User login
CDC issues guidance on worker precautions against Zika virus
As the Zika virus continues to spread, officials at the Occupational Safety and Health Administration (OSHA) and the Centers for Disease Control and Prevention have created a list of precautions to help outdoor workers, healthcare and laboratory personnel, and mosquito control workers avoid infection.
For outdoor workers, the prevention strategies center around using insect repellents, wearing clothing that provides a barrier against mosquitoes, and removing sources of standing water. For people working in healthcare settings and laboratories, OSHA and the CDC urge following good infection control and biosafety practices, including universal precautions to minimize the transmission of Zika virus, and when appropriate to wear gloves, gowns, masks, and eye protection.
Outdoor workers could be at the highest risk of catching the Zika virus, according to the guidance document.
Taking precautions to avoid mosquito bites is especially important when traveling to a Zika-affected area. OSHA and CDC also advised that workers should consider delaying travel if they may become pregnant, or have sexual partners who may become pregnant. The CDC recommends that pregnant women in any trimester avoid travel to an area with active Zika virus transmission.
“Even if they do not feel sick, travelers returning to the United States from an area with Zika should take steps to prevent mosquito bites for three weeks so they do not pass Zika to mosquitoes that could spread the virus to other people,” according to the guidance.
To find more information, click here.
As the Zika virus continues to spread, officials at the Occupational Safety and Health Administration (OSHA) and the Centers for Disease Control and Prevention have created a list of precautions to help outdoor workers, healthcare and laboratory personnel, and mosquito control workers avoid infection.
For outdoor workers, the prevention strategies center around using insect repellents, wearing clothing that provides a barrier against mosquitoes, and removing sources of standing water. For people working in healthcare settings and laboratories, OSHA and the CDC urge following good infection control and biosafety practices, including universal precautions to minimize the transmission of Zika virus, and when appropriate to wear gloves, gowns, masks, and eye protection.
Outdoor workers could be at the highest risk of catching the Zika virus, according to the guidance document.
Taking precautions to avoid mosquito bites is especially important when traveling to a Zika-affected area. OSHA and CDC also advised that workers should consider delaying travel if they may become pregnant, or have sexual partners who may become pregnant. The CDC recommends that pregnant women in any trimester avoid travel to an area with active Zika virus transmission.
“Even if they do not feel sick, travelers returning to the United States from an area with Zika should take steps to prevent mosquito bites for three weeks so they do not pass Zika to mosquitoes that could spread the virus to other people,” according to the guidance.
To find more information, click here.
As the Zika virus continues to spread, officials at the Occupational Safety and Health Administration (OSHA) and the Centers for Disease Control and Prevention have created a list of precautions to help outdoor workers, healthcare and laboratory personnel, and mosquito control workers avoid infection.
For outdoor workers, the prevention strategies center around using insect repellents, wearing clothing that provides a barrier against mosquitoes, and removing sources of standing water. For people working in healthcare settings and laboratories, OSHA and the CDC urge following good infection control and biosafety practices, including universal precautions to minimize the transmission of Zika virus, and when appropriate to wear gloves, gowns, masks, and eye protection.
Outdoor workers could be at the highest risk of catching the Zika virus, according to the guidance document.
Taking precautions to avoid mosquito bites is especially important when traveling to a Zika-affected area. OSHA and CDC also advised that workers should consider delaying travel if they may become pregnant, or have sexual partners who may become pregnant. The CDC recommends that pregnant women in any trimester avoid travel to an area with active Zika virus transmission.
“Even if they do not feel sick, travelers returning to the United States from an area with Zika should take steps to prevent mosquito bites for three weeks so they do not pass Zika to mosquitoes that could spread the virus to other people,” according to the guidance.
To find more information, click here.
Thousands of DNA modifications seen in infants of smoking mothers
The findings of a new, international study of 6,685 mothers and their newborns may explain why certain infant and child health problems frequently have been seen in the offspring of mothers who smoked during pregnancy, Kendall Morgan, Ph.D., wrote in the National Institutes of Health Director’s Blog.
The study, published in the American Journal of Human Genetics, “found significant differences between the epigenetic patterns of babies born to women who smoked during pregnancy and those born to nonsmokers, with many of the differences affecting genes known to play key roles in the development of the lungs, face, and nervous system,” Dr. Morgan wrote in the April 12 blog entry.
Smaller studies show there is evidence that maternal smoking can have epigenetic effects on a fetus. The new research from 13 research cohorts reaffirms and renders this finding more statistically powerful, Dr. Morgan wrote. In the infants of women who smoked every day during pregnancy, the researchers found more than 6,000 places where chemical marks on the DNA differed from those of babies born to mothers who did not smoke during pregnancy. The researchers also observed more than 4,600 epigenetic modifications in the DNA of babies of mothers who self-identified as falling under the broad category of having engaged in “any smoking during pregnancy.”
The genes thought to cause a cleft lip and/or palate were among the others to have been epigenetically modified in the fetuses of women who smoked while pregnant. The study also suggested that thousands of the epigenetic modifications seen affected children until at least age 4 years.
Read the study in the American Journal of Human Genetics (doi: 10.1016/j.ajhg.2016.02.019).
The findings of a new, international study of 6,685 mothers and their newborns may explain why certain infant and child health problems frequently have been seen in the offspring of mothers who smoked during pregnancy, Kendall Morgan, Ph.D., wrote in the National Institutes of Health Director’s Blog.
The study, published in the American Journal of Human Genetics, “found significant differences between the epigenetic patterns of babies born to women who smoked during pregnancy and those born to nonsmokers, with many of the differences affecting genes known to play key roles in the development of the lungs, face, and nervous system,” Dr. Morgan wrote in the April 12 blog entry.
Smaller studies show there is evidence that maternal smoking can have epigenetic effects on a fetus. The new research from 13 research cohorts reaffirms and renders this finding more statistically powerful, Dr. Morgan wrote. In the infants of women who smoked every day during pregnancy, the researchers found more than 6,000 places where chemical marks on the DNA differed from those of babies born to mothers who did not smoke during pregnancy. The researchers also observed more than 4,600 epigenetic modifications in the DNA of babies of mothers who self-identified as falling under the broad category of having engaged in “any smoking during pregnancy.”
The genes thought to cause a cleft lip and/or palate were among the others to have been epigenetically modified in the fetuses of women who smoked while pregnant. The study also suggested that thousands of the epigenetic modifications seen affected children until at least age 4 years.
Read the study in the American Journal of Human Genetics (doi: 10.1016/j.ajhg.2016.02.019).
The findings of a new, international study of 6,685 mothers and their newborns may explain why certain infant and child health problems frequently have been seen in the offspring of mothers who smoked during pregnancy, Kendall Morgan, Ph.D., wrote in the National Institutes of Health Director’s Blog.
The study, published in the American Journal of Human Genetics, “found significant differences between the epigenetic patterns of babies born to women who smoked during pregnancy and those born to nonsmokers, with many of the differences affecting genes known to play key roles in the development of the lungs, face, and nervous system,” Dr. Morgan wrote in the April 12 blog entry.
Smaller studies show there is evidence that maternal smoking can have epigenetic effects on a fetus. The new research from 13 research cohorts reaffirms and renders this finding more statistically powerful, Dr. Morgan wrote. In the infants of women who smoked every day during pregnancy, the researchers found more than 6,000 places where chemical marks on the DNA differed from those of babies born to mothers who did not smoke during pregnancy. The researchers also observed more than 4,600 epigenetic modifications in the DNA of babies of mothers who self-identified as falling under the broad category of having engaged in “any smoking during pregnancy.”
The genes thought to cause a cleft lip and/or palate were among the others to have been epigenetically modified in the fetuses of women who smoked while pregnant. The study also suggested that thousands of the epigenetic modifications seen affected children until at least age 4 years.
Read the study in the American Journal of Human Genetics (doi: 10.1016/j.ajhg.2016.02.019).
FROM THE AMERICAN JOURNAL OF HUMAN GENETICS
Women With Epilepsy Conceive at Normal Rate
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
AT THE AAN 2016 ANNUAL MEETING
Women with epilepsy conceive at normal rate
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: Women with epilepsy do not have lower ability to conceive.
Major finding: 70% of women with epilepsy and 67% of healthy control women became pregnant.
Data source: A prospective case-control study of 89 women with epilepsy and 109 healthy controls.
Disclosures: The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
Breastfeeding reduces infants’ respiratory symptoms early on
Breastfeeding during the first 27 weeks of life had a risk-specific effect on reducing respiratory symptoms in healthy term infants, based on data from a prospective cohort study of 436 children in Switzerland.
“Breastfeeding is generally accepted to be protective against respiratory symptoms in early life,” but most published studies on this topic are cross-sectional and more likely biased, wrote Dr. Olga Gorlanova of the University of Basel (Switzerland) and her colleagues.
The researchers studied infants enrolled in the Bern-Basel Infant Lung Development cohort via weekly telephone interviews during the first year of life. In addition, weekly measurements of environmental particulate matter were collected from local monitoring stations. Risk factors included maternal history of atopy, vaginal vs. cesarean delivery, parents’ level of education, smoking during and after pregnancy, number of older siblings, child care attendance, and housing conditions.
Overall, infants breastfed during the first 27 weeks of life had significantly reduced respiratory symptoms, compared with nonbreastfed infants (risk ratio, .70)
The study “suggests that breastfeeding attenuates the effects of risk factors such as sex, age, gestational age, cesarean delivery, and prenatal maternal tobacco smoking in healthy term infants,” Dr. Gorlanova and her associates wrote. No significant interaction was noted between breastfeeding and child care attendance, number of older siblings, maternal atopy, or environmental particulate matter.
Read the full study here (J Pediatr. 2016. doi: 10.1016/j.jpeds.2016.03.041).
Breastfeeding during the first 27 weeks of life had a risk-specific effect on reducing respiratory symptoms in healthy term infants, based on data from a prospective cohort study of 436 children in Switzerland.
“Breastfeeding is generally accepted to be protective against respiratory symptoms in early life,” but most published studies on this topic are cross-sectional and more likely biased, wrote Dr. Olga Gorlanova of the University of Basel (Switzerland) and her colleagues.
The researchers studied infants enrolled in the Bern-Basel Infant Lung Development cohort via weekly telephone interviews during the first year of life. In addition, weekly measurements of environmental particulate matter were collected from local monitoring stations. Risk factors included maternal history of atopy, vaginal vs. cesarean delivery, parents’ level of education, smoking during and after pregnancy, number of older siblings, child care attendance, and housing conditions.
Overall, infants breastfed during the first 27 weeks of life had significantly reduced respiratory symptoms, compared with nonbreastfed infants (risk ratio, .70)
The study “suggests that breastfeeding attenuates the effects of risk factors such as sex, age, gestational age, cesarean delivery, and prenatal maternal tobacco smoking in healthy term infants,” Dr. Gorlanova and her associates wrote. No significant interaction was noted between breastfeeding and child care attendance, number of older siblings, maternal atopy, or environmental particulate matter.
Read the full study here (J Pediatr. 2016. doi: 10.1016/j.jpeds.2016.03.041).
Breastfeeding during the first 27 weeks of life had a risk-specific effect on reducing respiratory symptoms in healthy term infants, based on data from a prospective cohort study of 436 children in Switzerland.
“Breastfeeding is generally accepted to be protective against respiratory symptoms in early life,” but most published studies on this topic are cross-sectional and more likely biased, wrote Dr. Olga Gorlanova of the University of Basel (Switzerland) and her colleagues.
The researchers studied infants enrolled in the Bern-Basel Infant Lung Development cohort via weekly telephone interviews during the first year of life. In addition, weekly measurements of environmental particulate matter were collected from local monitoring stations. Risk factors included maternal history of atopy, vaginal vs. cesarean delivery, parents’ level of education, smoking during and after pregnancy, number of older siblings, child care attendance, and housing conditions.
Overall, infants breastfed during the first 27 weeks of life had significantly reduced respiratory symptoms, compared with nonbreastfed infants (risk ratio, .70)
The study “suggests that breastfeeding attenuates the effects of risk factors such as sex, age, gestational age, cesarean delivery, and prenatal maternal tobacco smoking in healthy term infants,” Dr. Gorlanova and her associates wrote. No significant interaction was noted between breastfeeding and child care attendance, number of older siblings, maternal atopy, or environmental particulate matter.
Read the full study here (J Pediatr. 2016. doi: 10.1016/j.jpeds.2016.03.041).
FROM THE JOURNAL OF PEDIATRICS
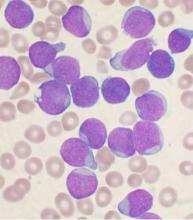
Prelabor cesarean delivery linked to increased risk of childhood ALL
An increased risk of acute lymphoblastic leukemia (ALL) was seen in young children born by prelabor cesarean delivery, in a pooled analysis of 13 case-control studies from nine countries.
The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018); there was not a significant association between ALL and all indications of cesarean delivery nor was there an association with emergency cesarean delivery. Further, the risk for childhood AML was not associated with cesarean delivery, prelabor cesarean delivery, or emergency cesarean delivery, reported Erin L. Marcotte, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
The association between ALL and prelabor cesarean delivery is based on 13 case-control studies from the Childhood Leukemia International Consortium. Birth delivery method was known for 97%-99% of 8,780 ALL cases, 1,332 AML cases, and 23,459 controls in those studies. In four of the studies, the indications for cesarean delivery were known for 1,061 of 4,313 ALL cases, 138 of 664 AML cases, and 1,401 of 5,884 controls. The multivariable logistic regression models used for the analysis were adjusted for birth weight, sex, age, ethnic origin, parental education, maternal age, and study.
If the association proves to be causal, “maladaptive immune activation due to an absence of stress response before birth in children born by prelabor caesarean delivery could be considered as a potential mechanism,” the researchers wrote (Lancet Haematol. 2016;3[4]:e176–e185).
ALL involves genetic and developmental aberrations that are probably modified by exposure and response to infectious agents. Early exposure to a variety of infections seems to decrease risk, and a vigorous response to infections (quantified by physician visits for infections) increases risk. During vaginal birth, the newborn is exposed to commensal bacteria that modulate immune development, Joseph Weimels, Ph.D., of the University of California at San Francisco, and Xiaomei Ma, Ph.D., of the Yale School of Public Health, New Haven, Conn., wrote in an editorial published in the same issue of The Lancet Haematology. Children delivered vaginally have different gut microbiomes and T-cell reactivity persisting up to age 2 years compared with children born by cesarean, they wrote.
The National Cancer Institute funded the study. The researchers had no relevant disclosures.
On Twitter @maryjodales
An increased risk of acute lymphoblastic leukemia (ALL) was seen in young children born by prelabor cesarean delivery, in a pooled analysis of 13 case-control studies from nine countries.
The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018); there was not a significant association between ALL and all indications of cesarean delivery nor was there an association with emergency cesarean delivery. Further, the risk for childhood AML was not associated with cesarean delivery, prelabor cesarean delivery, or emergency cesarean delivery, reported Erin L. Marcotte, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
The association between ALL and prelabor cesarean delivery is based on 13 case-control studies from the Childhood Leukemia International Consortium. Birth delivery method was known for 97%-99% of 8,780 ALL cases, 1,332 AML cases, and 23,459 controls in those studies. In four of the studies, the indications for cesarean delivery were known for 1,061 of 4,313 ALL cases, 138 of 664 AML cases, and 1,401 of 5,884 controls. The multivariable logistic regression models used for the analysis were adjusted for birth weight, sex, age, ethnic origin, parental education, maternal age, and study.
If the association proves to be causal, “maladaptive immune activation due to an absence of stress response before birth in children born by prelabor caesarean delivery could be considered as a potential mechanism,” the researchers wrote (Lancet Haematol. 2016;3[4]:e176–e185).
ALL involves genetic and developmental aberrations that are probably modified by exposure and response to infectious agents. Early exposure to a variety of infections seems to decrease risk, and a vigorous response to infections (quantified by physician visits for infections) increases risk. During vaginal birth, the newborn is exposed to commensal bacteria that modulate immune development, Joseph Weimels, Ph.D., of the University of California at San Francisco, and Xiaomei Ma, Ph.D., of the Yale School of Public Health, New Haven, Conn., wrote in an editorial published in the same issue of The Lancet Haematology. Children delivered vaginally have different gut microbiomes and T-cell reactivity persisting up to age 2 years compared with children born by cesarean, they wrote.
The National Cancer Institute funded the study. The researchers had no relevant disclosures.
On Twitter @maryjodales
An increased risk of acute lymphoblastic leukemia (ALL) was seen in young children born by prelabor cesarean delivery, in a pooled analysis of 13 case-control studies from nine countries.
The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018); there was not a significant association between ALL and all indications of cesarean delivery nor was there an association with emergency cesarean delivery. Further, the risk for childhood AML was not associated with cesarean delivery, prelabor cesarean delivery, or emergency cesarean delivery, reported Erin L. Marcotte, Ph.D., of the University of Minnesota, Minneapolis, and her associates.
The association between ALL and prelabor cesarean delivery is based on 13 case-control studies from the Childhood Leukemia International Consortium. Birth delivery method was known for 97%-99% of 8,780 ALL cases, 1,332 AML cases, and 23,459 controls in those studies. In four of the studies, the indications for cesarean delivery were known for 1,061 of 4,313 ALL cases, 138 of 664 AML cases, and 1,401 of 5,884 controls. The multivariable logistic regression models used for the analysis were adjusted for birth weight, sex, age, ethnic origin, parental education, maternal age, and study.
If the association proves to be causal, “maladaptive immune activation due to an absence of stress response before birth in children born by prelabor caesarean delivery could be considered as a potential mechanism,” the researchers wrote (Lancet Haematol. 2016;3[4]:e176–e185).
ALL involves genetic and developmental aberrations that are probably modified by exposure and response to infectious agents. Early exposure to a variety of infections seems to decrease risk, and a vigorous response to infections (quantified by physician visits for infections) increases risk. During vaginal birth, the newborn is exposed to commensal bacteria that modulate immune development, Joseph Weimels, Ph.D., of the University of California at San Francisco, and Xiaomei Ma, Ph.D., of the Yale School of Public Health, New Haven, Conn., wrote in an editorial published in the same issue of The Lancet Haematology. Children delivered vaginally have different gut microbiomes and T-cell reactivity persisting up to age 2 years compared with children born by cesarean, they wrote.
The National Cancer Institute funded the study. The researchers had no relevant disclosures.
On Twitter @maryjodales
THE LANCET HAEMATOLOGY
Key clinical point: Prelabor cesarean delivery was associated with an increased risk of childhood ALL, but not AML.
Major finding: The odds ratio was significant at 1.23 for an association between prelabor cesarean delivery and ALL (P = .018).
Data source: Thirteen case-control studies from the Childhood Leukemia International Consortium.
Disclosures: The National Cancer Institute funded the study. The researchers had no relevant disclosures.
Early predictors of GDM identified in women with PCOS
BOSTON – A prospective cohort study of women with polycystic ovarian syndrome who developed gestational diabetes mellitus during pregnancy has implicated fasting blood glucose, non–high density lipoprotein, and sex hormone–binding globulin as significant predictive factors for the development of GDM.
“Polycystic ovarian syndrome [PCOS] is the most common reproductive disorder in women of reproductive age and is commonly associated with metabolic disorders including diabetes and obesity. In women with GDM, a history of PCOS is associated with higher incidence of complications and postpregnancy glucose intolerance. Risk factors during early pregnancy in women with PCOS for development of GDM have not been well characterized,” said Dr. Wenyu Huang of Northwestern University, Chicago.
To provide some clarity, Dr. Huang and his colleagues conducted a prospective cohort study. Inclusion criteria were age 18-45 years, diagnosis of PCOS prior to conception, singlet pregnancy, and enrollment during the first trimester. Preexisting chronic disease including diabetes, hypertension, and thyroid, kidney, or cardiovascular disease was grounds for exclusion. The findings were presented at the annual meeting of the Endocrine Society.
The 248 women with PCOS enrolled from 2011 to 2013 from a screened population of 25,000 pregnant women were followed from their first prenatal visit (before week 18) to delivery. Blood was collected at the first visit for analysis of metabolic hormones. A 75-g oral glucose tolerance test (OGTT) was carried out at week 24-28 and diagnosis of GDM was according to 2013 American Diabetes Association OGTT criteria.
Of the 248 women, 75 (30.2%) developed GDM, and 173 (69.8%) women had normal OGTT results. Examination over the same time period early in pregnancy revealed a higher incidence of GDM in women with PCOS.
In a univariate analysis, PCOS patients who developed GDM had higher fasting blood glucose (FBG), Homeostasis Model Assessment-Insulin resistance (HOMA-IR) score, total cholesterol, low-density lipoprotein cholesterol, non-HDL cholesterol, systolic and diastolic blood pressures, and free testosterone index. These patients also had lower levels of sex hormone–binding globulin (SHBG) and higher likelihood of family history of diabetes and earlier delivery.
Multiple logistic regression revealed associations between increased incidence of GDM and FBG greater than or equal to 4.86 mmol/L, non-HDL cholesterol greater than or equal to 2.84 mmol/L, and SHBG greater than or equal to 222 nmol/L. The predictive power of the three factors for the development of GDM in PCOS was relatively strong.
Future studies could aim to validate the prediction model and clarify the pathogenic basis of GDM in PCOS women, according to the researchers .
The study was funded by the Beijing Science Committee. Dr. Huang had no disclosures.
BOSTON – A prospective cohort study of women with polycystic ovarian syndrome who developed gestational diabetes mellitus during pregnancy has implicated fasting blood glucose, non–high density lipoprotein, and sex hormone–binding globulin as significant predictive factors for the development of GDM.
“Polycystic ovarian syndrome [PCOS] is the most common reproductive disorder in women of reproductive age and is commonly associated with metabolic disorders including diabetes and obesity. In women with GDM, a history of PCOS is associated with higher incidence of complications and postpregnancy glucose intolerance. Risk factors during early pregnancy in women with PCOS for development of GDM have not been well characterized,” said Dr. Wenyu Huang of Northwestern University, Chicago.
To provide some clarity, Dr. Huang and his colleagues conducted a prospective cohort study. Inclusion criteria were age 18-45 years, diagnosis of PCOS prior to conception, singlet pregnancy, and enrollment during the first trimester. Preexisting chronic disease including diabetes, hypertension, and thyroid, kidney, or cardiovascular disease was grounds for exclusion. The findings were presented at the annual meeting of the Endocrine Society.
The 248 women with PCOS enrolled from 2011 to 2013 from a screened population of 25,000 pregnant women were followed from their first prenatal visit (before week 18) to delivery. Blood was collected at the first visit for analysis of metabolic hormones. A 75-g oral glucose tolerance test (OGTT) was carried out at week 24-28 and diagnosis of GDM was according to 2013 American Diabetes Association OGTT criteria.
Of the 248 women, 75 (30.2%) developed GDM, and 173 (69.8%) women had normal OGTT results. Examination over the same time period early in pregnancy revealed a higher incidence of GDM in women with PCOS.
In a univariate analysis, PCOS patients who developed GDM had higher fasting blood glucose (FBG), Homeostasis Model Assessment-Insulin resistance (HOMA-IR) score, total cholesterol, low-density lipoprotein cholesterol, non-HDL cholesterol, systolic and diastolic blood pressures, and free testosterone index. These patients also had lower levels of sex hormone–binding globulin (SHBG) and higher likelihood of family history of diabetes and earlier delivery.
Multiple logistic regression revealed associations between increased incidence of GDM and FBG greater than or equal to 4.86 mmol/L, non-HDL cholesterol greater than or equal to 2.84 mmol/L, and SHBG greater than or equal to 222 nmol/L. The predictive power of the three factors for the development of GDM in PCOS was relatively strong.
Future studies could aim to validate the prediction model and clarify the pathogenic basis of GDM in PCOS women, according to the researchers .
The study was funded by the Beijing Science Committee. Dr. Huang had no disclosures.
BOSTON – A prospective cohort study of women with polycystic ovarian syndrome who developed gestational diabetes mellitus during pregnancy has implicated fasting blood glucose, non–high density lipoprotein, and sex hormone–binding globulin as significant predictive factors for the development of GDM.
“Polycystic ovarian syndrome [PCOS] is the most common reproductive disorder in women of reproductive age and is commonly associated with metabolic disorders including diabetes and obesity. In women with GDM, a history of PCOS is associated with higher incidence of complications and postpregnancy glucose intolerance. Risk factors during early pregnancy in women with PCOS for development of GDM have not been well characterized,” said Dr. Wenyu Huang of Northwestern University, Chicago.
To provide some clarity, Dr. Huang and his colleagues conducted a prospective cohort study. Inclusion criteria were age 18-45 years, diagnosis of PCOS prior to conception, singlet pregnancy, and enrollment during the first trimester. Preexisting chronic disease including diabetes, hypertension, and thyroid, kidney, or cardiovascular disease was grounds for exclusion. The findings were presented at the annual meeting of the Endocrine Society.
The 248 women with PCOS enrolled from 2011 to 2013 from a screened population of 25,000 pregnant women were followed from their first prenatal visit (before week 18) to delivery. Blood was collected at the first visit for analysis of metabolic hormones. A 75-g oral glucose tolerance test (OGTT) was carried out at week 24-28 and diagnosis of GDM was according to 2013 American Diabetes Association OGTT criteria.
Of the 248 women, 75 (30.2%) developed GDM, and 173 (69.8%) women had normal OGTT results. Examination over the same time period early in pregnancy revealed a higher incidence of GDM in women with PCOS.
In a univariate analysis, PCOS patients who developed GDM had higher fasting blood glucose (FBG), Homeostasis Model Assessment-Insulin resistance (HOMA-IR) score, total cholesterol, low-density lipoprotein cholesterol, non-HDL cholesterol, systolic and diastolic blood pressures, and free testosterone index. These patients also had lower levels of sex hormone–binding globulin (SHBG) and higher likelihood of family history of diabetes and earlier delivery.
Multiple logistic regression revealed associations between increased incidence of GDM and FBG greater than or equal to 4.86 mmol/L, non-HDL cholesterol greater than or equal to 2.84 mmol/L, and SHBG greater than or equal to 222 nmol/L. The predictive power of the three factors for the development of GDM in PCOS was relatively strong.
Future studies could aim to validate the prediction model and clarify the pathogenic basis of GDM in PCOS women, according to the researchers .
The study was funded by the Beijing Science Committee. Dr. Huang had no disclosures.
Key clinical point: Several factors may be predictive of early development of gestational diabetes mellitus in pregnant women with polycystic ovarian syndrome.
Major finding: Multiple logistic regression revealed associations between increased incidence of gestational diabetes mellitus and fasting blood glucose greater than or equal to 4.86 mmol/L, non-HDL cholesterol greater than or equal to 2.84 mmol/L, and sex hormone–binding globulin greater than or equal to 222 nmol/L.
Data source: Prospective cohort study involving 248 women.
Disclosures: The study was funded by the Beijing Science Committee. Dr. Huang had no disclosures.
Intracranial calcification, hypomyelination seen with Zika virus congenital microcephaly
A CT imaging study in 23 infants with Zika virus–linked congenital microcephaly has revealed severe brain anomalies, in particular intracranial calcifications mainly in the frontal and parietal lobes that were mostly punctate, often with a bandlike distribution.
Head CT images were taken between 3 days and 5 months after birth (mean age, 36 days) revealing ventriculomegaly in all infants, which was severe in more than half, according to a letter published online April 6 in the New England Journal of Medicine.
Researchers also observed global hypogyration in the cerebral cortex in all the infants (severe in 78%) and cerebellar hypoplasia in 74%, as well as an abnormally low density of white matter in all cases (N Engl J Med. 2016 April 6. doi: 10.1056/NEJMc1603617).
“The global presence of cortical hypogyration and white-matter hypomyelination or dysmyelination in all the infants, and cerebellar hypoplasia in the majority of them, suggest that ZIKV [Zika virus] is associated with a disruption in brain development rather than a destruction of brain,” wrote Dr. Adriano N. Hazin of the Instituto di Medicina Integral Professor Fernando Figueira, Recife, Brazil, and coauthors who reported the findings for the Microcephaly Epidemic Research Group.
Two authors declared grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico. No other conflicts of interest were declared.
A CT imaging study in 23 infants with Zika virus–linked congenital microcephaly has revealed severe brain anomalies, in particular intracranial calcifications mainly in the frontal and parietal lobes that were mostly punctate, often with a bandlike distribution.
Head CT images were taken between 3 days and 5 months after birth (mean age, 36 days) revealing ventriculomegaly in all infants, which was severe in more than half, according to a letter published online April 6 in the New England Journal of Medicine.
Researchers also observed global hypogyration in the cerebral cortex in all the infants (severe in 78%) and cerebellar hypoplasia in 74%, as well as an abnormally low density of white matter in all cases (N Engl J Med. 2016 April 6. doi: 10.1056/NEJMc1603617).
“The global presence of cortical hypogyration and white-matter hypomyelination or dysmyelination in all the infants, and cerebellar hypoplasia in the majority of them, suggest that ZIKV [Zika virus] is associated with a disruption in brain development rather than a destruction of brain,” wrote Dr. Adriano N. Hazin of the Instituto di Medicina Integral Professor Fernando Figueira, Recife, Brazil, and coauthors who reported the findings for the Microcephaly Epidemic Research Group.
Two authors declared grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico. No other conflicts of interest were declared.
A CT imaging study in 23 infants with Zika virus–linked congenital microcephaly has revealed severe brain anomalies, in particular intracranial calcifications mainly in the frontal and parietal lobes that were mostly punctate, often with a bandlike distribution.
Head CT images were taken between 3 days and 5 months after birth (mean age, 36 days) revealing ventriculomegaly in all infants, which was severe in more than half, according to a letter published online April 6 in the New England Journal of Medicine.
Researchers also observed global hypogyration in the cerebral cortex in all the infants (severe in 78%) and cerebellar hypoplasia in 74%, as well as an abnormally low density of white matter in all cases (N Engl J Med. 2016 April 6. doi: 10.1056/NEJMc1603617).
“The global presence of cortical hypogyration and white-matter hypomyelination or dysmyelination in all the infants, and cerebellar hypoplasia in the majority of them, suggest that ZIKV [Zika virus] is associated with a disruption in brain development rather than a destruction of brain,” wrote Dr. Adriano N. Hazin of the Instituto di Medicina Integral Professor Fernando Figueira, Recife, Brazil, and coauthors who reported the findings for the Microcephaly Epidemic Research Group.
Two authors declared grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico. No other conflicts of interest were declared.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Zika virus–linked congenital microcephaly is characterized by severe brain anomalies including intracranial calcifications, ventriculomegaly, and hypomyelination.
Major finding: Hypomyelination and ventriculomegaly were present in all infants with Zika virus–associated congenital microcephaly.
Data source: A CT imaging study in 23 infants with Zika virus–associated congenital microcephaly.
Disclosures: Two authors declared grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico. No other conflicts of interest were declared.
Fetal malformation risk not increased after exposure to lamotrigine
A new analysis of registry data from European countries does not support a risk of orofacial cleft and clubfoot with exposure to lamotrigine monotherapy, in contrast to signals from previous studies of the antiepileptic drug.
First author Helen Dolk, Dr.P.H., professor of epidemiology and health services research and the head of the center for maternal, fetal, and infant research at the University of Ulster in Coleraine, Northern Ireland, and her colleagues analyzed data from 10.1 million births exposed to antiepileptic drugs including lamotrigine (Lamictal) as a monotherapy during the first trimester between 1995 and 2011. The births were recorded in 21 population-based registries from 16 European countries. The outcomes of interest were major congenital malformations in general, as well as orofacial clefts and clubfoot (Neurology. 2016 April 6. doi: 10.1212/WNL.0000000000002540).
Assessment of all antiepileptic drug-exposed congenital malformation registrations revealed that 12% of pregnant registrants were exposed to lamotrigine monotherapy, with an additional 7% exposed to lamotrigine as part of polytherapy. A total of 77.1% of pregnant women exposed to lamotrigine monotherapy had records indicative of a diagnosis of epilepsy. The proportion of lamotrigine monotherapy exposures was observed to have increased over the study period, likely based on a movement away from the traditional use of valproate because of teratogenic concerns.
A total of 147 lamotrigine monotherapy-exposed babies with congenital malformations not attributable to chromosomal irregularities were identified from the total sample. The odds ratio for having a child with orofacial clefts after exposure to lamotrigine monotherapy was 1.31 (95% confidence interval, 0.73-2.33). Based on these data, the authors said they estimated exposure to lamotrigine would result in orofacial clefts in fewer than 1 in every 550 exposed babies.
The odds ratio for having a child with clubfoot after exposure to lamotrigine monotherapy was 1.83 (95% CI, 1.01-3.31). Although the study results confirmed the statistically significant signal for an overall excess of clubfoot risk found in a previous study conducted by this research team that analyzed births during 1995-2005, the investigators could not reproduce this result in an independent study population of 6.3 million births during 2005-2011(odds ratio, 1.43; 95% CI, 0.66-3.08). There were no significant differences in the risk for developing any other congenital malformations associated with lamotrigine monotherapy, the investigators said.
The authors said their results were in accord with those from several previous studies that did not detect an increased risk of orofacial clefts. In addition, they said statistically significant independent evidence of a clubfoot excess was not detected in the current study, despite findings from their previous study suggesting an increased risk.
The EUROCAT Central Database was funded by the EU Public Health Programme. GlaxoSmithKline, which markets lamotrigine, provided a grant for additional funding of this study. Dr. Dolk and her coauthors reported that their institutions received funding from GlaxoSmithKline for data or staff time contributed to this study.
A new analysis of registry data from European countries does not support a risk of orofacial cleft and clubfoot with exposure to lamotrigine monotherapy, in contrast to signals from previous studies of the antiepileptic drug.
First author Helen Dolk, Dr.P.H., professor of epidemiology and health services research and the head of the center for maternal, fetal, and infant research at the University of Ulster in Coleraine, Northern Ireland, and her colleagues analyzed data from 10.1 million births exposed to antiepileptic drugs including lamotrigine (Lamictal) as a monotherapy during the first trimester between 1995 and 2011. The births were recorded in 21 population-based registries from 16 European countries. The outcomes of interest were major congenital malformations in general, as well as orofacial clefts and clubfoot (Neurology. 2016 April 6. doi: 10.1212/WNL.0000000000002540).
Assessment of all antiepileptic drug-exposed congenital malformation registrations revealed that 12% of pregnant registrants were exposed to lamotrigine monotherapy, with an additional 7% exposed to lamotrigine as part of polytherapy. A total of 77.1% of pregnant women exposed to lamotrigine monotherapy had records indicative of a diagnosis of epilepsy. The proportion of lamotrigine monotherapy exposures was observed to have increased over the study period, likely based on a movement away from the traditional use of valproate because of teratogenic concerns.
A total of 147 lamotrigine monotherapy-exposed babies with congenital malformations not attributable to chromosomal irregularities were identified from the total sample. The odds ratio for having a child with orofacial clefts after exposure to lamotrigine monotherapy was 1.31 (95% confidence interval, 0.73-2.33). Based on these data, the authors said they estimated exposure to lamotrigine would result in orofacial clefts in fewer than 1 in every 550 exposed babies.
The odds ratio for having a child with clubfoot after exposure to lamotrigine monotherapy was 1.83 (95% CI, 1.01-3.31). Although the study results confirmed the statistically significant signal for an overall excess of clubfoot risk found in a previous study conducted by this research team that analyzed births during 1995-2005, the investigators could not reproduce this result in an independent study population of 6.3 million births during 2005-2011(odds ratio, 1.43; 95% CI, 0.66-3.08). There were no significant differences in the risk for developing any other congenital malformations associated with lamotrigine monotherapy, the investigators said.
The authors said their results were in accord with those from several previous studies that did not detect an increased risk of orofacial clefts. In addition, they said statistically significant independent evidence of a clubfoot excess was not detected in the current study, despite findings from their previous study suggesting an increased risk.
The EUROCAT Central Database was funded by the EU Public Health Programme. GlaxoSmithKline, which markets lamotrigine, provided a grant for additional funding of this study. Dr. Dolk and her coauthors reported that their institutions received funding from GlaxoSmithKline for data or staff time contributed to this study.
A new analysis of registry data from European countries does not support a risk of orofacial cleft and clubfoot with exposure to lamotrigine monotherapy, in contrast to signals from previous studies of the antiepileptic drug.
First author Helen Dolk, Dr.P.H., professor of epidemiology and health services research and the head of the center for maternal, fetal, and infant research at the University of Ulster in Coleraine, Northern Ireland, and her colleagues analyzed data from 10.1 million births exposed to antiepileptic drugs including lamotrigine (Lamictal) as a monotherapy during the first trimester between 1995 and 2011. The births were recorded in 21 population-based registries from 16 European countries. The outcomes of interest were major congenital malformations in general, as well as orofacial clefts and clubfoot (Neurology. 2016 April 6. doi: 10.1212/WNL.0000000000002540).
Assessment of all antiepileptic drug-exposed congenital malformation registrations revealed that 12% of pregnant registrants were exposed to lamotrigine monotherapy, with an additional 7% exposed to lamotrigine as part of polytherapy. A total of 77.1% of pregnant women exposed to lamotrigine monotherapy had records indicative of a diagnosis of epilepsy. The proportion of lamotrigine monotherapy exposures was observed to have increased over the study period, likely based on a movement away from the traditional use of valproate because of teratogenic concerns.
A total of 147 lamotrigine monotherapy-exposed babies with congenital malformations not attributable to chromosomal irregularities were identified from the total sample. The odds ratio for having a child with orofacial clefts after exposure to lamotrigine monotherapy was 1.31 (95% confidence interval, 0.73-2.33). Based on these data, the authors said they estimated exposure to lamotrigine would result in orofacial clefts in fewer than 1 in every 550 exposed babies.
The odds ratio for having a child with clubfoot after exposure to lamotrigine monotherapy was 1.83 (95% CI, 1.01-3.31). Although the study results confirmed the statistically significant signal for an overall excess of clubfoot risk found in a previous study conducted by this research team that analyzed births during 1995-2005, the investigators could not reproduce this result in an independent study population of 6.3 million births during 2005-2011(odds ratio, 1.43; 95% CI, 0.66-3.08). There were no significant differences in the risk for developing any other congenital malformations associated with lamotrigine monotherapy, the investigators said.
The authors said their results were in accord with those from several previous studies that did not detect an increased risk of orofacial clefts. In addition, they said statistically significant independent evidence of a clubfoot excess was not detected in the current study, despite findings from their previous study suggesting an increased risk.
The EUROCAT Central Database was funded by the EU Public Health Programme. GlaxoSmithKline, which markets lamotrigine, provided a grant for additional funding of this study. Dr. Dolk and her coauthors reported that their institutions received funding from GlaxoSmithKline for data or staff time contributed to this study.
FROM NEUROLOGY
Key clinical point:Babies born to mothers exposed to lamotrigine monotherapy do not show evidence for an increased incidence of orofacial clefts or clubfoot.
Major finding: The odds ratios for having a child with orofacial clefts or clubfoot after exposure to lamotrigine monotherapy were 1.31 and 1.83, respectively.
Data source: A 16-year, observational study comparing the rate of lamotrigine exposure among births with orofacial clefts or clubfoot in 10.1 million births recorded in 21 population-based registries from 16 European countries.
Disclosures: The EUROCAT Central Database was funded by the EU Public Health Programme. GlaxoSmithKline, which markets lamotrigine, provided a grant for additional funding of this study. Dr. Dolk and her coauthors reported that their institutions received funding from GlaxoSmithKline for data or staff time contributed to this study.
HHS calls on Congress to approve supplemental Zika funding
The White House implored Congress on April 6 to act quickly on requests to allocate substantial funding for combating the Zika virus, as the Department of Health and Human Services revealed that it will be tapping into emergency funds allocated for last year’s Ebola outbreak to keep preventive efforts against the Zika virus alive.
“The American people shouldn’t have to be panicked for Congress to do their job,” Shaun Donovan, director of the Office of Management and Budget, said during a teleconference with reporters. “The administration, this president, we’re doing our job, [now] Congress needs to do their job and get the resources we need to take the steps [to] protect our citizens, communities, and families.
“We submitted to Congress a request for emergency supplemental funding in February to fortify our efforts to combat, and stay ahead of, this disease, but Congress has yet to act,” Mr. Donovan said, adding that in the nearly 2 months since that request was sent, “the situation continues to grow more critical.”
Sylvia Mathews Burwell, secretary of the Department of Health and Human Services, revealed that local transmission of the Zika virus in the continental United States is “likely” during the coming spring and summer months, and that efforts to increase the number of Zika virus tests being produced, as well establishing labs capable of running those tests, are continuing in order to meet the expected demand.
To facilitate that, Secretary Burwell and Mr. Donovan revealed that $589 million in existing funds have been identified as being immediately available to assist with the ongoing preventive efforts against the Zika virus. Of those funds, $510 million were designated to combat the Ebola virus outbreak of late 2014 and into last year.
“Yesterday, the State Department transmitted to Congress a determination under Section 7058C of the Fiscal Year 2015 Appropriations Act that the international outbreak of the Zika virus is sustained, severe, and spreading internationally, and that it is in the U.S. national interest to respond to this public health emergency,” explained Heather Higginbottom, deputy secretary for management and resources in the Department of State, regarding how funds were freed up from the Ebola crisis to combat the ongoing Zika virus outbreak.
While the reallocated funding will provide a measure of financial relief, all three speakers warned that the money was only a temporary fix, and that without proper Congressional support, ongoing Zika virus activities will have to be either “delayed, or curtailed, or stopped within months,” according to Mr. Donovan.
These efforts include the ongoing development of a Zika virus vaccine. Secretary Burwell gave an update on the search for a viable vaccine, stating that “five to six vaccine candidates” are set to begin phase I trials in September. Furthermore, prevention efforts in Puerto Rico have been ramped up with the creation of more field offices to combat the virus closer to the source.
“As of April 1, there were 672 confirmed cases of Zika in the continental U.S. and territories,” said Secretary Burwell. “That count includes 64 women who have [been] confirmed for Zika and are pregnant, which you all know is important because the WHO [World Health Organization] recently confirmed that there is strong scientific evidence that the virus itself is the cause of microcephaly, Guillain-Barre syndrome, and other neurological disorders.” She also mentioned that the HHS has confirmed one case of an infant born with microcephaly in Hawaii, to a mother who tested positive for the Zika virus during pregnancy.
The White House implored Congress on April 6 to act quickly on requests to allocate substantial funding for combating the Zika virus, as the Department of Health and Human Services revealed that it will be tapping into emergency funds allocated for last year’s Ebola outbreak to keep preventive efforts against the Zika virus alive.
“The American people shouldn’t have to be panicked for Congress to do their job,” Shaun Donovan, director of the Office of Management and Budget, said during a teleconference with reporters. “The administration, this president, we’re doing our job, [now] Congress needs to do their job and get the resources we need to take the steps [to] protect our citizens, communities, and families.
“We submitted to Congress a request for emergency supplemental funding in February to fortify our efforts to combat, and stay ahead of, this disease, but Congress has yet to act,” Mr. Donovan said, adding that in the nearly 2 months since that request was sent, “the situation continues to grow more critical.”
Sylvia Mathews Burwell, secretary of the Department of Health and Human Services, revealed that local transmission of the Zika virus in the continental United States is “likely” during the coming spring and summer months, and that efforts to increase the number of Zika virus tests being produced, as well establishing labs capable of running those tests, are continuing in order to meet the expected demand.
To facilitate that, Secretary Burwell and Mr. Donovan revealed that $589 million in existing funds have been identified as being immediately available to assist with the ongoing preventive efforts against the Zika virus. Of those funds, $510 million were designated to combat the Ebola virus outbreak of late 2014 and into last year.
“Yesterday, the State Department transmitted to Congress a determination under Section 7058C of the Fiscal Year 2015 Appropriations Act that the international outbreak of the Zika virus is sustained, severe, and spreading internationally, and that it is in the U.S. national interest to respond to this public health emergency,” explained Heather Higginbottom, deputy secretary for management and resources in the Department of State, regarding how funds were freed up from the Ebola crisis to combat the ongoing Zika virus outbreak.
While the reallocated funding will provide a measure of financial relief, all three speakers warned that the money was only a temporary fix, and that without proper Congressional support, ongoing Zika virus activities will have to be either “delayed, or curtailed, or stopped within months,” according to Mr. Donovan.
These efforts include the ongoing development of a Zika virus vaccine. Secretary Burwell gave an update on the search for a viable vaccine, stating that “five to six vaccine candidates” are set to begin phase I trials in September. Furthermore, prevention efforts in Puerto Rico have been ramped up with the creation of more field offices to combat the virus closer to the source.
“As of April 1, there were 672 confirmed cases of Zika in the continental U.S. and territories,” said Secretary Burwell. “That count includes 64 women who have [been] confirmed for Zika and are pregnant, which you all know is important because the WHO [World Health Organization] recently confirmed that there is strong scientific evidence that the virus itself is the cause of microcephaly, Guillain-Barre syndrome, and other neurological disorders.” She also mentioned that the HHS has confirmed one case of an infant born with microcephaly in Hawaii, to a mother who tested positive for the Zika virus during pregnancy.
The White House implored Congress on April 6 to act quickly on requests to allocate substantial funding for combating the Zika virus, as the Department of Health and Human Services revealed that it will be tapping into emergency funds allocated for last year’s Ebola outbreak to keep preventive efforts against the Zika virus alive.
“The American people shouldn’t have to be panicked for Congress to do their job,” Shaun Donovan, director of the Office of Management and Budget, said during a teleconference with reporters. “The administration, this president, we’re doing our job, [now] Congress needs to do their job and get the resources we need to take the steps [to] protect our citizens, communities, and families.
“We submitted to Congress a request for emergency supplemental funding in February to fortify our efforts to combat, and stay ahead of, this disease, but Congress has yet to act,” Mr. Donovan said, adding that in the nearly 2 months since that request was sent, “the situation continues to grow more critical.”
Sylvia Mathews Burwell, secretary of the Department of Health and Human Services, revealed that local transmission of the Zika virus in the continental United States is “likely” during the coming spring and summer months, and that efforts to increase the number of Zika virus tests being produced, as well establishing labs capable of running those tests, are continuing in order to meet the expected demand.
To facilitate that, Secretary Burwell and Mr. Donovan revealed that $589 million in existing funds have been identified as being immediately available to assist with the ongoing preventive efforts against the Zika virus. Of those funds, $510 million were designated to combat the Ebola virus outbreak of late 2014 and into last year.
“Yesterday, the State Department transmitted to Congress a determination under Section 7058C of the Fiscal Year 2015 Appropriations Act that the international outbreak of the Zika virus is sustained, severe, and spreading internationally, and that it is in the U.S. national interest to respond to this public health emergency,” explained Heather Higginbottom, deputy secretary for management and resources in the Department of State, regarding how funds were freed up from the Ebola crisis to combat the ongoing Zika virus outbreak.
While the reallocated funding will provide a measure of financial relief, all three speakers warned that the money was only a temporary fix, and that without proper Congressional support, ongoing Zika virus activities will have to be either “delayed, or curtailed, or stopped within months,” according to Mr. Donovan.
These efforts include the ongoing development of a Zika virus vaccine. Secretary Burwell gave an update on the search for a viable vaccine, stating that “five to six vaccine candidates” are set to begin phase I trials in September. Furthermore, prevention efforts in Puerto Rico have been ramped up with the creation of more field offices to combat the virus closer to the source.
“As of April 1, there were 672 confirmed cases of Zika in the continental U.S. and territories,” said Secretary Burwell. “That count includes 64 women who have [been] confirmed for Zika and are pregnant, which you all know is important because the WHO [World Health Organization] recently confirmed that there is strong scientific evidence that the virus itself is the cause of microcephaly, Guillain-Barre syndrome, and other neurological disorders.” She also mentioned that the HHS has confirmed one case of an infant born with microcephaly in Hawaii, to a mother who tested positive for the Zika virus during pregnancy.