User login
Test all perinatally exposed infants for HCV: CDC
In utero–exposed infants should be tested at 2-6 months of life, much earlier than the current strategy of testing at 18 months.
HCV infection, which can lead to liver fibrosis and cirrhosis, liver failure, hepatic cancer, and transplant, will develop in 6%-7% of all perinatally exposed infants and children. Curative therapy with direct-acting antivirals can be administered starting at age 3, the CDC noted in Morbidity and Mortality Week Report (MMWR).
About 70% of children 18 months and older are not being tested with the current strategy of anti-HCV testing.
This current MMWR report supplements the 2020 CDC recommendations for adult HCV screening, which includes universal screening among pregnant persons during each pregnancy.
The new recommendations
- Perinatally exposed infants should receive a nucleic acid amplification test for HCV RNA at 2-6 months of age to identify those who might develop chronic HCV infection if not treated.
- Those with detectable HCV RNA should be managed in consultation with an expert in pediatric HCV.
- Infants with undetectable HCV RNA do not require further follow-up unless clinically warranted.
“Testing perinatally exposed infants beginning at age 2 months with a NAT for HCV RNA is cost-effective and allows for earlier linkage to care, appropriate evaluation, and the opportunity to provide curative, life-saving therapy,” the MMWR report said.
A growing problem
The CDC noted that rates of HCV infections during pregnancy are on the rise, corresponding with the ongoing opioid crisis and intravenous drug use.
Yet most perinatally exposed children are not tested for HCV infection and are not referred for hepatitis C care. Reasons might include lack of awareness of perinatal exposure by pediatric providers, lack of regular pediatric care among exposed children, and switching of health care providers before the former recommended testing age of 18 months.
The CDC’s testing recommendation is welcome news to Dawnette A. Lewis, MD, a maternal fetal medicine specialist at Northwell Health in New Hyde Park, N.Y. “As opposed to data for hep B and HIV, we have traditionally had little information and experience regarding the transmission and impact of hep C in pregnant women and their babies. We’ve been having that conversation about the lack of information for some time, and now there’s an opportunity to get evolving data on hep C and how it affects the baby, ” she said.
In her view, mothers will likely be quite accepting of testing for their infants. “It could be integrated into the routine newborn screening panel, so there should not be barriers to accessibility if they’re getting prenatal and neonatal care.”
Commenting on HCV testing for babies in an interview at his institution, Ravi R. Jhaveri, MD, division head of pediatric infectious diseases at Northwestern Medicine’s Ann & Robert H. Lurie Children’s Hospital of Chicago, said, “This is a terrific way to capitalize on the fact that infants already come to the doctor for many visits during the first months of life for their vaccines and their well-child check. And so this should be an easy way to streamline our testing strategy and hopefully lose many fewer patients.”
Northwestern Medicine is an innovative clinic offering HCV testing and treatment outside of clinical trials for pregnant women and their infants with the goal of preventing transmission from mother to child.
Northwestern is launching a clinical trial of treatment for HCV-positive pregnant patients during regular prenatal care. “With very simple treatments similar to taking a prenatal vitamin, it would be easy and seamless to fit into the existing schedule,” said Lyn Yee, MD, a Northwestern maternal-fetal medicine specialist.
Dr. Yee stressed that eliminating hepatitis C will likely be one of the most significant health advancements of the decade.
Dr. Lewis, Dr. Jhaveri, and Dr. Yee had no relevant conflicts of interest to declare with regard to their comments.
In utero–exposed infants should be tested at 2-6 months of life, much earlier than the current strategy of testing at 18 months.
HCV infection, which can lead to liver fibrosis and cirrhosis, liver failure, hepatic cancer, and transplant, will develop in 6%-7% of all perinatally exposed infants and children. Curative therapy with direct-acting antivirals can be administered starting at age 3, the CDC noted in Morbidity and Mortality Week Report (MMWR).
About 70% of children 18 months and older are not being tested with the current strategy of anti-HCV testing.
This current MMWR report supplements the 2020 CDC recommendations for adult HCV screening, which includes universal screening among pregnant persons during each pregnancy.
The new recommendations
- Perinatally exposed infants should receive a nucleic acid amplification test for HCV RNA at 2-6 months of age to identify those who might develop chronic HCV infection if not treated.
- Those with detectable HCV RNA should be managed in consultation with an expert in pediatric HCV.
- Infants with undetectable HCV RNA do not require further follow-up unless clinically warranted.
“Testing perinatally exposed infants beginning at age 2 months with a NAT for HCV RNA is cost-effective and allows for earlier linkage to care, appropriate evaluation, and the opportunity to provide curative, life-saving therapy,” the MMWR report said.
A growing problem
The CDC noted that rates of HCV infections during pregnancy are on the rise, corresponding with the ongoing opioid crisis and intravenous drug use.
Yet most perinatally exposed children are not tested for HCV infection and are not referred for hepatitis C care. Reasons might include lack of awareness of perinatal exposure by pediatric providers, lack of regular pediatric care among exposed children, and switching of health care providers before the former recommended testing age of 18 months.
The CDC’s testing recommendation is welcome news to Dawnette A. Lewis, MD, a maternal fetal medicine specialist at Northwell Health in New Hyde Park, N.Y. “As opposed to data for hep B and HIV, we have traditionally had little information and experience regarding the transmission and impact of hep C in pregnant women and their babies. We’ve been having that conversation about the lack of information for some time, and now there’s an opportunity to get evolving data on hep C and how it affects the baby, ” she said.
In her view, mothers will likely be quite accepting of testing for their infants. “It could be integrated into the routine newborn screening panel, so there should not be barriers to accessibility if they’re getting prenatal and neonatal care.”
Commenting on HCV testing for babies in an interview at his institution, Ravi R. Jhaveri, MD, division head of pediatric infectious diseases at Northwestern Medicine’s Ann & Robert H. Lurie Children’s Hospital of Chicago, said, “This is a terrific way to capitalize on the fact that infants already come to the doctor for many visits during the first months of life for their vaccines and their well-child check. And so this should be an easy way to streamline our testing strategy and hopefully lose many fewer patients.”
Northwestern Medicine is an innovative clinic offering HCV testing and treatment outside of clinical trials for pregnant women and their infants with the goal of preventing transmission from mother to child.
Northwestern is launching a clinical trial of treatment for HCV-positive pregnant patients during regular prenatal care. “With very simple treatments similar to taking a prenatal vitamin, it would be easy and seamless to fit into the existing schedule,” said Lyn Yee, MD, a Northwestern maternal-fetal medicine specialist.
Dr. Yee stressed that eliminating hepatitis C will likely be one of the most significant health advancements of the decade.
Dr. Lewis, Dr. Jhaveri, and Dr. Yee had no relevant conflicts of interest to declare with regard to their comments.
In utero–exposed infants should be tested at 2-6 months of life, much earlier than the current strategy of testing at 18 months.
HCV infection, which can lead to liver fibrosis and cirrhosis, liver failure, hepatic cancer, and transplant, will develop in 6%-7% of all perinatally exposed infants and children. Curative therapy with direct-acting antivirals can be administered starting at age 3, the CDC noted in Morbidity and Mortality Week Report (MMWR).
About 70% of children 18 months and older are not being tested with the current strategy of anti-HCV testing.
This current MMWR report supplements the 2020 CDC recommendations for adult HCV screening, which includes universal screening among pregnant persons during each pregnancy.
The new recommendations
- Perinatally exposed infants should receive a nucleic acid amplification test for HCV RNA at 2-6 months of age to identify those who might develop chronic HCV infection if not treated.
- Those with detectable HCV RNA should be managed in consultation with an expert in pediatric HCV.
- Infants with undetectable HCV RNA do not require further follow-up unless clinically warranted.
“Testing perinatally exposed infants beginning at age 2 months with a NAT for HCV RNA is cost-effective and allows for earlier linkage to care, appropriate evaluation, and the opportunity to provide curative, life-saving therapy,” the MMWR report said.
A growing problem
The CDC noted that rates of HCV infections during pregnancy are on the rise, corresponding with the ongoing opioid crisis and intravenous drug use.
Yet most perinatally exposed children are not tested for HCV infection and are not referred for hepatitis C care. Reasons might include lack of awareness of perinatal exposure by pediatric providers, lack of regular pediatric care among exposed children, and switching of health care providers before the former recommended testing age of 18 months.
The CDC’s testing recommendation is welcome news to Dawnette A. Lewis, MD, a maternal fetal medicine specialist at Northwell Health in New Hyde Park, N.Y. “As opposed to data for hep B and HIV, we have traditionally had little information and experience regarding the transmission and impact of hep C in pregnant women and their babies. We’ve been having that conversation about the lack of information for some time, and now there’s an opportunity to get evolving data on hep C and how it affects the baby, ” she said.
In her view, mothers will likely be quite accepting of testing for their infants. “It could be integrated into the routine newborn screening panel, so there should not be barriers to accessibility if they’re getting prenatal and neonatal care.”
Commenting on HCV testing for babies in an interview at his institution, Ravi R. Jhaveri, MD, division head of pediatric infectious diseases at Northwestern Medicine’s Ann & Robert H. Lurie Children’s Hospital of Chicago, said, “This is a terrific way to capitalize on the fact that infants already come to the doctor for many visits during the first months of life for their vaccines and their well-child check. And so this should be an easy way to streamline our testing strategy and hopefully lose many fewer patients.”
Northwestern Medicine is an innovative clinic offering HCV testing and treatment outside of clinical trials for pregnant women and their infants with the goal of preventing transmission from mother to child.
Northwestern is launching a clinical trial of treatment for HCV-positive pregnant patients during regular prenatal care. “With very simple treatments similar to taking a prenatal vitamin, it would be easy and seamless to fit into the existing schedule,” said Lyn Yee, MD, a Northwestern maternal-fetal medicine specialist.
Dr. Yee stressed that eliminating hepatitis C will likely be one of the most significant health advancements of the decade.
Dr. Lewis, Dr. Jhaveri, and Dr. Yee had no relevant conflicts of interest to declare with regard to their comments.
Adverse events related to embryo transfer catheters may be underreported to the FDA
, according to a new study presented at the American Society for Reproductive Medicine’s 2023 meeting.
ETCs are medical devices used routinely in assisted reproduction. The findings highlight the need for increased vigilance in tracking and reporting adverse events associated with these devices, according to the investigators.
“With hundreds of thousands of embryo transfers being performed per year, surveillance of the safety, performance, and quality of embryo transfer catheter devices is critical and should not be taken for granted,” said Anita Madison, MD, MPH, from the division of reproductive endocrinology and infertility at Johns Hopkins School of Medicine, Baltimore, who led the study. “There are a variety of transfer catheters with different indications, with little data on the superiority and safety of the brands compared to one another.”
Although the number of reported adverse events associated with ETCs is relatively small, the problems can significantly affect patient care, the researchers said.
Dr. Madison and her colleagues used the Manufacturer and User Facility Device Experience (MAUDE) database to identify adverse events associated with ETC devices. The MAUDE database is a voluntary reporting system that holds hundreds of thousands of medical device reports of suspected device-associated deaths, injuries, and malfunctions reported to the FDA annually.
For each adverse event in the database linked to an ECT, the researchers collected information related to the brand of the device, the nature of the event, and the nature of the reporter. The researchers omitted the device and manufacturer names from the presentation of the study findings, delineating them only as “Brand 1,” “Brand 2,” “Brand 3,” “Brand 4,” or “Other.”
Problems with devices included contamination, packaging problems, malfunction, mechanical flaws, and material separation. Patient-level adverse events included retaining of foreign body, trauma, malfunction, or failed embryo transfer.
Between 2014 and 2023, Dr. Madison and her colleagues identified 101 adverse events associated with ECTs in the database. About 25% of these occurred in 2018, with 27 cases reported. Contamination was the most prevalent problem, found in 68 reports; oil was the most common contaminant.
The distribution of types of adverse events varied, depending on ETC brand. A breakdown of occurrences revealed high numbers for Brand 2, with 52 adverse events. Although Brand 3 accounted for only 16 adverse events, the majority of these were related to device separation.
“That finding stood out,” Dr. Madison said.
Nearly 1 in 4 (22%) of all reported incidents led to overt patient harm. Retention of a foreign body was the prime type of injury, occurring in 12 cases. Malfunction and injury were found in four cases each, with two failed embryo transfers reported, Dr. Madison said.
Because the majority of these adverse event reports were submitted by manufacturers (87%) and were rarely submitted by end users (for example, physicians, lab staff), the researchers said their findings likely underestimate such problems.
“I’m surprised the [number of reported adverse events] is as low as it is,” said Kimball Pomeroy, PhD, scientific director at the World Egg and Sperm Bank, Scottsdale, Ariz., who was not part of the study team. “Laboratories are required to report failed devices; they have to have a plan for that.”
“It just comes down to underreporting,” added Valerie L. Baker, MD, director in the Division of Reproductive Endocrinology and Infertility at Johns Hopkins Medicine, Lutherville, Md., who was not affiliated with the study.
“In two of these reports, they failed to transfer the embryo; they actually lost the embryo,” Dr. Pomeroy added. “That’s drastic for those patients; it’s a serious problem that needs to be addressed.”
Citing these findings, the authors underscored the need for heightened surveillance of ETC devices and recommend further studies to assess the sensitivity of these procedures for attempting pregnancy. They urge physicians and lab staff involved in these procedures to exercise continued vigilance and to improve the reporting of problems with ETC devices.
Dr. Madison, Dr. Baker, and Dr. Pomeroy report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a new study presented at the American Society for Reproductive Medicine’s 2023 meeting.
ETCs are medical devices used routinely in assisted reproduction. The findings highlight the need for increased vigilance in tracking and reporting adverse events associated with these devices, according to the investigators.
“With hundreds of thousands of embryo transfers being performed per year, surveillance of the safety, performance, and quality of embryo transfer catheter devices is critical and should not be taken for granted,” said Anita Madison, MD, MPH, from the division of reproductive endocrinology and infertility at Johns Hopkins School of Medicine, Baltimore, who led the study. “There are a variety of transfer catheters with different indications, with little data on the superiority and safety of the brands compared to one another.”
Although the number of reported adverse events associated with ETCs is relatively small, the problems can significantly affect patient care, the researchers said.
Dr. Madison and her colleagues used the Manufacturer and User Facility Device Experience (MAUDE) database to identify adverse events associated with ETC devices. The MAUDE database is a voluntary reporting system that holds hundreds of thousands of medical device reports of suspected device-associated deaths, injuries, and malfunctions reported to the FDA annually.
For each adverse event in the database linked to an ECT, the researchers collected information related to the brand of the device, the nature of the event, and the nature of the reporter. The researchers omitted the device and manufacturer names from the presentation of the study findings, delineating them only as “Brand 1,” “Brand 2,” “Brand 3,” “Brand 4,” or “Other.”
Problems with devices included contamination, packaging problems, malfunction, mechanical flaws, and material separation. Patient-level adverse events included retaining of foreign body, trauma, malfunction, or failed embryo transfer.
Between 2014 and 2023, Dr. Madison and her colleagues identified 101 adverse events associated with ECTs in the database. About 25% of these occurred in 2018, with 27 cases reported. Contamination was the most prevalent problem, found in 68 reports; oil was the most common contaminant.
The distribution of types of adverse events varied, depending on ETC brand. A breakdown of occurrences revealed high numbers for Brand 2, with 52 adverse events. Although Brand 3 accounted for only 16 adverse events, the majority of these were related to device separation.
“That finding stood out,” Dr. Madison said.
Nearly 1 in 4 (22%) of all reported incidents led to overt patient harm. Retention of a foreign body was the prime type of injury, occurring in 12 cases. Malfunction and injury were found in four cases each, with two failed embryo transfers reported, Dr. Madison said.
Because the majority of these adverse event reports were submitted by manufacturers (87%) and were rarely submitted by end users (for example, physicians, lab staff), the researchers said their findings likely underestimate such problems.
“I’m surprised the [number of reported adverse events] is as low as it is,” said Kimball Pomeroy, PhD, scientific director at the World Egg and Sperm Bank, Scottsdale, Ariz., who was not part of the study team. “Laboratories are required to report failed devices; they have to have a plan for that.”
“It just comes down to underreporting,” added Valerie L. Baker, MD, director in the Division of Reproductive Endocrinology and Infertility at Johns Hopkins Medicine, Lutherville, Md., who was not affiliated with the study.
“In two of these reports, they failed to transfer the embryo; they actually lost the embryo,” Dr. Pomeroy added. “That’s drastic for those patients; it’s a serious problem that needs to be addressed.”
Citing these findings, the authors underscored the need for heightened surveillance of ETC devices and recommend further studies to assess the sensitivity of these procedures for attempting pregnancy. They urge physicians and lab staff involved in these procedures to exercise continued vigilance and to improve the reporting of problems with ETC devices.
Dr. Madison, Dr. Baker, and Dr. Pomeroy report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a new study presented at the American Society for Reproductive Medicine’s 2023 meeting.
ETCs are medical devices used routinely in assisted reproduction. The findings highlight the need for increased vigilance in tracking and reporting adverse events associated with these devices, according to the investigators.
“With hundreds of thousands of embryo transfers being performed per year, surveillance of the safety, performance, and quality of embryo transfer catheter devices is critical and should not be taken for granted,” said Anita Madison, MD, MPH, from the division of reproductive endocrinology and infertility at Johns Hopkins School of Medicine, Baltimore, who led the study. “There are a variety of transfer catheters with different indications, with little data on the superiority and safety of the brands compared to one another.”
Although the number of reported adverse events associated with ETCs is relatively small, the problems can significantly affect patient care, the researchers said.
Dr. Madison and her colleagues used the Manufacturer and User Facility Device Experience (MAUDE) database to identify adverse events associated with ETC devices. The MAUDE database is a voluntary reporting system that holds hundreds of thousands of medical device reports of suspected device-associated deaths, injuries, and malfunctions reported to the FDA annually.
For each adverse event in the database linked to an ECT, the researchers collected information related to the brand of the device, the nature of the event, and the nature of the reporter. The researchers omitted the device and manufacturer names from the presentation of the study findings, delineating them only as “Brand 1,” “Brand 2,” “Brand 3,” “Brand 4,” or “Other.”
Problems with devices included contamination, packaging problems, malfunction, mechanical flaws, and material separation. Patient-level adverse events included retaining of foreign body, trauma, malfunction, or failed embryo transfer.
Between 2014 and 2023, Dr. Madison and her colleagues identified 101 adverse events associated with ECTs in the database. About 25% of these occurred in 2018, with 27 cases reported. Contamination was the most prevalent problem, found in 68 reports; oil was the most common contaminant.
The distribution of types of adverse events varied, depending on ETC brand. A breakdown of occurrences revealed high numbers for Brand 2, with 52 adverse events. Although Brand 3 accounted for only 16 adverse events, the majority of these were related to device separation.
“That finding stood out,” Dr. Madison said.
Nearly 1 in 4 (22%) of all reported incidents led to overt patient harm. Retention of a foreign body was the prime type of injury, occurring in 12 cases. Malfunction and injury were found in four cases each, with two failed embryo transfers reported, Dr. Madison said.
Because the majority of these adverse event reports were submitted by manufacturers (87%) and were rarely submitted by end users (for example, physicians, lab staff), the researchers said their findings likely underestimate such problems.
“I’m surprised the [number of reported adverse events] is as low as it is,” said Kimball Pomeroy, PhD, scientific director at the World Egg and Sperm Bank, Scottsdale, Ariz., who was not part of the study team. “Laboratories are required to report failed devices; they have to have a plan for that.”
“It just comes down to underreporting,” added Valerie L. Baker, MD, director in the Division of Reproductive Endocrinology and Infertility at Johns Hopkins Medicine, Lutherville, Md., who was not affiliated with the study.
“In two of these reports, they failed to transfer the embryo; they actually lost the embryo,” Dr. Pomeroy added. “That’s drastic for those patients; it’s a serious problem that needs to be addressed.”
Citing these findings, the authors underscored the need for heightened surveillance of ETC devices and recommend further studies to assess the sensitivity of these procedures for attempting pregnancy. They urge physicians and lab staff involved in these procedures to exercise continued vigilance and to improve the reporting of problems with ETC devices.
Dr. Madison, Dr. Baker, and Dr. Pomeroy report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASRM 2023
Perinatal depression rarely stands alone
Mental health conditions are the leading cause of pregnancy-related death in Illinois (40%) and across the United States (21%).1,2 Funding bodies, such as the Agency for Healthcare Research and Quality3 and the Health Resources and Service Administration,4 have spotlights on improving screening and access to care for depression and substance use disorders (SUDs). However, the needs of individuals with multiple mental health conditions still often go unrecognized and unaddressed in perinatal health settings.
The U.S. Preventive Services Task Force recommends that all adults be screened for depression, alcohol use, and drug use, and will be recommending screening for anxiety.5,6 The American College of Obstetrics and Gynecology recommends screening for perinatal mental health conditions including depression, anxiety, bipolar disorder, acute postpartum psychosis, and suicidality; however, despite these recommendations, screening and treatment for comorbid mental health disorders during pregnancy and the postpartum is not standard practice.7
Addressing perinatal mental health is critical because untreated mental health conditions during the perinatal period can cause long-term adverse psychiatric and medical outcomes for the birthing person, the baby, and the family.8 This commentary highlights the importance of recognizing and screening for perinatal mental health comorbidities, improving referral rates for mental health treatment, and raising awareness of the importance of addressing rural perinatal mental health.
Perinatal mental health comorbidities
Major depressive disorder is the most common mental health condition during the perinatal period9 and is often comorbid.10-12 In “Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities,” Craemer et al.13 reported that nearly half of the perinatal patients who screened positive for MDD also screened positive for at least one other mental health condition, among them general anxiety disorder (GAD), SUD, posttraumatic stress disorder (PTSD), and suicidality.
Many (9%) of the perinatal patients with MDD had a severe comorbidity profile characterized by four diagnoses – MDD, GAD, SUD, and PTSD. In routine medical care these comorbidities often go undetected even though the risk to mothers and babies increases with more severe mental health symptoms.8
The high frequency of perinatal mental health comorbidities Craemer et al.13 found demonstrates a compelling need for comorbid mental health screening during the perinatal period, particularly for low-income Black, Hispanic, and rural birthing persons. Positive screens for perinatal mental health disorders may reflect the onset of these disorders in pregnancy or the postpartum, or preexisting disorders that have gone undetected or untreated before pregnancy.
For many patients, the perinatal period is the first time they are screened for any mental health disorder; typically, they are screened solely for depression. Screening alone can have a positive impact on perinatal mental health. In fact, the USPSTF found that programs to screen perinatal patients, with or without treatment-related support, resulted in a 2%-9% absolute reduction in depression prevalence.14 However, screening for MDD is too infrequent for many reasons, including the logistics of integrating screening into the clinic workflow and limited provider availability, time, and training in mental health.
We recommend screening perinatal patients for mental health comorbidities. This recommendation may seem impractical given the lack of screening tools for comorbid mental health conditions; however, the Computerized Adaptive Test for Mental Health (CAT-MH), the validated tool15-17 used in this study, is an ideal option. CAT-MH is uniquely capable of screening for MDD, GAD, PTSD, SUD, and suicidality in one platform and is routinely used in diverse settings including the Veterans Administration,18 foster care,19 and universities.20 The main limitation of this more comprehensive screening is that it takes about 10 minutes per patient. However, CAT-MH is self-administered and can be done in the waiting room or on a mobile device prior to a clinic visit.
CAT-MH can also be easily integrated into clinical workflow when added to the Electronic Medical Record21, and is a more comprehensive tool than existing perinatal depression tools such as the Perinatal Health Questionaire-9 (PHQ-9) and Edinburgh Perinatal Depression Scale (EPDS).22 Another limitation is cost – currently $5.00 per assessment – however, this is less than routine blood work.23 If CAT-MH is not an option, we recommend a stepped approach of screening for GAD when perinatal patients screen positive for MDD, as this is the most common comorbidity profile. The GAD-7 is a free and widely available tool.24
Barriers to care
In Craemer et al,13 nearly two-thirds (64.9%) of perinatal patients with a positive screen did not receive a referral to follow-up care or a medication prescription. These low referral rates may reflect a variety of widely recognized barriers to care, including lack of referral options, provider and/or patient reluctance to pursue referrals, barriers to insurance coverage, or inadequate behavioral health infrastructure to ensure referral and diagnostic follow-up.
Further, rural residing perinatal patients are an underserved population that need more resources and screening. Despite an on-site behavioral specialist at the rural clinic, Craemer et al13 found a stark disparity in referral rates: referrals to treatment for a positive diagnosis was over two times less at the rural clinic (23.9%), compared with the urban clinics (51.6%). The most common treatment offered at the rural clinic was a prescription for medication (17.4%), while referral to follow-up care was the most common at the urban clinics (35.5%). Rural areas not only have a shortage of health care providers, but community members seeking mental health care often encounter greater stigma, compared with urban residents.25,26
These data highlight an unmet need for referrals to treatment for patients in rural communities, particularly in Illinois where the pregnancy-related mortality ratio attributable to mental health conditions is three times greater in rural areas, compared with those residing in urban Cook County (Chicago).2 Increasing access and availability to mental health treatment and prevention resources in Illinois, especially in rural areas, is an opportunity to prevent pregnancy-related mortality attributable to mental health conditions.
Overall, there is a critical need for screening for perinatal mental health comorbidities, increased attention to low rates of referral to mental health treatment, and investing in rural perinatal mental health. Addressing perinatal mental health disorders is key to decreasing the burden of maternal mortality, particularly in Illinois.
Ms. Craemer and Ms. Sayah are senior research specialists at the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Duffecy is a professor of clinical psychiatry at the University of Illinois at Chicago. Dr. Geller is a professor of obstetrics & gynecology and director of the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Maki is a professor of psychiatry, psychology, and obstetrics & gynecology at the University of Illinois at Chicago.
References
1. Trost S et al. Pregnancy-related deaths: Data from maternal mortality review committees in 36 states, 2017-2019. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, 2022.
2. Illinois Department of Public Health. Illinois maternal morbidity and mortality report 2016-2017. 2021.
3. AHRQ. Funding opportunities to address opioid and other substance use disorders. Updated 2023.
4. HRSA. Screening and treatment for maternal mental health and substance use disorders.
5. U.S. Preventive Services Task Force. Recommendations for primary care practice. Accessed May 26, 2023.
6. U.S. Preventive Services Task Force. Draft recommendation statement: Anxiety in adults: Screening. 2022.
7. ACOG. Screening and diagnosis of mental health conditions during pregnancy and postpartum. Clinical Practice Guideline. Number 4. 2023 June.
8. Meltzer-Brody S and Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014 Jan. doi: 10.1016/j.bpobgyn.2013.08.009.
9. Van Niel MS and Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May. doi: 10.3949/ccjm.87a.19054.
10. Wisner KL et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. 2013 May. doi: 10.1001/jamapsychiatry.2013.87.
11. Falah-Hassani K et al. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychol Med. 2017 Sep. doi: 10.1017/S0033291717000617.
12. Pentecost R et al. Scoping review of the associations between perinatal substance use and perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2021 Jul. doi: 10.1016/j.jogn.2021.02.008.
13. Craemer KA et al. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen Hosp Psychiatry. 2023 Jul-Aug. doi: 10.1016/j.genhosppsych.2023.05.007.
14. O’Connor E et al. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016 Jan 26. doi: 10.1001/jama.2015.18948.
15. Kozhimannil KB et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011 Jun. doi: 10.1176/ps.62.6.pss6206_0619.
16. Wenzel ES et al. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch Womens Ment Health. 2021 Dec. doi: 10.1007/s00737-021-01139-y.
17. Gibbons RD et al. Development of a computerized adaptive substance use disorder scale for screening and measurement: The CAT‐SUD. Addiction. 2020 Jul. doi: 10.1111/add.14938.
18. Brenner LA et al. Validation of a computerized adaptive test suicide scale (CAT-SS) among united states military veterans. PloS One. 2022 Jan 21. doi: 10.1371/journal.pone.0261920.
19. The Center for State Child Welfare Data. Using technology to diagnose and report on behavioral health challenges facing foster youth. 2018.
20. Kim JJ et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016 Oct. doi: 10.1007/s00737-016-0632-6.
21. Tepper MC et al. Toward population health: Using a learning behavioral health system and measurement-based care to improve access, care, outcomes, and disparities. Community Ment Health J. 2022 Nov. doi: 10.1007/s10597-022-00957-3.
22. Wenzel E et al. Using computerised adaptive tests to screen for perinatal depression in underserved women of colour. Evid Based Ment Health. 2022 Feb. doi: 10.1136/ebmental-2021-300262.
23. Sanger-Katz M. They want it to be secret: How a common blood test can cost $11 or almost $1,000. New York Times. 2019 Apr 19.
24. Spitzer RL et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006 May 22. doi: 10.1001/archinte.166.10.1092.
25. Mollard E et al. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs. 2016 Jun. doi: 10.1016/j.apnu.2015.12.003.
26. Anglim AJ and Radke SM. Rural maternal health care outcomes, drivers, and patient perspectives. Clin Obstet Gynecol. 2022 Dec 1. doi: 10.1097/GRF.0000000000000753.
Mental health conditions are the leading cause of pregnancy-related death in Illinois (40%) and across the United States (21%).1,2 Funding bodies, such as the Agency for Healthcare Research and Quality3 and the Health Resources and Service Administration,4 have spotlights on improving screening and access to care for depression and substance use disorders (SUDs). However, the needs of individuals with multiple mental health conditions still often go unrecognized and unaddressed in perinatal health settings.
The U.S. Preventive Services Task Force recommends that all adults be screened for depression, alcohol use, and drug use, and will be recommending screening for anxiety.5,6 The American College of Obstetrics and Gynecology recommends screening for perinatal mental health conditions including depression, anxiety, bipolar disorder, acute postpartum psychosis, and suicidality; however, despite these recommendations, screening and treatment for comorbid mental health disorders during pregnancy and the postpartum is not standard practice.7
Addressing perinatal mental health is critical because untreated mental health conditions during the perinatal period can cause long-term adverse psychiatric and medical outcomes for the birthing person, the baby, and the family.8 This commentary highlights the importance of recognizing and screening for perinatal mental health comorbidities, improving referral rates for mental health treatment, and raising awareness of the importance of addressing rural perinatal mental health.
Perinatal mental health comorbidities
Major depressive disorder is the most common mental health condition during the perinatal period9 and is often comorbid.10-12 In “Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities,” Craemer et al.13 reported that nearly half of the perinatal patients who screened positive for MDD also screened positive for at least one other mental health condition, among them general anxiety disorder (GAD), SUD, posttraumatic stress disorder (PTSD), and suicidality.
Many (9%) of the perinatal patients with MDD had a severe comorbidity profile characterized by four diagnoses – MDD, GAD, SUD, and PTSD. In routine medical care these comorbidities often go undetected even though the risk to mothers and babies increases with more severe mental health symptoms.8
The high frequency of perinatal mental health comorbidities Craemer et al.13 found demonstrates a compelling need for comorbid mental health screening during the perinatal period, particularly for low-income Black, Hispanic, and rural birthing persons. Positive screens for perinatal mental health disorders may reflect the onset of these disorders in pregnancy or the postpartum, or preexisting disorders that have gone undetected or untreated before pregnancy.
For many patients, the perinatal period is the first time they are screened for any mental health disorder; typically, they are screened solely for depression. Screening alone can have a positive impact on perinatal mental health. In fact, the USPSTF found that programs to screen perinatal patients, with or without treatment-related support, resulted in a 2%-9% absolute reduction in depression prevalence.14 However, screening for MDD is too infrequent for many reasons, including the logistics of integrating screening into the clinic workflow and limited provider availability, time, and training in mental health.
We recommend screening perinatal patients for mental health comorbidities. This recommendation may seem impractical given the lack of screening tools for comorbid mental health conditions; however, the Computerized Adaptive Test for Mental Health (CAT-MH), the validated tool15-17 used in this study, is an ideal option. CAT-MH is uniquely capable of screening for MDD, GAD, PTSD, SUD, and suicidality in one platform and is routinely used in diverse settings including the Veterans Administration,18 foster care,19 and universities.20 The main limitation of this more comprehensive screening is that it takes about 10 minutes per patient. However, CAT-MH is self-administered and can be done in the waiting room or on a mobile device prior to a clinic visit.
CAT-MH can also be easily integrated into clinical workflow when added to the Electronic Medical Record21, and is a more comprehensive tool than existing perinatal depression tools such as the Perinatal Health Questionaire-9 (PHQ-9) and Edinburgh Perinatal Depression Scale (EPDS).22 Another limitation is cost – currently $5.00 per assessment – however, this is less than routine blood work.23 If CAT-MH is not an option, we recommend a stepped approach of screening for GAD when perinatal patients screen positive for MDD, as this is the most common comorbidity profile. The GAD-7 is a free and widely available tool.24
Barriers to care
In Craemer et al,13 nearly two-thirds (64.9%) of perinatal patients with a positive screen did not receive a referral to follow-up care or a medication prescription. These low referral rates may reflect a variety of widely recognized barriers to care, including lack of referral options, provider and/or patient reluctance to pursue referrals, barriers to insurance coverage, or inadequate behavioral health infrastructure to ensure referral and diagnostic follow-up.
Further, rural residing perinatal patients are an underserved population that need more resources and screening. Despite an on-site behavioral specialist at the rural clinic, Craemer et al13 found a stark disparity in referral rates: referrals to treatment for a positive diagnosis was over two times less at the rural clinic (23.9%), compared with the urban clinics (51.6%). The most common treatment offered at the rural clinic was a prescription for medication (17.4%), while referral to follow-up care was the most common at the urban clinics (35.5%). Rural areas not only have a shortage of health care providers, but community members seeking mental health care often encounter greater stigma, compared with urban residents.25,26
These data highlight an unmet need for referrals to treatment for patients in rural communities, particularly in Illinois where the pregnancy-related mortality ratio attributable to mental health conditions is three times greater in rural areas, compared with those residing in urban Cook County (Chicago).2 Increasing access and availability to mental health treatment and prevention resources in Illinois, especially in rural areas, is an opportunity to prevent pregnancy-related mortality attributable to mental health conditions.
Overall, there is a critical need for screening for perinatal mental health comorbidities, increased attention to low rates of referral to mental health treatment, and investing in rural perinatal mental health. Addressing perinatal mental health disorders is key to decreasing the burden of maternal mortality, particularly in Illinois.
Ms. Craemer and Ms. Sayah are senior research specialists at the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Duffecy is a professor of clinical psychiatry at the University of Illinois at Chicago. Dr. Geller is a professor of obstetrics & gynecology and director of the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Maki is a professor of psychiatry, psychology, and obstetrics & gynecology at the University of Illinois at Chicago.
References
1. Trost S et al. Pregnancy-related deaths: Data from maternal mortality review committees in 36 states, 2017-2019. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, 2022.
2. Illinois Department of Public Health. Illinois maternal morbidity and mortality report 2016-2017. 2021.
3. AHRQ. Funding opportunities to address opioid and other substance use disorders. Updated 2023.
4. HRSA. Screening and treatment for maternal mental health and substance use disorders.
5. U.S. Preventive Services Task Force. Recommendations for primary care practice. Accessed May 26, 2023.
6. U.S. Preventive Services Task Force. Draft recommendation statement: Anxiety in adults: Screening. 2022.
7. ACOG. Screening and diagnosis of mental health conditions during pregnancy and postpartum. Clinical Practice Guideline. Number 4. 2023 June.
8. Meltzer-Brody S and Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014 Jan. doi: 10.1016/j.bpobgyn.2013.08.009.
9. Van Niel MS and Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May. doi: 10.3949/ccjm.87a.19054.
10. Wisner KL et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. 2013 May. doi: 10.1001/jamapsychiatry.2013.87.
11. Falah-Hassani K et al. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychol Med. 2017 Sep. doi: 10.1017/S0033291717000617.
12. Pentecost R et al. Scoping review of the associations between perinatal substance use and perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2021 Jul. doi: 10.1016/j.jogn.2021.02.008.
13. Craemer KA et al. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen Hosp Psychiatry. 2023 Jul-Aug. doi: 10.1016/j.genhosppsych.2023.05.007.
14. O’Connor E et al. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016 Jan 26. doi: 10.1001/jama.2015.18948.
15. Kozhimannil KB et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011 Jun. doi: 10.1176/ps.62.6.pss6206_0619.
16. Wenzel ES et al. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch Womens Ment Health. 2021 Dec. doi: 10.1007/s00737-021-01139-y.
17. Gibbons RD et al. Development of a computerized adaptive substance use disorder scale for screening and measurement: The CAT‐SUD. Addiction. 2020 Jul. doi: 10.1111/add.14938.
18. Brenner LA et al. Validation of a computerized adaptive test suicide scale (CAT-SS) among united states military veterans. PloS One. 2022 Jan 21. doi: 10.1371/journal.pone.0261920.
19. The Center for State Child Welfare Data. Using technology to diagnose and report on behavioral health challenges facing foster youth. 2018.
20. Kim JJ et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016 Oct. doi: 10.1007/s00737-016-0632-6.
21. Tepper MC et al. Toward population health: Using a learning behavioral health system and measurement-based care to improve access, care, outcomes, and disparities. Community Ment Health J. 2022 Nov. doi: 10.1007/s10597-022-00957-3.
22. Wenzel E et al. Using computerised adaptive tests to screen for perinatal depression in underserved women of colour. Evid Based Ment Health. 2022 Feb. doi: 10.1136/ebmental-2021-300262.
23. Sanger-Katz M. They want it to be secret: How a common blood test can cost $11 or almost $1,000. New York Times. 2019 Apr 19.
24. Spitzer RL et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006 May 22. doi: 10.1001/archinte.166.10.1092.
25. Mollard E et al. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs. 2016 Jun. doi: 10.1016/j.apnu.2015.12.003.
26. Anglim AJ and Radke SM. Rural maternal health care outcomes, drivers, and patient perspectives. Clin Obstet Gynecol. 2022 Dec 1. doi: 10.1097/GRF.0000000000000753.
Mental health conditions are the leading cause of pregnancy-related death in Illinois (40%) and across the United States (21%).1,2 Funding bodies, such as the Agency for Healthcare Research and Quality3 and the Health Resources and Service Administration,4 have spotlights on improving screening and access to care for depression and substance use disorders (SUDs). However, the needs of individuals with multiple mental health conditions still often go unrecognized and unaddressed in perinatal health settings.
The U.S. Preventive Services Task Force recommends that all adults be screened for depression, alcohol use, and drug use, and will be recommending screening for anxiety.5,6 The American College of Obstetrics and Gynecology recommends screening for perinatal mental health conditions including depression, anxiety, bipolar disorder, acute postpartum psychosis, and suicidality; however, despite these recommendations, screening and treatment for comorbid mental health disorders during pregnancy and the postpartum is not standard practice.7
Addressing perinatal mental health is critical because untreated mental health conditions during the perinatal period can cause long-term adverse psychiatric and medical outcomes for the birthing person, the baby, and the family.8 This commentary highlights the importance of recognizing and screening for perinatal mental health comorbidities, improving referral rates for mental health treatment, and raising awareness of the importance of addressing rural perinatal mental health.
Perinatal mental health comorbidities
Major depressive disorder is the most common mental health condition during the perinatal period9 and is often comorbid.10-12 In “Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities,” Craemer et al.13 reported that nearly half of the perinatal patients who screened positive for MDD also screened positive for at least one other mental health condition, among them general anxiety disorder (GAD), SUD, posttraumatic stress disorder (PTSD), and suicidality.
Many (9%) of the perinatal patients with MDD had a severe comorbidity profile characterized by four diagnoses – MDD, GAD, SUD, and PTSD. In routine medical care these comorbidities often go undetected even though the risk to mothers and babies increases with more severe mental health symptoms.8
The high frequency of perinatal mental health comorbidities Craemer et al.13 found demonstrates a compelling need for comorbid mental health screening during the perinatal period, particularly for low-income Black, Hispanic, and rural birthing persons. Positive screens for perinatal mental health disorders may reflect the onset of these disorders in pregnancy or the postpartum, or preexisting disorders that have gone undetected or untreated before pregnancy.
For many patients, the perinatal period is the first time they are screened for any mental health disorder; typically, they are screened solely for depression. Screening alone can have a positive impact on perinatal mental health. In fact, the USPSTF found that programs to screen perinatal patients, with or without treatment-related support, resulted in a 2%-9% absolute reduction in depression prevalence.14 However, screening for MDD is too infrequent for many reasons, including the logistics of integrating screening into the clinic workflow and limited provider availability, time, and training in mental health.
We recommend screening perinatal patients for mental health comorbidities. This recommendation may seem impractical given the lack of screening tools for comorbid mental health conditions; however, the Computerized Adaptive Test for Mental Health (CAT-MH), the validated tool15-17 used in this study, is an ideal option. CAT-MH is uniquely capable of screening for MDD, GAD, PTSD, SUD, and suicidality in one platform and is routinely used in diverse settings including the Veterans Administration,18 foster care,19 and universities.20 The main limitation of this more comprehensive screening is that it takes about 10 minutes per patient. However, CAT-MH is self-administered and can be done in the waiting room or on a mobile device prior to a clinic visit.
CAT-MH can also be easily integrated into clinical workflow when added to the Electronic Medical Record21, and is a more comprehensive tool than existing perinatal depression tools such as the Perinatal Health Questionaire-9 (PHQ-9) and Edinburgh Perinatal Depression Scale (EPDS).22 Another limitation is cost – currently $5.00 per assessment – however, this is less than routine blood work.23 If CAT-MH is not an option, we recommend a stepped approach of screening for GAD when perinatal patients screen positive for MDD, as this is the most common comorbidity profile. The GAD-7 is a free and widely available tool.24
Barriers to care
In Craemer et al,13 nearly two-thirds (64.9%) of perinatal patients with a positive screen did not receive a referral to follow-up care or a medication prescription. These low referral rates may reflect a variety of widely recognized barriers to care, including lack of referral options, provider and/or patient reluctance to pursue referrals, barriers to insurance coverage, or inadequate behavioral health infrastructure to ensure referral and diagnostic follow-up.
Further, rural residing perinatal patients are an underserved population that need more resources and screening. Despite an on-site behavioral specialist at the rural clinic, Craemer et al13 found a stark disparity in referral rates: referrals to treatment for a positive diagnosis was over two times less at the rural clinic (23.9%), compared with the urban clinics (51.6%). The most common treatment offered at the rural clinic was a prescription for medication (17.4%), while referral to follow-up care was the most common at the urban clinics (35.5%). Rural areas not only have a shortage of health care providers, but community members seeking mental health care often encounter greater stigma, compared with urban residents.25,26
These data highlight an unmet need for referrals to treatment for patients in rural communities, particularly in Illinois where the pregnancy-related mortality ratio attributable to mental health conditions is three times greater in rural areas, compared with those residing in urban Cook County (Chicago).2 Increasing access and availability to mental health treatment and prevention resources in Illinois, especially in rural areas, is an opportunity to prevent pregnancy-related mortality attributable to mental health conditions.
Overall, there is a critical need for screening for perinatal mental health comorbidities, increased attention to low rates of referral to mental health treatment, and investing in rural perinatal mental health. Addressing perinatal mental health disorders is key to decreasing the burden of maternal mortality, particularly in Illinois.
Ms. Craemer and Ms. Sayah are senior research specialists at the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Duffecy is a professor of clinical psychiatry at the University of Illinois at Chicago. Dr. Geller is a professor of obstetrics & gynecology and director of the Center for Research on Women & Gender, University of Illinois at Chicago. Dr. Maki is a professor of psychiatry, psychology, and obstetrics & gynecology at the University of Illinois at Chicago.
References
1. Trost S et al. Pregnancy-related deaths: Data from maternal mortality review committees in 36 states, 2017-2019. Atlanta: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, 2022.
2. Illinois Department of Public Health. Illinois maternal morbidity and mortality report 2016-2017. 2021.
3. AHRQ. Funding opportunities to address opioid and other substance use disorders. Updated 2023.
4. HRSA. Screening and treatment for maternal mental health and substance use disorders.
5. U.S. Preventive Services Task Force. Recommendations for primary care practice. Accessed May 26, 2023.
6. U.S. Preventive Services Task Force. Draft recommendation statement: Anxiety in adults: Screening. 2022.
7. ACOG. Screening and diagnosis of mental health conditions during pregnancy and postpartum. Clinical Practice Guideline. Number 4. 2023 June.
8. Meltzer-Brody S and Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014 Jan. doi: 10.1016/j.bpobgyn.2013.08.009.
9. Van Niel MS and Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020 May. doi: 10.3949/ccjm.87a.19054.
10. Wisner KL et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. 2013 May. doi: 10.1001/jamapsychiatry.2013.87.
11. Falah-Hassani K et al. The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychol Med. 2017 Sep. doi: 10.1017/S0033291717000617.
12. Pentecost R et al. Scoping review of the associations between perinatal substance use and perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2021 Jul. doi: 10.1016/j.jogn.2021.02.008.
13. Craemer KA et al. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen Hosp Psychiatry. 2023 Jul-Aug. doi: 10.1016/j.genhosppsych.2023.05.007.
14. O’Connor E et al. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016 Jan 26. doi: 10.1001/jama.2015.18948.
15. Kozhimannil KB et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011 Jun. doi: 10.1176/ps.62.6.pss6206_0619.
16. Wenzel ES et al. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch Womens Ment Health. 2021 Dec. doi: 10.1007/s00737-021-01139-y.
17. Gibbons RD et al. Development of a computerized adaptive substance use disorder scale for screening and measurement: The CAT‐SUD. Addiction. 2020 Jul. doi: 10.1111/add.14938.
18. Brenner LA et al. Validation of a computerized adaptive test suicide scale (CAT-SS) among united states military veterans. PloS One. 2022 Jan 21. doi: 10.1371/journal.pone.0261920.
19. The Center for State Child Welfare Data. Using technology to diagnose and report on behavioral health challenges facing foster youth. 2018.
20. Kim JJ et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016 Oct. doi: 10.1007/s00737-016-0632-6.
21. Tepper MC et al. Toward population health: Using a learning behavioral health system and measurement-based care to improve access, care, outcomes, and disparities. Community Ment Health J. 2022 Nov. doi: 10.1007/s10597-022-00957-3.
22. Wenzel E et al. Using computerised adaptive tests to screen for perinatal depression in underserved women of colour. Evid Based Ment Health. 2022 Feb. doi: 10.1136/ebmental-2021-300262.
23. Sanger-Katz M. They want it to be secret: How a common blood test can cost $11 or almost $1,000. New York Times. 2019 Apr 19.
24. Spitzer RL et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006 May 22. doi: 10.1001/archinte.166.10.1092.
25. Mollard E et al. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs. 2016 Jun. doi: 10.1016/j.apnu.2015.12.003.
26. Anglim AJ and Radke SM. Rural maternal health care outcomes, drivers, and patient perspectives. Clin Obstet Gynecol. 2022 Dec 1. doi: 10.1097/GRF.0000000000000753.
Air pollution tied to postpartum depression
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers analyzed data on 340,679 women who had singleton live births at Kaiser Permanente Southern California facilities between 2008 and 2016.
- Ambient air pollution exposures were assessed based on maternal residential addresses using monthly averages of particulate matter ≤ 2.5 mcm (PM2.5), PM ≤ 10 mcm (PM10), nitrogen dioxide, and ozone from Environmental Protection Agency monitoring stations.
- Constituents of PM2.5 (sulfate, nitrate, ammonium, organic matter, and black carbon) were obtained from models based on satellite, ground-based monitor, and chemical transport modeling data.
- Women with an Edinburgh Postnatal Depression Scale score of at least 10 during the first 6 months postpartum were referred for further assessment, including diagnosis and treatment.
TAKEAWAY:
- A total of 25,674 women had PPD (7.5%).
- Positive associations were observed between PPD ozone (adjusted odds ratio, 1.09), PM10 (aOR, 1.02), and PM2.5 (aOR, 1.02), with no statistically significant association with nitrogen dioxide.
- Among PM2.5 constituents, black carbon had the strongest association with PPD (OR 1.04).
- Overall, a higher risk of PPD was associated with ozone exposure during the entire pregnancy and postpartum periods and with PM exposure during the late pregnancy and postpartum periods.
IN PRACTICE:
“These findings suggest that long-term antepartum and postpartum air pollution exposure is a potentially modifiable environmental risk factor for PPD and an important public health issue to address for improved maternal mental health,” the authors wrote.
SOURCE:
The study, with first author Yi Sun, PhD, Chinese Academy of Medical Sciences and Peking Medical College, Beijing, was published online in JAMA Network Open.
LIMITATIONS:
Postpartum exposures were estimated using only maternal address at delivery, which may have led to exposure misclassification. Potential exposure misclassifications may also exist since indoor and personal exposure levels could not be estimated. Although several covariates were adjusted for, some residual or unmeasured covariates were inevitable due to data unavailability, such as psychiatric history, adverse life events, and marital status, which may affect mental health.
DISCLOSURES:
This study was supported by a grant from the National Institute of Environmental Health Sciences. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Obesity boosts gestational diabetes risk in women with PCOS
In a population-based cohort study that included more than 1.2 million hospital live births, PCOS was associated with a 5% increase in risk for gestational diabetes. Almost 90% of this association was mediated by obesity.
“Women with PCOS are at higher risk, but it’s only 5% higher than the general population. However, that risk rises substantially with obesity,” senior author Maria P. Velez, MD, PhD, clinician-scientist and associate professor of obstetrics and gynecology at Queen’s University, Kingston, Ont., said in an interview. “Our study highlights the need for counseling our patients about the importance of weight optimization, ideally starting with lifestyle changes like diet and exercise.”The findings were published in the Journal of Obstetrics and Gynaecology Canada.
Major mediator
The estimated prevalence of PCOS is 8%-13%, and affected patients often present with anovulation, hyperandrogenism, obesity, metabolic syndrome, and infertility. Prepregnancy insulin resistance is common among women with PCOS and may play a major part in the pathogenesis of gestational diabetes. In addition, PCOS is often accompanied by excess weight gain; about 60% of women with PCOS are overweight or obese.
Previous research has shown that PCOS is a risk factor for gestational diabetes independent of obesity, while other research has shown that obesity has an important effect on this risk.
For the current study, the researchers used causal mediation analysis to elucidate more clearly the effect of obesity on the development of gestational diabetes among patients with PCOS. No previous study has used causal mediation analysis to examine this relationship.
Using data from linked universal health databases in Ontario, the researchers analyzed data on 1,268,901 births between 2006 and 2018. Of these births, 386,748 were associated with maternal PCOS.
The rate of gestational diabetes was higher among women with PCOS (60.2 per 1000 births), compared with women without PCOS (48.6 per 1,000 births). The finding resulted in an adjusted relative risk of 1.05. Obesity mediated 89.7% of this association.
“We hope that these data will inform preconception counseling and gestational diabetes screening in pregnant women with PCOS,” said Dr. Velez. “We have the data now to counsel our patients on the importance of weight management before pregnancy. But we need more resources, such as specialized clinics, to help these patients cope with managing their weight. We can tell our patients to work on their weight management, but they need much more support from the health care system.”
Results ‘not surprising’
Commenting on the study, Francine Hippolyte, MD, vice chair of obstetrics and gynecology at Long Island Jewish Medical Center, Katz Women’s Hospital, New Hyde Park, N.Y., said that the results are “not at all surprising.” Dr. Hippolyte was not involved in the research.
“We do know that PCOS is and should be treated as a metabolic syndrome. It’s a lot more than just infertility or changes or abnormalities with one’s menstrual cycle. It impacts a woman’s risk for diabetes, prediabetes, and abnormal lipid profile, regardless of whether or not she is obese,” said Dr. Hippolyte.
She agrees with the need for specialized clinics to help such vulnerable patients manage their weight.
“It would be great if insurances would cover things like nutritional counseling or have nutritionists on their roster so that patients can easily access that service. Many patients want to do right, especially preconceptually, but it is difficult without having access to resources. Unfortunately, as clinicians, we’re not as well versed in nutrition as we would like to be or should be, so we need a multidisciplinary approach. We need nutrition and weight loss clinics and proper services to really help these patients.”
The study was supported by the Canadian Institute of Health Research and ICES. Dr. Velez and Dr. Hippolyte reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a population-based cohort study that included more than 1.2 million hospital live births, PCOS was associated with a 5% increase in risk for gestational diabetes. Almost 90% of this association was mediated by obesity.
“Women with PCOS are at higher risk, but it’s only 5% higher than the general population. However, that risk rises substantially with obesity,” senior author Maria P. Velez, MD, PhD, clinician-scientist and associate professor of obstetrics and gynecology at Queen’s University, Kingston, Ont., said in an interview. “Our study highlights the need for counseling our patients about the importance of weight optimization, ideally starting with lifestyle changes like diet and exercise.”The findings were published in the Journal of Obstetrics and Gynaecology Canada.
Major mediator
The estimated prevalence of PCOS is 8%-13%, and affected patients often present with anovulation, hyperandrogenism, obesity, metabolic syndrome, and infertility. Prepregnancy insulin resistance is common among women with PCOS and may play a major part in the pathogenesis of gestational diabetes. In addition, PCOS is often accompanied by excess weight gain; about 60% of women with PCOS are overweight or obese.
Previous research has shown that PCOS is a risk factor for gestational diabetes independent of obesity, while other research has shown that obesity has an important effect on this risk.
For the current study, the researchers used causal mediation analysis to elucidate more clearly the effect of obesity on the development of gestational diabetes among patients with PCOS. No previous study has used causal mediation analysis to examine this relationship.
Using data from linked universal health databases in Ontario, the researchers analyzed data on 1,268,901 births between 2006 and 2018. Of these births, 386,748 were associated with maternal PCOS.
The rate of gestational diabetes was higher among women with PCOS (60.2 per 1000 births), compared with women without PCOS (48.6 per 1,000 births). The finding resulted in an adjusted relative risk of 1.05. Obesity mediated 89.7% of this association.
“We hope that these data will inform preconception counseling and gestational diabetes screening in pregnant women with PCOS,” said Dr. Velez. “We have the data now to counsel our patients on the importance of weight management before pregnancy. But we need more resources, such as specialized clinics, to help these patients cope with managing their weight. We can tell our patients to work on their weight management, but they need much more support from the health care system.”
Results ‘not surprising’
Commenting on the study, Francine Hippolyte, MD, vice chair of obstetrics and gynecology at Long Island Jewish Medical Center, Katz Women’s Hospital, New Hyde Park, N.Y., said that the results are “not at all surprising.” Dr. Hippolyte was not involved in the research.
“We do know that PCOS is and should be treated as a metabolic syndrome. It’s a lot more than just infertility or changes or abnormalities with one’s menstrual cycle. It impacts a woman’s risk for diabetes, prediabetes, and abnormal lipid profile, regardless of whether or not she is obese,” said Dr. Hippolyte.
She agrees with the need for specialized clinics to help such vulnerable patients manage their weight.
“It would be great if insurances would cover things like nutritional counseling or have nutritionists on their roster so that patients can easily access that service. Many patients want to do right, especially preconceptually, but it is difficult without having access to resources. Unfortunately, as clinicians, we’re not as well versed in nutrition as we would like to be or should be, so we need a multidisciplinary approach. We need nutrition and weight loss clinics and proper services to really help these patients.”
The study was supported by the Canadian Institute of Health Research and ICES. Dr. Velez and Dr. Hippolyte reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a population-based cohort study that included more than 1.2 million hospital live births, PCOS was associated with a 5% increase in risk for gestational diabetes. Almost 90% of this association was mediated by obesity.
“Women with PCOS are at higher risk, but it’s only 5% higher than the general population. However, that risk rises substantially with obesity,” senior author Maria P. Velez, MD, PhD, clinician-scientist and associate professor of obstetrics and gynecology at Queen’s University, Kingston, Ont., said in an interview. “Our study highlights the need for counseling our patients about the importance of weight optimization, ideally starting with lifestyle changes like diet and exercise.”The findings were published in the Journal of Obstetrics and Gynaecology Canada.
Major mediator
The estimated prevalence of PCOS is 8%-13%, and affected patients often present with anovulation, hyperandrogenism, obesity, metabolic syndrome, and infertility. Prepregnancy insulin resistance is common among women with PCOS and may play a major part in the pathogenesis of gestational diabetes. In addition, PCOS is often accompanied by excess weight gain; about 60% of women with PCOS are overweight or obese.
Previous research has shown that PCOS is a risk factor for gestational diabetes independent of obesity, while other research has shown that obesity has an important effect on this risk.
For the current study, the researchers used causal mediation analysis to elucidate more clearly the effect of obesity on the development of gestational diabetes among patients with PCOS. No previous study has used causal mediation analysis to examine this relationship.
Using data from linked universal health databases in Ontario, the researchers analyzed data on 1,268,901 births between 2006 and 2018. Of these births, 386,748 were associated with maternal PCOS.
The rate of gestational diabetes was higher among women with PCOS (60.2 per 1000 births), compared with women without PCOS (48.6 per 1,000 births). The finding resulted in an adjusted relative risk of 1.05. Obesity mediated 89.7% of this association.
“We hope that these data will inform preconception counseling and gestational diabetes screening in pregnant women with PCOS,” said Dr. Velez. “We have the data now to counsel our patients on the importance of weight management before pregnancy. But we need more resources, such as specialized clinics, to help these patients cope with managing their weight. We can tell our patients to work on their weight management, but they need much more support from the health care system.”
Results ‘not surprising’
Commenting on the study, Francine Hippolyte, MD, vice chair of obstetrics and gynecology at Long Island Jewish Medical Center, Katz Women’s Hospital, New Hyde Park, N.Y., said that the results are “not at all surprising.” Dr. Hippolyte was not involved in the research.
“We do know that PCOS is and should be treated as a metabolic syndrome. It’s a lot more than just infertility or changes or abnormalities with one’s menstrual cycle. It impacts a woman’s risk for diabetes, prediabetes, and abnormal lipid profile, regardless of whether or not she is obese,” said Dr. Hippolyte.
She agrees with the need for specialized clinics to help such vulnerable patients manage their weight.
“It would be great if insurances would cover things like nutritional counseling or have nutritionists on their roster so that patients can easily access that service. Many patients want to do right, especially preconceptually, but it is difficult without having access to resources. Unfortunately, as clinicians, we’re not as well versed in nutrition as we would like to be or should be, so we need a multidisciplinary approach. We need nutrition and weight loss clinics and proper services to really help these patients.”
The study was supported by the Canadian Institute of Health Research and ICES. Dr. Velez and Dr. Hippolyte reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF OBSTETRICS AND GYNAECOLOGY CANADA
A dozen genes emerge as dangerous during pregnancy
Single gene disorders remain a leading cause of morbidity and mortality in newborns and children, but carrier screening for such disorders was limited until recent advances in DNA sequencing, wrote Vivienne Souter, MD, of Natera in Austin, Tex., and colleagues.
Identifying single gene disorders in carrier screening also includes the discovery of genetic variants that could affect the carrier parent during pregnancy, they said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 91,637 female patients who underwent testing via a 274-gene carrier screening panel. The median age of the participants was 32.8 years, and approximately half were pregnant at the time of the testing.
Based on previously published reports, the researchers identified 12 genes with potential for carrier manifestations during pregnancy; of these, 9 had manifestations whether or not the fetus was affected by the genetic condition (ABCB11, COL4A3, COL4A4, COL4A5, DMD, F9, F11, GLA, and OTC) and 3 had manifestations only if the fetus was affected by the condition (CPT1A, CYP19A1, and HADHA).
Overall, 66% of the tests were positive for at least one of the 274 genes; the frequency of potentially pathogenic variants for the 12 genes that could manifest as complications during pregnancy ranged from 1 in 117 individuals for the F11 gene to 1 in 8,331 for the OTC gene.
A total of 2.3% of the participant tests were associated a pathogenic or likely pathogenic variant in at least 1 of the 12 genes, which accounted for 3.5% of all positive samples, and 2.0% were identified as carriers for 1 of the 9 genes that could affect women during pregnancy regardless of fetal genetic status.
“People of Ashkenazi Jewish heritage were over-represented in the carrier group, representing 6.0% of carriers but only 1.9% of the entire study cohort,” the researchers noted.
Manifestations related to the 12 genes included cardiomyopathy, hemorrhage, gestational hypertensive disorders, cholestasis of pregnancy, acute fatty liver, hyperammonemic crisis, and maternal virilization.
“The reported incidence of pregnancy complications in carriers ranged from 10% to 62% depending on the gene involved, but information was limited for most of the conditions,” and published literature identified management recommendations for 11 of the 12 genes, the researchers wrote.
The findings were limited by several factors including the use of cases received by the laboratory, which might have yielded more women with above-average risk because of family history, the researchers noted. Other limitations included a lack of data on further evaluation or counseling after the screening, and the lack of separation of the results according to the specific variant, they said. Also, the study population was limited to those who had access to carrier screening, and may not be generalizable to the population at large.
However, the results support the value of carrier screening, and pretest counseling should inform individuals of the potential identification of genes that might increase their risk of complications during pregnancy, the researchers said.
“Obstetric care professionals should also be aware that carrier status for certain conditions can be important for risk assessment and management in pregnancy,” and post-test genetic counseling, follow-up testing, and clinical management can help reduce risks, which could potentially be identified prior to pregnancy, they concluded.
The study was funded by Natera. Dr. Souter is an employee of Natera.
Single gene disorders remain a leading cause of morbidity and mortality in newborns and children, but carrier screening for such disorders was limited until recent advances in DNA sequencing, wrote Vivienne Souter, MD, of Natera in Austin, Tex., and colleagues.
Identifying single gene disorders in carrier screening also includes the discovery of genetic variants that could affect the carrier parent during pregnancy, they said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 91,637 female patients who underwent testing via a 274-gene carrier screening panel. The median age of the participants was 32.8 years, and approximately half were pregnant at the time of the testing.
Based on previously published reports, the researchers identified 12 genes with potential for carrier manifestations during pregnancy; of these, 9 had manifestations whether or not the fetus was affected by the genetic condition (ABCB11, COL4A3, COL4A4, COL4A5, DMD, F9, F11, GLA, and OTC) and 3 had manifestations only if the fetus was affected by the condition (CPT1A, CYP19A1, and HADHA).
Overall, 66% of the tests were positive for at least one of the 274 genes; the frequency of potentially pathogenic variants for the 12 genes that could manifest as complications during pregnancy ranged from 1 in 117 individuals for the F11 gene to 1 in 8,331 for the OTC gene.
A total of 2.3% of the participant tests were associated a pathogenic or likely pathogenic variant in at least 1 of the 12 genes, which accounted for 3.5% of all positive samples, and 2.0% were identified as carriers for 1 of the 9 genes that could affect women during pregnancy regardless of fetal genetic status.
“People of Ashkenazi Jewish heritage were over-represented in the carrier group, representing 6.0% of carriers but only 1.9% of the entire study cohort,” the researchers noted.
Manifestations related to the 12 genes included cardiomyopathy, hemorrhage, gestational hypertensive disorders, cholestasis of pregnancy, acute fatty liver, hyperammonemic crisis, and maternal virilization.
“The reported incidence of pregnancy complications in carriers ranged from 10% to 62% depending on the gene involved, but information was limited for most of the conditions,” and published literature identified management recommendations for 11 of the 12 genes, the researchers wrote.
The findings were limited by several factors including the use of cases received by the laboratory, which might have yielded more women with above-average risk because of family history, the researchers noted. Other limitations included a lack of data on further evaluation or counseling after the screening, and the lack of separation of the results according to the specific variant, they said. Also, the study population was limited to those who had access to carrier screening, and may not be generalizable to the population at large.
However, the results support the value of carrier screening, and pretest counseling should inform individuals of the potential identification of genes that might increase their risk of complications during pregnancy, the researchers said.
“Obstetric care professionals should also be aware that carrier status for certain conditions can be important for risk assessment and management in pregnancy,” and post-test genetic counseling, follow-up testing, and clinical management can help reduce risks, which could potentially be identified prior to pregnancy, they concluded.
The study was funded by Natera. Dr. Souter is an employee of Natera.
Single gene disorders remain a leading cause of morbidity and mortality in newborns and children, but carrier screening for such disorders was limited until recent advances in DNA sequencing, wrote Vivienne Souter, MD, of Natera in Austin, Tex., and colleagues.
Identifying single gene disorders in carrier screening also includes the discovery of genetic variants that could affect the carrier parent during pregnancy, they said.
In a study published in Obstetrics and Gynecology, the researchers reviewed data from 91,637 female patients who underwent testing via a 274-gene carrier screening panel. The median age of the participants was 32.8 years, and approximately half were pregnant at the time of the testing.
Based on previously published reports, the researchers identified 12 genes with potential for carrier manifestations during pregnancy; of these, 9 had manifestations whether or not the fetus was affected by the genetic condition (ABCB11, COL4A3, COL4A4, COL4A5, DMD, F9, F11, GLA, and OTC) and 3 had manifestations only if the fetus was affected by the condition (CPT1A, CYP19A1, and HADHA).
Overall, 66% of the tests were positive for at least one of the 274 genes; the frequency of potentially pathogenic variants for the 12 genes that could manifest as complications during pregnancy ranged from 1 in 117 individuals for the F11 gene to 1 in 8,331 for the OTC gene.
A total of 2.3% of the participant tests were associated a pathogenic or likely pathogenic variant in at least 1 of the 12 genes, which accounted for 3.5% of all positive samples, and 2.0% were identified as carriers for 1 of the 9 genes that could affect women during pregnancy regardless of fetal genetic status.
“People of Ashkenazi Jewish heritage were over-represented in the carrier group, representing 6.0% of carriers but only 1.9% of the entire study cohort,” the researchers noted.
Manifestations related to the 12 genes included cardiomyopathy, hemorrhage, gestational hypertensive disorders, cholestasis of pregnancy, acute fatty liver, hyperammonemic crisis, and maternal virilization.
“The reported incidence of pregnancy complications in carriers ranged from 10% to 62% depending on the gene involved, but information was limited for most of the conditions,” and published literature identified management recommendations for 11 of the 12 genes, the researchers wrote.
The findings were limited by several factors including the use of cases received by the laboratory, which might have yielded more women with above-average risk because of family history, the researchers noted. Other limitations included a lack of data on further evaluation or counseling after the screening, and the lack of separation of the results according to the specific variant, they said. Also, the study population was limited to those who had access to carrier screening, and may not be generalizable to the population at large.
However, the results support the value of carrier screening, and pretest counseling should inform individuals of the potential identification of genes that might increase their risk of complications during pregnancy, the researchers said.
“Obstetric care professionals should also be aware that carrier status for certain conditions can be important for risk assessment and management in pregnancy,” and post-test genetic counseling, follow-up testing, and clinical management can help reduce risks, which could potentially be identified prior to pregnancy, they concluded.
The study was funded by Natera. Dr. Souter is an employee of Natera.
FROM OBSTETRICS & GYNECOLOGY
A focus on women with diabetes and their offspring
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 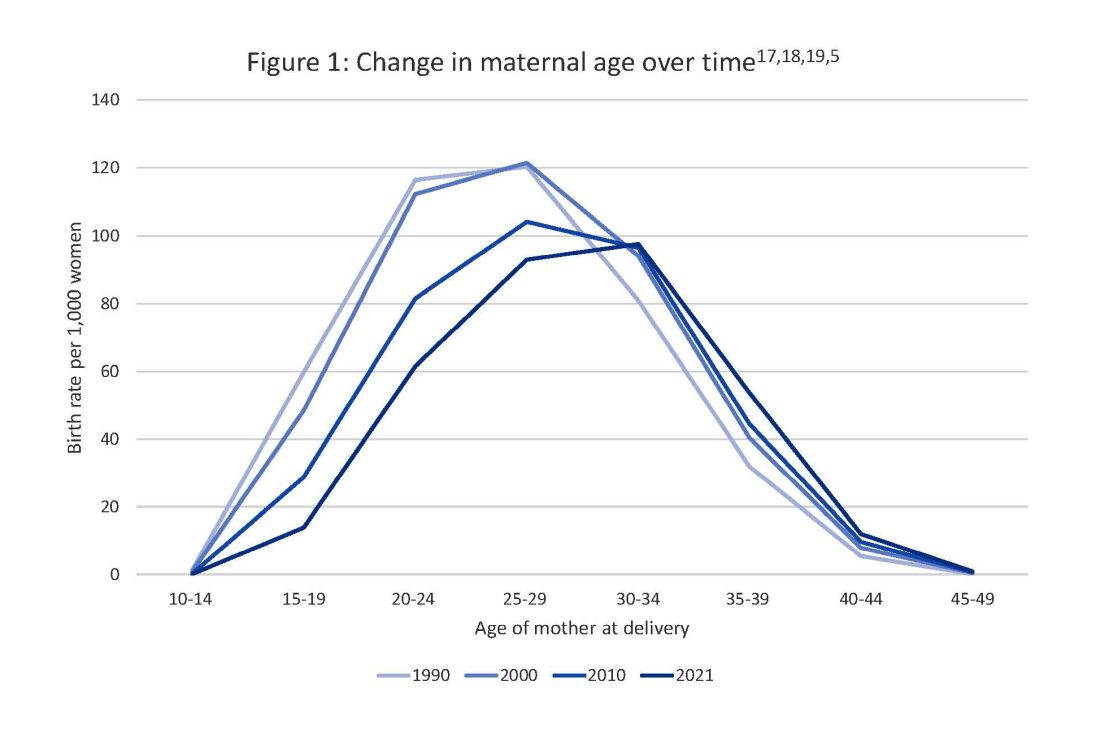
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 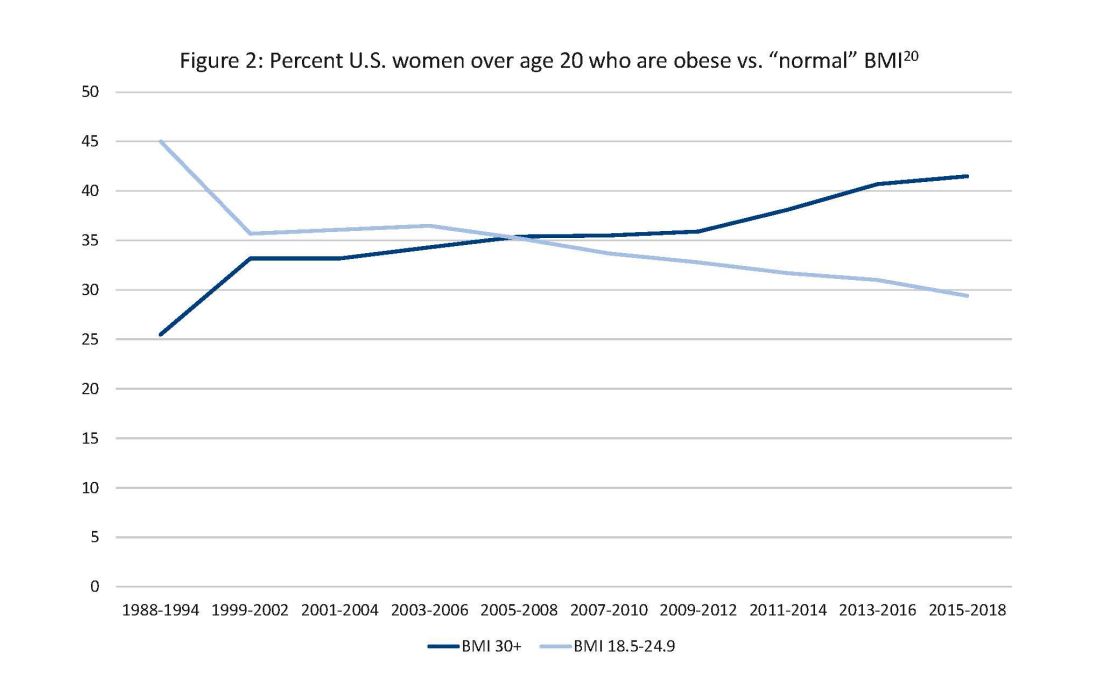
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 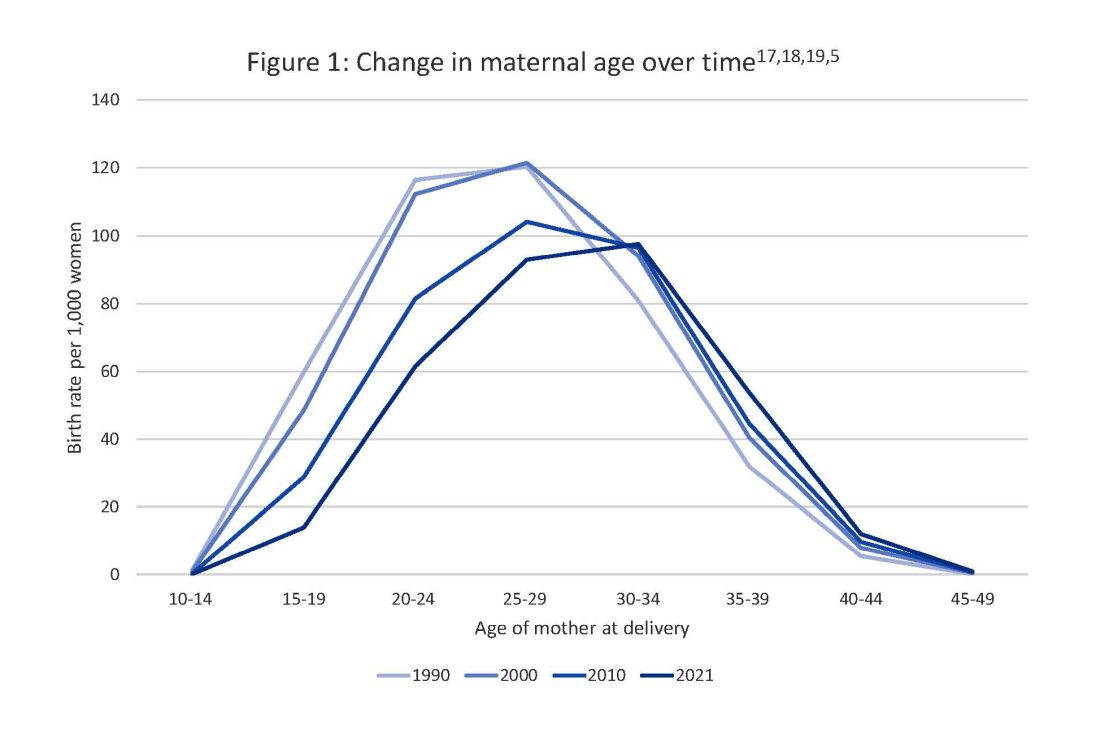
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 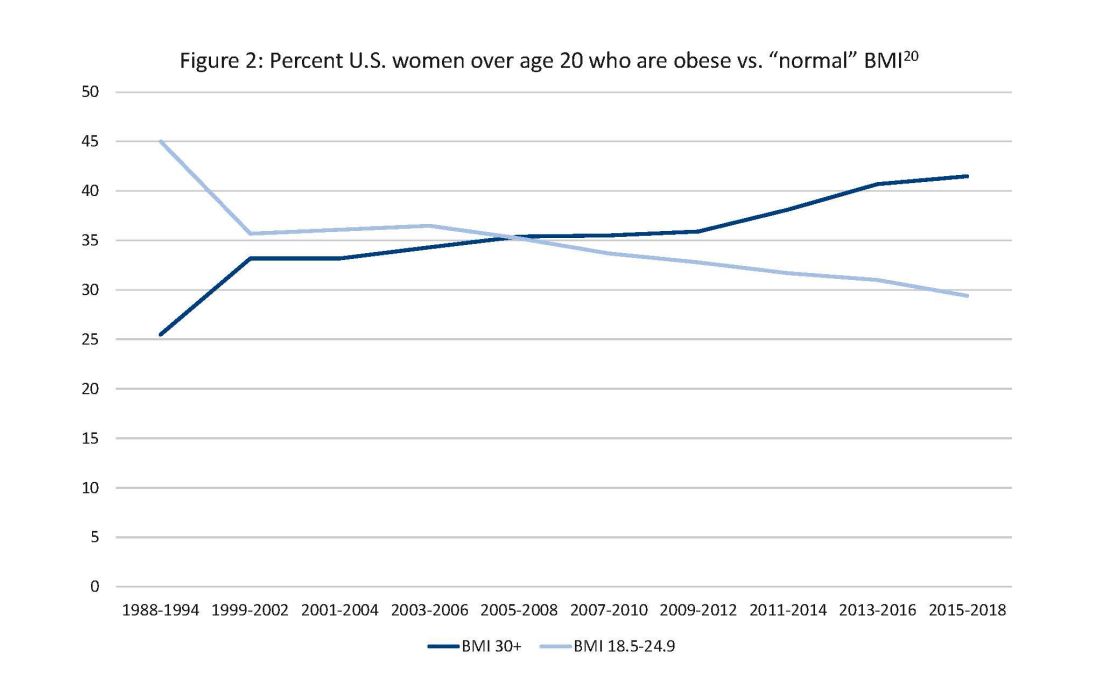
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 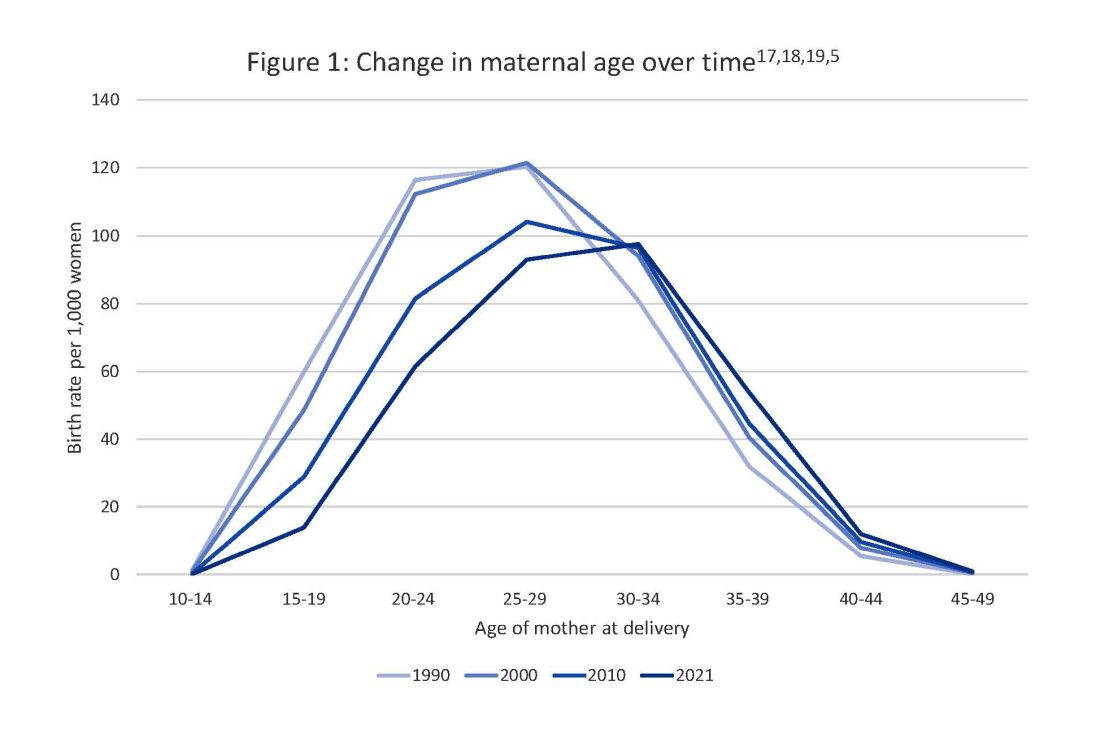
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 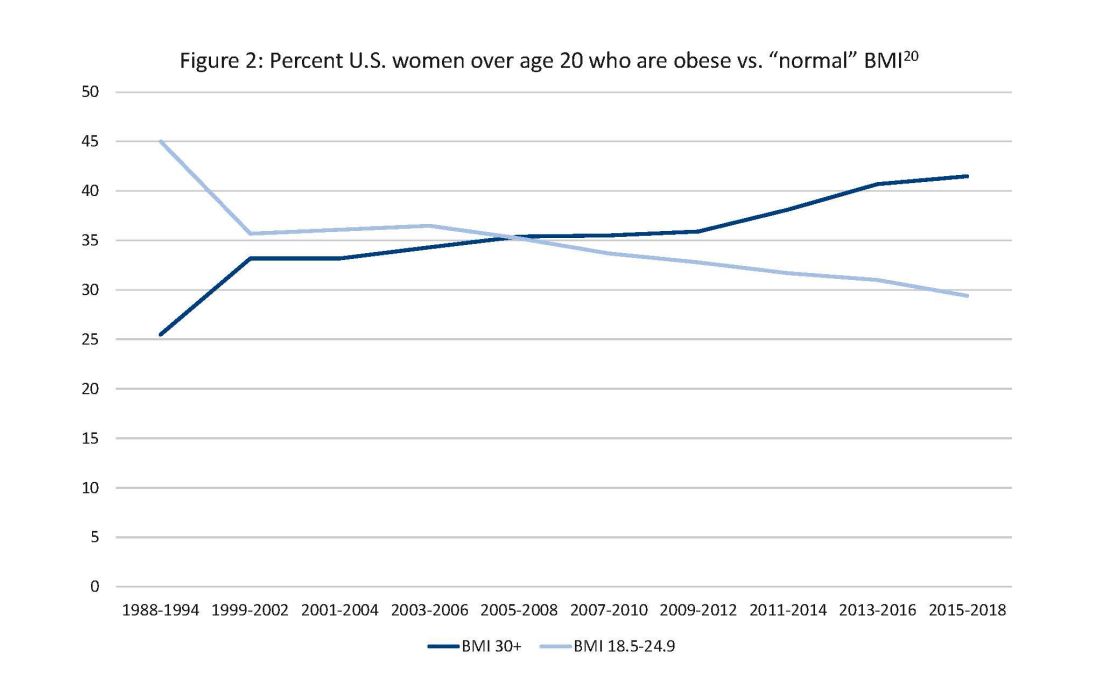
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
Maternal perinatal mortality: A pediatric issue
Checking on the well-being of mothers is one of the important acknowledged aspects of primary pediatric care. “How are you doing?” directed to the child’s mother has long been considered an appropriate question. The AAP recommends several checks in the Bright Futures Guidelines, including conducting several formal screens for depression and asking about “getting time alone with your partner” as well as other supports.
But I have recently become aware of new data that changes my ideas about what we pediatricians need to be doing as part of our care for children and their families, especially in the first year: Considering the risks to the mother of dying.
Maternal mortality increased by 26.6% from 2000 to 2014 across the United States such that it is higher now than it was for our own mothers. The U.S. now has the highest rates of maternal mortality among high-income nations, especially for Black, American Indian, or Alaska Native women, those of lower socioeconomic status, and those under 18 or over 35 years old.
You may be thinking, well, that is an issue for ob.gyns. Indeed, the most common reasons for maternal death are cardiovascular: hemorrhage, hypertensive disorders, deep vein thrombosis, and stroke, all usually occurring at or in the first week after birth. You may have heard about sudden unexpected heart failure from postpartum cardiomyopathy, although rare (1 in 1,000-4,000), presenting from 1 month pre birth to 5 months post delivery, which is when we may be the main clinicians seeing the mother, not the ob.gyns. This can be easily missed since it presents with shortness of breath and decreased exercise tolerance, fatigue, palpitations, and/or leg swelling. Serious eclampsia may have only symptoms of headache or abdominal pain. All of these may easily be mistaken for lingering pregnancy symptoms. But in higher income countries, such as the U.S., 38% of maternal deaths occur from 8 to 42 days after birth, the period for fatal infections as well as cardiac complications. Elevated risk for all of these causes of mortality include Black race, obesity, tobacco use, congenital heart disease, and being older than 40.
As pediatric providers, we may see mothers along with their infants as newborns in the hospital, at day 2, at 2 weeks, or even at 1-2 months after birth, potentially before their one recommended postnatal obstetric visit at 3-8 weeks. Asking the mother how she is feeling at those times should not just be a social nicety but rather an additional check for serious postnatal complications.
Additional concerns
But wait, it gets worse.
Did you know that the leading cause of maternal death from pregnancy up to 1 year after a birth is homicide?
Maternal perinatal mortality figures have not usually included “perinatal-associated” deaths, a maternal death attributable to a condition that is unaffected by the pregnancy and occurring within 1 year of delivery (that I will cite as perinatal henceforth). While half of maternal deaths occur during pregnancy, another half occur in the year following. There were 3.62 homicides per 100,000 live births among females who were pregnant or within 1 year postpartum, 16% more than for similarly aged nonpregnant and nonpostpartum women (3.12 deaths/100,000 population, P < .05). Homicides made up 8.4% of reported perinatal maternal deaths from all causes, with a rate of 1.7 per 100,000 live births, twice the rate of any one of the other leading causes noted above. Black women had seven times the risk of perinatal homicide as that of White women. Females under 20, many of them our own pediatric patients, had a greater than six times higher risk and those aged 20-24 had a 65% higher risk of pregnancy-associated homicide across race and ethnic groups. Homicide is most likely before 21 weeks of pregnancy, decreases in the third trimester, but increases again after birth. Two-thirds of pregnancy-associated homicide deaths occurred in the home, with the perpetrator a current or prior partner (> 59%, with 98% being male), 45%-50% were associated with reported intimate partner violence (IPV), and the most common method was a firearm (55%). Often the same women had histories of substance abuse, serious mental illness, and/or prior IPV, all risk factors for pregnancy-associated deaths, including from homicide.
Homicide? “Not the mothers in my practice,” you may say, but, if not homicide, drug-related deaths (3.68 per 100,000 person-years) and suicide (1.42 per 100,000 person-years) together comprise 18% of all maternal deaths. Non-Hispanic White women, Medicaid-insured women, and women residing in smaller cities were especially likely to die from drugs or suicide. More than half (54.3%) of perinatal suicides involve intimate partner conflict, which increases the risk ninefold. Perinatal mood disorders, affecting up to 15% of pregnant and postpartum U.S. women, is also a risk factor in substance abuse, opioid overdose death, and suicide.
And substance use has gotten more dangerous with the increase in fentanyl lacing. Pregnancy-associated deaths (4%-10% of deaths) involving opioids more than doubled between 2007 and 2016, and, although the rates are higher for Black women, the increase has been greater for non-Hispanic White women. Two-thirds of those deaths occur between 6 and 12 months postpartum, on our watch. Although many women decrease substance use during pregnancy, they may fall back into substance use (rates increase 4 times by 7-12 months after delivery) and not continue to receive treatment. Although pharmacotherapy (e.g., methadone, buprenorphine treatment) is the current standard of care for opioid use disorder (OUD) during pregnancy, nearly half receiving treatment in publicly funded centers are not receiving these medications and others may lose insurance or access to pregnancy-related treatment programs after delivery, increasing risk of relapse. Stigma, and punitive or discriminatory approaches to pregnant women with OUD (e.g., jail, removal of children) can dissuade them from participating in treatment, increasing overdose risk.
It is important to note that in more than half of the 41 deaths from violent trauma in one study (including 22 homicides), obstetrical providers knew of or suspected IPV. Also, the vast majority (74%) of those who died by drugs or suicide had made one or more emergency department or hospital visit between their delivery and death, and 39% had made three or more visits. Without knowing if anything was done in those cases, we also know that, in addition to thorough, compassionate providers, there is sometimes segmentation of responsibility, insensitivity, discrimination, racism, stigma, inequity, lack of resources, lack of access, lack of payment mechanisms, legal issues for immigrants, time constraints, and other systemic deficits that may hinder effective care for these and subsequent women.
Awareness and action
What should we, who are primary care pediatric providers, do about these threats to the mothers and pregnant young women we care for? Clearly, their children, our main patients, would be terribly and permanently hurt by harm coming to their mothers – the extreme adverse childhood experiences and social determinants of health to which we are already committed.
I hope this article will help alert pediatric providers to what is being published, mainly as women’s health and public health issues.
First, we need awareness of the physical symptoms that may come up in our interactions with pregnant and postpartum women so that we can educate them and expedite any indicated emergency care.
Next, we need to expand our routine screening of mothers and pregnant women from just the most impactful social determinants of health (including depression, substance use, and IPV) to include anxiety, past suicide attempts and current suicidal ideation, and the presence of firearms, early and repeatedly in the first year of the child’s life. Adults and teens are more likely to disclose risk for sensitive issues through questionnaires than through interviews, perhaps even more so when the identified patient is their child rather than themselves. Any screen can have false negatives, so asking directly when risk is suspected is important. The reason for screening could be framed as caring for the caregiver who is the most important person for the child. It could be accompanied by acknowledging that pregnancy and the first year of life can be difficult for mothers and their partners and that we want to support them and connect them to resources, if needed. When substance use disorder is acknowledged, we should prescribe and teach about Narcan for overdose. When there is IPV, we should discuss firearm removal/locking as well as counseling on a personal safety plan.
Working as part of an on-site or virtual team that includes professionals who know about community resources and can coordinate care is essential, in addition to educating about 211 for services and 988 for suicide risk.
Finally, we can advocate and vote for programs, people, and laws that support and safeguard women and families, address substance use, and reduce access to firearms.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Checking on the well-being of mothers is one of the important acknowledged aspects of primary pediatric care. “How are you doing?” directed to the child’s mother has long been considered an appropriate question. The AAP recommends several checks in the Bright Futures Guidelines, including conducting several formal screens for depression and asking about “getting time alone with your partner” as well as other supports.
But I have recently become aware of new data that changes my ideas about what we pediatricians need to be doing as part of our care for children and their families, especially in the first year: Considering the risks to the mother of dying.
Maternal mortality increased by 26.6% from 2000 to 2014 across the United States such that it is higher now than it was for our own mothers. The U.S. now has the highest rates of maternal mortality among high-income nations, especially for Black, American Indian, or Alaska Native women, those of lower socioeconomic status, and those under 18 or over 35 years old.
You may be thinking, well, that is an issue for ob.gyns. Indeed, the most common reasons for maternal death are cardiovascular: hemorrhage, hypertensive disorders, deep vein thrombosis, and stroke, all usually occurring at or in the first week after birth. You may have heard about sudden unexpected heart failure from postpartum cardiomyopathy, although rare (1 in 1,000-4,000), presenting from 1 month pre birth to 5 months post delivery, which is when we may be the main clinicians seeing the mother, not the ob.gyns. This can be easily missed since it presents with shortness of breath and decreased exercise tolerance, fatigue, palpitations, and/or leg swelling. Serious eclampsia may have only symptoms of headache or abdominal pain. All of these may easily be mistaken for lingering pregnancy symptoms. But in higher income countries, such as the U.S., 38% of maternal deaths occur from 8 to 42 days after birth, the period for fatal infections as well as cardiac complications. Elevated risk for all of these causes of mortality include Black race, obesity, tobacco use, congenital heart disease, and being older than 40.
As pediatric providers, we may see mothers along with their infants as newborns in the hospital, at day 2, at 2 weeks, or even at 1-2 months after birth, potentially before their one recommended postnatal obstetric visit at 3-8 weeks. Asking the mother how she is feeling at those times should not just be a social nicety but rather an additional check for serious postnatal complications.
Additional concerns
But wait, it gets worse.
Did you know that the leading cause of maternal death from pregnancy up to 1 year after a birth is homicide?
Maternal perinatal mortality figures have not usually included “perinatal-associated” deaths, a maternal death attributable to a condition that is unaffected by the pregnancy and occurring within 1 year of delivery (that I will cite as perinatal henceforth). While half of maternal deaths occur during pregnancy, another half occur in the year following. There were 3.62 homicides per 100,000 live births among females who were pregnant or within 1 year postpartum, 16% more than for similarly aged nonpregnant and nonpostpartum women (3.12 deaths/100,000 population, P < .05). Homicides made up 8.4% of reported perinatal maternal deaths from all causes, with a rate of 1.7 per 100,000 live births, twice the rate of any one of the other leading causes noted above. Black women had seven times the risk of perinatal homicide as that of White women. Females under 20, many of them our own pediatric patients, had a greater than six times higher risk and those aged 20-24 had a 65% higher risk of pregnancy-associated homicide across race and ethnic groups. Homicide is most likely before 21 weeks of pregnancy, decreases in the third trimester, but increases again after birth. Two-thirds of pregnancy-associated homicide deaths occurred in the home, with the perpetrator a current or prior partner (> 59%, with 98% being male), 45%-50% were associated with reported intimate partner violence (IPV), and the most common method was a firearm (55%). Often the same women had histories of substance abuse, serious mental illness, and/or prior IPV, all risk factors for pregnancy-associated deaths, including from homicide.
Homicide? “Not the mothers in my practice,” you may say, but, if not homicide, drug-related deaths (3.68 per 100,000 person-years) and suicide (1.42 per 100,000 person-years) together comprise 18% of all maternal deaths. Non-Hispanic White women, Medicaid-insured women, and women residing in smaller cities were especially likely to die from drugs or suicide. More than half (54.3%) of perinatal suicides involve intimate partner conflict, which increases the risk ninefold. Perinatal mood disorders, affecting up to 15% of pregnant and postpartum U.S. women, is also a risk factor in substance abuse, opioid overdose death, and suicide.
And substance use has gotten more dangerous with the increase in fentanyl lacing. Pregnancy-associated deaths (4%-10% of deaths) involving opioids more than doubled between 2007 and 2016, and, although the rates are higher for Black women, the increase has been greater for non-Hispanic White women. Two-thirds of those deaths occur between 6 and 12 months postpartum, on our watch. Although many women decrease substance use during pregnancy, they may fall back into substance use (rates increase 4 times by 7-12 months after delivery) and not continue to receive treatment. Although pharmacotherapy (e.g., methadone, buprenorphine treatment) is the current standard of care for opioid use disorder (OUD) during pregnancy, nearly half receiving treatment in publicly funded centers are not receiving these medications and others may lose insurance or access to pregnancy-related treatment programs after delivery, increasing risk of relapse. Stigma, and punitive or discriminatory approaches to pregnant women with OUD (e.g., jail, removal of children) can dissuade them from participating in treatment, increasing overdose risk.
It is important to note that in more than half of the 41 deaths from violent trauma in one study (including 22 homicides), obstetrical providers knew of or suspected IPV. Also, the vast majority (74%) of those who died by drugs or suicide had made one or more emergency department or hospital visit between their delivery and death, and 39% had made three or more visits. Without knowing if anything was done in those cases, we also know that, in addition to thorough, compassionate providers, there is sometimes segmentation of responsibility, insensitivity, discrimination, racism, stigma, inequity, lack of resources, lack of access, lack of payment mechanisms, legal issues for immigrants, time constraints, and other systemic deficits that may hinder effective care for these and subsequent women.
Awareness and action
What should we, who are primary care pediatric providers, do about these threats to the mothers and pregnant young women we care for? Clearly, their children, our main patients, would be terribly and permanently hurt by harm coming to their mothers – the extreme adverse childhood experiences and social determinants of health to which we are already committed.
I hope this article will help alert pediatric providers to what is being published, mainly as women’s health and public health issues.
First, we need awareness of the physical symptoms that may come up in our interactions with pregnant and postpartum women so that we can educate them and expedite any indicated emergency care.
Next, we need to expand our routine screening of mothers and pregnant women from just the most impactful social determinants of health (including depression, substance use, and IPV) to include anxiety, past suicide attempts and current suicidal ideation, and the presence of firearms, early and repeatedly in the first year of the child’s life. Adults and teens are more likely to disclose risk for sensitive issues through questionnaires than through interviews, perhaps even more so when the identified patient is their child rather than themselves. Any screen can have false negatives, so asking directly when risk is suspected is important. The reason for screening could be framed as caring for the caregiver who is the most important person for the child. It could be accompanied by acknowledging that pregnancy and the first year of life can be difficult for mothers and their partners and that we want to support them and connect them to resources, if needed. When substance use disorder is acknowledged, we should prescribe and teach about Narcan for overdose. When there is IPV, we should discuss firearm removal/locking as well as counseling on a personal safety plan.
Working as part of an on-site or virtual team that includes professionals who know about community resources and can coordinate care is essential, in addition to educating about 211 for services and 988 for suicide risk.
Finally, we can advocate and vote for programs, people, and laws that support and safeguard women and families, address substance use, and reduce access to firearms.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Checking on the well-being of mothers is one of the important acknowledged aspects of primary pediatric care. “How are you doing?” directed to the child’s mother has long been considered an appropriate question. The AAP recommends several checks in the Bright Futures Guidelines, including conducting several formal screens for depression and asking about “getting time alone with your partner” as well as other supports.
But I have recently become aware of new data that changes my ideas about what we pediatricians need to be doing as part of our care for children and their families, especially in the first year: Considering the risks to the mother of dying.
Maternal mortality increased by 26.6% from 2000 to 2014 across the United States such that it is higher now than it was for our own mothers. The U.S. now has the highest rates of maternal mortality among high-income nations, especially for Black, American Indian, or Alaska Native women, those of lower socioeconomic status, and those under 18 or over 35 years old.
You may be thinking, well, that is an issue for ob.gyns. Indeed, the most common reasons for maternal death are cardiovascular: hemorrhage, hypertensive disorders, deep vein thrombosis, and stroke, all usually occurring at or in the first week after birth. You may have heard about sudden unexpected heart failure from postpartum cardiomyopathy, although rare (1 in 1,000-4,000), presenting from 1 month pre birth to 5 months post delivery, which is when we may be the main clinicians seeing the mother, not the ob.gyns. This can be easily missed since it presents with shortness of breath and decreased exercise tolerance, fatigue, palpitations, and/or leg swelling. Serious eclampsia may have only symptoms of headache or abdominal pain. All of these may easily be mistaken for lingering pregnancy symptoms. But in higher income countries, such as the U.S., 38% of maternal deaths occur from 8 to 42 days after birth, the period for fatal infections as well as cardiac complications. Elevated risk for all of these causes of mortality include Black race, obesity, tobacco use, congenital heart disease, and being older than 40.
As pediatric providers, we may see mothers along with their infants as newborns in the hospital, at day 2, at 2 weeks, or even at 1-2 months after birth, potentially before their one recommended postnatal obstetric visit at 3-8 weeks. Asking the mother how she is feeling at those times should not just be a social nicety but rather an additional check for serious postnatal complications.
Additional concerns
But wait, it gets worse.
Did you know that the leading cause of maternal death from pregnancy up to 1 year after a birth is homicide?
Maternal perinatal mortality figures have not usually included “perinatal-associated” deaths, a maternal death attributable to a condition that is unaffected by the pregnancy and occurring within 1 year of delivery (that I will cite as perinatal henceforth). While half of maternal deaths occur during pregnancy, another half occur in the year following. There were 3.62 homicides per 100,000 live births among females who were pregnant or within 1 year postpartum, 16% more than for similarly aged nonpregnant and nonpostpartum women (3.12 deaths/100,000 population, P < .05). Homicides made up 8.4% of reported perinatal maternal deaths from all causes, with a rate of 1.7 per 100,000 live births, twice the rate of any one of the other leading causes noted above. Black women had seven times the risk of perinatal homicide as that of White women. Females under 20, many of them our own pediatric patients, had a greater than six times higher risk and those aged 20-24 had a 65% higher risk of pregnancy-associated homicide across race and ethnic groups. Homicide is most likely before 21 weeks of pregnancy, decreases in the third trimester, but increases again after birth. Two-thirds of pregnancy-associated homicide deaths occurred in the home, with the perpetrator a current or prior partner (> 59%, with 98% being male), 45%-50% were associated with reported intimate partner violence (IPV), and the most common method was a firearm (55%). Often the same women had histories of substance abuse, serious mental illness, and/or prior IPV, all risk factors for pregnancy-associated deaths, including from homicide.
Homicide? “Not the mothers in my practice,” you may say, but, if not homicide, drug-related deaths (3.68 per 100,000 person-years) and suicide (1.42 per 100,000 person-years) together comprise 18% of all maternal deaths. Non-Hispanic White women, Medicaid-insured women, and women residing in smaller cities were especially likely to die from drugs or suicide. More than half (54.3%) of perinatal suicides involve intimate partner conflict, which increases the risk ninefold. Perinatal mood disorders, affecting up to 15% of pregnant and postpartum U.S. women, is also a risk factor in substance abuse, opioid overdose death, and suicide.
And substance use has gotten more dangerous with the increase in fentanyl lacing. Pregnancy-associated deaths (4%-10% of deaths) involving opioids more than doubled between 2007 and 2016, and, although the rates are higher for Black women, the increase has been greater for non-Hispanic White women. Two-thirds of those deaths occur between 6 and 12 months postpartum, on our watch. Although many women decrease substance use during pregnancy, they may fall back into substance use (rates increase 4 times by 7-12 months after delivery) and not continue to receive treatment. Although pharmacotherapy (e.g., methadone, buprenorphine treatment) is the current standard of care for opioid use disorder (OUD) during pregnancy, nearly half receiving treatment in publicly funded centers are not receiving these medications and others may lose insurance or access to pregnancy-related treatment programs after delivery, increasing risk of relapse. Stigma, and punitive or discriminatory approaches to pregnant women with OUD (e.g., jail, removal of children) can dissuade them from participating in treatment, increasing overdose risk.
It is important to note that in more than half of the 41 deaths from violent trauma in one study (including 22 homicides), obstetrical providers knew of or suspected IPV. Also, the vast majority (74%) of those who died by drugs or suicide had made one or more emergency department or hospital visit between their delivery and death, and 39% had made three or more visits. Without knowing if anything was done in those cases, we also know that, in addition to thorough, compassionate providers, there is sometimes segmentation of responsibility, insensitivity, discrimination, racism, stigma, inequity, lack of resources, lack of access, lack of payment mechanisms, legal issues for immigrants, time constraints, and other systemic deficits that may hinder effective care for these and subsequent women.
Awareness and action
What should we, who are primary care pediatric providers, do about these threats to the mothers and pregnant young women we care for? Clearly, their children, our main patients, would be terribly and permanently hurt by harm coming to their mothers – the extreme adverse childhood experiences and social determinants of health to which we are already committed.
I hope this article will help alert pediatric providers to what is being published, mainly as women’s health and public health issues.
First, we need awareness of the physical symptoms that may come up in our interactions with pregnant and postpartum women so that we can educate them and expedite any indicated emergency care.
Next, we need to expand our routine screening of mothers and pregnant women from just the most impactful social determinants of health (including depression, substance use, and IPV) to include anxiety, past suicide attempts and current suicidal ideation, and the presence of firearms, early and repeatedly in the first year of the child’s life. Adults and teens are more likely to disclose risk for sensitive issues through questionnaires than through interviews, perhaps even more so when the identified patient is their child rather than themselves. Any screen can have false negatives, so asking directly when risk is suspected is important. The reason for screening could be framed as caring for the caregiver who is the most important person for the child. It could be accompanied by acknowledging that pregnancy and the first year of life can be difficult for mothers and their partners and that we want to support them and connect them to resources, if needed. When substance use disorder is acknowledged, we should prescribe and teach about Narcan for overdose. When there is IPV, we should discuss firearm removal/locking as well as counseling on a personal safety plan.
Working as part of an on-site or virtual team that includes professionals who know about community resources and can coordinate care is essential, in addition to educating about 211 for services and 988 for suicide risk.
Finally, we can advocate and vote for programs, people, and laws that support and safeguard women and families, address substance use, and reduce access to firearms.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Biomarkers may help women with RA to decide on medications in pregnancy
Rheumatoid arthritis can’t be cured, but it can significantly improve naturally during pregnancy in 50%-75% of women, prior research has established. It may worsen or stay the same during pregnancy in others.
As of yet, there’s no way to tell which experience a woman with RA will have. RA occurs in 1% of adults globally and is three times more likely to occur in women.
However, a novel study of 19 women with RA suggests that blood biomarkers before pregnancy may predict who will get better or worse during pregnancy. If confirmed with larger studies, the discovery could lead to personalizing medication choices for women with RA who are seeking to become pregnant and change prepregnancy counseling for physicians.
Findings from the research, conducted by first author Matthew Wright, MS, of Children’s Hospital Oakland (Calif.) Research Institute and colleagues were published online in Arthritis Research & Therapy.
A risky choice for women
Currently, the choice is difficult because stopping medications during pregnancy could cause disease flare and continuing could risk possible harm to the baby as some of the medications have toxic side effects.
This is the first study to analyze genetic differences in women with RA who plan to get pregnant, senior author Damini Jawaheer, PhD, research associate professor of medicine in rheumatology at Northwestern University, Chicago, said in an interview.
Identifying women who have the disease and confirming they were planning to get pregnant has been extremely difficult, she noted, especially since the start of their research predated electronic health records (EHRs).
The researchers were able to develop a cohort from work they were already doing with researchers in Denmark, which has a national registry that included both women with RA and women of reproductive age. From there they could contact women about their pregnancy intentions and build the cohort for this study.
Healthy women and women with RA of Danish descent who planned to get pregnant were enrolled and were prospectively followed.
Genetic differences at prepregnancy baseline
Researchers analyzed genetic differences through RNA sequencing before pregnancy from 19 women with RA and 13 healthy women.
Of the 19 women with RA, disease activity improved during pregnancy in 14 and worsened in 5.
Before pregnancy, the researchers found, several neutrophil-related genes were significantly overexpressed in women whose RA later improved during pregnancy. Genes related to B cells were highly expressed among women who worsened. Those elevated B-cell–related gene levels were not seen in the group who improved during pregnancy, Dr. Jawaheer added.
“We don’t understand at this point why that is,” she said.
They also compared the blood samples with women in the control group who did not have RA.
“Comparisons to healthy women revealed that the B-cell signature was specific” to women with worsened RA, the authors wrote. “Thus, at the prepregnancy stage, the two groups of RA women differed significantly from each other in terms of B-cell function.”
Information could help to eliminate fear
Dr. Jawaheer said almost all the women in the cohort who have RA said they were afraid to take medications during pregnancy even if the medications they are taking are considered safe.
“If we could reliably predict who’s going to improve, those women would not have to be scared,” she said. They could stop their medications if they know they’re going to improve naturally.
“Women who are predicted to worsen could then work together with their rheumatologist so that they get treatment to prevent them from getting worse,” Dr. Jawaheer said. “Treatment could be focused on that group only.”
Arthur Kavanaugh, MD, a rheumatologist at University of California San Diego Health and director of the UCSD Center for Innovative Therapy, who was not part of the study, said his patients planning pregnancy struggle with the choices the researchers describe and that investigating potential biomarkers is important.
“Ideally, people would not want to be on anything when they’re pregnant,” he says.
He found the results “intriguing and hypothesis-generating,” but he said the small sample size makes it hard to draw conclusions about the work before it is replicated on a larger scale.
Beth L. Jonas, MD, chief of the division of rheumatology, allergy, and immunology at the University of North Carolina, Chapel Hill, also not a part of the study, said the small study size must be considered, but if the findings are validated in larger studies, the potential is “huge.”
She said doctors used to tell their patients years ago that there’s an excellent chance they will be in remission in pregnancy.
Now, she says, “We’ve tempered our advice to say there’s a good chance you’ll still have disease activity during your pregnancy.”
Rheumatologists would be very interested in a predictive biomarker, she said, as would colleagues in obstetrics/gynecology and maternal-fetal medicine physicians who manage high-risk pregnancies and do prepregnancy counseling.
She said she would also like to see these data followed over multiple pregnancies for each woman, noting that some of her patients have seen RA improve in one pregnancy and worsen in another.
A question she has is, “with a single patient with RA, could you measure this multiple times and get different results?”
Tackling the unanswered questions
Next, the researchers want to conduct the study with a larger sample in the United States and one that is more diverse than the Danish cohort, which included only White patients. Now, Dr. Jawaheer and her team will have the help of EHRs.
A big part of Dr. Jawaheer’s lab’s focus is to find out why many with RA report “never feeling better” during pregnancy – some even experience remission – and why women who improve during pregnancy report that their disease flares 3-6 months after pregnancy, she said.
Her team is also studying what happens biologically when some women worsen in pregnancy.
Those answers “will give us an indication of what could be a potential drug target,” she said.
The authors and Dr. Kavanaugh and Dr. Jonas reported no relevant financial relationships.
Rheumatoid arthritis can’t be cured, but it can significantly improve naturally during pregnancy in 50%-75% of women, prior research has established. It may worsen or stay the same during pregnancy in others.
As of yet, there’s no way to tell which experience a woman with RA will have. RA occurs in 1% of adults globally and is three times more likely to occur in women.
However, a novel study of 19 women with RA suggests that blood biomarkers before pregnancy may predict who will get better or worse during pregnancy. If confirmed with larger studies, the discovery could lead to personalizing medication choices for women with RA who are seeking to become pregnant and change prepregnancy counseling for physicians.
Findings from the research, conducted by first author Matthew Wright, MS, of Children’s Hospital Oakland (Calif.) Research Institute and colleagues were published online in Arthritis Research & Therapy.
A risky choice for women
Currently, the choice is difficult because stopping medications during pregnancy could cause disease flare and continuing could risk possible harm to the baby as some of the medications have toxic side effects.
This is the first study to analyze genetic differences in women with RA who plan to get pregnant, senior author Damini Jawaheer, PhD, research associate professor of medicine in rheumatology at Northwestern University, Chicago, said in an interview.
Identifying women who have the disease and confirming they were planning to get pregnant has been extremely difficult, she noted, especially since the start of their research predated electronic health records (EHRs).
The researchers were able to develop a cohort from work they were already doing with researchers in Denmark, which has a national registry that included both women with RA and women of reproductive age. From there they could contact women about their pregnancy intentions and build the cohort for this study.
Healthy women and women with RA of Danish descent who planned to get pregnant were enrolled and were prospectively followed.
Genetic differences at prepregnancy baseline
Researchers analyzed genetic differences through RNA sequencing before pregnancy from 19 women with RA and 13 healthy women.
Of the 19 women with RA, disease activity improved during pregnancy in 14 and worsened in 5.
Before pregnancy, the researchers found, several neutrophil-related genes were significantly overexpressed in women whose RA later improved during pregnancy. Genes related to B cells were highly expressed among women who worsened. Those elevated B-cell–related gene levels were not seen in the group who improved during pregnancy, Dr. Jawaheer added.
“We don’t understand at this point why that is,” she said.
They also compared the blood samples with women in the control group who did not have RA.
“Comparisons to healthy women revealed that the B-cell signature was specific” to women with worsened RA, the authors wrote. “Thus, at the prepregnancy stage, the two groups of RA women differed significantly from each other in terms of B-cell function.”
Information could help to eliminate fear
Dr. Jawaheer said almost all the women in the cohort who have RA said they were afraid to take medications during pregnancy even if the medications they are taking are considered safe.
“If we could reliably predict who’s going to improve, those women would not have to be scared,” she said. They could stop their medications if they know they’re going to improve naturally.
“Women who are predicted to worsen could then work together with their rheumatologist so that they get treatment to prevent them from getting worse,” Dr. Jawaheer said. “Treatment could be focused on that group only.”
Arthur Kavanaugh, MD, a rheumatologist at University of California San Diego Health and director of the UCSD Center for Innovative Therapy, who was not part of the study, said his patients planning pregnancy struggle with the choices the researchers describe and that investigating potential biomarkers is important.
“Ideally, people would not want to be on anything when they’re pregnant,” he says.
He found the results “intriguing and hypothesis-generating,” but he said the small sample size makes it hard to draw conclusions about the work before it is replicated on a larger scale.
Beth L. Jonas, MD, chief of the division of rheumatology, allergy, and immunology at the University of North Carolina, Chapel Hill, also not a part of the study, said the small study size must be considered, but if the findings are validated in larger studies, the potential is “huge.”
She said doctors used to tell their patients years ago that there’s an excellent chance they will be in remission in pregnancy.
Now, she says, “We’ve tempered our advice to say there’s a good chance you’ll still have disease activity during your pregnancy.”
Rheumatologists would be very interested in a predictive biomarker, she said, as would colleagues in obstetrics/gynecology and maternal-fetal medicine physicians who manage high-risk pregnancies and do prepregnancy counseling.
She said she would also like to see these data followed over multiple pregnancies for each woman, noting that some of her patients have seen RA improve in one pregnancy and worsen in another.
A question she has is, “with a single patient with RA, could you measure this multiple times and get different results?”
Tackling the unanswered questions
Next, the researchers want to conduct the study with a larger sample in the United States and one that is more diverse than the Danish cohort, which included only White patients. Now, Dr. Jawaheer and her team will have the help of EHRs.
A big part of Dr. Jawaheer’s lab’s focus is to find out why many with RA report “never feeling better” during pregnancy – some even experience remission – and why women who improve during pregnancy report that their disease flares 3-6 months after pregnancy, she said.
Her team is also studying what happens biologically when some women worsen in pregnancy.
Those answers “will give us an indication of what could be a potential drug target,” she said.
The authors and Dr. Kavanaugh and Dr. Jonas reported no relevant financial relationships.
Rheumatoid arthritis can’t be cured, but it can significantly improve naturally during pregnancy in 50%-75% of women, prior research has established. It may worsen or stay the same during pregnancy in others.
As of yet, there’s no way to tell which experience a woman with RA will have. RA occurs in 1% of adults globally and is three times more likely to occur in women.
However, a novel study of 19 women with RA suggests that blood biomarkers before pregnancy may predict who will get better or worse during pregnancy. If confirmed with larger studies, the discovery could lead to personalizing medication choices for women with RA who are seeking to become pregnant and change prepregnancy counseling for physicians.
Findings from the research, conducted by first author Matthew Wright, MS, of Children’s Hospital Oakland (Calif.) Research Institute and colleagues were published online in Arthritis Research & Therapy.
A risky choice for women
Currently, the choice is difficult because stopping medications during pregnancy could cause disease flare and continuing could risk possible harm to the baby as some of the medications have toxic side effects.
This is the first study to analyze genetic differences in women with RA who plan to get pregnant, senior author Damini Jawaheer, PhD, research associate professor of medicine in rheumatology at Northwestern University, Chicago, said in an interview.
Identifying women who have the disease and confirming they were planning to get pregnant has been extremely difficult, she noted, especially since the start of their research predated electronic health records (EHRs).
The researchers were able to develop a cohort from work they were already doing with researchers in Denmark, which has a national registry that included both women with RA and women of reproductive age. From there they could contact women about their pregnancy intentions and build the cohort for this study.
Healthy women and women with RA of Danish descent who planned to get pregnant were enrolled and were prospectively followed.
Genetic differences at prepregnancy baseline
Researchers analyzed genetic differences through RNA sequencing before pregnancy from 19 women with RA and 13 healthy women.
Of the 19 women with RA, disease activity improved during pregnancy in 14 and worsened in 5.
Before pregnancy, the researchers found, several neutrophil-related genes were significantly overexpressed in women whose RA later improved during pregnancy. Genes related to B cells were highly expressed among women who worsened. Those elevated B-cell–related gene levels were not seen in the group who improved during pregnancy, Dr. Jawaheer added.
“We don’t understand at this point why that is,” she said.
They also compared the blood samples with women in the control group who did not have RA.
“Comparisons to healthy women revealed that the B-cell signature was specific” to women with worsened RA, the authors wrote. “Thus, at the prepregnancy stage, the two groups of RA women differed significantly from each other in terms of B-cell function.”
Information could help to eliminate fear
Dr. Jawaheer said almost all the women in the cohort who have RA said they were afraid to take medications during pregnancy even if the medications they are taking are considered safe.
“If we could reliably predict who’s going to improve, those women would not have to be scared,” she said. They could stop their medications if they know they’re going to improve naturally.
“Women who are predicted to worsen could then work together with their rheumatologist so that they get treatment to prevent them from getting worse,” Dr. Jawaheer said. “Treatment could be focused on that group only.”
Arthur Kavanaugh, MD, a rheumatologist at University of California San Diego Health and director of the UCSD Center for Innovative Therapy, who was not part of the study, said his patients planning pregnancy struggle with the choices the researchers describe and that investigating potential biomarkers is important.
“Ideally, people would not want to be on anything when they’re pregnant,” he says.
He found the results “intriguing and hypothesis-generating,” but he said the small sample size makes it hard to draw conclusions about the work before it is replicated on a larger scale.
Beth L. Jonas, MD, chief of the division of rheumatology, allergy, and immunology at the University of North Carolina, Chapel Hill, also not a part of the study, said the small study size must be considered, but if the findings are validated in larger studies, the potential is “huge.”
She said doctors used to tell their patients years ago that there’s an excellent chance they will be in remission in pregnancy.
Now, she says, “We’ve tempered our advice to say there’s a good chance you’ll still have disease activity during your pregnancy.”
Rheumatologists would be very interested in a predictive biomarker, she said, as would colleagues in obstetrics/gynecology and maternal-fetal medicine physicians who manage high-risk pregnancies and do prepregnancy counseling.
She said she would also like to see these data followed over multiple pregnancies for each woman, noting that some of her patients have seen RA improve in one pregnancy and worsen in another.
A question she has is, “with a single patient with RA, could you measure this multiple times and get different results?”
Tackling the unanswered questions
Next, the researchers want to conduct the study with a larger sample in the United States and one that is more diverse than the Danish cohort, which included only White patients. Now, Dr. Jawaheer and her team will have the help of EHRs.
A big part of Dr. Jawaheer’s lab’s focus is to find out why many with RA report “never feeling better” during pregnancy – some even experience remission – and why women who improve during pregnancy report that their disease flares 3-6 months after pregnancy, she said.
Her team is also studying what happens biologically when some women worsen in pregnancy.
Those answers “will give us an indication of what could be a potential drug target,” she said.
The authors and Dr. Kavanaugh and Dr. Jonas reported no relevant financial relationships.
FROM ARTHRITIS RESEARCH & THERAPY
Should women of childbearing age eat a plant-based diet?
The prospective cohort study followed 11,459 women older than 18 years and evaluated their diet from the beginning using a validated questionnaire about the frequency and quality of plant-based foods. The participants had taken part in the Nurses’ Health Study II (1991-2009). From responses on the questionnaire, the investigators calculated the plant-based diet index (PDI) even among participants with an omnivorous diet. A higher score indicated greater adherence to the PDI.
“We wanted to know how one’s diet leading up to pregnancy influences the pregnancy, so we monitored women for virtually their entire reproductive life – almost 20 years – and gained an awareness of their typical diet before pregnancy,” study author Jorge E. Chavarro, MD, ScD, told this news organization. Dr. Chavarro is a professor of nutrition, epidemiology, and medicine at Harvard Medical School, Boston, and Harvard University’s School of Public Health in Cambridge, Mass. He researches how nutrition and lifestyle influence reproductive health and overall lifelong health in women.
Analysis of the data from the Nurses’ Health Study II revealed that as the proportion of animal products in diets decreased and the proportion of plant-based products increased, the risk of women experiencing hypertensive disorders of pregnancy decreased as well. Women in the highest PDI quintile had a significantly lower risk of hypertensive disorders of pregnancy, in comparison with those in the lowest quintile (relative risk, 0.76). This association was slightly stronger for pregnancy-related hypertension (RR, 0.77) than for preeclampsia (RR, 0.80).
Women in the highest PDI quintile had a 24% lower risk of hypertensive disorders of pregnancy than those in the lowest quintile; the risk of pregnancy-related hypertension decreased in a linear fashion as PDI increased, while the relationship of PDI to preeclampsia was restricted to women in the quintile with the highest adherence.
“It was clearer for pregnancy-related hypertension than for preeclampsia, but a diet made up primarily of plant-based foods seemed to be protective for both,” said Dr. Chavarro. He added that in addition to the problems these conditions cause during pregnancy, both increase the risk of subsequently developing other chronic diseases. “Could it be that modifiable lifestyle factors before and during pregnancy may not only help reduce problems during gestation but also prevent women’s health problems years later? That was the general motivation for this study.”
Mercedes Sotos-Prieto, PhD, a researcher at the Autonomous University of Madrid and an associate professor at Harvard University’s School of Public Health, told this news organization that the study’s methodology was very robust and that the investigators utilized appropriate statistical techniques for the analysis. She highlighted the fact that they used a validated food frequency questionnaire. She believes the study is also important because of the population group it focused on. “There has always been greater resistance when it comes to the diet of pregnant women, and the same is true for older adults. But we have seen that this type of diet, if it’s a quality diet, may be associated with health benefits.” She did not participate in the study.
Dr. Sotos-Prieto has a doctorate in nutritional epidemiology and public health. She works with large epidemiologic cohorts, such as the cohort of American nurses on which this study was based, and ENRICA, a cohort that is representative of the Spanish population and the population of older adults. She is the author of other studies that, like this one, found an association between a plant-based diet and a lower risk of frailty, both in the study involving American nurses and in a study involving a cohort of individuals aged 60 years or older in Spain (ENRICA-1).
Dr. Sotos-Prieto is also principal investigator on a project assessing the risk of cardiovascular disease based on modifiable lifestyles. For this project, the researchers created a tool, the healthy heart test, that can be used to evaluate diet quality “in 5 minutes, because we all know that doctors don’t have any time.” She thinks this test could be implemented in clinical practice to identify lifestyle behaviors that can be improved, such as by replacing refined cereals with whole grains or increasing legume consumption.
Tomatoes and French fries
The greatest benefit of a plant-based diet comes from the diet overall, not from any single food item. That said, these studies use a scoring system to reflect which items are healthy and which are not.
Diet was assessed every 4 years, starting in 1991, using a semiquantitative food frequency questionnaire that recorded the consumption of 131 foods and drinks during the previous year. The researchers determined the average frequency with which participants consumed each food. Eighteen food groups were sorted into three categories: healthy plant-based foods (whole grains, fruits, vegetables, nuts, legumes, vegetable oils, tea, and coffee), unhealthy plant-based foods (fruit juices, refined grains, potatoes, sugary drinks, sweets, and desserts), and animal-based foods (dairy, eggs, fish or shellfish, meat, and various foods of animal origin).
Healthy plant-based foods were given positive scores, while less healthy plant-based foods and the animal-based food groups were given negative scores. The consumption of each food group was classified into PDI using quintiles.
Women in the highest PDI quintile had a significantly lower risk for hypertensive disorders of pregnancy, compared with women in the lowest quintile. There was a negative dose-response relationship between PDI and risk of the disease. “A vegetarian diet isn’t necessarily healthier than a nonvegetarian diet if it’s made up of superfluous foods like French fries and soft drinks,” said Dr. Sotos-Prieto. “The difference lies in the quality of the plant-based foods. That’s what makes the difference between a healthy and an unhealthy diet.”
Give up meat?
Dr. Chavarro said that removing meat from his dinner menu 22 years ago was one of the hardest things he ever did. “Now, it’s no problem,” he said. But he understands that there are people for whom changing the diet by replacing animal products with nonanimal products is difficult. But meat need not be entirely abandoned.
“The women in the highest quintile aren’t necessarily vegetarian or vegan, but they consume much fewer animal-based foods than the others,” he noted. He added that vegetarian or vegan diets are not incompatible with a healthy pregnancy. “All vegans know how to get vitamin B12 from supplements.”
Diet or weight loss?
Much of the benefit observed in the study appears to be related to better weight control. The body mass index between dietary assessment and pregnancy accounted for 39% of the relationship between PDI and hypertensive disorders of pregnancy and 48% of the relationship between PDI and pregnancy-related hypertension.
“Part of the association seems to be explained by better weight control over long periods,” explained Dr. Chavarro. Women who adopted diets with more plant-based foods gained weight more slowly than those who consumed more animal-based foods. “They are different in terms of their weight trajectory over many years. So, part of the association that we observe is related to better long-term weight control. But the other half of the association is attributable to the diet itself and not necessarily to weight.” The authors suggest mechanisms of action such as endothelial dysfunction, inflammation, or blood pressure before pregnancy to explain the association.
Dr. Sotos-Prieto believes that this point is “extremely relevant.” In her opinion, it reveals that controlling weight at the start of pregnancy is important for pregnant women. Weight control may also improve other factors, like gestational diabetes. “I think preventive measures should focus on that. These results show that interventions are needed to increase the likelihood of going into pregnancy with an appropriate weight. And this includes modifying diet.”
Generalizable results?
More than 90% of the participants in the Nurses’ Health Study were White, not Hispanic. Can the results be extrapolated to other populations? “The answer: The study needs to be repeated in other populations,” said Dr. Chavarro, “and that’s going to take time. But even without that information, I think we can use this study to inform other populations, regardless of ethnicity.”
Dr. Sotos-Prieto admitted that this hypothesis has not yet been tested in the Spanish population, but she is the author of a similar study that followed nearly 12,000 Spanish adults for a decade using the same PDI. In this study, every 10-point increase in PDI was associated with a 14% lower risk of mortality from any cause (hazard ratio, 0.86) and a 37% lower risk of death from cardiovascular disease (HR, 0.63). She also believes that the recommendations derived from the study could be generalized to other populations “as long as each country’s culture is taken into account, to see how it can be culturally adapted. If it’s a population that consumes a lot of refined cereals, for example, make small changes to whole grains.”
Weighing the evidence
The study has strengths and limitations, owing to its methodology, and Dr. Chavarro himself recognizes that “in terms of hypertensive disorders of pregnancy specifically, this won’t be the last word.” But there is a pressing need to find answers.
The American College of Obstetricians and Gynecologists and the World Health Organization encourage women to follow healthy diets before and during pregnancy. But they provide little guidance on what constitutes a healthy diet when it comes to minimizing the risks of adverse pregnancy outcomes. “They are quite ambiguous and vague,” said Dr. Chavarro.
These new findings suggest that plant-based diets may be one such strategy, particularly because some evidence was found that these diets may be beneficial for women older than 35 years, who are considered a high-risk group.
“There are certainly many ways to eat healthily, but if we think about these pregnancy complications that can have serious consequences for the mother and the fetus, we might consider this as a healthy diet option,” Dr. Chavarro noted.
But is the evidence robust enough to recommend that patients make changes? “Ideally, there will be more studies,” stated Dr. Chavarro. “There are two ways to understand the problem. One is not making recommendations until you have three controlled clinical trials, which, even with the willingness and funding to do so, will take 15-20 years. But if we have to provide the best available information to those who need it today, I think these are solid results for guiding behavior.
“It’s always better if we can make decisions based on solid, incontrovertible information. But it’s not always available, and you must learn to live in both worlds and make decisions with uncertainties,” he concluded.
Dr. Sotos-Prieto and Dr. Chavarro have disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version of this article first appeared on Medscape.com.
The prospective cohort study followed 11,459 women older than 18 years and evaluated their diet from the beginning using a validated questionnaire about the frequency and quality of plant-based foods. The participants had taken part in the Nurses’ Health Study II (1991-2009). From responses on the questionnaire, the investigators calculated the plant-based diet index (PDI) even among participants with an omnivorous diet. A higher score indicated greater adherence to the PDI.
“We wanted to know how one’s diet leading up to pregnancy influences the pregnancy, so we monitored women for virtually their entire reproductive life – almost 20 years – and gained an awareness of their typical diet before pregnancy,” study author Jorge E. Chavarro, MD, ScD, told this news organization. Dr. Chavarro is a professor of nutrition, epidemiology, and medicine at Harvard Medical School, Boston, and Harvard University’s School of Public Health in Cambridge, Mass. He researches how nutrition and lifestyle influence reproductive health and overall lifelong health in women.
Analysis of the data from the Nurses’ Health Study II revealed that as the proportion of animal products in diets decreased and the proportion of plant-based products increased, the risk of women experiencing hypertensive disorders of pregnancy decreased as well. Women in the highest PDI quintile had a significantly lower risk of hypertensive disorders of pregnancy, in comparison with those in the lowest quintile (relative risk, 0.76). This association was slightly stronger for pregnancy-related hypertension (RR, 0.77) than for preeclampsia (RR, 0.80).
Women in the highest PDI quintile had a 24% lower risk of hypertensive disorders of pregnancy than those in the lowest quintile; the risk of pregnancy-related hypertension decreased in a linear fashion as PDI increased, while the relationship of PDI to preeclampsia was restricted to women in the quintile with the highest adherence.
“It was clearer for pregnancy-related hypertension than for preeclampsia, but a diet made up primarily of plant-based foods seemed to be protective for both,” said Dr. Chavarro. He added that in addition to the problems these conditions cause during pregnancy, both increase the risk of subsequently developing other chronic diseases. “Could it be that modifiable lifestyle factors before and during pregnancy may not only help reduce problems during gestation but also prevent women’s health problems years later? That was the general motivation for this study.”
Mercedes Sotos-Prieto, PhD, a researcher at the Autonomous University of Madrid and an associate professor at Harvard University’s School of Public Health, told this news organization that the study’s methodology was very robust and that the investigators utilized appropriate statistical techniques for the analysis. She highlighted the fact that they used a validated food frequency questionnaire. She believes the study is also important because of the population group it focused on. “There has always been greater resistance when it comes to the diet of pregnant women, and the same is true for older adults. But we have seen that this type of diet, if it’s a quality diet, may be associated with health benefits.” She did not participate in the study.
Dr. Sotos-Prieto has a doctorate in nutritional epidemiology and public health. She works with large epidemiologic cohorts, such as the cohort of American nurses on which this study was based, and ENRICA, a cohort that is representative of the Spanish population and the population of older adults. She is the author of other studies that, like this one, found an association between a plant-based diet and a lower risk of frailty, both in the study involving American nurses and in a study involving a cohort of individuals aged 60 years or older in Spain (ENRICA-1).
Dr. Sotos-Prieto is also principal investigator on a project assessing the risk of cardiovascular disease based on modifiable lifestyles. For this project, the researchers created a tool, the healthy heart test, that can be used to evaluate diet quality “in 5 minutes, because we all know that doctors don’t have any time.” She thinks this test could be implemented in clinical practice to identify lifestyle behaviors that can be improved, such as by replacing refined cereals with whole grains or increasing legume consumption.
Tomatoes and French fries
The greatest benefit of a plant-based diet comes from the diet overall, not from any single food item. That said, these studies use a scoring system to reflect which items are healthy and which are not.
Diet was assessed every 4 years, starting in 1991, using a semiquantitative food frequency questionnaire that recorded the consumption of 131 foods and drinks during the previous year. The researchers determined the average frequency with which participants consumed each food. Eighteen food groups were sorted into three categories: healthy plant-based foods (whole grains, fruits, vegetables, nuts, legumes, vegetable oils, tea, and coffee), unhealthy plant-based foods (fruit juices, refined grains, potatoes, sugary drinks, sweets, and desserts), and animal-based foods (dairy, eggs, fish or shellfish, meat, and various foods of animal origin).
Healthy plant-based foods were given positive scores, while less healthy plant-based foods and the animal-based food groups were given negative scores. The consumption of each food group was classified into PDI using quintiles.
Women in the highest PDI quintile had a significantly lower risk for hypertensive disorders of pregnancy, compared with women in the lowest quintile. There was a negative dose-response relationship between PDI and risk of the disease. “A vegetarian diet isn’t necessarily healthier than a nonvegetarian diet if it’s made up of superfluous foods like French fries and soft drinks,” said Dr. Sotos-Prieto. “The difference lies in the quality of the plant-based foods. That’s what makes the difference between a healthy and an unhealthy diet.”
Give up meat?
Dr. Chavarro said that removing meat from his dinner menu 22 years ago was one of the hardest things he ever did. “Now, it’s no problem,” he said. But he understands that there are people for whom changing the diet by replacing animal products with nonanimal products is difficult. But meat need not be entirely abandoned.
“The women in the highest quintile aren’t necessarily vegetarian or vegan, but they consume much fewer animal-based foods than the others,” he noted. He added that vegetarian or vegan diets are not incompatible with a healthy pregnancy. “All vegans know how to get vitamin B12 from supplements.”
Diet or weight loss?
Much of the benefit observed in the study appears to be related to better weight control. The body mass index between dietary assessment and pregnancy accounted for 39% of the relationship between PDI and hypertensive disorders of pregnancy and 48% of the relationship between PDI and pregnancy-related hypertension.
“Part of the association seems to be explained by better weight control over long periods,” explained Dr. Chavarro. Women who adopted diets with more plant-based foods gained weight more slowly than those who consumed more animal-based foods. “They are different in terms of their weight trajectory over many years. So, part of the association that we observe is related to better long-term weight control. But the other half of the association is attributable to the diet itself and not necessarily to weight.” The authors suggest mechanisms of action such as endothelial dysfunction, inflammation, or blood pressure before pregnancy to explain the association.
Dr. Sotos-Prieto believes that this point is “extremely relevant.” In her opinion, it reveals that controlling weight at the start of pregnancy is important for pregnant women. Weight control may also improve other factors, like gestational diabetes. “I think preventive measures should focus on that. These results show that interventions are needed to increase the likelihood of going into pregnancy with an appropriate weight. And this includes modifying diet.”
Generalizable results?
More than 90% of the participants in the Nurses’ Health Study were White, not Hispanic. Can the results be extrapolated to other populations? “The answer: The study needs to be repeated in other populations,” said Dr. Chavarro, “and that’s going to take time. But even without that information, I think we can use this study to inform other populations, regardless of ethnicity.”
Dr. Sotos-Prieto admitted that this hypothesis has not yet been tested in the Spanish population, but she is the author of a similar study that followed nearly 12,000 Spanish adults for a decade using the same PDI. In this study, every 10-point increase in PDI was associated with a 14% lower risk of mortality from any cause (hazard ratio, 0.86) and a 37% lower risk of death from cardiovascular disease (HR, 0.63). She also believes that the recommendations derived from the study could be generalized to other populations “as long as each country’s culture is taken into account, to see how it can be culturally adapted. If it’s a population that consumes a lot of refined cereals, for example, make small changes to whole grains.”
Weighing the evidence
The study has strengths and limitations, owing to its methodology, and Dr. Chavarro himself recognizes that “in terms of hypertensive disorders of pregnancy specifically, this won’t be the last word.” But there is a pressing need to find answers.
The American College of Obstetricians and Gynecologists and the World Health Organization encourage women to follow healthy diets before and during pregnancy. But they provide little guidance on what constitutes a healthy diet when it comes to minimizing the risks of adverse pregnancy outcomes. “They are quite ambiguous and vague,” said Dr. Chavarro.
These new findings suggest that plant-based diets may be one such strategy, particularly because some evidence was found that these diets may be beneficial for women older than 35 years, who are considered a high-risk group.
“There are certainly many ways to eat healthily, but if we think about these pregnancy complications that can have serious consequences for the mother and the fetus, we might consider this as a healthy diet option,” Dr. Chavarro noted.
But is the evidence robust enough to recommend that patients make changes? “Ideally, there will be more studies,” stated Dr. Chavarro. “There are two ways to understand the problem. One is not making recommendations until you have three controlled clinical trials, which, even with the willingness and funding to do so, will take 15-20 years. But if we have to provide the best available information to those who need it today, I think these are solid results for guiding behavior.
“It’s always better if we can make decisions based on solid, incontrovertible information. But it’s not always available, and you must learn to live in both worlds and make decisions with uncertainties,” he concluded.
Dr. Sotos-Prieto and Dr. Chavarro have disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version of this article first appeared on Medscape.com.
The prospective cohort study followed 11,459 women older than 18 years and evaluated their diet from the beginning using a validated questionnaire about the frequency and quality of plant-based foods. The participants had taken part in the Nurses’ Health Study II (1991-2009). From responses on the questionnaire, the investigators calculated the plant-based diet index (PDI) even among participants with an omnivorous diet. A higher score indicated greater adherence to the PDI.
“We wanted to know how one’s diet leading up to pregnancy influences the pregnancy, so we monitored women for virtually their entire reproductive life – almost 20 years – and gained an awareness of their typical diet before pregnancy,” study author Jorge E. Chavarro, MD, ScD, told this news organization. Dr. Chavarro is a professor of nutrition, epidemiology, and medicine at Harvard Medical School, Boston, and Harvard University’s School of Public Health in Cambridge, Mass. He researches how nutrition and lifestyle influence reproductive health and overall lifelong health in women.
Analysis of the data from the Nurses’ Health Study II revealed that as the proportion of animal products in diets decreased and the proportion of plant-based products increased, the risk of women experiencing hypertensive disorders of pregnancy decreased as well. Women in the highest PDI quintile had a significantly lower risk of hypertensive disorders of pregnancy, in comparison with those in the lowest quintile (relative risk, 0.76). This association was slightly stronger for pregnancy-related hypertension (RR, 0.77) than for preeclampsia (RR, 0.80).
Women in the highest PDI quintile had a 24% lower risk of hypertensive disorders of pregnancy than those in the lowest quintile; the risk of pregnancy-related hypertension decreased in a linear fashion as PDI increased, while the relationship of PDI to preeclampsia was restricted to women in the quintile with the highest adherence.
“It was clearer for pregnancy-related hypertension than for preeclampsia, but a diet made up primarily of plant-based foods seemed to be protective for both,” said Dr. Chavarro. He added that in addition to the problems these conditions cause during pregnancy, both increase the risk of subsequently developing other chronic diseases. “Could it be that modifiable lifestyle factors before and during pregnancy may not only help reduce problems during gestation but also prevent women’s health problems years later? That was the general motivation for this study.”
Mercedes Sotos-Prieto, PhD, a researcher at the Autonomous University of Madrid and an associate professor at Harvard University’s School of Public Health, told this news organization that the study’s methodology was very robust and that the investigators utilized appropriate statistical techniques for the analysis. She highlighted the fact that they used a validated food frequency questionnaire. She believes the study is also important because of the population group it focused on. “There has always been greater resistance when it comes to the diet of pregnant women, and the same is true for older adults. But we have seen that this type of diet, if it’s a quality diet, may be associated with health benefits.” She did not participate in the study.
Dr. Sotos-Prieto has a doctorate in nutritional epidemiology and public health. She works with large epidemiologic cohorts, such as the cohort of American nurses on which this study was based, and ENRICA, a cohort that is representative of the Spanish population and the population of older adults. She is the author of other studies that, like this one, found an association between a plant-based diet and a lower risk of frailty, both in the study involving American nurses and in a study involving a cohort of individuals aged 60 years or older in Spain (ENRICA-1).
Dr. Sotos-Prieto is also principal investigator on a project assessing the risk of cardiovascular disease based on modifiable lifestyles. For this project, the researchers created a tool, the healthy heart test, that can be used to evaluate diet quality “in 5 minutes, because we all know that doctors don’t have any time.” She thinks this test could be implemented in clinical practice to identify lifestyle behaviors that can be improved, such as by replacing refined cereals with whole grains or increasing legume consumption.
Tomatoes and French fries
The greatest benefit of a plant-based diet comes from the diet overall, not from any single food item. That said, these studies use a scoring system to reflect which items are healthy and which are not.
Diet was assessed every 4 years, starting in 1991, using a semiquantitative food frequency questionnaire that recorded the consumption of 131 foods and drinks during the previous year. The researchers determined the average frequency with which participants consumed each food. Eighteen food groups were sorted into three categories: healthy plant-based foods (whole grains, fruits, vegetables, nuts, legumes, vegetable oils, tea, and coffee), unhealthy plant-based foods (fruit juices, refined grains, potatoes, sugary drinks, sweets, and desserts), and animal-based foods (dairy, eggs, fish or shellfish, meat, and various foods of animal origin).
Healthy plant-based foods were given positive scores, while less healthy plant-based foods and the animal-based food groups were given negative scores. The consumption of each food group was classified into PDI using quintiles.
Women in the highest PDI quintile had a significantly lower risk for hypertensive disorders of pregnancy, compared with women in the lowest quintile. There was a negative dose-response relationship between PDI and risk of the disease. “A vegetarian diet isn’t necessarily healthier than a nonvegetarian diet if it’s made up of superfluous foods like French fries and soft drinks,” said Dr. Sotos-Prieto. “The difference lies in the quality of the plant-based foods. That’s what makes the difference between a healthy and an unhealthy diet.”
Give up meat?
Dr. Chavarro said that removing meat from his dinner menu 22 years ago was one of the hardest things he ever did. “Now, it’s no problem,” he said. But he understands that there are people for whom changing the diet by replacing animal products with nonanimal products is difficult. But meat need not be entirely abandoned.
“The women in the highest quintile aren’t necessarily vegetarian or vegan, but they consume much fewer animal-based foods than the others,” he noted. He added that vegetarian or vegan diets are not incompatible with a healthy pregnancy. “All vegans know how to get vitamin B12 from supplements.”
Diet or weight loss?
Much of the benefit observed in the study appears to be related to better weight control. The body mass index between dietary assessment and pregnancy accounted for 39% of the relationship between PDI and hypertensive disorders of pregnancy and 48% of the relationship between PDI and pregnancy-related hypertension.
“Part of the association seems to be explained by better weight control over long periods,” explained Dr. Chavarro. Women who adopted diets with more plant-based foods gained weight more slowly than those who consumed more animal-based foods. “They are different in terms of their weight trajectory over many years. So, part of the association that we observe is related to better long-term weight control. But the other half of the association is attributable to the diet itself and not necessarily to weight.” The authors suggest mechanisms of action such as endothelial dysfunction, inflammation, or blood pressure before pregnancy to explain the association.
Dr. Sotos-Prieto believes that this point is “extremely relevant.” In her opinion, it reveals that controlling weight at the start of pregnancy is important for pregnant women. Weight control may also improve other factors, like gestational diabetes. “I think preventive measures should focus on that. These results show that interventions are needed to increase the likelihood of going into pregnancy with an appropriate weight. And this includes modifying diet.”
Generalizable results?
More than 90% of the participants in the Nurses’ Health Study were White, not Hispanic. Can the results be extrapolated to other populations? “The answer: The study needs to be repeated in other populations,” said Dr. Chavarro, “and that’s going to take time. But even without that information, I think we can use this study to inform other populations, regardless of ethnicity.”
Dr. Sotos-Prieto admitted that this hypothesis has not yet been tested in the Spanish population, but she is the author of a similar study that followed nearly 12,000 Spanish adults for a decade using the same PDI. In this study, every 10-point increase in PDI was associated with a 14% lower risk of mortality from any cause (hazard ratio, 0.86) and a 37% lower risk of death from cardiovascular disease (HR, 0.63). She also believes that the recommendations derived from the study could be generalized to other populations “as long as each country’s culture is taken into account, to see how it can be culturally adapted. If it’s a population that consumes a lot of refined cereals, for example, make small changes to whole grains.”
Weighing the evidence
The study has strengths and limitations, owing to its methodology, and Dr. Chavarro himself recognizes that “in terms of hypertensive disorders of pregnancy specifically, this won’t be the last word.” But there is a pressing need to find answers.
The American College of Obstetricians and Gynecologists and the World Health Organization encourage women to follow healthy diets before and during pregnancy. But they provide little guidance on what constitutes a healthy diet when it comes to minimizing the risks of adverse pregnancy outcomes. “They are quite ambiguous and vague,” said Dr. Chavarro.
These new findings suggest that plant-based diets may be one such strategy, particularly because some evidence was found that these diets may be beneficial for women older than 35 years, who are considered a high-risk group.
“There are certainly many ways to eat healthily, but if we think about these pregnancy complications that can have serious consequences for the mother and the fetus, we might consider this as a healthy diet option,” Dr. Chavarro noted.
But is the evidence robust enough to recommend that patients make changes? “Ideally, there will be more studies,” stated Dr. Chavarro. “There are two ways to understand the problem. One is not making recommendations until you have three controlled clinical trials, which, even with the willingness and funding to do so, will take 15-20 years. But if we have to provide the best available information to those who need it today, I think these are solid results for guiding behavior.
“It’s always better if we can make decisions based on solid, incontrovertible information. But it’s not always available, and you must learn to live in both worlds and make decisions with uncertainties,” he concluded.
Dr. Sotos-Prieto and Dr. Chavarro have disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY













