User login
Rash goes undetected
Rash goes undetected
As a urogynecologist, in the past 5 years I have had 2 urgent emergency department referrals from 2 towns. The patients had excruciating flank pain and had a negative computed tomography scan and normal pelvic and renal examinations, but no physical exam. They were subsequently found to have shingles!
Bunan Alnaif, MD
Chesapeake, Virginia
Physical exam revealed suspicious mass
Two years ago a regular gynecologic patient of mine came in 2 months early for her Pap test because she was concerned about a pressure in her genital area. I had delivered her 3 children. She was now in her mid-40s. She had visited her usual physician about the problem; she was not physically examined but was advised to see a gastrointestinal specialist, since the pressure caused constipation with discomfort. She then consulted a gastroenterologist, who performed a colonoscopy that was reported as normal. The patient related that she had no pelvic or rectal examination at that time, although it is possible that one could have been done while she was under anesthesia.
She arrived at my office 3 weeks later, and while doing the pelvic and rectal exam, I noted she had a 3- to 4-cm perirectal mass, which I thought was a Bartholin’s tumor. I referred her to a gynecologic oncologist who happened to write a paper on this subject. My diagnosis was wrong—she had a rectal carcinoma, which fortunately was Stage 1.
The patient subsequently has done well. The delay in diagnosis could have been averted if a simple rectal examination had been performed by the first doctor.
James Moran, MD
Santa Monica, California
Case of an almost missed diagnosis
I have many examples of how not performing a physical examination can cause problems, but here is a recent one. This involved a 70-year-old woman who had been seeing only her primary care physician for the past 30 years, with no pelvic examinations done. She had symptoms of vaginal discharge and itch for which she was given multiple courses of antifungals and topical steroids. Finally, she was referred to me. Examination revealed findings of extensive raised, erythematous, hyperkeratotic, macerated lesions throughout the vulva. A punch biopsy revealed severe vulvar dysplasia with areas suspicious for squamous cell carcinoma. I referred the patient to a gynecologic oncologist, who performed a simple vulvectomy. There were extensive foci of vulvar intraepithelial neoplasia 3.
Susan Richman, MD
New Haven, Connecticut
Lack of physical exam leads to tortuous dx course
Here is a story of a patient who must have gone without having a pelvic examination or any evaluation for years. This 83-year-old woman had a previous transvaginal hysterectomy at age 49 for fibroids and bleeding. She is quite healthy and active for her age. She had problems with recurrent urinary tract infection for several years before being referred to a gynecologist. She had emergency room visits and multiple urgent care visits. She saw her primary care physician 3 times in 4 weeks for bladder pain and a sensation of incomplete bladder emptying. She reported that when she got up in the morning, it felt like her urine slowly leaked out for several hours. She was referred to a urologist, who saw her twice and did pelvic ultrasonography and postvoid residual urine testing—without a pelvic exam.
After 2 months of regular visits, an examination by her primary care physician revealed a complete fusion of the labia. Six months after her initial urology visit, the patient had an examination with a plan for cystoscopy, and the urologist ended up doing a “dilation of labial fusion” in the office. The patient’s urinary symptoms were improved slightly, and she had visits to the emergency room or urgent care once monthly for dysuria after dilation of the labia.
At that point she was referred to me. We tried topical estrogen for several months with minimal improvement in symptoms, and I performed a surgical separation of labial fusion in the operating room under monitored anesthesia care. After surgery the patient said that she felt like “I got my life back,” and she never knew how happy she could be to pee in the morning.
Theresa Gipps, MD
Walnut Creek, California
Agrees with importance of clinical exam
I fully agree that clinical examination skill is a dying art. But the American College of Obstetricians and Gynecologists has issued guidelines stating that pelvic examination is not required, especially in asymptomatic women. Another area of concern is hair removal procedures like waxing and laser treatments in the pubic area, and whether these do harm in any way or increase the likelihood of skin problems.
Manju Hotchandani, MD
New Delhi, India
Dr. Barbieri responds
I thank Drs. Alnaif, Moran, Richman, Gipps, and Hotchandani for sharing their comments and important clinical vignettes concerning the primacy of the physical examination with our readers. In clinical practice there are many competing demands on the time of clinicians, but we should strive to preserve time for a good physical examination. If not us, who is going to perform a competent physical examination?
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Rash goes undetected
As a urogynecologist, in the past 5 years I have had 2 urgent emergency department referrals from 2 towns. The patients had excruciating flank pain and had a negative computed tomography scan and normal pelvic and renal examinations, but no physical exam. They were subsequently found to have shingles!
Bunan Alnaif, MD
Chesapeake, Virginia
Physical exam revealed suspicious mass
Two years ago a regular gynecologic patient of mine came in 2 months early for her Pap test because she was concerned about a pressure in her genital area. I had delivered her 3 children. She was now in her mid-40s. She had visited her usual physician about the problem; she was not physically examined but was advised to see a gastrointestinal specialist, since the pressure caused constipation with discomfort. She then consulted a gastroenterologist, who performed a colonoscopy that was reported as normal. The patient related that she had no pelvic or rectal examination at that time, although it is possible that one could have been done while she was under anesthesia.
She arrived at my office 3 weeks later, and while doing the pelvic and rectal exam, I noted she had a 3- to 4-cm perirectal mass, which I thought was a Bartholin’s tumor. I referred her to a gynecologic oncologist who happened to write a paper on this subject. My diagnosis was wrong—she had a rectal carcinoma, which fortunately was Stage 1.
The patient subsequently has done well. The delay in diagnosis could have been averted if a simple rectal examination had been performed by the first doctor.
James Moran, MD
Santa Monica, California
Case of an almost missed diagnosis
I have many examples of how not performing a physical examination can cause problems, but here is a recent one. This involved a 70-year-old woman who had been seeing only her primary care physician for the past 30 years, with no pelvic examinations done. She had symptoms of vaginal discharge and itch for which she was given multiple courses of antifungals and topical steroids. Finally, she was referred to me. Examination revealed findings of extensive raised, erythematous, hyperkeratotic, macerated lesions throughout the vulva. A punch biopsy revealed severe vulvar dysplasia with areas suspicious for squamous cell carcinoma. I referred the patient to a gynecologic oncologist, who performed a simple vulvectomy. There were extensive foci of vulvar intraepithelial neoplasia 3.
Susan Richman, MD
New Haven, Connecticut
Lack of physical exam leads to tortuous dx course
Here is a story of a patient who must have gone without having a pelvic examination or any evaluation for years. This 83-year-old woman had a previous transvaginal hysterectomy at age 49 for fibroids and bleeding. She is quite healthy and active for her age. She had problems with recurrent urinary tract infection for several years before being referred to a gynecologist. She had emergency room visits and multiple urgent care visits. She saw her primary care physician 3 times in 4 weeks for bladder pain and a sensation of incomplete bladder emptying. She reported that when she got up in the morning, it felt like her urine slowly leaked out for several hours. She was referred to a urologist, who saw her twice and did pelvic ultrasonography and postvoid residual urine testing—without a pelvic exam.
After 2 months of regular visits, an examination by her primary care physician revealed a complete fusion of the labia. Six months after her initial urology visit, the patient had an examination with a plan for cystoscopy, and the urologist ended up doing a “dilation of labial fusion” in the office. The patient’s urinary symptoms were improved slightly, and she had visits to the emergency room or urgent care once monthly for dysuria after dilation of the labia.
At that point she was referred to me. We tried topical estrogen for several months with minimal improvement in symptoms, and I performed a surgical separation of labial fusion in the operating room under monitored anesthesia care. After surgery the patient said that she felt like “I got my life back,” and she never knew how happy she could be to pee in the morning.
Theresa Gipps, MD
Walnut Creek, California
Agrees with importance of clinical exam
I fully agree that clinical examination skill is a dying art. But the American College of Obstetricians and Gynecologists has issued guidelines stating that pelvic examination is not required, especially in asymptomatic women. Another area of concern is hair removal procedures like waxing and laser treatments in the pubic area, and whether these do harm in any way or increase the likelihood of skin problems.
Manju Hotchandani, MD
New Delhi, India
Dr. Barbieri responds
I thank Drs. Alnaif, Moran, Richman, Gipps, and Hotchandani for sharing their comments and important clinical vignettes concerning the primacy of the physical examination with our readers. In clinical practice there are many competing demands on the time of clinicians, but we should strive to preserve time for a good physical examination. If not us, who is going to perform a competent physical examination?
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Rash goes undetected
As a urogynecologist, in the past 5 years I have had 2 urgent emergency department referrals from 2 towns. The patients had excruciating flank pain and had a negative computed tomography scan and normal pelvic and renal examinations, but no physical exam. They were subsequently found to have shingles!
Bunan Alnaif, MD
Chesapeake, Virginia
Physical exam revealed suspicious mass
Two years ago a regular gynecologic patient of mine came in 2 months early for her Pap test because she was concerned about a pressure in her genital area. I had delivered her 3 children. She was now in her mid-40s. She had visited her usual physician about the problem; she was not physically examined but was advised to see a gastrointestinal specialist, since the pressure caused constipation with discomfort. She then consulted a gastroenterologist, who performed a colonoscopy that was reported as normal. The patient related that she had no pelvic or rectal examination at that time, although it is possible that one could have been done while she was under anesthesia.
She arrived at my office 3 weeks later, and while doing the pelvic and rectal exam, I noted she had a 3- to 4-cm perirectal mass, which I thought was a Bartholin’s tumor. I referred her to a gynecologic oncologist who happened to write a paper on this subject. My diagnosis was wrong—she had a rectal carcinoma, which fortunately was Stage 1.
The patient subsequently has done well. The delay in diagnosis could have been averted if a simple rectal examination had been performed by the first doctor.
James Moran, MD
Santa Monica, California
Case of an almost missed diagnosis
I have many examples of how not performing a physical examination can cause problems, but here is a recent one. This involved a 70-year-old woman who had been seeing only her primary care physician for the past 30 years, with no pelvic examinations done. She had symptoms of vaginal discharge and itch for which she was given multiple courses of antifungals and topical steroids. Finally, she was referred to me. Examination revealed findings of extensive raised, erythematous, hyperkeratotic, macerated lesions throughout the vulva. A punch biopsy revealed severe vulvar dysplasia with areas suspicious for squamous cell carcinoma. I referred the patient to a gynecologic oncologist, who performed a simple vulvectomy. There were extensive foci of vulvar intraepithelial neoplasia 3.
Susan Richman, MD
New Haven, Connecticut
Lack of physical exam leads to tortuous dx course
Here is a story of a patient who must have gone without having a pelvic examination or any evaluation for years. This 83-year-old woman had a previous transvaginal hysterectomy at age 49 for fibroids and bleeding. She is quite healthy and active for her age. She had problems with recurrent urinary tract infection for several years before being referred to a gynecologist. She had emergency room visits and multiple urgent care visits. She saw her primary care physician 3 times in 4 weeks for bladder pain and a sensation of incomplete bladder emptying. She reported that when she got up in the morning, it felt like her urine slowly leaked out for several hours. She was referred to a urologist, who saw her twice and did pelvic ultrasonography and postvoid residual urine testing—without a pelvic exam.
After 2 months of regular visits, an examination by her primary care physician revealed a complete fusion of the labia. Six months after her initial urology visit, the patient had an examination with a plan for cystoscopy, and the urologist ended up doing a “dilation of labial fusion” in the office. The patient’s urinary symptoms were improved slightly, and she had visits to the emergency room or urgent care once monthly for dysuria after dilation of the labia.
At that point she was referred to me. We tried topical estrogen for several months with minimal improvement in symptoms, and I performed a surgical separation of labial fusion in the operating room under monitored anesthesia care. After surgery the patient said that she felt like “I got my life back,” and she never knew how happy she could be to pee in the morning.
Theresa Gipps, MD
Walnut Creek, California
Agrees with importance of clinical exam
I fully agree that clinical examination skill is a dying art. But the American College of Obstetricians and Gynecologists has issued guidelines stating that pelvic examination is not required, especially in asymptomatic women. Another area of concern is hair removal procedures like waxing and laser treatments in the pubic area, and whether these do harm in any way or increase the likelihood of skin problems.
Manju Hotchandani, MD
New Delhi, India
Dr. Barbieri responds
I thank Drs. Alnaif, Moran, Richman, Gipps, and Hotchandani for sharing their comments and important clinical vignettes concerning the primacy of the physical examination with our readers. In clinical practice there are many competing demands on the time of clinicians, but we should strive to preserve time for a good physical examination. If not us, who is going to perform a competent physical examination?
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Treatment includes surgery
Treatment includes surgery
Thank you for the great article about hidradenitis suppurativa. It was very informative as usual, but a little shortsighted. As ObGyns we tend not to focus so much on these dermatologic conditions. However, I think something very important is missing in the article. I do not see it mentioned that hidradenitis suppurativa is a type of acne, also called acne inversa. As such, it should be treated like acne, with special attention to diet with zero dairy products as a prevention measure. Also, metformin is very important, as noted in the article. Retinoids are also needed, maybe for years.
According to experts, the primary approach to this condition is surgical, with punch biopsies and unroofing of the lesions, with medical therapies as prevention strategies. Fortunately, special task forces are now tackling this condition, especially in Europe. I strongly recommend the book, Acne: Causes and Practical Management, by F. William Danby.
Ivan Valencia, MD
Quito, Ecuador
Dr. Barbieri responds
Dr. Valencia provides an important perspective on the surgical treatment of hidradenitis suppurativa (HS). I agree that surgery is an important treatment for Stage III HS, but nonsurgical approaches are preferred and often effective for Stage I HS, a stage most likely to be treated by a gynecologist.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Treatment includes surgery
Thank you for the great article about hidradenitis suppurativa. It was very informative as usual, but a little shortsighted. As ObGyns we tend not to focus so much on these dermatologic conditions. However, I think something very important is missing in the article. I do not see it mentioned that hidradenitis suppurativa is a type of acne, also called acne inversa. As such, it should be treated like acne, with special attention to diet with zero dairy products as a prevention measure. Also, metformin is very important, as noted in the article. Retinoids are also needed, maybe for years.
According to experts, the primary approach to this condition is surgical, with punch biopsies and unroofing of the lesions, with medical therapies as prevention strategies. Fortunately, special task forces are now tackling this condition, especially in Europe. I strongly recommend the book, Acne: Causes and Practical Management, by F. William Danby.
Ivan Valencia, MD
Quito, Ecuador
Dr. Barbieri responds
Dr. Valencia provides an important perspective on the surgical treatment of hidradenitis suppurativa (HS). I agree that surgery is an important treatment for Stage III HS, but nonsurgical approaches are preferred and often effective for Stage I HS, a stage most likely to be treated by a gynecologist.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Treatment includes surgery
Thank you for the great article about hidradenitis suppurativa. It was very informative as usual, but a little shortsighted. As ObGyns we tend not to focus so much on these dermatologic conditions. However, I think something very important is missing in the article. I do not see it mentioned that hidradenitis suppurativa is a type of acne, also called acne inversa. As such, it should be treated like acne, with special attention to diet with zero dairy products as a prevention measure. Also, metformin is very important, as noted in the article. Retinoids are also needed, maybe for years.
According to experts, the primary approach to this condition is surgical, with punch biopsies and unroofing of the lesions, with medical therapies as prevention strategies. Fortunately, special task forces are now tackling this condition, especially in Europe. I strongly recommend the book, Acne: Causes and Practical Management, by F. William Danby.
Ivan Valencia, MD
Quito, Ecuador
Dr. Barbieri responds
Dr. Valencia provides an important perspective on the surgical treatment of hidradenitis suppurativa (HS). I agree that surgery is an important treatment for Stage III HS, but nonsurgical approaches are preferred and often effective for Stage I HS, a stage most likely to be treated by a gynecologist.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Incision site for cesarean delivery is important in infection prevention
Incision site for cesarean delivery is important in infection prevention
Dr. Barbieri’s editorial very nicely explained strategies to reduce the risk of post–cesarean delivery surgical site infection (SSI). However, what was not mentioned, in my opinion, is the most important preventive strategy. Selecting the site for the initial skin incision plays a great role in whether or not the patient will develop an infection postoperatively.
Pfannenstiel incisions are popular because of their obvious cosmetic benefit. In nonemergent cesarean deliveries, most ObGyns try to use this incision. However, exactly where the incision is placed plays a large role in the genesis of a postoperative wound infection. The worst place for such incisions is in the crease above the pubis and below the panniculus. Invariably, this area remains moist and macerated, especially in obese patients, thus providing a fertile breeding ground for bacteria. This problem can be avoided by incising the skin approximately 2 cm cranial to and parallel to the aforementioned crease, provided that the panniculus is not too large. The point is that the incision should be placed in an area where it has a chance to stay dry.
Sometimes patients who are hugely obese require great creativity in the placement of their transverse skin incision. I recall one patient, pregnant with triplets, whose abdomen was so large that her umbilicus was over the region of the lower uterine segment when she was supine on the operating room table. Some would have lifted up her immense panniculus and placed the incision in the usual crease site. This would be problematic for obtaining adequate exposure to deliver the babies, and the risk of developing an incisional infection would be very high. Therefore, a transverse incision was made just below her umbilicus. The panniculus was a nonissue regarding gaining adequate exposure and, when closed, the incision remained completely dry and uninfected. The patient did extremely well postoperatively and had no infectious sequelae.
David L. Zisow, MD
Baltimore, Maryland
Extraperitoneal approach should be considered
I enjoyed the editorial on reducing surgical site infection, especially the references to the historical Halsted principles of surgery. “He was the first in this country to promulgate the philosophy of ‘safe’ surgery.”1 Regarding surgical principles of cesarean delivery, the pioneering German obstetricians in the 1930s were keenly aware that avoiding the peritoneal cavity was instrumental in reducing morbidity and mortality. They championed the safety of the extraperitoneal approach as the fundamental principle of cesarean delivery for maternal safety.2
I learned to embrace the principles of Kaboth while learning the technique in 1968–1972. Thus, for more than 30 years, I used the extraperitoneal approach to access the lower uterine segment, avoiding entrance into the abdominal cavity. My patients seemed to benefit. As the surgeon, I also benefited: with short operative delivery times, less postoperative pain and minor morbidities, fewer phone calls from nursing staff, and less difficulty for my patients. I had not contaminated the peritoneal cavity and avoided all those inherent problems. The decision to open the peritoneal cavity has not been subjected to the rigors of critical analysis.3 I think that Kaboth’s principles remain worthy of consideration even today.
Contemporary experiences in large populations such as in India and China that use the extraperitoneal cesarean approach seem to implicitly support Kaboth’s principles. However, in the milieu of evidence-based medicine, extraperitoneal cesarean delivery has not been adequately studied.4 Just maybe the extraperitoneal approach should be considered and understood as a primary surgical technique for cesarean deliveries; just maybe it deserves a historical asterisk alongside the Halsted dicta.
Hedric Hanson, MD
Anchorage, Alaska
Dr. Barbieri responds
I thank Drs. Zisow and Hanson for their great recommendations and clinical pearls. I agree with Dr. Zisow that I should have mentioned the importance of optimal placement of the transverse skin incision. Incision in a skin crease that is perpetually moist increases the risk for a postoperative complication. When the abdomen is prepped for surgery, the skin crease above the pubis appears to be very inviting for placement of the skin incision. Dr. Hanson highlights the important option of an extraperitoneal approach to cesarean delivery. I have not thought about using this approach since the mid-1980s. Dr. Hanson’s recommendation that a randomized trial be performed comparing the SSI rate and other outcomes for extraperitoneal and intraperitoneal cesarean delivery is a great idea.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Cameron JL. William Steward Halsted: our surgical heritage. Ann Surg. 1997;225(5):445–458.
- Kaboth G. Die Technik des extraperitonealen Entibindungschnittes. Zentralblatt fur Gynakologie.1934;58(6):310–311.
- Berghella V, Baxter JK Chauhan SP. Evidence-based surgery for cesarean section. Am J Obstet Gynecol. 2005;193(5):1607–1617.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev. 2008; CD004662.
Incision site for cesarean delivery is important in infection prevention
Dr. Barbieri’s editorial very nicely explained strategies to reduce the risk of post–cesarean delivery surgical site infection (SSI). However, what was not mentioned, in my opinion, is the most important preventive strategy. Selecting the site for the initial skin incision plays a great role in whether or not the patient will develop an infection postoperatively.
Pfannenstiel incisions are popular because of their obvious cosmetic benefit. In nonemergent cesarean deliveries, most ObGyns try to use this incision. However, exactly where the incision is placed plays a large role in the genesis of a postoperative wound infection. The worst place for such incisions is in the crease above the pubis and below the panniculus. Invariably, this area remains moist and macerated, especially in obese patients, thus providing a fertile breeding ground for bacteria. This problem can be avoided by incising the skin approximately 2 cm cranial to and parallel to the aforementioned crease, provided that the panniculus is not too large. The point is that the incision should be placed in an area where it has a chance to stay dry.
Sometimes patients who are hugely obese require great creativity in the placement of their transverse skin incision. I recall one patient, pregnant with triplets, whose abdomen was so large that her umbilicus was over the region of the lower uterine segment when she was supine on the operating room table. Some would have lifted up her immense panniculus and placed the incision in the usual crease site. This would be problematic for obtaining adequate exposure to deliver the babies, and the risk of developing an incisional infection would be very high. Therefore, a transverse incision was made just below her umbilicus. The panniculus was a nonissue regarding gaining adequate exposure and, when closed, the incision remained completely dry and uninfected. The patient did extremely well postoperatively and had no infectious sequelae.
David L. Zisow, MD
Baltimore, Maryland
Extraperitoneal approach should be considered
I enjoyed the editorial on reducing surgical site infection, especially the references to the historical Halsted principles of surgery. “He was the first in this country to promulgate the philosophy of ‘safe’ surgery.”1 Regarding surgical principles of cesarean delivery, the pioneering German obstetricians in the 1930s were keenly aware that avoiding the peritoneal cavity was instrumental in reducing morbidity and mortality. They championed the safety of the extraperitoneal approach as the fundamental principle of cesarean delivery for maternal safety.2
I learned to embrace the principles of Kaboth while learning the technique in 1968–1972. Thus, for more than 30 years, I used the extraperitoneal approach to access the lower uterine segment, avoiding entrance into the abdominal cavity. My patients seemed to benefit. As the surgeon, I also benefited: with short operative delivery times, less postoperative pain and minor morbidities, fewer phone calls from nursing staff, and less difficulty for my patients. I had not contaminated the peritoneal cavity and avoided all those inherent problems. The decision to open the peritoneal cavity has not been subjected to the rigors of critical analysis.3 I think that Kaboth’s principles remain worthy of consideration even today.
Contemporary experiences in large populations such as in India and China that use the extraperitoneal cesarean approach seem to implicitly support Kaboth’s principles. However, in the milieu of evidence-based medicine, extraperitoneal cesarean delivery has not been adequately studied.4 Just maybe the extraperitoneal approach should be considered and understood as a primary surgical technique for cesarean deliveries; just maybe it deserves a historical asterisk alongside the Halsted dicta.
Hedric Hanson, MD
Anchorage, Alaska
Dr. Barbieri responds
I thank Drs. Zisow and Hanson for their great recommendations and clinical pearls. I agree with Dr. Zisow that I should have mentioned the importance of optimal placement of the transverse skin incision. Incision in a skin crease that is perpetually moist increases the risk for a postoperative complication. When the abdomen is prepped for surgery, the skin crease above the pubis appears to be very inviting for placement of the skin incision. Dr. Hanson highlights the important option of an extraperitoneal approach to cesarean delivery. I have not thought about using this approach since the mid-1980s. Dr. Hanson’s recommendation that a randomized trial be performed comparing the SSI rate and other outcomes for extraperitoneal and intraperitoneal cesarean delivery is a great idea.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Incision site for cesarean delivery is important in infection prevention
Dr. Barbieri’s editorial very nicely explained strategies to reduce the risk of post–cesarean delivery surgical site infection (SSI). However, what was not mentioned, in my opinion, is the most important preventive strategy. Selecting the site for the initial skin incision plays a great role in whether or not the patient will develop an infection postoperatively.
Pfannenstiel incisions are popular because of their obvious cosmetic benefit. In nonemergent cesarean deliveries, most ObGyns try to use this incision. However, exactly where the incision is placed plays a large role in the genesis of a postoperative wound infection. The worst place for such incisions is in the crease above the pubis and below the panniculus. Invariably, this area remains moist and macerated, especially in obese patients, thus providing a fertile breeding ground for bacteria. This problem can be avoided by incising the skin approximately 2 cm cranial to and parallel to the aforementioned crease, provided that the panniculus is not too large. The point is that the incision should be placed in an area where it has a chance to stay dry.
Sometimes patients who are hugely obese require great creativity in the placement of their transverse skin incision. I recall one patient, pregnant with triplets, whose abdomen was so large that her umbilicus was over the region of the lower uterine segment when she was supine on the operating room table. Some would have lifted up her immense panniculus and placed the incision in the usual crease site. This would be problematic for obtaining adequate exposure to deliver the babies, and the risk of developing an incisional infection would be very high. Therefore, a transverse incision was made just below her umbilicus. The panniculus was a nonissue regarding gaining adequate exposure and, when closed, the incision remained completely dry and uninfected. The patient did extremely well postoperatively and had no infectious sequelae.
David L. Zisow, MD
Baltimore, Maryland
Extraperitoneal approach should be considered
I enjoyed the editorial on reducing surgical site infection, especially the references to the historical Halsted principles of surgery. “He was the first in this country to promulgate the philosophy of ‘safe’ surgery.”1 Regarding surgical principles of cesarean delivery, the pioneering German obstetricians in the 1930s were keenly aware that avoiding the peritoneal cavity was instrumental in reducing morbidity and mortality. They championed the safety of the extraperitoneal approach as the fundamental principle of cesarean delivery for maternal safety.2
I learned to embrace the principles of Kaboth while learning the technique in 1968–1972. Thus, for more than 30 years, I used the extraperitoneal approach to access the lower uterine segment, avoiding entrance into the abdominal cavity. My patients seemed to benefit. As the surgeon, I also benefited: with short operative delivery times, less postoperative pain and minor morbidities, fewer phone calls from nursing staff, and less difficulty for my patients. I had not contaminated the peritoneal cavity and avoided all those inherent problems. The decision to open the peritoneal cavity has not been subjected to the rigors of critical analysis.3 I think that Kaboth’s principles remain worthy of consideration even today.
Contemporary experiences in large populations such as in India and China that use the extraperitoneal cesarean approach seem to implicitly support Kaboth’s principles. However, in the milieu of evidence-based medicine, extraperitoneal cesarean delivery has not been adequately studied.4 Just maybe the extraperitoneal approach should be considered and understood as a primary surgical technique for cesarean deliveries; just maybe it deserves a historical asterisk alongside the Halsted dicta.
Hedric Hanson, MD
Anchorage, Alaska
Dr. Barbieri responds
I thank Drs. Zisow and Hanson for their great recommendations and clinical pearls. I agree with Dr. Zisow that I should have mentioned the importance of optimal placement of the transverse skin incision. Incision in a skin crease that is perpetually moist increases the risk for a postoperative complication. When the abdomen is prepped for surgery, the skin crease above the pubis appears to be very inviting for placement of the skin incision. Dr. Hanson highlights the important option of an extraperitoneal approach to cesarean delivery. I have not thought about using this approach since the mid-1980s. Dr. Hanson’s recommendation that a randomized trial be performed comparing the SSI rate and other outcomes for extraperitoneal and intraperitoneal cesarean delivery is a great idea.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Cameron JL. William Steward Halsted: our surgical heritage. Ann Surg. 1997;225(5):445–458.
- Kaboth G. Die Technik des extraperitonealen Entibindungschnittes. Zentralblatt fur Gynakologie.1934;58(6):310–311.
- Berghella V, Baxter JK Chauhan SP. Evidence-based surgery for cesarean section. Am J Obstet Gynecol. 2005;193(5):1607–1617.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev. 2008; CD004662.
- Cameron JL. William Steward Halsted: our surgical heritage. Ann Surg. 1997;225(5):445–458.
- Kaboth G. Die Technik des extraperitonealen Entibindungschnittes. Zentralblatt fur Gynakologie.1934;58(6):310–311.
- Berghella V, Baxter JK Chauhan SP. Evidence-based surgery for cesarean section. Am J Obstet Gynecol. 2005;193(5):1607–1617.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev. 2008; CD004662.
How more midwives may mean healthier mothers
Since ProPublica launched Lost Mothers, we’ve covered many facets of the U.S. maternal mortality crisis. Despite spending more per capita on health care than any other country, the U.S. has the highest rate of deaths related to pregnancy and childbirth in the industrialized world.
Source: Vox and ProPublica
But what makes maternal health care in other affluent countries look so different than the U.S.? Among other things, midwives. Midwives in the U.S. participate in less than 10 percent of births. But in Sweden, Denmark and France, they lead around three-quarters of deliveries. In Great Britain, they deliver half of all babies, including all three of Kate Middleton’s. So if the midwifery model works for royal babies, why not our own?
Check out the video to find out how midwives have been at the center of a culture war that’s deeply rooted in race and class in America.
Today we see vestiges of that history in states with restrictive midwifery laws and barriers to entry for midwives. Earlier this year, one study was the first systematic look at how and where they practice, offering new evidence that empowering them could significantly boost maternal and infant health. Many of the states with poor health outcomes and hostility to midwives also have large black populations. And with black mothers three to four times more likely to die in pregnancy or childbirth, the study raises the possibility that greater use of midwives could reduce racial disparities in maternal health.
This story makes up the eighth installment in Vox’s collaboration with ProPublica. You can find this video and all of Vox’s videos on YouTube. Subscribe and stay tuned for more from our partnership.
Since ProPublica launched Lost Mothers, we’ve covered many facets of the U.S. maternal mortality crisis. Despite spending more per capita on health care than any other country, the U.S. has the highest rate of deaths related to pregnancy and childbirth in the industrialized world.
Source: Vox and ProPublica
But what makes maternal health care in other affluent countries look so different than the U.S.? Among other things, midwives. Midwives in the U.S. participate in less than 10 percent of births. But in Sweden, Denmark and France, they lead around three-quarters of deliveries. In Great Britain, they deliver half of all babies, including all three of Kate Middleton’s. So if the midwifery model works for royal babies, why not our own?
Check out the video to find out how midwives have been at the center of a culture war that’s deeply rooted in race and class in America.
Today we see vestiges of that history in states with restrictive midwifery laws and barriers to entry for midwives. Earlier this year, one study was the first systematic look at how and where they practice, offering new evidence that empowering them could significantly boost maternal and infant health. Many of the states with poor health outcomes and hostility to midwives also have large black populations. And with black mothers three to four times more likely to die in pregnancy or childbirth, the study raises the possibility that greater use of midwives could reduce racial disparities in maternal health.
This story makes up the eighth installment in Vox’s collaboration with ProPublica. You can find this video and all of Vox’s videos on YouTube. Subscribe and stay tuned for more from our partnership.
Since ProPublica launched Lost Mothers, we’ve covered many facets of the U.S. maternal mortality crisis. Despite spending more per capita on health care than any other country, the U.S. has the highest rate of deaths related to pregnancy and childbirth in the industrialized world.
Source: Vox and ProPublica
But what makes maternal health care in other affluent countries look so different than the U.S.? Among other things, midwives. Midwives in the U.S. participate in less than 10 percent of births. But in Sweden, Denmark and France, they lead around three-quarters of deliveries. In Great Britain, they deliver half of all babies, including all three of Kate Middleton’s. So if the midwifery model works for royal babies, why not our own?
Check out the video to find out how midwives have been at the center of a culture war that’s deeply rooted in race and class in America.
Today we see vestiges of that history in states with restrictive midwifery laws and barriers to entry for midwives. Earlier this year, one study was the first systematic look at how and where they practice, offering new evidence that empowering them could significantly boost maternal and infant health. Many of the states with poor health outcomes and hostility to midwives also have large black populations. And with black mothers three to four times more likely to die in pregnancy or childbirth, the study raises the possibility that greater use of midwives could reduce racial disparities in maternal health.
This story makes up the eighth installment in Vox’s collaboration with ProPublica. You can find this video and all of Vox’s videos on YouTube. Subscribe and stay tuned for more from our partnership.
Product Update: FUJIFILM; Freemie, Preventeza, and C-Panty
NEW VISUALIZATION SYSTEMS FROM FUJIFILM
FUJIFILM New Development, USA, has introduced 2 visualization systems for minimally invasive surgery. Using proprietary technology, the Ultra-Slim Video Laparoscope System (EL-580FN) delivers enhanced image resolution, color fidelity, and display quality, says FUJIFILM. The product features include “Chip on the Tip” high-definition digital imaging processing, less fogging, autoclave sterilization reprocessing, and a low profile, lightweight ergonomic handle. The 3.8-mm-diameter distal end was designed to improve workflow, reduce physician fatigue, and potentially reduce the size of incisions. The accompanying Digital Video Processor System is used for endoscopic procedures with automatic light control, an anti-blur function for motion images, and digital zoom.
FUJIFILM reports that the Full High Definition Surgical Visualization System is designed for a wide variety of surgical applications and offers edge enhancement, automatic gain control, dynamic contrast function, selective color enhancement, smoke reduction, and grid removal features. It includes a portfolio of rigid scopes, cameras, and video processing systems.
FOR MORE INFORMATION, VISIT: http://www.fujifilmusa.com
FREEMIE BREAST MILK COLLECTION SYSTEM
Freemie® offers a hands-free breast-milk collection system with the Freemie Liberty Mobile Hands Free Breast Pump System and Next Generation Freemie Closed System Collection Cups.
The concealable pump has a rechargeable battery and hospital-power suction for single or double pumping. Programmable memory buttons allow the mother to preset or adjust speed and suction functions. Tubing lengths can be changed so that the pump can be placed on a desk, worn with a detachable belt clip, or carried in a bag.
Freemie says the cups are lower-profile and more compact than other pump system cups, and when placed on the breast under the mother’s bra, can be easily removed so that milk can be transferred to storage. Each cup, with a 25 mm or 28 mm funnel and valve, holds 8 oz of milk.
FOR MORE INFORMATION, VISIT: http://www.freemie.com
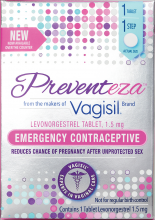
PREVENTEZA: EMERGENCY CONTRACEPTIVE
Combe, Inc, the maker of Vagisil®, has launched Preventeza™ (levonorgestrel tablet, 1.5 mg), an emergency contraceptive for the prevention of pregnancy if unprotected sex or failed birth control occurs.
Available online or over-the-counter as a single tablet, Preventeza is a proven option to help women prevent pregnancy before it starts by using a higher dose of levonorgestrel than most birth control pills. It must be used within 72 hours of unprotected intercourse, and is not intended to be used as regular birth control. Combe says that Preventeza works mainly by stopping the release of an egg from the ovary and may also prevent fertilization of an egg or prevent a fertilized egg from implanting in the uterus. Combe also says that levonorgestrel 1.5 mg will not work if the woman is already pregnant and will not affect an existing pregnancy.
FOR MORE INFORMATION, VISIT: https://www.vagisil.com/products/preventeza-emergency-contraceptive
UPSPRING’S C-PANTY FOR POSTCESAREAN RECOVERY
UpSpring® says that its patented C-Panty® undergarment provides medical-grade compression and speeds recovery after cesarean delivery. C-Panty helps to reduce swelling and discomfort, supports weakened muscles, and reduces the incision bulge without hooks, straps, or Velcro that might irritate the incision area.
C-Panty’s medical-grade silicone panel suppresses the formation of excess or improperly formed collagen, which can contribute to scarring, says UpSpring. The silicone may help reduce itchiness, and can lessen the chance of infection at the incision area. The silicone is durable, washable, and integrated into the panty, eliminating the need for scar gel or scar gel pads.
The C-Panty can be worn immediately after birth and for up to 12 months. If worn when the incision is not healed, the silicone panel should be covered with a panty liner or pad. Once the incision has healed, the covering can be discontinued.
FOR MORE INFORMATION, VISIT: https://www.upspringbaby.com/cpanty
NEW VISUALIZATION SYSTEMS FROM FUJIFILM
FUJIFILM New Development, USA, has introduced 2 visualization systems for minimally invasive surgery. Using proprietary technology, the Ultra-Slim Video Laparoscope System (EL-580FN) delivers enhanced image resolution, color fidelity, and display quality, says FUJIFILM. The product features include “Chip on the Tip” high-definition digital imaging processing, less fogging, autoclave sterilization reprocessing, and a low profile, lightweight ergonomic handle. The 3.8-mm-diameter distal end was designed to improve workflow, reduce physician fatigue, and potentially reduce the size of incisions. The accompanying Digital Video Processor System is used for endoscopic procedures with automatic light control, an anti-blur function for motion images, and digital zoom.
FUJIFILM reports that the Full High Definition Surgical Visualization System is designed for a wide variety of surgical applications and offers edge enhancement, automatic gain control, dynamic contrast function, selective color enhancement, smoke reduction, and grid removal features. It includes a portfolio of rigid scopes, cameras, and video processing systems.
FOR MORE INFORMATION, VISIT: http://www.fujifilmusa.com
FREEMIE BREAST MILK COLLECTION SYSTEM
Freemie® offers a hands-free breast-milk collection system with the Freemie Liberty Mobile Hands Free Breast Pump System and Next Generation Freemie Closed System Collection Cups.
The concealable pump has a rechargeable battery and hospital-power suction for single or double pumping. Programmable memory buttons allow the mother to preset or adjust speed and suction functions. Tubing lengths can be changed so that the pump can be placed on a desk, worn with a detachable belt clip, or carried in a bag.
Freemie says the cups are lower-profile and more compact than other pump system cups, and when placed on the breast under the mother’s bra, can be easily removed so that milk can be transferred to storage. Each cup, with a 25 mm or 28 mm funnel and valve, holds 8 oz of milk.
FOR MORE INFORMATION, VISIT: http://www.freemie.com
PREVENTEZA: EMERGENCY CONTRACEPTIVE
Combe, Inc, the maker of Vagisil®, has launched Preventeza™ (levonorgestrel tablet, 1.5 mg), an emergency contraceptive for the prevention of pregnancy if unprotected sex or failed birth control occurs.
Available online or over-the-counter as a single tablet, Preventeza is a proven option to help women prevent pregnancy before it starts by using a higher dose of levonorgestrel than most birth control pills. It must be used within 72 hours of unprotected intercourse, and is not intended to be used as regular birth control. Combe says that Preventeza works mainly by stopping the release of an egg from the ovary and may also prevent fertilization of an egg or prevent a fertilized egg from implanting in the uterus. Combe also says that levonorgestrel 1.5 mg will not work if the woman is already pregnant and will not affect an existing pregnancy.
FOR MORE INFORMATION, VISIT: https://www.vagisil.com/products/preventeza-emergency-contraceptive
UPSPRING’S C-PANTY FOR POSTCESAREAN RECOVERY
UpSpring® says that its patented C-Panty® undergarment provides medical-grade compression and speeds recovery after cesarean delivery. C-Panty helps to reduce swelling and discomfort, supports weakened muscles, and reduces the incision bulge without hooks, straps, or Velcro that might irritate the incision area.
C-Panty’s medical-grade silicone panel suppresses the formation of excess or improperly formed collagen, which can contribute to scarring, says UpSpring. The silicone may help reduce itchiness, and can lessen the chance of infection at the incision area. The silicone is durable, washable, and integrated into the panty, eliminating the need for scar gel or scar gel pads.
The C-Panty can be worn immediately after birth and for up to 12 months. If worn when the incision is not healed, the silicone panel should be covered with a panty liner or pad. Once the incision has healed, the covering can be discontinued.
FOR MORE INFORMATION, VISIT: https://www.upspringbaby.com/cpanty
NEW VISUALIZATION SYSTEMS FROM FUJIFILM
FUJIFILM New Development, USA, has introduced 2 visualization systems for minimally invasive surgery. Using proprietary technology, the Ultra-Slim Video Laparoscope System (EL-580FN) delivers enhanced image resolution, color fidelity, and display quality, says FUJIFILM. The product features include “Chip on the Tip” high-definition digital imaging processing, less fogging, autoclave sterilization reprocessing, and a low profile, lightweight ergonomic handle. The 3.8-mm-diameter distal end was designed to improve workflow, reduce physician fatigue, and potentially reduce the size of incisions. The accompanying Digital Video Processor System is used for endoscopic procedures with automatic light control, an anti-blur function for motion images, and digital zoom.
FUJIFILM reports that the Full High Definition Surgical Visualization System is designed for a wide variety of surgical applications and offers edge enhancement, automatic gain control, dynamic contrast function, selective color enhancement, smoke reduction, and grid removal features. It includes a portfolio of rigid scopes, cameras, and video processing systems.
FOR MORE INFORMATION, VISIT: http://www.fujifilmusa.com
FREEMIE BREAST MILK COLLECTION SYSTEM
Freemie® offers a hands-free breast-milk collection system with the Freemie Liberty Mobile Hands Free Breast Pump System and Next Generation Freemie Closed System Collection Cups.
The concealable pump has a rechargeable battery and hospital-power suction for single or double pumping. Programmable memory buttons allow the mother to preset or adjust speed and suction functions. Tubing lengths can be changed so that the pump can be placed on a desk, worn with a detachable belt clip, or carried in a bag.
Freemie says the cups are lower-profile and more compact than other pump system cups, and when placed on the breast under the mother’s bra, can be easily removed so that milk can be transferred to storage. Each cup, with a 25 mm or 28 mm funnel and valve, holds 8 oz of milk.
FOR MORE INFORMATION, VISIT: http://www.freemie.com
PREVENTEZA: EMERGENCY CONTRACEPTIVE
Combe, Inc, the maker of Vagisil®, has launched Preventeza™ (levonorgestrel tablet, 1.5 mg), an emergency contraceptive for the prevention of pregnancy if unprotected sex or failed birth control occurs.
Available online or over-the-counter as a single tablet, Preventeza is a proven option to help women prevent pregnancy before it starts by using a higher dose of levonorgestrel than most birth control pills. It must be used within 72 hours of unprotected intercourse, and is not intended to be used as regular birth control. Combe says that Preventeza works mainly by stopping the release of an egg from the ovary and may also prevent fertilization of an egg or prevent a fertilized egg from implanting in the uterus. Combe also says that levonorgestrel 1.5 mg will not work if the woman is already pregnant and will not affect an existing pregnancy.
FOR MORE INFORMATION, VISIT: https://www.vagisil.com/products/preventeza-emergency-contraceptive
UPSPRING’S C-PANTY FOR POSTCESAREAN RECOVERY
UpSpring® says that its patented C-Panty® undergarment provides medical-grade compression and speeds recovery after cesarean delivery. C-Panty helps to reduce swelling and discomfort, supports weakened muscles, and reduces the incision bulge without hooks, straps, or Velcro that might irritate the incision area.
C-Panty’s medical-grade silicone panel suppresses the formation of excess or improperly formed collagen, which can contribute to scarring, says UpSpring. The silicone may help reduce itchiness, and can lessen the chance of infection at the incision area. The silicone is durable, washable, and integrated into the panty, eliminating the need for scar gel or scar gel pads.
The C-Panty can be worn immediately after birth and for up to 12 months. If worn when the incision is not healed, the silicone panel should be covered with a panty liner or pad. Once the incision has healed, the covering can be discontinued.
FOR MORE INFORMATION, VISIT: https://www.upspringbaby.com/cpanty
GDM, subsequent diabetes predictive of later renal damage
Women with a history of gestational diabetes mellitus who later develop diabetes had an elevated urinary albumin-to-creatinine ratio an average of 13 years later, indicating renal damage, according to a new study.
Those with a history of gestational diabetes mellitus (GDM) – but no subsequent development of diabetes – did not show an increased urinary albumin-to-creatinine ratio (UACR) but did have a higher estimated glomerular filtration rate (eGFR), hinting at early stages of glomerular hyperfiltration and renal damage.
“Our findings suggest that in women with a history of GDM, deterioration of renal function may potentially precede the development of overt diabetes, although clinically relevant outcomes such as elevated UACR may manifest only after progression to diabetes,” wrote Shristi Rawal, PhD, a postdoctoral fellow at the National Institute of Child Health and Human Development and her associates.
“These findings suggest that women with GDM-complicated pregnancies may represent a high-risk group that could benefit from regular monitoring for early-stage renal damage, timely detection of which may help clinicians initiate treatment to prevent or delay further disease progression,” they wrote.
The investigators compared outcomes among 1,226 Danish women 9-16 years after their index pregnancy during 1996-2002; a predominantly white study population, which limited the study’s generalizability to other demographic groups, the authors acknowledged. A total of 607 women had had GDM during their first pregnancy, 183 of whom developed type 1 or 2 diabetes. Of the 619 women who did not have GDM, 9 developed diabetes.
Serum creatinine and urinary albumin and creatinine measurements were taken to determine eGFR and UACR. Women with a previous GDM diagnosis had higher eGFR and UACR than women without previous GDM. The higher eGFR remained significant after adjustments for age at first pregnancy, completion of high school, smoking during pregnancy, a family history of diabetes, prepregnancy hypertension, and prepregnancy body mass index (BMI). UACR differences were not significant after adjustment.
Women with GDM and subsequent diabetes had a significantly higher UACR than women without either and had more than twice the risk of an elevated UACR of at least 20 mg/g (adjusted relative risk, 2.3), even after confounder adjustment.
The association with increased UACR was significant with the combination of a GDM history and a subsequent diabetes diagnosis, but not individually. The increased eGFR, however, remained significant after adjustment even for women with only a history of GDM, regardless of whether they later developed diabetes or even prediabetes.
“The independent association of GDM with eGFR also remained significant when we excluded women with conditions that might influence renal function markers at follow-up, including type 1 diabetes, preeclampsia/eclampsia or any hypertension complication during the index pregnancy, regular use of cholesterol-lowering drugs, or recent use of ACE inhibitors, diuretics, or H2 blockers,” the authors reported.
“Furthermore, no effect modification was observed when we stratified the analyses by clinical and lifestyle characteristics at follow-up, including current BMI, smoking, antihypertension medication use, family history of diabetes, physical activity, and median time since index pregnancy. Associations in some strata became statistically insignificant due to reduced sample size [all P for interaction = .05],” they wrote.
The research was funded by the National Institute of Child Health and Human Development at the National Institutes of Health, the Innovation Fund Denmark, March of Dimes Birth Defects Foundation, Health Foundation, Heart Foundation and European Union.
Coauthor Allan Vaag, MD, PhD is a vice president at AstraZeneca. No other authors had disclosures.
SOURCE: Rawal S et al. Diabetes Care. 2018 May 4. doi: 10.2337/dc17-2629.
Women with a history of gestational diabetes mellitus who later develop diabetes had an elevated urinary albumin-to-creatinine ratio an average of 13 years later, indicating renal damage, according to a new study.
Those with a history of gestational diabetes mellitus (GDM) – but no subsequent development of diabetes – did not show an increased urinary albumin-to-creatinine ratio (UACR) but did have a higher estimated glomerular filtration rate (eGFR), hinting at early stages of glomerular hyperfiltration and renal damage.
“Our findings suggest that in women with a history of GDM, deterioration of renal function may potentially precede the development of overt diabetes, although clinically relevant outcomes such as elevated UACR may manifest only after progression to diabetes,” wrote Shristi Rawal, PhD, a postdoctoral fellow at the National Institute of Child Health and Human Development and her associates.
“These findings suggest that women with GDM-complicated pregnancies may represent a high-risk group that could benefit from regular monitoring for early-stage renal damage, timely detection of which may help clinicians initiate treatment to prevent or delay further disease progression,” they wrote.
The investigators compared outcomes among 1,226 Danish women 9-16 years after their index pregnancy during 1996-2002; a predominantly white study population, which limited the study’s generalizability to other demographic groups, the authors acknowledged. A total of 607 women had had GDM during their first pregnancy, 183 of whom developed type 1 or 2 diabetes. Of the 619 women who did not have GDM, 9 developed diabetes.
Serum creatinine and urinary albumin and creatinine measurements were taken to determine eGFR and UACR. Women with a previous GDM diagnosis had higher eGFR and UACR than women without previous GDM. The higher eGFR remained significant after adjustments for age at first pregnancy, completion of high school, smoking during pregnancy, a family history of diabetes, prepregnancy hypertension, and prepregnancy body mass index (BMI). UACR differences were not significant after adjustment.
Women with GDM and subsequent diabetes had a significantly higher UACR than women without either and had more than twice the risk of an elevated UACR of at least 20 mg/g (adjusted relative risk, 2.3), even after confounder adjustment.
The association with increased UACR was significant with the combination of a GDM history and a subsequent diabetes diagnosis, but not individually. The increased eGFR, however, remained significant after adjustment even for women with only a history of GDM, regardless of whether they later developed diabetes or even prediabetes.
“The independent association of GDM with eGFR also remained significant when we excluded women with conditions that might influence renal function markers at follow-up, including type 1 diabetes, preeclampsia/eclampsia or any hypertension complication during the index pregnancy, regular use of cholesterol-lowering drugs, or recent use of ACE inhibitors, diuretics, or H2 blockers,” the authors reported.
“Furthermore, no effect modification was observed when we stratified the analyses by clinical and lifestyle characteristics at follow-up, including current BMI, smoking, antihypertension medication use, family history of diabetes, physical activity, and median time since index pregnancy. Associations in some strata became statistically insignificant due to reduced sample size [all P for interaction = .05],” they wrote.
The research was funded by the National Institute of Child Health and Human Development at the National Institutes of Health, the Innovation Fund Denmark, March of Dimes Birth Defects Foundation, Health Foundation, Heart Foundation and European Union.
Coauthor Allan Vaag, MD, PhD is a vice president at AstraZeneca. No other authors had disclosures.
SOURCE: Rawal S et al. Diabetes Care. 2018 May 4. doi: 10.2337/dc17-2629.
Women with a history of gestational diabetes mellitus who later develop diabetes had an elevated urinary albumin-to-creatinine ratio an average of 13 years later, indicating renal damage, according to a new study.
Those with a history of gestational diabetes mellitus (GDM) – but no subsequent development of diabetes – did not show an increased urinary albumin-to-creatinine ratio (UACR) but did have a higher estimated glomerular filtration rate (eGFR), hinting at early stages of glomerular hyperfiltration and renal damage.
“Our findings suggest that in women with a history of GDM, deterioration of renal function may potentially precede the development of overt diabetes, although clinically relevant outcomes such as elevated UACR may manifest only after progression to diabetes,” wrote Shristi Rawal, PhD, a postdoctoral fellow at the National Institute of Child Health and Human Development and her associates.
“These findings suggest that women with GDM-complicated pregnancies may represent a high-risk group that could benefit from regular monitoring for early-stage renal damage, timely detection of which may help clinicians initiate treatment to prevent or delay further disease progression,” they wrote.
The investigators compared outcomes among 1,226 Danish women 9-16 years after their index pregnancy during 1996-2002; a predominantly white study population, which limited the study’s generalizability to other demographic groups, the authors acknowledged. A total of 607 women had had GDM during their first pregnancy, 183 of whom developed type 1 or 2 diabetes. Of the 619 women who did not have GDM, 9 developed diabetes.
Serum creatinine and urinary albumin and creatinine measurements were taken to determine eGFR and UACR. Women with a previous GDM diagnosis had higher eGFR and UACR than women without previous GDM. The higher eGFR remained significant after adjustments for age at first pregnancy, completion of high school, smoking during pregnancy, a family history of diabetes, prepregnancy hypertension, and prepregnancy body mass index (BMI). UACR differences were not significant after adjustment.
Women with GDM and subsequent diabetes had a significantly higher UACR than women without either and had more than twice the risk of an elevated UACR of at least 20 mg/g (adjusted relative risk, 2.3), even after confounder adjustment.
The association with increased UACR was significant with the combination of a GDM history and a subsequent diabetes diagnosis, but not individually. The increased eGFR, however, remained significant after adjustment even for women with only a history of GDM, regardless of whether they later developed diabetes or even prediabetes.
“The independent association of GDM with eGFR also remained significant when we excluded women with conditions that might influence renal function markers at follow-up, including type 1 diabetes, preeclampsia/eclampsia or any hypertension complication during the index pregnancy, regular use of cholesterol-lowering drugs, or recent use of ACE inhibitors, diuretics, or H2 blockers,” the authors reported.
“Furthermore, no effect modification was observed when we stratified the analyses by clinical and lifestyle characteristics at follow-up, including current BMI, smoking, antihypertension medication use, family history of diabetes, physical activity, and median time since index pregnancy. Associations in some strata became statistically insignificant due to reduced sample size [all P for interaction = .05],” they wrote.
The research was funded by the National Institute of Child Health and Human Development at the National Institutes of Health, the Innovation Fund Denmark, March of Dimes Birth Defects Foundation, Health Foundation, Heart Foundation and European Union.
Coauthor Allan Vaag, MD, PhD is a vice president at AstraZeneca. No other authors had disclosures.
SOURCE: Rawal S et al. Diabetes Care. 2018 May 4. doi: 10.2337/dc17-2629.
FROM DIABETES CARE
Key clinical point: Gestational diabetes mellitus may be a risk factor for future development of renal damage.
Major finding: Women with previous GDM and a subsequent diagnosis of diabetes were over twice as likely to show evidence of existing renal damage.
Data source: The findings are based on 9-16 years of prospective follow-up of 607 women with and 619 women without a history of GDM.
Disclosures: The research was funded by the National Institute of Child Health and Human Development at the National Institutes of Health, the Innovation Fund Denmark, March of Dimes Birth Defects Foundation, Health Foundation, Heart Foundation and European Union. Coauthor Allan Vaag is an employee of AstraZeneca. No other authors had disclosures.
Source: Rawal S et al. Diabetes Care. 2018 May 4. doi: 10.2337/dc17-2629.
The FDA’s novel drugs approved in 2017
Novel drugs are innovative new products that have never before been used in clinical practice. Among the 46 that the Food and Drug Administration approved in 2017, 45 could be used in pregnancy. One, cerliponase alfa (Brineura), is indicated for pediatric patients 3 years of age or older, for treatment of late infantile neuronal ceroid lipofuscinosis type 2. It is doubtful that this drug would be used in pregnancy or during breastfeeding.
With the two exceptions noted below, there are no human pregnancy data for these drugs. It is important to consider that although high molecular weight (MW) drugs (for example, greater than 1,000) probably do not usually cross the placenta in the first half of pregnancy, they may do so in late pregnancy. The cited MWs are shown as the nearest whole number. Animal reproductive data are also cited because, although not definitive, they can provide some measure of the human embryo-fetal risk.
Anti-infectives
Benznidazole (same trade name) (MW 441), given orally, is indicated for pediatric patients aged 2-12 years for treatment of Chagas disease (American trypanosomiasis) caused by Trypanosoma cruzi. However, there are international reports describing its use in pregnancy and breastfeeding. No fetal harm from these exposures were noted. Nevertheless, because of the low MW and the reported animal risk, avoiding the drug during the first half of pregnancy appears to be the best choice. Delafloxacin (Baxdela) (MW 441), a fluoroquinolone antimicrobial given intravenously or orally, is indicated for acute bacterial skin infections. The animal data suggest low risk. However, like other fluoroquinolones, it is contraindicated in pregnancy and should be used only if there are no other alternatives.
Sofosbuvir/velpatasvir /voxilaprevir (Vosevi) (MWs 529, 883, 869), a fixed oral dose combination of three antivirals, is indicated for the treatment of hepatitis C virus infection. The MWs suggest that all three will cross the human placenta. The animal data suggest low risk. Secnidazole (Solosec) (MW 185), given orally, is indicated for the treatment of bacterial vaginosis. It is closely related to metronidazole. No evidence of embryo-fetal toxicity was observed in rats and rabbits, suggesting that the human risk is low. In a report from Brazil, 134 pregnant women with bacterial vaginosis were treated with secnidazole, metronidazole, or tinidazole in the second and third trimesters. Treatment significantly decreased the incidence of premature rupture of membranes, preterm labor, preterm birth, and low birth weight. No fetal harm was reported.
Antineoplastics
[Note: All of the drugs in this category are best avoided, if possible, in pregnancy and breastfeeding.]
Abemaciclib (Verzenio) (MW 507), an oral inhibitor of cyclin-dependent kinases, is indicated for the treatment of breast cancer. The drug is teratogenic in rats. Acalabrutinib (Calquence) (MW 466) is an oral kinase inhibitor indicated for mantle cell lymphoma. The drug had no effect on the rat embryo-fetus but caused decreased fetal body weights and delayed skeletal ossification in rabbits. Avelumab (Bavencio) (MW 147,000) is given intravenously for the treatment of metastatic Merkel cell carcinoma and metastatic urothelial carcinoma. Animal reproduction studies have not been conducted. However, based on its mechanism of action, fetal exposure may increase the risk of developing immune-related disorders or altering the normal immune response.
Brigatinib (Alunbrig) (MW 584) is given orally for the treatment of metastatic non–small-cell lung cancer. In rats, doses less than or slightly above the human exposure caused multiple anomalies in the fetuses of pregnant rats. Copanlisib (Aliqopa) (MW 553) is a kinase inhibitor that is given intravenously for relapsed follicular lymphoma. In rats during organogenesis, doses based on body surface area that were a fraction of the human dose caused embryo-fetal death and fetal defects. Durvalumab (Imfinzi) (MW 146,000), given intravenously, is indicated for the treatment of metastatic urothelial carcinoma and non–small-cell lung cancer. Monkeys given the drug from organogenesis through delivery experienced increased premature birth, fetal loss, and premature neonatal death. Women of reproductive potential should use effective contraception during treatment and for at least 3 months after the last dose.
Enasidenib (Idhifa) (MW 569), given orally, is indicated for the treatment of myeloid leukemia. The drug caused maternal toxicity and adverse embryo-fetal effects (postimplantation loss, resorptions, decrease viable fetuses, lower fetal birth weights, and skeletal variations) in rats and spontaneous abortions in rabbits. Inotuzumab ozogamicin (Besponsa) (MW 160,000), given intravenously, is indicated for relapsed or refractory B-cell precursor acute lymphoblastic leukemia. The drug caused fetal harm in rats but not in rabbits. Midostaurin (Rydapt) (MW 571) is an oral kinase inhibitor indicated for myeloid leukemia. In rats, a dose given during the first week of pregnancy that was a small fraction of the human exposure caused pre- and postimplantation loss. When very small doses were given during organogenesis to rats and rabbits there was significant maternal and fetal toxicity.
Neratinib (Nerlynx) (MW 673) is an oral kinase inhibitor for breast cancer. Although the drug did not cause embryo-fetal toxicity in rats, it did cause this toxicity in rabbits. Doses that resulted in exposures that were less than the human exposure caused maternal toxicity, abortions, and embryo-fetal death. Lower doses caused multiple fetal anomalies. Niraparib (Zejula) (MW 511) is indicated for treatment of epithelial ovarian, fallopian, or peritoneal cancer. Because of the potential human embryo-fetal risk based on its mechanism of action, pregnant animal studies were not conducted. Women with reproductive potential should use effective contraception during treatment and for 6 months after the last dose. Ribociclib (Kisqali) (MW 553) is an oral kinase inhibitor indicated for postmenopausal women with breast cancer. In rats, the drug cause reduced fetal weights and skeletal changes. Increased incidences of fetal abnormalities and lower fetal weights were observed in rabbits.
Cardiovascular
Angiotensin II (Giapreza) (MW 1,046) is a naturally occurring peptide hormone given as an intravenous infusion. It is indicated as a vasoconstrictor to increase blood pressure in adults with septic or other distributive shock. Animal reproduction studies have not been conducted. Because septic or other distributive shock is a medical emergency that can be fatal, the use of this agent in pregnancy should not be withheld.
Central nervous system
Deutetrabenazine (Austedo) (MW 324) is an oral drug indicated for the treatment of chorea associated with Huntington’s disease and for tardive dyskinesia. When given to rats during organogenesis there was no clear effect on embryo-fetal development.
Edaravone (Radicava) (MW 174), given as an intravenous infusion, is indicated for the treatment of amyotrophic lateral sclerosis. Doses that were not maternal toxic did not cause embryo-fetal toxicity in rats and rabbits. However, the no-effect dose for developmental toxicity was less than the recommended human dose. Naldemedine (Symproic) (MW 743) is an opioid antagonist indicated for the treatment of opioid-induced constipation. The drug crosses the human placenta and may precipitate opioid withdrawal in the fetus. The drug caused no embryo-fetal adverse effects, even at high doses, in pregnant rats and rabbits.
Ocrelizumab (Ocrevus) (MW 145,000), an intravenous agent, is used to treat patients with multiple sclerosis. The MW is high but immunoglobulins are known to cross the placenta. When given to monkeys at doses similar to or greater than the human dose, there was increased perinatal mortality, depletion of B-cell populations, and renal, bone marrow, and testicular toxicity in the offspring in the absence of maternal toxicity. Safinamide (Xadago) (MW 399) is an oral drug indicated as adjunctive treatment to levodopa/carbidopa in Parkinson’s disease. In rats, the drug was teratogenic (mainly urogenital defects) at all doses. When it was combined with levodopa/carbidopa or used alone, increased rates of fetal visceral and skeletal defects occurred at all doses studied. In rabbits, given the combination throughout organogenesis, there was an increased incidence of embryo-fetal death and cardiac and skeletal defects. Based on these data, avoiding the drug in pregnancy appears to be the best course.
Valbenazine (Ingrezza) (MW 419) is indicated for the treatment of tardive dyskinesia. The drug caused no malformations in rats and rabbits. However, in rats given the drug during organogenesis through lactation, an increase in the number of stillborn pups and postnatal pup mortalities was observed.
Dermatologic
Brodalumab (Siliq) (MW 144,000), given subcutaneously, is indicated for the treatment of moderate to severe plaque psoriasis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In monkeys, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from mothers given weekly subcutaneous doses of the drug. Dupilumab (Dupixent) (MW 144,000) is given subcutaneously for the treatment of atopic dermatitis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In pregnant monkeys given subcutaneous doses of the drug, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from birth to 6 months of age.
Guselkumab (Tremfya) (MW 143,600) is given subcutaneously for the treatment of moderate to severe plaque psoriasis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In pregnant monkeys given subcutaneous doses of the drug, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from birth to 6 months of age. However, neonatal deaths were observed in three monkeys given six times the maximum recommended human dose.
Endocrine/metabolic
Deflazacort (Emflaza) (MW 442) is an oral corticosteroid prodrug indicated for the treatment of Duchenne muscular dystrophy. The drug is converted in vivo to an active metabolite. The drug readily crosses the placenta. Although animal reproduction studies have not been conducted, such studies with other corticosteroids in various animal species have shown an increased incidence of cleft palate. In some species, there was an increase in embryo-fetal death, intrauterine growth restriction, and constriction of the ductus arteriosus.
Ertugliflozin (Steglatro) (MW 566) is an oral drug indicated to improve glycemic control in adults with type 2 diabetes mellitus. In juvenile rats, doses that were about 13 times the human dose caused increased kidney weight, renal tubule and renal pelvis dilatation, and renal mineralization. These effects occurred during periods of rat renal development that correspond to the late second and third trimester of human renal development, and did not fully reverse within a 1-month recovery period. Etelcalcetide (Parsabiv) (MW 1,048), an intravenous calcium-sensing receptor agonist, is indicated for patients on hemodialysis who have secondary hyperparathyroidism. In rats and rabbits given the drug during organogenesis, there was reduced fetal growth. In rats given the drug during organogenesis through birth and weaning, there was a slight increase in pup mortality, delay in parturition, and transient effects on pup growth, but there were no effects on sexual maturation, neurobehavioral, or reproductive function. Macimorelin (Macrilen) (MW 535) is an oral growth hormone secretagogue receptor agonist. It is indicated for adult growth hormone deficiency. Animal reproduction studies have not been conducted.
Semaglutide (Ozempic) (MW 4,114), given subcutaneously, is a glucagon-like peptide indicated to improve glycemic control in type 2 diabetes mellitus. In rats given the drug during organogenesis, embryo-fetal death, structural defects, and alterations in growth were observed. In rabbits and monkeys given the drug during organogenesis, there were early pregnancy losses and structural abnormalities. In addition, there was marked maternal body weight loss in both animal species. Vestronidase alfa-vjbk (Mepsevii) is given intravenously. It is indicated for the treatment of Mucopolysaccharidosis VII (Sly syndrome). The calculated average MW of each nonglycosylated peptide chain is 72,562. In rats and rabbits given the drug during organogenesis, there was no maternal toxicity or adverse developmental outcomes.
Gastrointestinal
Plecanatide (Trulance) (MW 1,682) is an oral drug indicated for the treatment of constipation. The drug and its active metabolite are negligibly absorbed systemically and fetal exposure to the drug is not expected. In mice and rabbits given the oral drug during organogenesis, no effects on embryo-fetal development were observed. Telotristat ethyl (Xermelo) (MW 754) is an oral drug indicated for the treatment of carcinoid syndrome diarrhea in combination with somatostatin analog (MW not specified) therapy in adults not controlled by somatostatin analog. When given during organogenesis in rats, there was no effect on embryo-fetal development at doses that were about nine times the recommended human dose. However, an increased incidence of mortality in rat offspring was observed when the drug was given from organogenesis through lactation. During organogenesis in rabbits, the drug had no embryo-fetal effects at doses that were 10 or more times the human dose.
Hematologics
Betrixaban (Bevyxxa) (MW 568) is an oral factor Xa inhibitor indicated for the prophylaxis of venous thromboembolism. The drug was not associated with adverse developmental fetal outcomes in rats and rabbits. However, maternal hemorrhage did occur. In humans, there is an increased risk of hemorrhage during pregnancy and delivery. Emicizumab (Hemlibra) (MW 145,600), given subcutaneously, is indicated for routine prophylaxis to prevent or reduce the frequency of bleeding in patients with hemophilia A with factor VIII inhibitors. Animal reproduction studies have not been conducted. It is a human monoclonal IgG antibody and, though the MW is high, IgG antibodies are known to cross the placenta.
Immunologic
Sarilumab (Kevzara) (MW 150,000) is given subcutaneously. It is indicated for patients with moderate to severe rheumatoid arthritis. Reproduction studies were conducted in pregnant monkeys. There was no evidence of embryo toxicity or fetal malformations. Based on this data, the human pregnancy risk is low.
Ophthalmic
Latanoprostene bunod (Vyzulta) (MW 508) is a prostaglandin analog that is indicated to reduce intraocular pressure. No quantifiable plasma concentrations of latanoprostene bunod were detected in nonpregnant patients. However, very low levels of latanoprost acid (51-59 pg/mL), the active metabolite, were detected with the maximal plasma concentration occurring 5 minutes after administration. When given intravenously to pregnant rabbits, the drug was shown to be abortifacient and teratogenic, but these effects were not observed in pregnant rats. Netarsudil (Rhopressa) (MW 454) is a kinase inhibitor indicated to reduce intraocular pressure in patients with open-angle glaucoma or ocular hypertension. No quantifiable plasma concentrations of netarsudil were detected in 18 subjects. For the active metabolite, a plasma level of 0.11 ng/mL was found in one subject. Intravenous doses to pregnant rats and rabbits during organogenesis did not cause embryo-fetal adverse effects at clinically relevant systemic exposures.
Parathyroid hormone
Abaloparatide (Tymlos) (MW 3,961), given subcutaneously, is a human parathyroid hormone related peptide analog that is indicated for postmenopausal women with osteoporosis at high risk for fracture. Reproduction studies in animals have not been conducted. Because of the indication, it is doubtful if the agent will be used in pregnancy or during breastfeeding.
Respiratory
Benralizumab (Fasenra) (MW 150,000), given subcutaneously, is indicated for the add-on maintenance treatment of severe eosinophilic asthma. It is a human monoclonal IgG antibody and, though the MW is high, IgG antibodies are known to cross the placenta. Studies in monkeys found no evidence of fetal harm with intravenous doses throughout pregnancy that produced exposures up to about 310 times the exposure at the maximum recommended human dose.
The potential adverse effects in an infant when the mother is taking one of the above drugs while breastfeeding will be covered in my next column.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. He coauthored “Drugs in Pregnancy and Lactation” and coedited “Diseases, Complications, and Drug Therapy in Obstetrics.” He reported having no relevant financial disclosures.
Novel drugs are innovative new products that have never before been used in clinical practice. Among the 46 that the Food and Drug Administration approved in 2017, 45 could be used in pregnancy. One, cerliponase alfa (Brineura), is indicated for pediatric patients 3 years of age or older, for treatment of late infantile neuronal ceroid lipofuscinosis type 2. It is doubtful that this drug would be used in pregnancy or during breastfeeding.
With the two exceptions noted below, there are no human pregnancy data for these drugs. It is important to consider that although high molecular weight (MW) drugs (for example, greater than 1,000) probably do not usually cross the placenta in the first half of pregnancy, they may do so in late pregnancy. The cited MWs are shown as the nearest whole number. Animal reproductive data are also cited because, although not definitive, they can provide some measure of the human embryo-fetal risk.
Anti-infectives
Benznidazole (same trade name) (MW 441), given orally, is indicated for pediatric patients aged 2-12 years for treatment of Chagas disease (American trypanosomiasis) caused by Trypanosoma cruzi. However, there are international reports describing its use in pregnancy and breastfeeding. No fetal harm from these exposures were noted. Nevertheless, because of the low MW and the reported animal risk, avoiding the drug during the first half of pregnancy appears to be the best choice. Delafloxacin (Baxdela) (MW 441), a fluoroquinolone antimicrobial given intravenously or orally, is indicated for acute bacterial skin infections. The animal data suggest low risk. However, like other fluoroquinolones, it is contraindicated in pregnancy and should be used only if there are no other alternatives.
Sofosbuvir/velpatasvir /voxilaprevir (Vosevi) (MWs 529, 883, 869), a fixed oral dose combination of three antivirals, is indicated for the treatment of hepatitis C virus infection. The MWs suggest that all three will cross the human placenta. The animal data suggest low risk. Secnidazole (Solosec) (MW 185), given orally, is indicated for the treatment of bacterial vaginosis. It is closely related to metronidazole. No evidence of embryo-fetal toxicity was observed in rats and rabbits, suggesting that the human risk is low. In a report from Brazil, 134 pregnant women with bacterial vaginosis were treated with secnidazole, metronidazole, or tinidazole in the second and third trimesters. Treatment significantly decreased the incidence of premature rupture of membranes, preterm labor, preterm birth, and low birth weight. No fetal harm was reported.
Antineoplastics
[Note: All of the drugs in this category are best avoided, if possible, in pregnancy and breastfeeding.]
Abemaciclib (Verzenio) (MW 507), an oral inhibitor of cyclin-dependent kinases, is indicated for the treatment of breast cancer. The drug is teratogenic in rats. Acalabrutinib (Calquence) (MW 466) is an oral kinase inhibitor indicated for mantle cell lymphoma. The drug had no effect on the rat embryo-fetus but caused decreased fetal body weights and delayed skeletal ossification in rabbits. Avelumab (Bavencio) (MW 147,000) is given intravenously for the treatment of metastatic Merkel cell carcinoma and metastatic urothelial carcinoma. Animal reproduction studies have not been conducted. However, based on its mechanism of action, fetal exposure may increase the risk of developing immune-related disorders or altering the normal immune response.
Brigatinib (Alunbrig) (MW 584) is given orally for the treatment of metastatic non–small-cell lung cancer. In rats, doses less than or slightly above the human exposure caused multiple anomalies in the fetuses of pregnant rats. Copanlisib (Aliqopa) (MW 553) is a kinase inhibitor that is given intravenously for relapsed follicular lymphoma. In rats during organogenesis, doses based on body surface area that were a fraction of the human dose caused embryo-fetal death and fetal defects. Durvalumab (Imfinzi) (MW 146,000), given intravenously, is indicated for the treatment of metastatic urothelial carcinoma and non–small-cell lung cancer. Monkeys given the drug from organogenesis through delivery experienced increased premature birth, fetal loss, and premature neonatal death. Women of reproductive potential should use effective contraception during treatment and for at least 3 months after the last dose.
Enasidenib (Idhifa) (MW 569), given orally, is indicated for the treatment of myeloid leukemia. The drug caused maternal toxicity and adverse embryo-fetal effects (postimplantation loss, resorptions, decrease viable fetuses, lower fetal birth weights, and skeletal variations) in rats and spontaneous abortions in rabbits. Inotuzumab ozogamicin (Besponsa) (MW 160,000), given intravenously, is indicated for relapsed or refractory B-cell precursor acute lymphoblastic leukemia. The drug caused fetal harm in rats but not in rabbits. Midostaurin (Rydapt) (MW 571) is an oral kinase inhibitor indicated for myeloid leukemia. In rats, a dose given during the first week of pregnancy that was a small fraction of the human exposure caused pre- and postimplantation loss. When very small doses were given during organogenesis to rats and rabbits there was significant maternal and fetal toxicity.
Neratinib (Nerlynx) (MW 673) is an oral kinase inhibitor for breast cancer. Although the drug did not cause embryo-fetal toxicity in rats, it did cause this toxicity in rabbits. Doses that resulted in exposures that were less than the human exposure caused maternal toxicity, abortions, and embryo-fetal death. Lower doses caused multiple fetal anomalies. Niraparib (Zejula) (MW 511) is indicated for treatment of epithelial ovarian, fallopian, or peritoneal cancer. Because of the potential human embryo-fetal risk based on its mechanism of action, pregnant animal studies were not conducted. Women with reproductive potential should use effective contraception during treatment and for 6 months after the last dose. Ribociclib (Kisqali) (MW 553) is an oral kinase inhibitor indicated for postmenopausal women with breast cancer. In rats, the drug cause reduced fetal weights and skeletal changes. Increased incidences of fetal abnormalities and lower fetal weights were observed in rabbits.
Cardiovascular
Angiotensin II (Giapreza) (MW 1,046) is a naturally occurring peptide hormone given as an intravenous infusion. It is indicated as a vasoconstrictor to increase blood pressure in adults with septic or other distributive shock. Animal reproduction studies have not been conducted. Because septic or other distributive shock is a medical emergency that can be fatal, the use of this agent in pregnancy should not be withheld.
Central nervous system
Deutetrabenazine (Austedo) (MW 324) is an oral drug indicated for the treatment of chorea associated with Huntington’s disease and for tardive dyskinesia. When given to rats during organogenesis there was no clear effect on embryo-fetal development.
Edaravone (Radicava) (MW 174), given as an intravenous infusion, is indicated for the treatment of amyotrophic lateral sclerosis. Doses that were not maternal toxic did not cause embryo-fetal toxicity in rats and rabbits. However, the no-effect dose for developmental toxicity was less than the recommended human dose. Naldemedine (Symproic) (MW 743) is an opioid antagonist indicated for the treatment of opioid-induced constipation. The drug crosses the human placenta and may precipitate opioid withdrawal in the fetus. The drug caused no embryo-fetal adverse effects, even at high doses, in pregnant rats and rabbits.
Ocrelizumab (Ocrevus) (MW 145,000), an intravenous agent, is used to treat patients with multiple sclerosis. The MW is high but immunoglobulins are known to cross the placenta. When given to monkeys at doses similar to or greater than the human dose, there was increased perinatal mortality, depletion of B-cell populations, and renal, bone marrow, and testicular toxicity in the offspring in the absence of maternal toxicity. Safinamide (Xadago) (MW 399) is an oral drug indicated as adjunctive treatment to levodopa/carbidopa in Parkinson’s disease. In rats, the drug was teratogenic (mainly urogenital defects) at all doses. When it was combined with levodopa/carbidopa or used alone, increased rates of fetal visceral and skeletal defects occurred at all doses studied. In rabbits, given the combination throughout organogenesis, there was an increased incidence of embryo-fetal death and cardiac and skeletal defects. Based on these data, avoiding the drug in pregnancy appears to be the best course.
Valbenazine (Ingrezza) (MW 419) is indicated for the treatment of tardive dyskinesia. The drug caused no malformations in rats and rabbits. However, in rats given the drug during organogenesis through lactation, an increase in the number of stillborn pups and postnatal pup mortalities was observed.
Dermatologic
Brodalumab (Siliq) (MW 144,000), given subcutaneously, is indicated for the treatment of moderate to severe plaque psoriasis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In monkeys, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from mothers given weekly subcutaneous doses of the drug. Dupilumab (Dupixent) (MW 144,000) is given subcutaneously for the treatment of atopic dermatitis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In pregnant monkeys given subcutaneous doses of the drug, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from birth to 6 months of age.
Guselkumab (Tremfya) (MW 143,600) is given subcutaneously for the treatment of moderate to severe plaque psoriasis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In pregnant monkeys given subcutaneous doses of the drug, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from birth to 6 months of age. However, neonatal deaths were observed in three monkeys given six times the maximum recommended human dose.
Endocrine/metabolic
Deflazacort (Emflaza) (MW 442) is an oral corticosteroid prodrug indicated for the treatment of Duchenne muscular dystrophy. The drug is converted in vivo to an active metabolite. The drug readily crosses the placenta. Although animal reproduction studies have not been conducted, such studies with other corticosteroids in various animal species have shown an increased incidence of cleft palate. In some species, there was an increase in embryo-fetal death, intrauterine growth restriction, and constriction of the ductus arteriosus.
Ertugliflozin (Steglatro) (MW 566) is an oral drug indicated to improve glycemic control in adults with type 2 diabetes mellitus. In juvenile rats, doses that were about 13 times the human dose caused increased kidney weight, renal tubule and renal pelvis dilatation, and renal mineralization. These effects occurred during periods of rat renal development that correspond to the late second and third trimester of human renal development, and did not fully reverse within a 1-month recovery period. Etelcalcetide (Parsabiv) (MW 1,048), an intravenous calcium-sensing receptor agonist, is indicated for patients on hemodialysis who have secondary hyperparathyroidism. In rats and rabbits given the drug during organogenesis, there was reduced fetal growth. In rats given the drug during organogenesis through birth and weaning, there was a slight increase in pup mortality, delay in parturition, and transient effects on pup growth, but there were no effects on sexual maturation, neurobehavioral, or reproductive function. Macimorelin (Macrilen) (MW 535) is an oral growth hormone secretagogue receptor agonist. It is indicated for adult growth hormone deficiency. Animal reproduction studies have not been conducted.
Semaglutide (Ozempic) (MW 4,114), given subcutaneously, is a glucagon-like peptide indicated to improve glycemic control in type 2 diabetes mellitus. In rats given the drug during organogenesis, embryo-fetal death, structural defects, and alterations in growth were observed. In rabbits and monkeys given the drug during organogenesis, there were early pregnancy losses and structural abnormalities. In addition, there was marked maternal body weight loss in both animal species. Vestronidase alfa-vjbk (Mepsevii) is given intravenously. It is indicated for the treatment of Mucopolysaccharidosis VII (Sly syndrome). The calculated average MW of each nonglycosylated peptide chain is 72,562. In rats and rabbits given the drug during organogenesis, there was no maternal toxicity or adverse developmental outcomes.
Gastrointestinal
Plecanatide (Trulance) (MW 1,682) is an oral drug indicated for the treatment of constipation. The drug and its active metabolite are negligibly absorbed systemically and fetal exposure to the drug is not expected. In mice and rabbits given the oral drug during organogenesis, no effects on embryo-fetal development were observed. Telotristat ethyl (Xermelo) (MW 754) is an oral drug indicated for the treatment of carcinoid syndrome diarrhea in combination with somatostatin analog (MW not specified) therapy in adults not controlled by somatostatin analog. When given during organogenesis in rats, there was no effect on embryo-fetal development at doses that were about nine times the recommended human dose. However, an increased incidence of mortality in rat offspring was observed when the drug was given from organogenesis through lactation. During organogenesis in rabbits, the drug had no embryo-fetal effects at doses that were 10 or more times the human dose.
Hematologics
Betrixaban (Bevyxxa) (MW 568) is an oral factor Xa inhibitor indicated for the prophylaxis of venous thromboembolism. The drug was not associated with adverse developmental fetal outcomes in rats and rabbits. However, maternal hemorrhage did occur. In humans, there is an increased risk of hemorrhage during pregnancy and delivery. Emicizumab (Hemlibra) (MW 145,600), given subcutaneously, is indicated for routine prophylaxis to prevent or reduce the frequency of bleeding in patients with hemophilia A with factor VIII inhibitors. Animal reproduction studies have not been conducted. It is a human monoclonal IgG antibody and, though the MW is high, IgG antibodies are known to cross the placenta.
Immunologic
Sarilumab (Kevzara) (MW 150,000) is given subcutaneously. It is indicated for patients with moderate to severe rheumatoid arthritis. Reproduction studies were conducted in pregnant monkeys. There was no evidence of embryo toxicity or fetal malformations. Based on this data, the human pregnancy risk is low.
Ophthalmic
Latanoprostene bunod (Vyzulta) (MW 508) is a prostaglandin analog that is indicated to reduce intraocular pressure. No quantifiable plasma concentrations of latanoprostene bunod were detected in nonpregnant patients. However, very low levels of latanoprost acid (51-59 pg/mL), the active metabolite, were detected with the maximal plasma concentration occurring 5 minutes after administration. When given intravenously to pregnant rabbits, the drug was shown to be abortifacient and teratogenic, but these effects were not observed in pregnant rats. Netarsudil (Rhopressa) (MW 454) is a kinase inhibitor indicated to reduce intraocular pressure in patients with open-angle glaucoma or ocular hypertension. No quantifiable plasma concentrations of netarsudil were detected in 18 subjects. For the active metabolite, a plasma level of 0.11 ng/mL was found in one subject. Intravenous doses to pregnant rats and rabbits during organogenesis did not cause embryo-fetal adverse effects at clinically relevant systemic exposures.
Parathyroid hormone
Abaloparatide (Tymlos) (MW 3,961), given subcutaneously, is a human parathyroid hormone related peptide analog that is indicated for postmenopausal women with osteoporosis at high risk for fracture. Reproduction studies in animals have not been conducted. Because of the indication, it is doubtful if the agent will be used in pregnancy or during breastfeeding.
Respiratory
Benralizumab (Fasenra) (MW 150,000), given subcutaneously, is indicated for the add-on maintenance treatment of severe eosinophilic asthma. It is a human monoclonal IgG antibody and, though the MW is high, IgG antibodies are known to cross the placenta. Studies in monkeys found no evidence of fetal harm with intravenous doses throughout pregnancy that produced exposures up to about 310 times the exposure at the maximum recommended human dose.
The potential adverse effects in an infant when the mother is taking one of the above drugs while breastfeeding will be covered in my next column.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. He coauthored “Drugs in Pregnancy and Lactation” and coedited “Diseases, Complications, and Drug Therapy in Obstetrics.” He reported having no relevant financial disclosures.
Novel drugs are innovative new products that have never before been used in clinical practice. Among the 46 that the Food and Drug Administration approved in 2017, 45 could be used in pregnancy. One, cerliponase alfa (Brineura), is indicated for pediatric patients 3 years of age or older, for treatment of late infantile neuronal ceroid lipofuscinosis type 2. It is doubtful that this drug would be used in pregnancy or during breastfeeding.
With the two exceptions noted below, there are no human pregnancy data for these drugs. It is important to consider that although high molecular weight (MW) drugs (for example, greater than 1,000) probably do not usually cross the placenta in the first half of pregnancy, they may do so in late pregnancy. The cited MWs are shown as the nearest whole number. Animal reproductive data are also cited because, although not definitive, they can provide some measure of the human embryo-fetal risk.
Anti-infectives
Benznidazole (same trade name) (MW 441), given orally, is indicated for pediatric patients aged 2-12 years for treatment of Chagas disease (American trypanosomiasis) caused by Trypanosoma cruzi. However, there are international reports describing its use in pregnancy and breastfeeding. No fetal harm from these exposures were noted. Nevertheless, because of the low MW and the reported animal risk, avoiding the drug during the first half of pregnancy appears to be the best choice. Delafloxacin (Baxdela) (MW 441), a fluoroquinolone antimicrobial given intravenously or orally, is indicated for acute bacterial skin infections. The animal data suggest low risk. However, like other fluoroquinolones, it is contraindicated in pregnancy and should be used only if there are no other alternatives.
Sofosbuvir/velpatasvir /voxilaprevir (Vosevi) (MWs 529, 883, 869), a fixed oral dose combination of three antivirals, is indicated for the treatment of hepatitis C virus infection. The MWs suggest that all three will cross the human placenta. The animal data suggest low risk. Secnidazole (Solosec) (MW 185), given orally, is indicated for the treatment of bacterial vaginosis. It is closely related to metronidazole. No evidence of embryo-fetal toxicity was observed in rats and rabbits, suggesting that the human risk is low. In a report from Brazil, 134 pregnant women with bacterial vaginosis were treated with secnidazole, metronidazole, or tinidazole in the second and third trimesters. Treatment significantly decreased the incidence of premature rupture of membranes, preterm labor, preterm birth, and low birth weight. No fetal harm was reported.
Antineoplastics
[Note: All of the drugs in this category are best avoided, if possible, in pregnancy and breastfeeding.]
Abemaciclib (Verzenio) (MW 507), an oral inhibitor of cyclin-dependent kinases, is indicated for the treatment of breast cancer. The drug is teratogenic in rats. Acalabrutinib (Calquence) (MW 466) is an oral kinase inhibitor indicated for mantle cell lymphoma. The drug had no effect on the rat embryo-fetus but caused decreased fetal body weights and delayed skeletal ossification in rabbits. Avelumab (Bavencio) (MW 147,000) is given intravenously for the treatment of metastatic Merkel cell carcinoma and metastatic urothelial carcinoma. Animal reproduction studies have not been conducted. However, based on its mechanism of action, fetal exposure may increase the risk of developing immune-related disorders or altering the normal immune response.
Brigatinib (Alunbrig) (MW 584) is given orally for the treatment of metastatic non–small-cell lung cancer. In rats, doses less than or slightly above the human exposure caused multiple anomalies in the fetuses of pregnant rats. Copanlisib (Aliqopa) (MW 553) is a kinase inhibitor that is given intravenously for relapsed follicular lymphoma. In rats during organogenesis, doses based on body surface area that were a fraction of the human dose caused embryo-fetal death and fetal defects. Durvalumab (Imfinzi) (MW 146,000), given intravenously, is indicated for the treatment of metastatic urothelial carcinoma and non–small-cell lung cancer. Monkeys given the drug from organogenesis through delivery experienced increased premature birth, fetal loss, and premature neonatal death. Women of reproductive potential should use effective contraception during treatment and for at least 3 months after the last dose.
Enasidenib (Idhifa) (MW 569), given orally, is indicated for the treatment of myeloid leukemia. The drug caused maternal toxicity and adverse embryo-fetal effects (postimplantation loss, resorptions, decrease viable fetuses, lower fetal birth weights, and skeletal variations) in rats and spontaneous abortions in rabbits. Inotuzumab ozogamicin (Besponsa) (MW 160,000), given intravenously, is indicated for relapsed or refractory B-cell precursor acute lymphoblastic leukemia. The drug caused fetal harm in rats but not in rabbits. Midostaurin (Rydapt) (MW 571) is an oral kinase inhibitor indicated for myeloid leukemia. In rats, a dose given during the first week of pregnancy that was a small fraction of the human exposure caused pre- and postimplantation loss. When very small doses were given during organogenesis to rats and rabbits there was significant maternal and fetal toxicity.
Neratinib (Nerlynx) (MW 673) is an oral kinase inhibitor for breast cancer. Although the drug did not cause embryo-fetal toxicity in rats, it did cause this toxicity in rabbits. Doses that resulted in exposures that were less than the human exposure caused maternal toxicity, abortions, and embryo-fetal death. Lower doses caused multiple fetal anomalies. Niraparib (Zejula) (MW 511) is indicated for treatment of epithelial ovarian, fallopian, or peritoneal cancer. Because of the potential human embryo-fetal risk based on its mechanism of action, pregnant animal studies were not conducted. Women with reproductive potential should use effective contraception during treatment and for 6 months after the last dose. Ribociclib (Kisqali) (MW 553) is an oral kinase inhibitor indicated for postmenopausal women with breast cancer. In rats, the drug cause reduced fetal weights and skeletal changes. Increased incidences of fetal abnormalities and lower fetal weights were observed in rabbits.
Cardiovascular
Angiotensin II (Giapreza) (MW 1,046) is a naturally occurring peptide hormone given as an intravenous infusion. It is indicated as a vasoconstrictor to increase blood pressure in adults with septic or other distributive shock. Animal reproduction studies have not been conducted. Because septic or other distributive shock is a medical emergency that can be fatal, the use of this agent in pregnancy should not be withheld.
Central nervous system
Deutetrabenazine (Austedo) (MW 324) is an oral drug indicated for the treatment of chorea associated with Huntington’s disease and for tardive dyskinesia. When given to rats during organogenesis there was no clear effect on embryo-fetal development.
Edaravone (Radicava) (MW 174), given as an intravenous infusion, is indicated for the treatment of amyotrophic lateral sclerosis. Doses that were not maternal toxic did not cause embryo-fetal toxicity in rats and rabbits. However, the no-effect dose for developmental toxicity was less than the recommended human dose. Naldemedine (Symproic) (MW 743) is an opioid antagonist indicated for the treatment of opioid-induced constipation. The drug crosses the human placenta and may precipitate opioid withdrawal in the fetus. The drug caused no embryo-fetal adverse effects, even at high doses, in pregnant rats and rabbits.
Ocrelizumab (Ocrevus) (MW 145,000), an intravenous agent, is used to treat patients with multiple sclerosis. The MW is high but immunoglobulins are known to cross the placenta. When given to monkeys at doses similar to or greater than the human dose, there was increased perinatal mortality, depletion of B-cell populations, and renal, bone marrow, and testicular toxicity in the offspring in the absence of maternal toxicity. Safinamide (Xadago) (MW 399) is an oral drug indicated as adjunctive treatment to levodopa/carbidopa in Parkinson’s disease. In rats, the drug was teratogenic (mainly urogenital defects) at all doses. When it was combined with levodopa/carbidopa or used alone, increased rates of fetal visceral and skeletal defects occurred at all doses studied. In rabbits, given the combination throughout organogenesis, there was an increased incidence of embryo-fetal death and cardiac and skeletal defects. Based on these data, avoiding the drug in pregnancy appears to be the best course.
Valbenazine (Ingrezza) (MW 419) is indicated for the treatment of tardive dyskinesia. The drug caused no malformations in rats and rabbits. However, in rats given the drug during organogenesis through lactation, an increase in the number of stillborn pups and postnatal pup mortalities was observed.
Dermatologic
Brodalumab (Siliq) (MW 144,000), given subcutaneously, is indicated for the treatment of moderate to severe plaque psoriasis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In monkeys, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from mothers given weekly subcutaneous doses of the drug. Dupilumab (Dupixent) (MW 144,000) is given subcutaneously for the treatment of atopic dermatitis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In pregnant monkeys given subcutaneous doses of the drug, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from birth to 6 months of age.
Guselkumab (Tremfya) (MW 143,600) is given subcutaneously for the treatment of moderate to severe plaque psoriasis. It is a human monoclonal IgG antibody and, even though the MW is high, IgG antibodies are known to cross the placenta. In pregnant monkeys given subcutaneous doses of the drug, no drug-related effects on embryo-fetal toxicity or malformations, or on morphological, functional, or immunological development were observed in infants from birth to 6 months of age. However, neonatal deaths were observed in three monkeys given six times the maximum recommended human dose.
Endocrine/metabolic
Deflazacort (Emflaza) (MW 442) is an oral corticosteroid prodrug indicated for the treatment of Duchenne muscular dystrophy. The drug is converted in vivo to an active metabolite. The drug readily crosses the placenta. Although animal reproduction studies have not been conducted, such studies with other corticosteroids in various animal species have shown an increased incidence of cleft palate. In some species, there was an increase in embryo-fetal death, intrauterine growth restriction, and constriction of the ductus arteriosus.
Ertugliflozin (Steglatro) (MW 566) is an oral drug indicated to improve glycemic control in adults with type 2 diabetes mellitus. In juvenile rats, doses that were about 13 times the human dose caused increased kidney weight, renal tubule and renal pelvis dilatation, and renal mineralization. These effects occurred during periods of rat renal development that correspond to the late second and third trimester of human renal development, and did not fully reverse within a 1-month recovery period. Etelcalcetide (Parsabiv) (MW 1,048), an intravenous calcium-sensing receptor agonist, is indicated for patients on hemodialysis who have secondary hyperparathyroidism. In rats and rabbits given the drug during organogenesis, there was reduced fetal growth. In rats given the drug during organogenesis through birth and weaning, there was a slight increase in pup mortality, delay in parturition, and transient effects on pup growth, but there were no effects on sexual maturation, neurobehavioral, or reproductive function. Macimorelin (Macrilen) (MW 535) is an oral growth hormone secretagogue receptor agonist. It is indicated for adult growth hormone deficiency. Animal reproduction studies have not been conducted.
Semaglutide (Ozempic) (MW 4,114), given subcutaneously, is a glucagon-like peptide indicated to improve glycemic control in type 2 diabetes mellitus. In rats given the drug during organogenesis, embryo-fetal death, structural defects, and alterations in growth were observed. In rabbits and monkeys given the drug during organogenesis, there were early pregnancy losses and structural abnormalities. In addition, there was marked maternal body weight loss in both animal species. Vestronidase alfa-vjbk (Mepsevii) is given intravenously. It is indicated for the treatment of Mucopolysaccharidosis VII (Sly syndrome). The calculated average MW of each nonglycosylated peptide chain is 72,562. In rats and rabbits given the drug during organogenesis, there was no maternal toxicity or adverse developmental outcomes.
Gastrointestinal
Plecanatide (Trulance) (MW 1,682) is an oral drug indicated for the treatment of constipation. The drug and its active metabolite are negligibly absorbed systemically and fetal exposure to the drug is not expected. In mice and rabbits given the oral drug during organogenesis, no effects on embryo-fetal development were observed. Telotristat ethyl (Xermelo) (MW 754) is an oral drug indicated for the treatment of carcinoid syndrome diarrhea in combination with somatostatin analog (MW not specified) therapy in adults not controlled by somatostatin analog. When given during organogenesis in rats, there was no effect on embryo-fetal development at doses that were about nine times the recommended human dose. However, an increased incidence of mortality in rat offspring was observed when the drug was given from organogenesis through lactation. During organogenesis in rabbits, the drug had no embryo-fetal effects at doses that were 10 or more times the human dose.
Hematologics
Betrixaban (Bevyxxa) (MW 568) is an oral factor Xa inhibitor indicated for the prophylaxis of venous thromboembolism. The drug was not associated with adverse developmental fetal outcomes in rats and rabbits. However, maternal hemorrhage did occur. In humans, there is an increased risk of hemorrhage during pregnancy and delivery. Emicizumab (Hemlibra) (MW 145,600), given subcutaneously, is indicated for routine prophylaxis to prevent or reduce the frequency of bleeding in patients with hemophilia A with factor VIII inhibitors. Animal reproduction studies have not been conducted. It is a human monoclonal IgG antibody and, though the MW is high, IgG antibodies are known to cross the placenta.
Immunologic
Sarilumab (Kevzara) (MW 150,000) is given subcutaneously. It is indicated for patients with moderate to severe rheumatoid arthritis. Reproduction studies were conducted in pregnant monkeys. There was no evidence of embryo toxicity or fetal malformations. Based on this data, the human pregnancy risk is low.
Ophthalmic
Latanoprostene bunod (Vyzulta) (MW 508) is a prostaglandin analog that is indicated to reduce intraocular pressure. No quantifiable plasma concentrations of latanoprostene bunod were detected in nonpregnant patients. However, very low levels of latanoprost acid (51-59 pg/mL), the active metabolite, were detected with the maximal plasma concentration occurring 5 minutes after administration. When given intravenously to pregnant rabbits, the drug was shown to be abortifacient and teratogenic, but these effects were not observed in pregnant rats. Netarsudil (Rhopressa) (MW 454) is a kinase inhibitor indicated to reduce intraocular pressure in patients with open-angle glaucoma or ocular hypertension. No quantifiable plasma concentrations of netarsudil were detected in 18 subjects. For the active metabolite, a plasma level of 0.11 ng/mL was found in one subject. Intravenous doses to pregnant rats and rabbits during organogenesis did not cause embryo-fetal adverse effects at clinically relevant systemic exposures.
Parathyroid hormone
Abaloparatide (Tymlos) (MW 3,961), given subcutaneously, is a human parathyroid hormone related peptide analog that is indicated for postmenopausal women with osteoporosis at high risk for fracture. Reproduction studies in animals have not been conducted. Because of the indication, it is doubtful if the agent will be used in pregnancy or during breastfeeding.
Respiratory
Benralizumab (Fasenra) (MW 150,000), given subcutaneously, is indicated for the add-on maintenance treatment of severe eosinophilic asthma. It is a human monoclonal IgG antibody and, though the MW is high, IgG antibodies are known to cross the placenta. Studies in monkeys found no evidence of fetal harm with intravenous doses throughout pregnancy that produced exposures up to about 310 times the exposure at the maximum recommended human dose.
The potential adverse effects in an infant when the mother is taking one of the above drugs while breastfeeding will be covered in my next column.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. He coauthored “Drugs in Pregnancy and Lactation” and coedited “Diseases, Complications, and Drug Therapy in Obstetrics.” He reported having no relevant financial disclosures.
CARPREG II fine-tunes assessment of cardiac complication risk in pregnancy
A study of pregnant women with heart disease has yielded a new risk index that improves on its predecessor by integrating general, lesion-specific, and delivery-of-care variables, investigators say.
“Compared with other published risk indices, including the original CARPREG [Cardiac Disease in Pregnancy] score, CARPREG II risk index had the highest discriminative and calibrative accuracy in our study group,” investigators said in a report published in the Journal of the American College of Cardiology.
First author on the report was Candice K. Silversides, MD, division of cardiology, University of Toronto pregnancy and heart disease research program, Mount Sinai Hospital/Sinai Health System.
The widely used, original CARPREG risk index was the first to predict maternal cardiac complications based on general clinical and echocardiographic data from the baseline antepartum visit, the researchers wrote in their report.
The new index developed by Dr. Silversides and her colleagues stems from a study of pregnant women with heart disease receiving care at two large Canadian obstetric centers.
Based on analysis of 1,938 pregnancies progressing beyond 20 weeks of gestation, the investigators found that cardiac complications were overall quite common in pregnant women with heart disease, occurring in 16% of participants. However, maternal cardiac deaths or cardiac arrests were rare, they said, occurring in just 11 (0.6%) of the pregnancies.
Most complications (64%) occurred in the antepartum period, according to the report.
Looking at patient data before or after 2001, investigators found the rates of most complications were consistent over time. However, rates of pulmonary edema decreased in the post-2001 period.
Multivariate analysis of these findings revealed 10 predictors of adverse cardiac events. Those included five general factors, including previous cardiac events or arrhythmia, four lesion-specific variables including pulmonary hypertension and coronary artery disease, and one process of care variable: late pregnancy assessment.
Only 4 of those 10 factors were included in the original CARPREG index, investigators noted.
In CARPREG II, each of the 10 factors is weighted with 1-3 points, depending on risk. For example, history of prior cardiac events was associated with a higher odds ratio, and so was assigned 3 points.
The predicted risk of primary cardiac events ranges from 5% for women with a total of 0-1 points, up to 41% for women with 5 or more points.
The finding that some predictors had higher odds ratios than others reinforces the “foundational role” of clinical assessment, investigators said in the report.
“There may be other factors that affect outcomes,” they wrote. “Risk assessment for the individual patient will need to integrate risk score estimates, known lesion-specific information, and clinical judgment by an experienced physician.”
Dr. Silversides and her coauthors reported that they had no relationships to disclose relevant to the contents of their report on the study.
SOURCE: Silversides CK et al. J Am Coll Cardiol. 2018;71:2419-30.
This update and expansion of the original CARPREG scoring system is a “useful starting point” for prediction of the risk of pregnancy in women with cardiac disease, according to Uri Elkayam, MD.
However, a detailed and lesion specific evaluation is still required for a more precise determination of risk for any given patient, Dr. Elkayam cautioned in an editorial accompanying the article.
Clinicians need to thoroughly understand how the patient’s cardiac condition could be affected by hemodynamic changes during pregnancy, labor, delivery, and the postpartum period, Dr. Elkayam added in his comments.
To fully take advantage of CARPREG II, clinicians need to take into account the limitations of the scoring system, he said, including the fact that it is based on population studies.
“Although the system presented is designed to examine all adverse cardiac events that could have an impact on maternal health, it is less effective for distinguishing between mild and easily manageable events that do not have serious effects on maternal or fetal outcomes and those that may be severe, life-threatening, or require hospitalizations or early delivery,” he wrote.
Dr. Elkayam is with the department of medicine, division of cardiovascular medicine, and the department of obstetrics and gynecology, University of Southern California, Los Angeles. These comments are derived from his editorial in the Journal of the American College of Cardiology . Dr. Elkayam reported he had no relationships relevant to the contents of this paper to disclose.
This update and expansion of the original CARPREG scoring system is a “useful starting point” for prediction of the risk of pregnancy in women with cardiac disease, according to Uri Elkayam, MD.
However, a detailed and lesion specific evaluation is still required for a more precise determination of risk for any given patient, Dr. Elkayam cautioned in an editorial accompanying the article.
Clinicians need to thoroughly understand how the patient’s cardiac condition could be affected by hemodynamic changes during pregnancy, labor, delivery, and the postpartum period, Dr. Elkayam added in his comments.
To fully take advantage of CARPREG II, clinicians need to take into account the limitations of the scoring system, he said, including the fact that it is based on population studies.
“Although the system presented is designed to examine all adverse cardiac events that could have an impact on maternal health, it is less effective for distinguishing between mild and easily manageable events that do not have serious effects on maternal or fetal outcomes and those that may be severe, life-threatening, or require hospitalizations or early delivery,” he wrote.
Dr. Elkayam is with the department of medicine, division of cardiovascular medicine, and the department of obstetrics and gynecology, University of Southern California, Los Angeles. These comments are derived from his editorial in the Journal of the American College of Cardiology . Dr. Elkayam reported he had no relationships relevant to the contents of this paper to disclose.
This update and expansion of the original CARPREG scoring system is a “useful starting point” for prediction of the risk of pregnancy in women with cardiac disease, according to Uri Elkayam, MD.
However, a detailed and lesion specific evaluation is still required for a more precise determination of risk for any given patient, Dr. Elkayam cautioned in an editorial accompanying the article.
Clinicians need to thoroughly understand how the patient’s cardiac condition could be affected by hemodynamic changes during pregnancy, labor, delivery, and the postpartum period, Dr. Elkayam added in his comments.
To fully take advantage of CARPREG II, clinicians need to take into account the limitations of the scoring system, he said, including the fact that it is based on population studies.
“Although the system presented is designed to examine all adverse cardiac events that could have an impact on maternal health, it is less effective for distinguishing between mild and easily manageable events that do not have serious effects on maternal or fetal outcomes and those that may be severe, life-threatening, or require hospitalizations or early delivery,” he wrote.
Dr. Elkayam is with the department of medicine, division of cardiovascular medicine, and the department of obstetrics and gynecology, University of Southern California, Los Angeles. These comments are derived from his editorial in the Journal of the American College of Cardiology . Dr. Elkayam reported he had no relationships relevant to the contents of this paper to disclose.
A study of pregnant women with heart disease has yielded a new risk index that improves on its predecessor by integrating general, lesion-specific, and delivery-of-care variables, investigators say.
“Compared with other published risk indices, including the original CARPREG [Cardiac Disease in Pregnancy] score, CARPREG II risk index had the highest discriminative and calibrative accuracy in our study group,” investigators said in a report published in the Journal of the American College of Cardiology.
First author on the report was Candice K. Silversides, MD, division of cardiology, University of Toronto pregnancy and heart disease research program, Mount Sinai Hospital/Sinai Health System.
The widely used, original CARPREG risk index was the first to predict maternal cardiac complications based on general clinical and echocardiographic data from the baseline antepartum visit, the researchers wrote in their report.
The new index developed by Dr. Silversides and her colleagues stems from a study of pregnant women with heart disease receiving care at two large Canadian obstetric centers.
Based on analysis of 1,938 pregnancies progressing beyond 20 weeks of gestation, the investigators found that cardiac complications were overall quite common in pregnant women with heart disease, occurring in 16% of participants. However, maternal cardiac deaths or cardiac arrests were rare, they said, occurring in just 11 (0.6%) of the pregnancies.
Most complications (64%) occurred in the antepartum period, according to the report.
Looking at patient data before or after 2001, investigators found the rates of most complications were consistent over time. However, rates of pulmonary edema decreased in the post-2001 period.
Multivariate analysis of these findings revealed 10 predictors of adverse cardiac events. Those included five general factors, including previous cardiac events or arrhythmia, four lesion-specific variables including pulmonary hypertension and coronary artery disease, and one process of care variable: late pregnancy assessment.
Only 4 of those 10 factors were included in the original CARPREG index, investigators noted.
In CARPREG II, each of the 10 factors is weighted with 1-3 points, depending on risk. For example, history of prior cardiac events was associated with a higher odds ratio, and so was assigned 3 points.
The predicted risk of primary cardiac events ranges from 5% for women with a total of 0-1 points, up to 41% for women with 5 or more points.
The finding that some predictors had higher odds ratios than others reinforces the “foundational role” of clinical assessment, investigators said in the report.
“There may be other factors that affect outcomes,” they wrote. “Risk assessment for the individual patient will need to integrate risk score estimates, known lesion-specific information, and clinical judgment by an experienced physician.”
Dr. Silversides and her coauthors reported that they had no relationships to disclose relevant to the contents of their report on the study.
SOURCE: Silversides CK et al. J Am Coll Cardiol. 2018;71:2419-30.
A study of pregnant women with heart disease has yielded a new risk index that improves on its predecessor by integrating general, lesion-specific, and delivery-of-care variables, investigators say.
“Compared with other published risk indices, including the original CARPREG [Cardiac Disease in Pregnancy] score, CARPREG II risk index had the highest discriminative and calibrative accuracy in our study group,” investigators said in a report published in the Journal of the American College of Cardiology.
First author on the report was Candice K. Silversides, MD, division of cardiology, University of Toronto pregnancy and heart disease research program, Mount Sinai Hospital/Sinai Health System.
The widely used, original CARPREG risk index was the first to predict maternal cardiac complications based on general clinical and echocardiographic data from the baseline antepartum visit, the researchers wrote in their report.
The new index developed by Dr. Silversides and her colleagues stems from a study of pregnant women with heart disease receiving care at two large Canadian obstetric centers.
Based on analysis of 1,938 pregnancies progressing beyond 20 weeks of gestation, the investigators found that cardiac complications were overall quite common in pregnant women with heart disease, occurring in 16% of participants. However, maternal cardiac deaths or cardiac arrests were rare, they said, occurring in just 11 (0.6%) of the pregnancies.
Most complications (64%) occurred in the antepartum period, according to the report.
Looking at patient data before or after 2001, investigators found the rates of most complications were consistent over time. However, rates of pulmonary edema decreased in the post-2001 period.
Multivariate analysis of these findings revealed 10 predictors of adverse cardiac events. Those included five general factors, including previous cardiac events or arrhythmia, four lesion-specific variables including pulmonary hypertension and coronary artery disease, and one process of care variable: late pregnancy assessment.
Only 4 of those 10 factors were included in the original CARPREG index, investigators noted.
In CARPREG II, each of the 10 factors is weighted with 1-3 points, depending on risk. For example, history of prior cardiac events was associated with a higher odds ratio, and so was assigned 3 points.
The predicted risk of primary cardiac events ranges from 5% for women with a total of 0-1 points, up to 41% for women with 5 or more points.
The finding that some predictors had higher odds ratios than others reinforces the “foundational role” of clinical assessment, investigators said in the report.
“There may be other factors that affect outcomes,” they wrote. “Risk assessment for the individual patient will need to integrate risk score estimates, known lesion-specific information, and clinical judgment by an experienced physician.”
Dr. Silversides and her coauthors reported that they had no relationships to disclose relevant to the contents of their report on the study.
SOURCE: Silversides CK et al. J Am Coll Cardiol. 2018;71:2419-30.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: A newly developed risk index enhances the ability to predict maternal cardiac complications by combining general, lesion-specific, and delivery-of-care variables.
Major finding: Investigators developed the CARPREG II risk index based on 10 predictors of maternal cardiac complications (5 general, 4 lesion-specific, and 1 related to delivery of care).
Study details: The CARPREG II Study, which included more than 2,000 prospectively enrolled consecutive pregnant women with heart disease seen at one of two large Canadian obstetric centers.
Disclosures: Authors reported that they had no relationships to disclose relevant to the contents of their report on the study.
Source: Silversides CK et al. J Am Coll Cardiol. 2018;71:2419-30.
Drug-related deaths continue to rise in United States
TORONTO – Drug-related deaths in America are rising faster than ever.
Rear Adm. Wanda D. Barfield, MD shared recent data from the U.S. National Center for Health Statistics on people aged 15 years and older at the Pediatric Academic Societies annual meeting. Between 1999 and 2016, for example, the number of drug overdose deaths rose more than threefold, from 6.1/100,000 standard population in 1999 to 19.8/100,000 in 2016. For males, the rate increased from 8.2/100,000 in 1999 to 26.2/100,000 in 2016. For females, the rate increased from 3.9/100,000 in 1999 to 13.4/100,000 in 2016.
Dr. Barfield, director of the division of reproductive health at the Centers for Disease Control and Prevention, said that in 2016, the NCHS also found that 22 states and the District of Columbia had drug overdoses that were significantly higher than the national average. The states with the highest number of drug overdose deaths were the District of Columbia, New Hampshire, Pennsylvania, and West Virginia while the states with the lowest observed rates were Nebraska, North Dakota, South Dakota, and Texas.
“Many of these drug overdose deaths are linked to opioids, but not exclusively,” Dr. Barfield said. “In the past, the overall opioid-related overdose deaths were mainly attributed to commonly prescribed opioid medications. However, in recent years, we’re seeing more deaths due to illicit drugs such as heroin and fentanyl.”
The NCHS found that the age-adjusted rate for drug overdose deaths involving synthetic opioids other than methadone doubled from 2015 to 2016, and that drug overdose deaths involving synthetic opioids other than methadone increased from 0.3/100,000 in 1999 to 6.2/100,000 in 2016. The rate increased an average of 18% per year from 1999 to 2006, remained steady from 2006 to 2013, but increased by 88% per year from 2013 to 2016. At the same time, drug overdose deaths involving heroin increased from 0.7/100,000 in 1999 to 1/100,000 in 2010, to 4.9/100,000 in 2016.
According to Dr. Barfield, the spike in opioid use since 1999 stems directly from increased prescribing rates. “In 2015, the number of opioids prescribed was enough so that every American could be medicated around the clock for 3 weeks,” she said. “In addition to the number of prescriptions, the average day’s supply of prescription opioids increased from 2006 to 2015, from 13.3 days in 2006 to 17.7 days in 2015.” What’s more, a recent CDC Vital Signs found that the amount of opioids prescribed per person varied widely among U.S. counties in 2015. “The wide variation among counties suggests a lack of consistency among providers when prescribing opioids,” Dr. Barfield said. “It’s concerning, as higher opioid prescribing puts patients at risk for addiction.”
At the same time, opioid overdose ED visits continue to rise. Data from the CDC’s National Syndromic Surveillance Program found that from July 2016 to September 2017, opioid overdose ED visits increased by 30% for men, by 24% for women, and for all adult age groups (31% among those aged 25-34 years, 36% among those aged 35-54 years, and 32% among those aged 55 years and older).
There’s a problem of prescription opioid use among pregnant women. Published estimates indicate that 14%-22% of women filled an opioid prescription during pregnancy, Dr. Barfield said. Among pregnant women, the prevalence of maternal opioid use or dependence during hospitalization for delivery has increased 127%, from 1.7 /1,000 delivery admissions in 1998 to 3.9/1,000 delivery admissions in 2011 (Anesthesiology 2014;121[6]:1158-65). There also has been a significant increase in neonatal abstinence syndrome (NAS), which is most commonly attributed to opioid exposure during pregnancy, from 1.2/1,000 U.S. hospital births in 2000 to 8/1,000 U.S. hospital births in 2014. “NAS is still on the rise,” Dr. Barfield said. “In 2012, we saw one baby with NAS born every 25 minutes. In 2014, that number jumped to one baby born with NAS every 15 minutes. That means about 96 infants with NAS are born daily,” she said. “Where do you think we’re going to be when we look at 2018 data?”
Role for pediatricians
Dr. Barfield closed her presentation by underscoring the role pediatricians play in counseling patients about opioid abuse or dependence during pregnancy. “We know that providers have a tremendous impact on patients and their families,” she said. “We also know that issues leading to a newborn having NAS are complex, so adopting a public health approach focused on prevention, expansion of treatment, and improvements in child welfare systems is vital.” Specifically, she said, health care providers can “bridge the gap” between clinical care and public health; lead in their communities, not just within their hospital or practice; work as a team member with colleagues in other fields of medicine such as obstetrics, family medicine, and addiction care when caring for infants with NAS, and by considering the social determinants of health.
“One way to adopt a public health perspective is to remember that the health of the fetus and baby rely on more than just prenatal care,” Dr. Barfield said. “We’re all part of a larger whole, surrounded by our families, communities, regions, state, and even our countries of origin. What’s going on with the mom, her family, and the larger community impacts the baby’s health. In other words, the social determinants of health matter, and are an important part of the conversation on NAS.”
She reported having no financial disclosures.
TORONTO – Drug-related deaths in America are rising faster than ever.
Rear Adm. Wanda D. Barfield, MD shared recent data from the U.S. National Center for Health Statistics on people aged 15 years and older at the Pediatric Academic Societies annual meeting. Between 1999 and 2016, for example, the number of drug overdose deaths rose more than threefold, from 6.1/100,000 standard population in 1999 to 19.8/100,000 in 2016. For males, the rate increased from 8.2/100,000 in 1999 to 26.2/100,000 in 2016. For females, the rate increased from 3.9/100,000 in 1999 to 13.4/100,000 in 2016.
Dr. Barfield, director of the division of reproductive health at the Centers for Disease Control and Prevention, said that in 2016, the NCHS also found that 22 states and the District of Columbia had drug overdoses that were significantly higher than the national average. The states with the highest number of drug overdose deaths were the District of Columbia, New Hampshire, Pennsylvania, and West Virginia while the states with the lowest observed rates were Nebraska, North Dakota, South Dakota, and Texas.
“Many of these drug overdose deaths are linked to opioids, but not exclusively,” Dr. Barfield said. “In the past, the overall opioid-related overdose deaths were mainly attributed to commonly prescribed opioid medications. However, in recent years, we’re seeing more deaths due to illicit drugs such as heroin and fentanyl.”
The NCHS found that the age-adjusted rate for drug overdose deaths involving synthetic opioids other than methadone doubled from 2015 to 2016, and that drug overdose deaths involving synthetic opioids other than methadone increased from 0.3/100,000 in 1999 to 6.2/100,000 in 2016. The rate increased an average of 18% per year from 1999 to 2006, remained steady from 2006 to 2013, but increased by 88% per year from 2013 to 2016. At the same time, drug overdose deaths involving heroin increased from 0.7/100,000 in 1999 to 1/100,000 in 2010, to 4.9/100,000 in 2016.
According to Dr. Barfield, the spike in opioid use since 1999 stems directly from increased prescribing rates. “In 2015, the number of opioids prescribed was enough so that every American could be medicated around the clock for 3 weeks,” she said. “In addition to the number of prescriptions, the average day’s supply of prescription opioids increased from 2006 to 2015, from 13.3 days in 2006 to 17.7 days in 2015.” What’s more, a recent CDC Vital Signs found that the amount of opioids prescribed per person varied widely among U.S. counties in 2015. “The wide variation among counties suggests a lack of consistency among providers when prescribing opioids,” Dr. Barfield said. “It’s concerning, as higher opioid prescribing puts patients at risk for addiction.”
At the same time, opioid overdose ED visits continue to rise. Data from the CDC’s National Syndromic Surveillance Program found that from July 2016 to September 2017, opioid overdose ED visits increased by 30% for men, by 24% for women, and for all adult age groups (31% among those aged 25-34 years, 36% among those aged 35-54 years, and 32% among those aged 55 years and older).
There’s a problem of prescription opioid use among pregnant women. Published estimates indicate that 14%-22% of women filled an opioid prescription during pregnancy, Dr. Barfield said. Among pregnant women, the prevalence of maternal opioid use or dependence during hospitalization for delivery has increased 127%, from 1.7 /1,000 delivery admissions in 1998 to 3.9/1,000 delivery admissions in 2011 (Anesthesiology 2014;121[6]:1158-65). There also has been a significant increase in neonatal abstinence syndrome (NAS), which is most commonly attributed to opioid exposure during pregnancy, from 1.2/1,000 U.S. hospital births in 2000 to 8/1,000 U.S. hospital births in 2014. “NAS is still on the rise,” Dr. Barfield said. “In 2012, we saw one baby with NAS born every 25 minutes. In 2014, that number jumped to one baby born with NAS every 15 minutes. That means about 96 infants with NAS are born daily,” she said. “Where do you think we’re going to be when we look at 2018 data?”
Role for pediatricians
Dr. Barfield closed her presentation by underscoring the role pediatricians play in counseling patients about opioid abuse or dependence during pregnancy. “We know that providers have a tremendous impact on patients and their families,” she said. “We also know that issues leading to a newborn having NAS are complex, so adopting a public health approach focused on prevention, expansion of treatment, and improvements in child welfare systems is vital.” Specifically, she said, health care providers can “bridge the gap” between clinical care and public health; lead in their communities, not just within their hospital or practice; work as a team member with colleagues in other fields of medicine such as obstetrics, family medicine, and addiction care when caring for infants with NAS, and by considering the social determinants of health.
“One way to adopt a public health perspective is to remember that the health of the fetus and baby rely on more than just prenatal care,” Dr. Barfield said. “We’re all part of a larger whole, surrounded by our families, communities, regions, state, and even our countries of origin. What’s going on with the mom, her family, and the larger community impacts the baby’s health. In other words, the social determinants of health matter, and are an important part of the conversation on NAS.”
She reported having no financial disclosures.
TORONTO – Drug-related deaths in America are rising faster than ever.
Rear Adm. Wanda D. Barfield, MD shared recent data from the U.S. National Center for Health Statistics on people aged 15 years and older at the Pediatric Academic Societies annual meeting. Between 1999 and 2016, for example, the number of drug overdose deaths rose more than threefold, from 6.1/100,000 standard population in 1999 to 19.8/100,000 in 2016. For males, the rate increased from 8.2/100,000 in 1999 to 26.2/100,000 in 2016. For females, the rate increased from 3.9/100,000 in 1999 to 13.4/100,000 in 2016.
Dr. Barfield, director of the division of reproductive health at the Centers for Disease Control and Prevention, said that in 2016, the NCHS also found that 22 states and the District of Columbia had drug overdoses that were significantly higher than the national average. The states with the highest number of drug overdose deaths were the District of Columbia, New Hampshire, Pennsylvania, and West Virginia while the states with the lowest observed rates were Nebraska, North Dakota, South Dakota, and Texas.
“Many of these drug overdose deaths are linked to opioids, but not exclusively,” Dr. Barfield said. “In the past, the overall opioid-related overdose deaths were mainly attributed to commonly prescribed opioid medications. However, in recent years, we’re seeing more deaths due to illicit drugs such as heroin and fentanyl.”
The NCHS found that the age-adjusted rate for drug overdose deaths involving synthetic opioids other than methadone doubled from 2015 to 2016, and that drug overdose deaths involving synthetic opioids other than methadone increased from 0.3/100,000 in 1999 to 6.2/100,000 in 2016. The rate increased an average of 18% per year from 1999 to 2006, remained steady from 2006 to 2013, but increased by 88% per year from 2013 to 2016. At the same time, drug overdose deaths involving heroin increased from 0.7/100,000 in 1999 to 1/100,000 in 2010, to 4.9/100,000 in 2016.
According to Dr. Barfield, the spike in opioid use since 1999 stems directly from increased prescribing rates. “In 2015, the number of opioids prescribed was enough so that every American could be medicated around the clock for 3 weeks,” she said. “In addition to the number of prescriptions, the average day’s supply of prescription opioids increased from 2006 to 2015, from 13.3 days in 2006 to 17.7 days in 2015.” What’s more, a recent CDC Vital Signs found that the amount of opioids prescribed per person varied widely among U.S. counties in 2015. “The wide variation among counties suggests a lack of consistency among providers when prescribing opioids,” Dr. Barfield said. “It’s concerning, as higher opioid prescribing puts patients at risk for addiction.”
At the same time, opioid overdose ED visits continue to rise. Data from the CDC’s National Syndromic Surveillance Program found that from July 2016 to September 2017, opioid overdose ED visits increased by 30% for men, by 24% for women, and for all adult age groups (31% among those aged 25-34 years, 36% among those aged 35-54 years, and 32% among those aged 55 years and older).
There’s a problem of prescription opioid use among pregnant women. Published estimates indicate that 14%-22% of women filled an opioid prescription during pregnancy, Dr. Barfield said. Among pregnant women, the prevalence of maternal opioid use or dependence during hospitalization for delivery has increased 127%, from 1.7 /1,000 delivery admissions in 1998 to 3.9/1,000 delivery admissions in 2011 (Anesthesiology 2014;121[6]:1158-65). There also has been a significant increase in neonatal abstinence syndrome (NAS), which is most commonly attributed to opioid exposure during pregnancy, from 1.2/1,000 U.S. hospital births in 2000 to 8/1,000 U.S. hospital births in 2014. “NAS is still on the rise,” Dr. Barfield said. “In 2012, we saw one baby with NAS born every 25 minutes. In 2014, that number jumped to one baby born with NAS every 15 minutes. That means about 96 infants with NAS are born daily,” she said. “Where do you think we’re going to be when we look at 2018 data?”
Role for pediatricians
Dr. Barfield closed her presentation by underscoring the role pediatricians play in counseling patients about opioid abuse or dependence during pregnancy. “We know that providers have a tremendous impact on patients and their families,” she said. “We also know that issues leading to a newborn having NAS are complex, so adopting a public health approach focused on prevention, expansion of treatment, and improvements in child welfare systems is vital.” Specifically, she said, health care providers can “bridge the gap” between clinical care and public health; lead in their communities, not just within their hospital or practice; work as a team member with colleagues in other fields of medicine such as obstetrics, family medicine, and addiction care when caring for infants with NAS, and by considering the social determinants of health.
“One way to adopt a public health perspective is to remember that the health of the fetus and baby rely on more than just prenatal care,” Dr. Barfield said. “We’re all part of a larger whole, surrounded by our families, communities, regions, state, and even our countries of origin. What’s going on with the mom, her family, and the larger community impacts the baby’s health. In other words, the social determinants of health matter, and are an important part of the conversation on NAS.”
She reported having no financial disclosures.
EXPERT ANALYSIS FROM PAS 2018
FDA warns of birth defect risks from dolutegravir
The Food and Drug Administration has issued a Drug Safety Communication alert that serious cases of neural tube birth defects have been reported in babies born to women treated with dolutegravir for human immunodeficiency virus. Reported defects have involved the brain, spine, and spinal cord.
To date, in this observational study, there are no reported cases of babies born with neural tube defects to women starting dolutegravir later in pregnancy, according to the FDA. “We are investigating this new safety issue and will update the public when we have more information,” the alert stated.
Dolutegravir is an FDA-approved antiretroviral used to treat HIV. The drug is available as a single ingredient under the brand name Tivicay and as a combination tablet with other HIV medicines under the brand names Juluca and Triumeq.
Medwatch also released an alert for medical practitioners to report adverse events related to this issue.
The Food and Drug Administration has issued a Drug Safety Communication alert that serious cases of neural tube birth defects have been reported in babies born to women treated with dolutegravir for human immunodeficiency virus. Reported defects have involved the brain, spine, and spinal cord.
To date, in this observational study, there are no reported cases of babies born with neural tube defects to women starting dolutegravir later in pregnancy, according to the FDA. “We are investigating this new safety issue and will update the public when we have more information,” the alert stated.
Dolutegravir is an FDA-approved antiretroviral used to treat HIV. The drug is available as a single ingredient under the brand name Tivicay and as a combination tablet with other HIV medicines under the brand names Juluca and Triumeq.
Medwatch also released an alert for medical practitioners to report adverse events related to this issue.
The Food and Drug Administration has issued a Drug Safety Communication alert that serious cases of neural tube birth defects have been reported in babies born to women treated with dolutegravir for human immunodeficiency virus. Reported defects have involved the brain, spine, and spinal cord.
To date, in this observational study, there are no reported cases of babies born with neural tube defects to women starting dolutegravir later in pregnancy, according to the FDA. “We are investigating this new safety issue and will update the public when we have more information,” the alert stated.
Dolutegravir is an FDA-approved antiretroviral used to treat HIV. The drug is available as a single ingredient under the brand name Tivicay and as a combination tablet with other HIV medicines under the brand names Juluca and Triumeq.
Medwatch also released an alert for medical practitioners to report adverse events related to this issue.