User login
USPSTF recommends counseling for perinatal depression prevention
according to a B recommendation from the U.S. Preventive Services Task Force.
The Task Force determined that counseling interventions are effective in preventing perinatal depression, defined as a major or minor depressive episode during pregnancy or within the first year after delivery. The condition affects an estimated 12% of new mothers in the United States each year, according to lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and her colleagues.
The recommendation, published in JAMA, applies to “pregnant persons and persons who are less than 1 year postpartum who do not have a current diagnosis of depression but are at increased risk of developing depression,” according to the authors (JAMA. 2019 Feb 12;321(6):580-7).
Risk factors for development of perinatal depression include:
- Past history of depression.
- Current depressive symptoms (that do not reach a diagnostic threshold).
- History of physical or sexual abuse.
- Unplanned or unwanted pregnancy.
- Stressful life events.
- Lack of social and financial support.
- Intimate partner violence.
- Pregestational or gestational diabetes.
- Complications during pregnancy.
- Adolescent parenthood.
- Low socioeconomic status.
- Lack of social support.
After reviewing the evidence, the USPSTF found a moderate net benefit for counseling interventions, particularly cognitive behavioral therapy and interpersonal therapy, for preventing perinatal depression in women at risk. Counseling sessions reviewed for this recommendation ranged from 4 to 20 meetings (median, 8 meetings).
The USPSTF found inadequate evidence to assess the harms and benefits of other noncounseling interventions, including pharmacologic therapy.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente, Portland, Ore., and her colleagues analyzed data from 50 studies including 22,385 individuals; 20 of these studies were randomized, controlled trials of counseling interventions (JAMA. 2019 Feb 12;321(6):588-601).
Overall, the likelihood of perinatal depression was significantly lower among women who received counseling, compared with controls, among more than 3,000 women in those studies (pooled risk ratio 0.61). Absolute risk differences for perinatal depression ranged from a 1% increased reduction in controls to a 32% increased reduction among women who received counseling. The effects were strongest for cognitive behavioral therapy and interpersonal therapy as interventions. No adverse events were reported in the counseling intervention studies.
In three studies of health system interventions, the researchers found a benefit for interventions vs. controls, but the difference was not statistically significant.
Trials of most other alternative interventions including infant sleep advice, birth-experience postpartum debriefing, omega-3 fatty acid supplementation, expressive writing, antidepressants, and yoga did not show statistical significance in benefit for reducing perinatal depression.
Only one of three randomized controlled trials of physical activity found a statistically significant group difference.
A trial of nortriptyline to prevent perinatal depression showed no benefit, compared with placebo. A sertraline study of found “a smaller percentage of participants taking sertraline had a depression recurrence, compared with those taking placebo,” the investigators wrote. In these two studies, women who took nortriptyline showed no adverse effects, and those in a trial involving sertraline reported significantly more dizziness and drowsiness compared with placebo patients.
The evidence review was limited by the small number of quality studies, especially studies of alternative interventions. More research is needed; however, the findings support data from similar reviews and support the potential for counseling to prevent perinatal depression, particularly in women at increased risk for perinatal depression, Dr. O’Connor and her associates said.
The USPSTF is supported by the Agency for Healthcare Research and Quality. Coauthor Dr. Michelle L. Henninger reported receiving grants from Pfizer IGLC (Independent Grants for Learning & Change) outside the submitted work. Coauthor Dr. Bradley N. Gaynes reported receiving personal fees from LivaNova and Johnson & Johnson outside the submitted work. The remaining researchers had no financial conflicts to disclose.
SOURCE: Curry SJ et al. JAMA. 2019;321(6):580-7; O’Connor E et al. JAMA. 2019;321(6):588-601.
A proactive approach to prevention and management of perinatal depression as recommended by the USPSTF can potentially improve outcomes for new mothers and their babies, Marlene P. Freeman, MD, wrote in an accompanying editorial. She identified three key challenges to implementing the USPSTF recommendations: identifying women at risk, connecting them to evidence-based treatment, and assessing outcomes after treatment.
The development of screening tools would help clinicians identify women at risk for perinatal depression, Dr. Freeman said. No such tool currently exists, but in the meantime, “women at risk may be identified by targeting those with histories of depression, subthreshold depressive symptoms, and certain sociodemographic factors (i.e., economically disadvantaged, single/young, unplanned pregnancy).”
The counseling interventions shown to be effective in preventing perinatal depression – cognitive behavioral therapy and interpersonal psychotherapy – require education and training outside the time limitations and expertise of many clinicians providing obstetric care, she noted.
“The delivery of effective care on a large scale will require creative solutions,” such as the use of telehealth and smartphone platforms, and the involvement of multidisciplinary teams to care for women with severe illness, Dr. Freeman said. “In addition, a substantial number of reproductive-aged women have serious psychiatric disorders and will be identified as at risk for perinatal depression, although their needs may be more comprehensive,” she wrote. “Women who are identified as at risk for perinatal depression may have psychotic disorders, bipolar spectrum disorders, anxiety disorders, and substance use disorders, and there is comorbidity among psychiatric disorders. Therefore, systematic provisions for referral and treatment for other psychiatric disorders should be considered.” Further research is needed to explore treatment options including pharmacotherapy for women with severe psychiatric disorders.
However, she expressed optimism that the recommendations for screening and counseling for perinatal depression are valuable, and they “may return great dividends in the form of enhanced well-being of mothers and their offspring.”
Dr. Freeman is affiliated with the department of psychiatry at Massachusetts General Hospital, Boston. She commented in an editorial accompanying the article by Curry et al. (JAMA. 2019 Feb 12;321[6]:550-2). Dr. Freeman disclosed relationships with companies including Takeda, JayMac, Sage, Otsuka, Alkermes, Janssen, and Sunovion; she also disclosed serving on an independent data safety and monitoring committee for Janssen (Johnson & Johnson); and editing the GOED (Global Organization for EPA & DHA Omega-3) newsletter.
A proactive approach to prevention and management of perinatal depression as recommended by the USPSTF can potentially improve outcomes for new mothers and their babies, Marlene P. Freeman, MD, wrote in an accompanying editorial. She identified three key challenges to implementing the USPSTF recommendations: identifying women at risk, connecting them to evidence-based treatment, and assessing outcomes after treatment.
The development of screening tools would help clinicians identify women at risk for perinatal depression, Dr. Freeman said. No such tool currently exists, but in the meantime, “women at risk may be identified by targeting those with histories of depression, subthreshold depressive symptoms, and certain sociodemographic factors (i.e., economically disadvantaged, single/young, unplanned pregnancy).”
The counseling interventions shown to be effective in preventing perinatal depression – cognitive behavioral therapy and interpersonal psychotherapy – require education and training outside the time limitations and expertise of many clinicians providing obstetric care, she noted.
“The delivery of effective care on a large scale will require creative solutions,” such as the use of telehealth and smartphone platforms, and the involvement of multidisciplinary teams to care for women with severe illness, Dr. Freeman said. “In addition, a substantial number of reproductive-aged women have serious psychiatric disorders and will be identified as at risk for perinatal depression, although their needs may be more comprehensive,” she wrote. “Women who are identified as at risk for perinatal depression may have psychotic disorders, bipolar spectrum disorders, anxiety disorders, and substance use disorders, and there is comorbidity among psychiatric disorders. Therefore, systematic provisions for referral and treatment for other psychiatric disorders should be considered.” Further research is needed to explore treatment options including pharmacotherapy for women with severe psychiatric disorders.
However, she expressed optimism that the recommendations for screening and counseling for perinatal depression are valuable, and they “may return great dividends in the form of enhanced well-being of mothers and their offspring.”
Dr. Freeman is affiliated with the department of psychiatry at Massachusetts General Hospital, Boston. She commented in an editorial accompanying the article by Curry et al. (JAMA. 2019 Feb 12;321[6]:550-2). Dr. Freeman disclosed relationships with companies including Takeda, JayMac, Sage, Otsuka, Alkermes, Janssen, and Sunovion; she also disclosed serving on an independent data safety and monitoring committee for Janssen (Johnson & Johnson); and editing the GOED (Global Organization for EPA & DHA Omega-3) newsletter.
A proactive approach to prevention and management of perinatal depression as recommended by the USPSTF can potentially improve outcomes for new mothers and their babies, Marlene P. Freeman, MD, wrote in an accompanying editorial. She identified three key challenges to implementing the USPSTF recommendations: identifying women at risk, connecting them to evidence-based treatment, and assessing outcomes after treatment.
The development of screening tools would help clinicians identify women at risk for perinatal depression, Dr. Freeman said. No such tool currently exists, but in the meantime, “women at risk may be identified by targeting those with histories of depression, subthreshold depressive symptoms, and certain sociodemographic factors (i.e., economically disadvantaged, single/young, unplanned pregnancy).”
The counseling interventions shown to be effective in preventing perinatal depression – cognitive behavioral therapy and interpersonal psychotherapy – require education and training outside the time limitations and expertise of many clinicians providing obstetric care, she noted.
“The delivery of effective care on a large scale will require creative solutions,” such as the use of telehealth and smartphone platforms, and the involvement of multidisciplinary teams to care for women with severe illness, Dr. Freeman said. “In addition, a substantial number of reproductive-aged women have serious psychiatric disorders and will be identified as at risk for perinatal depression, although their needs may be more comprehensive,” she wrote. “Women who are identified as at risk for perinatal depression may have psychotic disorders, bipolar spectrum disorders, anxiety disorders, and substance use disorders, and there is comorbidity among psychiatric disorders. Therefore, systematic provisions for referral and treatment for other psychiatric disorders should be considered.” Further research is needed to explore treatment options including pharmacotherapy for women with severe psychiatric disorders.
However, she expressed optimism that the recommendations for screening and counseling for perinatal depression are valuable, and they “may return great dividends in the form of enhanced well-being of mothers and their offspring.”
Dr. Freeman is affiliated with the department of psychiatry at Massachusetts General Hospital, Boston. She commented in an editorial accompanying the article by Curry et al. (JAMA. 2019 Feb 12;321[6]:550-2). Dr. Freeman disclosed relationships with companies including Takeda, JayMac, Sage, Otsuka, Alkermes, Janssen, and Sunovion; she also disclosed serving on an independent data safety and monitoring committee for Janssen (Johnson & Johnson); and editing the GOED (Global Organization for EPA & DHA Omega-3) newsletter.
according to a B recommendation from the U.S. Preventive Services Task Force.
The Task Force determined that counseling interventions are effective in preventing perinatal depression, defined as a major or minor depressive episode during pregnancy or within the first year after delivery. The condition affects an estimated 12% of new mothers in the United States each year, according to lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and her colleagues.
The recommendation, published in JAMA, applies to “pregnant persons and persons who are less than 1 year postpartum who do not have a current diagnosis of depression but are at increased risk of developing depression,” according to the authors (JAMA. 2019 Feb 12;321(6):580-7).
Risk factors for development of perinatal depression include:
- Past history of depression.
- Current depressive symptoms (that do not reach a diagnostic threshold).
- History of physical or sexual abuse.
- Unplanned or unwanted pregnancy.
- Stressful life events.
- Lack of social and financial support.
- Intimate partner violence.
- Pregestational or gestational diabetes.
- Complications during pregnancy.
- Adolescent parenthood.
- Low socioeconomic status.
- Lack of social support.
After reviewing the evidence, the USPSTF found a moderate net benefit for counseling interventions, particularly cognitive behavioral therapy and interpersonal therapy, for preventing perinatal depression in women at risk. Counseling sessions reviewed for this recommendation ranged from 4 to 20 meetings (median, 8 meetings).
The USPSTF found inadequate evidence to assess the harms and benefits of other noncounseling interventions, including pharmacologic therapy.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente, Portland, Ore., and her colleagues analyzed data from 50 studies including 22,385 individuals; 20 of these studies were randomized, controlled trials of counseling interventions (JAMA. 2019 Feb 12;321(6):588-601).
Overall, the likelihood of perinatal depression was significantly lower among women who received counseling, compared with controls, among more than 3,000 women in those studies (pooled risk ratio 0.61). Absolute risk differences for perinatal depression ranged from a 1% increased reduction in controls to a 32% increased reduction among women who received counseling. The effects were strongest for cognitive behavioral therapy and interpersonal therapy as interventions. No adverse events were reported in the counseling intervention studies.
In three studies of health system interventions, the researchers found a benefit for interventions vs. controls, but the difference was not statistically significant.
Trials of most other alternative interventions including infant sleep advice, birth-experience postpartum debriefing, omega-3 fatty acid supplementation, expressive writing, antidepressants, and yoga did not show statistical significance in benefit for reducing perinatal depression.
Only one of three randomized controlled trials of physical activity found a statistically significant group difference.
A trial of nortriptyline to prevent perinatal depression showed no benefit, compared with placebo. A sertraline study of found “a smaller percentage of participants taking sertraline had a depression recurrence, compared with those taking placebo,” the investigators wrote. In these two studies, women who took nortriptyline showed no adverse effects, and those in a trial involving sertraline reported significantly more dizziness and drowsiness compared with placebo patients.
The evidence review was limited by the small number of quality studies, especially studies of alternative interventions. More research is needed; however, the findings support data from similar reviews and support the potential for counseling to prevent perinatal depression, particularly in women at increased risk for perinatal depression, Dr. O’Connor and her associates said.
The USPSTF is supported by the Agency for Healthcare Research and Quality. Coauthor Dr. Michelle L. Henninger reported receiving grants from Pfizer IGLC (Independent Grants for Learning & Change) outside the submitted work. Coauthor Dr. Bradley N. Gaynes reported receiving personal fees from LivaNova and Johnson & Johnson outside the submitted work. The remaining researchers had no financial conflicts to disclose.
SOURCE: Curry SJ et al. JAMA. 2019;321(6):580-7; O’Connor E et al. JAMA. 2019;321(6):588-601.
according to a B recommendation from the U.S. Preventive Services Task Force.
The Task Force determined that counseling interventions are effective in preventing perinatal depression, defined as a major or minor depressive episode during pregnancy or within the first year after delivery. The condition affects an estimated 12% of new mothers in the United States each year, according to lead author Susan J. Curry, PhD, of the University of Iowa, Iowa City, and her colleagues.
The recommendation, published in JAMA, applies to “pregnant persons and persons who are less than 1 year postpartum who do not have a current diagnosis of depression but are at increased risk of developing depression,” according to the authors (JAMA. 2019 Feb 12;321(6):580-7).
Risk factors for development of perinatal depression include:
- Past history of depression.
- Current depressive symptoms (that do not reach a diagnostic threshold).
- History of physical or sexual abuse.
- Unplanned or unwanted pregnancy.
- Stressful life events.
- Lack of social and financial support.
- Intimate partner violence.
- Pregestational or gestational diabetes.
- Complications during pregnancy.
- Adolescent parenthood.
- Low socioeconomic status.
- Lack of social support.
After reviewing the evidence, the USPSTF found a moderate net benefit for counseling interventions, particularly cognitive behavioral therapy and interpersonal therapy, for preventing perinatal depression in women at risk. Counseling sessions reviewed for this recommendation ranged from 4 to 20 meetings (median, 8 meetings).
The USPSTF found inadequate evidence to assess the harms and benefits of other noncounseling interventions, including pharmacologic therapy.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente, Portland, Ore., and her colleagues analyzed data from 50 studies including 22,385 individuals; 20 of these studies were randomized, controlled trials of counseling interventions (JAMA. 2019 Feb 12;321(6):588-601).
Overall, the likelihood of perinatal depression was significantly lower among women who received counseling, compared with controls, among more than 3,000 women in those studies (pooled risk ratio 0.61). Absolute risk differences for perinatal depression ranged from a 1% increased reduction in controls to a 32% increased reduction among women who received counseling. The effects were strongest for cognitive behavioral therapy and interpersonal therapy as interventions. No adverse events were reported in the counseling intervention studies.
In three studies of health system interventions, the researchers found a benefit for interventions vs. controls, but the difference was not statistically significant.
Trials of most other alternative interventions including infant sleep advice, birth-experience postpartum debriefing, omega-3 fatty acid supplementation, expressive writing, antidepressants, and yoga did not show statistical significance in benefit for reducing perinatal depression.
Only one of three randomized controlled trials of physical activity found a statistically significant group difference.
A trial of nortriptyline to prevent perinatal depression showed no benefit, compared with placebo. A sertraline study of found “a smaller percentage of participants taking sertraline had a depression recurrence, compared with those taking placebo,” the investigators wrote. In these two studies, women who took nortriptyline showed no adverse effects, and those in a trial involving sertraline reported significantly more dizziness and drowsiness compared with placebo patients.
The evidence review was limited by the small number of quality studies, especially studies of alternative interventions. More research is needed; however, the findings support data from similar reviews and support the potential for counseling to prevent perinatal depression, particularly in women at increased risk for perinatal depression, Dr. O’Connor and her associates said.
The USPSTF is supported by the Agency for Healthcare Research and Quality. Coauthor Dr. Michelle L. Henninger reported receiving grants from Pfizer IGLC (Independent Grants for Learning & Change) outside the submitted work. Coauthor Dr. Bradley N. Gaynes reported receiving personal fees from LivaNova and Johnson & Johnson outside the submitted work. The remaining researchers had no financial conflicts to disclose.
SOURCE: Curry SJ et al. JAMA. 2019;321(6):580-7; O’Connor E et al. JAMA. 2019;321(6):588-601.
FROM JAMA
Interactive parenting, life skill intervention improves self-esteem in teen mothers
than did those who received standard care, according to Joanne E. Cox, MD, director of primary care at Boston Children’s Hospital and Harvard Medical School, and her associates.
A total of 140 mothers who were aged less than 19 years when they delivered and whose child was aged less than 12 months were included in the study published in Pediatrics. Of this group, 72 received the intervention, which included a series of five 1-hour, one-on-one, interactive modules adapted from the Nurturing and Ansell-Casey Life Skills curricula, delivered over the infant’s first 15 months, in addition to standard teen-tot clinic care. The remaining 68 mothers received teen-tot care alone.
While overall maternal self-esteem decreased in both the intervention and control groups when measured at 36 months, the intervention group experienced a significantly smaller decrease from baseline (P = .011). Similarly, the intervention group had higher scores regarding preparedness for motherhood (P = .011), acceptance of infant (P = .008), and expected relationship with infant (P = .029).
Of the 52 mothers in the intervention group and 48 mothers in the control group for whom pregnancy data was available at 36 months, 42% in the intervention group had a repeat pregnancy, compared with 67% in the control group (adjusted odds ratio, 0.20; 95% confidence interval, 0.06-0.75; P = .017).
The study findings “highlight the positive impact of pairing medical services with comprehensive social services and parenting education and can inform future policy and services for teen parents. These positive effects also have potential to improve long-term outcomes for teens and their children,” Dr. Cox and her associates concluded.
The study authors reported no conflicts of interest. The study was supported in part by a grant from the Office of Adolescent Pregnancy Programs, the Edgerley Family Endowment, a Leadership Education in Adolescent Health training grant, the Maternal and Child Health Bureau, and the Health Resources and Services Administration.
[email protected]
SOURCE: Cox JE et al. Pediatrics. 2019 Feb 12. doi: 10.1542/peds.2018-2303.
than did those who received standard care, according to Joanne E. Cox, MD, director of primary care at Boston Children’s Hospital and Harvard Medical School, and her associates.
A total of 140 mothers who were aged less than 19 years when they delivered and whose child was aged less than 12 months were included in the study published in Pediatrics. Of this group, 72 received the intervention, which included a series of five 1-hour, one-on-one, interactive modules adapted from the Nurturing and Ansell-Casey Life Skills curricula, delivered over the infant’s first 15 months, in addition to standard teen-tot clinic care. The remaining 68 mothers received teen-tot care alone.
While overall maternal self-esteem decreased in both the intervention and control groups when measured at 36 months, the intervention group experienced a significantly smaller decrease from baseline (P = .011). Similarly, the intervention group had higher scores regarding preparedness for motherhood (P = .011), acceptance of infant (P = .008), and expected relationship with infant (P = .029).
Of the 52 mothers in the intervention group and 48 mothers in the control group for whom pregnancy data was available at 36 months, 42% in the intervention group had a repeat pregnancy, compared with 67% in the control group (adjusted odds ratio, 0.20; 95% confidence interval, 0.06-0.75; P = .017).
The study findings “highlight the positive impact of pairing medical services with comprehensive social services and parenting education and can inform future policy and services for teen parents. These positive effects also have potential to improve long-term outcomes for teens and their children,” Dr. Cox and her associates concluded.
The study authors reported no conflicts of interest. The study was supported in part by a grant from the Office of Adolescent Pregnancy Programs, the Edgerley Family Endowment, a Leadership Education in Adolescent Health training grant, the Maternal and Child Health Bureau, and the Health Resources and Services Administration.
[email protected]
SOURCE: Cox JE et al. Pediatrics. 2019 Feb 12. doi: 10.1542/peds.2018-2303.
than did those who received standard care, according to Joanne E. Cox, MD, director of primary care at Boston Children’s Hospital and Harvard Medical School, and her associates.
A total of 140 mothers who were aged less than 19 years when they delivered and whose child was aged less than 12 months were included in the study published in Pediatrics. Of this group, 72 received the intervention, which included a series of five 1-hour, one-on-one, interactive modules adapted from the Nurturing and Ansell-Casey Life Skills curricula, delivered over the infant’s first 15 months, in addition to standard teen-tot clinic care. The remaining 68 mothers received teen-tot care alone.
While overall maternal self-esteem decreased in both the intervention and control groups when measured at 36 months, the intervention group experienced a significantly smaller decrease from baseline (P = .011). Similarly, the intervention group had higher scores regarding preparedness for motherhood (P = .011), acceptance of infant (P = .008), and expected relationship with infant (P = .029).
Of the 52 mothers in the intervention group and 48 mothers in the control group for whom pregnancy data was available at 36 months, 42% in the intervention group had a repeat pregnancy, compared with 67% in the control group (adjusted odds ratio, 0.20; 95% confidence interval, 0.06-0.75; P = .017).
The study findings “highlight the positive impact of pairing medical services with comprehensive social services and parenting education and can inform future policy and services for teen parents. These positive effects also have potential to improve long-term outcomes for teens and their children,” Dr. Cox and her associates concluded.
The study authors reported no conflicts of interest. The study was supported in part by a grant from the Office of Adolescent Pregnancy Programs, the Edgerley Family Endowment, a Leadership Education in Adolescent Health training grant, the Maternal and Child Health Bureau, and the Health Resources and Services Administration.
[email protected]
SOURCE: Cox JE et al. Pediatrics. 2019 Feb 12. doi: 10.1542/peds.2018-2303.
FROM PEDIATRICS
Woman loses hands and feet after cystectomy
Woman loses hands and feet after cystectomy: $109M award
On November 1, a 45-year-old woman underwent laparoscopic excision of a benign ovarian cyst performed by a minimally invasive gynecologic (MIG) surgeon. After surgery, the patient’s blood pressure (BP) declined. She was given fluids, but her BP remained low. The next day, she became incoherent and her BP could not be stabilized. Twenty-seven hours after surgery, the 5-cm umbilical incision opened while the patient was attempting to stand up from the commode. A large amount of bloody discharge drained.
At 11:00
At 4:30
The patient remained unconscious from the time of the exploratory operation until the end of January. She required additional surgeries to control the bacteria as well as amputation of both hands above the wrists and both feet above the ankles due to gangrene. Because she no longer had an abdominal wall, a skin sac was created to hold her intestines outside of her body. When a fistula developed, a colostomy was performed.
She went to a Maryland hospital for rehab, where she learned to walk with prosthetic feet and to use her prosthetic hands. Currently, she has constant abdominal pain, can walk a short distance, and uses a wheelchair. She requires 24/7 assistance for everyday tasks. She can no longer work and is on disability.
PATIENT’S CLAIM: The patient sued the university health system that employed the MIG surgeon. During the cystectomy, he almost completely transected her small intestine, but did not find the injury during surgery. This allowed bacteria to enter the abdominal cavity, causing sepsis and necrotizing fasciitis. The trauma surgeon referred to the injury as an enterotomy, not a tear.
During the procedure, the surgeon used ADEPT, a solution to prevent the formation of adhesions. The patient’s ObGyn expert concluded that ADEPT created an environment that allowed the necrotizing fasciitis to flourish.
The ICU physicians concluded that the patient was stable enough to be transported for a CT scan, but the surgeon repeatedly delayed the procedure and did not call for a surgical consult until 12 hours later. Had the CT scan or exploratory surgery occurred earlier, the diagnosis would have been discovered, and the bacteria would have been prevented from spreading. She would not have required extensive doses of vasopressors, which increase BP by cutting off blood circulation to the 4 extremities. In this case, use of vasopressors led to gangrene and the subsequent amputations.
Continue to: DEFENDANTS’ DEFENSE...
DEFENDANTS’ DEFENSE: The defendants denied all allegations. The expert witness for the defense opined that the surgeon had only nicked the intestine and that the main injury was a tear that had occurred on its own. The defense also claimed that the surgeon did not call for a CT scan because it would not have shown the source of the patient’s condition.
VERDICT: After 2 trials ended with hung juries, a $109 million Florida verdict was returned against the university health system. Under Florida’s sovereign immunity statute, the patient must seek recovery of all but $100,000 of the award through the Florida legislature in a separate claims bill.
Child has hypoxic brain injury: $7.75M settlement
At 41 weeks’ gestation, a mother presented to the emergency department (ED) for delivery after an unremarkable pregnancy. During the last 90 minutes of labor, fetal heart-rate (FHR) monitoring showed nonreassuring findings. After a vaginal delivery, the infant was found to have a hypoxic brain injury.
PARENT’S CLAIM: Even though nonreassuring FHR monitoring findings occurred, the physicians did not offer cesarean delivery (CD). The pediatrician and ED physician were negligent in failing to provide proper neonatal resuscitation and in recognizing a problem with the infants’ intubation. The delay in delivery and poor resuscitation procedure caused the child’s injury.
DEFENDANTS’ DEFENSE: All allegations were denied. There was no deviation from the standard of care.
VERDICT: A $7.75 million Massachusetts settlement was reached.
Kidney failed after hysterectomy
A 46-year-old woman underwent a hysterectomy performed by her ObGyn. Surgery went well but the patient continued to report symptoms. A year later, she underwent an oophorectomy. Two years later, the patient reported blood in her urine and underwent a computed tomography scan, which revealed an obstructed left ureter that had caused injury to the left kidney. Seven months later, the kidney was removed.
PATIENT’S CLAIM: Her kidney loss was a direct result of the ObGyn’s initial surgical procedure. He had placed several clips near the ureter and did not verify their position or protect the ureter. He also failed to address her reported symptoms in a timely manner.
PHYSICIAN’S DEFENSE: The damage to the ureter is a known risk of hysterectomy and oophorectomy. The obstruction developed over time, not as an immediate result of the surgery.
VERDICT: A Kentucky defense verdict was returned.
History of shoulder dystocia, Erb's palsy: $1.2M settlement
An obese mother was admitted to the hospital at 39 weeks’ gestation with signs of labor. She requested a CD and was advised that she had progressed too far for that to be an option, and that vaginal delivery would be safe. During the second stage of labor, shoulder dystocia was encountered. The ObGyn made several attempts to deliver using downward traction, but was unsuccessful. A second ObGyn swept the shoulder with an internal maneuver of his hand and delivered the baby. The child has a severe brachial plexus injury at multiple spinal levels resulting in Erb’s palsy.
PARENT’S CLAIM: A CD should have been performed. The first ObGyn failed to provide a CD and repeatedly applied excessive downward traction, causing the infant’s injury.
Continue to: PHYSICIAN’S DEFENSE...
PHYSICIAN’S DEFENSE: Shoulder dystocia is unpredictable and an unpreventable obstetric emergency. The ObGyn used proper maneuvers to release the shoulder dystocia.
VERDICT: A $1.2 million Virginia settlement was reached.
Ureter injured during hysterectomy
When a patient was found to have multiple, symptomatic fibroids and an enlarged uterus, her gynecologist suggested a total laparoscopic hysterectomy. During the procedure, when he inspected the pelvis and found multiple fibroids in and around the uterus, the gynecologist converted to a supracervical hysterectomy. Surgery was difficult because of a large myoma on the right broad ligament.
The patient tolerated surgery well and was released home the next day. At follow-up one week later, she had no signs or symptoms of ureter injury. Later that same evening, she experienced sharp flank pain and nausea. When she called the gynecologist, he sent her to the emergency department. A computed tomography scan showed extravasation of the right ureter. She underwent months of stent placements and replacements, nephrostomies, and ultimately ureteral reimplantation surgery.
PATIENT’S CLAIM: The gynecologist caused a thermal injury to her right ureter during the hysterectomy by misusing an electrocautery device. There was a delay in timely diagnosis postsurgery.
PHYSICIAN’S DEFENSE: The gynecologist contended that he employed proper surgical technique, and that he reacted properly when the patient reported the pain.
VERDICT: A Virginia defense verdict was returned.
Woman loses hands and feet after cystectomy: $109M award
On November 1, a 45-year-old woman underwent laparoscopic excision of a benign ovarian cyst performed by a minimally invasive gynecologic (MIG) surgeon. After surgery, the patient’s blood pressure (BP) declined. She was given fluids, but her BP remained low. The next day, she became incoherent and her BP could not be stabilized. Twenty-seven hours after surgery, the 5-cm umbilical incision opened while the patient was attempting to stand up from the commode. A large amount of bloody discharge drained.
At 11:00
At 4:30
The patient remained unconscious from the time of the exploratory operation until the end of January. She required additional surgeries to control the bacteria as well as amputation of both hands above the wrists and both feet above the ankles due to gangrene. Because she no longer had an abdominal wall, a skin sac was created to hold her intestines outside of her body. When a fistula developed, a colostomy was performed.
She went to a Maryland hospital for rehab, where she learned to walk with prosthetic feet and to use her prosthetic hands. Currently, she has constant abdominal pain, can walk a short distance, and uses a wheelchair. She requires 24/7 assistance for everyday tasks. She can no longer work and is on disability.
PATIENT’S CLAIM: The patient sued the university health system that employed the MIG surgeon. During the cystectomy, he almost completely transected her small intestine, but did not find the injury during surgery. This allowed bacteria to enter the abdominal cavity, causing sepsis and necrotizing fasciitis. The trauma surgeon referred to the injury as an enterotomy, not a tear.
During the procedure, the surgeon used ADEPT, a solution to prevent the formation of adhesions. The patient’s ObGyn expert concluded that ADEPT created an environment that allowed the necrotizing fasciitis to flourish.
The ICU physicians concluded that the patient was stable enough to be transported for a CT scan, but the surgeon repeatedly delayed the procedure and did not call for a surgical consult until 12 hours later. Had the CT scan or exploratory surgery occurred earlier, the diagnosis would have been discovered, and the bacteria would have been prevented from spreading. She would not have required extensive doses of vasopressors, which increase BP by cutting off blood circulation to the 4 extremities. In this case, use of vasopressors led to gangrene and the subsequent amputations.
Continue to: DEFENDANTS’ DEFENSE...
DEFENDANTS’ DEFENSE: The defendants denied all allegations. The expert witness for the defense opined that the surgeon had only nicked the intestine and that the main injury was a tear that had occurred on its own. The defense also claimed that the surgeon did not call for a CT scan because it would not have shown the source of the patient’s condition.
VERDICT: After 2 trials ended with hung juries, a $109 million Florida verdict was returned against the university health system. Under Florida’s sovereign immunity statute, the patient must seek recovery of all but $100,000 of the award through the Florida legislature in a separate claims bill.
Child has hypoxic brain injury: $7.75M settlement
At 41 weeks’ gestation, a mother presented to the emergency department (ED) for delivery after an unremarkable pregnancy. During the last 90 minutes of labor, fetal heart-rate (FHR) monitoring showed nonreassuring findings. After a vaginal delivery, the infant was found to have a hypoxic brain injury.
PARENT’S CLAIM: Even though nonreassuring FHR monitoring findings occurred, the physicians did not offer cesarean delivery (CD). The pediatrician and ED physician were negligent in failing to provide proper neonatal resuscitation and in recognizing a problem with the infants’ intubation. The delay in delivery and poor resuscitation procedure caused the child’s injury.
DEFENDANTS’ DEFENSE: All allegations were denied. There was no deviation from the standard of care.
VERDICT: A $7.75 million Massachusetts settlement was reached.
Kidney failed after hysterectomy
A 46-year-old woman underwent a hysterectomy performed by her ObGyn. Surgery went well but the patient continued to report symptoms. A year later, she underwent an oophorectomy. Two years later, the patient reported blood in her urine and underwent a computed tomography scan, which revealed an obstructed left ureter that had caused injury to the left kidney. Seven months later, the kidney was removed.
PATIENT’S CLAIM: Her kidney loss was a direct result of the ObGyn’s initial surgical procedure. He had placed several clips near the ureter and did not verify their position or protect the ureter. He also failed to address her reported symptoms in a timely manner.
PHYSICIAN’S DEFENSE: The damage to the ureter is a known risk of hysterectomy and oophorectomy. The obstruction developed over time, not as an immediate result of the surgery.
VERDICT: A Kentucky defense verdict was returned.
History of shoulder dystocia, Erb's palsy: $1.2M settlement
An obese mother was admitted to the hospital at 39 weeks’ gestation with signs of labor. She requested a CD and was advised that she had progressed too far for that to be an option, and that vaginal delivery would be safe. During the second stage of labor, shoulder dystocia was encountered. The ObGyn made several attempts to deliver using downward traction, but was unsuccessful. A second ObGyn swept the shoulder with an internal maneuver of his hand and delivered the baby. The child has a severe brachial plexus injury at multiple spinal levels resulting in Erb’s palsy.
PARENT’S CLAIM: A CD should have been performed. The first ObGyn failed to provide a CD and repeatedly applied excessive downward traction, causing the infant’s injury.
Continue to: PHYSICIAN’S DEFENSE...
PHYSICIAN’S DEFENSE: Shoulder dystocia is unpredictable and an unpreventable obstetric emergency. The ObGyn used proper maneuvers to release the shoulder dystocia.
VERDICT: A $1.2 million Virginia settlement was reached.
Ureter injured during hysterectomy
When a patient was found to have multiple, symptomatic fibroids and an enlarged uterus, her gynecologist suggested a total laparoscopic hysterectomy. During the procedure, when he inspected the pelvis and found multiple fibroids in and around the uterus, the gynecologist converted to a supracervical hysterectomy. Surgery was difficult because of a large myoma on the right broad ligament.
The patient tolerated surgery well and was released home the next day. At follow-up one week later, she had no signs or symptoms of ureter injury. Later that same evening, she experienced sharp flank pain and nausea. When she called the gynecologist, he sent her to the emergency department. A computed tomography scan showed extravasation of the right ureter. She underwent months of stent placements and replacements, nephrostomies, and ultimately ureteral reimplantation surgery.
PATIENT’S CLAIM: The gynecologist caused a thermal injury to her right ureter during the hysterectomy by misusing an electrocautery device. There was a delay in timely diagnosis postsurgery.
PHYSICIAN’S DEFENSE: The gynecologist contended that he employed proper surgical technique, and that he reacted properly when the patient reported the pain.
VERDICT: A Virginia defense verdict was returned.
Woman loses hands and feet after cystectomy: $109M award
On November 1, a 45-year-old woman underwent laparoscopic excision of a benign ovarian cyst performed by a minimally invasive gynecologic (MIG) surgeon. After surgery, the patient’s blood pressure (BP) declined. She was given fluids, but her BP remained low. The next day, she became incoherent and her BP could not be stabilized. Twenty-seven hours after surgery, the 5-cm umbilical incision opened while the patient was attempting to stand up from the commode. A large amount of bloody discharge drained.
At 11:00
At 4:30
The patient remained unconscious from the time of the exploratory operation until the end of January. She required additional surgeries to control the bacteria as well as amputation of both hands above the wrists and both feet above the ankles due to gangrene. Because she no longer had an abdominal wall, a skin sac was created to hold her intestines outside of her body. When a fistula developed, a colostomy was performed.
She went to a Maryland hospital for rehab, where she learned to walk with prosthetic feet and to use her prosthetic hands. Currently, she has constant abdominal pain, can walk a short distance, and uses a wheelchair. She requires 24/7 assistance for everyday tasks. She can no longer work and is on disability.
PATIENT’S CLAIM: The patient sued the university health system that employed the MIG surgeon. During the cystectomy, he almost completely transected her small intestine, but did not find the injury during surgery. This allowed bacteria to enter the abdominal cavity, causing sepsis and necrotizing fasciitis. The trauma surgeon referred to the injury as an enterotomy, not a tear.
During the procedure, the surgeon used ADEPT, a solution to prevent the formation of adhesions. The patient’s ObGyn expert concluded that ADEPT created an environment that allowed the necrotizing fasciitis to flourish.
The ICU physicians concluded that the patient was stable enough to be transported for a CT scan, but the surgeon repeatedly delayed the procedure and did not call for a surgical consult until 12 hours later. Had the CT scan or exploratory surgery occurred earlier, the diagnosis would have been discovered, and the bacteria would have been prevented from spreading. She would not have required extensive doses of vasopressors, which increase BP by cutting off blood circulation to the 4 extremities. In this case, use of vasopressors led to gangrene and the subsequent amputations.
Continue to: DEFENDANTS’ DEFENSE...
DEFENDANTS’ DEFENSE: The defendants denied all allegations. The expert witness for the defense opined that the surgeon had only nicked the intestine and that the main injury was a tear that had occurred on its own. The defense also claimed that the surgeon did not call for a CT scan because it would not have shown the source of the patient’s condition.
VERDICT: After 2 trials ended with hung juries, a $109 million Florida verdict was returned against the university health system. Under Florida’s sovereign immunity statute, the patient must seek recovery of all but $100,000 of the award through the Florida legislature in a separate claims bill.
Child has hypoxic brain injury: $7.75M settlement
At 41 weeks’ gestation, a mother presented to the emergency department (ED) for delivery after an unremarkable pregnancy. During the last 90 minutes of labor, fetal heart-rate (FHR) monitoring showed nonreassuring findings. After a vaginal delivery, the infant was found to have a hypoxic brain injury.
PARENT’S CLAIM: Even though nonreassuring FHR monitoring findings occurred, the physicians did not offer cesarean delivery (CD). The pediatrician and ED physician were negligent in failing to provide proper neonatal resuscitation and in recognizing a problem with the infants’ intubation. The delay in delivery and poor resuscitation procedure caused the child’s injury.
DEFENDANTS’ DEFENSE: All allegations were denied. There was no deviation from the standard of care.
VERDICT: A $7.75 million Massachusetts settlement was reached.
Kidney failed after hysterectomy
A 46-year-old woman underwent a hysterectomy performed by her ObGyn. Surgery went well but the patient continued to report symptoms. A year later, she underwent an oophorectomy. Two years later, the patient reported blood in her urine and underwent a computed tomography scan, which revealed an obstructed left ureter that had caused injury to the left kidney. Seven months later, the kidney was removed.
PATIENT’S CLAIM: Her kidney loss was a direct result of the ObGyn’s initial surgical procedure. He had placed several clips near the ureter and did not verify their position or protect the ureter. He also failed to address her reported symptoms in a timely manner.
PHYSICIAN’S DEFENSE: The damage to the ureter is a known risk of hysterectomy and oophorectomy. The obstruction developed over time, not as an immediate result of the surgery.
VERDICT: A Kentucky defense verdict was returned.
History of shoulder dystocia, Erb's palsy: $1.2M settlement
An obese mother was admitted to the hospital at 39 weeks’ gestation with signs of labor. She requested a CD and was advised that she had progressed too far for that to be an option, and that vaginal delivery would be safe. During the second stage of labor, shoulder dystocia was encountered. The ObGyn made several attempts to deliver using downward traction, but was unsuccessful. A second ObGyn swept the shoulder with an internal maneuver of his hand and delivered the baby. The child has a severe brachial plexus injury at multiple spinal levels resulting in Erb’s palsy.
PARENT’S CLAIM: A CD should have been performed. The first ObGyn failed to provide a CD and repeatedly applied excessive downward traction, causing the infant’s injury.
Continue to: PHYSICIAN’S DEFENSE...
PHYSICIAN’S DEFENSE: Shoulder dystocia is unpredictable and an unpreventable obstetric emergency. The ObGyn used proper maneuvers to release the shoulder dystocia.
VERDICT: A $1.2 million Virginia settlement was reached.
Ureter injured during hysterectomy
When a patient was found to have multiple, symptomatic fibroids and an enlarged uterus, her gynecologist suggested a total laparoscopic hysterectomy. During the procedure, when he inspected the pelvis and found multiple fibroids in and around the uterus, the gynecologist converted to a supracervical hysterectomy. Surgery was difficult because of a large myoma on the right broad ligament.
The patient tolerated surgery well and was released home the next day. At follow-up one week later, she had no signs or symptoms of ureter injury. Later that same evening, she experienced sharp flank pain and nausea. When she called the gynecologist, he sent her to the emergency department. A computed tomography scan showed extravasation of the right ureter. She underwent months of stent placements and replacements, nephrostomies, and ultimately ureteral reimplantation surgery.
PATIENT’S CLAIM: The gynecologist caused a thermal injury to her right ureter during the hysterectomy by misusing an electrocautery device. There was a delay in timely diagnosis postsurgery.
PHYSICIAN’S DEFENSE: The gynecologist contended that he employed proper surgical technique, and that he reacted properly when the patient reported the pain.
VERDICT: A Virginia defense verdict was returned.
Most pregnant women want guidance on prenatal whole-genome sequencing
according to results from a survey published in Obstetrics & Gynecology.
Nearly half said they would want clear guidance from clinicians before undergoing the noninvasive procedure.
“Prenatal whole-genome sequencing offers significantly more fetal information than women can currently receive, and it is not surprising that, when faced with a tremendous range of information, many women want recommendations from their clinicians,” Haley K. Sullivan from the National Institutes of Health Clinical Center and National Human Genome Research Institute and colleagues wrote. “Our data suggest that most women prefer a directive interaction with their clinician when deciding what types of genetic information to receive from prenatal whole-genome sequencing.”
Research coordinators from the Inova Translational Medicine Institute offered 805 pregnant women a survey on their preferences for prenatal whole-genome sequencing between June and August 2017; of these, 553 women answered (69% response rate). The women responded to questions about what type of information they would like to receive if they were to undergo prenatal whole-genome sequencing and what role a clinician would preferably play in the decision-making process. The researchers divided the survey into sections based on actionability, severity, prevalence, and age of onset.
According to the survey results, 90% of respondents wanted information on serious treatable childhood-onset diseases from prenatal whole-genome sequencing results, while 40% said they did not want to receive results based on nonmedical traits such as eye color, height, or athletic ability.
With regard to clinician role, 45% of women said they wanted all options presented with clear recommendations from a clinician on which tests to order, 26% wanted all options presented but with a joint decision-making process, 13% wanted all options presented but independent decision making, and 11% wanted the clear recommendation from clinicians alone.
The respondents said the most common reason for wanting to undergo prenatal whole-genome sequencing was to prepare “financially, medically, or psychologically” for a child with special needs, the researchers said.
“This represents a departure from the current state of genetic counseling, where nondirectiveness is a central tenet, and is contrary to the 45% of ob.gyns. who said in a previous survey that they should not be at all directive when counseling patients on prenatal whole-genome sequencing,” the authors wrote. “Given this clear patient desire for guidance, there is a vital opportunity for the American College of Obstetricians and Gynecologists to provide leadership and recommendations as prenatal whole-genome sequencing is adopted into clinical practice.”
Limitations in the study include asking the respondents to make hypothetical decisions, using examples to describe genetic conditions that might have skewed decision making; asking women to pick only one reason for wanting the sequencing information from a list of predetermined options, when many reasons may be important to them; social desirability bias in the responses, if women are reluctant to pick a choice they perceive as less socially acceptable; and a potential systematic difference between women who were and were not enrolled as survey participants. The respondents also were from the Northern Virginia area, which may not be generalizable to a national population of patients, the researchers said.
This study was supported by the Intramural Research Program of the National Human Genome Research Institute and the Clinical Center Department of Bioethics, National Institutes of Health. The authors reported no relevant conflicts of interest.
SOURCE: Sullivan HK et al. Obstet Gynecol. 2019 Mar. doi: 10.1097/AOG.0000000000003121.
according to results from a survey published in Obstetrics & Gynecology.
Nearly half said they would want clear guidance from clinicians before undergoing the noninvasive procedure.
“Prenatal whole-genome sequencing offers significantly more fetal information than women can currently receive, and it is not surprising that, when faced with a tremendous range of information, many women want recommendations from their clinicians,” Haley K. Sullivan from the National Institutes of Health Clinical Center and National Human Genome Research Institute and colleagues wrote. “Our data suggest that most women prefer a directive interaction with their clinician when deciding what types of genetic information to receive from prenatal whole-genome sequencing.”
Research coordinators from the Inova Translational Medicine Institute offered 805 pregnant women a survey on their preferences for prenatal whole-genome sequencing between June and August 2017; of these, 553 women answered (69% response rate). The women responded to questions about what type of information they would like to receive if they were to undergo prenatal whole-genome sequencing and what role a clinician would preferably play in the decision-making process. The researchers divided the survey into sections based on actionability, severity, prevalence, and age of onset.
According to the survey results, 90% of respondents wanted information on serious treatable childhood-onset diseases from prenatal whole-genome sequencing results, while 40% said they did not want to receive results based on nonmedical traits such as eye color, height, or athletic ability.
With regard to clinician role, 45% of women said they wanted all options presented with clear recommendations from a clinician on which tests to order, 26% wanted all options presented but with a joint decision-making process, 13% wanted all options presented but independent decision making, and 11% wanted the clear recommendation from clinicians alone.
The respondents said the most common reason for wanting to undergo prenatal whole-genome sequencing was to prepare “financially, medically, or psychologically” for a child with special needs, the researchers said.
“This represents a departure from the current state of genetic counseling, where nondirectiveness is a central tenet, and is contrary to the 45% of ob.gyns. who said in a previous survey that they should not be at all directive when counseling patients on prenatal whole-genome sequencing,” the authors wrote. “Given this clear patient desire for guidance, there is a vital opportunity for the American College of Obstetricians and Gynecologists to provide leadership and recommendations as prenatal whole-genome sequencing is adopted into clinical practice.”
Limitations in the study include asking the respondents to make hypothetical decisions, using examples to describe genetic conditions that might have skewed decision making; asking women to pick only one reason for wanting the sequencing information from a list of predetermined options, when many reasons may be important to them; social desirability bias in the responses, if women are reluctant to pick a choice they perceive as less socially acceptable; and a potential systematic difference between women who were and were not enrolled as survey participants. The respondents also were from the Northern Virginia area, which may not be generalizable to a national population of patients, the researchers said.
This study was supported by the Intramural Research Program of the National Human Genome Research Institute and the Clinical Center Department of Bioethics, National Institutes of Health. The authors reported no relevant conflicts of interest.
SOURCE: Sullivan HK et al. Obstet Gynecol. 2019 Mar. doi: 10.1097/AOG.0000000000003121.
according to results from a survey published in Obstetrics & Gynecology.
Nearly half said they would want clear guidance from clinicians before undergoing the noninvasive procedure.
“Prenatal whole-genome sequencing offers significantly more fetal information than women can currently receive, and it is not surprising that, when faced with a tremendous range of information, many women want recommendations from their clinicians,” Haley K. Sullivan from the National Institutes of Health Clinical Center and National Human Genome Research Institute and colleagues wrote. “Our data suggest that most women prefer a directive interaction with their clinician when deciding what types of genetic information to receive from prenatal whole-genome sequencing.”
Research coordinators from the Inova Translational Medicine Institute offered 805 pregnant women a survey on their preferences for prenatal whole-genome sequencing between June and August 2017; of these, 553 women answered (69% response rate). The women responded to questions about what type of information they would like to receive if they were to undergo prenatal whole-genome sequencing and what role a clinician would preferably play in the decision-making process. The researchers divided the survey into sections based on actionability, severity, prevalence, and age of onset.
According to the survey results, 90% of respondents wanted information on serious treatable childhood-onset diseases from prenatal whole-genome sequencing results, while 40% said they did not want to receive results based on nonmedical traits such as eye color, height, or athletic ability.
With regard to clinician role, 45% of women said they wanted all options presented with clear recommendations from a clinician on which tests to order, 26% wanted all options presented but with a joint decision-making process, 13% wanted all options presented but independent decision making, and 11% wanted the clear recommendation from clinicians alone.
The respondents said the most common reason for wanting to undergo prenatal whole-genome sequencing was to prepare “financially, medically, or psychologically” for a child with special needs, the researchers said.
“This represents a departure from the current state of genetic counseling, where nondirectiveness is a central tenet, and is contrary to the 45% of ob.gyns. who said in a previous survey that they should not be at all directive when counseling patients on prenatal whole-genome sequencing,” the authors wrote. “Given this clear patient desire for guidance, there is a vital opportunity for the American College of Obstetricians and Gynecologists to provide leadership and recommendations as prenatal whole-genome sequencing is adopted into clinical practice.”
Limitations in the study include asking the respondents to make hypothetical decisions, using examples to describe genetic conditions that might have skewed decision making; asking women to pick only one reason for wanting the sequencing information from a list of predetermined options, when many reasons may be important to them; social desirability bias in the responses, if women are reluctant to pick a choice they perceive as less socially acceptable; and a potential systematic difference between women who were and were not enrolled as survey participants. The respondents also were from the Northern Virginia area, which may not be generalizable to a national population of patients, the researchers said.
This study was supported by the Intramural Research Program of the National Human Genome Research Institute and the Clinical Center Department of Bioethics, National Institutes of Health. The authors reported no relevant conflicts of interest.
SOURCE: Sullivan HK et al. Obstet Gynecol. 2019 Mar. doi: 10.1097/AOG.0000000000003121.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: A majority of pregnant women surveyed said they wanted information on childhood-onset genetic diseases, with almost half wanting clear clinical recommendations before deciding to undergo noninvasive prenatal whole-genome sequencing.
Major finding: Of the respondents, 90% said they wanted information on serious treatable childhood-onset conditions.
Study details: A survey of 553 pregnant women coordinated by the Inova Translational Medicine Institute.
Disclosures: This study was supported by the Intramural Research Program of the National Human Genome Research Institute and the Clinical Center Department of Bioethics, National Institutes of Health. The authors reported no relevant conflicts of interest.
Source: Sullivan HK et al. Obstet Gynecol. 2019 Mar. doi: 10.1097/AOG.0000000000003121.
Obstetric hospitalists can screen for postpartum depression
Postpartum depression (PPD) is the most common complication of pregnancy, and onset can occur at any time from pregnancy until up to 1 year post partum.1,2 The immediate postpartum period is a time during which care is shared among multiple providers for both mother and child, and the transition from inpatient to outpatient postpartum care can impede communication between those caring for the patient in each setting. In 2018, the American College of Obstetricians and Gynecologists published a committee opinion emphasizing the importance of the “fourth trimester” and calling for health care providers to assist women in navigating the transition from pre- to postpartum care.3 An important consideration of perinatal care is mental health care for the mother, including screening and care for postpartum depression; however, the optimal role for the obstetric hospitalist in providing such services has been unclear.
Estimates of the prevalence of PPD in new mothers in the United States varied by state from 8% to 20% in 2012, with an overall average of 12%.2 Left untreated, PPD may result in significant negative outcomes for women, their children, and families. The depressive symptoms of PPD may persist for months or years afterward,4 with one study finding elevated depressive symptoms in women up to 11 years post partum.5 Suicide is also a leading cause of pregnancy-related mortality associated with depressive symptoms.6-9 In addition, maternal postpartum depression symptoms have been associated with impaired mother-infant bonding at 6 months of age10 and decreased cognitive and fine motor development of children at 18 months.11
Importance of screening
Evidence from the literature shows that, without proper screening, approximately 50% of cases of PPD go undiagnosed, and that increasing the number of women being screened by perinatal providers is an important first step to improving outcomes.12-18 Current recommendations for the timing and frequency of screening for PPD vary among the published guidelines. ACOG recommends screening at least once during the perinatal period for depression and anxiety using a standardized, validated tool; an update of the ACOG committee opinion in 2018 also states: “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.”19 The American Medical Association adopted new policies in 2017 promoting the implementation of a routine protocol for depression screening of perinatal women.20 The American Academy of Pediatrics recommends more frequent screening, with assessments at the 1-, 2-, 4-, and 6-month visits.21 Finally, the U.S. Preventive Services Task Force recommends screening for depression in the general population including pregnant and postpartum women.22
Multiple standardized, validated screening instruments are available for detecting possible symptoms of PPD, including the most widely used tools: the Edinburgh Postnatal Depression Scale (EPDS)19,23 and the Patient Health Questionnaire (PHQ-9).24 Two recent studies have shown that screening women for symptoms of PPD with a validated tool may reduce the duration or severity of depressive symptoms,25,26 further reinforcing the need to ensure that women experiencing symptoms of PPD are identified and treated early.
The inpatient hospitalization for labor, delivery, and birth of a child has not traditionally been viewed as an opportunity for PPD screening. While private practitioners and obstetric medical group practices typically have inquired about and documented the individual patient’s mental health history and risk factors for PPD, the obstetric hospitalist is most commonly meeting a patient in labor or in a postpartum encounter for the first time. As obstetric practices grow ever more consolidated, and as obstetric hospitalist care is implemented for a variety of reasons including, but not limited to, preventing burnout among private practitioners, serving as a safety net for all inpatient obstetric services, and increasing standardization in obstetric triage and obstetric emergency departments,
Barriers remain
Despite the need for early detection of PPD, screening practices remain inconsistent. A literature review of health care provider practices showed only one in four physicians reported using screening tools; obstetrician-gynecologists were most likely (36%) to use screening tools, followed by family practitioners (31%), with pediatricians the least likely (7%).27 This low rate is at least partially the result of perceived barriers to screening among health care providers, which contributes to underdiagnosis. A survey of more than 200 physicians who were members of ACOG showed that the top three barriers restricting screening practices were time constraints, inadequate training, and a lack of knowledge of the diagnostic criteria.28
Since 2017, Dignity Health has instituted routine screening of all inpatient postpartum patients at its 29 birth centers in Arizona, California, and Nevada. In this program, of which I am a physician participant, more than 30,000 women have been screened with the EPDS. In addition to providing screening, Dignity Health staff (physicians, certified nurse midwives, nurse practitioners, registered nurses, social workers, mental health therapists, lactation consultants, health educators, and others) have received in-person Perinatal Mental Health training. In this way, the entire care team coordinates inpatient screening and referral to outpatient care providers – thus bridging the gap in postpartum mental health care. For those patients who screen positive while an inpatient, a psychiatric telemedicine appointment is provided and, if necessary, short-course medications can be prescribed until the patient has outpatient follow-up and continuity of care. While we as obstetric hospitalists and community obstetrician-gynecologists recognize that inpatient postpartum screening may be limited in its sensitivity for capturing all women who will go on to develop PPD, there is definitely a benefit to having a discussion about PPD and maternal mental health early and often throughout the postpartum period. For many women suffering in silence, a 6-week postpartum outpatient visit is too late, especially given that approximately one-third of women are lost to postpartum follow-up.29,30
Addressing barriers
A growing number of states have enacted policies to address the challenge of peripartum behavioral health needs, and several states – Illinois, Massachusetts, New Jersey, and West Virginia – now mandate routine PPD screening by health care providers.31 However, few of these laws or policies contain specific guidance, such as the optimal timing for screening, instead leaving the details to providers.32 The proper identification and management of PPD cannot be achieved by state-level policy mandates alone, but must include clinician buy-in and participation.
Obstetricians play an essential role in the identification and treatment of PPD. Among nonpsychiatric specialists, obstetrician-gynecologists are the most likely providers to see and screen during the perinatal period.33 In addition, women prefer to receive help for PPD from either their obstetric practitioners or a mental-health specialists located at the obstetric clinic, and are more likely to receive mental-health services if they are provided at the same location as that of the obstetric provider.34,35 According to ACOG’s new guidance on the fourth trimester, obstetricians are encouraged to take responsibility for women’s care immediately after birth, and this care would include contact with all mothers within the first 3 weeks post partum, at follow-up visits as needed, and for a comprehensive postpartum visit at 12 weeks.3
Our specialty has and will continue to evolve, and obstetric hospitalists will play an ever more essential role in the care of women during their inpatient obstetric admission. Whether we are a patient’s primary inpatient obstetric provider or a practice extender for single or multigroup practice, we are in a unique role to screen, begin treatment for, and offer anticipatory guidance for maternal mental health and postpartum depression disorders. Obstetric hospitalists can be a bridge between inpatient and outpatient follow-up and catalysts for implementing universal inpatient PPD screening. Our role presents an opportunity to start the discussion early and often in the fourth trimester and to make a significant difference in addressing this critical unmet need in postnatal care.
Dr. van Dis is the medical director of the Ob Hospitalist Group in Burbank, Calif. She disclosed she received editorial assistance from Erik MacLaren, PhD, of Boston Strategic Partners Inc., with funding support from Sage Therapeutics Inc. E-mail [email protected].
References
1. Centers for Disease Control and Prevention. Postpartum Depression. 2017.
2. Morb Mortal Wkly Rep. 2017;66(6):153-8.
3. Obstet Gynecol. 2018;131(5):e140-e150.
4. Harv Rev Psychiatry. 2014;22(1):1-22.
5. JAMA Psychiatry. 2018;75(3):247-53.
6. J Womens Health (Larchmt). 2016;25(12):1219-24.
7. J Psychiatr Res. 2017;84:284-91.
8. Br J Psychiatry. 2003;183:279-81.
9. Obstet Gynecol Surv. 2005;60(3):183-90.
10. Arch Womens Ment Health. 2016;19(1):87-94.
11. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335-45.
12. J Reprod Med. 1999;44(4):351-8.
13. J Behav Health Serv Res. 2004;31(2):117-33.
14. J Clin Psychiatry. 2016;77(9):1189-200.
15. Am J Obstet Gynecol. 2000;182(5):1080-2.
16. J Fam Pract. 2001;50(2):117-22.
17. Obstet Gynecol. 1999;93(5 Pt 1):653-7.
18. J Womens Health (Larchmt). 2010;19(3):477-90.
19. Obstet Gynecol. 2018;132:e208-12.
20. “Physicians back programs to address maternal mortality, depression,” AMA, Nov. 15, 2017
21. Pediatrics. 2019 Jan 1;143(1):e20183260.
22. JAMA. 2016;315(4):380-7.
23. Br J Psychiatry. 1987;150:782-6.
24. Ann Fam Med. 2009;7(1):63-70.
25. Obstet Gynecol. 2016;127(5):917-25.
26. Pediatrics. 2017 Oct;140(4). pii: e20170110.
27. Womens Health Issues. 2015;25(6):703-10.
28. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
29. Matern Child Health J. 2016;20(Suppl 1):22-7.
30. National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC). 2018.
31. Psychiatr Serv. 2015;66(3):324-8.
32. Postpartum Support International. Legislation. 2018.
33. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, eds. Guidelines for Perinatal Care. 7th ed. (Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; Oct 2012.)
34. Birth. 2009;36(1):60-9.
35. Gen Hosp Psychiatry. 2009;31(2):155-62.
Postpartum depression (PPD) is the most common complication of pregnancy, and onset can occur at any time from pregnancy until up to 1 year post partum.1,2 The immediate postpartum period is a time during which care is shared among multiple providers for both mother and child, and the transition from inpatient to outpatient postpartum care can impede communication between those caring for the patient in each setting. In 2018, the American College of Obstetricians and Gynecologists published a committee opinion emphasizing the importance of the “fourth trimester” and calling for health care providers to assist women in navigating the transition from pre- to postpartum care.3 An important consideration of perinatal care is mental health care for the mother, including screening and care for postpartum depression; however, the optimal role for the obstetric hospitalist in providing such services has been unclear.
Estimates of the prevalence of PPD in new mothers in the United States varied by state from 8% to 20% in 2012, with an overall average of 12%.2 Left untreated, PPD may result in significant negative outcomes for women, their children, and families. The depressive symptoms of PPD may persist for months or years afterward,4 with one study finding elevated depressive symptoms in women up to 11 years post partum.5 Suicide is also a leading cause of pregnancy-related mortality associated with depressive symptoms.6-9 In addition, maternal postpartum depression symptoms have been associated with impaired mother-infant bonding at 6 months of age10 and decreased cognitive and fine motor development of children at 18 months.11
Importance of screening
Evidence from the literature shows that, without proper screening, approximately 50% of cases of PPD go undiagnosed, and that increasing the number of women being screened by perinatal providers is an important first step to improving outcomes.12-18 Current recommendations for the timing and frequency of screening for PPD vary among the published guidelines. ACOG recommends screening at least once during the perinatal period for depression and anxiety using a standardized, validated tool; an update of the ACOG committee opinion in 2018 also states: “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.”19 The American Medical Association adopted new policies in 2017 promoting the implementation of a routine protocol for depression screening of perinatal women.20 The American Academy of Pediatrics recommends more frequent screening, with assessments at the 1-, 2-, 4-, and 6-month visits.21 Finally, the U.S. Preventive Services Task Force recommends screening for depression in the general population including pregnant and postpartum women.22
Multiple standardized, validated screening instruments are available for detecting possible symptoms of PPD, including the most widely used tools: the Edinburgh Postnatal Depression Scale (EPDS)19,23 and the Patient Health Questionnaire (PHQ-9).24 Two recent studies have shown that screening women for symptoms of PPD with a validated tool may reduce the duration or severity of depressive symptoms,25,26 further reinforcing the need to ensure that women experiencing symptoms of PPD are identified and treated early.
The inpatient hospitalization for labor, delivery, and birth of a child has not traditionally been viewed as an opportunity for PPD screening. While private practitioners and obstetric medical group practices typically have inquired about and documented the individual patient’s mental health history and risk factors for PPD, the obstetric hospitalist is most commonly meeting a patient in labor or in a postpartum encounter for the first time. As obstetric practices grow ever more consolidated, and as obstetric hospitalist care is implemented for a variety of reasons including, but not limited to, preventing burnout among private practitioners, serving as a safety net for all inpatient obstetric services, and increasing standardization in obstetric triage and obstetric emergency departments,
Barriers remain
Despite the need for early detection of PPD, screening practices remain inconsistent. A literature review of health care provider practices showed only one in four physicians reported using screening tools; obstetrician-gynecologists were most likely (36%) to use screening tools, followed by family practitioners (31%), with pediatricians the least likely (7%).27 This low rate is at least partially the result of perceived barriers to screening among health care providers, which contributes to underdiagnosis. A survey of more than 200 physicians who were members of ACOG showed that the top three barriers restricting screening practices were time constraints, inadequate training, and a lack of knowledge of the diagnostic criteria.28
Since 2017, Dignity Health has instituted routine screening of all inpatient postpartum patients at its 29 birth centers in Arizona, California, and Nevada. In this program, of which I am a physician participant, more than 30,000 women have been screened with the EPDS. In addition to providing screening, Dignity Health staff (physicians, certified nurse midwives, nurse practitioners, registered nurses, social workers, mental health therapists, lactation consultants, health educators, and others) have received in-person Perinatal Mental Health training. In this way, the entire care team coordinates inpatient screening and referral to outpatient care providers – thus bridging the gap in postpartum mental health care. For those patients who screen positive while an inpatient, a psychiatric telemedicine appointment is provided and, if necessary, short-course medications can be prescribed until the patient has outpatient follow-up and continuity of care. While we as obstetric hospitalists and community obstetrician-gynecologists recognize that inpatient postpartum screening may be limited in its sensitivity for capturing all women who will go on to develop PPD, there is definitely a benefit to having a discussion about PPD and maternal mental health early and often throughout the postpartum period. For many women suffering in silence, a 6-week postpartum outpatient visit is too late, especially given that approximately one-third of women are lost to postpartum follow-up.29,30
Addressing barriers
A growing number of states have enacted policies to address the challenge of peripartum behavioral health needs, and several states – Illinois, Massachusetts, New Jersey, and West Virginia – now mandate routine PPD screening by health care providers.31 However, few of these laws or policies contain specific guidance, such as the optimal timing for screening, instead leaving the details to providers.32 The proper identification and management of PPD cannot be achieved by state-level policy mandates alone, but must include clinician buy-in and participation.
Obstetricians play an essential role in the identification and treatment of PPD. Among nonpsychiatric specialists, obstetrician-gynecologists are the most likely providers to see and screen during the perinatal period.33 In addition, women prefer to receive help for PPD from either their obstetric practitioners or a mental-health specialists located at the obstetric clinic, and are more likely to receive mental-health services if they are provided at the same location as that of the obstetric provider.34,35 According to ACOG’s new guidance on the fourth trimester, obstetricians are encouraged to take responsibility for women’s care immediately after birth, and this care would include contact with all mothers within the first 3 weeks post partum, at follow-up visits as needed, and for a comprehensive postpartum visit at 12 weeks.3
Our specialty has and will continue to evolve, and obstetric hospitalists will play an ever more essential role in the care of women during their inpatient obstetric admission. Whether we are a patient’s primary inpatient obstetric provider or a practice extender for single or multigroup practice, we are in a unique role to screen, begin treatment for, and offer anticipatory guidance for maternal mental health and postpartum depression disorders. Obstetric hospitalists can be a bridge between inpatient and outpatient follow-up and catalysts for implementing universal inpatient PPD screening. Our role presents an opportunity to start the discussion early and often in the fourth trimester and to make a significant difference in addressing this critical unmet need in postnatal care.
Dr. van Dis is the medical director of the Ob Hospitalist Group in Burbank, Calif. She disclosed she received editorial assistance from Erik MacLaren, PhD, of Boston Strategic Partners Inc., with funding support from Sage Therapeutics Inc. E-mail [email protected].
References
1. Centers for Disease Control and Prevention. Postpartum Depression. 2017.
2. Morb Mortal Wkly Rep. 2017;66(6):153-8.
3. Obstet Gynecol. 2018;131(5):e140-e150.
4. Harv Rev Psychiatry. 2014;22(1):1-22.
5. JAMA Psychiatry. 2018;75(3):247-53.
6. J Womens Health (Larchmt). 2016;25(12):1219-24.
7. J Psychiatr Res. 2017;84:284-91.
8. Br J Psychiatry. 2003;183:279-81.
9. Obstet Gynecol Surv. 2005;60(3):183-90.
10. Arch Womens Ment Health. 2016;19(1):87-94.
11. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335-45.
12. J Reprod Med. 1999;44(4):351-8.
13. J Behav Health Serv Res. 2004;31(2):117-33.
14. J Clin Psychiatry. 2016;77(9):1189-200.
15. Am J Obstet Gynecol. 2000;182(5):1080-2.
16. J Fam Pract. 2001;50(2):117-22.
17. Obstet Gynecol. 1999;93(5 Pt 1):653-7.
18. J Womens Health (Larchmt). 2010;19(3):477-90.
19. Obstet Gynecol. 2018;132:e208-12.
20. “Physicians back programs to address maternal mortality, depression,” AMA, Nov. 15, 2017
21. Pediatrics. 2019 Jan 1;143(1):e20183260.
22. JAMA. 2016;315(4):380-7.
23. Br J Psychiatry. 1987;150:782-6.
24. Ann Fam Med. 2009;7(1):63-70.
25. Obstet Gynecol. 2016;127(5):917-25.
26. Pediatrics. 2017 Oct;140(4). pii: e20170110.
27. Womens Health Issues. 2015;25(6):703-10.
28. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
29. Matern Child Health J. 2016;20(Suppl 1):22-7.
30. National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC). 2018.
31. Psychiatr Serv. 2015;66(3):324-8.
32. Postpartum Support International. Legislation. 2018.
33. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, eds. Guidelines for Perinatal Care. 7th ed. (Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; Oct 2012.)
34. Birth. 2009;36(1):60-9.
35. Gen Hosp Psychiatry. 2009;31(2):155-62.
Postpartum depression (PPD) is the most common complication of pregnancy, and onset can occur at any time from pregnancy until up to 1 year post partum.1,2 The immediate postpartum period is a time during which care is shared among multiple providers for both mother and child, and the transition from inpatient to outpatient postpartum care can impede communication between those caring for the patient in each setting. In 2018, the American College of Obstetricians and Gynecologists published a committee opinion emphasizing the importance of the “fourth trimester” and calling for health care providers to assist women in navigating the transition from pre- to postpartum care.3 An important consideration of perinatal care is mental health care for the mother, including screening and care for postpartum depression; however, the optimal role for the obstetric hospitalist in providing such services has been unclear.
Estimates of the prevalence of PPD in new mothers in the United States varied by state from 8% to 20% in 2012, with an overall average of 12%.2 Left untreated, PPD may result in significant negative outcomes for women, their children, and families. The depressive symptoms of PPD may persist for months or years afterward,4 with one study finding elevated depressive symptoms in women up to 11 years post partum.5 Suicide is also a leading cause of pregnancy-related mortality associated with depressive symptoms.6-9 In addition, maternal postpartum depression symptoms have been associated with impaired mother-infant bonding at 6 months of age10 and decreased cognitive and fine motor development of children at 18 months.11
Importance of screening
Evidence from the literature shows that, without proper screening, approximately 50% of cases of PPD go undiagnosed, and that increasing the number of women being screened by perinatal providers is an important first step to improving outcomes.12-18 Current recommendations for the timing and frequency of screening for PPD vary among the published guidelines. ACOG recommends screening at least once during the perinatal period for depression and anxiety using a standardized, validated tool; an update of the ACOG committee opinion in 2018 also states: “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.”19 The American Medical Association adopted new policies in 2017 promoting the implementation of a routine protocol for depression screening of perinatal women.20 The American Academy of Pediatrics recommends more frequent screening, with assessments at the 1-, 2-, 4-, and 6-month visits.21 Finally, the U.S. Preventive Services Task Force recommends screening for depression in the general population including pregnant and postpartum women.22
Multiple standardized, validated screening instruments are available for detecting possible symptoms of PPD, including the most widely used tools: the Edinburgh Postnatal Depression Scale (EPDS)19,23 and the Patient Health Questionnaire (PHQ-9).24 Two recent studies have shown that screening women for symptoms of PPD with a validated tool may reduce the duration or severity of depressive symptoms,25,26 further reinforcing the need to ensure that women experiencing symptoms of PPD are identified and treated early.
The inpatient hospitalization for labor, delivery, and birth of a child has not traditionally been viewed as an opportunity for PPD screening. While private practitioners and obstetric medical group practices typically have inquired about and documented the individual patient’s mental health history and risk factors for PPD, the obstetric hospitalist is most commonly meeting a patient in labor or in a postpartum encounter for the first time. As obstetric practices grow ever more consolidated, and as obstetric hospitalist care is implemented for a variety of reasons including, but not limited to, preventing burnout among private practitioners, serving as a safety net for all inpatient obstetric services, and increasing standardization in obstetric triage and obstetric emergency departments,
Barriers remain
Despite the need for early detection of PPD, screening practices remain inconsistent. A literature review of health care provider practices showed only one in four physicians reported using screening tools; obstetrician-gynecologists were most likely (36%) to use screening tools, followed by family practitioners (31%), with pediatricians the least likely (7%).27 This low rate is at least partially the result of perceived barriers to screening among health care providers, which contributes to underdiagnosis. A survey of more than 200 physicians who were members of ACOG showed that the top three barriers restricting screening practices were time constraints, inadequate training, and a lack of knowledge of the diagnostic criteria.28
Since 2017, Dignity Health has instituted routine screening of all inpatient postpartum patients at its 29 birth centers in Arizona, California, and Nevada. In this program, of which I am a physician participant, more than 30,000 women have been screened with the EPDS. In addition to providing screening, Dignity Health staff (physicians, certified nurse midwives, nurse practitioners, registered nurses, social workers, mental health therapists, lactation consultants, health educators, and others) have received in-person Perinatal Mental Health training. In this way, the entire care team coordinates inpatient screening and referral to outpatient care providers – thus bridging the gap in postpartum mental health care. For those patients who screen positive while an inpatient, a psychiatric telemedicine appointment is provided and, if necessary, short-course medications can be prescribed until the patient has outpatient follow-up and continuity of care. While we as obstetric hospitalists and community obstetrician-gynecologists recognize that inpatient postpartum screening may be limited in its sensitivity for capturing all women who will go on to develop PPD, there is definitely a benefit to having a discussion about PPD and maternal mental health early and often throughout the postpartum period. For many women suffering in silence, a 6-week postpartum outpatient visit is too late, especially given that approximately one-third of women are lost to postpartum follow-up.29,30
Addressing barriers
A growing number of states have enacted policies to address the challenge of peripartum behavioral health needs, and several states – Illinois, Massachusetts, New Jersey, and West Virginia – now mandate routine PPD screening by health care providers.31 However, few of these laws or policies contain specific guidance, such as the optimal timing for screening, instead leaving the details to providers.32 The proper identification and management of PPD cannot be achieved by state-level policy mandates alone, but must include clinician buy-in and participation.
Obstetricians play an essential role in the identification and treatment of PPD. Among nonpsychiatric specialists, obstetrician-gynecologists are the most likely providers to see and screen during the perinatal period.33 In addition, women prefer to receive help for PPD from either their obstetric practitioners or a mental-health specialists located at the obstetric clinic, and are more likely to receive mental-health services if they are provided at the same location as that of the obstetric provider.34,35 According to ACOG’s new guidance on the fourth trimester, obstetricians are encouraged to take responsibility for women’s care immediately after birth, and this care would include contact with all mothers within the first 3 weeks post partum, at follow-up visits as needed, and for a comprehensive postpartum visit at 12 weeks.3
Our specialty has and will continue to evolve, and obstetric hospitalists will play an ever more essential role in the care of women during their inpatient obstetric admission. Whether we are a patient’s primary inpatient obstetric provider or a practice extender for single or multigroup practice, we are in a unique role to screen, begin treatment for, and offer anticipatory guidance for maternal mental health and postpartum depression disorders. Obstetric hospitalists can be a bridge between inpatient and outpatient follow-up and catalysts for implementing universal inpatient PPD screening. Our role presents an opportunity to start the discussion early and often in the fourth trimester and to make a significant difference in addressing this critical unmet need in postnatal care.
Dr. van Dis is the medical director of the Ob Hospitalist Group in Burbank, Calif. She disclosed she received editorial assistance from Erik MacLaren, PhD, of Boston Strategic Partners Inc., with funding support from Sage Therapeutics Inc. E-mail [email protected].
References
1. Centers for Disease Control and Prevention. Postpartum Depression. 2017.
2. Morb Mortal Wkly Rep. 2017;66(6):153-8.
3. Obstet Gynecol. 2018;131(5):e140-e150.
4. Harv Rev Psychiatry. 2014;22(1):1-22.
5. JAMA Psychiatry. 2018;75(3):247-53.
6. J Womens Health (Larchmt). 2016;25(12):1219-24.
7. J Psychiatr Res. 2017;84:284-91.
8. Br J Psychiatry. 2003;183:279-81.
9. Obstet Gynecol Surv. 2005;60(3):183-90.
10. Arch Womens Ment Health. 2016;19(1):87-94.
11. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335-45.
12. J Reprod Med. 1999;44(4):351-8.
13. J Behav Health Serv Res. 2004;31(2):117-33.
14. J Clin Psychiatry. 2016;77(9):1189-200.
15. Am J Obstet Gynecol. 2000;182(5):1080-2.
16. J Fam Pract. 2001;50(2):117-22.
17. Obstet Gynecol. 1999;93(5 Pt 1):653-7.
18. J Womens Health (Larchmt). 2010;19(3):477-90.
19. Obstet Gynecol. 2018;132:e208-12.
20. “Physicians back programs to address maternal mortality, depression,” AMA, Nov. 15, 2017
21. Pediatrics. 2019 Jan 1;143(1):e20183260.
22. JAMA. 2016;315(4):380-7.
23. Br J Psychiatry. 1987;150:782-6.
24. Ann Fam Med. 2009;7(1):63-70.
25. Obstet Gynecol. 2016;127(5):917-25.
26. Pediatrics. 2017 Oct;140(4). pii: e20170110.
27. Womens Health Issues. 2015;25(6):703-10.
28. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
29. Matern Child Health J. 2016;20(Suppl 1):22-7.
30. National Committee for Quality Assurance. Prenatal and Postpartum Care (PPC). 2018.
31. Psychiatr Serv. 2015;66(3):324-8.
32. Postpartum Support International. Legislation. 2018.
33. American Academy of Pediatrics, American College of Obstetricians and Gynecologists, eds. Guidelines for Perinatal Care. 7th ed. (Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; Oct 2012.)
34. Birth. 2009;36(1):60-9.
35. Gen Hosp Psychiatry. 2009;31(2):155-62.
2019 Update on fertility
Professional societies, global organizations, and advocacy groups are continually working toward the goal of having the costs of infertility care covered by insurance carriers. Paramount to that effort is obtaining recognition of infertility as a burdensome disease. In this Update, we summarize national and international initiatives and societal trends that are helping to move us closer to that goal, and we encourage ObGyns to lead advocacy efforts.
Next, we detail several notable new features available in the annual report of the Society for Assisted Reproductive Technology (SART), an online interactive document that can be used to assist clinicians and patients in treatment decisions.
We also tackle the complexities of embryo selection for in vitro fertilization (IVF) and describe a potentially promising aneuploidy screening test, and explore its limitations.
Advances in recognizing infertility as a disease that merits insurance coverage
Major reproductive medicine organizations globally have endorsed the definition of infertility as a disease that "generates disability as an impairment of function" (TABLE 1).2 Fortunately, medical, societal, and judicial changes have resulted in progress for the 6.1 million women (and equivalent number of men) affected by infertility in the United States.3
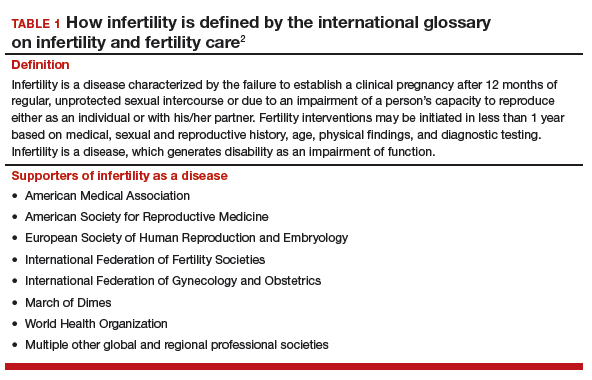
Professional group advocacy efforts, and judicial rulings
The World Health Organization (WHO) has addressed infertility over the past several decades, with the organization's standards on semen analysis being the most recognized outcome. Progress has been limited, however, regarding global or national policy that recognizes the importance of infertility as a medical and public health problem.
In 2009, the glossary published by the WHO with the International Committee for Monitoring Assisted Reproductive Technology (ICMART) defined infertility as a disease.4 This recognition is important because it aids policy making, insurance coverage, and/or other payments for services.
The WHO also has begun the process of developing new infertility guidelines. Recently, the WHO held a summit on safety and access to fertility care, which was attended by many representatives of nation-state governments and international experts. It is hoped that a document from those proceedings will reinforce the public health importance of infertility and support the need to promote equality in access to safe fertility care. WHO initiatives matter because they apply to nation-states.
In the United States, the American Society for Reproductive Medicine (ASRM) for many years has recognized infertility as a disease. Only in 2017, however, did delegates at the American Medical Association's annual meeting vote to support the WHO's designation of infertility as a disease.
Continue to: Judicial views
Judicial views. In 1998, the US Supreme Court held that infertility is a disability under the Americans with Disabilities Act (ADA). The Court subsequently held, however, that a person is not considered disabled under the act if the disability can be overcome by mitigating or corrective measures. In 2000, a lower court held that, while infertility is a disability, an employer's health plan that excludes treatment for it is not discriminatory under the ADA if it applies to all employees.
Societal recognition. Interestingly, improved technology for oocyte cryopreservation has resulted in greater recognition of reproductive issues and the disparity in reproductive health societal norms and rights between men and women.
Media stories and gender issues in employment, especially in such high-profile industries as technology and finance, have highlighted long-standing inequities, many of which concern reproductive issues. These issues have been further disseminated by the #metoo movement. Some employers are beginning to respond by recognizing their employees' reproductive needs and providing improved benefits for reproductive care.
ObGyns must continue to lead advocacy
Not all has been progress. Personhood bills in several states threaten basic reproductive rights of women and men. The ASRM and Resolve (the National Infertility Association) have taken leading roles in opposing these legislative initiatives and supporting reproductive rights.5
Advocacy efforts through events and trends have resulted in gradually improving the recognition of the burden of infertility, inadequate insurance coverage, and continuing gender inequalities in reproduction. Today, patients, professionals, and national and international organizations are coalescing around demands for recognition, access to care, and gender and diversity equality. While much remains to be done, progress is being made in society, government, the workplace, and the health care system.
ObGyns and other women's health care providers can help continue the progress toward equality in reproductive rights, including access to infertility care, by discussing insurance inequities with patients, informing insurance companies that infertility is a disease, and encouraging patients to challenge inadequate and unequal insurance coverage of needed reproductive health care.
The time is now for ObGyns and other women’s health care providers to advocate for insurance coverage of infertility care. When our patients have inadequate coverage, we should encourage them to take action by contacting their insurance company and their employers to explain the reasons and argue for better coverage. Also, contact RESOLVE for additional information.
Latest SART report offers new features to aid in treatment decision making
Knowledge of the prognosis and its various treatment options is an important aspect of infertility treatment. The SART recently updated its annual Clinic Summary Report (CSR), which includes valuable new features for patients and physicians considering assisted reproductive technology (ART) treatment.6
SART compiles complex data and reports outcomes
The SART has been reporting IVF outcomes and other ART outcomes since 1988. The society's annual report is widely read by consumers, patients, physicians, and policy makers, and it has many important uses. However, the report is complicated and difficult to interpret for many reasons. For example, treatments are complex and varied (especially with application of new cryopreservation technology), and there are variations among clinics with respect to patient selection, protocols used, philosophy of practice, and numerous other variables.
Continue to: Because of this...
Because of this, the SART states, "The SART Clinic Summary Report (CSR) allows patients to view national and individual clinic IVF success rates. The data presented in this report should not be used for comparing clinics. Clinics may have differences in patient selection and treatment approaches which may artificially inflate or lower pregnancy rates relative to another clinic. Please discuss this with your doctor."6
Nevertheless, the CSR is extremely useful because it reports outcomes, which can lead to more informed patients and physicians and thus better access to safe and effective use of ART. The SART has redesigned the CSR to make it more useful.
Redesigned CSR focuses on outcomes important to patients
In recent years, new technologies have increased dramatically the use of embryo cryopreservation, genetic testing, and single embryo transfer (SET). The new CSR format is more patient focused and identifies more directly the treatment burden: ovarian stimulation, egg retrieval, intracytoplasmic sperm injection, preimplantation genetic testing (PGT), cryopreservation, frozen embryo transfer, and multiple cycles. It also focuses on the important patient outcomes, including live birth of a healthy child, multiple pregnancy, number of cycles, and chances of success per patient over time (including both fresh and frozen embryo transfers).
Notable changes
A major change in the CSR is that there is a preliminary report for a given year and then a final report the following year. This helps to more accurately report cycles that have been "delayed" because of egg retrieval and embryo freezing performed in the reported year but then transferred in the following reporting year.
Cycle counting. A cycle is counted when a woman has started medications for an ART procedure or, in a "natural" cycle when no medications are used, the first day of menses of the ART cycle. If several cycles are performed to bank eggs or embryos, each will be counted in the denominator when calculating the pregnancy rate. This more accurately reflects the patient treatment burden and costs. A cycle cancelled before egg retrieval is still counted as a cycle.
Defining success. Success is characterized as delivery of a child, since this is the outcome patients desire. Singleton deliveries are emphasized, since twin and higher-order multiple pregnancies have a higher risk of prematurity, morbidity, mortality, and cost. The percentages of triplet, twin, and singleton births contributing to the live birth rate are provided for each cycle group, as is prematurity (TABLE 2).6
The end point of a treatment cycle can vary. The new CSR captures the success rate following one or more egg retrievals and the first embryo transfer (primary outcome), the success of subsequent cycles using frozen eggs or embryos not transferred in the first embryo transfer, and the combined contribution of the primary and subsequent cycles to the cumulative live birth rate for a patient both in the preliminary report and the final report for any given year. The live birth rate per patient also is reported and includes the outcomes for patients who are new to an infertility center and starting their first cycle for retrieval of their own eggs during the reporting year.
Continue to: Outcomes and prognostic factors...
Outcomes and prognostic factors. Outcomes are reported by multiple factors, including patient age and source of the eggs. These are important prognostic factors; separating the data allows you to obtain a better idea of both national and individual clinic experience by these factors.
The CSR also contains filters for infertility diagnosis, stimulation type, and other treatment details (FIGURE).6 The filter is a useful feature because multiple types of treatment can be included or excluded. The outcome of different treatment interventions can then be estimated based on outcomes from the entire sample of US patients with similar characteristics and interventions. This powerful tool can help patients and physicians choose the best treatment based on prognosis.
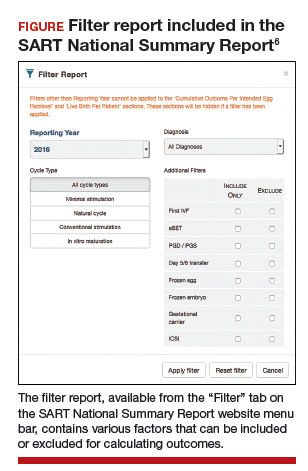
Personalized prognosis. An important new feature is the SART Patient Predictor (https://www.sartcorsonline.com/predictor/patient), a model that permits an individual patient to obtain a more personalized prognosis. While the SART predictor uses only basic patient information, such as age, body mass index, and diagnosis, its estimate is based on the entire US sample of reported ART experience and therefore can help patients in decision making. Furthermore, the predictor calculates percentages for the outcome of one transfer of 2 embryos, and 2 transfers of a single embryo, to demonstrate the advantages of SET that result in a higher live birth rate but a significantly lower multiple pregnancy rate.
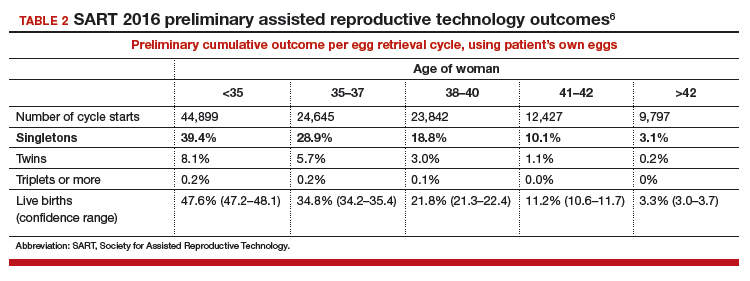
Summing up
The SART's new CSR is extremely useful to patients and to any physician who cares for infertility patients. It can help users both understand the expected results from different ART treatments and enable better physician-patient communication and decision making.
The updated annual SART Clinic Summary Report is an exceptionally valuable and easy-to-use online tool for you and your infertility patients.
Embryo selection techniques refined with use of newer technologies
Since the introduction of IVF in 1978, the final cumulative live birth rates per cycle initiated for oocyte retrieval after all resulting embryos have been trasferred continue to rise, currently standing at 54% for women younger than age 35 in the United States.7 A number of achievements have contributed to this remarkable success, namely, improvements in IVF laboratory and embryo culture systems, advances in cryopreservation technology, availability of highly effective gonadotropins and gonadotropin-releasing hormone analogues, improved ultrasound technology, and the introduction of soft catheters for atraumatic embryo transfers.
Treatment now focuses on improved embryo selection
Now that excellent success rates have been attained, the focus of optimizing efforts in fertility treatment has shifted to improving safety by reducing the rates of multiple pregnancy through elective single embryo transfer (eSET), reducing the rates of miscarriage, and shortening the time to live birth. Methods to improve embryo selection lie at the forefront of these initiatives. These vary and include extended culture to blastocyst stage, standard morphologic evaluation as well as morphokinetic assessment of embryonic development via time-lapse imaging, and more recently the reintroduction of preimplantation genetic testing for aneuploidy (PGT-A), formerly known as preimplantation genetic screening (PGS).
Chromosomal abnormalities of the embryo, or embryo aneuploidies, are the most common cause of treatment failure following embryo transfer in IVF. The proportion of embryos affected with aneuploidies significantly increases with advancing maternal age: 40% to 50% of blastocysts in women younger than age 35 and about 90% of blastocysts in women older than age 42.8 The premise with PGT-A is to identify these aneuploid embryos and increase the chances of success per embryo transfer by transferring euploid embryos.
Continue to: That concept was initially applied...
That concept was initially applied to cleavage-stage embryos through the use of fluorescence in situ hybridization (FISH) technology to interrogate a maximum of 5 to 9 chromosomes in a single cell (single blastomere); however, although initial results from observational studies were encouraging, subsequent randomized controlled studies unexpectedly showed a reduction in pregnancy rates.9 This was attributed to several factors, including biopsy-related damage to the cleavage-stage embryo, inability of FISH technology to assess aneuploidies of more than 5 to 9 chromosomes, mosaicism, and technical limitations associated with single-cell analysis.
Second-generation PGT-A testing has promise, and limitations
The newer PGT-A tests the embryos at the blastocyst stage by using biopsy samples from the trophectoderm (which will form the future placenta); this is expected to spare the inner cell mass ([ICM] which will give rise to the embryo proper) from biopsy-related injury.
On the genetics side, newer technologies, such as array comparative genomic hybridization, single nucleotide polymorphism arrays, quantitative polymerase chain reaction, and next-generation sequencing, offer the opportunity to assess all 24 chromosomes in a single biopsy specimen. Although a detailed discussion of these testing platforms is beyond the scope of this Update, certain points are worth mentioning. All these technologies require some form of genetic material amplification (most commonly whole genome amplification or multiplex polymerase chain reaction) to increase the relatively scant amount of DNA obtained from a sample of 4 to 6 cells. These amplification techniques have limitations that can subsequently impact the validity of the test results.
Furthermore, there is no consistency in depth of coverage for various parts of the genome, and subchromosomal (segmental) copy number variations below 3 to 5 Mb may not be detected. The threshold used in bioinformatics algorithms employed to interpret the raw data is subject to several biases and is not consistent among laboratories. As a result, the same sample assessed in different laboratories can potentially yield different results.
In addition to these technical limitations, mosaicism can pose another biologic limitation, as the biopsied trophectoderm cells may not accurately represent the chromosomal makeup of the ICM. Also, an embryo may be able to undergo self-correction during subsequent stages of development, and therefore even a documented trophectoderm abnormality at the blastocyst stage may not necessarily preclude that embryo from developing into a healthy baby.
Standardization is needed. Despite widespread promotion of PGT-A, well-designed randomized clinical trials (RCTs) have not yet consistently shown its benefits in improving pregnancy rates or reducing miscarriage rates. Although the initial small RCTs in a selected group of good prognosis patients suggested a beneficial effect in ongoing pregnancy rates per transfer, the largest multicenter RCT to date did not show any improvement in pregnancy rates or reduction in miscarriage rates.10 In that study, a post hoc subgroup analysis suggested a possible beneficial effect in women aged 35 to 40. However, those results must be validated and reproduced with randomization at the start of stimulation, with the primary outcome being the live birth rate per initiated cycle, instead of per transfer, before PGT-A can be adopted universally in clinical practice.
Continue to: With all the above considerations...
With all the above considerations, the ASRM has appropriately concluded that "the value of preimplantation genetic testing for aneuploidy (PGT-A) as a screening test for IVF patients has yet to be determined."11
Standardization of clinical and laboratory protocols and additional studies to assess the effects of PGT-A on live birth rates per initiated cycles are recommended before this new technology is widely adopted in routine clinical practice. In our practice, we routinely offer and perform extended culture to blastocyst stage and standard morphologic assessment. After a thorough counseling on the current status of PGT-A, about 15% to 20% of our patients opt to undergo PGT-A.
- United Nations website. General Assembly resolution 217A: Declaration of human rights. December 10, 1948. http://www.un.org/en/universal-declara tion-human-rights/. Accessed January 11, 2019.
- Zegers-Hochschild F, Adamson GD, Dyer S, et al. The international glossary on infertility and fertility care, 2017. Fertil Steril. 2017;108:393-406.
- US Department of Health and Human Services Office on Women's Health website. Infertility. https://www.womenshealth.gov/a-z-topics/infertility. Accessed January 24, 2019.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al; International Committee for Monitoring Assisted Reproductive Technology, World Health Organization. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520-1524.
- RESOLVE: The National Infertility Association website. Opposing personhood: Resolve fights to keep fertility medical treatments legal in the US. https://resolve.org/get-involved/advocate-for-access/our-issues/opposing-personhood/. Accessed January 11, 2019.
- Society for Assisted Reproductive Technology website. National summary report. 2016 Preliminary national data. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?reportingYear=2016 . Accessed January 12, 2019.
- Society for Assisted Reproductive Technology website. National summary report 2015. https://www.sartcorsonline,com/rptCSR_PublicMultYear.aspx ?reportingYear=2015. Accessed January 12, 2019.
- Harton GL, Munne S, Surrey M, et al; PGD Practitioners Group. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100:1695-1703.
- Mastenbroek S, Twisk M, van Echten-Arends, et al. In vitro fertilization with preimplantation genetic screening. N Engl J Med. 2007;357:9-17
- Munne S, Kaplan B, Frattarelli JL, et al. Global multicenter randomized controlled trial comparing single embryo transfer with embryo selected by preimplantation genetic screening using next-generation sequencing versus morphologic assessment [abstract O-43]. Fertil Steril. 2017;108(suppl):e19.
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109:429-436.
Professional societies, global organizations, and advocacy groups are continually working toward the goal of having the costs of infertility care covered by insurance carriers. Paramount to that effort is obtaining recognition of infertility as a burdensome disease. In this Update, we summarize national and international initiatives and societal trends that are helping to move us closer to that goal, and we encourage ObGyns to lead advocacy efforts.
Next, we detail several notable new features available in the annual report of the Society for Assisted Reproductive Technology (SART), an online interactive document that can be used to assist clinicians and patients in treatment decisions.
We also tackle the complexities of embryo selection for in vitro fertilization (IVF) and describe a potentially promising aneuploidy screening test, and explore its limitations.
Advances in recognizing infertility as a disease that merits insurance coverage
Major reproductive medicine organizations globally have endorsed the definition of infertility as a disease that "generates disability as an impairment of function" (TABLE 1).2 Fortunately, medical, societal, and judicial changes have resulted in progress for the 6.1 million women (and equivalent number of men) affected by infertility in the United States.3
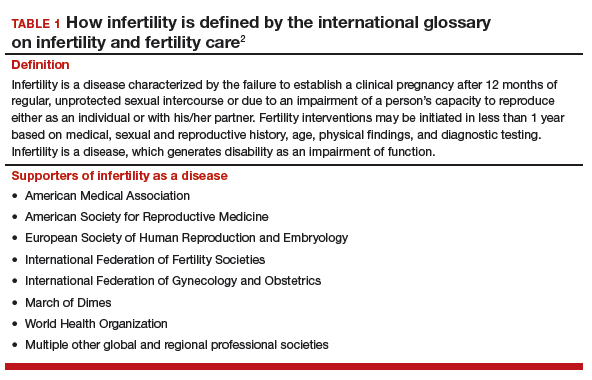
Professional group advocacy efforts, and judicial rulings
The World Health Organization (WHO) has addressed infertility over the past several decades, with the organization's standards on semen analysis being the most recognized outcome. Progress has been limited, however, regarding global or national policy that recognizes the importance of infertility as a medical and public health problem.
In 2009, the glossary published by the WHO with the International Committee for Monitoring Assisted Reproductive Technology (ICMART) defined infertility as a disease.4 This recognition is important because it aids policy making, insurance coverage, and/or other payments for services.
The WHO also has begun the process of developing new infertility guidelines. Recently, the WHO held a summit on safety and access to fertility care, which was attended by many representatives of nation-state governments and international experts. It is hoped that a document from those proceedings will reinforce the public health importance of infertility and support the need to promote equality in access to safe fertility care. WHO initiatives matter because they apply to nation-states.
In the United States, the American Society for Reproductive Medicine (ASRM) for many years has recognized infertility as a disease. Only in 2017, however, did delegates at the American Medical Association's annual meeting vote to support the WHO's designation of infertility as a disease.
Continue to: Judicial views
Judicial views. In 1998, the US Supreme Court held that infertility is a disability under the Americans with Disabilities Act (ADA). The Court subsequently held, however, that a person is not considered disabled under the act if the disability can be overcome by mitigating or corrective measures. In 2000, a lower court held that, while infertility is a disability, an employer's health plan that excludes treatment for it is not discriminatory under the ADA if it applies to all employees.
Societal recognition. Interestingly, improved technology for oocyte cryopreservation has resulted in greater recognition of reproductive issues and the disparity in reproductive health societal norms and rights between men and women.
Media stories and gender issues in employment, especially in such high-profile industries as technology and finance, have highlighted long-standing inequities, many of which concern reproductive issues. These issues have been further disseminated by the #metoo movement. Some employers are beginning to respond by recognizing their employees' reproductive needs and providing improved benefits for reproductive care.
ObGyns must continue to lead advocacy
Not all has been progress. Personhood bills in several states threaten basic reproductive rights of women and men. The ASRM and Resolve (the National Infertility Association) have taken leading roles in opposing these legislative initiatives and supporting reproductive rights.5
Advocacy efforts through events and trends have resulted in gradually improving the recognition of the burden of infertility, inadequate insurance coverage, and continuing gender inequalities in reproduction. Today, patients, professionals, and national and international organizations are coalescing around demands for recognition, access to care, and gender and diversity equality. While much remains to be done, progress is being made in society, government, the workplace, and the health care system.
ObGyns and other women's health care providers can help continue the progress toward equality in reproductive rights, including access to infertility care, by discussing insurance inequities with patients, informing insurance companies that infertility is a disease, and encouraging patients to challenge inadequate and unequal insurance coverage of needed reproductive health care.
The time is now for ObGyns and other women’s health care providers to advocate for insurance coverage of infertility care. When our patients have inadequate coverage, we should encourage them to take action by contacting their insurance company and their employers to explain the reasons and argue for better coverage. Also, contact RESOLVE for additional information.
Latest SART report offers new features to aid in treatment decision making
Knowledge of the prognosis and its various treatment options is an important aspect of infertility treatment. The SART recently updated its annual Clinic Summary Report (CSR), which includes valuable new features for patients and physicians considering assisted reproductive technology (ART) treatment.6
SART compiles complex data and reports outcomes
The SART has been reporting IVF outcomes and other ART outcomes since 1988. The society's annual report is widely read by consumers, patients, physicians, and policy makers, and it has many important uses. However, the report is complicated and difficult to interpret for many reasons. For example, treatments are complex and varied (especially with application of new cryopreservation technology), and there are variations among clinics with respect to patient selection, protocols used, philosophy of practice, and numerous other variables.
Continue to: Because of this...
Because of this, the SART states, "The SART Clinic Summary Report (CSR) allows patients to view national and individual clinic IVF success rates. The data presented in this report should not be used for comparing clinics. Clinics may have differences in patient selection and treatment approaches which may artificially inflate or lower pregnancy rates relative to another clinic. Please discuss this with your doctor."6
Nevertheless, the CSR is extremely useful because it reports outcomes, which can lead to more informed patients and physicians and thus better access to safe and effective use of ART. The SART has redesigned the CSR to make it more useful.
Redesigned CSR focuses on outcomes important to patients
In recent years, new technologies have increased dramatically the use of embryo cryopreservation, genetic testing, and single embryo transfer (SET). The new CSR format is more patient focused and identifies more directly the treatment burden: ovarian stimulation, egg retrieval, intracytoplasmic sperm injection, preimplantation genetic testing (PGT), cryopreservation, frozen embryo transfer, and multiple cycles. It also focuses on the important patient outcomes, including live birth of a healthy child, multiple pregnancy, number of cycles, and chances of success per patient over time (including both fresh and frozen embryo transfers).
Notable changes
A major change in the CSR is that there is a preliminary report for a given year and then a final report the following year. This helps to more accurately report cycles that have been "delayed" because of egg retrieval and embryo freezing performed in the reported year but then transferred in the following reporting year.
Cycle counting. A cycle is counted when a woman has started medications for an ART procedure or, in a "natural" cycle when no medications are used, the first day of menses of the ART cycle. If several cycles are performed to bank eggs or embryos, each will be counted in the denominator when calculating the pregnancy rate. This more accurately reflects the patient treatment burden and costs. A cycle cancelled before egg retrieval is still counted as a cycle.
Defining success. Success is characterized as delivery of a child, since this is the outcome patients desire. Singleton deliveries are emphasized, since twin and higher-order multiple pregnancies have a higher risk of prematurity, morbidity, mortality, and cost. The percentages of triplet, twin, and singleton births contributing to the live birth rate are provided for each cycle group, as is prematurity (TABLE 2).6
The end point of a treatment cycle can vary. The new CSR captures the success rate following one or more egg retrievals and the first embryo transfer (primary outcome), the success of subsequent cycles using frozen eggs or embryos not transferred in the first embryo transfer, and the combined contribution of the primary and subsequent cycles to the cumulative live birth rate for a patient both in the preliminary report and the final report for any given year. The live birth rate per patient also is reported and includes the outcomes for patients who are new to an infertility center and starting their first cycle for retrieval of their own eggs during the reporting year.
Continue to: Outcomes and prognostic factors...
Outcomes and prognostic factors. Outcomes are reported by multiple factors, including patient age and source of the eggs. These are important prognostic factors; separating the data allows you to obtain a better idea of both national and individual clinic experience by these factors.
The CSR also contains filters for infertility diagnosis, stimulation type, and other treatment details (FIGURE).6 The filter is a useful feature because multiple types of treatment can be included or excluded. The outcome of different treatment interventions can then be estimated based on outcomes from the entire sample of US patients with similar characteristics and interventions. This powerful tool can help patients and physicians choose the best treatment based on prognosis.
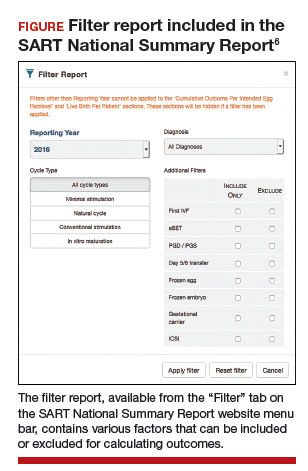
Personalized prognosis. An important new feature is the SART Patient Predictor (https://www.sartcorsonline.com/predictor/patient), a model that permits an individual patient to obtain a more personalized prognosis. While the SART predictor uses only basic patient information, such as age, body mass index, and diagnosis, its estimate is based on the entire US sample of reported ART experience and therefore can help patients in decision making. Furthermore, the predictor calculates percentages for the outcome of one transfer of 2 embryos, and 2 transfers of a single embryo, to demonstrate the advantages of SET that result in a higher live birth rate but a significantly lower multiple pregnancy rate.
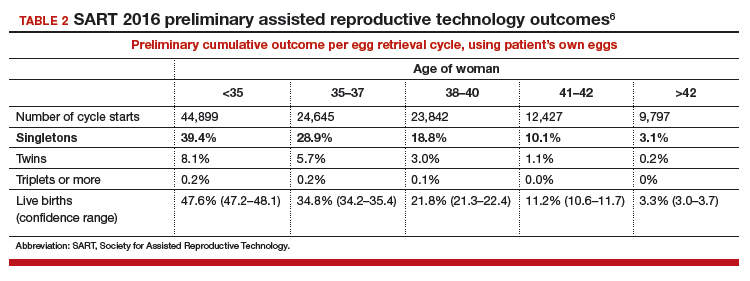
Summing up
The SART's new CSR is extremely useful to patients and to any physician who cares for infertility patients. It can help users both understand the expected results from different ART treatments and enable better physician-patient communication and decision making.
The updated annual SART Clinic Summary Report is an exceptionally valuable and easy-to-use online tool for you and your infertility patients.
Embryo selection techniques refined with use of newer technologies
Since the introduction of IVF in 1978, the final cumulative live birth rates per cycle initiated for oocyte retrieval after all resulting embryos have been trasferred continue to rise, currently standing at 54% for women younger than age 35 in the United States.7 A number of achievements have contributed to this remarkable success, namely, improvements in IVF laboratory and embryo culture systems, advances in cryopreservation technology, availability of highly effective gonadotropins and gonadotropin-releasing hormone analogues, improved ultrasound technology, and the introduction of soft catheters for atraumatic embryo transfers.
Treatment now focuses on improved embryo selection
Now that excellent success rates have been attained, the focus of optimizing efforts in fertility treatment has shifted to improving safety by reducing the rates of multiple pregnancy through elective single embryo transfer (eSET), reducing the rates of miscarriage, and shortening the time to live birth. Methods to improve embryo selection lie at the forefront of these initiatives. These vary and include extended culture to blastocyst stage, standard morphologic evaluation as well as morphokinetic assessment of embryonic development via time-lapse imaging, and more recently the reintroduction of preimplantation genetic testing for aneuploidy (PGT-A), formerly known as preimplantation genetic screening (PGS).
Chromosomal abnormalities of the embryo, or embryo aneuploidies, are the most common cause of treatment failure following embryo transfer in IVF. The proportion of embryos affected with aneuploidies significantly increases with advancing maternal age: 40% to 50% of blastocysts in women younger than age 35 and about 90% of blastocysts in women older than age 42.8 The premise with PGT-A is to identify these aneuploid embryos and increase the chances of success per embryo transfer by transferring euploid embryos.
Continue to: That concept was initially applied...
That concept was initially applied to cleavage-stage embryos through the use of fluorescence in situ hybridization (FISH) technology to interrogate a maximum of 5 to 9 chromosomes in a single cell (single blastomere); however, although initial results from observational studies were encouraging, subsequent randomized controlled studies unexpectedly showed a reduction in pregnancy rates.9 This was attributed to several factors, including biopsy-related damage to the cleavage-stage embryo, inability of FISH technology to assess aneuploidies of more than 5 to 9 chromosomes, mosaicism, and technical limitations associated with single-cell analysis.
Second-generation PGT-A testing has promise, and limitations
The newer PGT-A tests the embryos at the blastocyst stage by using biopsy samples from the trophectoderm (which will form the future placenta); this is expected to spare the inner cell mass ([ICM] which will give rise to the embryo proper) from biopsy-related injury.
On the genetics side, newer technologies, such as array comparative genomic hybridization, single nucleotide polymorphism arrays, quantitative polymerase chain reaction, and next-generation sequencing, offer the opportunity to assess all 24 chromosomes in a single biopsy specimen. Although a detailed discussion of these testing platforms is beyond the scope of this Update, certain points are worth mentioning. All these technologies require some form of genetic material amplification (most commonly whole genome amplification or multiplex polymerase chain reaction) to increase the relatively scant amount of DNA obtained from a sample of 4 to 6 cells. These amplification techniques have limitations that can subsequently impact the validity of the test results.
Furthermore, there is no consistency in depth of coverage for various parts of the genome, and subchromosomal (segmental) copy number variations below 3 to 5 Mb may not be detected. The threshold used in bioinformatics algorithms employed to interpret the raw data is subject to several biases and is not consistent among laboratories. As a result, the same sample assessed in different laboratories can potentially yield different results.
In addition to these technical limitations, mosaicism can pose another biologic limitation, as the biopsied trophectoderm cells may not accurately represent the chromosomal makeup of the ICM. Also, an embryo may be able to undergo self-correction during subsequent stages of development, and therefore even a documented trophectoderm abnormality at the blastocyst stage may not necessarily preclude that embryo from developing into a healthy baby.
Standardization is needed. Despite widespread promotion of PGT-A, well-designed randomized clinical trials (RCTs) have not yet consistently shown its benefits in improving pregnancy rates or reducing miscarriage rates. Although the initial small RCTs in a selected group of good prognosis patients suggested a beneficial effect in ongoing pregnancy rates per transfer, the largest multicenter RCT to date did not show any improvement in pregnancy rates or reduction in miscarriage rates.10 In that study, a post hoc subgroup analysis suggested a possible beneficial effect in women aged 35 to 40. However, those results must be validated and reproduced with randomization at the start of stimulation, with the primary outcome being the live birth rate per initiated cycle, instead of per transfer, before PGT-A can be adopted universally in clinical practice.
Continue to: With all the above considerations...
With all the above considerations, the ASRM has appropriately concluded that "the value of preimplantation genetic testing for aneuploidy (PGT-A) as a screening test for IVF patients has yet to be determined."11
Standardization of clinical and laboratory protocols and additional studies to assess the effects of PGT-A on live birth rates per initiated cycles are recommended before this new technology is widely adopted in routine clinical practice. In our practice, we routinely offer and perform extended culture to blastocyst stage and standard morphologic assessment. After a thorough counseling on the current status of PGT-A, about 15% to 20% of our patients opt to undergo PGT-A.
Professional societies, global organizations, and advocacy groups are continually working toward the goal of having the costs of infertility care covered by insurance carriers. Paramount to that effort is obtaining recognition of infertility as a burdensome disease. In this Update, we summarize national and international initiatives and societal trends that are helping to move us closer to that goal, and we encourage ObGyns to lead advocacy efforts.
Next, we detail several notable new features available in the annual report of the Society for Assisted Reproductive Technology (SART), an online interactive document that can be used to assist clinicians and patients in treatment decisions.
We also tackle the complexities of embryo selection for in vitro fertilization (IVF) and describe a potentially promising aneuploidy screening test, and explore its limitations.
Advances in recognizing infertility as a disease that merits insurance coverage
Major reproductive medicine organizations globally have endorsed the definition of infertility as a disease that "generates disability as an impairment of function" (TABLE 1).2 Fortunately, medical, societal, and judicial changes have resulted in progress for the 6.1 million women (and equivalent number of men) affected by infertility in the United States.3
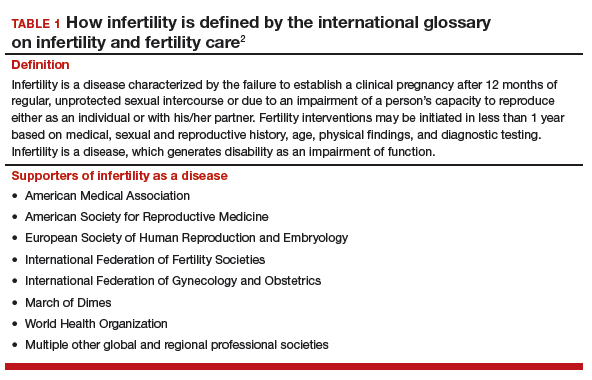
Professional group advocacy efforts, and judicial rulings
The World Health Organization (WHO) has addressed infertility over the past several decades, with the organization's standards on semen analysis being the most recognized outcome. Progress has been limited, however, regarding global or national policy that recognizes the importance of infertility as a medical and public health problem.
In 2009, the glossary published by the WHO with the International Committee for Monitoring Assisted Reproductive Technology (ICMART) defined infertility as a disease.4 This recognition is important because it aids policy making, insurance coverage, and/or other payments for services.
The WHO also has begun the process of developing new infertility guidelines. Recently, the WHO held a summit on safety and access to fertility care, which was attended by many representatives of nation-state governments and international experts. It is hoped that a document from those proceedings will reinforce the public health importance of infertility and support the need to promote equality in access to safe fertility care. WHO initiatives matter because they apply to nation-states.
In the United States, the American Society for Reproductive Medicine (ASRM) for many years has recognized infertility as a disease. Only in 2017, however, did delegates at the American Medical Association's annual meeting vote to support the WHO's designation of infertility as a disease.
Continue to: Judicial views
Judicial views. In 1998, the US Supreme Court held that infertility is a disability under the Americans with Disabilities Act (ADA). The Court subsequently held, however, that a person is not considered disabled under the act if the disability can be overcome by mitigating or corrective measures. In 2000, a lower court held that, while infertility is a disability, an employer's health plan that excludes treatment for it is not discriminatory under the ADA if it applies to all employees.
Societal recognition. Interestingly, improved technology for oocyte cryopreservation has resulted in greater recognition of reproductive issues and the disparity in reproductive health societal norms and rights between men and women.
Media stories and gender issues in employment, especially in such high-profile industries as technology and finance, have highlighted long-standing inequities, many of which concern reproductive issues. These issues have been further disseminated by the #metoo movement. Some employers are beginning to respond by recognizing their employees' reproductive needs and providing improved benefits for reproductive care.
ObGyns must continue to lead advocacy
Not all has been progress. Personhood bills in several states threaten basic reproductive rights of women and men. The ASRM and Resolve (the National Infertility Association) have taken leading roles in opposing these legislative initiatives and supporting reproductive rights.5
Advocacy efforts through events and trends have resulted in gradually improving the recognition of the burden of infertility, inadequate insurance coverage, and continuing gender inequalities in reproduction. Today, patients, professionals, and national and international organizations are coalescing around demands for recognition, access to care, and gender and diversity equality. While much remains to be done, progress is being made in society, government, the workplace, and the health care system.
ObGyns and other women's health care providers can help continue the progress toward equality in reproductive rights, including access to infertility care, by discussing insurance inequities with patients, informing insurance companies that infertility is a disease, and encouraging patients to challenge inadequate and unequal insurance coverage of needed reproductive health care.
The time is now for ObGyns and other women’s health care providers to advocate for insurance coverage of infertility care. When our patients have inadequate coverage, we should encourage them to take action by contacting their insurance company and their employers to explain the reasons and argue for better coverage. Also, contact RESOLVE for additional information.
Latest SART report offers new features to aid in treatment decision making
Knowledge of the prognosis and its various treatment options is an important aspect of infertility treatment. The SART recently updated its annual Clinic Summary Report (CSR), which includes valuable new features for patients and physicians considering assisted reproductive technology (ART) treatment.6
SART compiles complex data and reports outcomes
The SART has been reporting IVF outcomes and other ART outcomes since 1988. The society's annual report is widely read by consumers, patients, physicians, and policy makers, and it has many important uses. However, the report is complicated and difficult to interpret for many reasons. For example, treatments are complex and varied (especially with application of new cryopreservation technology), and there are variations among clinics with respect to patient selection, protocols used, philosophy of practice, and numerous other variables.
Continue to: Because of this...
Because of this, the SART states, "The SART Clinic Summary Report (CSR) allows patients to view national and individual clinic IVF success rates. The data presented in this report should not be used for comparing clinics. Clinics may have differences in patient selection and treatment approaches which may artificially inflate or lower pregnancy rates relative to another clinic. Please discuss this with your doctor."6
Nevertheless, the CSR is extremely useful because it reports outcomes, which can lead to more informed patients and physicians and thus better access to safe and effective use of ART. The SART has redesigned the CSR to make it more useful.
Redesigned CSR focuses on outcomes important to patients
In recent years, new technologies have increased dramatically the use of embryo cryopreservation, genetic testing, and single embryo transfer (SET). The new CSR format is more patient focused and identifies more directly the treatment burden: ovarian stimulation, egg retrieval, intracytoplasmic sperm injection, preimplantation genetic testing (PGT), cryopreservation, frozen embryo transfer, and multiple cycles. It also focuses on the important patient outcomes, including live birth of a healthy child, multiple pregnancy, number of cycles, and chances of success per patient over time (including both fresh and frozen embryo transfers).
Notable changes
A major change in the CSR is that there is a preliminary report for a given year and then a final report the following year. This helps to more accurately report cycles that have been "delayed" because of egg retrieval and embryo freezing performed in the reported year but then transferred in the following reporting year.
Cycle counting. A cycle is counted when a woman has started medications for an ART procedure or, in a "natural" cycle when no medications are used, the first day of menses of the ART cycle. If several cycles are performed to bank eggs or embryos, each will be counted in the denominator when calculating the pregnancy rate. This more accurately reflects the patient treatment burden and costs. A cycle cancelled before egg retrieval is still counted as a cycle.
Defining success. Success is characterized as delivery of a child, since this is the outcome patients desire. Singleton deliveries are emphasized, since twin and higher-order multiple pregnancies have a higher risk of prematurity, morbidity, mortality, and cost. The percentages of triplet, twin, and singleton births contributing to the live birth rate are provided for each cycle group, as is prematurity (TABLE 2).6
The end point of a treatment cycle can vary. The new CSR captures the success rate following one or more egg retrievals and the first embryo transfer (primary outcome), the success of subsequent cycles using frozen eggs or embryos not transferred in the first embryo transfer, and the combined contribution of the primary and subsequent cycles to the cumulative live birth rate for a patient both in the preliminary report and the final report for any given year. The live birth rate per patient also is reported and includes the outcomes for patients who are new to an infertility center and starting their first cycle for retrieval of their own eggs during the reporting year.
Continue to: Outcomes and prognostic factors...
Outcomes and prognostic factors. Outcomes are reported by multiple factors, including patient age and source of the eggs. These are important prognostic factors; separating the data allows you to obtain a better idea of both national and individual clinic experience by these factors.
The CSR also contains filters for infertility diagnosis, stimulation type, and other treatment details (FIGURE).6 The filter is a useful feature because multiple types of treatment can be included or excluded. The outcome of different treatment interventions can then be estimated based on outcomes from the entire sample of US patients with similar characteristics and interventions. This powerful tool can help patients and physicians choose the best treatment based on prognosis.
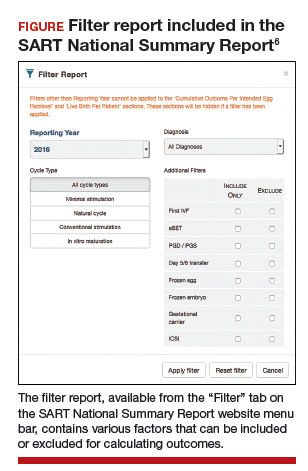
Personalized prognosis. An important new feature is the SART Patient Predictor (https://www.sartcorsonline.com/predictor/patient), a model that permits an individual patient to obtain a more personalized prognosis. While the SART predictor uses only basic patient information, such as age, body mass index, and diagnosis, its estimate is based on the entire US sample of reported ART experience and therefore can help patients in decision making. Furthermore, the predictor calculates percentages for the outcome of one transfer of 2 embryos, and 2 transfers of a single embryo, to demonstrate the advantages of SET that result in a higher live birth rate but a significantly lower multiple pregnancy rate.
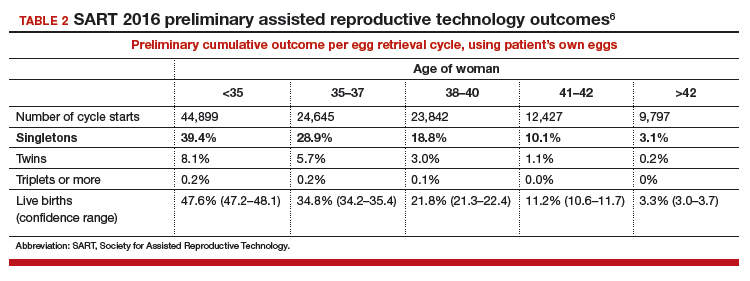
Summing up
The SART's new CSR is extremely useful to patients and to any physician who cares for infertility patients. It can help users both understand the expected results from different ART treatments and enable better physician-patient communication and decision making.
The updated annual SART Clinic Summary Report is an exceptionally valuable and easy-to-use online tool for you and your infertility patients.
Embryo selection techniques refined with use of newer technologies
Since the introduction of IVF in 1978, the final cumulative live birth rates per cycle initiated for oocyte retrieval after all resulting embryos have been trasferred continue to rise, currently standing at 54% for women younger than age 35 in the United States.7 A number of achievements have contributed to this remarkable success, namely, improvements in IVF laboratory and embryo culture systems, advances in cryopreservation technology, availability of highly effective gonadotropins and gonadotropin-releasing hormone analogues, improved ultrasound technology, and the introduction of soft catheters for atraumatic embryo transfers.
Treatment now focuses on improved embryo selection
Now that excellent success rates have been attained, the focus of optimizing efforts in fertility treatment has shifted to improving safety by reducing the rates of multiple pregnancy through elective single embryo transfer (eSET), reducing the rates of miscarriage, and shortening the time to live birth. Methods to improve embryo selection lie at the forefront of these initiatives. These vary and include extended culture to blastocyst stage, standard morphologic evaluation as well as morphokinetic assessment of embryonic development via time-lapse imaging, and more recently the reintroduction of preimplantation genetic testing for aneuploidy (PGT-A), formerly known as preimplantation genetic screening (PGS).
Chromosomal abnormalities of the embryo, or embryo aneuploidies, are the most common cause of treatment failure following embryo transfer in IVF. The proportion of embryos affected with aneuploidies significantly increases with advancing maternal age: 40% to 50% of blastocysts in women younger than age 35 and about 90% of blastocysts in women older than age 42.8 The premise with PGT-A is to identify these aneuploid embryos and increase the chances of success per embryo transfer by transferring euploid embryos.
Continue to: That concept was initially applied...
That concept was initially applied to cleavage-stage embryos through the use of fluorescence in situ hybridization (FISH) technology to interrogate a maximum of 5 to 9 chromosomes in a single cell (single blastomere); however, although initial results from observational studies were encouraging, subsequent randomized controlled studies unexpectedly showed a reduction in pregnancy rates.9 This was attributed to several factors, including biopsy-related damage to the cleavage-stage embryo, inability of FISH technology to assess aneuploidies of more than 5 to 9 chromosomes, mosaicism, and technical limitations associated with single-cell analysis.
Second-generation PGT-A testing has promise, and limitations
The newer PGT-A tests the embryos at the blastocyst stage by using biopsy samples from the trophectoderm (which will form the future placenta); this is expected to spare the inner cell mass ([ICM] which will give rise to the embryo proper) from biopsy-related injury.
On the genetics side, newer technologies, such as array comparative genomic hybridization, single nucleotide polymorphism arrays, quantitative polymerase chain reaction, and next-generation sequencing, offer the opportunity to assess all 24 chromosomes in a single biopsy specimen. Although a detailed discussion of these testing platforms is beyond the scope of this Update, certain points are worth mentioning. All these technologies require some form of genetic material amplification (most commonly whole genome amplification or multiplex polymerase chain reaction) to increase the relatively scant amount of DNA obtained from a sample of 4 to 6 cells. These amplification techniques have limitations that can subsequently impact the validity of the test results.
Furthermore, there is no consistency in depth of coverage for various parts of the genome, and subchromosomal (segmental) copy number variations below 3 to 5 Mb may not be detected. The threshold used in bioinformatics algorithms employed to interpret the raw data is subject to several biases and is not consistent among laboratories. As a result, the same sample assessed in different laboratories can potentially yield different results.
In addition to these technical limitations, mosaicism can pose another biologic limitation, as the biopsied trophectoderm cells may not accurately represent the chromosomal makeup of the ICM. Also, an embryo may be able to undergo self-correction during subsequent stages of development, and therefore even a documented trophectoderm abnormality at the blastocyst stage may not necessarily preclude that embryo from developing into a healthy baby.
Standardization is needed. Despite widespread promotion of PGT-A, well-designed randomized clinical trials (RCTs) have not yet consistently shown its benefits in improving pregnancy rates or reducing miscarriage rates. Although the initial small RCTs in a selected group of good prognosis patients suggested a beneficial effect in ongoing pregnancy rates per transfer, the largest multicenter RCT to date did not show any improvement in pregnancy rates or reduction in miscarriage rates.10 In that study, a post hoc subgroup analysis suggested a possible beneficial effect in women aged 35 to 40. However, those results must be validated and reproduced with randomization at the start of stimulation, with the primary outcome being the live birth rate per initiated cycle, instead of per transfer, before PGT-A can be adopted universally in clinical practice.
Continue to: With all the above considerations...
With all the above considerations, the ASRM has appropriately concluded that "the value of preimplantation genetic testing for aneuploidy (PGT-A) as a screening test for IVF patients has yet to be determined."11
Standardization of clinical and laboratory protocols and additional studies to assess the effects of PGT-A on live birth rates per initiated cycles are recommended before this new technology is widely adopted in routine clinical practice. In our practice, we routinely offer and perform extended culture to blastocyst stage and standard morphologic assessment. After a thorough counseling on the current status of PGT-A, about 15% to 20% of our patients opt to undergo PGT-A.
- United Nations website. General Assembly resolution 217A: Declaration of human rights. December 10, 1948. http://www.un.org/en/universal-declara tion-human-rights/. Accessed January 11, 2019.
- Zegers-Hochschild F, Adamson GD, Dyer S, et al. The international glossary on infertility and fertility care, 2017. Fertil Steril. 2017;108:393-406.
- US Department of Health and Human Services Office on Women's Health website. Infertility. https://www.womenshealth.gov/a-z-topics/infertility. Accessed January 24, 2019.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al; International Committee for Monitoring Assisted Reproductive Technology, World Health Organization. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520-1524.
- RESOLVE: The National Infertility Association website. Opposing personhood: Resolve fights to keep fertility medical treatments legal in the US. https://resolve.org/get-involved/advocate-for-access/our-issues/opposing-personhood/. Accessed January 11, 2019.
- Society for Assisted Reproductive Technology website. National summary report. 2016 Preliminary national data. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?reportingYear=2016 . Accessed January 12, 2019.
- Society for Assisted Reproductive Technology website. National summary report 2015. https://www.sartcorsonline,com/rptCSR_PublicMultYear.aspx ?reportingYear=2015. Accessed January 12, 2019.
- Harton GL, Munne S, Surrey M, et al; PGD Practitioners Group. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100:1695-1703.
- Mastenbroek S, Twisk M, van Echten-Arends, et al. In vitro fertilization with preimplantation genetic screening. N Engl J Med. 2007;357:9-17
- Munne S, Kaplan B, Frattarelli JL, et al. Global multicenter randomized controlled trial comparing single embryo transfer with embryo selected by preimplantation genetic screening using next-generation sequencing versus morphologic assessment [abstract O-43]. Fertil Steril. 2017;108(suppl):e19.
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109:429-436.
- United Nations website. General Assembly resolution 217A: Declaration of human rights. December 10, 1948. http://www.un.org/en/universal-declara tion-human-rights/. Accessed January 11, 2019.
- Zegers-Hochschild F, Adamson GD, Dyer S, et al. The international glossary on infertility and fertility care, 2017. Fertil Steril. 2017;108:393-406.
- US Department of Health and Human Services Office on Women's Health website. Infertility. https://www.womenshealth.gov/a-z-topics/infertility. Accessed January 24, 2019.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al; International Committee for Monitoring Assisted Reproductive Technology, World Health Organization. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520-1524.
- RESOLVE: The National Infertility Association website. Opposing personhood: Resolve fights to keep fertility medical treatments legal in the US. https://resolve.org/get-involved/advocate-for-access/our-issues/opposing-personhood/. Accessed January 11, 2019.
- Society for Assisted Reproductive Technology website. National summary report. 2016 Preliminary national data. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?reportingYear=2016 . Accessed January 12, 2019.
- Society for Assisted Reproductive Technology website. National summary report 2015. https://www.sartcorsonline,com/rptCSR_PublicMultYear.aspx ?reportingYear=2015. Accessed January 12, 2019.
- Harton GL, Munne S, Surrey M, et al; PGD Practitioners Group. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100:1695-1703.
- Mastenbroek S, Twisk M, van Echten-Arends, et al. In vitro fertilization with preimplantation genetic screening. N Engl J Med. 2007;357:9-17
- Munne S, Kaplan B, Frattarelli JL, et al. Global multicenter randomized controlled trial comparing single embryo transfer with embryo selected by preimplantation genetic screening using next-generation sequencing versus morphologic assessment [abstract O-43]. Fertil Steril. 2017;108(suppl):e19.
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109:429-436.
How do you feel about expectantly managing a well-dated pregnancy past 41 weeks’ gestation?
Most people know that preterm birth is a major contributor to perinatal morbidity and mortality. Consequently, strict guidelines have been enforced to prevent non–medically indicated scheduled deliveries before 39 weeks’ gestation. Fewer people recognize that late-term birth is also an important and avoidable contributor to perinatal morbidity. To improve pregnancy outcomes, we may need enhanced guidelines about minimizing expectant management of pregnancy beyond 41 weeks’ gestation.
For the fetus, what is the optimal duration of a healthy pregnancy?
When pregnancy progresses past the date of the confinement, the risk of fetal or newborn injury or death increases, especially after 41 weeks’ gestation. Analysis of this risk, day by day, suggests that after 40 weeks’ and 3 days’ gestation there is no medical benefit to the fetus to remain in utero because, compared with induced delivery, expectant management of the pregnancy is associated with a greater rate of fetal and newborn morbidity and mortality.1
The fetal and newborn benefits of delivery, rather than expectant management, at term include: a decrease in stillbirth and perinatal death rates, a decrease in admissions to the neonatal intensive care unit (NICU), a decrease in meconium-stained amniotic fluid and meconium aspiration syndrome, a decrease in low Apgar scores, and a decrease in problems related to uteroplacental insufficiency, including oligohydramnios.2 In a comprehensive meta-analysis, induction of labor at or beyond term reduced the risk of perinatal death or stillbirth by 67%, the risk of a 5-minute Apgar score below 7 by 30%, and the risk of NICU admission by 12%.2 The number of women that would need to be induced to prevent 1 perinatal death was estimated to be 426.2
Maternal benefits of avoiding late-term pregnancy
The maternal benefits of avoiding continuing a pregnancy past 41 weeks’ gestation include a reduction in labor dystocia and the risk of cesarean delivery (CD).2,3 In one clinical trial, 3,407 women with low-risk pregnancy were randomly assigned to induction of labor at 41 weeks’ gestation or expectant management, awaiting the onset of labor with serial antenatal monitoring (nonstress tests and assessment of amniotic fluid volume).4 The CD rate was lower among the women randomized to induction of labor at 41 weeks’ (21.2% vs 24.5% in the expectant management group, P = .03). The rate of meconium-stained fluid was lower in the induction of labor group (25.0% vs 28.7%, P = .009). The rate of CD due to fetal distress also was lower in the induction of labor group (5.7% vs 8.3%, P = .003). The risks of maternal postpartum hemorrhage, sepsis, and endometritis did not differ between the groups. There were 2 stillbirths in the expectant management group (2/1,706) and none in the induction of labor group (0/1,701). There were no neonatal deaths in this study.4
Obstetric management, including accurate dating of pregnancy and membrane sweeping at term, can help to reduce the risk that a pregnancy will progress beyond 41 weeks’ gestation.5
Continue to: Routinely use ultrasound to accurately establish gestational age
Routinely use ultrasound to accurately establish gestational age
First trimester ultrasound should be offered to all pregnant women because it is a more accurate assessment of gestational age and will result in fewer pregnancies that are thought to be at or beyond 41 weeks’ gestation.5 In a meta-analysis of 8 studies, including 25,516 women, early ultrasonography reduced the rate of intervention for postterm pregnancy by 42% (31/1,000 to 18/1,000 pregnant women).6

Membrane sweeping (or stripping)
Membrane sweeping, which causes the release of prostaglandins, has been reported to reduce the risk of late-term and postterm induction of labor.7,8 In the most recent Cochrane review on the topic, sweeping membranes reduced the rate of induction of labor at 41 weeks by 41% and at 42 weeks by 72%.7 To avoid one induction of labor for late-term or postterm pregnancy, sweeping of membranes would need to be performed on 8 women. In a recent meta-analysis, membrane sweeping reduced the rate of induction of labor for postmaturity by 48%.9
Membrane sweeping is associated with pain and an increased rate of vaginal bleeding.10 It does not increase the rate of maternal or neonatal infection, however. It also does not reduce the CD rate. In the United Kingdom, the National Institute for Health and Clinical Excellence recommends that all clinicians have a discussion of membrane sweeping with their patients at 38 weeks’ gestation and offer membrane stripping at 40 weeks to increase the rate of timely spontaneous labor and to avoid the risks of prolonged pregnancy.11 Of note, in one randomized study of women planning a trial of labor after CD, membrane sweeping did not impact the duration of pregnancy, onset of spontaneous labor, or the CD rate.12
Steps from an expert. A skillfull midwife practicing in the United Kingdom provides the following guidance on how to perform membrane sweeping.13
- Prepare the patient. Explain the procedure, have the patient empty her bladder, and encourage relaxed breathing if the vaginal examination causes pain.
- Abdominal exam. Assess uterine size, fetal lie and presentation, and fetal heart tones.
- Vaginal exam. Ascertain cervical dilation, effacement, and position. If the cervix is closed a sweep may not be possible. In this case, massaging the vaginal fornices may help to release prostaglandins and stimulate uterine contractions. If the cervix is closed but soft, massage of the cervix may permit the insertion of a finger. If the cervix is favorable for sweeping, insert one finger in the cervix and rotate the finger in a circle to separate the amnion from the cervix.
- After the procedure. Provide the woman with a sanitary pad and recommend acetaminophen and a warm bath if she has discomfort or painful contractions. Advise her to come to the maternity unit in the following situations: severe pain, significant bleeding, or spontaneous rupture of the membranes.
Membrane sweeping can be performed as frequently as every 3 days. Formal cervical ripening and induction of labor may need to be planned if membrane sweeping does not result in the initiation of regular contractions.
Continue to: Collaborative decision making
Collaborative decision making
All clinicians recognize the primacy of patient autonomy.14 Competent patients have the right to select the course of care that they believe is optimal. When a patient decides to continue her pregnancy past 41 weeks, it is helpful to endorse respect for the decision and inquire about the patient’s reasons for continuing the pregnancy. Understanding the patient’s concerns may begin a conversation that will result in the patient accepting a plan for induction near 41 weeks’ gestation. If the patient insists on expectant management well beyond 41 weeks, the medical record should contain a summary of the clinician recommendation to induce labor at or before 41 weeks’ gestation and the patient’s preference for expectant management and her understanding of the decision’s risks.
Obstetricians and midwives constantly face the challenge of balancing the desire to avoid meddlesome interference in a pregnancy with the need to act to prevent adverse pregnancy outcomes. The challenge is daunting. A comprehensive meta-analysis of the benefit of induction of labor at or beyond term, estimated that 426 inductions would need to be initiated to prevent one perinatal death.2 From one perspective it is meddlesome to intervene on more than 400 women to prevent one perinatal death. However, substantial data indicate that expectant management of a well-dated pregnancy at 41 weeks’ gestation will result in adverse outcomes that likely could be prevented by induction of labor. If you ran an airline and could take an action to prevent one airplane crash for every 400 flights, you would likely move heaven and earth to try to prevent that disaster. Unless the patient strongly prefers expectant management, well-managed induction of labor at or before 41 weeks’ gestation is likely to reduce the rate of adverse pregnancy events and, hence, is warranted.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Divon MY, Ferber A, Sanderson M, et al. A functional definition of prolonged pregnancy based on daily fetal and neonatal mortality rates. Ultrasound Obstet Gynecol. 2004;23:423-426.
- Middleton P, Shepherd E, Crowther CA. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2018;5:CD004945.
- Caughey AB, Sundaram V, Kaimal AJ, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med. 2009;151:252-263.
- Hannah ME, Hannah WJ, Hellmann J, et al; Canadian Multicenter Post-term Pregnancy Trial Group. Induction of labor as compared with serial antenatal monitoring in post-term pregnancy. N Engl J Med. 1992;326:1587-1592.
- Delaney M, Roggensack A. No. 214-Guidelines for the management of pregnancy at 41+0 to 42+0 weeks. J Obstet Gynaecol Can. 2017;39:e164-e174.
- Whitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2015;7:CD007058.
- Boulvain M, Stan C, Irion O. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2005;1:CD000451.
- Berghella V, Rogers RA, Lescale K. Stripping of membranes as a safe method to reduce prolonged pregnancies. Obstet Gynecol. 1996;87:927-931.
- Avdiyovski H, Haith-Cooper M, Scally A. Membrane sweeping at term to promote spontaneous labour and reduce the likelihood of a formal induction of labour for postmaturity: a systematic review and meta-analysis. J Obstet Gynaecol. 2018:1-9.
- de Miranda E, van der Bom JG, Bonsel G, et al. Membrane sweeping and prevention of post-term pregnancy in low-risk pregnancies: a randomised controlled trial. BJOG. 2006;113:402-408.
- National Collaborating Centre for Women's and Children's Health. NICE Guideline 70. Induction of labour; July 2008. https://www.nice.org.uk/guidance/cg70/evidence/cg70-induction-of-labour-full-guideline2. Accessed January 23, 2019.
- Hamdan M, Sidhu K, Sabir N, et al. Serial membrane sweeping at term in planned vaginal birth after cesarean: a randomized controlled trial. Obstet Gynecol. 2009;114:745-751.
- Gibbon K. How to perform a stretch and sweep. Midwives Magazine. 2012. https://www.rcm.org.uk/news-views-and-analysis/analysis/how-to%E2%80%A6-perform-a-stretch-and-sweep. Accessed January 23, 2019.
- Ryan KJ. Erosion of the rights of pregnant women: in the interest of fetal well-being. Womens Health Issues. 1990;1:21-24.
Most people know that preterm birth is a major contributor to perinatal morbidity and mortality. Consequently, strict guidelines have been enforced to prevent non–medically indicated scheduled deliveries before 39 weeks’ gestation. Fewer people recognize that late-term birth is also an important and avoidable contributor to perinatal morbidity. To improve pregnancy outcomes, we may need enhanced guidelines about minimizing expectant management of pregnancy beyond 41 weeks’ gestation.
For the fetus, what is the optimal duration of a healthy pregnancy?
When pregnancy progresses past the date of the confinement, the risk of fetal or newborn injury or death increases, especially after 41 weeks’ gestation. Analysis of this risk, day by day, suggests that after 40 weeks’ and 3 days’ gestation there is no medical benefit to the fetus to remain in utero because, compared with induced delivery, expectant management of the pregnancy is associated with a greater rate of fetal and newborn morbidity and mortality.1
The fetal and newborn benefits of delivery, rather than expectant management, at term include: a decrease in stillbirth and perinatal death rates, a decrease in admissions to the neonatal intensive care unit (NICU), a decrease in meconium-stained amniotic fluid and meconium aspiration syndrome, a decrease in low Apgar scores, and a decrease in problems related to uteroplacental insufficiency, including oligohydramnios.2 In a comprehensive meta-analysis, induction of labor at or beyond term reduced the risk of perinatal death or stillbirth by 67%, the risk of a 5-minute Apgar score below 7 by 30%, and the risk of NICU admission by 12%.2 The number of women that would need to be induced to prevent 1 perinatal death was estimated to be 426.2
Maternal benefits of avoiding late-term pregnancy
The maternal benefits of avoiding continuing a pregnancy past 41 weeks’ gestation include a reduction in labor dystocia and the risk of cesarean delivery (CD).2,3 In one clinical trial, 3,407 women with low-risk pregnancy were randomly assigned to induction of labor at 41 weeks’ gestation or expectant management, awaiting the onset of labor with serial antenatal monitoring (nonstress tests and assessment of amniotic fluid volume).4 The CD rate was lower among the women randomized to induction of labor at 41 weeks’ (21.2% vs 24.5% in the expectant management group, P = .03). The rate of meconium-stained fluid was lower in the induction of labor group (25.0% vs 28.7%, P = .009). The rate of CD due to fetal distress also was lower in the induction of labor group (5.7% vs 8.3%, P = .003). The risks of maternal postpartum hemorrhage, sepsis, and endometritis did not differ between the groups. There were 2 stillbirths in the expectant management group (2/1,706) and none in the induction of labor group (0/1,701). There were no neonatal deaths in this study.4
Obstetric management, including accurate dating of pregnancy and membrane sweeping at term, can help to reduce the risk that a pregnancy will progress beyond 41 weeks’ gestation.5
Continue to: Routinely use ultrasound to accurately establish gestational age
Routinely use ultrasound to accurately establish gestational age
First trimester ultrasound should be offered to all pregnant women because it is a more accurate assessment of gestational age and will result in fewer pregnancies that are thought to be at or beyond 41 weeks’ gestation.5 In a meta-analysis of 8 studies, including 25,516 women, early ultrasonography reduced the rate of intervention for postterm pregnancy by 42% (31/1,000 to 18/1,000 pregnant women).6

Membrane sweeping (or stripping)
Membrane sweeping, which causes the release of prostaglandins, has been reported to reduce the risk of late-term and postterm induction of labor.7,8 In the most recent Cochrane review on the topic, sweeping membranes reduced the rate of induction of labor at 41 weeks by 41% and at 42 weeks by 72%.7 To avoid one induction of labor for late-term or postterm pregnancy, sweeping of membranes would need to be performed on 8 women. In a recent meta-analysis, membrane sweeping reduced the rate of induction of labor for postmaturity by 48%.9
Membrane sweeping is associated with pain and an increased rate of vaginal bleeding.10 It does not increase the rate of maternal or neonatal infection, however. It also does not reduce the CD rate. In the United Kingdom, the National Institute for Health and Clinical Excellence recommends that all clinicians have a discussion of membrane sweeping with their patients at 38 weeks’ gestation and offer membrane stripping at 40 weeks to increase the rate of timely spontaneous labor and to avoid the risks of prolonged pregnancy.11 Of note, in one randomized study of women planning a trial of labor after CD, membrane sweeping did not impact the duration of pregnancy, onset of spontaneous labor, or the CD rate.12
Steps from an expert. A skillfull midwife practicing in the United Kingdom provides the following guidance on how to perform membrane sweeping.13
- Prepare the patient. Explain the procedure, have the patient empty her bladder, and encourage relaxed breathing if the vaginal examination causes pain.
- Abdominal exam. Assess uterine size, fetal lie and presentation, and fetal heart tones.
- Vaginal exam. Ascertain cervical dilation, effacement, and position. If the cervix is closed a sweep may not be possible. In this case, massaging the vaginal fornices may help to release prostaglandins and stimulate uterine contractions. If the cervix is closed but soft, massage of the cervix may permit the insertion of a finger. If the cervix is favorable for sweeping, insert one finger in the cervix and rotate the finger in a circle to separate the amnion from the cervix.
- After the procedure. Provide the woman with a sanitary pad and recommend acetaminophen and a warm bath if she has discomfort or painful contractions. Advise her to come to the maternity unit in the following situations: severe pain, significant bleeding, or spontaneous rupture of the membranes.
Membrane sweeping can be performed as frequently as every 3 days. Formal cervical ripening and induction of labor may need to be planned if membrane sweeping does not result in the initiation of regular contractions.
Continue to: Collaborative decision making
Collaborative decision making
All clinicians recognize the primacy of patient autonomy.14 Competent patients have the right to select the course of care that they believe is optimal. When a patient decides to continue her pregnancy past 41 weeks, it is helpful to endorse respect for the decision and inquire about the patient’s reasons for continuing the pregnancy. Understanding the patient’s concerns may begin a conversation that will result in the patient accepting a plan for induction near 41 weeks’ gestation. If the patient insists on expectant management well beyond 41 weeks, the medical record should contain a summary of the clinician recommendation to induce labor at or before 41 weeks’ gestation and the patient’s preference for expectant management and her understanding of the decision’s risks.
Obstetricians and midwives constantly face the challenge of balancing the desire to avoid meddlesome interference in a pregnancy with the need to act to prevent adverse pregnancy outcomes. The challenge is daunting. A comprehensive meta-analysis of the benefit of induction of labor at or beyond term, estimated that 426 inductions would need to be initiated to prevent one perinatal death.2 From one perspective it is meddlesome to intervene on more than 400 women to prevent one perinatal death. However, substantial data indicate that expectant management of a well-dated pregnancy at 41 weeks’ gestation will result in adverse outcomes that likely could be prevented by induction of labor. If you ran an airline and could take an action to prevent one airplane crash for every 400 flights, you would likely move heaven and earth to try to prevent that disaster. Unless the patient strongly prefers expectant management, well-managed induction of labor at or before 41 weeks’ gestation is likely to reduce the rate of adverse pregnancy events and, hence, is warranted.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Most people know that preterm birth is a major contributor to perinatal morbidity and mortality. Consequently, strict guidelines have been enforced to prevent non–medically indicated scheduled deliveries before 39 weeks’ gestation. Fewer people recognize that late-term birth is also an important and avoidable contributor to perinatal morbidity. To improve pregnancy outcomes, we may need enhanced guidelines about minimizing expectant management of pregnancy beyond 41 weeks’ gestation.
For the fetus, what is the optimal duration of a healthy pregnancy?
When pregnancy progresses past the date of the confinement, the risk of fetal or newborn injury or death increases, especially after 41 weeks’ gestation. Analysis of this risk, day by day, suggests that after 40 weeks’ and 3 days’ gestation there is no medical benefit to the fetus to remain in utero because, compared with induced delivery, expectant management of the pregnancy is associated with a greater rate of fetal and newborn morbidity and mortality.1
The fetal and newborn benefits of delivery, rather than expectant management, at term include: a decrease in stillbirth and perinatal death rates, a decrease in admissions to the neonatal intensive care unit (NICU), a decrease in meconium-stained amniotic fluid and meconium aspiration syndrome, a decrease in low Apgar scores, and a decrease in problems related to uteroplacental insufficiency, including oligohydramnios.2 In a comprehensive meta-analysis, induction of labor at or beyond term reduced the risk of perinatal death or stillbirth by 67%, the risk of a 5-minute Apgar score below 7 by 30%, and the risk of NICU admission by 12%.2 The number of women that would need to be induced to prevent 1 perinatal death was estimated to be 426.2
Maternal benefits of avoiding late-term pregnancy
The maternal benefits of avoiding continuing a pregnancy past 41 weeks’ gestation include a reduction in labor dystocia and the risk of cesarean delivery (CD).2,3 In one clinical trial, 3,407 women with low-risk pregnancy were randomly assigned to induction of labor at 41 weeks’ gestation or expectant management, awaiting the onset of labor with serial antenatal monitoring (nonstress tests and assessment of amniotic fluid volume).4 The CD rate was lower among the women randomized to induction of labor at 41 weeks’ (21.2% vs 24.5% in the expectant management group, P = .03). The rate of meconium-stained fluid was lower in the induction of labor group (25.0% vs 28.7%, P = .009). The rate of CD due to fetal distress also was lower in the induction of labor group (5.7% vs 8.3%, P = .003). The risks of maternal postpartum hemorrhage, sepsis, and endometritis did not differ between the groups. There were 2 stillbirths in the expectant management group (2/1,706) and none in the induction of labor group (0/1,701). There were no neonatal deaths in this study.4
Obstetric management, including accurate dating of pregnancy and membrane sweeping at term, can help to reduce the risk that a pregnancy will progress beyond 41 weeks’ gestation.5
Continue to: Routinely use ultrasound to accurately establish gestational age
Routinely use ultrasound to accurately establish gestational age
First trimester ultrasound should be offered to all pregnant women because it is a more accurate assessment of gestational age and will result in fewer pregnancies that are thought to be at or beyond 41 weeks’ gestation.5 In a meta-analysis of 8 studies, including 25,516 women, early ultrasonography reduced the rate of intervention for postterm pregnancy by 42% (31/1,000 to 18/1,000 pregnant women).6

Membrane sweeping (or stripping)
Membrane sweeping, which causes the release of prostaglandins, has been reported to reduce the risk of late-term and postterm induction of labor.7,8 In the most recent Cochrane review on the topic, sweeping membranes reduced the rate of induction of labor at 41 weeks by 41% and at 42 weeks by 72%.7 To avoid one induction of labor for late-term or postterm pregnancy, sweeping of membranes would need to be performed on 8 women. In a recent meta-analysis, membrane sweeping reduced the rate of induction of labor for postmaturity by 48%.9
Membrane sweeping is associated with pain and an increased rate of vaginal bleeding.10 It does not increase the rate of maternal or neonatal infection, however. It also does not reduce the CD rate. In the United Kingdom, the National Institute for Health and Clinical Excellence recommends that all clinicians have a discussion of membrane sweeping with their patients at 38 weeks’ gestation and offer membrane stripping at 40 weeks to increase the rate of timely spontaneous labor and to avoid the risks of prolonged pregnancy.11 Of note, in one randomized study of women planning a trial of labor after CD, membrane sweeping did not impact the duration of pregnancy, onset of spontaneous labor, or the CD rate.12
Steps from an expert. A skillfull midwife practicing in the United Kingdom provides the following guidance on how to perform membrane sweeping.13
- Prepare the patient. Explain the procedure, have the patient empty her bladder, and encourage relaxed breathing if the vaginal examination causes pain.
- Abdominal exam. Assess uterine size, fetal lie and presentation, and fetal heart tones.
- Vaginal exam. Ascertain cervical dilation, effacement, and position. If the cervix is closed a sweep may not be possible. In this case, massaging the vaginal fornices may help to release prostaglandins and stimulate uterine contractions. If the cervix is closed but soft, massage of the cervix may permit the insertion of a finger. If the cervix is favorable for sweeping, insert one finger in the cervix and rotate the finger in a circle to separate the amnion from the cervix.
- After the procedure. Provide the woman with a sanitary pad and recommend acetaminophen and a warm bath if she has discomfort or painful contractions. Advise her to come to the maternity unit in the following situations: severe pain, significant bleeding, or spontaneous rupture of the membranes.
Membrane sweeping can be performed as frequently as every 3 days. Formal cervical ripening and induction of labor may need to be planned if membrane sweeping does not result in the initiation of regular contractions.
Continue to: Collaborative decision making
Collaborative decision making
All clinicians recognize the primacy of patient autonomy.14 Competent patients have the right to select the course of care that they believe is optimal. When a patient decides to continue her pregnancy past 41 weeks, it is helpful to endorse respect for the decision and inquire about the patient’s reasons for continuing the pregnancy. Understanding the patient’s concerns may begin a conversation that will result in the patient accepting a plan for induction near 41 weeks’ gestation. If the patient insists on expectant management well beyond 41 weeks, the medical record should contain a summary of the clinician recommendation to induce labor at or before 41 weeks’ gestation and the patient’s preference for expectant management and her understanding of the decision’s risks.
Obstetricians and midwives constantly face the challenge of balancing the desire to avoid meddlesome interference in a pregnancy with the need to act to prevent adverse pregnancy outcomes. The challenge is daunting. A comprehensive meta-analysis of the benefit of induction of labor at or beyond term, estimated that 426 inductions would need to be initiated to prevent one perinatal death.2 From one perspective it is meddlesome to intervene on more than 400 women to prevent one perinatal death. However, substantial data indicate that expectant management of a well-dated pregnancy at 41 weeks’ gestation will result in adverse outcomes that likely could be prevented by induction of labor. If you ran an airline and could take an action to prevent one airplane crash for every 400 flights, you would likely move heaven and earth to try to prevent that disaster. Unless the patient strongly prefers expectant management, well-managed induction of labor at or before 41 weeks’ gestation is likely to reduce the rate of adverse pregnancy events and, hence, is warranted.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Divon MY, Ferber A, Sanderson M, et al. A functional definition of prolonged pregnancy based on daily fetal and neonatal mortality rates. Ultrasound Obstet Gynecol. 2004;23:423-426.
- Middleton P, Shepherd E, Crowther CA. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2018;5:CD004945.
- Caughey AB, Sundaram V, Kaimal AJ, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med. 2009;151:252-263.
- Hannah ME, Hannah WJ, Hellmann J, et al; Canadian Multicenter Post-term Pregnancy Trial Group. Induction of labor as compared with serial antenatal monitoring in post-term pregnancy. N Engl J Med. 1992;326:1587-1592.
- Delaney M, Roggensack A. No. 214-Guidelines for the management of pregnancy at 41+0 to 42+0 weeks. J Obstet Gynaecol Can. 2017;39:e164-e174.
- Whitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2015;7:CD007058.
- Boulvain M, Stan C, Irion O. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2005;1:CD000451.
- Berghella V, Rogers RA, Lescale K. Stripping of membranes as a safe method to reduce prolonged pregnancies. Obstet Gynecol. 1996;87:927-931.
- Avdiyovski H, Haith-Cooper M, Scally A. Membrane sweeping at term to promote spontaneous labour and reduce the likelihood of a formal induction of labour for postmaturity: a systematic review and meta-analysis. J Obstet Gynaecol. 2018:1-9.
- de Miranda E, van der Bom JG, Bonsel G, et al. Membrane sweeping and prevention of post-term pregnancy in low-risk pregnancies: a randomised controlled trial. BJOG. 2006;113:402-408.
- National Collaborating Centre for Women's and Children's Health. NICE Guideline 70. Induction of labour; July 2008. https://www.nice.org.uk/guidance/cg70/evidence/cg70-induction-of-labour-full-guideline2. Accessed January 23, 2019.
- Hamdan M, Sidhu K, Sabir N, et al. Serial membrane sweeping at term in planned vaginal birth after cesarean: a randomized controlled trial. Obstet Gynecol. 2009;114:745-751.
- Gibbon K. How to perform a stretch and sweep. Midwives Magazine. 2012. https://www.rcm.org.uk/news-views-and-analysis/analysis/how-to%E2%80%A6-perform-a-stretch-and-sweep. Accessed January 23, 2019.
- Ryan KJ. Erosion of the rights of pregnant women: in the interest of fetal well-being. Womens Health Issues. 1990;1:21-24.
- Divon MY, Ferber A, Sanderson M, et al. A functional definition of prolonged pregnancy based on daily fetal and neonatal mortality rates. Ultrasound Obstet Gynecol. 2004;23:423-426.
- Middleton P, Shepherd E, Crowther CA. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2018;5:CD004945.
- Caughey AB, Sundaram V, Kaimal AJ, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med. 2009;151:252-263.
- Hannah ME, Hannah WJ, Hellmann J, et al; Canadian Multicenter Post-term Pregnancy Trial Group. Induction of labor as compared with serial antenatal monitoring in post-term pregnancy. N Engl J Med. 1992;326:1587-1592.
- Delaney M, Roggensack A. No. 214-Guidelines for the management of pregnancy at 41+0 to 42+0 weeks. J Obstet Gynaecol Can. 2017;39:e164-e174.
- Whitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2015;7:CD007058.
- Boulvain M, Stan C, Irion O. Membrane sweeping for induction of labour. Cochrane Database Syst Rev. 2005;1:CD000451.
- Berghella V, Rogers RA, Lescale K. Stripping of membranes as a safe method to reduce prolonged pregnancies. Obstet Gynecol. 1996;87:927-931.
- Avdiyovski H, Haith-Cooper M, Scally A. Membrane sweeping at term to promote spontaneous labour and reduce the likelihood of a formal induction of labour for postmaturity: a systematic review and meta-analysis. J Obstet Gynaecol. 2018:1-9.
- de Miranda E, van der Bom JG, Bonsel G, et al. Membrane sweeping and prevention of post-term pregnancy in low-risk pregnancies: a randomised controlled trial. BJOG. 2006;113:402-408.
- National Collaborating Centre for Women's and Children's Health. NICE Guideline 70. Induction of labour; July 2008. https://www.nice.org.uk/guidance/cg70/evidence/cg70-induction-of-labour-full-guideline2. Accessed January 23, 2019.
- Hamdan M, Sidhu K, Sabir N, et al. Serial membrane sweeping at term in planned vaginal birth after cesarean: a randomized controlled trial. Obstet Gynecol. 2009;114:745-751.
- Gibbon K. How to perform a stretch and sweep. Midwives Magazine. 2012. https://www.rcm.org.uk/news-views-and-analysis/analysis/how-to%E2%80%A6-perform-a-stretch-and-sweep. Accessed January 23, 2019.
- Ryan KJ. Erosion of the rights of pregnant women: in the interest of fetal well-being. Womens Health Issues. 1990;1:21-24.
Click for Credit: Missed HIV screening opps; aspirin & preeclampsia; more
Here are 5 articles from the February issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Short-term lung function better predicts mortality risk in SSc
To take the posttest, go to: https://bit.ly/2RrRuIY
Expires November 26, 2019
2. Healthier lifestyle in midlife women reduces subclinical carotid atherosclerosis
To take the posttest, go to: https://bit.ly/2TvDH5G
Expires November 28, 2019
3. Three commonly used quick cognitive assessments often yield flawed results
To take the posttest, go to: https://bit.ly/2G1qkHn
Expires November 28, 2019
4. Missed HIV screening opportunities found among subsequently infected youth
To take the posttest, go to: https://bit.ly/2HGa8Nm
Expires November 29, 2019
5. Aspirin appears underused to prevent preeclampsia in SLE patients
To take the posttest, go to: https://bit.ly/2G0dU2v
Expires January 2, 2019
Here are 5 articles from the February issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Short-term lung function better predicts mortality risk in SSc
To take the posttest, go to: https://bit.ly/2RrRuIY
Expires November 26, 2019
2. Healthier lifestyle in midlife women reduces subclinical carotid atherosclerosis
To take the posttest, go to: https://bit.ly/2TvDH5G
Expires November 28, 2019
3. Three commonly used quick cognitive assessments often yield flawed results
To take the posttest, go to: https://bit.ly/2G1qkHn
Expires November 28, 2019
4. Missed HIV screening opportunities found among subsequently infected youth
To take the posttest, go to: https://bit.ly/2HGa8Nm
Expires November 29, 2019
5. Aspirin appears underused to prevent preeclampsia in SLE patients
To take the posttest, go to: https://bit.ly/2G0dU2v
Expires January 2, 2019
Here are 5 articles from the February issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Short-term lung function better predicts mortality risk in SSc
To take the posttest, go to: https://bit.ly/2RrRuIY
Expires November 26, 2019
2. Healthier lifestyle in midlife women reduces subclinical carotid atherosclerosis
To take the posttest, go to: https://bit.ly/2TvDH5G
Expires November 28, 2019
3. Three commonly used quick cognitive assessments often yield flawed results
To take the posttest, go to: https://bit.ly/2G1qkHn
Expires November 28, 2019
4. Missed HIV screening opportunities found among subsequently infected youth
To take the posttest, go to: https://bit.ly/2HGa8Nm
Expires November 29, 2019
5. Aspirin appears underused to prevent preeclampsia in SLE patients
To take the posttest, go to: https://bit.ly/2G0dU2v
Expires January 2, 2019
Pregnancy problems predict cardiovascular future
SNOWMASS, COLO. – Think of pregnancy as a cardiovascular stress test, Carole A. Warnes, MD, urged at the Annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
Pregnancy complications may unmask a predisposition to premature cardiovascular disease. Yet a woman’s reproductive history is often overlooked in this regard, despite the fact that cardiovascular disease is the number-one cause of death in women, observed Dr. Warnes, the Snowmass conference director and professor of medicine at the Mayo Clinic in Rochester, Minn.
“I think reproductive history is often overlooked as a predictor of cardiovascular and even peripheral vascular events. I suspect many of us don’t routinely ask our patients about miscarriages and stillbirths. We might think about preeclampsia, but these are also hallmarks of trouble to come,” the cardiologist said.
Indeed, this point was underscored in a retrospective Danish national population-based cohort registry study of more than 1 million women followed for nearly 16 million person-years after one or more miscarriages, stillbirths, or live singleton births. Women with stillbirths were 2.69-fold more likely to have an MI, 2.42-fold more likely to develop renovascular hypertension, and 1.74-fold more likely to have a stroke during follow-up than those with no stillbirths.
Moreover, women with miscarriages were 1.13-, 1.2-, and 1.16-fold more likely to have an MI, renovascular hypertension, and stroke, respectively, than women with no miscarriages. And the risks were additive: For each additional miscarriage, the risks of MI, renovascular hypertension, and stroke increased by 9%, 19%, and 13%, respectively (Circulation. 2013;127[17]:1775-82).
The concept of maternal placental syndromes encompasses four events believed to originate from diseased placental blood vessels: preeclampsia, gestational hypertension, placental abruption, and placental infarction. In a population-based retrospective study known as CHAMPS (Cardiovascular Health After Maternal Placental Syndromes), conducted in more than 1 million Ontario women who were free from cardiovascular disease prior to their first delivery, 7% were diagnosed with a maternal placental syndrome. Their incidence of a composite endpoint comprised of hospitalization or revascularization for CAD, peripheral artery disease, or cerebrovascular disease at least 90 days after delivery discharge was double that of women without a maternal placental syndrome.
“These women manifested their first cardiovascular event at an average age of 38, not 50 or 60,” Dr. Warnes said.
The risk of premature cardiovascular disease was magnified 4.4-fold in women with a maternal placental syndrome plus an intrauterine fetal death, compared with those with neither, after adjustment for sociodemographic factors and other potential confounders, and by 3.1-fold in women with a maternal placental syndrome and poor fetal growth (Lancet. 2005;366[9499]:1797-803).
These findings were independently confirmed recently in a population-based retrospective study of nearly 303,000 Florida women free of prepregnancy hypertension, diabetes, heart disease, or renal disease who were followed for a median of 4.9 years after their first delivery. During that relative brief follow-up period, the adjusted risk of cardiovascular disease was increased by 19% in those with a maternal placental syndrome, compared with those without. And the risk was additive: women with more than one maternal placental syndrome had a 43% greater short-term risk of developing cardiovascular disease, compared with those with none. And when women with a maternal placental syndrome also had a preterm birth or a small-for-gestational age baby, their risk increased 45% (Am J Obstet Gynecol. 2016;215[4]:484.e1-484.e14).
It’s not just preeclampsia, which affects 3%-5% of all pregnancies, and gestational hypertension – defined as high blood pressure arising only after 20 weeks’ gestation and without proteinuria – that have been linked to future premature cardiovascular disease. In the Northern Finland Birth Cohort 1966, in which investigators have followed 10,314 women born in that year for 39 years, any form of high blood pressure during pregnancy was a harbinger of subsequent cardiovascular disease, diabetes, and chronic kidney disease. That included chronic isolated systolic and isolated diastolic hypertension (Circulation. 2013;127[6]:681-90).
The pathophysiologic processes involved in complicated pregnancies echo those of CAD and stroke: inflammation, altered angiogenesis, vasculopathy, thrombosis, and insulin resistance. Still unsettled, however, is the chicken-versus-egg question of whether preeclampsia and other pregnancy complications represent the initial expression of an adverse phenotype associated with early development of cardiovascular disease or the complications injure the vascular endothelium and thereby trigger accelerated atherosclerosis. In any case, markers of endothelial activation have been documented up to 15 years after an episode of preeclampsia, Dr. Warnes said.
All of these data underscore the importance of identifying at-risk women based upon reproductive history, scheduling additional medical checkups so they don’t drop off the radar for the next 20 years, encouraging lifestyle modification, and giving consideration to early initiation of antihypertensive and lipid-lowering therapies.
“Pregnancy complications give us a glimpse of this awful disease trajectory at a time when women are completely asymptomatic and we could intervene and perhaps change outcomes with targeted therapy when it might be expected to work better and patients might be more receptive to such interventions,” she said.
Dr. Warnes reported having no financial conflicts of interest.
SNOWMASS, COLO. – Think of pregnancy as a cardiovascular stress test, Carole A. Warnes, MD, urged at the Annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
Pregnancy complications may unmask a predisposition to premature cardiovascular disease. Yet a woman’s reproductive history is often overlooked in this regard, despite the fact that cardiovascular disease is the number-one cause of death in women, observed Dr. Warnes, the Snowmass conference director and professor of medicine at the Mayo Clinic in Rochester, Minn.
“I think reproductive history is often overlooked as a predictor of cardiovascular and even peripheral vascular events. I suspect many of us don’t routinely ask our patients about miscarriages and stillbirths. We might think about preeclampsia, but these are also hallmarks of trouble to come,” the cardiologist said.
Indeed, this point was underscored in a retrospective Danish national population-based cohort registry study of more than 1 million women followed for nearly 16 million person-years after one or more miscarriages, stillbirths, or live singleton births. Women with stillbirths were 2.69-fold more likely to have an MI, 2.42-fold more likely to develop renovascular hypertension, and 1.74-fold more likely to have a stroke during follow-up than those with no stillbirths.
Moreover, women with miscarriages were 1.13-, 1.2-, and 1.16-fold more likely to have an MI, renovascular hypertension, and stroke, respectively, than women with no miscarriages. And the risks were additive: For each additional miscarriage, the risks of MI, renovascular hypertension, and stroke increased by 9%, 19%, and 13%, respectively (Circulation. 2013;127[17]:1775-82).
The concept of maternal placental syndromes encompasses four events believed to originate from diseased placental blood vessels: preeclampsia, gestational hypertension, placental abruption, and placental infarction. In a population-based retrospective study known as CHAMPS (Cardiovascular Health After Maternal Placental Syndromes), conducted in more than 1 million Ontario women who were free from cardiovascular disease prior to their first delivery, 7% were diagnosed with a maternal placental syndrome. Their incidence of a composite endpoint comprised of hospitalization or revascularization for CAD, peripheral artery disease, or cerebrovascular disease at least 90 days after delivery discharge was double that of women without a maternal placental syndrome.
“These women manifested their first cardiovascular event at an average age of 38, not 50 or 60,” Dr. Warnes said.
The risk of premature cardiovascular disease was magnified 4.4-fold in women with a maternal placental syndrome plus an intrauterine fetal death, compared with those with neither, after adjustment for sociodemographic factors and other potential confounders, and by 3.1-fold in women with a maternal placental syndrome and poor fetal growth (Lancet. 2005;366[9499]:1797-803).
These findings were independently confirmed recently in a population-based retrospective study of nearly 303,000 Florida women free of prepregnancy hypertension, diabetes, heart disease, or renal disease who were followed for a median of 4.9 years after their first delivery. During that relative brief follow-up period, the adjusted risk of cardiovascular disease was increased by 19% in those with a maternal placental syndrome, compared with those without. And the risk was additive: women with more than one maternal placental syndrome had a 43% greater short-term risk of developing cardiovascular disease, compared with those with none. And when women with a maternal placental syndrome also had a preterm birth or a small-for-gestational age baby, their risk increased 45% (Am J Obstet Gynecol. 2016;215[4]:484.e1-484.e14).
It’s not just preeclampsia, which affects 3%-5% of all pregnancies, and gestational hypertension – defined as high blood pressure arising only after 20 weeks’ gestation and without proteinuria – that have been linked to future premature cardiovascular disease. In the Northern Finland Birth Cohort 1966, in which investigators have followed 10,314 women born in that year for 39 years, any form of high blood pressure during pregnancy was a harbinger of subsequent cardiovascular disease, diabetes, and chronic kidney disease. That included chronic isolated systolic and isolated diastolic hypertension (Circulation. 2013;127[6]:681-90).
The pathophysiologic processes involved in complicated pregnancies echo those of CAD and stroke: inflammation, altered angiogenesis, vasculopathy, thrombosis, and insulin resistance. Still unsettled, however, is the chicken-versus-egg question of whether preeclampsia and other pregnancy complications represent the initial expression of an adverse phenotype associated with early development of cardiovascular disease or the complications injure the vascular endothelium and thereby trigger accelerated atherosclerosis. In any case, markers of endothelial activation have been documented up to 15 years after an episode of preeclampsia, Dr. Warnes said.
All of these data underscore the importance of identifying at-risk women based upon reproductive history, scheduling additional medical checkups so they don’t drop off the radar for the next 20 years, encouraging lifestyle modification, and giving consideration to early initiation of antihypertensive and lipid-lowering therapies.
“Pregnancy complications give us a glimpse of this awful disease trajectory at a time when women are completely asymptomatic and we could intervene and perhaps change outcomes with targeted therapy when it might be expected to work better and patients might be more receptive to such interventions,” she said.
Dr. Warnes reported having no financial conflicts of interest.
SNOWMASS, COLO. – Think of pregnancy as a cardiovascular stress test, Carole A. Warnes, MD, urged at the Annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
Pregnancy complications may unmask a predisposition to premature cardiovascular disease. Yet a woman’s reproductive history is often overlooked in this regard, despite the fact that cardiovascular disease is the number-one cause of death in women, observed Dr. Warnes, the Snowmass conference director and professor of medicine at the Mayo Clinic in Rochester, Minn.
“I think reproductive history is often overlooked as a predictor of cardiovascular and even peripheral vascular events. I suspect many of us don’t routinely ask our patients about miscarriages and stillbirths. We might think about preeclampsia, but these are also hallmarks of trouble to come,” the cardiologist said.
Indeed, this point was underscored in a retrospective Danish national population-based cohort registry study of more than 1 million women followed for nearly 16 million person-years after one or more miscarriages, stillbirths, or live singleton births. Women with stillbirths were 2.69-fold more likely to have an MI, 2.42-fold more likely to develop renovascular hypertension, and 1.74-fold more likely to have a stroke during follow-up than those with no stillbirths.
Moreover, women with miscarriages were 1.13-, 1.2-, and 1.16-fold more likely to have an MI, renovascular hypertension, and stroke, respectively, than women with no miscarriages. And the risks were additive: For each additional miscarriage, the risks of MI, renovascular hypertension, and stroke increased by 9%, 19%, and 13%, respectively (Circulation. 2013;127[17]:1775-82).
The concept of maternal placental syndromes encompasses four events believed to originate from diseased placental blood vessels: preeclampsia, gestational hypertension, placental abruption, and placental infarction. In a population-based retrospective study known as CHAMPS (Cardiovascular Health After Maternal Placental Syndromes), conducted in more than 1 million Ontario women who were free from cardiovascular disease prior to their first delivery, 7% were diagnosed with a maternal placental syndrome. Their incidence of a composite endpoint comprised of hospitalization or revascularization for CAD, peripheral artery disease, or cerebrovascular disease at least 90 days after delivery discharge was double that of women without a maternal placental syndrome.
“These women manifested their first cardiovascular event at an average age of 38, not 50 or 60,” Dr. Warnes said.
The risk of premature cardiovascular disease was magnified 4.4-fold in women with a maternal placental syndrome plus an intrauterine fetal death, compared with those with neither, after adjustment for sociodemographic factors and other potential confounders, and by 3.1-fold in women with a maternal placental syndrome and poor fetal growth (Lancet. 2005;366[9499]:1797-803).
These findings were independently confirmed recently in a population-based retrospective study of nearly 303,000 Florida women free of prepregnancy hypertension, diabetes, heart disease, or renal disease who were followed for a median of 4.9 years after their first delivery. During that relative brief follow-up period, the adjusted risk of cardiovascular disease was increased by 19% in those with a maternal placental syndrome, compared with those without. And the risk was additive: women with more than one maternal placental syndrome had a 43% greater short-term risk of developing cardiovascular disease, compared with those with none. And when women with a maternal placental syndrome also had a preterm birth or a small-for-gestational age baby, their risk increased 45% (Am J Obstet Gynecol. 2016;215[4]:484.e1-484.e14).
It’s not just preeclampsia, which affects 3%-5% of all pregnancies, and gestational hypertension – defined as high blood pressure arising only after 20 weeks’ gestation and without proteinuria – that have been linked to future premature cardiovascular disease. In the Northern Finland Birth Cohort 1966, in which investigators have followed 10,314 women born in that year for 39 years, any form of high blood pressure during pregnancy was a harbinger of subsequent cardiovascular disease, diabetes, and chronic kidney disease. That included chronic isolated systolic and isolated diastolic hypertension (Circulation. 2013;127[6]:681-90).
The pathophysiologic processes involved in complicated pregnancies echo those of CAD and stroke: inflammation, altered angiogenesis, vasculopathy, thrombosis, and insulin resistance. Still unsettled, however, is the chicken-versus-egg question of whether preeclampsia and other pregnancy complications represent the initial expression of an adverse phenotype associated with early development of cardiovascular disease or the complications injure the vascular endothelium and thereby trigger accelerated atherosclerosis. In any case, markers of endothelial activation have been documented up to 15 years after an episode of preeclampsia, Dr. Warnes said.
All of these data underscore the importance of identifying at-risk women based upon reproductive history, scheduling additional medical checkups so they don’t drop off the radar for the next 20 years, encouraging lifestyle modification, and giving consideration to early initiation of antihypertensive and lipid-lowering therapies.
“Pregnancy complications give us a glimpse of this awful disease trajectory at a time when women are completely asymptomatic and we could intervene and perhaps change outcomes with targeted therapy when it might be expected to work better and patients might be more receptive to such interventions,” she said.
Dr. Warnes reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM ACC SNOWMASS 2019
Preventing postpartum depression: Start with women at greatest risk
The last decade has brought appropriate attention to the high prevalence of postpartum mood and anxiety disorders, with postpartum depression (PPD) constituting the most common complication in modern obstetrics.
There have been very substantial efforts in more than 40 states in the United States to enhance screening for PPD and to increase support groups for women with postpartum depressive or anxiety symptoms. However, less focus has been paid to the outcomes of these screening initiatives.
A question that comes to mind is whether patients who are screened actually get referred for treatment, and if they do receive treatment, whether they recover and become well. One study referenced previously in this column noted that even in settings where women are screened for PPD, the vast majority of women are not referred, and of those who are referred, even fewer of those are treated or become well.1
It is noteworthy, then, that the U.S. Preventive Services Task Force has recommended screening for perinatal depression (just before and after birth) and issued draft recommendations regarding prevention of perinatal depression where it is suggested that patients at risk for perinatal depression be referred for appropriate “counseling interventions” – specifically, either cognitive-behavioral therapy (CBT) or interpersonal psychotherapy (IPT).2
The recommendation is a striking one because of the volume of patients who would be included. For example, the USPSTF recommends patients with histories of depression, depression during pregnancy, a history of child abuse, or even a family history of depression should receive preventive interventions with CBT or IPT. The recommendation is puzzling because of the data on risk for perinatal depression in those populations and the lack of available resources for patients who would be deemed “at risk.” Women with histories of depression are at a threefold increased risk for PPD (25%-30%). Depression during pregnancy is the strongest predictor of PPD and risk for PPD among these patients is as high as 75%.
So, there are a vast number of women who may be “at risk” for perinatal depression. But even with some data suggesting that IPT and CBT may be able to prevent perinatal depression, the suggestion that resources be made available to patients who are at risk is naive, because counseling interventions such as IPT or CBT, or even simply referrals to psychiatrists are not available even to patients who screen in for perinatal depression in real time during pregnancy and the postpartum period. I have previously written that the follow-up of women post partum who suffer from PPD is still far from meeting the needs who suffer from the disorder, and early detection and referrals to appropriate clinicians who are facile with both pharmacologic and nonpharmacologic interventions seem the most effective way to manage these patients and to see that they receive treatment.
The question then becomes: If the numbers or scale of the prevention initiative suggested in this draft recommendation from the USPSTF is an overreach, is there a group of patients for whom a preventive intervention could be pursued? The patients at highest risk for PPD include those with a history of PPD (50%), bipolar disorder (50%-60%), or postpartum psychosis (80%). And while there is not substantial literature for specifically using IPT, CBT, or other counseling interventions to mitigate risk for recurrence in women with histories of PPD, bipolar disorder, or postpartum psychosis, there are ways of identifying this population at risk and following them closely to mitigate the risk for recurrence.
To make this recommendation feasible, an infrastructure needs to be in place in both low resource settings and in all communities so that these patients can be referred and effectively treated. If we move to prevention, we ought to start with the populations that we already know are at greatest risk and that we can inquire about, and there are very easy-to-use screens that screen for bipolar disorder or that screen for past history of depression with which these women can be identified.
In committee opinion 757, the American College of Obstetricians and Gynecologists recommends women be screened at least once during the perinatal period for depression and anxiety symptoms and highlighted several validated tools, such as the Edinburgh Postnatal Depression Scale.3 We also need a better system of early detection and early intervention so that women at less-considerable risk for perinatal depression would have the opportunity for early identification, treatment, and referral, which we do not have at the current time.
An update of the ACOG committee opinion also states, “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.” This is recommended in addition to any screening for depression and anxiety during the pregnancy.
It is exciting that after decades of failing to attend to such a common complication of modern obstetrics, particularly now that we understand the adverse effects of PPD as it affects child development, family functioning, and risk for later childhood psychopathology. But in addition to recognizing the problem, we must come up with methods to carefully identify a navigable route for the women suffering from PPD to get their needs met. The route includes publicly identifying the illness, understanding which treatments are most effective and can be scaled for delivery to large numbers of women, and then, most critically, configuring social systems to absorb, effectively manage, and monitor the women we identify as needing treatment.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
References
1. J Clin Psychiatry. 2016 Sep;77[9]:1189-200.
2. Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. U.S. Preventive Services Task Force. Aug 2018.
The last decade has brought appropriate attention to the high prevalence of postpartum mood and anxiety disorders, with postpartum depression (PPD) constituting the most common complication in modern obstetrics.
There have been very substantial efforts in more than 40 states in the United States to enhance screening for PPD and to increase support groups for women with postpartum depressive or anxiety symptoms. However, less focus has been paid to the outcomes of these screening initiatives.
A question that comes to mind is whether patients who are screened actually get referred for treatment, and if they do receive treatment, whether they recover and become well. One study referenced previously in this column noted that even in settings where women are screened for PPD, the vast majority of women are not referred, and of those who are referred, even fewer of those are treated or become well.1
It is noteworthy, then, that the U.S. Preventive Services Task Force has recommended screening for perinatal depression (just before and after birth) and issued draft recommendations regarding prevention of perinatal depression where it is suggested that patients at risk for perinatal depression be referred for appropriate “counseling interventions” – specifically, either cognitive-behavioral therapy (CBT) or interpersonal psychotherapy (IPT).2
The recommendation is a striking one because of the volume of patients who would be included. For example, the USPSTF recommends patients with histories of depression, depression during pregnancy, a history of child abuse, or even a family history of depression should receive preventive interventions with CBT or IPT. The recommendation is puzzling because of the data on risk for perinatal depression in those populations and the lack of available resources for patients who would be deemed “at risk.” Women with histories of depression are at a threefold increased risk for PPD (25%-30%). Depression during pregnancy is the strongest predictor of PPD and risk for PPD among these patients is as high as 75%.
So, there are a vast number of women who may be “at risk” for perinatal depression. But even with some data suggesting that IPT and CBT may be able to prevent perinatal depression, the suggestion that resources be made available to patients who are at risk is naive, because counseling interventions such as IPT or CBT, or even simply referrals to psychiatrists are not available even to patients who screen in for perinatal depression in real time during pregnancy and the postpartum period. I have previously written that the follow-up of women post partum who suffer from PPD is still far from meeting the needs who suffer from the disorder, and early detection and referrals to appropriate clinicians who are facile with both pharmacologic and nonpharmacologic interventions seem the most effective way to manage these patients and to see that they receive treatment.
The question then becomes: If the numbers or scale of the prevention initiative suggested in this draft recommendation from the USPSTF is an overreach, is there a group of patients for whom a preventive intervention could be pursued? The patients at highest risk for PPD include those with a history of PPD (50%), bipolar disorder (50%-60%), or postpartum psychosis (80%). And while there is not substantial literature for specifically using IPT, CBT, or other counseling interventions to mitigate risk for recurrence in women with histories of PPD, bipolar disorder, or postpartum psychosis, there are ways of identifying this population at risk and following them closely to mitigate the risk for recurrence.
To make this recommendation feasible, an infrastructure needs to be in place in both low resource settings and in all communities so that these patients can be referred and effectively treated. If we move to prevention, we ought to start with the populations that we already know are at greatest risk and that we can inquire about, and there are very easy-to-use screens that screen for bipolar disorder or that screen for past history of depression with which these women can be identified.
In committee opinion 757, the American College of Obstetricians and Gynecologists recommends women be screened at least once during the perinatal period for depression and anxiety symptoms and highlighted several validated tools, such as the Edinburgh Postnatal Depression Scale.3 We also need a better system of early detection and early intervention so that women at less-considerable risk for perinatal depression would have the opportunity for early identification, treatment, and referral, which we do not have at the current time.
An update of the ACOG committee opinion also states, “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.” This is recommended in addition to any screening for depression and anxiety during the pregnancy.
It is exciting that after decades of failing to attend to such a common complication of modern obstetrics, particularly now that we understand the adverse effects of PPD as it affects child development, family functioning, and risk for later childhood psychopathology. But in addition to recognizing the problem, we must come up with methods to carefully identify a navigable route for the women suffering from PPD to get their needs met. The route includes publicly identifying the illness, understanding which treatments are most effective and can be scaled for delivery to large numbers of women, and then, most critically, configuring social systems to absorb, effectively manage, and monitor the women we identify as needing treatment.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
References
1. J Clin Psychiatry. 2016 Sep;77[9]:1189-200.
2. Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. U.S. Preventive Services Task Force. Aug 2018.
The last decade has brought appropriate attention to the high prevalence of postpartum mood and anxiety disorders, with postpartum depression (PPD) constituting the most common complication in modern obstetrics.
There have been very substantial efforts in more than 40 states in the United States to enhance screening for PPD and to increase support groups for women with postpartum depressive or anxiety symptoms. However, less focus has been paid to the outcomes of these screening initiatives.
A question that comes to mind is whether patients who are screened actually get referred for treatment, and if they do receive treatment, whether they recover and become well. One study referenced previously in this column noted that even in settings where women are screened for PPD, the vast majority of women are not referred, and of those who are referred, even fewer of those are treated or become well.1
It is noteworthy, then, that the U.S. Preventive Services Task Force has recommended screening for perinatal depression (just before and after birth) and issued draft recommendations regarding prevention of perinatal depression where it is suggested that patients at risk for perinatal depression be referred for appropriate “counseling interventions” – specifically, either cognitive-behavioral therapy (CBT) or interpersonal psychotherapy (IPT).2
The recommendation is a striking one because of the volume of patients who would be included. For example, the USPSTF recommends patients with histories of depression, depression during pregnancy, a history of child abuse, or even a family history of depression should receive preventive interventions with CBT or IPT. The recommendation is puzzling because of the data on risk for perinatal depression in those populations and the lack of available resources for patients who would be deemed “at risk.” Women with histories of depression are at a threefold increased risk for PPD (25%-30%). Depression during pregnancy is the strongest predictor of PPD and risk for PPD among these patients is as high as 75%.
So, there are a vast number of women who may be “at risk” for perinatal depression. But even with some data suggesting that IPT and CBT may be able to prevent perinatal depression, the suggestion that resources be made available to patients who are at risk is naive, because counseling interventions such as IPT or CBT, or even simply referrals to psychiatrists are not available even to patients who screen in for perinatal depression in real time during pregnancy and the postpartum period. I have previously written that the follow-up of women post partum who suffer from PPD is still far from meeting the needs who suffer from the disorder, and early detection and referrals to appropriate clinicians who are facile with both pharmacologic and nonpharmacologic interventions seem the most effective way to manage these patients and to see that they receive treatment.
The question then becomes: If the numbers or scale of the prevention initiative suggested in this draft recommendation from the USPSTF is an overreach, is there a group of patients for whom a preventive intervention could be pursued? The patients at highest risk for PPD include those with a history of PPD (50%), bipolar disorder (50%-60%), or postpartum psychosis (80%). And while there is not substantial literature for specifically using IPT, CBT, or other counseling interventions to mitigate risk for recurrence in women with histories of PPD, bipolar disorder, or postpartum psychosis, there are ways of identifying this population at risk and following them closely to mitigate the risk for recurrence.
To make this recommendation feasible, an infrastructure needs to be in place in both low resource settings and in all communities so that these patients can be referred and effectively treated. If we move to prevention, we ought to start with the populations that we already know are at greatest risk and that we can inquire about, and there are very easy-to-use screens that screen for bipolar disorder or that screen for past history of depression with which these women can be identified.
In committee opinion 757, the American College of Obstetricians and Gynecologists recommends women be screened at least once during the perinatal period for depression and anxiety symptoms and highlighted several validated tools, such as the Edinburgh Postnatal Depression Scale.3 We also need a better system of early detection and early intervention so that women at less-considerable risk for perinatal depression would have the opportunity for early identification, treatment, and referral, which we do not have at the current time.
An update of the ACOG committee opinion also states, “It is recommended that all obstetrician-gynecologists and other obstetric care providers complete a full assessment of mood and emotional well-being (including screening for PPD and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient.” This is recommended in addition to any screening for depression and anxiety during the pregnancy.
It is exciting that after decades of failing to attend to such a common complication of modern obstetrics, particularly now that we understand the adverse effects of PPD as it affects child development, family functioning, and risk for later childhood psychopathology. But in addition to recognizing the problem, we must come up with methods to carefully identify a navigable route for the women suffering from PPD to get their needs met. The route includes publicly identifying the illness, understanding which treatments are most effective and can be scaled for delivery to large numbers of women, and then, most critically, configuring social systems to absorb, effectively manage, and monitor the women we identify as needing treatment.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email him at [email protected].
References
1. J Clin Psychiatry. 2016 Sep;77[9]:1189-200.
2. Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. U.S. Preventive Services Task Force. Aug 2018.