User login
Disrupted placenta: Infant anemia
Disrupted placenta: Infant anemia
An Obgyn recommended an elective transverse low incision cesarean delivery at a prenatal visit. Due to severe weather, the ObGyn was unable to come to the hospital; an on-call ObGyn consulted with the ObGyn by phone. Cesarean delivery resulted in disruption of the placenta. When the infant’s blood gasses test results were abnormal, he was transferred to the neonatal intensive care unit, where anemia was diagnosed. The infant was hospitalized for 31 days.
PARENTS’ CLAIM:
The on-call ObGyn caused the child’s injury by performing a transverse low incision. A testifying radiology expert said that ultrasonography (US) taken 5 weeks before delivery showed an anterior low-lying placenta but a clear field existed that would have allowed a vertical incision without placental disruption.
PHYSICIAN’S DEFENSE:
The delivery was within the standard of care. The ObGyn did not have access to the US cited by the testifying radiologist; standard of care did not require that she have access to them. A transverse incision minimizes blood loss; a vertical incision would have disrupted a larger area of placenta. The infant had normal blood gasses at delivery; any injury was not related to placental disruption.
VERDICT:
A Virginia defense verdict was returned.
Child has spastic CP after long labor
A 17-year-old woman's baby was delivered using vacuum extraction after a prolonged labor. Two days after birth, US results revealed diffuse brain edema in the baby. Magnetic resonance imaging demonstrated an absence of brain parenchyma in the left and right hemispheres. The baby received a diagnosis of spastic cerebral palsy (CP). She has little voluntary movement and requires a feeding tube, a portable aspiration device, and in-home attendant care.
PARENT’S CLAIM:
The baby underwent a hypoxic ischemic event during labor. Four hospital physicians
DEFENDANTS’ DEFENSE:
The fetus did not have a fetal heart rate pattern that would have required an earlier delivery. The injury sustained by the baby was not compatible with a prolonged hypoxic event and was more likely caused by a genetic defect. The infant suffered a subacute brain injury at least 1 week before delivery.
VERDICT:
The hospital settled for $1.25 million. A California defense verdict was returned for the physicians.
Misdiagnosed ectopic pregnancy
After a home pregnancy test was positive, a 27-year-old woman reported vaginal spotting and cramping to her ObGyn. When no uterine contents showed on US, the ObGyn suspected an ectopic pregnancy and recommended termination of pregnancy. The woman requested another US; an appointment was scheduled for the next day. Instead of waiting, the woman went to an emergency department (ED) that night. Bloodwork confirmed the pregnancy but US results showed no evidence of an intrauterine pregnancy. The ED physician diagnosed an ectopic pregnancy. The on-call ObGyn concurred and recommended termination of pregnancy by surgical intervention or methotrexate. The patient chose methotrexate, which was administered, and she was discharged.
In the on-call ObGyn’s office a week later, the patient’s beta-hGC levels had not decreased. US revealed 2 intrauterine pregnancies, one with a heartbeat. The on-call ObGyn immediately referred the patient to a maternal-fetal medicine specialist. New US results showed evidence of an abnormal intrauterine pregnancy and a second gestational sac with no embryo. Two days later US showed a twin pregnancy: a 6-week fetal pole with no heartbeat and the other with no fetal pole or yolk sac. A dilation and curettage was performed.
PARENTS’ CLAIM:
The on-call ObGyn misdiagnosed an ectopic pregnancy, failed to order additional testing, and failed to observe the patient for 48 to 72 hours before administering methotrexate. This led to the loss of twins.
DEFENDANTS’ DEFENSE:
An ectopic pregnancy is an emergency that requires prompt diagnosis and treatment. There were sufficient signs for the on-call ObGyn to diagnose an ectopic pregnancy. She would have violated the standard of care if she had not administered treatment.
VERDICT:
The hospital settled for $127,000 before trial. An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Disrupted placenta: Infant anemia
An Obgyn recommended an elective transverse low incision cesarean delivery at a prenatal visit. Due to severe weather, the ObGyn was unable to come to the hospital; an on-call ObGyn consulted with the ObGyn by phone. Cesarean delivery resulted in disruption of the placenta. When the infant’s blood gasses test results were abnormal, he was transferred to the neonatal intensive care unit, where anemia was diagnosed. The infant was hospitalized for 31 days.
PARENTS’ CLAIM:
The on-call ObGyn caused the child’s injury by performing a transverse low incision. A testifying radiology expert said that ultrasonography (US) taken 5 weeks before delivery showed an anterior low-lying placenta but a clear field existed that would have allowed a vertical incision without placental disruption.
PHYSICIAN’S DEFENSE:
The delivery was within the standard of care. The ObGyn did not have access to the US cited by the testifying radiologist; standard of care did not require that she have access to them. A transverse incision minimizes blood loss; a vertical incision would have disrupted a larger area of placenta. The infant had normal blood gasses at delivery; any injury was not related to placental disruption.
VERDICT:
A Virginia defense verdict was returned.
Child has spastic CP after long labor
A 17-year-old woman's baby was delivered using vacuum extraction after a prolonged labor. Two days after birth, US results revealed diffuse brain edema in the baby. Magnetic resonance imaging demonstrated an absence of brain parenchyma in the left and right hemispheres. The baby received a diagnosis of spastic cerebral palsy (CP). She has little voluntary movement and requires a feeding tube, a portable aspiration device, and in-home attendant care.
PARENT’S CLAIM:
The baby underwent a hypoxic ischemic event during labor. Four hospital physicians
DEFENDANTS’ DEFENSE:
The fetus did not have a fetal heart rate pattern that would have required an earlier delivery. The injury sustained by the baby was not compatible with a prolonged hypoxic event and was more likely caused by a genetic defect. The infant suffered a subacute brain injury at least 1 week before delivery.
VERDICT:
The hospital settled for $1.25 million. A California defense verdict was returned for the physicians.
Misdiagnosed ectopic pregnancy
After a home pregnancy test was positive, a 27-year-old woman reported vaginal spotting and cramping to her ObGyn. When no uterine contents showed on US, the ObGyn suspected an ectopic pregnancy and recommended termination of pregnancy. The woman requested another US; an appointment was scheduled for the next day. Instead of waiting, the woman went to an emergency department (ED) that night. Bloodwork confirmed the pregnancy but US results showed no evidence of an intrauterine pregnancy. The ED physician diagnosed an ectopic pregnancy. The on-call ObGyn concurred and recommended termination of pregnancy by surgical intervention or methotrexate. The patient chose methotrexate, which was administered, and she was discharged.
In the on-call ObGyn’s office a week later, the patient’s beta-hGC levels had not decreased. US revealed 2 intrauterine pregnancies, one with a heartbeat. The on-call ObGyn immediately referred the patient to a maternal-fetal medicine specialist. New US results showed evidence of an abnormal intrauterine pregnancy and a second gestational sac with no embryo. Two days later US showed a twin pregnancy: a 6-week fetal pole with no heartbeat and the other with no fetal pole or yolk sac. A dilation and curettage was performed.
PARENTS’ CLAIM:
The on-call ObGyn misdiagnosed an ectopic pregnancy, failed to order additional testing, and failed to observe the patient for 48 to 72 hours before administering methotrexate. This led to the loss of twins.
DEFENDANTS’ DEFENSE:
An ectopic pregnancy is an emergency that requires prompt diagnosis and treatment. There were sufficient signs for the on-call ObGyn to diagnose an ectopic pregnancy. She would have violated the standard of care if she had not administered treatment.
VERDICT:
The hospital settled for $127,000 before trial. An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Disrupted placenta: Infant anemia
An Obgyn recommended an elective transverse low incision cesarean delivery at a prenatal visit. Due to severe weather, the ObGyn was unable to come to the hospital; an on-call ObGyn consulted with the ObGyn by phone. Cesarean delivery resulted in disruption of the placenta. When the infant’s blood gasses test results were abnormal, he was transferred to the neonatal intensive care unit, where anemia was diagnosed. The infant was hospitalized for 31 days.
PARENTS’ CLAIM:
The on-call ObGyn caused the child’s injury by performing a transverse low incision. A testifying radiology expert said that ultrasonography (US) taken 5 weeks before delivery showed an anterior low-lying placenta but a clear field existed that would have allowed a vertical incision without placental disruption.
PHYSICIAN’S DEFENSE:
The delivery was within the standard of care. The ObGyn did not have access to the US cited by the testifying radiologist; standard of care did not require that she have access to them. A transverse incision minimizes blood loss; a vertical incision would have disrupted a larger area of placenta. The infant had normal blood gasses at delivery; any injury was not related to placental disruption.
VERDICT:
A Virginia defense verdict was returned.
Child has spastic CP after long labor
A 17-year-old woman's baby was delivered using vacuum extraction after a prolonged labor. Two days after birth, US results revealed diffuse brain edema in the baby. Magnetic resonance imaging demonstrated an absence of brain parenchyma in the left and right hemispheres. The baby received a diagnosis of spastic cerebral palsy (CP). She has little voluntary movement and requires a feeding tube, a portable aspiration device, and in-home attendant care.
PARENT’S CLAIM:
The baby underwent a hypoxic ischemic event during labor. Four hospital physicians
DEFENDANTS’ DEFENSE:
The fetus did not have a fetal heart rate pattern that would have required an earlier delivery. The injury sustained by the baby was not compatible with a prolonged hypoxic event and was more likely caused by a genetic defect. The infant suffered a subacute brain injury at least 1 week before delivery.
VERDICT:
The hospital settled for $1.25 million. A California defense verdict was returned for the physicians.
Misdiagnosed ectopic pregnancy
After a home pregnancy test was positive, a 27-year-old woman reported vaginal spotting and cramping to her ObGyn. When no uterine contents showed on US, the ObGyn suspected an ectopic pregnancy and recommended termination of pregnancy. The woman requested another US; an appointment was scheduled for the next day. Instead of waiting, the woman went to an emergency department (ED) that night. Bloodwork confirmed the pregnancy but US results showed no evidence of an intrauterine pregnancy. The ED physician diagnosed an ectopic pregnancy. The on-call ObGyn concurred and recommended termination of pregnancy by surgical intervention or methotrexate. The patient chose methotrexate, which was administered, and she was discharged.
In the on-call ObGyn’s office a week later, the patient’s beta-hGC levels had not decreased. US revealed 2 intrauterine pregnancies, one with a heartbeat. The on-call ObGyn immediately referred the patient to a maternal-fetal medicine specialist. New US results showed evidence of an abnormal intrauterine pregnancy and a second gestational sac with no embryo. Two days later US showed a twin pregnancy: a 6-week fetal pole with no heartbeat and the other with no fetal pole or yolk sac. A dilation and curettage was performed.
PARENTS’ CLAIM:
The on-call ObGyn misdiagnosed an ectopic pregnancy, failed to order additional testing, and failed to observe the patient for 48 to 72 hours before administering methotrexate. This led to the loss of twins.
DEFENDANTS’ DEFENSE:
An ectopic pregnancy is an emergency that requires prompt diagnosis and treatment. There were sufficient signs for the on-call ObGyn to diagnose an ectopic pregnancy. She would have violated the standard of care if she had not administered treatment.
VERDICT:
The hospital settled for $127,000 before trial. An Illinois defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Puerperal NSAIDs show no hypertension risk
LAS VEGAS – Puerperal NSAID treatment appeared safe for women with severe preeclampsia and hypertension postpartum in a single-center, retrospective analysis with 324 women.
Given that an opioid is generally the alternative to analgesia with a nonsteroidal anti-inflammatory drug, these new data help refute a recent call to limit puerperal NSAID use, Oscar A. Viteri, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Given the apparent safety of NSAIDs in this new analysis, their safety for nursing women, and concerns about opiates, it makes sense to defer any recommendations about avoiding NSAIDs in women with hypertension postpartum until their harm is proven in a adequately powered randomized trial, said Dr. Viteri, a maternal fetal medicine specialist at the University of Texas, Houston. “Opiates are a public health problem,” he stressed.
His analysis used data collected from all women who delivered at Children’s Memorial Hermann Hospital in Houston during 2013-2015. In that group he identified 399 mothers with preeclampsia with severe features that had been diagnosed prior to delivery, and among them 324 mothers had hypertension (a systolic blood pressure of at least 140 mm Hg, a diastolic pressure of at least 90 mm Hg, or both) at or after 24 hours following delivery. Within this subgroup of 324 mothers, 243 (75%) received puerperal NSAID treatment and 81 women (25%) did not. Dr. Viteri highlighted that three-quarters of the women in the study subgroup had received NSAIDs “despite” the 2013 Task Force recommendation.
“Many units” continue to use puerperal NSAIDs in women with hypertension postpartum, commented Mary E. D’Alton, MD, professor and chair of ob.gyn. at Columbia University, New York.
Dr. Viteri defined persistent hypertension in these women as a systolic blood pressure of at least 150 mm Hg, a diastolic pressure of at least 100 mm Hg, or both measured after delivery at least twice at an interval of at least 4 hours. This primary endpoint occurred in 70% of the women treated with an NSAID and in 73% of those who received no NSAID, a difference that was not statistically significant after adjustment for laboratory abnormalities, gestational age, and mode of delivery, Dr. Viteri reported. The women who received NSAIDs also showed a numerically lower rate of receiving new or additional antihypertensive drugs of 20%, compared with 31% among those not on NSAIDs, a nonsignificant difference.
The analysis also showed no differences between the women on NSAIDs and those who did not take them for all the other parameters examined, including highest, average, and discharge systolic and diastolic blood pressures. In addition, among the women who received NSAIDs the results showed no differences in blood pressures regardless of whether the women also were receiving antihypertensive treatment with labetalol or nifedipine. This is the largest study yet reported to examine the effect of puerperal NSAID treatment on women with hypertension, and also the first data on the impact of NSAID treatment on blood pressure in women taking various types of antihypertensive drugs, Dr. Viteri noted.
Despite this reassuring data “it is important to be cautious” when using NSAIDs to treat the type of women enrolled in this study, Dr. D’Alton said in an interview. One concern to keep in mind is the risk for renal injury from NSAID use in women with a history of severe hypertension. Although Dr. D’Alton believed that it is not necessary to monitor renal function routinely in hypertensive women receiving puerperal NSAID treatment, the impact of this practice on the kidneys was worth further investigation, she said.
Dr. Viteri and Dr. D’Alton had no disclosures.
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Puerperal NSAID treatment appeared safe for women with severe preeclampsia and hypertension postpartum in a single-center, retrospective analysis with 324 women.
Given that an opioid is generally the alternative to analgesia with a nonsteroidal anti-inflammatory drug, these new data help refute a recent call to limit puerperal NSAID use, Oscar A. Viteri, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Given the apparent safety of NSAIDs in this new analysis, their safety for nursing women, and concerns about opiates, it makes sense to defer any recommendations about avoiding NSAIDs in women with hypertension postpartum until their harm is proven in a adequately powered randomized trial, said Dr. Viteri, a maternal fetal medicine specialist at the University of Texas, Houston. “Opiates are a public health problem,” he stressed.
His analysis used data collected from all women who delivered at Children’s Memorial Hermann Hospital in Houston during 2013-2015. In that group he identified 399 mothers with preeclampsia with severe features that had been diagnosed prior to delivery, and among them 324 mothers had hypertension (a systolic blood pressure of at least 140 mm Hg, a diastolic pressure of at least 90 mm Hg, or both) at or after 24 hours following delivery. Within this subgroup of 324 mothers, 243 (75%) received puerperal NSAID treatment and 81 women (25%) did not. Dr. Viteri highlighted that three-quarters of the women in the study subgroup had received NSAIDs “despite” the 2013 Task Force recommendation.
“Many units” continue to use puerperal NSAIDs in women with hypertension postpartum, commented Mary E. D’Alton, MD, professor and chair of ob.gyn. at Columbia University, New York.
Dr. Viteri defined persistent hypertension in these women as a systolic blood pressure of at least 150 mm Hg, a diastolic pressure of at least 100 mm Hg, or both measured after delivery at least twice at an interval of at least 4 hours. This primary endpoint occurred in 70% of the women treated with an NSAID and in 73% of those who received no NSAID, a difference that was not statistically significant after adjustment for laboratory abnormalities, gestational age, and mode of delivery, Dr. Viteri reported. The women who received NSAIDs also showed a numerically lower rate of receiving new or additional antihypertensive drugs of 20%, compared with 31% among those not on NSAIDs, a nonsignificant difference.
The analysis also showed no differences between the women on NSAIDs and those who did not take them for all the other parameters examined, including highest, average, and discharge systolic and diastolic blood pressures. In addition, among the women who received NSAIDs the results showed no differences in blood pressures regardless of whether the women also were receiving antihypertensive treatment with labetalol or nifedipine. This is the largest study yet reported to examine the effect of puerperal NSAID treatment on women with hypertension, and also the first data on the impact of NSAID treatment on blood pressure in women taking various types of antihypertensive drugs, Dr. Viteri noted.
Despite this reassuring data “it is important to be cautious” when using NSAIDs to treat the type of women enrolled in this study, Dr. D’Alton said in an interview. One concern to keep in mind is the risk for renal injury from NSAID use in women with a history of severe hypertension. Although Dr. D’Alton believed that it is not necessary to monitor renal function routinely in hypertensive women receiving puerperal NSAID treatment, the impact of this practice on the kidneys was worth further investigation, she said.
Dr. Viteri and Dr. D’Alton had no disclosures.
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Puerperal NSAID treatment appeared safe for women with severe preeclampsia and hypertension postpartum in a single-center, retrospective analysis with 324 women.
Given that an opioid is generally the alternative to analgesia with a nonsteroidal anti-inflammatory drug, these new data help refute a recent call to limit puerperal NSAID use, Oscar A. Viteri, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Given the apparent safety of NSAIDs in this new analysis, their safety for nursing women, and concerns about opiates, it makes sense to defer any recommendations about avoiding NSAIDs in women with hypertension postpartum until their harm is proven in a adequately powered randomized trial, said Dr. Viteri, a maternal fetal medicine specialist at the University of Texas, Houston. “Opiates are a public health problem,” he stressed.
His analysis used data collected from all women who delivered at Children’s Memorial Hermann Hospital in Houston during 2013-2015. In that group he identified 399 mothers with preeclampsia with severe features that had been diagnosed prior to delivery, and among them 324 mothers had hypertension (a systolic blood pressure of at least 140 mm Hg, a diastolic pressure of at least 90 mm Hg, or both) at or after 24 hours following delivery. Within this subgroup of 324 mothers, 243 (75%) received puerperal NSAID treatment and 81 women (25%) did not. Dr. Viteri highlighted that three-quarters of the women in the study subgroup had received NSAIDs “despite” the 2013 Task Force recommendation.
“Many units” continue to use puerperal NSAIDs in women with hypertension postpartum, commented Mary E. D’Alton, MD, professor and chair of ob.gyn. at Columbia University, New York.
Dr. Viteri defined persistent hypertension in these women as a systolic blood pressure of at least 150 mm Hg, a diastolic pressure of at least 100 mm Hg, or both measured after delivery at least twice at an interval of at least 4 hours. This primary endpoint occurred in 70% of the women treated with an NSAID and in 73% of those who received no NSAID, a difference that was not statistically significant after adjustment for laboratory abnormalities, gestational age, and mode of delivery, Dr. Viteri reported. The women who received NSAIDs also showed a numerically lower rate of receiving new or additional antihypertensive drugs of 20%, compared with 31% among those not on NSAIDs, a nonsignificant difference.
The analysis also showed no differences between the women on NSAIDs and those who did not take them for all the other parameters examined, including highest, average, and discharge systolic and diastolic blood pressures. In addition, among the women who received NSAIDs the results showed no differences in blood pressures regardless of whether the women also were receiving antihypertensive treatment with labetalol or nifedipine. This is the largest study yet reported to examine the effect of puerperal NSAID treatment on women with hypertension, and also the first data on the impact of NSAID treatment on blood pressure in women taking various types of antihypertensive drugs, Dr. Viteri noted.
Despite this reassuring data “it is important to be cautious” when using NSAIDs to treat the type of women enrolled in this study, Dr. D’Alton said in an interview. One concern to keep in mind is the risk for renal injury from NSAID use in women with a history of severe hypertension. Although Dr. D’Alton believed that it is not necessary to monitor renal function routinely in hypertensive women receiving puerperal NSAID treatment, the impact of this practice on the kidneys was worth further investigation, she said.
Dr. Viteri and Dr. D’Alton had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: The incidence of persistent hypertension was 70% in women who received NSAIDs and 73% in women not on NSAISDs.
Data source: Retrospective analysis of data from 324 women at a single U.S. center.
Disclosures: Dr. Viteri and Dr. D’Alton had no disclosures.
Postpartum depression risk 20 times greater among women with depression history
Women with a history of depression have a risk of postpartum depression that is more than 20 times greater than women without such a history, according to Michael E. Silverman, PhD, and his associates. In addition, pre- and perinatal risk factors also raise the postpartum depression risk, they reported.
In a nationwide prospective cohort study, Dr. Silverman and his associates identified 707,701 women with live singleton births in Sweden from 1997-2008. Results showed that, compared with women without a history of depression, there was a statistically increased risk for postpartum depression in women with a history of depression (relative risk, 21.03; 95% confidence interval, 19.72-22.42).
Pregnancy length and depression history also proved significant in the mothers’ development of postpartum depression. The risk of postpartum depression, for example, was higher among women with a history of depression who gave birth before week 32 (RR, 1.12; 95% CI, 0.73-1.74), compared with women who gave birth before the 32nd week without a depression history (RR, 1.53; 95% CI, 1.12-2.10).
The existence of diabetic disease was another significant factor. Among women with gestational diabetes with a history of depression, the risk of postpartum depression was slightly higher (RR, 1.69; 95% CI, 1.18-2.43) than it was for women in that group without a depression history (RR, 1.67; 95% CI, 1.25-2.23). The differences were more dramatic among women with pregestational diabetes. Those with pregestational diabetes with a history of depression had a far greater risk of developing postpartum depression (RR, 1.49; 95% CI, 1.01-2.21) than did women with pregestational diabetes without a history of depression (RR, 1.16; 95% CI, 0.73-1.83), reported Dr. Silverman, of the department of psychiatry at the Icahn Medicine at Mount Sinai, New York, and his associates.
“For the first time, we show how maternal and obstetric risk factors for [postpartum depression] may differ between new mothers with and without a history of depression,” the investigators wrote. “Never shown before, some of the risks associated with obstetric and perinatal factors are modified by a history of depression, suggesting differences in the etiology of [postpartum depression] between women with and without a personal history of depression.”
Read the full study in Depression and Anxiety (doi: 10.1002/da.22597).
Women with a history of depression have a risk of postpartum depression that is more than 20 times greater than women without such a history, according to Michael E. Silverman, PhD, and his associates. In addition, pre- and perinatal risk factors also raise the postpartum depression risk, they reported.
In a nationwide prospective cohort study, Dr. Silverman and his associates identified 707,701 women with live singleton births in Sweden from 1997-2008. Results showed that, compared with women without a history of depression, there was a statistically increased risk for postpartum depression in women with a history of depression (relative risk, 21.03; 95% confidence interval, 19.72-22.42).
Pregnancy length and depression history also proved significant in the mothers’ development of postpartum depression. The risk of postpartum depression, for example, was higher among women with a history of depression who gave birth before week 32 (RR, 1.12; 95% CI, 0.73-1.74), compared with women who gave birth before the 32nd week without a depression history (RR, 1.53; 95% CI, 1.12-2.10).
The existence of diabetic disease was another significant factor. Among women with gestational diabetes with a history of depression, the risk of postpartum depression was slightly higher (RR, 1.69; 95% CI, 1.18-2.43) than it was for women in that group without a depression history (RR, 1.67; 95% CI, 1.25-2.23). The differences were more dramatic among women with pregestational diabetes. Those with pregestational diabetes with a history of depression had a far greater risk of developing postpartum depression (RR, 1.49; 95% CI, 1.01-2.21) than did women with pregestational diabetes without a history of depression (RR, 1.16; 95% CI, 0.73-1.83), reported Dr. Silverman, of the department of psychiatry at the Icahn Medicine at Mount Sinai, New York, and his associates.
“For the first time, we show how maternal and obstetric risk factors for [postpartum depression] may differ between new mothers with and without a history of depression,” the investigators wrote. “Never shown before, some of the risks associated with obstetric and perinatal factors are modified by a history of depression, suggesting differences in the etiology of [postpartum depression] between women with and without a personal history of depression.”
Read the full study in Depression and Anxiety (doi: 10.1002/da.22597).
Women with a history of depression have a risk of postpartum depression that is more than 20 times greater than women without such a history, according to Michael E. Silverman, PhD, and his associates. In addition, pre- and perinatal risk factors also raise the postpartum depression risk, they reported.
In a nationwide prospective cohort study, Dr. Silverman and his associates identified 707,701 women with live singleton births in Sweden from 1997-2008. Results showed that, compared with women without a history of depression, there was a statistically increased risk for postpartum depression in women with a history of depression (relative risk, 21.03; 95% confidence interval, 19.72-22.42).
Pregnancy length and depression history also proved significant in the mothers’ development of postpartum depression. The risk of postpartum depression, for example, was higher among women with a history of depression who gave birth before week 32 (RR, 1.12; 95% CI, 0.73-1.74), compared with women who gave birth before the 32nd week without a depression history (RR, 1.53; 95% CI, 1.12-2.10).
The existence of diabetic disease was another significant factor. Among women with gestational diabetes with a history of depression, the risk of postpartum depression was slightly higher (RR, 1.69; 95% CI, 1.18-2.43) than it was for women in that group without a depression history (RR, 1.67; 95% CI, 1.25-2.23). The differences were more dramatic among women with pregestational diabetes. Those with pregestational diabetes with a history of depression had a far greater risk of developing postpartum depression (RR, 1.49; 95% CI, 1.01-2.21) than did women with pregestational diabetes without a history of depression (RR, 1.16; 95% CI, 0.73-1.83), reported Dr. Silverman, of the department of psychiatry at the Icahn Medicine at Mount Sinai, New York, and his associates.
“For the first time, we show how maternal and obstetric risk factors for [postpartum depression] may differ between new mothers with and without a history of depression,” the investigators wrote. “Never shown before, some of the risks associated with obstetric and perinatal factors are modified by a history of depression, suggesting differences in the etiology of [postpartum depression] between women with and without a personal history of depression.”
Read the full study in Depression and Anxiety (doi: 10.1002/da.22597).
FROM DEPRESSION AND ANXIETY
5% dextrose speeds induced-labor delivery
LAS VEGAS – Adding 5% dextrose to the hydrating solution given to women undergoing induced labor safely led to a median 76-minute decrease in labor duration in a single-center randomized study.
Normal saline with 5% dextrose “should be considered the default solute during labor induction in nulliparous women,” Josianne Paré, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. “The uterus is a muscle, and glucose is its main energy substrate.”
During January 2013 to January 2015, women who met these criteria and required induction received either normal saline or normal saline plus 5% dextrose when they began their oxytocin drip, at a rate of 250 mL/hour.
Treatment with the assigned hydrating solutions continued until delivery or C-section. Participants averaged 28 years old, their average body mass index was 26 kg/m2 and average birth weight was about 3,450 g.
The study’s primary outcome was total duration of labor. This was a median of 423 minutes in 96 women who received dextrose and were available for analysis, and a median of 499 minutes in 97 evaluable women who received the saline control, a median difference of 76 minutes that was statistically significant, Dr. Paré reported. Most of the difference in labor duration happened during the first stage, which showed a median 70-minute reduction between the control group and the women receiving dextrose.
“These results support findings from prior studies. Women need glucose during labor,” Elliott Main, MD, commented in an interview. “There is no evidence for a need to exclude glucose from intravenous fluids. Adding some form of glucose is not standard practice today, but the time has come to do it, either by adding glucose to hydrating fluid or have women in labor eat and drink more,” said Dr. Main, medical director of the California Maternal Quality Care Collaborative in Stanford.
Dr. Paré reported having no financial disclosures.
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Adding 5% dextrose to the hydrating solution given to women undergoing induced labor safely led to a median 76-minute decrease in labor duration in a single-center randomized study.
Normal saline with 5% dextrose “should be considered the default solute during labor induction in nulliparous women,” Josianne Paré, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. “The uterus is a muscle, and glucose is its main energy substrate.”
During January 2013 to January 2015, women who met these criteria and required induction received either normal saline or normal saline plus 5% dextrose when they began their oxytocin drip, at a rate of 250 mL/hour.
Treatment with the assigned hydrating solutions continued until delivery or C-section. Participants averaged 28 years old, their average body mass index was 26 kg/m2 and average birth weight was about 3,450 g.
The study’s primary outcome was total duration of labor. This was a median of 423 minutes in 96 women who received dextrose and were available for analysis, and a median of 499 minutes in 97 evaluable women who received the saline control, a median difference of 76 minutes that was statistically significant, Dr. Paré reported. Most of the difference in labor duration happened during the first stage, which showed a median 70-minute reduction between the control group and the women receiving dextrose.
“These results support findings from prior studies. Women need glucose during labor,” Elliott Main, MD, commented in an interview. “There is no evidence for a need to exclude glucose from intravenous fluids. Adding some form of glucose is not standard practice today, but the time has come to do it, either by adding glucose to hydrating fluid or have women in labor eat and drink more,” said Dr. Main, medical director of the California Maternal Quality Care Collaborative in Stanford.
Dr. Paré reported having no financial disclosures.
[email protected]
On Twitter @mitchelzoler
LAS VEGAS – Adding 5% dextrose to the hydrating solution given to women undergoing induced labor safely led to a median 76-minute decrease in labor duration in a single-center randomized study.
Normal saline with 5% dextrose “should be considered the default solute during labor induction in nulliparous women,” Josianne Paré, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. “The uterus is a muscle, and glucose is its main energy substrate.”
During January 2013 to January 2015, women who met these criteria and required induction received either normal saline or normal saline plus 5% dextrose when they began their oxytocin drip, at a rate of 250 mL/hour.
Treatment with the assigned hydrating solutions continued until delivery or C-section. Participants averaged 28 years old, their average body mass index was 26 kg/m2 and average birth weight was about 3,450 g.
The study’s primary outcome was total duration of labor. This was a median of 423 minutes in 96 women who received dextrose and were available for analysis, and a median of 499 minutes in 97 evaluable women who received the saline control, a median difference of 76 minutes that was statistically significant, Dr. Paré reported. Most of the difference in labor duration happened during the first stage, which showed a median 70-minute reduction between the control group and the women receiving dextrose.
“These results support findings from prior studies. Women need glucose during labor,” Elliott Main, MD, commented in an interview. “There is no evidence for a need to exclude glucose from intravenous fluids. Adding some form of glucose is not standard practice today, but the time has come to do it, either by adding glucose to hydrating fluid or have women in labor eat and drink more,” said Dr. Main, medical director of the California Maternal Quality Care Collaborative in Stanford.
Dr. Paré reported having no financial disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: Median labor duration fell by 76 minutes among women who received 5% dextrose, compared with controls.
Data source: DEXTRONS, a single-center, randomized study that enrolled 200 pregnant women.
Disclosures: Dr. Paré reported having no financial disclosures.
Universal cervical length screening reduces preterm birth rate
LAS VEGAS – Universal cervical length screening by transvaginal ultrasound in a low-risk cohort resulted in a significant reduction in spontaneous preterm births.
In a single-center retrospective cohort study of more than 13,000 deliveries, the overall preterm birth rate decreased from 3.8% to 2.4% on implementation of universal cervical length screening (P less than .001).
Screening reduced the numbers of both early and late preterm birth rates. Preterm births occurring earlier than 28 weeks’ gestation dropped from 0.3% to 0.1% (P = .04); preterm births before 34 weeks dropped from 1% to 0.5% (P less than .001); and preterm births before 37 weeks dropped from 2.5% to 1.8% (P = .004).
The data were presented by Alex Argyelan, MD, an ob.gyn. resident at St. Joseph Mercy Hospital–Ann Arbor, Mich., at the Annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Argyelan noted that the current Society for Maternal-Fetal Medicine (SMFM) position regarding cervical length screening is that it should not yet be universally mandated for singleton pregnancies without a prior history of preterm birth. However, a 2016 SMFM guideline stated, “Nonetheless, implementation of such a screening strategy can be viewed as reasonable and can be considered by individual practitioners.” This statement was made, he said, in recognition of the fact that “a sonographic short cervix is a powerful predictor of spontaneous preterm birth,” and that progesterone administration for gravid women with shortening cervixes can, for many, forestall spontaneous preterm labor.
First author Pooja Mittal Green, MD, a maternal-fetal medicine specialist at St. Joseph Mercy Hospital, and her associates looked at preterm delivery data before and after implementation of a universal cervical length screening protocol at a single tertiary referral center. The data collection period spanned from January 2013 to May 2014, with implementation of universal cervical length screening in October 2014.
A total of 13,396 women were included in the study, with a small minority of just 0.5% having experienced a prior spontaneous preterm birth. The mean patient age was just under 30 years; most patients were white, mirroring the demographics of the county where the study took place. Pre- and postintervention patient characteristics did not vary significantly.
Almost all patients agreed to cervical length screening by ultrasound, with the numbers climbing from 93% during the first year after implementing the universal screening protocol, to 99.2% in 2016.
All of the sonographers participating in the study were Cervical Length Education and Review (CLEAR) certified, and the institution’s lead sonographer carried out a ongoing quality assurance program.
A shortened cervix (25 mm or less) was found in a total of 114 women (1.7%) who underwent cervical length screening. According to the protocol, if maternal cervical length was 25 mm or less, women were offered treatment to attempt to stave off preterm delivery, according to the usual standard of care.
For women with no prior history of preterm delivery, treatment was vaginal progesterone. For women who had a prior preterm birth, cervical cerclage was offered, as well as vaginal progesterone if the patient was not already on 17-alpha-hydroxyprogesterone caproate.
The determination whether spontaneous preterm birth had occurred was made by reviewing labor and delivery birth logs, with a subsequent individual chart review to make sure that the delivery happened after either spontaneous labor or preterm premature rupture of membranes.
Only women who received prenatal care at the study institution were included in the study, and women who had not received any prenatal care were excluded.
Dr. Argyelan and his colleagues did not see any significant differences between the preterm and term delivery groups in maternal age, body mass index, or ethnicity.
“Among spontaneous preterm deliveries in low-risk women, the proportion of deliveries before 34 weeks was decreased” after the intervention, said Dr. Argyelan, who reported seeing a decrease from 28% early (less than 34 weeks’ gestation) preterm births before the intervention to 17% after the intervention.
In response to an audience question, Dr. Argyelan noted that his institution charges $186 for an ultrasound examination that includes assessment of cervical length, saying, “We have not had significant issues being reimbursed.”
Another audience member asked what the institution policy had been before the universal screening program was implemented. “Before the universal screening study, there was a policy of screening those with a history of preterm birth; also, if sonographers saw what looked like a short cervix on transabdominal exam, then they would do a transvaginal scan to further assess the cervix,” Dr. Argyelan said.
Dr. Argyelan reported having no financial disclosures.
[email protected]
On Twitter @karioakes
LAS VEGAS – Universal cervical length screening by transvaginal ultrasound in a low-risk cohort resulted in a significant reduction in spontaneous preterm births.
In a single-center retrospective cohort study of more than 13,000 deliveries, the overall preterm birth rate decreased from 3.8% to 2.4% on implementation of universal cervical length screening (P less than .001).
Screening reduced the numbers of both early and late preterm birth rates. Preterm births occurring earlier than 28 weeks’ gestation dropped from 0.3% to 0.1% (P = .04); preterm births before 34 weeks dropped from 1% to 0.5% (P less than .001); and preterm births before 37 weeks dropped from 2.5% to 1.8% (P = .004).
The data were presented by Alex Argyelan, MD, an ob.gyn. resident at St. Joseph Mercy Hospital–Ann Arbor, Mich., at the Annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Argyelan noted that the current Society for Maternal-Fetal Medicine (SMFM) position regarding cervical length screening is that it should not yet be universally mandated for singleton pregnancies without a prior history of preterm birth. However, a 2016 SMFM guideline stated, “Nonetheless, implementation of such a screening strategy can be viewed as reasonable and can be considered by individual practitioners.” This statement was made, he said, in recognition of the fact that “a sonographic short cervix is a powerful predictor of spontaneous preterm birth,” and that progesterone administration for gravid women with shortening cervixes can, for many, forestall spontaneous preterm labor.
First author Pooja Mittal Green, MD, a maternal-fetal medicine specialist at St. Joseph Mercy Hospital, and her associates looked at preterm delivery data before and after implementation of a universal cervical length screening protocol at a single tertiary referral center. The data collection period spanned from January 2013 to May 2014, with implementation of universal cervical length screening in October 2014.
A total of 13,396 women were included in the study, with a small minority of just 0.5% having experienced a prior spontaneous preterm birth. The mean patient age was just under 30 years; most patients were white, mirroring the demographics of the county where the study took place. Pre- and postintervention patient characteristics did not vary significantly.
Almost all patients agreed to cervical length screening by ultrasound, with the numbers climbing from 93% during the first year after implementing the universal screening protocol, to 99.2% in 2016.
All of the sonographers participating in the study were Cervical Length Education and Review (CLEAR) certified, and the institution’s lead sonographer carried out a ongoing quality assurance program.
A shortened cervix (25 mm or less) was found in a total of 114 women (1.7%) who underwent cervical length screening. According to the protocol, if maternal cervical length was 25 mm or less, women were offered treatment to attempt to stave off preterm delivery, according to the usual standard of care.
For women with no prior history of preterm delivery, treatment was vaginal progesterone. For women who had a prior preterm birth, cervical cerclage was offered, as well as vaginal progesterone if the patient was not already on 17-alpha-hydroxyprogesterone caproate.
The determination whether spontaneous preterm birth had occurred was made by reviewing labor and delivery birth logs, with a subsequent individual chart review to make sure that the delivery happened after either spontaneous labor or preterm premature rupture of membranes.
Only women who received prenatal care at the study institution were included in the study, and women who had not received any prenatal care were excluded.
Dr. Argyelan and his colleagues did not see any significant differences between the preterm and term delivery groups in maternal age, body mass index, or ethnicity.
“Among spontaneous preterm deliveries in low-risk women, the proportion of deliveries before 34 weeks was decreased” after the intervention, said Dr. Argyelan, who reported seeing a decrease from 28% early (less than 34 weeks’ gestation) preterm births before the intervention to 17% after the intervention.
In response to an audience question, Dr. Argyelan noted that his institution charges $186 for an ultrasound examination that includes assessment of cervical length, saying, “We have not had significant issues being reimbursed.”
Another audience member asked what the institution policy had been before the universal screening program was implemented. “Before the universal screening study, there was a policy of screening those with a history of preterm birth; also, if sonographers saw what looked like a short cervix on transabdominal exam, then they would do a transvaginal scan to further assess the cervix,” Dr. Argyelan said.
Dr. Argyelan reported having no financial disclosures.
[email protected]
On Twitter @karioakes
LAS VEGAS – Universal cervical length screening by transvaginal ultrasound in a low-risk cohort resulted in a significant reduction in spontaneous preterm births.
In a single-center retrospective cohort study of more than 13,000 deliveries, the overall preterm birth rate decreased from 3.8% to 2.4% on implementation of universal cervical length screening (P less than .001).
Screening reduced the numbers of both early and late preterm birth rates. Preterm births occurring earlier than 28 weeks’ gestation dropped from 0.3% to 0.1% (P = .04); preterm births before 34 weeks dropped from 1% to 0.5% (P less than .001); and preterm births before 37 weeks dropped from 2.5% to 1.8% (P = .004).
The data were presented by Alex Argyelan, MD, an ob.gyn. resident at St. Joseph Mercy Hospital–Ann Arbor, Mich., at the Annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Argyelan noted that the current Society for Maternal-Fetal Medicine (SMFM) position regarding cervical length screening is that it should not yet be universally mandated for singleton pregnancies without a prior history of preterm birth. However, a 2016 SMFM guideline stated, “Nonetheless, implementation of such a screening strategy can be viewed as reasonable and can be considered by individual practitioners.” This statement was made, he said, in recognition of the fact that “a sonographic short cervix is a powerful predictor of spontaneous preterm birth,” and that progesterone administration for gravid women with shortening cervixes can, for many, forestall spontaneous preterm labor.
First author Pooja Mittal Green, MD, a maternal-fetal medicine specialist at St. Joseph Mercy Hospital, and her associates looked at preterm delivery data before and after implementation of a universal cervical length screening protocol at a single tertiary referral center. The data collection period spanned from January 2013 to May 2014, with implementation of universal cervical length screening in October 2014.
A total of 13,396 women were included in the study, with a small minority of just 0.5% having experienced a prior spontaneous preterm birth. The mean patient age was just under 30 years; most patients were white, mirroring the demographics of the county where the study took place. Pre- and postintervention patient characteristics did not vary significantly.
Almost all patients agreed to cervical length screening by ultrasound, with the numbers climbing from 93% during the first year after implementing the universal screening protocol, to 99.2% in 2016.
All of the sonographers participating in the study were Cervical Length Education and Review (CLEAR) certified, and the institution’s lead sonographer carried out a ongoing quality assurance program.
A shortened cervix (25 mm or less) was found in a total of 114 women (1.7%) who underwent cervical length screening. According to the protocol, if maternal cervical length was 25 mm or less, women were offered treatment to attempt to stave off preterm delivery, according to the usual standard of care.
For women with no prior history of preterm delivery, treatment was vaginal progesterone. For women who had a prior preterm birth, cervical cerclage was offered, as well as vaginal progesterone if the patient was not already on 17-alpha-hydroxyprogesterone caproate.
The determination whether spontaneous preterm birth had occurred was made by reviewing labor and delivery birth logs, with a subsequent individual chart review to make sure that the delivery happened after either spontaneous labor or preterm premature rupture of membranes.
Only women who received prenatal care at the study institution were included in the study, and women who had not received any prenatal care were excluded.
Dr. Argyelan and his colleagues did not see any significant differences between the preterm and term delivery groups in maternal age, body mass index, or ethnicity.
“Among spontaneous preterm deliveries in low-risk women, the proportion of deliveries before 34 weeks was decreased” after the intervention, said Dr. Argyelan, who reported seeing a decrease from 28% early (less than 34 weeks’ gestation) preterm births before the intervention to 17% after the intervention.
In response to an audience question, Dr. Argyelan noted that his institution charges $186 for an ultrasound examination that includes assessment of cervical length, saying, “We have not had significant issues being reimbursed.”
Another audience member asked what the institution policy had been before the universal screening program was implemented. “Before the universal screening study, there was a policy of screening those with a history of preterm birth; also, if sonographers saw what looked like a short cervix on transabdominal exam, then they would do a transvaginal scan to further assess the cervix,” Dr. Argyelan said.
Dr. Argyelan reported having no financial disclosures.
[email protected]
On Twitter @karioakes
AT THE ANNUAL PREGNANCY MEETING
Key clinical point:
Major finding: Preterm births dropped from 3.8% to 2.4% (P less than .001) after implementing a universal cervical length screening program.
Data source: Retrospective single-site cohort study of 13,396 singleton pregnancies.
Disclosures: Dr. Argyelan reported having no financial disclosures.
Complex congenital heart conditions call for complex care in pregnancy
A new scientific statement from the American Heart Association (AHA) brings together recommendations for management of pregnancy for women with serious congenital heart disease. The 38-page document addresses a wide range of complex congenital heart conditions, presenting a newly unified set of recommendations for care that ranges from preconception counseling, through pregnancy, labor, and delivery, to the postpartum period.
Caring for women with complex congenital heart lesions is becoming more commonplace, as more infants undergo successful repairs of previously-unsurvivable cardiac anomalies. “More moms with congenital heart disease are showing up pregnant, having survived the tumultuous peripartum and neonatal period, and are now facing a new set of risks in pregnancy,” Michael Foley, MD, chair of the department of obstetrics and gynecology at the University of Arizona, Phoenix, said in an interview.
Joseph Kay, MD, a cardiologist and professor of medicine and pediatrics at the University of Colorado, Aurora, said that one big benefit of the new scientific statement is having a single reference point for care of these patients. “The scientific statement brings all of the information about caring for these patients together into one document. This will be a very valuable resource for trainees to get a sense of what’s important; it also represents a platform for new programs to understand the scope of services needed,” said Dr. Kay in an interview.
The document provides a thorough review of the physiologic changes of pregnancy and the intrapartum and postpartum periods, noting that the heterogeneity of congenital heart disease means that women who have different lesions carry different risks in pregnancy.
Examples of lesions presenting intermediate risk include most arrhythmias (category II), hypertrophic cardiomyopathy, and a repaired coarctation (both category II-III). The most severe lesions carry a contraindication for pregnancy; the WHO guidelines suggest discussing termination should women with a category IV lesion become pregnant. Severe mitral stenosis, severe symptomatic aortic stenosis, and severe systemic ventricular dysfunction all place women into category IV.
Beginning with pregnancy risk category III, the WHO guidelines recommend intensive cardiac and obstetric monitoring throughout pregnancy, childbirth, and the puerperium. Several maternal-fetal medicine specialists interviewed all agreed that an interdisciplinary team is a must for good obstetric care in this population.
How interdisciplinary care plays out can depend on geography and facility-dependent resources. Dr. Kay said that his facility is the referral site for pregnant women with complex congenital lesions in an area that spans the Canadian and the Mexican borders from north to south, and ranges from parts of Kansas to eastern Montana from east to west. Still, Dr. Kay said that even for patients with lower-risk lesions, “We will see patients at least once, at approximately the midpoint of pregnancy, and again during the third trimester if possible.” The specifics of care depend on “the nature of the lesion and the complexity of the disease,” said Dr. Kay.
In his facility, said Dr. Kay, telemetry is available for all of the labor and delivery unit beds. This means that the mother and infant can usually stay together and receive postpartum nursing and lactation care from a skilled staff.
In no circumstances should ob.gyns. go it alone, said Dr. Foley. “The conversation with the ob.gyn. needs to be about comanaging these patients, at the very least. Even the most learned maternal-fetal medicine specialist needs to be working with a cardiologist and an anesthesiologist to create a delivery plan that includes pain management, fluid management, and consideration for intrapartum hemodynamic monitoring,” he said.
And the team needs to be in place long before delivery, Dr. Foley pointed out. “In many hospitals, the care delivery gap may be the inability to have this consistent proactive approach. You can’t expect the best outcomes when you have to hurriedly assemble an unfamiliar ad hoc team when a woman with congenital heart disease presents in labor. Despite their best intentions, inconsistent team members may not have the knowledge and experience to provide the safest care for these patients,” he said.
Though an individualized labor and delivery plan is a must, and a multispecialty team should be assembled, maternal congenital heart disease doesn’t necessarily consign a woman to cesarean delivery. “Most women can and should have a vaginal delivery. It’s safer for them. If a natural delivery may increase risk of issues, we may consider a facilitated second stage of labor with epidural anesthesia and forceps- or vacuum-assisted delivery,” said Dr. Kay.
It’s important to understand the nuances of an individual patient’s health and risk status, said Dr. Norton. “A simplified view is often bad. It’s not the case that ‘it’s always better to deliver’ or ‘it’s always better to have a cesarean delivery.’”
Especially for women who need anticoagulation or who may have lesions that put them at great risk should pregnancy occur, preconception counseling is a vital part of their care, and guidance in the scientific statement can help specialists avoid the complications that can occur in the absence of evidence-based treatment. Said Dr. Kay, “I have seen an unfortunate case or two of patients whose anticoagulation was stopped or changed, contrary to guidelines, and who suffered strokes. I hope more people will see this document.”
Ms. Canobbio echoed the sentiment: “You don’t want to have to backpedal once a young woman presents with a pregnancy. Appropriate contraceptive counseling needs to be part of the conversation.”
One key concept underscored in the scientific statement is that elevated risk persists into the postpartum period. “Following delivery, the mother is still at risk for an extended period of time. The greatest risk for mortality in these patients is post delivery, when a large volume of blood is expelled from the uterus back into the maternal circulation,” said Ms. Canobbio. “These women need close follow-up; we can’t say they are home free until several weeks to 2 months after delivery. The need for vigilance and surveillance continues.”
Since the scientific statement is not a new set of guidelines, but rather a compilation of currently existing reference documents, the authors noted that management differences may exist in some cases, but did not assign greater value to one practice than another. “We addressed that there are differences between the European and the American guidelines. For example, with regard to anticoagulation, both would agree to use Lovenox [enoxaparin], but the difference is whether it should be used for the entire pregnancy or for parts of the pregnancy,” said Ms. Canobbio.
Looking forward, more women with complex congenital heart disease will bear children, but their future is not certain. Said Ms. Canobbio: “The data are growing that if the patient is clinically stable at the time of pregnancy, it’s likely we can get them through safely. What’s not yet known is whether the burden of pregnancy in a woman who is otherwise healthy will shorten her lifespan. However, early data are promising, and it’s looking like these women can fare well.”
Topics covered in the scientific statement include:
- Defining which patients are at increased risk in pregnancy.
- Physiological adaptations of pregnancy, the puerperium, and the postpartum period, with an emphasis on hemodynamic changes.
- Assessment and evaluation in the preconception and early prenatal periods.
- Pregnancy management, including appropriate testing.
- Medications in pregnancy, including a table of common cardiac drugs and their pregnancy categories and lactation risks.
- Breakdown of suggested prenatal care by trimester.
- Intrapartum care, including indications for fluid management, ECG and hemodynamic monitoring, and management of the second stage of delivery.
- Postpartum care, with attention to the very rapid increase in blood volume and concomitant leap in stroke volume and cardiac output.
- Considerations when choosing contraceptive method.
- Cardiac complications seen in pregnancy, including arrhythmias, managing mechanical valves and anticoagulation, heart failure, and cyanosis.
- Indications for and risks associated with interventional therapies during pregnancy.
- Detailed discussion of management of pregnancy for women with specific lesions.
None of the members of the writing committee for the scientific statement had relevant disclosures. Dr. Foley and Dr. Kay reported no disclosures. Dr. Norton reported that she has received research funding from Natera and Ultragenyx.
[email protected]
On Twitter @karioakes
A new scientific statement from the American Heart Association (AHA) brings together recommendations for management of pregnancy for women with serious congenital heart disease. The 38-page document addresses a wide range of complex congenital heart conditions, presenting a newly unified set of recommendations for care that ranges from preconception counseling, through pregnancy, labor, and delivery, to the postpartum period.
Caring for women with complex congenital heart lesions is becoming more commonplace, as more infants undergo successful repairs of previously-unsurvivable cardiac anomalies. “More moms with congenital heart disease are showing up pregnant, having survived the tumultuous peripartum and neonatal period, and are now facing a new set of risks in pregnancy,” Michael Foley, MD, chair of the department of obstetrics and gynecology at the University of Arizona, Phoenix, said in an interview.
Joseph Kay, MD, a cardiologist and professor of medicine and pediatrics at the University of Colorado, Aurora, said that one big benefit of the new scientific statement is having a single reference point for care of these patients. “The scientific statement brings all of the information about caring for these patients together into one document. This will be a very valuable resource for trainees to get a sense of what’s important; it also represents a platform for new programs to understand the scope of services needed,” said Dr. Kay in an interview.
The document provides a thorough review of the physiologic changes of pregnancy and the intrapartum and postpartum periods, noting that the heterogeneity of congenital heart disease means that women who have different lesions carry different risks in pregnancy.
Examples of lesions presenting intermediate risk include most arrhythmias (category II), hypertrophic cardiomyopathy, and a repaired coarctation (both category II-III). The most severe lesions carry a contraindication for pregnancy; the WHO guidelines suggest discussing termination should women with a category IV lesion become pregnant. Severe mitral stenosis, severe symptomatic aortic stenosis, and severe systemic ventricular dysfunction all place women into category IV.
Beginning with pregnancy risk category III, the WHO guidelines recommend intensive cardiac and obstetric monitoring throughout pregnancy, childbirth, and the puerperium. Several maternal-fetal medicine specialists interviewed all agreed that an interdisciplinary team is a must for good obstetric care in this population.
How interdisciplinary care plays out can depend on geography and facility-dependent resources. Dr. Kay said that his facility is the referral site for pregnant women with complex congenital lesions in an area that spans the Canadian and the Mexican borders from north to south, and ranges from parts of Kansas to eastern Montana from east to west. Still, Dr. Kay said that even for patients with lower-risk lesions, “We will see patients at least once, at approximately the midpoint of pregnancy, and again during the third trimester if possible.” The specifics of care depend on “the nature of the lesion and the complexity of the disease,” said Dr. Kay.
In his facility, said Dr. Kay, telemetry is available for all of the labor and delivery unit beds. This means that the mother and infant can usually stay together and receive postpartum nursing and lactation care from a skilled staff.
In no circumstances should ob.gyns. go it alone, said Dr. Foley. “The conversation with the ob.gyn. needs to be about comanaging these patients, at the very least. Even the most learned maternal-fetal medicine specialist needs to be working with a cardiologist and an anesthesiologist to create a delivery plan that includes pain management, fluid management, and consideration for intrapartum hemodynamic monitoring,” he said.
And the team needs to be in place long before delivery, Dr. Foley pointed out. “In many hospitals, the care delivery gap may be the inability to have this consistent proactive approach. You can’t expect the best outcomes when you have to hurriedly assemble an unfamiliar ad hoc team when a woman with congenital heart disease presents in labor. Despite their best intentions, inconsistent team members may not have the knowledge and experience to provide the safest care for these patients,” he said.
Though an individualized labor and delivery plan is a must, and a multispecialty team should be assembled, maternal congenital heart disease doesn’t necessarily consign a woman to cesarean delivery. “Most women can and should have a vaginal delivery. It’s safer for them. If a natural delivery may increase risk of issues, we may consider a facilitated second stage of labor with epidural anesthesia and forceps- or vacuum-assisted delivery,” said Dr. Kay.
It’s important to understand the nuances of an individual patient’s health and risk status, said Dr. Norton. “A simplified view is often bad. It’s not the case that ‘it’s always better to deliver’ or ‘it’s always better to have a cesarean delivery.’”
Especially for women who need anticoagulation or who may have lesions that put them at great risk should pregnancy occur, preconception counseling is a vital part of their care, and guidance in the scientific statement can help specialists avoid the complications that can occur in the absence of evidence-based treatment. Said Dr. Kay, “I have seen an unfortunate case or two of patients whose anticoagulation was stopped or changed, contrary to guidelines, and who suffered strokes. I hope more people will see this document.”
Ms. Canobbio echoed the sentiment: “You don’t want to have to backpedal once a young woman presents with a pregnancy. Appropriate contraceptive counseling needs to be part of the conversation.”
One key concept underscored in the scientific statement is that elevated risk persists into the postpartum period. “Following delivery, the mother is still at risk for an extended period of time. The greatest risk for mortality in these patients is post delivery, when a large volume of blood is expelled from the uterus back into the maternal circulation,” said Ms. Canobbio. “These women need close follow-up; we can’t say they are home free until several weeks to 2 months after delivery. The need for vigilance and surveillance continues.”
Since the scientific statement is not a new set of guidelines, but rather a compilation of currently existing reference documents, the authors noted that management differences may exist in some cases, but did not assign greater value to one practice than another. “We addressed that there are differences between the European and the American guidelines. For example, with regard to anticoagulation, both would agree to use Lovenox [enoxaparin], but the difference is whether it should be used for the entire pregnancy or for parts of the pregnancy,” said Ms. Canobbio.
Looking forward, more women with complex congenital heart disease will bear children, but their future is not certain. Said Ms. Canobbio: “The data are growing that if the patient is clinically stable at the time of pregnancy, it’s likely we can get them through safely. What’s not yet known is whether the burden of pregnancy in a woman who is otherwise healthy will shorten her lifespan. However, early data are promising, and it’s looking like these women can fare well.”
Topics covered in the scientific statement include:
- Defining which patients are at increased risk in pregnancy.
- Physiological adaptations of pregnancy, the puerperium, and the postpartum period, with an emphasis on hemodynamic changes.
- Assessment and evaluation in the preconception and early prenatal periods.
- Pregnancy management, including appropriate testing.
- Medications in pregnancy, including a table of common cardiac drugs and their pregnancy categories and lactation risks.
- Breakdown of suggested prenatal care by trimester.
- Intrapartum care, including indications for fluid management, ECG and hemodynamic monitoring, and management of the second stage of delivery.
- Postpartum care, with attention to the very rapid increase in blood volume and concomitant leap in stroke volume and cardiac output.
- Considerations when choosing contraceptive method.
- Cardiac complications seen in pregnancy, including arrhythmias, managing mechanical valves and anticoagulation, heart failure, and cyanosis.
- Indications for and risks associated with interventional therapies during pregnancy.
- Detailed discussion of management of pregnancy for women with specific lesions.
None of the members of the writing committee for the scientific statement had relevant disclosures. Dr. Foley and Dr. Kay reported no disclosures. Dr. Norton reported that she has received research funding from Natera and Ultragenyx.
[email protected]
On Twitter @karioakes
A new scientific statement from the American Heart Association (AHA) brings together recommendations for management of pregnancy for women with serious congenital heart disease. The 38-page document addresses a wide range of complex congenital heart conditions, presenting a newly unified set of recommendations for care that ranges from preconception counseling, through pregnancy, labor, and delivery, to the postpartum period.
Caring for women with complex congenital heart lesions is becoming more commonplace, as more infants undergo successful repairs of previously-unsurvivable cardiac anomalies. “More moms with congenital heart disease are showing up pregnant, having survived the tumultuous peripartum and neonatal period, and are now facing a new set of risks in pregnancy,” Michael Foley, MD, chair of the department of obstetrics and gynecology at the University of Arizona, Phoenix, said in an interview.
Joseph Kay, MD, a cardiologist and professor of medicine and pediatrics at the University of Colorado, Aurora, said that one big benefit of the new scientific statement is having a single reference point for care of these patients. “The scientific statement brings all of the information about caring for these patients together into one document. This will be a very valuable resource for trainees to get a sense of what’s important; it also represents a platform for new programs to understand the scope of services needed,” said Dr. Kay in an interview.
The document provides a thorough review of the physiologic changes of pregnancy and the intrapartum and postpartum periods, noting that the heterogeneity of congenital heart disease means that women who have different lesions carry different risks in pregnancy.
Examples of lesions presenting intermediate risk include most arrhythmias (category II), hypertrophic cardiomyopathy, and a repaired coarctation (both category II-III). The most severe lesions carry a contraindication for pregnancy; the WHO guidelines suggest discussing termination should women with a category IV lesion become pregnant. Severe mitral stenosis, severe symptomatic aortic stenosis, and severe systemic ventricular dysfunction all place women into category IV.
Beginning with pregnancy risk category III, the WHO guidelines recommend intensive cardiac and obstetric monitoring throughout pregnancy, childbirth, and the puerperium. Several maternal-fetal medicine specialists interviewed all agreed that an interdisciplinary team is a must for good obstetric care in this population.
How interdisciplinary care plays out can depend on geography and facility-dependent resources. Dr. Kay said that his facility is the referral site for pregnant women with complex congenital lesions in an area that spans the Canadian and the Mexican borders from north to south, and ranges from parts of Kansas to eastern Montana from east to west. Still, Dr. Kay said that even for patients with lower-risk lesions, “We will see patients at least once, at approximately the midpoint of pregnancy, and again during the third trimester if possible.” The specifics of care depend on “the nature of the lesion and the complexity of the disease,” said Dr. Kay.
In his facility, said Dr. Kay, telemetry is available for all of the labor and delivery unit beds. This means that the mother and infant can usually stay together and receive postpartum nursing and lactation care from a skilled staff.
In no circumstances should ob.gyns. go it alone, said Dr. Foley. “The conversation with the ob.gyn. needs to be about comanaging these patients, at the very least. Even the most learned maternal-fetal medicine specialist needs to be working with a cardiologist and an anesthesiologist to create a delivery plan that includes pain management, fluid management, and consideration for intrapartum hemodynamic monitoring,” he said.
And the team needs to be in place long before delivery, Dr. Foley pointed out. “In many hospitals, the care delivery gap may be the inability to have this consistent proactive approach. You can’t expect the best outcomes when you have to hurriedly assemble an unfamiliar ad hoc team when a woman with congenital heart disease presents in labor. Despite their best intentions, inconsistent team members may not have the knowledge and experience to provide the safest care for these patients,” he said.
Though an individualized labor and delivery plan is a must, and a multispecialty team should be assembled, maternal congenital heart disease doesn’t necessarily consign a woman to cesarean delivery. “Most women can and should have a vaginal delivery. It’s safer for them. If a natural delivery may increase risk of issues, we may consider a facilitated second stage of labor with epidural anesthesia and forceps- or vacuum-assisted delivery,” said Dr. Kay.
It’s important to understand the nuances of an individual patient’s health and risk status, said Dr. Norton. “A simplified view is often bad. It’s not the case that ‘it’s always better to deliver’ or ‘it’s always better to have a cesarean delivery.’”
Especially for women who need anticoagulation or who may have lesions that put them at great risk should pregnancy occur, preconception counseling is a vital part of their care, and guidance in the scientific statement can help specialists avoid the complications that can occur in the absence of evidence-based treatment. Said Dr. Kay, “I have seen an unfortunate case or two of patients whose anticoagulation was stopped or changed, contrary to guidelines, and who suffered strokes. I hope more people will see this document.”
Ms. Canobbio echoed the sentiment: “You don’t want to have to backpedal once a young woman presents with a pregnancy. Appropriate contraceptive counseling needs to be part of the conversation.”
One key concept underscored in the scientific statement is that elevated risk persists into the postpartum period. “Following delivery, the mother is still at risk for an extended period of time. The greatest risk for mortality in these patients is post delivery, when a large volume of blood is expelled from the uterus back into the maternal circulation,” said Ms. Canobbio. “These women need close follow-up; we can’t say they are home free until several weeks to 2 months after delivery. The need for vigilance and surveillance continues.”
Since the scientific statement is not a new set of guidelines, but rather a compilation of currently existing reference documents, the authors noted that management differences may exist in some cases, but did not assign greater value to one practice than another. “We addressed that there are differences between the European and the American guidelines. For example, with regard to anticoagulation, both would agree to use Lovenox [enoxaparin], but the difference is whether it should be used for the entire pregnancy or for parts of the pregnancy,” said Ms. Canobbio.
Looking forward, more women with complex congenital heart disease will bear children, but their future is not certain. Said Ms. Canobbio: “The data are growing that if the patient is clinically stable at the time of pregnancy, it’s likely we can get them through safely. What’s not yet known is whether the burden of pregnancy in a woman who is otherwise healthy will shorten her lifespan. However, early data are promising, and it’s looking like these women can fare well.”
Topics covered in the scientific statement include:
- Defining which patients are at increased risk in pregnancy.
- Physiological adaptations of pregnancy, the puerperium, and the postpartum period, with an emphasis on hemodynamic changes.
- Assessment and evaluation in the preconception and early prenatal periods.
- Pregnancy management, including appropriate testing.
- Medications in pregnancy, including a table of common cardiac drugs and their pregnancy categories and lactation risks.
- Breakdown of suggested prenatal care by trimester.
- Intrapartum care, including indications for fluid management, ECG and hemodynamic monitoring, and management of the second stage of delivery.
- Postpartum care, with attention to the very rapid increase in blood volume and concomitant leap in stroke volume and cardiac output.
- Considerations when choosing contraceptive method.
- Cardiac complications seen in pregnancy, including arrhythmias, managing mechanical valves and anticoagulation, heart failure, and cyanosis.
- Indications for and risks associated with interventional therapies during pregnancy.
- Detailed discussion of management of pregnancy for women with specific lesions.
None of the members of the writing committee for the scientific statement had relevant disclosures. Dr. Foley and Dr. Kay reported no disclosures. Dr. Norton reported that she has received research funding from Natera and Ultragenyx.
[email protected]
On Twitter @karioakes
Childhood obesity tied to maternal obesity, cesarean birth
NEW ORLEANS – Maternal obesity and cesarean delivery were each independently associated with increased rates of overweight or obesity during childhood in a prospective study of 1,441 mothers and their children.
In addition, these risks for childhood obesity appeared to interact in an additive way, so that women who were both obese and delivered by C-section had a nearly threefold increased rate of having a child who was overweight or obese at about 5 years of age, compared with children born to normal-weight women who delivered vaginally, Noel T. Mueller, PhD, said at the American Heart Association Scientific Sessions.
This finding of a link between maternal overweight and obesity and childhood obesity in the next generation supports results from previously reported studies. The new results “also add to the growing evidence for an association between C-section and obesity [in offspring], as well as C-section and immune-related disorders such as asthma and allergies” in offspring, Dr. Mueller said in an interview.
He hypothesized that delivery mode may contribute to a child’s obesity risk by producing an abnormal gastrointestinal microbiome. For example, vaginal delivery seems to associate with a higher prevalence of Bacteroides species in a child’s gut, bacteria that aid in the digestion of breast milk, Dr. Mueller said.
His study used data collected in the Boston Birth Cohort from 1,441 mothers and their children from full-term, singleton pregnancies born to women with a body mass index of at least 18.5 kg/m2 during 1998-2014. The child’s weight was measured at a median age of 4.8 years, with an interquartile range of 3-6 years. Children were deemed overweight if they were at or above the 85th percentile for weight, according to standards from the Centers for Disease Control and Prevention.
Just under half the women were normal weight, slightly more than a quarter were overweight, and a quarter were obese. The incidence of 5-year-old children who were overweight or obese was 70% higher in children of overweight mothers and 80% higher in those with obese mothers, compared with children with normal-weight mothers in an analysis that adjusted for maternal age at delivery, race or ethnicity, and education. Both were statistically significant differences, Dr. Mueller reported.
Two-thirds of the women had vaginal deliveries and a third had C-sections. Overweight or obesity occurred in 40% more of the children delivered by C-section, compared with children born vaginally, a statistically significant difference in an analysis that controlled for the same three covariates as well as prepregnancy body mass index, pregnancy weight gain, and other variables.
When Dr. Mueller and his associates ran a combined analysis they found that the highest risk for childhood overweight or obesity was in children born to obese mothers by C-section, and it was a 2.8-fold higher rate than that in the children born to normal-weight mothers by vaginal delivery, a statistically significant difference.
Dr. Mueller had no disclosures.
[email protected]
On Twitter @mitchelzoler
NEW ORLEANS – Maternal obesity and cesarean delivery were each independently associated with increased rates of overweight or obesity during childhood in a prospective study of 1,441 mothers and their children.
In addition, these risks for childhood obesity appeared to interact in an additive way, so that women who were both obese and delivered by C-section had a nearly threefold increased rate of having a child who was overweight or obese at about 5 years of age, compared with children born to normal-weight women who delivered vaginally, Noel T. Mueller, PhD, said at the American Heart Association Scientific Sessions.
This finding of a link between maternal overweight and obesity and childhood obesity in the next generation supports results from previously reported studies. The new results “also add to the growing evidence for an association between C-section and obesity [in offspring], as well as C-section and immune-related disorders such as asthma and allergies” in offspring, Dr. Mueller said in an interview.
He hypothesized that delivery mode may contribute to a child’s obesity risk by producing an abnormal gastrointestinal microbiome. For example, vaginal delivery seems to associate with a higher prevalence of Bacteroides species in a child’s gut, bacteria that aid in the digestion of breast milk, Dr. Mueller said.
His study used data collected in the Boston Birth Cohort from 1,441 mothers and their children from full-term, singleton pregnancies born to women with a body mass index of at least 18.5 kg/m2 during 1998-2014. The child’s weight was measured at a median age of 4.8 years, with an interquartile range of 3-6 years. Children were deemed overweight if they were at or above the 85th percentile for weight, according to standards from the Centers for Disease Control and Prevention.
Just under half the women were normal weight, slightly more than a quarter were overweight, and a quarter were obese. The incidence of 5-year-old children who were overweight or obese was 70% higher in children of overweight mothers and 80% higher in those with obese mothers, compared with children with normal-weight mothers in an analysis that adjusted for maternal age at delivery, race or ethnicity, and education. Both were statistically significant differences, Dr. Mueller reported.
Two-thirds of the women had vaginal deliveries and a third had C-sections. Overweight or obesity occurred in 40% more of the children delivered by C-section, compared with children born vaginally, a statistically significant difference in an analysis that controlled for the same three covariates as well as prepregnancy body mass index, pregnancy weight gain, and other variables.
When Dr. Mueller and his associates ran a combined analysis they found that the highest risk for childhood overweight or obesity was in children born to obese mothers by C-section, and it was a 2.8-fold higher rate than that in the children born to normal-weight mothers by vaginal delivery, a statistically significant difference.
Dr. Mueller had no disclosures.
[email protected]
On Twitter @mitchelzoler
NEW ORLEANS – Maternal obesity and cesarean delivery were each independently associated with increased rates of overweight or obesity during childhood in a prospective study of 1,441 mothers and their children.
In addition, these risks for childhood obesity appeared to interact in an additive way, so that women who were both obese and delivered by C-section had a nearly threefold increased rate of having a child who was overweight or obese at about 5 years of age, compared with children born to normal-weight women who delivered vaginally, Noel T. Mueller, PhD, said at the American Heart Association Scientific Sessions.
This finding of a link between maternal overweight and obesity and childhood obesity in the next generation supports results from previously reported studies. The new results “also add to the growing evidence for an association between C-section and obesity [in offspring], as well as C-section and immune-related disorders such as asthma and allergies” in offspring, Dr. Mueller said in an interview.
He hypothesized that delivery mode may contribute to a child’s obesity risk by producing an abnormal gastrointestinal microbiome. For example, vaginal delivery seems to associate with a higher prevalence of Bacteroides species in a child’s gut, bacteria that aid in the digestion of breast milk, Dr. Mueller said.
His study used data collected in the Boston Birth Cohort from 1,441 mothers and their children from full-term, singleton pregnancies born to women with a body mass index of at least 18.5 kg/m2 during 1998-2014. The child’s weight was measured at a median age of 4.8 years, with an interquartile range of 3-6 years. Children were deemed overweight if they were at or above the 85th percentile for weight, according to standards from the Centers for Disease Control and Prevention.
Just under half the women were normal weight, slightly more than a quarter were overweight, and a quarter were obese. The incidence of 5-year-old children who were overweight or obese was 70% higher in children of overweight mothers and 80% higher in those with obese mothers, compared with children with normal-weight mothers in an analysis that adjusted for maternal age at delivery, race or ethnicity, and education. Both were statistically significant differences, Dr. Mueller reported.
Two-thirds of the women had vaginal deliveries and a third had C-sections. Overweight or obesity occurred in 40% more of the children delivered by C-section, compared with children born vaginally, a statistically significant difference in an analysis that controlled for the same three covariates as well as prepregnancy body mass index, pregnancy weight gain, and other variables.
When Dr. Mueller and his associates ran a combined analysis they found that the highest risk for childhood overweight or obesity was in children born to obese mothers by C-section, and it was a 2.8-fold higher rate than that in the children born to normal-weight mothers by vaginal delivery, a statistically significant difference.
Dr. Mueller had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Children from obese mothers who had cesarean sections had a 2.8-fold higher obesity rate, compared with children from normal-weight mothers who had vaginal deliveries.
Data source: The Boston Birth Cohort, with prospective data from 1,441 pregnant women and their children.
Disclosures: Dr. Mueller had no disclosures.
Symptoms don’t worsen during pregnancy in most PsA patients
Psoriatic arthritis disease activity tended to improve or stabilize during pregnancy and the first year after giving birth, even outpacing controls, in a small retrospective cohort study.
“The outcome of pregnancy in PsA [psoriatic arthritis] patients is excellent,” investigators from the University of Toronto Psoriatic Arthritis Program reported. They found that “arthritis activity has a favorable course during pregnancy in almost 60% of the pregnancies, while the skin disease shows a favorable course in close to 90% of the pregnancies.”
According to the researchers, led by Ari Polachek, MD, of the Centre for Prognosis Studies in the Rheumatic Diseases at Toronto Western Hospital, previous research has found that rheumatoid arthritis improves in most pregnant women with the condition but then worsens in the year after birth, while most patients with ankylosing spondylitis don’t get better or worse. Limited research suggests psoriasis tends to improve during pregnancy and then flares afterward.
For the new study, researchers tracked 29 pregnant PsA patients with 42 total pregnancies who had a mean age of about 34 years at the beginning of pregnancy and matched them with 67 control patients with PsA who were not pregnant and had an average age of about 35 years. They had all visited the University of Toronto Psoriatic Arthritis Clinic during 1990-2015 (Semin Arthritis Rheum. 2017 Jan 16. doi: 10.1016/j.semarthrit.2017.01.002).
Among the 41 pregnancies in women who began follow-up prior to pregnancy, 13 (32%) had an unfavorable course of disease activity marked by worsening during 8 (20%) of the pregnancies or stable high disease activity during 5 (12%). The course of disease activity was more favorable for 24 (59%) pregnancies, in which it improved in 11 (27%) and stayed stable at a low disease level in 13 (32%). Four pregnancies (10%) had a mixed pattern of improvement followed by worsening.
The 1-year postpartum period during 40 pregnancies showed that stable or worsening symptoms were most common: 8 (20%) had improvement and 13 (32.5%) had stable low disease activity, while another 16 (4%) worsened and 3 (8%) had a mixed course of improvement followed by worsening.
After they controlled the results to account for various factors, the researchers found that pregnancy appeared to be especially beneficial for skin-related PsA symptoms. The likelihood of improved skin activity during pregnancy rose significantly (odds ratio, 7.7; 95% confidence interval, 1.8-23.5; P = .004) when compared with a matched period among controls, but this was no longer the case during the year after birth (OR, 0.4; 95% CI, 0.2-1.4; P = .60).
The likelihood of improved joint symptoms during pregnancy also rose, but not to a significant extent (OR, 2.1; 95% CI, 0.8-5.1; P = .10), and the effect on joints was not significant in the year after pregnancy (OR, 1.4; 95% CI, 0.5-3.4; P = .50).
There was a declining use of medications among the patients during pregnancy, particularly in the second and third trimesters, but two-thirds of the patients were treated with medications for PsA during this time, including NSAIDs (41%), disease-modifying antirheumatic drugs (35%), and biologic agents (26%).
The researchers speculated that hormonal changes during pregnancy may explain the improvement in skin activity. However, they noted that women with PsA who have multiple pregnancies don’t tend to have the same experiences each time: “Most of the women with more than one pregnancy had different joint disease course during their own different pregnancies and postpartum periods. Accordingly, this suggests that each woman needs specific evaluation and treatment adjustment during each pregnancy.”
The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. Dr. Polachek is supported by an educational grant from Janssen Canada.
Psoriatic arthritis disease activity tended to improve or stabilize during pregnancy and the first year after giving birth, even outpacing controls, in a small retrospective cohort study.
“The outcome of pregnancy in PsA [psoriatic arthritis] patients is excellent,” investigators from the University of Toronto Psoriatic Arthritis Program reported. They found that “arthritis activity has a favorable course during pregnancy in almost 60% of the pregnancies, while the skin disease shows a favorable course in close to 90% of the pregnancies.”
According to the researchers, led by Ari Polachek, MD, of the Centre for Prognosis Studies in the Rheumatic Diseases at Toronto Western Hospital, previous research has found that rheumatoid arthritis improves in most pregnant women with the condition but then worsens in the year after birth, while most patients with ankylosing spondylitis don’t get better or worse. Limited research suggests psoriasis tends to improve during pregnancy and then flares afterward.
For the new study, researchers tracked 29 pregnant PsA patients with 42 total pregnancies who had a mean age of about 34 years at the beginning of pregnancy and matched them with 67 control patients with PsA who were not pregnant and had an average age of about 35 years. They had all visited the University of Toronto Psoriatic Arthritis Clinic during 1990-2015 (Semin Arthritis Rheum. 2017 Jan 16. doi: 10.1016/j.semarthrit.2017.01.002).
Among the 41 pregnancies in women who began follow-up prior to pregnancy, 13 (32%) had an unfavorable course of disease activity marked by worsening during 8 (20%) of the pregnancies or stable high disease activity during 5 (12%). The course of disease activity was more favorable for 24 (59%) pregnancies, in which it improved in 11 (27%) and stayed stable at a low disease level in 13 (32%). Four pregnancies (10%) had a mixed pattern of improvement followed by worsening.
The 1-year postpartum period during 40 pregnancies showed that stable or worsening symptoms were most common: 8 (20%) had improvement and 13 (32.5%) had stable low disease activity, while another 16 (4%) worsened and 3 (8%) had a mixed course of improvement followed by worsening.
After they controlled the results to account for various factors, the researchers found that pregnancy appeared to be especially beneficial for skin-related PsA symptoms. The likelihood of improved skin activity during pregnancy rose significantly (odds ratio, 7.7; 95% confidence interval, 1.8-23.5; P = .004) when compared with a matched period among controls, but this was no longer the case during the year after birth (OR, 0.4; 95% CI, 0.2-1.4; P = .60).
The likelihood of improved joint symptoms during pregnancy also rose, but not to a significant extent (OR, 2.1; 95% CI, 0.8-5.1; P = .10), and the effect on joints was not significant in the year after pregnancy (OR, 1.4; 95% CI, 0.5-3.4; P = .50).
There was a declining use of medications among the patients during pregnancy, particularly in the second and third trimesters, but two-thirds of the patients were treated with medications for PsA during this time, including NSAIDs (41%), disease-modifying antirheumatic drugs (35%), and biologic agents (26%).
The researchers speculated that hormonal changes during pregnancy may explain the improvement in skin activity. However, they noted that women with PsA who have multiple pregnancies don’t tend to have the same experiences each time: “Most of the women with more than one pregnancy had different joint disease course during their own different pregnancies and postpartum periods. Accordingly, this suggests that each woman needs specific evaluation and treatment adjustment during each pregnancy.”
The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. Dr. Polachek is supported by an educational grant from Janssen Canada.
Psoriatic arthritis disease activity tended to improve or stabilize during pregnancy and the first year after giving birth, even outpacing controls, in a small retrospective cohort study.
“The outcome of pregnancy in PsA [psoriatic arthritis] patients is excellent,” investigators from the University of Toronto Psoriatic Arthritis Program reported. They found that “arthritis activity has a favorable course during pregnancy in almost 60% of the pregnancies, while the skin disease shows a favorable course in close to 90% of the pregnancies.”
According to the researchers, led by Ari Polachek, MD, of the Centre for Prognosis Studies in the Rheumatic Diseases at Toronto Western Hospital, previous research has found that rheumatoid arthritis improves in most pregnant women with the condition but then worsens in the year after birth, while most patients with ankylosing spondylitis don’t get better or worse. Limited research suggests psoriasis tends to improve during pregnancy and then flares afterward.
For the new study, researchers tracked 29 pregnant PsA patients with 42 total pregnancies who had a mean age of about 34 years at the beginning of pregnancy and matched them with 67 control patients with PsA who were not pregnant and had an average age of about 35 years. They had all visited the University of Toronto Psoriatic Arthritis Clinic during 1990-2015 (Semin Arthritis Rheum. 2017 Jan 16. doi: 10.1016/j.semarthrit.2017.01.002).
Among the 41 pregnancies in women who began follow-up prior to pregnancy, 13 (32%) had an unfavorable course of disease activity marked by worsening during 8 (20%) of the pregnancies or stable high disease activity during 5 (12%). The course of disease activity was more favorable for 24 (59%) pregnancies, in which it improved in 11 (27%) and stayed stable at a low disease level in 13 (32%). Four pregnancies (10%) had a mixed pattern of improvement followed by worsening.
The 1-year postpartum period during 40 pregnancies showed that stable or worsening symptoms were most common: 8 (20%) had improvement and 13 (32.5%) had stable low disease activity, while another 16 (4%) worsened and 3 (8%) had a mixed course of improvement followed by worsening.
After they controlled the results to account for various factors, the researchers found that pregnancy appeared to be especially beneficial for skin-related PsA symptoms. The likelihood of improved skin activity during pregnancy rose significantly (odds ratio, 7.7; 95% confidence interval, 1.8-23.5; P = .004) when compared with a matched period among controls, but this was no longer the case during the year after birth (OR, 0.4; 95% CI, 0.2-1.4; P = .60).
The likelihood of improved joint symptoms during pregnancy also rose, but not to a significant extent (OR, 2.1; 95% CI, 0.8-5.1; P = .10), and the effect on joints was not significant in the year after pregnancy (OR, 1.4; 95% CI, 0.5-3.4; P = .50).
There was a declining use of medications among the patients during pregnancy, particularly in the second and third trimesters, but two-thirds of the patients were treated with medications for PsA during this time, including NSAIDs (41%), disease-modifying antirheumatic drugs (35%), and biologic agents (26%).
The researchers speculated that hormonal changes during pregnancy may explain the improvement in skin activity. However, they noted that women with PsA who have multiple pregnancies don’t tend to have the same experiences each time: “Most of the women with more than one pregnancy had different joint disease course during their own different pregnancies and postpartum periods. Accordingly, this suggests that each woman needs specific evaluation and treatment adjustment during each pregnancy.”
The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. Dr. Polachek is supported by an educational grant from Janssen Canada.
Key clinical point:
Major finding: PsA symptoms improved in 27% of pregnancies, stabilized at a low level in 32%, and worsened in 20%.
Data source: 29 pregnant PsA patients with 42 total pregnancies and 67 non-pregnant PsA patients.
Disclosures: The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. Dr. Polachek is supported by an educational grant from Janssen Canada.
Ohio progestogen program reduced early preterm births
A statewide progestogen promotion program that aimed to reduce early premature births in Ohio by 10% is exceeding its goals, thanks to a joint effort of maternity hospitals and clinics, Ohio’s Medicaid program, Medicaid insurers, and service agencies.
The organizations joined forces via the Ohio Perinatal Quality Collaborative (PQC) beginning in 2014, and by February 2016 a sustained reduction in singleton births before 32 weeks of gestation was evident. The reduction was particularly pronounced among women with a prior preterm birth, African American women, and women on Medicaid, with reductions of 20.5%, 20.3%, and 17.1%, respectively, according to Jay D. Iams, MD, the obstetrics lead for the collaborative and emeritus professor at Ohio State University; Mary S. Applegate, MD, medical director for the Ohio Department of Medicaid; and their colleagues.
What was the key driver of their success? A collaborative effort among local- and system-level organizations and individuals to overcome the numerous barriers to providing the preventive, highly effective progestogen treatments to at-risk women, according to Dr. Iams and Dr. Applegate.
“Ohio has one of the worst rates of infant mortality and a high rate of premature birth – especially very early premature birth [before 32 weeks],” Dr. Iams said in an interview.
Those very early births account for more than half of infants who die before their first birthday, so while 13% may seem like a small number, it has the potential to have a very large effect on long-term health and infant mortality, he said.
The Ohio program was developed in the wake of practice guidelines from the Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists, both issued in 2012, on the use of progestogens to reduce the incidence of preterm birth (Am J Obstet Gynecol 2012;206:376-86 and Obstet Gynecol 2012;120:964-73).
Large, high-quality, randomized placebo-controlled trials supported the use of 17-alpha hydroxyprogesterone caproate (17-p) injections or progesterone administered vaginally, and the Ohio Department of Medicaid and Ohio Department of Health asked the Ohio PQC – a volunteer network of stakeholders dedicated to improving perinatal health outcomes – to design a statewide quality improvement project to promote progestogen prescribing for eligible women.
To facilitate identification and management of women at risk for preterm birth, clinicians were asked to notify the Ohio Medicaid agency when a patient became pregnant so that a care manager could be assigned to help remove barriers to care.
“It turned out that piece of it was key,” she said. “It was the communication between these two, and then just dealing with whatever the issues were that actually made the difference.”
Care managers helped the patients navigate the system by notifying the county to make sure they didn’t “fall off Medicaid,” by addressing transportation issues to ensure patients could get to their weekly treatment visits, and by addressing cultural issues, for instance.
“It never really occurred to clinicians that Medicaid could actually be helpful in finding women and actually doing the right thing for them,” Dr. Applegate said, explaining that most only thought of Medicaid as “after the fact ... the doctors do what they need to and afterward we pay claims.”
“So this was kind of a new concept to them,” she added.
In fact, a quality improvement plan was structured on the managed care plan side, just like one was structured on the clinical side, she said. “In essence we have these parallel systems that were actually connecting, identifying barriers as we went,” Dr. Applegate said.
In the article in Obstetrics & Gynecology, the investigators describe the quality improvement processes, including training, evidence reviews, and strategy sharing. Steps toward efficient identification of eligible patients and prescription of progestogens were developed, and participating sites were encouraged to follow them.
At the system level, efforts focused on maintaining the patient’s Medicaid coverage, expanding eligibility for Medicaid, and streamlining forms and processes to improve efficiency and improve data collection.
The effects of these cumulative efforts emerged over time, with the drop in early premature births becoming apparent about 16-18 months after the project started. The investigators reviewed other possible causes for the decrease, such as an increase in the rate of cervical cerclage, but confirmed that the change was likely the result of the progestogen promotion program, Dr. Iams said.
In all, 2,562 women were eligible for progestogen at participating clinics between Jan. 1, 2014, and Nov. 30, 2015. Most (93%) were eligible because of a prior preterm birth, and the remainder had a short cervix on ultrasound. A progestogen was prescribed at or before 20 6/7 weeks of gestation in 64%, and at or before 24 6/7 weeks gestation in 72%. Injections were prescribed in 65%, and vaginal preparations in 30%; 5% were prescribed both or had no documentation of the formulation.
The progestogen program had no effect on the overall rate of births before 37 weeks. “So we can’t say that we changed the prematurity rate, but we changed the rate of births that are most likely to result in infant death and we were pretty excited about that,” Dr. Iams said.
Next steps for the program include expansion to rural areas and development of an electronic notification system to further streamline communication between the various players (pharmacies, insurance companies, Medicaid, etc.). Dr. Applegate said she also hopes to harness the lessons of this program for use in other high-risk scenarios, such as pregnancies complicated by substance abuse.
As for whether other states will follow Ohio’s lead, Dr. Iams said almost all the states are involved in quality improvement efforts, including several with programs similar to Ohio’s.
In fact, the Centers for Disease Control and Prevention is currently providing support to PQCs in California, Illinois, Massachusetts, North Carolina, and New York, in addition to the Ohio PQC, according to Zsakeba Henderson, MD, a medical officer on the CDC division of reproductive health in Atlanta.
“CDC has developed a resource guide to help develop and advance the work of state PQCs, and in collaboration with March of Dimes has spearheaded the development and launch of the National Network of Perinatal Quality Collaboratives,” she said. “This network is a consultative resource for state PQCs, with a mission is to support the development and enhance the ability of state perinatal quality collaboratives to make measurable improvements in statewide maternal and infant health care and health outcomes.”
Dr. Applegate stressed the importance of collaboration in achieving results.
“I think the message is you can’t do it in a silo. It really has taken this collaborative and fairly comprehensive approach to understand not only how complex the system is, but how complicated people’s lives are. You just have to hang in there over lots and lots of weeks to get the outcome you want,” she said, adding that the effort is well worth it.
“These are babies that are born weighing less than a pound and a half. When we’re helping them be born closer to term that changes the next 60 years of their life,” she said. “It totally changes not just that baby’s life, but the hardship that comes to that family as well, so the impact is actually huge.”
A statewide progestogen promotion program that aimed to reduce early premature births in Ohio by 10% is exceeding its goals, thanks to a joint effort of maternity hospitals and clinics, Ohio’s Medicaid program, Medicaid insurers, and service agencies.
The organizations joined forces via the Ohio Perinatal Quality Collaborative (PQC) beginning in 2014, and by February 2016 a sustained reduction in singleton births before 32 weeks of gestation was evident. The reduction was particularly pronounced among women with a prior preterm birth, African American women, and women on Medicaid, with reductions of 20.5%, 20.3%, and 17.1%, respectively, according to Jay D. Iams, MD, the obstetrics lead for the collaborative and emeritus professor at Ohio State University; Mary S. Applegate, MD, medical director for the Ohio Department of Medicaid; and their colleagues.
What was the key driver of their success? A collaborative effort among local- and system-level organizations and individuals to overcome the numerous barriers to providing the preventive, highly effective progestogen treatments to at-risk women, according to Dr. Iams and Dr. Applegate.
“Ohio has one of the worst rates of infant mortality and a high rate of premature birth – especially very early premature birth [before 32 weeks],” Dr. Iams said in an interview.
Those very early births account for more than half of infants who die before their first birthday, so while 13% may seem like a small number, it has the potential to have a very large effect on long-term health and infant mortality, he said.
The Ohio program was developed in the wake of practice guidelines from the Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists, both issued in 2012, on the use of progestogens to reduce the incidence of preterm birth (Am J Obstet Gynecol 2012;206:376-86 and Obstet Gynecol 2012;120:964-73).
Large, high-quality, randomized placebo-controlled trials supported the use of 17-alpha hydroxyprogesterone caproate (17-p) injections or progesterone administered vaginally, and the Ohio Department of Medicaid and Ohio Department of Health asked the Ohio PQC – a volunteer network of stakeholders dedicated to improving perinatal health outcomes – to design a statewide quality improvement project to promote progestogen prescribing for eligible women.
To facilitate identification and management of women at risk for preterm birth, clinicians were asked to notify the Ohio Medicaid agency when a patient became pregnant so that a care manager could be assigned to help remove barriers to care.
“It turned out that piece of it was key,” she said. “It was the communication between these two, and then just dealing with whatever the issues were that actually made the difference.”
Care managers helped the patients navigate the system by notifying the county to make sure they didn’t “fall off Medicaid,” by addressing transportation issues to ensure patients could get to their weekly treatment visits, and by addressing cultural issues, for instance.
“It never really occurred to clinicians that Medicaid could actually be helpful in finding women and actually doing the right thing for them,” Dr. Applegate said, explaining that most only thought of Medicaid as “after the fact ... the doctors do what they need to and afterward we pay claims.”
“So this was kind of a new concept to them,” she added.
In fact, a quality improvement plan was structured on the managed care plan side, just like one was structured on the clinical side, she said. “In essence we have these parallel systems that were actually connecting, identifying barriers as we went,” Dr. Applegate said.
In the article in Obstetrics & Gynecology, the investigators describe the quality improvement processes, including training, evidence reviews, and strategy sharing. Steps toward efficient identification of eligible patients and prescription of progestogens were developed, and participating sites were encouraged to follow them.
At the system level, efforts focused on maintaining the patient’s Medicaid coverage, expanding eligibility for Medicaid, and streamlining forms and processes to improve efficiency and improve data collection.
The effects of these cumulative efforts emerged over time, with the drop in early premature births becoming apparent about 16-18 months after the project started. The investigators reviewed other possible causes for the decrease, such as an increase in the rate of cervical cerclage, but confirmed that the change was likely the result of the progestogen promotion program, Dr. Iams said.
In all, 2,562 women were eligible for progestogen at participating clinics between Jan. 1, 2014, and Nov. 30, 2015. Most (93%) were eligible because of a prior preterm birth, and the remainder had a short cervix on ultrasound. A progestogen was prescribed at or before 20 6/7 weeks of gestation in 64%, and at or before 24 6/7 weeks gestation in 72%. Injections were prescribed in 65%, and vaginal preparations in 30%; 5% were prescribed both or had no documentation of the formulation.
The progestogen program had no effect on the overall rate of births before 37 weeks. “So we can’t say that we changed the prematurity rate, but we changed the rate of births that are most likely to result in infant death and we were pretty excited about that,” Dr. Iams said.
Next steps for the program include expansion to rural areas and development of an electronic notification system to further streamline communication between the various players (pharmacies, insurance companies, Medicaid, etc.). Dr. Applegate said she also hopes to harness the lessons of this program for use in other high-risk scenarios, such as pregnancies complicated by substance abuse.
As for whether other states will follow Ohio’s lead, Dr. Iams said almost all the states are involved in quality improvement efforts, including several with programs similar to Ohio’s.
In fact, the Centers for Disease Control and Prevention is currently providing support to PQCs in California, Illinois, Massachusetts, North Carolina, and New York, in addition to the Ohio PQC, according to Zsakeba Henderson, MD, a medical officer on the CDC division of reproductive health in Atlanta.
“CDC has developed a resource guide to help develop and advance the work of state PQCs, and in collaboration with March of Dimes has spearheaded the development and launch of the National Network of Perinatal Quality Collaboratives,” she said. “This network is a consultative resource for state PQCs, with a mission is to support the development and enhance the ability of state perinatal quality collaboratives to make measurable improvements in statewide maternal and infant health care and health outcomes.”
Dr. Applegate stressed the importance of collaboration in achieving results.
“I think the message is you can’t do it in a silo. It really has taken this collaborative and fairly comprehensive approach to understand not only how complex the system is, but how complicated people’s lives are. You just have to hang in there over lots and lots of weeks to get the outcome you want,” she said, adding that the effort is well worth it.
“These are babies that are born weighing less than a pound and a half. When we’re helping them be born closer to term that changes the next 60 years of their life,” she said. “It totally changes not just that baby’s life, but the hardship that comes to that family as well, so the impact is actually huge.”
A statewide progestogen promotion program that aimed to reduce early premature births in Ohio by 10% is exceeding its goals, thanks to a joint effort of maternity hospitals and clinics, Ohio’s Medicaid program, Medicaid insurers, and service agencies.
The organizations joined forces via the Ohio Perinatal Quality Collaborative (PQC) beginning in 2014, and by February 2016 a sustained reduction in singleton births before 32 weeks of gestation was evident. The reduction was particularly pronounced among women with a prior preterm birth, African American women, and women on Medicaid, with reductions of 20.5%, 20.3%, and 17.1%, respectively, according to Jay D. Iams, MD, the obstetrics lead for the collaborative and emeritus professor at Ohio State University; Mary S. Applegate, MD, medical director for the Ohio Department of Medicaid; and their colleagues.
What was the key driver of their success? A collaborative effort among local- and system-level organizations and individuals to overcome the numerous barriers to providing the preventive, highly effective progestogen treatments to at-risk women, according to Dr. Iams and Dr. Applegate.
“Ohio has one of the worst rates of infant mortality and a high rate of premature birth – especially very early premature birth [before 32 weeks],” Dr. Iams said in an interview.
Those very early births account for more than half of infants who die before their first birthday, so while 13% may seem like a small number, it has the potential to have a very large effect on long-term health and infant mortality, he said.
The Ohio program was developed in the wake of practice guidelines from the Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists, both issued in 2012, on the use of progestogens to reduce the incidence of preterm birth (Am J Obstet Gynecol 2012;206:376-86 and Obstet Gynecol 2012;120:964-73).
Large, high-quality, randomized placebo-controlled trials supported the use of 17-alpha hydroxyprogesterone caproate (17-p) injections or progesterone administered vaginally, and the Ohio Department of Medicaid and Ohio Department of Health asked the Ohio PQC – a volunteer network of stakeholders dedicated to improving perinatal health outcomes – to design a statewide quality improvement project to promote progestogen prescribing for eligible women.
To facilitate identification and management of women at risk for preterm birth, clinicians were asked to notify the Ohio Medicaid agency when a patient became pregnant so that a care manager could be assigned to help remove barriers to care.
“It turned out that piece of it was key,” she said. “It was the communication between these two, and then just dealing with whatever the issues were that actually made the difference.”
Care managers helped the patients navigate the system by notifying the county to make sure they didn’t “fall off Medicaid,” by addressing transportation issues to ensure patients could get to their weekly treatment visits, and by addressing cultural issues, for instance.
“It never really occurred to clinicians that Medicaid could actually be helpful in finding women and actually doing the right thing for them,” Dr. Applegate said, explaining that most only thought of Medicaid as “after the fact ... the doctors do what they need to and afterward we pay claims.”
“So this was kind of a new concept to them,” she added.
In fact, a quality improvement plan was structured on the managed care plan side, just like one was structured on the clinical side, she said. “In essence we have these parallel systems that were actually connecting, identifying barriers as we went,” Dr. Applegate said.
In the article in Obstetrics & Gynecology, the investigators describe the quality improvement processes, including training, evidence reviews, and strategy sharing. Steps toward efficient identification of eligible patients and prescription of progestogens were developed, and participating sites were encouraged to follow them.
At the system level, efforts focused on maintaining the patient’s Medicaid coverage, expanding eligibility for Medicaid, and streamlining forms and processes to improve efficiency and improve data collection.
The effects of these cumulative efforts emerged over time, with the drop in early premature births becoming apparent about 16-18 months after the project started. The investigators reviewed other possible causes for the decrease, such as an increase in the rate of cervical cerclage, but confirmed that the change was likely the result of the progestogen promotion program, Dr. Iams said.
In all, 2,562 women were eligible for progestogen at participating clinics between Jan. 1, 2014, and Nov. 30, 2015. Most (93%) were eligible because of a prior preterm birth, and the remainder had a short cervix on ultrasound. A progestogen was prescribed at or before 20 6/7 weeks of gestation in 64%, and at or before 24 6/7 weeks gestation in 72%. Injections were prescribed in 65%, and vaginal preparations in 30%; 5% were prescribed both or had no documentation of the formulation.
The progestogen program had no effect on the overall rate of births before 37 weeks. “So we can’t say that we changed the prematurity rate, but we changed the rate of births that are most likely to result in infant death and we were pretty excited about that,” Dr. Iams said.
Next steps for the program include expansion to rural areas and development of an electronic notification system to further streamline communication between the various players (pharmacies, insurance companies, Medicaid, etc.). Dr. Applegate said she also hopes to harness the lessons of this program for use in other high-risk scenarios, such as pregnancies complicated by substance abuse.
As for whether other states will follow Ohio’s lead, Dr. Iams said almost all the states are involved in quality improvement efforts, including several with programs similar to Ohio’s.
In fact, the Centers for Disease Control and Prevention is currently providing support to PQCs in California, Illinois, Massachusetts, North Carolina, and New York, in addition to the Ohio PQC, according to Zsakeba Henderson, MD, a medical officer on the CDC division of reproductive health in Atlanta.
“CDC has developed a resource guide to help develop and advance the work of state PQCs, and in collaboration with March of Dimes has spearheaded the development and launch of the National Network of Perinatal Quality Collaboratives,” she said. “This network is a consultative resource for state PQCs, with a mission is to support the development and enhance the ability of state perinatal quality collaboratives to make measurable improvements in statewide maternal and infant health care and health outcomes.”
Dr. Applegate stressed the importance of collaboration in achieving results.
“I think the message is you can’t do it in a silo. It really has taken this collaborative and fairly comprehensive approach to understand not only how complex the system is, but how complicated people’s lives are. You just have to hang in there over lots and lots of weeks to get the outcome you want,” she said, adding that the effort is well worth it.
“These are babies that are born weighing less than a pound and a half. When we’re helping them be born closer to term that changes the next 60 years of their life,” she said. “It totally changes not just that baby’s life, but the hardship that comes to that family as well, so the impact is actually huge.”
Zika virus slowdown continues
Zika activity is slowing as winter progresses, with less than a hundred new cases of pregnant women with laboratory evidence of infection reported over the 2 weeks ending Jan. 10, according to data from the Centers for Disease Control and Prevention.
The most recent CDC data show that, for the first time since early August, the majority of new cases of Zika infection among pregnant women were reported in the 50 states and the District of Columbia, compared with the U.S. territories. There were a total of 98 new cases, with 55 reported in the states and 43 in the U.S. territories.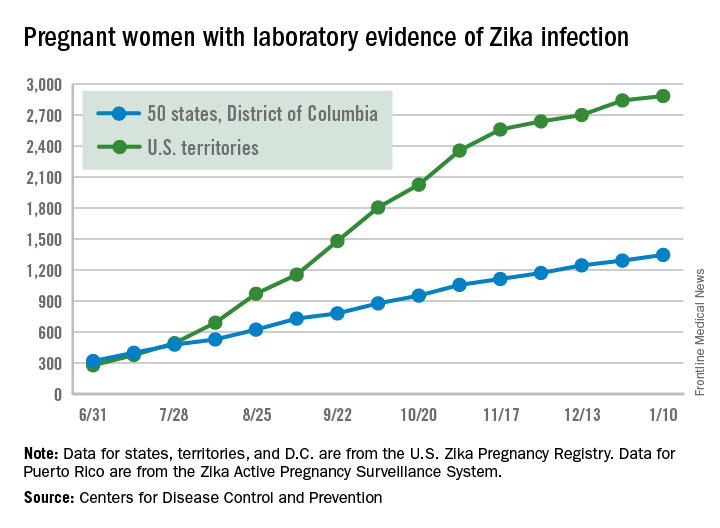
The total number of Zika-infected pregnant women in the United States is now 4,232 for 2016-2017. There have been 2,885 cases in the territories and 1,347 cases reported in the states/D.C. Among the cases in the states/D.C., 940 pregnancies have been completed, with Zika-related birth defects seen in 37 live-born infants and five pregnancy losses, the CDC said. The CDC is no longer reporting adverse pregnancy outcomes for the territories because Puerto Rico is not using the same inclusion criteria.
Zika cases among all Americans are still being reported weekly by the CDC, and the increase there has slowed as well: Total cases were up by 146 for the week ending Jan. 18, compared with 294 and 205 for each of the previous 2 weeks, according to CDC reports.
Zika-related birth defects reported by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Zika activity is slowing as winter progresses, with less than a hundred new cases of pregnant women with laboratory evidence of infection reported over the 2 weeks ending Jan. 10, according to data from the Centers for Disease Control and Prevention.
The most recent CDC data show that, for the first time since early August, the majority of new cases of Zika infection among pregnant women were reported in the 50 states and the District of Columbia, compared with the U.S. territories. There were a total of 98 new cases, with 55 reported in the states and 43 in the U.S. territories.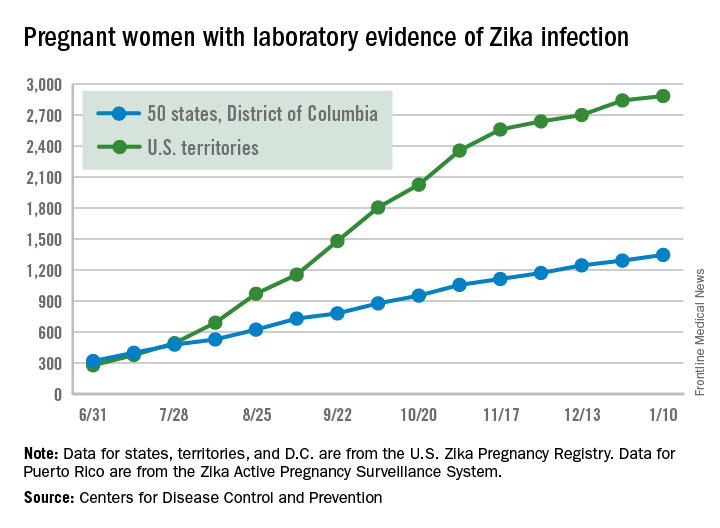
The total number of Zika-infected pregnant women in the United States is now 4,232 for 2016-2017. There have been 2,885 cases in the territories and 1,347 cases reported in the states/D.C. Among the cases in the states/D.C., 940 pregnancies have been completed, with Zika-related birth defects seen in 37 live-born infants and five pregnancy losses, the CDC said. The CDC is no longer reporting adverse pregnancy outcomes for the territories because Puerto Rico is not using the same inclusion criteria.
Zika cases among all Americans are still being reported weekly by the CDC, and the increase there has slowed as well: Total cases were up by 146 for the week ending Jan. 18, compared with 294 and 205 for each of the previous 2 weeks, according to CDC reports.
Zika-related birth defects reported by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Zika activity is slowing as winter progresses, with less than a hundred new cases of pregnant women with laboratory evidence of infection reported over the 2 weeks ending Jan. 10, according to data from the Centers for Disease Control and Prevention.
The most recent CDC data show that, for the first time since early August, the majority of new cases of Zika infection among pregnant women were reported in the 50 states and the District of Columbia, compared with the U.S. territories. There were a total of 98 new cases, with 55 reported in the states and 43 in the U.S. territories.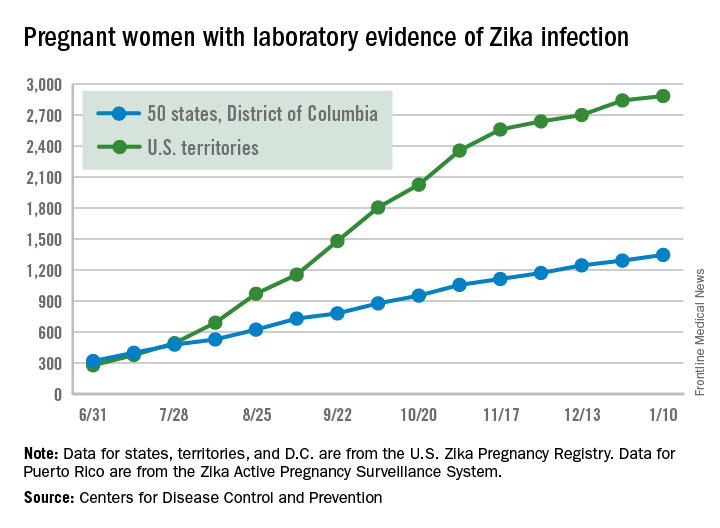
The total number of Zika-infected pregnant women in the United States is now 4,232 for 2016-2017. There have been 2,885 cases in the territories and 1,347 cases reported in the states/D.C. Among the cases in the states/D.C., 940 pregnancies have been completed, with Zika-related birth defects seen in 37 live-born infants and five pregnancy losses, the CDC said. The CDC is no longer reporting adverse pregnancy outcomes for the territories because Puerto Rico is not using the same inclusion criteria.
Zika cases among all Americans are still being reported weekly by the CDC, and the increase there has slowed as well: Total cases were up by 146 for the week ending Jan. 18, compared with 294 and 205 for each of the previous 2 weeks, according to CDC reports.
Zika-related birth defects reported by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.




















