantification.
The median percentage of infant-to-mother concentration was 28.9% for lamotrigine, 5.3% for levetiracetam, 44.2% for zonisamide, 5.7% for carbamazepine, 5.4% for carbamazepine epoxide, 0.3% for oxcarbazepine, 17.2% for topiramate, and 21.4% for valproic acid. Multiple linear regression models indicated that maternal concentration was significantly associated with lamotrigine concentration in infants, but not levetiracetam concentration in infants.
“Prior studies at delivery demonstrated that umbilical-cord concentrations were nearly equal to maternal concentrations, suggesting extensive placental passage to the fetus,” wrote Dr. Birnbaum and colleagues. “Therefore, the amount of AED exposure via breast milk is likely substantially lower than fetal exposure during pregnancy and appears unlikely to confer any additional risks beyond those that might be associated with exposure in pregnancy, especially given prior studies showing no adverse neurodevelopmental effects of breastfeeding while taking AEDs.”
The investigators acknowledged several limitations of their research, including the observational design of the MONEAD study. The amount of AED in participants’ breast milk is unknown, and the investigators could not calculate relative infant dosages. Only one blood sample was taken per infant, thus the results may not reflect infants’ total exposure over time.
The National Institute of Neurological Disorders and Stroke and the National Institute of Child Health and Development funded the research. The authors reported receiving research support from various pharmaceutical companies.
SOURCE: Birnbaum AK et al. JAMA Neurol. 2019 Dec 30. doi: 10.1001/jamaneurol.2019.4443.
FROM JAMA NEUROLOGY
High infantile spasm risk should contraindicate sodium channel blocker antiepileptics
BALTIMORE – “This is scary and warrants caution,” said senior investigator and pediatric neurologist Shaun Hussain, MD, a pediatric neurologist at Mattel Children’s Hospital at UCLA. Because of the findings, “we are avoiding the use of voltage-gated sodium channel blockade in any child at risk for infantile spasms. More broadly, we are avoiding [them] in any infant if there is a good alternative medication, of which there are many in most cases.”
There have been a few previous case reports linking voltage-gated sodium channel blockers (SCBs) – which include oxcarbazepine, carbamazepine, lacosamide, and phenytoin – to infantile spasms, but they are still commonly used for infant seizures. There was some disagreement at UCLA whether there really was a link, so Dr. Hussain and his team took a look at the university’s experience. They matched 50 children with nonsyndromic epilepsy who subsequently developed video-EEG confirmed infantile spasms (cases) to 50 children who also had nonsyndromic epilepsy but did not develop spasms, based on follow-up duration and age and date of epilepsy onset.
The team then looked to see what drugs they had been on; it turned out that cases and controls were about equally as likely to have been treated with any specific antiepileptic, including SCBs. Infantile spasms were substantially more likely with SCB exposure in children with spasm risk factors, which also include focal cortical dysplasia, Aicardi syndrome, and other problems (HR 7.0; 95%; CI 2.5-19.8; P less than .001). Spasms were also more likely among even low-risk children treated with SCBs, although the trend was not statistically significant.
In the end, “we wonder how many cases of infantile spasms could [have been] prevented entirely if we had avoided sodium channel blockade,” Dr. Hussain said at the annual meeting of the American Epilepsy Society.
With so many other seizure options available – levetiracetam, topiramate, and phenobarbital, to name just a few – maybe it would be best “to stay away from” SCBs entirely in “infants with any form of epilepsy,” said lead investigator Jaeden Heesch, an undergraduate researcher who worked with Dr. Hussain.
It is unclear why SCBs increase infantile spasm risk; maybe nonselective voltage-gated sodium channel blockade interferes with proper neuron function in susceptible children, similar to the effects of sodium voltage-gated channel alpha subunit 1 mutations in Dravet syndrome, Dr. Hussain said. Perhaps the findings will inspire drug development. “If nonselective sodium channel blockade is bad, perhaps selective modulation of voltage-gated sodium currents [could be] beneficial or protective,” he said.
The age of epilepsy onset in the study was around 2 months. Children who went on to develop infantile spasms had an average of almost two seizures per day, versus fewer than one among controls, and were on an average of two, versus about 1.5 antiepileptics. The differences were not statistically significant.
The study looked at SCB exposure overall, but it’s possible that infantile spasm risk differs among the various class members.
The work was funded by the Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute. The investigators didn’t have any relevant disclosures.
SOURCE: Heesch J et al. AES 2019. Abstract 2.234.
BALTIMORE – “This is scary and warrants caution,” said senior investigator and pediatric neurologist Shaun Hussain, MD, a pediatric neurologist at Mattel Children’s Hospital at UCLA. Because of the findings, “we are avoiding the use of voltage-gated sodium channel blockade in any child at risk for infantile spasms. More broadly, we are avoiding [them] in any infant if there is a good alternative medication, of which there are many in most cases.”
There have been a few previous case reports linking voltage-gated sodium channel blockers (SCBs) – which include oxcarbazepine, carbamazepine, lacosamide, and phenytoin – to infantile spasms, but they are still commonly used for infant seizures. There was some disagreement at UCLA whether there really was a link, so Dr. Hussain and his team took a look at the university’s experience. They matched 50 children with nonsyndromic epilepsy who subsequently developed video-EEG confirmed infantile spasms (cases) to 50 children who also had nonsyndromic epilepsy but did not develop spasms, based on follow-up duration and age and date of epilepsy onset.
The team then looked to see what drugs they had been on; it turned out that cases and controls were about equally as likely to have been treated with any specific antiepileptic, including SCBs. Infantile spasms were substantially more likely with SCB exposure in children with spasm risk factors, which also include focal cortical dysplasia, Aicardi syndrome, and other problems (HR 7.0; 95%; CI 2.5-19.8; P less than .001). Spasms were also more likely among even low-risk children treated with SCBs, although the trend was not statistically significant.
In the end, “we wonder how many cases of infantile spasms could [have been] prevented entirely if we had avoided sodium channel blockade,” Dr. Hussain said at the annual meeting of the American Epilepsy Society.
With so many other seizure options available – levetiracetam, topiramate, and phenobarbital, to name just a few – maybe it would be best “to stay away from” SCBs entirely in “infants with any form of epilepsy,” said lead investigator Jaeden Heesch, an undergraduate researcher who worked with Dr. Hussain.
It is unclear why SCBs increase infantile spasm risk; maybe nonselective voltage-gated sodium channel blockade interferes with proper neuron function in susceptible children, similar to the effects of sodium voltage-gated channel alpha subunit 1 mutations in Dravet syndrome, Dr. Hussain said. Perhaps the findings will inspire drug development. “If nonselective sodium channel blockade is bad, perhaps selective modulation of voltage-gated sodium currents [could be] beneficial or protective,” he said.
The age of epilepsy onset in the study was around 2 months. Children who went on to develop infantile spasms had an average of almost two seizures per day, versus fewer than one among controls, and were on an average of two, versus about 1.5 antiepileptics. The differences were not statistically significant.
The study looked at SCB exposure overall, but it’s possible that infantile spasm risk differs among the various class members.
The work was funded by the Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute. The investigators didn’t have any relevant disclosures.
SOURCE: Heesch J et al. AES 2019. Abstract 2.234.
BALTIMORE – “This is scary and warrants caution,” said senior investigator and pediatric neurologist Shaun Hussain, MD, a pediatric neurologist at Mattel Children’s Hospital at UCLA. Because of the findings, “we are avoiding the use of voltage-gated sodium channel blockade in any child at risk for infantile spasms. More broadly, we are avoiding [them] in any infant if there is a good alternative medication, of which there are many in most cases.”
There have been a few previous case reports linking voltage-gated sodium channel blockers (SCBs) – which include oxcarbazepine, carbamazepine, lacosamide, and phenytoin – to infantile spasms, but they are still commonly used for infant seizures. There was some disagreement at UCLA whether there really was a link, so Dr. Hussain and his team took a look at the university’s experience. They matched 50 children with nonsyndromic epilepsy who subsequently developed video-EEG confirmed infantile spasms (cases) to 50 children who also had nonsyndromic epilepsy but did not develop spasms, based on follow-up duration and age and date of epilepsy onset.
The team then looked to see what drugs they had been on; it turned out that cases and controls were about equally as likely to have been treated with any specific antiepileptic, including SCBs. Infantile spasms were substantially more likely with SCB exposure in children with spasm risk factors, which also include focal cortical dysplasia, Aicardi syndrome, and other problems (HR 7.0; 95%; CI 2.5-19.8; P less than .001). Spasms were also more likely among even low-risk children treated with SCBs, although the trend was not statistically significant.
In the end, “we wonder how many cases of infantile spasms could [have been] prevented entirely if we had avoided sodium channel blockade,” Dr. Hussain said at the annual meeting of the American Epilepsy Society.
With so many other seizure options available – levetiracetam, topiramate, and phenobarbital, to name just a few – maybe it would be best “to stay away from” SCBs entirely in “infants with any form of epilepsy,” said lead investigator Jaeden Heesch, an undergraduate researcher who worked with Dr. Hussain.
It is unclear why SCBs increase infantile spasm risk; maybe nonselective voltage-gated sodium channel blockade interferes with proper neuron function in susceptible children, similar to the effects of sodium voltage-gated channel alpha subunit 1 mutations in Dravet syndrome, Dr. Hussain said. Perhaps the findings will inspire drug development. “If nonselective sodium channel blockade is bad, perhaps selective modulation of voltage-gated sodium currents [could be] beneficial or protective,” he said.
The age of epilepsy onset in the study was around 2 months. Children who went on to develop infantile spasms had an average of almost two seizures per day, versus fewer than one among controls, and were on an average of two, versus about 1.5 antiepileptics. The differences were not statistically significant.
The study looked at SCB exposure overall, but it’s possible that infantile spasm risk differs among the various class members.
The work was funded by the Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute. The investigators didn’t have any relevant disclosures.
SOURCE: Heesch J et al. AES 2019. Abstract 2.234.
REPORTING FROM AES 2019
Newborns’ maternal protection against measles wanes within 6 months
according to new research.
In fact, most of the 196 infants’ maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics.
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The findings are not surprising for a setting in which measles has been eliminated and align with results from past research, Huong Q. McLean, PhD, MPH, of the Marshfield (Wis.) Clinic Research Institute and Walter A. Orenstein, MD, of Emory University in Atlanta wrote in an accompanying editorial (Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-2541).
However, this susceptibility prior to receiving the MMR has taken on a new significance more recently, Dr. McLean and Dr. Orenstein suggested.
“In light of increasing measles outbreaks during the past year reaching levels not recorded in the United States since 1992 and increased measles elsewhere, coupled with the risk of severe illness in infants, there is increased concern regarding the protection of infants against measles,” the editorialists wrote.
Dr. Science and colleagues tested serum samples from 196 term infants, all under 12 months old, for antibodies against measles. The sera had been previously collected at a single tertiary care center in Ontario for clinical testing and then stored. Measles has been eliminated in Canada since 1998.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days); 2 months (61-89 days); 3 months (90-119 days); 4 months; 5 months; 6-9 months; and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test (PRNT) to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay (ELISA) because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL) , and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Dr. McLean and Dr. Orenstein noted in their editorial.
They discussed the rationale for various changes in the recommended schedule for measles immunization, based on changes in epidemiology of the disease and improved understanding of the immune response to vaccination since the vaccine became available in 1963. Then they posed the question of whether the recommendation should be revised again.
“Ideally, the schedule should minimize the risk of measles and its complications and optimize vaccine-induced protection,” Dr. McLean and Dr. Orenstein wrote.
They argued that the evidence cannot currently support changing the first MMR dose to a younger age because measles incidence in the United States remains extremely low outside of the extraordinary outbreaks in 2014 and 2019. Further, infants under 12 months of age make up less than 15% of measles cases during outbreaks, and unvaccinated people make up more than 70% of cases.
Rather, they stated, this new study emphasizes the importance of following the current schedule, with consideration of an earlier schedule only warranted during outbreaks.
“Health care providers must work to maintain high levels of coverage with 2 doses of MMR among vaccine-eligible populations and minimize pockets of susceptibility to prevent transmission to infants and prevent reestablishment of endemic transmission,” they concluded.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures. The editorialists had no external funding and no relevant financial disclosures.
SOURCE: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
according to new research.
In fact, most of the 196 infants’ maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics.
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The findings are not surprising for a setting in which measles has been eliminated and align with results from past research, Huong Q. McLean, PhD, MPH, of the Marshfield (Wis.) Clinic Research Institute and Walter A. Orenstein, MD, of Emory University in Atlanta wrote in an accompanying editorial (Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-2541).
However, this susceptibility prior to receiving the MMR has taken on a new significance more recently, Dr. McLean and Dr. Orenstein suggested.
“In light of increasing measles outbreaks during the past year reaching levels not recorded in the United States since 1992 and increased measles elsewhere, coupled with the risk of severe illness in infants, there is increased concern regarding the protection of infants against measles,” the editorialists wrote.
Dr. Science and colleagues tested serum samples from 196 term infants, all under 12 months old, for antibodies against measles. The sera had been previously collected at a single tertiary care center in Ontario for clinical testing and then stored. Measles has been eliminated in Canada since 1998.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days); 2 months (61-89 days); 3 months (90-119 days); 4 months; 5 months; 6-9 months; and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test (PRNT) to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay (ELISA) because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL) , and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Dr. McLean and Dr. Orenstein noted in their editorial.
They discussed the rationale for various changes in the recommended schedule for measles immunization, based on changes in epidemiology of the disease and improved understanding of the immune response to vaccination since the vaccine became available in 1963. Then they posed the question of whether the recommendation should be revised again.
“Ideally, the schedule should minimize the risk of measles and its complications and optimize vaccine-induced protection,” Dr. McLean and Dr. Orenstein wrote.
They argued that the evidence cannot currently support changing the first MMR dose to a younger age because measles incidence in the United States remains extremely low outside of the extraordinary outbreaks in 2014 and 2019. Further, infants under 12 months of age make up less than 15% of measles cases during outbreaks, and unvaccinated people make up more than 70% of cases.
Rather, they stated, this new study emphasizes the importance of following the current schedule, with consideration of an earlier schedule only warranted during outbreaks.
“Health care providers must work to maintain high levels of coverage with 2 doses of MMR among vaccine-eligible populations and minimize pockets of susceptibility to prevent transmission to infants and prevent reestablishment of endemic transmission,” they concluded.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures. The editorialists had no external funding and no relevant financial disclosures.
SOURCE: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
according to new research.
In fact, most of the 196 infants’ maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics.
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The findings are not surprising for a setting in which measles has been eliminated and align with results from past research, Huong Q. McLean, PhD, MPH, of the Marshfield (Wis.) Clinic Research Institute and Walter A. Orenstein, MD, of Emory University in Atlanta wrote in an accompanying editorial (Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-2541).
However, this susceptibility prior to receiving the MMR has taken on a new significance more recently, Dr. McLean and Dr. Orenstein suggested.
“In light of increasing measles outbreaks during the past year reaching levels not recorded in the United States since 1992 and increased measles elsewhere, coupled with the risk of severe illness in infants, there is increased concern regarding the protection of infants against measles,” the editorialists wrote.
Dr. Science and colleagues tested serum samples from 196 term infants, all under 12 months old, for antibodies against measles. The sera had been previously collected at a single tertiary care center in Ontario for clinical testing and then stored. Measles has been eliminated in Canada since 1998.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days); 2 months (61-89 days); 3 months (90-119 days); 4 months; 5 months; 6-9 months; and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test (PRNT) to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay (ELISA) because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL) , and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Dr. McLean and Dr. Orenstein noted in their editorial.
They discussed the rationale for various changes in the recommended schedule for measles immunization, based on changes in epidemiology of the disease and improved understanding of the immune response to vaccination since the vaccine became available in 1963. Then they posed the question of whether the recommendation should be revised again.
“Ideally, the schedule should minimize the risk of measles and its complications and optimize vaccine-induced protection,” Dr. McLean and Dr. Orenstein wrote.
They argued that the evidence cannot currently support changing the first MMR dose to a younger age because measles incidence in the United States remains extremely low outside of the extraordinary outbreaks in 2014 and 2019. Further, infants under 12 months of age make up less than 15% of measles cases during outbreaks, and unvaccinated people make up more than 70% of cases.
Rather, they stated, this new study emphasizes the importance of following the current schedule, with consideration of an earlier schedule only warranted during outbreaks.
“Health care providers must work to maintain high levels of coverage with 2 doses of MMR among vaccine-eligible populations and minimize pockets of susceptibility to prevent transmission to infants and prevent reestablishment of endemic transmission,” they concluded.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures. The editorialists had no external funding and no relevant financial disclosures.
SOURCE: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
FROM PEDIATRICS
Key clinical point: Infants’ maternal measles antibodies fell below protective levels by 6 months old.
Major finding: Infants were twice as likely not to have protective immunity against measles for each month of age after birth (odds ratio, 2.13).
Study details: The findings are based on measles antibody testing of 196 serum samples from infants born in a tertiary care center in Ontario.
Disclosures: The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Source: Science M et al. Pediatrics. 2019 Nov 21. doi: 10.1542/peds.2019-0630.
In utero Zika exposure can have delayed consequences
WASHINGTON – Evidence continues to mount that infants born to moms infected with Zika virus during pregnancy can have neurodevelopmental abnormalities as they age even if they showed no defects at birth, based on follow-up of 890 Colombian children tracked by epidemiologists from the U.S. Centers for Disease Control and Prevention.
Among the 890 neonates born to mothers apparently infected with Zika during pregnancy and followed for up to 2 years, 40 of the 852 (5%) without a detectable birth defect at delivery went on to show some type of neurodevelopmental sequelae during up to 24 months of age, Margaret Honein, PhD, said at an annual scientific meeting on infectious diseases.
In addition, among the children without birth defects at delivery who received follow-up examinations out to about 2 years, the incidence of “alerts” for possible neurodevelopmental issues was 15%-20% for each of the four domains studied (gross motor, fine motor, hearing and language, and personal and social functions), said Dr. Honein, an epidemiologist and chief of the birth defects branch of the CDC. In contrast, 17 of the 38 children (45%) followed who had identifiable birth defects at delivery also showed neurodevelopmental abnormalities when reexamined as long as 2 years after birth. These possible neurodevelopmental abnormalities, designated as alerts, were identified in comparison with a contemporaneous cohort of children born to uninfected mothers in the same regions of Colombia and assessed by the CDC researchers.
This cohort of children born to mothers who became infected with Zika virus during the 2016 Colombian epidemic will not undergo any planned, additional follow-up beyond the initial 2 years, Dr. Honein noted.
The findings she reported were consistent with observations from a much smaller cohort of 70 infants born to Colombian mothers infected with Zika virus while pregnant who had a normal head circumference and a normal clinical examination at delivery. When assessed once or twice 4-18 months after birth, these 70 infants showed an overall greater than one standard deviation (z-score) drop in their scores on the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) metric by 12 months after birth and continuing out to 18 months, said Sarah B. Mulkey, MD, a fetal-neonatal neurologist at Children’s National Health System in Washington. These deficits were especially pronounced in the mobility and social cognition domains of the four-domain WIDEA metric. The social cognition domain is an important predictor of later problems with executive function and other neurologic disorders, Dr. Mulkey said while reporting her findings in a separate talk at the meeting. She acknowledged that the analysis was flawed by comparing the WIDEA outcomes of the Zika virus–exposed children to healthy children from either inner-city Chicago or Canada. Dr. Mulkey said that she and her associates plan to characterize a population of Zika virus–unexposed children in Colombia to use for future comparisons.
The study reported by Dr. Honein involved an enhanced surveillance program launched by the CDC in 2016 in three regions of Colombia and included 1,190 pregnancies accompanied by Zika symptoms in the mother and with a reported pregnancy outcome, including 1,185 live births. Nearly half of the Zika infections occurred during the first trimester, and 34% occurred during the second trimester. However, fewer than a third of the pregnant women underwent some type of laboratory testing to confirm their infection, either by serology or by a DNA-based assay, and of these 28% had a positive finding. Dr. Honein cautioned that many of the specimens that tested negative for Zika virus may have been false negatives.
The birth defects identified among the infants born from an apparently affected pregnancy included brain abnormalities, eye anomalies, and microcephaly, with 5% of the 1,185 live births showing one or more of these outcomes. The neurodevelopmental deficits identified during follow-up of 890 of the children out to 2 years included seizures; abnormalities of tone, movement, or swallowing; and impairments of vision or hearing.
WASHINGTON – Evidence continues to mount that infants born to moms infected with Zika virus during pregnancy can have neurodevelopmental abnormalities as they age even if they showed no defects at birth, based on follow-up of 890 Colombian children tracked by epidemiologists from the U.S. Centers for Disease Control and Prevention.
Among the 890 neonates born to mothers apparently infected with Zika during pregnancy and followed for up to 2 years, 40 of the 852 (5%) without a detectable birth defect at delivery went on to show some type of neurodevelopmental sequelae during up to 24 months of age, Margaret Honein, PhD, said at an annual scientific meeting on infectious diseases.
In addition, among the children without birth defects at delivery who received follow-up examinations out to about 2 years, the incidence of “alerts” for possible neurodevelopmental issues was 15%-20% for each of the four domains studied (gross motor, fine motor, hearing and language, and personal and social functions), said Dr. Honein, an epidemiologist and chief of the birth defects branch of the CDC. In contrast, 17 of the 38 children (45%) followed who had identifiable birth defects at delivery also showed neurodevelopmental abnormalities when reexamined as long as 2 years after birth. These possible neurodevelopmental abnormalities, designated as alerts, were identified in comparison with a contemporaneous cohort of children born to uninfected mothers in the same regions of Colombia and assessed by the CDC researchers.
This cohort of children born to mothers who became infected with Zika virus during the 2016 Colombian epidemic will not undergo any planned, additional follow-up beyond the initial 2 years, Dr. Honein noted.
The findings she reported were consistent with observations from a much smaller cohort of 70 infants born to Colombian mothers infected with Zika virus while pregnant who had a normal head circumference and a normal clinical examination at delivery. When assessed once or twice 4-18 months after birth, these 70 infants showed an overall greater than one standard deviation (z-score) drop in their scores on the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) metric by 12 months after birth and continuing out to 18 months, said Sarah B. Mulkey, MD, a fetal-neonatal neurologist at Children’s National Health System in Washington. These deficits were especially pronounced in the mobility and social cognition domains of the four-domain WIDEA metric. The social cognition domain is an important predictor of later problems with executive function and other neurologic disorders, Dr. Mulkey said while reporting her findings in a separate talk at the meeting. She acknowledged that the analysis was flawed by comparing the WIDEA outcomes of the Zika virus–exposed children to healthy children from either inner-city Chicago or Canada. Dr. Mulkey said that she and her associates plan to characterize a population of Zika virus–unexposed children in Colombia to use for future comparisons.
The study reported by Dr. Honein involved an enhanced surveillance program launched by the CDC in 2016 in three regions of Colombia and included 1,190 pregnancies accompanied by Zika symptoms in the mother and with a reported pregnancy outcome, including 1,185 live births. Nearly half of the Zika infections occurred during the first trimester, and 34% occurred during the second trimester. However, fewer than a third of the pregnant women underwent some type of laboratory testing to confirm their infection, either by serology or by a DNA-based assay, and of these 28% had a positive finding. Dr. Honein cautioned that many of the specimens that tested negative for Zika virus may have been false negatives.
The birth defects identified among the infants born from an apparently affected pregnancy included brain abnormalities, eye anomalies, and microcephaly, with 5% of the 1,185 live births showing one or more of these outcomes. The neurodevelopmental deficits identified during follow-up of 890 of the children out to 2 years included seizures; abnormalities of tone, movement, or swallowing; and impairments of vision or hearing.
WASHINGTON – Evidence continues to mount that infants born to moms infected with Zika virus during pregnancy can have neurodevelopmental abnormalities as they age even if they showed no defects at birth, based on follow-up of 890 Colombian children tracked by epidemiologists from the U.S. Centers for Disease Control and Prevention.
Among the 890 neonates born to mothers apparently infected with Zika during pregnancy and followed for up to 2 years, 40 of the 852 (5%) without a detectable birth defect at delivery went on to show some type of neurodevelopmental sequelae during up to 24 months of age, Margaret Honein, PhD, said at an annual scientific meeting on infectious diseases.
In addition, among the children without birth defects at delivery who received follow-up examinations out to about 2 years, the incidence of “alerts” for possible neurodevelopmental issues was 15%-20% for each of the four domains studied (gross motor, fine motor, hearing and language, and personal and social functions), said Dr. Honein, an epidemiologist and chief of the birth defects branch of the CDC. In contrast, 17 of the 38 children (45%) followed who had identifiable birth defects at delivery also showed neurodevelopmental abnormalities when reexamined as long as 2 years after birth. These possible neurodevelopmental abnormalities, designated as alerts, were identified in comparison with a contemporaneous cohort of children born to uninfected mothers in the same regions of Colombia and assessed by the CDC researchers.
This cohort of children born to mothers who became infected with Zika virus during the 2016 Colombian epidemic will not undergo any planned, additional follow-up beyond the initial 2 years, Dr. Honein noted.
The findings she reported were consistent with observations from a much smaller cohort of 70 infants born to Colombian mothers infected with Zika virus while pregnant who had a normal head circumference and a normal clinical examination at delivery. When assessed once or twice 4-18 months after birth, these 70 infants showed an overall greater than one standard deviation (z-score) drop in their scores on the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) metric by 12 months after birth and continuing out to 18 months, said Sarah B. Mulkey, MD, a fetal-neonatal neurologist at Children’s National Health System in Washington. These deficits were especially pronounced in the mobility and social cognition domains of the four-domain WIDEA metric. The social cognition domain is an important predictor of later problems with executive function and other neurologic disorders, Dr. Mulkey said while reporting her findings in a separate talk at the meeting. She acknowledged that the analysis was flawed by comparing the WIDEA outcomes of the Zika virus–exposed children to healthy children from either inner-city Chicago or Canada. Dr. Mulkey said that she and her associates plan to characterize a population of Zika virus–unexposed children in Colombia to use for future comparisons.
The study reported by Dr. Honein involved an enhanced surveillance program launched by the CDC in 2016 in three regions of Colombia and included 1,190 pregnancies accompanied by Zika symptoms in the mother and with a reported pregnancy outcome, including 1,185 live births. Nearly half of the Zika infections occurred during the first trimester, and 34% occurred during the second trimester. However, fewer than a third of the pregnant women underwent some type of laboratory testing to confirm their infection, either by serology or by a DNA-based assay, and of these 28% had a positive finding. Dr. Honein cautioned that many of the specimens that tested negative for Zika virus may have been false negatives.
The birth defects identified among the infants born from an apparently affected pregnancy included brain abnormalities, eye anomalies, and microcephaly, with 5% of the 1,185 live births showing one or more of these outcomes. The neurodevelopmental deficits identified during follow-up of 890 of the children out to 2 years included seizures; abnormalities of tone, movement, or swallowing; and impairments of vision or hearing.
REPORTING FROM ID WEEK 2019
Poor neonatal outcomes tied to excessive, insufficient weight gain during twin pregnancies
Lisa M. Bodnar, PhD, and colleagues determined.
The risks of cesarean section and neonatal death were elevated for those mothers who were overweight before pregnancy and then gained too much. But infants of underweight women who didn’t gain enough faced risks as well, wrote Dr. Bodnar of the University of Pittsburgh and associates in Obstetrics & Gynecology.
Among the most severely overweight women (obesity grade 2 or 3) who gained the most weight (43 kg) at 37 weeks’ gestation, there were 6 fewer small-for-gestational-age (SGA) infants per 100 births, but 14 more large-for-gestational-age (LGA) infants, 4 more cesarean deliveries, and 2 more neonatal deaths per 100 births. By contrast, among the most severely underweight women who gained the least amount of weight (9 kg), there were 18 more SGA infants, 3 fewer LGA infants, and 11 fewer cesareans, but 6 more preterm births before 32 weeks’ gestation.
The same U-shaped pattern also occurred within the individual weight categories. For example, compared with the outcomes among the most underweight women who gained least, among underweight women who gained the most (37 kg), there were eight fewer SGA infants, but four more LGA infants, 16 excess preterm births, and 9 excess infant deaths.
“If the associations we observed are even partially reflective of causality, targeted modification of pregnancy weight gain in women carrying twins might improve pregnancy outcomes,” wrote Dr. Bodnar and her team. “Data on a wide range of short- and long-term outcomes and information on the relative seriousness of these outcomes are needed to determine optimal gestational weight gain ranges for twin pregnancies.”
The cohort comprised 54,836 live-born twins from 27,723 twin pregnancies who were included in the MOMs database maintained by the University of Pennsylvania, Philadelphia. The population-based study tracks maternal obesity, gestational weight gain, and adverse birth outcomes. The information came from infant birth and death vital statistics records from 2003 to 2013.
However, this very source puts the findings in some degree of uncertainty, Ozhan Turan, MD, said in an interview.
“It’s a very nice study, and the statistics are very well done,” said Dr. Turan, who is the director of fetal therapy and complex obstetric surgery at the University of Maryland School of Medicine. “But that kind of data has pitfalls that are unavoidable. For example, they don’t have access to maternal medical comorbidities which are mostly related to the outcome, particularly gestational diabetes and preeclampsia. They also don’t have the information on chorionicity – and we know that monochorionic twins face much greater risk for these outcomes than dichorionic twins.”
The investigators calculated total gestational weight gain by subtracting prepregnancy weight from maternal weight at delivery. The analysis controlled for race and ethnicity, education, neonatal care, level of birth facility, parity, payment at delivery, smoking during pregnancy, marital status, year of birth, height, maternal age, preexisting diabetes or hypertension, infertility treatment, neonatal sex, and racial composition of neighborhood, as a proxy of neighborhood-level socioeconomic status. Approximately 16% of mothers received infertility treatment.
Of the cohort, 3% were underweight, 48% were normal weight, 24% were overweight, 13% were grade 1 obese, 7% grade 2 obese, and 5% grade 3 obese.
“Pregnancy weight gain was negatively associated with SGA and positively associated with LGA and cesarean delivery in all [body mass index] groups. For example, among normal-weight women, compared with a pregnancy weight gain equivalent to 20 kg at 37 weeks’ of gestation, a weight gain of 27 kg at 37 weeks’ of gestation was associated with 2.2 fewer cases of SGA but 2.9 more cases of LGA and 3.7 more cases of cesarean delivery,” Dr. Bodnar and associates wrote.
The investigators found that “weight gains well above or well below the [Institute of Medicine] provisional guidelines (less than 14 kg or more than 27 kg in underweight or normal-weight women, less than 11 kg or more than 28 kg in overweight women, and less than 6.4 kg or more than 26 kg in women with obesity) were associated with the highest risk of adverse outcomes.”
“I would not say this is practice-changing information,” said Dr. Turan. “We already know all this. What would be very helpful is an algorithm to tell us, if a patient is pregnant with twins, this is the amount of weight you have to gain.”
For overweight patients, Dr. Turan tries to impart the key message of moderate or slight weight gain, according to prepregnancy body mass index. For underweight patients, the picture is a bit more complex.
“There are not that many who are underweight before pregnancy, so first thing I look for is the reason a woman is underweight. Is she just not eating properly? Is there a drug dependence issue, alcohol dependence, HIV? Is there smoking? A gut problem that causes malnutrition. You can’t just say ‘eat more.’ That does not solve the problem. We need to find out why she is underweight and fix that first,” said Dr. Turan.
Neither Dr. Bodnar nor Dr. Turan had any relevant financial disclosures. One coauthor disclosed her institution received funds from the University of Pittsburgh. The study was funded by National Institutes of Health grants.
SOURCE: Bodnar LM et al. Obstet Gynecol. 2019;134:1075-86.
Lisa M. Bodnar, PhD, and colleagues determined.
The risks of cesarean section and neonatal death were elevated for those mothers who were overweight before pregnancy and then gained too much. But infants of underweight women who didn’t gain enough faced risks as well, wrote Dr. Bodnar of the University of Pittsburgh and associates in Obstetrics & Gynecology.
Among the most severely overweight women (obesity grade 2 or 3) who gained the most weight (43 kg) at 37 weeks’ gestation, there were 6 fewer small-for-gestational-age (SGA) infants per 100 births, but 14 more large-for-gestational-age (LGA) infants, 4 more cesarean deliveries, and 2 more neonatal deaths per 100 births. By contrast, among the most severely underweight women who gained the least amount of weight (9 kg), there were 18 more SGA infants, 3 fewer LGA infants, and 11 fewer cesareans, but 6 more preterm births before 32 weeks’ gestation.
The same U-shaped pattern also occurred within the individual weight categories. For example, compared with the outcomes among the most underweight women who gained least, among underweight women who gained the most (37 kg), there were eight fewer SGA infants, but four more LGA infants, 16 excess preterm births, and 9 excess infant deaths.
“If the associations we observed are even partially reflective of causality, targeted modification of pregnancy weight gain in women carrying twins might improve pregnancy outcomes,” wrote Dr. Bodnar and her team. “Data on a wide range of short- and long-term outcomes and information on the relative seriousness of these outcomes are needed to determine optimal gestational weight gain ranges for twin pregnancies.”
The cohort comprised 54,836 live-born twins from 27,723 twin pregnancies who were included in the MOMs database maintained by the University of Pennsylvania, Philadelphia. The population-based study tracks maternal obesity, gestational weight gain, and adverse birth outcomes. The information came from infant birth and death vital statistics records from 2003 to 2013.
However, this very source puts the findings in some degree of uncertainty, Ozhan Turan, MD, said in an interview.
“It’s a very nice study, and the statistics are very well done,” said Dr. Turan, who is the director of fetal therapy and complex obstetric surgery at the University of Maryland School of Medicine. “But that kind of data has pitfalls that are unavoidable. For example, they don’t have access to maternal medical comorbidities which are mostly related to the outcome, particularly gestational diabetes and preeclampsia. They also don’t have the information on chorionicity – and we know that monochorionic twins face much greater risk for these outcomes than dichorionic twins.”
The investigators calculated total gestational weight gain by subtracting prepregnancy weight from maternal weight at delivery. The analysis controlled for race and ethnicity, education, neonatal care, level of birth facility, parity, payment at delivery, smoking during pregnancy, marital status, year of birth, height, maternal age, preexisting diabetes or hypertension, infertility treatment, neonatal sex, and racial composition of neighborhood, as a proxy of neighborhood-level socioeconomic status. Approximately 16% of mothers received infertility treatment.
Of the cohort, 3% were underweight, 48% were normal weight, 24% were overweight, 13% were grade 1 obese, 7% grade 2 obese, and 5% grade 3 obese.
“Pregnancy weight gain was negatively associated with SGA and positively associated with LGA and cesarean delivery in all [body mass index] groups. For example, among normal-weight women, compared with a pregnancy weight gain equivalent to 20 kg at 37 weeks’ of gestation, a weight gain of 27 kg at 37 weeks’ of gestation was associated with 2.2 fewer cases of SGA but 2.9 more cases of LGA and 3.7 more cases of cesarean delivery,” Dr. Bodnar and associates wrote.
The investigators found that “weight gains well above or well below the [Institute of Medicine] provisional guidelines (less than 14 kg or more than 27 kg in underweight or normal-weight women, less than 11 kg or more than 28 kg in overweight women, and less than 6.4 kg or more than 26 kg in women with obesity) were associated with the highest risk of adverse outcomes.”
“I would not say this is practice-changing information,” said Dr. Turan. “We already know all this. What would be very helpful is an algorithm to tell us, if a patient is pregnant with twins, this is the amount of weight you have to gain.”
For overweight patients, Dr. Turan tries to impart the key message of moderate or slight weight gain, according to prepregnancy body mass index. For underweight patients, the picture is a bit more complex.
“There are not that many who are underweight before pregnancy, so first thing I look for is the reason a woman is underweight. Is she just not eating properly? Is there a drug dependence issue, alcohol dependence, HIV? Is there smoking? A gut problem that causes malnutrition. You can’t just say ‘eat more.’ That does not solve the problem. We need to find out why she is underweight and fix that first,” said Dr. Turan.
Neither Dr. Bodnar nor Dr. Turan had any relevant financial disclosures. One coauthor disclosed her institution received funds from the University of Pittsburgh. The study was funded by National Institutes of Health grants.
SOURCE: Bodnar LM et al. Obstet Gynecol. 2019;134:1075-86.
Lisa M. Bodnar, PhD, and colleagues determined.
The risks of cesarean section and neonatal death were elevated for those mothers who were overweight before pregnancy and then gained too much. But infants of underweight women who didn’t gain enough faced risks as well, wrote Dr. Bodnar of the University of Pittsburgh and associates in Obstetrics & Gynecology.
Among the most severely overweight women (obesity grade 2 or 3) who gained the most weight (43 kg) at 37 weeks’ gestation, there were 6 fewer small-for-gestational-age (SGA) infants per 100 births, but 14 more large-for-gestational-age (LGA) infants, 4 more cesarean deliveries, and 2 more neonatal deaths per 100 births. By contrast, among the most severely underweight women who gained the least amount of weight (9 kg), there were 18 more SGA infants, 3 fewer LGA infants, and 11 fewer cesareans, but 6 more preterm births before 32 weeks’ gestation.
The same U-shaped pattern also occurred within the individual weight categories. For example, compared with the outcomes among the most underweight women who gained least, among underweight women who gained the most (37 kg), there were eight fewer SGA infants, but four more LGA infants, 16 excess preterm births, and 9 excess infant deaths.
“If the associations we observed are even partially reflective of causality, targeted modification of pregnancy weight gain in women carrying twins might improve pregnancy outcomes,” wrote Dr. Bodnar and her team. “Data on a wide range of short- and long-term outcomes and information on the relative seriousness of these outcomes are needed to determine optimal gestational weight gain ranges for twin pregnancies.”
The cohort comprised 54,836 live-born twins from 27,723 twin pregnancies who were included in the MOMs database maintained by the University of Pennsylvania, Philadelphia. The population-based study tracks maternal obesity, gestational weight gain, and adverse birth outcomes. The information came from infant birth and death vital statistics records from 2003 to 2013.
However, this very source puts the findings in some degree of uncertainty, Ozhan Turan, MD, said in an interview.
“It’s a very nice study, and the statistics are very well done,” said Dr. Turan, who is the director of fetal therapy and complex obstetric surgery at the University of Maryland School of Medicine. “But that kind of data has pitfalls that are unavoidable. For example, they don’t have access to maternal medical comorbidities which are mostly related to the outcome, particularly gestational diabetes and preeclampsia. They also don’t have the information on chorionicity – and we know that monochorionic twins face much greater risk for these outcomes than dichorionic twins.”
The investigators calculated total gestational weight gain by subtracting prepregnancy weight from maternal weight at delivery. The analysis controlled for race and ethnicity, education, neonatal care, level of birth facility, parity, payment at delivery, smoking during pregnancy, marital status, year of birth, height, maternal age, preexisting diabetes or hypertension, infertility treatment, neonatal sex, and racial composition of neighborhood, as a proxy of neighborhood-level socioeconomic status. Approximately 16% of mothers received infertility treatment.
Of the cohort, 3% were underweight, 48% were normal weight, 24% were overweight, 13% were grade 1 obese, 7% grade 2 obese, and 5% grade 3 obese.
“Pregnancy weight gain was negatively associated with SGA and positively associated with LGA and cesarean delivery in all [body mass index] groups. For example, among normal-weight women, compared with a pregnancy weight gain equivalent to 20 kg at 37 weeks’ of gestation, a weight gain of 27 kg at 37 weeks’ of gestation was associated with 2.2 fewer cases of SGA but 2.9 more cases of LGA and 3.7 more cases of cesarean delivery,” Dr. Bodnar and associates wrote.
The investigators found that “weight gains well above or well below the [Institute of Medicine] provisional guidelines (less than 14 kg or more than 27 kg in underweight or normal-weight women, less than 11 kg or more than 28 kg in overweight women, and less than 6.4 kg or more than 26 kg in women with obesity) were associated with the highest risk of adverse outcomes.”
“I would not say this is practice-changing information,” said Dr. Turan. “We already know all this. What would be very helpful is an algorithm to tell us, if a patient is pregnant with twins, this is the amount of weight you have to gain.”
For overweight patients, Dr. Turan tries to impart the key message of moderate or slight weight gain, according to prepregnancy body mass index. For underweight patients, the picture is a bit more complex.
“There are not that many who are underweight before pregnancy, so first thing I look for is the reason a woman is underweight. Is she just not eating properly? Is there a drug dependence issue, alcohol dependence, HIV? Is there smoking? A gut problem that causes malnutrition. You can’t just say ‘eat more.’ That does not solve the problem. We need to find out why she is underweight and fix that first,” said Dr. Turan.
Neither Dr. Bodnar nor Dr. Turan had any relevant financial disclosures. One coauthor disclosed her institution received funds from the University of Pittsburgh. The study was funded by National Institutes of Health grants.
SOURCE: Bodnar LM et al. Obstet Gynecol. 2019;134:1075-86.
FROM OBSTETRICS & GYNECOLOGY
Faster enteral feeding does not up adverse outcomes risk in preterm infants
including moderate or severe neurodevelopmental disability and necrotizing enterocolitis, according to recent research published in the New England Journal of Medicine.
Although some data have shown rapidly increasing the speed of enteral-feeding volumes for preterm infants can raise the risk of necrotizing enterocolitis, these data are from observational case-control and uncontrolled studies, said Jon Dorling, MD, of the division of neonatal–perinatal medicine at Dalhousie University in Halifax, N.S., and colleagues in their study.
Dr. Doring and colleagues randomized 2,804 infants who were either very preterm or with a very low birth weight to receive daily milk increments at different volumes until the infants reached full feeding volume. Infants in the faster-increment group received daily milk at 30 mL per kg of body weight, while the slower-increment group received 18 mL per kg of body weight each day. The researchers analyzed infant survival without moderate or severe neurodevelopmental disability, with secondary outcomes of sepsis, necrotizing enterocolitis, and cerebral palsy at 24 months.
Overall, the researchers had information on the primary outcome for 87.4% of infants in the faster-increment group and 88.7% of infants in the slower-increment group. They found that 65.5% of infants in the faster-increment group and 68.1% of infants in the slower-increment group achieved an outcome of survival without moderate or severe neurodevelopmental disability at 24 months (adjusted risk ratio, 0.96; 95% confidence interval, 0.92-1.01; P equals .16). Secondary outcomes showed similar rates of adverse outcomes in the two groups, with 29.8% of infants in the faster-increment group and 31.1% of infants in the slower-increment group developing late-onset sepsis (aRR, 0.96; 95% CI, 0.86-1.07). Infants in the faster-increment group also had a similar rate of necrotizing enterocolitis (5.0%), compared with infants in the slower-increment group (5.6%) (aRR, 0.88; 95% CI, 0.68-1.16). Motor impairment was higher among infants in the faster-increment group (7.5%), compared with the slow-increment group (5.0%).
In the faster-increment group, the median number of days to reach full milk-feeding volumes was 7 vs. 10 in the slower-increment group.
“Although these feeding outcomes seem to favor faster increments, the risk of moderate or severe motor impairment was unexpectedly higher in the faster-increment group than in the slower-increment group,” the researchers said. “This observation is unexplained, and there were not more cases of late-onset sepsis or necrotizing enterocolitis in the faster-increment group.”
It is possible that it is a chance finding, since it was one of multiple secondary outcomes assessed, but biologically plausible explanations include increased cardiorespiratory events from pressure on the diaphragm or inability to absorb enteral nutrition,” they added.
The researchers said one potential limitation of the study was that it was unblinded.
This study was funded by the Health Technology Assessment Programme of the National Institute for Health Research. The authors reported various relationships with Baxter Bioscience, Chiesi Farmaceutici, Danone Early Life Nutrition, Fresenius Kabi USA LLC, National Institute for Health Research, Nestle Nutrition Institute, Nutrina, Medical Research Council, and Prolacta Biosciences in the form of consultancies, grants, travel reimbursement, board memberships, and editorial board appointments.
SOURCE: Doring J et al. N Eng J Med. 2019. doi: 10.1056/NEJMoa1816654.
including moderate or severe neurodevelopmental disability and necrotizing enterocolitis, according to recent research published in the New England Journal of Medicine.
Although some data have shown rapidly increasing the speed of enteral-feeding volumes for preterm infants can raise the risk of necrotizing enterocolitis, these data are from observational case-control and uncontrolled studies, said Jon Dorling, MD, of the division of neonatal–perinatal medicine at Dalhousie University in Halifax, N.S., and colleagues in their study.
Dr. Doring and colleagues randomized 2,804 infants who were either very preterm or with a very low birth weight to receive daily milk increments at different volumes until the infants reached full feeding volume. Infants in the faster-increment group received daily milk at 30 mL per kg of body weight, while the slower-increment group received 18 mL per kg of body weight each day. The researchers analyzed infant survival without moderate or severe neurodevelopmental disability, with secondary outcomes of sepsis, necrotizing enterocolitis, and cerebral palsy at 24 months.
Overall, the researchers had information on the primary outcome for 87.4% of infants in the faster-increment group and 88.7% of infants in the slower-increment group. They found that 65.5% of infants in the faster-increment group and 68.1% of infants in the slower-increment group achieved an outcome of survival without moderate or severe neurodevelopmental disability at 24 months (adjusted risk ratio, 0.96; 95% confidence interval, 0.92-1.01; P equals .16). Secondary outcomes showed similar rates of adverse outcomes in the two groups, with 29.8% of infants in the faster-increment group and 31.1% of infants in the slower-increment group developing late-onset sepsis (aRR, 0.96; 95% CI, 0.86-1.07). Infants in the faster-increment group also had a similar rate of necrotizing enterocolitis (5.0%), compared with infants in the slower-increment group (5.6%) (aRR, 0.88; 95% CI, 0.68-1.16). Motor impairment was higher among infants in the faster-increment group (7.5%), compared with the slow-increment group (5.0%).
In the faster-increment group, the median number of days to reach full milk-feeding volumes was 7 vs. 10 in the slower-increment group.
“Although these feeding outcomes seem to favor faster increments, the risk of moderate or severe motor impairment was unexpectedly higher in the faster-increment group than in the slower-increment group,” the researchers said. “This observation is unexplained, and there were not more cases of late-onset sepsis or necrotizing enterocolitis in the faster-increment group.”
It is possible that it is a chance finding, since it was one of multiple secondary outcomes assessed, but biologically plausible explanations include increased cardiorespiratory events from pressure on the diaphragm or inability to absorb enteral nutrition,” they added.
The researchers said one potential limitation of the study was that it was unblinded.
This study was funded by the Health Technology Assessment Programme of the National Institute for Health Research. The authors reported various relationships with Baxter Bioscience, Chiesi Farmaceutici, Danone Early Life Nutrition, Fresenius Kabi USA LLC, National Institute for Health Research, Nestle Nutrition Institute, Nutrina, Medical Research Council, and Prolacta Biosciences in the form of consultancies, grants, travel reimbursement, board memberships, and editorial board appointments.
SOURCE: Doring J et al. N Eng J Med. 2019. doi: 10.1056/NEJMoa1816654.
including moderate or severe neurodevelopmental disability and necrotizing enterocolitis, according to recent research published in the New England Journal of Medicine.
Although some data have shown rapidly increasing the speed of enteral-feeding volumes for preterm infants can raise the risk of necrotizing enterocolitis, these data are from observational case-control and uncontrolled studies, said Jon Dorling, MD, of the division of neonatal–perinatal medicine at Dalhousie University in Halifax, N.S., and colleagues in their study.
Dr. Doring and colleagues randomized 2,804 infants who were either very preterm or with a very low birth weight to receive daily milk increments at different volumes until the infants reached full feeding volume. Infants in the faster-increment group received daily milk at 30 mL per kg of body weight, while the slower-increment group received 18 mL per kg of body weight each day. The researchers analyzed infant survival without moderate or severe neurodevelopmental disability, with secondary outcomes of sepsis, necrotizing enterocolitis, and cerebral palsy at 24 months.
Overall, the researchers had information on the primary outcome for 87.4% of infants in the faster-increment group and 88.7% of infants in the slower-increment group. They found that 65.5% of infants in the faster-increment group and 68.1% of infants in the slower-increment group achieved an outcome of survival without moderate or severe neurodevelopmental disability at 24 months (adjusted risk ratio, 0.96; 95% confidence interval, 0.92-1.01; P equals .16). Secondary outcomes showed similar rates of adverse outcomes in the two groups, with 29.8% of infants in the faster-increment group and 31.1% of infants in the slower-increment group developing late-onset sepsis (aRR, 0.96; 95% CI, 0.86-1.07). Infants in the faster-increment group also had a similar rate of necrotizing enterocolitis (5.0%), compared with infants in the slower-increment group (5.6%) (aRR, 0.88; 95% CI, 0.68-1.16). Motor impairment was higher among infants in the faster-increment group (7.5%), compared with the slow-increment group (5.0%).
In the faster-increment group, the median number of days to reach full milk-feeding volumes was 7 vs. 10 in the slower-increment group.
“Although these feeding outcomes seem to favor faster increments, the risk of moderate or severe motor impairment was unexpectedly higher in the faster-increment group than in the slower-increment group,” the researchers said. “This observation is unexplained, and there were not more cases of late-onset sepsis or necrotizing enterocolitis in the faster-increment group.”
It is possible that it is a chance finding, since it was one of multiple secondary outcomes assessed, but biologically plausible explanations include increased cardiorespiratory events from pressure on the diaphragm or inability to absorb enteral nutrition,” they added.
The researchers said one potential limitation of the study was that it was unblinded.
This study was funded by the Health Technology Assessment Programme of the National Institute for Health Research. The authors reported various relationships with Baxter Bioscience, Chiesi Farmaceutici, Danone Early Life Nutrition, Fresenius Kabi USA LLC, National Institute for Health Research, Nestle Nutrition Institute, Nutrina, Medical Research Council, and Prolacta Biosciences in the form of consultancies, grants, travel reimbursement, board memberships, and editorial board appointments.
SOURCE: Doring J et al. N Eng J Med. 2019. doi: 10.1056/NEJMoa1816654.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Congenital syphilis continues to rise at an alarming rate
One of the nation’s most preventable diseases is killing newborns in ever-increasing numbers.
Seventy-eight of those babies were stillborn, and 16 died after birth.
In California, cases of congenital syphilis – the term used when a mother passes the infection to her baby during pregnancy – continued a stark 7-year climb, to 332 cases, an 18.1% increase from 2017, according to the federal data. Only Texas, Nevada, Louisiana, and Arizona had congenital syphilis rates higher than California’s. Those five states combined made up nearly two-thirds of total cases, although all but 17 states saw increases in their congenital syphilis rates.
The state-by-state numbers were released as part of a broader report from the Centers for Disease Control and Prevention tracking trends in sexually transmitted diseases. Cases of syphilis, gonorrhea, and chlamydia combined reached an all-time high in 2018. Cases of the most infectious stage of syphilis rose 14% to more than 35,000 cases; gonorrhea increased 5% to more than 580,000 cases; and chlamydia increased 3% to more than 1.7 million cases.
For veteran public health workers, the upward trend in congenital syphilis numbers is particularly disturbing because the condition is so easy to prevent. Blood tests can identify infection in pregnant women. The treatment is relatively simple and effective. When caught during pregnancy, transmission from mother to baby generally can be stopped.
“When we see a case of congenital syphilis, it is a hallmark of a health system and a health care failure,” said Virginia Bowen, PhD, an epidemiologist with the CDC and an author of the report.
It takes just a few shots of antibiotics to prevent a baby from getting syphilis from its mother. Left untreated, Treponema pallidum, the corkscrew-shaped organism that causes syphilis, can wiggle its way through a mother’s placenta and into a fetus. Once there, it can multiply furiously, invading every part of the body.
The effects on a newborn can be devastating. Philip Cheng, MD, is a neonatologist at St. Joseph’s Medical Center in Stockton, a city in San Joaquin County in California’s Central Valley. Twenty-six babies were infected last year in San Joaquin County, according to state data.
The brain of one of Cheng’s patients didn’t develop properly and the baby died shortly after birth. Other young patients survive but battle blood abnormalities, bone deformities, and organ damage. Congenital syphilis can cause blindness and excruciating pain.
Public health departments across the Central Valley, a largely rural expanse, report similar experiences. Following the release of the CDC report Tuesday, the California Department of Public Health released its county-by-county numbers for 2018. The report showed syphilis, gonorrhea, and chlamydia levels at their highest in 30 years, and attributed 22 stillbirths or neonatal deaths to congenital syphilis.
For the past several years, Fresno County, which had 63 cases of congenital syphilis in 2017, had the highest rate in California. In 2018, Fresno fell to fourth, behind Yuba, Kern, and San Joaquin counties. But the epidemic is far from under control. “I couldn’t even tell you how soon I think we’re going to see a decrease,” said Jena Adams, who oversees HIV and STD programs for Fresno County.
Syphilis was once a prolific and widely feared STD. But by the 1940s, penicillin was found to have a near-perfect cure rate for the disease. By 2000, syphilis rates were so low in the U.S. that the federal government launched a plan to eliminate the disease. Today, that goal is a distant memory.
Health departments once tracked down every person who tested positive for chlamydia, gonorrhea, or syphilis, to make sure they and their partners got treatment. With limited funds and climbing caseloads, many states now devote resources only to tracking syphilis. The caseloads are so high in some California counties that they track only women of childbearing age or just pregnant women.
“A lot of the funding for day-to-day public health work isn’t there,” said Jeffrey Klausner, MD, a professor at the University of California-Los Angeles who ran San Francisco’s STD program for more than a decade.
The bulk of STD prevention funding is appropriated by Congress to the CDC, which passes it on to states. That funding has been largely flat since 2003, according to data from the National Coalition of STD Directors, which represents health departments across the country. Take into account inflation and the growing caseloads, and the money is spread thinner. “It takes money, it takes training, it takes resources,” Dr. Klausner said, “and policymakers have just not prioritized that.”
A report this year by Trust for America’s Health, a public health policy research and advocacy group, estimated that 55,000 jobs were cut from local public health departments from 2008 to 2017. “We have our hands tied as much as [states] do,” said Dr. Bowen of the CDC. “We take what we’re given and try to distribute it as fairly as we can.”
San Joaquin County health officials have reorganized the department and applied for grants to increase the number of investigators available while congenital syphilis has spiked, said Hemal Parikh, county coordinator for STD control. But even with new hires and cutting back to tracking only women of childbearing age with syphilis, an investigator can have anywhere from 20 to 30 open cases at a time. In other counties, the caseload can be double that.
In 2018, Jennifer Wagman, PhD, a UCLA professor who studies infectious diseases and gender inequality, was part of a group that received CDC funding to look into what is causing the spike in congenital syphilis in California’s Central Valley.
Dr. Wagman said that, after years of studying health systems in other countries, she was shocked to see how much basic public health infrastructure has crumbled in California. In many parts of the Central Valley, county walk-in clinics that tested for and treated STDs were shuttered in the wake of the recession. That left few places for drop-in care, and investigators with no place to take someone for immediate treatment. Investigators or their patients must make appointments at one of the few providers who carry the right kind of treatment and hope the patients can keep the appointment when the time comes.
In focus groups, women told Dr. Wagman that working hourly jobs, or dealing with chaotic lives involving homelessness, abusive partners, and drug use, can make it all but impossible to stick to the appointments required at private clinics.
Dr. Wagman found that women in these high-risk groups were seeking care, though sometimes late in their pregnancy. They were just more likely to visit an emergency room, urgent care, or even a methadone clinic – places that take drop-ins but don’t necessarily routinely test for or treat syphilis.
“These people already have a million barriers,” said Jenny Malone, the public health nurse for San Joaquin County. “Now there are more.”
The most challenging cases in California are wrapped up with the state’s growing housing crisis and a methamphetamine epidemic with few treatment options. Women who are homeless often have unreliable contact information and are unlikely to have a primary care doctor. That makes them tough to track down to give a positive diagnosis or to follow up on a treatment plan.
Louisiana had the highest rate of congenital syphilis in the country for several years – until 2018. After a 22% drop in its rate, combined with increases in other states, Louisiana now ranks behind Texas and Nevada. That drop is the direct result of $550 million in temporary supplemental funding that the CDC gave the state to combat the epidemic, said Chaquetta Johnson, DNP, deputy director of operations for the state’s STD/HIV/hepatitis program. The money helped bolster the state’s lagging public health infrastructure. It was used to host two conferences for providers in the hardest-hit areas, hire two case managers and a nurse educator, create a program for in-home treatment, and improve data systems to track cases, among other things.
In California, more than 40% of pregnant women with syphilis passed it on to their baby in 2016, the most recent year for which data is available. Gov. Gavin Newsom (D) made additional funding available this year, but it’s a “drop in the bucket,” said Sergio Morales of Essential Access Health, a nonprofit that focuses on sexual and reproductive health and is working with Kern County on congenital syphilis. “We are seeing the results of years of inaction and a lack of prioritization of STD prevention, and we’re now paying the price.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
[Update: This story was revised at 6:50 p.m. ET on Oct. 8 to reflect news developments.]
One of the nation’s most preventable diseases is killing newborns in ever-increasing numbers.
Seventy-eight of those babies were stillborn, and 16 died after birth.
In California, cases of congenital syphilis – the term used when a mother passes the infection to her baby during pregnancy – continued a stark 7-year climb, to 332 cases, an 18.1% increase from 2017, according to the federal data. Only Texas, Nevada, Louisiana, and Arizona had congenital syphilis rates higher than California’s. Those five states combined made up nearly two-thirds of total cases, although all but 17 states saw increases in their congenital syphilis rates.
The state-by-state numbers were released as part of a broader report from the Centers for Disease Control and Prevention tracking trends in sexually transmitted diseases. Cases of syphilis, gonorrhea, and chlamydia combined reached an all-time high in 2018. Cases of the most infectious stage of syphilis rose 14% to more than 35,000 cases; gonorrhea increased 5% to more than 580,000 cases; and chlamydia increased 3% to more than 1.7 million cases.
For veteran public health workers, the upward trend in congenital syphilis numbers is particularly disturbing because the condition is so easy to prevent. Blood tests can identify infection in pregnant women. The treatment is relatively simple and effective. When caught during pregnancy, transmission from mother to baby generally can be stopped.
“When we see a case of congenital syphilis, it is a hallmark of a health system and a health care failure,” said Virginia Bowen, PhD, an epidemiologist with the CDC and an author of the report.
It takes just a few shots of antibiotics to prevent a baby from getting syphilis from its mother. Left untreated, Treponema pallidum, the corkscrew-shaped organism that causes syphilis, can wiggle its way through a mother’s placenta and into a fetus. Once there, it can multiply furiously, invading every part of the body.
The effects on a newborn can be devastating. Philip Cheng, MD, is a neonatologist at St. Joseph’s Medical Center in Stockton, a city in San Joaquin County in California’s Central Valley. Twenty-six babies were infected last year in San Joaquin County, according to state data.
The brain of one of Cheng’s patients didn’t develop properly and the baby died shortly after birth. Other young patients survive but battle blood abnormalities, bone deformities, and organ damage. Congenital syphilis can cause blindness and excruciating pain.
Public health departments across the Central Valley, a largely rural expanse, report similar experiences. Following the release of the CDC report Tuesday, the California Department of Public Health released its county-by-county numbers for 2018. The report showed syphilis, gonorrhea, and chlamydia levels at their highest in 30 years, and attributed 22 stillbirths or neonatal deaths to congenital syphilis.
For the past several years, Fresno County, which had 63 cases of congenital syphilis in 2017, had the highest rate in California. In 2018, Fresno fell to fourth, behind Yuba, Kern, and San Joaquin counties. But the epidemic is far from under control. “I couldn’t even tell you how soon I think we’re going to see a decrease,” said Jena Adams, who oversees HIV and STD programs for Fresno County.
Syphilis was once a prolific and widely feared STD. But by the 1940s, penicillin was found to have a near-perfect cure rate for the disease. By 2000, syphilis rates were so low in the U.S. that the federal government launched a plan to eliminate the disease. Today, that goal is a distant memory.
Health departments once tracked down every person who tested positive for chlamydia, gonorrhea, or syphilis, to make sure they and their partners got treatment. With limited funds and climbing caseloads, many states now devote resources only to tracking syphilis. The caseloads are so high in some California counties that they track only women of childbearing age or just pregnant women.
“A lot of the funding for day-to-day public health work isn’t there,” said Jeffrey Klausner, MD, a professor at the University of California-Los Angeles who ran San Francisco’s STD program for more than a decade.
The bulk of STD prevention funding is appropriated by Congress to the CDC, which passes it on to states. That funding has been largely flat since 2003, according to data from the National Coalition of STD Directors, which represents health departments across the country. Take into account inflation and the growing caseloads, and the money is spread thinner. “It takes money, it takes training, it takes resources,” Dr. Klausner said, “and policymakers have just not prioritized that.”
A report this year by Trust for America’s Health, a public health policy research and advocacy group, estimated that 55,000 jobs were cut from local public health departments from 2008 to 2017. “We have our hands tied as much as [states] do,” said Dr. Bowen of the CDC. “We take what we’re given and try to distribute it as fairly as we can.”
San Joaquin County health officials have reorganized the department and applied for grants to increase the number of investigators available while congenital syphilis has spiked, said Hemal Parikh, county coordinator for STD control. But even with new hires and cutting back to tracking only women of childbearing age with syphilis, an investigator can have anywhere from 20 to 30 open cases at a time. In other counties, the caseload can be double that.
In 2018, Jennifer Wagman, PhD, a UCLA professor who studies infectious diseases and gender inequality, was part of a group that received CDC funding to look into what is causing the spike in congenital syphilis in California’s Central Valley.
Dr. Wagman said that, after years of studying health systems in other countries, she was shocked to see how much basic public health infrastructure has crumbled in California. In many parts of the Central Valley, county walk-in clinics that tested for and treated STDs were shuttered in the wake of the recession. That left few places for drop-in care, and investigators with no place to take someone for immediate treatment. Investigators or their patients must make appointments at one of the few providers who carry the right kind of treatment and hope the patients can keep the appointment when the time comes.
In focus groups, women told Dr. Wagman that working hourly jobs, or dealing with chaotic lives involving homelessness, abusive partners, and drug use, can make it all but impossible to stick to the appointments required at private clinics.
Dr. Wagman found that women in these high-risk groups were seeking care, though sometimes late in their pregnancy. They were just more likely to visit an emergency room, urgent care, or even a methadone clinic – places that take drop-ins but don’t necessarily routinely test for or treat syphilis.
“These people already have a million barriers,” said Jenny Malone, the public health nurse for San Joaquin County. “Now there are more.”
The most challenging cases in California are wrapped up with the state’s growing housing crisis and a methamphetamine epidemic with few treatment options. Women who are homeless often have unreliable contact information and are unlikely to have a primary care doctor. That makes them tough to track down to give a positive diagnosis or to follow up on a treatment plan.
Louisiana had the highest rate of congenital syphilis in the country for several years – until 2018. After a 22% drop in its rate, combined with increases in other states, Louisiana now ranks behind Texas and Nevada. That drop is the direct result of $550 million in temporary supplemental funding that the CDC gave the state to combat the epidemic, said Chaquetta Johnson, DNP, deputy director of operations for the state’s STD/HIV/hepatitis program. The money helped bolster the state’s lagging public health infrastructure. It was used to host two conferences for providers in the hardest-hit areas, hire two case managers and a nurse educator, create a program for in-home treatment, and improve data systems to track cases, among other things.
In California, more than 40% of pregnant women with syphilis passed it on to their baby in 2016, the most recent year for which data is available. Gov. Gavin Newsom (D) made additional funding available this year, but it’s a “drop in the bucket,” said Sergio Morales of Essential Access Health, a nonprofit that focuses on sexual and reproductive health and is working with Kern County on congenital syphilis. “We are seeing the results of years of inaction and a lack of prioritization of STD prevention, and we’re now paying the price.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
[Update: This story was revised at 6:50 p.m. ET on Oct. 8 to reflect news developments.]
One of the nation’s most preventable diseases is killing newborns in ever-increasing numbers.
Seventy-eight of those babies were stillborn, and 16 died after birth.
In California, cases of congenital syphilis – the term used when a mother passes the infection to her baby during pregnancy – continued a stark 7-year climb, to 332 cases, an 18.1% increase from 2017, according to the federal data. Only Texas, Nevada, Louisiana, and Arizona had congenital syphilis rates higher than California’s. Those five states combined made up nearly two-thirds of total cases, although all but 17 states saw increases in their congenital syphilis rates.
The state-by-state numbers were released as part of a broader report from the Centers for Disease Control and Prevention tracking trends in sexually transmitted diseases. Cases of syphilis, gonorrhea, and chlamydia combined reached an all-time high in 2018. Cases of the most infectious stage of syphilis rose 14% to more than 35,000 cases; gonorrhea increased 5% to more than 580,000 cases; and chlamydia increased 3% to more than 1.7 million cases.
For veteran public health workers, the upward trend in congenital syphilis numbers is particularly disturbing because the condition is so easy to prevent. Blood tests can identify infection in pregnant women. The treatment is relatively simple and effective. When caught during pregnancy, transmission from mother to baby generally can be stopped.
“When we see a case of congenital syphilis, it is a hallmark of a health system and a health care failure,” said Virginia Bowen, PhD, an epidemiologist with the CDC and an author of the report.
It takes just a few shots of antibiotics to prevent a baby from getting syphilis from its mother. Left untreated, Treponema pallidum, the corkscrew-shaped organism that causes syphilis, can wiggle its way through a mother’s placenta and into a fetus. Once there, it can multiply furiously, invading every part of the body.
The effects on a newborn can be devastating. Philip Cheng, MD, is a neonatologist at St. Joseph’s Medical Center in Stockton, a city in San Joaquin County in California’s Central Valley. Twenty-six babies were infected last year in San Joaquin County, according to state data.
The brain of one of Cheng’s patients didn’t develop properly and the baby died shortly after birth. Other young patients survive but battle blood abnormalities, bone deformities, and organ damage. Congenital syphilis can cause blindness and excruciating pain.
Public health departments across the Central Valley, a largely rural expanse, report similar experiences. Following the release of the CDC report Tuesday, the California Department of Public Health released its county-by-county numbers for 2018. The report showed syphilis, gonorrhea, and chlamydia levels at their highest in 30 years, and attributed 22 stillbirths or neonatal deaths to congenital syphilis.
For the past several years, Fresno County, which had 63 cases of congenital syphilis in 2017, had the highest rate in California. In 2018, Fresno fell to fourth, behind Yuba, Kern, and San Joaquin counties. But the epidemic is far from under control. “I couldn’t even tell you how soon I think we’re going to see a decrease,” said Jena Adams, who oversees HIV and STD programs for Fresno County.
Syphilis was once a prolific and widely feared STD. But by the 1940s, penicillin was found to have a near-perfect cure rate for the disease. By 2000, syphilis rates were so low in the U.S. that the federal government launched a plan to eliminate the disease. Today, that goal is a distant memory.
Health departments once tracked down every person who tested positive for chlamydia, gonorrhea, or syphilis, to make sure they and their partners got treatment. With limited funds and climbing caseloads, many states now devote resources only to tracking syphilis. The caseloads are so high in some California counties that they track only women of childbearing age or just pregnant women.
“A lot of the funding for day-to-day public health work isn’t there,” said Jeffrey Klausner, MD, a professor at the University of California-Los Angeles who ran San Francisco’s STD program for more than a decade.
The bulk of STD prevention funding is appropriated by Congress to the CDC, which passes it on to states. That funding has been largely flat since 2003, according to data from the National Coalition of STD Directors, which represents health departments across the country. Take into account inflation and the growing caseloads, and the money is spread thinner. “It takes money, it takes training, it takes resources,” Dr. Klausner said, “and policymakers have just not prioritized that.”
A report this year by Trust for America’s Health, a public health policy research and advocacy group, estimated that 55,000 jobs were cut from local public health departments from 2008 to 2017. “We have our hands tied as much as [states] do,” said Dr. Bowen of the CDC. “We take what we’re given and try to distribute it as fairly as we can.”
San Joaquin County health officials have reorganized the department and applied for grants to increase the number of investigators available while congenital syphilis has spiked, said Hemal Parikh, county coordinator for STD control. But even with new hires and cutting back to tracking only women of childbearing age with syphilis, an investigator can have anywhere from 20 to 30 open cases at a time. In other counties, the caseload can be double that.
In 2018, Jennifer Wagman, PhD, a UCLA professor who studies infectious diseases and gender inequality, was part of a group that received CDC funding to look into what is causing the spike in congenital syphilis in California’s Central Valley.
Dr. Wagman said that, after years of studying health systems in other countries, she was shocked to see how much basic public health infrastructure has crumbled in California. In many parts of the Central Valley, county walk-in clinics that tested for and treated STDs were shuttered in the wake of the recession. That left few places for drop-in care, and investigators with no place to take someone for immediate treatment. Investigators or their patients must make appointments at one of the few providers who carry the right kind of treatment and hope the patients can keep the appointment when the time comes.
In focus groups, women told Dr. Wagman that working hourly jobs, or dealing with chaotic lives involving homelessness, abusive partners, and drug use, can make it all but impossible to stick to the appointments required at private clinics.
Dr. Wagman found that women in these high-risk groups were seeking care, though sometimes late in their pregnancy. They were just more likely to visit an emergency room, urgent care, or even a methadone clinic – places that take drop-ins but don’t necessarily routinely test for or treat syphilis.
“These people already have a million barriers,” said Jenny Malone, the public health nurse for San Joaquin County. “Now there are more.”
The most challenging cases in California are wrapped up with the state’s growing housing crisis and a methamphetamine epidemic with few treatment options. Women who are homeless often have unreliable contact information and are unlikely to have a primary care doctor. That makes them tough to track down to give a positive diagnosis or to follow up on a treatment plan.
Louisiana had the highest rate of congenital syphilis in the country for several years – until 2018. After a 22% drop in its rate, combined with increases in other states, Louisiana now ranks behind Texas and Nevada. That drop is the direct result of $550 million in temporary supplemental funding that the CDC gave the state to combat the epidemic, said Chaquetta Johnson, DNP, deputy director of operations for the state’s STD/HIV/hepatitis program. The money helped bolster the state’s lagging public health infrastructure. It was used to host two conferences for providers in the hardest-hit areas, hire two case managers and a nurse educator, create a program for in-home treatment, and improve data systems to track cases, among other things.
In California, more than 40% of pregnant women with syphilis passed it on to their baby in 2016, the most recent year for which data is available. Gov. Gavin Newsom (D) made additional funding available this year, but it’s a “drop in the bucket,” said Sergio Morales of Essential Access Health, a nonprofit that focuses on sexual and reproductive health and is working with Kern County on congenital syphilis. “We are seeing the results of years of inaction and a lack of prioritization of STD prevention, and we’re now paying the price.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
[Update: This story was revised at 6:50 p.m. ET on Oct. 8 to reflect news developments.]