User login
Hypertension in SLE pregnancy: Is it lupus flare or preeclampsia?
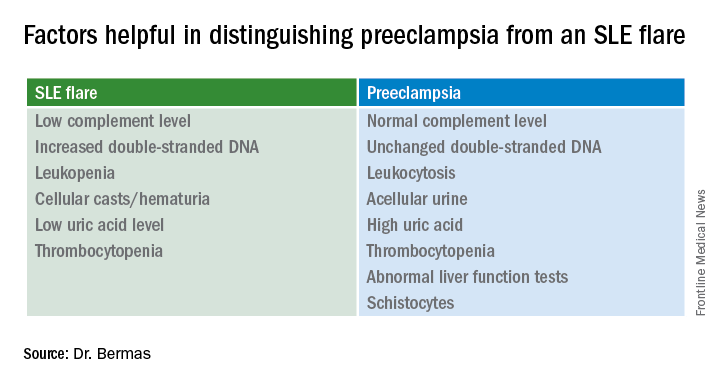
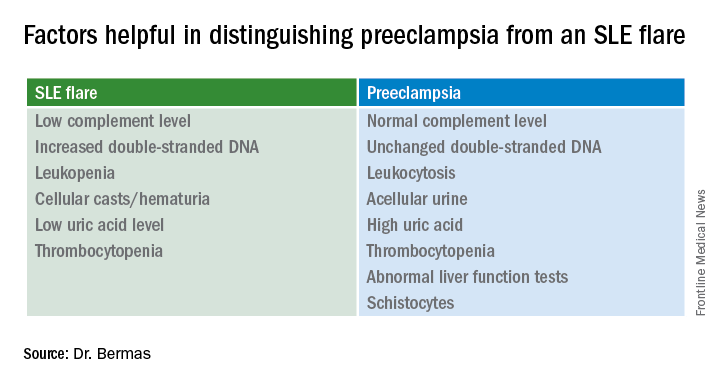
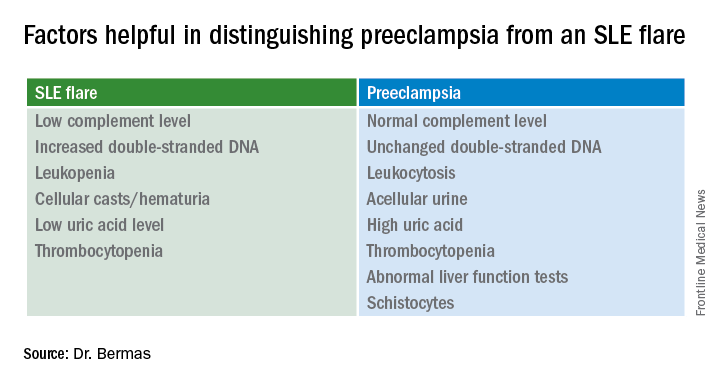
SNOWMASS, COLO. – No hard and fast test exists that would enable a physician to tell a flare of systemic lupus erythematosus from preeclampsia in a pregnant lupus patient who becomes hypertensive and ill, but there are highly useful clues, Bonnie L. Bermas, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“There is no perfect way of distinguishing between a lupus flare and preeclampsia. I’ve never walked away from the labor floor and said, ‘This is great – I know this is a lupus flare,’ or ‘I know this is preeclampsia.’ But you make your best guess as to which one it is, and that will inform your management,” explained Dr. Bermas, a rheumatologist and director of the clinical lupus program at Brigham and Women’s Hospital in Boston.
“Why do we care? Because if it’s preeclampsia the mother needs to be delivered immediately for her safety, while if it’s an SLE flare sometimes you can treat it and get the fetus to a more viable age. A 23-week-old baby isn’t at all likely to make it, but a 27-week-old could,” Dr. Bermas said.
The fact that the patient has thrombocytopenia isn’t helpful in making the distinction, since that feature is shared in common by SLE flares and preeclampsia. But the uric acid level is a useful clue.
It’s quite possible that much of the current guesswork in predicting preeclampsia and other adverse pregnancy outcomes in lupus patients will give way to reliable risk testing within the next several years. Investigators in the U.S. multicenter prospective PROMISSE (Predictors of Pregnancy Outcome: Biomarkers in APL Syndrome and SLE) study have reported that circulating levels of the angiogenic factors soluble fms-like tyrosine kinase-1 and placental growth factor were abnormal as early as gestational weeks 12-15 in patients who went on to develop preeclampsia or other adverse pregnancy outcomes.
Indeed, monthly testing demonstrated that SLE patients in the top quartile for soluble fms-like tyrosine kinase-1 at weeks 12-15 had an adjusted 17.3-fold greater likelihood of experiencing a severe adverse pregnancy outcome than did those in the lowest quartile. A high level had a positive predictive value of 61% and a negative predictive value of 93% (Am J Obstet Gynecol. 2016 Jan;214[1]:108.e1-14). These findings are being further explored in ongoing studies.
“Hopefully, in another few years we’re going to be able to say early in pregnancy, ‘This person is set up to get preeclampsia.’ Maybe that will lead to better treatment as well,” Dr. Bermas said.
The risk of preeclampsia has been shown to be threefold higher in women with SLE than in the general population of pregnant women in a study of more than 16.7 million admissions for childbirth in the United States during a 4-year period. The SLE patients were also at 2.4-fold increased risk for preterm labor. Their risks of infection, thrombosis, thrombocytopenia, and transfusion were each three- to seven-fold higher as well (Am J Obstet Gynecol. 2008 Aug;199[2]:127.e1-16).
Dr. Bermas reported serving as a consultant to UCB.
SNOWMASS, COLO. – No hard and fast test exists that would enable a physician to tell a flare of systemic lupus erythematosus from preeclampsia in a pregnant lupus patient who becomes hypertensive and ill, but there are highly useful clues, Bonnie L. Bermas, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“There is no perfect way of distinguishing between a lupus flare and preeclampsia. I’ve never walked away from the labor floor and said, ‘This is great – I know this is a lupus flare,’ or ‘I know this is preeclampsia.’ But you make your best guess as to which one it is, and that will inform your management,” explained Dr. Bermas, a rheumatologist and director of the clinical lupus program at Brigham and Women’s Hospital in Boston.
“Why do we care? Because if it’s preeclampsia the mother needs to be delivered immediately for her safety, while if it’s an SLE flare sometimes you can treat it and get the fetus to a more viable age. A 23-week-old baby isn’t at all likely to make it, but a 27-week-old could,” Dr. Bermas said.
The fact that the patient has thrombocytopenia isn’t helpful in making the distinction, since that feature is shared in common by SLE flares and preeclampsia. But the uric acid level is a useful clue.
It’s quite possible that much of the current guesswork in predicting preeclampsia and other adverse pregnancy outcomes in lupus patients will give way to reliable risk testing within the next several years. Investigators in the U.S. multicenter prospective PROMISSE (Predictors of Pregnancy Outcome: Biomarkers in APL Syndrome and SLE) study have reported that circulating levels of the angiogenic factors soluble fms-like tyrosine kinase-1 and placental growth factor were abnormal as early as gestational weeks 12-15 in patients who went on to develop preeclampsia or other adverse pregnancy outcomes.
Indeed, monthly testing demonstrated that SLE patients in the top quartile for soluble fms-like tyrosine kinase-1 at weeks 12-15 had an adjusted 17.3-fold greater likelihood of experiencing a severe adverse pregnancy outcome than did those in the lowest quartile. A high level had a positive predictive value of 61% and a negative predictive value of 93% (Am J Obstet Gynecol. 2016 Jan;214[1]:108.e1-14). These findings are being further explored in ongoing studies.
“Hopefully, in another few years we’re going to be able to say early in pregnancy, ‘This person is set up to get preeclampsia.’ Maybe that will lead to better treatment as well,” Dr. Bermas said.
The risk of preeclampsia has been shown to be threefold higher in women with SLE than in the general population of pregnant women in a study of more than 16.7 million admissions for childbirth in the United States during a 4-year period. The SLE patients were also at 2.4-fold increased risk for preterm labor. Their risks of infection, thrombosis, thrombocytopenia, and transfusion were each three- to seven-fold higher as well (Am J Obstet Gynecol. 2008 Aug;199[2]:127.e1-16).
Dr. Bermas reported serving as a consultant to UCB.
SNOWMASS, COLO. – No hard and fast test exists that would enable a physician to tell a flare of systemic lupus erythematosus from preeclampsia in a pregnant lupus patient who becomes hypertensive and ill, but there are highly useful clues, Bonnie L. Bermas, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
“There is no perfect way of distinguishing between a lupus flare and preeclampsia. I’ve never walked away from the labor floor and said, ‘This is great – I know this is a lupus flare,’ or ‘I know this is preeclampsia.’ But you make your best guess as to which one it is, and that will inform your management,” explained Dr. Bermas, a rheumatologist and director of the clinical lupus program at Brigham and Women’s Hospital in Boston.
“Why do we care? Because if it’s preeclampsia the mother needs to be delivered immediately for her safety, while if it’s an SLE flare sometimes you can treat it and get the fetus to a more viable age. A 23-week-old baby isn’t at all likely to make it, but a 27-week-old could,” Dr. Bermas said.
The fact that the patient has thrombocytopenia isn’t helpful in making the distinction, since that feature is shared in common by SLE flares and preeclampsia. But the uric acid level is a useful clue.
It’s quite possible that much of the current guesswork in predicting preeclampsia and other adverse pregnancy outcomes in lupus patients will give way to reliable risk testing within the next several years. Investigators in the U.S. multicenter prospective PROMISSE (Predictors of Pregnancy Outcome: Biomarkers in APL Syndrome and SLE) study have reported that circulating levels of the angiogenic factors soluble fms-like tyrosine kinase-1 and placental growth factor were abnormal as early as gestational weeks 12-15 in patients who went on to develop preeclampsia or other adverse pregnancy outcomes.
Indeed, monthly testing demonstrated that SLE patients in the top quartile for soluble fms-like tyrosine kinase-1 at weeks 12-15 had an adjusted 17.3-fold greater likelihood of experiencing a severe adverse pregnancy outcome than did those in the lowest quartile. A high level had a positive predictive value of 61% and a negative predictive value of 93% (Am J Obstet Gynecol. 2016 Jan;214[1]:108.e1-14). These findings are being further explored in ongoing studies.
“Hopefully, in another few years we’re going to be able to say early in pregnancy, ‘This person is set up to get preeclampsia.’ Maybe that will lead to better treatment as well,” Dr. Bermas said.
The risk of preeclampsia has been shown to be threefold higher in women with SLE than in the general population of pregnant women in a study of more than 16.7 million admissions for childbirth in the United States during a 4-year period. The SLE patients were also at 2.4-fold increased risk for preterm labor. Their risks of infection, thrombosis, thrombocytopenia, and transfusion were each three- to seven-fold higher as well (Am J Obstet Gynecol. 2008 Aug;199[2]:127.e1-16).
Dr. Bermas reported serving as a consultant to UCB.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
VIDEO: Dual antibiotic prophylaxis cuts cesarean SSIs
LAS VEGAS – Two days of prophylaxis with two oral antibiotics cut the surgical site infection rate by more than half in a randomized trial with more than 400 obese women who had cesarean deliveries.
The protective effect from combined treatment with cephalexin and metronidazole was especially powerful in the most at-risk patients, women with ruptured membranes before cesarean surgery. In this subgroup prophylaxis with the two antibiotics for 2 days cut surgical site infections (SSIs) during the 30 days after surgery, from a rate of 33% in control women who received placebo to a 10% rate, a 77% relative risk reduction that was statistically significant, Carri R. Warshak, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal and Fetal Medicine.
“I am very excited that we found a way to help the kinds of women in the study, very-high-risk women, with an effective way to reduce their risk of infection,” Dr. Warshak of the University of Cincinnati said in a video interview. The obese women enrolled in the study, especially those with ruptured membranes, “have a very high risk of morbidity, so it’s very exciting that we found a way to help prevent” SSIs.
“Our study is the first to target postpartum interventions to reduce SSIs specifically in this high-risk population” of obese mothers, said Amy M. Valent, DO, a maternal fetal medicine clinician at Oregon Health & Science University in Portland, who ran the trial with Dr. Warshak.
The trial randomized women with a body mass index of at least 30 kg/m2 who underwent a planned or unplanned cesarean delivery at the University of Cincinnati during 2010-2015. Following standard management during cesarean delivery, the women received either 500 mg oral cephalexin and 500 mg oral metronidazole or placebo every 8 hours for 48 hours following delivery. The primary outcome was the incidence of SSIs, and randomization was stratified so that similar numbers of women with ruptured membranes got into each treatment arm. The enrolled women averaged 28 years of age, and average BMI was about 40 kg/m2. Nearly a third of the women had ruptured membranes at the time of surgery, more than a quarter of the enrolled women used tobacco, and more than a fifth had preeclampsia.
Additional analyses reported at the meeting by Dr. Valent showed that other risk factors that significantly boosted the rate of SSIs were labor prior to delivery, use of internal monitoring, and operative time of more than 90 minutes. Antibiotic prophylaxis was able to significantly reduce SSI rates in women with any of these additional risk factors, compared with placebo. A cost effectiveness analysis she ran estimated that if the antibiotic prophylaxis tested in the study were used on the roughly 460,000 obese U.S. women having cesarean deliveries annually, it would be cost saving as long as the antibiotic regimen cost no more than $357 a person. Factoring in the SSIs and long-term morbidity that prophylaxis would prevent, and the quality-adjusted life-years it would add, showed that prophylaxis would be cost-effective up to a cost of $33,557 per woman.
The prophylaxis carries a “relatively low cost and is easy to use,” Dr. Valent said.
Safety of the antibiotic combination was a question raised by Laura E. Riley, MD, director of ob.gyn. infectious disease and labor and delivery at Massachusetts General Hospital in Boston. “My biggest concern is 48 hours of these antibiotics,” and whether prophylaxis could be achieved with fewer doses, she said in an interview. “I’d want to minimize the dosage, and also try other, nondrug approaches to minimizing SSI risk in obese women.”
“I wouldn’t say that universally, every obstetrical program should do this, but clinicians should look at the comorbidities their mothers have and their SSI rates. There are populations out there at lower risk, but there are also populations like ours, with a SSI rate of 10%-20%,” Dr. Warshak said.
She also acknowledged that even her own obstetrical group in Cincinnati needs to now reach a consensus on an appropriate strategy for expanded cesarean-delivery prophylaxis. That’s because a 2016 report from a large, randomized trial documented another successful strategy for limiting infections following cesarean delivery: a preoperative intravenous dose of azithromycin as a supplement to standard cefazolin. The Cesarean Section Optimal Antibiotic Prophylaxis (C/SOAP) trial, done in women with any BMI but specifically nonelective cesarean deliveries, showed a significant reduction in the combined rate of SSIs, endometritis, or any other infection during 6 weeks of follow-up among women who received azithromycin on top of standard prophylaxis (N Engl J Med. 2016 Sept 29;375[13]:1231-41).
“The bottom line is that, a couple of grams of cefazolin [administered before the incision] isn’t enough, especially for women with risk factors for infection. We see infection rates of more than 10% because cefazolin alone is simply inadequate. The results from both our study and the 2016 study show we can do better to reduce morbidity,” said Dr. Warshak.
“In high-risk women, such as those who are obese, we probably need to expand the spectrum and duration of prophylaxis,” agreed Dr. Main. “Obesity is one high-risk group, but there are others.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Two days of prophylaxis with two oral antibiotics cut the surgical site infection rate by more than half in a randomized trial with more than 400 obese women who had cesarean deliveries.
The protective effect from combined treatment with cephalexin and metronidazole was especially powerful in the most at-risk patients, women with ruptured membranes before cesarean surgery. In this subgroup prophylaxis with the two antibiotics for 2 days cut surgical site infections (SSIs) during the 30 days after surgery, from a rate of 33% in control women who received placebo to a 10% rate, a 77% relative risk reduction that was statistically significant, Carri R. Warshak, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal and Fetal Medicine.
“I am very excited that we found a way to help the kinds of women in the study, very-high-risk women, with an effective way to reduce their risk of infection,” Dr. Warshak of the University of Cincinnati said in a video interview. The obese women enrolled in the study, especially those with ruptured membranes, “have a very high risk of morbidity, so it’s very exciting that we found a way to help prevent” SSIs.
“Our study is the first to target postpartum interventions to reduce SSIs specifically in this high-risk population” of obese mothers, said Amy M. Valent, DO, a maternal fetal medicine clinician at Oregon Health & Science University in Portland, who ran the trial with Dr. Warshak.
The trial randomized women with a body mass index of at least 30 kg/m2 who underwent a planned or unplanned cesarean delivery at the University of Cincinnati during 2010-2015. Following standard management during cesarean delivery, the women received either 500 mg oral cephalexin and 500 mg oral metronidazole or placebo every 8 hours for 48 hours following delivery. The primary outcome was the incidence of SSIs, and randomization was stratified so that similar numbers of women with ruptured membranes got into each treatment arm. The enrolled women averaged 28 years of age, and average BMI was about 40 kg/m2. Nearly a third of the women had ruptured membranes at the time of surgery, more than a quarter of the enrolled women used tobacco, and more than a fifth had preeclampsia.
Additional analyses reported at the meeting by Dr. Valent showed that other risk factors that significantly boosted the rate of SSIs were labor prior to delivery, use of internal monitoring, and operative time of more than 90 minutes. Antibiotic prophylaxis was able to significantly reduce SSI rates in women with any of these additional risk factors, compared with placebo. A cost effectiveness analysis she ran estimated that if the antibiotic prophylaxis tested in the study were used on the roughly 460,000 obese U.S. women having cesarean deliveries annually, it would be cost saving as long as the antibiotic regimen cost no more than $357 a person. Factoring in the SSIs and long-term morbidity that prophylaxis would prevent, and the quality-adjusted life-years it would add, showed that prophylaxis would be cost-effective up to a cost of $33,557 per woman.
The prophylaxis carries a “relatively low cost and is easy to use,” Dr. Valent said.
Safety of the antibiotic combination was a question raised by Laura E. Riley, MD, director of ob.gyn. infectious disease and labor and delivery at Massachusetts General Hospital in Boston. “My biggest concern is 48 hours of these antibiotics,” and whether prophylaxis could be achieved with fewer doses, she said in an interview. “I’d want to minimize the dosage, and also try other, nondrug approaches to minimizing SSI risk in obese women.”
“I wouldn’t say that universally, every obstetrical program should do this, but clinicians should look at the comorbidities their mothers have and their SSI rates. There are populations out there at lower risk, but there are also populations like ours, with a SSI rate of 10%-20%,” Dr. Warshak said.
She also acknowledged that even her own obstetrical group in Cincinnati needs to now reach a consensus on an appropriate strategy for expanded cesarean-delivery prophylaxis. That’s because a 2016 report from a large, randomized trial documented another successful strategy for limiting infections following cesarean delivery: a preoperative intravenous dose of azithromycin as a supplement to standard cefazolin. The Cesarean Section Optimal Antibiotic Prophylaxis (C/SOAP) trial, done in women with any BMI but specifically nonelective cesarean deliveries, showed a significant reduction in the combined rate of SSIs, endometritis, or any other infection during 6 weeks of follow-up among women who received azithromycin on top of standard prophylaxis (N Engl J Med. 2016 Sept 29;375[13]:1231-41).
“The bottom line is that, a couple of grams of cefazolin [administered before the incision] isn’t enough, especially for women with risk factors for infection. We see infection rates of more than 10% because cefazolin alone is simply inadequate. The results from both our study and the 2016 study show we can do better to reduce morbidity,” said Dr. Warshak.
“In high-risk women, such as those who are obese, we probably need to expand the spectrum and duration of prophylaxis,” agreed Dr. Main. “Obesity is one high-risk group, but there are others.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Two days of prophylaxis with two oral antibiotics cut the surgical site infection rate by more than half in a randomized trial with more than 400 obese women who had cesarean deliveries.
The protective effect from combined treatment with cephalexin and metronidazole was especially powerful in the most at-risk patients, women with ruptured membranes before cesarean surgery. In this subgroup prophylaxis with the two antibiotics for 2 days cut surgical site infections (SSIs) during the 30 days after surgery, from a rate of 33% in control women who received placebo to a 10% rate, a 77% relative risk reduction that was statistically significant, Carri R. Warshak, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal and Fetal Medicine.
“I am very excited that we found a way to help the kinds of women in the study, very-high-risk women, with an effective way to reduce their risk of infection,” Dr. Warshak of the University of Cincinnati said in a video interview. The obese women enrolled in the study, especially those with ruptured membranes, “have a very high risk of morbidity, so it’s very exciting that we found a way to help prevent” SSIs.
“Our study is the first to target postpartum interventions to reduce SSIs specifically in this high-risk population” of obese mothers, said Amy M. Valent, DO, a maternal fetal medicine clinician at Oregon Health & Science University in Portland, who ran the trial with Dr. Warshak.
The trial randomized women with a body mass index of at least 30 kg/m2 who underwent a planned or unplanned cesarean delivery at the University of Cincinnati during 2010-2015. Following standard management during cesarean delivery, the women received either 500 mg oral cephalexin and 500 mg oral metronidazole or placebo every 8 hours for 48 hours following delivery. The primary outcome was the incidence of SSIs, and randomization was stratified so that similar numbers of women with ruptured membranes got into each treatment arm. The enrolled women averaged 28 years of age, and average BMI was about 40 kg/m2. Nearly a third of the women had ruptured membranes at the time of surgery, more than a quarter of the enrolled women used tobacco, and more than a fifth had preeclampsia.
Additional analyses reported at the meeting by Dr. Valent showed that other risk factors that significantly boosted the rate of SSIs were labor prior to delivery, use of internal monitoring, and operative time of more than 90 minutes. Antibiotic prophylaxis was able to significantly reduce SSI rates in women with any of these additional risk factors, compared with placebo. A cost effectiveness analysis she ran estimated that if the antibiotic prophylaxis tested in the study were used on the roughly 460,000 obese U.S. women having cesarean deliveries annually, it would be cost saving as long as the antibiotic regimen cost no more than $357 a person. Factoring in the SSIs and long-term morbidity that prophylaxis would prevent, and the quality-adjusted life-years it would add, showed that prophylaxis would be cost-effective up to a cost of $33,557 per woman.
The prophylaxis carries a “relatively low cost and is easy to use,” Dr. Valent said.
Safety of the antibiotic combination was a question raised by Laura E. Riley, MD, director of ob.gyn. infectious disease and labor and delivery at Massachusetts General Hospital in Boston. “My biggest concern is 48 hours of these antibiotics,” and whether prophylaxis could be achieved with fewer doses, she said in an interview. “I’d want to minimize the dosage, and also try other, nondrug approaches to minimizing SSI risk in obese women.”
“I wouldn’t say that universally, every obstetrical program should do this, but clinicians should look at the comorbidities their mothers have and their SSI rates. There are populations out there at lower risk, but there are also populations like ours, with a SSI rate of 10%-20%,” Dr. Warshak said.
She also acknowledged that even her own obstetrical group in Cincinnati needs to now reach a consensus on an appropriate strategy for expanded cesarean-delivery prophylaxis. That’s because a 2016 report from a large, randomized trial documented another successful strategy for limiting infections following cesarean delivery: a preoperative intravenous dose of azithromycin as a supplement to standard cefazolin. The Cesarean Section Optimal Antibiotic Prophylaxis (C/SOAP) trial, done in women with any BMI but specifically nonelective cesarean deliveries, showed a significant reduction in the combined rate of SSIs, endometritis, or any other infection during 6 weeks of follow-up among women who received azithromycin on top of standard prophylaxis (N Engl J Med. 2016 Sept 29;375[13]:1231-41).
“The bottom line is that, a couple of grams of cefazolin [administered before the incision] isn’t enough, especially for women with risk factors for infection. We see infection rates of more than 10% because cefazolin alone is simply inadequate. The results from both our study and the 2016 study show we can do better to reduce morbidity,” said Dr. Warshak.
“In high-risk women, such as those who are obese, we probably need to expand the spectrum and duration of prophylaxis,” agreed Dr. Main. “Obesity is one high-risk group, but there are others.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: Surgical site infections occurred in 7% of women who received oral prophylaxis and 16% of controls during 30-day follow-up.
Data source: A single-center randomized trial with 382 evaluable women.
Disclosures: Dr. Warshak had no relevant disclosures.
Study highlights importance of genotyping in von Willebrand disease
Patients with genetically confirmed von Willebrand disease (VWD) type 2M have a relatively mild clinical phenotype, according to findings from a retrospective cross-sectional study.
In fact, three of 31 patients included in the study had a near normal laboratory phenotype. Additionally, patients with the p.Val1360Ala mutation had significantly higher values of all von Willebrand factor (VWF)-related laboratory parameters, compared with those with the p.Arg1374Cys or p.Phe1293Leu mutation, Dominique Maas reported at the European Association for Haemophilia and Allied Disorders annual meeting.
The findings underscore the importance of genotyping for making a correct diagnosis of VWD type 2M, said Ms. Maas of Radboud University Medical Center, Nijmegen, The Netherlands.
The study subjects, who had a least one VWD type 2M mutation, had a median age of 34 years and a median bleeding score of 6. Most suffered from mucocutaneous bleeding, but with low frequency compared with other VWD subtypes. The incidence of muscle hematomas, postpartum hemorrhage, and postsurgery bleeding were relatively high, however. Age and bleeding score were strongly positively correlated.
Subjects had a median VWF antigen level of 24 IU dL-1, median VWF ristocetin cofactor activity of 6 IU dL-1, and median VSF:RCo/VWF:Ag ratio of 0.29. The VSF collagen binding activity and VWF:Ag ratio was normal, she said.
Genotyping is a powerful diagnostic tool for making an appropriate diagnosis and classification of VWD. The current findings are important because understanding the correlation between genotype and phenotype improves the understanding of VWD pathogenesis and has important implications for treatment, follow-up, and genetic counseling, but has not been throughly investigated in fully genotyped patients with VWD type 2M, she said.
Ms. Maas reported having no disclosures.
Patients with genetically confirmed von Willebrand disease (VWD) type 2M have a relatively mild clinical phenotype, according to findings from a retrospective cross-sectional study.
In fact, three of 31 patients included in the study had a near normal laboratory phenotype. Additionally, patients with the p.Val1360Ala mutation had significantly higher values of all von Willebrand factor (VWF)-related laboratory parameters, compared with those with the p.Arg1374Cys or p.Phe1293Leu mutation, Dominique Maas reported at the European Association for Haemophilia and Allied Disorders annual meeting.
The findings underscore the importance of genotyping for making a correct diagnosis of VWD type 2M, said Ms. Maas of Radboud University Medical Center, Nijmegen, The Netherlands.
The study subjects, who had a least one VWD type 2M mutation, had a median age of 34 years and a median bleeding score of 6. Most suffered from mucocutaneous bleeding, but with low frequency compared with other VWD subtypes. The incidence of muscle hematomas, postpartum hemorrhage, and postsurgery bleeding were relatively high, however. Age and bleeding score were strongly positively correlated.
Subjects had a median VWF antigen level of 24 IU dL-1, median VWF ristocetin cofactor activity of 6 IU dL-1, and median VSF:RCo/VWF:Ag ratio of 0.29. The VSF collagen binding activity and VWF:Ag ratio was normal, she said.
Genotyping is a powerful diagnostic tool for making an appropriate diagnosis and classification of VWD. The current findings are important because understanding the correlation between genotype and phenotype improves the understanding of VWD pathogenesis and has important implications for treatment, follow-up, and genetic counseling, but has not been throughly investigated in fully genotyped patients with VWD type 2M, she said.
Ms. Maas reported having no disclosures.
Patients with genetically confirmed von Willebrand disease (VWD) type 2M have a relatively mild clinical phenotype, according to findings from a retrospective cross-sectional study.
In fact, three of 31 patients included in the study had a near normal laboratory phenotype. Additionally, patients with the p.Val1360Ala mutation had significantly higher values of all von Willebrand factor (VWF)-related laboratory parameters, compared with those with the p.Arg1374Cys or p.Phe1293Leu mutation, Dominique Maas reported at the European Association for Haemophilia and Allied Disorders annual meeting.
The findings underscore the importance of genotyping for making a correct diagnosis of VWD type 2M, said Ms. Maas of Radboud University Medical Center, Nijmegen, The Netherlands.
The study subjects, who had a least one VWD type 2M mutation, had a median age of 34 years and a median bleeding score of 6. Most suffered from mucocutaneous bleeding, but with low frequency compared with other VWD subtypes. The incidence of muscle hematomas, postpartum hemorrhage, and postsurgery bleeding were relatively high, however. Age and bleeding score were strongly positively correlated.
Subjects had a median VWF antigen level of 24 IU dL-1, median VWF ristocetin cofactor activity of 6 IU dL-1, and median VSF:RCo/VWF:Ag ratio of 0.29. The VSF collagen binding activity and VWF:Ag ratio was normal, she said.
Genotyping is a powerful diagnostic tool for making an appropriate diagnosis and classification of VWD. The current findings are important because understanding the correlation between genotype and phenotype improves the understanding of VWD pathogenesis and has important implications for treatment, follow-up, and genetic counseling, but has not been throughly investigated in fully genotyped patients with VWD type 2M, she said.
Ms. Maas reported having no disclosures.
FROM EAHAD 2017
Key clinical point:
Major finding: Three of 31 patients included in the study had a near normal laboratory phenotype.
Data source: A retrospective cross-sectional study of 31 patients.
Disclosures: Ms. Maas reported having no disclosures.
Maternal mental health: New consensus on optimal care
A new consensus bundle of recommendations calls on ob.gyns. to integrate mental health care into their care of pregnant and postpartum women.
The interdisciplinary Council on Patient Safety in Women’s Health Care issued a consensus document summarizing existing recommendations on maternal mental health and pairing them with appropriate screening and other resources. The bundle of recommendations was jointly issued by the American College of Obstetricians and Gynecologists, the National Association of Nurse Practitioners in Women’s Health, and other groups (Obstet Gynecol. 2017 Mar;129(3):422-430)*.
While no novel information is included in the bundle, the goal is to provide a streamlined document that pairs previous recommendations with resources and tools.
“Embedding a mental health professional with the women’s health care provider would seem to be the ideal, [but] in reality, this may not be available in every setting or geographic location,” Susan Kendig, JD, MSN, WHNP-BC, FAANP, policy director for the National Association of Nurse Practitioners in Women’s Health, and one of the authors of the document, said in an interview. “The purpose of the consensus bundle is to provide a framework for women’s health care providers to use in developing a system of care that includes standardized risk assessment for existing or emerging mental health issues, strategies for brief interventions, identification of community resources available to the woman, and/or resources to support the provider in addressing the woman’s needs and facilitating appropriate referrals, and addressing emergencies to prevent harm.”
The framework is grouped in four domains: readiness, recognition and prevention, response, and reporting and systems learning.
Readiness is focused largely on setting up clinical and administrative protocols, including mental health screening that is seamlessly integrated into the patient visit, established algorithms that are triggered according to screening results, and designated staff to both educate colleagues on the protocols and to drive their implementation.
The goal for physicians in all settings, according to the authors, is to balance cost, availability of tools, ease of use, and the validity of the tools against the need to capture often unrecognized signs and symptoms of mood and anxiety disorders, including changes in sleep patterns, appetite, or anxiety levels that often are attributed to the physiologic and neuroendocrinologic changes inherent in childbirth. More than 80% of women know something is “off” but do not bring up their symptoms to their clinician, according to the recommendation document.
“Coordination and team cohesiveness is not necessarily dependent on co-location,” Ms. Kendig said. “Virtual teams, where care is coordinated among providers at different locations, can also achieve positive outcomes.”
The follow-on to this – recognition and prevention – views every patient visit as an opportunity to draw a thorough picture of mental and physical health by taking a complete family and patient history, maintaining routine screening, and offering psychoeducation to patients and their families or others on whom they rely for emotional support.
When a woman does screen positive for perinatal mood or anxiety disorders, the next bundle offers a rough outline of a stage-based response for intervention and follow-up.
“Screening alone does not appear to improve pregnancy or maternal-child outcomes,” the authors wrote.
Several possible algorithms are included in the document, including for emergent mental health concerns such as suicidal or homicidal ideation.
The final domain relies on data capture, taking a systems approach to not only delivering care, but also improving it. This includes scheduling regular staff debriefings after severe maternal mental health crises, troubleshooting why some patients become lost to follow-up, and examining data to see patterns.
On Twitter @whitneymcknight
CORRECTION, 3/20/17: An earlier version of this article misstated the citation.
A new consensus bundle of recommendations calls on ob.gyns. to integrate mental health care into their care of pregnant and postpartum women.
The interdisciplinary Council on Patient Safety in Women’s Health Care issued a consensus document summarizing existing recommendations on maternal mental health and pairing them with appropriate screening and other resources. The bundle of recommendations was jointly issued by the American College of Obstetricians and Gynecologists, the National Association of Nurse Practitioners in Women’s Health, and other groups (Obstet Gynecol. 2017 Mar;129(3):422-430)*.
While no novel information is included in the bundle, the goal is to provide a streamlined document that pairs previous recommendations with resources and tools.
“Embedding a mental health professional with the women’s health care provider would seem to be the ideal, [but] in reality, this may not be available in every setting or geographic location,” Susan Kendig, JD, MSN, WHNP-BC, FAANP, policy director for the National Association of Nurse Practitioners in Women’s Health, and one of the authors of the document, said in an interview. “The purpose of the consensus bundle is to provide a framework for women’s health care providers to use in developing a system of care that includes standardized risk assessment for existing or emerging mental health issues, strategies for brief interventions, identification of community resources available to the woman, and/or resources to support the provider in addressing the woman’s needs and facilitating appropriate referrals, and addressing emergencies to prevent harm.”
The framework is grouped in four domains: readiness, recognition and prevention, response, and reporting and systems learning.
Readiness is focused largely on setting up clinical and administrative protocols, including mental health screening that is seamlessly integrated into the patient visit, established algorithms that are triggered according to screening results, and designated staff to both educate colleagues on the protocols and to drive their implementation.
The goal for physicians in all settings, according to the authors, is to balance cost, availability of tools, ease of use, and the validity of the tools against the need to capture often unrecognized signs and symptoms of mood and anxiety disorders, including changes in sleep patterns, appetite, or anxiety levels that often are attributed to the physiologic and neuroendocrinologic changes inherent in childbirth. More than 80% of women know something is “off” but do not bring up their symptoms to their clinician, according to the recommendation document.
“Coordination and team cohesiveness is not necessarily dependent on co-location,” Ms. Kendig said. “Virtual teams, where care is coordinated among providers at different locations, can also achieve positive outcomes.”
The follow-on to this – recognition and prevention – views every patient visit as an opportunity to draw a thorough picture of mental and physical health by taking a complete family and patient history, maintaining routine screening, and offering psychoeducation to patients and their families or others on whom they rely for emotional support.
When a woman does screen positive for perinatal mood or anxiety disorders, the next bundle offers a rough outline of a stage-based response for intervention and follow-up.
“Screening alone does not appear to improve pregnancy or maternal-child outcomes,” the authors wrote.
Several possible algorithms are included in the document, including for emergent mental health concerns such as suicidal or homicidal ideation.
The final domain relies on data capture, taking a systems approach to not only delivering care, but also improving it. This includes scheduling regular staff debriefings after severe maternal mental health crises, troubleshooting why some patients become lost to follow-up, and examining data to see patterns.
On Twitter @whitneymcknight
CORRECTION, 3/20/17: An earlier version of this article misstated the citation.
A new consensus bundle of recommendations calls on ob.gyns. to integrate mental health care into their care of pregnant and postpartum women.
The interdisciplinary Council on Patient Safety in Women’s Health Care issued a consensus document summarizing existing recommendations on maternal mental health and pairing them with appropriate screening and other resources. The bundle of recommendations was jointly issued by the American College of Obstetricians and Gynecologists, the National Association of Nurse Practitioners in Women’s Health, and other groups (Obstet Gynecol. 2017 Mar;129(3):422-430)*.
While no novel information is included in the bundle, the goal is to provide a streamlined document that pairs previous recommendations with resources and tools.
“Embedding a mental health professional with the women’s health care provider would seem to be the ideal, [but] in reality, this may not be available in every setting or geographic location,” Susan Kendig, JD, MSN, WHNP-BC, FAANP, policy director for the National Association of Nurse Practitioners in Women’s Health, and one of the authors of the document, said in an interview. “The purpose of the consensus bundle is to provide a framework for women’s health care providers to use in developing a system of care that includes standardized risk assessment for existing or emerging mental health issues, strategies for brief interventions, identification of community resources available to the woman, and/or resources to support the provider in addressing the woman’s needs and facilitating appropriate referrals, and addressing emergencies to prevent harm.”
The framework is grouped in four domains: readiness, recognition and prevention, response, and reporting and systems learning.
Readiness is focused largely on setting up clinical and administrative protocols, including mental health screening that is seamlessly integrated into the patient visit, established algorithms that are triggered according to screening results, and designated staff to both educate colleagues on the protocols and to drive their implementation.
The goal for physicians in all settings, according to the authors, is to balance cost, availability of tools, ease of use, and the validity of the tools against the need to capture often unrecognized signs and symptoms of mood and anxiety disorders, including changes in sleep patterns, appetite, or anxiety levels that often are attributed to the physiologic and neuroendocrinologic changes inherent in childbirth. More than 80% of women know something is “off” but do not bring up their symptoms to their clinician, according to the recommendation document.
“Coordination and team cohesiveness is not necessarily dependent on co-location,” Ms. Kendig said. “Virtual teams, where care is coordinated among providers at different locations, can also achieve positive outcomes.”
The follow-on to this – recognition and prevention – views every patient visit as an opportunity to draw a thorough picture of mental and physical health by taking a complete family and patient history, maintaining routine screening, and offering psychoeducation to patients and their families or others on whom they rely for emotional support.
When a woman does screen positive for perinatal mood or anxiety disorders, the next bundle offers a rough outline of a stage-based response for intervention and follow-up.
“Screening alone does not appear to improve pregnancy or maternal-child outcomes,” the authors wrote.
Several possible algorithms are included in the document, including for emergent mental health concerns such as suicidal or homicidal ideation.
The final domain relies on data capture, taking a systems approach to not only delivering care, but also improving it. This includes scheduling regular staff debriefings after severe maternal mental health crises, troubleshooting why some patients become lost to follow-up, and examining data to see patterns.
On Twitter @whitneymcknight
CORRECTION, 3/20/17: An earlier version of this article misstated the citation.
FROM OBSTETRICS & GYNECOLOGY
Guidelines needed for outpatient opioid use after vaginal delivery
A new study of pregnant Medicaid patients in Pennsylvania found that 12% filled prescriptions for opioids within 5 days of vaginal delivery, even though fewer than one-third of the women had pain-inducing conditions.
“Our study raises the question: Why is outpatient opioid use not rare after vaginal delivery?” lead author Marian Jarlenski, PhD, MPH, said in an interview. “Outpatient opioid prescriptions after a hospitalization may be one potential pathway to opioid use disorder. I hope the study will prompt some thought about why opioids are being prescribed for women after vaginal delivery and how to best manage postdelivery pain. This is especially important in areas of the country that have extraordinarily high rates of opioid use disorder.”
A total of 12% of the women (18,131) filled an outpatient prescription for an opioid with 5 days of giving birth. Of those, just 28.2% (5,110) had one or more conditions that cause an increased level of pain after delivery, such as bilateral tubal ligation, certain kinds of lacerations, and episiotomy.
During the first 5 days after birth, the most commonly prescribed opioid was oxycodone-acetaminophen (53.3%), followed by acetaminophen-codeine (20.5%), and hydrocodone-acetaminophen (19.6%).
Of the 18,131 women with an early postdelivery opioid prescription, 14% (2,592) filled at least one other opioid prescription within 6-60 days – that’s 1.6% of all the women in the study.
“On a positive note, we saw the supply of opioid prescriptions was generally short at 3-7 days,” Dr. Jarlenski said.
The researchers linked tobacco use and a mental health condition (both adjusted odds ratio 1.3; 95% confidence interval, 1.2-1.4) to a higher risk of filling a prescription without being diagnosed with a pain-causing disorder. They also found an association between substance use disorder (not related to opioids) and a higher risk of these types of prescriptions, but only for filling a second opioid prescription in the 6-60 day period (aOR 1.4; 95% CI, 1.2-1.6).
The researchers called for national guidelines regarding the use of opioids after birth.
“Several organizations have developed opioid prescribing guidelines for chronic and acute pain,” Dr. Jarlenski said. “These guidelines are necessary because the risk of opioid use disorder and subsequent overdose events is well established. Although delivery is the most common reason for hospitalization in the United States, there are no national guidelines for outpatient opioid use after vaginal delivery.”
The study was partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
A new study of pregnant Medicaid patients in Pennsylvania found that 12% filled prescriptions for opioids within 5 days of vaginal delivery, even though fewer than one-third of the women had pain-inducing conditions.
“Our study raises the question: Why is outpatient opioid use not rare after vaginal delivery?” lead author Marian Jarlenski, PhD, MPH, said in an interview. “Outpatient opioid prescriptions after a hospitalization may be one potential pathway to opioid use disorder. I hope the study will prompt some thought about why opioids are being prescribed for women after vaginal delivery and how to best manage postdelivery pain. This is especially important in areas of the country that have extraordinarily high rates of opioid use disorder.”
A total of 12% of the women (18,131) filled an outpatient prescription for an opioid with 5 days of giving birth. Of those, just 28.2% (5,110) had one or more conditions that cause an increased level of pain after delivery, such as bilateral tubal ligation, certain kinds of lacerations, and episiotomy.
During the first 5 days after birth, the most commonly prescribed opioid was oxycodone-acetaminophen (53.3%), followed by acetaminophen-codeine (20.5%), and hydrocodone-acetaminophen (19.6%).
Of the 18,131 women with an early postdelivery opioid prescription, 14% (2,592) filled at least one other opioid prescription within 6-60 days – that’s 1.6% of all the women in the study.
“On a positive note, we saw the supply of opioid prescriptions was generally short at 3-7 days,” Dr. Jarlenski said.
The researchers linked tobacco use and a mental health condition (both adjusted odds ratio 1.3; 95% confidence interval, 1.2-1.4) to a higher risk of filling a prescription without being diagnosed with a pain-causing disorder. They also found an association between substance use disorder (not related to opioids) and a higher risk of these types of prescriptions, but only for filling a second opioid prescription in the 6-60 day period (aOR 1.4; 95% CI, 1.2-1.6).
The researchers called for national guidelines regarding the use of opioids after birth.
“Several organizations have developed opioid prescribing guidelines for chronic and acute pain,” Dr. Jarlenski said. “These guidelines are necessary because the risk of opioid use disorder and subsequent overdose events is well established. Although delivery is the most common reason for hospitalization in the United States, there are no national guidelines for outpatient opioid use after vaginal delivery.”
The study was partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
A new study of pregnant Medicaid patients in Pennsylvania found that 12% filled prescriptions for opioids within 5 days of vaginal delivery, even though fewer than one-third of the women had pain-inducing conditions.
“Our study raises the question: Why is outpatient opioid use not rare after vaginal delivery?” lead author Marian Jarlenski, PhD, MPH, said in an interview. “Outpatient opioid prescriptions after a hospitalization may be one potential pathway to opioid use disorder. I hope the study will prompt some thought about why opioids are being prescribed for women after vaginal delivery and how to best manage postdelivery pain. This is especially important in areas of the country that have extraordinarily high rates of opioid use disorder.”
A total of 12% of the women (18,131) filled an outpatient prescription for an opioid with 5 days of giving birth. Of those, just 28.2% (5,110) had one or more conditions that cause an increased level of pain after delivery, such as bilateral tubal ligation, certain kinds of lacerations, and episiotomy.
During the first 5 days after birth, the most commonly prescribed opioid was oxycodone-acetaminophen (53.3%), followed by acetaminophen-codeine (20.5%), and hydrocodone-acetaminophen (19.6%).
Of the 18,131 women with an early postdelivery opioid prescription, 14% (2,592) filled at least one other opioid prescription within 6-60 days – that’s 1.6% of all the women in the study.
“On a positive note, we saw the supply of opioid prescriptions was generally short at 3-7 days,” Dr. Jarlenski said.
The researchers linked tobacco use and a mental health condition (both adjusted odds ratio 1.3; 95% confidence interval, 1.2-1.4) to a higher risk of filling a prescription without being diagnosed with a pain-causing disorder. They also found an association between substance use disorder (not related to opioids) and a higher risk of these types of prescriptions, but only for filling a second opioid prescription in the 6-60 day period (aOR 1.4; 95% CI, 1.2-1.6).
The researchers called for national guidelines regarding the use of opioids after birth.
“Several organizations have developed opioid prescribing guidelines for chronic and acute pain,” Dr. Jarlenski said. “These guidelines are necessary because the risk of opioid use disorder and subsequent overdose events is well established. Although delivery is the most common reason for hospitalization in the United States, there are no national guidelines for outpatient opioid use after vaginal delivery.”
The study was partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
FROM OBSTETRICS AND GYNECOLOGY
Key clinical point:
Major finding: A total of 12% of women on Medicaid filled opioid prescriptions within 5 days of delivery; just 28.2% of those patients had a pain-inducing condition.
Data source: A retrospective cohort study of 164,720 women enrolled in Medicaid in Pennsylvania who delivered live-born babies vaginally from 2008 to 2013.
Disclosures: The study is partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
Review offers reassurance on prenatal Tdap vaccination safety
Combined tetanus, diphtheria, and pertussis (Tdap) vaccination during the second or third trimester of pregnancy does not appear to be associated with clinically significant harm to the fetus or neonate, according to findings from a systematic review of the literature.
However, the findings are limited by a dearth of randomized, placebo-controlled trials.
Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60, Mark McMillan of the University of Adelaide, North Adelaide, Australia and his colleagues reported (Obstet Gynecol. 2017;129:560-73).
“Statistical imprecision for combined ‘all anomalies’ outcomes meant that upper 95% [confidence intervals] were 2.0 or above,” the researchers wrote. “Statistical imprecision was even greater in the individual congenital anomaly outcomes and little confidence can be placed in these estimates.”
Additionally, one of three studies assessing chorioamnionitis showed a small but significant increase in risk (relative risk, 1.19) after vaccination.
Among the studies examining medically attended adverse events, no association was seen between vaccination and such events or reactions, including neurologic events, gestational diabetes, preeclampsia or eclampsia, and cardiac events. Maternal effects included fever in 1%-3% of subjects, and headache, malaise, and myalgia, which were more common.
“Overall, despite the limitations described, the review offers reassurance for antenatal Tdap or Tdap-IPV [diphtheria, tetanus, pertussis, and polio] vaccination administered during the second or third trimester of pregnancy,” the researchers wrote. “These findings need to be interpreted in the context of the evidence of effectiveness of antenatal vaccination programs at preventing serious morbidity and mortality from pertussis in young infants.”
Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
Combined tetanus, diphtheria, and pertussis (Tdap) vaccination during the second or third trimester of pregnancy does not appear to be associated with clinically significant harm to the fetus or neonate, according to findings from a systematic review of the literature.
However, the findings are limited by a dearth of randomized, placebo-controlled trials.
Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60, Mark McMillan of the University of Adelaide, North Adelaide, Australia and his colleagues reported (Obstet Gynecol. 2017;129:560-73).
“Statistical imprecision for combined ‘all anomalies’ outcomes meant that upper 95% [confidence intervals] were 2.0 or above,” the researchers wrote. “Statistical imprecision was even greater in the individual congenital anomaly outcomes and little confidence can be placed in these estimates.”
Additionally, one of three studies assessing chorioamnionitis showed a small but significant increase in risk (relative risk, 1.19) after vaccination.
Among the studies examining medically attended adverse events, no association was seen between vaccination and such events or reactions, including neurologic events, gestational diabetes, preeclampsia or eclampsia, and cardiac events. Maternal effects included fever in 1%-3% of subjects, and headache, malaise, and myalgia, which were more common.
“Overall, despite the limitations described, the review offers reassurance for antenatal Tdap or Tdap-IPV [diphtheria, tetanus, pertussis, and polio] vaccination administered during the second or third trimester of pregnancy,” the researchers wrote. “These findings need to be interpreted in the context of the evidence of effectiveness of antenatal vaccination programs at preventing serious morbidity and mortality from pertussis in young infants.”
Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
Combined tetanus, diphtheria, and pertussis (Tdap) vaccination during the second or third trimester of pregnancy does not appear to be associated with clinically significant harm to the fetus or neonate, according to findings from a systematic review of the literature.
However, the findings are limited by a dearth of randomized, placebo-controlled trials.
Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60, Mark McMillan of the University of Adelaide, North Adelaide, Australia and his colleagues reported (Obstet Gynecol. 2017;129:560-73).
“Statistical imprecision for combined ‘all anomalies’ outcomes meant that upper 95% [confidence intervals] were 2.0 or above,” the researchers wrote. “Statistical imprecision was even greater in the individual congenital anomaly outcomes and little confidence can be placed in these estimates.”
Additionally, one of three studies assessing chorioamnionitis showed a small but significant increase in risk (relative risk, 1.19) after vaccination.
Among the studies examining medically attended adverse events, no association was seen between vaccination and such events or reactions, including neurologic events, gestational diabetes, preeclampsia or eclampsia, and cardiac events. Maternal effects included fever in 1%-3% of subjects, and headache, malaise, and myalgia, which were more common.
“Overall, despite the limitations described, the review offers reassurance for antenatal Tdap or Tdap-IPV [diphtheria, tetanus, pertussis, and polio] vaccination administered during the second or third trimester of pregnancy,” the researchers wrote. “These findings need to be interpreted in the context of the evidence of effectiveness of antenatal vaccination programs at preventing serious morbidity and mortality from pertussis in young infants.”
Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60.
Data source: A systematic review of 21 studies.
Disclosures: Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
Hypertensive disease of pregnancy linked to earlier mortality
LAS VEGAS – Women who develop any form of hypertensive disease during pregnancy have a significantly increased mortality rate until they reach age 50, compared with women without the condition.
The findings, presented at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, are based on a review of more than 2 million mothers who delivered babies in Utah during 1939-2012.
The relatively increased mortality rate linked with hypertensive disease of pregnancy (HDP) reached its peak during the first decade immediately following the index delivery and was dramatically higher in women for whom the index HDP was preceded by at least one earlier HDP. Increased mortality was especially elevated for certain types of deaths including stroke, diabetes, circulatory disease, and ischemic heart disease, said Lauren Theilen, MD, a maternal-fetal medicine researcher at the University of Utah in Salt Lake City.
She calculated that during the decade following an index case of HDP, life expectancy among mothers who had two or more HDP-affected pregnancies was about 49 years, life expectancy among women with a history of one HDP was 52 years, and postpartum women without HDP had a life expectancy of 55 years.
The data came from 2,083,331 singleton pregnancies delivered in Utah during 1939-2012 where the mother remained in Utah for at least 1 year following delivery. From this group, Dr. Theilen and her associates identified 67,384 women (3%) with HDP, including 49,598 women without a prior history of HDP and 7,786 with at least one prior HDP pregnancy. They included four different diagnoses as HDP: gestational hypertension, preeclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), or eclampsia.
The analysis excluded women with chronic hypertension, antiphospholipid syndrome, pregestational diabetes, or chronic kidney disease. It also excluded women who died within a year of the index delivery. For each of the included 67,384 cases with HDP, the researchers selected two controls with a delivery unaffected by HDP and matched them to a case by age, year of childbirth, and parity.
The women in the study were 26 years old on average. Gestational age at delivery among the HDP cases averaged 1 week less than among the controls, 37.8 weeks compared with 38.9 weeks, a statistically significant difference. Average birth weight also differed by a significant amount, 3,079 grams in the HDP neonates and 3,319 grams in the control newborns. During follow-up, 8% of the HDP women died, compared with 6% of the control women.
Analysis showed that relative mortality rates in HDP women were especially elevated for certain types of death: endocrine and metabolic, circulatory, genitourinary, infectious disease, and digestive. In most types of death, the increased risk linked with HDP was markedly higher in the women with recurrent HDP.
Dr. Theilen reported the relative risks of death for certain specific mortality causes (Am J Obstet Gynecol. 2017 Jan;216[1][suppl]:S32-3). In women with a single index case of HDP, the mortality rate compared to women with no HDP was threefold higher for diabetes, twofold higher for ischemic heart disease, and 85% higher for stroke. In women with recurrent HDP, the relative mortality risks were fourfold higher for diabetes, threefold higher for ischemic heart disease, and fivefold higher for stroke.
For all causes of death except stroke, the increased relative risk from HDP existed only for women younger than 51 years. Once HDP women passed the age of 50, their excess mortality risk was substantially muted, even in women with recurrent HDP. But for stroke mortality, the added risk persisted among older women with a history of at least two HDPs. In this subgroup, stroke deaths were nearly fourfold higher than in the matched controls.
Dr. Theilen reported having no financial disclosures.
[email protected]
On Twitter @mitchelzoler
The findings Dr. Theilen and her associates made in this study confirm results reported several decades ago that first established a link between hypertensive disease of pregnancy (HDP) and significantly reduced life expectancy. We have known for some time that HDP identifies women with a long-term mortality risk. The real question is: Can we ameliorate the risk linked with HDP?
We know that HDP requires acute management, but we are not sure how to best manage these women once they have delivered. To address that, we need prospective studies.
Not all women who experience HDP receive appropriate follow-up after delivery. We need to ensure a better handoff of women who developed HDP from the physicians who cared for these women during pregnancy to the physicians who care for these women postpartum and during the balance of their life. Ideally, a primary care physician should closely follow and manage blood pressure and other risk factors of HDP women once they are no longer pregnant.
Mary E. D’Alton, MD , is professor and chair of ob.gyn. at Columbia University Medical Center in New York City. She is on the advisory board of Merck for Mothers. She made these comments in an interview.
The findings Dr. Theilen and her associates made in this study confirm results reported several decades ago that first established a link between hypertensive disease of pregnancy (HDP) and significantly reduced life expectancy. We have known for some time that HDP identifies women with a long-term mortality risk. The real question is: Can we ameliorate the risk linked with HDP?
We know that HDP requires acute management, but we are not sure how to best manage these women once they have delivered. To address that, we need prospective studies.
Not all women who experience HDP receive appropriate follow-up after delivery. We need to ensure a better handoff of women who developed HDP from the physicians who cared for these women during pregnancy to the physicians who care for these women postpartum and during the balance of their life. Ideally, a primary care physician should closely follow and manage blood pressure and other risk factors of HDP women once they are no longer pregnant.
Mary E. D’Alton, MD , is professor and chair of ob.gyn. at Columbia University Medical Center in New York City. She is on the advisory board of Merck for Mothers. She made these comments in an interview.
The findings Dr. Theilen and her associates made in this study confirm results reported several decades ago that first established a link between hypertensive disease of pregnancy (HDP) and significantly reduced life expectancy. We have known for some time that HDP identifies women with a long-term mortality risk. The real question is: Can we ameliorate the risk linked with HDP?
We know that HDP requires acute management, but we are not sure how to best manage these women once they have delivered. To address that, we need prospective studies.
Not all women who experience HDP receive appropriate follow-up after delivery. We need to ensure a better handoff of women who developed HDP from the physicians who cared for these women during pregnancy to the physicians who care for these women postpartum and during the balance of their life. Ideally, a primary care physician should closely follow and manage blood pressure and other risk factors of HDP women once they are no longer pregnant.
Mary E. D’Alton, MD , is professor and chair of ob.gyn. at Columbia University Medical Center in New York City. She is on the advisory board of Merck for Mothers. She made these comments in an interview.
LAS VEGAS – Women who develop any form of hypertensive disease during pregnancy have a significantly increased mortality rate until they reach age 50, compared with women without the condition.
The findings, presented at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, are based on a review of more than 2 million mothers who delivered babies in Utah during 1939-2012.
The relatively increased mortality rate linked with hypertensive disease of pregnancy (HDP) reached its peak during the first decade immediately following the index delivery and was dramatically higher in women for whom the index HDP was preceded by at least one earlier HDP. Increased mortality was especially elevated for certain types of deaths including stroke, diabetes, circulatory disease, and ischemic heart disease, said Lauren Theilen, MD, a maternal-fetal medicine researcher at the University of Utah in Salt Lake City.
She calculated that during the decade following an index case of HDP, life expectancy among mothers who had two or more HDP-affected pregnancies was about 49 years, life expectancy among women with a history of one HDP was 52 years, and postpartum women without HDP had a life expectancy of 55 years.
The data came from 2,083,331 singleton pregnancies delivered in Utah during 1939-2012 where the mother remained in Utah for at least 1 year following delivery. From this group, Dr. Theilen and her associates identified 67,384 women (3%) with HDP, including 49,598 women without a prior history of HDP and 7,786 with at least one prior HDP pregnancy. They included four different diagnoses as HDP: gestational hypertension, preeclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), or eclampsia.
The analysis excluded women with chronic hypertension, antiphospholipid syndrome, pregestational diabetes, or chronic kidney disease. It also excluded women who died within a year of the index delivery. For each of the included 67,384 cases with HDP, the researchers selected two controls with a delivery unaffected by HDP and matched them to a case by age, year of childbirth, and parity.
The women in the study were 26 years old on average. Gestational age at delivery among the HDP cases averaged 1 week less than among the controls, 37.8 weeks compared with 38.9 weeks, a statistically significant difference. Average birth weight also differed by a significant amount, 3,079 grams in the HDP neonates and 3,319 grams in the control newborns. During follow-up, 8% of the HDP women died, compared with 6% of the control women.
Analysis showed that relative mortality rates in HDP women were especially elevated for certain types of death: endocrine and metabolic, circulatory, genitourinary, infectious disease, and digestive. In most types of death, the increased risk linked with HDP was markedly higher in the women with recurrent HDP.
Dr. Theilen reported the relative risks of death for certain specific mortality causes (Am J Obstet Gynecol. 2017 Jan;216[1][suppl]:S32-3). In women with a single index case of HDP, the mortality rate compared to women with no HDP was threefold higher for diabetes, twofold higher for ischemic heart disease, and 85% higher for stroke. In women with recurrent HDP, the relative mortality risks were fourfold higher for diabetes, threefold higher for ischemic heart disease, and fivefold higher for stroke.
For all causes of death except stroke, the increased relative risk from HDP existed only for women younger than 51 years. Once HDP women passed the age of 50, their excess mortality risk was substantially muted, even in women with recurrent HDP. But for stroke mortality, the added risk persisted among older women with a history of at least two HDPs. In this subgroup, stroke deaths were nearly fourfold higher than in the matched controls.
Dr. Theilen reported having no financial disclosures.
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Women who develop any form of hypertensive disease during pregnancy have a significantly increased mortality rate until they reach age 50, compared with women without the condition.
The findings, presented at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine, are based on a review of more than 2 million mothers who delivered babies in Utah during 1939-2012.
The relatively increased mortality rate linked with hypertensive disease of pregnancy (HDP) reached its peak during the first decade immediately following the index delivery and was dramatically higher in women for whom the index HDP was preceded by at least one earlier HDP. Increased mortality was especially elevated for certain types of deaths including stroke, diabetes, circulatory disease, and ischemic heart disease, said Lauren Theilen, MD, a maternal-fetal medicine researcher at the University of Utah in Salt Lake City.
She calculated that during the decade following an index case of HDP, life expectancy among mothers who had two or more HDP-affected pregnancies was about 49 years, life expectancy among women with a history of one HDP was 52 years, and postpartum women without HDP had a life expectancy of 55 years.
The data came from 2,083,331 singleton pregnancies delivered in Utah during 1939-2012 where the mother remained in Utah for at least 1 year following delivery. From this group, Dr. Theilen and her associates identified 67,384 women (3%) with HDP, including 49,598 women without a prior history of HDP and 7,786 with at least one prior HDP pregnancy. They included four different diagnoses as HDP: gestational hypertension, preeclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), or eclampsia.
The analysis excluded women with chronic hypertension, antiphospholipid syndrome, pregestational diabetes, or chronic kidney disease. It also excluded women who died within a year of the index delivery. For each of the included 67,384 cases with HDP, the researchers selected two controls with a delivery unaffected by HDP and matched them to a case by age, year of childbirth, and parity.
The women in the study were 26 years old on average. Gestational age at delivery among the HDP cases averaged 1 week less than among the controls, 37.8 weeks compared with 38.9 weeks, a statistically significant difference. Average birth weight also differed by a significant amount, 3,079 grams in the HDP neonates and 3,319 grams in the control newborns. During follow-up, 8% of the HDP women died, compared with 6% of the control women.
Analysis showed that relative mortality rates in HDP women were especially elevated for certain types of death: endocrine and metabolic, circulatory, genitourinary, infectious disease, and digestive. In most types of death, the increased risk linked with HDP was markedly higher in the women with recurrent HDP.
Dr. Theilen reported the relative risks of death for certain specific mortality causes (Am J Obstet Gynecol. 2017 Jan;216[1][suppl]:S32-3). In women with a single index case of HDP, the mortality rate compared to women with no HDP was threefold higher for diabetes, twofold higher for ischemic heart disease, and 85% higher for stroke. In women with recurrent HDP, the relative mortality risks were fourfold higher for diabetes, threefold higher for ischemic heart disease, and fivefold higher for stroke.
For all causes of death except stroke, the increased relative risk from HDP existed only for women younger than 51 years. Once HDP women passed the age of 50, their excess mortality risk was substantially muted, even in women with recurrent HDP. But for stroke mortality, the added risk persisted among older women with a history of at least two HDPs. In this subgroup, stroke deaths were nearly fourfold higher than in the matched controls.
Dr. Theilen reported having no financial disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: Postpartum life expectancy was 49 years in women with two or more hypertensive pregnancies and 55 years in women without hypertension.
Data source: Retrospective, case-control study of 2,083,331 singleton pregnancies delivered in Utah during 1939-2012.
Disclosures: Dr. Theilen reported having no financial disclosures.
Aspirin reduces recurrent preeclampsia in real-world study
LAS VEGAS – Using low-dose aspirin during pregnancy significantly reduced the risk of recurrent preeclampsia, according to results of a new study.
“The net benefit of aspirin is substantial,” Mary Catherine Tolcher, MD, the study’s lead author said. “The number needed to treat to prevent one case of recurrent preeclampsia is six... The cost of daily low-dose aspirin for the duration of one pregnancy is about $4.00. Comparatively, the cost to prevent one case of eclampsia is approximately $21,000.”
Dr. Tolcher, a postdoctorate fellow in ob.gyn. at Baylor College of Medicine, Houston, and her colleagues found a total of 417 at-risk women in the institution’s labor and delivery database during the August 2011–June 2016 study period; 284 were identified before the guidelines were implemented in 2014, while 133 women were identified as high-risk after guideline implementation.
While nearly one-third (32.4%) of women with a history of preeclampsia had a recurrence in the before group, the recurrence rate fell to 16.5% in the after group, who had been instructed to take low-dose aspirin in accordance with the guidelines. When the investigators calculated the fully adjusted odds ratio for recurrent preeclampsia, they found a reduction of about 30% in recurrent preeclampsia [aOR, 0.71; 95% confidence interval, 0.52-0.95].
“This decrease is greater than the approximately 10 to 15 percent reduction that has been previously reported in clinical trials, and different from the meta-analysis that prompted the national recommendations,” Dr. Tolcher said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
She and her colleagues hypothesize that the greater effect size may be attributable to limiting the study population to the higher-risk group of women with a history of preeclampsia. Alternatively, she said, aspirin’s pharmacodynamics can differ by race, so racial differences between study populations may also be at play.
One of the causative mechanisms for preeclampsia is thought to be impaired trophoblastic remodeling that impedes development of the low-resistance vascular system of the maternal-fetal unit. “The resulting pathophysiology is multisystemic and includes vascular and endothelial dysfunction, placental ischemia, and an inflammatory and stress response,” Dr. Tolcher said. Overproduction of thromboxanes, she said, plays a role in this process. Aspirin’s inhibition of cyclooxygenase-2 (COX-2) enzymes and thromboxanes is thought to mitigate the vasoconstriction and endothelial dysfunction seen in preeclampsia, she said.
A secondary outcome measure in the study was use of magnesium sulfate, and after guideline implementation “there was a trend toward reduced use of magnesium sulfate, which we reserved for preeclampsia with severe features,” Dr. Tolcher said.
There was no difference in the incidence of preterm deliveries, another secondary outcome measure, after the aspirin guidelines were implemented.
There were some differences in characteristics between the before and after groups: the ratio of Hispanic women with preeclampsia was significantly lower in the after group (P less than .0001). The distribution of method of payment shifted, with more private pay patients, fewer Children’s Health Insurance Program (CHIP) patients, and fewer “other” payment method patients in the after group. Though Dr. Tolcher reported that type 1 diabetes was seen more often in the after group, the rates of any kind of pre-pregnancy diabetes were similar between the groups (6.33% before; 4.26% after).
Potentially confounding variables were controlled by means of logistic regression analysis. Women with multiple gestations were excluded, and only the first pregnancy after a previous episode of preeclampsia was studied.
Otherwise, demographics and other patient characteristics – including rates of chronic hypertension, were similar between the before and after groups. About a quarter of the patients in each group had a history of preterm delivery, and the median age at delivery for both was 38 years.
Within the total group that had recurrent preeclampsia, “maternal age greater than 35, type 2 diabetes, chronic hypertension, and a history of preterm preeclampsia were significantly associated with recurrent preeclampsia,” Dr. Tolcher said.
Study limitations included the retrospective nature, the inclusion of only women who had a prior history of preeclampsia, and the investigators’ inability to determine whether patients were adherent to recommendations for aspirin use. However, the study represents actual clinical use, Dr. Tolcher said, and addresses a real need. “Preeclampsia is responsible for 75,000 maternal deaths annually, and accounts for 15% of the preterm births in the U.S.,” she said.
Dr. Tolcher reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
LAS VEGAS – Using low-dose aspirin during pregnancy significantly reduced the risk of recurrent preeclampsia, according to results of a new study.
“The net benefit of aspirin is substantial,” Mary Catherine Tolcher, MD, the study’s lead author said. “The number needed to treat to prevent one case of recurrent preeclampsia is six... The cost of daily low-dose aspirin for the duration of one pregnancy is about $4.00. Comparatively, the cost to prevent one case of eclampsia is approximately $21,000.”
Dr. Tolcher, a postdoctorate fellow in ob.gyn. at Baylor College of Medicine, Houston, and her colleagues found a total of 417 at-risk women in the institution’s labor and delivery database during the August 2011–June 2016 study period; 284 were identified before the guidelines were implemented in 2014, while 133 women were identified as high-risk after guideline implementation.
While nearly one-third (32.4%) of women with a history of preeclampsia had a recurrence in the before group, the recurrence rate fell to 16.5% in the after group, who had been instructed to take low-dose aspirin in accordance with the guidelines. When the investigators calculated the fully adjusted odds ratio for recurrent preeclampsia, they found a reduction of about 30% in recurrent preeclampsia [aOR, 0.71; 95% confidence interval, 0.52-0.95].
“This decrease is greater than the approximately 10 to 15 percent reduction that has been previously reported in clinical trials, and different from the meta-analysis that prompted the national recommendations,” Dr. Tolcher said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
She and her colleagues hypothesize that the greater effect size may be attributable to limiting the study population to the higher-risk group of women with a history of preeclampsia. Alternatively, she said, aspirin’s pharmacodynamics can differ by race, so racial differences between study populations may also be at play.
One of the causative mechanisms for preeclampsia is thought to be impaired trophoblastic remodeling that impedes development of the low-resistance vascular system of the maternal-fetal unit. “The resulting pathophysiology is multisystemic and includes vascular and endothelial dysfunction, placental ischemia, and an inflammatory and stress response,” Dr. Tolcher said. Overproduction of thromboxanes, she said, plays a role in this process. Aspirin’s inhibition of cyclooxygenase-2 (COX-2) enzymes and thromboxanes is thought to mitigate the vasoconstriction and endothelial dysfunction seen in preeclampsia, she said.
A secondary outcome measure in the study was use of magnesium sulfate, and after guideline implementation “there was a trend toward reduced use of magnesium sulfate, which we reserved for preeclampsia with severe features,” Dr. Tolcher said.
There was no difference in the incidence of preterm deliveries, another secondary outcome measure, after the aspirin guidelines were implemented.
There were some differences in characteristics between the before and after groups: the ratio of Hispanic women with preeclampsia was significantly lower in the after group (P less than .0001). The distribution of method of payment shifted, with more private pay patients, fewer Children’s Health Insurance Program (CHIP) patients, and fewer “other” payment method patients in the after group. Though Dr. Tolcher reported that type 1 diabetes was seen more often in the after group, the rates of any kind of pre-pregnancy diabetes were similar between the groups (6.33% before; 4.26% after).
Potentially confounding variables were controlled by means of logistic regression analysis. Women with multiple gestations were excluded, and only the first pregnancy after a previous episode of preeclampsia was studied.
Otherwise, demographics and other patient characteristics – including rates of chronic hypertension, were similar between the before and after groups. About a quarter of the patients in each group had a history of preterm delivery, and the median age at delivery for both was 38 years.
Within the total group that had recurrent preeclampsia, “maternal age greater than 35, type 2 diabetes, chronic hypertension, and a history of preterm preeclampsia were significantly associated with recurrent preeclampsia,” Dr. Tolcher said.
Study limitations included the retrospective nature, the inclusion of only women who had a prior history of preeclampsia, and the investigators’ inability to determine whether patients were adherent to recommendations for aspirin use. However, the study represents actual clinical use, Dr. Tolcher said, and addresses a real need. “Preeclampsia is responsible for 75,000 maternal deaths annually, and accounts for 15% of the preterm births in the U.S.,” she said.
Dr. Tolcher reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
LAS VEGAS – Using low-dose aspirin during pregnancy significantly reduced the risk of recurrent preeclampsia, according to results of a new study.
“The net benefit of aspirin is substantial,” Mary Catherine Tolcher, MD, the study’s lead author said. “The number needed to treat to prevent one case of recurrent preeclampsia is six... The cost of daily low-dose aspirin for the duration of one pregnancy is about $4.00. Comparatively, the cost to prevent one case of eclampsia is approximately $21,000.”
Dr. Tolcher, a postdoctorate fellow in ob.gyn. at Baylor College of Medicine, Houston, and her colleagues found a total of 417 at-risk women in the institution’s labor and delivery database during the August 2011–June 2016 study period; 284 were identified before the guidelines were implemented in 2014, while 133 women were identified as high-risk after guideline implementation.
While nearly one-third (32.4%) of women with a history of preeclampsia had a recurrence in the before group, the recurrence rate fell to 16.5% in the after group, who had been instructed to take low-dose aspirin in accordance with the guidelines. When the investigators calculated the fully adjusted odds ratio for recurrent preeclampsia, they found a reduction of about 30% in recurrent preeclampsia [aOR, 0.71; 95% confidence interval, 0.52-0.95].
“This decrease is greater than the approximately 10 to 15 percent reduction that has been previously reported in clinical trials, and different from the meta-analysis that prompted the national recommendations,” Dr. Tolcher said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
She and her colleagues hypothesize that the greater effect size may be attributable to limiting the study population to the higher-risk group of women with a history of preeclampsia. Alternatively, she said, aspirin’s pharmacodynamics can differ by race, so racial differences between study populations may also be at play.
One of the causative mechanisms for preeclampsia is thought to be impaired trophoblastic remodeling that impedes development of the low-resistance vascular system of the maternal-fetal unit. “The resulting pathophysiology is multisystemic and includes vascular and endothelial dysfunction, placental ischemia, and an inflammatory and stress response,” Dr. Tolcher said. Overproduction of thromboxanes, she said, plays a role in this process. Aspirin’s inhibition of cyclooxygenase-2 (COX-2) enzymes and thromboxanes is thought to mitigate the vasoconstriction and endothelial dysfunction seen in preeclampsia, she said.
A secondary outcome measure in the study was use of magnesium sulfate, and after guideline implementation “there was a trend toward reduced use of magnesium sulfate, which we reserved for preeclampsia with severe features,” Dr. Tolcher said.
There was no difference in the incidence of preterm deliveries, another secondary outcome measure, after the aspirin guidelines were implemented.
There were some differences in characteristics between the before and after groups: the ratio of Hispanic women with preeclampsia was significantly lower in the after group (P less than .0001). The distribution of method of payment shifted, with more private pay patients, fewer Children’s Health Insurance Program (CHIP) patients, and fewer “other” payment method patients in the after group. Though Dr. Tolcher reported that type 1 diabetes was seen more often in the after group, the rates of any kind of pre-pregnancy diabetes were similar between the groups (6.33% before; 4.26% after).
Potentially confounding variables were controlled by means of logistic regression analysis. Women with multiple gestations were excluded, and only the first pregnancy after a previous episode of preeclampsia was studied.
Otherwise, demographics and other patient characteristics – including rates of chronic hypertension, were similar between the before and after groups. About a quarter of the patients in each group had a history of preterm delivery, and the median age at delivery for both was 38 years.
Within the total group that had recurrent preeclampsia, “maternal age greater than 35, type 2 diabetes, chronic hypertension, and a history of preterm preeclampsia were significantly associated with recurrent preeclampsia,” Dr. Tolcher said.
Study limitations included the retrospective nature, the inclusion of only women who had a prior history of preeclampsia, and the investigators’ inability to determine whether patients were adherent to recommendations for aspirin use. However, the study represents actual clinical use, Dr. Tolcher said, and addresses a real need. “Preeclampsia is responsible for 75,000 maternal deaths annually, and accounts for 15% of the preterm births in the U.S.,” she said.
Dr. Tolcher reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: The adjusted odds ratio for recurrent preeclampsia was 0.71 after implementing U.S. Preventive Services Task Force (USPSTF) guidelines for aspirin administration.
Data source: Retrospective cohort study of 17,256 deliveries at a single academic medical center before and after implementation of USPSTF aspirin guidelines, with 417 cases of recurrent preeclampsia identified.
Disclosures: Dr. Tolcher reported having no relevant financial disclosures.
Toddlers’ neurodevelopmental deficits linked with maternal diabetes
LAS VEGAS – Children born to obese women with insulin resistance during pregnancy showed significantly impaired neurodevelopment at 2 years of age, compared with children born to obese mothers without insulin resistance in a prospective observational study with 75 pregnant women.
The neurodevelopmental deficits were specific for the domains of motor function and attention, and the deficits correlated with several markers of abnormal glucose and fat metabolism in the insulin-resistant women, Alison G. Cahill, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“The differences in neurodevelopment appear to not be global but instead specifically affect domains of motor development and attention,” said Dr. Cahill, chief of maternal fetal medicine at Washington University in St. Louis. “These findings are consistent with results from animal studies that suggest certain brain regions are more sensitive than others to metabolic abnormalities” while in utero.
“These are among the first data in humans to characterize the impact of metabolic abnormalities on brain development,” she added.
Dr. Cahill said that results from the lean mothers uniformly matched those from the obese mothers without insulin resistance, and so for brevity she only reported results from the obese control group.
Average gestational age at birth was 37 weeks in the insulin-resistant mothers and 38.7 weeks among the obese mothers without insulin resistance, a significant difference. Birth weight averaged 3,617 g in the mothers with insulin resistance and 3,373 g in the mothers without insulin resistance, a difference that was not statistically significant.
Dr. Cahill and her associates assessed the 2-year-olds with a battery of behavioral and functional assessments. They measured motor function, cognition, and language with the Bayley Scales of Infant and Toddler Development, prespecified as the study’s primary endpoint. They also applied the Modified Checklist for Autism in Toddlers (M-CHAT), as well as the Infant-Toddler Social and Emotional Assessment (ITSEA) to assess competence, externalizing, internalizing, and dysregulation.
The results of these analyses showed statistically significant deficits for the motor composite score on the Bayley assessment and for the competence component of the ITSEA assessment, Dr. Cahill reported. The average composite Bayley motor score was 88 in children from mothers with insulin resistance and 98 in the control children, a statistically significant difference.
Further analyses showed that the motor deficit was primarily in fine motor function, and that motor scores were depressed throughout the entire cohort of children born to mothers with insulin resistance.
Depressed competence scores on the ITSEA assessment reflect attention abnormalities, she explained.
A final analysis examined the correlation between the motor deficits identified and various metabolic tests of fat, glucose, and protein metabolism run on the enrolled mothers during the last weeks of gestation. This showed significant links between depressed motor development and maternal lipolytic rate, plasma free fatty acids, and hepatic glucose output.
This finding “suggests an association between abnormal lipid and glucose metabolism in mothers and aspects of neurodevelopment” in their children, Dr. Cahill said.
Dr. Cahill had no disclosures.
[email protected] On Twitter @mitchelzoler
LAS VEGAS – Children born to obese women with insulin resistance during pregnancy showed significantly impaired neurodevelopment at 2 years of age, compared with children born to obese mothers without insulin resistance in a prospective observational study with 75 pregnant women.
The neurodevelopmental deficits were specific for the domains of motor function and attention, and the deficits correlated with several markers of abnormal glucose and fat metabolism in the insulin-resistant women, Alison G. Cahill, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“The differences in neurodevelopment appear to not be global but instead specifically affect domains of motor development and attention,” said Dr. Cahill, chief of maternal fetal medicine at Washington University in St. Louis. “These findings are consistent with results from animal studies that suggest certain brain regions are more sensitive than others to metabolic abnormalities” while in utero.
“These are among the first data in humans to characterize the impact of metabolic abnormalities on brain development,” she added.
Dr. Cahill said that results from the lean mothers uniformly matched those from the obese mothers without insulin resistance, and so for brevity she only reported results from the obese control group.
Average gestational age at birth was 37 weeks in the insulin-resistant mothers and 38.7 weeks among the obese mothers without insulin resistance, a significant difference. Birth weight averaged 3,617 g in the mothers with insulin resistance and 3,373 g in the mothers without insulin resistance, a difference that was not statistically significant.
Dr. Cahill and her associates assessed the 2-year-olds with a battery of behavioral and functional assessments. They measured motor function, cognition, and language with the Bayley Scales of Infant and Toddler Development, prespecified as the study’s primary endpoint. They also applied the Modified Checklist for Autism in Toddlers (M-CHAT), as well as the Infant-Toddler Social and Emotional Assessment (ITSEA) to assess competence, externalizing, internalizing, and dysregulation.
The results of these analyses showed statistically significant deficits for the motor composite score on the Bayley assessment and for the competence component of the ITSEA assessment, Dr. Cahill reported. The average composite Bayley motor score was 88 in children from mothers with insulin resistance and 98 in the control children, a statistically significant difference.
Further analyses showed that the motor deficit was primarily in fine motor function, and that motor scores were depressed throughout the entire cohort of children born to mothers with insulin resistance.
Depressed competence scores on the ITSEA assessment reflect attention abnormalities, she explained.
A final analysis examined the correlation between the motor deficits identified and various metabolic tests of fat, glucose, and protein metabolism run on the enrolled mothers during the last weeks of gestation. This showed significant links between depressed motor development and maternal lipolytic rate, plasma free fatty acids, and hepatic glucose output.
This finding “suggests an association between abnormal lipid and glucose metabolism in mothers and aspects of neurodevelopment” in their children, Dr. Cahill said.
Dr. Cahill had no disclosures.
[email protected] On Twitter @mitchelzoler
LAS VEGAS – Children born to obese women with insulin resistance during pregnancy showed significantly impaired neurodevelopment at 2 years of age, compared with children born to obese mothers without insulin resistance in a prospective observational study with 75 pregnant women.
The neurodevelopmental deficits were specific for the domains of motor function and attention, and the deficits correlated with several markers of abnormal glucose and fat metabolism in the insulin-resistant women, Alison G. Cahill, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“The differences in neurodevelopment appear to not be global but instead specifically affect domains of motor development and attention,” said Dr. Cahill, chief of maternal fetal medicine at Washington University in St. Louis. “These findings are consistent with results from animal studies that suggest certain brain regions are more sensitive than others to metabolic abnormalities” while in utero.
“These are among the first data in humans to characterize the impact of metabolic abnormalities on brain development,” she added.
Dr. Cahill said that results from the lean mothers uniformly matched those from the obese mothers without insulin resistance, and so for brevity she only reported results from the obese control group.
Average gestational age at birth was 37 weeks in the insulin-resistant mothers and 38.7 weeks among the obese mothers without insulin resistance, a significant difference. Birth weight averaged 3,617 g in the mothers with insulin resistance and 3,373 g in the mothers without insulin resistance, a difference that was not statistically significant.
Dr. Cahill and her associates assessed the 2-year-olds with a battery of behavioral and functional assessments. They measured motor function, cognition, and language with the Bayley Scales of Infant and Toddler Development, prespecified as the study’s primary endpoint. They also applied the Modified Checklist for Autism in Toddlers (M-CHAT), as well as the Infant-Toddler Social and Emotional Assessment (ITSEA) to assess competence, externalizing, internalizing, and dysregulation.
The results of these analyses showed statistically significant deficits for the motor composite score on the Bayley assessment and for the competence component of the ITSEA assessment, Dr. Cahill reported. The average composite Bayley motor score was 88 in children from mothers with insulin resistance and 98 in the control children, a statistically significant difference.
Further analyses showed that the motor deficit was primarily in fine motor function, and that motor scores were depressed throughout the entire cohort of children born to mothers with insulin resistance.
Depressed competence scores on the ITSEA assessment reflect attention abnormalities, she explained.
A final analysis examined the correlation between the motor deficits identified and various metabolic tests of fat, glucose, and protein metabolism run on the enrolled mothers during the last weeks of gestation. This showed significant links between depressed motor development and maternal lipolytic rate, plasma free fatty acids, and hepatic glucose output.
This finding “suggests an association between abnormal lipid and glucose metabolism in mothers and aspects of neurodevelopment” in their children, Dr. Cahill said.
Dr. Cahill had no disclosures.
[email protected] On Twitter @mitchelzoler
Key clinical point:
Major finding: The Bayley motor scale score averaged 88 in children from insulin-resistant mothers and 98 when no insulin resistance existed.
Data source: Prospective, single-center observational study with 75 pregnant women.
Disclosures: Dr. Cahill had no disclosures.
Capping gestational weight gain didn’t deliver better pregnancy outcomes
LAS VEGAS – Two similar behavioral interventions during pregnancy both succeeded in capping gestational weight gain in two independent randomized trials, but neither intervention produced improvements in obstetrical outcomes.
Results from several prior studies linked excess gestational weight gain (GWG) with adverse outcomes, including gestational diabetes, hypertension, macrosomia, and cesarean delivery. But none of the rates of these complications fell among women in the study groups that received intervention and had reduced GWG, compared with controls.
“The clinical significance of the difference in GWG we saw is not known,” said Alison G. Cahill, MD, who presented one of the two reports at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. In the study she led, women who received a behavioral intervention averaged about 3.5 pounds less GWG through 36 weeks of pregnancy.
“Our findings call into question the association between GWG and adverse pregnancy outcomes,” said Alan M. Peaceman, MD, who presented the second study, in which women receiving the behavioral intervention averaged 4 pounds less in GWG, compared with control women.
Dr. Peaceman reported results from the Maternal Offspring Metabolics: Family Intervention Trial (MOMFIT), a trial run at Northwestern University in Chicago that randomized 263 pregnant women. The women had to be at less than 16 weeks singleton gestation with a body mass index of 25-40 kg/m2, no pregestational diabetes, and a first trimester weight gain of no more than 15 pounds.
The researchers randomized participants to receive either an intervention that included an individualized diet, Internet-based self monitoring of diet adherence, recommendations on physical activity, and weekly coaching calls and opportunities for group meetings, webinars and podcasts; or a control regimen of electronic newsletters and website access that dispensed pregnancy information without mentioning diet. The participants averaged 33 years old, their average body mass index was 31 kg/m2, and about 55% were obese, with a body mass index of 30 kg/m2 or greater.
The study’s primary outcome was weight gain from enrollment through 36 weeks of gestation, which averaged 19.1 pounds among women who received the intervention and 23.7 pounds among controls, an average 4.6 pounds difference that was statistically significant, Dr. Peaceman reported.
The percentage of patients exceeding the GWG recommendations made in 2009 by the Institute of Medicine (IOM) was 68% in the intervention group and 86% among the controls, an 18 percentage-point difference that was statistically significant.
Despite these differences, the two groups showed very similar rates for the incidence of gestational diabetes, preeclampsia or hypertension, birth weight above 4,000 g, and gestational age at delivery (39 weeks on average for both subgroups).
The rate of cesarean delivery (40%) was higher in the women who received the intervention and had less GWG, compared with 27% among the control women. Despite meeting the statistical test for significance, it is most likely a chance result, said Dr. Peaceman, chief of maternal fetal medicine at Northwestern.
He stressed that while no benefit from reduced GWG has yet been found in the MOMFIT results, additional endpoints are under study, such as neonatal metabolism, infant metabolism at 1 year, and maternal weight retention.
Dr. Cahill reported very similar findings from her study, run as part of the Weight Management in Obese Pregnant Underserved African American Women (LIFE-Moms) trial. She enrolled 267 socioeconomically disadvantaged African American women with singleton, normal-anatomy pregnancies who presented for prenatal care at her clinic at less than 16 weeks gestation and were overweight or obese.
The study randomized these women to receive either an exercise and lifestyle intervention along with home visits from the Parents as Teachers program, or just home visits without the exercise and lifestyle component. The enrolled women averaged about 25 years old, and their average body mass index was about 32 kg/m2, with two-thirds of patients being obese.
The study’s primary endpoint, the percentage of women who exceeded the IOM’s 2009 recommendations on GWG, was 37% among women who received the exercise and lifestyle intervention and 46% among those who did not, a difference that was not statistically significant in the full intention-to-treat analysis, Dr. Cahill reported.
A subgroup analysis showed that most of the benefit focused in obese participants, where 34% of women who received the extra intervention had a GWG greater than the IOM recommendation, compared with a 49% rate among controls, a 15 percentage-point difference that fell just short of statistical significance.
For the secondary endpoint of average amount of GWG, women in the intervention arm had a 8.05 kg average, compared with 9.64 kg among the controls, an average GWG reduction of 1.59 kg (3.5 pounds) in the intervention arm. This difference was statistically significant, said Dr. Cahill, chief of maternal fetal medicine at Washington University in St. Louis.
Dr. Cahill also ran a modified intention-to-treat analysis that excluded women with missing GWG data at term, those with fetal death or miscarriage, and one women mistakenly enrolled who was of normal weight. Among the remaining 240 women, the impact of the exercise and lifestyle intervention was even more pronounced, resulting in an average reduction in GWG of 4 pounds and a 12 percentage-point reduction in women exceeding the IOM’s GWG recommendations.
Despite these favorable effects on GWG, the two study arms showed no significant differences in the incidence of gestational diabetes, gestational hypertension, preterm births, or cesarean delivery.
Dr. Cahill said that she too planned to look at additional outcomes that might be affected by controlling GWG, including maternal weight retention and neurodevelopment in the children.
[email protected] On Twitter @mitchelzoler
LAS VEGAS – Two similar behavioral interventions during pregnancy both succeeded in capping gestational weight gain in two independent randomized trials, but neither intervention produced improvements in obstetrical outcomes.
Results from several prior studies linked excess gestational weight gain (GWG) with adverse outcomes, including gestational diabetes, hypertension, macrosomia, and cesarean delivery. But none of the rates of these complications fell among women in the study groups that received intervention and had reduced GWG, compared with controls.
“The clinical significance of the difference in GWG we saw is not known,” said Alison G. Cahill, MD, who presented one of the two reports at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. In the study she led, women who received a behavioral intervention averaged about 3.5 pounds less GWG through 36 weeks of pregnancy.
“Our findings call into question the association between GWG and adverse pregnancy outcomes,” said Alan M. Peaceman, MD, who presented the second study, in which women receiving the behavioral intervention averaged 4 pounds less in GWG, compared with control women.
Dr. Peaceman reported results from the Maternal Offspring Metabolics: Family Intervention Trial (MOMFIT), a trial run at Northwestern University in Chicago that randomized 263 pregnant women. The women had to be at less than 16 weeks singleton gestation with a body mass index of 25-40 kg/m2, no pregestational diabetes, and a first trimester weight gain of no more than 15 pounds.
The researchers randomized participants to receive either an intervention that included an individualized diet, Internet-based self monitoring of diet adherence, recommendations on physical activity, and weekly coaching calls and opportunities for group meetings, webinars and podcasts; or a control regimen of electronic newsletters and website access that dispensed pregnancy information without mentioning diet. The participants averaged 33 years old, their average body mass index was 31 kg/m2, and about 55% were obese, with a body mass index of 30 kg/m2 or greater.
The study’s primary outcome was weight gain from enrollment through 36 weeks of gestation, which averaged 19.1 pounds among women who received the intervention and 23.7 pounds among controls, an average 4.6 pounds difference that was statistically significant, Dr. Peaceman reported.
The percentage of patients exceeding the GWG recommendations made in 2009 by the Institute of Medicine (IOM) was 68% in the intervention group and 86% among the controls, an 18 percentage-point difference that was statistically significant.
Despite these differences, the two groups showed very similar rates for the incidence of gestational diabetes, preeclampsia or hypertension, birth weight above 4,000 g, and gestational age at delivery (39 weeks on average for both subgroups).
The rate of cesarean delivery (40%) was higher in the women who received the intervention and had less GWG, compared with 27% among the control women. Despite meeting the statistical test for significance, it is most likely a chance result, said Dr. Peaceman, chief of maternal fetal medicine at Northwestern.
He stressed that while no benefit from reduced GWG has yet been found in the MOMFIT results, additional endpoints are under study, such as neonatal metabolism, infant metabolism at 1 year, and maternal weight retention.
Dr. Cahill reported very similar findings from her study, run as part of the Weight Management in Obese Pregnant Underserved African American Women (LIFE-Moms) trial. She enrolled 267 socioeconomically disadvantaged African American women with singleton, normal-anatomy pregnancies who presented for prenatal care at her clinic at less than 16 weeks gestation and were overweight or obese.
The study randomized these women to receive either an exercise and lifestyle intervention along with home visits from the Parents as Teachers program, or just home visits without the exercise and lifestyle component. The enrolled women averaged about 25 years old, and their average body mass index was about 32 kg/m2, with two-thirds of patients being obese.
The study’s primary endpoint, the percentage of women who exceeded the IOM’s 2009 recommendations on GWG, was 37% among women who received the exercise and lifestyle intervention and 46% among those who did not, a difference that was not statistically significant in the full intention-to-treat analysis, Dr. Cahill reported.
A subgroup analysis showed that most of the benefit focused in obese participants, where 34% of women who received the extra intervention had a GWG greater than the IOM recommendation, compared with a 49% rate among controls, a 15 percentage-point difference that fell just short of statistical significance.
For the secondary endpoint of average amount of GWG, women in the intervention arm had a 8.05 kg average, compared with 9.64 kg among the controls, an average GWG reduction of 1.59 kg (3.5 pounds) in the intervention arm. This difference was statistically significant, said Dr. Cahill, chief of maternal fetal medicine at Washington University in St. Louis.
Dr. Cahill also ran a modified intention-to-treat analysis that excluded women with missing GWG data at term, those with fetal death or miscarriage, and one women mistakenly enrolled who was of normal weight. Among the remaining 240 women, the impact of the exercise and lifestyle intervention was even more pronounced, resulting in an average reduction in GWG of 4 pounds and a 12 percentage-point reduction in women exceeding the IOM’s GWG recommendations.
Despite these favorable effects on GWG, the two study arms showed no significant differences in the incidence of gestational diabetes, gestational hypertension, preterm births, or cesarean delivery.
Dr. Cahill said that she too planned to look at additional outcomes that might be affected by controlling GWG, including maternal weight retention and neurodevelopment in the children.
[email protected] On Twitter @mitchelzoler
LAS VEGAS – Two similar behavioral interventions during pregnancy both succeeded in capping gestational weight gain in two independent randomized trials, but neither intervention produced improvements in obstetrical outcomes.
Results from several prior studies linked excess gestational weight gain (GWG) with adverse outcomes, including gestational diabetes, hypertension, macrosomia, and cesarean delivery. But none of the rates of these complications fell among women in the study groups that received intervention and had reduced GWG, compared with controls.
“The clinical significance of the difference in GWG we saw is not known,” said Alison G. Cahill, MD, who presented one of the two reports at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. In the study she led, women who received a behavioral intervention averaged about 3.5 pounds less GWG through 36 weeks of pregnancy.
“Our findings call into question the association between GWG and adverse pregnancy outcomes,” said Alan M. Peaceman, MD, who presented the second study, in which women receiving the behavioral intervention averaged 4 pounds less in GWG, compared with control women.
Dr. Peaceman reported results from the Maternal Offspring Metabolics: Family Intervention Trial (MOMFIT), a trial run at Northwestern University in Chicago that randomized 263 pregnant women. The women had to be at less than 16 weeks singleton gestation with a body mass index of 25-40 kg/m2, no pregestational diabetes, and a first trimester weight gain of no more than 15 pounds.
The researchers randomized participants to receive either an intervention that included an individualized diet, Internet-based self monitoring of diet adherence, recommendations on physical activity, and weekly coaching calls and opportunities for group meetings, webinars and podcasts; or a control regimen of electronic newsletters and website access that dispensed pregnancy information without mentioning diet. The participants averaged 33 years old, their average body mass index was 31 kg/m2, and about 55% were obese, with a body mass index of 30 kg/m2 or greater.
The study’s primary outcome was weight gain from enrollment through 36 weeks of gestation, which averaged 19.1 pounds among women who received the intervention and 23.7 pounds among controls, an average 4.6 pounds difference that was statistically significant, Dr. Peaceman reported.
The percentage of patients exceeding the GWG recommendations made in 2009 by the Institute of Medicine (IOM) was 68% in the intervention group and 86% among the controls, an 18 percentage-point difference that was statistically significant.
Despite these differences, the two groups showed very similar rates for the incidence of gestational diabetes, preeclampsia or hypertension, birth weight above 4,000 g, and gestational age at delivery (39 weeks on average for both subgroups).
The rate of cesarean delivery (40%) was higher in the women who received the intervention and had less GWG, compared with 27% among the control women. Despite meeting the statistical test for significance, it is most likely a chance result, said Dr. Peaceman, chief of maternal fetal medicine at Northwestern.
He stressed that while no benefit from reduced GWG has yet been found in the MOMFIT results, additional endpoints are under study, such as neonatal metabolism, infant metabolism at 1 year, and maternal weight retention.
Dr. Cahill reported very similar findings from her study, run as part of the Weight Management in Obese Pregnant Underserved African American Women (LIFE-Moms) trial. She enrolled 267 socioeconomically disadvantaged African American women with singleton, normal-anatomy pregnancies who presented for prenatal care at her clinic at less than 16 weeks gestation and were overweight or obese.
The study randomized these women to receive either an exercise and lifestyle intervention along with home visits from the Parents as Teachers program, or just home visits without the exercise and lifestyle component. The enrolled women averaged about 25 years old, and their average body mass index was about 32 kg/m2, with two-thirds of patients being obese.
The study’s primary endpoint, the percentage of women who exceeded the IOM’s 2009 recommendations on GWG, was 37% among women who received the exercise and lifestyle intervention and 46% among those who did not, a difference that was not statistically significant in the full intention-to-treat analysis, Dr. Cahill reported.
A subgroup analysis showed that most of the benefit focused in obese participants, where 34% of women who received the extra intervention had a GWG greater than the IOM recommendation, compared with a 49% rate among controls, a 15 percentage-point difference that fell just short of statistical significance.
For the secondary endpoint of average amount of GWG, women in the intervention arm had a 8.05 kg average, compared with 9.64 kg among the controls, an average GWG reduction of 1.59 kg (3.5 pounds) in the intervention arm. This difference was statistically significant, said Dr. Cahill, chief of maternal fetal medicine at Washington University in St. Louis.
Dr. Cahill also ran a modified intention-to-treat analysis that excluded women with missing GWG data at term, those with fetal death or miscarriage, and one women mistakenly enrolled who was of normal weight. Among the remaining 240 women, the impact of the exercise and lifestyle intervention was even more pronounced, resulting in an average reduction in GWG of 4 pounds and a 12 percentage-point reduction in women exceeding the IOM’s GWG recommendations.
Despite these favorable effects on GWG, the two study arms showed no significant differences in the incidence of gestational diabetes, gestational hypertension, preterm births, or cesarean delivery.
Dr. Cahill said that she too planned to look at additional outcomes that might be affected by controlling GWG, including maternal weight retention and neurodevelopment in the children.
[email protected] On Twitter @mitchelzoler
Key clinical point:
Major finding: Behavioral interventions linked with average reductions in gestational weight gain of 4.6 pounds in MOMFIT and 3.5 pounds in LIFE-Moms.
Data source: MOMFIT and LIFE-Moms, two single-center randomized trials with 263 and 267 mothers, respectively.
Disclosures: Neither trial had commercial support. Dr. Peaceman and Dr. Cahill had no relevant disclosures.