User login
Stand up for research benefiting our patients, and more
Focus on decreasing unintended pregnanciesI found the letters in response to Dr. Barbieri’s Editorial on inadequate contraception to be much overwrought. Dr. Will’s suggestion to have “automatic contraception … for all reproductive-age women including ‘children’ who are … menstruating” is excessive. Shouldn’t parents have the final decision making in their minor children’s health care?
An anonymous clinician ex-presses frustration with a Catholichealth care system for not allowing prescription of contraceptives, which does actually stay true to the religious beliefs of the institution, and proposes decreased reimbursements to these facilities across the board as a form of financial punishment for these practices. Not only would that be illegal and unconstitutional but it also demonstrates a lack of understanding of our First Amendment protections.
Overall, these letters and Dr. Barbieri’s response show a very narrow understanding of the issues involved. I think we can and should be focused on decreasing unintended pregnancies while also respecting the rights of all without resorting to Draconian and totalitarian solutions.
Myles Dotto, MD
Oradell, New Jersey
Dr. Barbieri respondsI share Dr. Dotto’s concern that government mandates regarding health care are potentially very dangerous. It is better for communities of clinicians and patients to develop optimal approaches to health care, without government interference.
“THE CRUSHING OF INNOVATION FOR TREATING FEMALE PELVIC FLOOR DISORDERS: A STORY OF ‘LEAD OR BE LED’”ANDREW CASSIDENTI, MD (GUEST EDITORIAL; APRIL 2016)Stand up for research benefiting our patientsI salute Dr. Cassidenti’s courage to call surgeons and the respective professional organizations to step up to defend the research and expose inappropriate expert testimony. We should be ashamed to be scattered like dogs because of fear and lack of courage to be advocates for what is in the best interest of our patients. Please continue the campaign to encourage physicians and surgeons to stand up.
Cleve Waters, MD
Chattanooga, Tennessee
Caving to class action litigation is a mistakeIn his Guest Editorial Dr. Cassidenti clarifies the importance of looking forward regarding mesh devices for pelvic organ prolapse (POP) treatment. As an advocate for women with POP and Founder/Executive Director of the Association for Pelvic Organ Prolapse Support—a US-based 501(c)(3)advocacy agency with global arms focused on generating awareness of POP and providing guidance and support to women navigating POP treatment—I found Endo International’s decision to close its Astora Women’s Health division extremely unsettling.
The nature of medicine is to continually advance, and that includes learning from experience and recognizing paths to evolution. Caving to class action litigation is a mistake. Research findings frequently indicate that up to half of the female population will experience POP and/or comorbid conditions.1 It is imperative that health care, industry, research, academia, policy, and advocacy agencies continue to shine a light on this much needed field in women’s health.
Sherrie Palm
Milwaukee, Wisconsin
Reference
- Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–1790.
Avoidance: the greatest tool to address shoulder dystociaAlthough avoiding endometrial injury at cesarean delivery, including the possibility of later pathologic implantation, can be attained with vaginal delivery, vaginal birth at all cost leads to a dangerous situation. The emergency environment of shoulder dystocia is not a preferable or safer stratagem.
It is granted that shoulder dystocia will happen at some point but avoidance, by employing cesarean delivery when it is indicated, is the greatest tool for addressing this very dangerous problem.
J. Michael Arnold, MD
Oconto Falls, Wisconsin
Another suggestion for shoulder dystociaMy senior partner taught me a technique that works well, although I do not know its name. After suprapubic and McRoberts maneuvers fail and the shoulders do not deliver with gentle downward guidance in one direction, I rotate the head 180° and try again. Usually this works. I have taught this technique to several midwives, and they swear by it.
Annette Fineberg, MD
Davis, California
Dr. Barbieri respondsI thank Drs. Arnold and Fineberg for sharing their perspective and experience with our readers. Dr. Arnold notes that recommending cesarean delivery in high-risk situations such as cases in which the mother has diabetes and the fetus is macrosomic would surely reduce the frequency of shoulder dystocia. I respect Dr. Fineberg’s recommendation, based on extensive clinical experience, that by rotating the fetal head the shoulder dystocia may be resolved. My concern with this technique is that the torque transmitted to the neck might cause fetal damage. I think that rotating the shoulders (Rubin or Wood maneuver) would be less likely to result in fetal injury.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Focus on decreasing unintended pregnanciesI found the letters in response to Dr. Barbieri’s Editorial on inadequate contraception to be much overwrought. Dr. Will’s suggestion to have “automatic contraception … for all reproductive-age women including ‘children’ who are … menstruating” is excessive. Shouldn’t parents have the final decision making in their minor children’s health care?
An anonymous clinician ex-presses frustration with a Catholichealth care system for not allowing prescription of contraceptives, which does actually stay true to the religious beliefs of the institution, and proposes decreased reimbursements to these facilities across the board as a form of financial punishment for these practices. Not only would that be illegal and unconstitutional but it also demonstrates a lack of understanding of our First Amendment protections.
Overall, these letters and Dr. Barbieri’s response show a very narrow understanding of the issues involved. I think we can and should be focused on decreasing unintended pregnancies while also respecting the rights of all without resorting to Draconian and totalitarian solutions.
Myles Dotto, MD
Oradell, New Jersey
Dr. Barbieri respondsI share Dr. Dotto’s concern that government mandates regarding health care are potentially very dangerous. It is better for communities of clinicians and patients to develop optimal approaches to health care, without government interference.
“THE CRUSHING OF INNOVATION FOR TREATING FEMALE PELVIC FLOOR DISORDERS: A STORY OF ‘LEAD OR BE LED’”ANDREW CASSIDENTI, MD (GUEST EDITORIAL; APRIL 2016)Stand up for research benefiting our patientsI salute Dr. Cassidenti’s courage to call surgeons and the respective professional organizations to step up to defend the research and expose inappropriate expert testimony. We should be ashamed to be scattered like dogs because of fear and lack of courage to be advocates for what is in the best interest of our patients. Please continue the campaign to encourage physicians and surgeons to stand up.
Cleve Waters, MD
Chattanooga, Tennessee
Caving to class action litigation is a mistakeIn his Guest Editorial Dr. Cassidenti clarifies the importance of looking forward regarding mesh devices for pelvic organ prolapse (POP) treatment. As an advocate for women with POP and Founder/Executive Director of the Association for Pelvic Organ Prolapse Support—a US-based 501(c)(3)advocacy agency with global arms focused on generating awareness of POP and providing guidance and support to women navigating POP treatment—I found Endo International’s decision to close its Astora Women’s Health division extremely unsettling.
The nature of medicine is to continually advance, and that includes learning from experience and recognizing paths to evolution. Caving to class action litigation is a mistake. Research findings frequently indicate that up to half of the female population will experience POP and/or comorbid conditions.1 It is imperative that health care, industry, research, academia, policy, and advocacy agencies continue to shine a light on this much needed field in women’s health.
Sherrie Palm
Milwaukee, Wisconsin
Reference
- Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–1790.
Avoidance: the greatest tool to address shoulder dystociaAlthough avoiding endometrial injury at cesarean delivery, including the possibility of later pathologic implantation, can be attained with vaginal delivery, vaginal birth at all cost leads to a dangerous situation. The emergency environment of shoulder dystocia is not a preferable or safer stratagem.
It is granted that shoulder dystocia will happen at some point but avoidance, by employing cesarean delivery when it is indicated, is the greatest tool for addressing this very dangerous problem.
J. Michael Arnold, MD
Oconto Falls, Wisconsin
Another suggestion for shoulder dystociaMy senior partner taught me a technique that works well, although I do not know its name. After suprapubic and McRoberts maneuvers fail and the shoulders do not deliver with gentle downward guidance in one direction, I rotate the head 180° and try again. Usually this works. I have taught this technique to several midwives, and they swear by it.
Annette Fineberg, MD
Davis, California
Dr. Barbieri respondsI thank Drs. Arnold and Fineberg for sharing their perspective and experience with our readers. Dr. Arnold notes that recommending cesarean delivery in high-risk situations such as cases in which the mother has diabetes and the fetus is macrosomic would surely reduce the frequency of shoulder dystocia. I respect Dr. Fineberg’s recommendation, based on extensive clinical experience, that by rotating the fetal head the shoulder dystocia may be resolved. My concern with this technique is that the torque transmitted to the neck might cause fetal damage. I think that rotating the shoulders (Rubin or Wood maneuver) would be less likely to result in fetal injury.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Focus on decreasing unintended pregnanciesI found the letters in response to Dr. Barbieri’s Editorial on inadequate contraception to be much overwrought. Dr. Will’s suggestion to have “automatic contraception … for all reproductive-age women including ‘children’ who are … menstruating” is excessive. Shouldn’t parents have the final decision making in their minor children’s health care?
An anonymous clinician ex-presses frustration with a Catholichealth care system for not allowing prescription of contraceptives, which does actually stay true to the religious beliefs of the institution, and proposes decreased reimbursements to these facilities across the board as a form of financial punishment for these practices. Not only would that be illegal and unconstitutional but it also demonstrates a lack of understanding of our First Amendment protections.
Overall, these letters and Dr. Barbieri’s response show a very narrow understanding of the issues involved. I think we can and should be focused on decreasing unintended pregnancies while also respecting the rights of all without resorting to Draconian and totalitarian solutions.
Myles Dotto, MD
Oradell, New Jersey
Dr. Barbieri respondsI share Dr. Dotto’s concern that government mandates regarding health care are potentially very dangerous. It is better for communities of clinicians and patients to develop optimal approaches to health care, without government interference.
“THE CRUSHING OF INNOVATION FOR TREATING FEMALE PELVIC FLOOR DISORDERS: A STORY OF ‘LEAD OR BE LED’”ANDREW CASSIDENTI, MD (GUEST EDITORIAL; APRIL 2016)Stand up for research benefiting our patientsI salute Dr. Cassidenti’s courage to call surgeons and the respective professional organizations to step up to defend the research and expose inappropriate expert testimony. We should be ashamed to be scattered like dogs because of fear and lack of courage to be advocates for what is in the best interest of our patients. Please continue the campaign to encourage physicians and surgeons to stand up.
Cleve Waters, MD
Chattanooga, Tennessee
Caving to class action litigation is a mistakeIn his Guest Editorial Dr. Cassidenti clarifies the importance of looking forward regarding mesh devices for pelvic organ prolapse (POP) treatment. As an advocate for women with POP and Founder/Executive Director of the Association for Pelvic Organ Prolapse Support—a US-based 501(c)(3)advocacy agency with global arms focused on generating awareness of POP and providing guidance and support to women navigating POP treatment—I found Endo International’s decision to close its Astora Women’s Health division extremely unsettling.
The nature of medicine is to continually advance, and that includes learning from experience and recognizing paths to evolution. Caving to class action litigation is a mistake. Research findings frequently indicate that up to half of the female population will experience POP and/or comorbid conditions.1 It is imperative that health care, industry, research, academia, policy, and advocacy agencies continue to shine a light on this much needed field in women’s health.
Sherrie Palm
Milwaukee, Wisconsin
Reference
- Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–1790.
Avoidance: the greatest tool to address shoulder dystociaAlthough avoiding endometrial injury at cesarean delivery, including the possibility of later pathologic implantation, can be attained with vaginal delivery, vaginal birth at all cost leads to a dangerous situation. The emergency environment of shoulder dystocia is not a preferable or safer stratagem.
It is granted that shoulder dystocia will happen at some point but avoidance, by employing cesarean delivery when it is indicated, is the greatest tool for addressing this very dangerous problem.
J. Michael Arnold, MD
Oconto Falls, Wisconsin
Another suggestion for shoulder dystociaMy senior partner taught me a technique that works well, although I do not know its name. After suprapubic and McRoberts maneuvers fail and the shoulders do not deliver with gentle downward guidance in one direction, I rotate the head 180° and try again. Usually this works. I have taught this technique to several midwives, and they swear by it.
Annette Fineberg, MD
Davis, California
Dr. Barbieri respondsI thank Drs. Arnold and Fineberg for sharing their perspective and experience with our readers. Dr. Arnold notes that recommending cesarean delivery in high-risk situations such as cases in which the mother has diabetes and the fetus is macrosomic would surely reduce the frequency of shoulder dystocia. I respect Dr. Fineberg’s recommendation, based on extensive clinical experience, that by rotating the fetal head the shoulder dystocia may be resolved. My concern with this technique is that the torque transmitted to the neck might cause fetal damage. I think that rotating the shoulders (Rubin or Wood maneuver) would be less likely to result in fetal injury.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Examining the fetal origins of obesity
The figures and trends behind the obesity epidemic are alarming: More than one-third of all adults in the United States are obese, as are 34% of women aged 20-39, and 17% of youth aged 2-19, according to data for 2011-2014 from the National Health and Nutrition Examination Survey.
In our ob.gyn. practices, many of us have witnessed the significant climb in national obesity rates over the past several decades. We’ve seen a continued increase in the prevalence of obesity among childbearing women, and a steady increase in the incidence of high-birth-weight babies. The percentage of women weighing 200 pounds has more than doubled since 1980, and up to 3-4 times as many children and teens in various age subsets are obese today as in the 1970s.
The obesity epidemic is often attributed to a high-fat and/or calorie-dense diet and decreased activity levels. However, this is only part of the picture. There has been growing recognition in recent years that obesity may be programmed by the in utero and newborn environment, particularly as it relates to nutritional permutations. We now have evidence, in fact, that developmental programming is likely a primary cause of the obesity epidemic.
Exposure to maternal obesity and being born with a low birth weight – especially a low birth weight paired with rapid catch-up growth – are both associated with a significantly increased risk of childhood and adult obesity.
Research has demonstrated that newborns may be programmed, in both of these scenarios, with an increased appetite and a predisposition to storing calories as fat. In addition, data are accumulating that exposure to bisphenol A and other endocrine-disruptive chemicals, other environmental toxins, and corticosteroids may exert similar programming effects.
This window into the origins of obesity has significant implications for the practice of ob.gyn., where we have the opportunity to address the programming effects of the in utero and early life environment. Most importantly, we must counsel women before pregnancy about the importance of losing weight, guide them during pregnancy to achieve optimal pregnancy nutrition and weight gain, and prepare them to adopt optimal newborn feeding strategies that will guard against overconsumption.
Programming of obesity
The current obesity epidemic is only minimally due to genetics. Although select genetic mutations may be associated with obesity, these mutations account for an exceedingly small proportion of the obese population. Instead, much of the obesity epidemic involves epigenetic change – in this case, largely epigenetic deregulation of gene expression – and more broadly what we call gestational, or developmental, programming.
Developmental programming is a process by which a stress or stimulus at a critical or sensitive period of development has long-term effects. The major part of the developmental process pertaining to cell division occurs during intrauterine life; more than 90% of the cell divisions necessary to make an adult human occur before birth. Although there are important effects of the early newborn period, developmental programming is therefore largely gestational programming. Depending on when an in utero stress or perturbation occurs, it may permanently change cell number and/or cell differentiation, organ structure, metabolic set points, and gene expression.
The late physician Dr. David Barker got us thinking about in utero programming when he demonstrated an association between low birth weight, rapid weight gain in early life, and adult cardiovascular mortality. His theory about how nutrition and growth before birth may affect cardiovascular health later on, as well as other adult chronic diseases and conditions, became known as the Barker Hypothesis.
Many studies, both animal research and human epidemiological studies, have since confirmed and expanded our understanding of this phenomena. Research has demonstrated associations, for instance, between low birth weight and later risks of insulin resistance, diabetes, fatty liver, and the often-underlying metabolic syndrome.
Obesity is also central to the development of the metabolic syndrome, and we now have irrefutable evidence to show that low birth weight infants have a higher risk of obesity than do normal weight infants. We also know, as Dr. Barker and his colleagues had surmised, that the greatest risks occur when there is rapid catch-up growth of low-birth-weight infants in the early years of life.
Moreover, we now understand that maternal obesity has programming effects that are similar to those of an in utero environment of undernutrition and growth restriction. In the past several decades, the marked increase in maternal obesity has resulted in this programming process having an ever-increasing impact.
Both animal and human studies have shown that infants born to obese mothers have the same increased risks for adult chronic disease – including the risk of becoming obese – as those of low birth weight infants. This increased risk is often, but not always, associated with high birth weight, and it is independent of whether the mother has gestational diabetes mellitus (GDM). Having a high birth weight is more likely in the setting of maternal obesity and itself raises the risk of eventual obesity (as does GDM), but an infant’s exposure to maternal obesity in and of itself is a risk factor.
The mechanisms
The programming mechanisms that predispose offspring to obesity are similar in infants of obese mothers and intrauterine growth restricted newborns, though they involve different epigenetic signals. Both involve dysregulation of appetite/satiety and of adipogenesis.
Appetite is primarily controlled by a complex circuit of neurons in the hypothalamus of the brain called the hypothalamic arcuate nucleus. Some neurons are orexigenic and stimulate or increase appetite, while others are anorexigenic and suppress appetite by promoting satiety.
During fetal development, hypothalamic neural stem cells proliferate and differentiate into various cell types. Neurons destined for the arcuate nucleus then differentiate into these so-called appetite neurons and satiety neurons. Though there is continued neural development and maturation during newborn life, hypothalamic control of appetite and satiety is largely set during this period.
Differentiation to appetite or satiety neurons is regulated by a complex interplay of pathways that may be significantly altered by the nutrient environment. Research in our laboratory and others has shown that both limited and excess nutrition can program the structure and function of the arcuate nucleus – changing its wiring, in essence – such that there is an increased ratio of appetite to satiety neurons (Clin Obstet Gynecol. 2013 Sep;56[3]:529-36).
There also appears to be a programmed down-regulation in the reward pathway of the brain, and some studies have shown that children of obese mothers and children who were born with low birth weights have a higher preference for sweet and high-calorie foods. This all begins at the neural stem cell level.
With more appetite neurons and fewer satiety neurons, as well as a down-regulation of reward – and an abundance of available food – a newborn is at high risk of becoming obese. Eating for this child will not only be pleasurable; it will be driven by an enhanced appetite, an inability to feel full after reasonable amounts of food, and a down-regulation of reward (potentially requiring greater amounts of food or a shift in preference for high fat/sweet food to achieve the pleasure from eating).
In addition to alterations in appetite/satiety, the nutrition environment in utero can alter adipose tissue development and function.
Like neural development, adipogenesis – the process by which preadipocytes proliferate and differentiate into mature adipocytes – is tightly regulated by a cascade of transcription factors that are expressed in response to stimuli, including nutrients. In animal studies we have found an up-regulation of adipogenic and lipogenic transcription factors in intrauterine growth restricted offspring as well as in offspring of obese mothers (Reprod Sci. 2008 Oct;15[8]:785-96 and Curr Diab Rep. 2013 Feb;13[1]:27-33).
This up-regulation leads to greater proliferation of preadipocytes and greater lipid synthesis and storage in mature adipocytes. Not only will the newborn have an increased number of adipocytes, but he or she will have an increased number of hypertrophic lipid-filled fat cells. The enhanced adipogenesis will contribute to the newborn’s programmed propensity for obesity, and the directive to “just eat less” will likely be ineffective throughout childhood and beyond.
Programmed offspring are resistant to both central and peripheral effects of leptin and insulin, resulting in impaired satiety (i.e., overeating) and manifestations of GDM. Responses to an array of additional energy regulatory factors (e.g., ghrelin) demonstrate a similar programmed dysfunction.
In practice
There are several approaches that ob.gyns. can take to prevent childhood and lifelong obesity. Most importantly, we must counsel our obese patients to lose weight before pregnancy. In doing so, it may be meaningful and effective to ask the patient to think about her baby’s future as an obese adult.
Patients who have experienced the challenges of trying to lose weight, and who are told about the developmental origins of obesity and how obesity can be programmed, may be more motivated to lose weight to avoid passing on to their children the burden and challenges that they’ve experienced. We can tell obese patients that their children may well be predisposed through the current in utero environment to have an increased appetite and a propensity to store body fat, and that they subsequently will face higher risks of diabetes and other serious chronic conditions.
We should also appropriately counsel women on healthy weight gain during pregnancy, and urge them not to gain excessive weight.
Newborn feeding strategies are also important for babies exposed to gestational programming of obesity, but especially small babies given the high risk of obesity when there is rapid catch-up growth. We must encourage good growth of both the low-birth-weight and macrosomic infant during the newborn period, but not overgrowth.
The importance of breastfeeding cannot be overestimated, as it has been demonstrated to reduce the occurrence of excessive newborn weight gain and improve long term infant health. We should encourage breastfeeding for the natural opportunity it provides to avoid excessive feeding, in addition to its other benefits. And for newborns who are bottle fed, we should counsel the new mother on optimal feeding and strategies for comforting a crying baby, which will protect against overfeeding.
Regarding environmental exposures, this area of developmental programming is continuing to evolve at a rapid rate. Both animal research and epidemiological studies support the association of developmental exposure to BPA and other chemicals with obesity.
For the present, we should educate our patients regarding optimal nutrition prior to and during pregnancy, and the avoidance of potentially toxic or metabolically-active chemicals or drugs. We look forward to continued research into the mechanisms and preventive/therapeutic strategies for optimization of childhood and adult health.
Dr. Ross is professor of obstetrics and gynecology at the University of California, Los Angeles. Dr. Desai is assistant professor of ob.gyn. at the university. They reported having no relevant financial disclosures.
The figures and trends behind the obesity epidemic are alarming: More than one-third of all adults in the United States are obese, as are 34% of women aged 20-39, and 17% of youth aged 2-19, according to data for 2011-2014 from the National Health and Nutrition Examination Survey.
In our ob.gyn. practices, many of us have witnessed the significant climb in national obesity rates over the past several decades. We’ve seen a continued increase in the prevalence of obesity among childbearing women, and a steady increase in the incidence of high-birth-weight babies. The percentage of women weighing 200 pounds has more than doubled since 1980, and up to 3-4 times as many children and teens in various age subsets are obese today as in the 1970s.
The obesity epidemic is often attributed to a high-fat and/or calorie-dense diet and decreased activity levels. However, this is only part of the picture. There has been growing recognition in recent years that obesity may be programmed by the in utero and newborn environment, particularly as it relates to nutritional permutations. We now have evidence, in fact, that developmental programming is likely a primary cause of the obesity epidemic.
Exposure to maternal obesity and being born with a low birth weight – especially a low birth weight paired with rapid catch-up growth – are both associated with a significantly increased risk of childhood and adult obesity.
Research has demonstrated that newborns may be programmed, in both of these scenarios, with an increased appetite and a predisposition to storing calories as fat. In addition, data are accumulating that exposure to bisphenol A and other endocrine-disruptive chemicals, other environmental toxins, and corticosteroids may exert similar programming effects.
This window into the origins of obesity has significant implications for the practice of ob.gyn., where we have the opportunity to address the programming effects of the in utero and early life environment. Most importantly, we must counsel women before pregnancy about the importance of losing weight, guide them during pregnancy to achieve optimal pregnancy nutrition and weight gain, and prepare them to adopt optimal newborn feeding strategies that will guard against overconsumption.
Programming of obesity
The current obesity epidemic is only minimally due to genetics. Although select genetic mutations may be associated with obesity, these mutations account for an exceedingly small proportion of the obese population. Instead, much of the obesity epidemic involves epigenetic change – in this case, largely epigenetic deregulation of gene expression – and more broadly what we call gestational, or developmental, programming.
Developmental programming is a process by which a stress or stimulus at a critical or sensitive period of development has long-term effects. The major part of the developmental process pertaining to cell division occurs during intrauterine life; more than 90% of the cell divisions necessary to make an adult human occur before birth. Although there are important effects of the early newborn period, developmental programming is therefore largely gestational programming. Depending on when an in utero stress or perturbation occurs, it may permanently change cell number and/or cell differentiation, organ structure, metabolic set points, and gene expression.
The late physician Dr. David Barker got us thinking about in utero programming when he demonstrated an association between low birth weight, rapid weight gain in early life, and adult cardiovascular mortality. His theory about how nutrition and growth before birth may affect cardiovascular health later on, as well as other adult chronic diseases and conditions, became known as the Barker Hypothesis.
Many studies, both animal research and human epidemiological studies, have since confirmed and expanded our understanding of this phenomena. Research has demonstrated associations, for instance, between low birth weight and later risks of insulin resistance, diabetes, fatty liver, and the often-underlying metabolic syndrome.
Obesity is also central to the development of the metabolic syndrome, and we now have irrefutable evidence to show that low birth weight infants have a higher risk of obesity than do normal weight infants. We also know, as Dr. Barker and his colleagues had surmised, that the greatest risks occur when there is rapid catch-up growth of low-birth-weight infants in the early years of life.
Moreover, we now understand that maternal obesity has programming effects that are similar to those of an in utero environment of undernutrition and growth restriction. In the past several decades, the marked increase in maternal obesity has resulted in this programming process having an ever-increasing impact.
Both animal and human studies have shown that infants born to obese mothers have the same increased risks for adult chronic disease – including the risk of becoming obese – as those of low birth weight infants. This increased risk is often, but not always, associated with high birth weight, and it is independent of whether the mother has gestational diabetes mellitus (GDM). Having a high birth weight is more likely in the setting of maternal obesity and itself raises the risk of eventual obesity (as does GDM), but an infant’s exposure to maternal obesity in and of itself is a risk factor.
The mechanisms
The programming mechanisms that predispose offspring to obesity are similar in infants of obese mothers and intrauterine growth restricted newborns, though they involve different epigenetic signals. Both involve dysregulation of appetite/satiety and of adipogenesis.
Appetite is primarily controlled by a complex circuit of neurons in the hypothalamus of the brain called the hypothalamic arcuate nucleus. Some neurons are orexigenic and stimulate or increase appetite, while others are anorexigenic and suppress appetite by promoting satiety.
During fetal development, hypothalamic neural stem cells proliferate and differentiate into various cell types. Neurons destined for the arcuate nucleus then differentiate into these so-called appetite neurons and satiety neurons. Though there is continued neural development and maturation during newborn life, hypothalamic control of appetite and satiety is largely set during this period.
Differentiation to appetite or satiety neurons is regulated by a complex interplay of pathways that may be significantly altered by the nutrient environment. Research in our laboratory and others has shown that both limited and excess nutrition can program the structure and function of the arcuate nucleus – changing its wiring, in essence – such that there is an increased ratio of appetite to satiety neurons (Clin Obstet Gynecol. 2013 Sep;56[3]:529-36).
There also appears to be a programmed down-regulation in the reward pathway of the brain, and some studies have shown that children of obese mothers and children who were born with low birth weights have a higher preference for sweet and high-calorie foods. This all begins at the neural stem cell level.
With more appetite neurons and fewer satiety neurons, as well as a down-regulation of reward – and an abundance of available food – a newborn is at high risk of becoming obese. Eating for this child will not only be pleasurable; it will be driven by an enhanced appetite, an inability to feel full after reasonable amounts of food, and a down-regulation of reward (potentially requiring greater amounts of food or a shift in preference for high fat/sweet food to achieve the pleasure from eating).
In addition to alterations in appetite/satiety, the nutrition environment in utero can alter adipose tissue development and function.
Like neural development, adipogenesis – the process by which preadipocytes proliferate and differentiate into mature adipocytes – is tightly regulated by a cascade of transcription factors that are expressed in response to stimuli, including nutrients. In animal studies we have found an up-regulation of adipogenic and lipogenic transcription factors in intrauterine growth restricted offspring as well as in offspring of obese mothers (Reprod Sci. 2008 Oct;15[8]:785-96 and Curr Diab Rep. 2013 Feb;13[1]:27-33).
This up-regulation leads to greater proliferation of preadipocytes and greater lipid synthesis and storage in mature adipocytes. Not only will the newborn have an increased number of adipocytes, but he or she will have an increased number of hypertrophic lipid-filled fat cells. The enhanced adipogenesis will contribute to the newborn’s programmed propensity for obesity, and the directive to “just eat less” will likely be ineffective throughout childhood and beyond.
Programmed offspring are resistant to both central and peripheral effects of leptin and insulin, resulting in impaired satiety (i.e., overeating) and manifestations of GDM. Responses to an array of additional energy regulatory factors (e.g., ghrelin) demonstrate a similar programmed dysfunction.
In practice
There are several approaches that ob.gyns. can take to prevent childhood and lifelong obesity. Most importantly, we must counsel our obese patients to lose weight before pregnancy. In doing so, it may be meaningful and effective to ask the patient to think about her baby’s future as an obese adult.
Patients who have experienced the challenges of trying to lose weight, and who are told about the developmental origins of obesity and how obesity can be programmed, may be more motivated to lose weight to avoid passing on to their children the burden and challenges that they’ve experienced. We can tell obese patients that their children may well be predisposed through the current in utero environment to have an increased appetite and a propensity to store body fat, and that they subsequently will face higher risks of diabetes and other serious chronic conditions.
We should also appropriately counsel women on healthy weight gain during pregnancy, and urge them not to gain excessive weight.
Newborn feeding strategies are also important for babies exposed to gestational programming of obesity, but especially small babies given the high risk of obesity when there is rapid catch-up growth. We must encourage good growth of both the low-birth-weight and macrosomic infant during the newborn period, but not overgrowth.
The importance of breastfeeding cannot be overestimated, as it has been demonstrated to reduce the occurrence of excessive newborn weight gain and improve long term infant health. We should encourage breastfeeding for the natural opportunity it provides to avoid excessive feeding, in addition to its other benefits. And for newborns who are bottle fed, we should counsel the new mother on optimal feeding and strategies for comforting a crying baby, which will protect against overfeeding.
Regarding environmental exposures, this area of developmental programming is continuing to evolve at a rapid rate. Both animal research and epidemiological studies support the association of developmental exposure to BPA and other chemicals with obesity.
For the present, we should educate our patients regarding optimal nutrition prior to and during pregnancy, and the avoidance of potentially toxic or metabolically-active chemicals or drugs. We look forward to continued research into the mechanisms and preventive/therapeutic strategies for optimization of childhood and adult health.
Dr. Ross is professor of obstetrics and gynecology at the University of California, Los Angeles. Dr. Desai is assistant professor of ob.gyn. at the university. They reported having no relevant financial disclosures.
The figures and trends behind the obesity epidemic are alarming: More than one-third of all adults in the United States are obese, as are 34% of women aged 20-39, and 17% of youth aged 2-19, according to data for 2011-2014 from the National Health and Nutrition Examination Survey.
In our ob.gyn. practices, many of us have witnessed the significant climb in national obesity rates over the past several decades. We’ve seen a continued increase in the prevalence of obesity among childbearing women, and a steady increase in the incidence of high-birth-weight babies. The percentage of women weighing 200 pounds has more than doubled since 1980, and up to 3-4 times as many children and teens in various age subsets are obese today as in the 1970s.
The obesity epidemic is often attributed to a high-fat and/or calorie-dense diet and decreased activity levels. However, this is only part of the picture. There has been growing recognition in recent years that obesity may be programmed by the in utero and newborn environment, particularly as it relates to nutritional permutations. We now have evidence, in fact, that developmental programming is likely a primary cause of the obesity epidemic.
Exposure to maternal obesity and being born with a low birth weight – especially a low birth weight paired with rapid catch-up growth – are both associated with a significantly increased risk of childhood and adult obesity.
Research has demonstrated that newborns may be programmed, in both of these scenarios, with an increased appetite and a predisposition to storing calories as fat. In addition, data are accumulating that exposure to bisphenol A and other endocrine-disruptive chemicals, other environmental toxins, and corticosteroids may exert similar programming effects.
This window into the origins of obesity has significant implications for the practice of ob.gyn., where we have the opportunity to address the programming effects of the in utero and early life environment. Most importantly, we must counsel women before pregnancy about the importance of losing weight, guide them during pregnancy to achieve optimal pregnancy nutrition and weight gain, and prepare them to adopt optimal newborn feeding strategies that will guard against overconsumption.
Programming of obesity
The current obesity epidemic is only minimally due to genetics. Although select genetic mutations may be associated with obesity, these mutations account for an exceedingly small proportion of the obese population. Instead, much of the obesity epidemic involves epigenetic change – in this case, largely epigenetic deregulation of gene expression – and more broadly what we call gestational, or developmental, programming.
Developmental programming is a process by which a stress or stimulus at a critical or sensitive period of development has long-term effects. The major part of the developmental process pertaining to cell division occurs during intrauterine life; more than 90% of the cell divisions necessary to make an adult human occur before birth. Although there are important effects of the early newborn period, developmental programming is therefore largely gestational programming. Depending on when an in utero stress or perturbation occurs, it may permanently change cell number and/or cell differentiation, organ structure, metabolic set points, and gene expression.
The late physician Dr. David Barker got us thinking about in utero programming when he demonstrated an association between low birth weight, rapid weight gain in early life, and adult cardiovascular mortality. His theory about how nutrition and growth before birth may affect cardiovascular health later on, as well as other adult chronic diseases and conditions, became known as the Barker Hypothesis.
Many studies, both animal research and human epidemiological studies, have since confirmed and expanded our understanding of this phenomena. Research has demonstrated associations, for instance, between low birth weight and later risks of insulin resistance, diabetes, fatty liver, and the often-underlying metabolic syndrome.
Obesity is also central to the development of the metabolic syndrome, and we now have irrefutable evidence to show that low birth weight infants have a higher risk of obesity than do normal weight infants. We also know, as Dr. Barker and his colleagues had surmised, that the greatest risks occur when there is rapid catch-up growth of low-birth-weight infants in the early years of life.
Moreover, we now understand that maternal obesity has programming effects that are similar to those of an in utero environment of undernutrition and growth restriction. In the past several decades, the marked increase in maternal obesity has resulted in this programming process having an ever-increasing impact.
Both animal and human studies have shown that infants born to obese mothers have the same increased risks for adult chronic disease – including the risk of becoming obese – as those of low birth weight infants. This increased risk is often, but not always, associated with high birth weight, and it is independent of whether the mother has gestational diabetes mellitus (GDM). Having a high birth weight is more likely in the setting of maternal obesity and itself raises the risk of eventual obesity (as does GDM), but an infant’s exposure to maternal obesity in and of itself is a risk factor.
The mechanisms
The programming mechanisms that predispose offspring to obesity are similar in infants of obese mothers and intrauterine growth restricted newborns, though they involve different epigenetic signals. Both involve dysregulation of appetite/satiety and of adipogenesis.
Appetite is primarily controlled by a complex circuit of neurons in the hypothalamus of the brain called the hypothalamic arcuate nucleus. Some neurons are orexigenic and stimulate or increase appetite, while others are anorexigenic and suppress appetite by promoting satiety.
During fetal development, hypothalamic neural stem cells proliferate and differentiate into various cell types. Neurons destined for the arcuate nucleus then differentiate into these so-called appetite neurons and satiety neurons. Though there is continued neural development and maturation during newborn life, hypothalamic control of appetite and satiety is largely set during this period.
Differentiation to appetite or satiety neurons is regulated by a complex interplay of pathways that may be significantly altered by the nutrient environment. Research in our laboratory and others has shown that both limited and excess nutrition can program the structure and function of the arcuate nucleus – changing its wiring, in essence – such that there is an increased ratio of appetite to satiety neurons (Clin Obstet Gynecol. 2013 Sep;56[3]:529-36).
There also appears to be a programmed down-regulation in the reward pathway of the brain, and some studies have shown that children of obese mothers and children who were born with low birth weights have a higher preference for sweet and high-calorie foods. This all begins at the neural stem cell level.
With more appetite neurons and fewer satiety neurons, as well as a down-regulation of reward – and an abundance of available food – a newborn is at high risk of becoming obese. Eating for this child will not only be pleasurable; it will be driven by an enhanced appetite, an inability to feel full after reasonable amounts of food, and a down-regulation of reward (potentially requiring greater amounts of food or a shift in preference for high fat/sweet food to achieve the pleasure from eating).
In addition to alterations in appetite/satiety, the nutrition environment in utero can alter adipose tissue development and function.
Like neural development, adipogenesis – the process by which preadipocytes proliferate and differentiate into mature adipocytes – is tightly regulated by a cascade of transcription factors that are expressed in response to stimuli, including nutrients. In animal studies we have found an up-regulation of adipogenic and lipogenic transcription factors in intrauterine growth restricted offspring as well as in offspring of obese mothers (Reprod Sci. 2008 Oct;15[8]:785-96 and Curr Diab Rep. 2013 Feb;13[1]:27-33).
This up-regulation leads to greater proliferation of preadipocytes and greater lipid synthesis and storage in mature adipocytes. Not only will the newborn have an increased number of adipocytes, but he or she will have an increased number of hypertrophic lipid-filled fat cells. The enhanced adipogenesis will contribute to the newborn’s programmed propensity for obesity, and the directive to “just eat less” will likely be ineffective throughout childhood and beyond.
Programmed offspring are resistant to both central and peripheral effects of leptin and insulin, resulting in impaired satiety (i.e., overeating) and manifestations of GDM. Responses to an array of additional energy regulatory factors (e.g., ghrelin) demonstrate a similar programmed dysfunction.
In practice
There are several approaches that ob.gyns. can take to prevent childhood and lifelong obesity. Most importantly, we must counsel our obese patients to lose weight before pregnancy. In doing so, it may be meaningful and effective to ask the patient to think about her baby’s future as an obese adult.
Patients who have experienced the challenges of trying to lose weight, and who are told about the developmental origins of obesity and how obesity can be programmed, may be more motivated to lose weight to avoid passing on to their children the burden and challenges that they’ve experienced. We can tell obese patients that their children may well be predisposed through the current in utero environment to have an increased appetite and a propensity to store body fat, and that they subsequently will face higher risks of diabetes and other serious chronic conditions.
We should also appropriately counsel women on healthy weight gain during pregnancy, and urge them not to gain excessive weight.
Newborn feeding strategies are also important for babies exposed to gestational programming of obesity, but especially small babies given the high risk of obesity when there is rapid catch-up growth. We must encourage good growth of both the low-birth-weight and macrosomic infant during the newborn period, but not overgrowth.
The importance of breastfeeding cannot be overestimated, as it has been demonstrated to reduce the occurrence of excessive newborn weight gain and improve long term infant health. We should encourage breastfeeding for the natural opportunity it provides to avoid excessive feeding, in addition to its other benefits. And for newborns who are bottle fed, we should counsel the new mother on optimal feeding and strategies for comforting a crying baby, which will protect against overfeeding.
Regarding environmental exposures, this area of developmental programming is continuing to evolve at a rapid rate. Both animal research and epidemiological studies support the association of developmental exposure to BPA and other chemicals with obesity.
For the present, we should educate our patients regarding optimal nutrition prior to and during pregnancy, and the avoidance of potentially toxic or metabolically-active chemicals or drugs. We look forward to continued research into the mechanisms and preventive/therapeutic strategies for optimization of childhood and adult health.
Dr. Ross is professor of obstetrics and gynecology at the University of California, Los Angeles. Dr. Desai is assistant professor of ob.gyn. at the university. They reported having no relevant financial disclosures.
The far-reaching implications of weight gain in pregnancy
It is not surprising that a pregnant woman’s actions heavily influence her developing baby. Ob.gyns. advise patients to stop smoking or to stop using illicit drugs, and limit their alcohol consumption during pregnancy because we know that these substances can cause serious, even fatal, consequences for the fetus. Although we routinely provide nutrition information and guidelines on healthy weight gain in pregnancy, we may not stress the importance of healthy eating to the same degree as we may emphasize the need to eliminate tobacco use. But should we?
In 2011, a study by researchers at Yale University, the University of Texas, and Arizona State University suggested that food can have effects on the brain similar to those of addictive substances (Arch Gen Psychiatry. 2011 Aug;68[8]:808-16). Using MRI, the investigators examined which areas of the brain became active in response to the consumption of a chocolate milkshake, and compared these results to brain scans of people addicted to opioids. The study enrolled 48 women who were lean to obese, based on body mass index. The researchers found that people who were obese had brain activity patterns in response to food that were similar to patterns that people with drug addiction had in response to opioids. Although the sample size was small, the investigators showed, in essence, that food is a “drug.”
Ob.gyns. working with patients who are overweight or obese typically encourage weight loss prior to pregnancy, or suggest limited weight gain during gestation, because obesity increases complications for both the pregnant mother and her unborn baby. If, as the 2011 study suggests, we were to think of food addiction as we do any other drug addiction – tobacco, opioids, alcohol – that should be curbed out of concern for the developing baby, ob.gyns. might tell our patients to reduce or completely eliminate their “trans-fat food habit” before and during pregnancy.
Importantly, a mother’s nutrition, or lack thereof, may exert harmful effects on her child’s long-term health. This idea was intimated decades ago when Dr. David Barker proposed that a person’s future risk for disease began during pregnancy. Exactly how this type of early programming may occur remains to be determined. Therefore, this month we examine the fetal origins of obesity, and have invited Dr. Michael G. Ross, professor of obstetrics and gynecology, and Mina Desai, Ph.D., assistant professor of obstetrics and gynecology, at the University of California, Los Angeles, to discuss this important topic.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
It is not surprising that a pregnant woman’s actions heavily influence her developing baby. Ob.gyns. advise patients to stop smoking or to stop using illicit drugs, and limit their alcohol consumption during pregnancy because we know that these substances can cause serious, even fatal, consequences for the fetus. Although we routinely provide nutrition information and guidelines on healthy weight gain in pregnancy, we may not stress the importance of healthy eating to the same degree as we may emphasize the need to eliminate tobacco use. But should we?
In 2011, a study by researchers at Yale University, the University of Texas, and Arizona State University suggested that food can have effects on the brain similar to those of addictive substances (Arch Gen Psychiatry. 2011 Aug;68[8]:808-16). Using MRI, the investigators examined which areas of the brain became active in response to the consumption of a chocolate milkshake, and compared these results to brain scans of people addicted to opioids. The study enrolled 48 women who were lean to obese, based on body mass index. The researchers found that people who were obese had brain activity patterns in response to food that were similar to patterns that people with drug addiction had in response to opioids. Although the sample size was small, the investigators showed, in essence, that food is a “drug.”
Ob.gyns. working with patients who are overweight or obese typically encourage weight loss prior to pregnancy, or suggest limited weight gain during gestation, because obesity increases complications for both the pregnant mother and her unborn baby. If, as the 2011 study suggests, we were to think of food addiction as we do any other drug addiction – tobacco, opioids, alcohol – that should be curbed out of concern for the developing baby, ob.gyns. might tell our patients to reduce or completely eliminate their “trans-fat food habit” before and during pregnancy.
Importantly, a mother’s nutrition, or lack thereof, may exert harmful effects on her child’s long-term health. This idea was intimated decades ago when Dr. David Barker proposed that a person’s future risk for disease began during pregnancy. Exactly how this type of early programming may occur remains to be determined. Therefore, this month we examine the fetal origins of obesity, and have invited Dr. Michael G. Ross, professor of obstetrics and gynecology, and Mina Desai, Ph.D., assistant professor of obstetrics and gynecology, at the University of California, Los Angeles, to discuss this important topic.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
It is not surprising that a pregnant woman’s actions heavily influence her developing baby. Ob.gyns. advise patients to stop smoking or to stop using illicit drugs, and limit their alcohol consumption during pregnancy because we know that these substances can cause serious, even fatal, consequences for the fetus. Although we routinely provide nutrition information and guidelines on healthy weight gain in pregnancy, we may not stress the importance of healthy eating to the same degree as we may emphasize the need to eliminate tobacco use. But should we?
In 2011, a study by researchers at Yale University, the University of Texas, and Arizona State University suggested that food can have effects on the brain similar to those of addictive substances (Arch Gen Psychiatry. 2011 Aug;68[8]:808-16). Using MRI, the investigators examined which areas of the brain became active in response to the consumption of a chocolate milkshake, and compared these results to brain scans of people addicted to opioids. The study enrolled 48 women who were lean to obese, based on body mass index. The researchers found that people who were obese had brain activity patterns in response to food that were similar to patterns that people with drug addiction had in response to opioids. Although the sample size was small, the investigators showed, in essence, that food is a “drug.”
Ob.gyns. working with patients who are overweight or obese typically encourage weight loss prior to pregnancy, or suggest limited weight gain during gestation, because obesity increases complications for both the pregnant mother and her unborn baby. If, as the 2011 study suggests, we were to think of food addiction as we do any other drug addiction – tobacco, opioids, alcohol – that should be curbed out of concern for the developing baby, ob.gyns. might tell our patients to reduce or completely eliminate their “trans-fat food habit” before and during pregnancy.
Importantly, a mother’s nutrition, or lack thereof, may exert harmful effects on her child’s long-term health. This idea was intimated decades ago when Dr. David Barker proposed that a person’s future risk for disease began during pregnancy. Exactly how this type of early programming may occur remains to be determined. Therefore, this month we examine the fetal origins of obesity, and have invited Dr. Michael G. Ross, professor of obstetrics and gynecology, and Mina Desai, Ph.D., assistant professor of obstetrics and gynecology, at the University of California, Los Angeles, to discuss this important topic.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Cardiovascular consequences of extreme prematurity persist into late adolescence
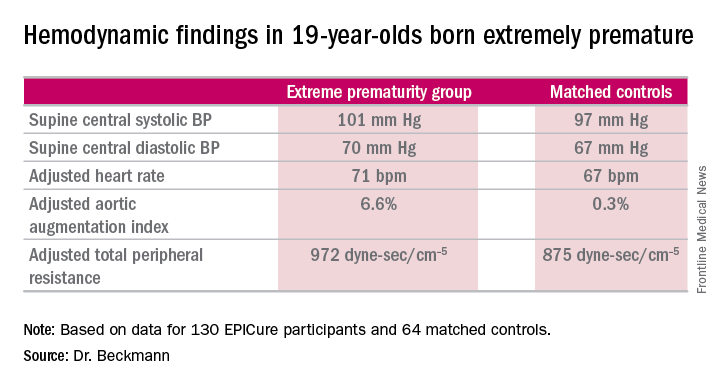
CHICAGO – The abnormal arterial hemodynamics identified in 11-year-olds with an extremely preterm birth persist at age 19, according to an update from the landmark longitudinal EPICure study.
“Given the implications of these significant findings, cardiovascular monitoring and risk prevention would be highly recommended for all individuals born extremely preterm,” Dr. Joanne Beckmann said in presenting the EPICure results on the long-term consequences of extreme prematurity at the annual meeting of the American College of Cardiology.
EPICure is a longitudinal study investigating health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks’ gestation in the United Kingdom during 1995-1996. It is the longest such study conducted anywhere.
“Neonatal survival at the lowest gestations has improved significantly since the 1990s with the advancement in neonatal care treatments and the implementation of evidence-based practices. Therefore, long-term health outcomes following extremely preterm birth will have increasing relevance to adult physicians,” observed Dr. Beckmann of University College London.
She reported on the results of detailed cardiovascular assessments conducted in 130 extremely premature EPICure participants and 64 matched controls who made it to London for 2 days of health testing when they turned 19 years of age. The findings update the results of similar comprehensive examinations done at age 11 years.
The extremely premature birth (EP) subjects were shorter and weighed less than did the controls. The two groups had similar seated systolic and diastolic blood pressure, and cardiac index didn’t differ between the two groups. However, the EP group had significantly higher supine central systolic and diastolic blood pressure and a higher heart rate.
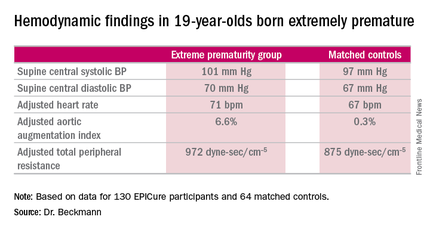
Moreover, the increases in aortic augmentation index – a composite of arterial stiffness and global wave reflections – and total peripheral resistance seen in the EP group at age 11 years persisted at the 19-year mark. It’s unclear whether the abnormal peripheral resistance in the EP group is structural or functional in nature. All hemodynamic differences between the two groups remained significant after adjustment for potential confounders.
Aortic pulse wave velocity was not significantly different between the two groups of 19-year-olds.
Data pertaining to other aspects of health in the 19-year-olds are now being analyzed. At the age-11 assessment, the EP group was found to have significantly impaired lung function (J Pediatr. 2012 Oct;161[4]:595-601.e2), high risk for neurodevelopmental disability (Pediatrics. 2009 Aug;124[2]:3249-57), a high rate of learning impairments, and an 18-fold increased risk of poor academic attainment compared to their matched peers (Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94[4]:F283-9).
EPICure is funded by the Medical Research Council. Dr. Beckmann reported having no financial conflicts of interest.
CHICAGO – The abnormal arterial hemodynamics identified in 11-year-olds with an extremely preterm birth persist at age 19, according to an update from the landmark longitudinal EPICure study.
“Given the implications of these significant findings, cardiovascular monitoring and risk prevention would be highly recommended for all individuals born extremely preterm,” Dr. Joanne Beckmann said in presenting the EPICure results on the long-term consequences of extreme prematurity at the annual meeting of the American College of Cardiology.
EPICure is a longitudinal study investigating health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks’ gestation in the United Kingdom during 1995-1996. It is the longest such study conducted anywhere.
“Neonatal survival at the lowest gestations has improved significantly since the 1990s with the advancement in neonatal care treatments and the implementation of evidence-based practices. Therefore, long-term health outcomes following extremely preterm birth will have increasing relevance to adult physicians,” observed Dr. Beckmann of University College London.
She reported on the results of detailed cardiovascular assessments conducted in 130 extremely premature EPICure participants and 64 matched controls who made it to London for 2 days of health testing when they turned 19 years of age. The findings update the results of similar comprehensive examinations done at age 11 years.
The extremely premature birth (EP) subjects were shorter and weighed less than did the controls. The two groups had similar seated systolic and diastolic blood pressure, and cardiac index didn’t differ between the two groups. However, the EP group had significantly higher supine central systolic and diastolic blood pressure and a higher heart rate.
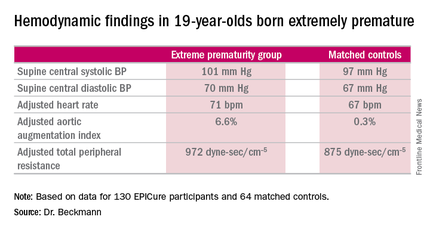
Moreover, the increases in aortic augmentation index – a composite of arterial stiffness and global wave reflections – and total peripheral resistance seen in the EP group at age 11 years persisted at the 19-year mark. It’s unclear whether the abnormal peripheral resistance in the EP group is structural or functional in nature. All hemodynamic differences between the two groups remained significant after adjustment for potential confounders.
Aortic pulse wave velocity was not significantly different between the two groups of 19-year-olds.
Data pertaining to other aspects of health in the 19-year-olds are now being analyzed. At the age-11 assessment, the EP group was found to have significantly impaired lung function (J Pediatr. 2012 Oct;161[4]:595-601.e2), high risk for neurodevelopmental disability (Pediatrics. 2009 Aug;124[2]:3249-57), a high rate of learning impairments, and an 18-fold increased risk of poor academic attainment compared to their matched peers (Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94[4]:F283-9).
EPICure is funded by the Medical Research Council. Dr. Beckmann reported having no financial conflicts of interest.
CHICAGO – The abnormal arterial hemodynamics identified in 11-year-olds with an extremely preterm birth persist at age 19, according to an update from the landmark longitudinal EPICure study.
“Given the implications of these significant findings, cardiovascular monitoring and risk prevention would be highly recommended for all individuals born extremely preterm,” Dr. Joanne Beckmann said in presenting the EPICure results on the long-term consequences of extreme prematurity at the annual meeting of the American College of Cardiology.
EPICure is a longitudinal study investigating health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks’ gestation in the United Kingdom during 1995-1996. It is the longest such study conducted anywhere.
“Neonatal survival at the lowest gestations has improved significantly since the 1990s with the advancement in neonatal care treatments and the implementation of evidence-based practices. Therefore, long-term health outcomes following extremely preterm birth will have increasing relevance to adult physicians,” observed Dr. Beckmann of University College London.
She reported on the results of detailed cardiovascular assessments conducted in 130 extremely premature EPICure participants and 64 matched controls who made it to London for 2 days of health testing when they turned 19 years of age. The findings update the results of similar comprehensive examinations done at age 11 years.
The extremely premature birth (EP) subjects were shorter and weighed less than did the controls. The two groups had similar seated systolic and diastolic blood pressure, and cardiac index didn’t differ between the two groups. However, the EP group had significantly higher supine central systolic and diastolic blood pressure and a higher heart rate.
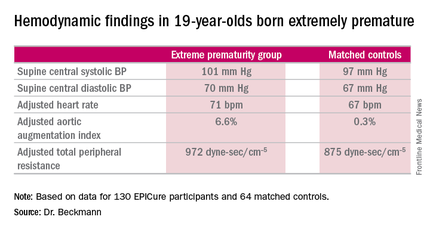
Moreover, the increases in aortic augmentation index – a composite of arterial stiffness and global wave reflections – and total peripheral resistance seen in the EP group at age 11 years persisted at the 19-year mark. It’s unclear whether the abnormal peripheral resistance in the EP group is structural or functional in nature. All hemodynamic differences between the two groups remained significant after adjustment for potential confounders.
Aortic pulse wave velocity was not significantly different between the two groups of 19-year-olds.
Data pertaining to other aspects of health in the 19-year-olds are now being analyzed. At the age-11 assessment, the EP group was found to have significantly impaired lung function (J Pediatr. 2012 Oct;161[4]:595-601.e2), high risk for neurodevelopmental disability (Pediatrics. 2009 Aug;124[2]:3249-57), a high rate of learning impairments, and an 18-fold increased risk of poor academic attainment compared to their matched peers (Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94[4]:F283-9).
EPICure is funded by the Medical Research Council. Dr. Beckmann reported having no financial conflicts of interest.
AT ACC 16
Key clinical point: At age 19 years, persons born extremely premature still show significant abnormalities in arterial hemodynamics and peripheral resistance.
Major finding: The adjusted aortic augmentation index was 6.6% in 19-year-olds born at 22-25 weeks gestation compared with 0.3% in matched controls.
Data source: EPICure, a longitudinal study of health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks gestation in the United Kingdom during 1995-1996.
Disclosures: EPICure is funded by the Medical Research Council. The presenter reported having no financial conflicts of interest.
CDC Reports Major Drop in Teen Birth Rates Among Minorities
Pregnancy rates among Hispanic and black teens are at an all-time low, reflecting overall declines in teen birth rates, new data show.
The Centers for Disease Control and Prevention reported on April 28 that the rate of Hispanic teens giving birth in the United States has dropped by more than half since 2006. During that same time period, there was a 44% drop in the birth rate for black teens.
Although these dramatic declines occurred against the backdrop of an overall decrease of about 40% in teen birth rates during the last decade, the CDC also reported that birth rates among Hispanics and black teens are still twice as high as they are for whites.
“The United States has made remarkable progress in reducing both teen pregnancy and racial and ethnic differences, but the reality is, too many American teens are still having babies,” Dr. Tom Frieden, CDC director, said in a statement. “By better understanding the many factors that contribute to teen pregnancy, we can better design, implement, evaluate, and improve prevention interventions and further reduce disparities.”
Overall, the birth rate among girls aged 15-19 years dropped from 41.1 to 24.2 per 1,000 from 2006 to 2014. The largest decline occurred in Hispanics, going from 77.4 to 38.0 per 1,000. The next biggest rate decline was in black teens, which fell from 61.9 to 34.9 per 1,000. The rate for white teens declined by 35%, falling from 26.7 to 17.3 per 1,000 (MMWR Morb Mortal Wkly Rep. 2016 Apr;65:409-14).
The CDC report indicated state- and community-level patterns, including that rates were notably higher among all races and ethnicities where unemployment is also high, but income and education levels are low. In some states with low overall birth rates, certain counties experienced higher rates. The highest rates nationwide tended to be in counties located in southern and southwestern states.
“These data underscore that the solution to our nation’s teen pregnancy problem is not going to be a one-size-fits-all – teen birth rates vary greatly across state lines and even within states,” Lisa Romero, Dr.P.H., a health scientist in the CDC’s Division of Reproductive Health, and the report’s lead author, said in a statement. “We can ensure the success of teen pregnancy prevention efforts by capitalizing on the expertise of our state and local public health colleagues. Together, we can work to implement proven prevention programs that take into account unique, local needs.”
The study is based on statistics for births to girls aged 15-19 years occurring between 2006 and 2014, taken from the National Vital Statistics System (NVSS). County-level NVSS data from 2013 and 2014 was also used, as were data from the American Community Survey between 2010 and 2014.
Pregnancy rates among Hispanic and black teens are at an all-time low, reflecting overall declines in teen birth rates, new data show.
The Centers for Disease Control and Prevention reported on April 28 that the rate of Hispanic teens giving birth in the United States has dropped by more than half since 2006. During that same time period, there was a 44% drop in the birth rate for black teens.
Although these dramatic declines occurred against the backdrop of an overall decrease of about 40% in teen birth rates during the last decade, the CDC also reported that birth rates among Hispanics and black teens are still twice as high as they are for whites.
“The United States has made remarkable progress in reducing both teen pregnancy and racial and ethnic differences, but the reality is, too many American teens are still having babies,” Dr. Tom Frieden, CDC director, said in a statement. “By better understanding the many factors that contribute to teen pregnancy, we can better design, implement, evaluate, and improve prevention interventions and further reduce disparities.”
Overall, the birth rate among girls aged 15-19 years dropped from 41.1 to 24.2 per 1,000 from 2006 to 2014. The largest decline occurred in Hispanics, going from 77.4 to 38.0 per 1,000. The next biggest rate decline was in black teens, which fell from 61.9 to 34.9 per 1,000. The rate for white teens declined by 35%, falling from 26.7 to 17.3 per 1,000 (MMWR Morb Mortal Wkly Rep. 2016 Apr;65:409-14).
The CDC report indicated state- and community-level patterns, including that rates were notably higher among all races and ethnicities where unemployment is also high, but income and education levels are low. In some states with low overall birth rates, certain counties experienced higher rates. The highest rates nationwide tended to be in counties located in southern and southwestern states.
“These data underscore that the solution to our nation’s teen pregnancy problem is not going to be a one-size-fits-all – teen birth rates vary greatly across state lines and even within states,” Lisa Romero, Dr.P.H., a health scientist in the CDC’s Division of Reproductive Health, and the report’s lead author, said in a statement. “We can ensure the success of teen pregnancy prevention efforts by capitalizing on the expertise of our state and local public health colleagues. Together, we can work to implement proven prevention programs that take into account unique, local needs.”
The study is based on statistics for births to girls aged 15-19 years occurring between 2006 and 2014, taken from the National Vital Statistics System (NVSS). County-level NVSS data from 2013 and 2014 was also used, as were data from the American Community Survey between 2010 and 2014.
Pregnancy rates among Hispanic and black teens are at an all-time low, reflecting overall declines in teen birth rates, new data show.
The Centers for Disease Control and Prevention reported on April 28 that the rate of Hispanic teens giving birth in the United States has dropped by more than half since 2006. During that same time period, there was a 44% drop in the birth rate for black teens.
Although these dramatic declines occurred against the backdrop of an overall decrease of about 40% in teen birth rates during the last decade, the CDC also reported that birth rates among Hispanics and black teens are still twice as high as they are for whites.
“The United States has made remarkable progress in reducing both teen pregnancy and racial and ethnic differences, but the reality is, too many American teens are still having babies,” Dr. Tom Frieden, CDC director, said in a statement. “By better understanding the many factors that contribute to teen pregnancy, we can better design, implement, evaluate, and improve prevention interventions and further reduce disparities.”
Overall, the birth rate among girls aged 15-19 years dropped from 41.1 to 24.2 per 1,000 from 2006 to 2014. The largest decline occurred in Hispanics, going from 77.4 to 38.0 per 1,000. The next biggest rate decline was in black teens, which fell from 61.9 to 34.9 per 1,000. The rate for white teens declined by 35%, falling from 26.7 to 17.3 per 1,000 (MMWR Morb Mortal Wkly Rep. 2016 Apr;65:409-14).
The CDC report indicated state- and community-level patterns, including that rates were notably higher among all races and ethnicities where unemployment is also high, but income and education levels are low. In some states with low overall birth rates, certain counties experienced higher rates. The highest rates nationwide tended to be in counties located in southern and southwestern states.
“These data underscore that the solution to our nation’s teen pregnancy problem is not going to be a one-size-fits-all – teen birth rates vary greatly across state lines and even within states,” Lisa Romero, Dr.P.H., a health scientist in the CDC’s Division of Reproductive Health, and the report’s lead author, said in a statement. “We can ensure the success of teen pregnancy prevention efforts by capitalizing on the expertise of our state and local public health colleagues. Together, we can work to implement proven prevention programs that take into account unique, local needs.”
The study is based on statistics for births to girls aged 15-19 years occurring between 2006 and 2014, taken from the National Vital Statistics System (NVSS). County-level NVSS data from 2013 and 2014 was also used, as were data from the American Community Survey between 2010 and 2014.
FROM MMWR
CDC reports major drop in teen birth rates among minorities
Pregnancy rates among Hispanic and black teens are at an all-time low, reflecting overall declines in teen birth rates, new data show.
The Centers for Disease Control and Prevention reported on April 28 that the rate of Hispanic teens giving birth in the United States has dropped by more than half since 2006. During that same time period, there was a 44% drop in the birth rate for black teens.
Although these dramatic declines occurred against the backdrop of an overall decrease of about 40% in teen birth rates during the last decade, the CDC also reported that birth rates among Hispanics and black teens are still twice as high as they are for whites.
“The United States has made remarkable progress in reducing both teen pregnancy and racial and ethnic differences, but the reality is, too many American teens are still having babies,” Dr. Tom Frieden, CDC director, said in a statement. “By better understanding the many factors that contribute to teen pregnancy, we can better design, implement, evaluate, and improve prevention interventions and further reduce disparities.”
Overall, the birth rate among girls aged 15-19 years dropped from 41.1 to 24.2 per 1,000 from 2006 to 2014. The largest decline occurred in Hispanics, going from 77.4 to 38.0 per 1,000. The next biggest rate decline was in black teens, which fell from 61.9 to 34.9 per 1,000. The rate for white teens declined by 35%, falling from 26.7 to 17.3 per 1,000 (MMWR Morb Mortal Wkly Rep. 2016 Apr;65:409-14).
The CDC report indicated state- and community-level patterns, including that rates were notably higher among all races and ethnicities where unemployment is also high, but income and education levels are low. In some states with low overall birth rates, certain counties experienced higher rates. The highest rates nationwide tended to be in counties located in southern and southwestern states.
“These data underscore that the solution to our nation’s teen pregnancy problem is not going to be a one-size-fits-all – teen birth rates vary greatly across state lines and even within states,” Lisa Romero, Dr.P.H., a health scientist in the CDC’s Division of Reproductive Health, and the report’s lead author, said in a statement. “We can ensure the success of teen pregnancy prevention efforts by capitalizing on the expertise of our state and local public health colleagues. Together, we can work to implement proven prevention programs that take into account unique, local needs.”
The study is based on statistics for births to girls aged 15-19 years occurring between 2006 and 2014, taken from the National Vital Statistics System (NVSS). County-level NVSS data from 2013 and 2014 was also used, as were data from the American Community Survey between 2010 and 2014.
On Twitter @whitneymcknight
Pregnancy rates among Hispanic and black teens are at an all-time low, reflecting overall declines in teen birth rates, new data show.
The Centers for Disease Control and Prevention reported on April 28 that the rate of Hispanic teens giving birth in the United States has dropped by more than half since 2006. During that same time period, there was a 44% drop in the birth rate for black teens.
Although these dramatic declines occurred against the backdrop of an overall decrease of about 40% in teen birth rates during the last decade, the CDC also reported that birth rates among Hispanics and black teens are still twice as high as they are for whites.
“The United States has made remarkable progress in reducing both teen pregnancy and racial and ethnic differences, but the reality is, too many American teens are still having babies,” Dr. Tom Frieden, CDC director, said in a statement. “By better understanding the many factors that contribute to teen pregnancy, we can better design, implement, evaluate, and improve prevention interventions and further reduce disparities.”
Overall, the birth rate among girls aged 15-19 years dropped from 41.1 to 24.2 per 1,000 from 2006 to 2014. The largest decline occurred in Hispanics, going from 77.4 to 38.0 per 1,000. The next biggest rate decline was in black teens, which fell from 61.9 to 34.9 per 1,000. The rate for white teens declined by 35%, falling from 26.7 to 17.3 per 1,000 (MMWR Morb Mortal Wkly Rep. 2016 Apr;65:409-14).
The CDC report indicated state- and community-level patterns, including that rates were notably higher among all races and ethnicities where unemployment is also high, but income and education levels are low. In some states with low overall birth rates, certain counties experienced higher rates. The highest rates nationwide tended to be in counties located in southern and southwestern states.
“These data underscore that the solution to our nation’s teen pregnancy problem is not going to be a one-size-fits-all – teen birth rates vary greatly across state lines and even within states,” Lisa Romero, Dr.P.H., a health scientist in the CDC’s Division of Reproductive Health, and the report’s lead author, said in a statement. “We can ensure the success of teen pregnancy prevention efforts by capitalizing on the expertise of our state and local public health colleagues. Together, we can work to implement proven prevention programs that take into account unique, local needs.”
The study is based on statistics for births to girls aged 15-19 years occurring between 2006 and 2014, taken from the National Vital Statistics System (NVSS). County-level NVSS data from 2013 and 2014 was also used, as were data from the American Community Survey between 2010 and 2014.
On Twitter @whitneymcknight
Pregnancy rates among Hispanic and black teens are at an all-time low, reflecting overall declines in teen birth rates, new data show.
The Centers for Disease Control and Prevention reported on April 28 that the rate of Hispanic teens giving birth in the United States has dropped by more than half since 2006. During that same time period, there was a 44% drop in the birth rate for black teens.
Although these dramatic declines occurred against the backdrop of an overall decrease of about 40% in teen birth rates during the last decade, the CDC also reported that birth rates among Hispanics and black teens are still twice as high as they are for whites.
“The United States has made remarkable progress in reducing both teen pregnancy and racial and ethnic differences, but the reality is, too many American teens are still having babies,” Dr. Tom Frieden, CDC director, said in a statement. “By better understanding the many factors that contribute to teen pregnancy, we can better design, implement, evaluate, and improve prevention interventions and further reduce disparities.”
Overall, the birth rate among girls aged 15-19 years dropped from 41.1 to 24.2 per 1,000 from 2006 to 2014. The largest decline occurred in Hispanics, going from 77.4 to 38.0 per 1,000. The next biggest rate decline was in black teens, which fell from 61.9 to 34.9 per 1,000. The rate for white teens declined by 35%, falling from 26.7 to 17.3 per 1,000 (MMWR Morb Mortal Wkly Rep. 2016 Apr;65:409-14).
The CDC report indicated state- and community-level patterns, including that rates were notably higher among all races and ethnicities where unemployment is also high, but income and education levels are low. In some states with low overall birth rates, certain counties experienced higher rates. The highest rates nationwide tended to be in counties located in southern and southwestern states.
“These data underscore that the solution to our nation’s teen pregnancy problem is not going to be a one-size-fits-all – teen birth rates vary greatly across state lines and even within states,” Lisa Romero, Dr.P.H., a health scientist in the CDC’s Division of Reproductive Health, and the report’s lead author, said in a statement. “We can ensure the success of teen pregnancy prevention efforts by capitalizing on the expertise of our state and local public health colleagues. Together, we can work to implement proven prevention programs that take into account unique, local needs.”
The study is based on statistics for births to girls aged 15-19 years occurring between 2006 and 2014, taken from the National Vital Statistics System (NVSS). County-level NVSS data from 2013 and 2014 was also used, as were data from the American Community Survey between 2010 and 2014.
On Twitter @whitneymcknight
FROM MMWR
Shoulder dystocia: Taking the fear out of management
FDA Evaluating the Use of Oral Fluconazole in Pregnancy
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
FDA evaluating the use of oral fluconazole in pregnancy
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
Infantile Hemangiomas Increasing, Linked to Prematurity, Low Birth Weight
WAIKOLOA, HAWAII – The incidence of infantile hemangiomas has climbed steadily in recent decades in concert with rising rates of prematurity and low birth weight, Dr. Sheila Fallon Friedlander said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“We spend a lot of time talking about port wine stains, but guess what? They’re much less frequent than are infantile hemangiomas, which most studies agree have an incidence of about 5%, as compared to 0.1%-0.3% for port wine stains,” observed Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego.
Most of these lesions resolve over time, but some are disfiguring or even life threatening. With the availability of safe and effective therapies in the form of propranolol, nadolol, timolol, and lasers, it’s incumbent on physicians to make the diagnosis early and intervene in a timely manner when appropriate to avoid complications, the pediatric dermatologist emphasized.
She highlighted a recent population-based study of infants born in Olmsted County, Minn., during 1976-2010. The Mayo Clinic investigators found that the incidence of infantile hemangiomas climbed from 0.97 to 1.97 per 100 person-years over that time span. Meanwhile, the average gestational age at birth among babies with infantile hemangiomas in the county fell from 39.2 weeks to 38.3 weeks, and their average birth weight dropped from 3,383 g to 3,185 g (J Am Acad Dermatol. 2016;74[1]:120-6).
Dr. Friedlander was senior investigator for a unique study, the first prospective U.S. study to track the incidence of infantile hemangiomas from birth through 9 months of age. The study included 578 mothers enrolled in pregnancy and their 594 offspring. All of the neonates were examined by a pediatric dermatologist within 48 hours after delivery, allowing for precise differentiation between infantile hemangiomas and other neonatal vascular lesions.
The incidence of infantile hemangiomas was 4.5%. The majority of the lesions occurred on the trunk or extremities. Of note, only one infantile hemangioma required intervention. Twenty percent of the infantile hemangiomas were small focal lesions with abortive or telangiectatic morphology that stopped growing by 3 months of age.
As in the Mayo Clinic study, Dr. Friedlander noted, the risk of infantile hemangioma in this San Diego–area study population increased with decreasing gestational age and weight. The incidence was 3.9% in term infants, 7.4% in premature infants, and 14.3% in those who were very premature. Similarly, infantile hemangiomas occurred in 4% of normal-birth-weight babies but in 16.6% of those who were very low birth weight (Br J Dermatol. 2014;170[4]:907-13).
Abnormalities of placental perfusion occurred in nearly 35% of pregnancies that produced babies with infantile hemangiomas, a rate twice that seen in pregnancies not associated with a subsequent infantile hemangioma. This and other evidence points to hypoxia as a key factor in precipitating the development of infantile hemangiomas.
“We believe that these lesions are related to embolization of tissue, perhaps placental, or hypoxia in utero,” Dr. Friedlander said. “Extreme prematurity, low birth weight, Caucasian race, placental anomalies, increased maternal age, use of fertility drugs – these are all things that will up your ante for having a child with an infantile hemangioma.”
She reported receiving grant/research support from Merz and Valeant Pharmaceuticals, and serving as a consultant for Sandoz.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – The incidence of infantile hemangiomas has climbed steadily in recent decades in concert with rising rates of prematurity and low birth weight, Dr. Sheila Fallon Friedlander said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“We spend a lot of time talking about port wine stains, but guess what? They’re much less frequent than are infantile hemangiomas, which most studies agree have an incidence of about 5%, as compared to 0.1%-0.3% for port wine stains,” observed Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego.
Most of these lesions resolve over time, but some are disfiguring or even life threatening. With the availability of safe and effective therapies in the form of propranolol, nadolol, timolol, and lasers, it’s incumbent on physicians to make the diagnosis early and intervene in a timely manner when appropriate to avoid complications, the pediatric dermatologist emphasized.
She highlighted a recent population-based study of infants born in Olmsted County, Minn., during 1976-2010. The Mayo Clinic investigators found that the incidence of infantile hemangiomas climbed from 0.97 to 1.97 per 100 person-years over that time span. Meanwhile, the average gestational age at birth among babies with infantile hemangiomas in the county fell from 39.2 weeks to 38.3 weeks, and their average birth weight dropped from 3,383 g to 3,185 g (J Am Acad Dermatol. 2016;74[1]:120-6).
Dr. Friedlander was senior investigator for a unique study, the first prospective U.S. study to track the incidence of infantile hemangiomas from birth through 9 months of age. The study included 578 mothers enrolled in pregnancy and their 594 offspring. All of the neonates were examined by a pediatric dermatologist within 48 hours after delivery, allowing for precise differentiation between infantile hemangiomas and other neonatal vascular lesions.
The incidence of infantile hemangiomas was 4.5%. The majority of the lesions occurred on the trunk or extremities. Of note, only one infantile hemangioma required intervention. Twenty percent of the infantile hemangiomas were small focal lesions with abortive or telangiectatic morphology that stopped growing by 3 months of age.
As in the Mayo Clinic study, Dr. Friedlander noted, the risk of infantile hemangioma in this San Diego–area study population increased with decreasing gestational age and weight. The incidence was 3.9% in term infants, 7.4% in premature infants, and 14.3% in those who were very premature. Similarly, infantile hemangiomas occurred in 4% of normal-birth-weight babies but in 16.6% of those who were very low birth weight (Br J Dermatol. 2014;170[4]:907-13).
Abnormalities of placental perfusion occurred in nearly 35% of pregnancies that produced babies with infantile hemangiomas, a rate twice that seen in pregnancies not associated with a subsequent infantile hemangioma. This and other evidence points to hypoxia as a key factor in precipitating the development of infantile hemangiomas.
“We believe that these lesions are related to embolization of tissue, perhaps placental, or hypoxia in utero,” Dr. Friedlander said. “Extreme prematurity, low birth weight, Caucasian race, placental anomalies, increased maternal age, use of fertility drugs – these are all things that will up your ante for having a child with an infantile hemangioma.”
She reported receiving grant/research support from Merz and Valeant Pharmaceuticals, and serving as a consultant for Sandoz.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – The incidence of infantile hemangiomas has climbed steadily in recent decades in concert with rising rates of prematurity and low birth weight, Dr. Sheila Fallon Friedlander said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“We spend a lot of time talking about port wine stains, but guess what? They’re much less frequent than are infantile hemangiomas, which most studies agree have an incidence of about 5%, as compared to 0.1%-0.3% for port wine stains,” observed Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego.
Most of these lesions resolve over time, but some are disfiguring or even life threatening. With the availability of safe and effective therapies in the form of propranolol, nadolol, timolol, and lasers, it’s incumbent on physicians to make the diagnosis early and intervene in a timely manner when appropriate to avoid complications, the pediatric dermatologist emphasized.
She highlighted a recent population-based study of infants born in Olmsted County, Minn., during 1976-2010. The Mayo Clinic investigators found that the incidence of infantile hemangiomas climbed from 0.97 to 1.97 per 100 person-years over that time span. Meanwhile, the average gestational age at birth among babies with infantile hemangiomas in the county fell from 39.2 weeks to 38.3 weeks, and their average birth weight dropped from 3,383 g to 3,185 g (J Am Acad Dermatol. 2016;74[1]:120-6).
Dr. Friedlander was senior investigator for a unique study, the first prospective U.S. study to track the incidence of infantile hemangiomas from birth through 9 months of age. The study included 578 mothers enrolled in pregnancy and their 594 offspring. All of the neonates were examined by a pediatric dermatologist within 48 hours after delivery, allowing for precise differentiation between infantile hemangiomas and other neonatal vascular lesions.
The incidence of infantile hemangiomas was 4.5%. The majority of the lesions occurred on the trunk or extremities. Of note, only one infantile hemangioma required intervention. Twenty percent of the infantile hemangiomas were small focal lesions with abortive or telangiectatic morphology that stopped growing by 3 months of age.
As in the Mayo Clinic study, Dr. Friedlander noted, the risk of infantile hemangioma in this San Diego–area study population increased with decreasing gestational age and weight. The incidence was 3.9% in term infants, 7.4% in premature infants, and 14.3% in those who were very premature. Similarly, infantile hemangiomas occurred in 4% of normal-birth-weight babies but in 16.6% of those who were very low birth weight (Br J Dermatol. 2014;170[4]:907-13).
Abnormalities of placental perfusion occurred in nearly 35% of pregnancies that produced babies with infantile hemangiomas, a rate twice that seen in pregnancies not associated with a subsequent infantile hemangioma. This and other evidence points to hypoxia as a key factor in precipitating the development of infantile hemangiomas.
“We believe that these lesions are related to embolization of tissue, perhaps placental, or hypoxia in utero,” Dr. Friedlander said. “Extreme prematurity, low birth weight, Caucasian race, placental anomalies, increased maternal age, use of fertility drugs – these are all things that will up your ante for having a child with an infantile hemangioma.”
She reported receiving grant/research support from Merz and Valeant Pharmaceuticals, and serving as a consultant for Sandoz.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR