User login
All isn’t well with HIV-exposed uninfected infants
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
AT ESPID 2017
Key clinical point:
Major finding: The rate of hospitalization for a serious infectious illness during the first 12 months of life was 21% in HIV-exposed uninfected children, significantly greater than the 11% rate in HIV-unexposed babies.
Data source: This prospective observational study included 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds and their offspring, followed to date through the infants’ first birthday.
Disclosures: Dr. Adler reported having no financial conflicts of interest.
Intra-amniotic sludge: Does its presence rule out cerclage for short cervix?
CASE: Woman with short cervix, intra-amniotic sludge, and prior preterm delivery
An asymptomatic 32-year-old woman with a prior preterm delivery, presently pregnant with a singleton at 17 weeks of gestation, underwent transvaginal ultrasonography and was found to have a cervical length of 22 mm and dense intra-amniotic sludge. She received one dose of 17α-hydroxyprogesterone caproate (17P) at 16 weeks of gestation. What are your next steps in management?
Intra-amniotic sludge is a conundrum
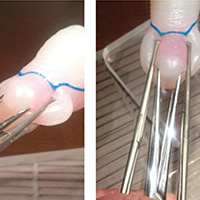
Intra-amniotic sludge is a sonographic finding of free-floating, hyperechoic, particulate matter in the amniotic fluid close to the internal os. The precise nature of this material varies, and it may include blood, meconium, or vernix and may signal inflammation or infection. In a retrospective case-control study, 27% of asymptomatic women with sludge and a short cervix had positive amniotic fluid cultures, and 27% had evidence of inflammation in the amniotic fluid (>50 white blood cells/mm3).1 In a separate report, the authors proposed that "the detection of amniotic fluid 'sludge' represents a sign that microbial invasion of the amniotic cavity and an inflammatory process are in progress."2
Benefit of cerclage in high-risk women. Several systematic reviews have highlighted the benefit of cerclage for women with a singleton pregnancy, short cervix, and previous preterm birth or second-trimester loss (ultrasound-indicated cerclage for high-risk women).3 Cerclage is presumed to work by providing some degree of structural support and by maintaining a barrier to protect the fetal membranes against exposure to ascending pathogens.4
Since dense intra-amniotic sludge may represent chronic intra-amniotic infection, can cerclage still be expected to be beneficial when microbiologic invasion of the amniotic cavity already has occurred? Furthermore, intra-amniotic infection has been cited as a possible complication of ultrasound-indicated cerclage, with a rate of 10%.5 The traditional view is that the presence of subclinical intra-amniotic infection may further increase this risk and therefore should be considered a contraindication to cerclage.6
Evaluating the patient for cerclage placement
The patient history and physical examination should focus on the signs and symptoms of labor, vaginal bleeding, amniotic membrane rupture, and intra-amniotic infection. Particular attention should be paid to maternal temperature, pulse, and the presence of uterine tenderness or foul-smelling vaginal discharge. A sterile speculum examination followed by digital examination would complement the ultrasonography evaluation in assessing cervical dilation and effacement. The ultrasonography evaluation should be completed to confirm a viable pregnancy with accurate dating and the absence of detectable fetal anomalies.
Currently, evidence is insufficient for recommending routine amniocentesis to exclude intra-amniotic infection in an asymptomatic woman prior to ultrasound-indicated cerclage, even in the presence of intra-amniotic sludge, as there are no data demonstrating improved outcomes.4 In addition, intra-amniotic sludge has been associated with intra-amniotic infection and/or inflammation in the form of microbial biofilms, which may prevent detection of infection by routine culture techniques.7
Related Article:
Universal cervical length screening–saving babies lives
Study results offer limited guidance
Data are limited on the clinical implications of intra-amniotic sludge in women with cervical cerclage. In a retrospective cohort of 177 patients with cerclage, 60 had evidence of sludge and 46 of those with sludge underwent ultrasound-indicated cerclage.8 There were no significant differences in the mean gestational age at delivery, neonatal outcomes, rate of preterm delivery, preterm premature rupture of membranes, or intra-amniotic infection between women with or without intra-amniotic sludge. A subanalysis was performed comparing women with sludge detected before or after cerclage and, again, no difference was found in measured outcomes.
Similarly, in a small (N = 20) retrospective review of the Arabin pessary used as a noninvasive intervention for short cervix, the presence of intra-amniotic sludge in 5 cases did not appear to impact outcomes.9
Case patient: How would you manage her care?
Based on her obstetric history and ultrasonography findings, the patient described in the case vignette is at high risk for preterm delivery. The presence of both intra-amniotic sludge and short cervix is associated with an increased risk for spontaneous preterm delivery. After evaluating for clinical intra-amniotic infection and performing a work-up for other contraindications to cerclage placement, cerclage placement may be offered--even in the presence of intra-amniotic sludge.
The next practical question is whether 17P, already started, should be continued after cerclage placement. From the literature on 17P, it is unclear whether progesterone provides additional benefit. One randomized, placebo-controlled study in women with at least 2 preterm deliveries or mid-trimester losses and cerclage in place showed that the 17P-treated women had a significant reduction in preterm delivery compared with the control group, from 37.8% to 16.1%.10
By contrast, in a secondary analysis of a randomized trial evaluating cerclage in high-risk women with short cervix in the current pregnancy, addition of 17P to cerclage was not beneficial.11 Results of 2 retrospective cohort studies showed the same lack of difference on preterm delivery rates with the addition of 17P.12,13
Accepting that the interpretation of these data is challenging, in our practice we would choose to continue the progesterone supplementation, siding with other recently expressed expert opinions.14
The bottom line
While clinical intra-amniotic infection is a contraindication to cerclage, there is no evidence to support withholding cerclage from eligible women due to the presence of intra-amniotic fluid sludge alone.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid "sludge" in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
- Romero R, Kusanovic JP, Espinoza J, et al. What is amniotic fluid "sludge"? Ultrasound Obstet Gynecol. 2007;30(5):793-798.
- Alfirevic Z, Stampalija T, Roberts D, Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4:CD008991.
- Abbott D, To M, Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52(3):220-223.
- Drassinower D, Poggi SH, Landy HJ, Gilo N, Benson JE, Ghidini A. Perioperative complications of history-indicated and ultrasound-indicated cervical cerclage. Am J Obstet Gynecol. 2011;205(1):53.e1-e5.
- Mays JK, Figueroa R, Shah J, Khakoo H, Kaminsky S, Tejani N. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95(5):652-655.
- Vaisbuch E, Romero R, Erez IO, et al. Clinical significance of early (<20 weeks) vs late (20-24 weeks) detection of sonographic short cervix in asymptomatic women in the mid-trimester. Ultrasound Obstet Gynecol. 2010;36(4):471-481.
- Gorski LA, Huang WH, Iriye BK, Hancock J. Clinical implication of intra-amniotic sludge on ultrasound in patients with cervical cerclage. Ultrasound Obstet Gynecol. 2010;36(4):482-485.
- Ting YH, Lao TT, Wa Law LW, et al. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25(12):2693-2695.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574-577.
- Berghella V, Figueroa D, Szychowski JM, et al; Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1-e6.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271-275.
- Stetson B, Hibbard JU, Wilkins I, Leftwich H. Outcomes with cerclage alone compared with cerclage plus 17 α-hydroxyprogesterone caproate. Obstet Gynecol. 2016;128(5):983-988.
- Iams JD. Identification of candidates for progesterone: why, who, how, and when? Obstet Gynecol. 2014;123(6):1317-1326.
CASE: Woman with short cervix, intra-amniotic sludge, and prior preterm delivery
An asymptomatic 32-year-old woman with a prior preterm delivery, presently pregnant with a singleton at 17 weeks of gestation, underwent transvaginal ultrasonography and was found to have a cervical length of 22 mm and dense intra-amniotic sludge. She received one dose of 17α-hydroxyprogesterone caproate (17P) at 16 weeks of gestation. What are your next steps in management?
Intra-amniotic sludge is a conundrum
Intra-amniotic sludge is a sonographic finding of free-floating, hyperechoic, particulate matter in the amniotic fluid close to the internal os. The precise nature of this material varies, and it may include blood, meconium, or vernix and may signal inflammation or infection. In a retrospective case-control study, 27% of asymptomatic women with sludge and a short cervix had positive amniotic fluid cultures, and 27% had evidence of inflammation in the amniotic fluid (>50 white blood cells/mm3).1 In a separate report, the authors proposed that "the detection of amniotic fluid 'sludge' represents a sign that microbial invasion of the amniotic cavity and an inflammatory process are in progress."2
Benefit of cerclage in high-risk women. Several systematic reviews have highlighted the benefit of cerclage for women with a singleton pregnancy, short cervix, and previous preterm birth or second-trimester loss (ultrasound-indicated cerclage for high-risk women).3 Cerclage is presumed to work by providing some degree of structural support and by maintaining a barrier to protect the fetal membranes against exposure to ascending pathogens.4
Since dense intra-amniotic sludge may represent chronic intra-amniotic infection, can cerclage still be expected to be beneficial when microbiologic invasion of the amniotic cavity already has occurred? Furthermore, intra-amniotic infection has been cited as a possible complication of ultrasound-indicated cerclage, with a rate of 10%.5 The traditional view is that the presence of subclinical intra-amniotic infection may further increase this risk and therefore should be considered a contraindication to cerclage.6
Evaluating the patient for cerclage placement
The patient history and physical examination should focus on the signs and symptoms of labor, vaginal bleeding, amniotic membrane rupture, and intra-amniotic infection. Particular attention should be paid to maternal temperature, pulse, and the presence of uterine tenderness or foul-smelling vaginal discharge. A sterile speculum examination followed by digital examination would complement the ultrasonography evaluation in assessing cervical dilation and effacement. The ultrasonography evaluation should be completed to confirm a viable pregnancy with accurate dating and the absence of detectable fetal anomalies.
Currently, evidence is insufficient for recommending routine amniocentesis to exclude intra-amniotic infection in an asymptomatic woman prior to ultrasound-indicated cerclage, even in the presence of intra-amniotic sludge, as there are no data demonstrating improved outcomes.4 In addition, intra-amniotic sludge has been associated with intra-amniotic infection and/or inflammation in the form of microbial biofilms, which may prevent detection of infection by routine culture techniques.7
Related Article:
Universal cervical length screening–saving babies lives
Study results offer limited guidance
Data are limited on the clinical implications of intra-amniotic sludge in women with cervical cerclage. In a retrospective cohort of 177 patients with cerclage, 60 had evidence of sludge and 46 of those with sludge underwent ultrasound-indicated cerclage.8 There were no significant differences in the mean gestational age at delivery, neonatal outcomes, rate of preterm delivery, preterm premature rupture of membranes, or intra-amniotic infection between women with or without intra-amniotic sludge. A subanalysis was performed comparing women with sludge detected before or after cerclage and, again, no difference was found in measured outcomes.
Similarly, in a small (N = 20) retrospective review of the Arabin pessary used as a noninvasive intervention for short cervix, the presence of intra-amniotic sludge in 5 cases did not appear to impact outcomes.9
Case patient: How would you manage her care?
Based on her obstetric history and ultrasonography findings, the patient described in the case vignette is at high risk for preterm delivery. The presence of both intra-amniotic sludge and short cervix is associated with an increased risk for spontaneous preterm delivery. After evaluating for clinical intra-amniotic infection and performing a work-up for other contraindications to cerclage placement, cerclage placement may be offered--even in the presence of intra-amniotic sludge.
The next practical question is whether 17P, already started, should be continued after cerclage placement. From the literature on 17P, it is unclear whether progesterone provides additional benefit. One randomized, placebo-controlled study in women with at least 2 preterm deliveries or mid-trimester losses and cerclage in place showed that the 17P-treated women had a significant reduction in preterm delivery compared with the control group, from 37.8% to 16.1%.10
By contrast, in a secondary analysis of a randomized trial evaluating cerclage in high-risk women with short cervix in the current pregnancy, addition of 17P to cerclage was not beneficial.11 Results of 2 retrospective cohort studies showed the same lack of difference on preterm delivery rates with the addition of 17P.12,13
Accepting that the interpretation of these data is challenging, in our practice we would choose to continue the progesterone supplementation, siding with other recently expressed expert opinions.14
The bottom line
While clinical intra-amniotic infection is a contraindication to cerclage, there is no evidence to support withholding cerclage from eligible women due to the presence of intra-amniotic fluid sludge alone.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: Woman with short cervix, intra-amniotic sludge, and prior preterm delivery
An asymptomatic 32-year-old woman with a prior preterm delivery, presently pregnant with a singleton at 17 weeks of gestation, underwent transvaginal ultrasonography and was found to have a cervical length of 22 mm and dense intra-amniotic sludge. She received one dose of 17α-hydroxyprogesterone caproate (17P) at 16 weeks of gestation. What are your next steps in management?
Intra-amniotic sludge is a conundrum
Intra-amniotic sludge is a sonographic finding of free-floating, hyperechoic, particulate matter in the amniotic fluid close to the internal os. The precise nature of this material varies, and it may include blood, meconium, or vernix and may signal inflammation or infection. In a retrospective case-control study, 27% of asymptomatic women with sludge and a short cervix had positive amniotic fluid cultures, and 27% had evidence of inflammation in the amniotic fluid (>50 white blood cells/mm3).1 In a separate report, the authors proposed that "the detection of amniotic fluid 'sludge' represents a sign that microbial invasion of the amniotic cavity and an inflammatory process are in progress."2
Benefit of cerclage in high-risk women. Several systematic reviews have highlighted the benefit of cerclage for women with a singleton pregnancy, short cervix, and previous preterm birth or second-trimester loss (ultrasound-indicated cerclage for high-risk women).3 Cerclage is presumed to work by providing some degree of structural support and by maintaining a barrier to protect the fetal membranes against exposure to ascending pathogens.4
Since dense intra-amniotic sludge may represent chronic intra-amniotic infection, can cerclage still be expected to be beneficial when microbiologic invasion of the amniotic cavity already has occurred? Furthermore, intra-amniotic infection has been cited as a possible complication of ultrasound-indicated cerclage, with a rate of 10%.5 The traditional view is that the presence of subclinical intra-amniotic infection may further increase this risk and therefore should be considered a contraindication to cerclage.6
Evaluating the patient for cerclage placement
The patient history and physical examination should focus on the signs and symptoms of labor, vaginal bleeding, amniotic membrane rupture, and intra-amniotic infection. Particular attention should be paid to maternal temperature, pulse, and the presence of uterine tenderness or foul-smelling vaginal discharge. A sterile speculum examination followed by digital examination would complement the ultrasonography evaluation in assessing cervical dilation and effacement. The ultrasonography evaluation should be completed to confirm a viable pregnancy with accurate dating and the absence of detectable fetal anomalies.
Currently, evidence is insufficient for recommending routine amniocentesis to exclude intra-amniotic infection in an asymptomatic woman prior to ultrasound-indicated cerclage, even in the presence of intra-amniotic sludge, as there are no data demonstrating improved outcomes.4 In addition, intra-amniotic sludge has been associated with intra-amniotic infection and/or inflammation in the form of microbial biofilms, which may prevent detection of infection by routine culture techniques.7
Related Article:
Universal cervical length screening–saving babies lives
Study results offer limited guidance
Data are limited on the clinical implications of intra-amniotic sludge in women with cervical cerclage. In a retrospective cohort of 177 patients with cerclage, 60 had evidence of sludge and 46 of those with sludge underwent ultrasound-indicated cerclage.8 There were no significant differences in the mean gestational age at delivery, neonatal outcomes, rate of preterm delivery, preterm premature rupture of membranes, or intra-amniotic infection between women with or without intra-amniotic sludge. A subanalysis was performed comparing women with sludge detected before or after cerclage and, again, no difference was found in measured outcomes.
Similarly, in a small (N = 20) retrospective review of the Arabin pessary used as a noninvasive intervention for short cervix, the presence of intra-amniotic sludge in 5 cases did not appear to impact outcomes.9
Case patient: How would you manage her care?
Based on her obstetric history and ultrasonography findings, the patient described in the case vignette is at high risk for preterm delivery. The presence of both intra-amniotic sludge and short cervix is associated with an increased risk for spontaneous preterm delivery. After evaluating for clinical intra-amniotic infection and performing a work-up for other contraindications to cerclage placement, cerclage placement may be offered--even in the presence of intra-amniotic sludge.
The next practical question is whether 17P, already started, should be continued after cerclage placement. From the literature on 17P, it is unclear whether progesterone provides additional benefit. One randomized, placebo-controlled study in women with at least 2 preterm deliveries or mid-trimester losses and cerclage in place showed that the 17P-treated women had a significant reduction in preterm delivery compared with the control group, from 37.8% to 16.1%.10
By contrast, in a secondary analysis of a randomized trial evaluating cerclage in high-risk women with short cervix in the current pregnancy, addition of 17P to cerclage was not beneficial.11 Results of 2 retrospective cohort studies showed the same lack of difference on preterm delivery rates with the addition of 17P.12,13
Accepting that the interpretation of these data is challenging, in our practice we would choose to continue the progesterone supplementation, siding with other recently expressed expert opinions.14
The bottom line
While clinical intra-amniotic infection is a contraindication to cerclage, there is no evidence to support withholding cerclage from eligible women due to the presence of intra-amniotic fluid sludge alone.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid "sludge" in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
- Romero R, Kusanovic JP, Espinoza J, et al. What is amniotic fluid "sludge"? Ultrasound Obstet Gynecol. 2007;30(5):793-798.
- Alfirevic Z, Stampalija T, Roberts D, Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4:CD008991.
- Abbott D, To M, Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52(3):220-223.
- Drassinower D, Poggi SH, Landy HJ, Gilo N, Benson JE, Ghidini A. Perioperative complications of history-indicated and ultrasound-indicated cervical cerclage. Am J Obstet Gynecol. 2011;205(1):53.e1-e5.
- Mays JK, Figueroa R, Shah J, Khakoo H, Kaminsky S, Tejani N. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95(5):652-655.
- Vaisbuch E, Romero R, Erez IO, et al. Clinical significance of early (<20 weeks) vs late (20-24 weeks) detection of sonographic short cervix in asymptomatic women in the mid-trimester. Ultrasound Obstet Gynecol. 2010;36(4):471-481.
- Gorski LA, Huang WH, Iriye BK, Hancock J. Clinical implication of intra-amniotic sludge on ultrasound in patients with cervical cerclage. Ultrasound Obstet Gynecol. 2010;36(4):482-485.
- Ting YH, Lao TT, Wa Law LW, et al. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25(12):2693-2695.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574-577.
- Berghella V, Figueroa D, Szychowski JM, et al; Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1-e6.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271-275.
- Stetson B, Hibbard JU, Wilkins I, Leftwich H. Outcomes with cerclage alone compared with cerclage plus 17 α-hydroxyprogesterone caproate. Obstet Gynecol. 2016;128(5):983-988.
- Iams JD. Identification of candidates for progesterone: why, who, how, and when? Obstet Gynecol. 2014;123(6):1317-1326.
- Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid "sludge" in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
- Romero R, Kusanovic JP, Espinoza J, et al. What is amniotic fluid "sludge"? Ultrasound Obstet Gynecol. 2007;30(5):793-798.
- Alfirevic Z, Stampalija T, Roberts D, Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4:CD008991.
- Abbott D, To M, Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52(3):220-223.
- Drassinower D, Poggi SH, Landy HJ, Gilo N, Benson JE, Ghidini A. Perioperative complications of history-indicated and ultrasound-indicated cervical cerclage. Am J Obstet Gynecol. 2011;205(1):53.e1-e5.
- Mays JK, Figueroa R, Shah J, Khakoo H, Kaminsky S, Tejani N. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95(5):652-655.
- Vaisbuch E, Romero R, Erez IO, et al. Clinical significance of early (<20 weeks) vs late (20-24 weeks) detection of sonographic short cervix in asymptomatic women in the mid-trimester. Ultrasound Obstet Gynecol. 2010;36(4):471-481.
- Gorski LA, Huang WH, Iriye BK, Hancock J. Clinical implication of intra-amniotic sludge on ultrasound in patients with cervical cerclage. Ultrasound Obstet Gynecol. 2010;36(4):482-485.
- Ting YH, Lao TT, Wa Law LW, et al. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25(12):2693-2695.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574-577.
- Berghella V, Figueroa D, Szychowski JM, et al; Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1-e6.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271-275.
- Stetson B, Hibbard JU, Wilkins I, Leftwich H. Outcomes with cerclage alone compared with cerclage plus 17 α-hydroxyprogesterone caproate. Obstet Gynecol. 2016;128(5):983-988.
- Iams JD. Identification of candidates for progesterone: why, who, how, and when? Obstet Gynecol. 2014;123(6):1317-1326.
OSA in pregnancy linked to congenital anomalies
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
AT SLEEP 2017
Key clinical point: This large cohort study is the first study to show an increased risk of congenital anomalies and resuscitation at birth in newborns born to mothers with diagnosed obstructive sleep apnea (OSA).
Major finding: Of babies born to a mother with OSA, 17.3% had a congenital anomaly, compared with 10.6% of those born to mothers without OSA (P less than .001). This difference remained significant after adjusting for potential confounders.
Data source: A national cohort study including more than 1.4 million linked maternal and newborn records with a delivery hospitalization during 2010-2014.
Disclosures: Dr. Bourjeily received research equipment support from Respironics.
Study sheds light on pregnancy outcomes following ocrelizumab treatment
NEW ORLEANS – Data from the ocrelizumab clinical development program gives clinicians a first look at pregnancy outcomes after exposure to the drug, but the small size limits the ability to draw firm conclusions.
In the United States, prescribing information for ocrelizumab states that women of childbearing potential should use contraception while receiving ocrelizumab and for 6 months after the last infusion. At the annual meeting of the Consortium of Multiple Sclerosis Centers, researchers led by Sibyl Wray, MD, set out to assess the pregnancy, fetal, neonatal and infant outcomes in patients who became pregnant during ocrelizumab trials in MS, rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE) through Sept. 15, 2015.
The analysis included ocrelizumab-exposed women in primarily European-based clinical trials in patients with MS, RA, or SLE, in whom doses ranged from 20 mg to 2,000 mg. These included three randomized trials of its use in MS, totaling 1,876 patients with a mean age of 40 years; four trials of its use in RA, totaling 2,759 patients with a mean age of 53 years; and one trial of its use in SLE, totaling 381 patients with a mean age of 31 years. Between 2008 and Sept. 14, 2015, a total of 48 women who were enrolled in the trials reported pregnancies.
MS data
Of the 15 pregnancies in the MS trials, three involved the delivery of full term, healthy newborns. In one case, the last ocrelizumab infusion was given 28 months before conception. In the second case, an infusion was given 20 weeks before conception, and a further infusion was given 17 days after conception. In the third case, the last ocrelizumab infusion was given 26.5 weeks before conception.
One live term birth occurred with an abnormal finding. In this case, the last infusion of ocrelizumab was 23 weeks prior to the last menstrual period or about 6 months prior to conception. The embryo/fetus was not exposed to the drug in utero. The researchers also found that seven elective terminations occurred among MS patients and that four pregnancies were ongoing at the time of this report.
“We have to be cautious because we don’t have enough data yet to know, but it’s encouraging to see that, if you follow the guidelines, the patient population and the newborns seem to be healthy in these exposed individuals,” Dr. Wray said.
RA data
Data from the RA clinical trials revealed 22 pregnancies in 21 patients exposed to ocrelizumab. Of these, eight pregnancies resulted in healthy term babies; four resulted in live births with abnormal findings (structural malformation, growth abnormality) or preterm birth; and eight pregnancies in seven women resulted in spontaneous abortion (one patient experienced a spontaneous abortion on two occasions), missed abortion, or an embryonic pregnancy. One pregnancy was lost to follow-up and another resulted in elective termination.
SLE data
During the SLE trials, 11 pregnancies occurred in 10 patients. Three pregnancies in two women resulted in healthy term babies. Three other pregnancies resulted in live births with an abnormal finding (structural malformation, functional deficit, growth abnormality) and/or preterm birth. Two pregnancies resulted in spontaneous/missed abortion. One pregnancy resulted in fetal death at 7.5 months’ gestation secondary to fatal pulmonary embolism in the mother; one pregnancy resulted in elective termination; and one pregnancy resulted in a healthy baby born at an unknown gestational week.
Dr. Wray emphasized that the small numbers of patients studied make it difficult to draw conclusions about pregnancy outcomes following ocrelizumab in patients with MS and other autoimmune diseases. “We need to pay attention to the half-life of this drug, the time it takes to clear, and how to plan pregnancies around that,” she said. She noted that pregnancy outcomes in ongoing ocrelizumab studies and postmarketing experiences will continue to be collected and assessed.
The study was funded by Roche, Basel, Switzerland. Dr. Wray reported that she has received honoraria and/or research funding from Actelion, Alkermes, Biogen, Celgene, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Novartis, and TG Therapeutics.
NEW ORLEANS – Data from the ocrelizumab clinical development program gives clinicians a first look at pregnancy outcomes after exposure to the drug, but the small size limits the ability to draw firm conclusions.
In the United States, prescribing information for ocrelizumab states that women of childbearing potential should use contraception while receiving ocrelizumab and for 6 months after the last infusion. At the annual meeting of the Consortium of Multiple Sclerosis Centers, researchers led by Sibyl Wray, MD, set out to assess the pregnancy, fetal, neonatal and infant outcomes in patients who became pregnant during ocrelizumab trials in MS, rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE) through Sept. 15, 2015.
The analysis included ocrelizumab-exposed women in primarily European-based clinical trials in patients with MS, RA, or SLE, in whom doses ranged from 20 mg to 2,000 mg. These included three randomized trials of its use in MS, totaling 1,876 patients with a mean age of 40 years; four trials of its use in RA, totaling 2,759 patients with a mean age of 53 years; and one trial of its use in SLE, totaling 381 patients with a mean age of 31 years. Between 2008 and Sept. 14, 2015, a total of 48 women who were enrolled in the trials reported pregnancies.
MS data
Of the 15 pregnancies in the MS trials, three involved the delivery of full term, healthy newborns. In one case, the last ocrelizumab infusion was given 28 months before conception. In the second case, an infusion was given 20 weeks before conception, and a further infusion was given 17 days after conception. In the third case, the last ocrelizumab infusion was given 26.5 weeks before conception.
One live term birth occurred with an abnormal finding. In this case, the last infusion of ocrelizumab was 23 weeks prior to the last menstrual period or about 6 months prior to conception. The embryo/fetus was not exposed to the drug in utero. The researchers also found that seven elective terminations occurred among MS patients and that four pregnancies were ongoing at the time of this report.
“We have to be cautious because we don’t have enough data yet to know, but it’s encouraging to see that, if you follow the guidelines, the patient population and the newborns seem to be healthy in these exposed individuals,” Dr. Wray said.
RA data
Data from the RA clinical trials revealed 22 pregnancies in 21 patients exposed to ocrelizumab. Of these, eight pregnancies resulted in healthy term babies; four resulted in live births with abnormal findings (structural malformation, growth abnormality) or preterm birth; and eight pregnancies in seven women resulted in spontaneous abortion (one patient experienced a spontaneous abortion on two occasions), missed abortion, or an embryonic pregnancy. One pregnancy was lost to follow-up and another resulted in elective termination.
SLE data
During the SLE trials, 11 pregnancies occurred in 10 patients. Three pregnancies in two women resulted in healthy term babies. Three other pregnancies resulted in live births with an abnormal finding (structural malformation, functional deficit, growth abnormality) and/or preterm birth. Two pregnancies resulted in spontaneous/missed abortion. One pregnancy resulted in fetal death at 7.5 months’ gestation secondary to fatal pulmonary embolism in the mother; one pregnancy resulted in elective termination; and one pregnancy resulted in a healthy baby born at an unknown gestational week.
Dr. Wray emphasized that the small numbers of patients studied make it difficult to draw conclusions about pregnancy outcomes following ocrelizumab in patients with MS and other autoimmune diseases. “We need to pay attention to the half-life of this drug, the time it takes to clear, and how to plan pregnancies around that,” she said. She noted that pregnancy outcomes in ongoing ocrelizumab studies and postmarketing experiences will continue to be collected and assessed.
The study was funded by Roche, Basel, Switzerland. Dr. Wray reported that she has received honoraria and/or research funding from Actelion, Alkermes, Biogen, Celgene, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Novartis, and TG Therapeutics.
NEW ORLEANS – Data from the ocrelizumab clinical development program gives clinicians a first look at pregnancy outcomes after exposure to the drug, but the small size limits the ability to draw firm conclusions.
In the United States, prescribing information for ocrelizumab states that women of childbearing potential should use contraception while receiving ocrelizumab and for 6 months after the last infusion. At the annual meeting of the Consortium of Multiple Sclerosis Centers, researchers led by Sibyl Wray, MD, set out to assess the pregnancy, fetal, neonatal and infant outcomes in patients who became pregnant during ocrelizumab trials in MS, rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE) through Sept. 15, 2015.
The analysis included ocrelizumab-exposed women in primarily European-based clinical trials in patients with MS, RA, or SLE, in whom doses ranged from 20 mg to 2,000 mg. These included three randomized trials of its use in MS, totaling 1,876 patients with a mean age of 40 years; four trials of its use in RA, totaling 2,759 patients with a mean age of 53 years; and one trial of its use in SLE, totaling 381 patients with a mean age of 31 years. Between 2008 and Sept. 14, 2015, a total of 48 women who were enrolled in the trials reported pregnancies.
MS data
Of the 15 pregnancies in the MS trials, three involved the delivery of full term, healthy newborns. In one case, the last ocrelizumab infusion was given 28 months before conception. In the second case, an infusion was given 20 weeks before conception, and a further infusion was given 17 days after conception. In the third case, the last ocrelizumab infusion was given 26.5 weeks before conception.
One live term birth occurred with an abnormal finding. In this case, the last infusion of ocrelizumab was 23 weeks prior to the last menstrual period or about 6 months prior to conception. The embryo/fetus was not exposed to the drug in utero. The researchers also found that seven elective terminations occurred among MS patients and that four pregnancies were ongoing at the time of this report.
“We have to be cautious because we don’t have enough data yet to know, but it’s encouraging to see that, if you follow the guidelines, the patient population and the newborns seem to be healthy in these exposed individuals,” Dr. Wray said.
RA data
Data from the RA clinical trials revealed 22 pregnancies in 21 patients exposed to ocrelizumab. Of these, eight pregnancies resulted in healthy term babies; four resulted in live births with abnormal findings (structural malformation, growth abnormality) or preterm birth; and eight pregnancies in seven women resulted in spontaneous abortion (one patient experienced a spontaneous abortion on two occasions), missed abortion, or an embryonic pregnancy. One pregnancy was lost to follow-up and another resulted in elective termination.
SLE data
During the SLE trials, 11 pregnancies occurred in 10 patients. Three pregnancies in two women resulted in healthy term babies. Three other pregnancies resulted in live births with an abnormal finding (structural malformation, functional deficit, growth abnormality) and/or preterm birth. Two pregnancies resulted in spontaneous/missed abortion. One pregnancy resulted in fetal death at 7.5 months’ gestation secondary to fatal pulmonary embolism in the mother; one pregnancy resulted in elective termination; and one pregnancy resulted in a healthy baby born at an unknown gestational week.
Dr. Wray emphasized that the small numbers of patients studied make it difficult to draw conclusions about pregnancy outcomes following ocrelizumab in patients with MS and other autoimmune diseases. “We need to pay attention to the half-life of this drug, the time it takes to clear, and how to plan pregnancies around that,” she said. She noted that pregnancy outcomes in ongoing ocrelizumab studies and postmarketing experiences will continue to be collected and assessed.
The study was funded by Roche, Basel, Switzerland. Dr. Wray reported that she has received honoraria and/or research funding from Actelion, Alkermes, Biogen, Celgene, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Novartis, and TG Therapeutics.
AT THE CMSC ANNUAL MEETING
Key clinical point:
Major finding: Of 15 pregnancies in the MS trials, three involved the delivery of three full term, healthy newborns; one live term birth occurred with an abnormal finding; seven elective terminations occurred; and four pregnancies were ongoing.
Data source: A review of 48 pregnancies among women enrolled in clinical trials for ocrelizumab in MS, rheumatoid arthritis, and systemic lupus erythematosus.
Disclosures: The study was funded by Roche, Basel, Switzerland. Dr. Wray reported that she has received honoraria and/or research funding from Actelion, Alkermes, Biogen, Celgene, EMD Serono, Genentech/Roche, Genzyme/Sanofi, Novartis, and TG Therapeutics.
DMD use during pregnancy low, study finds
NEW ORLEANS – The proportion of women with multiple sclerosis with a live birth receiving disease-modifying drug therapy was low and declined during the prepregnancy and pregnancy periods, results from a large analysis of national claims data found.
“Multiple sclerosis is up to three times more common in women than in men, and the clinical onset is often during childbearing years,” researchers led by Maria K. Houtchens, MD, wrote in an abstract presented during the annual meeting of the Consortium of Multiple Sclerosis Centers. “A better understanding of the ‘real world’ disease-modifying drug treatment patterns in women with MS and a pregnancy is essential in order to improve available clinical support, health care services, and quality of life for women with MS of childbearing age.”
Dr. Houtchens, a neurologist at Brigham and Women’s Hospital, Boston, and her associates reported results from 2,518 women who were included in the final analysis. Their mean age was 30 years, and 99% had commercial health insurance.
Overall, the proportion of women with MS and a live birth receiving DMD treatment was low, ranging from 1.9% to 25.5%, and the rate of treatment declined during the prepregnancy and pregnancy periods.
During pregnancy, the proportion of women treated with a DMD decreased to 12.05% during the first trimester and to 1.90% during the second trimester, and then increased to 2.97% during the third trimester. At 9-12 months postpartum, the proportion of women treated with a DMD was 25.5%. Most patients were treated with self-injectable DMDs (from 1.7% to 19.6%), while the use of oral and infusion agents was low (0.1%-3.1% and 0%-0.2%, respectively).
The researchers also found that the proportion of women with DMD treatment before and after pregnancy increased significantly with the number of relapses experienced prepregnancy. A greater number of relapses before pregnancy led to more patients treated with DMDs.
They acknowledged certain limitations of the study, including its reliance on information from patients with health insurance administered by regional health plans. “Results may not be generalizable to patients who self-pay or patients without employer-sponsored commercial health insurance.”
The study was supported by EMD Serono. Dr. Houtchens reported that she has received funding support from EMD Serono and that she serves on the scientific advisory boards for Biogen, Novartis, Sanofi Genzyme, and Teva Neuroscience. She also has received research support from Sanofi Genzyme.
NEW ORLEANS – The proportion of women with multiple sclerosis with a live birth receiving disease-modifying drug therapy was low and declined during the prepregnancy and pregnancy periods, results from a large analysis of national claims data found.
“Multiple sclerosis is up to three times more common in women than in men, and the clinical onset is often during childbearing years,” researchers led by Maria K. Houtchens, MD, wrote in an abstract presented during the annual meeting of the Consortium of Multiple Sclerosis Centers. “A better understanding of the ‘real world’ disease-modifying drug treatment patterns in women with MS and a pregnancy is essential in order to improve available clinical support, health care services, and quality of life for women with MS of childbearing age.”
Dr. Houtchens, a neurologist at Brigham and Women’s Hospital, Boston, and her associates reported results from 2,518 women who were included in the final analysis. Their mean age was 30 years, and 99% had commercial health insurance.
Overall, the proportion of women with MS and a live birth receiving DMD treatment was low, ranging from 1.9% to 25.5%, and the rate of treatment declined during the prepregnancy and pregnancy periods.
During pregnancy, the proportion of women treated with a DMD decreased to 12.05% during the first trimester and to 1.90% during the second trimester, and then increased to 2.97% during the third trimester. At 9-12 months postpartum, the proportion of women treated with a DMD was 25.5%. Most patients were treated with self-injectable DMDs (from 1.7% to 19.6%), while the use of oral and infusion agents was low (0.1%-3.1% and 0%-0.2%, respectively).
The researchers also found that the proportion of women with DMD treatment before and after pregnancy increased significantly with the number of relapses experienced prepregnancy. A greater number of relapses before pregnancy led to more patients treated with DMDs.
They acknowledged certain limitations of the study, including its reliance on information from patients with health insurance administered by regional health plans. “Results may not be generalizable to patients who self-pay or patients without employer-sponsored commercial health insurance.”
The study was supported by EMD Serono. Dr. Houtchens reported that she has received funding support from EMD Serono and that she serves on the scientific advisory boards for Biogen, Novartis, Sanofi Genzyme, and Teva Neuroscience. She also has received research support from Sanofi Genzyme.
NEW ORLEANS – The proportion of women with multiple sclerosis with a live birth receiving disease-modifying drug therapy was low and declined during the prepregnancy and pregnancy periods, results from a large analysis of national claims data found.
“Multiple sclerosis is up to three times more common in women than in men, and the clinical onset is often during childbearing years,” researchers led by Maria K. Houtchens, MD, wrote in an abstract presented during the annual meeting of the Consortium of Multiple Sclerosis Centers. “A better understanding of the ‘real world’ disease-modifying drug treatment patterns in women with MS and a pregnancy is essential in order to improve available clinical support, health care services, and quality of life for women with MS of childbearing age.”
Dr. Houtchens, a neurologist at Brigham and Women’s Hospital, Boston, and her associates reported results from 2,518 women who were included in the final analysis. Their mean age was 30 years, and 99% had commercial health insurance.
Overall, the proportion of women with MS and a live birth receiving DMD treatment was low, ranging from 1.9% to 25.5%, and the rate of treatment declined during the prepregnancy and pregnancy periods.
During pregnancy, the proportion of women treated with a DMD decreased to 12.05% during the first trimester and to 1.90% during the second trimester, and then increased to 2.97% during the third trimester. At 9-12 months postpartum, the proportion of women treated with a DMD was 25.5%. Most patients were treated with self-injectable DMDs (from 1.7% to 19.6%), while the use of oral and infusion agents was low (0.1%-3.1% and 0%-0.2%, respectively).
The researchers also found that the proportion of women with DMD treatment before and after pregnancy increased significantly with the number of relapses experienced prepregnancy. A greater number of relapses before pregnancy led to more patients treated with DMDs.
They acknowledged certain limitations of the study, including its reliance on information from patients with health insurance administered by regional health plans. “Results may not be generalizable to patients who self-pay or patients without employer-sponsored commercial health insurance.”
The study was supported by EMD Serono. Dr. Houtchens reported that she has received funding support from EMD Serono and that she serves on the scientific advisory boards for Biogen, Novartis, Sanofi Genzyme, and Teva Neuroscience. She also has received research support from Sanofi Genzyme.
AT THE CMSC ANNUAL MEETING
Key clinical point:
Major finding: Overall, the proportion of women with multiple sclerosis and a live birth receiving DMD treatment was low, ranging from 1.9% to 25.5%.
Data source: A retrospective analysis of claims data from 2,518 women with MS.
Disclosures: The study was supported by EMD Serono. Dr. Houtchens reported that she has received funding support from EMD Serono and that she serves on the scientific advisory boards for Biogen, Novartis, Sanofi Genzyme, and Teva Neuroscience. She also has received research support from Sanofi Genzyme.
Loud, frequent snoring increases preterm delivery risk
BOSTON – Women who were prepregnancy, frequent, and loud snorers during pregnancy had a significantly higher risk of preterm or early term delivery, in a study presented at the annual meeting of the Associated Professional Sleep Societies.
“The fact that there is an association between snoring and time to delivery in a cohort which is not hypertensive is alarming, and I think that treatment for snoring earlier on in pregnancy may alleviate some of these outcomes,” reported Galit Levi Dunietz, PhD, MPH, of the University of Michigan in a session at the meeting.
Compared with nonsnorers, frequently loud snorers had about a 60% increased risk of preterm delivery even after adjusting for baseline body mass index, smoking, education, race, and parity. Pregnancy-onset snoring and infrequent or quiet snoring were not associated with preterm birth.
A limitation on the findings was that only a small number of women (4% of the sample) fell into the chronic, frequent, and loud snoring category. These women, however, had significantly lower mean gestational age, mean baseline BMI, and were more likely to be smokers, as compared with nonsnorers and quiet frequent or infrequent snorers.
“I think this is excellent work because it’s a big question,” said Dr. Omavi Gbodossou Bailey, MD, MPH from the University of Arizona, Pheonix, in a Q&A session at the conference. “As a primary care physician, I deliver babies and I also deal with sleep and when I ask the ob.gyns. about sleep apnea in this patient population, they’re not usually interested.”
Dr. Bailey noted in an interview that, often, women who had uncomplicated first pregnancies return with later pregnancies heavier, more sleep deprived, and snoring. “Then, they have higher risk for complications in the second or third pregnancy,” he said.
Snoring is common in pregnancy, affecting about 35% of women, and pregnancy itself is a risk factor for snoring. Previous studies have associated snoring with key pregnancy morbidities including hypertension, preeclampsia, and gestational diabetes, but, prior to this research, the few studies that had looked at snoring and preterm delivery had shown inconsistent results.
The researchers recruited 904 pregnant women in their third trimester and without hypertension or diabetes from prenatal clinics at the University of Michigan cared for between 2008 and 2011. The women were queried on the frequency of their snoring (from never to three or more times per week) along with its intensity (from nonsnoring to loud or very loud snoring). They were also categorized, based on self-report, as either chronic/prepregnancy snorers or incident/pregnancy-onset snorers.
In this low-risk cohort, 25% of the women reported incident snoring and 9% reported chronic prepregnancy snoring.
“The combination of snoring frequency and intensity may be a clinically useful marker to identify otherwise low-risk women who are likely to deliver earlier,” said Dr. Dunietz.
This study was funded by the Gilmore Fund for Sleep Research, the University of Michigan Institute for Clinical and Health Research, and the National Heart, Lung, and Blood Institute. Dr. Dunietz reported having no financial disclosures.
BOSTON – Women who were prepregnancy, frequent, and loud snorers during pregnancy had a significantly higher risk of preterm or early term delivery, in a study presented at the annual meeting of the Associated Professional Sleep Societies.
“The fact that there is an association between snoring and time to delivery in a cohort which is not hypertensive is alarming, and I think that treatment for snoring earlier on in pregnancy may alleviate some of these outcomes,” reported Galit Levi Dunietz, PhD, MPH, of the University of Michigan in a session at the meeting.
Compared with nonsnorers, frequently loud snorers had about a 60% increased risk of preterm delivery even after adjusting for baseline body mass index, smoking, education, race, and parity. Pregnancy-onset snoring and infrequent or quiet snoring were not associated with preterm birth.
A limitation on the findings was that only a small number of women (4% of the sample) fell into the chronic, frequent, and loud snoring category. These women, however, had significantly lower mean gestational age, mean baseline BMI, and were more likely to be smokers, as compared with nonsnorers and quiet frequent or infrequent snorers.
“I think this is excellent work because it’s a big question,” said Dr. Omavi Gbodossou Bailey, MD, MPH from the University of Arizona, Pheonix, in a Q&A session at the conference. “As a primary care physician, I deliver babies and I also deal with sleep and when I ask the ob.gyns. about sleep apnea in this patient population, they’re not usually interested.”
Dr. Bailey noted in an interview that, often, women who had uncomplicated first pregnancies return with later pregnancies heavier, more sleep deprived, and snoring. “Then, they have higher risk for complications in the second or third pregnancy,” he said.
Snoring is common in pregnancy, affecting about 35% of women, and pregnancy itself is a risk factor for snoring. Previous studies have associated snoring with key pregnancy morbidities including hypertension, preeclampsia, and gestational diabetes, but, prior to this research, the few studies that had looked at snoring and preterm delivery had shown inconsistent results.
The researchers recruited 904 pregnant women in their third trimester and without hypertension or diabetes from prenatal clinics at the University of Michigan cared for between 2008 and 2011. The women were queried on the frequency of their snoring (from never to three or more times per week) along with its intensity (from nonsnoring to loud or very loud snoring). They were also categorized, based on self-report, as either chronic/prepregnancy snorers or incident/pregnancy-onset snorers.
In this low-risk cohort, 25% of the women reported incident snoring and 9% reported chronic prepregnancy snoring.
“The combination of snoring frequency and intensity may be a clinically useful marker to identify otherwise low-risk women who are likely to deliver earlier,” said Dr. Dunietz.
This study was funded by the Gilmore Fund for Sleep Research, the University of Michigan Institute for Clinical and Health Research, and the National Heart, Lung, and Blood Institute. Dr. Dunietz reported having no financial disclosures.
BOSTON – Women who were prepregnancy, frequent, and loud snorers during pregnancy had a significantly higher risk of preterm or early term delivery, in a study presented at the annual meeting of the Associated Professional Sleep Societies.
“The fact that there is an association between snoring and time to delivery in a cohort which is not hypertensive is alarming, and I think that treatment for snoring earlier on in pregnancy may alleviate some of these outcomes,” reported Galit Levi Dunietz, PhD, MPH, of the University of Michigan in a session at the meeting.
Compared with nonsnorers, frequently loud snorers had about a 60% increased risk of preterm delivery even after adjusting for baseline body mass index, smoking, education, race, and parity. Pregnancy-onset snoring and infrequent or quiet snoring were not associated with preterm birth.
A limitation on the findings was that only a small number of women (4% of the sample) fell into the chronic, frequent, and loud snoring category. These women, however, had significantly lower mean gestational age, mean baseline BMI, and were more likely to be smokers, as compared with nonsnorers and quiet frequent or infrequent snorers.
“I think this is excellent work because it’s a big question,” said Dr. Omavi Gbodossou Bailey, MD, MPH from the University of Arizona, Pheonix, in a Q&A session at the conference. “As a primary care physician, I deliver babies and I also deal with sleep and when I ask the ob.gyns. about sleep apnea in this patient population, they’re not usually interested.”
Dr. Bailey noted in an interview that, often, women who had uncomplicated first pregnancies return with later pregnancies heavier, more sleep deprived, and snoring. “Then, they have higher risk for complications in the second or third pregnancy,” he said.
Snoring is common in pregnancy, affecting about 35% of women, and pregnancy itself is a risk factor for snoring. Previous studies have associated snoring with key pregnancy morbidities including hypertension, preeclampsia, and gestational diabetes, but, prior to this research, the few studies that had looked at snoring and preterm delivery had shown inconsistent results.
The researchers recruited 904 pregnant women in their third trimester and without hypertension or diabetes from prenatal clinics at the University of Michigan cared for between 2008 and 2011. The women were queried on the frequency of their snoring (from never to three or more times per week) along with its intensity (from nonsnoring to loud or very loud snoring). They were also categorized, based on self-report, as either chronic/prepregnancy snorers or incident/pregnancy-onset snorers.
In this low-risk cohort, 25% of the women reported incident snoring and 9% reported chronic prepregnancy snoring.
“The combination of snoring frequency and intensity may be a clinically useful marker to identify otherwise low-risk women who are likely to deliver earlier,” said Dr. Dunietz.
This study was funded by the Gilmore Fund for Sleep Research, the University of Michigan Institute for Clinical and Health Research, and the National Heart, Lung, and Blood Institute. Dr. Dunietz reported having no financial disclosures.
AT SLEEP 2017
Key clinical point: Compared with those who were nonloud, nonfrequent, or pregnancy-onset snorers, chronic, loud, and frequent snorers were at significantly greater risk for preterm delivery.
Major finding: Of women determined to be chronic, prepregnancy, frequent, and loud snorers, 25% had preterm delivery.
Data source: An observational study including 904 pregnant women in the third trimester.
Disclosures: This study was funded by the Gilmore Fund for Sleep Research, the University of Michigan Institute for Clinical and Health Research, and the National Heart, Lung, and Blood Institute. Dr. Dunietz reported having no financial disclosures.
First trimester lithium exposure ups risk of cardiac malformations
Cardiac malformations are three times more likely to occur in infants exposed to lithium during the first trimester of gestation than in unexposed infants.
The increased risk could account for one additional cardiac malformation per 100 live births, Elisabetta Patorno, MD, and her colleagues wrote in the June 8 issue of the New England Journal of Medicine (2017;376:2245-54).
Dr. Patorno’s study is the largest conducted since then. It comprised more than 1.3 million pregnancies included in the U.S. Medicaid Analytic eXtract database during 2000-2010. Of these, 663 had first trimester lithium exposure. These were compared with 1,945 pregnancies with first trimester exposure to lamotrigine, another mood stabilizer, and to the remaining 1.3 million pregnancies unexposed to either drug.
There were 16 cardiac malformations in the lithium group (2.41%); 27 in the lamotrigine group (1.39%); and 15,251 in the unexposed group (1.15%). Lithium conferred a 65% increased risk of cardiac defect, compared with unexposed pregnancies. It more than doubled the risk when compared with lamotrigine-exposed pregnancies (risk ratio, 2.25).
The risk was dose dependent, however, with an 11% increase associated with 600 mg/day or less and a 60% increase associated with 601-900 mg/day. Infants exposed to more than 900 mg per day in the first trimester, however, were more than 300% more likely to have a cardiac malformation (RR, 3.22).
The investigators also examined the association of lithium with cardiac defects consistent with Ebstein’s anomaly. Lithium more than doubled the risk, compared with unexposed infants (RR, 2.66). This risk was also dose dependent; all of the right ventricular outflow defects occurred in infants exposed to more than 600 mg/day.
Dr. Patorno reported grant support from National Institute of Mental Health during the study and grant support from Boehringer Ingelheim and GlaxoSmithKline outside of the study. Other authors reported receiving grants or personal fees from various pharmaceutical companies.
[email protected]
On Twitter @Alz_gal
Cardiac malformations are three times more likely to occur in infants exposed to lithium during the first trimester of gestation than in unexposed infants.
The increased risk could account for one additional cardiac malformation per 100 live births, Elisabetta Patorno, MD, and her colleagues wrote in the June 8 issue of the New England Journal of Medicine (2017;376:2245-54).
Dr. Patorno’s study is the largest conducted since then. It comprised more than 1.3 million pregnancies included in the U.S. Medicaid Analytic eXtract database during 2000-2010. Of these, 663 had first trimester lithium exposure. These were compared with 1,945 pregnancies with first trimester exposure to lamotrigine, another mood stabilizer, and to the remaining 1.3 million pregnancies unexposed to either drug.
There were 16 cardiac malformations in the lithium group (2.41%); 27 in the lamotrigine group (1.39%); and 15,251 in the unexposed group (1.15%). Lithium conferred a 65% increased risk of cardiac defect, compared with unexposed pregnancies. It more than doubled the risk when compared with lamotrigine-exposed pregnancies (risk ratio, 2.25).
The risk was dose dependent, however, with an 11% increase associated with 600 mg/day or less and a 60% increase associated with 601-900 mg/day. Infants exposed to more than 900 mg per day in the first trimester, however, were more than 300% more likely to have a cardiac malformation (RR, 3.22).
The investigators also examined the association of lithium with cardiac defects consistent with Ebstein’s anomaly. Lithium more than doubled the risk, compared with unexposed infants (RR, 2.66). This risk was also dose dependent; all of the right ventricular outflow defects occurred in infants exposed to more than 600 mg/day.
Dr. Patorno reported grant support from National Institute of Mental Health during the study and grant support from Boehringer Ingelheim and GlaxoSmithKline outside of the study. Other authors reported receiving grants or personal fees from various pharmaceutical companies.
[email protected]
On Twitter @Alz_gal
Cardiac malformations are three times more likely to occur in infants exposed to lithium during the first trimester of gestation than in unexposed infants.
The increased risk could account for one additional cardiac malformation per 100 live births, Elisabetta Patorno, MD, and her colleagues wrote in the June 8 issue of the New England Journal of Medicine (2017;376:2245-54).
Dr. Patorno’s study is the largest conducted since then. It comprised more than 1.3 million pregnancies included in the U.S. Medicaid Analytic eXtract database during 2000-2010. Of these, 663 had first trimester lithium exposure. These were compared with 1,945 pregnancies with first trimester exposure to lamotrigine, another mood stabilizer, and to the remaining 1.3 million pregnancies unexposed to either drug.
There were 16 cardiac malformations in the lithium group (2.41%); 27 in the lamotrigine group (1.39%); and 15,251 in the unexposed group (1.15%). Lithium conferred a 65% increased risk of cardiac defect, compared with unexposed pregnancies. It more than doubled the risk when compared with lamotrigine-exposed pregnancies (risk ratio, 2.25).
The risk was dose dependent, however, with an 11% increase associated with 600 mg/day or less and a 60% increase associated with 601-900 mg/day. Infants exposed to more than 900 mg per day in the first trimester, however, were more than 300% more likely to have a cardiac malformation (RR, 3.22).
The investigators also examined the association of lithium with cardiac defects consistent with Ebstein’s anomaly. Lithium more than doubled the risk, compared with unexposed infants (RR, 2.66). This risk was also dose dependent; all of the right ventricular outflow defects occurred in infants exposed to more than 600 mg/day.
Dr. Patorno reported grant support from National Institute of Mental Health during the study and grant support from Boehringer Ingelheim and GlaxoSmithKline outside of the study. Other authors reported receiving grants or personal fees from various pharmaceutical companies.
[email protected]
On Twitter @Alz_gal
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: The dose-dependent increased risks ranged from 11% to more than 300%, compared with unexposed pregnancies.
Data source: The Medicaid database review comprised more than 1.3 million pregnancies.
Disclosures: Dr. Patorno reported grant support from National Institute of Mental Health during the study and grant support from Boehringer Ingelheim and GlaxoSmithKline outside of the study. Other authors reported receiving grants or personal fees from various pharmaceutical companies.
Weight gain in pregnancy: Too much and too little can be harmful
Both high and low gestational weight gain, compared with the recommended weight gain, are associated with increased risks of adverse perinatal outcomes, according to a systematic review and meta-analysis.
Researchers reviewed 302 studies that categorized women by their prepregnancy body mass index and followed them for gestational weight gain, as well as maternal and neonatal outcomes. They included in their meta-analysis 23 cohort studies involving 1,309,136 pregnancies in 10 countries. Only studies assessing singleton pregnancies in women aged 18 years and older were included.
Compared with the recommended gestational weight gain, low weight gain was associated with a 5% higher risk of a small-for-gestational-age (SGA) neonate and a 5% higher risk of preterm birth. However, low weight gain reduced the risks of a large-for-gestational-age (LGA) neonate and macrosomia.
Compared with the recommended gestational weight gain, high weight gain was associated with a 4% higher risk of cesarean delivery, a 4% higher risk of a LGA neonate, and a 6% higher risk of macrosomia. However, high weight gain reduced the risk of an SGA neonate by 3% and that of preterm birth by 2%, the researchers reported (JAMA. 2017;317[21]:2207-25).
These increases and decreases in risks remained consistent regardless of the mother’s prepregnancy BMI, they noted.
The effect of either high or low gestational weight gain on the risk of gestational diabetes could not be determined because of inconsistencies across the 23 cohort studies concerning definitions and treatments.
The Australian Department of Education and Training and the Australian National Health and Medical Research Council supported the study. Dr. Goldstein reported having no relevant financial disclosures; one of her associates reported serving on the Women’s Health Global Advisory Board for Pfizer.
The findings by Goldstein et al. raise the question: Can clinicians change the amount of weight women gain in pregnancy?
Behavioral economics has demonstrated that loss avoidance is a stronger motivator than the promise of a gain. So rather than positive incentives for adherent behavior, emphasizing how a pregnant woman’s nonadherent behavior will lead to greater harm to her developing baby may be more effective in changing behavior. Sending a message that gaining too much weight could potentially lead to an increased risk of obesity in her child and that gaining too little weight could lead to growth restriction in the child may be better than a simple positive message that eating well leads to greater health for both the mother and infant.
Given the overwhelming environment of constant advertising of high-caloric foods that pregnant women are exposed to, such reminders need to be delivered persistently and frequently – perhaps with the enhanced messaging capacity of social media and public health campaigns.
Aaron B. Caughey, MD, PhD, is in the department of ob.gyn. at Oregon Health & Science University, Portland. He reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (JAMA 2017;317[21]:2175-6).
The findings by Goldstein et al. raise the question: Can clinicians change the amount of weight women gain in pregnancy?
Behavioral economics has demonstrated that loss avoidance is a stronger motivator than the promise of a gain. So rather than positive incentives for adherent behavior, emphasizing how a pregnant woman’s nonadherent behavior will lead to greater harm to her developing baby may be more effective in changing behavior. Sending a message that gaining too much weight could potentially lead to an increased risk of obesity in her child and that gaining too little weight could lead to growth restriction in the child may be better than a simple positive message that eating well leads to greater health for both the mother and infant.
Given the overwhelming environment of constant advertising of high-caloric foods that pregnant women are exposed to, such reminders need to be delivered persistently and frequently – perhaps with the enhanced messaging capacity of social media and public health campaigns.
Aaron B. Caughey, MD, PhD, is in the department of ob.gyn. at Oregon Health & Science University, Portland. He reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (JAMA 2017;317[21]:2175-6).
The findings by Goldstein et al. raise the question: Can clinicians change the amount of weight women gain in pregnancy?
Behavioral economics has demonstrated that loss avoidance is a stronger motivator than the promise of a gain. So rather than positive incentives for adherent behavior, emphasizing how a pregnant woman’s nonadherent behavior will lead to greater harm to her developing baby may be more effective in changing behavior. Sending a message that gaining too much weight could potentially lead to an increased risk of obesity in her child and that gaining too little weight could lead to growth restriction in the child may be better than a simple positive message that eating well leads to greater health for both the mother and infant.
Given the overwhelming environment of constant advertising of high-caloric foods that pregnant women are exposed to, such reminders need to be delivered persistently and frequently – perhaps with the enhanced messaging capacity of social media and public health campaigns.
Aaron B. Caughey, MD, PhD, is in the department of ob.gyn. at Oregon Health & Science University, Portland. He reported having no relevant financial disclosures. These remarks are adapted from an accompanying editorial (JAMA 2017;317[21]:2175-6).
Both high and low gestational weight gain, compared with the recommended weight gain, are associated with increased risks of adverse perinatal outcomes, according to a systematic review and meta-analysis.
Researchers reviewed 302 studies that categorized women by their prepregnancy body mass index and followed them for gestational weight gain, as well as maternal and neonatal outcomes. They included in their meta-analysis 23 cohort studies involving 1,309,136 pregnancies in 10 countries. Only studies assessing singleton pregnancies in women aged 18 years and older were included.
Compared with the recommended gestational weight gain, low weight gain was associated with a 5% higher risk of a small-for-gestational-age (SGA) neonate and a 5% higher risk of preterm birth. However, low weight gain reduced the risks of a large-for-gestational-age (LGA) neonate and macrosomia.
Compared with the recommended gestational weight gain, high weight gain was associated with a 4% higher risk of cesarean delivery, a 4% higher risk of a LGA neonate, and a 6% higher risk of macrosomia. However, high weight gain reduced the risk of an SGA neonate by 3% and that of preterm birth by 2%, the researchers reported (JAMA. 2017;317[21]:2207-25).
These increases and decreases in risks remained consistent regardless of the mother’s prepregnancy BMI, they noted.
The effect of either high or low gestational weight gain on the risk of gestational diabetes could not be determined because of inconsistencies across the 23 cohort studies concerning definitions and treatments.
The Australian Department of Education and Training and the Australian National Health and Medical Research Council supported the study. Dr. Goldstein reported having no relevant financial disclosures; one of her associates reported serving on the Women’s Health Global Advisory Board for Pfizer.
Both high and low gestational weight gain, compared with the recommended weight gain, are associated with increased risks of adverse perinatal outcomes, according to a systematic review and meta-analysis.
Researchers reviewed 302 studies that categorized women by their prepregnancy body mass index and followed them for gestational weight gain, as well as maternal and neonatal outcomes. They included in their meta-analysis 23 cohort studies involving 1,309,136 pregnancies in 10 countries. Only studies assessing singleton pregnancies in women aged 18 years and older were included.
Compared with the recommended gestational weight gain, low weight gain was associated with a 5% higher risk of a small-for-gestational-age (SGA) neonate and a 5% higher risk of preterm birth. However, low weight gain reduced the risks of a large-for-gestational-age (LGA) neonate and macrosomia.
Compared with the recommended gestational weight gain, high weight gain was associated with a 4% higher risk of cesarean delivery, a 4% higher risk of a LGA neonate, and a 6% higher risk of macrosomia. However, high weight gain reduced the risk of an SGA neonate by 3% and that of preterm birth by 2%, the researchers reported (JAMA. 2017;317[21]:2207-25).
These increases and decreases in risks remained consistent regardless of the mother’s prepregnancy BMI, they noted.
The effect of either high or low gestational weight gain on the risk of gestational diabetes could not be determined because of inconsistencies across the 23 cohort studies concerning definitions and treatments.
The Australian Department of Education and Training and the Australian National Health and Medical Research Council supported the study. Dr. Goldstein reported having no relevant financial disclosures; one of her associates reported serving on the Women’s Health Global Advisory Board for Pfizer.
FROM JAMA
Key clinical point: Both high and low gestational weight gain are associated with increased risks of adverse perinatal outcomes.
Major finding: Low gestational weight gain was associated with a 5% higher risk of an SGA neonate and a 5% higher risk of preterm birth, while high weight gain was associated with a 4% higher risk of cesarean delivery, a 4% higher risk of an LGA neonate, and a 6% higher risk of macrosomia.
Data source: A systematic review and meta-analysis of 23 studies involving 1,309,136 pregnancies from diverse international cohorts.
Disclosures: The Australian Department of Education and Training and the Australian National Health and Medical Research Council supported the study. Dr. Goldstein reported having no relevant financial disclosures; one of her associates reported serving on the Women’s Health Global Advisory Board for Pfizer.
Health inequities take a societal toll
Arguably one of the most important public health issues in our nation is the gap between high-quality care and the people who need it most. The passage of the Affordable Care Act was meant, in part, to reduce this gap and increase health equity in terms of both eligibility for, and access to, care. However, lower-income residents, especially those from minority groups, are more likely to be hospitalized for asthma, hypertension, heart disease, and diabetes, and to experience infertility, preterm birth, and fetal death.
Health disparities, or inequities, translate not only into greater suffering for certain segments of the population, but also to significantly greater health care costs for everyone. Racial health disparities are associated with an estimated $35 billion annually in excess expenditures, $10 billion in lost productivity, and nearly $200 billion in premature deaths, according to an article in the Harvard Business Review. A 2013 study estimated that reducing racial disparities in adverse pregnancy outcomes – preeclampsia, preterm birth, gestational diabetes mellitus, and fetal death/stillbirth – could generate health care cost savings of up to $214 million per year (Matern Child Health J. 2013 Oct;17[8]:1518-25).
Several years ago, the State of Maryland took a unique approach to reducing health disparities by passing the Maryland Health Improvement and Disparities Reduction Act. One of the major components of this legislation was the creation of Health Enterprise Zones (HEZs), distinct geographical areas across the state dedicated to addressing health disparities and improving access to high-quality care. This incentive-based program provides state-funded resources to primary care providers and community-based health organizations specifically to help the neighborhoods they serve. I was deeply honored to serve as chairman of the task force that recommended the establishment of the HEZs.
For this Master Class, I have invited Melissa A. Simon, MD, the George H. Gardner, MD, Professor of Clinical Gynecology and professor of obstetrics and gynecology at Northwestern University, Chicago, to provide some practical advice on how to create greater health equity.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Arguably one of the most important public health issues in our nation is the gap between high-quality care and the people who need it most. The passage of the Affordable Care Act was meant, in part, to reduce this gap and increase health equity in terms of both eligibility for, and access to, care. However, lower-income residents, especially those from minority groups, are more likely to be hospitalized for asthma, hypertension, heart disease, and diabetes, and to experience infertility, preterm birth, and fetal death.
Health disparities, or inequities, translate not only into greater suffering for certain segments of the population, but also to significantly greater health care costs for everyone. Racial health disparities are associated with an estimated $35 billion annually in excess expenditures, $10 billion in lost productivity, and nearly $200 billion in premature deaths, according to an article in the Harvard Business Review. A 2013 study estimated that reducing racial disparities in adverse pregnancy outcomes – preeclampsia, preterm birth, gestational diabetes mellitus, and fetal death/stillbirth – could generate health care cost savings of up to $214 million per year (Matern Child Health J. 2013 Oct;17[8]:1518-25).
Several years ago, the State of Maryland took a unique approach to reducing health disparities by passing the Maryland Health Improvement and Disparities Reduction Act. One of the major components of this legislation was the creation of Health Enterprise Zones (HEZs), distinct geographical areas across the state dedicated to addressing health disparities and improving access to high-quality care. This incentive-based program provides state-funded resources to primary care providers and community-based health organizations specifically to help the neighborhoods they serve. I was deeply honored to serve as chairman of the task force that recommended the establishment of the HEZs.
For this Master Class, I have invited Melissa A. Simon, MD, the George H. Gardner, MD, Professor of Clinical Gynecology and professor of obstetrics and gynecology at Northwestern University, Chicago, to provide some practical advice on how to create greater health equity.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Arguably one of the most important public health issues in our nation is the gap between high-quality care and the people who need it most. The passage of the Affordable Care Act was meant, in part, to reduce this gap and increase health equity in terms of both eligibility for, and access to, care. However, lower-income residents, especially those from minority groups, are more likely to be hospitalized for asthma, hypertension, heart disease, and diabetes, and to experience infertility, preterm birth, and fetal death.
Health disparities, or inequities, translate not only into greater suffering for certain segments of the population, but also to significantly greater health care costs for everyone. Racial health disparities are associated with an estimated $35 billion annually in excess expenditures, $10 billion in lost productivity, and nearly $200 billion in premature deaths, according to an article in the Harvard Business Review. A 2013 study estimated that reducing racial disparities in adverse pregnancy outcomes – preeclampsia, preterm birth, gestational diabetes mellitus, and fetal death/stillbirth – could generate health care cost savings of up to $214 million per year (Matern Child Health J. 2013 Oct;17[8]:1518-25).
Several years ago, the State of Maryland took a unique approach to reducing health disparities by passing the Maryland Health Improvement and Disparities Reduction Act. One of the major components of this legislation was the creation of Health Enterprise Zones (HEZs), distinct geographical areas across the state dedicated to addressing health disparities and improving access to high-quality care. This incentive-based program provides state-funded resources to primary care providers and community-based health organizations specifically to help the neighborhoods they serve. I was deeply honored to serve as chairman of the task force that recommended the establishment of the HEZs.
For this Master Class, I have invited Melissa A. Simon, MD, the George H. Gardner, MD, Professor of Clinical Gynecology and professor of obstetrics and gynecology at Northwestern University, Chicago, to provide some practical advice on how to create greater health equity.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Moving toward health equity in practice
Of all the medical professions, obstetrics and gynecology should be the strongest champion for equity in women’s health in this country and globally. The question is, what does this mean in the reality of 2017 and moving forward in the 21st century? What does it mean in the context of our own practices and in the landscape of current policy and politics?
Finding answers to these questions requires both a deep understanding of the meaning of health equity and a willingness to rethink the architecture and engineering of how we currently provide care.
The terms equity and equality are sometimes used interchangeably, but they actually have quite different meanings. Imagine three women of different heights standing underneath the lowest branch of a tall apple tree. None of the three women are tall enough to pick an apple from the branch.
If we think about equality, we would assist each woman by giving her a box to stand on, and all three boxes would be the same size. This means that while the tallest woman will now be able to pick an apple, the medium-height woman may be able to touch but not pick the apple, and the shortest woman still may not be able to reach the apple at all.
However, if we think about equity, we’d acknowledge that each woman needs her own personalized box to be able to pick the apple. For instance, the shortest woman may need a box that is three times the height of the box used by the tallest woman.
Achieving true population health for all women requires that we similarly eliminate inequities by providing each patient with her own personalized care plan to help her reach and maintain her health.
Women from minority groups have higher rates of low birth weight, preterm birth, stillbirth, gestational diabetes and its complications, HIV, breast cancer mortality and cervical cancer incidence and mortality, infertility and response to fertility treatment, and maternal mortality.
Yet inequity runs deeper than racial/ethnic labels; disparities also are created by a host of other factors, from cognitive or physical disabilities to gender or sexual identity or orientation, one’s ZIP code, working environment, language, and health literacy.
More than ever, the art of medicine involves understanding how to meet every patient where she is – given her own context and beliefs and levels of support – so that every woman has the opportunity to stand on the right-sized box and pick the apple and thrive.
Our practices
Provider bias and stereotyping can impact health care and health outcomes, and it is important that we work to prevent this in ourselves and in our staff. This means not making assumptions. It means really listening to our patients in ways that we may not have before.
Women who have experienced health inequity may have unique barriers to success. Therefore, we must listen for cues and inquire about our patients’ environment and circumstances, as well as their partnerships and support – or lack thereof. We should then acknowledge and communicate that certain social and environmental factors may impact our ability to achieve a desired outcome.
How can we impact the diet of a patient with gestational diabetes, for instance, if we have not adequately communicated what medical nutritional therapy means in the context of her own culture and ability to access food? If she lives in a food desert or has food insecurity or lives in a violence-ridden neighborhood that keeps her from going to a grocery store regularly, we must think outside the box. Ob.gyns. and their clinical care teams can work with women who have less access to nutritious foods, or who have certain cultural food staples, to suggest recipes and grocery lists that make sense with respect to the types of stores they shop in or their cultural preferences.
When it comes to cancer prevention and treatment, how can we expect a woman to be compliant with screening if we cannot help her understand that she can get screening services for free with her health insurance? How can we help a woman who has coverage for, or access to, free screening but then no funding or coverage for a diagnostic test or cancer treatment? How can we support a patient with abnormal cancer screening results who hasn’t followed up for months because she is afraid to leave home without her partner’s permission?
Such questions and circumstances often involve what we call “social determinants of health,” and they force us to rethink how we can better deliver and optimize care. Re-engineering our practices for health equity may involve employing a more diverse practice staff, linking patients with community resources, modifying our practice hours to align better with working women’s schedules, or finding creative ways to discern patients’ motivating factors and then piggyback on these factors.
We may also need to modify how we approach the number of return visits that we request of women so that follow-up care aligns better with their ability to leave work or find childcare. Simply put, we should strive to set up our patients for success, not failure.
We can pointedly ask patients about the kinds of information and support they want and need. We might ask, for instance: What do you need, and how can I work with you, so that you can effectively monitor and control your glucose levels? How can I work with you to help you get onto a trajectory to stop smoking? How can I help you better understand what tests and procedures are covered under your insurance plan, or whether you qualify for free services?
Patients with lower health literacy may need teach-back methods to validate understanding, or messaging that is more focused and limited at any one time. Self-efficacy through patient-centered education and support should be our goal.
Practices and clinics may also be able to adapt elements of the National Cancer Institute’s multicenter Patient Navigation Research Program, in which community health workers or other “patient navigators” address women’s personal barriers to the timely follow-up of abnormal breast and cervical cancer screening results. Patient navigation through this program and similar projects, including programs that we’ve adapted for different racial and ethnic communities in and around Chicago, has reduced or eliminated delays in diagnostic resolution of gynecologic cancer (Cancer. 2015 Nov 15;121[22]:4025-34, Breast Cancer Res Treat. 2016 Aug;158[3]:523-34, Am J Public Health. 2015 May;105[5]:e87-94).
The patient navigation model is increasingly being adapted and used in a variety of contexts outside of cancer care as well. In a postpartum patient navigation program that we tested at Northwestern University’s Medicaid-based outpatient clinic, a navigator was hired to communicate with patients and support them between delivery and completion of their postpartum care. Patients were reminded through calls and/or texts of their postpartum visits and of the benefits of breastfeeding, effective contraception, and other postpartum practices.
The demonstration project was impactful: Women who were enrolled in the program were more likely to return for postpartum care, to receive World Health Organization Tier 1 or 2 contraception, and to have postpartum screening and vaccinations, compared with women who received care before the program began (Obstet Gynecol. 2017 May;129[5]:925-33).
Connections to our patients will help us to achieve health equity. This includes connections between the primary care we provide and the specialty care our patients sometimes require, both inside and outside of our field. We may refer a patient to an oncology team, for instance, and in the process, unwittingly transfer her care such that other conditions that we’ve been managing – hypertension, depression, or diabetes – fall by the wayside.
Instead, we have to re-engineer our processes so that we maintain personalized connections back to these patients. For example, the referring ob.gyn. could develop and send to the oncologist or gynecologic-oncologist a care plan that includes the patient’s comorbid conditions and how they could be managed. This would allow for clearer communication.
Our communities
As ob.gyns., we have a common goal of championing health equity and true population health for every woman, regardless of whether she lives in rural, urban, or suburban America and regardless of whether she has conservative or liberal values. To do so, we must extend ourselves beyond our own practices.
In a committee opinion on Racial and Ethnic Disparities in Obstetrics and Gynecology, the American College of Obstetricians and Gynecologists advises that ob.gyns. take a number of actions to increase health equity. These include raising awareness about inequity and its effects on health outcomes, promoting quality improvement projects that target disparities, working with public health leadership, and helping recruit ob.gyns. and other health care providers from racial and ethnic minority groups (Obstet Gynecol 2015;126:e130-4).
In Chicago, where 1 out of 5 people lives in poverty and 1 out of 10 lives in deep poverty, we are still in our infancy in combating health inequities. However, with partnerships between academic institutions, departments of health, and other organizations across various sectors, we are beginning to move the needle on these entrenched health inequities.
For example, in 2007, there was a 60% difference in breast cancer mortality between black and white women in Chicago. This disparity sparked the development of the Metropolitan Chicago Breast Cancer Task Force and a series of on-the-ground patient navigator programs, along with several key policy changes and new state laws.
State actions included requiring quality reporting on mammography and increasing the Medicaid reimbursement rate for mammography to the Medicare rate. Nationally, beneficial changes were made to Medicare’s quality metrics and to the National Breast and Cervical Cancer Early Detection Program. All told, through a combination of studies and initiatives focused on improving knowledge, trust, access to care, and quality of care, we have been able to decrease the breast cancer mortality gap by 20%.
We also have a role to play in nurturing and developing a workforce that better aligns with our evolving demographics. This involves redesigning how we plant seeds of opportunity among high school students, undergraduates, and young medical students, and how we seek job applicants. Moreover, when we help people get to the next step in their careers, we need to make sure there is continuous support to retain them and help propel them to the next level.
We should think creatively to establish programs or launch initiatives that can help level the playing field for all women. For example, I created a Massive Open Online Course called “Career 911: Your Future Job in Medicine and Healthcare” as a free workforce development pipeline program. It is accessible on a global platform (https://www.coursera.org/learn/healthcarejobs) and is one example of how we as ob.gyns. can leverage our skills and resources.
Along the way, we also need to train our students and residents – and ourselves – to be more familiar with, and articulate about, health care policy. We need to understand how policy is made and modified and how we can be good communicators and thought leaders.
Right now, our ability to articulate our patients’ stories to policy makers and to the public seems underdeveloped and undertapped. The onus is on us to write and speak about how all women must have the opportunity to not only access care but to access high-quality care and preventive services that are important for full health. Providing health equity isn’t about giving someone a handout, but about giving her a helping hand to take control of her health.
Achieving health equity will involve changing our approach to research. If medical research on women’s health continues to be dominated by studies in which participants are homogeneous and from mainly white or well-resourced populations, we will never have output that is generalizable. As practicing ob.gyns., we can look for opportunities to advocate for diversity in research. We can also acknowledge that, for some women, there is historically-rooted distrust of the health care system that serves as a barrier both to obtaining care and enrolling in trials.
By meeting women where they are, and by tailoring their individual boxes as best we can – in research, in workforce development, and in clinical care delivery – we can work toward solutions.
Strategies for achieving women’s health equity
• Modify office hours/dates to allow flexibility for women who have challenges scheduling childcare and time off from work.
• Ensure handouts, educational materials, and all communications are at appropriate health literacy levels.
• Acknowledge and understand an individual woman’s barriers to care, including social determinants of health, and create a care plan that is achievable for her.
• Learn about and refer women to local community resources needed to overcome barriers to care, such as childcare, social services support, support services for intimate partner violence, and substance abuse counseling.
• Examine office processes to optimize the number of visits women have to attend for a particular health issue. Are there ways to explain results and next steps in a care plan without having to make her come back for an office visit?
Dr. Simon is the George H. Gardner Professor of Clinical Gynecology at Northwestern University, Chicago, and director of the Chicago Cancer Health Equity Collaborative. She is a member of the U.S. Preventive Services Task Force, but the views expressed in this piece are her own.
Of all the medical professions, obstetrics and gynecology should be the strongest champion for equity in women’s health in this country and globally. The question is, what does this mean in the reality of 2017 and moving forward in the 21st century? What does it mean in the context of our own practices and in the landscape of current policy and politics?
Finding answers to these questions requires both a deep understanding of the meaning of health equity and a willingness to rethink the architecture and engineering of how we currently provide care.
The terms equity and equality are sometimes used interchangeably, but they actually have quite different meanings. Imagine three women of different heights standing underneath the lowest branch of a tall apple tree. None of the three women are tall enough to pick an apple from the branch.
If we think about equality, we would assist each woman by giving her a box to stand on, and all three boxes would be the same size. This means that while the tallest woman will now be able to pick an apple, the medium-height woman may be able to touch but not pick the apple, and the shortest woman still may not be able to reach the apple at all.
However, if we think about equity, we’d acknowledge that each woman needs her own personalized box to be able to pick the apple. For instance, the shortest woman may need a box that is three times the height of the box used by the tallest woman.
Achieving true population health for all women requires that we similarly eliminate inequities by providing each patient with her own personalized care plan to help her reach and maintain her health.
Women from minority groups have higher rates of low birth weight, preterm birth, stillbirth, gestational diabetes and its complications, HIV, breast cancer mortality and cervical cancer incidence and mortality, infertility and response to fertility treatment, and maternal mortality.
Yet inequity runs deeper than racial/ethnic labels; disparities also are created by a host of other factors, from cognitive or physical disabilities to gender or sexual identity or orientation, one’s ZIP code, working environment, language, and health literacy.
More than ever, the art of medicine involves understanding how to meet every patient where she is – given her own context and beliefs and levels of support – so that every woman has the opportunity to stand on the right-sized box and pick the apple and thrive.
Our practices
Provider bias and stereotyping can impact health care and health outcomes, and it is important that we work to prevent this in ourselves and in our staff. This means not making assumptions. It means really listening to our patients in ways that we may not have before.
Women who have experienced health inequity may have unique barriers to success. Therefore, we must listen for cues and inquire about our patients’ environment and circumstances, as well as their partnerships and support – or lack thereof. We should then acknowledge and communicate that certain social and environmental factors may impact our ability to achieve a desired outcome.
How can we impact the diet of a patient with gestational diabetes, for instance, if we have not adequately communicated what medical nutritional therapy means in the context of her own culture and ability to access food? If she lives in a food desert or has food insecurity or lives in a violence-ridden neighborhood that keeps her from going to a grocery store regularly, we must think outside the box. Ob.gyns. and their clinical care teams can work with women who have less access to nutritious foods, or who have certain cultural food staples, to suggest recipes and grocery lists that make sense with respect to the types of stores they shop in or their cultural preferences.
When it comes to cancer prevention and treatment, how can we expect a woman to be compliant with screening if we cannot help her understand that she can get screening services for free with her health insurance? How can we help a woman who has coverage for, or access to, free screening but then no funding or coverage for a diagnostic test or cancer treatment? How can we support a patient with abnormal cancer screening results who hasn’t followed up for months because she is afraid to leave home without her partner’s permission?
Such questions and circumstances often involve what we call “social determinants of health,” and they force us to rethink how we can better deliver and optimize care. Re-engineering our practices for health equity may involve employing a more diverse practice staff, linking patients with community resources, modifying our practice hours to align better with working women’s schedules, or finding creative ways to discern patients’ motivating factors and then piggyback on these factors.
We may also need to modify how we approach the number of return visits that we request of women so that follow-up care aligns better with their ability to leave work or find childcare. Simply put, we should strive to set up our patients for success, not failure.
We can pointedly ask patients about the kinds of information and support they want and need. We might ask, for instance: What do you need, and how can I work with you, so that you can effectively monitor and control your glucose levels? How can I work with you to help you get onto a trajectory to stop smoking? How can I help you better understand what tests and procedures are covered under your insurance plan, or whether you qualify for free services?
Patients with lower health literacy may need teach-back methods to validate understanding, or messaging that is more focused and limited at any one time. Self-efficacy through patient-centered education and support should be our goal.
Practices and clinics may also be able to adapt elements of the National Cancer Institute’s multicenter Patient Navigation Research Program, in which community health workers or other “patient navigators” address women’s personal barriers to the timely follow-up of abnormal breast and cervical cancer screening results. Patient navigation through this program and similar projects, including programs that we’ve adapted for different racial and ethnic communities in and around Chicago, has reduced or eliminated delays in diagnostic resolution of gynecologic cancer (Cancer. 2015 Nov 15;121[22]:4025-34, Breast Cancer Res Treat. 2016 Aug;158[3]:523-34, Am J Public Health. 2015 May;105[5]:e87-94).
The patient navigation model is increasingly being adapted and used in a variety of contexts outside of cancer care as well. In a postpartum patient navigation program that we tested at Northwestern University’s Medicaid-based outpatient clinic, a navigator was hired to communicate with patients and support them between delivery and completion of their postpartum care. Patients were reminded through calls and/or texts of their postpartum visits and of the benefits of breastfeeding, effective contraception, and other postpartum practices.
The demonstration project was impactful: Women who were enrolled in the program were more likely to return for postpartum care, to receive World Health Organization Tier 1 or 2 contraception, and to have postpartum screening and vaccinations, compared with women who received care before the program began (Obstet Gynecol. 2017 May;129[5]:925-33).
Connections to our patients will help us to achieve health equity. This includes connections between the primary care we provide and the specialty care our patients sometimes require, both inside and outside of our field. We may refer a patient to an oncology team, for instance, and in the process, unwittingly transfer her care such that other conditions that we’ve been managing – hypertension, depression, or diabetes – fall by the wayside.
Instead, we have to re-engineer our processes so that we maintain personalized connections back to these patients. For example, the referring ob.gyn. could develop and send to the oncologist or gynecologic-oncologist a care plan that includes the patient’s comorbid conditions and how they could be managed. This would allow for clearer communication.
Our communities
As ob.gyns., we have a common goal of championing health equity and true population health for every woman, regardless of whether she lives in rural, urban, or suburban America and regardless of whether she has conservative or liberal values. To do so, we must extend ourselves beyond our own practices.
In a committee opinion on Racial and Ethnic Disparities in Obstetrics and Gynecology, the American College of Obstetricians and Gynecologists advises that ob.gyns. take a number of actions to increase health equity. These include raising awareness about inequity and its effects on health outcomes, promoting quality improvement projects that target disparities, working with public health leadership, and helping recruit ob.gyns. and other health care providers from racial and ethnic minority groups (Obstet Gynecol 2015;126:e130-4).
In Chicago, where 1 out of 5 people lives in poverty and 1 out of 10 lives in deep poverty, we are still in our infancy in combating health inequities. However, with partnerships between academic institutions, departments of health, and other organizations across various sectors, we are beginning to move the needle on these entrenched health inequities.
For example, in 2007, there was a 60% difference in breast cancer mortality between black and white women in Chicago. This disparity sparked the development of the Metropolitan Chicago Breast Cancer Task Force and a series of on-the-ground patient navigator programs, along with several key policy changes and new state laws.
State actions included requiring quality reporting on mammography and increasing the Medicaid reimbursement rate for mammography to the Medicare rate. Nationally, beneficial changes were made to Medicare’s quality metrics and to the National Breast and Cervical Cancer Early Detection Program. All told, through a combination of studies and initiatives focused on improving knowledge, trust, access to care, and quality of care, we have been able to decrease the breast cancer mortality gap by 20%.
We also have a role to play in nurturing and developing a workforce that better aligns with our evolving demographics. This involves redesigning how we plant seeds of opportunity among high school students, undergraduates, and young medical students, and how we seek job applicants. Moreover, when we help people get to the next step in their careers, we need to make sure there is continuous support to retain them and help propel them to the next level.
We should think creatively to establish programs or launch initiatives that can help level the playing field for all women. For example, I created a Massive Open Online Course called “Career 911: Your Future Job in Medicine and Healthcare” as a free workforce development pipeline program. It is accessible on a global platform (https://www.coursera.org/learn/healthcarejobs) and is one example of how we as ob.gyns. can leverage our skills and resources.
Along the way, we also need to train our students and residents – and ourselves – to be more familiar with, and articulate about, health care policy. We need to understand how policy is made and modified and how we can be good communicators and thought leaders.
Right now, our ability to articulate our patients’ stories to policy makers and to the public seems underdeveloped and undertapped. The onus is on us to write and speak about how all women must have the opportunity to not only access care but to access high-quality care and preventive services that are important for full health. Providing health equity isn’t about giving someone a handout, but about giving her a helping hand to take control of her health.
Achieving health equity will involve changing our approach to research. If medical research on women’s health continues to be dominated by studies in which participants are homogeneous and from mainly white or well-resourced populations, we will never have output that is generalizable. As practicing ob.gyns., we can look for opportunities to advocate for diversity in research. We can also acknowledge that, for some women, there is historically-rooted distrust of the health care system that serves as a barrier both to obtaining care and enrolling in trials.
By meeting women where they are, and by tailoring their individual boxes as best we can – in research, in workforce development, and in clinical care delivery – we can work toward solutions.
Strategies for achieving women’s health equity
• Modify office hours/dates to allow flexibility for women who have challenges scheduling childcare and time off from work.
• Ensure handouts, educational materials, and all communications are at appropriate health literacy levels.
• Acknowledge and understand an individual woman’s barriers to care, including social determinants of health, and create a care plan that is achievable for her.
• Learn about and refer women to local community resources needed to overcome barriers to care, such as childcare, social services support, support services for intimate partner violence, and substance abuse counseling.
• Examine office processes to optimize the number of visits women have to attend for a particular health issue. Are there ways to explain results and next steps in a care plan without having to make her come back for an office visit?
Dr. Simon is the George H. Gardner Professor of Clinical Gynecology at Northwestern University, Chicago, and director of the Chicago Cancer Health Equity Collaborative. She is a member of the U.S. Preventive Services Task Force, but the views expressed in this piece are her own.
Of all the medical professions, obstetrics and gynecology should be the strongest champion for equity in women’s health in this country and globally. The question is, what does this mean in the reality of 2017 and moving forward in the 21st century? What does it mean in the context of our own practices and in the landscape of current policy and politics?
Finding answers to these questions requires both a deep understanding of the meaning of health equity and a willingness to rethink the architecture and engineering of how we currently provide care.
The terms equity and equality are sometimes used interchangeably, but they actually have quite different meanings. Imagine three women of different heights standing underneath the lowest branch of a tall apple tree. None of the three women are tall enough to pick an apple from the branch.
If we think about equality, we would assist each woman by giving her a box to stand on, and all three boxes would be the same size. This means that while the tallest woman will now be able to pick an apple, the medium-height woman may be able to touch but not pick the apple, and the shortest woman still may not be able to reach the apple at all.
However, if we think about equity, we’d acknowledge that each woman needs her own personalized box to be able to pick the apple. For instance, the shortest woman may need a box that is three times the height of the box used by the tallest woman.
Achieving true population health for all women requires that we similarly eliminate inequities by providing each patient with her own personalized care plan to help her reach and maintain her health.
Women from minority groups have higher rates of low birth weight, preterm birth, stillbirth, gestational diabetes and its complications, HIV, breast cancer mortality and cervical cancer incidence and mortality, infertility and response to fertility treatment, and maternal mortality.
Yet inequity runs deeper than racial/ethnic labels; disparities also are created by a host of other factors, from cognitive or physical disabilities to gender or sexual identity or orientation, one’s ZIP code, working environment, language, and health literacy.
More than ever, the art of medicine involves understanding how to meet every patient where she is – given her own context and beliefs and levels of support – so that every woman has the opportunity to stand on the right-sized box and pick the apple and thrive.
Our practices
Provider bias and stereotyping can impact health care and health outcomes, and it is important that we work to prevent this in ourselves and in our staff. This means not making assumptions. It means really listening to our patients in ways that we may not have before.
Women who have experienced health inequity may have unique barriers to success. Therefore, we must listen for cues and inquire about our patients’ environment and circumstances, as well as their partnerships and support – or lack thereof. We should then acknowledge and communicate that certain social and environmental factors may impact our ability to achieve a desired outcome.
How can we impact the diet of a patient with gestational diabetes, for instance, if we have not adequately communicated what medical nutritional therapy means in the context of her own culture and ability to access food? If she lives in a food desert or has food insecurity or lives in a violence-ridden neighborhood that keeps her from going to a grocery store regularly, we must think outside the box. Ob.gyns. and their clinical care teams can work with women who have less access to nutritious foods, or who have certain cultural food staples, to suggest recipes and grocery lists that make sense with respect to the types of stores they shop in or their cultural preferences.
When it comes to cancer prevention and treatment, how can we expect a woman to be compliant with screening if we cannot help her understand that she can get screening services for free with her health insurance? How can we help a woman who has coverage for, or access to, free screening but then no funding or coverage for a diagnostic test or cancer treatment? How can we support a patient with abnormal cancer screening results who hasn’t followed up for months because she is afraid to leave home without her partner’s permission?
Such questions and circumstances often involve what we call “social determinants of health,” and they force us to rethink how we can better deliver and optimize care. Re-engineering our practices for health equity may involve employing a more diverse practice staff, linking patients with community resources, modifying our practice hours to align better with working women’s schedules, or finding creative ways to discern patients’ motivating factors and then piggyback on these factors.
We may also need to modify how we approach the number of return visits that we request of women so that follow-up care aligns better with their ability to leave work or find childcare. Simply put, we should strive to set up our patients for success, not failure.
We can pointedly ask patients about the kinds of information and support they want and need. We might ask, for instance: What do you need, and how can I work with you, so that you can effectively monitor and control your glucose levels? How can I work with you to help you get onto a trajectory to stop smoking? How can I help you better understand what tests and procedures are covered under your insurance plan, or whether you qualify for free services?
Patients with lower health literacy may need teach-back methods to validate understanding, or messaging that is more focused and limited at any one time. Self-efficacy through patient-centered education and support should be our goal.
Practices and clinics may also be able to adapt elements of the National Cancer Institute’s multicenter Patient Navigation Research Program, in which community health workers or other “patient navigators” address women’s personal barriers to the timely follow-up of abnormal breast and cervical cancer screening results. Patient navigation through this program and similar projects, including programs that we’ve adapted for different racial and ethnic communities in and around Chicago, has reduced or eliminated delays in diagnostic resolution of gynecologic cancer (Cancer. 2015 Nov 15;121[22]:4025-34, Breast Cancer Res Treat. 2016 Aug;158[3]:523-34, Am J Public Health. 2015 May;105[5]:e87-94).
The patient navigation model is increasingly being adapted and used in a variety of contexts outside of cancer care as well. In a postpartum patient navigation program that we tested at Northwestern University’s Medicaid-based outpatient clinic, a navigator was hired to communicate with patients and support them between delivery and completion of their postpartum care. Patients were reminded through calls and/or texts of their postpartum visits and of the benefits of breastfeeding, effective contraception, and other postpartum practices.
The demonstration project was impactful: Women who were enrolled in the program were more likely to return for postpartum care, to receive World Health Organization Tier 1 or 2 contraception, and to have postpartum screening and vaccinations, compared with women who received care before the program began (Obstet Gynecol. 2017 May;129[5]:925-33).
Connections to our patients will help us to achieve health equity. This includes connections between the primary care we provide and the specialty care our patients sometimes require, both inside and outside of our field. We may refer a patient to an oncology team, for instance, and in the process, unwittingly transfer her care such that other conditions that we’ve been managing – hypertension, depression, or diabetes – fall by the wayside.
Instead, we have to re-engineer our processes so that we maintain personalized connections back to these patients. For example, the referring ob.gyn. could develop and send to the oncologist or gynecologic-oncologist a care plan that includes the patient’s comorbid conditions and how they could be managed. This would allow for clearer communication.
Our communities
As ob.gyns., we have a common goal of championing health equity and true population health for every woman, regardless of whether she lives in rural, urban, or suburban America and regardless of whether she has conservative or liberal values. To do so, we must extend ourselves beyond our own practices.
In a committee opinion on Racial and Ethnic Disparities in Obstetrics and Gynecology, the American College of Obstetricians and Gynecologists advises that ob.gyns. take a number of actions to increase health equity. These include raising awareness about inequity and its effects on health outcomes, promoting quality improvement projects that target disparities, working with public health leadership, and helping recruit ob.gyns. and other health care providers from racial and ethnic minority groups (Obstet Gynecol 2015;126:e130-4).
In Chicago, where 1 out of 5 people lives in poverty and 1 out of 10 lives in deep poverty, we are still in our infancy in combating health inequities. However, with partnerships between academic institutions, departments of health, and other organizations across various sectors, we are beginning to move the needle on these entrenched health inequities.
For example, in 2007, there was a 60% difference in breast cancer mortality between black and white women in Chicago. This disparity sparked the development of the Metropolitan Chicago Breast Cancer Task Force and a series of on-the-ground patient navigator programs, along with several key policy changes and new state laws.
State actions included requiring quality reporting on mammography and increasing the Medicaid reimbursement rate for mammography to the Medicare rate. Nationally, beneficial changes were made to Medicare’s quality metrics and to the National Breast and Cervical Cancer Early Detection Program. All told, through a combination of studies and initiatives focused on improving knowledge, trust, access to care, and quality of care, we have been able to decrease the breast cancer mortality gap by 20%.
We also have a role to play in nurturing and developing a workforce that better aligns with our evolving demographics. This involves redesigning how we plant seeds of opportunity among high school students, undergraduates, and young medical students, and how we seek job applicants. Moreover, when we help people get to the next step in their careers, we need to make sure there is continuous support to retain them and help propel them to the next level.
We should think creatively to establish programs or launch initiatives that can help level the playing field for all women. For example, I created a Massive Open Online Course called “Career 911: Your Future Job in Medicine and Healthcare” as a free workforce development pipeline program. It is accessible on a global platform (https://www.coursera.org/learn/healthcarejobs) and is one example of how we as ob.gyns. can leverage our skills and resources.
Along the way, we also need to train our students and residents – and ourselves – to be more familiar with, and articulate about, health care policy. We need to understand how policy is made and modified and how we can be good communicators and thought leaders.
Right now, our ability to articulate our patients’ stories to policy makers and to the public seems underdeveloped and undertapped. The onus is on us to write and speak about how all women must have the opportunity to not only access care but to access high-quality care and preventive services that are important for full health. Providing health equity isn’t about giving someone a handout, but about giving her a helping hand to take control of her health.
Achieving health equity will involve changing our approach to research. If medical research on women’s health continues to be dominated by studies in which participants are homogeneous and from mainly white or well-resourced populations, we will never have output that is generalizable. As practicing ob.gyns., we can look for opportunities to advocate for diversity in research. We can also acknowledge that, for some women, there is historically-rooted distrust of the health care system that serves as a barrier both to obtaining care and enrolling in trials.
By meeting women where they are, and by tailoring their individual boxes as best we can – in research, in workforce development, and in clinical care delivery – we can work toward solutions.
Strategies for achieving women’s health equity
• Modify office hours/dates to allow flexibility for women who have challenges scheduling childcare and time off from work.
• Ensure handouts, educational materials, and all communications are at appropriate health literacy levels.
• Acknowledge and understand an individual woman’s barriers to care, including social determinants of health, and create a care plan that is achievable for her.
• Learn about and refer women to local community resources needed to overcome barriers to care, such as childcare, social services support, support services for intimate partner violence, and substance abuse counseling.
• Examine office processes to optimize the number of visits women have to attend for a particular health issue. Are there ways to explain results and next steps in a care plan without having to make her come back for an office visit?
Dr. Simon is the George H. Gardner Professor of Clinical Gynecology at Northwestern University, Chicago, and director of the Chicago Cancer Health Equity Collaborative. She is a member of the U.S. Preventive Services Task Force, but the views expressed in this piece are her own.